www.healthawareness.co.uk Q2 2023 | A promotional supplement distributed on behalf of Mediaplanet, which takes sole responsibility for its content “AI could improve early detection and prevention rates, diagnosing difficult-to-detect cancers more effectively than humans.” Antonio Spina, Lead, Digital Health, World Economic Forum Page 02
of the biggest developments in recent years has been the incorporation of genomic testing into routine cancer care.”
Innovations in Oncology
“One
Page 06
Joseph Williams, Chair; Emma Foreman, Vice Chair; Jessica Pealing, Secretary, BOPA
As an already pressured NHS deals with a growing cancer patient backlog, clinicians face the challenge of delivering patient-centric care within a resource-constrained healthcare system.
Digital solutions can help resolve challenges by streamlining interactions between patients and healthcare providers. Vinehealth achieves this for clinicians, industry and academic researchers and patients alike. The Vinehealth ecosystem comprises an NHS England-endorsed smartphone app designed around the needs of people living with cancer and VinehealthPRO, a connected dashboard for clinicians.

Supported self-management to improve patient wellbeing
This ecosystem was launched in 2018 by former NHS doctor Dr Rayna Patel and Georgina Kirby, a data scientist. They recognised the potential for digital technology to combat the lack of day-to-day support experienced by many people living with cancer. Patients can use the app to access supportive content from the UK’s leading charities, manage their medications, receive appointment reminders and track their mood, physical activity and symptoms.
In addition to reducing information overload and the pressure to recall detailed information during brief appointments, supported self-management helps patients to feel in control of their treatment. Studies with patients from hospitals, such as The Royal Marsden and Cromwell Hospital, reported significant improvements in feelings of wellbeing.
Unparalleled patient insights for clinicians
People living with cancer can download and use the app without an invitation from their healthcare provider. But they may be invited onto the app by their clinician, who can then view the patient’s data in real time using the clinician dashboard.
This grants clinicians unparalleled insights into patient wellbeing at home, enabling them to identify and address deteriorations more rapidly. Clinicians using the dashboard report an improved understanding of how their patients are feeling between appointments, as well as opportunities to personalise care or prevent emergency admissions.
Pharmaceutical companies can also use this technology to support clinical trials, realworld evidence studies and patient support programmes. This patient-reported data enables researchers to develop a deeper understanding of how cancer therapies are affecting patients. This data is vital in reimagining the cancer pathway to improve the patient experience and overall outcomes for people living with cancer.
Digital health: the next frontier in the global fight against cancer
With one in six deaths still caused by cancer, experts are searching for digital health innovations that could one day turn the tide in the fight against it.
The rise of digital and data-driven technology in healthcare — such as artificial intelligence (AI), the internet of things (IoT) and robotics — could offer unprecedented potential in the fight against cancer.
technologies through regulatory mechanisms and ethical guidelines, given potential safety concerns with automation and security concerns with patient data.
Digitising the patient journey
Antonio Spina Lead, Digital Health, World Economic Forum

Digital health computing cancer cures
The rise of computational tools has unlocked new approaches to treatments. In particular, AI and machine learning hold the potential to revolutionise how drugs are matched to patients, taking personalised cancer care to the next level. Such technologies could also drastically transform the timeline for the development of new drugs, making it a matter of months rather than years.
Going beyond the pill: prevention and diagnosis
New digital technologies may transform health outcomes and improve the patient experience. For instance, digital tools have been employed to help patients and families manage some aspects of cancer care from home.

