The Evolution of AMD Therapies






The Sciences and Arts of Ophthalmology was the theme of APAO 2019, which was held in the city of smiles — Bangkok, Thailand — on March 6-9, 2019. That was the last physical conference that APAO had, and we (Media MICE and PIE/CAKE magazines) were the official media partner.
By the first quarter of 2020, the world stood still, err… was locked down. And then in 2021, APAO held its first-ever virtual event — APAO 2021, and then collaborated with the World Ophthalmology Congress (WOC) for the virtual WOC 2022.




This year, APAO is coming back stronger than ever as a full face-to-face conference — the 38th Asia-Pacific Academy of Ophthalmology Congress (APAO 2023) is happening in Kuala Lumpur, Malaysia, on February 23-26 at the highly acclaimed Kuala Lumpur Convention Centre (KLCC), next to the iconic and worldfamous Petronas Twin Towers. The theme, Reconnect and Collaborate is surely fitting as we all emerge from the pandemic of recent years. Indeed, it is time to reconnect once more.
In the words of APAO 2023 Congress President, Immediate Past President of the Malaysian Society of Ophthalmology, PIE magazine Advisory Board Member, our dear friend, Dr. Ken Fong, “Malaysia opened its international borders on 1 April 2022 and is committed to hosting our international delegates in a safe and conducive matter with focus on ensuring the biological safety of our visitors. APAO promises to be an academically stimulating conference with lots of exciting social events and local tourism attractions for you and your families.”
Our huge congratulations to Dr. Ken Fong and APAO 2023! The Media MICE team, together with our ophthalmic magazines — PIE and CAKE — are happy to be back as your official media partner. We cannot wait to bring the APAO Show Daily (the official congress news of APAO 2023), and the first quarter issues of PIE and CAKE magazines on the show floor… literally.

Jumpa lagi, APAO!
Best regards,
 Gloria D. Gamat Chief Editor, Media MICE PIE, CAKE and COOKIE magazines
Gloria D. Gamat Chief Editor, Media MICE PIE, CAKE and COOKIE magazines






Dr. Alay S. Banker
Banker’s Retina Clinic and Laser Centre
Ahmedabad, India
alay.banker@gmail.com
Prof. Gemmy Cheung

Singapore National Eye Centre (SNEC) Singapore
gemmy.cheung.c.m@singhealth.com.sg
Dr. Hudson Nakamura
Bank of Goias Eye Foundation
Goiânia, Brazil
hudson.nakamura@gmail.com
Dr. Kenneth Fong

OasisEye Specialists
Kuala Lumpur, Malaysia
kcsfong@gmail.com
Prof. Mark Gillies

University of Sydney Sydney, Australia
mark.gillies@sydney.edu.au
Dr. Saad Waheeb

King Faisal Specialist Hospital & Research Centre, Riyadh, Saudi Arabia
saadwaheeb@hotmail.com
Asia-Pacific Vitreo-retina Society
Orbis Singapore


Subthreshold Ophthalmic Laser Society
ASEAN Ophthalmology Society Arunodaya Charitable Trust (ACT)

Retinawesome Retina & Vitreous International

Vitreo-Retinal Society - India




Asia-Pacific Academy of Ophthalmology
He Eye Specialist Hospital Ophthalmology Innovation Summit

Russian Ophthalmology Society (ROS)

Young Ophthalmologists Society of India ( YOSI )



World Ophthalmology Congress

Age-related macular degeneration (AMD) and diabetic macular edema (DME) are heterogenous diseases that require an individualized treatment approach. In a recent Cybersight webinar, Dr. Arghavan Almony from North Carolina, USA, looked into novel and upcoming therapies that promise to reduce treatment burden for these diseases.
Macular degeneration is the leading cause of severe and irreversible visual loss worldwide, affecting about 8.7% of the global population. “The disease has a profound effect on the quality of life of not only the affected individuals but their loved ones as

well. It represents a major socioeconomic challenge for societies, due to the exponential increase in life expectancy, as well as environmental risks,” shared Dr. Almony.
Meanwhile, DME affects about 21 million people worldwide, and advanced diabetic retinopathy (DR) is a significant risk factor for sustained blindness, she added.
According to Dr. Almony, there’s currently no treatment for dry macular degeneration, and prevention is recommended. The latter includes self-monitoring, eating
a nutrient-dense diet, taking agerelated eye disease study (AREDS2) vitamins, smoking cessation, and having regular eye exams.
As for wet macular degeneration, anti-vascular endothelial growth factor (anti-VEGF) injections are the gold standard. “Since macular degeneration is a heterogeneous disease, it requires an individualized approach. We know that 10% to 20% of patients require injections every four weeks, and another 10% to 20% require injections every 10 to 12 weeks. Others fall in between those two groups,” she shared.

And as for DME, there are multiple treatment options, which include anti-VEGF injections, laser photocoagulation, corticosteroids, and pars plana vitrectomy in certain cases.
Even though intravitreal anti-VEGF therapies are the go-to treatments for both neovascular AMD (nAMD) and DME, they bring about a significant treatment burden.
“The burden of disease has turned into a burden of care,” shared Dr. Almony. “We know that anti-VEGFs are effective in reducing macular edema, reducing neovascularization, and ultimately improving or stabilizing sight.”
Unfortunately, frequent intravitreal injections are a burden for patients and their caregivers. Appointments for monitoring and injections are regular events that patients plan their lives around. Collectively, anti-VEGF therapy creates financial strain for both patients and caregivers.
“While AMD patients are usually retired and rely on caregivers to transport them for clinic visits, DME patients are typically working fulltime and have to take time off their jobs in order to receive treatment,” said Dr. Almony.
She shared that a study done on 75 patients with nAMD found that the mean time per visit, including preparation, travel, waiting, treatment, and recovery time from the injections, was almost 12 hours per patient.
“We also know that real-world experiences have been different compared with clinical trials,” she continued. “Real-world patients with nAMD or DME have been found to receive fewer injections and experience worse visual outcomes compared to [those in] clinical trials. Older patients and patients with poor baseline visual acuity are more likely to be under-treated.”
“Hence, the need for longer-lasting therapies is definitely at the top of the list. We also want new drug pathways beyond anti-VEGF, as well as non-invasive therapies,” she said, referring to the American Society of Retina Specialists PAT Survey 2021 on the greatest unmet needs regarding wet AMD treatment.

Thankfully, promising novel therapies are on the horizon, offering hope for reducing treatment burden. Firstly is the dual-targeted therapy that targets multiple underlying causes of DME and nAMD by combining two medications, noted Dr. Almony.
The dual-targeted therapy has the potential benefits of improved visual and anatomic outcomes, fewer injections and office visits, reduced anxiety and depression, and increased productivity.
“Faricimab (VABYSMO) is the latest drug available under this dual mechanism segment. The Faricimab molecule has an arm that binds to Ang-2 to reduce inflammation and vascular leakage, and another arm that binds to VEGF-A, inhibiting vascular leakage and neovascularization at the same time,” explained Dr. Almony. “It also has an inactivated region that is engineered to reduce systemic exposure and inflammatory potential. Through a novel mechanism of action, it is designed to stabilize blood vessels and reduce inflammation and leakage more than either pathway alone” she noted, adding that faricimab is the first bispecific immunoglobulinbased antibody designed for the eye approved by the US Food and Drug Administration (FDA) in October 2021.
Further, Dr. Almony mentioned
that clinical trials have looked at the safety, durability, and efficacy of faricimab for nAMD and DME.
“The TENAYA and LUCERNE trials compared faricimab with aflibercept in about 1,300 patients with AMD and found that faricimab has non-inferior vision gains to aflibercept at week 48. More than 50% of faricimab patients were treated every 16 weeks, rather than every eight weeks. And more than 75% of faricimab patients were treated every 12 weeks, rather than eight weeks. Faricimab seems to be a direct answer to the need for longerlasting therapies,” she shared.
“It is generally well-tolerated, with no new safety signals. And what’s really important is that faricimab is the first new class of medications that is effective for wet AMD in over 15 years,” Dr. Almony added.
Similar trials were performed for DME — the YOSEMITE and RHINE trials. “Again, we saw non-inferior vision gains when compared with aflibercept. More than 50% of faricimab patients were treated every 16 weeks versus every eight weeks with aflibercept. This was the first investigational drug to achieve this level of durability, which is very exciting for our patients,” she said.
When using VABYSMO for nAMD, Dr. Almony advised physicians to start with four monthly loading doses, followed by Q4 to Q16 weekly dosing, depending on the patient’s optical coherence tomography (OCT) result and visual acuity.
For diabetic macular edema, there are two options. Physicians can begin with four monthly loading doses or six monthly loading doses, followed by incremental extension or reduction, or intervals of every eight weeks.
She also mentioned that there is an upcoming inhibitor of VEGF-C and VEGF-D in the form of combination drug OPT-302. It is not yet available and studies are ongoing.
Meanwhile, the newest options in the US for wet AMD and DME are biosimilars, products that are highly similar (but not identical) to the
originator biologic (an FDA-approved product). These products have actually been available in other parts of the world for seven to eight years. Dr. Almony noted that the number of biosimilars across different medical specialties is increasing. There are now a total of 30 FDA-approved biosimilars representing 10 distinct reference products.
“The first ranibizumab biosimilar entered the US market this year. And the first aflibercept biosimilar is expected to enter the market in 2024,” she said.
An interesting drug currently under development as an investigational ophthalmic formulation of bevacizumab is Lytenava. If approved, it will be the first and only FDA-approved, on-label bevacizumab approved for the treatment of wet AMD and potentially for DME.
In addition, a number of molecules are under investigation for the treatment of geographic atrophy (GA), such as avacincaptad pegol, which prevents the proinflammatory effects of C5a and cell lysis and damage on RPE cells by MAC (C5b9). The GATHER1 trial found that the GA growth rate was reduced by about 27% when avacincaptad pegol 2 mg was used compared to sham, and 28% when 4 mg was used.
Last but not least, there is the SUSVIMO (ranibizumab injection), a refillable intraocular implant at the pars plana for the customization of ranibizumab treatment. Refillexchange procedures are performed in the office approximately every six months. However, there are concerns about septum dislodgement, and the product had undergone voluntary recall in October 2022.
The Cybersight webinar, The Therapeutic Pipeline for AgeRelated Macular Degeneration and Diabetic Macular Edema: Where Do We Stand and Where Are We Headed? by Dr. Arghavan Almony, was held on December 9, 2022. Reporting for this story took place during the event.
June 21 Registration and hotel reservations open to Academy and AAOE® members
July 12 Registration and hotel reservations open to nonmembers

