

The
2023–24



2023–24
Welcome to the 2023–24 annual report of the Mount Sinai Health System Department of Medicine. Inside you willfind a collection of articles that reflect some of the research, clinical,and academic excellence of our programs across the Department’s 14 divisions and seven hospitalsites over the past year. Additionally, there are stories that highlight our current initiatives in areas including education, faculty affairs, quality improvement, "diversity, equity, and inclusion", and more.
TheDepartmentofMedicineat MountSinaiHealth Systemisoneof thelargestandmostprestigious academictraininggrounds intheUnitedStates.We continuetocreateadynamicdepartmentthat upholdsgroundbreakingtranslationalresearchand exceptionalclinicaloutcomes.
The Health System’s largest department, the Department of Medicine comprises more than 1,800 full-timefaculty members and voluntary physicians, allof whom are affiliated with at least one of our hospitals. With robust grant funding of more than $147million from the National Institutes of Health, the Department of Medicine is ranked among the top 15medical school departments of its kind inthe United States, according to the Blue Ridge Institute for Medical Research.
Mount Sinai’s Department of Medicine attracts some of the world’s most talented medical students and trainees who seek to be taught by leading experts, many of whom have pioneered landmark therapies and treatments that are routinely used by their peers around the globe. Throughout its rich history of serving New Yorkers from all socioeconomic and ethnic backgrounds for more than 170 years, Mount Sinai’s Department of Medicine is committed to scientific research and clinical breakthroughs so that each and every one of our patients has the best possible outcomes, while teaching and exposing our students, residents, and fellows to the most advanced medical techniques, state-ofthe-art technology, and vigorous academic and training curricula.
Diversity, equity, and inclusion (DEI) are at the forefront of our work in the Department of
Medicine. We take pride in our ability and commitment to identify and recruit faculty and trainees who are from groups often underrepresented in medicine so we can remain strategically innovative in medicine while improving the care we provide to the communities we serve.
Whether you are a current or prospective patient, physician, researcher, resident, fellow, graduate student, or supporter, this report will allow you to discover and gain ataste of some of the most prominent clinical and research advances in the Department of Medicine.
Happy reading!



MonicaKraft,MD
Murray M. Rosenberg Professor of Medicine
Clickheretosupportthe MountSinaiDepartment ofMedicine'sclinical, education,andresearch goals.

For morethan a century, Mount Sinai has been the home of a premier Division of Cardiology
The Mount Sinai Hospital is ranked No. 4 in the nation for Cardiology, Heart and Vascular Surgery by U.S. News & World Report® for 202324, and Mount Sinai Fuster Heart Hospital is celebrated internationally as a world leader in all facets of cardiology.
TheDivisionof Cardiology’smissionistoimprove thehearthealthofpatientslocallyandglobally with dedicationtotheprevention,management, and eradicationofcardiovasculardiseases.Itcontinues topursueexcellenceinpatientcare,offering innovativepreventionandtreatments, pioneering researchandclinicaltrials,andtrainingfuture leadingcardiologistsbyitsworld-renownedexperts.

Deepak L. Bhatt, MD, MPH
Dr.ValentinFuster Professorof CardiovascularMedicine andDirector,MountSinai FusterHeartHospital

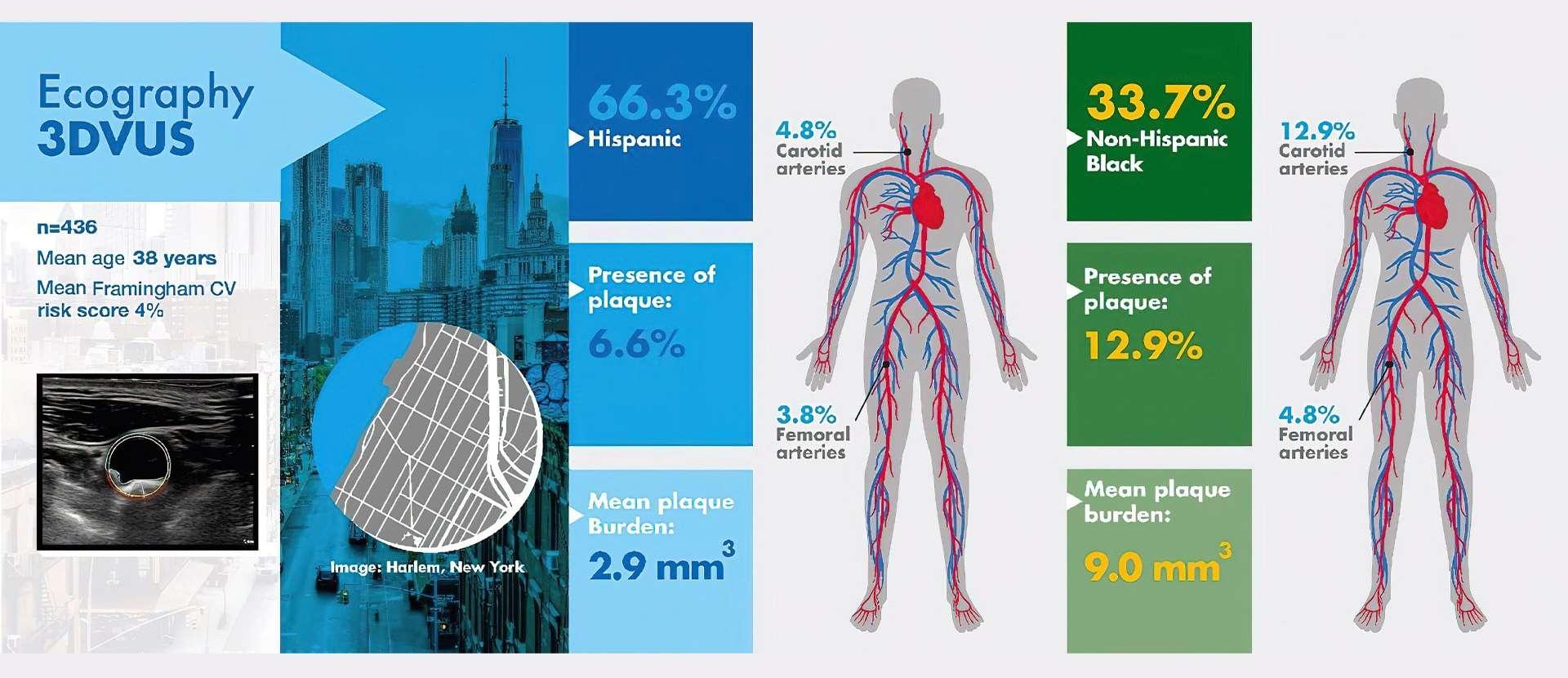
A unique MountSinai study focused on a multiethnic, underserved community in Harlem found that young non-Hispanic Black adult participants weretwice as likely to have atherosclerosisas young Hispanic adults.
The research, published in the Journal of the American College of Cardiology in July 2022, is part of the FAMILIAProject at Mount Sinai Heart, a pioneering trial created by Valentin Fuster, MD, PhD, President of Mount Sinai Heart and Physician-in-Chief of The Mount Sinai Hospital.
The new study is one of the first to evaluate atherosclerosis—theplaque build-up inthe arteries that can lead to a heart attack or stroke— in asymptomatic young populations. Its findings emphasizethe importance of early screening and lifestyle interventions inhigh-risk minority groups to improve their cardiovascular (CV) health.
“What’s interesting about this study isthatBlack individuals appear to be more vulnerableto atherosclerosis early in life than people of Hispanic origin, even when adjusting for known cardiovascular and lifestyle risk factors suchas smoking, unhealthy diet,lack of exercise, high blood pressure, and cholesterol,” Dr. Fuster says. “This can then put them at increased risk of cardiovascular disease, suggesting the existence of emerging or undiscovered cardiovascular risk factors inthis population.”
The study is part of a multinational effortto intervene early in the lives of children, their caretakers, and teachers so they can form a lifetime of heart-healthy habits. These new results come after highly successful interventions involving morethan 500 preschoolers, caretakers, and educators at 15 Head Start schools inthe Harlem section of Manhattan, an urban area that is socioeconomically disadvantaged—a situation commonly linked tohigher rates of obesity, heart disease, and other healthissues.
The FAMILIA team focused on 436 adults, including preschoolers’family members, caretakers, teachers, and school staff. Ofthat group, 147 participantswere non-Hispanic Black and 289 wereHispanic, with an average age of 38; 80percent were women. Non-Hispanic white, Asian, and Native American groups eachformeda small proportion of participants (2.3 percent, 2.3 percent, and 0.3 percent, respectively)and people in those groups were excluded from the analysis.
Each participant answered a comprehensive questionnaire at the start of thestudy, addressing their nutrition, physical activity, tobacco use, and
alcohol consumption, and whetherthey had conditions suchas heartdisease, hypertension, diabetes, or afamily history of health problems. They also had their weight recorded, and blood pressure and cholesterol checked.
Overall cardiovascular risk factors were prevalent for both ethnic groups atbaseline. Thirty percent of non-Hispanic Black participants had hypertension, almost triple the rate of the Hispanic group, 11 percent. Conversely, non-Hispanic Black participants had lower rates of dyslipidemia—unhealthy levels of lipids/fat inthe blood (18 percent) compared tothe Hispanic group at 27 percent, and bettereating habits, consuming more fruits and vegetables. Researchers used thesedata to calculatea predicted cardiovascularrisk score for eachgroup. They found the overallrisk of having a cardiovascular event in 10 years was lowfor both Black and Hispanic participants—around four percent for both groups.
Participants also had 3D vascular ultrasounds to determine if they had atherosclerosis in their carotid(neck) and femoral (leg) arteries. These vascular ultrasounds pointed to asignificant discrepancy between the groups. Overall, nine percent of participants had subclinical atherosclerosis (nearly one in ten participants showed at least one artery with plaque). Also, the rate of plaque build-up in the arteries wastwo times higher among non-Hispanic Black than Hispanic participants. The results were consistent even after adjustingfor classic cardiovascular risk factors including age, sex, bodymass index, hypertension, diabetes,and cholesterol; lifestyle factors including diet, physical activity, and tobacco use; and socioeconomic factors such as employment status.
The study noted some limitations and areas for further investigation. “The population included in the study was from aspecic area, Harlem, with known intrinsic health disparities compared with
other areas in New York City,” the study says. “This could, to some extent, limit our results’ generalizability.” In addition, “Given the heterogeneity among racialand ethnic groups, assessing associations between self-reported racial or ethnic identity and disease is complex and is vulnerabletoconfounding due to theeffects of socioeconomic inequality, environmental disparity, unequal access to care, and other possible emergingor unknown CV risk factors.”
However, the study is one of thefirst to assess the presence of subclinical atherosclerosis by 3D vascular ultrasounds in an underrepresented younger population, the research team says, and it contributes to the understanding of higher rates of CV diseaseobserved at an early age in disadvantaged communities.
“Thesefindings mayinpart helptoexplainthe observeddifferencesincardiovasculardisease prevalencebetweenracialandethnicgroups,” Dr. Fustersays. “Untilunderlyingbiologicalfactors and otherundiscoveredcardiovascular riskfactorsare better understoodandcanbeaddressedby precisionmedicine,affordablenoninvasiveimaging techniquessuchastheportable3Dvascular ultrasounds usedinthisstudy,whichareeasily usedandaffordable, canbeanimportantformof earlydetectioninunderservedcommunities, and providevaluableinformationaboutpopulation disparitiesandincreasetheprecisionof health promotionandprevention programs.”
Dr.Fusterandhisteamplantoexpandthe FAMILIAprogramtoschools acrossthefive boroughsofNewYorkCityinthenextfewyears. Thisproject willalsoevaluatehowfamily socioeconomicstatusandteachers’characteristics mayaffecttheimplementationandefficacy of school-basedhealthpromotionprograms.
The FAMILIA project was funded by a grant from the American Heart Association.
ValentinFuster, MD,PhD
President of Mount Sinai Fuster Heart Hospital, and Physician-in-Chief of The Mount Sinai Hospital

Mount Sinai Heart is launching a multispecialty Women's Heart and Vascular Center, with clinics specifically designed to screen, assess, and educate womenabout their level of individual risk through a team of cardiologists,subspecialists, and researchers with expertise in heart health issues specific to women.
The founding director of the Center is Roxana Mehran, MD, Professorof Medicine (Cardiology), and Population Health Science and Policy, and Director of Interventional Cardiovascular Research and Clinical Trials at the Icahn School of Medicine at Mount Sinai.
“Women need to bemore knowledgeable about their health, and our new Women's Heart and Vascular Center is designed togive them access to the very best specialists at Mount Sinai who can inform them of their risk for heart disease by
cardiomyopathy,andfibromusculardysplasia,which canleadtoheartattackandstrokeifuntreated. Instead,symptomssuchasanginaandchestpain triggeredbythesediseasesmaybediagnosedas anxietyorotherpsychosomaticdisorders.
“Women tend to bestereotyped into certain categories of health problems that miss the fact that what they really have is heart disease,” asserts Dr. Mehran, head of the Lancet Women and Cardiovascular Disease Commission, whose members from 11 countries have preparedthe


making sure they have a full understanding of numbers such as cholesterol, blood pressure, and hemoglobin A1C, which are critical to assessing their heart health,” saysDr. Mehran. “The truth is, cardiovascular disease is underrecognized, underdiagnosed, and undertreated inthis country, making it the No. 1 killer of women.”
Physiciansareoftennotfullytrainedtorecognize women-specificconditionssuchasspontaneous coronaryarterydissection(SCAD),coronary microvasculardysfunction,Takotsubo
first-ever global report and recommendations for decreasing the burden of cardiovascular disease in women. A lead author of the report was Birgit Vogel, MD, a clinical researcher in Cardiovascular Imaging andClinical Trials at Mount Sinai.
The clinics of the Heart and Vascular Center for Women arereaching out towomen at high risk due to pregnancy-related complications and to cancer treatment. According to Dr. Mehran, every woman who has experienced pregnancy-related issues such as premature delivery, gestational
diabetes, preeclampsia, or low birth weight of a child should have a cardiovascular risk assessment. Female cancer patients should also be evaluated, sheadds, as chemotherapeutic agents andradiation can adversely impact the heart and vascular tissue. Future clinics will be geared to detecting SCAD, ischemia, or myocardial infarction with nonobstructive coronary arteries, and peripheralarterial disease, which often affectwomen at a relatively young age.
The new Center is particularly committed to providing women from allsocioeconomic groups with access to top-tier cardiovascular care. Explains Dr. Mehran: “We know that women of color and minorities havethe highest risk of cardiovascular events, and one of our priorities is to bring them into our program so we can screen and educate them aboutpreventivemeasures they cantake to avoid aheart attack or stroke.” To that end, the Center hopes to eventually expand its clinics from their initial outpatient hospital setting to locations withinthe community.
Another goal of the Center is ensuring a greater presence for women in cardiovascular research. Not only are women greatly underrepresented nationally in terms of numbers intrials, but even when they are included in clinical studies, the data are often not disaggregated by sex, limiting the evidence-based information available to clinicians and patients. Inher leadrole with the global Lancet Commission, Dr. Mehran is focused on prioritizing sex-specific research onheartdisease in women, as wellas scaling up heart health programs in highly populated and underdeveloped regions of the world.
“Wewantwomentoknowthattheytrulymatter,” Dr.Mehransays,“andthatMountSinaiisconcerned enoughabouttheircardiovascularhealthtobring togetherunderoneroofanextraordinaryteamof specialistswhofullyunderstandandarereadyto providetheprimaryandsecondarypreventivecare theyneedanddeserve.”
Dr.Mehran,arenownedclinicianandresearcher, is alsodevotedtohelpingwomenadvanceinthefield of medicine. InNovember2022, theAmerican Heart Association’s CouncilonClinicalCardiology honoredherwiththe“WomeninCardiology MentoringAward,”recognizingheroutstanding recordofmentoringwomencardiologists.
“It is my life’s calling to help women, whether at the professional or patient level,” Dr. Mehran says. “Thereis always more to do in this regard, and I will continue to put my whole-hearted effort into this important cause, because there is muchto do, and we haveonly justbegun.”

RoxanaMehran, MD
Professor of Medicine (Cardiology), and Population Health Science and Policy

The Division of Clinical Immunology at Mount Sinai provides cutting-edge patient care, research, and educationin the fields of Allergy and Clinical Immunology. It leads the nation in the research of immune deficiency diseases and translating these findings to thedesign of pioneering treatments. Patients come to Mount Sinai’s Division of Clinical Immunology from across the country for the diagnosis and treatment of these immune disorders. The expert physicians in the Division provide comprehensiveoutpatient and inpatient consultations, and offer the latest advances in diagnostic procedures that may include examination of antibodies and cellfunctions and genetic analysis.
The Division launched theBiologics And Clinical Immunology Cohort at Sinai (BACICS) registry of patients with chronic immune-mediated diseases who are receiving biologics. The registry allows
state-of-the- art approaches to be applied to assess immunological and clinical responses that transcendprevious single-disease and static paradigms. BACICS is designed to determine shared signals in risk-associated regulatory pathways relevant to multiple immune disorders and the efficacy of their treatments across time. Unlike other registries which focus on one-organ diseases, this novel registry is most suited to help fill research gaps that are wider in scope and may generalize to molecularmechanisms of multiple chronic diseases.
The Division of Clinical Immunology is the largest provider of allergy care in New York City. In addition to providing comprehensive evaluations for allergic disorders,itsproviders are recognized nationally fortheir expertise inthe evaluation and treatment of asthma, atopic dermatitis, hereditary angioedema, and urticaria (hives).
The faculty is devoted tothe training of the next generation of leaders in Clinical Immunology, including physicians and scientists, through fellowship and mentoring programs.

Rachel Miller, MD
The Dr. David and Dorothy Merksamer Professor of Medicine (Allergy and Immunology)

Mount Sinai researchers have discovered that an inhibitor of Bruton’s tyrosine kinase (BTK), an important mediator of B-cell receptor signaling, could be used toshut off inflammation in cells of patients with primary immunodeficiency diseases in which B cells are either failingto make antibodies or making incorrect ones.
Mount Sinai researcherCharlotte CunninghamRundles, MD, PhD, andher team havediscovered that an inhibitor of Bruton’s tyrosine kinase(BTK), an important mediator of B-cellreceptor signaling, could be usedto shut off inflammation incells of patients with primary immunodeficiency diseases.
There are morethan 450 of thesediseases, and unraveling their puzzles involves confronting surprises and innovating responses. Part of the puzzle is the heterogeneity of immunodeficiency diseases: All components of the immune system can experience defects.
Among these defects are failures in lymphocytes called B cells, whichmature into plasma cells that last for years in bone marrow. B cells are responsible for making proteins called antibodies. The mostcommon immunodeficiency is whena patient’s B cells don’t make an antibody they need, which can lead to infections.
“The other side of the coin, however, is that the B cells may do something other than make a needed antibody—for example, make an
antibody against platelets, or red blood cells, or the GI tract, or maybe the skin,” Dr. CunninghamRundles explains. “So patients come through my door with autoimmunity almost as often as they do with infections.”
But Dr. Cunningham-Rundles, who is the Director of the Immunodeficiency Clinic, is undaunted by the complexity of the research. Rather, she finds it invigorating.
Genetics clearly influences the pathophysiology of immune deficiency diseases. Dr. CunninghamRundles, who is the David S. Gottesman Professor of Immunology at the Icahn School of Medicine at Mount Sinai and heads an eponymous research lab, authoreda 2020 report in Blood that identified anumber of genes affecting the process of generating antibodies.
“For the first 20to 30years that I worked on Bcell issues, peoplethought theremust be something

wrong with the B cell,” she says. “So, perhaps that antibody-making cellhas amalformation in the plasma cellor antibody recognition from a lymphocyte—but that turns out not to be true in most cases. It turns out there are a great number of additional genes thatare not unique to B cells that, when they don’t work, gives that personwhat looks like aB-cell problem.”
With colleagues inStockholm, Sweden, and Tehran, Iran, the researchers studiedthe genetics of more than 500 patients with common variable immunodeficiency (CVID),a primary immunodeficiency disease. The65 genes in the patients from the United States were predominantly autosomal dominant, whereas at the other twolocations the resultwas an approximately equal mix of dominant and recessive genes—further proof of the complexity of Bcell research.
Dr. Cunningham-Rundles is quick to point out that this finding is far from the final word. She found culprit genes in only about 30 percent of the patients tested, meaning another 70 percent or so are out therewaiting tobe discovered. “There are many moreto unpack,which is why wehave been doing a lot of whole exomesequencing, with colleagues at Rockefeller University, and wemay need to moveon to whole-genome sequencing.”
For Dr. Cunningham-Rundles, the endeavor to unravel themystery is both “confounding” and inspiring, and the ultimate beneficiaries of her work—her patients—are never far from hermind.
“I have patients who don’t make antibodies andI give them gamma globulin, sono problem. About 50 percent of those patients do fantastically. Some of them I’veseen for decades,” she says. “But the other 50 percent develop interstitial lung disease, liver fibrosis, rampant autoimmunedisease, granulomatous disease, and inflammatory diseases. Sothat’s the conundrum.”
Dr. Cunningham-Rundles and her team found thereare about 120 genetic indicatorsthatshow markers of inflammation. Using a novel assay developed in her lab, she found that thosepatients with an extreme inflammatory phenotype have larger amounts of bacterial DNA from gastrointestinal organisms in their blood. This DNA activated a numberof inflammatory pathways that could incite the conditions found in these patients. “Wewere pretty floored by this finding, but it is associated with alack of isotypeswitched B cells, whichmake immunoglobulin A [IgA]. What wefound suggests these patients have a mucosal-barrier defect.”
Unable toreplace the IgA, Dr. CunninghamRundles and team found that an inhibitor of BTK could shut down inflammation in cells of patients with immunodeficiency disorders. The primary immunodeficiency disease known as X-linked agammaglobulinemia is caused by mutations in the BTK gene, and patients with this disorder do not commonly have the inflammatory pathway disorders that are seen in CVID patients.
“It is counterintuitive to take someone who is immune deficient and say, OK, I will makeyou even more immune deficient. But wehave been using rituximab withsome CVID patients for years, and we’ve known that wiping out Bcells helps for some conditions in these patients. This is not permanent, since the cells thencome back in some months—it’s likemowing a lawn,”
Dr. Cunningham-Rundles explains. “But BTK is in a lot of cells that lead to inflammation in humans and a BTK inhibitorcould actually shut down the inflammation pathway.”
Dr. Cunningham-Rundles maintains an inventive approachto research and clinical care. For example, the mucosal-barrier defect mentioned above might be mitigated with the use of a small amino acid compound used in patients withceliac disease. She is looking into it. “Wearevery enthusiastic about what we do,” she explains. “One door opens up to another allthe time.”

Charlotte CunninghamRundles,MD,PhD
David S. Gottesman Professor of Immunology

Very few physicians specialize in treating hereditary angioedema (HAE), a rare and challenging genetic disease whose symptoms include swelling in the abdomen, extremities, face, and airway, the latter of which can be lifethreatening if not properly treated. Mount Sinai's Paula J. Busse, MD, not only treats these patients, but has helped develop the guidelines for managing this disease.
Paula J. Busse, MD, is a leader in the clinical care of patients with hereditary angioedema (HAE). And when it comesto fighting for her patients, Dr. Busse, Professor of Medicine (Clinical Immunology andAllergy) at the Icahn School of Medicine at Mount Sinai, is allin.
HAE is a rare and challenging genetic disease whose symptoms include swelling in the abdomen, extremities, face, and airway, the latter of which can be life-threatening if not properly treated. The number of those affected by the disorder is just a few thousand in the United States, and as a result there are very few physicians who specialize in treatingthe condition.
As explained in a 2020 review article in The New England Journal of Medicine co-authored by Dr. Busse, HAE causes vasodilation, which leads to fluid accumulation in tissues, producing angioedema. Angioedema of the gastrointestinal tract cancause severe abdominal pain and potential intestinal obstruction. Airway swelling can lead todeath by asphyxiation. Swelling in the
hands or feet can be painful and significantly limit activities of daily living.
HAE is an autosomal-dominant genetic disorder. In around 80percent of patients, aplasmaprotein known as C1-inhibitor (C1-INH) is both dysfunctional and present in deficient levels; this is known as HAE type 1. In those with HAE type2, C1-INH is dysfunctionalbut at appropriate levels. A very rare third type of HAE is found in those with normalC1-INH and functional levels, secondary to defects inother genes (some of which have been identified), causing HAE-like symptoms.
Allergicreactionscancauseangioedema, but those reactionsareinducedbyhistamine.InHAE,the angioedemaisinducedbybradykinin, apeptide that promotesvasculardilationwithsubsequent fluidextravasationtotissues.Bradykinin-mediated HAEisdistinct fromhistamine-mediated angioedemaanddoesnotrespondto antihistaminesor corticosteroids, whichareused forallergies. If not differentiatedbytheclinician,the result canbetreatmentthat isineffective—a perilousprospect if theairwayisinvolved.

There are twomajor sets of guidelines for the clinical care of the patient with HAE, and Dr. Busse has helped develop both. One stems from work by the United States Hereditary Angioedema Association, a U.S.-based patient organization on whose medicaladvisory board Dr. Busse sits. Working together,the advisory boardcreated guidelines for treatmentof HAE in 2013 that were updated in 2020. Dr.Busse, whowas the first author of this report, notes that the revised guidelines reflectadvancements in the understanding of HAE and significant changes in its clinical management.
Theothersetofguidelines,forwhichDr.Busse wasaco-author,is aninternationaleffortfromthe WorldAllergyOrganizationandEuropean Academyof AllergyandClinicalImmunology. Publishedin2022, theguidelines addressedslight differencesintreatmentphilosophies andaccessto therapiesbetweenU.S. andEuropeanclinicians. “At thispointtherearetwoguidelines, theU.S.and theinternational,” Dr.Busseexplains, “butthegap betweenthem ontreatmentrecommendationshas narrowedwiththelatestpublication.”
The costof HAE medications can beexpensive and prohibitive. One dose of a C-1inhibitor is severalthousand dollars. “Many emergency rooms arenot going to carry thesedrugs, although wehave it onformularyhere at Mount Sinai,” Dr. Busse notes.Because of the high cost,she often needs to fight forherpatients, spending hours on the phone debating themerits of health care coverage withreluctant insurers.
“I spend quite a bit of time working to get patients assistance, for example through the Hereditary Angioedema Association. There is an emotional hardship for some of these patients and their families because they can’t get medications or appropriate care,” she says. “Some of these patients don’t have the insurance to see a specialist like myself, so they go to other physicians, who perhaps have mismanaged them because they don’t have the expertise, and that can lead to morbidity and even mortality. That is pretty upsetting to me.”
Dr. Busse’s approach to the clinical careof patients with HAE is to be a leading expert on the diseaseandto keep fighting for them. “I have been able toget some companies to donate their medications and I spenda lot of time getting prior authorizations for thesepatients’medications,” Dr. Busse recalls.
Her weapon of choicefor these battles? The phone.

PaulaJ.Busse, MD
Professor of Medicine (ClinicalImmunology)

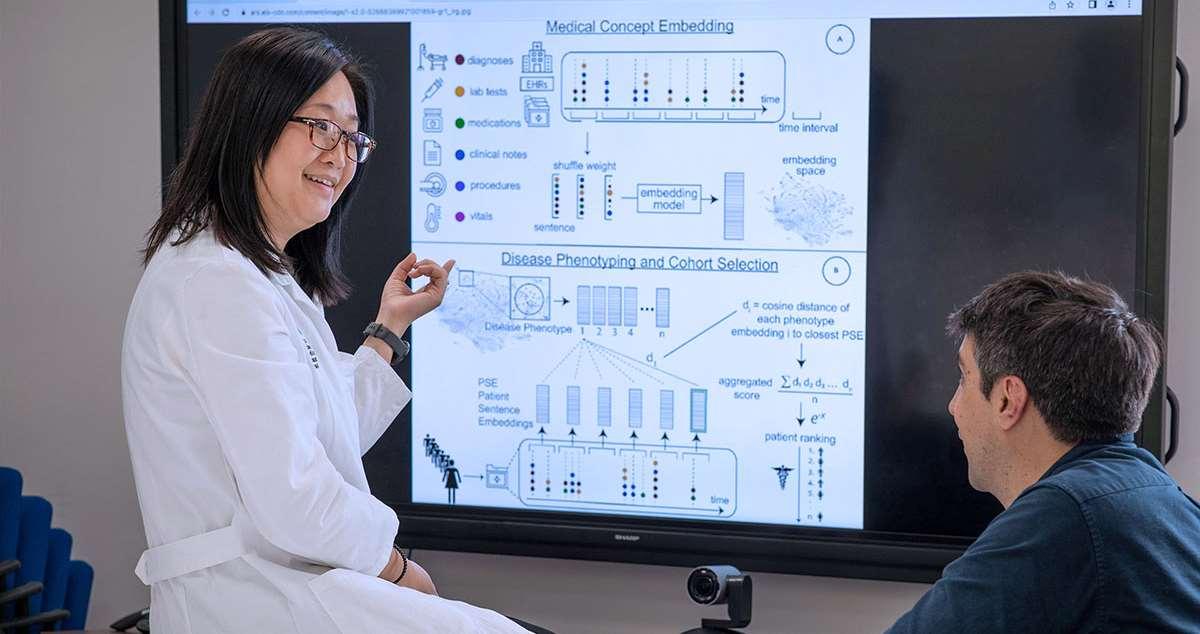
At a timewhen every medical decision, diagnosis, and treatment is underpinned by data, the Division of Data-Driven and Digital Medicine (D3M) is a leap towarda future where artificial intelligence (AI) and digital tools arenot simply integrated into, but become intrinsic to, clinical practice.
The Division is committed to bringing data-driven and digitalinnovation to research, education, and clinical care, thereby empowering each to reach its maximum potential.Modernmedicine’s transformativenew era is fueled by data science, AI, and digital health. The Division aims to be the epicenter of that transformation, catalyzing groundbreaking research, training the next generation of physicians, and ensuring a seamless translation of digital innovation into clinical practice.
Mount Sinai recognizes that through education, it can ensurethat its future biomedicalleaders are
pioneers in this newera of medicine, rather than justparticipants. The Division is committedto training medical students, residents, and fellows by introducing them to the possibilities of AI, data science, anddigital health innovation.

