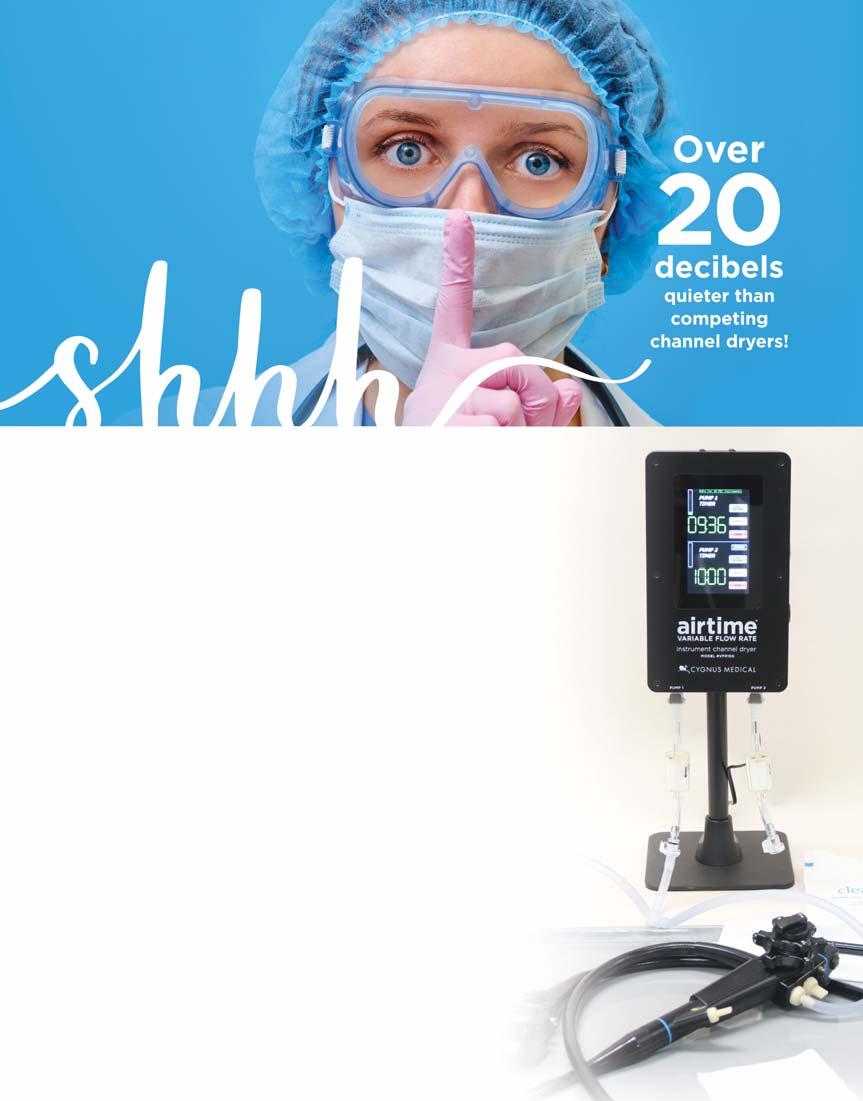
Endoscope Reprocessing & Infection Control





• NO SODIUM PHOSPHATE1
• SAFE AND EFFECTIVE1,2
• ACG-RECOMMENDED SPLIT-DOSE REGIMEN3

– Two SUTAB doses are required for a complete preparation1




Dose 1 consists of 12 tablets and 16 oz of water
Dose 2 consists of 12 tablets and 16 oz of water Each dose is followed by two additional 16 oz of water
92% OF PATIENTS IN TWO PIVOTAL TRIALS ACHIEVED SUCCESSFUL BOWEL CLEANSING WITH SUTAB1,2* 91% OF PATIENTS IN ONE PIVOTAL TRIAL RATED SUTAB AS TOLERABLE TO VERY EASY TO CONSUME2†
• 52% of all SUTAB and MoviPrep® patients reported at least one selected gastrointestinal adverse reaction1,2‡ considered severe2‡ 78% OF PATIENTS IN ONE PIVOTAL TRIAL WOULD REQUEST SUTAB AGAIN FOR A FUTURE COLONOSCOPY2†
* 3 (good) or 4 (excellent) by the blinded endoscopist; scores were assigned following completion of the colonoscopy. †Patients completed a preference questionnaire following completion of study drug to capture their perceptions of the preparation experience. This questionnaire has not undergone formal validation.
‡Patients were queried for selected gastrointestinal adverse reactions of upper abdominal pain, abdominal distension, nausea, and vomiting following completion of study drug, rating the intensity as mild, moderate, or severe.1,2

ACG=American College of Gastroenterology MoviPrep is a registered trademark of Velinor AG.
Packaging and tablets not shown actual size.
SUTAB® (sodium sulfate, magnesium sulfate, potassium chloride) tablets for oral use is an osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults. DOSAGE AND ADMINISTRATION: A low residue breakfast may be consumed. After breakfast, only clear liquids may be consumed until after the colonoscopy. Administration of two doses of SUTAB (24 tablets) are required for a complete preparation for colonoscopy. Twelve (12) tablets are equivalent to one dose. Water must be consumed with each dose of SUTAB and additional water must be consumed after each dose. Complete all SUTAB tablets and required water at least 2 hours before colonoscopy. CONTRAINDICATIONS: Use is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUTAB. WARNINGS AND PRECAUTIONS: : Encourage adequate hydration, assess concurrent medications and consider laboratory assessments prior to and after each use; Cardiac arrhythmias: Consider pre-dose and post-colonoscopy ECGs in patients at increased risk; Seizures: Use caution in patients with a history of seizures and patients at increased risk of seizures, including medications that lower the seizure threshold; Patients with renal impairment or taking concomitant medications that affect renal function: Use caution, ensure adequate hydration and consider laboratory testing; Colonic mucosal ulcerations
Suspected GI obstruction or perforation: Rule out the diagnosis before administration. Hypersensitivity reactions, including anaphylaxis: Inform patients to seek immediate medical care if symptoms occur. ADVERSE REACTIONS: Most common gastrointestinal adverse reactions are: nausea, abdominal distension, vomiting and upper abdominal pain.
DRUG INTERACTIONS:
Please see Brief Summary of Prescribing Information on reverse side. See Full Prescribing Information and Medication Guide at SUTAB.com