August 16 Early registration fee deadline
October 4 Advance pricing fee deadline Submit
March 9 Submissions open
April 11 Deadline aao.org/2023

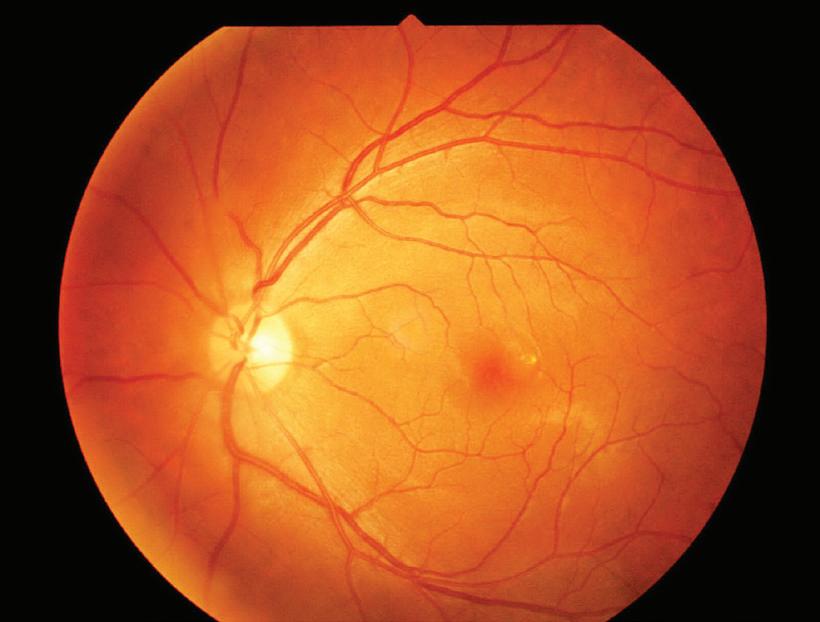
Biomarkers are medical signs that indicate the state of health and wellbeing of an individual objectively. OCT biomarkers help us predict visual acuity (VA) outcomes and treatment response. They play a significant role in patients with AMD by determining progression to advanced AMD, conversion of dry AMD to nAMD, and predicting treatment outcomes and visual prognosis. 1 OCT biomarkers can either be structural (retinal, choroidal, and vitreomacular interface) or based on fluid distribution.
by Dr. Sashwanthi Mohan and Dr. Arthi MohankumarAge-related macular degeneration (AMD) is a chronic degenerative condition of the macula and a leading cause of central visual loss worldwide. It is divided into dry and wet AMD or neovascular AMD (nAMD). Optical coherence tomography (OCT) is the most used investigative modality for diagnosis, follow-up, tracking progression, and monitoring treatment of patients with AMD, especially nAMD.
Central retinal thickness (CRT) is one of the first and most common OCT biomarkers for this. However, studies have revealed that CRT alone does not predict visual function well and that certain other biomarkers have better prognostic value.

Higher drusen volume is associated with an increased risk of progression to nAMD or geographic atrophy (GA).
The height of drusen is associated with a risk of late atrophic AMD, and the length of drusen is associated with conversion to nAMD.2 OCTreflective drusen substructures (ODS) in eyes with intermediate AMD are associated with a 5.6 risk of progression to GA and not nAMD. Drusen with subretinal fluid (SRF) may represent subclinical choroidal neovascularisation (CNV). Heterogeneous internal reflectivity material within drusen (HIRD) contains hydroxyapatite, an indicator of progression to advanced AMD. Drusenoid PED greater than 2 DD presenting with metamorphopsia have a high risk of progression to GA or nAMD after two years.
Reticular pseudodrusen or subretinal drusenoid deposits (SDD) are located above the retinal pigment epithelium (RPE) and found in the superior macula in 9% to 58% of AMD eyes. Their presence is associated with a two- to six-fold increase in the risk of
nAMD or central GA. SDDs located outside the macula are at a higher risk for progression.

Hyperreflective foci (HRF) are lesions within the retina that can either be found adjacent to the drusen apex or edge in the inner retina. They are strong predictors of AMD progression, with a five-fold high risk of progression to GA at two years. The inner location and cluster distribution of HRF are associated with the development of nAMD.3 HRF on OCT at baseline has a five-times higher risk of progression to GA at two years. In nAMD, HRF regression after anti-VEGF treatment is of good prognostic value for VA.
Outer retinal tubulations (ORTs) are ovoid or round hyporeflective lesions with hyperreflective borders at the outer nuclear layer and reflect photoreceptor rearrangement after
retinal injury. They are usually present in advanced AMD and are associated with GA or nAMD. The presence of ORTs has been associated with poorer vision in nAMD patients.
Subretinal hyperreflective material (SHRM) can be fluid, fibrin, scar, blood, or neovascularization. Its presence is associated with worse visual acuity. Subfoveal SHRM with increased height and width is associated with worse visual acuity.
Retinal pigment epithelium (RPE) rips are a complication of nAMD which occur in eyes with pigment epithelial detachments (PEDs); either spontaneously or secondary to laser or anti-VEGF therapy. They are associated with poor visual prognosis, especially if there is involvement of the fovea.
Abnormal RPE thinning can be associated with the development of atrophic AMD and also signifies the progression of GA when present at its margins. Incomplete retinal pigment epithelial and outer retinal atrophy, or iRora, is loss of outer plexiform and inner nuclear layer forming a hyporeflective wedge and is strongly associated with impending GA. Complete RPE and outer retinal atrophy — cRORA — is the end point of atrophy in the presence of drusen with diameters of 250 mm.
The ellipsoid zone (EZ) refers to the photoreceptor inner segment/ outer segment (IS/OS) junction on OCT. Disruption of the EZ is said to be associated with progression to advanced AMD — both GA and nAMD. Focal disruption of the RPE, RPE thickening, and irregularities of the retina or external limiting membrane (ELM) are other OCT features that are associated with progression to advanced AMD.

Hyperreflective columns under the RPE defects are associated with progression to nAMD or GA by three months. These defects affect the integrity of the RPE and allow the growth of new vessels into the subretinal space.
A higher number of intravitreal anti-VEGF injections is required to manage nAMD in patients with vitreomacular interface abnormalities, but there is no association with VA.
Choroidal thickness measurements below drusen of <135 µm suggest progression to GA. The choroidal thickness was found to have no prognostic value on VA. Early presentation of prechoroidal clefts can have a poor prognosis due to complications, such as RPE rips or hemorrhage. Choroidal caverns do not have any prognostic value.
Neovascular lesions on OCT in the absence of fluid are present in 6.25% to 27% of the fellow eyes of nAMD. They are at risk of progression to exudative AMD at one year.4
Intraretinal fluid in the form of intraretinal cystoid spaces (IRC) (white asterisk in image), correlates with poor VA. It is an important negative biomarker in AMD with an increased risk of development of fibrosis or atrophy and loss of vision. The presence of IRC correlates with poorer visual improvement after anti-VEGF therapy. Whereas, subretinal fluid (SRF) (yellow asterisk in image), if chronic, is said to have a protective effect on VA by protecting photoreceptors from toxic effects of the underlying diseased RPE. The sub-RPE fluid (red asterisk in image) does seem to affect VA prognosis unless associated with IRC or SRF.
A thick, double-layer sign (DLS), intraretinal HRF, or exudative macular neovascularization (MNV) in the fellow eye is at higher risk of conversion.5 These OCT signs help identify patients who require
1. Metrangolo C, Donati S, Mazzola M, et al. OCT Biomarkers in Neovascular Age-Related Macular Degeneration: A Narrative Review. J Ophthalmol. 2021;2021:9994098.
2. Flores R, Carneiro Â, Tenreiro S, Seabra MC. Retinal Progression Biomarkers of Early and Intermediate Age-Related Macular Degeneration. Life (Basel). 2021;12(1):36.
3. Phadikar P, Saxena S, Ruia S, Lai TY, Meyer CH, Eliott D. The potential of spectral domain optical coherence tomography imaging based retinal biomarkers. Int J Retina Vitreous. 2017;3:1.
4. Wakatsuki Y, Hirabayashi K, Yu HJ, et al. Optical Coherence Tomography Biomarkers for Conversion to Exudative Neovascular Age-related Macular Degeneration. Am J Ophthalmol. 2022;247:137-144.
5. Damian I, Nicoară SD. SD-OCT Biomarkers and the Current Status of Artificial Intelligence in Predicting Progression from Intermediate to Advanced AMD. Life (Basel). 2022;12(3):454.
frequent monitoring and early treatment.
Dr. Sashwanthi Mohan is a specialist ophthalmologist and vitreoretinal specialist at Medcare Eye Centre, Dubai. She completed her DNB Ophthalmology from L.V. Prasad Eye Institute in Hyderabad, India, and was awarded the Dr. G. Venkataswamy Gold Medal for Ophthalmology by the National Board of Examinations, followed by a vitreoretinal fellowship from Sankara Nethralaya, Chennai, where she was awarded as the best outgoing vitreoretinal fellow. She has a keen interest in research and has many peer-reviewed publications to her name. She is also interested in education and has an educational website called Ophthalmobytes. She is a fellow of the international council of Ophthalmology (FICO) and a member of the Royal College of Surgeons, Edinburgh (MRCS).