Emerging evidence even suggests that virtual reality could become a potential tool for cancer care. Some virtual solutions for pain management have already received FDA approval; similar technologies could potentially be translated into oncology.
AI and machine learning hold the potential to revolutionise how drugs are matched to patients.
Beyond developing and integrating new treatments, AI could improve early detection and prevention rates. Missed or incorrect medical diagnoses are a serious concern, and oncology is one of the highest-risk specialities. Research institutions are applying the latest AI advancements to diagnose common cancers, where algorithms can spot difficult-to-detect cancers more effectively than humans. However, authorities must ensure the responsible use of new
Expanding global access to care for all
With approximately 70% of cancer deaths occurring in low and middleincome countries (LMICs), new technologies must reach the most vulnerable. However, LMICs face roadblocks to digital health uptake, such as limited financial resources. International funding and support are key to bridging the technology and health gaps. As digital innovations in the fight against cancer advance, global leaders must ensure that digital health helps produce a more equitable and sustainable global health system.
WRITTEN BY Dr Rayna Patel CEO & Co-Founder

@HealthawarenessUK
@MediaplanetUK Please recycle
Project Manager: Millie Thompson millie.thompson@mediaplanet.com

Business Development Manager: Ciara Barker
Managing Director: Alex Williams Head of Business Development: Ellie McGregor | Head of Print & Design: Thomas Kent
Designer: Aimee Rayment Content Editor: Angelica Hackett O’Toole | Head of Digital Operations: Harvey O’Donnell
Paid Media Strategist: Jonni Asfaha Social & Web Editor: Henry Phillips Digital Assistant: Carolina Galbraith Duarte | All images supplied by Gettyimages, unless otherwise specified | Contact information: uk.info@mediaplanet.com or +44 (0) 203 642 0737
02 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
Paid for by Vinehealth
App revolutionises cancer care, easing pressure on clinicians and empowering patients
Learn more or download the app from our website vinehealth.ai or via the QR code.
Vinehealth
How biomarkers offer precision me dicine and positive vision for cancer patients
Biomarkers have provided a breakthrough in cancer care because they identify the make-up of individual tumours — and the targeted intervention that could stop them in their tracks.
On average, someone is diagnosed with cancer every 90 seconds in the UK, notes Dr Markus Kosch, Head of Oncology at healthcare company, Daiichi Sankyo.


“Which means that every 90 seconds, a husband, wife, father, mother, sister or brother has their life turned upside down,” he says. “There are now 3 million people living with cancer in the UK, and this figure is expected to rise to 5.3 million by 2040. So, it’s something that affects us all — directly or indirectly.”
Biomarker testing to assess disease and determine treatment
Because cancer is so biologically diverse with a myriad of subtypes, it can be a challenge for clinicians to identify the best treatment options for their patients. However, thanks to advances in the understanding of tumour biology, an innovation called ‘biomarker testing’ is now accelerating the fight against cancer.
Biomarkers can detect whether a disease or condition is present, how aggressive it is, what is helping it thrive — and, crucially, what specific treatment would potentially stop it. They are collected via routine tests such as biopsies or blood tests. The information they produce has the power to revolutionise how we think about and treat disease. For example, biomarkers identify a cancer’s ‘kryptonite’ — its weakness — so that specific tumour subtypes can be attacked in a more targeted way, making treatment more efficacious and, sometimes, side effects more tolerable.
Understanding biomarkers and how they advance precision medicine
Dr David Harland, Oncology Medical Affairs Lead at pharmaceutical and biotechnology company AstraZeneca, sees this as an exciting milestone in the field of oncology. “Biomarker testing is the emerging foundation of precision medicine,” he says. “You can’t deliver precision oncology treatment without an understanding and a breadth of biomarker testing.”
By studying different biomarkers — such as risk biomarkers, monitoring biomarkers, predictive biomarkers and prognostic biomarkers — clinicians can make better, more informed decisions for patients.

inappropriate medical care — in the interest of the patient, the physician and the healthcare system.
“At present, chemotherapy is the ultimate hammer to crack a nut,” says Dr Harland. “It wipes out everything in the hope that it also kills the cancer. However, precision medicine gives targeted treatment to the tumour — and only to patients who are likely to respond to it. Ethically, and from a health economic perspective, it’s the right thing to do.”
Document number: ADC/23/0482
Date of preparation: June 2023
For example, predictive biomarkers will tell them if a patient’s cancer can be treated by a specific type of agent, while prognostic biomarkers will indicate what an individual’s response to it will be. This can help avoid ‘overtreatment’— unnecessary and
Looking at the role of patient groups and future of cancer care