BRIEF SUMMARY: Before prescribing, please see Full Prescribing Information and Medication Guide for SUTAB® (sodium sulfate, magnesium sulfate, potassium chloride) tablets for oral use.
INDICATIONS AND USAGE: An osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults.
DOSAGE AND ADMINISTRATION: Split Dose (2-Day) Regimen: Dose 1 – On the day prior to colonoscopy: A low residue breakfast may be consumed. After breakfast, only clear liquids may be consumed until after the colonoscopy. Early in the evening prior to colonoscopy, open one bottle of 12 tablets. Fill the provided water and drink the entire amount over 15 to 20 minutes. Approximately one hour after
Packaging and tablets not shown actual size.
Dose 2 - Day of colonoscopy: Continue to consume only clear liquids until after the colonoscopy. The morning of colonoscopy (5 to 8 hours prior to the colonoscopy and no sooner than
CONTRAINDICATIONS: Use is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUTAB. WARNINGS AND PRECAUTIONS: Serious Fluid and Electrolyte Abnormalities: Advise all taking SUTAB, consider performing post-colonoscopy lab tests (electrolytes, creatinine, and BUN). Fluid and electrolyte disturbances can lead to
disturbances or may increase the risk of adverse events of seizure, arrhythmias, and renal impairment; Cardiac arrhythmias: Use caution when prescribing SUTAB for patients at increased risk of arrhythmias (e.g., patients with a history of prolonged QT, uncontrolled arrhythmias, recent myocardial infarction, unstable angina, congestive heart failure, or cardiomyopathy). Consider pre-dose and post-colonoscopy ECGs in patients at increased risk of serious cardiac arrhythmias; Seizures: Use caution when prescribing SUTAB for patients with a history of seizures and in patients at increased risk of seizure, such as patients taking medications that lower the seizure threshold (e.g., tricyclic antidepressants), patients withdrawing from alcohol or benzodiazepines, or patients with known or suspected hyponatremia; Use in Patients with Risk of Renal Injury: Use SUTAB with caution in patients with impaired renal function or patients taking concomitant medications that may affect renal function (such as diuretics,
for renal injury. Advise these patients of the importance of adequate hydration with SUTAB and consider performing baseline and post-colonoscopy laboratory tests (electrolytes, creatinine, and BUN) in these patients; Colonic Mucosal Ulcerations and Ischemic Colitis: Osmotic laxative products may produce colonic mucosal aphthous ulcerations, and there have been reports of more serious cases of ischemic colitis requiring hospitalization. Concurrent use of stimulant laxatives and SUTAB may increase these risks. Consider the potential for mucosal ulcerations resulting from the Use in Patients with Signifcant Gastrointestinal Disease: If gastrointestinal obstruction or perforation is suspected, perform appropriate diagnostic studies to rule out these conditions before administering SUTAB. Use with caution in patients with severe active ulcerative colitis. Hypersensitivity Reactions: Serious hypersensitivity reactions, including anaphylaxis, angioedema, dyspnea, rash, pruritis and urticaria have been reported with SUTAB. Inform patients of the signs and symptoms of anaphylaxis and instruct them to seek immediate medical care should signs and symptoms occur. ADVERSE REACTIONS: Most common gastrointestinal adverse reactions are: nausea, abdominal distension, vomiting and upper abdominal pain. Postmarketing Experience: Gastrointestinal: gastric ulceration, gastritis; Hypersensitivity: anaphylaxis, angioedema, dyspnea, rash, pruritus, urticaria.
POTENTIAL FOR DRUG ABSORPTION: SUTAB can reduce the absorption of other co-administered drugs. Administer oral medications at least one at least 2 hours before and not less than 6 hours after administration of each dose of SUTAB to avoid chelation with magnesium. Pregnancy: There are no available data on SUTAB use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. No reproduction or developmental studies in animals have been conducted with sodium sulfate, magnesium sulfate, and potassium chloride (SUTAB). Lactation: There are no available data on the presence of SUTAB in human or animal milk, the effects on the breastfed child, or the effects on milk production. Pediatric Use: Safety and effectiveness in pediatric patients has not been established. Geriatric Use: older. No differences in safety or effectiveness of SUTAB were observed between geriatric patients and younger patients. Elderly patients are more
abnormalities. STORAGE temperature. Rx only. Manufactured by Braintree Laboratories, Inc. Braintree, MA 02185
See Full Prescribing Information and Medication Guide at SUTAB.com.

References:1. SUTAB® [package insert]. Braintree, MA. 2 Di Palma JA, Bhandari R, Cleveland M, et al. A safety and subjects undergoing colonoscopy. Am J Gastroenterol 3. Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM; ACG. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol.
For additional information, please call 1-800-874-6756
©2022 Braintree Laboratories, Inc. All rights reserved. 201-289-v4-A February 2022
JOSEPH MALICHIO
Vice President, Medical Education jmalichio@mcmahonmed.com





MICHELE MCMAHON VELLE

Creative Director
JEANETTE MOONEY Senior Art Director
JAMES O’NEILL Senior Systems Manager
RON REDFERN Production Manager
ROB SINCLAIR Circulation Manager
VAN VELLE

President, Partner
MATTHEW MCMAHON General Manager, Partner
LAUREN SMITH
MICHAEL P. MCMAHON
MICHELE MCMAHON VELLE Partners
RAY & ROSANNE MCMAHON Co-founders
McMAHON PUBLISHING
Sales, Production and Editorial Offices: 545 West 45th Street, 8th Floor New York, NY 10036 Telephone: (212) 957-5300

Subscription: $95 for 1 year ($120 outside USA); Single Copies $15 ($20 outside USA)


Gastroenterology & Endoscopy News (ISSN 0883-8348) is published monthly by McMahon Publishing. Periodicals postage paid at New York, NY, and at additional mailing offices.
POSTMASTER: Send address changes to: Gastroenterology & Endoscopy News 545 West 45th Street, 8th Floor New York, NY 10036


















Commentaries and opinions do not necessarily reflect the views of the publication.
Disclosure Statement: We endeavor to obtain relevant financial disclosures from all interviewees and rely on our sources to accurately provide this information, which we believe can be important in evaluating the research discussed in this publication.
Copyright © 2022 McMahon Publishing Group, 545 West 45th Street, 8th Floor, New York, NY 10036. Printed in the USA. All rights reserved, including the right of reproduction, in whole or in part, in any form.




Imagine a work scenario where endoscopes are always available. You simply unpack a new, sterile gastroscope, connect it to the Ambu® aBox™ 2 display and processing unit and the standard ancillary equipment, and get to work.
Ambu single-use GI endoscopes are sterile and ready to use out of the pack. They offer consistent quality, feel and performance. Plus, the initial upfront investment is marginal compared with a reusable setup.
Learn more at www.ambuUSA.com/ single-use-gastroscope

channel shredding in a majority of reviewed scopes, according to a study presented at the 2022 annual meeting of the Association for Professionals in Infection Control and Epidemiology. However, the researchers did not identify any concerning microorganisms through routine culture of the scopes.
Borescopes—small devices equipped with a camera and light designed for the visual inspection of medical instruments—have been shown in multiple studies to find damage, abnormalities and retained materials in endoscopes, including those used in gastrointestinal endoscopy (Infect Control Hosp Epidemiol 2019;40[1]:40-46; Biomed Instrum Technol 2020;54[2]:146-152). But the most recent guidelines (ANSI/AAMI ST91:2021) on endoscope reprocessing do not include specific recommendations related to routine borescope examination or microbiological sampling.
‘ Structural damage can [protect] biofilms from high-level disinfection, and even though no microorganisms of concern were identified in microbial cultures, the need for routine culturing remains.’
—Mohamed Yassin, MD, PhD
University of Pittsburgh Medical Center
To examine the extent of damage in gastrointestinal, respiratory and urologic endoscopes used at the University of Pittsburgh Medical Center, Mohamed Yassin, MD, PhD, an associate professor of medicine and public health and the chief of the Division of Infectious Diseases, and his team conducted borescope examinations on 36 endoscopes (13 GI) and cultured 42 endoscopes
(18 GI); a small subset of 16 endoscopes underwent both borescope examination and microbial culture.








The GI endoscopes included gastroscopes, video duodenoscopes and colonoscopes. None of these scopes had discoloration, which was common in the urologic scopes, or dents, which were common in bronchoscopes. However, 10 GI scopes had retained fluid (Figure 1), nine showed channel shredding (Figure 2), five had filamentous debris (Figure 3), two had scratches and one had dried debris/substances detected on borescope examination. “We found moisture in almost every GI scope, except those that were sent for sterilization as part of reprocessing,” Dr. Yassin told Priority Report. “That is a cause for concern because of the possibility that [a scope] may harbor gram-negative bacteria.”
Of the GI endoscopes cultured, four were positive for microbial growth, all with less than 5 colonyforming units (CFU) and with only gram-positive colonies observed (either Bacillus or Staphylococcus species). In the subset of endoscopes cultured after borescope examination, the abnormalities did not appear to be related to microbial growth. In that
New research using borescope examination has found significant fluid retention and
group of 16 endoscopes, four (25%) had abnormalities or damage found during the borescope examinations, as well as microbial growth. “The type of abnormality/damage seen during the borescope examination did not correlate with positive microbial growth,” the authors noted.
Despite that finding, the extent and frequency of damage shown by the borescope examinations support the argument for routine borescope examination, Dr. Yassin said. “Structural damage can [protect] biofilms from high-level disinfection, and even though no microorganisms of concern were identified in microbial cultures, the need for routine culturing remains.”
Dr. Yassin acknowledged several limitations of the study. “We do not purchase our scopes; we lease them, so most of ours are almost brandnew,” he said, “and although we are an academic health center, we do not have any GI fellows, so all of our endoscopies are done by expert GI endoscopists. In addition, we do not do that many complicated procedures. We have one faculty member doing ERCP [endoscopic retrograde cholangiopancreatography], while the rest is mostly bread-and-butter GI work. Lastly, we have an excellent setup in our GI endoscopy suite, with the most up-to-date equipment and highly trained sterile processing technicians.”
Dr. Yassin’s workplace conducts borescope examinations of all of its GI endoscopes, with ERCP/ endoscopic ultrasound endoscopes examined three times per year and all other endoscopes twice annually. “We set up this schedule based on what we thought was best for us,” Dr. Yassin said. “If it were feasible to do it more frequently, I think that would be a good idea, but we had to start somewhere.”
Monique Barakat, MD, an assistant professor of pediatrics (gastroenterology) and medicine (gastroenterology and hepatology) at Stanford University and the associate director of pediatric endoscopy at the Lucile Salter Packard Children’s Hospital, praised the utility of the study. “It
illustrates that every center has its own different level of damage within the working channel, and it’s helpful to know that their cultures were negative,” she said. “We need much more research on borescopes. As this study illustrates, it’s hard to answer that million-dollar question of the correlation between working channel damage and microbial contamination. You can certainly say borescope examination is beneficial, but it requires more study to say whether it is truly necessary and, if so, what the frequency should be.”
She noted that “it takes a lot of manpower to inspect a scope like this, so it’s challenging to recommend that every center do so without additional data.”
An ongoing study by Dr. Barakat’s team (see page 10), involving prospective sequential borescope evaluation of accumulated endoscope working channel damage over the first three years of use, aims to help answer some of those questions.




