April 2017
mdmonthly.com
26 CAN DIABETES BE “CURED”? Dr. Subhash Reddy on how bariatric surgery can resolve Diabetes
30 BENEFITS OF
TELEHEALTH
Dr. Kasi Howard explains how Telehealth is helping Mental Health Patients receive better service
38 THE CREATIVITY OF COSMETIC SURGERY Dr. Constance Barone enjoys being on the cutting edge
56
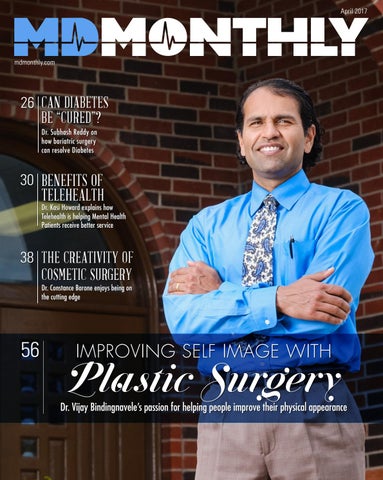
IMPROVING SELF IMAGE WITH
Plastic Surgery
Dr. Vijay Bindingnavele’s passion for helping people improve their physical appearance
BOERNE, TEXAS
NOW OPEN
Lounge on the broad, breezy wraparound porch, cocktail in hand. Step into a lovingly restored 19th century dining room to savor contemporary interpretations of Southern heritage foods and classic American dishes. Sit down to a familiar, casual, satisfying menu influenced by seasonal bounty from “As a kid growing up in Jourdanton, I watched my Mother and Grandma make everything from scratch every day. My Father and Grandfather were the Kings of Barbeque. I cooked some, too, but I did a lot more watching, tasting, and learning.”
area farms and the affinity of beef and mesquite smoke that is the soul of the Hill Country.
CHEF MARK BOHANAN
KENDALL INN
128 WEST BLANCO ROAD BOERNE TX 78006
t el 830.572.5000
w e b PEGGYSONTHEGREEN.COM
Hospice is a journey and we’re here to hold your hand every step of the way.
Alice | Austin | Bandera | Boerne Corpus Christi | Hondo | San Antonio
River City Hospice has earned The Joint Commission’s Gold Seal of Approval
compassionate Wecareprovide for our patients and
those who love them most. Our experienced team of professionals are here to support you during the challenges that come with a terminal illness.
Because Every Moment Counts rivercityhospice.com | 1.877.537.4837
Specializing In: •
Non-Surgical Intervention
•
Artificial Disc
•
Minimally Invasive Surgery
•
Degenerative Disc Disease
•
Sacroiliac Joint Fusion
•
Spinal Stenosis
• •
Cervical and Lumbar Fusion • • Spinal Decompressions
•
Robotic Surgery
Anthony Owusu M.D. Orthopedic Spine Surgeon
Sciatica Back and Neck Pain
13409 NW Military Hwy | San Antonio, TX 78231 NextGenOSI.com | 210.763.7149
PRACTICAL APPROACH SERVICES
Pediatrics, Pediatric Dentistry & Pediatric Urgent Care
Pediatric Care You can find the best pediatrician San Antonio has to offer right here at Practical Approach. From day one, Practical Approach Pediatrics helps children lead healthy and happy lives through a comprehensive approach to healthcare. Pediatric Dentistry From the first tooth to wisdom teeth, the pediatric dentists at Practical Approach are committed to providing beautiful and healthy smiles. When should your child have their first trip to the dentist? We provide all general pediatric dentist services.
9480 Huebner Road, Suite 400 | San Antonio, TX 78240 210.697.3900 | practicalapproachpediatrics.com
Pediatric Urgent Care San Antonio’s only Pediatric Medical and Pediatric Dental Urgent Care! Our practitioners at Practical Approach are fully trained to handle pediatric emergencies. Your child’s safety is very important to us and we take great pride in ensuring the quality of our pediatric emergency services!
Dr. Constance Barone is Honered to be Selected as
TOP DOCTOR IN AMERICA by Castle Connolly
Dr. Barone Services •
Abdominoplasty
•
Liposuction
•
Brachioplasty
•
Quciklift
•
Breast Augmentation
•
Quicklift Facelift
•
Mastopexy
•
Face Lift
•
Thigh Lift
•
Neck Lift
•
Blepharoplasty
•
Chin Implant
•
Brow Lift
•
Breast Reduction
•
Buttock Lift
•
Fat Injections
•
Gynecomastia
•
Otoplasty
•
Hair Graft
•
Rhinoplasty
•
Hair Transplantation
•
Thermi Tight
(SMARTGRAFT)
•
Thermi Rase
•
Lip Augmentation
Spa Services • • • • • •
Fillers Acne Laser Therapy BBL Chemical Peel Laser Hair Removal Micro Laser Peel
• • • • • •
Profractional Skin Tyte Thermi Smooth Micro Penning Nova Threads Microdermabrasion
9502 Huebner Rd, Bldg 2, Unit 202 | San Antonio, TX 78240 210.614.0400 | BaronePlasticSurgery.com
Dr. Constance M. Barone
PLASTIC SURGERY
Back to Normal S p i n e A s s o c i at e s
Comprehensive Spine Center Adult & Pediatric Orthopaedic Spine Specialists Spine Associates’ Comprehensive Spine Center creates a direct link between your primary care provider and the management of your spine injuries. Our Comprehensive Spine Center provides a full scope of spinal services including the evaluation, treatment of the cervical, thoracic and lumbar spine by a nationally recognized orthopedic spine specialist. Working together with referring physicians, our team ensures that each patient receives a personalized treatment plan specific to his or her circumstance and lifestyle. Spine Associates is equipped with the most state-of-the-art imaging and diagnostic technology which enables our spine specialists to effectively and accurately
THE SMARTER CHOICE FOR SPINE CARE Comprehensive Spine Care that follows you from diagnosis to treatment to recovery - and even follows you home AREAS OF EXPERTISE - Robotic Assisted Spine Surgery - Minimally Invasive Spine Surgery - Adult & Pediatric Scoliosis Correction - Reconstructive Spine Surgery - Physical Therapy - Interventional Pain Management
diagnose and treat you. We also offer a full range of leading-
STOP LIVING WITH PAIN
edge, non-surgical and surgical treatment options including
Call or email today and begin your personal treatment plan 800-9-SPINAL (800-977-4625) or info@myspineassociates.com
robotic assisted spine surgery and minimally invasive treatments to get you back to normal.
SPINE ASSOCIATES LOCATIONS: 9301 Southwest Freeway, Suite 600 | Houston, TX 77074 | 713-383-7100 3820 Pointe Parkway | Beaumont, TX 77706 | 409.767.8221 myspineassociates.com
April 2017 Production Media Digital Source Designer Meghan Goettl Project Manager Miranda Paredes Contributing Writers Rudy Arispe Edmond Ortiz Northwest Vista College Bailey Starnes Cynthia Huchingson Michelle Bishop Dr. Constance Barone Subhash Reddy Tim Taylor Dr. Kasi Howard Dr. Melissa Macias Dr. Jimenez-Shahed Francisco Arredondo Janet Montagne
Contributing Photographers
38
The Creativity of Cosmetic Surgery Dr. Constance Barone enjoys being on the cutting edge
56
26
Can Diabetes Be “Cured”?
Dr. Subhash Reddy on how bariatric surgery can resolve Diabetes
Improving Self Image with 26 Benefits of Telehealth Plastic Surgery Dr. Vijay Bindingnavele’s passion for helping people improve their physical appearance
8
MD Monthly
APRIL - 2017
Dr. Kasi Howard explains how Telehealth is helping Mental Health Patients receive better service.
Marc Arevalo Paul Marshall Jason Roberts FOR ADVERTISING INFORMATION, PLEASE CALL 210.373.2599 OR EMAIL HELLO@MDMONTHLY.COM. FOR EDITORIAL COMMENTS AND SUGGESTIONS, EMAIL EDITOR@MDMONTHLY.COM.
MDMonthly.com 22211 IH-10 W. #1206 | San Antonio, TX 78257
Cover Photo Dr. Barone – Marc Arevalo Cover Photo Dr. Bindingnavele – Paul Marshall
Stop the Pain Visit Us At AmericanSinus.com or SouthTexasSinusInstitute.com
Honrubia Technique™ for Balloon Sinuplasty
Patient Comfort and Safety Come First
The Honrubia Technique™ for Balloon Sinuplasty is a revolutionary, minimally invasive procedure for treating chronic sinusitis. The primary symptoms of chronic sinusitis are headaches, trouble sleeping, snoring, fatigue, facial pressure, ear discomfort, and post nasal drip. The Honrubia Technique™ addresses many of the primary symptoms of chronic sinusitis while maximizing the comfort and safety of the patient. It is recommended by our team of board certified ENT Physicians. This technique involves less pain than a traditional sinus surgery and therefore contributes to a quicker recovery. The Honrubia Technique™ for Balloon Sinuplasty is done under anesthesia. This ensures that patients have a more relaxing and positive experience than when the procedure is performed under a local anesthetic. It also allows us to address several other sinus related complaints. An anesthesia provider administers intravenous medications to keep patients lightly sedated and comfortable. Our American Sinus Institute team of specialists have performed thousands of procedures using the Honrubia Technique™ for Balloon Sinuplasty. Come see us at the American Sinus Institute. We Solve Sinus Problems.
Vincent F. Honrubia, M.D., F.A.C.S., Director
6363 De Zavala Road, Suite 200 San Antonio, TX 78249 (210) 225-5666 • (210) BALLOON 1801 Binz Street, Suite 400 Houston, TX 77004 (713) 225-5666 • (713) BALLOON
2821 2821Michaelangelo MichaelangeloDrive, Drive,Suite Suite201 201 Edinburg, Edinburg,TX TX78539 78539 (956) (956)661.8200 661.8200• (855) • (855)99SINUS 99SINUS
12
Healthy Living
Kinsanity: True Transformations College Exercise Class goes above and beyond lectures.
34
14 In The Community
Walk MS Expected to Surpass $1 Billion This Year Thousands will help achieve Milestone at Walk MS: San Antonio on March 11.
18
In The Community Honoring Dr. Ian Thompson During Spring Fundraiser for Contributions to Cancer Therapy & Research Center
! ! ! ! ! "
Informed Patient
Deep Brain Stimulations for Parkinson’s Disease Appropriate patient selection, pre-operative assessments, and careful patient counseling are all essential components to successful DBS in PD.
42
• • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • •
Feature/Profile
! myemma.com/nside
! !
Dr. Melissa Macias
• • • • • • • • • •
SA Cancer Council
!
Neurosurgeon, finds her way back home at a new practice.
20
46
Medical Business
Style & Substance
Financial Finger Pointing
Style by the Green
MD Anderson Asks: Is it an oversight of Epic Proportion?
24
Managing Partner at River City Hospice ,Janet Montagne, models clothing from Neiman Marcus.
54
Informed Patient
Taking the Plastic out of Surgery Emerging Trends in Aesthetic Medicine
Feature/Profile
Dr. Wassim Choucair Adds More Heart to Life A top heart doctor and cardiac electrophysiologist opens The Heart & Rhythm Institute of South Texas
60
Research & Innovation
INVOCell Break through technology for an affordable Fertility Solution
10
MD Monthly
APRIL - 2017
Act FAST – Be Stroke Smart! Learn how to spot a stroke F.A.S.T.
ST R RT OK IFI E E
CE
Rapid access to medical treatment can make the difference between a full recovery and permanent disability. Corpus Christi Rehabilitation Hospital encourages you to learn the warning signs of stroke.
D
F.A.S.T. is an easy way to identify the most common symptoms of a stroke:
F – Face drooping A – Arm weakness S – Speech difficulty T – Time to call 9-1-1
if you observe any of these symptoms LEARN THE WARNING SIGNS THAT CAN SAVE A LIFE. BE STROKE SMART!
CCRH.ERNESTHEALTH.COM
Follow Us
5726 Esplanade Drive • Corpus Christi, TX 78414 • ph: 361.906.3700
TRUE CONFIDENCE. TRUE YOU. Halcyon Med Spa & Wellness Center is now offering fast and easy treatments to contour the body and remove unwanted fat permanently. Show off this summer with a firmer, smoother, and more confident you!