As biomarker science advances, patients must understand its impact. “This is why the role of patient groups is so important,” stresses Dr Kosch. “For instance, we proactively work alongside organisations on initiatives that aim to improve patient outcomes through education and increased awareness.”
Dr Kosch believes that biomarkers can change both the narrative of cancer care and the trajectory of the disease. “Our vision is that, in the long-term, cancer will become a chronic disease, rather than a life sentence,” he says. “By enabling precision medicine, biomarkers are an important step towards transforming cancer from a life sentence to a chronic disease.”
Dr Harland agrees. “Our mission is to eliminate cancer as a cause of death,” he says. “We’ll only be able to do this with precision medicine. We’re now moving away from thinking of cancer as ‘locationbased’ and more towards the biomarkers we want to target. There’s still a huge amount of work to be done, especially in developing biomarkers and precision medicine.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 03 MEDIAPLANET
Find out more at daiichi-sankyo.co.uk astrazeneca.co.uk
Paid for by Daiichi Sankyo and AstraZeneca
Precision medicine gives targeted treatment to the tumour — and only to patients who are likely to respond to it.
INTERVIEW WITH Dr Markus Kosch Head of Oncology, Daiichi Sankyo
INTERVIEW WITH Dr David Harland Oncology Medical Affairs Lead, AstraZeneca
WRITTEN BY Tony Greenway
Biomarkers can change both the narrative of cancer care and the trajectory of the disease.
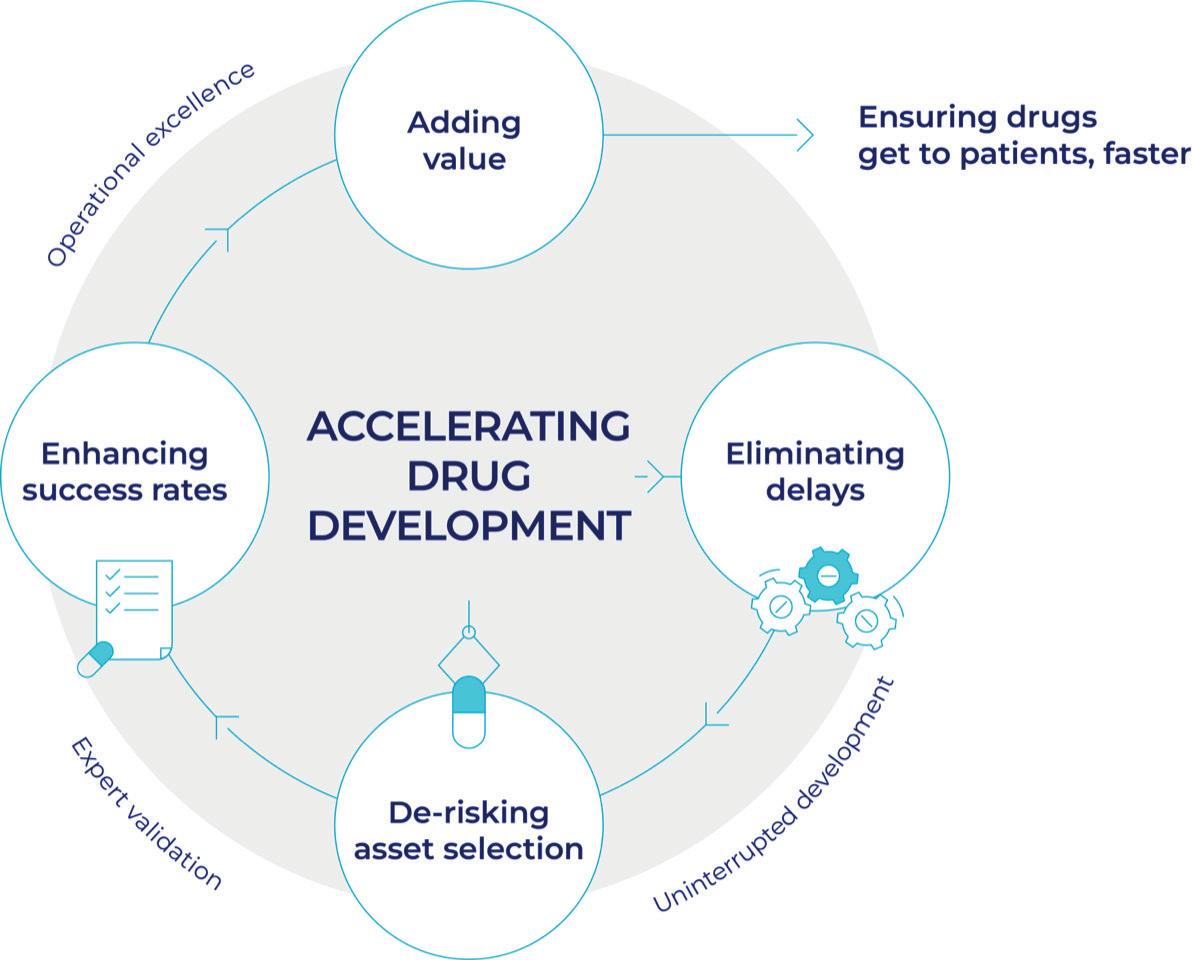
The united army of experts helping improve cancer treatment delivery
A drug development company has assembled one of the world’s largest and most diverse groups of global cancer experts to help accelerate the availability of new treatments for patients.
People with a range of cancers are seeing increasingly improved outcomes thanks to innovative drug development and new treatment regimes. Yet, despite these advances and high rates of recovery for patients, the development of new treatments often remains prolonged.
Contributing to cancer treatments
To overcome this, UK-based Ellipses Pharma — which focuses exclusively on the development of cancer medicine and treatments — has built a pioneering cloud-based platform to gather scientific and clinical insight from renowned cancer experts across the world.
More than 230 oncologists work independently within the company’s Scientific Affairs Group (SAG) to help validate the selection of new cancer medicines. They also select patients who may benefit from each medicine and provide unbiased input during the development of each drug using real-world evidence.
