FALL 2024


FALL 2024

THE MAGAZINE OF THE UNIVERSITY OF MARYLAND SCHOOL OF NURSING
This is a banner milestone year for UMSON, as the School celebrates not only its 135th anniversary (founded in 1889) but also the 45th anniversary of the Doctor of Philosophy program (ours was among the first 16 nursing PhD programs in the nation) and the 25th anniversary of the Living History Museum (see Page 28). We have already begun the many related celebrations, which will continue into the spring. In the meantime, we invite you to join us in festive commemoration by putting your UMSON knowledge to the test.
You’ll find the answers to these trivia questions scattered among the pages of this issue — just look for the balloon icon in the margins.
We’ve left the last question unanswered. Send us your answer to be entered for a chance to win an UMSON-themed prize.
1 When did the School of Nursing first adopt multimedia learning?
2 What was the name of the first simulation manikin used by the School of Nursing?
3 What does WRAIN stand for and what role did UMSON play in the Vietnam War?

4 When were pantsuits first allowed as uniforms for graduate nurses at University Hospital?
5 When did UMSON launch its BSN program?
6 When did the School of Nursing offer its first web-based course? Email us your answer at NRSCommunications @umaryland.edu


Building Trust in Crisis
Simulation offers UMSON students an authentic experience in state-of-the-art facilities to practice in a safe space, preparing them for excellence in the workplace. Take a peek behind the curtain to understand how it all works.
UMSON faculty members and students are championing a traumainformed care approach to nursing practice, which considers not only patients’ illnesses or injuries but their full life experiences – and recognizes and responds to the continuing impact of trauma.
A Special Partnership with Special Olympics Community Partner Spotlight Summer Global Field Experiences Building the Pathway with K-12 Schools
Combatting Chemotherapy Symptoms with Exercise Dismantling the Negative Power of Nocebos Inspired to Teach
Class Notes Alumni Profiles: The Heart of Research Embracing AI to Combat Health Disparities Events
Donor Profile: You Can Do Anything Legacy Society Honor Roll of Donors


The fall is always an exciting time of year, with students, faculty, and staff returning from summer with a sense of a new beginning. As we embrace the beauty of the season and a new semester – and our 135th anniversary – it is also a good time for reflection, refreshment, and hope.
As I enter my second year as dean, I look back at all that I learned during my first year. I had great moments of joy meeting with students, faculty, staff, and alumni during my many listening sessions. From students, I heard stories of social cohesion with peers and gratitude for faculty and staff who create an environment that is responsive and supportive. They also shared opportunities for our school to grow, expressing a desire for more information, communication, and connections.
Our alumni’s engagement is inspiring, and I was grateful to meet with more than 700 graduates. From our museum docents – who shared their recommendations for addressing workforce challenges – to young alumni – who attended an Orioles baseball game or an evening event at a local restaurant and shared post-pandemic stories of entering the workforce – it was great to hear their perspectives on the future of nursing and understand how it is so interconnected with our history. Many of our alumni expressed the desire to be more actively involved in our School, and through our UMSON Connect platform, we are linking them to opportunities to serve as preceptors and to inspire current students through interviews or letters or as donors to our Welcome Ceremonies or the Student Emergency Fund, which assists with food, transportation, and housing needs.
Our amazing faculty and staff are the heart of our School and the key to student success. Their commitment to excellence is undeniable. From our faculty and clinical partners, I heard a shared commitment to supporting students on their nursing school journey.
As you will read in the pages that follow, UMSON continues to thrive with new opportunities for learning and teaching, research, practice, and community engagement. We have begun a unique residency program for new faculty and continue our support for nurse faculty statewide, preparing nurses for teaching roles in Maryland nursing schools and for educator roles in clinical settings. Our research and scholarship program is flourishing with grants in maternal-child health, aging populations, and translational research and symptom science. And we continue our multiple health equity and community engagement partnerships, including projects with local libraries, Head Start programs, and community and faith-based institutions through the West Baltimore RICH Collaborative, as well as a program with the Special Olympics.
So, as I close the chapter on the last academic year and begin afresh, I look forward to another year of collaboration and action with colleagues, alumni, and external and community partners. Building on our 135-year legacy, we have many great reasons to move forward with hope.

Yolanda
Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN
The
Bill and Joanne Conway Dean of the University of Maryland School of Nursing
NURSING FOR/UM is published by the University of Maryland School of Nursing.
EDITOR-IN-CHIEF
Giordana Segneri
ASSOCIATE EDITORS
Jillian Dreicer
Erin Merino
Mary Therese Phelan
EDITORIAL BOARD
Stacey Conrad
Yvette Conyers
Amy Daniels
Elizabeth Galik
Jana Goodwin
Veronica Gutchell
Charlotte Nwogwugwu
Yolanda Ogbolu
Deborah Prout
Cynthia Renn
Barbara Resnick
Jennifer Schum
Cynthia Sikorski
Susan Wozenski
CONTRIBUTORS
Stacey Conrad
Nicole Nash
Deborah Prout
Lorrie Voytek
DESIGN
Skelton Sprouls
We welcome comments, suggestions, and story ideas from alumni, partners, and friends.
Send correspondence to Giordana Segneri, Editor-in-Chief, at nrscommunications@umaryland.edu or 410-706-4115.
© University of Maryland School of Nursing, 2024
UMSON Joins Forces with Special Olympics to Advance Equitable Care for Those with Disabilities
BY EMILY BLEIWEIS
Data shows just how necessary it is to ensure students who are working toward degrees in health and human services fields are educated to care for populations with intellectual and developmental disabilities (IDD) – who often face barriers when it comes to receiving treatment.
The American Nurses Association issued a revised position statement in 2019 on “Nurse’s Role in Providing Ethically and Developmentally Appropriate Care to People with IDD,” stating “Because of cognitive, physical, and communication challenges often faced by people with IDD, nurses must be sensitive to needs across the lifespan and in all settings. … Nurses must provide compassionate, comprehensive, and person-centered care to all people, inclusive of at-risk populations such as people with IDD who experience health disparities across practice settings.”
The Standardized Patient (SP) Program – housed at UMSON, a collaboration with the University of Maryland School of Medicine – in partnership with Special Olympics (SO) Maryland and SO International is working to ensure that the next generation of health care professionals is well prepared to work with and treat individuals with IDD, making the University of Maryland, Baltimore (UMB) only one of five universities in the country to partner with the SO.
The SP Program allows students to refine their clinical and communication skills with professional standardized participants who are trained to portray a patient in clinical instruction and assessment with students.
“Not only is this initiative expanding UMB’s inclusive and interprofessional curriculum, but it’s also breaking
“Not only is this initiative expanding UMB’s inclusive and interprofessional curriculum, but it’s also breaking down barriers, biases, stigmas, and misconceptions, all while encouraging a shared commitment to inclusive health care.”
REBECCA WESTON
down barriers, biases, stigmas, and misconceptions, all while encouraging a shared commitment to inclusive health care,” said Rebecca Weston, EdD, MSN, RN, CNE, assistant professor and principal investigator on the UMB interprofessional seed grant that funded the collaboration.
Last spring, students across multiple disciplines at UMB participated in simulations with SO Health Messenger athletes who were hired to serve as SPs; these athletes are specifically trained to talk about SO health programming and the impact the organization has made on their lives.
This partnership increases the representation of populations with IDD in the SP Program and offers the opportunity for students to practice with the actual representative population, as opposed to someone simulating a population, according to Nancy Budd Culpepper, MBA, director of the SP Program.
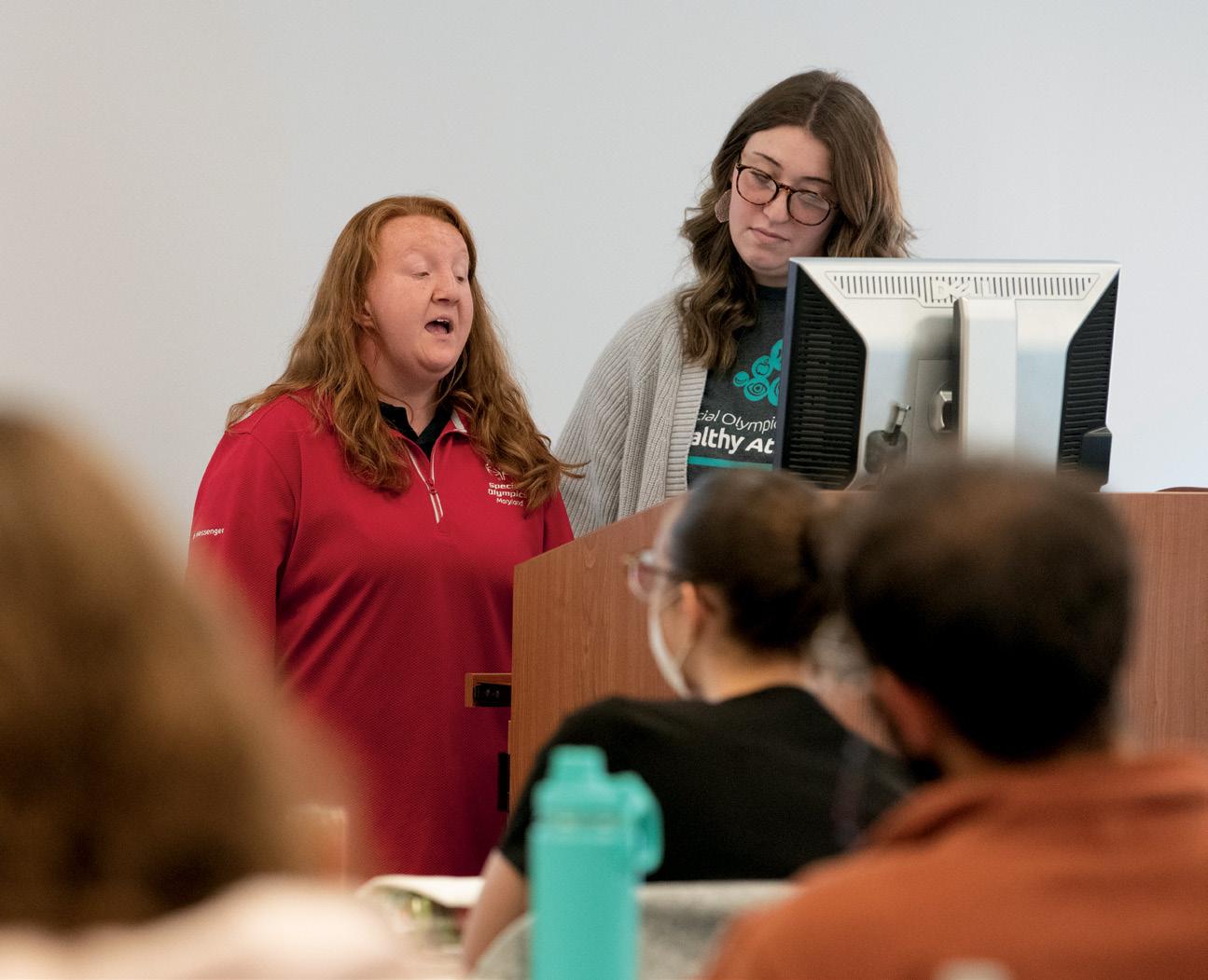
Speaking before a group of UMB students, Alexea Wentz (left), an SO Maryland Health Messenger athlete, and Abigail Bauman, manager, SO Young Athletes Program, discuss the importance of clear communication between health care providers and individuals with IDD.
“Bouncing ideas off of each other just creates a more holistic approach for the patient. I think that just improves the quality of care that we can give the patient.”
HALEY PERLSTEIN

“I think in this situation in particular, it’s not something you would be able to simulate authentically,” Culpepper said. “We have wonderful folks that work for us as SPs with acting backgrounds that can take on a good bit, but I think when you’re working with special populations, it’s tough to give an authentic response.”
Prior to the simulation, students heard from Anne D. Williams, DNP ’12, MS ’86, BSN ’82, RN, CPHQ, FAAN, vice president of health service and education for SO International, who helped lay the groundwork for what challenges those with IDD face, especially when it comes to receiving health care.
Populations with IDD die 16 - 20 years prematurely because of undiagnosed and untreated conditions, Williams said. Due to the stigma that remains around those with disabilities, their quality of and access to care can be compromised.
The participating students interacted with both an existing SP, in the role of a friend or family member of the patient, and an SO Health Messenger, who portrayed the patient. This dynamic is one that’s familiar for those who have IDD. Jimmy Tadlock, an SO Maryland Health Messenger, said his mother attends his doctor’s appointments with him so he and the doctor are communicating effectively. “This is my chance to help new doctors understand when their doctor-speak is not understood,” Tadlock said.
Haley Perlstein, a Bachelor of Science in Nursing student, said what makes this simulation an especially formative educational experience is the ability to work with students across multiple disciplines at UMB. “Bouncing ideas off of each other just creates a more holistic approach for the patient,” Perlstein said. “I think that just improves the quality of care that we can give the patient.”

Interprofessional education is an important, expanding aspect of the SP Program. Bringing together students from different UMB schools to work in a team model is “vital,” Culpepper said. “There’s so much to juggle in the health care system. When you bring them together in a comprehensive way – what an ideal situation.”
UMSON has been awarded a five-year, $5 million Health Equities Resource Communities grant from the Maryland Community Health Resources Commission (CHRC) to support the West Baltimore Reducing Inequities in Cardiovascular and Mental Health Collaborative - Stronger Together (RICH 2.0). This grant builds on the success of the West Baltimore RICH Collaborative, an initiative supported by a $2.4 million Pathways for Health Equity Grant from CHRC awarded two years ago.


Stella was her mother’s name, said former Maryland Sen. Shirley Nathan-Pulliam, DPS (Hon.) ’23, DHL (Hon.), MAS, BSN ’80, RN, FAAN, (right) an inaugural UMSON Visionary Pioneer, who served for nearly 25 years in the Maryland Legislature before retiring in 2019. Stella is also what she called a pivotal character in her autobiographical book released this year, “Saving Stella: Notes from a Nurse Turned Legislator.” The woman, a former patient during Nathan-Pulliam’s career as a bedside nurse, represented “a change in direction for her career,” Nathan-Pulliam said, when she began focusing on activism for health equity. She addressed an audience of UMSON faculty, staff, students, alumni, and others close to the former senator during a book-signing event May 21 for “Saving Stella.” The Office of Equity, Diversity, and Inclusion hosted the event as part of its national award-winning Booked for Lunch book club. Yvette Conyers, DNP, RN, FNP-C, CTN-B, CFCN, CFCS, CNE, FALDN, (left) assistant professor and associate dean for equity, diversity, and inclusion, moderated the discussion.
News from Sigma’s Pi at-Large Chapter at UMSON
UMSON’s Pi-at-Large Chapter has welcomed three new board members:
• Caitlin Donis, PhD, MS ’13, AG-ACNP, ACCNS-AG, assistant professor: treasurer
As with the original initiative, Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, leads the project. The West Baltimore RICH 2.0 aims to:
• address cardiovascular and mental health and three social determinants of health –housing, transportation, and economic stability – through community outreach
• expand partnerships with organizations to meet the need for mental health services and place-based care in senior housing facilities
• expand two mobile health programs for implementation in senior housing sites
• maintain nurse-led clinics throughout the city
• measure community assets, strengths, and resilience, assessing perceptions of hope and their association with social isolation, mental distress, stress, and anxiety.
— Mary Therese Phelan
• Amanda Fabien, MS, RN, CCRN, SRNA, Doctor of Nursing Practice student: chair, Leadership Succession Committee
• Sharon M. Weinstein, MS, RN, CRNI-R, CVP, FACW, FAAN, speaker and coach, SMW Group: chair, Program Planning and Continuing Education.
Over the past year, we continued our collaboration focusing on resilience in nursing with the Nu Beta at-Large Chapter of Sigma at the Johns Hopkins School of Nursing by co-hosting a webinar in February. Katie Boston-Leary, PhD, MBA, MHA, RN, NEA-BC, senior director of nursing programs at the American Nurses Association, addressed nurses’ health and wellbeing. These ongoing sessions enrich professional knowledge and foster collaboration across our institutions.

During the 2023 - 24 academic year, Pi at-Large Chapter welcomed 177 inductees who demonstrated a commitment to nursing excellence.
Pi at-Large Chapter members continue to volunteer at My Sister’s Place Women’s Center in Baltimore and the Greater DC Diaper Bank in Silver Spring, Maryland, contributing to vital community services and supporting vulnerable populations, integral to the chapter’s mission. Both agencies align with Sigma’s commitment to the United Nations’ Sustainable Development Goals, aimed at achieving a more sustainable future for all by 2030.
— Paul A. Thurman, PhD ’18, MSN ’07, RN, ACNPC, CCNS, CCRN, CNE, Assistant Professor and Pi at-Large Chapter President
This summer’s group of 10 UM Scholars is the largest at UMSON since the program began in 2016, resulting in a total of 35 students completing the program, of whom 32 have enrolled at UMSON (or are expected to).
The future of nursing research is looking golden, as a team of 10 UM Scholars, students from the University of Maryland, College Park (UMCP), spent the summer immersed in intensive projects with faculty researchers at the School of Nursing. They presented posters on their results in August, and several matriculated to UMSON this fall. Our take: A Perfect 10! The UM Scholars program, a competitive paid summer internship that connects students from UMCP with faculty throughout the University of Maryland, Baltimore to collaborate on research projects, is part of the University of Maryland Strategic Partnership: MPowering the State Here’s a roundup of what the 10 UM Scholars focused on:
RESEARCH FOCUS
SHARED DECISION-MAKING IN MATERNITY CARE
PAIN
NUTRITION AND CANCER
CANCER SYMPTOMS
FAMILY COMMUNICATION IN SERIOUS PEDIATRIC ILLNESS
HEALTH PROMOTION IN SENIOR HOUSING
—Giordana Segneri
FACULTY MENTOR
Rachel Blankstein Breman, PhD ’18, MPH, RN, FAWHONN
Luana Colloca, MD, PhD, MS
Amber Kleckner, PhD
Ian Kleckner, PhD, MPH
Kim Mooney-Doyle, PhD, RN, CPNP-AC
Barbara Resnick, PhD ’96, RN, CRNP, FAAN, FAANP
UMSON once again ranked in the top 10 across the board for public schools of nursing – and moved up in all six categories in which the School was ranked – in the 2024 edition of U.S. News & World Report’s “America’s Best Graduate Schools,” out of 651 accredited nursing schools surveyed.
Two UMSON specialties led the way in the rankings, both ranked No. 1 (tied) nationwide among public schools of nursing:
• Doctor of Nursing Practice (DNP) Adult-Gerontology Primary Care Nurse Practitioner specialty
• Master of Science in Nursing (MSN) Health Services Leadership and Management specialty.
UMSON is pleased to announce that two faculty members have been named to leadership roles, lending their significant expertise to enhancing teaching and learning, research and scholarship, and the student experience as the School strives to develop leaders in nursing education, research, and practice.