—Gina Shaw
Drs. Barakat and Yassin reported no relevant financial disclosures.
Figure 3. GI scope with filamentous debris. Figure 2. Channel shredding inside a GI scope.
Aerosol generation during endoscopy procedures varies, with particularly increased generation of particles observed during certain parts of some upper GI procedures, according to investigators at the University of Nottingham, in England.
The team evaluated aerosol and droplet production generated during peroral gastroscopy (n=36), transnasal endoscopy (n=11) and lower gastrointestinal endoscopy (n=48) ( Gastrointest Endosc 2022 Jun 22. doi:10.1016/ j.gie.2022.05.018). Using particle counters, they measured the number of background particles in the endoscopy suite before and after the procedures, and subtracted the pre-procedure particle amount to identify the number of aerosols and droplets generated during procedures.
Per-oral gastroscopy produced 1.96 times the level of background particles (P<0.001), and transnasal endoscopy produced twice the level of background particles (P<0.001). Lower GI endoscopy produced 2.4 times the number of particles generated by per-oral gastroscopy (P<0.001). Particle counts during specific parts of the procedures ranged from 150 times the background particle level during per-oral gastroscopy throat spray ( P<0.001) to 7.7 times during lower GI endoscopy rectal insufflation/retroflexion (P<0.001).
This study underscores that PPE is critical to protect healthcare workers during the COVID-19 pandemic, especially given that new virus variants arise intermittently.
“The number of aerosols generated during endoscopic procedures became a more significant concern during the COVID-19 pandemic because SARS-CoV-2 spreads through the air and can be transferred from a patient to their healthcare providers,” noted Prateek Sharma, MD, a professor of medicine at the University of Kansas School of Medicine, in Kansas City, commenting on the study “We do not know the amount of aerosol generation necessary to cause a provider to become infected with COVID-19. However, this study from the United Kingdom showed significant droplet dispersal during procedures involving the mouth, nose and rectum, pointing to the need to make highquality personal protective equipment always available.”
—Marcus A. Banks


can sustain significant damage to their working channels over the course of their lives, including shredding, scratches, dents and divots, discoloration, and retained moisture. While these types of damage may not be entirely normal, it is not clear how much they predispose a scope to developing biofilm and/or microbial contamination.

It’s a question many in the gastrointestinal endoscopy field have been trying to answer.
During Digestive Disease Week 2022, Monique Barakat, MD, an assistant professor of pediatrics (gastroenterology) and medicine (gastroenterology and hepatology) at Stanford University, and the associate director of pediatric endoscopy at the Lucile Salter Packard Children’s Hospital, presented data from an ongoing study using brand-new endoscopes to assess the progress of working channel damage in the life of an endoscope.
The three-year longitudinal study involves borescope inspection of 26 new endoscope working channels (gastroscopes, colonoscopes, echoendoscopes and duodenoscopes) using the SteriView borescope (Steris) at the following intervals:
• immediately after purchase/before initial reprocessing;
• after one, five, 10 and 25 uses;
• after every subsequent 25 uses through 100 uses; and
• after every 50 uses thereafter.
“We have published previous manuscripts [Gastrointest Endosc 2018;88[4]:601-611.e1] in which we did snapshot evaluations of what our scopes look like on the inside, showing the damage that the scopes incur, and we wanted to have a better sense of how and when that damage accumulates,” Dr. Barakat told Priority Report. “Serendipitously, we happened to be buying a new fleet of scopes and decided to start with them.”
The investigators evaluated scope damage using the Stanford rating scale developed by Dr. Barakat, along with her colleague Subhas Banerjee, MD, a professor of medicine at Stanford University, and their research group. Scratch characteristics, scratch abundance and scratch adherent peel are rated on a 0-to-3 scale from none to severe, and then the scope is given an overall grade of 0 to 4 (no damage to severe).
Almost all of the endoscopes, and all scope types, had superficial scratches by 50 uses. By the scopes’ midlife (100-300 uses), there was an increased rate of damage. Severe endoscope working channel damage is over five times more likely in “geriatric” scopes, with over 400 uses. Leak test failures were observed more often after 500 uses.
Something that stood out was that scopes can show damage fairly early in their life cycle. “We examined each endoscope very closely before the first use and after the first reprocessing, and the striking thing was that some of those superficial scratches happen even during that first reprocessing,” Dr. Barakat said.
“This is something that we also found in our study using borescopes to assess endoscope damage,” said V. Raman Muthusamy, MD, a professor of clinical medicine at the David Geffen School of Medicine at University of California, Los Angeles (UCLA) and the director of endoscopy for the UCLA Health System. “The scopes we examined had all been acquired within the previous year, and there was some early damage. Damage seems to occur somewhat earlier than expected both in this study and in ours.”
‘ We examined each endoscope very closely before the first use and after the first reprocessing, and the striking thing was that some of those superficial scratches happen even during that first reprocessing.’
—Monique Barakat, MD Stanford UniversityThe researchers had hypothesized that certain kinds of endoscopes might incur more damage than others, but they observed that damage tends to occur at relatively similar rates, according to Dr. Barakat. “There were little blips of increased damage for certain scopes that you might hypothesize could trace back to a particular procedure or two, but in general, if one scope showed worse damage for a period of time, then the other scopes would tend to catch up.”
According to Dr. Muthusamy, there is still uncertainty about the significance of the findings of endoscope damage on borescope examination. “You start categorizing these things ... that we know are not entirely normal, such as moisture, see Scope Life Cycle, page 28
to build competency in infection control among ambulatory clinic staff should pay off in improved patient safety, according to a presentation at the 2022 annual meeting of the Association for Professionals in Infection Control and Epidemiology. These efforts are paramount because many clinics are still functioning without sterilization or high-level disinfection standards, experts told Priority Report.
Presenter Joy Williams, RN, a-IPC, the sole infection preventionist for Piedmont Healthcare, which has approximately 250 ambulatory clinics, physician offices and urgent care centers throughout Georgia, said that inspections of various facilities in 2020 and 2021 showed that staff in different Piedmont clinics handled high-level disinfection, endoscope reprocessing and sterilization with tabletop autoclaves differently. “There was no official training or competency program in place for any of these processes in the ambulatory clinics,” Ms. Williams said. This variability prompted the system to develop a standardized competency program.








