RN Case Manager Helps Clients Find Long-Term Care
AI for Virtual Scribing: Opportunities and Pitfalls
Upcoming Fall & Winter Events


RN Case Manager Helps Clients Find Long-Term Care
AI for Virtual Scribing: Opportunities and Pitfalls
Upcoming Fall & Winter Events





Our pediatric specialty care is designed to meet families right where they are. At South Dakota’s only free-standing hospital just for kids, our team is specially trained to care for children with complex or chronic conditions, injuries and illnesses. Sanford Children’s Hospital 1600 W. 22nd St. (605) 312-1000 sanfordhealth.org/childrens-care

all in one place


VOLUME 15, NO. 6 ■ SEPTEMBER/OCTOBER

Douglas County Memorial Hospital nurses Misty Faulkner, Sydnaya Dunn, and Jessica Wright
■ By
Alex Strauss
South Dakota’s innovative approach to healing its rural healthcare gap is yielding results. Meet a recruitment success story and discover how state programs, from ‘Scrubs’ camps to loan repayments and rural residency, are cultivating a new generation of rural providers and keeping them in small communities.
Cover story photos by Scott Ymker
PAGE 6 | This Month Online
South Dakota moves up the ranks for best healthcare states, how to share your fall and winter events, and exclusive online content
PAGE 12 | [Sponsored]
RN Case Manager Joyfully Helps Clients Find Long-Term Care
Meet the RN case manager who’s transforming the long-term care experience for North Dakota families, one placement at a time.
PAGE 14 | Virtual Scribing:
Using AI in Medical Practices
■ By Alan Lembitz, MD
AI scribes in the exam room: revolutionary tool or regulatory minefield? Discover the crucial considerations for implementation.
PAGE 16 | NEWS & NOTES
A new Chief Mission Officer for Avera, Monument Health expands its urgent care coverage, Sanford hosts its 3rd Future of Rural Health Care Summit, and more
PAGE 19 | [Sponsored]
Dollars & Sense: Sioux Falls Doctors Value Trusted Partnership with their Banking Expert
PAGE 19 | [Sponsored]
USD School of Health Sciences
Success Spotlight: Nicole Freeman
PAGE 22 | [Sponsored]
Putting Pork on Your Plate this ‘Porktober’ and Beyond From farm to fork: A dietitian with a farm background explores pork’s unexpected health benefits and its modern lean profile
PAGE 23 | Upcoming Regional Events
STEFFANIE LISTON-HOLTROP
VP Sales & Marketing
appy Fall from all of us here at MED! It happens every year about this time . . . As the summer winds down, the news and events start ramping up. We have a full lineup of both for you in this issue. You'll find all the latest news including headlines you might have missed over the summer in News & Notes and some highlighted events on the inside back cover. Be sure to visit the website to see the full calendar (and submit your own events).
HPublisher / MED MAGAZINE, LLC
Sioux Falls, South Dakota
Vice President Sales & Marketing
STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Magazine Design / ANGELA CORBO GIER
Client Relationship Manager / BARBIE MUNOZ
Digital Media Director / HYA AMURAO
605-366-1479
Steff@MidwestMedicalEdition.com
ALEX STRAUSS
Editor in Chief
605-759-3295
Alex@ MidwestMedicalEdition.com
WEBSITE MidwestMedicalEdition.com
MAILING ADDRESS
PO Box 90646, Sioux Falls, SD 57109
On the cover of this issue, we are delighted to showcase a rural healthcare recruitment success story and some of the innovative state programs that helped make it possible. As workforce remains a major focus for facilities across South Dakota, we take a closer look at what's working now.
Also in this issue, the experts at COPIC take a deep dive into the emerging trend of virtual scribing using AI tools. Plus, you'll meet a Sanford case manager who finds joy in helping others navigate the complexities of long-term care.
We trust you will enjoy this issue of MED Magazine and hope to see some of you at SDAHO in September!
All the Best, Alex & Steff
JAN/FEB Dec 10
10
APRIL/MAY March 10
NEXT ISSUE
10
10
Editorial contributions due October 5
Ads due October 10
Children’s Nebraska’s pediatric surgeons understand the profound impact of expert, compassionate care for children and their families. As the largest and most experienced pediatric surgical team in the region, it offers unmatched comprehensive care across the full spectrum of surgical interventions – including special expertise in moderate to severe cases of chest wall deformities such as pectus excavatum and pectus carinatum.