UM SCHOLARS
Lisa Djimou Isabelle Watriss
Princess Atud Megha Chander Kayla Morris
Maria Rangwala
Vanessa Ho

Sara Robinson, DNP, RN, PMHNP-BC
Assistant Professor; Director, Doctor of Nursing Practice - Psychiatric Mental Health Nurse Practitioner Specialty
Charlotte A. Seckman, PhD, RN, NI-BC, CNE, FAAN
Associate Professor; Co-Director, Master of Science in NursingNursing Informatics Specialty

Nicolette Friedrich Khang Tran
Sylvia Joledo
UMSON also ranked in the top 10 among public schools of nursing for its:
• DNP Program (No. 4, tied)
• MSN Program (No. 9)
• DNP Family Nurse Practitioner specialty (No. 3)
• DNP Nurse Anesthesia specialty (No. 7, tied) M.T.P.
Careers4Nurses: Your Future Job Is Waiting 4 You!
Check out Careers4Nurses, UMSON’s new free online job search and career management platform. It serves as a one-stop shop for searching and applying to positions posted by employers, and it’s available to UMSON alumni and students 24/7.
Careers4Nurses allows you to:
• create an eye-catching profile
• upload resumes, CVs, cover letters, and unofficial transcripts
• search and apply for open positions posted by more than 100 employers – and growing by the day!
• filter searches by title, location, specialty, and employer.
Learn more at nursing.umaryland. edu/careers4nurses.
Answer:
1 In fall 1974, the Instructional Media Lab supported video and audio self-instruction and formed the basis of what is now UMSON’s Information and Learning Technology.
BY GIORDANA SEGNERI
LOCATION: COSTA RICA
WHO: Martine Kirwin, DNP, FNP-BC, RN, assistant professor; B. Elias Snyder, PhD, MS ’14, FNP-BC, ACHPN, assistant professor; six UMSON Bachelor of Science in Nursing students; and one UMSON PhD student
WHEN: June 21 - July 3
WHAT: Traveling from the capital, San José, to areas in the far southern and southwestern reaches of the country, close to the border with Panama, the group explored comparative global health and global learning. This included examining Costa Rica’s national health system and universal health insurance program; understanding migrant and indigenous rights and health issues; unraveling environmental health, including the impacts of crop growth, crop

exportation, and deforestation; and discussing planetary health. The field experience also focused on health equity, inner work, bias, and social justice. Of note was time spent at Asomobi, the Association of Organized Women of Biolley, a women’s entrepreneurial organization that started coffee farming and roasting to transform their community.

LOCATION: NIGERIA
WHO: Charlotte Nwogwugwu, DrPH, BSN, RN, HIV PCP, CPH-BC, assistant professor and interim director, Office of Global Health and Global Health Certificate; and two Master of Public Health students, one from the University of Maryland, Baltimore (UMB) and one from the University of New Haven (Connecticut)
WHEN: July 6 - 22
WHAT: As part of Nwogwugwu’s The BRAVE Project – Building Resilience and AIDS Care Through Mental Health Valor and Empowerment – supported by a UMB President’s Global Impact Fund grant, she involved the students in various site visits, collecting data at HIV clinics in Nigeria’s Imo State, during the first week. In week two, the students participated in a residential workshop in Owerri, serving as facilitators for a five-day intensive training on mental health. The BRAVE Project aims to integrate mental health services in HIV care by building the capacity of doctors, nurses, and community health extension workers in clinics to assess, diagnose, treat, and refer patients presenting with mental health conditions. It also involves collaborations with local strategic partners involved in ending the HIV epidemic.

clockwise from far left: students in Costa Rica examined the environmental health impacts of crop growing and exportation; students and faculty took in the view over palm oil plantations and the InterAmerican Highway in Costa Rica; Nwogwugwu (right) provided direction to the participating students during their time in Nigeria.
“Through her research and scholarship, her teaching and mentoring, and her service, she has brought national and international recognition and true distinction to the University.”
YOLANDA OGBOLU
Susan G. Dorsey, PhD ’01, MS ’98, RN, FAAN, professor, has been named by University of Maryland, Baltimore (UMB) President Bruce E. Jarrell, MD, FACS, as one of six 2024 Distinguished University Professors, the highest appointment bestowed on a faculty member at UMB. It recognizes Dorsey’s excellence, impact, and significant contributions to the nursing profession and practice.

In addition to her appointment at UMSON, Dorsey is a professor in the Department of Anesthesiology and the Department of Medicine at the University of Maryland School of Medicine and in the Department of Neural and Pain Sciences at the University of Maryland School of Dentistry.
She is nationally and internationally recognized for her research and scholarship related to chronic pain and for developing strategies for the use of multiomics (e.g., genomic, transcriptomic, epigenomic, metabolomic) methods to identify the biological mechanisms underlying symptoms and the self-management of symptoms. Her research has been consistently funded by the National Institutes of Health, which has awarded her more than $30 million as principal investigator or co-principal investigator.
Dorsey joined UMSON in 2004 and served as founding chair of its Department of Pain and Translational Symptom Science from 2014 - 22. She also was the founding co-director of the UMB Center to Advance Chronic Pain Research and assisted in securing funding from the National Institute of Nursing Research to create the center.
“Through her research and scholarship, her teaching and mentoring, and her service, she has brought national and international recognition and true distinction to the University,” wrote Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, in her letter of nomination. “She is highly deserving of the honor.”
Dorsey received her Distinguished University Professor medal from Jarrell, a blacksmith who created the medal himself, during UMB’s annual Faculty Convocation on Sept. 12.
— M.T.P.

Vanessa Fahie, PhD ’94, MS ’83, BSN ’76, RN, assistant professor, was honored as the University of Maryland School of Nursing Colleague Award recipient at the University of Maryland Medical Center’s (UMMC) Nursing Excellence Awards Ceremony during National Nurses Week in May. Fahie was recognized as an extraordinary partner to UMMC. The event program read, “As a consummate nurse educator, Dr. Fahie has spent decades developing generations of nursing students and opening the nursing pipeline for historically underrepresented groups. Using her passion, moral compass, and enthusiasm as her guide, she has instilled in countless young nurses the cultural competencies required to work with patients and families across diverse backgrounds as well as the highest exemplars of compassionate care. Whether she is securing millions of dollars in grants to introduce Baltimore City students to nursing or mentoring undergraduates to present papers and posters at conferences across the country, her dedication to nursing is unparalleled.”
Fahie was instrumental in assisting UMMC in implementing its Certified Nursing Assistant program and serves as a member of the program’s inaugural faculty, contributing to the development of the program’s successful curriculum.
— G.S.
Six faculty members have been named fellows in 2024:
• Susan L. Bindon, DNP ’11, MS ’96, RN, NPD-BC, CNE, FAAN, ANEF, associate professor and associate dean for faculty development; director, Institute for Educators and Teaching in Nursing and Health Professions Certificate: Academy of Nursing Education Fellow
• Rachel Blankstein Breman, PhD ’18, MPH, RN, FAWHONN, assistant professor: Fellow of the Association of Women’s Health, Obstetric, and Neonatal Nurses
• Yvette Conyers, DNP, RN, FNP-C, CTN-B, CFCN, CFCS, CNE, FADLN, assistant professor and associate dean for equity, diversity, and inclusion: Fellow of the Academy of Diversity Leaders in Nursing
• Bridgitte Gourley, DNP ’08, FNP-BC, FACU, associate professor and director, Doctor of Nursing Practice Family Nurse Practitioner specialty: Fellow of the Association of Clinicians for the Underserved
• Retired Col. Jacqueline C. Mitchell, MS ’07, CRNA, FAANA, director of clinical education: Fellow of the American Association of Nurse Anesthesiology
• Kim Mooney-Doyle, PhD, RN, CPNP-AC, assistant professor: Fellow of the American Academy of Nursing (induction scheduled for early November)



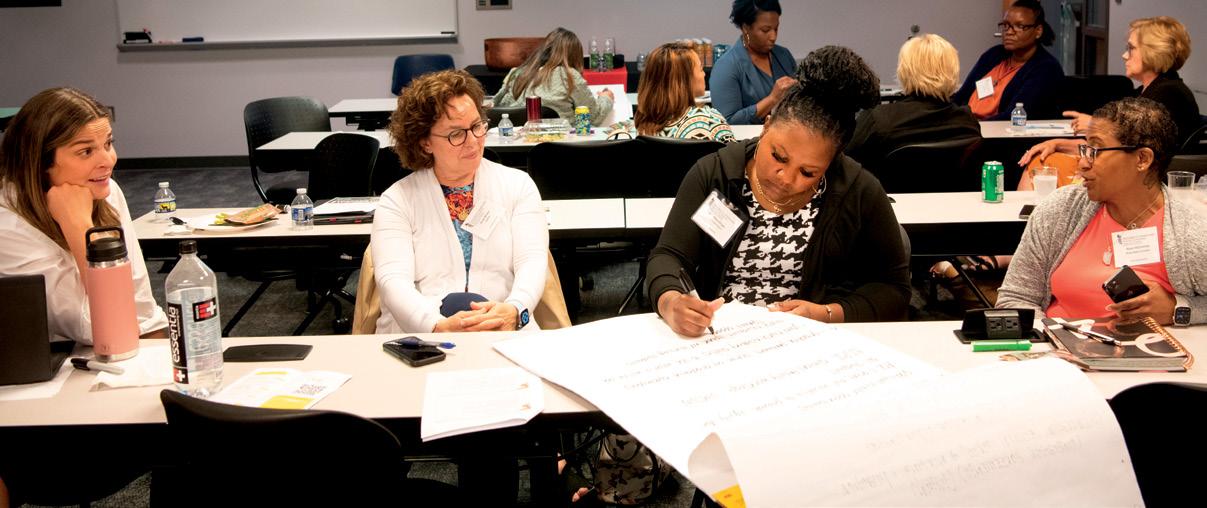
Attendees at the inaugural State of the Maryland Nursing Workforce Symposium on June 6 generated ideas for building successful academic-practice partnerships during a breakout session on nurse education/professional development and creating sustainable and mutually beneficial programming.
Whether happening for the first time, as with the UMSON Maryland Nursing Workforce Center’s inaugural State of the Maryland Nursing Workforce Symposium, or for more than three decades, as is the case for the Summer Institute in Nursing Informatics (SINI), UMSON conferences and symposia bring together the brightest minds in education, practice, research, and innovation. Here’s a quick rundown of a few 2024 offerings. —M.T.P.
EVENT Maryland Action Coalition Virtual Leadership Summit
DATE May 20
THEME Revolution vs. Rearrangement: How to Realistically Reimage Nursing Education and Practice
PURPOSE
Explore novel approaches to education and models of care that advance the profession and hold promise for the future



KEYNOTE “The Courage to See Hope” – Tad Worku, MS, RN, FNP-BC, mission coach, speaker, and musician
State of the Maryland Nursing Workforce Symposium
33rd Annual SINI
June 6 July 18 - 19
Learning from the Past, Valuing the Present, Shaping the Future
Health Care Informatics IQ: Fostering the Human Connection
Examine Maryland workforce data and trends and gain valuable insight into nursing supply, demand, and education
KEYNOTE’S KEY NOTE
“It’s safe to say that nursing and health care have experienced a collective trauma over the past four years that is ongoing. And yet, it’s also safe to say that hope remains within this reality.”
“The Intersection of Policy and the Nursing Workforce: Leveraging Resources for Stabilization” – Maryland state Del. Bonnie L. Cullison, MA (District 19, Montgomery County)
“I completely rely on you to inform me and my colleagues in the Legislature what factors affect your ability to practice at your highest levels and to practice effectively.”
Explore how artificial intelligence and other technologies can enhance the quality, safety, and efficiency of health care delivery and outcomes while addressing patients’ needs
“Artificial Intelligence: The Future of Nursing is Not What It Used to Be” – Tom Lawry, MS, managing director, Second Century Technology LLC
“Nursing school curriculum must include AI and its application to nursing. If you’re not providing that at the training level, I believe we’re turning out nurses that are not prepared for the future — probably not even prepared for present day.”
BY EMILY BLEIWEIS
Elshaddai Green, a Bachelor of Science in Nursing (BSN) student at the Universities at Shady Grove (USG) who is co-president of UMSON’s Black Student Nurse Association (BSNA), said she didn’t always intend to go into nursing.
While Green has known she wanted to pursue a career in health care – she started in a Certified Nursing Assistant program in high school – she initially thought she would get her medical assistant license and use it as a stepping stone on a path to medical school.
“That was the expected pathway that they taught us. If I had a person that was able to show me the different paths of nursing, I think it would have helped me cut down on a lot of that time that I spent wondering and going back and forth and being lost and confused,” Green said.
Now, she is hoping to be that person for middle and high school students in Montgomery County (Maryland) Public Schools (MCPS). UMSON at USG is working to make that happen through a growing initiative to create partnerships and encourage a pathway from MCPS to the nursing school.
Jana Goodwin, PhD, RN, CNE, assistant professor and department chair of UMSON at USG, has been working to develop a strong relationship with MCPS, which she hopes will help UMSON be on high school students’ radar long before they’re applying to nursing programs.

“We recognize the importance of engaging the students in Montgomery County very early on to get them to understand what health careers are all about,” Goodwin said.
Some of these connections have been made informally, such as when students from Gaithersburg High School reached out to Goodwin to invite nursing students to speak to their STEAM club, with a goal of exposing more students of color to STEAM (science, technology, engineering, art, and math) careers. Others are more formal partnerships, such as the Achieving Collegiate Excellence and Success (ACES) Summer Bridge Program called reachHIRE, a USG initiative that offers a series of summer events in collaboration with Montgomery College and MCPS. Each year, the ACES high school students participate in nursing simulations at UMSON at USG, Goodwin said.
The connections made at these visits pay off because students who go through the ACES program often attend Montgomery College, then make their way to UMSON programs at USG, Goodwin said.
Pat Schaefer, DNP, RN, CNE-cl, CHSE, CNE, assistant professor and director of the clinical simulation labs at USG, said that during these visits from ACES students and through other MCPS partnerships, the simulation team ensures the students are exposed to various options for nursing careers and beyond, including technologists who facilitate simulations.
Students such as Green are helping to make that happen. In addition
to the BSNA’s visits with MCPS students, nursing students involved in the Latinx Association of Nurses at University of Maryland (LANUM) have also met with high schoolers in the county to talk to them about potential nursing careers. Last spring, LANUM partnered with the Liberty’s Promise program at John F. Kennedy High School to engage with disadvantaged immigrant youth. The LANUM members shared their experiences as first-generation Latino students.
The LANUM team also demonstrated practical skills, such as taking blood pressure readings, and showcased life-saving equipment with the expertise of nurse anesthesia professionals. Joseph Alminagor, a BSN student and co-president of LANUM, spoke with students at Thomas Edison High School of Technology, something he said he would have been grateful for when he was in high school.
“The experience for me – it just is kind of full circle,” he said. “I was once a high school student thinking, ‘Wow, I want to be a nurse!’”
Developing these connections, with a focus on MCPS, specifically, is intentional, Goodwin said.
“I believe it’s really important for the community to take care of the community,” she said, adding that the middle and high school students who grow up in the county know the challenges its people may face. “These middle and high school students are different thinkers and learners. I don’t think we really know how they might contribute to nursing right now, but it can only be really valuable.”