Expertsfrom across the country have distilled multiple sets of guidelines into a new standard of care for endoscope safety. There were strong points of agreement in the various guidelines, the fruit of an almost decade-long effort to stop outbreaks of drug-resistant bacteria related to the scopes. But the different sets of endoscope reprocessing advice also proved to be highly varied.
There isn’t a gold standard for assessing adequate reprocessing, so it’s very challenging to measure how well a given employee, endoscopy unit or machine is doing.
“Because there are so many different guidelines, different institutions follow different ones,” said V. Raman Muthusamy, MD, the director of endoscopy for UCLA Health, in Los Angeles, and a co-author of the guidelines review. He and his co-authors emphasized that further research is critical to resolve points of uncertainty and disagreement to make endoscopy as safe as possible.
The authors analyzed guidelines from seven different medical authorities (Table). The different guidelines tended to agree on the broad
strokes of reprocessing, such as the need for training and verifying staff. But there was less agreement on the mechanisms to achieve those standards, such as how often and by what means to train staff and test their competency, Dr. Muthusamy said. He and his co-authors created two tables, one on the points of agreement and one on the discrepancies between guidelines (Gastrointest Endosc 2022;95[6]:1048-1059).
The first table covers 20 points of uniform consensus on everything from training, pre-cleaning and leak testing to rinsing, storing and evaluation. “No matter where you are or what you’re doing, you should do everything in [that] table,” Dr. Muthusamy advised endoscopy centers.
“In the last seven or eight years, a lot has been done to move the needle forward,” as the points of agreement in the uniform consensus table show, said Vivek Kaul, MD, the Segal-Watson Professor of Medicine in the Division of Gastroenterology and Hepatology at the University of Rochester Medical Center, in New York. “There is a litany of things everyone agrees on,” said Dr. Kaul, who agreed that the recommendations in the uniform consensus table are the “bare minimum” for any endoscopy unit to follow.
However, the second table reveals a lack of consensus, largely owing to a lack of data, on details such as the content of staff training, the optimal type of disinfectant solution, the quality of water used to rinse and how long a reprocessed scope can be stored.
“The list in [that second table] is quite worrisome because it’s quite long,” said Klaus Mergener, MD, PhD, an affiliate professor of medicine at the University of Washington School of Medicine, in Seattle. The lack of consensus in these details can make it especially difficult to train staff and ensure the manual cleaning process is properly followed, he said.
Manual cleaning is complex, sometimes taking longer than the procedure itself. But the only agreed-upon standard is that staff should follow the manufacturer’s guidelines, which can have over 100 steps, experts say. It’s nearly impossible for these staff to follow so many steps perfectly on a high number
Table.
Reprocessing Guidelines
American Society for Gastrointestinal Endoscopy
Association for the Advancement of Medical Instrumentation Association of periOperative Registered Nurses Association for Professionals in Infection Control and Epidemiology Society of Gastroenterology Nurses and Associates Healthcare Infection Control Practices Advisory Committee
European Society of Gastrointestinal Endoscopy
of scopes each day, Dr. Mergener said, especially when they feel rushed, as surveys suggest. Beyond that, staff in these positions see limited training, high turnover and sometimes low pay, he said.
“We would like to see simplicity in cleaning the device,” Dr. Muthusamy said. “No question it’s a tough job for these folks, … and lots of studies showing [staff] not doing all the steps exactly right is a real issue.”
The FDA ordered manufacturers of reusable duodenoscopes to conduct post-market surveillance, and the results released earlier this year were worse than expected (Use duodenoscopes with innovative designs to enhance safety: FDA Safety Communication; April 5, 2022.). When manufacturers pulled samples from high-performing endoscopy centers, as much as 6.6%—more than one in 20—were positive for a high-concern organism. That’s proof that reprocessing duodenoscopes is fundamentally challenging, Dr. Muthusamy said.
The review highlighted the kind of data that are still needed. Dr. Muthusamy said the field especially needs a standard for what makes a reusable scope clean. “How do we prove clean is clean? What is a benchmark for cleaning verification?” he said. There isn’t a gold standard for assessing adequate reprocessing, so it’s very challenging to measure how well a given employee, endoscopy unit or machine is doing.
“Stakeholders need to come to an agreement on what are the minimum criteria to assess if a unit is following the best guidelines,” Dr. Kaul agreed. This research will become more important as


Astep-by-step workflow for endoscope precleaning can be applied consistently for endoscopes in different outpatient clinics, saving time and improving patient and staff safety, according to a process improvement initiative presented at the 2022 annual meeting of the Association for Professionals in Infection Control and Epidemiology.
Precleaning kits, strategic placement of hand sanitizer and rehearsing workflows in mock clinical settings decreased the amount of time required to preclean an endoscope in an outpatient sigmoidoscopy clinic by half—from almost nine minutes before the project to less than five minutes.
“This process can save time while also creating a safer work environment for both patients and staff,” said lead researcher Michell Reyes, MT, CIC, FAPIC, an infection control manager at Memorial Sloan Kettering Cancer Center (MSKCC), in New York City.
At his institution, the final workflow efficiently interlinked tasks to minimize crosscontamination. He said this type of organized, safe and efficient precleaning workflow can be easily adapted to other specialty settings.
According to Mr. Reyes, he and his team wanted to design a better workflow that would make both staff and patients feel safe, while also following regulatory recommendations.
Before the initiative, he said, procedures were performed inconsistently. Staff did not follow a clean-to-dirty workflow, which resulted in contamination of clean supplies and clean areas while increasing the risk for staff and patient exposures to potentially infectious materials.
Mr. Reyes told Priority Report that he and his co-investigators set out to design a standardized, directional workflow to improve efficiency, safety and compliance with standards of care (Figures 1 and 2). They assembled a multidisciplinary team with nurses, patient care technicians, as well as support services and infection prevention staff.
Assembling a team made up of the front-line staff who are responsible for precleaning in outpatient clinics was important, he said, emphasizing the role of technicians and their invaluable contribution to the process improvement project. The technicians were able to contribute significantly to articulating barriers and suggesting realistic workflow strategies. In addition, Mr. Reyes and his co-investigators emphasized that the involvement of facility and departmental leadership also was integral to developing a solid workflow and addressing potential barriers, such as location of supplies and counter space.
“To implement a new process, we need to include the people actually doing the work on developing workflows,” Mr. Reyes said. “These workflows will fit in any clinical practices, private doctors’ offices or health centers where endoscopic procedures are done.”
Figure 1. Sequential tasks in workflow.Through regular progress meetings and observations held over a six-month period, the team addressed obstacles, including crosscontamination and front-line staff concerns about exposure to infectious materials due to perforated scope containers that can leak. They created detailed workflow maps outlining startto-finish precleaning procedures that would reduce cross-contamination while keeping staff members protected.
One important obstacle identified was inconvenient location of supplies and limited counter space. But, according to Mr. Reyes, the workflow can still be implemented successfully in sites with these limitations. “This process can work if staff use portable trays or stands and organize the layout of the rooms,” he explained. “The most important factor is that staff can identify the clean area versus the dirty area.”
As part of the initiative, technicians rehearsed and performed the precleaning workflow in various mock clinical settings and examination room layouts to identify areas for improvement and refine any steps, when necessary. Before implementation, related workflow tasks were separated into four distinct areas:
• Setup: The nursing staff assisted in delineating and identifying which tasks should be done in predetermined clean and dirty areas.
• Precleaning: Barriers identified during realworld observation were noted and corrected during simulation.
• Packaging: Uniform non-perforated scope containers were purchased and distributed to the entire clinic.
• Transport: Staff felt safe taking the used scope in a closed, fluid-resistant container to the soiled utility room.
Together, the multidisciplinary team was able to identify key concepts that tend to be misunderstood by staff members performing precleaning— for example, directional flow and clean versus dirty equipment.
“As a result of this systematic and organized improved initiative,” Mr. Reyes said, “the time spent precleaning decreased substantially” and safety was improved.
2. Example of workflow in specific exam room layout.
Asked to comment on the project, Amiee Mingus, RN, BSN, the vice president of clinical operations at PE GI Solutions in Jamison, Pa., agreed, emphasizing that the steps for precleaning cannot be skipped because they are an essential part of reprocessing an endoscope.
“Patient safety and infection prevention and control depend on every step being performed in a timely manner. If any step of precleaning is skipped or delayed, it can lead to bioburden buildup in the scope,” she said. “If space for performing precleaning is lacking, I’d investigate the possibility of using a rolling cart or table that can be moved around to accommodate the other necessary equipment in the room, but it may take some brainstorming to figure out how to accomplish the task in limited space.”
In addition, identifying and using proper personal protective equipment and providing hand sanitizer will continue to prevent workplace exposures for staff performing precleaning, she said.
Another key for the MSKCC team was collaboration with infection prevention staff to facilitate discussions about safety concerns. According to the project team, staff safety improved due to these conversations because safety was ultimately recognized as a top priority from leadership to front-line employees.
—Meg Barbor, MPH
Ms. Mingus and Mr. Reyes reported no relevant financial disclosures.
Figure Cabinets Counter Sinkcontinued from page 12
To begin, Ms. Williams developed a complete device inventory for every location, as well as lists of staff members and the jobs they performed. Next, she worked with a consultant to develop competency training programs in sterilization and high-level disinfection of endoscopes and ultrasound probes.
The sterilization and ultrasound probe trainings include online modules, live webinars and videos, whereas the endoscope reprocessing training occurs in person and online. Ms. Williams contracted with an endoscope manufacturer to provide the in-person trainings. Every training program includes an assessment to demonstrate competency.
Sometimes training videos provided by the manufacturer missed important steps, Ms. Williams noted, or training materials included language that some people could not understand. Consequently, Ms. Williams implemented live webinars to answer learners’ questions, and made sure that any in-person trainings were offered more than once so busy clinic staff could attend them.
Competency training program development took place from November 2020 to December 2021, Ms. Williams reported. By March 2022, all ambulatory clinic staff involved in sterilization or high-level disinfection had completed the training.
This program wasn’t just a friendly and extensive educational effort. There were consequences if staff members did not fulfill the requirements. “Those who were unable to complete the competency by the deadline were unable to continue performing that skill,” Ms. Williams said, adding that all infection control staff must demonstrate competency annually.
Piedmont’s approach is one response to the long-standing challenge of preventing infectious outbreaks in ambulatory care settings, where processes and procedures vary widely.
Compared with a traditional hospital that has infection control programs designed to ensure uniform procedures, infection control practices at community clinics run the gamut,
said Fozia Steinkuller, MPH, CIC, an infection control practitioner with UT Physicians at UTHealth Houston, who trains ambulatory care staff in how to prevent infection. Ultimately, the physicians who oversee these clinics are just as accountable as their hospital counterparts and are expected to follow best practices for preventing outbreaks at their facilities.
‘ All facilities should be safe, no matter how far they are from a hospital.’
—Fozia Steinkuller, MPH, CIC UTHealth Houston
Ms. Steinkuller told Priority Report that she offers the kind of training that Piedmont provided with a manufacturer consultant within the UTHealth system. Ms. Steinkuller said she advises physicians to invest in rigorous competency training for high-level disinfection and sterilization for their staff, using a mix of online and in-person methods as Ms. Williams has done. Ultimately, many infection control concepts could be taught with online modules, Ms. Steinkuller said, whereas some practical skill demonstrations, such as how to reprocess an endoscope, must be done in person.
As a first step, Ms. Steinkuller suggested using the CDC “Guide to Infection Prevention for Outpatient Settings: Minimum Expectations for Safe Care” checklist. This assessment would reveal the biggest gaps in staff knowledge, enabling development of tailored online and in-person training. Significant commitment is required at first, Ms. Steinkuller noted, but after that, staff would demonstrate competency annually and only new staff members would undergo the entire training.
“It’s worth the effort,” Ms. Steinkuller said. “All facilities should be safe, no matter how far they are from a hospital.”
—Marcus A. Banks
The sources reported no relevant financial disclosures.