Girish N. Nadkarni, MD
Irene and Dr. Arthur M.Fishberg Professor of Medicine

As data science and artificial intelligence become more central to the practiceof medicine, Mount Sinai is buildingout its efforts to educate budding physicians and scientists in these areas. It has also begun using these tools to enhanceits own admissions process.
Datascienceandartificialintelligence(AI)arenot onlybeingmeticulouslywovenintopatient care across theMountSinaiHealthSystem,butalso
“Much of today’s research uses machine learning, naturallanguage processing, and other data science methods and tools, making it difficult for
beingdeployedininnovativewaystoadvanceboth theselectionandongoingeducationof medical schoolstudents.Onewayishelpingclinicalfellows masterthelanguageof dataanalysisandscience atthestartoftheircareers; anotherisstreamlining themedicalschoolapplicationsprocesstomakeit lesslabor-intensiveforscreeners andmore equitableforapplicants.
Therapidlygrowinguse ofdatasciencein everydayclinicalcarehasunderscoredtheneedfor physicianstobefluent intheoftenarcanemedium. Tothat end, LiliChan,MD, AssociateProfessorof Medicine(Nephrology,andDataDrivenandDigital Medicine)at theIcahnSchoolofMedicineat Mount Sinai, isdevelopingacomprehensiveDataAnalysis andDataSciencecourse.
students who have no training in these disciplines,” says Dr. Chan, an expert in clinical researchand data science. “We’re addressing this gap through acurriculum that’s focused on teaching trainees the digital skills necessary to conduct clinicalresearch, or to simply digest the results of studies they read in leading journalsthat employ real-world healthcaredata.”
Amongtopicstobecoveredinthelecturephase aredatabases,followed bythebuildingof datasets that willbedeployedthroughtheremainderofthe course. Machinelearning(ML)willalsobe introduced, withafocusondecisiontrees,which formthebasisformanyadvancedMLtechniques.
“Webelieve this curriculum has the potential to transform traineeeducation,” emphasizes Dr. Chan, “by providing protected timefor students to learn the data analytics and data science skills they’ll need to actively pursue research pathways.”
Noless enticing are theopportunities toleverage data science to benefit the thousands of applicants each year toMount Sinai’s highly competitive medical school program, as well as the faculty members who voluntarily takeon the task of deciding which ones get selected. Aware of the challenges, Valerie Parkas, MD, Senior Associate Dean of Admissions and Recruitment for Icahn Mount Sinai, and Talia Swartz, MD, PhD, Director of the MD-PhDprogram, began looking for ways that ML could help streamline the complex process.
“Every application gets read by screeners who must sort through personal statements, letters of recommendation, and related materials, which is extremely time-consuming,” explains Dr. Chan, who collaborated withDrs. Parkas and Swartz, and Justin Kauffman, a student in theMaster in Data Science program, to brainstorm howML might streamline the process. “Our goal isto reducethe number of human hours required to make sure each application is thoroughly reviewed, and tocontinue to ensure the process is as objective as possible.”
The team came to recognize the power and potential of a computational solution. In the same way a machine learning algorithm can betrained on reams of electronic health records to phenotype patients, so a machine learning program might be built around medical school applications to facilitatethe reviewof candidates. “We’re still in the early data-gathering stage,” explains Dr. Chan, “but are focused on developing an algorithm through natural language processing that could identify and highlight fromeach application consistent themes, suchas leadership or resourcefulness, which are so important within the applicant pool.”
She concludes,“We can’t remove thehuman element from the selection process. But we can seek to create through digital technology an equitable system for selecting students for our medical school program—one that also helps our screeners who, after all, are very busy physicians and researchers.”


LiliChan,MD
Associate Professor of Medicine (Nephrology)
ValerieParkas,MD
Professor of Medical Education
TaliaSwartz, MD,PhD
Associate Professor of Medicine (Infectious Diseases), and Medical Education
A study by Mount Sinai's Division of Data-Driven and Digital Medicine provides evidence for the first time that molecular signatures associated with“long COVID” are detectable in the acute stage of infection of SARS-CoV-2.
A Mount Sinai study provides evidence for the first time thatmolecular signatures associated with “long COVID” are detectable in the acute stage of infection of SARS-CoV-2. The finding underscores the enormous potential of computation and data science tostatistically model and ultimately resolve some of thebiggest clinical challenges of our time.
At the center of that effort is the Department of Medicine’s two-year-oldDivision of Data-Driven and Digital Medicine (D3M), which led the longCOVID investigation and views it as emblematic of the expanding effort at Mount Sinai to integrate data science and digital tools intotranslational research and clinicalcare.
“Datascience is enabling us to understand disease on a muchdeeper molecular scale than ever before, and it’s clear that knowledge will play a transformative role in how we conduct research and practice medicine,”says Girish Nadkarni, MD, Irene and Dr. Arthur M. Fishberg Professor of
Medicine at the Icahn School of Medicine at Mount Sinai and Chief of the new Division. “Our team is already making a difference by integrating its work into the clinical side of the Mount Sinai Health System and acting as apowerful data resourcefor health careprofessionals who often find access to that information challenging.”
Indeed, the data-driven computational study of post-acute sequelae of SARS-CoV-2 infection (commonly referred to as long COVID), published in Nature Medicine, was a collaborative effortwith The Charles BronfmanInstitute of Personalized Medicine at IcahnMount Sinai and the clinical data science team.
“Webelieve this study exemplifies the type of meaningful partnerships that will evolve between D3M as a data science and precision medicine hub, and clinicians across Mount Sinai who manage the patient populations,”notes senior author NoamBeckmann, PhD, Assistant Professor of Medicine (Data Driven and Digital

Medicine). “Together, we can create rich, patientcentric datasetsthat allow us to investigate the big medical problems of our time.”
Tapping into the vast resources of the Mount Sinai COVID-19 Biobank, researchers examined gene expression data in blood samples from morethan 500 patients hospitalized with COVID-19 between April and June 2020. More than 160 provided selfreported assessments of a broad range of symptoms still present six months or more after hospitalization, including fatigue,dyspnea, sleep disruptions, and smell and taste problems. The team tested each gene expressed in the blood for association with each long COVID symptom,and then for associations specific to each of 13 different types of immune cells, including plasma cells. Finally, these associations were categorized by whether they matched up with changes in patients’levels of antibodies specific tothe virus.
Among the team’s breakthrough findings was the presence of twomolecularly distinct subsets of long COVID symptoms with opposing gene expression patterns, often observed in the same plasma cells (the immune system’s antibodyproducing cells).In patients who progressed to pulmonary problems, for example, antibodyproduction genes were less abundant, while in patients with non-respiratory issues, suchas loss of smell and taste or sleep problems, the same antibody-producing genes weremore abundant.
“These opposingpatterns point to the existence of multiple independent molecular processes leading to different longCOVIDphenotypes,” explains Dr.
Beckmann, whose omics skills include genomics, proteomics,andtranscriptomics. “Just as importantly, our data revealed that these processes arealready present during the acute infection stage of COVID-19. This finding has tremendous implications for the design of research studies as well as for the development of potential biomarkers,prevention strategies, andtreatment options for individuals who develop long COVID.”


NoamBeckmann, PhD
Assistant Professorof Medicine (Data-Driven and Digital Medicine)
GirishNadkarni, MD,MPH
Irene and Dr. Arthur M. Fishberg Professor of Medicine; Chief, Division of DataDriven and Digital Medicine
The Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetesand Bone Disease provides care for patients with endocrine diseases, including diabetes,throughout New York City by unifying protocols, programs, and treatments through outreach, education, and innovative community-based programs.
The Division is at the forefront of cutting-edge research on endocrine diseases and diabetes. It trains future leaders andinnovators in the field of endocrinology through aworld-renowned fellowship program, and is developing innovative quality improvement programs to achieve the highest quality standards in diabetes and endocrine patient care.
TheMountSinaiDiabetes,Obesity,andMetabolism InstituteattheIcahnSchoolofMedicineatMount Sinaiwascreatedtofindacureandtodevelop bettertherapeuticandpreventionstrategiesfor thosewhoexperiencediabetes,obesity,and
metabolicsyndromes.Physician-scientistsfrom variousspecialtiesacrosstheMountSinaiHealth System,includingendocrinology,surgery,genetics andgenomics,andpharmacologyandsystems therapeutics,areconductinggroundbreaking researchtorevolutionizetheapproachtoall metabolicdisorders.

Andrea Dunaif, MD
Lillian and Henry M. Stratton Professor of Molecular Medicine

Emily Gallagher, MD, PhD, received a Method to Extend Research in Time (MERIT) Award from the National Cancer Institute to study the role of high triglyceride levels in drivingtriple negative breast cancer growth and metastasis.
A Mount Sinai researcher in 2022 receiveda $2.5 million, five-year grant from the National Institutes of Health (NIH) to conduct a novel study into the mechanisms linking elevatedtriglyceride levels and triple negative breast cancer.
Emily Gallagher, MD, PhD, Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at theIcahn School of Medicine atMount Sinai, received theMethod to Extend Researchin Time (MERIT) Award from the National Cancer Institute (NCI), part of the NIH, to study therole of high triglyceride levels in driving triple negative breast cancer growth and metastasis. Dr. Gallagher is aphysician-scientist with a clinical practicein the field of onco-endocrinology, the management of endocrine and metabolic complications of cancer.
More than 50 percent of women with triple negative breast cancer have elevated circulating triglycerides andthese elevated levels are associated with reducedbreast cancer survival. Further, a number of factors, including obesity, diabetes, highcarbohydrate diets, and excess alcohol consumption can contribute to high circulating triglyceride levels. The link between hypertriglyceridemia (HTG)and triple negative breast cancer has been described in epidemiology studies, but checking and treating triglyceride levels in women with triple negative breast cancers is not part of standard oncology care.
Ultimately, my goal is to improve outcomes for women living with triplenegative breast cancer and metabolic conditions.
— Emily Gallagher, MD, PhD
“ThisgrantfromtheNIH/NCI willgiveusabetter understandingof howelevatedtriglycerides contributetotriplenegativebreast cancergrowth andmetastasis—somethingthat,mechanistically,
hasn’t beenpreviouslystudied,”saysDr. Gallagher, whoisalsoDirectoroftheResearchPathway, and AssociateProgramDirector of theInternalMedicine ResidencyProgram,bothatIcahnMountSinai.
The grant will allow Dr. Gallagher and her team to explore how human breast cancers take up triglycerides from circulation in the form of verylow-density lipoproteins. To understand the biological links between HTG and the progression of triple negative breast cancer, the team is employing preclinical models of hypertriglyceridemia in isolation from other metabolic abnormalities. In preliminary studies, the team found that the mice with HTG develop more rapid growth and metastasis of triple negative breast cancers.
The HTG micedemonstrated lipid profiles with elevated very-low-density lipoprotein (VLDL) and high circulating of phospholipids associated with elevated VLDL. The team hypothesized that HTG promotes the growthand progression of triple negative breast cancer by increased VLDL uptake through the VLDL receptor,which contributes to lipid peroxidation products in hypoxic tumors. They hypothesized that lipid peroxidation affects cellsignaling pathways, which enhance tumor cell survival and metastasis.
Theteamisalsoexploringtheimportanceoftumor VLDLreceptor expressioninHTG-drivencancer growthandmetastasisusingxenograftsderived fromhumantriplenegativebreastcancers. Additionally, theresearcherswillexamine therapeuticstrategiestolower triglycerides, which, if successful,couldbetranslatedintoclinicalcareto improveoutcomesforwomenwithhightriglyceride levelsandtriple-negativebreast cancer.
“In my oncoendocrinology clinical practice, I see many women whohave high triglycerides and breastcancer, sometimes as a result of their breastcancer treatment,” Dr. Gallagher says. “My hope is that through this funding, we will be able to determine in preclinical models if starving triple negative cancer cells ofthese lipids can be exploited as anoveltherapeutic strategy.
Ultimately, my goal is toimproveoutcomes for women living with triple negative breast cancer and metabolic conditions."

EmilyGallagher,MD, PhD
Associate
Professor
of Medicine (Endocrinology, Diabetes and Bone Disease)

Women with PCOS haveincreased prevalence rates of type 2 diabetes and metabolic syndrome, important risk factors for cardiovascular disease. However, there have been no definitive studies demonstrating that women with PCOS have increased cardiovascularevents, such as myocardial infarction and stroke.

Polycystic ovary syndrome (PCOS)is one of the most common disorders of women of reproductive age, affecting up to 20 percent of thispopulation worldwide, depending on the diagnostic criteria applied. It was originally described inthe 1930s as a reproductivedisorder characterized by irregular menstrual cycles, infertility,and hirsutism. Beginning in the 1980s, it was discovered that PCOS was amajor metabolic disorder. Women with PCOS werefound to have increased prevalence rates of type 2 diabetes and metabolic syndrome,important risk factors for cardiovascular disease. However,therehave been nodefinitive studies demonstrating that women with PCOS have increased cardiovascular events, such as myocardial infarction and stroke.
The question of whether PCOS actually confers increased cardiovascular disease risk is of considerable public health importance, given its high prevalence rates. To begin to address this question, atwo-day virtual workshop, “Cardiovascular (CV) Risk Across the Lifespan for Polycystic Ovary Syndrome,” was convened in October 2021 by the National Institutes of Health’s National Heart Lung andBlood Institute, Eunice Kennedy Shriver National Instituteof Child Health
and HumanDevelopment, National Cancer Institute, National Institute of Diabetes and Digestive and Kidney Diseases, andOffice of Disease Prevention. The objective of this workshop was to identify criticalresearch needs and knowledge gaps regarding cardiovascular disease risk inPCOS. Andrea Dunaif, MD, Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetesand Bone Disease at the Icahn School of Medicine at Mount Sinai, and a global authority on PCOS, was one of thethree workshop co-chairs who developed the workshop's scientific agenda.
A unique featureof thisworkshop was that it brought together preeminent experts in cardiology and epidemiology with leading investigators in PCOS. “Although there is a vast literature demonstrating that reproductive-age women with PCOS have surrogatemarkers for cardiovascular disease, the only way we’re going to conclusively determine whether PCOS increases cardiovascular disease is through long-term prospective studies that follow affected womento an age when they startto experience cardiovascular events, which is approximately 10 years after menopause, in their60s and onward,” says Dr. Dunaif. To be successful inthis
endeavor, it isessential that scientists engaged in cardiovascular science are attracted to thefieldto address the numerous unanswered questions regarding disease risk.
One particularly intriguing possibility is whether PCOS itself might confer protection against cardiovascular disease. “Given the substantially increased risk for type 2 diabetes in young women with PCOS, we would expect to see a similar increase in cardiovascular disease risk, since diabetes abolishes the protective effect of premenopausal status on this risk,” notes Dr. Dunaif. However, some studies suggest that there is delayed ovarian aging and menopause in PCOS. Genetic analyses support this observation by finding a relationship between PCOS and genetic variants associated with later age at menopause. “Whether later menopause itself or ‘anti-aging’ actions in other organ systems reduce cardiovascular disease risk in PCOS is a critical unanswered question,” Dr. Dunaif says.
PCOS presents a unique opportunity for cardiometabolic risk reduction. “Since we are able to diagnose PCOS in girls within a couple of years of the start of their menstrual cycle, we could begin modifying risk factors for cardiovascular disease at a very young age,” she says. “These preventive measures could include, for example, carefully monitoring and controlling weight gain, lipid abnormalities, and blood pressure. Currently, there is no attempt to diagnose PCOS at an early age and no counseling about the risk for diabetes, which is really sad because women who are vulnerable to PCOS aren’t getting the care they need.”
Indeed, womenwith PCOS are highly dissatisfied with the health care theyreceive. It usually takes more than twoyears and visits to three ormore health careproviders before PCOS is diagnosed. “Thereis clearly atremendous need for health care provider education regarding the diagnosis, multisystemmanifestations, and management of PCOS. A majorimpediment to educational initiatives is the name ‘PCOS’ itself. It is a misnomer in that thereare no cysts in the ovary. Further,the name focuses on the ovary when PCOS is actually muchmorethan a reproductive disorder,” says Dr. Dunaif.
The expert panel from the lastmajor NIH meeting on PCOS, the Evidence-Based Methodology Workshop, heldin 2012, recommended that the name bechanged toone that reflects the fact that it is acomplex endocrine and metabolic disorder affecting women across the lifespan. Efforts to change the name to onethat meets the requirements of all stakeholders, including patients, areongoing.

AndreaDunaif,MD
Lillian and Henry M. Stratton Professor of Molecular Medicine; Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes and Bone Disease


Useof an automated insulin delivery system improved glucose control among peoplewith type 2 diabetes,representing a potential option for those who are struggling to keep their glucose levels in range.
Use of an automated insulin delivery system improved glucose control among people with type 2 diabetes, a study conducted by Mount Sinai endocrinologist Carol J. Levy, MD, CDCES, has shown.
The system tested, from Tandem Diabetes Care, comprises a t:slim X2 insulin pump and a continuous glucose monitor (CGM), both worn on the body. Incorporated within the insulin pump is software called “Control-IQ” that uses the glucose numbers and trends from the CGM to direct semi-automated insulin delivery. This system was approved in early 2020 based on research performed by a consortium of expert investigators (including Dr. Levy’s team) from a pivotal trial sponsored by the National Institutes of Health.
This “closed loop,” or “artificial pancreas” technology is recommended for people with type 1 diabetes, and its useis growing in that population. The 2022 study by Dr. Levy and colleagues indicated that the technology may also benefit people with type 2 diabetes who require insulin, regardless of how they were taking insulin at baseline and whetherthey were also using other oral or injectable glucose-lowering medications.
“It’s not for everyone with type 2 diabetes but rather those already requiring insulin with or without other medications for type 2 diabetes. But I think this could represent an option for those who are struggling to keep their glucose levels in range,” says Dr. Levy, Professor of Medicine (Endocrinology, Diabetes and BoneDisease), and Director of the Mount Sinai Diabetes Center
She presented data from the prospective, singlearmtrial of 30 adults with type 2 diabetes in November2022, during the virtual meeting of the Diabetes Technology Society. The study was sponsored by Tandem Diabetes Care, Inc., maker of the t:slimX2 insulin pump.
It’s not for everyone with type 2 diabetes but rather those already requiring insulin with or without other medications for type 2 diabetes.
— Carol J. Levy, MD, CDCES
The participants had a mean age of 54 years, median diabetes duration of 14 years, and a mean hemoglobin A1C of 8.6 percent, considerably higher than the recommended target of less than 7 percent. They were a diverse group; with an enrollment consistent with what would be seen in people with type 2 diabetes based on race and ethnicity.
At baseline, just overhalf were using CGMs, 13 were using only basal insulin, and 17 were using both basal and pre-meal insulin. Among those17 participants, 15 wereusing multiple daily injections, and two were using insulin pumps.
Most participants werealso taking other medications, including sodium-glucose cotransporter-2 (SGLT2) inhibitors, glucagon-like peptide 1 (GLP-1)agonistsdipeptidylpeptidase 4 (DPP-4) inhibitors or a combination of morethan one medication in addition to insulin as is typical for people with type 2 diabetes. They continued taking these adjunctive medications throughout the trial.
After six weeks, the mean timespent inthe glucose range of 70-180mg/dL (the target recommended range for blood sugars) was 71 percent, the mean time spent with levels greater than 180 mg/dL was 29 percent, and time spent above 250mg/dL was just 2.9percent. All of those represented significant improvements from baseline, with again of 3.6 hours per day inrange and one fewerhour perday above 250 mg/dL.
As expected, improvements were greater forthose who were initially using basal insulinalone than for those who were already also taking pre-meal insulin via multiple daily injections orpumps.
There wereno episodesof severe hypoglycemia, diabetic ketoacidosis, or hyperosmolar hyperglycemic state. Time spent withglucose levels below70 mg/dL dropped by 0.03 percent, a significant improvement, while time below 54 mg/dL, rareto begin with, remained the same.
There was someweight gain, from 81.9 kg to 83.2 kg, acommon occurrence with improved glycemic control. Totaldaily insulin dose rose from 0.53U/kg to 64U/kg, also often seen with improvement in blood sugar control.
Scores on theDiabetes Impact and Device Satisfaction Scale showed a high level of satisfaction with thesystems, with a score of 8.8 on a scale of 1 to 10.
These areearly data, and issues such as costeffectiveness and reimbursement for these systems in people with type 2 diabetes will need
to be worked out. But, Dr. Levy believes even the protection from hypoglycemia alone argues in favor of theiruse.
“Theriskof negativeoutcomeswithhypoglycemia canbepronouncedinpeoplewithlonger duration of diabetes. Most of thestudyparticipantswerein their50s, withanother20to30yearstolive, sowe believethat improvementinglycemiaat leastfor thisyounger populationwillleadtoamorerobust outcomeandpotentially better qualityoflife.”

CarolJ.Levy,MD
ClinicalDirector of the MountSinai Diabetes Center, and Associate Professor of Medicine (Endocrinology,Diabetes and Bone Disease)

The mission of the Dr. Henry D. Janowitz Division of Gastroenterology at Mount Sinai is excellence in the delivery of patient care, research, and education in diseases ofthe GI tract. For more than a century, Mount Sinai gastroenterologists, surgeons, pathologists, and experts in related clinical and researchareas havebeen at the forefront of innovation, shaping the future of GI medicine and clinical practice. Our pioneering work has led to advances in the diagnosis, treatment, and management of inflammatory bowel disease, peptic ulcer disease, esophageal disorders, gastrointestinal cancers, and pancreatic and biliary diseases.
To achieve its mission, the Division of Gastroenterology has developed continually expanding, world-leading digestive disease centers of excellencethat include the Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center and the GI Motility Center. Each center, with its distinct subspecialty and focus area, allows us tofurther the science of gastroenterology on several fronts and keeps us
at the cutting edge of delivering the highest quality of patient care. Other programs of excellence include advanced colonoscopy and therapeutic endoscopy services andpancreatic cancer
The Division of Gastroenterology at TheMount Sinai Hospital was recently ranked No. 1 inNew York by Newsweek for 2024 and No. 6 in the United States by U.S. News & World Report® for 2023-24.

Bruce E. Sands, MD, MS
Dr. Burrill B. Crohn Professor of Medicine

Mount Sinai researchers have found strong evidence that before the first symptoms of Crohn’s diseaseand ulcerative colitis occur, there’s a preclinical phase inwhich immune and inflammatory pathways are already altered. By targeting and treating the early pathogenic events that promote IBD development, they believe, disease onset could be prevented or impeded.
Whilea torrent of new drugs and therapeutic targets has brought relief to patients with inflammatory bowel disease (IBD),disease modification and cure remain critically needed but elusive endpoints.
Jean-FredericColombel,MD,Professorof Medicine(Gastroenterology)at theIcahnSchoolof MedicineatMount Sinai,believesthoseholygrails areachievablethroughthepursuitof aboldnew targetthathasprovensuccessfulinother medical fields:diseaseprediction andprevention.Inother words, bytargetingandtreatingtheearly pathogeniceventsthat promoteIBDdevelopment, diseaseonset couldbepreventedor impeded,and atrueopportunitytochangeitscourserevealed.
“Wenowhavestrongevidencethat beforethefirst symptoms of Crohn’sdiseaseandulcerativecolitis ever occur,there’sapreclinicalphaseinwhich immuneandinflammatorypathwaysarealready altered,” saysDr.Colombel, whois Directorof Mount Sinai'sSusanand LeonardFeinstein InflammatoryBowelDiseaseClinicalCenter andits researchcounterpart,TheHelmsley Inflammatory
BowelDiseaseCenter. “Beingabletoidentifyinthe bloodorstoolthosedysregulatedpathwaysthrough biomarkers,suchas proteomics,metabolomics,gut microbiome, andantimicrobialantibodies, willlead tothedevelopmentof predictionmodels and preventionstrategies.”
Dr. Colombel has made measurable progress toward that goal through several new investigations. One study, in Gastroenterology, reported the presence of anti-granulocyte macrophage-stimulating factor autoantibodies (aGMAbs) in the sera of patients with Crohn’s disease up to six years before diagnosis, suggesting they could contribute to the pathophysiology of the disorder. “Our study demonstrated IgG2- and IgA-skewed isotopes of aGMAbs in patients with Crohn’s disease, indicating an origin within the intestinal mucosa,” explains Dr. Colombel. “We also found that aGMAbs not only predict the diagnosis of Crohn’s disease well in advance, but, in a subset of patients, they are associated with ileal involvement, disease severity, high relapse rates, and complications at disease onset.”
We now have strong evidence that before the first symptoms of Crohn’s disease and ulcerative colitis ever occur, there’s a preclinical phase in which immune and inflammatory pathways are already altered.
— Jean-Frederic Colombel, MD
To make new inroads into IBD prediction and prevention, Dr. Colombel’s team has reached beyond traditional epidemiological research platforms and pressed into service “multiomics,” an advanced methodology designed to leverage unbiased high-throughput data relevant to IBD. As outlined in a recent Mount Sinai study in Nature Reviews Gastroenterology and Hepatology, multiomics is uniquely equipped to find the critical links between the genome, microbiome, proteome, and exposome on the road to developing a model to characterize IBD risk factors and molecular pathways.
Nothing is more critical to IBD research, however, than Mount Sinai’s collaboration with a consortium of academic, industry, and government organizations. This partnership is drawing on a powerful resource: the U.S.
Department of Defense’s (DOD) serum repository. Its millions of blood samples were taken from soldiers when they enlisted, and every two years of service thereafter, from 1998 through 2013 as part of the United States Defense Medical Surveillance System. “Some of these soldiers go on to develop IBD, and we’re able to link these samples to their medical records and track the development of markers preceding the clinical diagnosis,” Dr. Colombel says.
“If we’regoing to finda way toprevent Crohn’s disease and ulcerative colitis, it will requirethe global GI community actively embracing this new paradigm of prediction and prevention,”declares Dr. Colombel. “Weare making great progress, but so much work remains.”

Jean-Frederic Colombel,MD
Professor of Medicine (Gastroenterology)

A clinical study of autologous stem cell transplantationfor severe Crohn's disease is offering the sickest of patients a transformative therapy that is achieving remarkableearly results in this group for whom nothing in the past has worked.
For people with severe Crohn’s disease, life often becomes a grueling carousel of narcotics and surgery, with no way off. Mount Sinai is startingto change that paradigm with a clinical study that is offering the sickest of patients a transformative therapy—autologous stem celltransplantation— that is achieving remarkable early results in this groupfor whom nothing in thepast has worked.
“We’re finding that autologous stemcell transplants benefit about 90 percent of Crohn’s disease patients who fitvery specific criteria, compared tomaybe 15 percent who benefit from new drugs when they’re introduced,”says Louis Cohen, MD, Assistant Professor of Medicine (Gastroenterology) at the Icahn School of Medicine at Mount Sinai, who is heading upthe trial. “Even whenthe disease returns, it seems to be in a different form, and patients suddenly become responsive tomedication. We’re conducting rigorous research to try and understand why.”
Autologous stem cell transplants for Crohn’s disease are offered by only a handfulof medical centers inthe world. LizPalen is one of the

beneficiaries. Diagnosed with Crohn’s in 2012, the 36-year-old registered nurse began a 10-year regimen of biologic injectables, steroids, surgical bowel resection, and a colostomy to try and control recurring symptoms. “I hadjoint pain, skin rashes, fatigue, nausea, and no appetite,” she recalls. “I was on allthemedications, and nothing seemed to improvemy quality of life for more than a brief time.”
Desperatefor a solution, she heard about the nascent field of stem cell transplants. With a referral from her local gastroenterologist, she wound up in Dr. Cohen’s office in November 2019. After determining that she met the entry criteria, Dr. Cohen carefully explained the procedure, which required nearly six weeks of hospitalization. After undergoing a baseline endoscopy, colonoscopy, andMRI to document mucosal disease activity, patientsare tapered off all medications in preparation for stem cell mobilization. That process involves low-dose chemotherapy; administration of growth factors; and harvesting healthy red blood cells, immune cells, and platelets fromthe patient’s hematopoietic system.

“We believe that in patients predisposed to Crohn’s disease, there are certain triggers that cause the immune system to essentially go wild,” explains Dr. Cohen. “Through stem cell transplants, we’re in essence resetting, or turning back, the immune system to a time when it functioned normally.”
Ms. Palen opted to divide the procedure into two in-hospitalsegments, allowing her some timein between to rest. For the stem cellmobilization phase, she entered The Mount Sinai Hospital in Manhattan in December 2019, and returned three weeks later tohave the harvested stem cells returnedto her bloodstream. Throughout her hospitalization, she was able to access as part of the clinical trial program a panoply of support services designed to relieve the inpatient burden. These included a team of nutritionists, palliative care specialists, a social worker, apsychologist, and even amassage therapist.
Within six weeks of discharge, Ms. Palen began noticing an improvement in herCrohn’s disease symptoms. At six months, she was in full remission. “I dida 180-degree turnabout in symptoms and energy level, and was ableto get back to activities such as camping and golfing, which I couldn’t do before. I also got married and bought a new home. There’s no question itwas a life-changing experiencefor me.”
As for medications, right after transplantation, Ms. Palen began taking vedolizumab—an antiintegrin agent that’s a critical part of the Mount
Sinai clinical trial regimen. “Our overriding goal is complete remission for our patients,” emphasizes Dr. Cohen, “and we think that vedolizumab is an outstanding way to achieve that by keeping the immune system in check and helping to turn back the clock on the disease.” Indeed, Ms. Palen reports she is now able to take medications that were previously off the table because of antibodies her body had developed against them.
Adds Dr. Cohen, “Noone has ever attempted this type of surgical and therapeutic approach before, but we believe it can open the door to stem cell transplants for growing numbers of people with Crohn’s disease before they spend years of their lives suffering.”