BOOK YOUR APPOINTMENT TODAY
361.452.2637 MONDAY-FRIDAY 9-5 SATURDAY 10-2
HalcyonMedSpa.com 1752 Santa Fe | Corpus Christi, TX 78404
HEALTHY LIVING/SAN ANTONIO
COLLEGE EXERCISE CLASS GOES BEYOND LECTURES TO MAKE
TRUE TRANSFORMATIONS
K
Contributed by Northwest Vista College
insanity – A new fitness craze is taking over San Antonio – well just Northwest Vista College and the focus is to help students and their friends and families learn about nutrition to make body transformations. Over the last several years, Northwest Vista College instructor Leland Hammonds II has taken his
12
MD Monthly
Concepts of Physical Fitness to a whole new level from just lectures and exercising. In this class, students can see true transformations.
partner which not only keeps them accountable but results in others outside of the class seeing positive results in their own bodies.
In fact, over the last four semesters, over 600 pounds of body composition change has occurred, which includes gaining muscle or losing weight and fat. And it’s not just students in the class. His students have to eventually find a
Recently in a class where students learned the essentials of making a healthy smoothie, he stressed fad diets or crazy workouts aren’t the key to weight loss long term. His energetic lecture had the students engaged with him, wanting to learn more and having
APRIL - 2017
MDMONTHLY.COM
HEALTHY LIVING/SAN ANTONIO
“Not only are the students interacting in a very cool and sincere way, but they invite friends and family members that want to live a healthier life to follow along with the class in real time,” Leland adds. “We have some awesome success stories of friends, siblings, parents etc. who have lost tons of weight and they aren’t even in the class, they just follow along on social media.”
“aha” moments about what they thought about health. “The clearer something is, the easier it is to follow. Don’t count calories but be mindful of them and portion sizes. By Spring Break, everyone should have a list of the foods that you like and will help you reach your goals,” said Leland who has a master’s degree in Kinesiology from the University of Texas Permian Basin and has coached people on health and wellness for the last 20 years in his personal fitness business. Leland even trademarked the term “Kinsanity” Body Transformation program. Leland said the term Kinsanity means doing kinesiology the sane way. His simple approach for students and clients is one that is also supported by the Academy of Nutrition and Dietetics. Its theme for National
Nutrition Month in March is “Put Your Best Fork Forward,” which serves as a reminder that each one of us holds the tool to make healthier food choices. Leland also utilizes social media to engage students and help them to make healthier choices. All of his readings, videos and assignment links are given out via Twitter. Just following Leland at @ProfessorLeland can be addicting. There’s a ton of helpful tips, meal planning photos and success stories on his Twitter feed. Also on his Instagram account (lelandhammonds), there are more photos of former and present students taking tracking their fitness goals.
While many students in Leland’s class are hoping to earn an Association of Arts with a Concentration in Kinesiology from Northwest Vista College, a part of the Alamo Colleges District, they find they get much more from the class. One student said online, “I learned a lot more than I expected from an exercise class. Goal setting for one, finding your passion, finances … to name a few. I have finally learned how to lose weight, know what to eat and how to exercise.”
For instance, Mathew Sosa said on Twitter that “It doesn’t matter the amount of calories you take in it’s the type of nutrition you take in. Are you giving your body the right fuel?” And Ignacio, who follows Leland on Twitter, said he got his mom to do some of the Kinsanity workouts that Leland gives to his class that combines short bouts of cardio and strength training. 2017 - APRIL MD Monthly
13
IN THE COMMUNITY/SAN ANTONIO
WALK MS EXPECTED TO SURPASS
$1 BILLION THIS YEAR
Thousands Will Help Achieve Milestone at Walk MS: San Antonio on March 11 By Bailey Starnes
S
ince 1988, hundreds of thousands of people have taken part in Walk MS events across the country raising critical funds and awareness for the National Multiple Sclerosis Society. This year, the cumulative fundraising is expected to surpass $1 billion. “Walk MS is a joyous gathering with a wonderful ‘we’re in this together’ feeling,” said Cyndi Zagieboylo, President and CEO of the National MS Society. “Every participant, volunteer, donor, and sponsor is helping to drive us toward this exciting $1 billion milestone. Together, we are accelerating progress in making life-changing breakthroughs -- so that each person with MS can live her or his best life.” More than 3,000 people are expected to raise more than $325,000 at Walk MS: San Antonio on March 11 at Texas A&M University, San Antonio. Walk MS is an opportunity for people living with MS and those who care about them to connect, join together, and be inspired. In 2016 alone, nearly 14
MD Monthly
300,000 people at more than 500 locations across the country walked to create a world free of MS, raising more than $40 million. Each walk is fully-accessible, includes multiple distance options (including a one-mile route option), and outstanding volunteer support for participants throughout. WHEN: March 11, 2017 – Site opens at 8 a.m., walk begins at 9 a.m. WHERE: Texas A&M University, San Antonio - One University Way, San Antonio, TX 78224 PARTICIPATION/ VOLUNTEER REGISTRATION: Visit walkMS. org, call 855-372-1331, or email FundraisingSupport@nmss.org. WHY: Walk MS unites teams of families, friends, neighbors and co-workers to raise funds that drive groundbreaking MS research, provide life-changing services and guarantee a supportive community for those who need it most.
HASHTAGS: #walkMS and #WalkTogether About Multiple Sclerosis Multiple sclerosis is an unpredictable, often disabling disease of the central nervous system that disrupts the flow of information within the brain, and between the brain and body. Symptoms range from numbness and tingling to blindness and paralysis. The progress, severity and specific symptoms of MS in any one person cannot yet be predicted, but advances in research and treatment are leading to better understanding and moving us closer to a world free of MS. Most people with MS are diagnosed between the ages of 20 and 50, with at least two to three times more women than men being diagnosed with the disease. MS affects more than 2.3 million worldwide. For more information about multiple sclerosis and the National MS Society go to nationalMSsociety.org or call 800-344-4867.
APRIL - 2017
MDMONTHLY.COM
Melissa Y. Macias, MD, PhD Neurosurgery Dr. Macias treats a spectrum of adult degernative spine and brain pathologies and conditions: • Complex Degenerative Spine Disease, Disc Herniations, Spinal Stenosis, Acquired Adult Scoliosis • Infections • Tumors • Stroke • Trauma Through compassionate and individualized care, Dr. Macias uses minimally destructive techniques, as well as stem cell technologies in her procedures. She also offers treatment of chronic pain and compressive peripheral nerve disorders.
A Healthy Spinal Axis is fundamental to an active and healthy lifestyle. SouthTexasBrainAndSpineCenter.com Corpus Christi Location: 361.883.4323 Fax: 361.883.4324
IN THE COMMUNITY/SAN ANTONIO
MAKING AN IMPACT ON THE COMMUNITY:
WOMEN-POWERED PHILANTHROPY “IMPACTS” COUNTLESS LIVES THROUGH COLLECTIVE GIVING, GRANT MAKING Special to MD Monthly
E
leven years ago, Dr. Ingrid Skop, an OB/GYN, heard about Impact San Antonio through a friend, who encouraged her to join the women’s philanthropic organization that impacts the community through the strength of their collective generosity.
a relatively small donation makes a tremendous impact for a lot of nonprofits,” she said. “I also like the fact that you can be as involved as you want or participate on your own terms, especially for those who want to get involved but don’t have a lot of free time on their hands.”
Members, either individually or in groups up to four women, contribute $1,000 annually with 100 percent of donations pooled to create multiple $100,000 grants awarded to nonprofits in one of five focus areas: Arts & Culture, Education, Environment/Recreation/Preservation, Family, and Health & Wellness.
Impact San Antonio invites women of all backgrounds to attend its Spring Fling membership event from 6 p.m. to 8:30 p.m. Tuesday, April 11 at the San Antonio Garden Center, 310 N. New Braunfels Ave. The event is part of the organization’s Drive for Five membership recruitment campaign.
Today, Dr. Skop’s membership is as strong as ever. “I like the way
“Drive for Five is about having the membership strength to award five
16
MD Monthly
$100,000 grants this year,” President Beverley McClure said. During the Spring Fling event, District Court Judges Lisa Jarrett and Daphne Previti Austin, and Annette Rodriguez, CEO of The Children’s Shelter, will discuss issues facing families and the collaborative work between our judicial system and social services to improve experiences and outcomes for children and adolescents. Admission is $25 for members and $15 for guests. In October 2016, Impact San Antonio awarded $400,000 to four local nonprofits including Alpha Home, Family Service Association,
APRIL - 2017
MDMONTHLY.COM
IN THE COMMUNITY/SAN ANTONIO
Bexar County Partners for Youth and Providence Place. Family Service Association, for instance, was awarded $100,000 in the Family category. “Thanks to the support of IMPACT, Family Service’s Kidshare program will continue to keep children safe, strengthen family relationships and break the multigenerational cycles of abuse and violence in our community,” said Nancy L. Hard, president and CEO. Alpha Home, meanwhile, was awarded $100,000 in the Health & Wellness category. The agency is restoring an existing home which provides residential drug and alcohol rehab for women, 18 years and older. Women in the residential program will have an enhanced quality of life and, as a result, will remain in residential treatment for a longer period, increasing long-term success. “This funding means the children visiting will know their mommies are being helped in a place that feels like
Impact SA awarded $100,000 to Family Services Association in October 2016 during the organization’s Grant Award Night. (Photo by Roberta Barnes)
home,” said CEO Angela White. Dr. Skop added that her involvement with Impact San Antonio has helped educate her to the wonderful work that so many nonprofits do on behalf of their clients. And she’s glad she joined 11 years ago. “It’s definitely worth the while,”
she said. “If money is an obstacle in your decision to join, you can do a shared membership as a gateway into Impact SA. It opens women’s eyes to the good work that is going on in the community.” To date, Impact San Antonio has awarded nonprofit agencies more than $2.2 million thanks to the collective strength of women committed to impacting and enriching lives throughout the city and surrounding areas. In addition to the Spring Fling on April 11, Impact San Antonio will host its Last Call recruitment membership event on May 17 at The Veranda. Learn more at impactsanantonio.org or call (210) 617-3280.
Impact San Antonio will host its Spring Fling membership recruitment event on April 11 at the San Antonio Garden Center. (Photo by Roberta Barnes) 2017 - APRIL MD Monthly
17
IN THE COMMUNITY/SAN ANTONIO
SA CANCER COUNCIL (formerly CTRC Council)
TO HONOR DR. IAN THOMPSON
During Spring Fundraiser for Contributions to
CANCER THERAPY & RESEARCH CENTER Special to MD Monthly
T
he SA Cancer Council (formerly the CTRC Council) will honor Dr. Ian Thompson, past director of the UT Health’s Cancer Therapy & Research Center, and Carla Bergner, Volunteer of the Year, during the organization’s Spring Luncheon fundraiser from 11:30 a.m. to 1 p.m. Monday, April 10 at the Omni Hotel San Antonio, 9821 Colonnade Blvd. “Dr. Thompson is compassionate, a brilliant scientist, and all around great man. We are happy that we can recognize him for his seven years of leadership at the CTRC. Not only has Dr. Thompson been a great leader, he has been our council’s closest and dearest friend,” said Board President Beverly Koehn. Featured speaker is Ed Whitacre Jr., former chairman and CEO of General Motors and AT&T. He will discuss the critical impact of UT Health’s cancer center to the Alamo City during a Q-and-A format led by
18
MD Monthly
Robert Rivard, director of The Rivard Report. Tickets are $75 per person. Table sponsorships are also available. To purchase tickets or tables, visit www.ctrccouncil.org/spring-luncheon or call (210) 450-5571. All proceeds support cancer research and patient assistance at UT Health San Antonio. The SA Cancer Council supports UT Health San Antonio in the fight against cancer by providing financial support for both cancer research and patient assistance, as well as volunteer resources for cancer patient treatment, education and community outreach. Dr. Ian Thompson Dr. Thompson became the president, CHRISTUS Santa Rosa Hospital - Medical Center & vice president Market Oncology Service Line in January 2017. After growing up in Columbia, Missouri, Dr. Thompson received his undergraduate degree from West Point and his MD degree from Tulane University. Following a
residency in urology in San Antonio, he completed a fellowship in Urologic Oncology at Memorial Sloan Kettering Cancer Center. He returned to San Antonio first as a faculty urologist at Brooke Army Medical Center (BAMC), then as chief of urology, and completed his military career as chairman of the Department of Surgery at BAMC. He joined UT Health in 1998 while on active duty as chief of urology and then retired on Dec. 31, 1999, joining the university as a tenured professor of urology. After taking the Division of Urology to full departmental status and attaining the highest level of National Institutes of Health funding for a Department of Urology in the United States, he was appointed director of the UT Health cancer center in 2009. He successfully led the cancer center through the NCI grant review process to maintain its support as an NCIdesignated Cancer Center three years after his appointment.