Professor Sir Chris Evans, the company chairman and founder, says: “From the outset, we decided to build the most extensive SAG anywhere, so we could pick oustanding potential cancer treatments quickly and accelerate their development to get them to patients.”
More input for better decisions
This approach was developed amid concerns that many cancer programmes fail to maximise this critical scientific advisory resource, resulting in poor decision-making, unnecessary delays in development and conflicts in the selection of potential treatments and the design of clinical trials.
Harnessing the expertise and input of the SAG enables Ellipses Pharma to capture a wider range of specialist views, leading to better decisions. Oncologists from leading cancer centres and research establishments around the world provide reviews of the scientific and clinical trial data for each asset alongside insights into local practices, patient populations and evidence of the competitive landscape.
Enabling targeted cancer treatment
Feedback is gathered from 50–70 experts simultaneously on each medicine taken forward. This scientific consensus can de-risk the development of new drugs by better understanding which patients will have the most benefit from each medicine.
The feedback can reveal new opportunities for those who may be candidates for the drug, for example, by showing that a particular molecule has applications in cancers that mutate and escape existing treatments, as well as in the tumours that it was originally intended to treat.
Increasing chances of success
The input from the SAG facilitates the adaptation of drug development in response to new data, with experts commenting on clinical trial design, patient stratification, biomarker selection and how to increase the chances of successfully developing a new drug.
The approach means the drug development company can open studies and enrol trial participants faster while the constant engagement with experts enables modification of treatment protocols, using real-world data from their clinics.
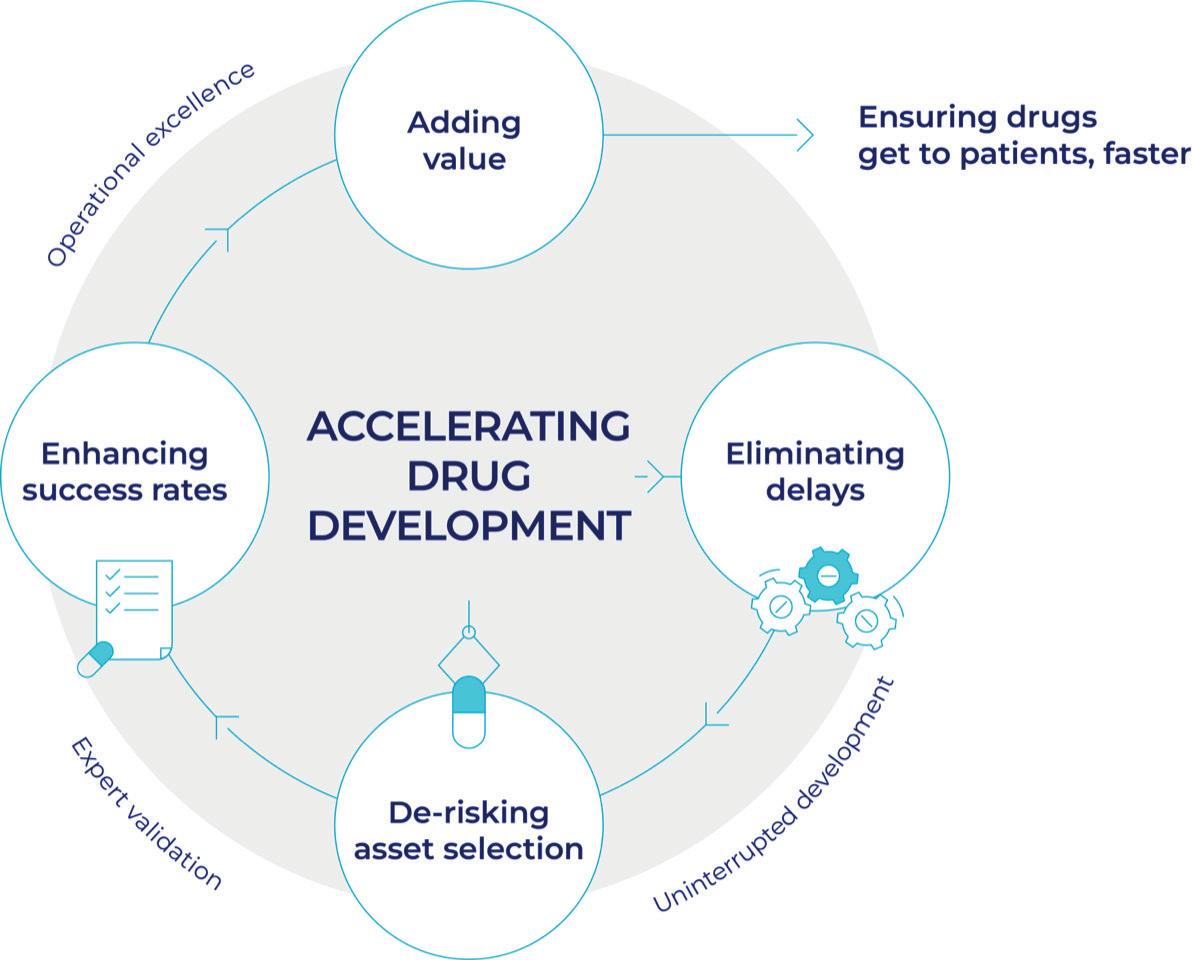
Fulfilment for oncology experts
The value of the approach is acknowledged by participating experts. A Newcastle University professor praised the ability to ‘evaluate in stages’ and complete work in their ‘own time, when more convenient’ while a professor at
Cambridge University described the role as ‘fulfilling academically and altruistically.’
An investigational cancer therapeutics specialist at the University of Texas, USA, adds: “Being part of the SAG allows me to make an impact in an even earlier stage of an asset when the investment decisions are made.”