LouisCohen,MD
Assistant Professor of Medicine (Gastroenterology)

Recent studies underscore the benefit of highrisk pancreatic surveillance programs that have helped push three-year survival rates as high as 85 percent in some cases, inlarge part by catching a higher proportion of malignant lesions while they are still resectable.
Pancreatic cancer—the third leading cause of cancer death inthe United States—is typically thought of as aterminal diagnosis, even by professionals in the field. The five-year survival rate for pancreatic adenocarcinoma remains around 9percent.
But the tide could well be turning thanks to advanced new treatments and aggressive surveillance. Indeed, recent studies have underscored the benefit of high-risk
genetic counselors. Tethered tothis program is a robust research initiativedriven by a registry of more than 800 high-risk patients who, inmany cases, have undergone surveillance and agreed to participate in clinical trials.
“In our program, patients areoffered a full risk assessment based on a very detailed threegeneration family historyfocused on pancreatic cancer, as well as otherneoplasms such as breast, ovarian, skin, and colon cancers,” says

pancreatic surveillance programs that have helped push the three-year survival rates as high as 85 percent in some cases, in large part by catching a higher proportion of malignant lesions while they are still resectable.
From the opening of its specialized pancreatic cancer surveillance program 10 years ago, Mount Sinai has been in the vanguard of the field. The focus ison early detection through active risk assessment—particularly in families where two or more immediate members have a history of the disease—led by a team of clinicians experienced in gastrointestinal cancers, working closely with
Aimee Lucas, MD, MS, Professor of Medicine (Gastroenterology) at the Icahn School of Medicine at Mount Sinai, who launched the surveillance clinic in 2012. “After seeing our genetic counselors, patients typically meet with meto plan a personalized clinical surveillance program, which may include endoscopic ultrasound or MRI. At the end of the visit, we draw blood for genetic testing and any clinical or researchlabs that might be indicated.”
About a third of patients screened at the Upper East Side clinic inManhattan show small, subcentimeter pancreatic cysts on imaging. “The
majority of cysts do nothing over time, so we simply watchthem,” Dr. Lucas says. Some features, however,can serve as markers for neoplastic progression to high-grade dysplasia or pancreatic cancer, including the presenceof multifocal cysts,cyst growth, or solid nodules.
In fact, telltale biomarkers are at the heart of Dr. Lucas’s growing body of research for detecting early pancreatic cancer. One study in which she was senior author found, for example, that highrisk patients with elevated hemoglobin A1c (HbA1c) were more likely to have pancreatic cysts compared to patients with lower levels observable through screening—findings that could be helpful in tailoring surveillance protocols for individuals at increased risk of developing pancreatic adenocarcinoma. Past research in the field has established new-onset diabetes mellitus as a precursor to pancreatic cancer, with approximately 85 percent of patients diagnosed with the malignancy also having impaired fasting blood glucose or diabetes.
In another study, Dr. Lucas significantly expanded the boundaries of that knowledge with the discovery that metabolic changes such as worsening glycemic control and weight loss may be harbingers of underlying pancreatic cancer. More specifically, she and her research team
learned that glycemic elevations may occur up to three years before diagnosis, and weight loss up to two years prior to diagnosis. For that reason, they recommended including markers of glucose intolerance and body mass index trends in predictive models of pancreatic cancer.
“One of themajor reasons pancreatic cancer remains so deadly is because of late detection,” Dr. Lucas points out. “That’s why we’re so focused on investigating genetic predisposition and biomarkers for early detection, andpairing that information with anaggressive surveillance program that could lead to improved outcomes.”

AimeeLucas, MD,MS
Professor of Medicine (Gastroenterology)
Chief, Division of Gastroenterology at MountSinai Morningside and Mount Sinai West

The Mount Sinai Division of GeneralInternal Medicine encompassesmuch morethan outstanding clinical care. Continuous qualityimprovement efforts, innovative care models, dynamic educational programs, and health services research characterize the Division. A personal and interdisciplinary approach involving colleagues and services in nursing, social work, medical and surgicalsubspecialties, psychiatry, and rehabilitation is often used to diagnose, treat, manage, and healthe whole patient. The Division of General InternalMedicine is able tomake referrals and coordinate care with a vastarray of outstanding specialty services, andcollaborate with them to create new models of care.
Faculty members areconsistently championing population health initiatives, an important step in the evolution of health care delivery. The Division is using information technology and data systems to tailor entire clinical programs that better manage chronic illnesses and preventivecare
efforts, thereby improving patients’ overall health and decreasing health care costs.
Over the last year, Internal Medicine Associates (IMA) has continued to focus onrefining teambased careprocesses for chronic disease management, as well as improving medication adherencerates, adherence to age-appropriate cancer screening, and transitions of care.
For diabetes, IMA continues to use a teambased model of care involving Certified Diabetes Educators and a dedicated high-A1c clinic staffed by our internal medicine interns with faculty oversight. In August 2022, our A1c >9% control rate reached 13.5 percent, which is below the goal of less than 15 percent. We have continued to meet or exceed that goal since then.
Among patients with hypertension, theIMAis increasing the controlrate from 60 percent to 70 percent with a goal of 75 percent. A robust
management guideline includes home blood pressure monitoring. TheDivision improved its home blood pressure monitor access via a partnership with Integra(a benefitsmanager that is responsible for providing homecuffs for patients)by creating a closed-loop feedback process to track orders. In 2021, fulfillment was 50-60 percent and it is now at 80-90 percent. IMA continues to work with its population healthteams on outreach efforts toconnect value-based contract patients to these programs.

Juan
Wisnivesky, MD,
DrPH
Drs. Richard and Mortimer Bader Professor of Medicine

Mount Sinai houses several National Institutes of Health (NIH)-funded T32 fellowships to train researchers. Among them are a program focusing on cancer prevention and control for clinical and non-clinical scientists, and aprogram focusing on disparities in aging and dementia.
Mount Sinai is not only a renowned center of medical research, but also a center for research training, housing several National Institutes of Health (NIH)-funded T32 fellowships. Diversity of background, training, and thought are important components of these fellowships, creating crosspollination that can significantly advancethe field.
Two T32 programs stand out. The two-year Cancer Prevention andControl (CPC) in Priority Populations T32 fellowship program, established in 2018, focuses on training clinical and nonclinical scientists whoseaim is to advance CPC in specific populations that are disproportionately vulnerable tocancer.
“CPCisawayof thinking aboutdoingresearchthat either looksat ways topreventcancerorcontrolit, usuallyintherealmofcancersurvivorship,” explainsJennyJ.Lin,MD, MPH, thesystem director formentoringandProfessorofMedicine (GeneralInternalMedicine)at theIcahnSchoolof MedicineatMount Sinai.Dr. Linisalsothe AssociateDirectorof theCPCprogram.
“The research can be about cancer treatment, but it is often about survivorship—for example, how cancer survivors manage comorbid illnesses or palliative care. This research is broad, tending to be about health servicesor epidemiology. Thereis also behavioral research, and quite a bit of work done on cancer prevention that focuses on patient education, patient outreach, and comparative effectiveness,” Dr. Lin says.
Alex Federman, MD, MPH, a mentor for the program, Professor of Medicine (General Internal Medicine), and Geriatrics and Palliative Medicine, and the Division’s Director of Research, adds, “One thing that characterizes this program and others is that we support multiple disciplines and methodologies.”
Indeed, one of the great strengths of the CPC fellowship is the diverse backgrounds from which the fellows come, allowing for crosspollination of ideas and expertise from divergent areas. One fellow is a nurse scientist, another an endocrinologist, a third a behavioral health scientist, the fourth a gastroenterologist.

Allhavestrongresearchinterestsinso-called prioritypopulations, whichisabroadtermdesigned tobeinclusiveof groupsthat areinsomeway vulnerable, andthusatriskfor worsehealth outcomes. “So,prioritypopulationsmightinclude minorities, theelderly,individuals withcertain comorbidities, thosewith differentsexual orientationsorlowsocioeconomicstatus, and thoselivinginaruralpopulation,”explainsProgram DirectorJuanWisnivesky, MD,DrPH, theDrs. RichardandMortimer BaderProfessorofMedicine andChiefof theDivisionof GeneralInternal Medicine.“Wealsoincludeindividualsexposedto theWorldTradeCenter sitebecauseit isaspecific populationthat is servedbyMount Sinaiandhas experiencedworsecanceroutcomes.”
The second notable two-year T32 training program is the Research on Disparities in Aging and Dementia fellowship—hence its acronym, DiAD—whose directorsare Drs. Lin and Federman, as well as Albert L. Siu, MD, Chair Emeritus of theBrookdaleDepartment of Geriatrics and Palliative Medicine
Theprogram,nowinitsthirdyear,focuseson peoplewithAlzheimer’sdiseaseandother dementias,aswellasolderadultsexperiencing inequitiesinhealthoutcomes.“Theprogramhasto dowithcognitiveimpairment,butitdoesn’t necessarilyhavetobeinolderadults,”Dr.Linnotes.
As with the CPC program, theDiAD program benefits greatly from the many disciplines of its fellows, which currently include a hospice and
palliative care physician-scientist, an internist, a nurse scientist, and a clinical neuropsychologist. “Ithink the uniqueness of these two programs is because we havesomany different peoplefrom different departments from different fields,” Dr. Lin says. “They are not all physicians, and that really promotes a lot of cross-disciplinary collaboration as wellas thinking.”
Both the CPC and DiAD programs include interdisciplinary curricula and are especially strong in mentorship, with as many as 20 faculty researchers supporting the fellows in each program. “There are multiple levels of mentorship,” Dr. Federman explains. “The most important is the trainee’s primary mentor, who is the person they are working with on their main project. That is often the closest working relationship that the fellows will have.
“But for both programs we strive to create a mentorship team for the trainees, whichwe aim to be a multidisciplinary experience. We look at the individual needs of the trainee. Those needs may be content-specific, or methodological, or general career direction. We link up the appropriate mentors witheach trainee.”
One of the goals of both the CPC and DiAD programs is to launch the careers of its fellows. By that measure the programs have been highly successful, with trainees continuing on to rewarding academic research careers at Mount Sinai and elsewhere and receiving career development awards and research grants from the NIH, American Society of Clinical Oncology, the American Cancer Society, and others.




AlexFederman, MD,MPH
Professor of Medicine (General Internal Medicine), and Geriatrics and Palliative Medicine
JennyJ.Lin, MD,MPH
Professor of Medicine (General Internal Medicine)
AlbertL.Siu,MD
Professor and Chair
Emeritus ofGeriatrics and Palliative Medicine; Professor of Medicine, and Population Health Science and Policy
JuanWisnivesky, MD,DrPH
Drs. Richard and Mortimer Bader
Professor of Medicine; Chief of theDivision of General InternalMedicine

The Mount Sinai Division of General Internal Medicine has developed several innovative models that provide for highly coordinated and multidisciplinary care to patient populations that often find themselves outside the mainstream.
Constantly looking for ways to improve the traditional delivery of health care, the Mount Sinai Division of General Internal Medicine has developed several innovative models that provide for highly coordinated and multidisciplinary care to patient populations that often find themselves outside the mainstream.
Acaseinpoint is thecreationof acomprehensive obesitymanagementprogramdirectedat individualsfromdisadvantagedgroupsthat disproportionatelystrugglewithweight issues, who oftenfindit difficult toaccessappropriateclinical services.Awareof thatvoid, theDivisionof General InternalMedicineat MountSinaiMorningsideand Mount SinaiWest openedaclinicinthefallof2023 underthedirectionof RebeccaShafer, MD, a certifiedobesitymanagementphysician. Knownas theCenterforHealthyWeight Management,it is believedtobethefirstofits kindintheNewYork metropolitanregionandisbeingruninpartnership withRyanHealth, which has beenprovidingawide
rangeofmedicalservices forthepast50years tounderservedcommunitiesinManhattan.
“We’ve developed a unique way to integrate an obesity management program into the primary care settingin order to give patients access to a specialized program they wouldn’t normally find at the community level,” said Fernando Carnavali, MD, Associate Professorof Medicine (General Internal Medicine) at the Icahn School of Medicine at Mount Sinai, and Chief of GeneralInternal Medicine at Mount SinaiMorningside and Mount Sinai West. “We’re focused on medication management, nutrition support, education, and mental health, allof which are closely aligned with the broad-basedmodel of care the Ryan network has sosuccessfully brought to the community.”
The framework forthis newest program began taking shape more than a year ago when Mount Sinai hired a physician with fellowship training in obesity management. The Division of Internal

Medicine is nowgrooming a number of residents pursuing primary caretracks to also become certified in that field. At the sametime, points out Dr. Carnavali, these clinical trainees aregaining valuableexposureto underserved populations and public health services by working alongside specialists at the Ryan sites, which include clinics and community outreachcenters offering adult medicine, women’s health, mental health, pediatrics, and otherspecialized forms of care.
The concept of a seamless health care environment for the community also figures heavily in the key role General Internal Medicine is playing in the recently opened Mount SinaiBehavioral Health Center in Lower Manhattan. Specifically, the $140 million facility co-locates on its second-floor outpatient psychiatry services with a primary care practice equipped to manage a full range of patient morbidities —an unusual and novel partnership by traditional health care standards.
“Our goal was to bring primary careto a community on theLower EastSide of Manhattan where access to suchquality services is sparse,” notes Leonard Amoruso, DO, Assistant Professor of Medicine (General Internal Medicine) at Icahn Mount Sinai, andChief of General Internal Medicine at Mount Sinai Beth Israel. “Now,while patients arevisiting the psychiatry clinic, they could walk down the hallway and have a sameday appointment with a primary care doctor for health carescreening, routine labs, or many other services they wouldn’t normally get, giventhe fact that mental illness often stands as a barrier to generalmedicalcare.”
In addition to creating innovative new approaches to health care delivery, the Division of General Internal Medicine takes pride in its ability to recruit in a post-pandemic world a rich crop of professsional talent for its faculty andtrainee ranks. “Amid all the competition, we’ve been
capturing people from all over the country, as well as from our own hospitals,” says Juan Wisnivesky, MD, DrPH, Drs. Richard and Mortimer Bader Professor of Medicine and System Chief of the Division of Internal Medicine. “We’re securing the future of our entire department by drawing people with fresh ideas and strategies on how to make health care work for growing populations of patients.”



FernandoCarnavali, MD
Associate Professor of Medicine (General Internal Medicine)
LeonardAmoruso, DO
Assistant Professorof Medicine (General Internal Medicine)
JuanWisnivesky,MD, DrPH
Drs. Richard and Mortimer Bader Professor of Medicine; Chief of the Division of GeneralInternalMedicine

Around the world, researchers, clinicians, and the generalpublic are recognizing the integral role of genomics within numerous areas of health and medicine. To positionthe Department of Medicine at the forefront of thisrapidly expanding landscape in the era of precisionmedicine, Mount Sinai established the Division of Genomic Medicine. Its mission is toadvance, implement, and scale genomic approaches toimprove the diagnosis, treatment, and prevention of disease.
The scarcity of genetics experts in health care, including medical geneticists and genetic counselors, limits the widespread use of meaningful genomic information. The need for delivery and interpretation of genomic results adds to growing demands on physicians in primary and specialty care, who are increasingly expectedto interpret genomic findings, recognize genomic risk, and assimilate genomics into the care of their patients.
Through patient-centeredclinicalapplications, collaborative research, and innovative outreach and training programs, the Division of Genomic Medicine is dedicated tocreating an individualized health careexperience in which genomic data are a routine part of patient care. The Division supports physicians andscientists across the MountSinai Health System to bring genomics into all aspects of medicine.

Michael Murray, MD Professor of Medicine

Mount Sinai's Division of Genomic Medicine has a goal as ambitious as it is sweeping: to make genomic medicine a routine partof patient care for the diagnosis, treatment, and prevention of all types of disease.
The Icahn School of Medicine at Mount Sinai has long been a pioneer in genetics, starting withthe establishment of BioMe, one of the country’s first medical record-linked biobanking programs in 2006, andcontinuing with the recently announced Mount Sinai Million Health Discoveries Program to genetically sequence 1million Mount Sinai patients within the next five years.
The Department ofMedicine’s newest entity, the Division of Genomic Medicine, builds on that work with a goal as ambitious as it is sweeping: tomake genomic medicine a routine part of patient carefor the diagnosis, treatment, and prevention of all types of disease.
“Genomics provides extremely rich data about an individual’s risk for diseaseover the course of their entire life, and we want to deliver on its enormous promise by integrating it into health care decisions that result in the most effective management of our patients,” says Eimear Kenny, PhD, Mount Sinai Professor ofGenomic Medicine. “That involves working closely with our primary and specialty care physicians toempower them with the knowledge and toolsthey need tointerpret genetic findings, recognize genomic risk, and use those insights to respond to each patient’s unique health careneeds.”
That effort is well underway through patientcentered clinical applications, collaborative research, and innovativeeducation and training programs. The Division’s Genomic HealthClinic, for example, is among the first of its type to engage directly with individuals seeking one-onone genomic risk evaluation and testing from an experienced medical geneticist-genetic counseling team (see our accompanying article on the Genomic Health Clinic).
In the field of research, the Division of Genomic Medicine partners with Mount Sinai's Institute for Genomic Health to conduct cutting-edge work “to bring genomic information into the clinic for everyday health care, and not just for some of the specialty areas where it currently fits,”
according to Dr. Kenny, who is Founding Director of the Institute.
A current clinical trial, forexample, is investigating the use of polygenic risk scores—which aggregate information spanning the entiregenome—to provide individuals fromdiverse populations with precision reports ontheir risk exposureto common diseases. For this study and others, the computation-driven Institute relies heavily on artificial intelligence and machine learning to scale up its research.
We are building programs to turn genomic results from the Discoveries Program when they are medically actionable into follow-up care designed to benefit our patients.
— Eimear Kenny, PhD
In education and training, the Division is one of the first to create a Genomic Medicine Training Track for residents, fellows, and interns interested in gaining a deeper knowledge of genomics and its applications within clinical care, especially ordering and interpreting genetic tests. The online curriculum, now in its third year with six participants, will receive National Institutes of Health support to carry out the next phase of its growth.
The Division’s influence is already being felt across Mount Sinai through its screening programs for a variety ofhereditary diseases. It has teamed up with Amy Kontorovich, MD, PhD, Director of the Center for Inherited Cardiovascular Disease, for instance,totest individuals for amyloidosis, a multisystemic disorder caused by a mutation in the transthyretin (TTR) gene. Amyloidosis manifests as cardiovascularneurological-musculoskeletal symptoms, and African Americanand African populations are
at higher risk for it.“We’ve successfully tested for this condition in patients enrolled in theMount Sinai BioMe Biobank and referred those who may have apredisposition to ourHigh-Risk Amyloidosis Clinic for professional care,” notes Dr. Kenny.
Similarly, the Division is leveraging the Health System’s massive bio repository to identify mutations in the breast and ovarian cancer susceptibility genes BRCA1 and BRCA2
As a result of this growing screening initiative, numerous patients have been referred for follow-up care to oncologists and other health specialists at Mount Sinai.
No project promises more profound results, however, than the Mount Sinai Million Health Discoveries Program, which will sequence and analyze the DNA of a million participating patients, the largest effort of its type ever undertaken by a health system. This trove of data will enable researchers to assess the true potential of genetics-based precision medicine approaches to guide everyday patient care.
The Division of Genomic Medicine is an important partner in this endeavor.
“We arebuilding programs to turngenomic results from the Discoveries Program when they are medically actionable into follow-up care designed
to benefit our patients,” says Dr. Kenny. “Weare committed to being a leader in the creative useof this data, and that takes on added significance given the fact Mount Sinai treats one of themost diverse patient populations, withties to more than 160 countries around the world.”


Kenny,PhD
MountSinai Professor of Genomic Health
AmyKontorovich, MD,PhD
Associate Professor of Medicine (Cardiology, and Medical Genomics)

Mount Sinai's Genomic Health Clinic—the only advanced service of its type in New York City and one of a handful in the country—is emerging as a vital ally to people who hope to understand the risks to themselves and familymembers from information embedded in their genomes.
As genetictesting moves beyond the realm of raredisease to mainstream disorders suchas cardiovascular disease and cancer, theDivision of Genomic Medicine’s GenomicHealth Clinic is emerging as avital ally to people who hope to understand the risks to themselves and family members from information embedded in their genome.
The only advanced service of its type in New York City and one of a handfulin the country, the Clinic connects patients with a highly skilled medical geneticist-genetic counselor team toidentify potential health hazards. If a geneticrisk is found, the team refersthe individual to appropriate physicians within the Mount Sinai Health System for monitoring or treatment before it becomes a serious issue.
Patients havetraditionally been referredfor a genetic evaluation whenthey havea strong personal or family history of certain diseases. But with genetic testing nowwidely accessible through direct-to-consumer products such as 23andMe and others, more peoplecan potentially benefit from a thoughtful analysis of their screening results or consideration of proactive genetic testing by genetic experts.
“We’re trying to help people recognize theremay be subtleclues in their family history that help explain many common diseases from a hereditary standpoint,” says Emily Soper, MS, Instructor in Medicine at the Icahn School of Medicine at Mount Sinai and a geneticcounselor at theGenomic Health Clinic. “That levelof information cantruly empower them to be much more proactive about their health—and not waitfor problems to develop beforethey take action.”
Launched in 2020, the Clinic currently sees four to six new patients a week, though that number is poised to grow exponentially as genetic screening becomes more deeply woven into the fabric of routine health care. As the Clinic’s medical geneticist, Ayuko Iverson, MD, points out, the opportunities to address potentially troublesome conditions are as unlimited as the human genome itself.
“Weoften get referrals for people witha family history of thrombophilia; various cancers such as breast, pancreatic, and colon; and Alzheimer’s disease or dementia,” says Dr. Iverson, Assistant Professor of Medicine, and Genetics andGenomic Sciences, at Icahn Mount Sinai. “But there are genes that play a role in developing common

diseases that weknow aretreatable or even preventable if caught early enough.”
The U.S. Centers for Disease Control and Prevention, for example, has identified three Tier 1 conditions associatedwith high genomic risk in 1 of every 75people, though as many as 90 percent are unawareofthe potentialthreat.
Those conditions are hereditary breast and ovarian cancer, Lynchsyndrome, and familial hypercholesterolemia. “Each of these conditions is actionable,” notes Dr. Iverson, “and if we detect any of them through genetic screening thereare specific care management and surveillance guidelines that can be implemented.”
A visit to the Genomic Health Clinic typically begins with a review of the individual’s personal and family health historygoing back three or four generations, anda physical examination. Based on this evaluation, the genomics team then discusses genetic testingoptions withthe patient —including any medically indicated tests as well as proactive screening—and what potential implications of testing should be considered. For patients seeking a better understanding of their responseto certain medications, a pharmacist also reviewsthe patient's medication history and discusses pharmacogenetic testing to evaluate how their genes affect the body’s metabolism of medications. If thepatient opts to proceed, ablood or salivasample is taken and sent to a clinical testing laboratory for analysis. A second visit is then scheduled at which the patient receives the results along with counseling and, when appropriate, referrals tospecialists such as a hematologist, cardiologist, endocrinologist, or oncologist. Other times, the genomic specialists may simply suggest that the patient confer with their primary care doctor.
Indeed, the Genomic Health Clinic is looking to expand its relationship with primary care practices within Mount Sinai, knowing they represent a major channel for preventive care and referrals. Other patients find theirway to the Clinic through web searches.
“People often come in after having done a directto-consumer or commercial self-driven genomic test and want to know what it means for their health care,” explains Ms. Soper. “We’re ableto interpret the datafor them in terms of risk tonot justthemselves but their family. Manytimes, the greatest benefit we provide patients is just being able to walk them through the results and reassurethem that something found in their test is not as worrisomeas they hadthought.”


AyukoIverson,MD
Assistant Professorof Genetics and Genomic Sciences, and Medicine (General Internal Medicine, and Medical Genomics)
EmilySoper,MS
Instructor of Medicine (Medical Genomics))

The Division of Hematology and Medical Oncology has experienced tremendous growth over the past several years, while also staying true to its dual mission of delivering the best, most compassionate care to patients and pursuing excellence in research and training.
The Division, as an integral component of The Tisch Cancer Institute at Mount Sinai, builds on a long history of excellence in hematology and hematological malignancies, as well as solid tumor oncology.
Through clinical and research collaborations, the Division is committed toproviding patients with the most advanced therapies, including access to revolutionary clinical trials.

Joseph A.Sparano, MD
EzraM. Greenspan, M.D. Professor in Clinical Cancer Therapeutics
The National Cancer Institute has again renewed its support for theMount Sinai-led Myeloproliferative Neoplasm Research Consortium, which is making progress on treatments for adult leukemias and myeloproliferative neoplasms.
Through its work advancing bold therapeutic solutions to a complex range of adult leukemias and myeloproliferativeneoplasms (MPNs) that compromise the lives of millions of patients,a 15member team of investigators fromMountSinai’s Department of Medicine continues to burnish its international credentials.
Reinforcing that reputation was the recent renewal for the fourth time of a National Cancer Institute (NCI)-funded grant supporting the Mount Sinai-led Myeloproliferative Neoplasm Research Consortium (MPN-RC), a unique group of translational researchers from 13 institutions across North America that has driven innovative clinical trials for such breakthroughs as Janus kinase 2 (JAK2) inhibitors for treating myelofibrosis, and restoring the tumor suppression activity of the TP53 gene, which encodes the p53 protein, through smallmolecule inhibitors of the MDM2 protein.
The focus of the renewed NCI grant, which originated in 2006, is to improve themedian sixyear survival rate of individuals with myelofibrosis, a chronic leukemia characterized by excessive production of inflammatory cytokines. Under the leadership of Principal Investigator Ronald Hoffman, MD, Albert A. and VeraG. List Professor of Medicine (Hematology) and Director of the Myeloproliferative Disorders Research Program at the Icahn School of Medicine at MountSinai, scientists areattempting to deplete the poolof cancer stem cells by targeting malignant hematopoieticstemcells and reversingtheir tumor-promoting microenvironment.
“Our combination laboratory-clinical team is trying to effectively eliminate themalignant stem cell from which the diseaseis derived and, ultimately, change thenaturalcourse of lethal blood cancers,” says John Mascarenhas,MD, Professor of Medicine (Hematology and Medical Oncology) at Icahn Mount Sinai, and Director of the Adult Leukemia Program andof the Centerof Excellence for Blood Cancers andMyeloid Disorders. As evidence of that dogged scientific pursuit he points to the team’s rational approaches
to silence such cytokines as IL-1and IL-8, which are pathologically overexpressed in myelofibrosis, with canakinumab and reparixin, respectively.
If we’re going to changethe trajectory of acuteleukemia and myeloid disease, we need to train and promote the next generation of clinical and laboratory scholars.
— John Mascarenhas,
MD
Just as importantly, MPN researchers have built on Dr. Hoffman’s considerable body of work over the years by activating the p53 pathway. These prior studies led to the observation that MDM2, a negative regulator of p53, is highly expressed in the CD34+ cells of patients with myeloproliferative neoplasms, and that it could be targeted by small-molecule antagonists known as nutlins, which occupy the p53 binding pocket of MDM2. From this seminal work has emerged a number of phase 3 registration trials for similar class compounds, as well as the development of cutting-edge combination approaches with BET protein inhibitors designed to dampen the myelofibrosis environment, which are poised to move from laboratory to the clinic. AnotherwayMountSinairesearchersaretaking combinationtherapytonewlevelsis throughthe developmentof targetedproteindegraders, which havebecomeoneofthehottestfieldsofcancer drugdiscoveryinrecentyears.PartneringwithJian Jin,PhD,Mount SinaiProfessor inTherapeutics DiscoveryandDirectoroftheMountSinaiCenter forTherapeuticsDiscovery,myeloidresearchers havedevelopedMDM2andPPM1Dprotein degradersthat arepartofanewtherapeutic class knownasproteolysis-targetingchimeras (PROTACs).Dr.Jin’spioneeringworkwith PROTACshascreatednumerousdegradersof a widerangeof oncogenicproteins,includingsome consideredundruggablefordecades.Thehopeis
that ongoinglaboratoryevaluationandagent optimizationwillsoonleadtoclinicaltestingin patientswithbloodcancers.
Among the most recent pivotal trials from the MPN/leukemia research program were those leading to approval of the JAK2 inhibitor pacritinib for patients with myelofibrosis and thrombocytopenia. “Previously these patients had an extremely poor prognosis,” explains Dr. Mascarenhas, who was lead investigator for the agent’s phase 3 registration trial. “The results of our PERSIST-2 study provided for the first time a promising therapeutic option for patients who are ineligible due to low platelets, or have failed therapy with the JAK1-JAK2 inhibitor ruxolitinib.”
Amid its flurry of past and current clinical work to arrest deadly blood cancers, Mount Sinai is also eagerly looking tothe future.
“If we’regoing tochange the trajectory of acute leukemia and myeloid disease, we need to train and promote the next generation of clinical and laboratory scholars,” Dr. Mascarenhas says. “For that reason, we’reparticularly proud of our talented team of junior faculty and fellows who have been awarded grants by the American Society of Hematology and Leukemia and LymphomaSociety to push the research envelope, and to hopefully develop curative approaches inour lifetime.”