APRIL - 2017
MDMONTHLY.COM
IN THE COMMUNITY/SAN ANTONIO
the food items with expiration dates, stocks the pantry shelves and packs food boxes for needy patients. She does all this at least once a month. To get the job done she has enlisted the assistance of her husband, neighbor and even her neighbor’s son, not to mention many dedicated SA Cancer Council members. Her commitment to helping cancer patients is amazing. Carla’s efforts make a huge difference in the lives of our patients and their families.
Dr. Thompson retired as a colonel from the U.S. Army. He served in Saudi Arabia and Iraq as a general surgeon in the 41st Combat Support Hospital in Saudi Arabia, Iraq, and Kuwait during Operation Desert Storm/Shield. He is the recipient of many military awards, including the Order of Military Medical Merit and the Legion of Merit. Dr. Thompson has practiced urologic oncology for more than 30 years with a special expertise in prostate cancer prevention, diagnosis, and treatment including surgical care of his patients.
better serve the needs of cancer patients. Carla’s and BJ’s initiative and tenacious advocacy led to the development of the first medicallybased Food Pantry in San Antonio.
Carla Bergner, Volunteer of the Year
Carla did not rest on her laurels. She wanted the pantry to succeed and knew that it would necessitate significant resources to sustain the service. This was no small feat. It required not only a considerable time commitment but organizational skills, managerial talent, physical strength and a large vehicle. Carla has kept the food pantry stocked for the past 3 plus years.
Carla first volunteered at the cancer center’s Information Desk, welcoming patients and helping them find the resources they needed. During this period, she discovered that many patients suffered from a lack of basic necessities, including food. She and Ms. B.J. Mamuzic reached out to the San Antonio Food Bank to explore the possibilities of developing a partnership to
She maintains the pantry’s inventory, communicates with staff about what needs to be ordered, organizes a team of volunteers to help with restocking the pantry, purchases the boxes to pack the food, drives to the San Antonio Food Bank to pick up the orders, loads and transports the food (some time in excess of 600 pounds), labels all
Sponsors of the Spring Luncheon are the Klesse Foundation, The Trust Company, Gurinsky’s Fine Jewelry, Jefferson Bank, Methodist Healthcare Ministries, Law Office of Laska A. Arnold PPLC, Frost Bank, Wortham Insurance & Risk Management, Amegy Bank, Chicago Title Company, Broadridge Financial Solutions, Masters Leadership Program, Mission Pharmacal Company, DOCUmation, Texas Capital Bank, UT Health SARadiology, UT Health SA-Office of the President and Virtuoso Builders.
2017 - APRIL MD Monthly
19
MEDICAL BUSINESS/AUSTIN
MD Anderson
FINANCIAL FINGER-POINTING
An Oversight of EPIC Proportion? By Cynthia Huchingson
A
disturbing chill reverberated through America’s healthcare system on May 12, 2016 as medical professionals read the shocking report in Becker’s Hospital Review: MD Anderson blames EHR costs for 56.5% drop in income. “It couldn’t be,” we shuddered. But one all-too-short quarter later, the same source confirmed our fears with an even more petrifying: MD Anderson points to Epic implementation for 77% drop in adjusted income. Epic is the well-known EHR (electronic health record) software platform MD Anderson Cancer Center transitioned to in March 2016. Although EHR implementations have systemically caused operational and financial stress across healthcare entities, MD Anderson’s quantified losses as attributed directly to their EHR catalyzed overwhelming fear. By January 5th, when every major national news outlet reported some variation of the headline: MD Anderson Cancer Center to cut 1000 jobs due to losses from EHR, doctors and administrators everywhere sat aghast wondering, “If MD Anderson can’t make it work, how can we?” So why did MD Anderson’s
20
MD Monthly
news launch the entire healthcare industry into cardiac arrest? One key factor was the defined and measured financial impact published in the headlines. Although most healthcare facilities can tell you they have experienced a high cost to acquire and “meaningfully use” an EHR system, many do not have the depth and breadth of accounting resources to distill an exact bottom line impact. They instead look for data from resource-backed places like MD Anderson to use as a benchmark from which their own outcomes can be reasonably predicted. If this were the new baseline, they would need life support. Further resounding the doomdoom-doom was the industry expectation that MD Anderson should, quite frankly, be able to do it better. They not only had the benefit of 476 staff members on their IT team during their planning phase in 2015, they also had access to multiple revenue streams outside of patient care. In fact, 19.2% of MD Anderson Cancer Center revenue in 2015 came from donations, grants, state funding, tuition and parking fees, investment income and dining revenue. To most
private practice physician groups and for-profit hospitals, this meant MD Anderson had access to a whopping “cushion” of $863,908,077 that they wouldn’t be afforded. So what exactly caused their tragedy? The news articles reported the following reasons: 1. The demand for a higher number of full time employees to support the new EHR system, which caused a significant increase in salaries and wages expense 2. Increased salaries of new staff required to support the effort 3. An increase in consulting fees associated with the EHR implementation But wait! This is where the story abruptly changes. I don’t doubt that the adjusted income figures MD Anderson reported are valid. But something gave me pause to ask: “Has anyone validated the assumptions connecting their putrid bottom line directly up to the “Epic” claims?” At that moment I knew I had two options – either pack up my bags as a healthcare consultant and move to a country where EHR’s weren’t
APRIL - 2017
MDMONTHLY.COM
MEDICAL BUSINESS/AUSTIN
about the kill the financial viability of every one of my clients, or do one of the things I love most - open my MacBook and do a little research and number-crunching. An Epic Oversight? Fascinatingly, when I looked at the data I couldn’t find an increase in the number of full time employees before, during, or after the March 2016 implementation. Nor did my much-loved, oft-used version of Excel calculate a higher cost for each new IT staff member. In fact, my calculation suggested just the opposite. And finally, when I extrapolated the consulting fee data to a full year both before and after implementation, the year-over-year increase in expense was less than the 2014 to 2015 increase between nonEHR years. I was beginning to think all the finger-pointing in the news may be been an epic oversight… Additional Staff The Texas Tribune has an incredible database of publicly reported information. Specifically, they have data on the positions, number of employees, and salaries within many government institutions. One of those institutions happens to be the MD Anderson Cancer Center. This means we can easily get verified data for MD Anderson by department. A quick download, sort and filter of the 585 departments at MD Anderson yield 8 associated with IT or the EHR. As of May 26th, 2016, there were 476 staff members employed within these 8 divisions, 57 of whom had been employed 1 year or less. The published news reports suggest that these 57 new hires were required as an increase over the “normal” number of staff in the IT department. This initially made sense, but then I started thinking, “Wait! Wasn’t there any attrition? There had to be!” I needed
a way to figure out how many of the 57 new hires were additions over the baseline and how many were simply replacing people who had left. A quick trip over to the State Auditor’s Office gave me just what I needed - turnover rates by year for MD Anderson staff that excluded administrators and doctors. Average staff turnover per year from 2010-2014 was 12.4%, without any significant year-over-year differences. With that figure in hand, I easily calculated naturally occurring attrition from the IT department of 59 employees. In my fancy spreadsheet, 57 new hires to replace 59 departures equals more staff. Things that make you go hmmm… More Expensive Staff If the cost overruns couldn’t be attributed to an additional staffing requirement, they must have been caused by the increased salary demands of the new, “much more talented” IT staff they had to hire, right? Oh contraire, my friend. A tiny exploration into that same darn public report on staff salaries shows that IT staff at MD Anderson who have been employed 1 year or less actually earn 8% less on average than IT staff members tenured between 1-10 years. By my calculations, those 57 new hires actually saved them about $1.8 million! Doesn’t anyone look at this stuff?
fiscal year ended August 31st, 2016 so I knew by now there must be additional data available. I found a report that showed actual consulting expenses in the last quarter of 2016, which was still only 6 months after implementation of the EHR. Extrapolating this figure through one additional quarter gave me enough data to project consulting expenses for a full year before and a full year after implementation, and then compare the increase to “normal” annual increase percentages from prior years. This yielded an annual consultant expense increase of closer to 5.4%, which is actually lower than the 6.7% “normal” increase between FY2014 and FY2015. Whew! I might still have a job next year after all! So if it’s getting a lot harder to point the finger at Epic for MD Anderson’s financial woes, who is to blame? You might just have to hire a darn consultant to find out… For more information visit cynexconsulting.com or call 210.910.6266. Cynex Consulting is located at 311 Bowie Street, Suite 1806 in Austin, TX 78703.
The Darn Consultants Consultants are a natural scapegoat; so let’s have some fun with this one since MD Anderson and the news so nonchalantly threw us into the mix. A cursory glance at MD Anderson’s publicly published “Expenditures by Natural Expense Classification” from FY 2015 and FY 2016 does reflect a 15.9% year-overyear increase in consulting fees. But this consultant couldn’t just stop right there because MD Anderson’s 2017 - APRIL MD Monthly
21
INFORMED PATIENT/SAN ANTONIO
Dental Care
DURING CANCER TREATMENT By Michele Bishop, DDS
I
n 2016, an estimated 1,685,210 new cases of cancer was diagnosed in the United States and 595,690 people died from the disease. Those are staggering numbers if you think about it. Of those people receiving treatment for their cancer 40% will develop oral complications regardless of the location of the cancer. Cancer treatments whether radiation or chemotherapy can wreak havoc on your immune system and weaken it making you more susceptible to infections. It can affect your salivary glands and
22
MD Monthly
reduce salivary flow causing dry mouth which in turn can cause dental sores and cavities. So what can you and your dentist do to help with those complications? Let’s talk about 3 different stages of dental care needed with your cancer diagnosis: 1. Before cancer treatment dental care 2. During cancer treatment dental care 3. After cancer treatment dental care Before any cancer treatment begins you should see your dentist
for a complete exam and x-rays to rule out any dental infections, areas of decay or periodontal disease. Any of these can delay your cancer treatment or cause complications with your treatment. Your dentist will also discuss side effects usually seen during your type of cancer treatment and some remedies that are available to help with the side effects. Your dentist may recommend fluoride trays be made ahead of any radiation to the head and neck. Radiation to the head and neck area can reduce salivary flow which can lead to rampant cavities. The fluoride trays are used with a small amount of fluoride that is allowed to sit along the teeth and
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/SAN ANTONIO
gums and help prevent those cavities. During cancer treatment you want to follow your regularly scheduled hygiene appointments so your dentist is able to stay on top of any cavities that have started, help you with any hygiene concerns and most importantly perform oral cancer exams to ensure that no signs of metastasis have arisen in the mouth. Some side effects from chemotherapy or radiation can include painful mouth sores. Your dentist can discuss options to help with those including warm salt water rinses or prescription rinses that can coat the mouth and provide pain relief. After cancer treatment it is recommended to continue with your scheduled appointments as
some salivary glands do not return to normal function after treatment and monitoring for rampant decay is important. Oral cancer exams should be performed regularly as well. Before, during and after cancer treatment it is essential to do
everything possible to keep the mouth clean and free of bacteria. Brushing your teeth often and flossing daily will help keep cavities at bay. Drinking lots of water as opposed to sugary sodas, juices, sports drinks or alcohol will help keep the mouth hydrated. Avoid spicy and hard foods if mouth sores or sensitive gums are present. Take the time to talk to your dentist about your cancer diagnosis and let them help you keep your mouth healthy during the process.