Following the manufacturer-recommended process for disinfection of scopes resulted in successful removal of carbapenem-resistant Enterobacteriaceae, negating the need for routine scope culturing, according to a preliminary review that analyzed one type of scope.




Advocate Lutheran General Hospital (ALGH) was one of many healthcare organizations worldwide that reported an outbreak of multidrugresistant infections linked to duodenoscopes used in endoscopic retrograde cholangiopancreatography (ERCP), specifically with CRE in 2013. In 2016, the institution transitioned to manual cleaning of each duodenoscope followed by automated endoscope reprocessing. The hospital used the TJF-Q180 scope from Olympus and the manufacturer’s OER-PRO reprocessing device.
Meghana Doniparthi, MD, a third-year GI fellow at ALGH, in Park Ridge, Ill., who presented the hospital’s data at the 2022 annual meeting of the American College of Gastroenterology, said that during the 2013 outbreak, the hospital reported CRE “as the primary organism that was linked in our cluster of patients that develop infections after ERCP.” Noting that the site was “part of the U.S. Senate investigation with the
CDC,” Dr. Doniparthi told Priority Report that officials visited the “site to investigate and try to figure out what the cause of these infections was.”
Since 2016, the reprocessing team has been following an institution-specific protocol based on guidelines from the FDA, American Society of Gastrointestinal Endoscopy and CDC and recommendations from the manufacturer, Olympus, which include one round of high-level disinfection. After disinfection, they would culture the scope channel or tip to check whether CRE had cleared with reprocessing and then temporarily quarantine the scope while the culture result was pending from the lab, according to Dr. Doniparthi.

Noting that such routine culture of duodenoscopes for CRE after reprocessing in non-outbreak settings results in excessive cost with undetermined benefit, she and her
co-investigators retrospectively reviewed culture reports of scopes used during patient cases at ALGH between January and December 2021 (abstract D0623). They included all scopes that had undergone the standardized reprocessing method and culture of channels for CRE. The research team also reviewed the costs associated with implementing scope quarantine after culture.
A total of 482 ERCPs were performed during the study period, and all scopes were cultured after reprocessing. The researchers reported that there were no positive culture results, and no scopes required additional processing. They found that the average time to receive the culture was 48 hours and the cost of each culture was $28—totaling $13,496 for the year.
The researchers concluded that following the manufacturer’s recommended process for disinfection of scopes was successful at eliminating CRE, the organism identified during the 2013 outbreak. They also noted that their data suggest that in a high-volume ERCP center, the cost of implementing a culture-and-quarantine policy may be prohibitive, and they support the discontinuation of routine culture after reprocessing in non-outbreak settings.
“We’ve actually now decided to stop culturing at our institution. We’re just doing the same highlevel disinfection with a manual cleaning automated scope preprocessor,” Dr. Doniparthi said.
They noted that they plan to conduct ongoing review of long-term data and cost-benefit analyses.
“I still believe that periodic sampling and culturing is a valuable quality assurance approach,” commented Michelle Alfa, MSc, PhD, FCCM, a certified clinical microbiologist and the CEO of AlfaMed Consulting, in Winnipeg, Canada. In an interview with Priority Report, Dr. Alfa raised concerns that since the researchers at ALGH used a protocol based on the previous recommendations, they may not be following the 2018 FDA, American Society for Microbiology (ASM), CDC’s Duodenoscope Surveillance Sampling & Culturing protocol step-by-step. She also cited a large, published clinical study in
which researchers that observed the presence of contamination even when optimal sample collection, culturing and quarantining was used (Infect Control Hosp Epidemiol 2022:1-9; Gastrointest Endosc 2020;91[6]:1328-1333).
‘ I still believe that periodic sampling and culturing is a valuable quality assurance approach.’
—Michelle Alfa, MSc, PhD, FCCM AlfaMed Consulting, Winnipeg, Canada
“I would be concerned that they may not have been detecting all organisms that may be present, and especially if they only focused on CRE organisms and didn’t look at the other high-concern organisms that are identified in the [FDA/ASM/ CDC] protocol,” Dr. Alfa said.
She also said the question of cost of culturing raised by the researchers was a moot point, noting that in an outbreak or if a patient is infected by a contaminated scope, it would cost the institution much more than the nearly $13,500 set aside for culturing.
Dr. Alfa suggested some strategies that could save clinicians time during the quarantining of scopes, one of which was to begin the endoscope sampling protocol later in the week so that by Monday morning, clinicians would have a clearer answer on whether or not it is safe to use a specific scope. “When you do that periodic culturing (e.g., monthly or quarterly),” she said, “doing it on a Thursday or Friday [is optimal] .... so that it wouldn’t actually require as long of a quarantine period that interferes with the clinical slate or the number of procedures.”
Dr. Alfa reported financial relationships with Healthmark, Karl Storz, Olympus and Steris. Dr. Doniparthi reported no relevant financial disclosures.