RonaldHoffman,MD
Albert A. and VeraG. List Professor of Medicine (Hematology)
JohnMascarenhas, MD
Professor of Medicine (Hematology and Medical Oncology)
JianJin,PhD
MountSinai Professor in Therapeutics Discovery

Standard treatment for muscle-invasivebladder cancer involves surgical removal of the bladder. Through a multitude of first-ever clinical trials, Mount Sinai scientists are deploying cutting-edge immunotherapeutic approaches to help patients avoid this life-changing operation and improve the length and quality of their lives.
Few research centers have done more over the past decade to dissect the biology and mechanisms of bladder cancer, along with their response and resistance to modern-day therapies, than the Icahn School of Medicine at Mount Sinai. Through a multitude of first-ever clinical trials, scientists are deploying cuttingedge immunotherapeutic approaches to not just improve the length and quality of life for patients but potentially cure a disease that accounts for more than 70,000 new cases and approximately 15,000 deaths each year in the United States.
Here are three majorareas of investigationthat encapsulate that targeted effort:
Standardtreatment for muscle-invasive bladder cancer involves surgical removal of the bladder, a life-changing operation. At the same time, when chemotherapy is given to these patients prior to bladder removal, about 30 percent show no residual traces of the tumor. This has created a dilemma for doctors since there is no way of knowing which patients have achieved a complete pathological response until after the bladder has been removed and analyzed under the microscope.
“We realized what a game changer it could be if wewere ableto combine immunotherapy with chemotherapy and identify through a battery of tests if acomplete response had occurred without removal of the bladder,” says MatthewGalsky, MD, Professor of Medicine (Hematology and Medical Oncology), and Urology, at Icahn Mount Sinai, and Co-Director of the Center of Excellence for Bladder Cancer at The Tisch Cancer Institute
“We could potentially treat patients curatively with chemotherapy plus immunotherapy and prevent them from losing their bladders.”
From that manifest need emerged the country’s first clinical trial, led by Dr. Galsky, to integrate chemotherapy and immunotherapy to advance a
bold new personalized medicine approach to bladder-sparing. After four cycles of chemotherapy, participants underwent a thorough assessment, and if their biopsy showed the cancer had been eradicated, they were offered immunotherapy alone—and spared bladder removal.
“Theresultswereveryencouragingfor patients,” Dr.Galskyreports, notingthattheyshoweda completeclinicalresponsein43percentof patients, andthat amongpatients whodidnot have surgerytoremovetheirbladders, approximately two-thirds showednosignsofrecurrencetwoor moreyearslater.“We’renowanalyzingbloodand tumorsamplestodevelopbiomarkersthatcouldbe usedtoidentifypatientswhocouldbenefit most fromthisbladder-sparingapproach, andhave hopesit couldeventually becomepart ofour standardtreatment.”
We could potentially treat patients curatively with chemotherapy plus immunotherapy and prevent them from losing their bladders.
— Matthew Galsky, MD
While immunecheckpoint inhibitors have transformed the treatment landscape for bladder cancer, only asubset of patients respond wellto this approach. Earlier research by Dr. Galsky and Nina Bhardwaj,MD, PhD, Ward-Coleman Chairin Cancer Research at Icahn Mount Sinai and a renowned immunology expert, revealed that macrophages play a pivotal role inthe resistance of bladder cancer patients to immunotherapy, suppressing the body’s natural defenses. Moreover, they believed that a specific protein was the source of the problem and that blocking it
with an existing immunotherapeutic agent could potentially overcome resistance.
The two scientists are now testing that hypothesis through a unique clinical trial combining drugs to target thesemacrophages in combination with immunotherapy. “This project will reveal important information about how immunotherapy interfaces with bladder cancer, and why the diseasein certain patients might resist treatment,” says Dr. Galsky. “Thisknowledge could then inform new treatment combinations that could render immune checkpoint inhibitors effective for greater numbers of patients.”
Havingalreadyestablishedthrough groundbreakingresearchthebenefitsof immunotherapyafter bladder cancersurgery, Dr. Galskyisnowinvestigatingtheuseofabiomarker knownascirculatingtumorDNA(ctDNA)to determinewhichpatients arelikelytorealizethe greatest gains.ctDNArefers tosmallfragmentsof DNAthat cancer cells releaseintothebloodstream, andcanbedetectedthroughbloodtests thatare usefulfordiagnosis,monitoring, andtreatment.
Dr. Galsky and his team are launching a phase 3 clinical trial, supported by the National Cancer Institute,that will enroll 1,200 patients nationally to undergo ctDNA testing after cystectomy. Those with detectable ctDNA willbe randomized to receive a single immunotherapeutic drug or a combination of drugs.
“In the absenceof any tests to detect micrometastatic cancer,we’ve treated all patients after surgery with systemic (also knownas adjuvant) therapy despite the fact that only a subset harbor the disease,” Dr.Galsky explains. “Findings from our study have thepotential to establish a ctDNA-based approach that could remove the guesswork from that process. And that would be a major step forward for patients with muscle-invasive bladder cancer.”


MatthewGalsky,MD
Professor of Medicine (Hematology and Medical Oncology), and Urology
NinaBhardwaj, MD,PhD
WardColeman Chairin Cancer Research

The Division of HospitalMedicine at the Icahn School of Medicine at Mount Sinai is a dynamic, innovative, andpatient-centered team dedicated to delivering exceptional care, advancing medical education, and driving groundbreaking research. Our hospitalists are at the forefront of transforming health caredelivery and providing comprehensive inpatient care across a wide range of specialized services. As leaders in medical education, weare passionate about nurturing the next generation of health careprofessionals. Our faculty hold key leadership positions throughout the medical school and are actively involved in shaping the curriculum at every level. Weoffer unparalleled mentorship and career development opportunities, equipping our trainees and faculty with the skills and knowledge needed to becometomorrow's health careleaders.
Our commitment to continuous improvement is evident in our robust quality and patient safety initiatives, which havegarnerednational recognition and prestigious awards. Through our multidisciplinary approach and innovative programs, we are constantly pushing the
boundaries to enhance patient outcomes and experiences. The Division of Hospital Medicine is also at the forefront of research.Our research spans a wide range of areas, from clinical care and health care delivery models to high-value care; humanism; diversity, equity, and inclusion; and medical education.
As we continue to expand our innovative care models, strengthen our educational programs, and deepen our research endeavors, we remain dedicated to advancing the field of hospital medicine.

Andrew S. Dunn, MD Professor of Medicine (Hospital Medicine)

The Department of Medicine’sStudent High Value Care Initiative enables around 20 medical, master’s, and nursingstudents to team up each year with a junior faculty member to create, implement, and monitor projects designed to improve patient care. Students learn the fundamentals of high-value care and design an improvement project during a sixmonth curriculum.
As if the first year of medical school isn’t hectic enough, a smallgroup of students is further enriching its learning experience through a unique program that’s improving the quality and cost of health care, at Mount Sinai and even beyond.
They are part of the Department of Medicine’s Student High Value Care Initiative, which enables around 20 trainees, including master’s and nursing students as well as those in the MD program, to team up each year with a junior faculty member to create, implement, and monitor projects designed to improve patient care. Some of these efforts gain national exposure through well-attended conferences and publication in academic journals.
“Educating trainees to practice high-value care is now recognized as critical to systemwide change,” says Anne Linker,MD, Assistant Professor of Medicine (HospitalMedicine) at theIcahn School of Medicine at Mount Sinai, and Co-Director of the Student High Value CareInitiative. “Our program gives students the chance tosee the health system as something that ischangeable and open to improvement, and ourhope is they’ll carry that
valuable lesson to theremainder of their training and, eventually, into their clinical careers.”
Aspartoftheeight-year-oldprogram, students learnthefundamentals of high-valuecare(HVC) anddesignanimprovementprojectduringasixmonthcurriculum ledby Dr. LinkerandCo-Director ReemAoun, MD, Assistant ProfessorofMedicine (HospitalMedicine)at IcahnMount Sinai.This introductionisfollowedby sixmonthsof implementationinwhich studentsaredividedinto teamsandcollaboratewithafacultymember, who mayalsoserveasamentor, astheyjointlypursue anHVCproject. Past andfutureinitiativeshave includedinterventionstoreduceunnecessary diagnostictests,mobilize patientsinwaysthat reducefallsandinjury, anddecreaseoveruseof continuousintravenousfluids.
Thesuccess of theseeffortsisreflectedinthe steadygrowthoftheStudentHighValueCare Initiative. “It’saninterestingprogramthathas grownorganicallyovertime, driveninlargepart by therealizationthatwecouldbeeffectiveinareas outsidejust hospitalmedicine,”explainsDr. Linker, whohasledavariety of projectstoimprovethe valueandqualityofpatient careatTheMountSinai

Hospital.“That mindset hasledustocreate partnershipswithothergroups, including EmergencyMedicine,ObstetricsandGynecology, InfectiousDisease,andPrimaryCare.”
One way the program gets achanceto truly shine is through its annual“Pitch Day.” This event, held in early December, allows each team to present its project in a“Shark Tank”-like setting to fellow medical students, residents, faculty, and hospital leaders. In the audienceare four judges who provide valuable feedback on project planning and implementationstrategy.
“It’s really exciting to see the enthusiasm and positivity this course generates,” notes Dr. Aoun, who was a project mentor before becoming Co-Director last year. She underscores how the initiative has grown in influence and visibility by citing Andrew Dunn, MD, Chief of the Division of Hospital Medicine, who has called it “one of the most important programs in our division.”
Oneexampleof thehigh-valuecareprojects that havewoncriticalpraiseisasleephygiene interventiontoimprovesleepqualityfor hospitalizedpatients.Awareofhowpoorsleepcan contributetoadversehealthoutcomes,first-year medicalstudentsdevelopedanonpharmacologic hygieneprotocolthatincludedoptionssuchas turninglightsoff, eyemasks,earplugs, lavenderscentedpads, andrelaxingmusic,allexplainedto thepatientusingastructuredscript. Front-line championswerealsoidentifiedtoaidwith implementation.Asdescribedin The Joint Commission Journal on Quality and Patient Safety, theteam’s studyof931patientsreportedimproved sleepdepth,decreasedawakeningsafter sleep onset, andenhancedquietat night.
Another study in the same journal outlined a program initiated by first-year students to improve physician adherence to prescribing guidelines for patients dischargedon opioids. During biweekly sessions held inresident lounges over donuts and coffee, the students opened a dialogue with physicians around best-practicerecommendations
from the Society of Hospital Medicine and the Centers for Disease Control and Prevention. Favorable outcomes from the program included a reduction inopioid prescriptions longer than seven days, increases in post-discharge appointments, and documentation of opioid prescription histories.
“We’re proud of how students have repeatedly used their creativity and innovation tobenefit the quality of care for our patients,” emphasizes Dr. Linker. “Wetypically launch three new projects a year, and the fact somany have achieved statistically significant results speaks volumes about the ongoing success of the Student High Value Care Initiative.”



AnneLinker,MD
Assistant Professor of Medicine (Hospital Medicine)
ReemAoun,MD
Assistant Professor of Medicine (Hospital Medicine)
AndrewDunn,MD
Professor of Medicine (Hospital Medicine); Chief, Division of Hospital Medicine


Many hospital at home programs now sprouting across the country have drawn from the model Mount Sinai established in 2014. Mount Sinai, meanwhile, continues to differentiate itself through its high standardof care and the breadth and depth of its at-home services.
For agrowing number of Mount Sinai patients, acute hospital care has taken on allthe comforts of home. That’s becausemany of the staples of inpatient care—from imaging and intravenous medications to regular bedside monitoring by nurses anddaily management by physicians— have been forwarded to their homes throughthe Mount Sinai Hospital atHome program.
Whilehospitalization at home has lately become a national movement, Mount Sinai can trace its roots to a Centers for Medicare and Medicaid Services (CMS)Innovation grant in 2014 to study the effectiveness of providing acute hospital care
Medicine (Hospital Medicine) at the Icahn School of Medicine at Mount Sinai. “At the same time, we’re creating a continuum of home care by recently launching Rehabilitation at Home, in addition to offering Palliative Care at Home. We’ve also built into that platform Community Paramedicine, Home Infusion, and Home Health to afford patients seamless transitions along their medical journey.”
MountSinai Hospital at Home, the largest of those complementary initiatives, plans to begin admitting between 50 and 60new patients amonth this year, roughly doubling its current monthly census


in the home. Based on that seminal work, Mount Sinai established itself as the pioneer in the field; many programs now sprouting across the country have drawnfrom the Mount Sinai model, which continues to differentiate itself through its high standardof care and thebreadth and depth of its at-home services.
“We’re committed to delivering quality services where patients most want to receive them, and that often means right in their homes,” says Tuyet-Trinh Truong, MD, Chief Medical Officer of Mount Sinai at Home and Associate Professor of
of about 30 patients. Referralsfrom the case managers, socialworkers, physicians, nurses, and other providers in the hospital setting are helping to drive that growth, as wellas the satisfaction of patients andfamilies who have experienced its level of carefirst-hand.
To be eligible, participants must demonstrate an inpatient-level need, live in New York City (except for Staten Island), and have an insurance plan with Healthfirst, Aetna, Empire, or Fee-forService Medicare if they wish to be admitted to Hospital at Home directly from an emergency
room. If the patient has been in the hospital for more than 48 hours, all insurance plans are accepted by the program.
“Wehaveateamof acute-carenurseswhovisit the patientintheir hometwiceadayand, dependingon theillness,areabletodrawblood;givediuretics, antibiotics,orotherIVmedications;administer respiratorytreatment,andmuchmore,”explains JoannaMecca,MD,MedicalDirectorof Hospitalat HomeandAssistant ProfessorofMedicine (HospitalMedicine)atIcahnMountSinai. “Patients canalsoaccess ourteamof physiciansandnurse practitionersaroundtheclockthroughourvirtual carecommandcenter.” Oneof thefeaturesofthat telemedicinecapability,shepointsout,isanaudioenhancedstethoscopethat allows cliniciansto remotelyhear heart andlungsounds asrecorded bynursesatthepatient’sbedside.
For oneelderlypatient whoexperiencedastroke andwasdoingpoorlyinthehospital, Mount Sinai’s home-basedprogram translatedintorapidresults. Surroundednowbyfamily,home-cookedmeals, and24/7professionalcare,thepatient’sappetite andalertnessreturnedandpreviousdiscussions abouttheuseofafeedingtubeorevenhospice carewerenolongerneeded. HospitalatHomealso provedablessingtoa40-year-oldwomanwho enteredtheemergencyroom withaseverekidney infection. Becauseshehadaschool-agesonand nofamilyorfriendstocarefor him,sherequested theinterventionof HospitalatHomeandwasable toreceivetheintensecare, includingintravenous fluidandantibiotics, sherequired.
“TherearemanydriversofHospitalatHome, but theonewe’reproudestofiskeepingpatientsout of thehospitalwhileachievinghealthoutcomesthat areasgoodif not betterthanthosepossiblewithan inpatientstay,”emphasizes AndrewDunn,MD, SystemChiefofHospitalMedicineandProfessor of MedicineatIcahnMountSinai.Indeed,arecent studyin Journal of the American Geriatric Society showedthat MedicaidpatientsenrolledinHospital atHomeexperiencedbetter outcomesthanthose
inthetraditionalhospitalsetting, withhospital readmissionsdownbyhalf andreturnvisitstothe emergencyroomlowerbytwo-thirds.
Satisfactionlevelsareas highamongthe program’snursesandcliniciansastheyarefor patients andtheirfamilies.
“Thepandemicforcedalotofpeopleinourfieldto reassesstheircareers,”saysDr.Truong,“andthey havesincegravitatedtohomehospitalization becauseitallowsthemtodeliverthehighest level of one-on-onepatientcarewithout feelingrushed or burnedout.”



Tuyet-TrinhTruong, MD
Associate Professor of Medicine (Hospital Medicine)
JoannaMecca,MD
Assistant Professor of Medicine (Hospital Medicine)
AndrewDunn,MD
Professor of Medicine (Hospital Medicine); Chief, Division of Hospital Medicine

The Division of Infectious Diseases within the Department of Medicine at the Icahn School of Medicine at Mount Sinai is a hub of innovation and expertise in combating infectious threats. We blend research, education, and patient care to address the complex challenges posed by various pathogens. Our Division specializes in preventing and treating infections, with particular emphasis on healthcare-associated infections, antimicrobial stewardship, and care for immunocompromised patients. By integrating diverse disciplines, we've cultivated a unique environment that fosters pioneering research and comprehensive care, positioning us to tackle both current and emerging infectious disease challenges.
Our team leads the charge in implementing evidence-based interventions to prevent healthcare-associated infections across the Mount Sinai Health System. We conduct surveillance of infections and multidrug-resistant organisms, create policies to prevent healthcareassociated infections, investigate outbreaks, and spearhead interventions to reduce the use of invasive devices. Wealso maintain educational
programs for healthcare workers and adviseon regulatory requirements,allwhile upholding health equity in our analyses and interventions.
Our strengths arefurther exemplified by our Antimicrobial Stewardship Program, established in 2004 and recognized as a Center of Excellence by the Infectious Diseases Society of America. This program—co-led by the Division’s physicians and clinical pharmacists—offers clinical consultations, leads research to advance the field, and provides specialized training opportunities for fellows interested inthis subspecialty. Additionally, faculty in our Transplant Infectious Diseases Program provide specialized care for immunocompromised patients, including solid organ transplant recipients and patients with hematologic malignancies. Lastly, ID fellows interested in further training in the immunocompromised host can complete a transplant ID track in their second year of fellowship.

Judith A. Aberg, MD
Dr. George Baehr Professor of Clinical Medicine

Liver, kidney, heart, lung, intestinal, pancreas, and bone marrow transplantation areall available at Mount Sinai, and the TransplantInfectious Diseases Program is an integral partof each. Theprogram includes three inpatient consultservices, an expanding ambulatory footprint, and a streamlined fellowshipprogram.
The Mount Sinai Hospital’s Transplant Infectious Diseases (ID) Program, already one of the nation’s largest with eight clinical faculty members, is building on its success with a streamlined fellowship track as well as a significant expansion in transplant ID clinical teams and services.
“What we do is prevent, manage, and treat infections inthe immunocompromised host— wehave special expertise in taking care of that particular patient population,” saysMeenakshi M. Rana, MD, the Program’s Director and an Associate Professor of Medicine (Infectious Diseases) at the Icahn School of Medicine at Mount Sinai
awaiting abdominal organ transplants at the Recanati/Miller TransplantationInstitute
TheimportanceoftransplantIDinthepre-evaluation andclearanceofpotentialtransplantpatientsisvital, asisthecaretheyprovideshouldinfectious complicationsensuefollowingtransplantation.
"Prevention of infection is a particular focus of ours,” Dr. Rana says. “We recommend vaccines, and any history of infections the patient may have had prior to transplant is reviewed. The most common viral infection we see after transplant is cytomegalovirus, so patients are onprophylaxis for several months after transplant to prevent this.”
Liver, kidney, heart, lung, intestinal, pancreas, and bone marrowtransplantation areall available at Mount Sinai. Dr. Rana and colleagues work as an integral part of the multidisciplinary team involved with any such transplant, seeing patients awaiting lung transplantation at the Mount Sinai – National Jewish Health Respiratory Institute and those
Thegrowingservicenowincludesthreeinpatient consultservicesdedicatedtotransplant ID. Thetransplant IDteam alsohasexpandedits outpatientambulatorycare, Dr.Ranasays:“We provideambulatory care, co-locatedwiththeir underlyingcondition, andweseepatientsinthe generalIDclinic.”
Mount Sinai is one of a select group of transplant centers approved for HOPE Act participation. The HIV Organ Policy Equity Act, enacted in 2013, approved research on organ transplantation between donors and recipients with HIV. The HOPE Act answered a need within the transplant community.
“Patients with HIV are vulnerable to long-term complications of kidneydisease and liver disease,” Dr. Rana explains. “For patients with HIV, who generally had longer wait times for transplant, they now had the opportunity to be on two lists: the one with everyone else waiting for a transplant, and a second list for thosegetting a transplant from a donorwith HIV—and that helps shortentheir wait timefor transplant.”For example, the wait time inNewYork City might be halved for a kidney from adonor with HIV.
“The HOPE Act allowed us to start doing HIV-toHIV transplantation in this country, and we have been doing that here as part of clinical research since 2016,” Dr. Rana says. “Wehavedone 126 of these transplants at Mount Sinai, making us one of the largest HIV-to-HIVtransplant centers in the country.”
Generally, thedonor with HIV is deceased, though living donors with HIV are possible in HIV-to-HIV kidney transplantation. The research program at Mount Sinai also includes deceased-donor HIV-toHIV liver transplantation. All recipients are on retroviral therapy and have well-controlled HIV with a suppressed viral load. “Wehave had good outcomes in this patient population,” Dr.Rana says. “Even though these patients have receiveda kidney or liver from adonor with HIV, theirHIVstill stays under good controlas long as they continue to take their antiretroviral therapy.”
With the large andgrowing transplant IDprogram coupled with the research stemming from the HOPE Act, there is an outstanding opportunity to educate IDfellows at Mount Sinai. The transplant ID team has created an innovative program witha curriculum that folds transplant ID training into its second year, rather thanrequiring athirdyear, which is often the case elsewhere.
“Fellows who complete the first year of fellowship who have a special interest in pursuing additional training in care of the immunocompromised host can go on to do extra training during their second year of fellowship, and this involves a few components,” Dr. Rana says. “There’s about four months of extra clinical time on the inpatient side, and then there is also an ambulatory component where they take care of patients in the outpatient transplant ID setting.
“They conduct a research project on infectious disease under the mentorship of a transplant ID faculty member as part of thetrack,” she says, adding, “Many of our fellows who havecompleted the track havebeen ableto go on and obtain transplant IDfaculty positions at other institutions.” The explicit purpose of the IDfellowship program is to“educate future academic leaders in our field,” and all evidence points tocontinued success withthis goal.
MeenakshiM.Rana, MD
Associate Professor of Medicine (Infectious Diseases)

Mount Sinai scientists are pursuing tworelated lines of research into the fundamental physiology of HIV: trying to understand how the major protein on the surface of the virus enables it to spread fromcell to cell, and whether the human immune system can be stimulated to create antibodies against it.
Approximately 40 million people in the world are HIV-positive, and though antiretroviral medications suppress viral replication and are clinically effective, not everyone can get or afford them. So long as the virus is out there unchecked, HIV remains a threat.
To address that threat, researchers at theIcahn School of Medicine at Mount Sinai are exploring everythingfrom HIV cellular physiology to translational clinical strategies.
by engineering either fluorescent viruses or viruses that turn on genetic switches.”
Bioengineered viruses that carry fluorescent proteins can be used to visualize cell-cell interactions that support HIV infection. This live imaging technique has revealed that when HIVinfected cells are co-cultured with uninfected cells, durable cell-cell interactions form adhesive contacts, called virological synapses, which in turn promote immune evasion. Dr. Chen and
The laboratory of Benjamin K.Chen, MD, PhD, Irene and Dr. Arthur M. Fishberg Professor of Medicine and Vice Chairfor Research in the Department of Medicine at Icahn Mount Sinai, has been focused on the pathogenesis of human immunodeficiency virus type 1 (HIV-1) infection, including a deep dive into cell-cell interactions.
“Cell-cell interactions are very important in how they allow HIV to spreadefficiently,” explains Dr. Chen, who is also a Professor of Microbiology, and Pharmacological Sciences. “We havebeen developing models toobserve and accurately measure different steps in thelifecycle of the virus
co-authors have explained howthe dynamic movements of the HIV Env protein support virological synapse formation in a study published in Viruses, and an emerging view of how these cell-cell infections affect the Env on the surface of cells and allow the virus to evade immune responses, published in mBio
“This approach has helped us understand how the virus spreads and how it evades immune responses,”Dr. Chen notes. “We have been focused ontrying to understand how the major proteinon thesurface of the virus, the envelope glycoprotein—which is also the maintarget of vaccines—enables it tospread from cellto cell,
and how itis different onthe surfaceof cells than it is on thesurface of viruses.”
An active area of HIVresearch has focused on stimulating a patient’s own immune systemto recognize and eliminate cells that areinfected with the virus. This line ofinquiry was prompted by the identification of individual antibodies isolatedfrom patients that can neutralize a variety of different HIV strains, so-called broadly neutralizing antibodies (bNAbs). These bNAbs are being tested clinically as a new immune-modulating therapeutic strategy.Thus far, however, this strategy by itself has notbeen shown to be capable of suppressing the virus in the longterm. In addition, which patients with HIV should be given which bNAb or bNAb combinations has yet to be elucidated.
Dr. Chen and his lab have recently received a National Institutes of Health grant to develop assays to test the sensitivity of HIV to bNAbs. “We have foundthat bNAbs arereally potent blockers of HIV infection,” Dr. Chen says. “These aremuch better at blocking cell-free virus infections than they are at blocking at the virological synapse. We are trying to better definethis and use it as a clue to identify antigens or vaccines that would block cell-cellinfections andcell-free virus infections.”
TheworkonvirologicalsynapsesandbNAbsbyDr. Chenandhislabcolleagueshasinformedthefight fornewdrugsandvaccinesagainstHIVinfection.
That fight has been taken up by, amongothers, FrancescaCossarini, MD, an Assistant Professor of Medicine (Infectious Diseases) at IcahnMount Sinai and an Infectious Diseases attending physician at TheMountSinai Hospital. As Dr. Chen explains, “Our research relates to Dr. Cossarini’s clinical trials, because these same bNAbs are beingtested as drugs to help recruit
the immune system to clean up infected cells in ways that the normalimmune responsecannot.”
Dr. Cossarini notes thatin the controlled phase of HIV infection, even as patients take antiretroviral therapy, the virus hides, persisting in long-lived immunecell subsets called the viralreservoir. “I have focused on thegastrointestinal (GI) tract, which is the major lymphoid tissue in the body,”
Dr. Cossarini explains. “Istarted off by working on howto better definetheresponses to the interaction of the GI immune cells with HIV and some of the environmental factors in theintestinal mucosa, specifically the intestinal microbiome.”
Dr.Cossarinihasbegun aclinicaltrialthatwill focusontheeffectsofproposedtreatmentsforHIV onthegastrointestinalimmunesystem—oneofthe sitesofthelymphoidviral reservoir.Thestudywill trackasmallgroupof patientsastheyaretreated withexperimentalHIVtreatments. Viacolonoscopy, GItissuewillbecollected andtheeffectofthe treatmentsontheGItract’sviralreservoirwillbe ascertained. Thefindings shouldhelpgaugethe therapeuticefficacyof differentapproaches.
BothDrs. ChenandCossarininotethatthehunt foranHIV-preventivevaccinehasfailedaftermore than40yearsof effort. Theproblem,asDr.Chen explains, isthat“allthevaccinesaretargetingthe glycoprotein,whichison thesurfaceofvirus particles.Butglycoproteinisalsoonthesurfaceof cellsmediatingspread,wherewethinkit assumes verydifferent conformationalstates.”Thediversity of HIV, whichmutatesreadily,isachallengefor creatingapreventivevaccine.
More promising, in theirview, is to usebNAbs or other molecules as HIV therapies to recruit the immunesystem to clear the latent viral reservoir. “Iwould venture to guess that wemight obtain a therapeutic strategy that is able toeliminate most of the residual virus before we have an effective preventive vaccine,” Dr.Cossarinisays.



BenjaminK.Chen, MD,PhD
Irene and Dr. Arthur M. Fishberg Professor of Medicine
FrancescaCossarini, MD
Assistant Professor of Medicine (Infectious Diseases)
JudithAberg,MD
Dr. George Baehr Professor of Clinical Medicine; Chief, Division of Infectious Diseases

Mount Sinai's Institute for Advanced Medicine is growing and moving. The Institute is a New York State Designated AIDS Center, whose core mission is to provide comprehensive care to people who have or are at risk for HIV.
Among severalrecent accomplishments of note for Mount Sinai’s Institute for AdvancedMedicine is one inbricks andmortar: the opening of a new space on West 124th Street off Adam Clayton PowellBoulevard in central Harlem.
The Institute decided tomerge its Morningside and Jack Martin clinics, which had been situated on Mount Sinai Health System hospital campuses in neighborhoods adjacent to Harlem and move them to this new address in order to bring its services directly toa population that needs them.
The Institute is a New York State Designated AIDS Center (DAC), whose core mission is to provide comprehensive care to people who have or are at risk for HIV. The Institute’s broader focus is on providing for the needs of the HIV/AIDS community, the LGBTQ+ community, those who were recently incarcerated and have been released, and people experiencing domestic violence, among others. The goal: “Quality care; every patient; every time.”
The location of the newclinic is recognition that Black and Latino populations constitute a considerable portion—about two-thirds—of the Institute’s patient demographics.
“Moving the whole operation toHarlem will really assist us inour efforts tohelp more peoplefrom those populations get primary care and testing, treatment, and prevention,” explains Michael Mullen, MD, Executive Director of theInstitute and a Professor of Medicine (Infectious Diseases) at the Icahn Schoolof Medicine at Mount Sinai
“The two programs, Morningside and Jack Martin, were bothbased within the hospitals,” adds Matt Baney, the senior administrative director ofthe Institute. “By combining these two programs, we are taking co-located services and bringing them out to wherethe people live. It is about increasing access to care. It’s an important shift for us to bring services into people’s neighborhoods rather than havethem come tous.”
We are taking co-located services and bringing them out to wherethe people live. It is about increasing access to care. It’s an important shift for us to bring services into people’s neighborhoods rather than have them come to us.
— Matt Baney
Innovating how and to whom care is delivered is a hallmark of the Institute. Other major medical centers in the New York area haveDACs, but the size of the Institute’s programs and number of services offered are extraordinary. For that, alot of credit must go to the Institute’s program development and grant-writing capabilities.
“Mount Sinai’s DAC has become a very, very large program,” Dr. Mullen says. “We have been very successful in getting grants for special populations. When we see a need, we go and write a grant for it, and get it.”
“Someofourserviceshavebecomemore expansivethansimilarserviceselsewhere,” Mr.Baneysays. “Partofthecreditgoestothe support fromourinstitution, MountSinai, which hasreallymadeacommitmenttothispopulation.”
Unusually, nearly 70 percent of the Institute’s350 employees are funded through grants. “Werealize our services are expensive,” Mr. Baney adds. “So we go out and get other funding.”
The Institutehas received many grants. Recent programs funded by grants include:
• The VIP (Voices in Partnership) program, which supports transgender,intersex, gendernon-conforming, andnon-binary peoplewith HIV/AIDS. The programworks to identify these individuals and offers enhanced HIV and psychosocial case management.
• The Food and Nutrition program, which helps HIV-positive individuals with food insecurity and chronic health conditions. The program offers food vouchers and medical nutrition therapy.
• The Coming Home program, which provides services to thosewho have recently been released from prison orjail or who havea history of incarceration.
Another unique programis the result of a partnership betweentheInstitute and Mount Sinai’s Brookdale Department of Geriatrics and Palliative Medicine, withsupport from the Keith Haring Foundation. “Themajority of our patients are older than50,” Dr. Mullen notes. “We know there aremany needs in the HIV-positive geriatric population that should be addressed; for example, comorbidities associated with HIV. Some of these patients have been on medications for 40 years, and that takes a tollon the body.”
Theprogramembraces anewcaremodelthat includescomprehensiveassessmentandtreatment ofboththephysicalandpsychologicalchallenges ofolderpatients withHIV.Thegrantalsohas enabledthecreationofafellowship-liketraining programthatwillhelpreplicatesimilar programs forthefuture.
The Institute’s programs also inform patients about additional help available in the community. “We know we can’t do everything, so to expand the continuum of care for our patients we have links to complementary services out in the community,” Mr. Baney says. “We have about 60 links with other groups within New York City, and others link with us. We are definitely a community-based program.”
Aspartofanacademicmedicalcenter,theInstitute isalsoinvolvedinresearchandeducatingthenext generationofcaregivers.Whetherinvolvedin clinicalcare,research, oreducation,theInstitute’s staff displayexceptionaldedication, whichis highlightedbyaremarkablefilmthatfocusesonthe Peter Krueger Clinic(seerelatedarticle).
As new challenges come their way, new innovations respond. An example is Tele-PrEP, an extension of the Institute’s Pre-Exposure Prophylaxis (PrEP) program that is delivered using telemedicine technology, which was first implemented in response to the COVID-19 pandemic. The program is web-based; patients interact with staff through video visits. With the exception of occasional lab tests, everything else is done on the internet. Recently introduced, the service—like the Institute itself—continues to grow.