“From balancing the demands of family and work to navigating the complexities of academic coursework and clinical experiences, we have faced moments of doubt and uncertainty. Yet, in the face of adversity, we have persevered.”
SHANEISHA MCMILLAN, DNP ’24, RN, CCRN, SRNA STUDENT SPEAKER
“Whether it was to provide comfort, hold a hand in need, advocate, or make evidence-based clinical decisions, nurses have stood at the forefront of health care.”
DIANA HERNANDEZ CABALLERO, BSN ’24 STUDENT SPEAKER

Friends and family of the Class of 2024 gathered on May 14 to celebrate the accomplishments of nearly 500 UMSON graduates at the School’s Convocation ceremonies at the Hippodrome Theatre in Baltimore.
“Throughout this journey, you relied on the support, encouragement, and sacrifices of your family, friends, and classmates who gave you the confidence to persevere, especially when you were sleep deprived, juggling many responsibilities, and didn’t think you would make it,” Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, told the graduates.
This year’s ceremony – which was split into two events – resulted in nearly 250 new nurses entering the workforce. The day began with the Bachelor of Science in Nursing and Master of Science in Nursing Clinical Nurse Leader Ceremony and was followed by the Master’s and Doctoral Ceremony.
Angela Barron McBride, PhD, RN, FAAN, FAANP, distinguished professor and university dean emerita at the Indiana University School of Nursing, was presented with the 2024 Dean’s

Medal for Distinguished Service, which recognizes individuals external to the School who have demonstrated an exceptional commitment to advancing UMSON and its mission. McBride was recognized for her seminal contributions to women’s health – particularly the psychology of parenthood – and to psychiatric nursing. Her first book, “The Growth and Development of Mothers,” was recognized as one of the best books of 1973 by The New York Times and the American Journal of Nursing.
At the second ceremony, Therese S. Richmond, PhD, RN, FAAN, the Andrea B. Laporte Professor of Nursing at the University of Pennsylvania School of Nursing, received an Honorary Doctor of Public Service degree from the University of Maryland, Baltimore. Richmond has an extensive program of research aimed at improving recovery from serious injury by addressing the interaction between injury and its psychological repercussions, including a focus on the prevention of violence and firearm violence.
— E.B. and M.T.P.
BY LISA ROWEN, DNSc, MS ’86, RN, CENP, BCC, FAONL, FAAN FORMER CHIEF NURSE EXECUTIVE, UNIVERSITY OF MARYLAND MEDICAL SYSTEM
Growing up, I didn’t aspire to be a nurse. I was unaware of the joy and fulfillment that goes hand in hand with our challenging profession. While in college, I learned from friends majoring in nursing that the profession offers a way to extend ourselves to others at their most vulnerable times in life and made the decision to become a nurse instead of an art historian. Lesson learned: Stay open to all opportunities.
My path to nursing was bumpy. I almost failed organic chemistry in college. My professor told me I’d never become a nurse because my test scores were poor. That motivated me, and I successfully passed the course. Lesson learned: Don’t let others define your potential.
Let yourself be drawn to what you are naturally interested in, and you will flourish.
I saw my organic chemistry professor several years later when he was my patient following a surgical procedure for pancreatic cancer. He motivated me yet again by asking me what area of specialty I particularly loved. My answer was quick and easy: leadership. I shared that I wanted to be a chief nursing officer. He asked me what path I would take to make that happen. Lesson learned: Create and update career goals frequently and have a specific plan to achieve them.
The most valuable lesson I’ve integrated in my professional life is to focus on my strengths and passions
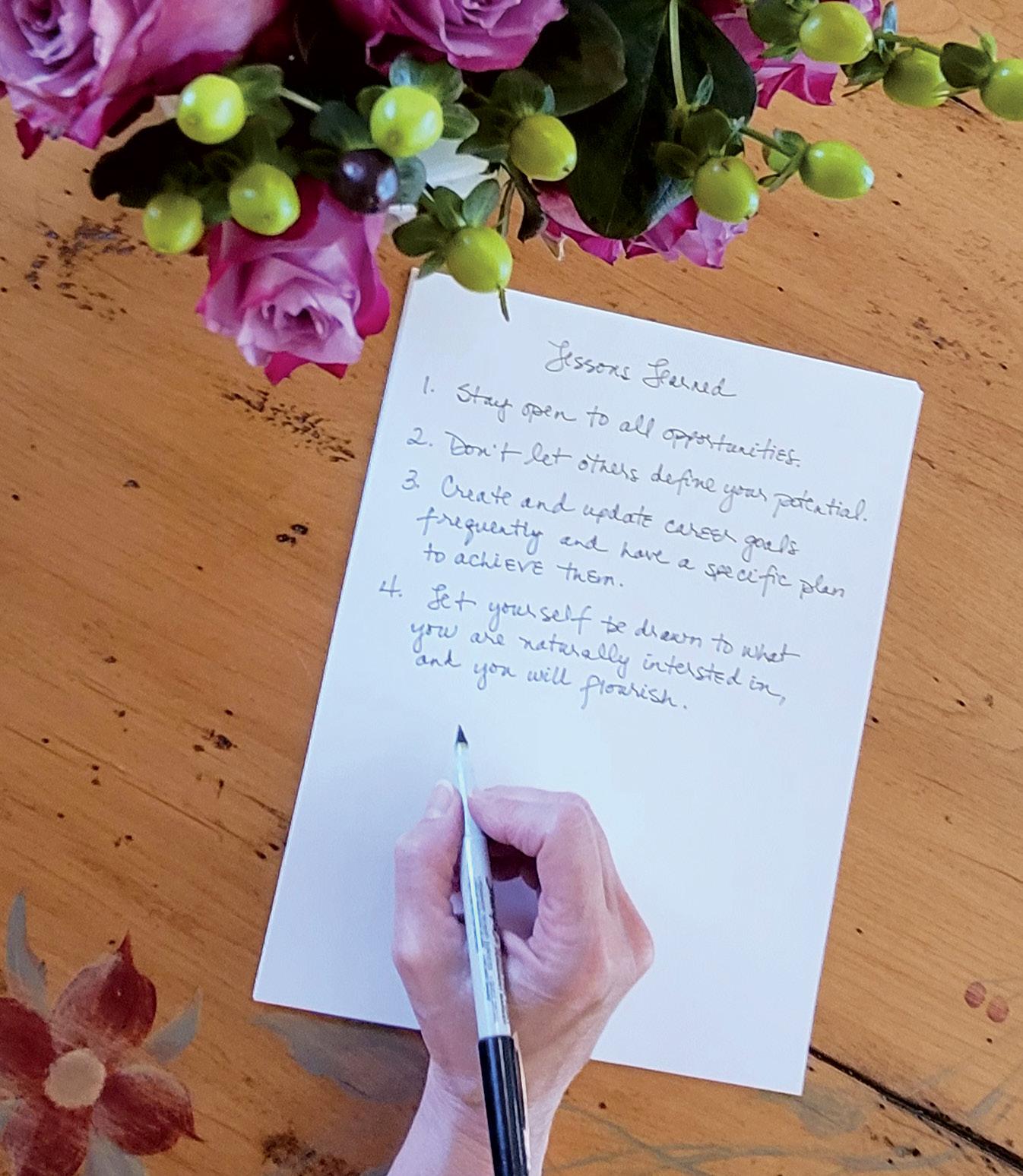

instead of areas where I’m average. I will be hard pressed to get an A+ in organic chemistry but I will more than likely ace a course or achieve a goal that I am passionate about. It is easier to move ourselves to excellence in areas we want to learn about. Lesson learned: Let yourself be drawn to what you are naturally interested in, and you will flourish.
A few months ago, I moved to retirement – or rewirement, as I like to think of it! One of the best things that happened in this process was meeting and handing my role and responsibilities off to Peggy Norton-Rosko, DNP, RN, NEA-BC, the nurse leader who succeeds me as the chief nurse executive at the University of Maryland Medical System (UMMS). Peggy is an
extraordinary professional with deep experience in top nursing leadership positions at multiple institutions. She’s smart, warm, collaborative, and will accomplish great things. Peggy will be a tremendous partner for the University of Maryland School of Nursing. The academic and practice partnership we’ve established between UMSON and UMMS will continue to flourish in exciting and innovative ways with her collaborative leadership with Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean. It has been a privilege and honor to serve my patients and colleagues over the past 42 years. Our profession is a gift that I will treasure forever, and I’m grateful for the path I’ve chosen – with its many meaningful lessons.
“In every nursing class, I am amazed by the intricacy of the human body, and how when looking at and conversing with people every day, there are millions of unseen pathways that facilitate human life. Nursing is not a field of study that can just be taught through lectures; instead, hands-on experience is important to translate the art from the class to practice.”
Phoebe Chan, BSN Student USNews.com, June 2024
BSN student Joseph Alminagor was one of nine Universities at Shady Grove students featured in The College Tour TV show, available on Prime Video. Watch the full episode by scanning this QR code.
During the 2023 - 24 school year, UMSON’s Booked for Lunch book club, hosted by the Office of Equity, Diversity, and Inclusion, read a total of 1,705 pages
Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, received the Lifetime Achievement Award at the second annual Maryland Nurses Association gala.
Over the past six years, 34 UMSON faculty have received a total of $170,000 in Academic Nurse Educator Certification (ANEC) Award funding from the Maryland Higher Education Commission through the Nurse Support Program II. In 2024, UMSON received nearly one-fifth of all ANEC funding statewide.
UMSON has 14 faculty and staff members trained as Restorative Justice (RJ) facilitators, equipping them to build community through restorative approaches to conflict resolution. RJ circles, which facilitate restorative communication, are integrated in three out of the four BSN semesters and are starting to be incorporated in the entry master’s curriculum.
Since its inception in 2015, UMSON’s Nurse Leadership Institute, a yearlong leadership development program that strengthens new and experienced nurse leaders, has graduated 286 fellows.
In the spring 2024 semester, 1,875 students were placed in 2,820 clinical slots across Maryland, Virginia, the District of Columbia, and Pennsylvania.
“We can help people develop a healthy habit that they can continue for the rest of their lives.”
IAN KLECKNER
BY DAN MEZIBOV
OUR
RESEARCHER
Ian Kleckner, PhD, MPH
Chemotherapy is a long-proven tool used to treat many cancers, including breast, prostate, lung, ovarian, testicular, gastrointestinal, lymphoma, leukemia, and others. But chemo can also add insult to injury by triggering a host of debilitating side effects that interfere with daily functioning, independence, and quality of life. Chemotherapy-induced peripheral neuropathy (CIPN) is a common side effect of chemotherapy drugs, presenting as numbness, tingling, shooting pain, or cramping in the fingers, toes, hands, and feet, as well as painful sensitivity to cold. As a result, CIPN’s toll can include difficulty writing, texting, buttoning clothes, or maintaining balance.
The SYNAPSE Center, an UMSON organized research center directed by Kleckner, focuses on understanding medical symptoms as mental states, or perceptions, influenced by biological, psychological, social, and spiritual factors.
“We’re trying to categorize” those factors to identify the best model among them to explain a given symptom, Kleckner says. Through his training in the psychology and neuroscience of emotion, he adds, “I knew these powerful ideas could help create a paradigm shift in the study of medical symptoms.”
CIPN is also tough to treat, particularly because of chemotherapy’s toxicity to the nervous system. CIPN is one of the few types of neuropathies that are “dose limiting,” meaning that chemo must be limited or stopped once side effects worsen.
Currently leading a series of randomized clinical trials – two in Baltimore and a third with 30 testing sites nationwide – Ian Kleckner, PhD, MPH, associate professor and director of UMSON’s Symptom Science Using Neuroscientific and Psychological Approaches (SYNAPSE) Center, is exploring whether regular exercise can alleviate CIPN symptoms. While not the first to test if exercise can dampen chemo’s side effects, Kleckner’s National Cancer Institute (NCI)-funded studies are the first nationwide clinical trials to combine the role of exercise in CIPN with the role of the brain.
“We already know that exercise is helpful for patients with cancer for their health-related quality of life and
mood. We don’t know about exercise for neuropathy, even though neuropathy is very common,” Kleckner says, noting that two-thirds of chemotherapy patients develop CIPN symptoms. Kleckner is investigating how people perceive, and how the brain processes, bodily sensations and whether exercise can treat or prevent CIPN. The multisite national trial is in collaboration with the University of Rochester Medical Center and is co-led by close collaborator Po-Ju Lin, PhD, RD, MPH, assistant research professor at that institution, as part of NCI’s Community Oncology Research Program.
The investigations employ at-home walking with a daily step goal tracked by a wrist monitor, 16 upperand lower-body exercises, stretching with resistance bands, as well as hand grip and balance tests to study men and women who are receiving chemotherapy for gastrointestinal, breast, and a range of other cancers. Before and at intervals during the trials, patients rate the severity of their CIPN symptoms by answering a 20-item questionnaire, while MRI scans and a specialized, portable neuroimaging skull cap measure brain activity and what neural networks are involved in exercise.
Preliminary results suggest that the brain is involved in CIPN and that exercise can influence the brain in ways that reduce CIPN symptoms.
“The knowledge we will gain by our work can improve standard of care by identifying the extent of possible benefits of exercise, who will benefit most, how to best use it, and what dose of exercise is minimally effective and maximally effective,” Kleckner explains. Moreover, he points out, “we can help people develop a healthy habit that they can continue for the rest of their lives.”
To help sustain and grow Kleckner’s research program, you can donate at nursing.umaryland.edu/give/synapse.


Scan this QR code for a free digital copy of “Placebo Effects: Through the Lens of Translational Research,” a newly released book edited by Colloca and other members of the UMB community.
BY ERIN MERINO
OUR EXPERT
Luana Colloca, MD, PhD, MS
Most people are familiar with the placebo effect, but there is a rarer, lesser-known phenomenon, the nocebo effect, that can occur in patients dealing with pain, chronic conditions, and cancer, among other conditions, explains Luana Colloca, MD, PhD, MS, professor and director of the Placebo Beyond Opinions (PBO) Center. According to Colloca, nocebos are a negative reaction to a diagnosis or medical treatment because of expectations: “Individuals begin to experience symptoms even in the absence of exposure to the factor that can cause adverse effects,” Colloca states.
Colloca, who has been researching placebos and nocebos for more than two decades, says “negative external and internal factors can trigger an

amplification of signaling in the brain that turns into worsening of symptoms.” An external factor may be a difficult relationship between patient and provider, while an internal factor could be a negative outlook. In her research conducted at UMSON, Colloca has demonstrated that “patients who suffer from catastrophizing and negative thoughts tend to experience higher nocebo effects, suggesting that outlook can be critical to our mental and physical well-being,” she explains. She offers recommendations for ways clinicians can convey necessary information without inducing noceboproducing anxiety in patients:
The language used by clinicians can significantly impact patients’ experiences of their symptoms. Avoid negative language or overstatements. “The words that we use can trigger worsening of fatigue, nausea, distress, anxiety, insomnia due to the nocebo effects that can amplify the side effects of medication,” Colloca states.
Focusing on the person in front of you is imperative. “The most concerning issue is that, when seeing patients, instead of making eye contact, we often find ourselves in front of our keyboards, typing while we talk,” Colloca says. Clinicians should ask the patient questions and listen. “Create this space where the patient feels safe to share what they are suffering from,” Colloca explains. Additionally, Colloca suggests asking questions such as “What do
you expect to improve with this treatment?” or “How long do you think this disease will be affecting you?” that allows you to understand how the patient is feeling and enables you to discuss ways to handle symptoms with the patient.
Provide honest information while also offering reassurance. The conversation should be a “balance between the truthful information that as clinicians we are meant to provide and comfort,” Colloca says. Make time to connect with patients, even during brief visits. “Provide them with resources and tools so that they don’t feel abandoned or alone in dealing with the problem,” she explains.
Encourage patients to participate actively in their healing process. “Frame the information in a way that balances empowerment of expectation and the ability to minimize the unwanted side effects, or nocebo effects,” Colloca explains. Patients “are told a lot about all the medical pharmacological approaches and very little about lifestyle changes in behaviors or access to a nonpharmacological approach or the impact of expectation on symptom perception,” she says. You don’t want patients to feel they are “a victim of the diagnosis and the symptoms, but rather have this intentional healing process where they can be part of that journey,” Colloca explains.
To learn more about placebo research, visit nursing.umaryland.edu/PBO.
Stephanie Harrison
BY ERIN MERINO
Stephanie Harrison, MS ’15, PCCN, a student in the Teaching in Nursing and Health Professions graduate certificate, had an unconventional journey to nursing, beginning with an undergraduate art degree. However, her mother, Jocelyn Farrar, DNP ’08, MSN ’87, BSN ’74, a nurse who served in various capacities, including as a faculty member at UMSON, inspired her to switch paths.
Farrar died in 2013 from cancer, but the compassionate care she received from nurses left a lasting impression on Harrison. “It wasn’t until my mother was the patient that I realized the impact that nurses truly have. I still remember some nurses that took care of her and realized I want to do this for other people,” Harrison says. This experience solidified her desire to follow in her mother’s footsteps and make a difference in patients’ lives. Harrison adds, “I couldn’t fill her shoes, but I picked up where she had to leave off.”
“It wasn’t until my mother was the patient that I realized the impact that nurses truly have. I still remember some nurses that took care of her and realized I want to do this for other people.”
STEPHANIE HARRISON
She enrolled in the master’s entryinto-nursing option at UMSON, and her career now spans 14 years (nine years as a nurse) at Frederick Health Hospital in Maryland, where she started out in a medical surgical telemetry unit and later gained experience in the intensive care unit. The COVID-19 pandemic prompted

her to reassess her goals and take on a new role in academia at Frederick Community College (FCC), teaching med-surg nursing. Harrison is now an assistant professor and course coordinator in FCC’s Associate Degree in Nursing program while continuing practice as a nurse at Frederick Health Hospital.
Harrison had the enthusiasm to teach but recognized the importance of a strong educational foundation, leading her to enroll in UMSON’s Teaching in Nursing and Health Professions Certificate. “It’s a big learning curve. You can know what heart failure is as a nurse, but teaching it is a different component,” she explains. After completing her first semester in the program, she already feels more equipped to teach, she says. She was awarded the Conway Scholarship – which covers tuition, fees, and books – as well as the New Nursing Faculty
Fellowship through the Maryland Higher Education Commission, which supports her educational and professional growth.
Harrison notes she can advance her education, balancing her roles at FCC and Frederick Health Hospital, all while raising four children, thanks to the certificate’s flexible, online format.
Inspired by her mother’s legacy, Harrison says she strives to nurture the next generation of nurses, ensuring they are well prepared to provide exceptional care.
“I love the impact that I’m able to make by helping these students become awesome nurses,” Harrison says, adding that she’s driven by the rewards of a nursing career. “It’s hard work, and it will take a lot out of you, but making people better, giving them what they need in the moment, is the reason to go and do the job every day.”

Working in health care can be intense, exciting, and emotional. The dramatic moments that occur especially in acute-care settings are regularly chronicled in popular television shows and movies. Yet rarely do nursing students get to participate in the kind of high-stakes cases that have made TV shows such as “ER” and “Grey’s Anatomy” so watchable.