“About 18 months ago, we started adding cryoablation to our pectus procedures,” explains Dr. Cusick. “This technique freezes four nerves, providing numbness for 3-6 months after surgery. It has been a game changer.”
“For a long time, we called pectus a cosmetic procedure, but recent studies show it can improve heart and lung function as well.” says Children’s pediatric surgeon Robert Cusick, M.D. “I love taking care of these patients because often the physical appearance can hurt their self-confidence at a key point in adolescence. These procedures can have drastic changes on their self-esteem.”
Located in Children’s state-of-the-art Hubbard Center for Children, which opened in 2021, the surgical team provides an exceptional, family-centered experience. The world-class surgical suites are equipped to offer minimally invasive surgical interventions, advanced robot-assisted technologies and techniques that promote faster recovery and healing, less pain, lower rates of infection and fewer complications. Each surgery is led by a multidisciplinary pediatric team with specialized pain management techniques, including cryotherapy and cryoablation.

Scan the QR code to learn more about Children’s pectus surgery team.
With a combined 100 years of experience, the Pediatric Surgery team is committed to keeping each child safe and comfortable throughout their entire surgical journey, from clinic consultation to the operating room and recovery. Children’s also offers surgical treatments for various medical conditions with expertise in bariatrics, colorectal issues, hernias, oncology, thyroid conditions and more.
“There is no greater privilege than caring for a sick child,” says Dr. Cusick. “Education and research allow us to improve children’s health into the future, but nothing matters more to our team than caring for and healing our patients today. Patients and their families deserve the best in surgical skills, compassion and a trusting relationship.”
The Pediatric Surgery division at Children’s continues to grow and innovate to meet the needs of children and families. Abdalla Zarroug, M.D., Robert Cusick, M.D., Megan Fuller, M.D., Kathy Schall, M.D., Adil Shah, MBBS, Melissa Suh, M.D., and Patrick Thomas, M.D., collaborate and embrace innovation, utilizing the latest techniques and technologies to deliver optimal care for pediatric patients.
This South Dakota company is silently transforming healthcare facilities across the Midwest, potentially including yours. Discover how this Rapid City-based innovator is tackling a critical issue plaguing medical staff daily. Learn about the surprising cost savings and unique approach that’s making waves in rural hospitals. Find out why their solution might be the key to retaining your best talent.

The 2024 SDAHO Annual Convention has announced a keynote speaker whose journey from battlefield to podium is sure to inspire this year’s attendees. A decorated veteran who faced a career-ending injury now leads extreme adventure races and uplifts thousands. With 27 military awards and an ESPY to her name, she also brings an unexpected companion to the stage. Learn more about the woman who’s set to galvanize South Dakota’s healthcare leaders this year.

A devastating stroke at 52 left David Hobler with 90% vision loss and paralyzed on one side. Two years later, he made a decision that would change everything. Discover how this South Dakota native’s journey led him from an engineering career to a USD nursing degree, the surprising statement he made about his stroke, and what unexpected offer from his mother set it all in motion.
SOUTH DAKOTA has made a remarkable leap in WalletHub’s 2024 “States with the Best & Worst Health Care” report, climbing to 3rd place overall from 9th last year. This comprehensive study, which evaluated 50 states and the District of Columbia across 44 key measures, highlights South Dakota’s strengths in several critical areas.
The state particularly excels in emergency care, ranking 3rd for average ER wait times. It also performs well in preventive care access, placing 9th for both hospital beds per capita and the percentage of at-risk adults with routine doctor visits. Dental care accessibility is another strong point, with South Dakota ranking 7th for adults receiving annual dental visits.
While the state shows strong performance in most areas, there’s room for improvement in retaining medical residents, where South Dakota ranks 21st. (See this month’s cover story for more on the ongoing efforts to attract and retain medical talent in the state.)
For a detailed breakdown of South Dakota’s performance across all 44 measures and to understand the implications for our healthcare system, visit our website to read the full report.
Overall Rank: 3rd
9 th Hospital Beds per Capita
3rd Average ER Wait Time
9 th % of At-Risk Adults with No Routine Doctor Visit in Past Two Years
7th % of Adults with No Dental Visit in Past Year
21st % of Medical Residents Retained
(1=Best; 25=Average)