The film From Darknessto Light captures the voices of patients and caregivers at the forefront of the HIV/AIDS crisis, highlighting the groundbreaking care provided by the Peter Krueger Clinic.
The Clinic, one of the first HIV/AIDS clinics inthe United States, was established at BethIsrael Medical Center, now Mount Sinai Beth Israel, in
1989. Started during theheight of the epidemic in New York City, the Peter Krueger Clinic boldly stood against the stigmaof the disease and served as a beacon of hope and amodelof care for those New Yorkers diagnosed with HIV/AIDS. This film tracks the clinic’s origins and its impact over the last three decades, as told by the patients and staff that have called it home.
Theworkofthecliniccontinuestodayasapart of theInstitutefor AdvancedMedicineatMountSinai.

MichaelMullen,
MD Professor of Medicine (Infectious Diseases); Director, Institutefor Advanced Medicine
Originally led by Hans Popper, MD, “The Father of ModernHepatology,”The Division of Liver Diseases has played a pivotal rolein the advancement of hepatology both within and beyond theUnited States. Today we continue this legacy within the Department of Medicine at the Icahn Schoolof Medicine at Mount Sinai, where weprovide outstanding clinical care, breakthrough research, and comprehensive training programs for the future pioneers of our field. The Division’s commitment to researchhas driven severalkey advances in hepatology. In partnership with the Recanati-Miller Transplantation Institutein 1988, we were the first to perform a liver transplantation in New York State. Additionally, wedeveloped the first effective oral therapy for liver cancer. We continue to test new therapies every day,striving torapidly
translatediscoveries into more effective treatments for a diverse range of liver diseases. Our multidisciplinary approach to clinical care has made Icahn Mount Sinai a magnet for those seeking personalized treatment for Hepatitis B and C virus infections, autoimmune and druginduced liver disease, hepatic fibrosis, steatotic liver disease (previously known as fatty liver disease), cirrhosis, and liver cancer. By closely collaborating with specialists in transplantation, pathology, radiology, and oncology, we deliver integrative plans that are tailored to each patient's needs. Within the Mount Sinai Health System, we offer advanced treatment at three sites: The Mount Sinai Hospital, Mount Sinai West, and Mount Sinai Morningside. We remain equally dedicated to training the next generation of premier hepatologists. The
Division’s Transplant Hepatology Fellowship at The Mount Sinai Hospitaloffers advanced clinical training to applicants who have alsocompleted a gastroenterology fellowship. This program was the first of its kind to be approved by the Accreditation Councilfor Graduate Medical Education (ACGME) in the Northeast and remains one of the largest such fellowships inthe United States.

Meena Bansal,
MD Professor of Medicine (Liver Diseases); System Chief, Division of Liver Diseases


Newly popular obesity drugs likeOzempic® and Wegovy® are among several undergoing clinical trials at Mount Sinai for metabolic dysfunctionassociated steatohepatitis (MASH), formerly known as nonalcoholic steatohepatitis (NASH).If the trials are successful,they would fill an important gap, as no medications are currently approved by the FDA for the growing population with this disease.
No drugs are currently approved by the Food and Drug Administration (FDA) for the treatment of metabolic dysfunction-associated steatohepatitis (MASH), formerly known as nonalcoholic steatohepatitis (NASH). But that may be about to change, thanks to work by Mount Sinai researchers who are conducting trials on a number of medications with different mechanisms of action against the growing threat.
Among the medications in trials for MASHare new drugs for treating diabetes and obesity that have been recently inthe spotlight, says Meena Bansal, MD, Director of the MASLD/MASHCenter of Excellence and Professor of Medicine (Liver Diseases) at the Icahn School of Medicine at Mount Sinai, and Chief of the Division of Liver Diseases for the MountSinai Health System.
“Both of those comorbidities are present in many people with MASH, and we know that if you lose 10 percent of your body weight, you can see improvement in MASH-related fibrosis,” Dr. Bansal says.
We know that ifyou lose 10 percent of your body weight, you cansee improvement inMASHrelated fibrosis.
— MeenaBansal, MD
Among the trials she and her team are running is a phase 3 trial involving semaglutide (sold under brand names that include Ozempic® and Wegovy®). A previous study published in 2021 in The New England Journal of Medicine foundthat patients treated with semaglutide experienced significantly more MASHresolution thanthoseon placebo. But the secondary endpoint— improvement in fibrosis stage with no worsening of MASH—produced inconclusive results because of unusually high rates of response inthe placebo group and overall smallnumbers.

The Mount Sinai trial, begun in 2022 and sponsored by the drug’s maker, Novo Nordisk, seeks toexamine whether a weekly subcutaneous dose of 2.4mg of semaglutide—the standard dose used for treating obesity—can improve either MASH or the degree of fibrosis,versus placebo, in patients with MASH and fibrosis stages 2and 3 (F2 and F3).
The trial’s primary endpoint will be either MASH resolution without worsening of fibrosis, or at least a one-stage regression of fibrosis without worsening MASH. Patients will be assessed via biopsy at 72 weeks and will continue to be followed for a total of 240 weeks and assessed for clinical outcomes ranging from esophageal bleeding to liver transplant.



unlike some other drugs under investigation for efficacy against MASH, is an oral medication.
The trial is one of eight at the MASH Center of Excellence that are currently seeking to enroll patients. Three of those trials involve resmetirom, a thyroid hormone receptor-²agonist; other drugs under investigation include lisinopril, an angiotensin-converting enzyme inhibitor, and lanifibranor, a pan-peroxisome proliferator–activated receptor agonist.
The resmetirom trials, for which Dr. Bansal is also the Principal Investigator, are exploring the hypothesis that metabolic dysfunctionassociated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD), is a result of relative intrahepatic hypothyroidism, and that increasing thyroid hormone signaling in the liver can lead to MASH resolution with no worsening of fibrosis, or at least a one-stage improvement in fibrosis with no worsening of MASH.
The initial phase 2 trialfound that daily oral resmetirom resulted in a significant reduction in liver fat content at 12 and 36 weeks compared with placebo. Resmetirom responders with>30 percent magnetic resonance imaging proton density fat fraction (MRI-PDFF) reduction at week 12 had higher rates of MASH resolution (37 percent) on week 36liver biopsy compared with nonresponders (4percent), suggesting that early MRI-PDFF response could predict future histologic improvement. Resmetirom alsopositively affected patients’lipid profiles by reducing blood levels of atherogenic lipids. Thus, itmay reducethe incidence of cardiovascular disease, which is the leading cause of mortality in patients with MASH.
Recent topline data from the phase 3trial looking at liverbiopsies after 52 weeks of treatment suggests that resmetirom can causeboth improvement of at leastone stage in fibrosis and MASHresolution in a subset of patients. Based on these data, the sponsor, Madrigal Pharmaceuticals, received accelerated approval from the FDA for the drug in March2024.
The ongoing studies at Mount Sinai are looking to see if continued therapy will ultimately improve liver-relatedoutcomes.
A third drug, obeticholic acid (OCA), was furthest along in trials; however, an FDA advisory panel voted inMay 2023 against accelerated approval of it to treat MASH and the FDA followed with a rejection of acceleratedapproval in June 2023, citing safety concerns. The decision came despite a trial, known as REGENERATE and led by Dr. Bansal as PI, that met its primary endpoint of an improvement in fibrosis by one stage without worsening of MASH. Based on this disappointing news, the drug's maker, Intercept Pharmaceuticals Inc., has decidedto halt further development of this compound for MASH.
The wave of medications progressingthrough clinical trials marks a sea change for thetreatment of MASH, Dr. Bansalsays.
“It has been very challenging to get MASH therapeutics to market,” she says. “Early optimism was dashed by the failure of numerous trials. However, the promising data for these newer medications should make us optimistic that we will finally have effective treatments for this growing condition.”

MeenaBansal,MD
Professor of Medicine (Liver Diseases); System Chief, Division of Liver Diseases

In the face of hepatitis B virus (HBV) levels in New York City significantly above the World Health Organization’s acceptable standard, Mount Sinai has launched a system of digital alerts that appear on the screens of primary care physicians when a patient in their offices is a candidate for testing, vaccination, or treatment for hepatitis B.
In the face of hepatitis B virus (HBV) levels in New York City significantly above the World Health Organization’s acceptable standard, Mount Sinai has responded with an initiative aimed at universal surveillance and vaccination of adults. As part of that effort, in August 2022 it launched a system of digital alerts that appear on the screens of primary care physicians when a patient in their offices is a candidate for testing, vaccination, or treatment for hepatitis B.
“If our laboratory records show no hep B or C serology results for a patient, then the primary care providers can simply click on their screens to order the right tests and learn how to interpret them,” says Douglas Dieterich, MD, Director of the Institute for Liver Medicine, which has responsibility for liver care across the Mount Sinai Health System.
“Iftheresultsarenegative,vaccinationwould betheappropriatenextsteptohelpthepatient acquirelifelongimmunity,”Dr. Dieterich,Professor ofMedicine(LiverDiseases)at theIcahnSchoolof
Medicineat MountSinai, adds.“Ifthesurface antigenispositive,however,wewanttoencourage thepatienttoseektreatment throughourInstitute forLiverMedicineand,if appropriate,offerthem a clinicaltrialthat’sfocusedonacure.”Ateamof navigatorsis availabletohelppatients withcare coordination,Dr.Dieterichadds.
In NewYork City, public health authorities have estimated thereare 241,000 individuals with chronic hepatitis B, of whom 46 percent are undiagnosed. Many children werevaccinated by pediatricians starting in 1991 as part of a nationwide effort, but because older teenagers were often missed, a sizable number of adults today never received protection.
Addingurgencytothevaccinationandsurveillance movementistheupsurgeinNewYorkCityandthe countryofthehighly contagioushepatitisDelta virus(HDV), asmallRNA virusthatusesthesame receptorashepatitisBtoenterthelivercelland requiresinfectionwithhepatitisBtoreplicate.

“We want to test for Delta in everyone who tests positive for hepatitis B,”notes Dr. Dieterich. “Delta is the most severeformof viralhepatitis, and we know there are many people in New York who are carrying the virus.It can progress to cirrhosis within five years and to hepatocellular carcinoma within 10 years andhas an extraordinarily high mortality rate.” The good news, he adds, is that several drugs could soon be approved for treating the Delta virus, including one that has worked very wellin Europe for the past three years.
Against that backdrop, Mount Sinai is doubling down on its goal of eliminating both hepatitis B and hepatitis C. A program of universal screening and treatment for hepatitis C, rolled out by Mount Sinai in 2015, is now returning to its prepandemic volumes. Moreover, it has been broadened to include hepatitis B and Delta. Also returning to full strength is Mount Sinai’s Hepatitis Outreach Network (HONE), which goes into the community to conduct hepatitis B and C screening events, then link individuals who test positive to specialized care. According to Dr. Dieterich, HONE is being expanded beyond the African immigrant community to include Chinese, Russian, and Latinx populations in New York City.
Significantly, a curealready exists for hepatitisC infectionthanks to several U.S. Food and Drug Administration (FDA)-approved direct-acting antivirals that work indifferent ways to prevent the virus from making copies of itself. For hepatitis B, Mount Sinai is part of several clinical trials that are making progress toward finding a “functional cure,” defined by the FDA as undetectable
hepatitis B virus surface antigens (HBsAg) of less than 0.05 international units per milliliter.
Among those studies is a phase 1b trial of a core inhibitor of hepatitis B (from Assembly Biosciences) that has shown increased potency against covalently closed circular DNA (cccDNA) formation, thus blocking delivery of the genetic code needed to build new viruses. Another clinical study involves a monoclonal antibody (from Vir Biotechnology) that neutralizes hepatitis B virus and has been engineered to also potentially act as a therapeutic vaccine. This investigational drug is designed to block entry of all 10 genotypes of HBV into hepatocytes, while reducing the levels of virions and subviral particles in the blood.
“We’re certainly encouraged by the many new drug candidates on the horizon,” emphasizes Dr. Dieterich, “and the role they could potentially play along with aggressive surveillance and treatment of hepatitis B and Cto bring these viruses under control, if not prevent them from ever occurring.”

DouglasDieterich,MD
Professor of Medicine (Liver Diseases); Director, Institutefor LiverMedicine
Two new grants from Pfizer will help Mount Sinai educate primary care providers on how to identify at-risk patients and address inequities in diagnosis and careof nonalcoholic steatohepatitis.
Two new grants from Pfizer will help theMount Sinai NASH Center of Excellence deliver on its dual mission: toprovide exemplary caretoall patients withmetabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH), and to increasescientific knowledge about the causes of these conditions. Thegrants will enable the Center to educate primary care providers on how to identify at-risk patients and address inequities in diagnosis and care.
A $250,000 educational grant awarded to the Center’s Director, Meena Bansal, MD, willsupport efforts to raise awareness about electronic health record system tools such as FIB-4, a noninvasive test that estimates a patient's degree of liver
fibrosis and is integratedinto Mount Sinai’s Epic system. Thesetools can assist primary care and other front-line providersin screening patients who are at risk ofdeveloping MASH with significant fibrosis and in making appropriate referrals for evaluation and treatment based on the American Gastroenterological Association’s Clinical Care Pathway.
Dr. Bansal says providers will receive customized reports that demonstrate both the value of screening patients for advanced fibrosis and the impact of adhering to the established care pathway, such as referring patients with intermediate MASLD fibrosis scores for a FibroScan®

“Primary care providersare the first line of defense, and they need to have appropriatetools to identify patients who should undergo further evaluation,” says Dr. Bansal, Professor of Medicine (Liver Diseases) at the Icahn School of Medicine at Mount Sinai. “By introducing them to these tools, showing them howthey work, and then providing feedback on the impact of using the care pathway, we believe we can promote continuous learning and quality development among primary care providers. Equally important, webelieve our efforts willlead to increased screening and identification of at-risk patients.”
A second Pfizer grant, valued at $140,000, is enabling Andrea D. Branch, PhD, and her colleagues to usethe National Health and Nutrition Examination Survey datasets to identify MASLD and fibrosis risk factors that differ among non-Hispanic Black, Mexican American, and nonHispanic white populations. The goal is to build a more comprehensive understanding of the unique risk factors among thesepopulations.
For example, in previous studies supported by the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health, Dr. Branch found that advanced liver scarring among non-Hispanic Black populations is not only associated with cadmium exposure —which is associated with scarring in all populations—but also with lead exposure and poverty. These findings suggest that toxic and environmental exposures play a larger role in liver scarring among non-Hispanic Black than among non-Hispanic white populations.
“We have assumptions about disease presentation and risk factors that are not appropriate for all demographic groups and that
can result in care policies that are not equitable,” says Dr. Branch, Professor of Medicine (Liver Diseases) at Icahn Mount Sinai. “I want to ensure that policies are equitable. My hope is that, through this grant, we will identify distinct factors that enable us to catch disease at an earlier stage among these populations. We plan to use these findings to develop an algorithm that will flag people at risk in our electronic health record system, enabling their early diagnosis and linkage to care.”
These grants complement several undertakings launched by the Center since its formation in January 2022thatseek to better understand disease drivers and thusachieve improved patient prognosis and treatment. Amongthe most notable is a longitudinal registry that will enroll 5,000 MountSinai patients across the whole spectrumof the disease—andMountSinai’s diverse patient population—to explore why inflammation and fibrosis are stimulated in some individuals but not others. The goal, given the heterogeneity of MASH, Dr.Bansal says, is to develop a rigorous algorithm that enables phenotyping and risk stratification of patients for likelihood of rapid fibrosis progression based on biological and social factors. This will facilitate earlier interventions that can betailored to the drivers of diseasein individual patients.
“We want to bethe leader inMASH in all aspects from basic sciencetoclinical,” Dr. Bansalsays. “Through our combinedexpertise, work, and our diverse patient population, I think we are uniquely positioned to make valuable contributions to understanding and treating this disease.”


MeenaBansal,MD
Professor of Medicine (Liver Diseases); System Chief, Division of Liver Diseases
AndreaD.Branch, PhD
Professor of Medicine (Liver Diseases)

The Dr. Barbara T. Murphy Division of Nephrology at Mount Sinai is dedicated to advancing the knowledge and understanding of renal disease and its development, progression, treatment, and prevention. TheDivision offers a broad array of opportunities for training in clinical nephrology and research. The faculty is nationally and internationally renowned for their research and clinical expertise; many are leading experts in renal development, polycystic kidney disease, HIV- associated nephropathy, diabeticrenal disease, hypertensive renal disease, gene therapy, transplantation,peritoneal dialysis, and hemodialysis.
With more than 21 National Institutes of Health (NIH)-fundedPrincipalInvestigators, theDivision is among the best NIH-funded divisions of its kind in the United States. Additionally, the Division has one of the largest and most well-recognized nephrology fellowship programs inthe country and has developed several innovative subspecialty tracks, including general nephrology, critical care nephrology, transplant nephrology, palliative care
nephrology, andhome dialysis. Regardless of the national challenges in nephrology fellowship recruitment, Mount Sinaihas been ableto successfully match top candidates eachyear.
Within theMount Sinai Health System, thereare nowmorethan 20 outpatient dialysis centers, covering more territory and expanding intomany parts of Manhattan, Brooklyn, and the Bronx, making dialysis more accessible to patients.

John Cijiang He,MD, PhD
Irene and Dr. Arthur M.Fishberg Professor of Medicine
More than a decade of work on kidney fibrosis has yielded a promising new anti-fibrosis agent that can target fibrotic pathways without risking the development of cancer. Clinical trials are expected later in2023.
Clinical trials are beginning on anew drug totreat kidney fibrosis—theculmination of more than a decade of work by John Cijiang He, MD, PhD, Chief of Nephrology at Mount Sinai Health System, and his team.
The journey began with the discovery by Dr. He’s laboratory of a specific regulator of kidney fibrosis called homeodomaininteracting protein kinase 2 (HIPK2). Researching further, they recently identified an allosteric small molecule of HIPK2 which several animal models of kidney disease have shown is an effective anti-fibrosis drug. Preclinical testing has yielded encouraging results.
It is a classic example of dogged scientific determination, in which an interesting finding leads eventually to a significant advance, but not without a side trip or two along the way.
Dr. He, Irene and Dr. Arthur M. FishbergProfessor of Medicine at the Icahn School of Medicine at Mount Sinai, is an advocate of a systems biology
approachto research, focusing on computational biology and bioinformatics to elucidate a fuller picture of interactions within an organism. By doing this, he strives toidentify key drivers of disease processes, which could be potential drug targets for kidney disease therapy.
Onefocusofhisresearchhasbeenkidney fibrosis, akeyelement oftheprogressionof chronickidney disease. Inapaperpublishedin2012in Nature Medicine, Dr.Heandcolleagues,performing transcriptomicandproteomicstudiesofglomerular cells, foundproteinkinasesthatregulategene expressioninthekidneys ofanimalmodelswith kidneyfibrosis.Theresearchteamwasableto identifyHIPK2,theregulator ofkidneyfibrosis, andfoundthatHIPK2wasupregulatedinhuman kidneyswithvarious typesofkidneydisease.
These findings were promising, sinceHIPK2 had never been identified as being important in the pathogenesis of kidney fibrosis. Clearly, this

protein kinase had become a possible target for therapeutic interventionin kidney disease.
But therewas aproblem.Inhibiting all HIPK2regulated pathways posed unwanted side effects. One downstream molecule, known as p53, could incite tumor growth if dysregulated by HIPK2. “If you inhibit HIPK2 you also inhibit p53,” Dr. He explains. “And becauseof that, there is a chance of developing cancer. That factexplains why several companies thatwere very interested in an anti-fibrosis drug walked away, their enthusiasmgreatly reduced.”
Five years after theiroriginal study was published, Dr. Heand his researchteam announced in the Journal of the American Society of Nephrology that they had identified BT173, which can specifically inhibit the TGF-²1S/ mad3 pathway— an important pro-fibrotic channel—without also significantly inhibiting HIPK2 kinase activity or p53 activation. That finding made it possible to attenuate the renal fibrosis of chronic kidney disease (CKD) without employing thebroad approach of inhibiting allHIPK2 pathways.
“This is a new compound,” Dr. He says. “It has a high potency and can be given as a PO dose daily instead of by IV injection.” TGF-²1is thought to be the mostimportant profibrotic element in kidney disease, and knockout of Smad3, a downstream target of HIPK2, has been found to reducekidney fibrosis in animal models. Thus, blocking this pathway should bean effective approach to treating kidney fibrosis. “Our inhibitor blocks specifically the Smad3 activation,” Dr. He says.
A 2020 study in JCI Insight continued this work, further elucidating the novel mechanisms behind the anti-fibrosis roleof HIPK2 in kidney disease. “This study will help develop better HIPK2 inhibitors for kidney disease,” Dr. Hesays.
Now, Dr. He and others, including Kyung Lee, PhD, Associate Professor of Medicine (Nephrology) at Icahn Mount Sinai, in collaboration with ShangPharma Innovation, Inc., have founded Rila Therapeutics, whose goal is to develop and bring to market antifibrotic therapies. Their focus will be on a small molecule developed from BT173. “Preclinical data have been very positive,” Dr. He says, adding they have so far seen no toxicity.
Clinical trials are expected tostartin the spring of 2024. “This has been areally big journey, a 10year story, but I think in the end a successful one,” says Dr. He.
Although Dr. He’s research is exciting, he is also quick topoint out theimpressive research being undertaken by his colleagues in the Division of Nephrology. The division has 20 National Institutes of Health (NIH)-funded Principal Investigators and receives about $15 million in NIH funding yearly—“one of the best-funded nephrology divisions inthe country,” Dr. He notes.
The Mount Sinai division maintains both a registry of patients with CKDthat numbers more than 150,000 and theBioMeBiobank with more than 10,000 specimens frompatients with CKD—all vital elements of nephrology research. There is also a kidney tissue biobank that adds another 100 samples annually.
MountSinai’s nephrology researchgenerates more than 100 high-impact papers in any given year, and investigators regularly engage in pharmaceutical company-sponsored randomized controlled trials. Licensing agreements with pharma companies and the generation of patents are ongoing.
Mount Sinai and Mount Sinai faculty members (Dr. He and Dr. Lee) have equity in Rila Therapeutics.



KyungLee,PhD
Associate Professor of Medicine (Nephrology)
JohnCijiangHe,MD, PhD
Irene and Dr. Arthur M. Fishberg Professor of Medicine; Chief, Division of Nephrology
Research Initiatives in the Division of Nephrology
The COVID-19 pandemic presented special challenges for dialysis patients and the providers serving them, but Mount Sinai Health System's Division of Nephrology rose to the test.
The response to the COVID-19 pandemic by the Department of Medicine’s large Division of Nephrology was multifactorial, as Joji Tokita, MD, Associate Professor of Medicine (Nephrology) at the Icahn School of Medicine at Mount Sinai, explains.
“Itwas amultifacetedtaskthatwasextraordinarily complex,” he says. “But as far as our work during the pandemic is concerned, I think it was a great success.”
Part of the response to the challenge of the pandemic included regular consultations with other local academic health systems, major national dialysis providers, supply chain management, the New York ESRD [end-stage renal disease] network, and the New York State Department of Health. Home dialysis programs ramped up, and novel solutions were developed to allow patients to continue home therapy while still receiving all necessary monitoring and care. At the height of the pandemic, urgent-start peritoneal dialysis was extended to support inpatients with acute kidney injury requiring dialysis. Telemedicine played a key role in allowing nephrologists to keep track of their patients’ health remotely.
The Division of Nephrology of the Mount Sinai Health System has nearly 100 nephrologists on staff and more than 25 clinical fellows. Central to the Division’s mission is its belief in health equity and access to care. As such, the Division has developed clinics in outer New York City boroughs and staffed nephrologists at more than 10 dialysis facilities across the city. Faculty members see patients in diverse locations throughout Manhattan and in Queens; Brooklyn; and Oceanside, Long Island.
During the pandemic, the size of the Health System was both a challenge and an opportunity, Dr. Tokita explains. “Large programs can generate a nexus of opportunity for thought and innovation.
However, they can becomplex to manage, and integration and standardization across geographies often takestime.”
Ensuring continuation of clinical operations throughout the HealthSystem was indeed challenging. “For example, most dialysis patients receive treatment at a nearby center three times per week and many have complex medical conditions,”Dr. Tokita says. “The needto travel to and from the center as well as share close quarters during several hours of treatment required us tothink about how best tomitigate these increased risks.” Health careworkers were also affected by the pandemic, presenting additional challenges in ensuring centers remained open.
“A major concern was that if those patients were unable to receive maintenance hemodialysis in their home facility, they would potentially flood hospital emergency rooms, which would threaten to collapse the health care system,” Dr. Tokita says. The Division needed to develop very clear plans right from the start to ensure that would not happen.
“Throughout the pandemic it was imperative that we ensure continuity of operations across all of our dialysis facilities,” Dr. Tokita says. That the Division was able to do just that proved to be a notable success of Mount Sinai’s pandemic health care.
Chronic kidney disease(CKD) is a significant and growing public health problem. The Centers for Disease Control and Prevention notes that approximately 15 percent of U.S. adults,or 37 million people, are thought to haveCKD. Diabetes and high blood pressureare leading causes of CKD, as are heartdisease, obesity, and genetic predisposition. Significantly, of the patients with CKD, as many as 90 percent do not know they have it, and of those with severeCKD, almost40
percent areunawareof the condition.Abouta quarter of adults with type 2 diabetes develop diabetic kidney disease, and every year about 50,000 patients progress to kidney failure, requiring dialysis or akidney transplant.
addresses issues including intra-individual variability of eGFR, uACR, and hyper-filtration that masks early diabetic kidney disease. It provides risk stratification, to appropriately triage care and minimize patient burden and resource use.

For these reasons, accurate risk stratification of susceptibility to progressive kidney disease is a key clinical objective. Risk stratification historically has used the Kidney Disease Improving Global Options (KDIGO) approach, in which progression is defined as a sustained drop in glomerular filtration rate (GFR) category and/or a 25 percent decrease from GFR baseline, while rapid progression is a decline in GFR of >5 ml/min/1.73m2 per year.
A novel bioprognostictest, KidneyIntelX, developed by Mount Sinai faculty and licensed to Renalytix AI, is a labtest that defines the risk of CKD progression in patients with type 2 diabetes and CKD stages 1-3. The test combines estimated GFR(eGFR), novel serum biomarkers (sTNFR1, sTNFR2, KIM-1), urine albumin-creatinine ratio (uACR), and electronic health record datato provide a low, intermediate, or high-risk score of kidney function decline in the next fiveyears. It
MountSinai is studying the impact of KidneyIntelX testing on clinical decision-making at its ambulatory practices in an IRB-approved Real World Evidence study. Interim results were published in 2022 in Journal of Primary Care & Community Health. These interim results from 1,686 patients with six months of data found:
• Type 2 diabetes care: a 10 percent improvement in hemoglobin A1c
• CKD care: a 15percent improvement in albuminuria in low-intermediate risk groups
• Early-stage diabetic kidney disease: Patients with high-risk scores received morefrequent clinical visits, guide-recommended care, and specialist referrals
• Fifty-three percent of high-risk patients followed up within one month of their test and 57 percent had some action taken (medication change or referral) within three months,
compared with 13percent and 35 percent, respectively, in low-risk individuals
• Twenty-five percent of high-risk patients started SGLT2 inhibitors, medications that reduce progression of CKD, compared with 7 percent in the low-risk group.
Gaps remain in the continuum of care forpatients with diabetic CKD. Based on these findings, KidneyIntelX testing should help. Dr. Tokita, the first author of thestudy, notes, “A key aspect of this work is improving patient andprovider awareness of the condition and early use of evidence-based therapies currently available to treat it and reduceprogression.”
KidneyIntelX is a commercially available, CLIAapproved predictive test that combines patient information and biomarker results. KidneyIntelX is based on innovative technology developed by Mount Sinai faculty and licensed to Renalytix AI. Mount Sinai faculty and Mount Sinai have equity ownership in Renalytix AI.


JojiTokita,MD
Associate Professor of Medicine (Nephrology)
JohnCijiangHe, MD,PhD
Irene and Dr. Arthur M. Fishberg Professor of Medicine; Chief, Division of Nephrology

The Catherineand Henry J. Gaisman Division of Pulmonary, Critical Careand Sleep Medicine provides state-of-the-art consultation, diagnostic testing, and clinical and multidisciplinary care to patients with simple and complex respiratory and respiratory-related diseases. The combined strengths of the site divisions at allhospitals within the Mount Sinai Health System havecreated a unique opportunity to significantly impact training and translational research.
Home of the Mount Sinai – National JewishHealth Respiratory Institute, theDivision conducts research, offers educational opportunities, and provides multidisciplinary care to patients with all forms of lung diseases, including asthma, cystic fibrosis, pneumonia, emphysema, andchronic
obstructive pulmonary disease. Its comprehensive Asthma Program offers personalized treatmentfor adults, incorporating the latest research intothe effectivemanagement of the condition. The Center for Sleep Medicine provides advanced diagnostic and treatment plans for patients with sleep-related disorders,and the Critical Care program uses sophisticated technology to provide specialized care for patients with various forms of lung disease. In addition, Mount Sinaihouses one of 10 Centers of Excellence for sarcoidosis researchin the nation and has one of thelargest programs of its kind in the world.
The Division of Pulmonary, Critical Care and Sleep Medicine at The Mount Sinai Hospital was recently ranked No. 8 in the world, No. 7
in the United States, and No. 1 in New York by Newsweek for 2024 andNo. 12 in the United States by U.S. News & World Report® for 2023-24.