2017 - APRIL MD Monthly
23
INFORMED PATIENT/SAN ANTONIO
Plastic
TAKING THE
Surgery: OUT OF
Emerging Trends in Aesthetic Medicine By Dr. Constance Barone
A
s a surgeon with my own practice, and over twenty years experience in cosmetic surgery, I witness a lot of emerging trends in the cosmetic industry. Recently, I’ve noticed a shift in my client's aesthetic goals… people are looking for more natural results, and less invasive procedures to accomplish them. Yet, the term “plastic surgery,” sometimes still conjures images of invasive procedures with artificial products. However, plastic surgery doesn’t have to feel invasive, or artificial at all. In fact, it’s never been less so. Then why use the word, “plastic,” in the name? In fact, plastic
24
MD Monthly
surgery gets its name from the Greek word plastikos, meaning to form or mold, not from the synthetic substance. So let’s focus on the advancements in form and function that are leading the way in making cosmetic surgery one of the most innovative fields. Here are some new products, and less invasive methodologies that I use at my office to provide patients with the natural, yet enhanced look they desire, and that are changing the face of cosmetic surgery. Ideal Implants: As a board-certified plastic surgeon who has been practicing cosmetic surgery for over two decades, I have seen the pendulum
swing back and forth in regard to breast implants. While silicone gel implants were once all the rage, a new option has emerged that’s introduced a more natural feel: the Ideal Implant. The ideal implant is a structured breast implant which combines natural feel with the safety of saline inside. It’s also incredibly safe: FDA data recently revealed that it also has the lowest rate of capsule contracture or scar formation around the implant and the lowest rupture or deflation rate. Amazingly, the Ideal Implant also comes with lifetime limited warranty. It’s not surprising that many of my patients choose Ideal Implants over other brands… and are loving it. When pursuing a natural
look and feel, the ideal implant is a breakthrough advancement and one of several innovations at the forefront aesthetic medicine. NovaThreads: Nov threads are dissolvable threads that help augment the face in a way that prevents puffiness. If you’re considering facial work, they truly are a breakout option in the market to take note of. While fillers may leave the face swollen, NovaThreads are dissolvable sutures that are absorbed by the skin, and don’t require surgery to put in place. With a painless and quick procedure, it’s one of the least invasive new advancements in aesthetic medicine. It’s also something I call a “lunchtime procedure”: many of my
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/SAN ANTONIO
patients come on their lunchbreak and return straight to work with NovaThreads, with no downtime, no bruising, no stitches, and no scarring, and skip the aftereffects of a facial lift. Healthwise, NovaThreads are one of the safest materials to be implanted in the body. Why? Your skin fully absorbs them within 4 to 6 months and won’t leave you with any scar tissue. Nova threads are an innovation I love to recommend to patients looking for a natural lift result. SmartGraft: When it came to helping patients with hair loss, hair restoration procedures used to require major surgery, leaving a large linear scar across the back of the head. Recovery time was slow and very uncomfortable. In recent years, newer follicular unit extraction (FUE) technologies have been developed, but are still slow and inefficient. SmartGraft, which takes an innovative approach to single hair follicle transplants, is a fantastic new option for both men and women searching for a permanent solution to hair loss. SmartGraft uses a combination of precision craftsmanship and stateof-the-art technology rather than a scalpel. The procedure can be done with more precision in less time than any other FUE method, and patients can go back to work in one or two days. What’s more, is it’s minimally invasive, and virtually pain-free. Most
importantly, SmartGraft garners incredible results: the look and feel is completely natural. Ultimately, as a surgeon, my practice philosophy has always centered around helping people to feel and look like their best selves. That means helping people achieve their aesthetic goals, while honoring their natural look and complementing their born features to create a seamless result. By embracing cutting-edge surgical techniques like Ideal Implant, Novathreads, and SmartGraft, my clients achieve the natural, improved look they desire. While these are some emerging, cutting edge products that anyone considering cosmetic surgery should consider, there are many more. As a surgeon who prides myself in learning new techniques and advancements, I look forward to discovering more and sharing them. Constance M. Barone, MD, FACS Past Chief of Plastic Surgery at the University of Texas San Antonio Board Certified Plastic Surgeon 9502 Huebner Road building 2 unit 202 San Antonio, Texas 78240 Telephone (210) 614-0400 baroneplasticsurgery.com
constancebarone1@yahoo.com
Dr. Charles Bailey is an interventional cardiologist and endovascular specialist. He is board certified in Internal medicine, cardiovascular disease and interventional cardiology. Dr. Wassim Choucair is an Electrophysiologist and is board certified in internal medicine, cardiovascular disease, echocardiography and electrophysiology. He specializes in treating the electrical abnormalities of the heart that require pacemakers, defibrillators and the latest in ablative techniques to treat rhythm disturbances. Dr. Feras El-Bash is an interventional cardiologist and endovascular specialist. He is board certified in internal medicine, cardiovascular disease, interventional cardiology, echocardiography, nuclear cardiology, and endovascular medicine. Our physicians treat cardiovascular disease, peripheral artery disease, rhythm disturbances, as well as the risk factors that cause these disorders, such as high blood pressure, high cholesterol and diabetes. They are skilled in performing procedures to identify and repair blocked arteries and treat electrical abnormalities using the latest tools and technology.
SAME DAY APPOINTMENT AVAILABLE
2017 - APRIL MD Monthly
25
1202 E. Sonterra Blvd., Building 6, Suite 604 San Antonio, TX 78258 | 210.844.2393
INFORMED PATIENT/SAN ANTONIO
CAN DIABETES BE
“Cured”? By Subhash Reddy, MD
M
etabolic syndrome refers to group of risk factors that increases the risk for heart diseases and other health conditions like diabetes, stroke, cancer and decreasing overall lifespan. These risk factors include obesity, high blood pressure, elevated cholesterol (high triglycerides, low HDL) and elevated blood sugar levels. The risk of having severe heart disease is increased over 20% during a 10 year period for those affected with metabolic syndrome. Over decades, doctors have focused on managing these risk factors with medications, diet and exercise. Despite optimal medical management, the prevalence of diabetes and heart disease is growing throughout the world! Overall, the obesity population has doubled since 1980 and adolescent obesity has quadrupled in the last three decades (21% in 2012). In Texas, over 30% of the adult 26
MD Monthly
population is obese (BMI > 30) and > 9% of adults were diabetic in 2014. Changes in lifestyle, environmental factors, physical inactivity, diet, medications and genetic factors are attributed to the growing obesity population. An estimated 26 million people in the United States have diabetes, and this figure is projected to nearly double by 2034. In 2012, the direct medical cost of diabetes in the United States was calculated at around $176 billion, and on top of that, the cost of lost productivity was $69 billion. Diabetes is alarmingly linked with heart attacks, amputations and even blindness amongst many other serious complications. As we all know, weight loss results in better control of metabolic syndrome but most people don’t have long-term success for weightloss using only diet, medications and exercise. Bariatric surgery has been proven to provide long-term weightloss which leads to the resolution
or optimal control of metabolic syndrome, decreasing the risk of diabetic complications, cancer and even death. Recent studies have shown that there is an overall 86% resolution of metabolic syndrome and more specifically a 78% complete remission of Diabetes up to 9 years after surgery! One of the studies from Cleveland clinic, Ohio published in the reputed New England Journal of Medicine compared treatment of diabetes between intensive medical therapy, gastric bypass and sleeve gastrectomy. This study showed that surgery was much more likely to result in diabetes resolution up to 3 years after surgery while patients treated with medication alone failed 80% of the time after just 1 year. The million-dollar question is why is it that surgery is so much better than medications alone? The answer is broken down into two parts. The first obvious answer is that surgery is much more likely to provide the
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/SAN ANTONIO
most sustained weight-loss. The second answer is more interesting in that many of the improvements in metabolic syndrome occur BEFORE THERE IS SUBSTANITAL WEIGHT LOSS!. In the gastric bypass, this is accounted for by rerouting the intestines which leads to rapid and direct exposure of nutrients to the distal small bowel which increases “chemicals” produced by the intestines such as glucagon like peptide (GLP -1) and YY peptides. GLP-1 increases insulin secretion and decreases glucagon which leads to better blood glucose control and decreased appetite. Bypassing also decreases anti-incretin production from the proximal small bowel which again improves insulin production. There are other attributes in the body that are changed by the gastric bypass operation. Gut microbiome consists of trillion of bacteria in the colon (normally) which play a role in nutrient metabolism and absorption. In obesity there is an imbalance in bacterial load (increased Fermicutes , decreased bacteroidetes type) in the gut which favor enhanced expression of genes responsible for absorption of carbohydrates and lipids at gut level. This causes rapid absorption of food products. A gastric bypass alters this bacterial load to reduce absorption in the gut. Another change seen in the body is the flow of bile (bile acids) produced from liver is altered by surgery which favors increased carbohydrate metabolism, decreases cholesterol load and helps to change gut microbiota. Finally, insulin sensitivity is increased in the liver post bariatric
surgery. Obesity is a chronic inflammatory state and continued weight loss reduces adipose tissue which in turn is related to reduced inflammation, change in concentration of adiponectin ( antiinflammatory product produced by adipose tissue) which in turn reduces insulin resistance. All the above factors contribute to stopping all anti diabetic medications after bariatric surgery (especially gastric bypass) in > 90% of individuals (type 2). In regards to type 1 diabetes mellitus (insulin dependent) the amount of daily insulin requirement will decrease but some may not be off of insulin completely since these patients don’t have the beta cells to secrete innate insulin. Recently we are seeing more cases of adolescents with type 1 Diabetes undergoing a gastric bypass with good outcomes, but more conclusive evidence is required to conclude superiority of sleeve or bypass in this group of patients. What are the types of bariatric surgery that are best for resolving Diabetes? The gastric bypass continues to be a great option for the reasons listed above. Gastric banding is almost phased out based on evidence of metabolic outcomes and also band related complications. The sleeve gastrectomy is showing popularity with patients and with bariatric surgeons, but is a newer procedure compared to the gastric bypass. At this point we don’t have enough evidence to say that sleeve is as good as a gastric bypass, since we are limited by long term results (5-7 yrs: which show similar
metabolic outcomes compared to gastric bypass). Another bariatric surgery, the Duodenal switch, is the gold standard for excellent long term diabetes remission in morbidly obese patients. Due to the nature of anatomical rearrangement with the duodenal switch, it has a higher risk for nutritional deficiencies, so currently this surgery is limited to selected patients. Patients with this surgery will need closer follow up and must be diligent in following the surgeon’s recommendations to avoid nutritional complications. The mini gastric bypass which is gaining momentum in Europe , India and South America is still not performed extensively in the United States (first performed in the US in 1997) considering the increased risk of bile reflux, marginal ulceration , and risk of gastric and esophageal cancer. Because of this, the gastric bypass will continue to be better option for type 2 diabetes for now, but not one surgery can fit everyone. The type of surgery chosen for each person is decided based on comorbidities, lifestyle, psychological condition, family history and finally by the expert (Surgeon). If you suffer from diabetes or metabolic syndrome, you should consider talking to a bariatric surgeon to see if surgery may be a reasonable option for you. For more information, visit texasbariatricspecialists.com or call 877.538.6909. The corporate headquarters for Texas Bariatric Specialists is located at 14603 Huebner, Building 2 in San Antonio, Texas 78230.
2017 - APRIL MD Monthly
27
INFORMED PATIENT/SAN ANTONIO
Are Scribes Worth It
FOR MY MEDICAL PRACTICE? By Tim Taylor, MD FACEP Founder and Chief Medical Officer at ProScribe
T
he days of a quickly written, barely legible, assessment and plan for your clinic patients are long gone. There are certainly pros and cons regarding the evolution to more thorough medical documentation with even more polarizing pros and cons surrounding Electronic Medical Records. Advantages aside, medical documentation especially of the “Electronic” variety is awkward, slow, repetitive, and impersonal. Assuming your medical practice has already made the transition to an electronic health record, you have probably seen a significant drop in productivity and a precipitous decline in provider satisfaction. Two of the questions that all medical practices must answer are… •
28
How can we make our practice more productive while
MD Monthly
•
also making our providers’ jobs more satisfying? Are Medical Scribes right for our practice?