FTER CHANGING HIS major from engineering to nursing, Dalten Bremer knew he wanted to work in a rural setting. His time at the University of South Dakota has only solidified his passion for serving a
Bremer, who is originally from the 500-person town of Ocheyedan, Iowa, initially pursued a degree in engineering at the University of Iowa. However, after working at a group home for people with intellectual disabilities, he discovered a calling in nursing. Bremer said he chose to attend USD to pursue his nursing degree because of its focus on rural healthcare.
“From the beginning, I wanted to work in a rural area,” said Bremer. “During my time so far in the USD nursing program, my passion for rural nursing has only grown. Our professors in the nursing program do a great job at highlighting what nursing looks like in both rural and urban areas. This helped me to solidify my desire to work in rural areas. Healthcare in rural areas faces unique challenges, and my goal is to be a part in dealing with these challenges and overcoming them.”
This summer, Bremer had the opportunity to work in a rural healthcare setting at Freeman Regional Health, an affiliate of Avera Health, in Freeman, South Dakota.
His experience was part of a grant from the Health Resources and Services Administration (HRSA) that provides students with real-world experiences in a rural clinical setting.
“It was an amazing learning experience,” Bremer says.
The Fall and Winter are a busy time for healthcare-related events throughout the region. (See our inside back cover for a few of them) If your organization is planning an event for healthcare professionals — whether it’s an awards banquet, a fundraiser, a CME opportunity, or something else — MED can help you spread the news to our thousands of website visitors and digital newsletter subscribers.












BY ALEX STRAUSS
ACROSS SOUTH DAKOTA, FROM the biggest cities to the smallest towns, a healthcare workforce crisis continues to unfold. While medical facilities in Sioux Falls and Rapid City are struggling to fill positions, rural communities face an even more acute shortage of providers with nurses topping the list of most in-demand positions..
Paradoxically, South Dakota’s distinction as the state with the lowest unemployment rate in the nation has only made matters worse. While that distinction is evidence of a robust economy, with so few job seekers to fill the open positions, it’s even harder to fully-staff healthcare facilities statewide.
But even in the midst of these challenges, there are success stories, thanks, in large part, to a host of state programs designed to cultivate and support the rural healthcare workforce. Dr. Maurice Chessmore, a family physician at Douglas

County Memorial Hospital in Armour, South Dakota is one such story.
Just two years out of residency, Dr. Chessmore serves as the sole physician for the town of about 600. His journey from business major to rural doctor showcases the potential of targeted recruitment initiatives coupled with personal commitment and offers some valuable insights into how South Dakota is working to heal its healthcare gaps.
SMALL-TOWN ROOTS, BIG MEDICAL DREAMS
Maurice Chessmore is no stranger to rural life. Raised in small towns with populations under 2,000, he initially charted a course for the financial sector and earned his undergraduate degree in business administration. But he quickly found that banking was not his calling.
“I just wasn’t enjoying it,” says Chessmore who, at the time, was already a father of three. “I came home one day and asked my wife if she
thought it would be OK if I pivoted to healthcare.”
As Chessmore progressed through his medical education at the University of Nebraska Medical Center in Omaha, he was drawn to the breadth of family medicine, even though he was worried about paying off student loans on the salary of a rural primary care physician.
“Once I decided on family medicine, I knew without a doubt that I wanted to be in a rural area,” he says.”But my biggest fear when I was looking at family medicine was my medical school debt.”
Dr. Chessmore would eventually find out that South Dakota was eager to help him. In the meantime, he made the leap into primary care on faith. After medical school, he had his first experience with one of the leading tools South Dakota relies on to develop its rural healthcare workforce —the Pierre Rural Family Medicine Residency Program.
Supported by the South Dakota Health Department and run through the Center for Family Medicine in Sioux Falls, the program is specifically designed to prepare physicians for the diverse demands of rural practice.
Residents spend their first year in Sioux Falls, gaining exposure to a wide range of medical specialties and procedures. They then transition to Pierre for their final two years, where they immerse themselves in the realities of rural healthcare delivery.
“There are not a lot of programs that train people to do a little bit of everything, which is what is needed when you are a rural provider,” says Dr. Chessmore. “I felt like the Pierre program did a great job. When I came
to Douglas County Memorial Hospital in Armour, I couldn’t have been better prepared.”
“At the South Dakota Office of Rural Health, our whole mission is to ensure access to healthcare in rural South Dakota,” says Kaitlin Sherer, Administrator of the South Dakota Health Department’s Office of Rural Health, underscoring the program’s strategic importance. “The residency program is the result of the governor’s Primary Care Task Force in 2012 aimed at increasing primary care in rural communities.”
The program is banking on statistics showing that physicians trained in rural settings are more likely to practice in similar environments post-residency.
After residency, a second South Dakota initiative came into play for Chessmore, who was weighing two job prospects — one in his home state of Nebraska and one in Armour, South Dakota.
“When it came down to it, the South Dakota recruitment program was significantly better,” he says. Through the South Dakota Department of Health’s Recruitment Assistance Program, physicians like Chessmore, as well as nurse practitioners, physician assistants, midwives, and dentists, can receive incentive payments for commiting to practice for three years in a community of fewer than 10,000 people.
A second recruitment program —the Rural Health Facility Recruitment Assistance Program— covers an even broader array of professionals including nurses, dieticians, physical,