Charles A. Powell, MD, MBA
Florette and Ernst Rosenfeld and Joseph Solomon Professor of Medicine
Chief Executive Officer, Mount Sinai –National Jewish Health Respiratory Institute

MountSinaiisundertakingseveralinitiativesto betterunderstandthefactorsthatcontributeto severeasthmaandidentifydifferentsubtypesofthe disease.Theworkisintendedtobringaprecision medicineapproachtoasthma.
Despite significant progress in therapeutic approaches over thepast decade, anestimated 5 percent to 10percent of patients withsevere asthmaare not wellserved by current therapies. Part of the problem, according to Linda Rogers, MD, is that researchershave traditionally approached asthma as asingle disease.
Dr. Rogers is playing a key role inone of several initiatives at Mount Sinaito better understandthe factors that contributetosevere asthma and identify new treatments. She is the site Principal Investigatorfor the Precision Interventions for Severe and/or Exacerbation-Prone Asthma (PrecISE) Network Study, funded by the National


“When we look at patients whose asthma is not controlled by existing therapies, we find that they are very heterogenous in terms of disease drivers,” says Dr. Rogers, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), Icahn School of Medicine at Mount Sinai; Clinical Director, Adult Asthma Program, Mount Sinai – National Jewish Health Respiratory Institute; and Clinical Director, Medicine Clinical Trials Office.
“Some of the therapies we administer do not necessarily treat the type of inflammationthey have, or their inflammation might be better controlled by other treatments—such as ones used totreat other diseases—based on disease mechanisms research we have done. Thus, we are interested inthe potential of a precision medicine approach totreating these patients.”
Heart, Lung, and Blood Institute. This study was designed with input fromMonica Kraft, MD, while she was at the University of Arizona; Dr. Kraft is now the Murray M. Rosenberg Professor of Medicine, and Chair of the Department of Medicine, at MountSinai Health System and Icahn Mount Sinai.
Through this study,morethan30 centers nationwide are working on developing precision medicine approaches tothe treatment of severe asthma. That includes investigating the possibility of using biomarkers and other patient factors to inform patient treatment.
“Although biomarkers such as blood eosinophil counts and exhaled nitric oxide levels havebeen used in the clinical setting to assess patient eligibility forcertain advanced therapeutics, this
studyiscollectingsamplessuchassputum,nasal brushings,andexhaledbreathcondensateto betterunderstandthediseaseandidentifymore biomarkersandtargetsfortherapy,”Dr.Rogers says.“Wearealsocollectinggeneticdataand usingthattoselectnoveltargetedtherapiesthat arenotcurrentlyusedinclinicalpractices.”
Thestudyisuniqueinthatitisusinganadaptive protocoltoassesstheefficacyoffivetherapeutic agents—imatinibmesylate,Broncho-Vaxom®, clazakizumab,mediumchaintriglycerides,and cavosonstat—among600participantswhohave severeasthmawithsymptomsthatarenotwell
“Adaptiveplatformstudieshavebeenusedinboth COVID-19andcancerclinicaltrialsbuttoour knowledgethisisoneofthefirsttimesthisprotocol hasbeenusedtodevelopprecisionmedicine therapeuticsforasthma,”Dr.Rogerssays.“Itwill enableustoconductaseriesoffiveparallelphase 2studiestoassessasthmatreatmentsthatare promisingbutthatarenotundercommercial developmentforanasthmaindication.Ifwe determineoneagentisunsuccessfulbasedon statisticalanalysis,wecanabandonittoexplore theefficacyofanotheragent,whichacceleratesthe drugdevelopmentprocess.”

controlledthroughhigh-doseinhaledcorticosteroids andothertherapies.Thesetherapeuticagents wereproposedbyparticipatingcentersbasedon preliminarydatafrommechanistic,animal,and otherstudiessuggestingefficacy.Eachparticipant willbeadministeredoneoftheseagents,ora placebo,foraperiodand,followingawashout,will beeligibletoreceiveuptofouradditionaltherapies overthecourseofthestudy.
AsDr.Rogersevaluatesaprecisionmedicine approachtotreatsevereasthma,SonaliBose, MD,MPH,isinvestigatingtheimpactof environmentalandnutritionalfactorsonasthma controlamongacohortof30pregnantindividuals. Hergoalistoidentifyopportunitiestoimprove healthoutcomesamongpregnantpatientsand potentiallyreducetheintergenerationalriskof respiratorydiseaseintheirchildren.
“Asthmais the most common respiratory disease in pregnancy and canhave a significant impact on both the healthof mom and baby. Poor asthma control during pregnancy has been associated with many complications of pregnancy and a higher risk of respiratory disease in the offspring. Since asthma control can be dynamic during pregnancy, it is important to capture asthma health throughout gestation in a way that willallow us tointervene in a timely manner,” says Dr. Bose, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Pediatrics, at Icahn Mount Sinai.
“We want to gaina better understanding of the determinants of asthmacontrol during pregnancy, particularly among urban Black and Hispanic populations, who have adisproportionate risk for asthmamorbidity and traditionally have the highest rates of pregnancy complications as well.”
Dr. Bose is conducting two pilot studies among this cohort. One, building on her prior work on the influence of indoor exposures on asthma in other populations, focuses on the impact of indoor air pollution, specifically indoor fine particulate matter exposure, on asthma during pregnancy among 20 participants. Eachtrimester, Dr. Boseand her research teamare collecting one week of data from two air monitors—atraditional modelthat captures particulate matter in real time and a PurpleAir sensor, a low-touch commercially available monitor. Simultaneously, her team is performing daily home spirometry tests and capturing home activities, asthma symptoms, and medication use. The one-week data collection duration was chosen tomaximize resources for the study.
The second study assesses whether a higher omega-3status is associated with improved asthmacontrol during pregnancy among 30 participants—15 recruited from her cohortand 15 from Duke University. The team is rigorously collecting nutritional intake dataas wellas measuring blood omegalevels repeatedly during
each trimesterof pregnancy. Previous studies have demonstrated that omega-3polyunsaturated fatty acids (PUFAs) have an anti-inflammatory influence, which couldhave therapeutic value among patients with asthma. The team is specifically interested in whether downstream metabolites of PUFAs called specialized proresolving mediators helpcombat the inflammation associated withasthma.
Dr. Bose is particularly interested inexploring that protective aspectat an individual level among pregnant people and is collaborating withthe MountSinai Maternal Fetal Medicine division, as well as researchers at the University of Nebraska, University of Colorado, and Duke University, to complete this work.
In addition to a better understanding of risk factors that influence the asthma health of the mother and its likely implications for the fetus, datagleaned from thesestudies will enable Dr. Boseto design larger follow-up studies that assess the efficacy of interventions suchas reduction of indoor air pollution or increased omega-3intake.
“Poor asthma control during pregnancy has been linked to consequences such as spontaneous premature birth, gestational hypertension, and gestational diabetes,” Dr. Bose says. “Through our work, we can gain more knowledge about upstream factors that impact asthma controland thus help improvematernal and fetalhealth.”
Dr. Bose's research is supported by a Mount Sinai Transdisciplinary Center on Early Environmental Exposures Pilot Research (P30) grant (grant number P30ES023515) and the American Lung Association Airways Clinical Research Center (ALA-ACRC) pilot award.

Video resource visible at https://youtu.be/ZfSbpEb oaSA




LindaRogers,MD
AssociateProfessorof Medicine(Pulmonary, CriticalCareand SleepMedicine)
MonicaKraft,MD
MurrayM.Rosenberg ProfessorofMedicine; SystemChairofthe DepartmentofMedicine
SonaliBose, MD,MPH
AssociateProfessorof Medicine(Pulmonary, CriticalCareand SleepMedicine), andPediatrics)
CharlesA.Powell, MD,MBA
SystemChiefof Pulmonary,CriticalCare andSleepMedicine; ChiefExecutiveOfficer, MountSinai–National JewishHealthRespiratory Institute
A first-of-its-kindstudy led by a Mount Sinai researcher suggests that even a brief withdrawal of continuous positive airway pressure therapy for sleep apnea might increase one’s risk of developing Alzheimer’s disease.
Skipping a few nights of continuous positive airway pressure (PAP) therapy for sleep apnea might not seem like abig deal. But a first-of-itskind study led by Mount Sinai neuroscientist AndrewW. Varga, MD, PhD, suggests that even a brief withdrawalmight increase one’s risk of developing Alzheimer’s disease (AD).
Dr.Vargafoundthat withdrawalfromPAPtherapy amongsubjects withseveresleepapnearesulted insignificantovernight changesinADbiomarkers andmarkersofneuralinjurymeasuredinblood,
“For the first time we are showing that sleep apnea significantly induces some measure of neural injury,” says Dr. Varga, Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine) at the Icahn School of Medicine at Mount Sinai. “However, we do not know whether that injury is reversible, so the long-term implications remain to be seen. That said, our findings do imply that if an individual continues to skip therapeutic PAP, cumulative neural injury could occur.”

andthat anobservedchangeinneurofilament light (NfL),amarkerof neuralinjury,was significantly associatedwithapnea-relatedincreasesin intermittenthypoxiaandsleepfragmentation.
The study, published in the American Journal of Respiratory and Critical Care Medicine, is the first to showan acute effectof sleep apnea on AD biomarkers—a field of exploration that is relatively nascent—but Dr. Vargacautions that these findings necessitate further study.
The findings were based on analysis of blood collected in the evening (10:40 pm) and the next morning (6:40 am) across a night of polysomnographically recorded sleep among 30 participants with severe sleep apnea during conditions of therapeutic PAP or the third consecutive night of acute withdrawal from PAP in a counterbalanced fashion. The average age of the participants was 51.5; 27 percent of the participants were women and 67 percent were non-Hispanic white.
Dr. Varga and theresearch team looked at overnight changes in four plasma biomarkers associated with neuralinjury and AD—total tau; brain amyloid-beta40 (Aβ40) and brain amyloidbeta42 (Aβ42),peptides that contributeto formation of amyloid plaques; and NfL, an axonal proteinthat is released in responseto neural injury and is highly correlatedwith the progression of the disease—betweenthe two sleep conditions. Plasma samples wereanalyzed using asingle molecular array (SIMOA) Neurology 3-Plex A assay kit, whichenables detection of picomolar concentrations of amyloid and tau, and NF-Light™ kits. All samples were tested in duplicateand samples with a coefficient of variation e20percent were excluded from theanalysis.
Looking at the samples, the researchers observed a significant decrease in Aβ40 and a significant increase in NfL among participants after a third consecutive night without PAP therapy versus the therapeutic PAP sleep condition. “When we withdrew PAP therapy and induced sleep apnea acutely, the strongest signalwe saw was the overnight increases in neurofilament light,” Dr. Varga says.
Although there was no significant difference observed inthe other two ADbiomarkers between the two sleep conditions, Dr. Varga says there appeared to be a signalfor increased tau in the PAP withdrawal condition, and this warrants further study. Therewas no difference inall four AD biomarkers between the two sleep conditions at the start of the night within subjects.
Based on thosefindings, Dr. Varga and the researchteam subsequently investigated whether thereare sleep physiology predictors of the biomarker changes that they observed. They looked at severalsleep physiology biomarkers driven by PAP withdrawal and found that the number of sleep stage transitions—a marker of sleep fragmentation—and the amount of time below 90 percent O2 saturation were significantly associated withNfL. However, no identifiedsleep physiology biomarkers predicted the overnight change in Aβ40.
“Thereis considerable debate in the apneafield about what the apnea hypopnea index, or AHI, means,” Dr. Varga says. “There are those who believe it is bad to have a high AHI even if no

events are associated with significant dips in oxygen. In the cardiovascular field, the consensus is that only intermittent hypoxia matters. Our findings suggest that it is both the dips in oxygen and the sleep segmentation that seem to predict change in this neural injury marker.”
Dr. Varga is exploring the significance of these findings further througha new study that is recruiting individuals ages 55 and older who have been newly diagnosed with sleep apnea. He will collect baseline measurements of the participants’ AD and neural injury biomarkers, administer PAP therapy, and measure biomarkers over a threemonth treatment period to assess changes.
Additionally, Dr. Varga will conduct high-field brain magnetic resonance imaging of the participants using a 7-Tesla brain MRI. This will enable him to resolve sleep-wake regulating centers in the brain and explorechanges in functional connectivity in the brain as aresult of treatment. That could yield
more vital insights on the impact of PAP therapy on thebiomarkers of ADand risk of developing the disease.
“Very few sleep scientists have really researched the impact of treatment with regardto sleep apnea,” Dr. Varga says. “Through our studies, we are filling that gapand our findings havethe potential to improve long-term outcomes for patients with sleep apnea.”

AndrewW.Varga,MD, PhD
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)
The Mount Sinai – National Jewish Health Respiratory Institute’s Pleural Service, launched in 2020, has used pleuroscopy to dramatically increase its reach and the number and acuity of patients it can serve.
Just three years ago, pleural disease diagnosis and management at Mount Sinai Health System involved invasive approaches suchas pleural biopsies and pleurodesis performed using videoassisted thoracoscopic surgery. Patients required generalanesthesia and hospital admission.
Realizing that many of the patients he sees are too ill to tolerate such procedures, interventional pulmonologist Udit S. Chaddha, MBBS, saw an opportunity to effect positive change.
“Nobody in our division was performing pleuroscopy at the time,” he says. “It is a minimally invasive procedure, and we are able to perform a biopsy or pleurodesis as a 20-minute outpatient procedure using moderate sedation and a single port. Once we introduced pleuroscopy, it resulted in a cultural change that led to Pulmonology being consulted on almost every patient with pleural disease. It also resulted in a dramatic increase in referrals, and that provided the impetus for us to start a formalized pleural disease program.”
Launched in 2020, the Mount Sinai – National Jewish Health Respiratory Institute’s Pleural Service has attracted considerable interest and referrals, resulting in a 100 percent growth in pleural procedures. Dr. Chaddha, the program’s director, attributes that accomplishment, in part, to state-of-the-art equipment, the implementation of patient management protocols, and the comprehensive array of services and expertise available through the program.
“Pleuroscopy is probably the main procedure we do,” says Dr. Chaddha, Assistant Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery; Associate Program Director of Interventional Pulmonology; and AssociateDirector of Interventional Pulmonology withthe Catherine andHenry J. Gaisman Division of Pulmonary, Critical Care and Sleep Medicine at the Icahn School of Medicine at MountSinai
“We also perform indwelling pleural catheter placement, large- and small-bore chest tubes,

thoracentesis, closed pleural biopsies and biopsies of pleural-based or chest wall masses using ultrasound, and pleurodesis. Additionally, we participate in the management of empyema patients, such as decisions on when to administer tissue plasminogen activator and deoxyribonuclease, and in the management of pneumothorax patients, managing them in the acute setting and conducting follow-ups to ensure their care is appropriate.”
The goal of the program is to provide timely delivery of treatment—within minutes for emergent situations and hours for all other cases. A dedicated weekly clinic staffed by Dr. Chaddha; a nurse, Lilibeth Simporios, RN; and a fellow has facilitated that effort, resulting in patients undergoing pleural procedures within one week of referral. Additionally, procedure time is reserved in endoscopy, so that all patients can be attended to without delay.
“It is a set system, which sounds simple, but it enables state-of-the-art care to be the norm here, which is not the case nationwide,” Dr. Chaddha says. “There are very few pleural programs nationwide, as there are only approximately 40 interventional pulmonology fellowship programs. And there are only 400 interventional pulmonologists who are fellowship-trained, which is a requirement for launching a program like this. This means that, for the next decade, it will not be possible for smaller hospitals to offer patients an allencompassing program.”
Dr.Chaddhaanticipatestheprogramwillfillthat gapthroughtheservicesit offersandthrougha dedicatedinterventionalpulmonology fellowship. LedbyTimothyHarkin, MD, AssociateProfessorof Medicine(Pulmonary,CriticalCareandSleep
Medicine),andThoracic Surgery,andDirector of Bronchoscopyat IcahnMountSinai, thefellowship isofferedtoonecandidateeachyear. Dr.Chaddha seesother waysthattheprogramcanhavean impact,suchasincreasedresearchandclinical trial activity to gain moreinsights onthe pathology of pleural disease and offer more therapeutic options to patients.
“Our goal istohave dedicated fellows and researchcoordinators inplace so that we can increasethat activity within the next two to three years,” he says. “That will enable our research efforts to be smoother and faster, andwe willbe able torecruitmore patients and address the unmet need for treatment.”

UditS.Chaddha, MBBS
Assistant Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery
TimothyHarkin,MD
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine), and Thoracic Surgery

A Mount Sinai physician has developed an algorithm that uses a range of electronic medical record data to identify patients who are ready to be liberated from ventilation. It's a goal that has long been elusive.
A simpletool that accurately calculates a patient’s readiness to be liberated from a mechanical ventilator has long been a holy grailfor intensive care unit(ICU) clinicians. Pranai Tandon, MD, believes he may have found it.
Dr.Tandonisassessingthepotentialof applying artificial intelligencetoclinicaldatatoenablemore accurateassessmentsofpatientreadiness. WorkingwithIcahnSchoolof Medicineat Mount SinaicolleaguesinPulmonology, ClinicalData Science,andData-DrivenandDigitalMedicine, hehasdevelopedandisstudyingapredictive algorithm thatusesarangeof electronicmedical record(EMR)datasuchaspatient breathsounds andPaO2/FiO2ratiotoidentifypatientswhoare ready tobeliberatedfromventilation.Ifsuccessful, Dr.Tandonbelievesthatthealgorithmcouldbe impactfulforbothICUsandpatients.
“Patients who are left ona ventilator too long not only experience a wide variety of health problems but also contributeto adecrease inoverallICU throughput, which has ramifications for outcomes among other patients requiring ventilation,” says Dr. Tandon, Assistant Professor ofMedicine (Pulmonary, Critical Care and Sleep Medicine) at Icahn Mount Sinai.
“Liberating patients too early from a ventilator can also cause harm, whether that is from the stress of not being able to breathe easily or the need to reintubate. For these reasons, thereis astrong desire among physicians for a simple tool or calculation to augment their expertise in making these determinations. Machine-learning algorithms are a potential solution,as they are not only able to synthesize the wide range of data necessary to make these complex decisions but also can provide customized predictions for each patient.”
The inspiration for Dr. Tandon’s algorithm originated with ReSCUE-ME (Realtime Streaming Clinical Use Engine for Medical Escalation), an innovative Mount Sinai clinical trialthat assessed the potential to usemachine-learning algorithms to predict clinical deterioration. A literaturereview revealed several successful studies involving
predictive algorithms, but Dr. Tandon notes that they were typically small, and the algorithms could not beapplied in patient care. “We havea large patient cohort, we arestreaming data from patients, and we havea clinically focused team. For thosereasons, I sawthat we could potentially develop an algorithm that wecould weave into actual care,” Dr. Tandon says.
Liberating a patient from ventilation neither too early nor too late
Initially, Dr. Tandon developed a simple algorithm to collect dataon intubation and extubationtimes from the EMRs of patients in TheMount Sinai Hospital ICU, which areupdated every two minutes. He thenpartnered with the department’s respiratory therapists for a two-month study to validate his findings. Hedemonstratedthat the algorithm captured moreaccurate intubation and extubation timesthan those recorded by hand. Dr. Tandon subsequently looked at other variables, such as average number of patients intubated at any given time inthe ICU, time of daythat extubation typically occurs, and percentage of patients whoare reintubated. These variables demonstrated an opportunity for improvement of the predictive algorithm, which Dr. Tandon trained onacohort of2,615MountSinaipatientswho underwentanextubation attempt atleast once between2011and2019. Thecutoffwaschosento excludeCOVID-19patients,dueinparttolowrates of successfulventilator liberation, andtoevolutions inbest practicesandpatientpopulationsthat would renderany modelobsolete.
“Wesplitthemintotesting, training, andvalidation trainingsetssowecoulddecidewhichvariables
shouldultimatelybeincludedinthemodel,” Dr. Tandonsays.“Theprocess requiresaconsiderable degreeofexperimentationinwhichyougenerate hundreds of different possiblemodelsandthenpick thebest-performingoneforvalidation.”
The model that Dr. Tandon chose for validation included predictive factors such as level of consciousness, PaO2/FiO2 ratio, lactate production, and patient breath sounds. The latter, which was the most powerful predictor, are categorized as clear, rhonchi, wheeze, diminished, or null (i.e., absent data) based
predictive value of 11.8percent. He found that his modelachieved an areaunder the curve of 75 percent versus 54 percent for the index. “What we observed was that the algorithm was similar to the index in terms of patients who wereready for extubation, but the difference was that the algorithm wasmore intelligently selecting the patients inwhich thedecision for extubation was no,” Dr. Tandon says.
But the question remains as to how well the algorithm is able to makepredictions based on live data. Dr. Tandon is currently analyzing the results

upon twice-daily assessments and descriptions provided by a respiratory therapist or nurse. The model produces numeric probabilities from 0 to 1, but for the purposes of validation, Dr. Tandon used a false positive/true positive balance threshold of 0.45, resulting in a positive predictive value of 89.5 percent and a negative predictive value of 50.6 percent.
Using the historic cohort, Dr. Tandon compared the predictive potential ofthis model against the rapid shallow breathing index—the most used index for determining patient liberation readiness—at thetraditional thresholdof 105 breaths/minute/liter, which has apositive predictive value of 85.5 percent and a negative
of a three-month study inwhich the algorithm was fed live EMR datafrom the ICU each day at 5 am. The results,which he is reviewing with his respiratory therapy colleagues, couldnecessitate further tweaks tothemodel or a returnto the drawing board. But success would enable himto proceed with a pilot study that demonstrates the potential impact of this tool.
“Our hope is that we achieve an algorithm that enables us to safely decrease the time patients spend on ventilators,enabling us to achieve improved outcomes for them,” Dr. Tandon says. “Even a decreaseof 12hours would greatly revolutionize the throughput of the ICUand enable us to achieve cost efficiencies in care.”

PranaiTandon,MD
Assistant Professor of Medicine (Pulmonary, CriticalCare and Sleep Medicine)

The Division of Rheumatology at Mount Sinai Health System has along tradition of clinical excellence, patient care,and educationfor medical students, medicine residents, and intraining rheumatology fellows. With Musculoskeletal ultrasound becoming a regular part of rheumatology practice, Mount Sinai established its own musculoskeletal ultrasound program, aiming toprovide a monthly opportunity for fellows tobecome familiar with the useof ultrasound forthe evaluationof rheumatic diseases.
Rheumatology fellows learn how to maneuver the ultrasound probe and adjust ultrasound settings for optimal image capture, as well as how to recognize effusions, synovitis, erosions, and signs of soft tissue injury. It also allows them to practice ultrasound-guided procedures, such as aspiration in patients with difficult anatomy, and guided injections of joints, tendon sheaths, and nerve tunnels.
Musculoskeletal ultrasound is also required for the guidance of synovial biopsies, performed as part of an institutional review board- approved study of patients with refractory inflammatory arthritis, and for selected clinical scenarios where indolent infections are suspected. In addition to the educational benefits for trainees, patients are receiving highly accurate diagnosis and intervention.
The establishment ofthe Inflammatory Bowel Disease-Arthritis (IBD- ART) Program led by Bahar Moghaddam, MD, and Abhik Bhattacharya, MD (Division of Gastroenterology), makes it possible for patients with Crohn’s disease or ulcerative colitis to be evaluated for rheumatic disease manifestations.Other newinitiatives include the launch of theLupus Program and the Osteoporosis Program, both housed at Mount Sinai Morningside.

Rachel
Miller, MD
The Dr. David and Dorothy Merksamer Professor of Medicine (Allergy and Immunology)

Lupus has a broad clinical presentation that means the diseasecan affect nearly all aspects of a person’s life. Mount Sinai's new Lupus Program takes acomprehensive approach to addressing thephysical and neuropsychiatric challenges this complex condition poses.
Lupus is an immense clinical challenge characterized by heterogeneous presentations that make diagnosis andtreatment both difficult and delayed. Add tothat neuropsychiatric, psychosocial, and cognitive threatsto the health of patients with lupus, and the need for a center dedicated tothe physical and behavioral careof these patients becomes clear.
Which is why the LupusProgram at Mount Sinai Morningside was recently created.
Lupus, or systemic lupus erythematosus, is an autoimmune diseaseinwhich the immune system misfires, attacking theskin, joints,kidneys, brain, lungs, heart, and other organs. It is fairly rare, afflicting 1 in 1,000 people. The vast majority of them are women, though the 10 percent or soof lupus patients who are male tendto have more severe disease. Lupus is often diagnosed in women between the ages of 20 and 40 and is an underappreciated leading cause of mortality in younger women, particularly Black women.
“Thereis often a very long lag time betweenthe onset of symptoms and the timethe patient presents tous in the rheumatology clinic,” explains Chrisanna Dobrowolski, MD, MS, Co-Director of the Lupus Program and Assistant Professor of Medicine (Rheumatology) at the Icahn Schoolof Medicine at Mount Sinai. Dr. Dobrowolski is an attending physician at The Mount Sinai Hospital and Mount Sinai Morningside
Symptoms of lupus might include fever, fatigue, rash, joint pain and swelling, swollen lymph nodes, mouthulcers, and chest pain, all of which are also complaints of myriad other conditions—one reasonfor the typically long timeit takes patients with lupus to receive correct diagnoses.
In addition to the abovesymptoms, Dr. Dobrowolski says, “Patients with lupus often have debilitating fatigue, brain fog, and diffuse myofascial pain, which are not necessarily responsive to lupus-specific treatments but regardless, havesignificant impacts on patients’ quality of life.”

The broad clinical presentation of lupus also means that the disease can affect nearly all aspects of a person’s life, explains Nicholas Kopple-Perry, DO, Associate Director of Psychiatry Education and Training at Mount Sinai Morningside andDirector of the Consultation Liaison Psychiatry Service at Mount Sinai Morningside and Mount Sinai West. Dr. KopplePerry has specialized training working with individuals with comorbid medicalillnesses that affect theirpsychiatric and psychological health —expertise that explains his role as Co-Director of the Lupus Program.
Theneuropsychiatricsymptomsof thedisease havebeenwelldocumented, withstudiesfinding that thosewithlupussuffermorelifetimemoodor anxietydisorders,majordepression, phobias,panic disorder,andobsessive-compulsivedisorderthan thoseinnon-lupuscomparativesamples.
“Peoplewithlupushavetwicetheincidenceof depressionandhigher levelsofanxietycompared tothegeneralpopulation,”Dr. Kopple-Perrysays. “Also, upto80percentofindividualslivingwith lupuswillhaveimpairedworkingmemory,impaired attention, andgeneralcognitiveslowingoverthe courseof theirlives,whichhasahugeimpactona person’s functioning. Financialissuesandhousing insecurity canbecomefactors,ascanregistering andrecallingtreatmentrecommendations.”
The disease tends to first appear in early adulthood, typically during a woman’s reproductive years, and the advent of the disease can have an effect on one’s sense of self. Cutaneous manifestations also can disrupt one’s body image. “This disease really hits every domain of a person’s life and can be quite crippling,” Dr. Kopple-Perry says, “so in some ways treating lupus is more than just managing symptoms but also its collateral effects.”
Lupus is known to be more common among people who have high levels of stress and among those with a lower socioeconomic status. Dr. Dobrowolski notes that there is a significant lupus population in Morningside Heights and surrounding areas of Manhattan. “Having the clinic in the area where current patients live provides easier and better access and is really important for reducing barriers to treatment.”
Themanypresentationsof lupus, andthewide disparityindiseaseacuity, meansthatmost people donothaveagoodunderstandingof thechallenge that patientsface.“Youhavethisillnessthat’s painfulanddebilitatingandchangesyourbody, affectingyour emotionsandyourabilitytothink,” Dr.Kopple-Perrynotes,“but thegeneralpopulation doesn’talwayshaveagreatunderstandingof the disease, whichcanmakefindingsocialsupportin one’scommunityachallenge.”
“These are patients with a high incidence of cognitive dysfunction, depression, and anxiety, for multiple reasons,” Dr. Dobrowolski says. “These issues present a huge barrier to proper lupus treatment, so addressing psychosocial aspects of the illness is really paramount to treating the patient.”
The unique spectrum of coverage of clinical and psychiatric manifestations of the diseasemakes the lupus clinic at Mount Sinai Morningside stand out. In addition, because the clinic is part of the MountSinai Health System, other specialists are readily available to augment patient care.
Although the lupus program is new, there are already discussions on how to grow it. One likely addition will be a patient support group, and both rheumatology and psychiatry fellows may soon help support the clinic as part of their educational experience.