Improving therapies while lowering costs
Early evidence shows that the approach is working. Seven of the nine potential treatments, so far, chosen and developed with expert input remain in active development, putting the company above the conventional one-in-eight success rate seen in cancer development.
The company, which plans to expand its SAG membership to 300, says that further increasing the success rate will mean more approved therapies for patients and lower drug development costs. Several of their medicines and clinical trials — treating a broad range of cancers including lung, thyroid, breast cancer and leukaemia — are now gaining international attention. Recently, the progress of Ellipses drugs currently in trials was reported to the prestigious American Society of Clinical Oncology conference.
04 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
SPREAD WRITTEN BY Mark Nicholls
INTERVIEW WITH
Professor Sir
Chris Evans
Chairman & Founder, Ellipses Pharma Image provided by Ellipses Pharma
Think like cancer to beat cancer: the race to develop better medicines
To beat cancer, drug developers need to “think like cancer.” That is the view of Dr Rajan Jethwa, chief executive and founder of Ellipses Pharma, who adds: “We need to constantly evolve, continually multiply and rapidly accelerate.” This, he believes, is the quickest way to get safe and effective drugs to patients when and where they need them.
Accelerating process to clinical trials

For a drug development company, that means a focus on accelerating the development of cancer medicines and treatments through innovative models. Pivotal to that is a combination of unbiased vetting to de-risk initial asset or drug candidate selection, with an uninterrupted funding flow to minimise the time it takes to advance products through clinical trials and reach patients.
Expanding on this approach adopted by the UK-based drug firm, its chairman and founder, Professor, Sir Chris Evans, says: “We are committed to maximising the breakthrough potential of the nascent treatments we take on, streamline their path through the clinic and shorten the time for them to have an impact on patients. Better, faster trials will mean more drugs for patients and more lives saved.”
Unique drug development proposition
With an expanding pipeline of potential new medicines, the company is rapidly advancing its disruptive drug development proposition.
Central to that is the blind review
process it has introduced with the Scientific Affairs Group — a global network of renowned cancer experts covering a range of cancer specialities with input from members focused on identifying the science with the clearest path toward translation into clinical application.
Once Ellipses adopts a potential medicine, the clinical and business development programmes are jointly built around clinical trials focused on patient needs and the commercial requirements for taking the drug forward.