As the town's only primary care physician, Dr. Chessmore sees patients of all ages.

occupational, and speech therapists, laboratory technologists, pharma cists, social workers, and more.

This facility-based recruitment program also offers financial incentives for working three years in a small community, but the cost is shared by the facility and the Department of Health. The smaller the community, the larger the share the state will shoulder.
“We also have a state loan repayment program that covers about 30 professions If they practice in a health profession shortfall area as designated by the Health Resources

and Services Administration,” says Sherer. “When they make a threeyear commitment, we actually pay the financial institution, as long as the student has qualifying educational loans of $30,000 or less.”
The recruitment and loan repayment programs are not the only ways South Dakota is seeking to build its rural healthcare workforce. In fact, Sherer says the efforts start as early as junior high school in many communities, where state-sponsored ‘Scrubs’ camps introduce students to healthcare career options.
High school students are eligible to attend longer ‘Camp Med’ events where they have more hands-on opportunities, like suturing pig’s feet, making a cast, or injecting a hotdog. For college students, there is the Rural Experiences for Health Professions Students (REPS) program.
“This is a program that pairs up health professions students to spend a four-week rotation in a rural community,” says Sherer. “What is cool about this is that it pairs folks up interdisciplinarily, because that is how healthcare is being delivered when you are working in a facility.”
“We are at a pivotal moment in our journey to advance public health in

South Dakota,” says Department of Health Secretary Melissa Magstadt. “From the groundbreaking of our Workforce Development and Education Center in April to the workforce summit in August to the rural healthcare incentive programs we offer, and the work that we continue to navigate with our tribal partners, my team and I are committed to enhancing the health and well-being of our fellow South Dakotans.”
As for Dr. Chessmore, he is happy with his choice and grateful for the programs and incentives that helped him get here. He starts each day with rounds at the critical access hospital (if there are inpatients) before opening his clinic. If an emergency comes through the ER, his patients know he must drop what he’s doing and go. He takes call one day a week and one weekend a month and sees patients for a few hours on Saturday mornings.
“Rural life is pretty good,” says Chessmore. “I am the only physician here but we have one nurse practitioner and three full-time physician assistants. The group takes turns staffing the Armour clinic and two outreach facilities in Corsica and Stickney. “In Armour, there are five of us that rotate through the clinic depending on the day of the week.
Dr. Maurice Chessmore and colleagues (l to r) nurse Brenda Punt, Jennifer Bietz, PA, and nurses Samantha Menning and Jenna Leibel
There are usually up to three of us there each day.”
Overall, the arrangement has made rural practice more enjoyable for Chessmore than it might otherwise be.
“I’m lucky to be in a place where people understand the challenges of rural medicine and they have created an environment where there is less stress,” he says. “When a provider doesn’t stay in a community, you have to look at the whole picture. Sometimes it’s the environment, sometimes it’s the administration, sometimes it’s a fellow provider that pushes them out. There’s not one easy fix.”
Melissa Magstadt agrees that good communication and flexibility are critical to attracting and maintaining a strong healthcare workforce, regardless of the size of the community.
“Managers, administrators, physicians, and other providers have to be willing to get creative in order to retain their employees,” says Magstadt. “Stay open and relevant, offer shared shifts and remote work, if possible. Employees have high expectations and it is up to us, as leaders, to stay accountable and committed to those whenever possible.”
Those kinds of creative approaches took center stage at the Department of Health’s first Healthcare Revolution Workforce Summit in Pierre in August, where the goal was to build on the momentum the state has established and take the lessons from success stories like Chessmore’s.
“We are always looking at problems, but do we ever look at what is working really well?” says Sherer. “The workforce summit was a chance to look at what’s working now and ask ‘What are they doing right?’” ❖