However, students at UMSON do get to play a role in various important care scenarios through simulation, a learner-centered, interactive teaching strategy. Sometimes there’s even a professional actor playing the role of a patient or family member.
The School’s simulation teams, both in Baltimore and at the Universities at Shady Grove (USG) in Rockville, Maryland, include 17 staff, clinical educators, and faculty members who create these simulated experiences, including critical events that students may encounter upon graduating into various roles in the workforce.
Clinical educators and faculty use simulation to create realistic learning and testing environments to build confidence and decision-making abilities with an emphasis on patient safety. “Simulation, including the manikin, standardized patients, class-based simulation, and virtual reality, offers an authentic experience for our learners to become more ready for practice as they strive for clinical competence,” says Dawn Mueller-Burke, PhD ’07, MS ’98, CRNP, NNP-BC, assistant professor and chair of UMSON’s taskforce for aligning its curriculum with the American Association of Colleges of Nursing’s (AACN) Essentials, an updated framework for nursing education. The Essentials emphasize competency-based education, or “students demonstrating that they have learned the knowledge, attitudes, motivations, self-perceptions, and skills expected of them,” according to AACN.
These authentic experiences include using an immersive virtual reality scenario to ensure that all students can participate in caring for a pregnant woman with a health condition that students may not observe during their obstetrics clinical rotation, says Patricia “Pat” Schaefer, DNP, RN, CNE-cl, CHSE, CNE, assistant professor and director of simulation at USG. In that scenario, the students slip on a virtual reality headset that displays a realistic, artificially intelligence-powered patient. Students then conduct a physical examination on the virtual patient, place an external fetal monitor on her, observe changes in her condition, and respond appropriately. UMSON uses simulation to allow students to practice multiple competencies in AACN’s Essentials –clinical reasoning, implicit bias, equitable treatment, and communication with diverse
populations – in safe, supervised experiences before applying those skills in direct patient care.
Developing these high-quality and high-fidelity experiences for students takes a surprising amount of behind-the-scenes work, says Amy L. Daniels, PhD ’18, MS ’12, BSN ’89, RN, CHSE-A, assistant professor and director of the Baltimore clinical simulation labs. “It’s really important to align with curriculum objectives and not just find a patient case that’s exciting and try to create a scenario,” she says. “There’s a whole pedagogy behind it.”
“It’s a calm environment with these instructors, which allows students to focus on the goal of the scenario without added stressors.”
JENINA SHEPPARD
Debriefing is an integral part of the experience, too. After the simulation activity is completed, the educator facilitates a conversation using a theory-based debriefing approach to unpack observations and understand the student’s perspective during the learning experience. “It’s more than saying, ‘I saw you do this, you should have done that,’” Daniels says. “It’s about giving specific details of what the educator saw, sharing the educator’s perspective on that action, and curiously inquiring about the student’s perspective on that action.”
Simulation technologists are the sometimes-unseen champions behind the cutting-edge simulation experiences that UMSON offers. “Their role is essential – you really can’t run a large sim program like we have without them,” Schaefer says. That large program includes 33 simulation labs between Baltimore and USG that replicate realistic practice environments and feature hospital, critical care, operating room, pediatric, maternity, and home care settings, as well as dedicated debriefing spaces. USG recently completed an $8.2 million renovation that added a five-bed Hospital Suite to its three floors of lab space.

“It’s super fulfilling to know that in a small way, I’m helping thousands of people I’ll never meet because I helped their nurse.”
KEVIN HARRIS
Harris often manages simulations from the technology-equipped control room that sits behind one-way glass in the Hospital Simulation Suite at USG.
The simulation technologists oversee all the technology that’s used in a scenario, such as audiovisual equipment, computers, and medication administration machines, while also providing operations support. They prepare the rooms and provide the necessary materials for a clinical scenario, including a headwall with oxygen and suction tools, an IV pole, and a patient monitor to display vital signs. The simulation technologists select the appropriate manikin to support the learning objectives, voice the patient, and maintain and update all the equipment.
Kevin Harris, an IT telecommunications associate at USG, has worked as a technologist in the simulation labs in Baltimore and USG for 16 years.
“I like to think of simulation as a one- or two-act play,” Harris says. “We develop a script that’s based on the objectives and curriculum in the course and the things we want the student to learn. The student script is based on their coursework and clinical experience, and they bring that into the play.”
Sim techs have a variety of backgrounds and come from different disciplines, including theater arts, film production, and IT, as well as health care.
Harris is passionate about simulation and how it helps develop nurses. “It’s super fulfilling to know that in a small way, I’m helping thousands of people I’ll never meet because I helped their nurse,” he says.
Jenina Sheppard, a Bachelor of Science in Nursing student, is one of those nurses that Harris and the USG simulation team have helped. She’s always wanted to be a labor and delivery nurse and was heavily influenced by the birth stories depicted in “Birth Day,” a TV series that documents the labor and delivery process.
She’s been enthusiastic in her evaluations of simulation. “Unlike an actual clinical setting on a hospital floor, you have your classmates working right along with you for support – it’s a team effort,” Sheppard says. “It’s a calm environment with these instructors, which allows students to focus on the goal of the scenario without added stressors.”
Sheppard and her classmates have participated in several scenarios featuring medication administration. In one experience, Sheppard and two other students used a provider-ordered sliding scale and performed a drug calculation in response to lab results. The

“Debriefing is essential to the simulation process because it’s better to see mistakes and correct them now than to make a mistake that could cost someone’s life in the real world.”
JENINA SHEPPARD
HAPPY BIRTHDAY TO U(MSON)!
Answer:
2 Annabelle Lee was UMSON’s first training manikin, named after a poem by famous Baltimorean Edgar Allan Poe (who is buried on the University of Maryland, Baltimore campus at Westminster Hall on Fayette Street).
In 1914, Annabelle Lee was a gift from the Women’s Auxiliary Board of the University Hospital.
students interpreted the results and followed the physician’s orders to make correct dosage decisions. In the School’s simulation Hospital Suite, students pull appropriate medications from a hospital-grade medication dispensing machine in a designated medication room.
“Medication delivery mimics clinical practice to improve student confidence in interpreting doctor’s orders, pulling medications, and administering them safely,” Schaefer says. “The fidelity of medication administration keeps patient safety at the forefront of simulation activities to enhance students transitioning to the actual clinical setting.”
A simulation is essentially a live performance starring nursing students. “Instructors watch us, see what we did right, see what we did wrong, help us to correct our mistakes and learn from them, and talk about it afterwards,” Sheppard says. “Debriefing is essential to the simulation process because it’s better to see mistakes and correct them now than to make a mistake that could cost someone’s life in the real world.”
“It’s a psychologically safe environment where mistakes can be made without repercussion.”
NANCY CULPEPPER
The School’s realistic, high-fidelity manikins are impressive, and donning a virtual reality headset to interact with AI-powered patients is undoubtedly cutting edge. But the human element of simulation provided by the Standardized Patient Program (SPP) is equally important.
The SPP was developed in 2001 as a collaboration between UMSON and the University of Maryland School of Medicine. The program is housed in the UMSON building in Baltimore and features 14 examination rooms equipped with full audiovisual capabilities. The center is designed with separate student and standardized participant (SP) entrances to maintain simulation fidelity as well as dedicated space for faculty viewing and debriefing.
The program employs 120 SPs, many of whom are professional actors. SPs are trained to portray a patient to simulate a set of symptoms or problems used for education, evaluation, and research. The SPs serve as unscripted models for students to practice taking a history and conducting physical exam skills. Or they may be trained to present meticulous patient case scenarios in the same way during every student encounter to ensure a standardized experience for learning and assessment.
“It’s the highest fidelity because you have a person, which obviously is the most real,” says Nancy Culpepper, MBA, director of the SPP. “It’s a psychologically safe environment where mistakes can be made without repercussion. Additionally, with an SP, you get verbal feedback from a human point of view.”
Nursing students are always seeking more opportunities to practice communicating with patients. The SPP provides that, with a real person who’s trained to give students feedback about their communication style, including how students asked physical examination questions and how those questions made the SP feel. Together, the various simulation modalities that UMSON offers ensure that students receive the full spectrum of practice scenarios. “Simulation is a really strong teaching approach because it supports all the domains of learning and includes elements for different types of learners,” Daniels says.
Attracting exceptional prospective nurses is a mission that begins before students finish their K-12 education. UMSON regularly hosts high schoolers, and even some middle schoolers, at the Baltimore and USG locations. These young students participate in a variety of hands-on activities, including simulation experiences.
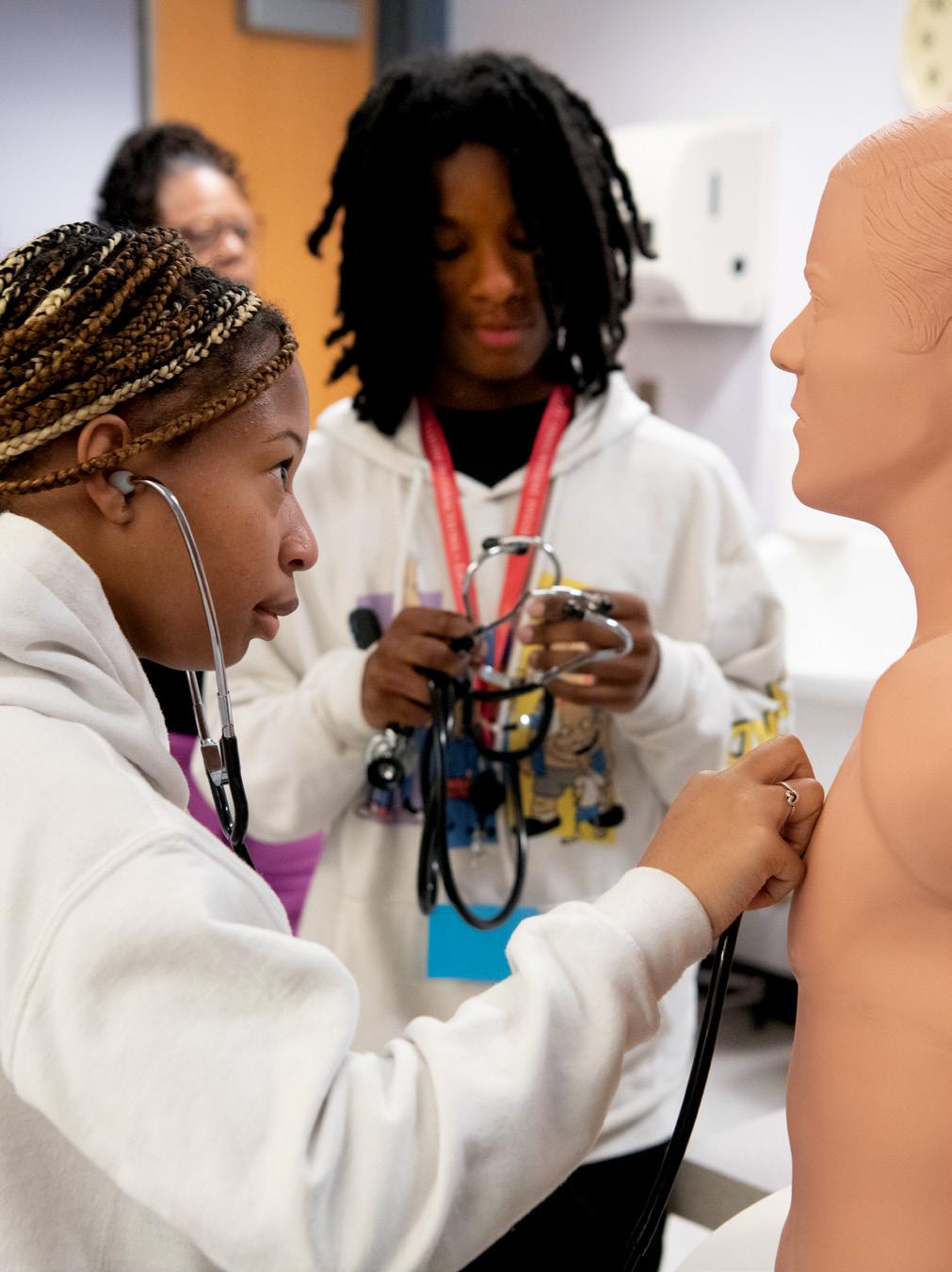
This past summer, Vanessa Fahie, PhD ’94, MS ’83, BSN ’76, RN, assistant professor, coordinated the Vivien T. Thomas Medical Arts Academy summer camp for high schoolers, and the campers visited the simulation labs in Baltimore. They completed three skills: donning sterile gloves (which is harder than it looks, one observer noted); conducting CPR on a high-fidelity manikin; and interacting with a student auscultation manikin, where the high school students used a stethoscope to listen for heart, lung, and bowel sounds, as pictured in the photo above.
Simulation technologists meet with students and discuss their own careers and how they found their way to UMSON. “Simulation is booming: This is an industry that has a lot of potential jobs for students,” Schaefer says. “Perhaps a student may not want to be a nurse, but we need to grow future technologists.”

BY MARY THERESE PHELAN
ILLUSTRATION BY ANTHONY RUSSO
As a nurse in one of Washington, D.C.’s busiest emergency departments, Socorro Berkland, RN, frequently treats victims of sexual assault. She knows providing trauma-informed care, a patient-centered approach focused on preventing re-traumatization, to such patients is critical.
“It’s especially important to understand how to provide care without basically making the patient re-live or feel as if they’re suffering a new trauma,” says Berkland, a student in the RN-to-Bachelor of Science in Nursing program.
Trauma-informed care (TIC) recognizes and responds to the impact of trauma on patients, such as mental health issues, substance use disorders, and intimate partner violence. It emphasizes creating a safe and supportive environment to facilitate healing and recovery. The goal is to improve trust and health outcomes through training interprofessional health care providers to recognize their own biases and communicate more effectively, providing care that considers a person’s full life experiences.
This is accomplished, according to the Substance Abuse and Mental Health Services Administration’s six guiding principles of TIC, by providing a sense of safety; instilling trustworthiness and transparency; providing opportunities for peer support; emphasizing partnership between providers and patients; empowering patients with a sense of control; and understanding and respecting cultural, historical, and gender issues. Without the lens of TIC, a provider might inadvertently attribute a patient’s stress-related symptoms to an anxiety disorder, when it might in fact be a traumatic stress response.
It’s this TIC approach that recently led Berkland to care for a sexual assault patient in an unconventional way. Berkland noticed a woman was visibly upset when asked to put on new clothing provided by the hospital once her own clothes were collected for evidence. The woman had pulled the new shirt away from her skin. It was a scratchy material and easily two sizes too big for her. Berkland quickly retrieved a top that was made of a softer fabric and was closer to the woman’s size, and the woman’s eyes began to well up in gratitude.
“She had already been through so much,” Berkland said. “I was not going to let her be uncomfortable for another minute.”
Several UMSON faculty members are championing a trauma-informed approach to practice, among them assistant professors Rosemarie Satyshur, PhD, RN; Trina Kumodzi, PhD, RN, CCRN; and Rachel Blankstein Breman, PhD ’18, MPH, RN, FAWHONN.
TIC has emerged as an interprofessional model in which nurses play a critical role, says Satyshur, former executive director of the Maryland Social Services Administration and now a member of the Maryland Department of Health’s Maternal Mortality Review Team. The team is charged with examining issues resulting in disparities in maternal deaths, reviewing the implementation status of previous recommendations, and identifying new recommendations to address disparities in maternal deaths.
Using a trauma-informed method of communication during perinatal care can foster trust between patients and birth workers, according to Breman, who last year received a $60,000 grant from the Maryland Department of Public Health to fund interactive webinars on how to implement TIC for all birth workers in Maryland.
With improved trust, birth workers can provide better care and offer resources to birthing people and their families as a result of their increased awareness of how trauma affects everyone, regardless of background, Breman says.
“Foundationally, all birth workers should use a traumainformed approach when consulting with their clients and during physical exams,” Breman says. “This work will help strengthen what is already being done in clinical care and explore areas for improvement and future implementation so that all birthing people feel safe in perinatal and women’s health care settings.”
In the past, trauma in health care was often viewed narrowly as a crisis experience, Satyshur says. In recent years, a trauma-informed approach has expanded to encompass a broader public health perspective, which
“ YOU DON’T JUST GO UP TO A PATIENT AND GET TO WORK. YOU HAVE TO HAVE A DIFFERENT APPROACH THAT PROMOTES A SAFE ENVIRONMENT.”
ROSEMARIE SATYSHUR
looks to address trauma beyond individual interventions and to understand trauma’s population impact. This shift acknowledges that trauma can be both physical and emotional, affecting not only patients but families, caregivers, and health care providers.
American Academy of Pediatrics statistics from 2021 show that in the United States, 34 million children under the age of 18 have faced at least one traumatic event, defined by the U.S. Centers for Disease Control and Prevention (CDC) as a physical, cognitive, and emotional response to harmful or life-threatening events or circumstances, and one out of every seven adults reports they’ve experienced or been exposed to four or more incidences, according to the CDC.
“We’re constantly working with people that have trauma that affects the way they think,” says Satyshur, who has nearly 50 years of experience working with vulnerable populations. “How you treat them is really important.”
For example, what may seem like a simple physical
exam to a health care provider could be experienced as an invasion of privacy to someone who has survived physical abuse or a sexual assault and could result in the patient reliving the trauma. “You don’t just go up to a patient and get to work. You have to have a different approach that promotes a safe environment,” Satyshur says.
In June, U.S. Surgeon General Vice Adm. Vivek Murthy, MD, MBA, issued a first-ever Surgeon General Advisory on Firearm Violence, declaring it to be a public health crisis in America.
Firearm violence is pervasive, with more than half of U.S. adults or their family members having experienced a firearm-related incident in their lives, the advisory states. Over the last decade, the number of people who have died from firearm-related injuries, including suicides, homicides, and accidental deaths, has risen, and firearm violence is now the leading cause of death among children and adolescents.
The advisory details the impact of gun violence beyond death and injury, describing the layers of cascading harm for youth, families, communities, and other populations. With nearly six in 10 U.S. adults worrying “sometimes,” “almost every day,” or “every day” about a loved one being a victim of firearm violence, the advisory states, the effects of the public health crisis extend well beyond physical health – it has led to a collective trauma across society that warrants heightened attention.
Assistant professor Kumodzi’s interest in TIC and violence as a public health issue stems from the time she spent completing a practicum at the R Adams Crowley Shock Trauma Center at the University of Maryland Medical Center.
“I saw a pattern when I was working bedside,” Kumodzi says. “Certain people, particularly young Black males in a certain neighborhood, and Baltimore in general, are coming in for interpersonal violence. And then at the same time, I saw white patients who were coming in, mostly not even from Baltimore, but being flown in from other parts of the state for suicidal violence. And our approach was largely one at an individual level” versus a TIC approach.
“An individual approach is treating the illness or injury that is right in front of you,” Kumodzi explains, indicating that this can “result in depersonalization of both the patient and the caregiver. A TIC approach is built on the question ‘What happened to you?’ versus ‘What’s wrong with you?’ ”
And it’s not only patients who need TIC, Kumodzi says. Particularly since the arrival of the COVID-19 pandemic, caregivers are also needing more TIC “to deal with the
1 SAFETY: ensuring physical and emotional safety for everyone involved
2 TRUSTWORTHINESS AND TRANSPARENCY: building trust through clear communication, consistency, and transparency in decisions
3 PEER SUPPORT: recognizing the value of support from others with similar experiences
4 COLLABORATION AND MUTUALITY: emphasizing partnership and the leveling of power differences between providers and patients
5 EMPOWERMENT, VOICE, AND CHOICE: empowering individuals by fostering a sense of control and autonomy
6 CULTURAL, HISTORICAL, AND GENDER ISSUES: understanding and respecting cultural, historical, and genderspecific factors that influence the individual’s experience
needs of patients,” Kumodzi explains. “We need to have that approach, not only for our patients and caregivers but for faculty, staff, and leadership because it’s hard to support people from an empty cup.”
Kumodzi completed her postdoctoral appointment at the University of Pennsylvania, where she was mentored by Therese S. Richmond, PhD, RN, FAAN, a renowned researcher on violence and trauma to whom the University of Maryland, Baltimore awarded an Honorary Doctor of Public Service degree in May (see “Convocation,” Page 11). Richmond has an extensive program of research aimed at improving recovery from serious injury by addressing the interaction between physical injury and its psychological repercussions. In 2022, she was the featured speaker for the School’s Virginia Lee Franklin Lecture, presenting “Shots Fired: Reducing the Impact of Firearm Violence.”
Drawing on her work with Richmond, Kumodzi teaches the course Public Health Approach to Violence and Violence Prevention, which she describes as an eyeopener of a class.
“As a student, you’re really thinking about building skills,” Kumodzi says. “But now, when they come into this class, it’s really seeing it like, ‘Oh, I need to see myself as part of a larger framework in restructuring the system of health care, not just as being a cog in the wheel, but that I have a part in changing the direction for both the hospital and for my patients.’”
Kumodzi says the violence course she teaches helps students consider their patients in the larger community context, encouraging them to think of how they can utilize their intellectual and clinical skills to improve patient outcomes through preventive measures.
“This is the critical-thinking component and the ultimate purpose for advanced nursing education,” Kumodzi says. THE SUBSTANCE ABUSE AND MENTAL HEALTH SERVICES ADMINISTRATION’S SIX PRINCIPLES THAT GUIDE A TRAUMA-INFORMED CARE APPROACH:
WE NEED YOU: VOLUNTEER DOCENTS MAKE A DIFFERENCE!
We invite you to volunteer as a docent and share the history of UMSON and the nursing profession with visitors of the Living History Museum.
Individuals interested in donating artifacts, documents, photographs, or other items of historical importance to the museum should contact the curator at 410-706-2822. Your materials help us tell our story; we can’t do it without you.