Infacilities with moderate to high rates of pathogen carriage, pointof-care testing for multidrug-resistant organisms may optimize resource use while minimizing the risk for between-patient pathogen transmission after endoscopic retrograde cholangiopancreatography, according to a new study presented at the 2022 annual meeting of the American College of Gastroenterology.
Preventing patient-to-patient transmission of infectious pathogens associated with reusable duodenoscopes is crucial, and device sterilization—commonly performed with ethylene oxide gas (ETO)—is the highest level of disinfection available for such scopes. However, ETO sterilization is not widely used for several reasons, including high cost, restrictions due to the environmental impact in some locales, the need for specialized facilities, and global shortages. Thus, facilities often use high-level disinfection and other methods to ensure their scopes are safe to use in patients.




To evaluate a systematic testing protocol to detect multidrug-resistant organism (MDRO) colonization among patients undergoing ERCP and determine the potential need for ETO sterilization, researchers at Mayo Clinic in Rochester, Minn., retrospectively analyzed data from patients treated with scopes processed using the health system’s testing and sterilization protocol. Under the protocol, scopes are processed through either a sterilization pathway involving washing plus ETO sterilization or a high-level disinfection pathway involving double washing and then MDRO testing. If the test result is positive, the scope undergoes sterilization. If it is negative, the scope is considered ready for reuse.
‘ This is an innovative approach to a problem that doesn’t have a one-size-fits-all solution.’
—Mandeep Sawhney, MD, MS, FASGE
Beth Israel Deaconess Medical Center, Boston
Jad AbiMansour, MD, along with coinvestigators including Bret T. Peterson, MD, in Mayo’s Division of Gastroenterology and Hepatology, looked at data from 557 patients who underwent MDRO testing via rectal swab at the time of ERCP at a tertiary care center and satellite community practices within the Mayo health system between January 2018 and May 2022 (abstract E0616). The polymerase chain reaction (PCR) test was performed for all patients at two community practices and after daily sterilization capacity was exceeded at the tertiary center (during a national ETO canister shortage in 2022) to assess for MDRO. Test targets included the enzymes oxacillin-hydrolyzing betalactamase, Klebsiella pneumoniae carbapenemase, New Delhi metallo-beta-lactamase and Verona metallo-beta-lactamase.
Testing yielded one positive (0.2%) and 554 (99.6%) negative results. Two tests were processed incorrectly, which prompted precautionary scope assignment to sterilization with ETO. All duodenoscopes used in patients with negative PCR tests were reprocessed with double washing and high-level disinfection. No patients in the study developed a healthcare-associated MDRO-related infection.
While noting that the results show the potential benefit of this approach, the researchers acknowledged that more studies are needed to evaluate the model’s performance in a wider patient population and to help determine costeffectiveness and environmental impact.
“I think this is an innovative approach to a problem that doesn’t have a one-size-fits-all solution,” commented Mandeep Sawhney, MD, MS, FASGE, an associate professor of medicine at Harvard Medical School and a practicing gastroenterologist at Beth Israel Deaconess Medical Center, in Boston. Beth Israel Deaconess uses “a rigorous culture protocol, where we culture a large proportion of our duodenoscopes regularly to assess for contamination after they have undergone high-level disinfection,” Dr. Sawhney said.
He noted that with the point-of-care model used in the study, the Mayo investigators found, “at least in their patient population, the number of patients who were colonized by drug-resistant organisms that have the potential to contaminate duodenoscopes to be very small. This meant that by using this approach, they had to rarely use sterilization techniques to reprocess their duodenoscopes. For the overwhelming majority of cases, they were able to safely use standard high-level disinfection,” Dr. Sawhney said.
He applauded the researchers for their study and noted that the large population size and real-world setting were important strengths. “Previous research has focused on improving duodenoscope design or reprocessing techniques to mitigate this problem. However, these researchers have validated a technique that may reduce the likelihood of duodenoscope contamination with drug-resistant organisms in the first place,” Dr. Sawhney told Priority Report
Noting that the investigators included data from both a tertiary care center and community practices and employed their technique “as part of routine clinical care, and not in a laboratory or part of a simulation study,” he said, “This is real-world data showing that such an approach is feasible.”
—Landon Gray Dr. Sawhney reported financial relationships
with Allurion and Immunovia.notedInastatementannouncingthenewguidance,AAMI thatit“has










fromsusofindustry,clinicians,andsterilizationprofessionals aroundtheworld.”Butaresponsefromsevenlead ininggastroenterologysocieties,allofwhichparticipated discussiontheAAMIEndoscopeReprocessingWorkingGroup’s





consensusintoquestion. scopes“ChangestoST91forflexibleandsemi-rigidendoimpractical,createobstaclestoimplementstandardsandoffer inappropriate,orconflictingguidance,”said
















Anautomated system for cleaning the channels of an endoscope substantially reduced the risk for post-processing positive cultures relative to manual cleaning, according to a randomized study.

“The automated system has great potential to replace manual channel brushing and lower the risk of endoscopy-associated infection,” according to Renduo Shang, MD, from the Department of Gastroenterology at Renmin Hospital of Wuhan University, in China.
The FDA and other regulatory agencies consider the channels of reusable endoscopes to be particularly challenging for sterilization. Several automated processors have been developed. Currently, automated endoscope reprocessors in the United States are considered to be class II devices that must be cleared by the FDA through a premarket 510(k) pathway, but even if cleared, they are still characterized by the FDA as being appropriate for supplemental use with manual cleaning.
In a single-center study, 409 endoscopes reprocessed over a two-month period were randomized to channel cleaning with an automated brushing system designed for a thorough and consistent elimination of biomaterial or to standard manual cleaning. The manual cleaning was performed according to the specifications of the endoscope manufacturer. The primary end point was positive cultures after disinfection and drying.
The lower positive culture rate in the 204 scopes that underwent automated cleaning of the channels relative to the 205 scopes that underwent manual cleaning (15.2% vs. 23.4%) translated into a 35% reduction in relative positive culture risk (relative risk, 0.649; P=0.035).
The findings supported the hypothesis that automated cleaning is more thorough, according to Dr. Shang. He suggested that the difference in the real-world setting, where manual cleaning might be performed less rigorously relative to that within a clinical trial, might be even greater.
Manual channel brushing is often suboptimal “due to the pressure of endoscope turnover, lack of reprocessing technicians and weak supervision,” noted Dr. Shang, who presented the data at the 2022 United European Gastroenterology Week (abstract P1044).
A series of case reports linking reprocessed endoscopes to infection has led the FDA to tighten the way in which manufacturers define
and validate instructions for reprocessing. The regulatory agency also has encouraged manufacturers of endoscopes to make design changes that will facilitate elimination of the bioburden during reprocessing. The goal is a 99.99% reduction of resistant microbes.
‘ Endoscopic reprocessing is a complex job, and those who do it are under pressure to work quickly. ... So, automated cleaning is very conceptually appealing.’
Positive cultures and, therefore, risk for infection with endoscope reuse have not been fully resolved, but the system proposed by Dr. Shang is designed for meticulous channel brushing, “providing a new idea for the optimization of reprocessing protocols.”
The premise of automated cleaning makes sense, according to Venkataraman R. Muthusamy, MD, the director of endoscopy at UCLA Health, in Los Angeles, and co-author of the recent American Society for Gastrointestinal Endoscopy guidance for endoscope reprocessing (Gastrointest Endosc 2022;95[6]:1048-1059. e2). “Endoscopic reprocessing is a complex job, and those who do it are under pressure to work quickly. ... So, automated cleaning is very conceptually appealing,” Dr. Muthusamy told Priority Report. However, he pointed out that cleaning of the channels is just one step among many.
He also cautioned that automation of this one process is a start, but many other steps must be completed correctly to achieve an adequately reduced risk for positive cultures.
Dr. Muthusamy pointed to several methodological issues with this study. Of note, the 35% reduction in the rate of positive cultures still left 15% of the endoscopes cleaned by automated processing with positive cultures. This is a higher rate than typically reported, even for manual cleaning.
Cleaning Systems, page 28
continued from page 11
discoloration, divots, peeling and shredding, but what does this mean? Does it predispose to biofilm and colonization/infection? Also, is there a hierarchy of damage? We don’t want to over- or underreact to these findings,” he said.
Dr. Muthusamy also noted that it would be helpful to have a clear definition of what intervals these scopes should be checked by the manufacturer, and to get input from manufacturers to help clinicians better understand the criteria for when a device should be removed from use.
Ultimately, Dr. Barakat said she hopes the study can provide a general time line for when endoscopes typically should be either sent back to the manufacturer for repair and channel replacement or taken out of service altogether.
“Right now, there are no evidence-based guidelines for that, and at this point in our study, it’s still a little early to make any determinations,”
she said. “We would also like to get comparative data from another center.”
Researchers from another institution recently joined the study, and Dr. Barakat said she also hopes to review accumulated scope damage in a community practice setting, although that will not be done during this initial study.
“I hope we’ll have long enough follow-up within a year to analyze our findings retrospectively, with additional data from the other institution as well,” she said. “This is a very practical study that we believe will improve practice, patient care and our understanding of the significance of these endoscope working-channel findings.”
continued from page 27
The types of organisms cultured were not reported, so Dr. Muthusamy speculated that this rate of positive cultures might have been the result of environmental contamination and not relevant to reduction in biomass, but the culture rates make the study difficult to interpret.
In the published abstract, Dr. Shang indicated that channel brushing is so difficult that it is “often omitted in practice.” Dr. Muthusamy said he was surprised by this characterization. “This is worrisome, because failing to clean the channels is something that we hope never occurs, at least in this country,” Dr. Muthusamy said.
However, he agreed with the underlying concept that effective automated cleaning would solve the problem of human error if it could be
applied uniformly to all steps of the process.
“Effective endoscope reprocessing must be performed according to a complicated set of steps that differ for each type or brand of endoscope,” Dr. Muthusamy said. He characterized this work as repetitive and tedious, which lends itself to inadequate performance or omission of steps. One way to solve this problem is to automate the entire process, but Dr. Muthusamy noted that “we are not there yet.”
—Ted BosworthDr. Muthusamy reported financial relationships with Boston Scientific, Covidien, Ethicon Endo-Surgery, Interpace Diagnostics, Mauna Kea Technologies, Medtronic and Pentax. Dr. Shang reported no relevant financial disclosures.
—Gina Shaw Dr. Barakat reported no relevant disclosures. Dr. Muthusamy reported a financial relationship with Boston Scientific.




