(Daily Scribe Cost) is less than, equal to, or greater than (Additional Daily Revenue). Financial Assumptions:
Two fundamental considerations in evaluating whether a medical scribe would benefit your practice: 1. What is the financial impact of using a Medical Scribe? 2. Will a Medical Scribe make our provider happier and their workday more satisfying? The easiest consideration to evaluate is the financial impact. It’s so easy to analyze, that most doctors can even do the math (btw, I’m an MD). Since the nation’s top scribe companies charge a flat hourly rate and most practices know how much they collect per patient, the equation can be this simple …
•
•
Lets assume a Scribe Cost of ($20) per hour. So, our Daily Scribe Cost is 8 hours times $20 = $160/day. We will estimate a collection rate of $80 per patient. A practice would need to see 2 additional patients to collect $180 to make the financial impact neutral.
Some practices are still trying to get back to their pre-EMR productivity and scribes can be an effective way to capture those lost visits. The scribe industry has involved rapidly over the past 5 years and the benefit of using a national scribe
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/SAN ANTONIO
company today is that the scribes are not employees of your practice. All of the insurance costs, health and 401k expenses, training expenses, HR headaches, and more fall on the backs of the scribe companies. So, the financial and training burdens are not felt by your practice. Scribes come into your practice fully trained in your specialty and trained on your EMR. Now, lets talk about lifestyle improvements… based on different estimates, providers click an EMR between 750-4000 times during a full day in the clinic and the hospital. Many Physicians are forced to stay late, work through lunch, or complete charting from home in the evenings and on weekends.
Lifestyle Assumptions: • • •
Using a scribe will eliminate almost all after hours charting Using a scribe will help assure charts are completed daily Using a scribe will allow you to spend more time with your patients
It is hard to put a price on time spent documenting during off hours, but lets agree getting charts done by the end of the day is better than completing them at night and on the weekends. Calculating the math on whether scribes make sense to improve job satisfaction and work-life balance shouldn’t need a calculator or a formula… SCRIBE + DOCTOR = YES! There is certainly more to the process of deciding whether
to use scribes in your practice than just lifestyle improvements and financial considerations. However, with the growing compliance and documentation requirements being added to Medical Practices, Physicians and Practice Administrators must find innovative ways to ease physician burnout and improve productivity. From my perspective, a scribe makes perfect sense and I will absolutely never work clinically again without one. For more information on how medical scribes can impact your practice, call 888-991-1773 or send an email to info@proscribemd.com.
2017 - APRIL MD Monthly
29
INFORMED PATIENT/SAN ANTONIO
BENEFITS ABOUND: TELEHEALTH IS HELPING THE WAY MENTAL HEALTH PATIENTS CAN RECEIVE BETTER SERVICE By Dr. Kasi Howard, Psy. D
I
t’s no secret that while many brick and mortar stores are closing, Amazon stock continues to rise at an astronomical rate. The way in which we do business has quickly changed. Smart phones allow us instantaneous access to almost any product or person in the world … except your health care providers. But that is quickly changing, too. The Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services defines telehealth as “the use of electronic information and telecommunications technologies to support and promote longdistance clinical health care, patient and professional health-related education, public health and health
30
MD Monthly
administration. Technologies include videoconferencing, the internet, streaming media, and cell phones.” According to the U.S. Healthcare Efficiency Index, an independent entity that gathers data on health insurance utilization, over 1.5 billion health care claims were filed in 2013. Less than 4,000 of those were telemedicine claims. That’s less than 0.000003 percent. Fortunately, Medicare created an initiative in 2015 to increase telemedicine services. And where Medicare leads, most private payers tend to follow. If the medical community is in the slow track of the digital age, the mental health community is just happy to be on the track. Often
underfunded, over-criticized and underutilized, mental health providers are usually left to their own devices to ensure their patients receive adequate care. Thus, telemedicine presents a unique opportunity for those in the mental health community to broaden their services to reach those who need it most. While some patients may be concerned about telehealth being impersonal, the benefits that it offers far outweigh the potential drawbacks. For example, those in rural - and even not so rural cities - often lack access to specialized care. = Driving 200 miles to the nearest metropolis for an appointment is simply not an option for your average American.
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/SAN ANTONIO
And doing it weekly for consistent appointments is just outlandish. Using a secure video platform, patients can now access psychologists specialized in treating everything from ADHD to PTSD from the comfort of their home. This is an added bonus for those who suffer from anxiety and find it difficult to leave home to attend regular appointments. Finding after hours appointments can also be difficult even for those who live in areas where treatment is readily available. Telehealth opens up opportunities for a patient to have an appointment on their lunch hour or other break in the day.
what do patients need to know about telehealth therapy before choosing a psychologist? • •
•
• With so many benefits, many people are gravitating toward telehealth as a viable option. So
Be aware that state licensure rules still apply. This means that you can only be seen by someone in your home state. Feel free to ask your psychologist what training they have in your particular area of need before making an appointment. For example, someone who specializes in trauma should be attending trainings in trauma treatment every year to stay on top of the latest treatments. Ensure that any provider is using HIPAA approved video software for all sessions. This ensures your privacy
and is a good indicator that you are dealing with a competent provider. Most states have parity laws that require claims for telehealth services be paid at the same rate as inperson services; however, it’s always best to confirm your benefits before making an appointment.
Telehealth is a convenient and viable option for most people. It’s just a matter of finding the best fit. Dr. Howard is a clinical psychologist treating eating disorders, anxiety, depression, and marriage issues in the San Antonio area. For more info, visit kasihoward.com.
2017 - APRIL MD Monthly
31
INFORMED PATIENT/CORPUS CHRISTI
BACK TOGETHER
Neck Pain By Melissa Y. Macias, MD PhD South Texas Brain and Spine Center
T
here are many causes of neck pain, from simple muscle tension or spasms to more complex degenerative cervical spine disease. The cervical spine is the spine component of the neck, and it consists of 7 bones, or vertebrae. The first two have a unique anatomy and are called the axis and the atlas; together they comprise the axial cervical spine that articulates with the base of the skull to support the head. The remaining 5 vertebrae are collectively called the subaxial cervical spine and they all have a similar anatomy; articulating together to protect the spinal cord and the spinal
32
MD Monthly
nerves and to provide structure and support in the neck area. Muscle tension or strain may occur with poor posture habits, work activities, prolonged sitting or inactivity, or a plethora of other reasons in day-to-day living, Though quite uncomfortable, this usually is not serious and may be effectively treated with stretching, massage therapy, or over-the-counter pain relief medications, such as acetaminophen or ibuprofen. More serious is neck pain due to degenerative changes in the spinal column. Degenerative conditions
are changes that occur to the bone, disc, facet (joint), and ligamentous structures. As the discs wear down and lose water and collagen content, strain is put on surrounding structures which begin to alter as well. Common changes include loss of disc height, disc bulging, osteophyte growth (also called bone spurs), facet (joint) arthropathy, and thickening of the ligaments. As these changes occur, they may bring about narrowing around the spinal cord or spinal nerves causing neurological symptoms and pain. The narrowing of the center canal is a condition called central
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/CORPUS CHRISTI
cervical stenosis and often leads to compression of the spinal cord, resulting in neurological changes called myelopathy. Symptoms of myelopathy include: • Difficulty with fine motor movements of the hands, i.e. clumsiness • Changes in writing ability • Heaviness or stiffness in the arms, along with weakness • Gait imbalance (difficulty balancing when walking) • Bowel or urinary changes • Possible neck and/or upper extremity pain or numbness This condition is quite serious, and if not treated may lead to permanent neurological deficit or functional loss. Surgical treatment to decompress and relieve the pressure from the spinal cord is usually required. When the narrowing occurs laterally rather than centrally, impingement of the spinal nerve may result in shooting pain down the arm. This type of pain is called radiculopathy as it “radiates” away from the neck into the arms. Two
spinal nerves exit at each level from both sides of the spinal cord to go into the left and right arm. Therefore symptoms may be uni- or bilateral, depending on whether the lateral narrowing is uni- or bilateral. Symptoms of lateral nerve impingement include: • Neck pain, stiffness • Radicular pain–often described as shooting, electric-type pain– down the arm or hand • Numbness of the afflicted arm/hand • Tingling or hypersensitivity • Weakness, clumsiness • Pain elicited with certain neck movements This condition may also lead to permanent neurological damage, resulting in neurologic deficits if not treated, but if caught early can often be treated with non-surgical care. However, if weakness is present, then surgical decompression may be required to prevent further loss of strength. Neck pain from degenerative changes in the spine, commonly
thought of as arthritis of the spine, may occur alone or be accompanied by the above symptoms. Neck pain due to these changes can also alter the curvature of the cervical spine, leading to more strain on the supportive anatomical areas such as muscles and tendons. In this manner it can become a vicious cycle until identified and treated. Non-surgical treatment options consist primarily of: • Physical therapy—which may include stretching, traction, or electrical stimulation • Ultrasound treatments • Pain management with nonsteroidal anti-inflammatory medications/muscle relaxants • Yoga/meditation • Massage therapy • Correcting ergonomics of work/ home environment • Steroid or analgesic injections Often, the treatments above, either alone or in some combination, may effectively treat neck pain. It is important to identify the cause and source of the pain if it is present for more than six weeks, progressively worsening, or associated with radicular or myelopathic symptoms such as those described above. As always, talk with your doctor if you experience neck pain issues so that the appropriate evaluation, such as X-rays, a CT scan or MRI, can be ordered to best assess your condition. Wishing you good spine health! For more information about South Texas Brain and Spine Center visit SouthTexasBrainAndSpineCenter.com or call 361.883.4323
2017 - APRIL MD Monthly
33
INFORMED PATIENT/HOUSTON
IDENTIFYING CANDIDATES FOR
DEEP BRAIN STIMULATION
FOR PARKINSON’S DISEASE
Appropriate patient selection, pre-operative assessments, and careful patient counseling are all essential components to successful DBS in PD. By Joohi Jimenez-Shahed, MD Key Points There are several steps in determining the appropriateness of deep brain stimulation (DBS) for patients with Parkinson’s disease (PD). First, confirm the clinical impression of idiopathic levodopa-responsive parkinsonism without atypical features to suggest secondary causes. Carefully review the DBS candidate’s medications to identify possible modifications to improve management. Inform candidates about the indications and risks/ benefits of DBS. A multidisciplinary team approach involving neurologists, neurosurgeons, and neuropsychologists is ideal to review candidates for DBS and make recommendations about unilateral
34
MD Monthly
vs. bilateral procedures and the site of stimulation. Appropriate counseling and education of the patient is essential. Expert analysis There are no evidence-based guidelines to help clinicians determine if or when PD patients are appropriate candidates for DBS, though decision tools exist.1,2 Generally accepted criteria include patients with idiopathic PD, a robust response to levodopa, complications of medical therapy (such as motor fluctuations or dyskinesias), lack of significant psychiatric and/or mood symptoms, and no dementia.3 DBS is also considered in PD when disabling tremor is refractory to
medical therapy. Individual risk/ benefit analyses and subjective considerations, such as impact on quality of life, may also be applied.4 For example, there are uncommon cases in which DBS may still be considered in the presence of severe, disabling, or painful dyskinesias despite evidence of cognitive impairment. In 2016, the U.S. Food and Drug Administration updated the DBS label for one manufacturer’s device to include its use in people with PD of at least four years duration and with recent onset of motor complications, or motor complications of longer-standing duration that are not adequately controlled with medication. Clinicians are therefore faced with important decisions about the right timing for referring a patient
APRIL - 2017
MDMONTHLY.COM
INFORMED PATIENT/HOUSTON
for surgical therapy. The first step in considering DBS in PD is confirming the clinical impression of idiopathic levodopa-responsive parkinsonism without atypical features to suggest secondary causes. This is generally established by routine clinical examination, careful history taking, and brain imaging, when appropriate. For example, atypical parkinsonism, such as multiple systems atrophy (MSA), can sometimes pose a dilemma to the treating neurologist, because it can begin with levodoparesponsive parkinsonism, often with fluctuations and dyskinesias. However, the parkinsonism is quite rapidly progressive, and more florid dysautonomia occurs early in the disease course. 5 Any patient presenting a management challenge that might seem amenable to DBS within five years of symptom onset, should signal the neurologist to consider an atypical cause of his/her parkinsonism. The next step is to carefully review the DBS candidate’s medications. Often, significant improvements in daily functioning can be achieved by maximizing dopaminergic medication dosing or using extended release formulations, limiting levodopa to the least amount required to turn “on,” or adding amantadine.6 Extended release formulations of dopaminergic drugs at night can be used to improve morning “off” periods (times when the medication is not working well). Botulinum toxin injections or anticholinergic medications may be used to address dystonic symptoms.7 Any or all of these strategies could be used with patients. However, these adjustments are temporizing for weeks or months, or side effects
may occur such that DBS may still be the ultimate recommendation. Third, the patient should be appropriately informed about the indications and risks/benefits of DBS. Ideally, the discussion and education process about DBS should begin at the time that the treating neurologist recognizes the presence of complications of PD therapy. The time it takes for these manipulations to run their course can be maximally utilized by the healthcare provider to prepare the patient and family for the ultimate choice to pursue DBS surgery. This can take the form of distribution of the increasingly numerous patient education materials (DVDs, monographs, books or websites), referral to a movement disorders specialist or other center with expertise in managing PD patients with DBS, or scheduling the appropriate pre-surgical evaluations when appropriate. Patients would certainly benefit from any of these possibilities. Once the decision is made for the patient to pursue DBS, he/ she should undergo pre-operative assessments to finalize his/her candidacy for the procedure. This type of assessment typically includes measurement of PD symptoms both “off” and “on” medications (to confirm levodoparesponsiveness and guide discussions of expectations from surgery), and neuropsychological testing to measure the DBS candidate’s emotional and cognitive well-being prior to surgery.8 Together, appropriate patient selection, pre-operative assessments and careful patient counseling can be used to ensure the most successful DBS outcomes for patients with PD.