sashu23@gmail.com
Dr. Arthi Mohankumar is a vitreoretinal surgeon at Rajan Ye Care Hospital, Chennai, India. She has completed her MS in ophthalmology from the Regional Institute of Ophthalmology, Madras Medical College, Chennai, India, and completed her training in medical and surgical retina training at Aravind Eye Hospital, Pondicherry, India. She has a keen interest in research and has multiple peer-reviewed publications in indexed journals. Her areas of interest include diabetic retinopathy, retinopathy of prematurity, and ocular inflammation.
Thus, several OCT features can serve as important biomarkers in tracking progression, conversion, and monitoring response to treatment in patients with AMD. OCT is an important tool that can help the clinician plan an individualized approach for AMD patients. drarthimohankumar@gmail.com















Hong Kong Convention and Exhibition Centre 1 5 - 1 7 D e c , 2 0 2 3















The 16th Asia-Pacific Vitreo-retina Society (APVRS) Congress












From anti-VEGF to home OCT — the quest for the most promising AMD treatment is on
 by April Ingram
by April Ingram
Although 2005 may not seem like ancient history — the first iPhone wasn’t available until 2007 — if you were diagnosed with neovascular (wet) age-related macular degeneration (AMD) before then, your prognosis was dismal.
The best available treatment at the time was photodynamic therapy, which, despite best efforts, resulted in the majority of eyes declining to visual acuity of 20/200 or poorer within the first year. Late 2004 saw the approval, and subsequent short lifespan, of intravitreal pegaptanib sodium. And in 2005, Philip Rosenfeld wowed the crowd at the 109th Annual Meeting of the American Academy of Ophthalmology in Chicago, discussing AMD treatment with intravitreal bevacizumab. In a 2006 issue of the New England Journal of Medicine, Rosenfeld and investigators had us all jumping on the nautical-themed (MARINA, HARBOR, ANCHOR) ranibizumab train — and then we were full speed ahead to antivascular endothelial growth factor (anti-VEGF) land.
For years, ranibizumab (LUCENTIS®) held its place of glory on the wet AMD landscape, with, of course, its bevacizumab (Avastin®) cousin stealing a little off-label thunder.
Fast forward to 2011, when aflibercept (Eylea®) entered the scene, and there we had our pillars of anti-VEGF treatment.
As we know in all subspecialties of ophthalmology, specifically in retina, we are forever on a quest for more effective, safer, and durable ways to treat our patients.
So, let’s fast forward to current times — when you may be reading this on an iPhone 14, Pro, or Max — and take a look at the ways we are diagnosing and treating AMD and the novel advancements on the horizon. Retina practices are always buzzing with patients, and there seems to be no shortage of ongoing clinical trials.
Two highly sought-after investigators that are at the forefront of recently approved AMD treatments and novel pipeline therapies are Dr. Christina Y. Weng — professor of ophthalmology
and the Vitreoretinal Diseases and Surgery Fellowship Program director at the Baylor College of Medicine, and Dr. Charles C. Wykoff — director of research at Retina Consultants of Texas, chairman of research at Retina Consultants of America, and deputy chair of ophthalmology for the Blanton Eye Institute, Houston Methodist Hospital, both in Houston, Texas, USA.
We had a chance to ask Dr. Weng and Dr. Wykoff about the evolution of AMD treatments and what novel therapies they are most excited about that may be coming soon to a clinic near you.
“The current generation anti-VEGF pharmacotherapies aflibercept and ranibizumab, as well as the dual VEGF and ANG2 inhibitor faricimab, are excellent for managing exudative retinal diseases including neovascular AMD,” Dr. Wykoff shared some of the currently available treatments in the US.
He added that a higher dose of a familiar face is also making waves. “Most recently, high-dose aflibercept, 8 mg, has demonstrated improved durability in trials with a potential label update anticipated for later this year,” Dr. Wykoff shared.
Dr. Weng agreed that the durability of high-dose aflibercept has been impressive. “It may allow patients to be treated as infrequently as every 16 weeks with no new safety signals observed.” [Editor’s Note: You can read more about the high-dose Eylea treatment regimen in PIE magazine’s issue 24X.]
Of all the data being released, and new molecules and devices being evaluated in the AMD space, we wanted to know if there were certain candidates, in addition to high-dose aflibercept, that Dr. Weng is excited
about or watching carefully.
“It’s honestly impossible to pick just one — what excites me the most is that there are so many promising therapeutics being investigated in parallel,” she explained. “Anything that can further elevate the high bar that has been set, whether it’s better efficacy or longer durability, will be a welcome addition to our toolboxes.”
Dr. Weng highlighted a few treatments that are on her watchlist. “I am fascinated by gene therapies, such as RGX-314 and ADVM-022, because they may be able to significantly reduce the treatment burden that challenges so many of our patients,” she continued. “However, their safety needs to be confirmed across larger-scale trials.”
Dr. Wykoff explained the mechanism of these gene therapy options.
“Gene therapies work by creating an intraocular biofactory to produce an anti-VEGF protein,” he said.
“RGX-314 is the most advanced in development, currently enrolling in two phase 3 trials; ADVM-022 and 4D-150 are both intravitreally delivered gene therapies in earlier stages of development.”
RGX-314 is being investigated by REGENXBIO (Maryland, USA) in collaboration with AbbVie (Illinois, USA), as a potential one-time treatment for wet AMD, diabetic retinopathy, and other chronic retinal conditions. RGX-314 gene therapy includes the NAV AAV8 vector containing a gene encoding for a monoclonal antibody fragment designed to inhibit VEGF.
ADVM-022 is Adverum Biotechnologies’ (California, USA) gene therapy product, an AAV vector encoding aflibercept. 4D-150 from 4D Molecular Therapeutics (California, USA) is a dual-transgene, intravitreal gene therapy designed to inhibit four distinct angiogenic factors.
“The current generation anti-VEGF pharmacotherapies aflibercept and ranibizumab, as well as the dual VEGF and ANG2 inhibitor faricimab, are excellent for managing exudative retinal diseases including neovascular AMD.”
— Dr. Charles C. Wykoff
Further, Dr. Weng shared her thoughts on OPT-302, an anti-VEGFC/-D being evaluated by Opthea (York, Canada) used as a combination treatment with anti-VEGF-A agents. “OPT-302 has a unique mechanism in its inhibition of VEGF-C and VEGF-D, which can be upregulated by blockade of VEGF-A. When OPT302 was used in combination with ranibizumab in a phase 2 study, patients had superior visual acuity outcomes compared to those who received ranibizumab alone,” she explained. “I look forward to seeing what the ongoing phase 3 trials will show.”
Dr. Wykoff agreed and is excited about what may be the next tool, or combination of tools, to be added to the retinal toolbox. “Looking ahead, next-generation treatments hold substantial promise to move our field forward,” he noted. “For example, OPT-302 inhibits VEGF-C and VEGF-D and in combination with antiVEGF-A therapies is being studied in the two global phase 3 randomized trials, COAST and SHORE. In the preceding phase 2 trial, the addition of OPT-302 to monthly ranibizumab treatment increased visual gain by about 5 letters, underscoring the potential for improved visual outcomes for patients beyond what is achievable with current agents,” he added.
Novel mechanisms of action and more durable treatment options always draw the attention of the AMD crowd. Durability is a hot topic, as it is no secret that patient compliance with frequent intravitreal injections remains a challenge.
(Massachusetts, USA) is conducting trials of EYP-1901, a sustained delivery anti-VEGF (vorolanib) tyrosine kinase inhibitor (TKI), in bioerodible Durasert®. Ocular Therapeutix (Massachusetts, USA) is also in the anti-angiogenic TKI space with OTX-TKI, an investigational bioresorbable, hydrogel implant incorporating axitinib. Clearside Biomedical (Georgia, USA) is also using a proprietary suspension of axitinib, CLS-AX, delivered via their suprachoroidal microinjector.
Dr. Wykoff shared the big potential
of these TKI in AMD. “Given that these small molecule inhibitors block signaling through multiple transmembrane receptor tyrosine kinases, it is possible that they may have additional benefits beyond simple fluid reduction as well, such as being anti-fibrosis,” he shared.
Dr. Weng explained why these two have caught her interest. “For similar reasons [unique mechanisms], I am also intrigued by TKIs, such as EYP-1901 and OTX-TKI, which work intracellularly and bind to domains of receptors like VEGFR and PDGRF to inhibit angiogenic activation pathways more broadly. The durability of these agents is on the scale of six to nine months, which could meaningfully alleviate the treatment burden for many,” she discussed.
Dry AMD remains a hot topic and a tremendous unmet need. But it looks like some hope for patients may be coming soon. “From a dry AMD perspective, we appear to be on the threshold of having access to therapeutics that can slow the progression of geographic atrophy (GA),” Dr. Wykoff explained.
“Pegcetacoplan has a pending PDUFA date of February 26th, and avacincaptad pegol is under FDA review. The introduction of one or both of these medications into the retina landscape would be a meaningful step forward as this progressive, blinding, irreversible disease process has no treatment options currently,” he added.
Taking things one step further, why stop at slowing progression when there may be opportunities to treat geographic atrophy? Annexon Inc. (California, USA) plans to share top line data from their phase 2 ARCHER trial evaluating its anti-C1q candidate, ANX007, in the first half of 2023. And ONL Therapeutics (Michigan, USA) is evaluating ONL1204, a novel, first-
in-class small molecule fatty acid synthase (FAS) inhibitor designed to protect key retinal cells, including photoreceptors, from cell death.
The ‘one and done’ strategy is also being studied in eyes with geographic atrophy. Gyroscope Therapeutics (a Novartis company) is investigating a gene therapy (GT005) for geographic atrophy, and Regenerative Patch Technologies (California, USA) has demonstrated safety and efficacy of their subretinally delivered CPCB-RPE1 (human embryonic stem cell-derived retinal pigment epithelial cells seeded on a polymeric substrate) in an early phase trial.
Dr. Wykoff is intrigued by the possibility of pipeline treatments for advanced, dry AMD. “Additional complement modulators under study are also fascinating, including ANX007, which has the potential for neuro-enhancement,” he said. “Finally, next-generation GA treatments including gene therapies, such as GT005, are under development, as well as noncomplement targeting molecules such as ONL1204, which inhibits cell death.”
In this arena of intravitreal, subretinal, and suprachoroidal AMD treatments, let’s not forget a new device that is a game changer in the management paradigm — home optical coherence tomography (OCT). Providing patients the opportunity to conduct OCTs at home may facilitate highly personalized retreatment decisions, with fewer unnecessary injections and clinic visits.
The Notal Home OCT from Notal Vision (Tel Aviv, USA) could significantly impact the way we manage our AMD patients, said Dr. Weng. “It is a small, portable device that patients can self-operate from the comforts of their own home. Leveraging a proprietary artificial-
“It can be easy for us to get lost in the weeds of molecules and data points galore. But at the end of the day, preserving patients’ ability to do the things they love is the common goal we all share.”
— Dr. Christina Y. Weng
intelligence algorithm, it can detect subtle anatomical changes (that could indicate disease activity) and alert the treating physician,” she explained.
“The DRCR Retina Network is developing a protocol that will compare Home OCT-guided treatment versus a more standard treat-and-extend approach for wet AMD patients,” added Dr. Weng. “I suspect we will learn a tremendous amount from this upcoming clinical trial.”
We can conduct the trials and review the data, but it is important to remember that in addition to treating the eye with AMD, the decisions being made impact the patient as a whole, their quality of life, and very often the lives of their families.
Dr. Weng shared some vital advice, recognizing the importance of good communication and relationships with patients. “Always remember to look beyond the Snellen acuity chart hanging in your exam lane,” she advised. “In my early career, I have learned that while patients appreciate knowing their visual acuity, seeing their OCT images, and understanding their disease, what they care about most is being able to watch their granddaughter on stage at her dance recital, drive to the neighborhood grocery store without having to bother their children, and read for pleasure or livelihood,” she continued.
“It can be easy for us to get lost in the weeds of molecules and data points galore. But at the end of the day, preserving patients’ ability to do the things they love is the common goal we all share,” enthused Dr. Weng.
In addition to the wider range of treatment options currently available for AMD patients, Dr. Wykoff is looking forward to the direction that AMD treatment is headed and the opportunities that may soon be available. “It is a fascinating and exciting time in retina, and our patients have a brighter future than ever,” he said.
As more treatment options move closer to entering the clinical space — with different modes of delivery, safety profiles, and mechanisms of action, Dr. Weng offered some key advice to retina specialists. “Keep yourself up-to-date, and don’t get ‘stuck’ in your comfort zone. Wet AMD is a rapidly evolving area, and there will likely be many new therapeutics emerging over the next decade, some of which will inevitably
Dr. Christina Y. Weng , MD, MBA, is a professor of ophthalmology and the vitreoretinal diseases & surgery fellowship program director at the Baylor College of Medicine in Houston, Texas. She has a faculty appointment at the Level 1 trauma center, Ben Taub General Hospital. Dr. Weng was a prior recipient of the Dan B. Jones Teaching Award. She graduated cum laude from Northwestern University and then went on to medical school at the University of Michigan, where she was elected to the Alpha Omega Alpha (AOA) Medical Society. While in Ann Arbor, Dr. Weng pursued an MBA degree from the University of Michigan-Ross School of Business and graduated with high distinction. She completed her ophthalmology residency at the Wilmer Eye Institute-Johns Hopkins University and her surgical retina fellowship at the Bascom Palmer Eye Institute-University of Miami. Dr. Weng is involved with multiple clinical trials, including the DRCR. net diabetic retinopathy trials and the AGTC Phase 1/2 intravitreal gene therapy study for X-linked retinoschisis. She also leads numerous research studies in her areas of interest: clinical/surgical outcomes, medical economics, healthcare quality metrics, and telemedicine.