Chrisanna Dobrowolski, MD,MS
Assistant Professor of Medicine (Rheumatology)
NicholasKopplePerry,DO
Assistant Professor of Psychiatry










Mount Sinai’s Center for Transgender Medicine and Surgery—the most comprehensive such program of its kind in the world—offers afull menu of health care options, including primarycare, hormonal therapy, endocrinology, gender-affirming plastic surgery, urology, gynecology, otolaryngology, social work, spiritual care,and mental healthservices.
Surveys suggest there maybemillions of transgender and gender-diverse peopleinthe UnitedStates.MountSinai’sCenter for Transgender Medicine and Surgery—themost comprehensive such program of its kind inthe world—is dedicated to supportingthem with health care, research, and education.
AnarchitectoftheCenterandatirelessengineof itssuccesshasbeenJoshua D. Safer, MD,FACP, theCenter’sfoundingExecutiveDirector,whoisa Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at the Icahn School of Medicine at Mount Sinai.
Since the Center’s inception in 2016, its services have expanded to include a full menu of health care options, including primary care, hormonal therapy,endocrinology, gender-affirming plastic surgery,urology,gynecology,otolaryngology, social work, spiritual care, and mental healthservices.
“Thereareperhaps30placesaroundthecountry thatoffercertainpartsofwhat we do,but we are farand awaythe largest program of this sort in the country,and eventhe world,”explains Dr.Safer, who joined the Center in2018.
The number of transgender people in the United States might seem insignificant, but that is not the case. “In anonymous surveys, somewhere between half a percent and a full percent of people say they are transgender,” Dr. Safer explains. “If you do the math, that could be up to 3 million or more people.”
At the Center, patient volumes, for both genderaffirming hormonal therapy and gender-affirming surgery, have steadily climbed.
The health care needs of this group of patients can be complex, which is why continued research, and education of the next generation of clinicians, are vitalaspects of the Center’s mission.
For example, Dr. Safer is interested inexploring the relative risks of various treatment regimens, since there is concern that some hormone therapy might create risks.
“People were worried that it might beunsafe to maintain estrogen therapy whilea patient is set for


surgery, anditwas commonpracticefor transgenderwomentostopestrogensduring theseveralweeksaroundsurgery,”Dr.Safer says. “Butwedon’tdothat forpostmenopausalwomen takingestrogensfor hormonereplacementtherapy, and, infact,wecanseenodifferenceandno benefittohavingtransgenderpeoplestoptheir hormones.I hopetodisabusepeopleof someof thesefears, andI thinkthereareopportunitiesto lookat what hormonesdotovarioustissuesata moresophisticatedlevel."
Dr. Safer was the inaugural president of the United States Professional Association for Transgender Health (USPATH) and oversaw Mount Sinai’s hosting in 2023, for the third time, of the live surgery conference of the World Professional Association for Transgender Health (WPATH). He serves on the board of directors of WPATH as well as on its Standards of Care revision committee. Dr. Safer co-wrote the Endocrine Society’s 2017 guidelines for the medical careof transgender patients, and is the chair of theSociety’s current committee to revise those guidelines. Healso co-wrote “Care of Transgender Persons,” a2019 clinical practice review in The New England Journal of Medicine
Dr. Safer and colleagues at the Center work hard to disseminate the knowledge they have accumulated. Dr. Safer was a co-author of a 2023 Endocrine Society scientific statement concerning health care disparities and endocrine health, which, he explains, “reframes increased morbidity in transgender people to be more connected to social determinants of health than to hormone treatment.” He also co-wrote “Update in Adult Transgender Medicine” for the Annual Review of Medicine, among several other publications, and coauthored several presentations at the 2023 Endocrine Society meeting, including a case report of occult endometriosis in the prostate of a transgender woman.
The Center has been innovative in its roleas educator, creating fellowship programs that are
unavailable elsewhere. “We at Mount Sinai established the first fellowship program for gender-affirming surgery, which sits with our plastic surgeons,” Dr. Safer says. “Wealso established the first fellowship program for gender-affirming psychiatry and wehave a genitourinary fellowshipprogram.”
“Wewere alsoasked bythe State of New York to host afellowship program fortransgender medicineformedicalproviders,andwe’lltrain twopeopleperyear,”
Dr. Safersays. And theendocrinology fellowship includes a core rotationon gender-affirming hormones, whichDr. Safer notes is “significant. We compete with the most prestigious programs nationally forthis reason, and it’s one of the reasons why fellows chooseourprogram.” Mount Sinai also offers afree online course for primary care providers of transgender healthcare, which has amassed thousandsof students worldwide.
Despite the political issues that have swirled around transgender health care, Dr. Safer and his colleagues plan to press on.
“I’mamazed that anyone thinks that it is okay to target a vulnerable group of people and try to take away their health care,”Dr. Safer says.“We are here at Mount Sinai, and we’re not political. We arejust trying to deliver healthcare to our patients,that’s all.”

JoshuaSafer,MD
Professor of Medicine (Endocrinology,Diabetes and Bone Disease); Director, Center for Transgender Medicine and Surgery

Even as Mount Sinai Beth Israel moves toward closure of its inpatient campus on 16th Street, its modern outpatient sites across a wide swath of downtown Manhattan are more vital than ever to the Mount Sinai Health System. They include a multispecialty ambulatory center withmore than 30 medical practices in Union Square and a recently opened, state-of-the-art behavioral health center.
Even as Mount Sinai Beth Israel moves toward closure of its inpatient campus on 16th Street, its modern outpatient sites across a wide swath of downtown Manhattan are more vital than ever to the Mount Sinai Health System. They offer a vast range of primary and specialty care under one roof, with high-quality, innovative medicine informed by Mount Sinai’s backbone as an academic medical center.
“We’reexpandingandimprovingour outpatient platformtomakesurepatientsaregettingthe specializedcareandsocialservices theyrequire,” saysMatthew Weissman, MD, MBA,Chair ofthe Department ofMedicinefor MountSinaiBethIsrael andDowntown. “Andwe’reconstantlyfindingnew waystodeliverthat carewheretheyneedit, whetherit’s at our renovatedUnionSquaresite, our newly openedMount Sinai-Behavioral Health Center,or throughagrowingnetworkofprimary carepracticesacrossdowntown.”
With more than 30 medical practices, imaging suites, a pharmacy, and an urgent care clinic,
Mount Sinai-Union Square has truly stepped up to meet the clinical demands of the diverse community it serves. Sometimes described as a “hospital without beds,” the huge facility has co-located primary care physicians and medical subspecialists on the same floor for the convenience of patients, as well as to promote collaborative care by its multidisciplinary teams. Patients who need a CT scan, for example, can simply walk up a floor, or down a floor, for physical therapy.
WhentheUnionSquarefacility,just stepsfromone of thecity’ssubwayhubs,took overMount Sinai’s sleepdisordersprograminthesummerof2022, siteleaderssawanotheropportunity tocaterto patients. Theyactivelypromotedanewgeneration of mobilesleep-monitoringkits that individualscan takehometotestforobstructivesleepapnea, insteadof committingtoanovernight stayina sleeplab.Oncethedataareuploadedtothe device,theyarereadandanalyzedby aspecialist at thesleepdisorderscenter, withresultsrelayedto thepatientwithinweeks, downfrommonthsunder

thesleeplabregimen. Presentedwiththisattractive alternative, patientsingrowingnumbershave gravitatedtothetake-homekits, increasingthe hospital’sdiagnosesofasleepdisorderwith potentiallyserioushealthconsequences.
The $140 million MountSinai-Behavioral Health Center inLower Manhattan takes the conceptof patient-sensitive healthcare to a newlevel, serving as a “one-stopshop” for mental health care, substance use treatment, and primary care. Specifically, the new center—representing the largest private investment in mentalhealth in the history of New York State—integrates general outpatient mental healthand substance-use disorder treatment services with primary care services, providing seamless access and comprehensive carefor its patient population.
“We’ve responded to the needs of a community that’s often underserved by primary care doctors by placing full-time hospitalists and internists at our Behavioral Health Center,” notes Dr. Weissman, who is a Professor of Medicine, and Pediatrics, at the Icahn School of Medicine at Mount Sinai. “And if patients there require consultation with an infectious disease, gastroenterology, endocrinology, or other specialist, we’ll use telemedicine to conveniently link them to Mount Sinai Beth Israel or Mount Sinai-Union Square. That’s how we’re effectively managing resources among different sites on behalf of a typically high-needs patient population.”
Sensitivity topatient needs is evident in other notable ways withinMount Sinai Beth Israel’s realm. For example, Danielle Loeb, MD,MPH, a primary care physician with experience in treating transgender patients, was recently hiredandhas begun training residents in providing culturally and medically appropriate care to this growing
population. In addition, several hospitalists serve as advocates for Chinese-speaking patients— breaking down language and cultural barriers for them and making surethey are connected to the right doctors and social services within the hospital and the healthcare community.
“Even when these hospitalists aren’t directly treating Chinese-speaking patients, they’ve made it a point to go tothe ICU to see them and family members to help broker, in some cases, end-oflife conversations, or to makesure there’s continuity of care with doctors in the community,” says Dr. Weissman. “It’s that kind of personalized care and commitment that strongly defines Mount Sinai Beth Israel and makes us feel very much a part of the community.”
That connection extends toindividuals who are stillexperiencing symptoms that originatedduring COVID-19. Mount SinaiBeth Israel is home tothe Center for Post-COVID Care, treating about 50 patients a week with such lingering health issues as shortness of breath, headaches, dizziness, and “brainfog,” which can include memory loss and difficulty focusing. The Center was the first in the country totreat so-called long COVIDcases when it opened in mid-2020.
“Though the volume andintensity of COVIDrelated illness have since diminished, we’re still seeing patients in our clinic who have failed to get better,” notes Zijian Chen, MD, Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease) and Director of theCenter for Post-COVID Care. “We use an array of imaging and clinical tools and theknowledge we’ve acquired to diagnose and treat theirconditions, including referring many to our rehabilitation specialists who are often able to restore a normal quality of life.”



ZijianChen,MD
Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease)
DanielleLoeb, MD,MPH
Associate Professor of Medicine (General Internal Medicine)
MatthewWeissman, MD,MBA
Professor of Medicine (General Internal Medicine), and Pediatrics; Chair, Department of Medicine, Mount Sinai Beth Israel


Since becoming part of the Mount Sinai Health System a decade ago, Mount Sinai Brooklyn has worked diligently to build an enviablereputation within the community for quality service in cardiology, stroke, vascular surgery, bariatric surgery, gastroenterology, and robotic surgery.
For patients entering Mount Sinai Brooklyn with complex medicalandsurgical needs, the Mount Sinai logo adorning the 200-bed hospital in the Midwood section is a reassuring sight. That’s because this busy acute-care center, serving the ethnically and racially diverse neighborhoods of southernBrooklyn, has become a gatewayfor more than 1,200 patients annually who are transferred to Mount Sinai hospitals in Manhattan for specialized care and advanced procedures.
Mount Sinai Brooklyn has worked diligently over the past decade, since becoming part of the tertiary and quaternary Mount Sinai Health System, to develop and grow that linkage across an array of medical and surgical fields. At the same time, it has built an enviable reputation within the community for its own quality service in cardiology, stroke, vascular surgery, bariatric surgery, gastroenterology, and robotic surgery. Discussions are underway with the parent Health System to widen that range by bringing in specialists from Manhattan weekly to treat patients for liver, endocrine, pulmonary, and immunologic disorders.
“The greatest change we’ve made over thepast decade is our ability to attract to our hospital MountSinai-caliber physicians to improvethe quality and delivery of health care and the overall patient experience,” says Scott Lorin, MD, MBA, President and Chief Operating Officerof Mount Sinai Brooklyn, whotook the helm in 2018. “That’s reflected in our quality metrics—particularly the hospital-acquired infection rate—that have improved dramatically from among the worst to the best within the Mount Sinai system, and the entire state.”
A major contributor has been a highly successful hospitalist program launched in the wake of COVID-19, when Radfan Gazali, MD, Assistant Professor of Medicine at the Icahn School of Medicine at Mount Sinai,was brought in from MountSinai Morningside to head up the fledgling effort as Chief of the Division of Hospital Medicine at Mount Sinai Brooklyn.Over thepast two years, the program has grownto 10 full-time Mount Sinai physicians who areresponsible for 30 percent of all hospital discharges. This team has also received specialtraining in end-of-life care and

now admits all inpatienthospice patients who were previously managed by an independent group. Underscoring themagnitude of this change isthe fact that 65 percent of Mount Sinai Brooklyn’s patients are older than 65, and 25 percent areolder than 85, an unusually high ratio for any hospital.
Further enhancing care has been the hospital’s expanded use of Mount Sinai’s telehealth programs, effectively bringing subspecialists from across the river in Manhattan to the bedside of patients in Brooklyn.
“We’ve worked closely with Mount Sinai to set up telehealth services that can connect patients and doctors from the Emergency Department or from inpatient units to medical experts in fields that range from stroke to dermatology to psychiatry,” notes Peter Shearer, MD, Chief Medical Officer and Vice President of Medical Affairs at Mount Sinai Brooklyn, and Associate Professor of Emergency Medicine at Icahn Mount Sinai. “We’re now looking to add more subspecialties, such as rheumatology and endocrinology, for medical consults.”
Accompanying themany changes have been extensive physical renovations and upgrades in recent years.The hospital now has, for example, two advanced128-slice computed tomography scanners, and in May 2023 dedicated a newstateof-the-art magneticresonance imaging machine. Moreover, thehospitalmigratedto Epic in2019, resulting in enhanced communication and care coordination around the transfer of patients among institutions. The transition toEpic included reconfiguring most inpatient floors to make them telemetry-capable, amove that has reduced intrahospital transfers of patients by 50 percent.
Housing muchof this activity is a renovated ambulatory care building on the hospital grounds, which has become a thriving faculty practice. “We recently opened the Tisch Cancer Center with 15 infusion chairs and a brand-new mammography suite, and our oncologists are actively participating in clinical trials,” points out Dr. Lorin, who is
Associate Professor of Medicine (Pulmonary, CriticalCare and Sleep Medicine) at Icahn Mount Sinai. “We also havea robust orthopedic practice, neurology, and stroke services in this building, and recentlymoved all outpatient surgicalservices toa renovated suite on the top floor with 12 exam and twominor procedure rooms.”
As a fast-growing member of the Mount Sinai family, the Brooklyn hospital has alsorealized significant gains in physician recruiting, whichin years past was achallenge. The solution lay in enticing graduates fromMount Sinai’s medical training programsto work at the Midwood site. “Weput a lot of effort into recruiting these graduates, who sometimes split their timewith the Manhattan hospitals,” acknowledges Dr.Lorin. “And their experience was so positivethat they began telling colleagues, who wereencouraged to come to Brooklyn. And that’s how we built our faculty practice, and how we continue tobuild a MountSinai levelof quality care.”


ScottLorin, MD,MBA President and Chief OperatingOfficer, MountSinai Brooklyn
RadfanGazali,MD
Assistant Professor of Medicine (Hospital Medicine); Chief of the Division of Hospital Medicine, Mount Sinai Brooklyn


Mount Sinai Health System's hospitals on the West Side of Manhattan—Mount Sinai Morningside and Mount Sinai West—offer expertise in areas ranging from lung cancer detection and screening to gastrointestinal disorders.
Aware of its essential role in meeting the medical needs of communities on Manhattan’s West Side, Mount Sinai Health System has worked diligently in recent years to ensure that residents have access to thecity’s leading specialists and most advanced clinical services and programs, anchored by the health care hubs of Mount Sinai Morningside and Mount Sinai West
That effort has met withremarkablesuccess, resulting in a 60 percent increase in Department of Medicine faculty since2015 and the strengthening of suchvitally needed services as primary care and lung cancer detection and screening. Also included are the development of centers of excellence for patients with pancreatic cancer and gastrointestinal physiology and motility disorders.
“Every medicalspecialty in our space has experienced significant growth interms of faculty and the level of expertise the public can readily tap into,”says SamuelSeward Jr., MD, Former Chair of Medicine for Mount SinaiMorningside and Mount Sinai West. “In primary care alone, we’ve hired, over the past two years, 12 newfulltime physicians and have transformedthis clinical program into one of thelargest of its kind within the Mount Sinai Health System, and withinthe city. And over the last few months, we’ve added an urgent carecenter asa way of growing the breadth and depth of our primary caremodelto include just-in-time care for patients.”
Noinitiative better encapsulates Mount Sinai’s growing commitment to residents on thecity’s West Side than the Incidental Lung Nodule Program. Launched recently atMount Sinai Morningside, this unique and ambitious effort is harnessing the expertise of the hospital’s pulmonary specialists andprimary care doctors in the Division of General Internal Medicine to establish the hospital as a screening hub for diagnosing and monitoring lung nodules identified in patients who have undergone CT scans for conditions suchas coronary disease, chest pain, or pulmonary embolism.
“Wewant tobesurewe’refindinglungcancers bothwhenwe’respecificallylookingfor themand whenwe’renot,throughourIncidentalLungNodule Program,”saysJavierZulueta,MD,Professorof MedicineandChiefof Pulmonary, CriticalCareand SleepMedicineat MountSinaiMorningside,who hasoverseenandchampionedtheprogram atthe hospital. Onceanincidentalnoduleisdetected throughaCTscan, heexplains,speciallydesigned softwarealertstheproviderwhoorderedtheimage andthepatient,urgingfollow-upwithahospitalbasedpulmonologist.
Adds Dr. Seward: “Because patients are often asymptomatic in the early stages of lung cancer, this program has enormous potential to save many lives through quick intervention by our pulmonary specialists. In just a few months we’ve already captured hundreds of patients who are following up based on the findings of our radiologists.”
We’ve definitely upped our game to meet the needs of patients by putting inplace the finest faculty and highest-quality medical care that’s accessible to them.
— Samuel Seward, Jr., MD
Timely intervention is also critical intreating patients with pancreaticand biliary cancers. For this reason, the Department of Medicine’s decision to move its Center of Excellence forPancreatic Cancer to Mount Sinai West has proven to be a huge asset to residents in surrounding communities. The program’s leadershipteam includes Edward Lung,MD, MPH, Professor of Medicine and Director ofEndoscopy for the Division of Gastroenterology at Mount Sinai West and Mount SinaiMorningside. A widely known expertin advancedendoscopy, Dr. Lung ensures
that every patient who arrives at the Center is surrounded by amultidisciplinary team that’s able to offer a wide range of personalized treatment options and clinical trials.
Mount Sinai’s rapid growth on the West Side is further showcased in its Center for Gastrointestinal Physiology and Motility, a highly specialized unit that has added within the past two years six faculty members, including experts in motility disorders throughout the GI tract and in pelvic floor dysfunction in women. The Center’s new Director is a nationally recognized expert in the field, Daniela Jodorkovsky, MD, Associate Professor of Medicine (Gastroenterology). Thanks to her group’s extraordinary growth and cutting-edge platform for diagnosing and treating both upper and lower GI motility disorders, it is now poised to be an international leader in that space.
“Rounding out our many clinical initiatives is a large residency training program that serves as a robust pipeline for the talent and services we’re constantly adding to our West Side operations,” notes Dr. Seward. “We’ve definitely upped our game to meet the needs of patients by putting in place thefinest faculty and highest-quality medical care that’s accessible to them, both as inpatients and, increasingly, at convenient sites within their communities.”
As a long-time physician at Mount Sinai Mount Sinai Morningside and Mount Sinai West, and as graduate of the internal medicine residency program, I am very excited to have been given the opportunity to serve as InterimSite Chair of the Department of Medicine. My goal is to increase access to the highest quality primary and subspecialty careavailable on the West Side of Manhattan while opening and establishing new, innovative programs to serve the needs of the community. An important strategic objective is the integration of more clinical research into our clinical careprograms.
— Amy Rosenberg, MD




JavierZulueta,MD
Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)
DanielaJodorkovsky, MD
Associate Professor of Medicine (Gastroenterology)
SamuelSeward,MD*
Professor of Medicine (General Internal Medicine); Former Chair, Department of Medicine, Mount Sinai Morningside and Mount Sinai West
AmyRosenberg,MD
Interim Site Chair, Mount Sinai Morningside and Mount Sinai West
* As of the publishing of this report, Dr. Seward has since left Mount Sinai.

In western Queens, a third of the patients don’t speak Englishand face other barriers to healthcare. To help them, Mount Sinai Queens in recent years has added a state-of-the-art stroke program, a massive investment in cardiovascular care, and an expanded presence in oncology, endocrinology, gastroenterology, and outpatient services, all conveniently available at several new ambulatory care sites.
Locatedinoneofthemostpolyethniccommunities inthecountry,MountSinaiQueensisanacutecarecenterkeenlyequippedtohandlethe population’scomplexand diversemedicalneeds. Inrecentyearsit hasaddedastate-of-the-art strokeprogram, amassiveinvestment in cardiovascularcare,andanexpandedpresencein oncology,endocrinology, gastroenterology, and outpatient services, allconvenientlyavailableat severalnewambulatorycaresites. Mostrecently, thehospitaladdedageriatriciantooptimizeitscare ofolderadults.
“There’s agreat interest nationally in disparities in health care, and nowhere are they on greater display than in westernQueens, wherea thirdof our patients don’t speak English,” says Kathy Navid, MD, Associate Professor ofMedicine (Hospital Medicine) at the Icahn School of Medicine at Mount Sinai, and Chair of the Department of Medicine at Mount Sinai Queens. “That’s what we’re focused on: takinga population that faces so many barriers to healthcare and working our hardest to offer them the same kind of specialized services andquality health carethey would enjoy if they lived in Manhattan.”
To that end, the 170-bed campus in the Astoria section of Queens is developing centers of excellence around cardiology, neurology, and oncology, drawing on the resources and expertise of The Mount Sinai Hospital, its parent across the East River. In launching a certified stroke program, for example, the hospital benefited from a highly skilled neurology subspecialty team that came over from The Mount SinaiHospital and took up round-the-clock residence at the main Astoria site. That huge investment enabled the hospital tobecomea thrombectomy-capable stroke center featuring astate-of-the-art CT machine withX-ray fluoroscopy thatcould be deployed for interventional procedures as well as scanning. The stroke center—the first of its kind in Queens—performed its first cerebral thrombectomy in 2017.
The real turning point for Mount Sinai Queens occurred the prior year, however, with the opening of a spacious newambulatory pavilion in Astoria, repletewith outpatient operatingrooms and a wide range of specialty and primary care offices. As part of the dramatic shift, the hospital also hired six physicians forits hospital medicine program

and started evolving into“more of a Mount Sinai presence,” as Dr. Navidputs it. Over the past two years, the expanding Department of Medicine footprint has included seven endocrinologists at five ambulatory care sites on and off the main hospital campus,and smaller but growing teams of gastroenterologists, nephrologists, infectious disease specialists, and renal doctors.
Nowhere has the growth been more impressive, however, than in cardiology, which now encompasses nine cardiologists and is tripling its physical size. “A cardiac catheterization unit was recently opened, the first one in the area, and all of our cardiovascular services are being consolidated in a new state-of-the-art building across the street from the hospital with a CT scanner, echocardiogram, and stress- and other advanced-testing modalities,” explains Stephen Sigworth, MD, Associate Professor of Medicine (General Internal Medicine) at Icahn Mount Sinai. Dr. Sigworth has been leading ambulatory care development for the past four years at Mount Sinai Queens and Mount Sinai Brooklyn.
The Mount Sinai investment inQueens is also paying dividends for individuals waiting for a kidney or liver transplant. “These patients are pretty sick, andtheir ability to travelis limited,” notes Dr. Navid. “They’renowableto get subspecialty carefrom transplant teams based at Mount Sinai that come overto Queens oncea week. They never had that option before.”
Given the sensitivity of Mount Sinai Queens tothe diverse population it serves, it’s not surprising that community outreach continues tobe an area of intense pride—and robust activity.
“Our patients havetremendous needs, and because many of our staff are from the community, they’re equipped to recognizeand address them,” acknowledges Dr. Navid, herself an internal medicine physician. “One area of focus, for example, is breast cancer screening in the Bangladeshi American community, as well as blood pressure testing, knowing the prevalence
of cardiovascular disease in this population. Our cardiologists look for opportunities to practice and advocate for disease detection and prevention in this community.”
That sensitivity is no less evident inthe inpatient setting. In a hospital where several dozen languages are spoken on thefloors, physicians and staff are equipped with a sophisticated video interpretation systemon their monitors and phones for instant onsite translation. Palliative care teams consisting of physicians, nurse practitioners, and socialworkers arealso attuned to the multiplicity of cultural needs, especially when having end-of-lifediscussions with patients and theirfamilies.
Sums upDr. Navid: “It’sreally gratifying to beable to bring this level of passionate and highly skilled care tothe small,closely knit neighborhoods of Queens. Even better, with the support of our tertiary care partner we continue toup our game.”


KathyNavid,MD
Associate Professor of Medicine (Hospital Medicine); Chair, Department of Medicine, Mount Sinai Queens
StephenSigworth,MD
Associate Professor of Medicine (General Internal Medicine)
The Department of Medicine at Mount Sinai South Nassau is bringing specialized medical services that were previouslyonly available in Manhattan to the roughly 900,000residents the hospital serves on Long Island’s South Shore.
Fiveyears afterbecomingMountSinai’sflagship hospitalonLongIsland,Mount SinaiSouthNassau isgrowing inawaythat isimpossibletomiss. Initiativesrangefromtheongoinghalf-billion-dollar constructionprojectthatincludesthesleek Feil Family PaviliononitsmaincampusinOceanside, toanexpandedinternal medicineresidencytraining program,toambitiousplansunderwaytobecomea regionalcenterforcardiacsurgeryand thrombectomy-capablestroketreatment.
For the roughly 900,000residents the hospital serves on the Island’s South Shore, that new footprint brings to their community the kind of specialized medicalservices they previously had to goto Manhattanto access.
“We were always a verysuccessful community hospital, but sincejoining Mount Sinai we’ve become aneven stronger and larger academic tertiary care center that still has a very unique and nice community hospitalfeel,”says Aaron Glatt, MD, MACP, Professor of Medicine (Infectious Diseases) at the Icahn School of Medicine at Mount Sinai and Chair of the Department of Medicine at Mount Sinai South Nassau. “We’ve enjoyed a very collegial relationship and exchange of services and doctors that areallowing our
patients to get the same great quality of Mount Sinai care right in their backyard.”
Cardiovascular care drives the point home. While the hospital has maintained for years a recognized Center for Cardiovascular Health— it’s the only acute-care center on Long Island’s South Shore to perform emergency and elective angioplasty—it has been limited by its lack of onsite cardiac surgery.
That will soon change upon completion of the Feil Family Pavilion, which includes new operating rooms, surgical beds, and an intensive care suite, setting the stage for a vastly expanded cardiac surgery and interventional cardiology program expected to begin in the summer of 2025. The program will include specialists from the Mount Sinai Health System (including Mount Sinai South Nassau) performing and training others in surgical procedures such as TAVR (transcatheter aortic valve replacement) for patients with severe aortic stenosis, and leftsided transseptal ablation for atrial fibrillation. Enhancing that capability will be the migration of Mount Sinai South Nassau to Mount Sinai’s Epic electronic health records system.

Cancer treatment is another specialty benefiting significantly from the Mount Sinai connection. A Joint Comprehensive Cancer Center at Mount Sinai South Nassau gives patients access to cutting-edge clinical trials and treatment in conjunction with Mount Sinai’s oncology team at its main campus in Manhattan. An integral and robust part of that joint effort is infusion services offered locally and regionally for both oncology and non-oncology patients across the Mount Sinai Health System. The program also plans to expand academically. Elaborates Dr. Glatt: “The potential for our hospital to offer fellowships in cardiology, oncology, and other medical specialties, in addition to our current gastroenterological fellowships, is one of the most exciting prospects on our horizon.”
Under the banner of Icahn Mount Sinai, Mount Sinai South Nassau has already received approval from the Accreditation Council for Graduate School Education to enlarge its InternalMedicine Physician Residency Program from 30 to 39 slots next summer. The hospital also maintains residency training in surgery,obstetrics and gynecology, podiatry, and family medicine.
Clinically,MountSinaiSouthNassauisworking towardhavingaLevelIIINeonatalIntensiveCare Unit, buildingonitsLevelII statuswhileenhancing high-riskobstetricalcareforLongIsland’s South Shore. Thehospitalcurrentlydeliversmorethan 2,000babiesayear.Interms ofambulatorycare, Mount SinaiSouthNassauhas37sitesoutsideits mainfacilitywherephysicianspracticeprimaryand specialtymedicine,andrecentlybuilt anadvanced 15,000-square-footmedicalartspavilioninLong Beach. That communityisalsothesiteofafreestanding,full-serviceEmergency Department (ED), oneof onlyahandfulinNewYorkState, andthe FeilFamilyPavilionproject willincludeadoubling insizeofthehospital’s mainED.
True to its roots as a community hospital, Mount Sinai South Nassau takes particular pride in its extensive outreach program. That effort gained
high visibility during COVID-19, when its distinctly marked mobile vaccination bus (the “Vaxmobile”) traveled up to six days a week to hard-hit communities toadminister vaccines and boosters toall eligibleresidents, as well as to provide treatments such as Paxlovid after they became available. The outreach now brings to the region’s towns and neighborhoods amultitude of health screening programs, including ones for breastcancer, cardiovascular/blood pressure, prostate cancer, and dermatological/melanoma. In addition, clinical professionals frequently appear beforecommunity groups to give lectures on proactive health care.
Given Mount Sinai South Nassau’s fullrange of clinical, ambulatory, and community services, it’s not surprising that the hospital is perennially ranked among the “Best Regional Hospitals” in the metropolitan area by U.S. News & World Report® with recognized expertise in 10 areas, plus recognition from the Infectious Diseases Society of America as a “Center of Excellence” in Antimicrobial Stewardship.
“Many of us live in the neighborhood,” acknowledges Dr. Glatt, himself a frequent community lecturer, “and we’ve all worked extremely hard to make Mount Sinai South Nassau a hospital where our own families and friends can get the finest-quality medical care around.”