To view the full article please visit: http://practicalneurology.com/2012/12/ identifying-candidates-for-deepbrain-stimulation-for-parkinsonsdisease?center=35 Dr. Jimenez-Shahed is Assistant Professor of Neurology, and Director of the DBS Program at Baylor College of Medicine, Parkinson’s Disease Center and Movement Disorders Clinic. 1. Okun, M.S., et al., Development and initial validation of a screening tool for Parkinson disease surgical candidates. Neurology, 2004. 63(1): p. 161-3. 2. http://www.medtronic.com/ physician/dbs/referral/index. html?c=dbsreferraladvisor, DBS Patient Referral Advisor. 3. Bronstein, J.M., et al., Deep brain stimulation for Parkinson disease: an expert consensus and review of key issues. Arch Neurol, 2011. 68(2): p. 165. 4. Morishita, T., et al., DBS candidates that fall short on a levodopa challenge test: alternative and important indications. Neurologist, 2011. 17(5): p. 263-8. 5. Wenning, G.K. and N. Stefanova, Recent developments in multiple system atrophy. J Neurol, 2009. 256(11): p. 1791-808. 6. Stocchi, F., M. Tagliati, and C.W. Olanow, Treatment of levodopainduced motor complications. Mov Disord, 2008. 23 Suppl 3: p. S599-612. 7. Sheffield, J.K. and J. Jankovic, Botulinum toxin in the treatment of tremors, dystonias, sialorrhea and other symptoms associated with Parkinson’s disease. Expert Rev Neurother, 2007. 7(6): p. 637-47. 8. Amick, M.M. and J. Grace, Deep brain stimulation surgery for Parkinson’s disease: the role of neuropsychological assessment. Med Health R I, 2006. 89(4): p. 130-3. 2017 - APRIL MD Monthly
35
F E A R to
P: 210.504.5053 www.MariaPalafoxMD.com " @PC? Q A?LACP BG?ELM G A?L QFPC?QCL LMQ MLJV ? TMK?L| JGDC @RQ FCP CJD AMLDGBCLAC 6GQF LCT RPEGA?J QCAFLGORC RPECML ?Q ?PC LMT ?@JC QM ?AFGCSC MNQGK?J AM KCQGA PC RJQ ?LB GKNPMSCB OR?JGQV MD JGDC DMP @PC? Q A?LACP N?QGCLQ #V NCPDMPKGLE )GBBCL A?P #PC? Q $?LACP RPECPV MRP RPECML CDDCAQGSCJV QPC?Q A?LACP TFGJC NPC CPSGLE QFC L?QRP?J F?NC MD QFC @PC? Q JC?SGLE LM SG G@JC PCKGLBCP @CFGLB
LEARN MORE AT
MyHiddenScar.com LIT 11968 Rev. A
CCTV | Hidden Cameras | Access Control | Alarm System | Night Vision Cameras | Intercom Systems
SMART HOME AND BUSINESS CONTROL Residential // Commercial // Small Business
AS LOW AS
$
2995
/mo.
TO INSTALL A SMART HOME CONTROL
The Dyezz HomeControl online portal lets you quickly and easily manage your system and monitor your home effortlessly from anywhere, using any standard web browser on your computer or mobile device. • ALARM SYSTEM • SECURITY CAMERAS • THERMOSTAT CONTROL • LOCK AND UNLOCK • LIGHTING CONTROL • GARAGE OPEN AND CLOSE • ALL REMOTELY FROM YOUR APP OR WEB PORTAL
• AUSTIN • SAN ANTONIO • EL PASO • HOUSTON • DALLAS
1.800.370.2762 / www.dyezz.com
Ser ving pat i ents t hrou gh Te l e h e a l t h Innova recovery is a telehealth treatment center for men and women ages 18 and older. Easily accessible from anywhere in the state, Innova is designed for clients who want exceptional treatment in a setting that is conducive to their lifestyle.
Therapy for Post Traumatic Stress Cognitive Behavioral Therapy (CBT) Exposure and Response Prevention (ERP) Family Therapy Dialectical Behavioral Therapy (DBT) Eye Movement Desensitization Reprocessing (EMDR) Meditation Therapy
innovarecoveryclinic.com | 210.254.3618
®
Dr. Constance Barone: ON THE CUTTING EDGE OF
Cosmetic Surgery By Rudy Arispe
D
r. Constance Barone was a young girl when her mother taught her the finer points of sewing, like the patience and keen eye for detail required to stitch the elaborate costumes she wore for childhood ballet performances. “My mom was an amazing and talented woman,” Dr. Barone said. “She would teach me how to look at a picture of a dress in a magazine and sew it freehand. When she was ill with breast cancer, I would show her Vogue magazine and tell her to pick a dress. I would go and buy the exact same material and make it for her.” Little did the young Constance know that decades later those sewing skills would prove invaluable when she was a general surgery resident at Temple University Hospital in Philadelphia in the 1980s and performed a number of head and neck surgeries.
40
MD Monthly
APRIL - 2017
“My mother’s sewing instructions were actually very helpful in surgery,” said Dr. Barone, who was the third woman to complete Temple’s general surgery residency and the first woman to receive the Caswell Teaching Award as a chief resident in general surgery. “We didn’t have staplers back then. We did all of the delicate thyroid and vascular surgeries. We hand sewed everything.”
life that led Dr. Barone to alter her course and choose a different medical career path. The first involved a patient who suffered from a severe and aggressive cancer to her jawline, which required complete removal of her jaw.
It was two profound incidents, however, in her work and personal
The second incident was the death of her mother from breast cancer that occurred on Dr. Barone’s 20th birthday.
I ENJOY THE CREATIVITY OF PLASTIC SURGERY AND BEING ON THE CUTTING EDGE.
-Dr. Constance Barone
“She was one of the sweetest people I have ever met,” Dr. Barone recalled. “I really wanted to help her with reconstructive surgery.”
“She had a mastectomy and was embarrassed because there was no breast reconstructive surgery back then. But we were just happy to have her alive,” she said. “In the early 1970s, reconstruction options were poor, and most surgeons would not even discuss it unless you were free from cancer for at PHOTOGRAPHS BY Marc Arevalo
MDMONTHLY.COM
least five years. Breast cancer education and early screening for breast cancer in the early ‘70s were in their infancy.” Those two impactful episodes led Dr. Barone to concentrate on cosmetic surgery. Now as a leading and respected plastic surgeon in San Antonio with a state-of-the-art facility and spa, she offers surgical treatments for the breast, body and face, as well as non-surgical cosmetic procedures for both men and women seeking a more youthful appearance. “I enjoy the creativity of plastic surgery and being on the cutting edge,” she said. “For instance, I do clinical trials for companies to get FDA approval on the latest
cosmetic equipment. Having my own accredited surgical center, I’m able to get state-of-the-art equipment without going through the bureaucracy of large hospitals.” The board certified plastic surgeon is also an instructor for NovaThreads, synthetic absorbable surgical sutures, which are considered especially effective for tightening the neck and jawline, according to its website. Lately, Dr. Barone has witnessed an upward trend in both men and women seeking to maintain excellent skin care. “Sixty is the new 40,” she said, “especially if you maintain your looks and stay active.” In fact, she has developed her own line of medical products for skin and body toning and to help erase brown spots and scars. Her spa also provides laser hair removal, skin regeneration, microdermabrasion and the newest in radio-frequency technology for skin tightening. She is also proud to offer a revolutionary new treatment in hair transplantation called SmartGraft that she said leaves no scars and is done under a local anesthetic. “The results are better graft take because the grafts get suctioned into a dish with the right humidity and temperature, so you have a 99 percent graft take,” she said. “It’s new for both men and women.”
Had she not chosen to become a physician, it’s likely that Dr. Barone would have followed in her family’s pharmacology footsteps. Her father, grandfather, an uncle and brother were all pharmacists. But it was medicine that fascinated her since childhood, she said. After deciding to focus on plastic surgery following her completion of a general surgery residency, Dr. Barone completed a plastic surgery residency at New York University School of Medicine. “NYU is where I had a phenomenal experience because they were on the cutting edge of cosmetic surgery and microsurgery,” she said. She also did a post-doctoral fellowship in craniofacial surgery and pediatric plastic surgery at Albert Einstein College of Medicine in New York. In 2004, the University of Texas Health Science Center recruited her, where she became the first woman professor and chief of plastic surgery until deciding to go into private practice in 2007. When she’s not busy with patients, Dr. Barone occasionally finds time to take needle and thread to fashion pieces of fabric together to create beautiful garments – just like her mother taught her. “I absolutely love being a plastic surgeon,” she said. “It allows me to be creative, be part of making patients self-confident and utilize the lessons taught to me by my mother.” Dr. Barone’s office is at 9502 Huebner Road. For more information, visit baroneplasticsurgery.com or call (210) 614-0400. 2017 - APRIL MD Monthly
41
FEATURE-PROFILE/CORPUS CHRISTI
Dr. Melissa Macias, NEUROSURGEON, FINDS HER WAY
BACK HOME AT NEW PRACTICE By Edmond Ortiz
D
r. Melissa Y. Macias knew from age five that all she wanted to do was become a doctor.