The Living History Museum’s hours are Tuesdays and Thursdays, 10 a.m. - 2 p.m. during the fall and spring semesters or by appointment.
For more information, contact the Office of Development and Alumni Relations at alumni.nursing@ umaryland.edu or 410-706-7640.

A quarter century has passed since UMSON’s Living History Museum, dedicated to honoring the critical role of nurses, opened in the School of Nursing building in Baltimore. Established in October 1999, Maryland’s only museum dedicated to the nursing profession displays hundreds of historic items, from nurse uniforms and medical instruments to wartime letters and photographs of those who served.
The collection began in 1916 when Louisa Parsons, UMSON’s first superintendent, bequeathed her military medals to the School. The UMSON Alumni Association continued to collect items over the decades, and in 1988, the association’s Archives Committee encouraged then-Dean Nan Hechenberger, PhD, RN, to establish the Heritage Room in Parsons Hall (pictured at left, in 1995) to house the growing collection. Led by Jean Warfield Keenan, DIN ’48; Margarett Culler Zell, DIN ’39; and Barbara Kurz, DIN ’45, the Alumni Association created an index card system to document gifts they received, which were displayed and accessible for research in the Heritage Room.
Before the new School of Nursing building opened in 1998, UMSON hired a team of museum professionals to work with an advisory committee to plan and develop exhibits for an official museum, which incorporated the collection from the Heritage Room.
Over the years, various curators have updated and refreshed portions of the exhibits to reflect current interests.
As the Living History Museum evolves to meet contemporary needs, curator Kirsten Hammerstrom, MFA, has spearheaded the launch of two digital collections-based experiences. Both will be available online and in the museum on a dedicated kiosk this fall.
— Jillian Dreicer
Let your fellow alumni know what’s happening in your professional life. Submitting an update to Class Notes is easy; just visit nursing.umaryland.edu/ classnotes or contact us at alumni.nursing@umaryland.edu or 410-706-7640. You can also send us mail courtesy of the University of Maryland School of Nursing Office of Development and Alumni Relations, Suite 516, 655 W. Lombard St., Baltimore, MD 21201.
As we are unable to confirm all alumni credentials, only UMSON degrees and graduation years are included.
Lawrence C. Washington, BSN ’69, was selected for inclusion in Marquis “Who’s Who” in a July profile, honoring him for his distinguished career in nursing and miliary service.
Barbara Moore, BSN ’72, pediatric nurse practitioner and clinical director of the Lead Poisoning Program at Mt. Washington Pediatric Hospital, was quoted in a November 2023 Washington Post story about lead poisoning caused by tainted foil-lined fruit puree pouches.
Diane L. Sondheimer, BSN ’73, retired after nearly three decades as deputy chief and acting chief of the U.S. Substance Abuse and Mental Health Services Administration’s Child, Adolescent, and Family Branch.
Patricia D. Balassone, MS ’79, BSN ’74, is enjoying retirement as a working artist and hospice visitor, and she enjoys traveling to Europe.
Georganne Katchmer, BSN ’74, retired in June 2023 from the Howell Township (New Jersey) School District after 35 years as a school nurse.
Marylou V. Robinson, BSN ’74, retired again, from the National Ski Patrol after 35 years of continuous service across the United States and Europe, after previously retiring from the U.S. Army, the University of Colorado College of Nursing, and Pacific Lutheran University School of Nursing and MultiCare Health System, both in Washington state.
Rebecca S. Shuster, BSN ’74, retired after 16 years as a nurse in pediatric oncology and the pediatric intensive care unit at CHI Health Creighton University Medical Center – Bergan Mercy in Nebraska.
Patrice A. McMullen, BSN ’75, retired after 31 years as nurse manager for reimbursement for the Johns Hopkins Bone Marrow Transplant Program.
Janet Selway, MS ’88, UMSON associate professor and director of the Doctor of Nursing Practice AdultGerontology Primary Care Nurse Practitioner specialty, was featured on WYPR, Baltimore’s NPR affiliate, in a special coverage report in February about two bills Maryland lawmakers were considering to improve the health care workforce.
Della Leister, BSN ’89, was appointed interim health officer for the Baltimore County Department of Health and acting director of the Baltimore County Department of Health and Human Services.
Meei-Ling Gau, MS ’92, is a professor in the Department of Nurse-Midwifery and Women’s Health at National Taipei University of Nursing and Health Sciences in Taiwan. Her main research interests focus on breastfeeding and mother-friendly care, trying to change the birth environment to be friendly and women centered.

Nicole Beeson, DNP ’23, MSN ’21, BSN ’11, was appointed to UMSON’s Board of Visitors in April, serving as one of 25 members. The board serves in an advisory role, communicates UMSON’s messages to local and regional professional communities, and partners with the School in strategic fundraising activities. Since September 2020, Beeson has served as the senior vice president of patient care services and chief nursing officer at the University of Maryland St. Joseph Medical Center in Towson, Maryland. Beeson’s career in the health care industry spans more than 25 years, and her areas of expertise are strategic planning, workforce development, and championing clinical initiatives.
In January, Beeson delivered the keynote address for UMSON’s Welcome Ceremony, the culminating event of the entry-into-nursing student orientation, providing keen insight and words of encouragement for incoming students.
Laila F. Farhood, PhD ’93, is a professor at American University of Beirut and a clinical associate in the Faculty of Medicine’s Department of Psychiatry, where she has a clinical practice to assess and treat individuals with depression, anxiety, and marital conflicts. Her research focuses on the impact of war on the mental health of civilians with post-traumatic stress disorder, depression, and chronic illnesses.
Ben Canha, PhD ’19, BSN ’96, was featured on News Channel Nebraska Southeast about his recent book, “Recovery Cartoons: the 12 Steps.”
Barbara Resnick, PhD ’96, UMSON professor, Sonya Ziporkin Gershowitz
Chair in Gerontology, and associate dean for research, co-authored a guest submission in McKnight’s Long-Term Care News about the effects of too much screen time on the health of older adults.
Wynne F. Aroom, MS ’97, is an adjunct instructor in the RN-to-Bachelor of Science in Nursing program at Stevenson University in Maryland and a wound ostomy nurse at the University of Maryland (UM) Shore Regional Health in Easton.
Kristy Duffey, MS ’98, was named chief nursing officer at Optum Health in Columbia, Maryland, in 2022.
Amy Loughlin, MS ’02, joined PeaceHealth Medical Group in Washington state as a midwife.
Jessica Genrich, BSN ’04, has been named director of Women and Children’s Service at UM Shore Regional Health.
Marcy Stoots, MS ’05, attended Dysautonomia Advocacy Day on Capitol Hill in Washington, D.C., in March.



Want the scoop from UMSON?
Visit nursing.umaryland.edu/classnotes to update your email address, and we’ll send you our monthly events and quarterly updates newsletters.
Bridgitte Gourley, DNP ’08, UMSON assistant professor, and Kathryn Handy, MS ’09, were among 35 nurse faculty who received the Maryland Higher Education Commission’s 2024 Dr. Peg E. Daw Nurse Faculty Annual Recognition Award.
Tinagene Pia L. Inguito, PhD ’08, was appointed a Fellow of Student Nurse Training in the Dr. Jeanne K. Buxbaum Scholars Program at the University of Delaware School of Nursing.
Ellie Kagan, MS ’08, nurse practitioner and diabetes educator at Mt. Washington Pediatric Hospital in Baltimore, was quoted in a February U.S. News & World Report story about the impacts of insulin on the body.
Johnny Gayden, MS ’14, BSN ’10, was featured in a DELCO.TODAY article in March about his background and his path to becoming a nurse anesthetist.
Marita A. Dell Aquila, MS ’11, is the director of undergraduate nursing practice at Belmont University in Tennessee.



UMMC Nursing Excellence Awards
Congratulations to the alumni whose excellence in their work at UMMC was recognized at the hospital’s annual nursing awards ceremony during Nurses Week in May.
Excellence in Leadership – Manager
Courtney Cioka, MS ’16
Excellence in Advanced Practice Nursing
Victoria V. Beltran, MS ’97, BSN ’88
Michael P. Broussard, MS ’07, BSN ’04
Excellence in Quality and Safety
Micaela Baca, MS ’22
The Carolyn Guinn Contagious Positive Attitude
Susie Park, MS ’11
HAPPY BIRTHDAY TO U(MSON)!
Answer:
3 In 1964, the School of Nursing became the first nursing school in the country to provide baccalaureate nursing education for the Department of the Army. Two years later, the first students entered the Walter Reed Army Institute of Nursing (WRAIN) in Washington, D.C. During WRAIN’s 14-year existence, more than 1,200 women and men graduated from the program and became commissioned officers in the Army Nurse Corps, in which they were required to serve three years.
UMSON is celebrating its 135th anniversary throughout 2024 - 25 and will be recognizing five outstanding alumni (living or deceased) as UMSON Visionary Pioneers. They will join the 30 previously selected honorees.
We invite you to nominate alumni who have made a significant impact on and contribution to the nursing profession through their leadership, innovation, or entrepreneurship. Those selected will be honored during a celebratory event in 2025. Nominate your colleagues, friends, and former classmates to give them the recognition they deserve!
Nomination Deadline: Jan. 15, 2025
Eligibility: Nominees must be graduates (living or deceased) of UMSON. Previous Distinguished Alumni Award recipients will be automatically nominated. Current UMSON faculty members are not eligible.
For more information and to nominate a Visionary Pioneer, please visit nursing.umaryland.edu/visionary, scan the QR code at right, or contact alumni.nursing@umaryland.edu

Oluwatosin Olateju, MS ’15, BSN ’11, was featured in a BusinessDay article in April about her nursing career path and her perspectives and insights about health care and policy in the United States and Nigeria.
Susie Park, MS ’11, clinical nurse II in the pediatric intensive care unit at the UM Medical Center, received the Team Member of the Quarter Award.
Dama Yekeson-Koffa, MS ’13, was appointed chief executive officer of JFK Hospital in Liberia, Africa. She was featured in an article in the Daily Observer in February about her new role and responsibilities.
Thomas Trobiano, DNP ’22, executive director of cardiovascular and neuroscience services and clinical operations at Beebe Healthcare in Delaware, was announced as the chair for the American Heart Association’s 2024 Southern Delaware Heart Walk, scheduled for Nov. 3 in Rehoboth Beach.
Cynthia Sikorski, BA, former executive director of alumni relations, retired in May after 15 years of dedicated service to UMSON’s alumni and other community members. Colleagues, friends, and family gathered at the University of Maryland, Baltimore to thank Sikorski for her countless contributions and to wish her well on her next chapter. During the ceremony, Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, NNP, FNAP, FAAN, the Bill and Joanne Conway Dean, and Tracie Schwoyer-Morgan, DNP ’10, MS ’00, ANP-BC, president of the UMSON Alumni Association, presented Sikorski with a certificate recognizing her as an honorary alumna.
Grace Harlow Klein, MS ’68, published the memoir “How Do We Become the Person That We Are? Creating a Life” in January. The book is the story of her experiences as a nurse, professor, and administrator. Though the book is about her life, Klein shares that “it’s not just about me; the ‘We’ in the title is meant to convey the universal drive to understand our self, our life’s journey to create a meaningful life.”
Klein works as a psychotherapist in the Center for Human Encouragement in Rochester, New York, which she opened in 2002. She offers a variety of services and programs, including trauma-informed care, grief counseling, and couples therapy. Prior to opening the center, Klein was an assistant professor at Georgetown University School of Nursing in Washington, D.C., and dean and professor of nursing at the Medical University of Ohio and Syracuse University in New York.

In August, Holly Cole, MA, joined the Office of Development and Alumni Relations as the new director of alumni engagement. Please feel free to reach out to her at hcole@umaryland.edu
Congratulations to the nine alumni who will be inducted as 2024 Fellows of the American Academy of Nursing (AAN) in November and the one alumna inducted as a 2024 Fellow of the American Association of Nurse Practitioners (AANP) in June. They join communities of more than 3,000 AAN and 975 AANP fellows worldwide.
Patsy Maloney, BSN ’74, teaching professor, University of Washington Tacoma School of Nursing and Healthcare Leadership
Beth M. King, MS ’80, associate professor, Florida Atlantic University Christine E. Lynn College of Nursing
Laurie Saletnik, BSN ’89, senior director of perioperative nursing and assistant professor of surgical nursing, The Johns Hopkins Hospital
Brig. Gen. Gwendolyn A. Foster, BSN ’95, director of staff for the U.S. Air Force surgeon general
Angela Ross, DNP ’14, MS ’98, assistant professor, Department of Clinical and Health Informatics, UTHealth Houston D. Bradley McWiliams School of Biomedical Informatics
Luz G. HuntingtonMoskos, BSN ’99, associate professor and director of Community Engagement Core, Center for Integrative Environmental Health Sciences, University of Louisville (Kentucky)
Anna E. Schoenbaum, DNP ’16, MS ’01, vice president of applications and digital health, Penn Medicine (Pennsylvania)
Gregory Raymond, DNP ’18, MS ’10, BSN ’05, vice president of nursing and patient care services, clinical practice and professional development, neuroscience, and inpatient psychiatry, University of Maryland Medical Center
Wen Liu, PhD ’15, associate professor, University of Iowa School of Nursing
Fellow of the American Association of Nurse Practitioners
Kelli Garber, MS ’96, director, DNP Advanced Practice Program, Old Dominion University Ellmer School of Nursing (Virginia)
Carolyn R. Bishop, DIN ’37
Emily Allman, DIN ’38
Rebecca Lillard Umstead, BSN ’45
Betty Jane Mincemoyer, DIN ’48
Barbara M. Tawney, DIN ’50
Marion B. Whitmer, DIN ’51
Suzanne S. Day, DIN ’52
Susan M. Schap, BSN ’55
Patricia Bergman, BSN ’56
Lillian M. Tilles, BSN ’56
Anne E. Bundy, BSN ’59
Carolyn F. McDaniel, BSN ’63
Jane M. Penny, BSN ’63
Madeline Ward, BSN ’63
Barbara Jean Foster, BSN ’64
Barbara J. Frazier, MS ’65
Evelyn M. McElroy, MS ’66
Marilyn C. McGrath, MS ’72, BSN ’68
Barbara A. Oblinger, MS ’68
Rosemary L. Sheehan, BSN ’68
Linda J. Burton, BSN ’69
Velma J. Eckhart, BSN ’69
Sandra L. Parrish, BSN ’69
Margaret C. Parry, BSN ’69
Mary Beth Balsamo, BSN ’70
Billie F. Herrin, MS ’70
Linda D. Cowan, BSN ’72
Elizabeth A. Harris, BSN ’72
Kathleen M. MacLeod, BSN ’72
Barbara E. Anderson, BSN ’74
Mary Lou Grundner, BSN ’74
Danielle C. Lewis, BSN ’74
Barbara E. Heath, BSN ’75
Joan M. Winter, MS ’75
Denise H. Harris, BSN ’77
Maureen A. Minch, BSN ’78
Elizabeth A. Kassel, BSN ’79
Barbara A. Latney, BSN ’79
Madeline C. Ennis, BSN ’80
Dorothy L. Sutch, MS ’86, BSN ’81
Harry J. Mimna, BSN ’82
Harriet W. Moore, MS ’83
Connie Lee Guynn, BSN ’86
Anita D. Hagin, BSN ’86
Marcia F. Haxall, BSN ’86
Susan R. Feldman, MS ’87
Cathy M. Creek, BSN ’88
Clementine L. Viands, BSN ’90
Shari L. Simone, DNP ’11, MS ’96
Diane P. Tedesco, BSN ’99
Miriam N. Woodfield, BSN ’99
Barbara A. Collins, MS ’00
Dawn P. Donohue, MS ’00
John H. Van Der Merwe, MS ’08, BSN ’04
Graclyn Mgbore Abosi, BSN ’09
This list includes notices the School of Nursing received from March 6 - July 8, 2024.