christina.weng@bcm.edu
Dr. Charles C. Wykoff , MD, PhD, is the director of research at Retina Consultants of Texas, chairman of research at Retina Consultants of America, and deputy chair of ophthalmology for the Blanton Eye Institute,

offer additional advantages over what our current agents do,” she shared.
She added that doing your own homework is key. “Evaluate each one critically for yourself, independent of outside influence. While always considering safety first, if the drug/ device appears promising, consider offering it to your patients who could benefit [from it],” Dr. Weng concluded.
Houston Methodist Hospital. He received his baccalaureate from MIT, PhD from Oxford University while on a Marshall Scholarship, and MD from Harvard Medical School. Dr. Wykoff completed his ophthalmology residency and vitreoretinal fellowship at Bascom Palmer Eye Institute where he served as Chief Resident/CoDirector of Ocular Trauma and received a Heed Fellowship and the Ronald G. Michels Award. He is an active medical and surgical retina specialist. Dr. Wykoff is passionate about translational research, clinical trial design, and accelerating drug-development programs. He has published over 250 peer-reviewed manuscripts, serves as principal investigator for dozens of clinical trials, and frequently speaks at national and international academic meetings. He serves on multiple scientific and medical advisory boards, safety monitoring committees, and global steering committees for endeavors spanning the innovative process from early to late-stage developments. He is the president of the Vit-Buckle Society (20212023), serves on the American Society of Retina Specialists Board of Directors, is a founding member of the Ophthalmology Retina Editorial Board, and is the chief medical editor for Retina Specialist . He has been awarded multiple Achievement, Honor and Senior Honor Awards, including the ASRS Young Investigator and the AAO Secretariat Awards. His guiding philosophy is to build and strengthen innovative, ethical teams focused on developing new approaches to improving outcomes for blinding diseases.
charleswykoff@gmail.com
Imaging lies at the heart of the detection, diagnosis and management of both vitreoretinal disease and glaucoma — and when sight is on the line, ophthalmologists turn to devices that deliver sharp snaps to boost outcomes. Thus, it’s no surprise that at the recent 15th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2022) in Taipei, all eyes were focused on Revolutionary in Fundus Imaging , a lunch symposium sponsored by Topcon Healthcare (Tokyo, Japan). During the one-hour talk, Drs. Tsukasa Hanemoto and Henry Shen-Lih Chen offered their perspective on how Topcon devices yield scans with such benefits they might just herald in a new era of diagnosis
and management of glaucoma and retinal disease.
An illuminating difference in slit scan fundus photography

With the various imaging devices available today, determining which system leads the pack in image quality and efficiency can be a difficult task for clinicians. To help separate the facts from the fluff, Dr. Tsukasa Hanemoto, director of Hanemoto Eye Clinic in Japan, shared his thoughts during his presentation, Clinical Benefit of New Slit Scanning Fundus Camera — Topcon NW500
At his private practice, Dr. Hanemoto
by Brooke Herronsees patients on both sides of the eye, with subspecialties in cataract, medical and surgical retina, as well as glaucoma. His talk zeroed in on the image quality of NW500, a nonmydriatic, robotic fundus camera. Using exclusive slit scan technology, the camera captures sharp and consistent images with a pupil size of 2.0 mm or more, regardless of miosis or lighting conditions — unlike conventional fundus cameras.
Dr. Hanemoto explained that Topcon’s NW500 beats out conventional fundus cameras thanks to its illumination: “NW500 uses two-zone lighting as opposed to conventional ring illumination. Since the upper and lower parts are separated and the outer diameter can be reduced, it is possible to illuminate
the fundus even through a 2.0 mm pupil.”
Another difference is the light source: Conventional fundus cameras use Xenon flash; NW500 uses Laser Excited Phosphor (LEP) + LED. Dr. Hanemoto said that the LEP light source has a broad spectrum and is very bright to help deliver high quality images in small pupils. It also improves imaging for patients with cataract or vitreous opacities: “The laser and LED light scanning has made it possible to decrease backscattering in lens opacities,” he explained. “Conventional fundus cameras use a one-time shutter which can create a lot of backscatter; NW500 disperses backscatter, so it’s less affected by cataracts.”
To share what these differences really mean to clinical practice — and importantly, to patient care and outcomes — Dr. Hanemoto then compared images detailing varying ophthalmic conditions … and in each case presented, images from the NW500 were sharper than those captured by other devices, including a conventional fundus camera and
Scan here to learn more about NW500
scanning laser ophthalmoscope.
Detection of retinal surface: In glaucoma patients, widening of the retinal nerve fiber layer (RNFL) defect (NFLD) is an important sign of glaucoma progression, leading to the functional deterioration of the visual field.1 “[NW500] picks up the reflection of the retinal surface so the detailed condition of the epiretinal membrane (ERM) and RNFL can be clearly understood,” he said. To illustrate, Dr. Hanemoto compared images of a 66-year-old male glaucoma patient. “[In the NW500], you can see the NFLD here … and with other models in the market, you can see the NFLD, but the sharpness is different,” he pointed out.
Detection of subretinal fluid: In central serous chorioretinopathy (CSCR), fluid builds up under the macula and leaks from the choroid.2 Leading with OCT and OCTA scans from a 59-year-old CSCR patient, Dr. Hanemoto then shared images from other imaging modalities: “FA (fluorescein angiography) shows the point of leakage and the conventional camera shows the fluid — but not clearly. However, with the NW500, you can see the retinal fluid and retinal ridges clearly; in other models available in the market, you can see the retinal ridge, but sharpness is different.”
Detection of retinal vessels: Leaky, damaged retinal blood vessels and diabetic retinopathy (DR) go hand-in-hand. In the case of a 61-year-old male DR patient, the NW500 showed shaperquality hemorrhages when compared with SLO. He then shared images from a patient with diabetic maculopathy. Both conventional fundus and OCT showed hard exudates around the fovea, as did SLO — but once again, NW500 prevailed with sharper images. “The reflection of the light source clearly shows the formation of retinal blood vessels and hemorrhages,” said Dr. Hanemoto, adding that NW500 also makes it easy to get peripheral retinal images, illustrated by a DME patient case.
Detection of subretina: “The use of laser and LEP light sources has made it possible to examine the deep part of
the retina better,” said Dr. Hanemoto before sharing images from a 79-yearold female patient with drusen — and once again, NW500 showed the drusen more sharply.
Dr. Hanemoto concluded that NW500 shows very detailed retinal conditions in non-mydriatic status, making it clinically useful in various conditions.
“In the last 40 years, and despite meaningful improvements in technology, therapeutic tools and knowledge of the disease, glaucoma patients continue to go blind,” said Dr. Henry Shen-Lih Chen from Chang Gung Memorial Hospital in Taiwan, during his talk, Untangle the Gordian Knot of Glaucoma Detection with Swept-Source Multimodal OCT: Implications for Clinical, Research and AI development
Glaucoma is characterized by the progressive death of retinal ganglion cells and optic nerve fiber loss, with changes in the appearance of the optic nerve head and RNFL; these changes are the most important aspect of a glaucoma diagnosis.3
Early detection is difficult because it depends on the comprehensive assessment of several structural and functional parameters and there is no proven screening methodology. Other reasons for diagnostic difficulty are highly variable visual field tests and the wide variation in the clinical appearance of a healthy optic disc, said Dr. Chen.