She recalls her mother taking her and her siblings to their pediatrician. Melissa had taken her Raggedy Ann doll with her into the doctor’s office. Melissa, seeming a bit sad, was asked if anything was the matter. She replied that her doll had lost her eye and was “sick.” The button eye had come off she explained, as she showed the black four-holed button to her beloved pediatrician. Surveying the situation, he commanded “emergency surgery” was needed for the doll; and he left the room with his nurse, doll in hand. Upon return to the room, he presented her with a restored Raggedy Ann. He had stitched up the button eye and even placed an eye patch over the treated eye, calling the doll good as new. “It was an amazing moment. I was
42
MD Monthly
enthralled and captivated. Medicine became my passion,” she explains. Dr. Macias has traveled a somewhat unconventional route to a neurosurgical career. A native of El Paso, she graduated magna cum laude from the University of Texas at El Paso in 1990 with a bachelor’s degree in biology and chemistry before pursuing a doctorate in cellular biology and neuroanatomy at the Medical College of Wisconsin. Upon her graduation, she continued at the Medical College, beginning medical school with a focus on becoming a neurosurgeon. After completing medical school, Dr. Macias returned home to Texas, to practice at the South Texas Brain and Spine Center in Corpus Christi. She practiced there between 2009 and 2012. In between it all, as the saying goes, life happened. During her collegiate career, Macias returned
to her native El Paso to help care for her younger sister after their mother succumbed to cancer. Yet Macias continued to achieve academically with other collegiate and professional opportunities, and she followed a path that included working for NASA. She participated in three space shuttle missions as part of her PhD research, investigating how leaving and re-entering the Earth’s gravitational field affects muscles and nerves. So, exactly how did her professional interest in the brain and spine come about? Her doctorate advisor in Wisconsin worked as a principal investigator in biosciences for NASA, with a focus on neurobiology. That piqued her curiosity. “This exposed me to neurosciences—more specifically the human nervous system, and the study of which I found to be the most challenging and rewarding of all
APRIL - 2017
MDMONTHLY.COM
FEATURE-PROFILE/CORPUS CHRISTI
fields,” Dr. Macias says. Working for NASA, Dr. Macias relished the exploration of antigravity’s impact on muscles and on the central nervous system. However, this was not all she was interested in connection with the applications of this research to future space travel. Such research can help physicians better understand how muscles and nerves cope when a patient is bedridden from prolonged illness or injury, is immobile, or suffers from some form of paralysis. Dr. Macias never looked back after observing her first neurosurgical surgery where the brain was exposed. She knew this is where she belonged. “I enjoy the challenges. This is the hardest, more competitive (medical) field to get into,” she adds. “It’s the longest residency. I’ve never taken the easy road.” During her educational career, Dr. Macias has received numerous scholarships, research grants, and graduate level fellowships, including invitations to the annual International Symposium on Neural Regeneration in 1996 and again in 2005. During her residency at the Medical College of Wisconsin, Dr. Macias continued her academic interest in studying applications of stem cell treatments for injured spinal cords, receiving grant funding for this research. Further, encompassed in her residency was 12-month period concentrating
on comprehensive surgical management of spinal diseases. She has written and published many abstracts and research articles in peer-reviewed journals. She has also presented her work in many national meetings of neurosurgery and spine societies. Her focus of these endeavors remains on treatments and approaches toward comprehensive and complex spine pathologies. Dr. Macias formally launched her neurosurgical career at the South Texas Brain and Spine Center in 2009. She left the Brain and Spine Center at the end of 2012 and spent two years as a neurosurgeon with the Illinois-based SwedishAmerican Medical Group. She followed that with a practice at Milwaukee-based Aurora Neuroscience Innovation Institute, beginning in 2015. Although she has family and friends in Wisconsin, a chance to again practice in Texas was irresistible to Dr. Macias. She was excited about her return to Coastal Bend and calls the Brain and Spine Center an ideal place to apply compassionate care in helping patients address afflictions related to the brain or spine. When asked what is at the core of her practice principles, she replies without pause, “It’s compassion for other people— people who are going through difficulties,” Dr. Macias explains. “I always want to apply simple human kindness to patients and their
families as they navigate through their disease or problem. I take individual approach to patient care very seriously, as each patient is unique in his or her own concerns and problems. My goal is to partner with them so that they may achieve the quality of life they seek; or in case of emergent surgeries, I aim to be present for the patient and their family as they navigate a difficult and often frightening situation.” Dr. Macias joins Drs. Mathew Alexander, P. Langham Gleason, and Howard Smith in practice at the South Texas Brain and Spine Center. Now with more than 25 years of education and clinical experience under her belt, Dr. Macias treats the full range of spinal diseases and disorders: from disc herniations and spinal stenosis to complex degenerative conditions such as acquired adult scoliosis, basilar invagination, and trauma, infections and tumors of the brain and spine. While the human spine is subject to an array of movements, it can be debilitating when the spine health is not at 100 percent. Mobility of one’s head or limbs can be seriously affected by some diseases or disorders. “Education is another core principle,” says Dr. Macias. “I believe patients should know and understand their medical condition and I make a concerted effort to always review films and thoroughly discuss with each patient their disease pathology and all treatment options—non-surgical and surgical. I
2017 - APRIL MD Monthly
43
FEATURE-PROFILE/CORPUS CHRISTI
my interests. It’s something that I’m fascinated by,” she adds. Dr. Macias has expressed her enthusiasm for again working along the Coastal Bend. “It’s exciting to be back, to be part of this wonderful community, and to help empower patients so they can make informed decisions.”
believe it is our duty as physicians to educate our patients. Anything less is a disservice” Neck and back pain take a toll on worker health and productivity. In 2013, the Integrated Benefits Institute (IBI) found that nearly one in four people at work experience low-back pain. As a result, costs employers $51,400 year per 100 employees in lost productivity and medical treatments. Low-back pain has led to lost work time and underperformance at work, costing employers $34,600 per 100 workers, according to the same 2013 IBI study. Degenerative spine disease is more and more of a common diagnosis, a natural result of the overall population getting older. “It’s commonly referred to as arthritis of the spine,” Dr. Macias said
44
MD Monthly
of degenerative spine disease, which can be impacted by one’s lifestyle risks, such as obesity or smoking, or by genetics. Dr. Macias and her colleagues use a broad spectrum of techniques in treating spine conditions, including minimally destructive methods, but also seek out ways to prevent surgery—or make surgery a last resort treatment.
She looks forward to spending many more years in neurosurgery. “The breadth of neurosurgical complexity in the spine and brain remains challenging and exciting to me,” she adds. Reflecting upon her professional journey, she has learned many things about being part of a medical group. “There’s a lot to be said about being in a practice with partners you trust and where you are valued,” she says. Then with a smile she adds, “Let’s just say I’m home again.”
“In chronic degenerative disease, surgery is really the last thing we want to do. It’s often the option after therapy and pain management have failed,” Dr. Macias adds. In surgeries requiring bone fusion, Dr. Macias uses adult stem cell technology, where appropriate, to optimize success of the fusion, which translates to a successful outcome for the patient. “Regenerative medicine is one of
APRIL - 2017
MDMONTHLY.COM
DON’T LET YOUR VISION SLOW YOU DOWN • Lasik, PRK, ICL
• Diabetic Eye Care
• Cataract Surgery
• Glaucoma
(Advanced Symfony IOLs)
• General Eye Exams
• Dry Eyes / Allergies • Aesthetic Care (Forehead, Eyes, & Chin)
Most insurance plans accepted. Financing Available.
BOOK YOUR APPOINTMENT TODAY! 210.692.1388 | SouthTexasEyeInstitute.com 2424 Babcock Road, Suite 101 | San Antonio, TX 78229
Marc Arevalo Miranda Paredes Grizelda Garza Janet Montagne Managing Partner, River City Hospice Make-Up Artist Sofia Allen Locations Peggy's on the Green Clothing Courtesy of Neiman Marcus
Photography Photo Assistant Stylist Models
White Floral Scuba Dress Teri Jon – $380 Neiman Marcus Gold Earrings Jose & Maria – $240 Neiman Marcus Gold Necklace Stephanie Kantis – $295 Neiman Marcus Coil Hinge Cuff Bracelet Alexis Bittar – $295 Neiman Marcus
White Sheath Dress Milly – $650 Neiman Marcus Crystal Earrings Alexis Bittar – $225 Neiman Marcus White Lace Satin Heel Louboutin – $795 Neiman Marcus
White Moto Jacket Joie – $998 Neiman Marcus Tunic Blouse Stella McCartney – $715 Neiman Marcus Polka Dot Skirt Dolce & Gabbana – $1,495 Neiman Marcus Stiletto Heel Sophia Webster – $595 Neiman Marcus Ball Drop Earring Oscar De La Renta – $475 Neiman Marcus
Lace & Velvet Flare Dress Sachin & Babi – $995 Neiman Marcus Crystal Drop Earrings Alexis Bittar – $225 Neiman Marcus Crystal Choker Necklace LuLu Frost – $225 Neiman Marcus
FEATURE-PROFILE/SAN ANTONIO
DR. WASSIM CHOUCAIR
ADDS MORE HEART TO LIFE AS HE OPENS
THE HEART & RHYTHM INSTITUTE OF SOUTH TEXAS: From the Coastal Bend to the Alamo City, he has built a reputation as a top heart doctor and cardiac electrophysiologist By Rudy Arispe
D
r. Wassim Choucair has nurtured a lifelong dream since he arrived 15 years ago from the East Coast to South Texas, specifically Corpus Christi, where he established himself as one of the top cardiologists in the Coastal Bend area. Now, his goal is being fulfilled. After moving to San Antonio two years ago, Dr. Choucair recently launched his own medical group, Heart & Rhythm Institute of South Texas, in the Medical Center at 8122 Datapoint Drive. In addition, Dr. Choucair is a
54
MD Monthly
APRIL - 2017
partner with the Heart Endovascular and Rhythm of Texas (HEART) in Stone Oak at 1202 E. Sonterra Blvd. “I love South Texas and am happy to be part of the San Antonio medical community with offices in the Medical Center and Stone Oak,” he said. “I am also grateful for the 12 years I spent in Corpus Christi, where I was able to treat many wonderful patients, not just in Corpus but from all over South Texas, such as Rockport, Beeville, Alice and Kingsville. I’m also glad to be seeing patients at HEART and working with colleagues where patients benefit from our combined expertise.”
Dr. Choucair’s medical group, Heart & Rhythm Institute of Texas, aptly reflects the cardiac electrophysiologist’s specialty: rhythm disorders of the heart, including palpitations, fainting spells, irregular, fast and slow heart beat problems, among others. His knowledge, skills and expertise have literally saved hundreds of lives – just like that of 73-year-old, McAllen resident Abraham Tannous Eleven years ago, Tannous was given a grim diagnosis: two months to live because of congestive heart failure. However, after being referred to Dr. Choucair to analyze his
PHOTOGRAPHS BY Jason Roberts
MDMONTHLY.COM
FEATURE-PROFILE/SAN ANTONIO
pacemaker, Tannous was given a new lease on life. “He detected that one of the wires was deactivated,” Tannous, a retired owner of a clothing factory for 40 years, said, “so it was actually disrupting the rhythm of my heart. As soon as he reconnected it and recalibrated my pacemaker, there was a tremendous improvement. He saved my life. I had congestive heart failure, and I was in and out of the hospital because no one could figure out the problem. His ability to detect the not so obvious is magnificent.” To say that Dr. Choucair was an overachiever in his youth is an understatement. At age 16, the young Wassim left his friends and familiar surroundings of Lebanon and boarded an oceanic flight with his family to Los Angeles, where he majored in biochemistry at UCLA. By age 20, he started medical school at Columbia University College of Physicians and Surgeons. “I was the youngest in my class at medical school. When the dean addressed the class during our first week, she mentioned that one of us was underage to drink,” he said with a laugh. After receiving his MD, Dr. Choucair completed his residency and fellowships in internal medicine, cardiology and electrophysiology from George Washington University, the National Institute of Health and Georgetown University Hospital. In addition to heart and rhythm disorders, he also focuses on cardiac
devices and ablation interventions. “I’ve always been one to take the road less traveled, so I chose electrophysiology and treating rhythm disorders instead of doing stents,” he said. “I love implanting defibrillators and pacemakers and fixing heart rhythm problems. It’s like a meditation for me. Prescribing the appropriate device therapy and seeing patients improve is a tremendous honor.” Mapping the heart is another area of expertise for Dr. Choucair. “If someone has a rhythm disorder, like a short circuit, I need to map it using special equipment to electrically find the trigger points that cause the arrhythmia, such as slow or fast rhythms,” he said. “It can cause cardiac arrest, chest pain or loss of consciousness, or sometimes they are benign like when your heart beats fast because you get excited or drink too much coffee.” Atrial fibrillation is a common heart problem when it beats too fast, too slow or with an irregular rhythm. This can lead to a risk for stroke when it is persistent, Dr. Choucair explained. “As a cardiologist, I need to treat the stroke risks as diligently as the rhythm problems,” he said. “One-third of all strokes in some populations are due to atrial fibrillation.”
what I call a ‘ticklish heart.’ I tell my patients they have a ticklish heart, or a short circuit in the heart, that is taking over the main rhythm or spark we are born with, which is called the sinus rhythm.” Meanwhile, although Dr. Choucair now lives and practices medicine in San Antonio, he still treats patients from the Coastal Bend region who come to see him in the Medical Center. “My biggest joy is that I’m able to be as busy in San Antonio because of the wealth of opportunities, but I hope I will continue to see my patients, who I previously treated in the Coastal Bend area. I’ll always be here for them.” And for any Spanish-speaking patients, they’ll be happy to know that Dr. Choucair habla espanol, which he learned from 12 years of practicing medicine in Corpus Christi. For more information about Heart & Rhythm Institute of Texas or to schedule an appointment, call (210) 998-6900.