Shari L. Simone, DNP ’11, MS ’96, CPNP-AC, FAANP, FAAN, FCCM, former UMSON assistant professor, died July 8.
She served as both an UMSON faculty member and an affiliate faculty member at the University of Maryland Medical Center (UMMC) and was involved in the development and continuing success of UMSON’s Pediatric Acute Care Nurse Practitioner specialty.
She served as a leader in UMMC’s advanced practice council, contributing to the hospital’s advanced practice structure. She became one of the first advanced practice program managers in 2009. Five years later, she led work to establish a professional advancement model for advanced practice that has served as an archetype nationwide.
Simone was the first nurse practitioner in the UMMC pediatric intensive care unit beginning in 1996 and focused on integrating the nurse practitioner role into critical care. She led 20 research studies, served as a faculty advisor for 20 UMSON Doctor of Nursing Practice
UMSON’s annual All-Alumni Reunion on April 27 brought more than 100 alumni and guests to the School to celebrate. Sue Ann Thomas, PhD, MS ’74, BSN ’69, RN, FAAN, received the Distinguished Alumni Award and shared remarks about her decades-long career as a faculty member and researcher and her contributions to UMSON’s PhD program (see “The Heart of Research,” Page 35). Nine members of her BSN class reunited for their 55th anniversary reunion and to celebrate her accomplishments.
The BSN Class of 1974 celebrated 50 years since their graduation at the Heritage Class induction ceremony and enjoyed a special class dinner later that evening. Class of 2024 BSN graduate Cindy Qi thanked alumni for their support of student scholarships during the reunion lunch.
The following day, more than 40 alumni and friends joined Yolanda Ogbolu, PhD ’11, MS ’05, BSN ’04, the Bill and Joanne Conway Dean, at Oriole Park at Camden Yards to watch the O’s take on the Oakland Athletics.
Stay tuned for more information about our 2025 All-Alumni Reunion!

Thomas (bottom row, second from right) and other members of the BSN Class of 1969, celebrating their 55th anniversary reunion
See more photos from the reunion at nursing.umaryland.edu/reunion.
quality improvement projects, authored 43 publications in peer-reviewed journals and textbooks, and presented at more than 100 conferences nationally and internationally. Her work in reducing delirium in children in the intensive care unit (ICU) setting is particularly notable.
Prior to coming to UMSON as a master’s student in 1992, she began her nursing career on a pediatric unit in Lubbock, Texas, before moving to a charge nurse role at Children’s Hospital Los Angeles, and then working on the pediatric ICU at Johns Hopkins Children’s Center in Baltimore.
Simone was inducted as a Fellow of Critical Care Medicine, a Fellow of the American Association of Nurse Practitioners, and a Fellow of the American Academy of Nursing.
In remembrance of Simone’s life and legacy, her family and friends have established the Shari L. Simone, DNP ’11, MS ’96, CPNP-AC, FAANP, FAAN, FCCM Scholarship Endowment at UMSON. To make a gift in support of the scholarship, visit nursing.umaryland.edu/give/ssimone
SHARE YOUR TIME AND TALENT HOW AND WHEN YOU CHOOSE
Your stories and experiences are invaluable to our students.
Are you passionate about nursing and education? Do you want to impact a student’s future positively? If so, the Office of Development and Alumni Relations is looking for a variety of nursing professionals to speak to students and alumni at various events, both virtually and in person at our Baltimore and Universities at Shady Grove locations.
Speaking sessions typically require less than an hour, can be at any time throughout the year, and can cover a variety of topics.
For more information, contact the Office of Development and Alumni Relations at alumni.nursing@umaryland.edu or 410-706-7640.
The following alumni have returned to UMSON in faculty or staff positions, shaping the next generation of nurses:
Lindsay Ward, MS ’14, BSN ’10, clinical instructor
Ozioma Erondu, DNP ’20, BSN ’14, assistant professor
Victoria Vykol, DNP ’21, MS ’15, assistant professor
Nyree Williams, DNP ’21, MS ’16, assistant professor
Sunny Park, DNP ’22, MS ’17, assistant professor
Molly McComiskey, DNP ’21, assistant professor
Taylor Melton, DNP ’21, assistant professor
Saleha Bharde, MSN ’22, professional development support specialist
Congratulations to the following alumni who received Excellence in Nursing awards from Baltimore magazine at a ceremony in May.
Sherry McGraw, BSN ’85, Psychiatric
Ann Marie Cullen, BSN ’87, Cardiovascular Intensive Care
Barbara O’Connor, MS ’93, BSN ’87, Management/ Nurse Executives
Muriel Larrimore, BSN ’88, Community Care/ Ambulatory Care/ School Nursing
Saundra Goralski, MS ’96, BSN ’92, Acute Care/Family Practice/General Medicine
Treza James, MS ’05, BSN ’96, Pediatrics: Neonatal
M. Tanishia Bailey, BSN ’00, Acute Care/Family Practice/General Medicine
Tracie Schwoyer-Morgan, DNP ’10, MS ’00, Hospice/ Home Health/Palliative Care
Beth Kilmoyer, MS ’01, Management/ Nurse Executives
Rachel Allen, MS ’02, Oncology
Shirley Ashutabi, BSN ’03, Neurology/Psychology/ Behavioral Health
Lynn Desrosiers, MS ’09, Cardiovascular
Kathryn Handy, MS ’09, Educator
Rebekah Friedrich, MS ’17, BSN ’10, Informatics
Lindsay O’Meara, MS ’10, Acute Care/Family Practice/ General Medicine
Jessica Chiappelli, MS ’20, BSN ’13, Educator
Leif Coble, BSN ’14, Informatics
Stacy Foertsch, MS ’17, Cardiovascular
M.J. Rosenthal, MS ’19, Pediatrics: Neonatal
Sue Ann Thomas, MS ’74, BSN ’69
BY GIORDANA SEGNERI
Sue Ann Thomas, PhD, MS ’74, BSN ’69, RN, FAAN, professor emerita, says that the 10 years she spent as assistant dean for the PhD program at UMSON composed the best decade of her academic career.
“It was just a wonderful experience working with these nurses who are so committed to their profession,” she says. “I’m just so, so proud of their accomplishments.”
During the time that Thomas led the program, beginning in 2003, more than 100 students graduated, many fully funded through federal dollars to support graduate assistantships. The Department of Education awarded funding to UMSON three times between 2006 - 12, supporting PhD students with more than $2 million.

“Whenever you go anywhere, there are UMSON alums. They’ve accomplished so much.”
SUE ANN THOMAS
Thomas’ path to the PhD program, and to research, began with her time as an undergraduate student at UMSON. Between her junior and senior years, her mother died. “She had heart disease and was in heart failure most of my life,” Thomas says. “Her chronic illness helped me understand the importance of caring for the whole person and family.” Following graduation, Thomas worked on coronary care units (“They were new at the time,” she says) in Washington, D.C., and Colorado. “I felt after two years in practice that I needed to learn more about the critical care arena,” Thomas explains. “I needed to know more about the heart and EKGs and the technical things you do as a critical care nurse.”
She returned to UMSON to earn her master’s degree; her thesis focused on
heart rate and rhythm in response to visitors – “and that’s when I started looking at how people affect each other’s hearts and minds,” she says. She took a job at what was then University Hospital, serving as one of its first clinical specialists, coordinating care for cardiac patients. She continued researching and publishing on the topic she first explored through her master’s thesis. Through this, she met Erika Friedmann, PhD, professor emerita, who was exploring psychosocial predictors for survival after heart attack, and they began working together. (Friedmann would later serve as UMSON’s associate dean for research.)
Thomas then earned her PhD in Human Development Education and was hired as a faculty member at UMSON in the mid-1970s. She was awarded four National Institute of Nursing Research grants and conducted three large clinical trials focused on the psychosocial factors
of cardiac health. Eventually, after moving back and forth between academia and clinical practice, she landed back at UMSON and in her assistant dean role. She continued to focus on cardiac patients in her research: “What we found was that patients who were depressed were more likely to die after a heart attack,” Thomas says. “We were among the first researchers to identify depression as a risk factor in cardiac patients.” Thomas, who was honored with the Distinguished Alumni Award during UMSON’s All-Alumni Reunion last spring, retired in 2013 and has been focusing on family, fitness, and travel. She remains involved with the School and served as co-chair of the coordinating committee for this fall’s 45th anniversary celebration for the PhD program. “Whenever you go anywhere, there are UMSON alums,” she says. “They’ve accomplished so much. It’s a wonderful sister- and brotherhood to be involved with.”
Sophia Walker Henry, MS ’13
BY JILLIAN DREICER
As a nurse with nearly 30 years of experience – including over two decades in emergency departments (EDs) – Sophia Walker Henry, MS ’13, RN, is no stranger to the ever-changing landscape of health care. One major advancement has been the integration of artificial intelligence (AI) to provide patients with the best level of care.
In 2015, while working as a triage nurse in the ED at Johns Hopkins Hospital, a biomedical engineer and data scientist developed the first AI clinical decision support (CDS) tool that uses data from the electronic medical record (EMR) to help support triage nurses in the ED to make clinical
“The potential to use AI to help fight health disparities is of the utmost importance to me. It is my life’s work.”
SOPHIA WALKER HENRY
decisions. Before the tool went live, the ED was struggling with overcrowding, and the Assigned Emergency Severity Index, a widely used five-level triage algorithm that sorts patients into groups of severity, was ineffective in categorizing patient needs.
Henry says that she was afraid the technology would replace the need for nurses’ expertise in triage; however, she transitioned from skeptic to AI advocate after seeing how the data recommendations still allowed for nurses’ clinical judgment in making the final decision. “I immediately saw that distributing and sorting the patients using this methodology was so much better
than what we were doing before,” Henry says. “It used probability to help us figure out which patients were at risk for bad outcomes and those who were safe to go home.”
Henry explains that by combining data from the EMR with the experience and judgment of the nursing professional, providers can make better decisions, avoiding the subjectivity that can unintentionally result in health disparities when nurses make health care decisions alone. “The potential to use AI to help fight health disparities is of the utmost importance to me. It is my life’s work,” she says. “We will never have a perfect world, but we can do better.”
A year later, Henry presented at the Emergency Nurses Association on the benefits of embracing this technology and how it can have positive effects on patient outcomes. As a result, the developers of the AI CDS tool, who had created a startup company, approached her with an opportunity to become a consultant to continue improving the product and spread awareness.
Since 2022, Henry has been working as a clinical consultant at Beckman Coulter Diagnostics, a company that has since acquired the AI technology that Hopkins first spearheaded. In this role, she strives to keep patient-facing nurses involved in the development of AI tools because of their valuable experience and ideas. “Nurses are creative, and those conversations will help make the tools better,” Henry explains. “I want nurses to be more educated about AI and the impact it can have on our profession and on our patients.”
In addition to her work as a nurse, Henry and her husband, Tony, have owned Sweet Home Jamaica, a restaurant in Brooklyn, Maryland, for the last decade. Tony Henry brings his Jamaican roots and 28

years of restaurant expertise to the operation, while Sophia Henry handles the business side. Their children, Ian and Nathan, are also involved in the business. “I’m super proud with what we’ve been able to do and what we’ve been able to show our children about hard work, perseverance, and pushing through.”
Above all, Sophia Henry is an educator at heart and loves teaching the next generation of nurses. When she began the Health Services Leadership and Management master’s specialty at UMSON, she was teaching at the Community College of Baltimore County (CCBC), Catonsville as a clinical instructor and then taught at Notre Dame of Maryland University in Baltimore in the RN-to-BSN program. Although she’s since taken a step back from the classroom to focus on translating her nursing experience to AI education, Henry keeps in touch with many of her first semester students from CCBC. Through the master’s program at UMSON, Henry says, she learned how to be a better teacher, leader, and worker. “I will forever be grateful for that education,” she says.
To give back to the School, Henry remains involved in the Alumni Council. “I really enjoy talking to students who are about to graduate and helping them prepare to enter this profession,” she says.

American Association of Colleges of Nursing Policy Summit Washington, D.C., March 24

Eastern Nursing Research Society Conference Boston, April 4 - 5
State of the School UMSON Baltimore, April 23


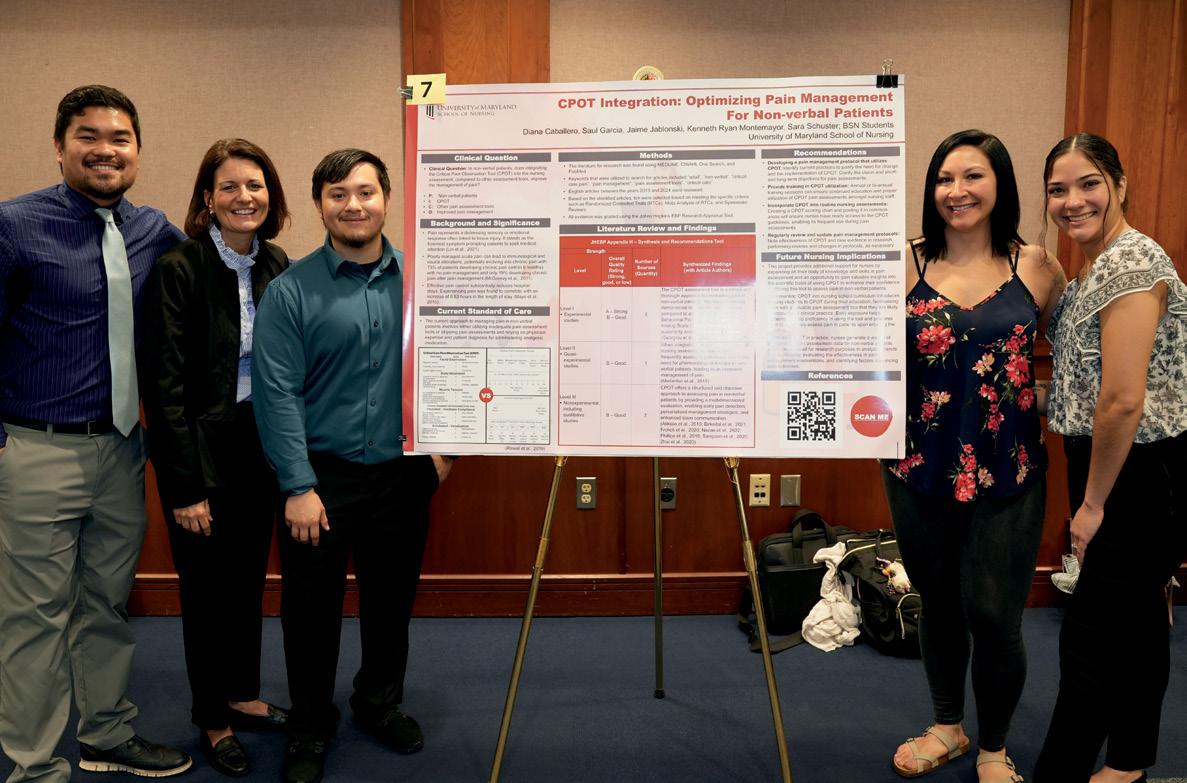
Conway Scholars Luncheon USG, April 16
Maryland Nurses Association Gala Baltimore, May 5


BSN and MSN Clinical Nurse Leader Poster Days USG, May 6 UMB, May 7
DNP Poster Day
UMB, May 10


Nurses Week USG, May 6 - 12
Faculty and Staff Luncheon
UMSON Baltimore, May 13

NLI Culminating Event
Turf Valley Resort, Ellicott City, Maryland, June 3
Living History Museum 25th Anniversary Thursday, Oct. 24
Master’s/Doctoral Online Open House Thursday, Oct. 24
Annapolis Alumni Networking Event Thursday, Nov. 14
COMING SPRING 2025: UMSON 135th Anniversary Celebration and Visionary Pioneer Induction
Stay tuned to UMSON communications for more information.
Learn more about these events and others at nursing.umaryland.edu/events


Welcome Ceremonies
USG, Aug. 13
UMSON Baltimore, Aug. 15

HAPPY BIRTHDAY TO U(MSON)!
Answer:
4 In 1970, tunics and pants were permitted, but tunics could not be worn as mini dresses.

Diane L. Thompkins, MS ’84, RN, wanted to work in computers. Or teaching. Nursing was third on the list. But her mother, who worked as a medical secretary at the local hospital, told her about being a candy striper.
“The more I was a candy striper, watching the nurses, I really liked what I saw – the constant patient contact,” Thompkins says, and it convinced her. But she already had a high school diploma and “I didn’t want two diplomas,” she explains, so she sought out a Bachelor of Science in Nursing program and earned her degree at the University of Buffalo in New York.
“The last day in my undergrad program, I remember the last piece of advice they gave us: ‘You’re going to end up in different places. There’s a place for everyone in nursing: It’s your challenge to find yours.’ You walk away with good critical-thinking skills, problem-solving skills. That’s why as a nurse, you can do anything.”
Once she was a nurse, Thompkins wanted to be an astronaut. Or in the military. She joined the U.S. Air Force and went to flight nursing school. But then her early dreams of teaching returned, and she earned her master’s degree at UMSON, specializing in education. She didn’t wind up teaching, per se, but she did spend 14 years in the National Institutes of Health Clinical Center’s Nursing Education Department.
That led to her expertise in credentialing and certification, which “opened up a whole new world,” she says. She retired last year from her role as certification accreditation manager at the American Nurses Association’s American Nurses Credentialing Center. She made such an impact on the field of specialty certification that the American Board of Nursing Specialties renamed its most prestigious award the Diane Thomkins Lifetime Achievement Award. In April, “I was able to present the first award in my name to the first awardee,” she says. Her mother was there to see it.
Last fall, Thompkins made a significant bequest gift to create the Diane L. Thompkins Scholarship Endowment at UMSON. “I’m the third of five children, and all of us went to college. I understand the benefit of having financial help,” she says. “You can have the ability and the skill, and the only thing in the way is the finances. Nursing is one of those careers that will set a family forward forever. It’s a good profession – I love it. I’m still smiling about it.” — G.S.