Developing medicines for any cancer type
Their drug development model centres on having a robust and diverse pipeline — from late preclinical to clinical stage and from solid tumours to blood cancers. It addresses more than a dozen different types of cancers, including acute myeloid leukaemia (AML), breast cancer, lung cancer, thyroid cancer and others.
Medicines in development stages range from preclinical/preinvestigational new drug (IND) to phase 2 clinical studies and encompass several therapeutic modalities, including small molecules, receptor modulators, fusion proteins and even nanoparticle drug conjugates. The pipeline also contains additional exploratory programmes in several bispecific, bifunctional and monoclonal antibodies to treat a range of tumours.
Uninterrupted clinical trials
An uninterrupted funding model allows the company to allocate capital to each new potential drug as soon as it is needed.
Coupled with agile patient recruitment strategies, they can design novel and effective clinical trials.
Dr Jethwa adds: “We have built a streamlined drug development engine that scales with asset acquisitions, ensuring we are always ready to run high-quality trials at the right time.
“By decoupling our fundraising from the asset development cycle, we can provide uninterrupted financial support for each development programme as required by individual programme needs and timelines.”
Wider accessibility to cancer therapies
Professor Evans adds: “Our mission is to make the very best drugs and therapies available — at unprecedented speed, to patients worldwide. To achieve this goal, we seek out scientific discoveries with the best chances of success, regardless of tumour type, development stage, molecular target or therapeutic modality.”
“Traditional drug development models have failed to keep pace with the speed and scale of cancer, so we decided to adopt a bold and ambitious approach that limits operational risk and maximises outcomes for patients,” says Dr Jethwa.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 05 MEDIAPLANET Find out more at ellipses.life
A fresh approach to cancer drug development can help minimise the time it takes to advance therapies through clinical trials and get them to patients.
Spread paid for by Ellipses Pharma
We seek out scientific discoveries with the best chances of success.
INTERVIEW WITH Dr Rajan Jethwa CEO & Founder, Ellipses Pharma
Traditional drug development models have failed to keep pace with the speed and scale of cancer.
New collaboration to improve access to quality cancer management in LMICs
More responsibility for cancer pharmacists and pharmacy technicians to improve care
Traditionally, the role of cancer pharmacists focused on prescription verification (the process of checking a prescription for appropriateness and accuracy) and the compounding of cancer medicines. Over the years, the role has become more clinical.
There is a huge gap in cancer mortality rates between high and lower-resource settings, with 70% of global cancer deaths occurring in low and middle-income countries (LMICs).
The gap in cancer mortality rates is due to non-existent or partial cancer screening strategies, late diagnoses, lack of trained health workers and infrastructures and insufficient inclusion of cancer in universal health coverage schemes. In oncology — breast cancer specifically — early diagnosis, timely treatment and full patient completion of treatment regimens are associated with better health outcomes for patients.
WRITTEN BY Ann-Lise Mikolajczak Manager, Global Health and Access, IFPMA