Recent observational studies have suggested that duodenoscopes with disposable tips are associated with lower rates of bacterial contamination compared with fully reusable duodenoscopes. However, it is still unclear whether the reprocessing of these scopes with disposable tips can be shortened without increasing the risk for contamination.
“The FDA recommendations are to wash duodenoscopes with two manual washes and then two [high-level disinfection] (HLD) washes, which is pretty time-consuming,” investigator HannahSofia Brown, MD, a resident at Duke University, in Durham, N.C., told Priority Report. “I have sat through a lot of the washings, and it takes a couple [of] hours. So, we were [evaluating whether you can] decrease part of the protocol without causing infection rates to go up,” Dr. Brown said.
To evaluate rates of duodenoscope bacterial growth after abbreviated disinfection protocols, Dr. Brown and her co-investigators conducted a two-phase prospective observational study using ED34-i10T2 duodenoscopes with disposable tips (Pentax).
Presenting the data at the 2022 annual meeting of the American College of Gastroenterology (abstract D0438), Dr. Brown said
The reprocessing of duodenoscopes with disposable tips can be abbreviated without compromising effectiveness for disinfection, according to new research.
phase 1, which involved an abbreviated protocol of one manual wash before one cycle of HLD, was conducted from October 2021 to March 2022, and phase 2, in which test samples were obtained after two manual washes and one HLD, was conducted from April to May 2022.
The investigators sampled four sites on each duodenoscope: the elevator tab, the instrument channel distal opening, the composite scope tip and the instrument channel. They plated the samples on routine media for enteric pathogens, including Clostridioides difficile and Enterococcus species, and analyzed for vancomycin-resistant enterococci (VRE) via polymerase chain reaction. They used a one-sided Fisher’s test to identify differences in bacterial growth at each sample site during both phases. The team defined contamination as more than 100 colony-forming units (CFU) raw growth, more than 1 CFU of C. difficile or VRE observed in each site.
In the first phase, 46 duodenoscopes were sampled, resulting in 184 sample events. After testing, eight scopes had raw growth. Four grew VRE and none showed signs of C. difficile growth.
In the second phase, 25 scopes were sampled, resulting in 100 sample events. After testing, two duodenoscopes had raw growth. Four grew VRE and no C. difficile growth was observed.
The researchers found no significant differences between the groups in total bacterial or VRE presence across all the sample sites. In phase 2, the 95% confidence interval for the rate of contamination after two manual washes was 0.1% to 20.4% for the instrument channel distal opening and the composite scope tip, respectively. They noted that this was higher than the rates of contamination in phase 1: instrument channel distal opening, 0% to 7.7% and composite scope tip, 0.1% to 11.5%.
Dr. Brown said if disinfection protocols could be changed safely and reduce the time required for reprocessing, that would allow more scopes to be “washed in the shortest amount of time.”
She and her co-investigators concluded that the data suggest that two manual washes may not be superior to one manual wash in achieving HLD in duodenoscopes with disposable tips, but they acknowledged that larger studies are needed to validate these findings.
“I wasn’t totally surprised by the research,” Jim Collins, BS, RN, CNOR, a registered nurse and an accreditation professional for the Digestive Disease & Surgical Institute at Cleveland Clinic in Ohio, said in an interview.
In 2015, when the FDA released supplemental measures for duodenoscope reprocessing to ensure patient safety, Cleveland Clinic worked to incorporate some of the additional reprocessing measures into practice, Mr. Collins said. “The measures that we’re using at the majority of the clinic facilities all depend on the equipment already on hand. Some facilities are using two times, or repeat high-level disinfection after manual cleaning ... and other facilities are using liquid chemical sterilization—just due to the fact that they already had the equipment in place to do so,” he added.
‘ Endoscope [or duodenoscope] reprocessing isn’t a one-and-done competency for the year. It is a continuing process. We’re not preparing for completing our competencies for the year. It’s for preparing ourselves for the next patient.’
“I dislike the verbiage of ‘abbreviated.’ I prefer to say ‘modified,’ because when we use abbreviate, it sounds like you’re leaving something out,” Mr. Collins said. “I don’t want the public to think we’re taking shortcuts.”
Stressing the need for ongoing efforts in this area, he said, “Endoscope [or duodenoscope] reprocessing isn’t a one-and-done competency for the year. It is a continuing process. We’re not preparing for completing our competencies for the year. It’s for preparing ourselves for the next patient. So, staying on top of and monitoring the process through various quality systems that an institution wishes to establish ... is always encouraged to ensure that reprocessing is done right.”
—Landon Gray Dr. Brown reported no financial disclosures. Mr. Collins reported financial relationships with Boston Scientific and Steris.

from a recent study published in the American Journal
of Infection Control point to a new strategy for balancing the benefits and drawbacks of alcohol flushes for preventing microbial outgrowth during flexible endoscope reprocessing.