AaronGlatt, MD,MACP
Chair of the Department of Medicine, Mount Sinai South Nassau

Efforts to grow and improve the delivery of ambulatory carehave led to an enormous increase in the volumeofoutpatient visits over the past few years. That has prompted a commensurate increase in the hiring of new physicians and their integration into Mount Sinai faculty practice offices, both at and beyond the eight hospitals of the Mount Sinai Health System.
As Mount Sinai Health System expands its ambulatory care footprint across New York City and beyond, itis working diligently to improve delivery of primary careand specialty services to patients in ways that address how, when, and where they need them.
Through video visits, for example, patients can speak directly to and coordinate their care among doctors in an extraordinary range of medical fields. Or they can make an outpatient appointment with a physician at a hospital-based office or standalone clinic or facility that’s close totheir home.
“Ensuring that patients have timely access within seven days to just about any ambulatory service they need, from primary care to multispecialty, continues to be our top priority,” says Aida Vega, MD, Associate Professor of Medicine (General Internal Medicine) at the Icahn School of Medicine at Mount Sinai and Vice Chair for Ambulatory Care of the Department of Medicine. “We’re also improving the patient experience in terms of how they get their care, which is helping us to reduce visits to emergency rooms along with hospital admissions.”
The success of these efforts is reflected in the enormous increase in the volume of outpatient visits overthe past few years. That has prompted a commensurateincrease in the hiring of new physicians and their integration intoMount Sinai faculty practice offices, both at and beyond the eight hospitals of the Mount Sinai Health System. The latter includes the newly renovatedMount Sinai-Union Square site, which houses 30 medical practices—nearly a hospital in itself—at a convenient downtown Manhattan location.
That co-location of services constitutes another important way ambulatory careis improving access for patients. At severalsites, including Union Square, Mount Sinai is interweaving psychology and primary care offices to facilitate coordination between both specialties. Similarly, the newMount Sinai-Behavioral Health Center in lower Manhattan includes primary careto complement its mental illness and substanceuse-disorder services.
“Around half, if not more, of the cases we see in primary care involve anxiety, depression, or other stress-related disorders,” says Dr. Vega. “So, we

see co-location as a great way to foster collaboration between psychologists and primary care doctors interms of prescribingmedications and behavioral treatments, such as short-term interventions with cognitive therapy, which psychologists canenact.”
Enhanced access to care also means new initiatives aimed at hypertension and diabetes control across entire populations of patients. On the hypertension side, ambulatory doctors are a crucial part of Mount Sinai’s aggressive drive to identify and manage patients with higher-thannormal blood pressure, treating them and bringing them back tothe office for follow-up checks until they are within nationally accepted guidelines. They are also playing aprominent rolein reducing hemoglobin A1c levels of diabetic patients to below 9 percent by collaborating with nutritionists, diabetes educators, andendocrinologists to reinforce best practices in patientsfor managing their conditions.
For Dr. Vega, the flipside of enhanced patient access to services such as theseis improving workflow within the system itself, thereby enabling doctors to commit their full time and attention to what they were trained to do: be excellent doctors. Nationwide, physicians are overwhelmed with the daily paperwork from their jobs and, more recently, with responding to the onrush of queries from patients over electronic portals. TheHealth System has launched an effort to address this challenge through more robust support at the practicelevel.
“We’re strengthening our team-based model through a huge effort this year to add advanced practice providers, particularly nurse practitioners and physician assistants, and to make sure every staff member is working at the top of their license,” notes Dr. Vega. As part of this wideranging workflow redesign, she adds, nurses and medical assistants are helping to screen and review patient calls and prioritize those that need a more timely response. And they’re working to ensure that test results are returned more quickly to patients.
“We’ve made tremendous gains over the past year in terms of productivity of our physicians and clinical staff and their responsiveness to patients,” reports Dr. Vega. “But we also realize we’re only halfway to our goal, and that we need to keep pushing hard to streamline our workflow at the same time we’re improving patient access to care.”

AidaVega,MD
Associate Professor of Medicine (General Internal Medicine); System Vice Chairfor Ambulatory Care, Department of Medicine

Mount Sinai's Department of Medicine has builtone of the largest and most sought-after Internal Medicine residency programs inthe country, with morethan 400 trainees at threeManhattan-based hospitals, in addition to 30 fellowship programs across a wealth of specialties. It has added programs in advanced fields such as genomics and point-ofcare ultrasound (POCUS) while building skills and knowledge in disciplines, such as primary care, transgender medicine, and geriatrics, where physicians can have clinical as well as societal impact in the course of their careers.
Stayinglaser-focusedon thefuturedirectionof medicinehas enabledtheIcahnSchoolof Medicine atMountSinaitotailor its trainingtotheevolving needsofInternalMedicineresidentsandfellows.
It has added programs in advanced fields such as genomics and point-of-care ultrasound (POCUS) while building skills and knowledge in disciplines, such as primary care, transgender medicine, and geriatrics, where physicians can have clinical as well as societal impact in the course of their careers. In the process, the Department of
programming we’reableto educate any medical student inthe country by personalizing a plan geared to their clinical and academic needs and interests. That makes our agenda unique.”
POCUS is a fitting example. As ultrasonography has become an increasingly important diagnostic tool at the patient’s bedside, Mount Sinai has responded with a robust curriculum for trainees developed by a newly hired associate program director for POCUS. That initiative includes an expansion of elective courses residents can take

Medicine has built one of the largest and most sought-after Internal Medicine residency programs in the country, with more than 400 trainees at three Manhattan-based hospitals, in addition to 30 fellowship programs across a wealth of specialties.
“We’re constantly thinking about wheremedicine needs to be in 2030 andbeyond, and what our residents will need toknow when they become faculty,”says David C.Thomas, MD, MHPE, Professor of Medicine (General Internal Medicine) at Icahn Mount Sinai, Dean for MedicalEducation, and System Vice Chair for Education for the Department of Medicine. “Through innovative
to ensure both didactic and hands-on experience with the sophisticated machines during their clinical rotations. The program also acquired two hand-held ultrasound devices, giving them access to training opportunities in more ways than ever before.
Also launched in recent years were several primary care tracks that, in addition to providing broad-basedclinical education, are helpingto change the notion of what good doctoring looks like in communities.
“Ourgoalis toencouragemoreresidentsto pursuecareersinprimarycare, whichis alwaysachallengeformedicine,”acknowledges
JohnAndrilli, MD, AssociateProfessor ofMedicine (GeneralInternalMedicine)at IcahnMount Sinai andDirectorof theInternalMedicineResidency ProgramatMountSinaiMorningsideandMount SinaiWest. “Ourresidentsnot onlyspendmore timeinprimarycareofficesthanother residents, butactually gooutintothecommunitytospenda dayor twoat seniorcitizencentersor towork closelywithotherlocalpartnerstounderstandthe typeofcareandservicespatientsarereceiving.”
According to Dr. Thomas, that type of outreach extends to residencies at The MountSinai Hospital as well as Mount Sinai Morningside and Mount Sinai West. “In addition totheir medicine component, our programs have a strong emphasis on understanding apatient’s social determinants and sendingtrainees into the communityto learn more,” he explains. With their feet on the ground, Mount Sinai residents have become actively involved in diabetes andhypertension screening and management programs, for example, as well as exploringthe socialbarriers to health carethat many community members face.
For studentsinsearchofaspecialtythat urgently needsmorepractitioners(suchas primarycare), geriatricsoffersafour-yearprogramthat incorporatesbothresidencyandfellowshiptraining.
Enhancingits appeal isthefactthatMountSinai’s BrookdaleDepartmentofGeriatricsandPalliative MedicineisconsistentlyrankedNo.1inthecountry by U.S. News & World Report®. “We’reinour secondyear ofrecruitingresidentswhowant to pursuecareersingeriatrics,”saysDr.Andrilli, “and areextremelyexcitedabout thewayswe’re growingthisprogram.”
Transgender medicine is another discipline where residents and fellows can get highly specialized training at one of the nation’s leading sites, the Mount Sinai Center for Transgender Medicine and Surgery. Embedded in that curriculum is exposure to a wide range of disciplines that are integral to delivering care to transgender and nonbinary people.
“Weadded gender-affirming care to our ambulatory curriculum this past year and hired faculty to develop an educationalprogram that integrates subspecialties such as endocrinology, urology, plastic surgery, behavioral health, and other supportive services,” says Sreekala Raghavan, MD, Associate Professor of Medicine (GeneralInternal Medicine), and Medical Education, at Icahn Mount Sinai and Director of the Internal Medicine Residency Program at MountSinai Beth Israel

As a large academic institution, Mount Sinai is also able to offer its trainees vast research opportunities that combine scholarly projects in countless investigative fields with evidence-based medicine and the experience of publishing their work for a national audience. Toguide their research and clinicaleducation, residents benefit from a highly structuredmentorship program tailored to their academic and clinical directions.
“Havingalargefacultymeanswe’reabletolink them tomentorsspanningtraditionalspecialties suchascardiologyandoncology,aswellasto nontraditionalfieldssuch asaddictionmedicine andweight management,” observes Dr.Raghavan. Indeed, traineescouldendupwithfiveor six mentors,eachwithadifferentfocus.
“Residents and fellows are ableto avail themselves of somuchwithin our healthcare system, including patients and pathologies that are among the most diverse inthe country,” emphasizes Dr. Thomas, who helped found the East Harlem Health Outreach Partnership, a student-run, attending-directed free clinicfor uninsured individuals. “As a result, we’ve seen amazing outcomes from our trainees who typically go on torewarding roles as physicians serving patients andtheir communities.”
Helping to ensure the steady growth and success of The Mount Sinai Hospital’s Internal Medicine Residency Program is the recent appointment of its new Program Director, Adrian Majid, MD. His passion for teaching and commitment to the professional and personal development of his trainees over the years are seen as a perfect fit for Mount Sinai’s nationally recognized residency program.
* Starting in July 2024, the Mount Sinai Beth Israel internal medicineresidency program will mergewith that ofMount Sinai Morningside andMountSinai West becoming the largest program of its kind in the United States.




DavidC.Thomas,MD, MHPE
Professor of Medicine (General Internal Medicine); System Vice Chairfor Education, Department of Medicine
Dean for Medical Education, MountSinai Health System
JohnAndrilli,MD
Associate Professor of Medicine (General Internal Medicine); Internal Medicine Residency Program Director, Mount Sinai Morningside and MountSinai West
SreekalaRaghavan, MD
Associate Professor of Medicine (General Internal Medicine), and Medical Education; Internal Medicine Residency Program Director, Mount Sinai Beth Israel
AdrianMajid,MD
Associate Professor of Medicine (Infectious Diseases); Internal Medicine Residency Program Director, The Mount Sinai Hospital

The Department of Medicine at the Icahn School of Medicine at Mount Sinai is not just helping to recruit top-flight talent, but working to change the culture ofthe institution and promote inclusive excellence. Initiatives include expanding thepool of people interested in doing theirtraining or research at Mount Sinai,and supporting them along that pathway through mentoring, networking, and other professional development opportunities.
The long-range success of the Icahn School of Medicine at Mount Sinai is rooted in its ability to attract the best and brightest students, trainees, and faculty. To that end,no organization within the institution has proven amore valuable ally than the Department of Medicine’s Diversity, Equity, and Inclusion (DEI) program. By taking full advantage of an array of national and homegrown career development initiatives, it has expanded the pipeline of future leaders, particularly from minority and underrepresented communities.
“We’re not just helping torecruit top-flight talent, but leveragingour program to showhow we can, over time, change the culture of our institutionand promote inclusive excellence,” says Kirk Campbell, MD, Irene and Dr. Arthur M. Fishberg Professor of Medicine and Former System Vice Chair for Diversity,Equity, and Inclusion in the Department of Medicine. “That means building a diverse workforce by expanding the pool of people interested in doing theirtraining or research here, and supporting them along that pathway through mentoring, networking, and other professional development opportunities.”
The active participation in the National Institutes of Health (NIH)-funded FIRST Program by the Department’s DEI initiative drives home the point. Through FIRST (acronym for Faculty Institutional Recruitment for Sustainable Transformation), Mount Sinai recruits andhires 12 early stage investigators from underrepresentedgroupsfor biomedical research. The Department of Medicine is front andcenterin this expanding program, which is focused on thefields of neuroscience, cancer, infectious disease, and health equity— perfect fits for MountSinai since each is a source of strength under its scientific umbrella, as well as a major NIH-funded priority. Specifically, the Department oversees the FIRST Faculty Development Core, which implements the education, training, mentorship, and networking activities of NIH FIRST faculty across the institution. Activities include individualized coaching, research team management guidance, and mentor training.
NIH FIRST is also a fitting complement to Mount Sinai’s own Biomedical Laureates Program, which recruitsjunior and seniorfaculty from traditionally underrepresented populations.
“Both programs significantly bolster our ability to attract the highest-caliber faculty from diverse backgrounds,” affirms Dr. Campbell. “They’re also a huge asset to our biomedical research by bringing into our academic environment people with unique perspectives, talents, and research interests.”
MountSinaiisfurtherpushingtheenvelopefor amorediverseworkforcethroughitsongoing sponsorshipoftheStudentNationalMedical Association(SNMA). Aspart ofthateffort, Icahn MountSinaihasincreaseditsprofileat theannual conferencesofbothSNMAandHowardUniversity CollegeofMedicine.SNMAisthelargestgathering of minority-groupmedicalandpremedicalstudents intheUnitedStates,andMountSinai’sboothatits conferencerecentlydrewseveralhundred prospectiveapplicantsfor its trainingprograms, withmanyexpressinganinterest ininternal medicineanditssubspecialites.
Icahn Mount Sinai has also made asignificant investment intheVisiting Electives Program for Students Underrepresented inMedicine (VEPSUM). This initiative helps feedthe school’s recruitment pipeline for residents while giving talentedfourth-year medical students from across the countrythe chanceto access excellent fourweek elective programsat Icahn Mount Sinai, choosing among a wealth of specialized fields, from emergency andfamily medicine toneurology, pediatrics, and pathology. The institution has been particularly successful inrecruiting VEPSUM studentsto its Internal Medicine and Med/Peds residency programs.
The DEI program is particularly proud of its work around mentoring, which links underrepresented and disadvantaged trainees with leaders in the Department of Medicine for valuable career guidance.

and Dr. Arthur M.
“We aregrooming futurefaculty by pairing them with leaders who serve as full-fledged sponsors rather than just scholarly project mentors,” emphasizes Dr. Campbell, “which allows our trainees to get themost out of their experience at Mount Sinai. They come to view us as a home for their future academic careers, andthat has turned into amajor strength for our institution.”

* As of May 1, 2024, Mirna Mohanraj,MD; Associate Professor of Medicine, was appointed as the new System Vice Chair for Diversity, Equity, and Inclusion in the Department of Medicine

Mount Sinai’s Department of Medicine is working to ease the transition from fellow to faculty, through supportive programs and tailored pathways designed togivejunior faculty members the traction, confidence, and resources they need to launch theirprofessional careers.
The road from fellow tofaculty is more challenging than ever for physician-scientists as they run the gantlet of applying for research funding, keeping up with ongoing training, and meeting the demands of the clinic, which compete with protected time in theresearch lab.
Mount Sinai’s Department of Medicine is working exceptionally hard to ease that burdenthrough supportiveprograms andtailored pathways designed to give junior faculty members the traction, confidence, and resources they need to launch theirprofessional careers.
“Our field is losing largenumbers of physicianscientists at a timewhen we should be nurturing more of them,” says Benjamin K. Chen, MD, PhD, System Vice Chair for Research of the Department of Medicine, and Irene and Dr. Arthur M. Fishberg Professor of Medicine at the Icahn School of Medicine at Mount Sinai. “The Department of Medicine has investedheavily in developing and transitioning our junior faculty through mentoring, grant-writing, and other
creativeways to support them along the long road to becoming independent researchers.”
AmongthemostvitalwaysistheJunior Faculty MentorshipProgram.Senior facultymentors,most of whomarespeciallytrainedfortheseroles,serve asmentorsandadvisors.Theyhelpmenteesput togetherathoughtfulIndividualDevelopmentPlan (IDP),similartowhat theNationalInstitutesof Health(NIH)hasincorporatedintoits degreegrantingprograms. “We try to tailor these IDPs to the more advanced research needs of junior faculty as they transition to their new role of independent investigator,” explains Dr. Chen.
To that end, the main goal of the programis to put junior faculty researchers on a track that makes them competitivefor independent grant funding. MountSinai is paving the way through a range of constructive programs, including grant-writing workshops, which bring in outside experts to help junior faculty hone theirgrant-writing skills through both classroom and individual instruction. This training is especially geared to the NIHK series of
career development awards, which aretypically awarded in the early stages of a scientist's career.
Reinforcing that effort is a unique Grants-Work-InProgress program, a biweekly series of seminars that allow grant applicants to air their ideas and get valuablefeedback from junior faculty peers at the same level of training, as well as from their own mentors or, in many cases, team ofmentors.
That training can again prove crucial once they have a career development (K-type) award in hand and are now making the “Kto R” transition to independent researcher, vying for R01 grants. To further bolsterthe pipeline of new physicianscientists, the Department of Medicine is planning a new supportive program for medical residents through a program known as StARR(Stimulating Access to Research during Residency). Expected soon through this vehicleis funding for a National Heart, Lung, and Blood Institute grant that ensures protected research timeduring residency training.
Junior faculty development is alsobeing leveraged to helpthe Department of Medicine achieve a more diverse investigative team. The mainstay here is the NIH FIRST (Faculty Institutional Recruitment for Sustainable Transformation) Program, which Mount Sinai departments actively participatein to recruit and hire 12 early stage investigators from underrepresentedgroupsfor biomedical research.
“Because our FIRST faculty members are often straight from postdoc programs and haven’t necessarily written grant proposals, we provide them with individualized transition support as we do for our junior faculty,” notes Dr. Chen, who coleads Mount Sinai’s FIRST Faculty Development Core implementing training, mentorship, and networking activities forFIRST faculty across the institution. “Through FIRST we’ve been able to get some amazingly accomplished junior faculty, and we’re working to ensure they have access to the resourcesthey need—particularly grant training— to make the leap to independence.”
The support network Dr. Chen and his team have put in place has yielded impressiveresults for all junior faculty. “We’ve enjoyed ongoing success by maintaining a robust pipeline of K awards, as well as a strong K-to-Rtransition rate,”he observes. “But we’re always trying to do better.”

Irene and Dr. Arthur M. Fishberg Professor of Medicine; System Vice Chairfor Research, Department of Medicine


Burnout, as wellas such issues as career development, work-life balance,promotions, and tenure, can affect not just the overall job satisfaction of faculty members at academic health centers, but their ability to care effectively for patients. At the Icahn School of Medicine at Mount Sinai’s Department of Medicine, the Office of Faculty Affairs is workingto address thesechallenges.
Allacademicmedicalcenters faceacommon challengetoday:thegruelingworkloads andlong hours spentinthelab, hospital, andclinicbyfaculty members canoftenleadtoexhaustionandburnout.
In the Icahn School of Medicine at Mount Sinai’s Department of Medicine, the Office of Faculty Affairs is carefully attuned to drivers of burnout, as well as to such issues as career development, work-life balance, promotions, and tenure. These can affect not just the overall job satisfaction of faculty but their ability to care effectively for patients. Overlying these variables for Faculty Affairs are the imperatives of employee recruitment and retention, which the office is uniquely equipped to address for its approximately 2,000 faculty members.
“Much of my role is making the jobs offaculty easier so they’re excitedabout coming to work each day and making adifference in the lives of patients,” says Neomi Shah, MD, MPH, Professor of Medicine (Pulmonary, Critical Care and Sleep
Medicine) at Icahn Mount Sinai and System Vice Chair for Faculty Affairs in the Department of Medicine. “Retention, in particular, is an acrossthe-boardproblem inthe field of healthcare now, and we’re working hard to solve it by improving the workplace culture for all of our faculty.”
Serving as thechampions of this effort arethe members of the FacultyWell-Being Committee, who havebeen named to represent their respective medical divisions, advocating for and expressing at the highest levels the needs, interests, and concernsof their colleagues.
“Well-Being Champions enable us to understand what the pressing issues areamong our faculty with regard to workplaceculture and efficiency, burnout, turnover, and much more,” explains Krishna Chokshi, MD, MS, Assistant Professor of Medicine (HospitalMedicine) at Icahn Mount Sinai and Faculty Well-being Director for the Department of Medicine.

Dr. Chokshiis developing a significant expansion of the faculty well-being program, using data collected by each clinical department to drive new projects and strategies in such areas as enhancing work-life balance, improving faculty appreciation efforts, andincreasing psychological safety among teams.
Mentoring is another critical touchpoint for the Office of Faculty Affairs. Already in place isa highly developed mentorship program that helps connect junior faculty to experienced clinical, educational, and/or research experts who can help them set career goals and support them at each step along the way.
“We put a lot of emphasis on helping junior faculty at the outset identify—and then grow with—the most appropriate mentors to show we’re as committed as they are tomoving their careers forward,” says Jenny J.Lin, MD, MPH, Professor of Medicine (General Internal Medicine) at Icahn Mount Sinai and System Director for Mentoring in the Department of Medicine. Tomake an established program even stronger, Dr.Lin has been focused on building a formal mentor-training component through seminars that encourage mentors to thoughtfully assess and thenhone the skills they’llneed to become moreeffective coaches and advocates for the faculty members under their wings.
Ensuring that all facultymembers aretreated equitably when it comes to appointments, promotions, and tenurealso comes under the wide-ranging umbrella of the Office of Faculty Affairs. And here, specialdiversity, equity,and inclusion (DEI) training has been introduced for members of the Department’s promotions committee. “We’ve recently trained our committee to view all applications in atotally transparent and equitable fashion,” notes Dr. Shah, adding that another program is beingrolled out to require every faculty member inthe Department to engage in three hours of DEI-related training or activities annually.
“We’re all working toward creating an environment that allows each facultymember to moveup the academic ladder fairly and in tune with their career goals,” points out Dr. Shah. “And that means using all the resources available to us at Faculty Affairs to ensure our faculty remain healthy and motivated so they’re able toheal others.”



NeomiShah,MD, MPH
Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine); System Vice Chairfor Faculty Affairs, Department of Medicine
KrishnaChokshi,MD, MS
Assistant Professor of Medicine (Hospital Medicine)
Director for Faculty Wellbeing in the Department of Medicine
JennyJ.Lin, MD,MPH
Professor of Medicine (General Internal Medicine) Director for Mentoring in the Department of Medicine

Mount Sinai's Department of Medicine has brought more than 100 post-pandemic projects to fruition that have achieved widespread improvements in the performance of services, systems, and processes that directly impact the quality of careprovided to patients.
From chronic disease screening to mortality review to hypertension control, the Department of Medicine’s Office of Quality and Patient Safety at Mount Sinai Health System has been extraordinarily active, bringing more than 100 post-pandemic projects to fruition that have achieved widespread improvements in the performance of services, systems, and processes that directly impact the quality of care provided to patients.
“These projects were successfully managed by our 38 Quality Champions who work closely with faculty, fellows, and residents at our hospitals,” says Beth Raucher, MD, Professor of Medicine (Infectious Diseases) at the Icahn School of Medicine at Mount Sinai and System Vice Chair for Quality and Clinical Affairs. “In the case of screening, monitoring, and educating patients with chronic disease, for example, that commitment translated into outstanding results by building best practices and quality measures
into each program.” Dr. Raucher leads a team of quality and data specialists who support the projects at each of the hospitals.
Mortality review reflects the breadth and depth of these initiatives. Led by on-site Quality Champions, each hospital death triggers an intense review todetermine whether all standards of care were met and where opportunities to improve systems of caremay lie. At the center of this process arethe Quality Improvement Peer Review Committees at each hospital, which meet monthlytoreview cases referred to them after an initialreview by a faculty member in the Division of Hospital Medicine
“What makes our program unique isthat residents, interns, nurses, and other hospital staff are brought into the review process in a collaborative, safe, and transparent learning environment,” observesVinh-Tung Nguyen, MD, Co-Chair of theQuality Improvement Committee

at The Mount Sinai Hospital. “We disseminate these lessons learned through improvement projects, didactics, or written policy changes based on our findings.”
The Office of Quality Improvement and Patient Safety also seeks to prevent future quality and performance missteps by daily monitoring of an internal website that reports safety concerns over the previous 24 hours—events that range from the seemingly trivial (a patient’s broken TV) to the more concerning (a patient who falls, or is given wrong medication). “Oftentimes we’re on top of these events before the hospital is,” says Umar Jalloh, MPA, Manager of Performance Improvement and Research, and a member of Dr. Raucher’s team who conducts the surveillance and briefs site quality leaders in the early morning for potential follow-up.
In amore proactive vein, the department’s quality and safety teams work to improve chronic disease management through robust efforts to control hypertension, diabetes,and hepatitis at each Mount Sinai hospital.
In the case of hypertension, for example, Amy Rosenberg, MD, Associate Chairfor AdministrativeAffairs, Department of Medicine at Mount Sinai Morningside and Mount Sinai West, observed that one of thequality projects focused on provider education by consistentlyreminding the professionalstaff about tools available to help them improve blood pressure management. These include remote homemonitoring of patients with higher-than-normal blood pressure, as wellas telehealth counseling to ensurethey remain on their medications. Another tool is direct telephone outreach to uncontrolled hypertensivepatients with the goal of bringing them back to the officefor follow-up checks by either a provider, nurse, or clinical pharmacist. Mount SinaiMorningside and Mount Sinai West achieved tremendous success with their programs by bringing at least 70 percent of hypertensive patients under the goalof 140/90 in 2022. Other practice sites also reached comparabletarget compliance.
Decreasing hemoglobin A1C (HbA1c)levels of diabetic patientsto less than 9 percent was a core goalof the quality teamat Mount Sinai Beth Israel’s Division of General Internal Medicine. Certified Diabetes Educators werepivotal to this effort, instilling in patients best practices for managing their condition and preventing complications.Moreover, the diabetes careteam employed continuous glucosemonitoring to improve patient motivation and knowledge of how food affects blood sugar. Providers werealso encouraged to schedulefrequent appointments with patients toclosely monitor their progress, while language interpreters weredeployed to improve outreach and care to non-English speaking patients.
Identifying individuals with hepatitis B or C—who are often unaware they have the disease—was a priority for the quality team in the Division of Liver Diseases at The Mount Sinai Hospital. In a city where more than 91,000people have chronic hepatitis C(HCV) infection, the Liver project team worked to increase therate at which patients are screened and,consequently, treatedfor their infections. Part of this strategy involved alerting providers to new Centers for Disease Control and Prevention guidelines encouraging HCV testing for all adults over 18 at least once intheir lifetime. Furthermore, providers were sent a list of screening-eligible patients with upcoming office appointments. HCV screening was also promoted to patients via social media and on monitors throughout the hospital campus. This project is nowbeing rolled out to the other hospitals in the Health System.
The Division of Pulmonary, Critical Care and Sleep Medicine at The Mount Sinai Hospital helped decrease the amount of timepatients need to wait for sleep testing by streamlining the scheduling workflowand optimizing Epic-referral work queues. Sleep studies are inhigh demand because they help to diagnose sleep disorders and can ultimatelyimprove patients’ quality of life. Jing Wang, MD, Co-Chair ofthe Quality Improvement Committeeat The Mount Sinai
Hospital, explained, “Sleep studies shed light on the underlying causes of sleep disorders to help us identify tailored interventions that lead to more restful and rejuvenatingsleep for our patients. Giving patients the tools to reclaim their nights leads to improved overallwell-being and a higher quality of life.”
The Department has also achieved major improvements around osteoporosis evaluation and education of patients admitted with hip fractures. At Mount Sinai Morningside and Mount Sinai West, the quality team in the Division of Endocrinology, Diabetes and Bone Disease informed patients of fall risk and fall prevention, and patients were given nutritional advice about calcium and vitamin D upon discharge. At the same time, providers were encouraged to add fragility fracture and osteoporosis as diagnoses in their discharge paperwork, and to refer the patient to endocrinology for further evaluation and treatment.
Particularly impressivein termsof qualitycare improvementwaswhat thePeterKruegerClinic partoftheInstituteforAdvancedMedicine,which
specializesininfectiousdiseasetreatmentand management—achievedinviralloadsuppression forpatientslivingwithHIV. Theclinicrecordeda67 percent reductioninthenumberofpatientswith unsuppressedviralloads throughthethirdquarter of 2022,comparedtoallof 2021. Responsiblefor thisdramaticshiftweresuchinterventions asactive patientmonitoringandoutreachtopatients to scheduleappointmentsandtoconfirmtheyare takingtheirantiviralmedications.
“The success of this program was shared by Peter Krueger with othersites withinthe Institute for Advanced Medicine and resulted in amazing across-the-board reductions in viral load,” says Patricia Dharapak, MD, Associate Professor of Medicine (GeneralInternal Medicine, and Hospital Medicine), and Chief of Quality for the Department of Medicine at MountSinai Beth Israel. “It’s another great example of how our teamof Quality Champions is significantly improving thewellbeing of patients across Mount Sinai through interventions that bringthem up to the stringent standards our organization has set.”



BethRaucher,MD
Professor of Medicine (Infectious Diseases); Vice Chair forQuality and Clinical Affairs, Department of Medicine

Vinh-TungNguyen, MD
Associate Professor of Medicine (Hospital Medicine)

AmyRosenberg,MD
Professor of Medicine (Infectious Diseases)
JingWang,MD
Associate Professor of Medicine (Pulmonary, Critical Care and Sleep Medicine)
PatriciaDharapak,MD
Associate Professor of Medicine (GeneralInternal Medicine, and Hospital Medicine)

A 20-member contingent from Mount Sinai Health System is working to improve the public health system in Guyana, one of South America's poorest countries.
Zijian Chen, MD, is an extremely busy endocrinologist atMount Sinai Beth Israel. He not only sees patients and serves as Site Director for Endocrinology and Rheumatology, but also heads up theMount Sinai Health System’s Center for Post-COVID Care
Why, then, is this much-in-demand professional 2,600 miles away in the remote nation of Guyana for severalweeks eachyear?
In one way, it’s no different from what he does in New York—advancing health care to promote a better quality of life for patients. Except in Guyana, the focus is on one of South America’s poorest populations within aresource-strapped environment. Dr. Chen is part of a20-member contingent from Mount Sinai International, which seeks toimprove localmedical care around the globe, and Mount Sinai’s ArnholdInstitutefor Global Health
“Our entire team is committed to elevating Guyana’s health care system, whether it’s by improving its supply chain for acquiring
medications and equipment, or by helping its doctors take better care of patients through enhanced education and updated medical practice guidelines,” says Dr. Chen. “I’m a diabetes specialist, so my role as part of an eight-member workstream is to rewrite the guidelines for diabetes management and to train doctors so they can become trainers for other providers and health care workers on the front lines.”
That mission has brought Dr. Chen and his colleagues to Guyana, anation of 741,800 in the northeastern corner of South America, threetimes over the past year for one-week visits, with at least twomore planned for the remainder of this year. While on the ground, they collaboratewith other physicians and administrators at Georgetown Public Hospital in the nation’s capital, while also traveling to local clinics and what are known as “healthposts” further inland in the hinterlands or the rainforest.
Already, thesejourneysare having an impact, especially in the field of diabetes.

“We’ve completed theguidelines, which will change theway diabetes care is delivered in the country, now and down the road,”reports Dr. Chen. “And thetraining we’ve started willbuild knowledge and expertise within the medical community, allowing doctors to focus on early detection andtreatment of diabetes, instead of end-stage complications involving dialysis and amputations. That’san advantage the peopleof Guyana have never hadbefore, and thethought of making that kind of difference in their lives is the most rewarding thing for all of us on the Mount Sinai team.”

ZijianChen,MD Assistant Professorof Medicine (Endocrinology, Diabetes, and Bone Disease); Medical Director,
Center for Post-COVIDCare


ClickheretosupporttheMountSinaiDepartment ofMedicine'sclinical,education,andresearchgoals.