The World Health Organization (WHO) is partnering with the City Cancer Challenge Foundation (C/Can) to implement the framework of the WHO Global Breast Cancer Initiative (GBCI), which aims to avoid 2.5 million breast cancer deaths globally by 2040.
Partnering to reduce breast cancer mortality
WRITTEN BY Harold Cottin Manager, Engagement and Partnership, City Cancer Challenge Foundation
The WHO GBCI Framework was published in early 2023 and provides a comprehensive approach for countries to address their breast cancer burden. C/Can is a nonprofit foundation that works with cities in LMICs to improve access to cancer care. It will support the WHO with its multisectoral city network to translate GBCI recommendations and national dialogues into actionable work plans.
This innovative collaboration will combine the convening power and global reach of WHO with the ‘on-the-ground’ implementation experience of C/Can — now operating in 13 cities around the world. It also seeks to leverage the resources and expertise of the private sector, which is actively supporting cancer access programmes. Amgen, AstraZeneca, Bristol Myers Squibb and MSD announced their commitment to the initiative with in-kind and financial contributions.
A domino effect for health systems
The capacity-building efforts laid out in the GBCI framework should create the right expertise, infrastructure and policies at city, regional and country levels. Health system improvements will not only benefit people living with breast cancer but can also be applied to other cancers and non-communicable diseases (NCDs).
By effectively combining the expertise and resources from both private and public sectors, this collaboration strives toward a vital common goal: improving the lives of people living with cancer in LMICs and underserved communities in well-resourced countries.
Cancer pharmacists now play an integral role in the multidisciplinary team, advising on all aspects of medicines use in cancer care. Since 2003, pharmacists have been able to train as non-medical prescribers, and the number of pharmacists prescribing within the speciality has grown — providing pharmacist-led and multi-professional clinics to review and optimise individual patients’ treatment.
Pharmacists expand to patient care and clinical leadership

Pharmacy professionals are at the forefront of service improvement, technological innovation and research. Some pharmacists and pharmacy technicians improve patient care by facilitating ‘closer to home’ treatment services such as homecare and self-administration schemes.
Others have developed expertise in genomics or advanced technology medicinal products such as CAR-T cells and gene therapy. In 2005, consultant pharmacist roles were introduced, designed to deliver clinical leadership, promote research and collaborate at a national level to improve practice. There are 161 consultant pharmacists in the UK; only 12 specialise in oncology, but the number is increasing each year.
Pharmacists engage in genomic testing for cancer


One of the biggest developments in recent years has been the incorporation of genomic testing into routine cancer care. In England, the NHS genomic medicine service has employed pharmacists to act as regional leads to advise on the use of genomic testing to improve the safety and efficacy of cancer treatments.