The study, conducted by researchers at Steris, followed previous research showing that alcohol flush led to increased endoscope channel drying time compared with water. The new findings, in addition to concerns about alcohol’s flammability, fixative properties and potential to be a tissue irritant, stand as notable drawbacks of the alcohol flush step in endoscope reprocessing. However, because of alcohol’s microbiocidal properties, the researchers sought to clarify the effectiveness of various concentrations of isopropyl alcohol (IPA) and, in the absence of IPA, various forced-air drying times in preventing Pseudomonas aeruginosa
outgrowth in endoscope channels (Am J Infect Prev doi:10.1016/j.ajic.2022.09.020).
‘
The study findings should … ‘wake people up and make them realize that if you’re using an [automated endoscope reprocessor], you really do need to be periodically testing the final rinse water to determine if it is contaminated, and then correct that problem.’
 —Michelle Alfa, PhD AlfaMed Consulting, Winnipeg, Canada
—Michelle Alfa, PhD AlfaMed Consulting, Winnipeg, Canada
The researchers, led by Michelle Nerandzic, BS, from Steris’ research and development team, used experimental endoscope air/water channels inoculated with P. aeruginosa to simulate contamination in the final rinse step of reprocessing. They allowed the inoculum to incubate for 30 minutes in the endoscope tubes, then drained the inoculum and allowed an additional hour of incubation. Next, they flushed the channels with various concentrations of IPA (70%, 50%, 30%) or a diluent, or dried them with forced air (until <10 mcL of liquid remained, until 0 mcL remained, or for three times the duration required to achieve 0 mcL [extended drying]), or left them untreated.
After 48 hours of storage in an endoscope cabinet, approximately 5.5 to 7.5 log10 colonyforming units (CFU) of P. aeruginosa were recovered in the untreated channels and approximately 4 log10 CFU were recovered in the channels
flushed with sterile diluent. Among the channels flushed with 70%, 50% or 30% IPA, no P. aeruginosa was recovered after 48 hours of cabinet storage.
To determine whether the antimicrobial effect seen in these alcohol-flushed channels was due to residual alcohol, some channels flushed with 70% IPA were dried using forced air. After 48 hours, no P. aeruginosa was recovered, indicating the prevention of P. aeruginosa outgrowth was not due to the residual alcohol.
Among the channels treated with compressed air only, those treated until 0 mcL of liquid remained had approximately 0.6 log10 CFU of P. aeruginosa recovered after 48 hours; there was no further reduction in the level of P. aeruginosa recovered in the channels treated with extended drying. Channels that were only dried until less than 10 mcL of liquid remained had no significant reduction in P. aeruginosa recovery after 48 hours relative to the untreated channels.
To evaluate how the IPA concentration influenced drying time, the researchers performed either final water rinse or alcohol flush at 70%, 50% or 30% IPA concentrations, followed by drying with forced air, using the suction/instrument channel to allow for the best visualization.
The mean time required to dry the suction/ instrument channel decreased as IPA concentration decreased (27.3 minutes for 70%, 18.9 minutes for 50%, 13.7minutes for 30%, and 8.6 minutes for water). The drying time was not significantly longer after the 30% IPA flush than after the water rinse.
Given that cases of rinse water contamination persist, the authors stressed that it is important to “retain the alcohol flush step in [high-level disinfection] procedures under conditions where effective drying cannot be verified.” They noted that their findings indicate, however, that “the working concentration of alcohol could be reevaluated for several reasons,” including their evidence that post-final rinse “alcohol flush … at reduced alcohol concentrations, may be effective for preventing contamination of endoscope channels and outgrowth of organisms during storage,” and that lowering the concentration of alcohol results in greater “drying efficiency.”
However, Cori Ofstead, MSPH, the president and CEO of Ofstead & Associates, who was not involved in the study, was unconvinced of alcohol’s utility, telling Priority Report that “the downsides of alcohol are concerning—it can make residual soil stick to the scope, it does not facilitate drying, and there are costs and occupational risks associated with its use.”

‘
The downsides of alcohol are concerning—it can make residual soil stick to the scope, it does not facilitate drying, and there are costs and occupational risks associated with its use.’
—Cori Ofstead, MSPH Ofstead & Associates, St. Paul, Minn.For Ms. Ofstead, the more salient takeaway from the study is that it “provides strong evidence that alcohol actually impedes the drying process for narrow lumens,” which she said is in line with previous research by her team and others. “The preponderance of evidence suggests that alcohol does not work as hoped by those who developed the [instructions for use] and guidelines.” In a 2018 study, Ms. Ofstead and her co-investigators “found microbes in more than 80% of scopes in two hospitals that flushed the channels with alcohol but had not used sufficient forced air to dry them [Am J Infect Control 2018;46[6]:689-696], and numerous other studies have found high rates of residual bioburden in spite of alcohol flushing post-HLD.“
Stressing the need for more studies, Ms. Ofstead noted that “the lab results are intriguing, but more research is needed to determine whether there’s a beneficial impact of reduced concentrations of alcohol on bioburden in real-world contexts where the endoscopes are also commonly damaged and dirty.”
Michelle Alfa, PhD, the president of AlfaMed Consulting in Winnipeg, Canada also noted potential limitations of being able to extend the Nerandzic et al findings to clinical practice, telling Priority Report, “they showed that 30% IPA resulted in no detectable organisms being present. But what they didn’t address is at 30%, are
continued from page 15
more new devices are introduced. Automated cleaning equipment and sterilizable scopes are under development, and disposable caps, disposable elevators and single-use scopes are already available and effective.
We would like to see simplicity in cleaning the device. No question it’s a tough job for these folks, … and lots of studies showing [staff] not doing all the steps exactly right is a real issue.’
‘
—V. Raman Muthusamy, MD UCLA Health, Los AngelesTo understand which devices and approaches best eliminate biofilm (and contamination) while allowing us to do our work at the same level of efficiency, Dr. Kaul said, we first need a measure of success.
The FDA recommends the use of new, innovative scope designs to reduce infection. However, all the experts agreed that it will take a variety of designs. Single-use scopes, for instance, are
attractive for their low risk for infection, but their high cost and waste are major drawbacks. And, they’re not practical for every single one of the 15 million colonoscopies done each year in the United States, Dr. Mergener said. So, a variety of duodenoscope designs and effective scope reprocessing will continue to be critical.
In the future, safer endoscopy will likely be achieved by a combination of device redesigns, simplified guidelines and clearer evaluation metrics, Dr. Muthusamy said. “Right now, we don’t have clear data to say one strategy is superior to another, but by highlighting those areas of disagreement, hopefully we can foster research to answer those questions.”
Dr. Kaul reported financial relationships with Ambu, CDX, Cook and Steris. Dr. Mergener reported financial relationships with Boston Scientific, Fujifilm, GI View, Kate Farms, Pentax and Sebela. Dr. Muthusamy reported financial relationships with Boston Scientific, Capsovision, EndoGastric Solutions, Medtronic and Motus GI. Drs. Kaul and Mergener are members of the Gastroenterology & Endoscopy News editorial board.
continued from page 33
they really killing the Pseudomonas that’s there? Or are they simply putting it into the viable but not culturable state, and, in actuality, those organisms, over time, may become culturable, and it could lead to biofilm formation?”
With the jury still out on the utility of alcohol flushes, Ms. Ofstead recommended that endoscopy practices use a drying indicator or boroscope to “evaluate the effectiveness of whatever drying method you’re using to determine whether it works with the scopes in your inventory and make adjustments after you have the data.”
Dr. Alfa also emphasized the importance of evaluation, but her focus was on the final rinse water. “I’m not negative about this publication at all…I do think that for clinics, this is useful information to emphasize the importance of how you need to thoroughly dry scopes after they’ve been fully reprocessed and especially during storage.” However, to her, the priority “should
be on making sure all the steps [of reprocessing] are working properly, not trying to remediate contaminated final rinse water.” While she acknowledged that “contaminated final rinse water is a reality,” she said she believes the impact of the study findings should be to “wake people up and make them realize that if you’re using an [automated endoscope reprocessor], you really do need to be periodically testing the final rinse water to determine if it is contaminated, and then correct that problem.” She said not doing so, and instead relying on low concentration alcohol to rectify contamination by rinse water is “not a good solution.”
—Natasha AlbanezeDr. Alfa reported financial relationships with Healthmark, Karl Storz, NanoSonics, Olympus and Steris.
Ms. Ofstead reported financial relationships with 3M, Ambu, ASP, Boston Scientific, Healthmark, Pentax and Steris/Cantel/Medivators.





