“In the past, it was suggested that there was a disconnect between the structure and the function of glaucoma. But we now know that a precise structure-function relationship exists in virtually all our patients throughout the glaucoma spectrum, even in very early disease,” he continued.
“Maybe we are entering an era of structure-structure assessment which will greatly change our need for other types of testing for many patients. Furthermore, there is growing evidence that macular damage is common in early glaucoma
— and we should notice that RNFL doesn’t tell the whole story,” he said, pointing to a study by Hood et al., that found that damage in the macular vulnerability zone is a more sensitive indicator of early glaucoma than damage in the cpRNFL.
“We should explore the relationship between anatomical and the functional changes in glaucoma and with widefield OCT to offer more insight about the pathology than the usual color metric-based diagnostics,” said Dr. Chen.

There are several unmet needs in glaucoma imaging and according to Dr. Chen, multimodal swept source OCT (SS-OCT), like Topcon’s DRI OCT Triton, could play a pivotal role in early detection. “Multimodal technology can provide a wide range of crucial image and data points to find an association with early glaucoma defects and untangle the Gordian knot of glaucoma detection,” he stated.
Triton’s swept-source technology allows visualization into deepest layers of the eye, through cataracts, hemorrhages, gas bubbles and media opacities, with a fast 100 kHz scanning speed and invisible scan beam. Dr. Chen said this technology, along with multimodal imaging, will improve clinicians’ workflow with fewer scans. Indeed, in a single scan, the Triton provides 3D
widefield visualization of a 12 x 9 mm area of the posterior pole, optic nerve head and macula.
Further, the widefield RNFL map and SS-OCT report can be a useful tool for early detection of glaucoma, as well as help improve the understanding of the relationship between optic nerve and macular damage. This can also minimize problems with alignment if comparing macular and circumpapillary data, and RNFL defects apart from the optic disc can be more easily visualized, explained Dr. Chen. “A single scan protocol can, in principle, be an effective screening tool. This is quite a significant improvement in OCT technology and most clinicians treating glaucoma are not taking advantage of the full potential of OCT.”
To streamline detection further, the Triton’s Glaucoma Hood Report acquires retinal thickness, RNFL, ganglion cell layer (GCL) and optic nerve metrics. “The Glaucoma Hood Report can help improve a clinician’s ability to treat early glaucoma before visual field changes, by displaying essential diagnostic cues in an intuitive one-page report,” said Dr. Chen. “This simplifies and accelerates the decision-making process with a correlation of structure and function.”
As an example, he shared a report from a typical glaucoma case. “The Hood report for this patient clearly demonstrates a superior temporal and an inferior temporal wedge-shaped defect on the RNFL thickness maps,” said Dr. Chen, noting that the visual field test showed no central defect — showing that structural defects could predict functional damage.
In addition to OCT — and thanks to those images — ophthalmologists could have another ally in glaucoma detection and diagnosis with artificial intelligence (AI). To date, numerous algorithms and studies have been carried out to determine if deep learning models can reliably detect glaucoma, as well assess damage and progression to improve diagnostic accuracy.4-6
Recently, Dr. Chen and colleagues developed and validated a novel deep learning model for early glaucoma detection.7 The algorithm extracted thickness information from the color space of fundus images, similar to that from OCT images, to provide information on RNFL defects. They found that the generated thickness map was sufficient for clinical glaucoma detection and that their proposed technique “may aid clinicians in early glaucoma detection, especially when only color fundus photographs are available.”
The ability to improve diagnostic accuracy in glaucoma through AI will undoubtedly save sight — and to a great social and economic benefit. It’s clear that “AI has the potential to revolutionize screening, diagnosis and the prediction of glaucoma in the near future,” Dr. Chen concluded.
1. Okamoto Y, Akagi T, Suda K. Longitudinal changes in superficial microvasculature in glaucomatous retinal nerve fiber layer defects after disc hemorrhage. Sci Rep. 2020;10(1):22058.
2. Rafieetary M, Haynes J, Attar R. Get Serious About Central Serous Chorioretinopathy. Review of Optometry. 2021 June 15.
3. Weinreb RN, Aung T, Medeiros FA. The Pathophysiology and Treatment of Glaucoma: A Review. AMA. 2014;311(18):1901-1911.
4. An G, Omodaka K, Hashimoto K, et al. Glaucoma Diagnosis with Machine Learning Based on Optical Coherence Tomography and Color Fundus Images. J Healthc Eng. 2019;2019:4061313.
5. Medeiros FA, Jammal AA, Mariottoni EB. Detection of Progressive Glaucomatous Optic Nerve Damage on Fundus Photographs with Deep Learning. Ophthalmology. 2021;128(3):383-392.
6. Medeiros FA, Jammal AA, Thompson AC. From Machine to Machine: An OCT-Trained Deep Learning Algorithm for Objective Quantification of Glaucomatous Damage in Fundus Photographs. Ophthalmology. 2019;126(4):513-521.
7. Chen HSL, Chen GA, Syu JY, et al. Early Glaucoma Detection by Using Style Transfer to Predict Retinal Nerve Fiber Layer Thickness Distribution on the Fundus Photograph. Ophthalmol Sci. 2022;2(3):100180.
The 15th Asia-Pacific Vitreoretina Society (APVRS) Congress took place in Taipei, Taiwan, from Nov. 18-20, 2022. Reporting for this story took place during the congress.

During the 15th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2022) the Media MICE team covered a number of topics where researchers are making leaps and bounds, all for the benefit of patients and significantly improved patient outcomes.
Case in point: The symposium on Advanced Retinal Imaging emphasized how imaging is revolutionizing the treatment of retinal diseases today.
To kick off the session, Dr. ShwuJiuan Sheu from the department of ophthalmology at Kaohsiung Medical University Hospital (Kaohsiung, Taiwan) gave an interesting presentation on Imaging in Posterior Uveitis.
While she covered a number of topics related to multi-modal imaging in the treatment of uveitis, the one that particularly caught our interest was fundus autofluorescence (FAF), a non-invasive imaging modality that can map naturally and pathologically occurring fluorophores in the posterior segment. Dr. Sheu reported that this technique is particularly useful as it can identify the hyperautofluorescence caused by uveitis, which occurs from a “loss of
by Andrew Sweeneybeneficial, especially for eyes with severe levels of DR, as its broad focus provides the best data for “optimal assessment and prognostication.” Finally, Dr. Sadda said that in one of his own studies, a deep learning model using UWF images was able to perform “at a level that suggests utility in a clinical environment,” and that a trial is currently underway to ascertain its performance in a realworld setting.
In another presentation —
Classification of AMD on OCT:
rhodopsin from photoreceptors.” In addition, she recommended the use of a multi-modal imaging approach when diagnosing and treating uveitis.
Dr. Srinivas Sadda, the director of the Artificial Intelligence & Imaging Research Department at the Doheny Eye Institute, and professor of ophthalmology at the University of California Los Angeles (UCLA) provided another excellent presentation — UWF Imaging in Screening DR: Implications from AI He pointed out the global need for improved diabetic retinopathy (DR) screening and treatment options, as by 2040 there will be “620 million people diagnosed with diabetes.”
The challenge, Dr. Sadda said, was intervening early enough with this new cohort of future patients to save their sight. As currently, only 29% of patients are meeting standard screening recommendations.
Dr. Sadda stated he believes that autonomous, AI-based approaches are now available that have the sufficient capacity and reliability to facilitate DR screening programs. The trick is that they must be able to “consider the entire retina area” while doing so. He points to the use of UWF imaging as being particularly
Update from CAM — Dr. Lim Tock Han, adjunct professor at the Lee Kong Chian School of Medicine in Singapore, introduced CAM, a group originally founded to investigate treatments for geographic atrophy (GA) and to manage chronic systemic disease related to macular atrophy. One of the recommendations that Dr. Han takes from this collective is that the use of color fundus photo is insufficient to “identify early stages of the disease,” especially for GA. He said that instead, clinicians should always opt for a multi-modal imaging technique to achieve the best diagnostic results.
Dr. Han also spoke about the importance of identifying cases of AMD drusen and cases associated with macular atrophy. He said that this requires a “deep dive into multimodal imaging” to differentiate AMD drusen from other cases as the treatment pathway is different from more conventional cases of AMD.
Finally, he said clinicians in general (from the Asia-Pacific region specifically) should adopt a population-based approach to managing patients with AMD by intervening early and promoting smoking cessation, which remains a major problem in the region.
The 15th Congress of the AsiaPacific Vitreo-retina Society (APVRS 2022) was held on November 18 to 20, 2022, in Taipei, Taiwan. Reporting for this story took place during the event. A version of this article was first published on piemagazine.org
Between artificial intelligence, genetic therapies, and a whole host of other technological developments that ophthalmology is able to take advantage of right now, it’s a very exciting time to be in our industry.