This December, UMSON will proudly celebrate a significant milestone: 135 years of leadership, innovation, and transformative impact in nursing education. Such a remarkable achievement is made possible by the unwavering support and dedication of our alumni, faculty, students, staff, and friends.
Each fall, our annual Honor Roll of Donors is published in this magazine, recognizing those who have generously directed their philanthropy to the School. We extend our heartfelt gratitude to you for entrusting UMSON with your donations and investing in our mission – 135 years strong!
Your contributions have supported a multitude of vital causes and projects, including:
• scholarships for students in all programs of study
• initiatives that serve our local, national, and global communities
• efforts addressing the nurse and nurse faculty shortages
• essential equipment for our clinical simulation labs
• and so much more!
This year, as every year, we are deeply grateful to those who have chosen to make a lasting impact on nursing education, whether through gifts of treasure, time, or talent (or all three!). The Office of Development and Alumni Relations looks forward to connecting with more of you – old friends and new –to discuss how we can continue this tradition of excellence together.
Your support is the cornerstone of our success, and with your help, we will continue to shape the next 135 years and beyond.
Stacey M. Conrad, MBA Associate Dean for Development and Alumni Relations
sconrad@umaryland.edu 410-706-7640
JULY 1, 2023 – JUNE 30, 2024
The annual Honor Roll of Donors rcognizes alumni, students, faculty, staff, parents, and friends who have contributed $100 or more to the University of Maryland School of Nursing, July 1, 2023 - June 30, 2024. A list of all donors is available online at nursing.umaryland.edu/honorroll.
As it is impossible to confirm all donors’ credentials, only UMSON degrees and graduation years are included.
$2,000,000+
Bedford Falls Fund of the Morgan Stanley Global Impact
Steven S. Cohen and Sandra D. Cohen
$500,000 - $999,999
Robert Wood Johnson Foundation†
$100,000 - $249,999
Alzheimer’s Association
Mary Catherine Bunting, MS ’72† MedStar Health
National Council on State Boards of Nursing
Regents of University of California
Diane L. Thompkins, MS ’84
$50,000 - $99,999
Marco A. Chacón and Debbie Chacón
John D. Guberski
James Hughes and Malinda Hughes
Miroslava J. Ness*
$25,000 - $49,999
Francis D. Drake
James G. Melonas University of Maryland Medical System†
$10,000 - $24,999
Janet D. Allan and Beverly Hall
Jeanne Ascosi, BSN ’74†
Baltimore Community Foundation
Carolyn J. Brownell, BSN ’86, and Dave Brownell
Marlene H. Cianci, MS ’66, BSN ’65†
Kathleen A. Clark, BSN ’73, and Charles R. Clark
Frank E. & Miriam Loveman Foundation Inc.
Kathryn Patchen Freer, BSN ’74, and Rob Walker Freer†
Judith A. Freitag, BSN ’77
Carol A. Huebner, PhD ’90, and Michael F. Huebner
Estate of Jeanette A. Jones, MS ’70*
Michelle M. Rivest, MS ’79, BSN ’75, and Jeffrey A. Rivest†
Susan L. Tancredi, MS ’79, BSN ’69†
Bertha & Olin Cooper Hoddinott Foundation Fund
$5,000 - $9,999
Estate of E.L. Bunderman, DIN ’31
Jean D. Chess
Wallace J. Hoff
Jane M. Kirschling
Anita M. Langford, MS ’79, BSN ’77†
Myrna E. Mamaril, MS ’93†
Sharon L. Michael, BSN ’71†
Mary Etta C. Mills, MS ’73, BSN ’71†
Elizabeth A. Ness, MS ’93†
Rosemary Noble, BSN ’66†
Joyce A. Parks, DNP ’14, MS ’93, and Kevin Parks
Sandra A. Schoenfisch, MS ’76†
Courtney Ann Kehoe Thomas, BSN ’66†
TRP Program for Charitable Giving Verizon Foundation
Virginia Lee Franklin Memorial Trust†
$2,500 - $4,999
American Association of Nurse Practitioners
Cecil J. Clark Jr., MS ’90†
Jill A. DeCesare, BSN ’69†
Emily P. Deitrick, BSN ’68
Barbara A. Dralnick, MS ’72
Winifred S. Hayes, MS ’74, BSN ’71†
Henrietta D. Hubbard, BSN ’73
Bruce E. Jarrell and Leslie Robinson
Jean M. Jones, BSN ’72
Joseph Jeff McKinney, BSN ’75
Elizabeth C. Minnigh
Glenda B. Motta, BSN ’71
Malinda M. Peeples, MS ’97
Linda E. Rose, PhD ’92, and William G. Smillie
Alyson C. Ross, PhD ’12, and Bennett Ross
Patricia A. Saunders, BSN ’68, and Brian S. Saunders†
Martha J. Shively, BSN ’72†
John P. “Sean” Skelley
Daniel J. Sundeen
John E. Sundeen
Janice M. Thompson, BSN ’62, and Phillip E. Thompson
$1,000 - $2,499
Nellie C. Bailey, MS ’93†
Shawn C. Becker, MS ’05†
Marjorie Stamler Bergemann†
Sally D. Brown, BSN ’74†
Carola Bruflat, BSN ’68†
Kim A. Burks, BSN ’01, and Robert Burks Jr.
Charities Aid Foundation of America
Sharon A. Childs, MS ’91†
Community Foundation of Frederick Co.
Lynne M. Connelly, MS ’78, BSN ’76
Linda K. Cook, PhD ’05, MS ’97
Regina M. Cusson, MS ’79
Emilie M. Deady, BSN ’72†
Janice M. DiGrazia, BSN ’81
Martha M. Dooley, BSN ’72
Rosa R. Goldstein, BSN ’58, and Lawrence Goldstein
Patricia A. Grinnell, MS ’65
Dinah L. Halopka, BSN ’74†
Janet R. Harris, PhD ’97
Patricia A. Hong, BSN ’72†
Jo A. Irving, MS ’70
Nadine A. Jacobs, BSN ’74†
George Johnson and Christine A. Johnson
Sally A. Kaltreider, MS ’88†
Joanne E. King, MS ’03, BSN ’80
Barbara G. Kormann, BSN ’66†
Loree S. La Chance, BSN ’89
Eve L. Layman, BSN ’73†
Angela L. Lee, MS ’93
Patrick T. Lee
Ruth J. Lee, DNP ’10, MS ’04
Nancy B. Lerner, DNP ’10, MS ’74, BSN ’66
Connie Mackowiak, BSN ’69†
Norma J. Melcolm, MS ’69†
Margot Kelley Miles, BSN ’70†
Betty Jane Mincemoyer, DIN ’48*
bold: Louisa Parsons Legacy Society † Cornerstone Club, recognizing those who have donated to UMSON for 20 years or more
* deceased
Kathryn Lothschuetz Montgomery, PhD ’97
Elizabeth S. Niemyer, BSN ’78, and John Niemyer
Joy Norton, MS ’64 Novartis
Elizabeth G. O’Connell, MS ’74, BSN ’73†
Barbara M. O’Connor, BSN ’71
Michael O’Connor
Yolanda A. Ogbolu, PhD ’11, MS ’05, BSN ’04
Cassandra A. Okechukwu, BSN ’00
Tyler Ostrowski and Kathryn M. Ostrowski
Laura J. Owenson
Thomas S. Paullin
Kathleen L. Pelch, BSN ’77, and Jerry F. Pelch Jr.
John M. Preto, MS ’82, BSN ’77, and Jane F. Preto
Elizabeth Boyer Reeder
Carol A. Romano, PhD ’93, MS ’85, BSN ’77†
Rosetta F. Sands, MS ’70, BSN ’66
Pamela Reik Schrank, BSN ’68, and W. Winslow Schrank†
Margaret K. Seuss, MS ’96
Susan E. Simms, BSN ’78
Jeanine Soliman, MS ’09
Rebecca S. Stanevich, BSN ’73†
Sheri B. Stern, MS ’91, BSN ’75, and Jeffrey Stern
Jacquelyn M. Jones Stone, MS ’71
Michael Tafelski and Theresa Tafelski
Neshat Tebyanian, MS ’08, BSN ’01
Anita Throwe, MS ’68
Marion Burns Tuck, MS ’80† Jo Gail Wenzel, BSN ’67, and Richard P. Wenzel
George A. Zangaro, PhD ’05, MS ’98
$500 - $999
Bimbola F. Akintade, PhD ’11, MS ’05, BSN ’03
Anna C. Alt-White, PhD ’87†
American Online Giving Foundation
Linda Daley Atila
Janet C. Austen, MS ’07
Robin Barthlow-Busan, BSN ’81
Deborah S. Beatty, MS ’96
Benevity Community Impact Fund
Christine Boltz, MS ’98
Marita S. Bowden, BSN ’66†
Deborah L. Bowers, BSN ’78
David S. Bush, MS ’09
Kevin M. Byrnes

Gifts provide incoming entry-into-nursing students with white scrub jackets and personal notes of encouragement from donors during the Welcome Ceremonies each semester. Thanks to this generosity, more than 600 students have received their coats free of charge.
Jeffrey S. Cain†
Honora E. Caldwell, BSN ’72
Thomas R. Coe, MS ’94
Stacey Conrad
Linda Costa, BSN ’76
Linda K. Diaconis, MS ’95
Jan M. DiSantostefano, MS ’93†
Sandra Dunnington, BSN ’76, and Kenneth R. Dunnington
Shirley B. Edwards, MS ’80, BSN ’78†
Linda P. Foreman
Kirsten M. Gaskin, MS ’03, and David Gaskin
Patricia Golembieski, BSN ’71†
Bridgitte C. Gourley, DNP ’08
Patricia A. Grady, MS ’68
Susan E. Gutkin, MS ’99
Dorna P. Hairston, PhD ’05, MS ’88†
Laurette L. Hankins
Hill Nurse Consulting LLC
Teri L. Jackson, BSN ’80†
Joseph H. Kelly, MS ’85, BSN ’77, and Mary C. Kelly
Rebecca J. Kelley, DNP ’22, and Ray Kelley
Olufowora M. Kuti, BSN ’77
Pamela A. Lentz, MS ’00, BSN ’84†
Sandra W. McLeskey
Debra L. Mendelsohn, BSN ’76†
Charlotte E. Naschinski, MS ’82†
Gina D. Negri, MS ’03
Lois H. Neuman, BSN ’63†
Yan Ni, BSN ’14
Katharine W. Parris, MS ’95, BSN ’69†
Margaret A. Pedersen, BSN ’74
Jeanette Barnes Priest, BSN ’71†
Julie K. Qashu, MS ’10
Robin O. Quivers, BSN ’74
Barbara M. Resnick, PhD ’96†
Barbara A. Reville, DNP ’11
Robert C. Rinehart
Teresa V. Robison, MS ’88, BSN ’80
Mohamad Amin Saad and Margaret Saad
Harold W. Smith, MS ’77, BSN ’72†
Janet R. Southby, MS ’71†
Joan M. Stanley, MS ’78
Barbara M. Sylvia, PhD ’90
Sue A. Thomas, MS ’73, BSN ’69†
Robin Varker, BSN ’75†
Kamala Via, MS ’12
Rebecca E. Wise, BSN ’69
$250 - $499
Beatrice V. Adderley-Kelly, MS ’71
Denika Baker, BSN ’22
Patricia K. Beneshan, BSN ’66
Andrea Caldwell Berndt, MS ’89
Voncelia S. Brown, MS ’82, BSN ’78
Colleen M. Burke, BSN ’77†
Mary Wolf Byrnes, BSN ’77
Valerie M. Capallo, MS ’84
Lynn Chen
Monica J. Clark-McGrew, BSN ’80
Justin Codd and Giordana Segneri
Barbara L. Conrad, BSN ’73†
Donna M. Dorsey, MS ’75†
Jewel L. Edmonds, BSN ’12
Kathleen O. Farrell, BSN ’73
Margaret A. Franckhauser, MS ’82
Denise C. Geiger, BSN ’79†
Crystal L. Greene, DNP ’15, BSN ’09
Melissa C. Holley, BSN ’93
Kristine R. Holmes, BSN ’74
Mary P. Howard, MS ’94, BSN ’73
William O. Howie, BSN ’82
Carolyn Hughes and Thomas O. Hughes
Iris F. Ingber, BSN ’71
Jane F. Kapustin, MS ’85†
Jade S. Kim, DNP ’19
Lynda A. King, BSN ’69
Diane T. Langford, BSN ’75†
Patricia A. Lewis, BSN ’80
Laurice P. Lucas, BSN ’82
Dianne L. Mackert, BSN ’72
Neda M. Mirjafary, BSN ’15
Mark Niedzwiecki and Kristen Niedzwiecki
Patricia B. O’Donnell, MS ’76, BSN ’70
Oluwakemi D. Ogunseye, DNP ’20
Raphael A. Onyedinma, BSN ’95
Promise Home Healt, Inc.
Robin Prothro, BSN ’79
Joanne S. Reifsnyder, PhD ’00
Natalie J. Rook, MS ’85, BSN ’72†
Elizabeth A. Ruiz, DNP ’21
Kay F. Sauers, MS ’78, BSN ’72
Marilyn S. Schmitter, BSN ’64†
Giovanna B. Schummer, BSN ’07
Susan K. Schurman, MS ’08, BSN ’99
Nayna Shah
Cynthia C. Sikorski and Richard J. Sikorski
Aliza Sollins
Debra A. Spencer, MS ’99
Dale R. Spielman, BSN ’95
Thomas C. Stewart, MS ’97, and Catherine Dischner
Florence C. Strawser, BSN ’71†
Anne Smyth Terry, BSN ’78
Margaret E. Trimble, BSN ’67
UnitedHealth Group
Barbara L. Van de Castle, DNP ’14
Dianna Vass
Cesar J. Visurraga, DNP ’18
Joan I. Warren, PhD ’04, MS ’88†
Mary L. Wetter, MS ’92
Katharine Wheaton, BSN ’15
Anne D. Williams, DNP ’12, MS ’86, BSN ’82
Margaret C. Wilmoth, MS ’79, BSN ’75†
$100 - $249
Nancy R. Alga, BSN ’76
Lisa Allman, BSN ’93†
Maureen S. Anderson, MS ’09, BSN ’01
Cheryl A. Andrews, MS ’99, BSN ’77
Cynthia A. Arnold, MS ’95, and Lamar Arnold
Edith E. Asirifi, BSN ’18
Oluchi J. Ayichi, DNP ’17, MS ’11, BSN ’01
Olayemi T. Ayilegbe, MS ’18
Janis L. Bahner, BSN ’71
Alicia R. Baker, BSN ’04
Candy Barbag, BSN ’72
Christine L. Barclay, BSN ’77
Mark B. Bauman, BSN ’89
Monika E. Bauman, MS ’10, BSN ’90
April J. Bauman-Dunlevy, MS ’12
LaKeisha D. Beasley, MS ’07
Abbe R. Bendell, BSN ’74
Joan R. Benfield, MS ’92†
Edna J.K. Benware, BSN ’76†
Eva K. Berkow, BSN ’59†
Mary Griffin Bey, BSN ’75
Pamela J. Biernacki, BSN ’83
Kimberlie A. Biever, MS ’07, MS ’00
Gloria E. Boedeker
Karen A. Boliek, MS ’93
Patricia J. Bosak, BSN ’69
Gloria Boseman, MS ’78
Patricia L. Botic, MS ’81
Margaret A. Bradford, MS ’76, BSN ’74†
Gregory H. Brandon
Blanche R. Brown, DNP ’15
Paul L. Brunson, BSN ’88
Barbara J. Bungard, MS ’11
Zivago Z. Bunting, DNP ’22, MS ’17, BSN ’00
Lisette K. Bunting-Perry, BSN ’83
Brooke K. Buppert, BSN ’06
Rose M. Burke, BSN ’74†
Susan C. Buskirk
E. Bronwyn Byron, BSN ’79
Kathryn A. Cadwell, MS ’93, BSN ’75†
Christopher F. Callaghan
April A. Campbell, BSN ’91†
Cynthia A. Carbo, BSN ’78
Berlyn S. Carlson, BSN ’73†
Debra L. Casson-Patton, BSN ’84
Rita K. Charney, BSN ’82, and Donald Joseph Charney
Carmiele E. Ciamillo, MS ’74
Michael E. Clarke, BSN ’23
Sandra M. Cleaver, MS ’84
Jane B. Clemmens, DIN ’50
Anne H. Cole, BSN ’67 †
Frona S. Colker, MS ’74†
Imogene S. Combs, BSN ’69†
Susan K. Connell, BSN ’68
Susan G. Conner-Guterl, MS ’89
Karen A. Cook-Henderson, BSN ’72
Laura A. Courtright, MSN ’21
P. Dale Every Creighton, BSN ’58
Georgia E. Cusack, MS ’99, BSN ’84
Kristine M. Daisley-Barron, BSN ’89
Leslie W. Daugherty, BSN ’75†
Charlotte E. Davies, MS ’68†
Linda Lindsey Davis, PhD ’84†
Dayton Foundation
Mary E. De Salvo, MS ’93
Beverly A. Dearing-Stuck, MS ’78, BSN ’69
Amanda H. D’Erasmo, BSN ’95
Marsha H. DeWeese, MS ’93
Valerie DeWeese, BSN ’81†
Carol A. Distasio, MS ’73, BSN ’71†
Patricia L. Dorio, BSN ’95
Carmalyn M. Dorsey, BSN ’73
Carol Swamidoss Douglas, BSN ’85
Patricia B. Eagen, BSN ’63†
Melissa A. Eakle, MS ’01, BSN ’99
Abaneh Ebangwese, BSN ’15
Kathleen F. Edwards, BSN ’67
Lori A. Edwards, BSN ’80
Rose Eisenbeiss, BSN ’09
Ann Louise Ellenson, BSN ’70†
Marjorie E. Ewertz, BSN ’74
Donna M. Feickert-Eichna, BSN ’73
Marylouise K. Felhofer, MS ’91
Corinne Fender, BSN ’86
Cheryl Fisher
Judith G. Flemmens, BSN ’67†
Dorrie K. Fontaine, MS ’77, and Barry Fontaine
Janet Tull Foreman, MS ’81, BSN ’76†
Julie C. Fortier, MS ’68†
Frances D. Fosbroke Cox, BSN ’74
Adalyn G. Frank, MS ’95
Edward G. Frank, BSN ’82
Silvia I. Freyre, BSN ’11
Wanona S. Fritz, MS ’78
Audrey G. Gift, PhD ’84, and James Gift
Robyn C. Gilden, PhD ’10, MS ’01
Vicki L. Gillmore, PhD ’90, MS ’77, BSN ’76†
Maggie Johnson Glover, PhD ’03
Antoinette M. Gonzalez, BSN ’55†
Ellen J. Gorman, MS ’93†
Mary J. Graham, MS ’80, and W. Barry Graham
Elizabeth H. Green, BSN ’21
Claire P. Greenhouse, BSN ’66†
Margaretta C. Grimm, MS ’86, BSN ’81†
Cecelia M. Grindel, PhD ’88†
Carole F. Hair, MS ’79
Billie J. Hamilton-Powell, BSN ’88
Maureen P. Hanold, BSN ’80
Debbra M. Hattery, MS ’96
Joan N. Hebden, MS ’85, BSN ’75
Pamela D. Heckler
Nancy A. Hedden, MS ’02, BSN ’72