Putting a patient on a blood thinner they can tolerate, he added, is key to reducing the stroke risk. “After the patient is stable, then I focus on how to do the ablation or pacemaker to remedy their rhythm problems, or
2017 - APRIL MD Monthly
55
Dr. Vijay Bindingnavele SEES PLASTIC SURGERY AS A WAY
to Improve Self-Image By Edmond Ortiz
D
r. Vijay Bindingnavele has a love for art. In his days in school, he drew just for the fun of it. But more than that, he has a passion for being creative and recreative. Dr. Bindingnavele also appreciates form—something that, being a plastic surgeon, he knows a lot about. “I’m drawn to form. Plastic surgery marries art and form,” he adds. Dr. Bindingnavele has been practicing plastic surgery for more than eight years. He currently practices at the Corpus Christi Institute of Cosmetic and Plastic Surgery. He is able to provide procedures, such as body contouring, and surgery to the breast, face, elbow, hand and wrist. His practice also provides nonsurgical procedures, such as dermal fillers and skin rejuvenation. Prior to entering private practice, Dr. Bindingnavele served as a United States Air Force surgeon for 10 years.
58
MD Monthly
APRIL - 2017
He earned bachelor and medical degrees as part of a program at the Rensselaer Polytechnic Institute in New York, where he graduated summa cum laude. He was also a member of the Alpha Omega Alpha honor society.
I LOVE SEEING THE LOOKS OF JOY ON THEIR FACES IN RESPONSE TO THE RESULTS THEY GET. -Dr. Vijay Bindingnavele Dr. Bindingnavele entered the U.S. Air Force, where he finished his internship and residency training in general surgery at David Grant USAF Medical Center at Travis Air Force Base in California. Afterwards he was a general surgeon at Landstuhl Regional
Medical Center in Germany. He also was chief of surgery at 379 Expeditionary Medical Support Hospital in Qatar. Serving as an Air Force major and being an instructor for health-related courses worldwide, Dr. Bindingnavele has received several honors, including the Air Force Expeditionary Service Ribbon, National Defense Service Medal, Air Force Achievement Award, and Air Force Commendation Medal. “I liked the immediacy of general surgery,” Dr. Bindingnavele recalls, having treated whatever cases came before him, such as gunshot wounds. But as Dr. Bindingnavele explains it, general surgery treats function, not form, and he wanted to address that. Following his departure from the military, Dr. Bindingnavele completed a plastic surgery residency at the University of Southern California, Los Angeles. He is currently board-certified in general surgery and plastic surgery.
PHOTOGRAPHS BY Paul Marshall
MDMONTHLY.COM
He holds membership with the American College of Surgeons and the American Society of Plastic Surgeons. Dr. Bindingnavele has long had a passion for helping people improve their physical appearance and boost their self-confidence. Plastic surgery patients have a certain idea of what they wish to look like physically. But that desire also affects their perception of self. “Our job is to have the person looking back at them from the mirror match the ideal of the person looking into the mirror,” he says. Treating every patient that comes into his practice like a family member is critical to a successful outcome, Dr. Bindingnavele says, regardless of whether that person winds up receiving surgery. “Everybody has a choice about whether to get surgery,” he says. “They are able to trust me because I treat them like they’re part of my family.” Dr. Bindingnavele says this level of mutual trust is important especially when the patient is considering reconstructive surgery following a traumatic event or a bout with breast or facial cancer. The conversations prior to any such procedure are filled with equal levels of information and empathy. “I love seeing the looks of joy on their faces in response to the results they get,” he says. In his line of work, Dr. Bindingnavele has seen an uptick in body contouring which typically involves any of the following: brachioplasty (arm-lift surgery), buttock augmentation (lift), liposuction, fat transfer thigh lift, or tummy tuck.
So-called “mommy makeovers” are another type of procedure that Dr. Bindingnavele gets to offer in his practice. Dr. Bindingnavele takes particular pride in conducting “mommy makeovers.” In some cases, mommy makeovers involve a combination of liposuction, abdominoplasty and other enhancements, such as breast augmentation. “We are returning (her body) to the appearance of a younger lady, before she had kids,” he says. “A patient can feel more youthful, athletic–sexier. It evokes very good feelings.” Additionally, Dr. Bindingnavele emphasizes the importance of preventative care to boost and maintain one’s physical appearance. “The basic cornerstone of prevention is better maintenance,” he says. “Prevention is the way to go to try to fight off every illness.” While breast cancer may not be prevented, Dr. Bindingnavele says a good diet, exercising and maintaining an adequate weight can help to reduce the cancer risk.
Dr. Bindingnavele many accolades in recent years. The organization Corpus Christi Under 40 named him one of the “40 Under 40” leaders in the community in 2011. The following year, the same program named him Person of the Year. Dr. Bindingnavele has also served as president of the Nueces County Medical Society. Actively involved with the medical society, he has been on several committees. In addition, Dr. Bindingnavele donates his services to area organizations. He and his wife, Pooja, have four daughters, ranging in age from six to twelve. He has nothing but pride in his practice and his chosen profession. “The reason we are here is for the patients who walk through the door. I enjoy matching their external image with their desired self-image,” he adds.
Protecting one’s skin in the sunlight, as well as limiting exposure to more polluted areas also can help lower the risk of developing skin cancer. “Until we change our nature, we have to optimize how we live,” he says. Having a generally positive outlook on life and keeping stress at bay can also benefit one’s physical appearance. Dr. Bindingnavele recalls how he gave yoga lessons to pilots while serving in the Air Force. This kind of professionalism, compassion and attention have won
2017 - APRIL MD Monthly
59
RESEARCH & INNOVATION/SAN ANTONIO
INVOCell:
BREAKTHROUGH TECHNOLOGY FOR AN
AFFORDABLE FERTILITY SOLUTION By Francisco Arredondo, MD MPH
L
ouise Brown, the world’s first test-tube baby, was born in July, 1978. Since then, countless efforts have been made to mimic, in a laboratory setting, the ideal environment present in the female’s uterus for effective egg and sperm fertilization. In the last 40 years the success rates to achieve a live birth with in vitro fertilization have increased from 1 in 12 to approximately 1 in 2 attempts. There is no debating that the science of fertility has come a long way— ultimately improving a woman’s odds to conceive and make the dream of a family a magnificent reality.
60
MD Monthly
Unfortunately, fertility doctors, scientists, and the in vitro fertilization industry of today have not been able to make these services affordable to many. The price tag is substantial: investments for the in vitro fertilization cycle range from $12,000 to $20,000 dollars per cycle performed. The access to fertility care is in nowhere near where it should be in the United States, let alone in other less-privileged countries. Of 100 women that need IVF, approximately only 15 are capable of pursuing such treatment. The majority of women who fail to receive adequate fertility care are burdened by financial constraints and cannot afford it.
Fortunately for these women their luck is about to change, thanks to the efforts of French specialist Claude Ranoux and his invention, INVOCell™. The technology associated with INVOCell™ though not a do-ityourself kind of deal is substantially more accessible to patients; and it is estimated that the cost for many candidates will drop by as much as 50-70% from the original price. Rather than relying on expensive and sophisticated machinery to attempt to replicate a woman’s corporal conditions, INVOCell™ allows the patient to act as her own incubator— essentially transforming the woman into her own laboratory and
APRIL - 2017
MDMONTHLY.COM
RESEARCH & INNOVATION/SAN ANTONIO
capitalizing on the fact that she has the right environmental conditions. INVOCell™ is a clever gadget; cylindrical in shape, about 1.5 inches long and 1 inch in diameter, and made of gas permeable polystyrene. It has two concentric chambers, thus preventing the bacteria from reaching the gametes in the inner chamber. The FDA has approved the device and several trials have already confirmed its safety. The new in vivo fertilization process, which we have termed S.M.A.R.T. IVF™, (Simple Mindful Affordable Reproductive Technology), allows us to reduce the total cost of the process by more than half the original price: 75% less cost in medication, 80% less in blood draws, and 50% less in monitoring.
us to mature and obtain anywhere between 4 and 10 eggs while the patient is under sedation. We then use the INVOCell device as the place where the sperm and egg meet. There is no discomfort whatsoever once the device is placed inside the patient. Finally, after a few days, we remove the device and identify the best embryo to transfer inside the uterus. We then wait 11 more days to test for pregnancy. Our experience at Reproductive Medicine Associates (RMA) of Texas and SMART IVF has yielded the same encouraging results as FDA studies have. For the correct patients, the clinical pregnancy rate (fetal heart rate present at 7 weeks) is around 55% after the first attempt. For example, patients that have had previous tubal ligation and are looking to have a cumbersome and expensive surgery to connect back their tubes now can use INVOCell™ in a more simple and inexpensive manner. While not every couple is a candidate
for this innovative system, and in vitro fertilization will continue to be the gold standard of difficult cases, many scientists are very excited about the countless opportunities for providing the marvel of parenthood to couples who were previously unable to afford it. INVOCell™ is certainly the right step towards democratizing fertility treatments and realizing the dream of having a family.
Francisco Arredondo, MD MPH, is the founder RMA of Texas and SMART IVF For More information visit RMATX.com or SMARTIVF.com
In vitro fertilization can be divided into 3 steps: 1. Egg collection 2. Fertilization 3. Embryo transfer. During a S.M.A.R.T. IVF cycle we perform a very gentle egg stimulation with medications such as Clomid and FSH (folliclestimulating hormone) that allow
2017 - APRIL MD Monthly
61
We hold ourselves to a very high standard of performance. We prize innovative ideas and the teamwork it takes to make them realities. We never stop asking ourselves how we can make the patient experience better, and every day, we find an answer.
THE PREMIER PRIMARY HEALTH CARE SYSTEM OF CHOICE.
We accept most private insurances, Medicaid/CHIP, and Medicare. Self-pay patients are welcomed. Now accepting new patients.
CommuniCare Health Centers is a full-service primary healthcare system serving in Bexar, Kendall and Hays counties. We offer an array of services and deliver our care through multiple clinic locations utilizing integrative primary care practices, highly trained healthcare providers, state of the art diagnostic equipment, and electronic health records.
• Family Medicine • Pediatrics • Women’s Health • WIC Services
• Dental for Children & • Vision Care services Adults are offered by UIW • Behavioral Health Rosenberg School of • Minor Surgery Optometry
4ALL4LIFE.ORG
Contact Phone: San Antonio- (210) 233-7000 Hays County- (512) 268-8900 Boerne - (830) 249-1717
LOSE WEIGHT, NOT HOPE GOOD-BYE DIABETES GOOD-BYE SLEEP APNEA HELLO WEIGHT LOSS
Benefits of Weight Loss Surgery •
WLS may improve obesity related health conditions such as diabetes, heart disease, high blood pressure, and obstructive sleep apnea, among others.
•
Diabetes cured in 80% of patients and resolved or improved in 90% of patients.
•
Hypertension is cured in 62% of patients and resolved or improved in 78.5%
•
Obstructive sleep apnea is cured in 86% of patients
•
Risk of death is decreased by 89%
•
Weight Loss Surgery (WLS) can enhance fertility and lead to successful full term pregnancies
•
Average weight loss is 50-70% of excess body weight
•
Improvement in arthritis with reduction in pain and increased mobility.
•
WLS is covered by 80% of insurances
•
Texas Bariatric Specialists accepts most major insurances including Medicare.
Nilesh A. Patel, MD, FACS
Subhash Reddy, MD
Leah A. Dill, D.O.
BypassDoc.com | 877.459.7065 San Antonio | Austin | Corpus Christi | San Angelo Kileen | New Braunfels | Del Rio | Laredo