SPONSORED ]

FOR MANY individuals and their families, finding placement in a long-term care center is a difficult and exhausting process. Having the help of a dedicated RN case manager in these scenarios can be an immense blessing for them.
RN case managers, like Brenda Holm of Good Samaritan Society, understand the system and the struggles these families face. And for people like Brenda, filling the role is more than a job — it’s a satisfying way to serve others.
BRENDA’S DECADES OF WORK IN LONG-TERM CARE
Brenda has spent most of her working life in long-term care, and she credits a lot of her
success to her previous roles in the organization.
“I’ve done a little bit of everything, from floor nurse to minimum data set coordinator,” said Brenda. “I started out with long-term care at Sanford Health, and then later joined a joint venture between Sanford Health and Good Samaritan Society called Prospera before they decided to fully combine in 2017. I’m still a part of the same organization after 23 years.”
Starting out as an RN gave Brenda a good perspective on what it means to provide care. She has always believed it’s crucial to develop a trusting relationship with patients and their families so they can reach their shared goal.
“One of the things I like the
most about my job is visiting with the potential resident and their family members,” said Brenda. “I love hearing their voices go from unsure to joyful and relieved. It’s my job to be a source of positivity for them, and by the end of conversations we end up forming a friendly bond with each other.”
These relationship-building moments encourage Brenda, and they help her approach the other aspects of her job with renewed energy.
HOW BRENDA HELPS PEOPLE GET THE CARE THEY NEED
Navigating the world of longterm care is no small task.
It requires diligence and a lot of specialized knowledge
to understand the process and effectively communicate with regulators, officials and providers.
As an RN case manager for four Good Samaritan Society locations in the Bismarck-Mandan area of North Dakota, Brenda helps people in need find a safe long-term care solution. Because of the complexities of each case, her work can be difficult, but Brenda doesn’t like to back away from a challenge.
“Our clients come from a lot of care settings, whether it’s in acute care, at home, or in another facility,” said Brenda. “Sometimes they are unsure of what the next step is going to be for them and how they’re going to get care. Our job is to help meet the needs of these applicants and their families, to resolve their medical issues, and to improve their quality of life.”
Many families struggle to provide care to their loved ones, especially if their loved one has a lot of care needs or lives a long distance away from their family. Long-term care can bring an amazing sense of relief to the entire family, but overcoming the access barriers can be tough. Those barriers motivate Brenda to do everything she can to help her clients.
“I like helping people in their moment of need,” said Brenda. “Family members often act as caretakers, so if I can help them find a safe place for their loved one to live, I can help them just be a family member again. It gives me a great amount of satisfaction knowing we can help those people.”
Having a dynamic and supportive team to work alongside is a huge benefit at any job, but when it comes to working in
long-term care, it’s a necessity.

Sanford Health and Good Samar itan Society, Brenda has worked with outstanding coworkers who value her input and help her with anything she needs. ment. There’s so much teamwork,” said Brenda. “When I’m having a tough day, I know I can reach out to my coworkers for support, and on other days I get to pay it forward and help them, even if it isn’t related to work.”
Her team is great at what they do, and a lot of this success comes from their manager who serves as a voice of reason and key motivator.
“She has been such a great career builder for me,” said Brenda. “I want to stay here because we have great resources that help us be the best we can be.”
Above all, Brenda is extremely grateful for Good Samaritan
thankful I work for this organization, and I think my job is just awesome. God has blessed me beyond belief.”
Careers at the Good Samaritan Society have excellent pay, comprehensive benefits, and above all, the opportunity to serve residents and clients. If you’re looking for a rewarding career with plenty of room to grow, start exploring our open positions today at sanfordcareers. com/good-samaritan-society. ❖