It’s only been just over a month since the start of 2023 and already news about artificial intelligence (AI) is all over our social media feeds and apps. From artists complaining about the rise of AIgenerated art taking their jobs away, to universities agonizing about how chatbots are beginning to interfere with the ability of professors to teach students properly (which, we think, is somewhat odd).
Barely two months into the new year and such wailing, tearing of cloth, and gnashing of teeth about AI in the wider community — yet last year, the atmosphere could’ve hardly been more different for the topic in ophthalmology.
During the 15th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2022), held in Taipei, Taiwan, AI was discussed in-depth in several symposiums.
One of the most fascinating talks was held on the penultimate day of the conference and was dedicated to investigating how AI technology can be used to significantly improve patient outcomes in retinal treatment. Artificial Intelligence in Retinal Diseases (we do like a concise title) covered ‘where the state of the art is, and where it may be going as AI has the potential to disrupt and improve the clinical practice of retina.’
The first presentation given during this symposium was AI for Retinal Disease Classification: Past, Present, and Future, provided by co-chair Dr. Peter Campbell, an associate professor of ophthalmology and
retina specialist at the Oregon Health & Science University (Portland, Oregon, USA).

Dr. Campbell emphasized that AI is best utilized when applied to tasks that it can do better than humans. And in ophthalmology, these tasks include imaging segmentation, assistive diagnosis, and potentially autonomous diagnosis. He views these factors as being split into two categories: the former two being what AI can do for clinicians now, and the latter, as what AI will be able to achieve in the (near) future.
For example, when it comes to assistive diagnosis, Dr. Campbell reported how AI technology can effectively triage patients by the acuity of diagnosis during a study on ‘diagnosis and referral rates’ in retinal diseases. When it comes to the future application of AI (which as he pointed out could be as early as months, not years or decades), it could soon replace humans in making full diagnoses where the ophthalmologist is taken completely out of the initial loop.
Dr. Campbell stated that this is most likely to occur with conditions that can be readily diagnosed via imaging, such as diabetic retinopathy, and
pointed to one study that found that ‘Eyenuk AI was more effective in diagnosing this disease than humanperformed dilation exams.’
AI — Are we nearly there yet?
The future of AI’s involvement in ophthalmology was a consistent theme throughout the symposium, as exemplified by another presentation we would like to highlight, RetinalImage Based Oculomics: Where Are We Going?
The presentation was provided by Dr. Yi-Ting Hsieh, an ophthalmologist at the National Taiwan University Hospital (Taipei, Taiwan), whose overview of what oculomics are and how it can be applied was particularly interesting as it is fundamentally predicated on AI.
According to Dr. Hsieh, an oculome is comprised of a complete set of macroscopic, microscopic, and molecular ophthalmic features associated with health and disease. Therefore, oculomics as an overall concept is made up of the comprehensive decrypting of the oculome by integrating the information generated by AI-driven multimodal imaging to identify the
specific ophthalmic biomarkers of systemic diseases.
Dr. Hsieh believes that oculomics is an ideal candidate for retinal imaging in ophthalmology due to its multimodal imaging component. And it should also find broad application in a number of other fields, ranging from cardiovascular diseases, neurodegenerative diseases (also with an ocular component), psychiatric conditions, and more.
AI, he said, will play an important role in pushing oculemics forward. The main challenge is that ‘ophthalmologists remain prickly or even skeptical about AI and its accuracy.’
One of the last presentations that really emphasized the validity of the metaphor ‘saving the best for last’ was provided by Dr. Emily Chew of the National Eye Insitute (Bethesda, Maryland, USA), in her presentation Data Privacy and Security for Retinal Disease
Her report was particularly interesting as, while it’s easy (and important) to focus on the technological advancements offered by AI technology, doctors and clinicians should also consider the ethical and privacy concerns that this technology raises. After all, Dr. Chew reported that every retinal image presents a unique vascular pattern that can be used to identify individual patients, thus presenting a considerable security issue.
A sub-committee that Dr. Chew is a member of at the National Eye Institute was set up to consider privacy issues that are of relevance to AI, in both retinal imaging and other related fields. Some of the recommendations that her subcommittee agreed on include using a federative/collaborative learning process to ensure that private data sets don’t leave individual institutions to boost security, and using an optin agreement system rather than opt-out to garner greater variety in patient feedback.
Dr. Chew also recommends promoting the highest quality
privacy-enhancing technology, recognizing ‘dignity and equal rights among patients,’ and constantly developing one’s knowledge about how data can potentially be used.

Keen to learn more about how AI can change retinal imaging? Or perhaps you might be concerned that one day a device looking vaguely like a 1980s-era Arnold Schwarzenegger will be delivered to your clinic and you want to forestall the coming robotrelated apocalypse? Well if you’re the latter, you may need to chill out. Otherwise, head over to the APVRS website to watch the symposium in full to find out more!
The 15th Congress of the AsiaPacific Vitreo-retina Society (APVRS 2022) was held on November 18 to 20, 2022, in Taipei, Taiwan. Reporting for this story took place during the event. A version of this article was first published in piemagazine.org

On the last day of the 15th Asia-Pacific Vitreo-retina Society (APVRS 2022) Congress, during an Alconsponsored symposium, experts explored the advantages of longer probe in highly myopic eyes, the benefits of small gauge probes in a retinal survey, as well as the best microscope for the NGENUITY® 3D Visualization System.
According to Dr. Tzyy-chang Ho from Chinese Taipei, several issues in myopic patients have raised concerns in operations, including increased axial length, epiretinal tissues visualization, dye toxicity, internal limiting membrane (ILM) peeling, macular hole (MH) closure, shaving vitreous tissue, and sclerotomy leakage.
Techniques to deal with such issues involved the use of an optical coherence tomography (OCT) system and a long-shaft probe, he noted.
“The NGENUITY system from Alcon is a 3D digital system with a camera and display that replaces the analog oculars of the scope,” shared Dr. Ho. “There are many advantages of using a 3D head-up viewing system, and one of them is optimizing the surgeon’s ergonomics when using the microscope,” he said, adding that
some surgeons had to resort to getting an artificial cervical joint replacement costing 8,000 US dollars each due to musculoskeletal problems.
He mentioned that when carrying out surgery in highly myopic eyes, an extended long-shaft vitrectomy probe provides tissue plane access for eyes with long axial length, enabling the removal of posterior hyaloid, cortical vitreous, and trimming of the ERM and ILM flap in the age of flap surgery.
“There’s no need to remove the cannula or indent sclerotomy to avoid intraoperative complications. Surgical complications of using the extended long-shaft probe are not found in our prospective study,” he said.

He further noted that the extended
long shaft vitrectomy probe that is 25 gauge and 30 mm long by Alcon, which can work with the Alcon Constellation system, is created to overcome the issue of a long eyeball in highly myopic patients.
The 30 mm probe can reach the
posterior pole better than the previous 27 mm version. “The high gravity brilliant blue green (BBG) and indocyanine green (ICG) can be removed efficiently and faster by the 30 mm probe to prevent extended retinal contact. This probe can be implemented in highly myopic eyes, including those with myopic traction maculopathy, macular hole retinal detachment, macular hole, epiretinal membrane (ERM), and lamellar hole w/o LHEP,” Dr. Ho said.
He showcased a few cases where he used the 30 mm probe, including trimming ILM in eyes with high myopia, ERM in highly myopic eyes, ERM with lamellar hole, and epiretinal proliferation.
“In ERM lamellar hole schisis, only the 30 mm probe can trim the ERM elegantly so that we can preserve proliferative tissue properly,” he concluded, sharing that a 27-gauge probe with a 30-mm-long shaft by Alcon will be available soon.
Next, Dr. Adrian Fung from Australia discussed the benefits of smallgauge retina surgeries.
“Small gauge vitrectomy involves the use of 25-gauge (0.55 diameter) and 27-gauge (0.4 mm) probes,” he shared. “The advantages of small gauge vitrectomy include more self-sealing wounds, less sutures are needed, and there will be less inflammation and pain. A smaller gauge also provides greater maneuverability, which is particularly useful in diabetic retinopathy. In addition, a smaller gauge also causes less hypotony due to more self-sealing wounds,” Dr. Fung shared.
Nevertheless, the smaller gauge vitrectomy comes with potential disadvantages, which include decreased vitreous flow, increased port closed time, increased surgery time, and unwanted flexibility.
“The new Hypervit® dual blade vitrectomy probe, however, does have the potential to mitigate some of these limitations due to its features, which include the ability to make 20,000 cuts per minute (CPM), a continuously open port,
dual-pneumatic drive, and a bevel tip design,” he said.
He also noted that the Hypervit Dual Blade Probe has a closer port proximity to the retina, and its continuously open port is designed to maximize control through improved efficacy and stability.
“With the Hypervit, we have a continuous vitreous flow rate of up to 90% higher in the 25-gauge probe and up to 48% in the 27-gauge probe (compared to a single-cutting 10,000 CPM probe) because the port is continuously open in the dual-pneumatic drive,” he shared. He added that there is also a reduced peak traction force due to the ability to make 20,000 cuts per minute.
“In terms of surgery time, the 27-gauge vitrectomy only took 90 seconds more than the 23-gauge vitrectomy,” Dr. Fung concluded.
Last but not least, Dr. Kazuhito Yoneda from Japan explored the best microscope for the NGENUITY 3D Visualization System in terms of anterior surgical view, fundus surgical view, and light path comparison.
Five different microscopes are compared in the same operating group and environment: the LuxOR® Revalia™ Ophthalmic Microscope, Microscope A and Microscope B from one company, and Microscope C and Microscope D from another company.
In the anterior segment, Dr. Yoneda and his colleagues compared the transillumination of the microscopes in various situations during cataract surgery. In regard to fundus observation, they compared the width and resolution of the fundus surgical view.
He said Revalia has outstanding performance in all situations during cataract surgery, while the others have reduced transillumination in certain situations.
“The reason Revalia was able to obtain very clear transillumination over a wide area is due to its unique structure, in which the illumination source is located closer to the eyes than the objective lens, hence the
light is not concentrated at one point but spread across a wide area of the eye, allowing 6x larger red reflex zone than standard analog microscopes,” he explained.
Besides, Revalia also provides a personalized LED illumination system where one can choose to use either warm white, cold white, or mixed white.
“Theoretically, mixed white can provide both good transillumination and sharp edge in the anterior chamber. But in actual practice, warm white is the best color combination during cataract surgery,” he said.
“In terms of fundus surgical view, Revalia and Microscope D have a very clear and an excellent width of view. Microscope C has a very, very narrow surgical view. Meanwhile, Microscope A is a little narrower than B. As for resolution, there is no difference between the microscopes when using NGENUITY.”
“In clinical use or surgery, it is very important not to have any failed score,” noted Dr. Yoneda. “Revalia and Microscope D can provide excellent fundus image. Revalia is better for anterior surgery, while Microscope D is better for posterior surgery. When comparing microscopes of the same company, a simple microscope is better for NGENUITY,” he noted.
After Dr. Yoneda’s talk, Dr. Maria Berrocal from Puerto Rico joined the panel discussion.
“I use the Revalia and NGEUITY, and I agree with Dr. Yoneda on what he said. I absolutely love the 27-gauge Hypervit probe. I use it for diabetic vitrectomy, and I think that it is very advantageous,” she said.
The 15th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2022) was held on 18-20 November in Taipei, Taiwan. Reporting for this story took place during the event. This article was first published in PIE Issue 24X.