Estate of Myrtle Ageton, DIN ’44, and Robert Ageton
Janet D. Allan Anonymous
Floraine B. Applefeld
Estate of Carolyn V. Arnold
Jeanne Ascosi, BSN ’74
Estate of Zabelle S. Howard Beard
Deborah S. Beatty, MS ’96
Abbe R. Bendell, BSN ’74
Estate of Ann F. Bennett, MS ’69
Marjorie Stamler Bergemann
Estate of Jean L. Bloom, DIN ’46
Estate of Margaret Brandt, DIN ’50
Estate of Mary J. Brewer
Estate of E.L. Bunderman, DIN ’31, and Clarence Q. Bunderman
Estate of Ann Ottney Cain
Estate of Dorothy C. Calafiore, BSN ’51
Estate of Shirley E. Callahan, BSN ’52
Sharon A. Childs, MS ’91
Estate of Avon B. Chisholm
Marlene H. Cianci, MS ’66, BSN ’65
Estate of Gladys B. Clagett and Lansdale G. Clagett
Estate of Bonnie L. Closson, BSN ’61
Jon B. Closson
Claudette C. Clunan, BSN ’72
Steven S. Cohen
Regina M. Cusson, MS ’79
Estate of Mary Jane Custer
Jill A. DeCesare, BSN ’69
Carol Distasio, MS ’73, BSN ’71
Nancy Donovan, BSN ’76
Susan G. Dorsey, PhD ’01, MS ’98
Carol Drake, BSN ’68*, and Francis D. Drake
Celeste A. Dye, BSN ’66
Kathleen F. Edwards, BSN ’67
Estate of Barbara Elgin, BSN ’54, and Lee Elgin
Estate of Lura Jane Emery, MS ’79
Julie C. Fortier, MS ’68
Judith A. Freitag, BSN ’77
Beth Ann Gan, BSN ’77
Estate of Mary H. Gilley, DIN ’44
Debbie Gilbert Glassman, MS ’79, BSN ’75
Estate of Judah Gudelsky
The School of Nursing’s Legacy Society is named in honor of pioneering nurse and philanthropist Louisa Parsons, the University of Maryland School of Nursing’s first superintendent; she made the first planned gift to the School in 1916. The Louisa Parsons Legacy Society comprises people who, like Parsons, are committed to supporting future generations of students and nurses by providing funding for scholarships, research, faculty positions, and other critical needs. Joining the Louisa Parsons Legacy Society allows you to make a significant difference to future nursing students without impacting your current lifestyle.
To learn more about making a planned gift, contact Stacey Conrad, associate dean for development and alumni relations, at sconrad@umaryland.edu or 410-706-7640.
Carolyn Cook Handa, BSN ’63*
Laurette L. Hankins
Sharon Hanopole, BSN ’66
Phyllis B. Heffron, BSN ’74
Barbara R. Heller
Estate of K. Cornelia Hesselbach
Estate of Marie L. Hesselbach
Estate of Kjerstine K. Hoffman, DIN ’47
Carol A. Huebner, PhD ’90, and Michael F. Huebner
Margaret H. Iles, DIN ’53
Catherine Ingle, BSN ’61
Estate of Mary McCotter Jackson
Estate of Jeanette Jones, MS ’70
Estate of Jean W. Keenan, DIN ’48
Jane M. Kirschling and Robert Flick*
Anita M. Langford, MS ’79, BSN ’77
Cynthia P. Lewis, BSN ’58, and Jack C. Lewis
Estate of Phyllis R. Luckenbaugh, MS ’79, BSN ’72, and Paul Luckenbaugh
Estate of Ann Madison, BSN ’62
Estate of Mildred Madsen, BSN ’73
Estate of Rita Malek, DIN ’49
Myrna E. Mamaril, MS ’93
Estate of Demetria Manandic, BSN ’54
Estate of Lois Marriott
Joan Nicholason Martellotto, BSN ’66
Margaret A. McEntee, MS ’73
Estate of Wealtha McGurn
Beverly J. Meadows, PhD ’06, MS ’84, BSN ’69
Norma J. Melcolm, MS ’69
Estate of Joan L. Meredith, BSN ’62
Sharon L. Michael, BSN ’71
Nancy J. Miller, BSN ’73
Patricia Gonce Morton, PhD ’89, MS ’79
Sondra M. Mroz, BSN ’66
Elizabeth A. Ness, MS ’93
Evelyn Norwitz
Elizabeth G. O’Connell, MS ’74, BSN ’73
Daniel J. O’Neal III, BSN ’66
Harriet Palmer-Willis, MS ’70, BSN ’68
Barbara J. Parker, PhD ’86, MS ’76
Charlene M. Passmore, BSN ’77
Thomas S. Paullin
Margot A. Regen, MS ’79
Ann E. Roberts, BSN ’93
Estate of Margaret Robinson
Linda E. Rose, PhD ’92, and William G. Smillie
Estate of Amelia Carol Sanders, DIN ’53
Patricia A. Saunders, BSN ’68
Estate of William Donald Schaefer
Estate of Phyllis J. Scharp, BSN ’50
Sandra A. Schoenfisch, MS ’76
Eleanor B. Schron, PhD ’08, MS ’79, and Spencer R. Schron
Estate of Alta Fay Schuster, BSN ’54
Estate of Beverly Seeley
Christine K. Shippen, MS ’98, BSN ’73
Martha J. Shively, BSN ’72
Deborah K. Shpritz, MS ’82, BSN ’78, and Louis Shpritz
Estate of Betty Lou Shubkagel, BSN ’54
Estate of Anna Mae Slacum
Estate of Connie Slewitzke, BSN ’71
Rebecca S. Stanevich, BSN ’73
Barbara A. Stepura, MS ’85
Estate of Marie V. Stimpson, MS ’89, BSN ’84
Jacquelyn M. Jones Stone, MS ’71
Estate of Sandra Sundeen, MS ’68
Estate of Ginger V. Swisher, DIN ’49
Susan L. Tancredi, MS ’79, BSN ’69, and Peter Tancredi
Courtney Ann Kehoe Thomas, BSN ’66
Diane L. Thompkins, MS ’84
Virginia D. Thorson, BSN ’55
Estate of Norma C. Tinker, BSN ’48
Estate of Martha C. Trate, BSN ’48
Marion Burns Tuck, MS ’80
Robin Varker, BSN ’75
Elena V. Virts, PhD ’15, BSN ’00
Joella D. Warner, BSN ’64
Estate of Helen Parker Wear
Doris Baumgardner Webb, BSN ’59, and John H. Webb*
Margaret C. Wilmoth, MS ’79, BSN ’75
Susan Dorsey Wilson, BSN ’66
Estate of Patricia Yow
As we are unable to confirm all alumni credentials, only UMSON degrees and graduation years are included.

Gifts have provided us with the funds necessary to create new displays and exhibits. This generosity ensures that we continually share the story of our rich and diverse past, celebrating our heritage and inspiring future generations.
Louise L. Heinz, BSN ’71
Regina F. Hendrix, BSN ’83
Kathleen M. Herberger, BSN ’85
Donna C. Herndon, BSN ’69
Eileen B. Hollander, MS ’89, BSN ’83, and Craig Hollander
Rebecca E. Holston, BSN ’19
Jane M. Houck, MS ’84†
Maeve Howett
Teresa Hughes
Brenda S. Jackson, MS ’77
Courtney B. James, BSN ’18
Karen A. Jeffries, MS ’91
Elizabeth C. Jesada, MS ’78, BSN ’74
Kathleen P. Johnson, MS ’96
William Jordan, BSN ’81†
Abidogun B. Kehinde, BSN ’99
Carol A. Kelley, BSN ’78
Christina A. Kelly, BSN ’10
Gail G. Kestler, BSN ’71†
Andrew Kotch
Elizabeth A. Krug, MS ’10
Vera Kuffour-Manu, PhD ’18 ’13, MS ’10
Shiree L. Kwash, BSN ’83
Nancy Lacy, BSN ’54
Linda S. Lammeree, BSN ’94
Mary Ann Lancaster, MS ’87†
Gloria R. Lay, MS ’14
Harriet Leap, BSN ’62†
Sheila E. Lee, BSN ’83
Amy E. Lewis, MS ’09, BSN ’05
Shirley Eppel Liberman, BSN ’55†
Carol A. Libonati, MS ’86, BSN ’68†
Dorothy Liddel, BSN ’61†
Judith D. Lobis, BSN ’67
Nancy Lougheed, BSN ’61
Barbara J. Major, BSN ’74†
Ellen G. Mann, BSN ’68
Jane E. Mansfield, BSN ’76†
Jo Ellen Marek, BSN ’64†
Susan Dullea Markus, MS ’06, BSN ’74
Beth A. Martucci, DNP ’10, MS ’99, BSN ’96
Jeanne A. Matthews, PhD ’91
Gail O. Mazzocco, MS ’74†
Nancy H. McAlduff, DNP ’23
Anne E. McArdle, BSN ’74 †
Donna Behler McArthur, PhD ’98, BSN ’76
Clayton S. McCarl Jr.
Lisa S. McCarl, MS ’84, BSN ’81
Mariah D. McCarthy, BSN ’72
Marie C. McCarthy, MS ’79
Kathleen G. McElroy, PhD ’16, MS ’10
Ann Scanlon McGinity, MS ’74
Josephine McKee, BSN ’71†
Christina L. McKenzie, BSN ’93
Pat McLaine
William J. McLennan
Beverly J. Meadows, PhD ’06, MS ’84, BSN ’69
Mary E. Merolla, BSN ’64
Amare G. Metaferia, BSN ’15
Lillian A. Milburn, BSN ’04
Susan C. Miles, MS ’04, BSN ’03
Gayle Sharon Miller, BSN ’66
Marilyn J. Miller, PhD ’00, MS ’81, BSN ’79
Priscilla O. Mills, BSN ’69
Sharon R. Mills, BSN ’79
Marik A. Moen, PhD ’18
Victoria A. Mohr, BSN ’73
Jacqueline M. Moore, PhD ’90
Nina Munck, BSN ’18
Kathleen T. Murphy, BSN ’87
Hannah Murphy Buc
Nicole L. Nash
Tesgera D. Negewo, BSN ’17
Mary A. Nichols
Myra N. Njapau-Dove, DNP ’20
Treen F. Null, BSN ’78
Anthony N. Nwaiwu, DNP ’18, MS ’14
Killian M. O’Donnell, MS ’98, BSN ’95
Bonnie Oettinger, BSN ’69
Diane E. Olechna, MS ’00
Daniel J. O’Neal III, BSN ’66
Lynn M. Oswald
Onyinyechi M. Ozoji, BSN ’18
Anna L. Parker, BSN ’68
Nicole B. Parson, MS ’11
Gaynelle L. Pearson, BSN ’74
Terry S. Peck, BSN ’82
Regina Phillips, MS ’79
Mark Pieters
Karen C. Poisker, MS ’81, BSN ’78†
Susan E. Postal, DNP ’14, MS ’06, BSN ’87
Nan K. Pue, BSN ’66†
Madonna Putz-Vitarello, BSN ’84
Geraldine L. Raber, MS ’13
Suzanne R. Ranson, BSN ’76†
Carol A. Rauen, MS ’91, BSN ’81†
Karen K. Reichert, BSN ’66
Laurel A. Renaud, BSN ’80†
Marianne E. Rhodes, BSN ’69
Loretta M. Richardson, MS ’71, BSN ’68†
Hjordis Richstein, BSN ’09
Eleanor M. Riordan, BSN ’47†
Ellen S. Ristorcelli, BSN ’81
Mary A. Rogers, BSN ’73
Caleb A. Rogovin, MS ’92†
Barbara A. Rose, MS ’93
Janet Rowan, MS ’63, BSN ’61†
Kathleen D. Sanford, BSN ’74
Jill S. Sanko, MS ’03
Barbara B. Scharf, PhD ’09
Carole Schauer, MS ’70†
Karen E. Scheu, DNP ’12
Barbara Schmitthenner, BSN ’57†
Deborah Lynne Schofield, DNP ’09, MS ’95
Katherine Scott, DNP ’19
Brian C. Sharkey, MS ’00, BSN ’98
Patricia A. Skelton, MS ’93
Andrea L. Smith, MS ’83
Claudia M. Smith, BSN ’65†
Marc C. Smith, DNP ’17
Laura M. Sorkin, MS ’96†
Katharine S. Speers, BSN ’54†
Eva F. Squibb, BSN ’13
Jean P. Staples, BSN ’68†
Laura E. Stephens, MS ’01
Mary E. Stewart, BSN ’81
Susan R. Stone, MS ’87, BSN ’82
Elizabeth K. Tanner, MS ’74, BSN ’70
Shirley B. Teffeau, BSN ’55†
Barbara N. Terry, BSN ’71†
Bernadette R. Thomas, BSN ’04
Rita H. Tonner, MS ’98, BSN ’71
Darlene Augins Tyson, BSN ’74
Nina K. Ungar, BSN ’83
Constance R. Uphold, PhD ’88
Kim L. VandenAssem, MS ’11, BSN ’87
Jane M. Vardaro, MS ’77, and Joseph E. Vardaro
H. Christian Vinyard, BSN ’19
Lorrie Voytek
Mary R. Walkup, DIN ’45
Mary Patricia Wall, PhD ’04
Jessie Wang, BSN ’00
Claire P. Watters, BSN ’74
Edward C. Watters
Linda Elaine Wendt, PhD ’91†
Robert W. West, BSN ’14
Ouida E. Westney, MS ’65
Mary E. White, BSN ’76
Paula A. Wiegel-Thrasher, BSN ’73
John W. Willis Jr., BSN ’93
J P. Wilson, BSN ’13
Adele Wilzack, MS ’66†
Barbara V. Wise, PhD ’99, MS ’82
Judith R. Wood, BSN ’71
Donna J. Wooditch, BSN ’74
Priscilla S. Worral, PhD ’86
Meghan Wyvill, BSN ’17
Vasso G. Yfantis, MS ’01, BSN ’97
Sherry L. Zane, BSN ’69
Teresa S. Zemel, MS ’87, BSN ’77†
Answer:
5 UMSON launched its BSN program in 1925 but there is no documentation of graduates until 1934. At the time, the program required five years to complete: two at the University of Maryland, College Park (UMCP) and three years in Baltimore. The length of the program limited its popularity. In 1952, a shortened BSN program (two years at UMCP, two years in Baltimore) was adopted under Dean Emerita Florence Gipe, EdD, RN.
May 6, the first day of National Nurses Week, was beautiful in Baltimore, a perfect day to kick off the weeklong celebration (and cool off from the heat of finals and the end of the semester) with an ice cream social in the UMSON courtyard. Students, faculty, staff, and nurses from the University of Maryland Medical Center descended upon the grassy area and patiently queued for a scoop or two of Baltimore’s famed Taharka Brothers Ice Cream and make-your-own-sundae toppings.

The event also featured smiles for miles at a selfie station, giveaways, and a surprise appearance by a famous local bird — all part of a sweet thank you from the School to the students, employees, and colleagues that make a difference for patients, families, and communities worldwide.
A similar celebratory event was held at UMSON at the Universities at Shady Grove the next day.
Office of Communications 655 W. Lombard St. Baltimore, MD 21201 nursing.umaryland.edu
“This scholarship will help me financially to further my education. I plan to take the Certified Nurse Educator exam and seek employment as a nurse educator. I will never forget your generosity by passing that generosity to future nursing students.”
Dirk W. Pennington, DNP, RN Teaching in Nursing and Health Professions Certificate Student
Dirk is a first-generation American, a former U.S. Navy Hospital Corpsman, and one of the first students admitted to the teaching certificate as a Conway Scholar in spring 2024, receiving a full scholarship that covers tuition, fees, and books. Support from alumni and friends helps UMSON combat the nursing faculty shortage. Will you consider investing in the future of nursing education? MAKE YOUR GIFT TODAY at nursing.umaryland.edu/give