Several genetic tests are now routinely used to identify which patients are likely to benefit from specific treatments and to identify those at greater risk of side effects. Cancer pharmacists can advise on the choice of treatment and any necessary dose modifications required based on the results of these tests.
Pharmacy technicians in medicine management
The pharmacy technician role is also evolving. Traditionally a supporting role, they now take the lead in medicines preparation, medicines management and patient counselling, with some developing extended roles such as prescription verification and medicines administration. Backed up by a team of pharmacy assistants and other support staff, they ensure a safe supply of medicines to patients in all areas of the hospital. The increasing clinical roles of pharmacists and pharmacy technicians could contribute to improved patient care across the UK.
WRITTEN BY Emma Foreman Vice Chair, BOPA
WRITTEN BY Jessica Pealing Secretary, BOPA
06 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK
WRITTEN BY Joseph Williams Chair, BOPA
Paid for by BOPA Find out more at bopa.org.uk
WRITTEN BY Nishan Sunthares Managing Director, Diagnostics,

Ways early cancer detection and diagnosis can improve healthcare
Early cancer detection and diagnosis can not only aid with earlier treatment interventions but it also shows potential in minimising cancer risks in the first place.
It is beyond doubt that cancer detected at an early stage saves lives. If diagnosed at the earliest stage, almost all women with breast cancer and more than 9 in 10 people with bowel cancer survive their disease for five years or more. This falls to around 3 in 10 women when breast cancer is diagnosed at the most advanced stage and drops to just 1 in 10 people for those with bowel cancer.
Targets for early cancer diagnosis
Ambitious targets, such as NHS England’s commitment to detecting 75% of cancers at stage I and II by 2028, have improved public awareness. Additionally, more streamlined diagnostic pathways all contribute to shifting our ability to accurately detect and diagnose cancer at an early stage. Yet, the true potential of early detection and diagnosis remains largely unexploited.
Multi-cancer early detection (MCED) tests have the potential to find more than one type of cancer from a single blood sample and revolutionise cancer screening. Investment in and research into the effectiveness of MCEDs continues apace.
How AI can aid diagnosis and treatment
As the amount of data generated from an individual’s healthcare journey increases, the application of artificial intelligence (AI) is expanding to determine new approaches

for cancer detection, screening and diagnosis. AI tools enable the incorporation and computational analysis of disparate, complex data streams to inform predictive treatment models, rendering possible precision oncology and personalised medicine.
Genome sequencing to minimise risk
At a molecular level, advances in genome sequencing provide evidence of genetic mutations which might predispose a patient to cancer. A route to risk-based detection and prevention is starting to emerge to support a life course approach to minimising risk factors and enhancing protective factors through evidence-based interventions at important life stages.
Accelerating early detection and diagnosis
Beyond the clear potential for health benefits, a shift to early diagnosis can alleviate the need for costly, long-term treatments, thus aiding the clinical workforce and easing pressures on the healthcare system itself. The UK can be a world leader in developing a thriving early detection and diagnosis industry, capitalising on its excellent science base, the unmatched diversity of health data and infrastructure and a history of collaborative efforts across an interlinked network of expertise.
A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK 07 MEDIAPLANET
ABHI
AI tools enable the incorporation and computational analysis of disparate, complex data streams to inform predictive treatment models.
Pharmacy professionals are at the forefront of service improvement, technological innovation and research.
~BOPA, Page 06

08 MEDIAPLANET A PROMOTIONAL SUPPLEMENT DISTRIBUTED ON BEHALF OF MEDIAPLANET, WHICH TAKES SOLE RESPONSIBILITY FOR ITS CONTENTS READ MORE AT HEALTHAWARENESS.CO.UK