Tengku Ain Kamalden talks about her passion for ophthalmology, finding that elusive balance, and building an oasis of growth
by Joanna LeeCatching a breath from her hectic schedule before embarking on another slew of meetings, Prof. Dr. Tengku Ain Fathlun Tengku Kamalden shared her thoughts on work and life with PIE Magazine , amid a sanctuary of tranquillity at her home.
“Being a clinician academician and scientist, I wear all the hats together. All my colleagues in all public university teaching hospitals also wear the same hats.”
“Being a clinician academician and scientist, I wear all the hats together. All my colleagues in all public university teaching hospitals also wear the same hats,” she shared.
The vitreoretinal specialist at the University of Malaya’s Department of Ophthalmology is the only vitreoretinal (VR) surgeon in the department — which means long hours being on call.
Clinical hours are interspersed with hands-on lectures, administrative duties, and conducting research work where she runs labs, even as a principal investigator. In addition, there are tutorial classes for undergraduate and nursing medical students.
Prof. Ain’s interest in the anatomy of the eye started when she was introduced to ophthalmology during a two-week undergraduate posting.
“It was a completely different field altogether, with different medical terms, different physiology. Everything was unique, and they seem to be talking in a different language. And so, that intrigued me,”

she said with a soft smile.
“The textbooks were one of the plus points, too. They were the only textbooks then that had real pictures, being very colorful and beautiful compared to other textbooks,” Prof. Ain continued.
“The more you learn, you realize that this is not just about sight,” she enthused. “Where else can we get a part of a solid human body that is transparent other than the eye?”
Besides, there was something else that made her ponder: “My name means ‘eye’ in Arabic, and even before I was in ophthalmology, I’ve always been intrigued by this — could this have been a sign?” she wondered aloud.
“It was a perfect match as I’d wanted something that had a medical and surgical combination, where you could be a physician and surgeon at the same time while dealing with microsurgery. So, my name, given by my grandmother, helped,” she shared.
Prof. Ain’s interest in healthcare was also ingrained at a young age when she observed her nurse mother’s dedication and humane sincerity towards her patients as a matron at the hospital wards.
This deeper realization also steered her path toward the medical field, especially with her passion for surgery. “It was at that crossroad when I was considering scholarships in the field that I had decided early on in life: We have 10 fingers. I could play musical instruments and write. I thought, if I could just maximize the ability of my hands in contributing to humanity, I could maximize the benefits of using my hands. That [realization] helped me,” she continued.
During the course of her undergraduate studies at the University of Malaya, her beloved older brother who was also in medical school abroad at that time was diagnosed with cancer. “It was a difficult point for our family, struggling for the first time with something so immediate and
serious. But it brought us closer,” she recounted.
The challenge seemed to mount further when she was pursuing her PhD abroad. Her brother had a relapse while her father was diagnosed with kidney failure and needing dialysis.
“It was a lot to take in, especially when you’re abroad and you have a close-knit family,” she said.
Besides the loneliness, there were struggles with the course itself, diving into the rigors of academia of doing her PhD with no patient contact.
know you can try to create bridges and have a bit more courage to go out there. And that carries on till now,” she enthused.
Prof. Ain has spent the last decade delving into translational research, specifically looking at protein signaling as biomarkers that could possibly exude warnings before the complications of diabetic retinopathy set in.
wanted something that had a medical and surgical combination, where you could be a physician and surgeon at the same time while dealing with microsurgery.”
“I literally started from scratch in research, doing lab work. You thought that being trained for at least 10 years in ophthalmology meant you would know something,” she recalled. “But you go into the lab and realize, it was like going back to an undergraduate degree, learning something completely different, including cell cultures, looking into protein cellular pathways, etc.”
“Then there was the politics in the lab,” she shared, adding that most PhD students have faced these challenges.
However, all that served a better purpose. “It helped me gain some strength and it helped me guide my juniors and colleagues who faced difficulties, too. You understand these things as a rite of passage for some, and you become empathetic to juniors. It helps you to see the world in a different light,” Prof. Ain shared.
Her time abroad in the UK also allowed her to experience various trials. She spoke about the loneliness, of facing racism, and being a minority in a foreign land.
“I think it was important to be abroad as you would never have learned this in your own comfort zone. It has helped me realize that you can go further, that there are ways to do this, and you get this competence that you
How does she make space to grow amidst an ultra-hectic schedule?
Acknowledging the expectations upon women to be stereotypical, she said the demands on women ophthalmologists especially in Malaysia are found mostly during their pursuits at the subspecialty level (if they choose to).
When it comes to juggling life with these demands and duties, Prof. Ain remembers veteran ophthalmologist Dr. Carol Shields’ wisdom on balance.
“One of the things she said was, ‘you don’t expect things to be perfect all the time.’ It’s okay if things are at 80% instead of 100%. If the vacuumed spot isn’t perfectly clean, it might mean you would have to do it [again], or the kids, or somebody else,” she shared. “As long as you learn about priorities and don’t fret about the little stuff, that’s how people [find] balance. And everybody has a different balance.”
“I think the challenge is for every woman ophthalmologist and every woman [in general] to find that fine balance between their career and personal life at every stage of life, while not compromising the important values in their personal life,” she added.
Having said that, Prof. Ain admits that she strives to keep work matters confined to office hours. Finding her balance includes indulging in
“It was a perfect match as I’d
her joy of gardening, a hobby she picked up during the pandemic.
“It’s now a little forest,” she chuckled, confessing that they need more regular trimmings now with her going back to the office. She also enjoys learning about herbs and has cultivated a bubbling pond with guppy fishes, besides rescuing cats and dogs off the street.

Prof. Ain also divulged that she finds joy in collecting books in her curiosity to learn about the origins of things.
So finally, what keeps Prof. Ain going and growing?

“In the time and opportunities given to us, keep learning and changing for the better as much as we possibly can — so that when our time is up, our efforts allow others to do even better and go even further. Do make a difference in the right direction, no matter how small our contributions may be,” she concluded.

Quietly prolific, Prof. Dr. Tengku Ain Kamalden graduated from the University of Malaya (Kuala Lumpur, Malaysia) with basic medical and master’s degrees in ophthalmology. She also obtained her masters in medicine (ophthalmology) from the National University of Singapore (M.Med), and memberships from the Royal College of Surgeons of Edinburgh and the Royal College of Ophthalmologists, London. Right after the completion of her DPhil studies at the University of Oxford, United Kingdom, in 2012, she was appointed as acting head of the University of Malaya Eye Research Centre from 2012 to 2013, during which time she set up the first basic science laboratory for ophthalmology
in the Faculty of Medicine, and established international collaborative research work with renowned institutions, such as the Johns Hopkins University (USA) and University of Liverpool (UK). The clinician-scientist presently holds the position of senior lecturer and clinical specialist at the Department of Ophthalmology, Faculty of Medicine at the University of Malaya. She was a Fulbright Visiting Researcher Scholar in 2018 and was awarded the Bronze medal in the AsiaPacific Vitreo-Retinal Society’s Leadership Development Program (2019), among other awards. taftkamalden@um.edu.my

 by Tan Sher Lynn
by Tan Sher Lynn
Like any other industry, ophthalmology also contributes to waste and greenhouse gas emissions. As such, it is important for all parties to make an effort to foster sustainability in our industry.
During The Royal Australian and New Zealand College of Ophthalmologists’ (RANZCO 2022) 53rd Annual Scientific Congress — held in Brisbane, Australia, in October last year — experts shared their thoughts on the topic.

Ever since the industrial revolution, atmospheric carbon dioxide (CO2) emissions have been steadily increasing, noted A/Prof. John Landers from Flinders Medical Centre, South Australia.
In Australia, healthcare contributed to 7% of total CO2 emissions, of which 40% come from low-value healthcare. According to A/Prof. Landers, major sources of CO2 emissions from ophthalmology can be divided into energy, travel,
and procurement (mainly due to single-use medication such as eye drops and tonometry equipment, medical records in servers, personal protective equipment [PPE], and intravitreal injections).
“Servers account for 2% of global emissions and are predicted to rise to 14% by 2040. In terms of PPE, globally, plastic waste almost tripled in 2020, discarded PPE increased by 10 times, and discarded masks increased by 84 times,” he shared.
Meanwhile, Dr. Sarah Welch from New Zealand noted that humans are living in a climate emergency that is more severe than anticipated and threatens the fate of humanity. She said medical colleges play an important role in helping doctors take the lead on climate change.
“Doctors are good in emergencies,” she opened. “We understand complex systems, work well in teams, understand the long-term view, and advocate for health. Health causes 5% to 10% of national carbon emissions, and so it is an important area to focus on to reduce waste and carbon footprint,” Dr. Welch said.
“A recent survey of medical and dental colleges in Australia and New Zealand found that nearly 60% had published statements or policies about sustainability,” she continued. “Colleges can demonstrate by example by embedding sustainability in college governance, quantifying and reducing college carbon footprints, investing responsibly and divesting from polluting industries, advocating for sustainability in all levels of government, and promoting sustainability among members, such as by facilitating the learning about sustainability at all levels of college membership,” she said, adding that she is pleased that RANZCO’s Vision 2030 has a sustainability focus.


Intravitreal injection, the most common intraocular procedure worldwide, has been rising exponentially since its introduction 15 years ago, according to Dr. Michelle Gajus, a RANZCO Sustainability Committee Member. Last year alone, about 600,000 procedures have been performed in Australia.
Dr. Gajus noted that the largest contributions of carbon emissions in intravitreal injections are patient/staff travel and procurement. “Therefore, the sustainability committee decided to survey our members to see what we use in order to encourage us to think about our carbon emission,” she shared.
Out of 1,100 RANZCO fellowship members, 707 responses were received and some of the results are as follows. More than 96% of the responders said that they perform intravitreal injections in the office/ treatment room, and only 3.5% inject exclusively in the operation theater. In terms of PPE, more than 99% use masks and more than 90% use sterile gloves. About 3% to 11% also use shoes, head covers, and gowns. In terms of local anesthetic, 31% of the responders use topical drops only, while 60% use a combination of topical and subconjunctival injection. When it comes to consumables, 55% use custom IVI packs, 37% use basic dressing packs, and the rest use individual items.
The survey also asked the members what they would like to change, if any. And many of them expressed concerns that the free IVI dressing packs that they receive are not often being used and had to be thrown away.
“About a third of the responders do not use any callipers or speculum. If you do, perhaps it’s time to rethink the prepackaged equipment and disposal equipment,” added Dr. Gajus.
“A UK study found that the removal of four items from the IVI pack reduced 0.5kg CO2eq, hence it is worthwhile to reduce even the little things in your pack. I encourage you to reflect on what you do and whether they are necessary, reject things that you don’t need, and react by doing something about it. There’s no place for post-treatment antibiotics as well,” she concluded.
Often, people with vision impairment need continuous care that extends beyond the clinician’s office. Following the talks on sustainability, Mr. Nabill Jacob from Vision Australia shared about the organization’s efforts in helping vision-impaired patients live better lives.
Vision Australia is a not-for-profit organization and the country’s leading provider of specialized blind or low-vision services to support
people of all ages and stages.
“We know that the impact of vision impairment is profound and risks increased with vision loss,” Mr. Jacob said, noting that in order to help these patients to live the life they choose, Vision Australia adopts strategies that include vision enhancement, vision substitution, and environmental adaptations.
Among the various services provided by Vision Australia include emotional support groups, occupational therapists, mobility specialists, orthoptists, education and employment support, aids and equipment, technology, and training, among others.
The technology used include devices with refreshable Braille, WeWALK Smart cane, desk magnifier, wireless virtual reality headset IrisVision, and Orcam — an artificial intelligence device that enables people who are blind or visually impaired to read text from any surface, recognize faces, identify colors, products, among others.
Mr. Jacob noted that an emphasis is placed on children’s vision loss as well, and efforts are made to prepare them for employment and meaningful life-long participation starting from school-age years.
He also shared the parameters of patient referral. “These parameters include a diagnosis of a permanent non-correctible or progressive eye condition: visual acuity of <6/12 (both eyes open [BEO]) and or a visual field of ≤ 30 degrees (BEO); when vision loss is putting the patient at risk of accidents and health conditions; and when they experience grief or loss related to vision changes or difficulty completing everyday tasks,” he concluded, adding that referrals can be done easily via Vision Australia’s homepage.
The Royal Australian and New Zealand College of Ophthalmologists’ (RANZCO) 53rd Annual Scientific Congress was held on October 28 to November 1, 2022, in Brisbane, Australia. Reporting for this story took place during the event.

At the recently held 15th Congress of the Asia-Pacific Vitreo-retina Society (APVRS 2022), held in Taipei, Taiwan, experts explored artificial intelligence (AI) and telemedicine as potential mitigators in the post-pandemic world, as well as discussed gene therapies and new drug approvals for retinal diseases.
While the pandemic has disrupted various aspects of our lives, it has also promoted increased use of AI and digital health solutions. For example, exciting technologies that emerged during the pandemic include the Johns Hopkins COVID-19 dashboard, AI for risk modeling in COVID-19, and AI for CT imaging for COVID-19 — noted Dr. Daniel Ting from Singapore during his presentation.
He mentioned that machine and
deep learning studies on PubMed have been showing exponential growth over the past years.
Dr. Ting also shared that in Singapore, for example, DR EYE was created to harness the power of AI and the Internet of Things (IoT) to promote eye health among patients, especially migrants who don’t speak good English. The app empowers patients to be more health conscious by keeping their own eye records and promotes better communication with patients and external partners
(e.g., community optometrists or opticians). The aim is to integrate state-of-the-art deep learning technologies with digital solutions, leveraging the IoT to deliver eye care via the cloud.
When it comes to the use of AI in ophthalmology, the sky is the limit. The various new technical areas of AI include federated machine learning, blockchain, adversarial attacks, driverless AI, segmentation AI, and synthetic AI with human-in-theloop. Meanwhile, digital innovations include remote monitoring; augmented, virtual vs. mixed realities; and the Metaverse, Dr. Ting further shared.
During his presentation, Dr. Xuejing Chen from the Boston University Eye Associates (USA) noted that telemedicine is not a new thing in ophthalmology. Traditionally, the store-and-forward model was used in age-related macular degeneration (AMD), retinopathy of prematurity (ROP), diabetic retinopathy (DR), and glaucoma, which bridged access due to distance or workforce limitations.
“However, during the pandemic, telemedicine assumed a new purpose, which is to provide care for patients while limiting physical contact. This allows vulnerable patients to seek the care they need,” she shared, noting that many centers had quickly developed virtual protocols to serve patients during the pandemic. However, a virtual-only telemedicine platform has its limitations, which include the absence of examination elements.
“The hybrid ophthalmology telemedicine was developed to address the shortcomings of a virtual-only telemedicine platform. This model includes an in-person imaging appointment administered by a trained technician (to perform necessary tests), followed by a virtual-only appointment with the doctor on a separate day,” she continued.
Dr. Chen described the implementation of the hybrid model in 889 patients in a hospital-based eye clinic in Boston from April 9 to December 30, 2022. The hybrid

model was primarily used for retina and glaucoma patients. At the end of the virtual appointment, most hybrid patients continued the same plan, but at least 9.7% required a change in management (procedure, change of medication, or consult), indicating that even ‘stable, non-procedural’ patients need follow-up and should not be continuously postponed.
She also noted that according to a survey done by the hospital, hybrid visits and in-person visits did not have any difference in terms of patient satisfaction. However, older patients were less satisfied than younger patients with hybrid visits, but were equally satisfied with inperson visits.

Meanwhile, there was another good news from Dr. Elliott Sohn from Iowa, USA. He shared that the technology and surgery needed to treat most inherited retinal diseases are available nowadays. However, he emphasized that clinical trials and pre-clinical work with RNA, DNA, and cell-based therapies are under intense investigation.
“The various gene therapy trials and approaches available nowadays include gene replacement, which is especially for recessive disorders (such as voretigene neparvoves for RPE65 mutation), CRISPR-based gene editing strategies, RNA-based therapies, and delivery of a gene to produce a protein necessary for cell or physiologic function — mainly for inherited retinal disease (IRD), AMD, and DR,” he shared. He noted that over 750 trials of gene and cell therapies have been carried out in 30,000 patients in medicine.
According to Dr. Sohn, it is important to mention that COVID-19 has accelerated innovations and unexpected solutions, such as the automation of induced pluripotent stem cells (iPSC) production with robotics, which increases throughput for cell generation.
“The pandemic has affected us in many different ways, but it also brought us closer as one world, one
globe, one humanity,” said Dr. Judy Kim from Wisconsin, USA. “For me, all the clinical trials that have been going on came to a halt. We could not see any research patients at all.”
She noted, however, that despite the pandemic, drug development and approval continued to be carried out. One of the drugs approved is the faricimab-svoa (VABYSMO™), the first bispecific antibody that acts through dual inhibition of both angiopoietin-2 and vascular endothelial growth factor A.
She mentioned that the 2018 ASRS PAT survey of US and international retina specialists revealed that the greatest unmet need with regard to neovascular age-related macular degeneration (nAMD) treatment is the need for reduced treatment burden, followed by long-acting/ sustained delivery.
As such, faricimab potentially meets the need for durability.
The TENAYA and LUCERNE trials showed that the acuity outcomes of faricimab on nAMD patients were non-inferior to aflibercept. In fact, with faricimab, about 45% of patients were able to be treated until Q16W, and almost 80% were able to be treated up to Q12W and longer.
Meanwhile, the YOSEMITE and RHINE trials showed that vision gains with faricimab Q8W and personalized treatment intervals (PTI) up to Q16W were non-inferior to aflibercept Q8W and maintained through year 2. The trials also showed that over 60% of diabetic macular edema (DME) patients were able to achieve Q16W dosing at week 96.
“Based on these favorable results, FDA approved faricimab for nAMD and DME treatment in January 2022,” she said.
She also mentioned that brolucizumab-dbll (BEOVU®) was approved for DME treatment in June 2022.
Dr. Kim also talked about biosimilars — biologics that are highly similar to the (originally licensed) reference product, noting that they have a different development pathway and approval process than drugs.
“It takes a company over 10 years and about $2.6 billion to bring a new drug to the market. But for biosimilars, it only takes five to nine years and $100 million,” she shared, noting that the first ophthalmology biosimilar approved by the FDA was ranibizumab-nuna (BYOOVIZ™) in September 2021 for nAMD, myopic choroidal neovascular membranes (CNVM), and macular edema from retinal vein occlusion.
The 15th Congress of the AsiaPacific Vitreo-retina Society (APVRS 2022) was held on November 18 to 20, 2022 in Taipei, Taiwan. Reporting for this story took place during the event.