BY ALAN LEMBITZ, MD
TH E BENEFITS OF USING AI TOOLS to quickly and accurately generate a record of clinical interactions are obvious. However, there are many considerations to examine before implementing the use of such tools.
Patients will need to be aware of and consent to the use of the recording devices in place to generate the records. Providers will need to learn to “narrate their examinations” to populate the record. A policy to erase the work product of the recording at regular, short intervals, as well as open access to the final record generated from that work product will help allay patients’ fears about how their information was captured and what is going in their permanent medical record.
The need to provide the processes required by the Cures Act will be even more important. One can also predict that patients’ awareness of the record and their requests to edit, amend, or delete materials in it will increase and the provider or their staff will need to be cognizant of the necessary HIPAA processes and documentation.
Is a HIPAA business associate agreement necessary?
Yes. Since AI/scribe functionality will almost invariably involve Protected Health Information (PHI), a Business Associate Agreement (BAA) is required by the HIPAA Privacy and Security Rules.
Do patients need to consent to the remote AI scribing? Verbal or written? What are the elements of that consent?
This depends entirely on state regulations. For “two party” states, where consent is required from both
Finally, and most importantly, given how AI works and its inherent ability to produce fluent but possibly inaccurate, misleading, or even harmful output, the provider will absolutely need to read and verify the content of the notes generated by AI. The option of “dictated but not read,” in this case becomes “AI generated but not read” and will not be an accepted practice.
parties to record a conversation, it is absolutely necessary to obtain patient consent. For “one-party” states in which both parties are not required to consent to recording, this may not be a legal necessity, but is still strongly encouraged. There are many ways to obtain this consent. It can be incorporated into a broader consent form that a patient might sign at the onset of treatment, or can be a specific document. The current state of the industry seems to be that providers obtain verbal consent which is then documented in the chart. That seems to be the minimum necessary standard that most healthcare organizations are using.
How long does the recording last and is it destroyed once the medical record is created?
This is completely vendor-dependent and not covered by any particular regulation. One major industry leader currently states that they hold on to the recordings for one full year, but we are seeing a trend towards the holding period becoming shorter. The medical record that was created from the recording is subject to the rules and policies for medical record retention and accessibility.
In the past, some providers included disclaimers about the possible irregularities of voice recognition (although our legal advice frowned against that, as it provided no relief and simply stated you were aware that it had errors and didn’t take steps to fix them). Is the healthcare community using disclaimers like this?
While guidance in the previous question states that transparency that AI was used to generate the clinical record is a best practice, the community is (rightly) moving away from additional disclaimers beyond that. They offer no real protection and may actually increase potential liability. By signing a document, providers are responsible for the content of that document, regardless of how that content was created. If some sort of disclaimer is still desired, a better practice would be to say something like “This document was created in part by using voice recognition software and was reviewed by the author. If errors are present, please bring them to our attention.” ❖
Information in this article is for general educational purposes and is not intended to establish practice guidelines or provide legal advice.

Sioux Falls physicians Muhammad Khan, MD, and his wife Maryam Sheikh, MD, specialize in managing the complex medical needs of hospitalized patients. So when it came to managing the complexities of their finances, they didn’t hesitate to hire a specialist.
“Liz’s role for us is similar to the role we play for our patients,” says Dr. Khan of Elizabeth Carlson, vice president of Private Banking at American Bank & Trust in Sioux Falls. “We never feel like she is working for a bank. She works for us and she is there to help us figure out what is best for us. We can gain literacy, but we will never have her knowledge and credentials.”

Carlson’s credentials are impressive. She helped launch AB&T’s private banking department and specializes in managing even the most intricate financial situations for high-net worth clients. It’s an approach that Sheikh and Khan say is essential for busy healthcare professionals.
“I think sometimes physicians don’t even realize that this kind of service is available to them,” says Dr. Sheikh. “But with both of us working full time, Liz’s flexibility and ease of communication have been invaluable to us. She has actually come to the hospital to bring us documents or come to our home to get things notarized.”
Khan and Sheikh, who own property internationally, even recalled a time when Liz met them at the airport to facilitate an international wire transfer prior to a flight.
“Maybe 50 years ago, you would hear of people doing that kind of thing, but it’s rare these days,” says Dr. Khan. “Doctors don’t do home calls anymore and a lot of people don’t go out of their way to help with things the way Liz does.”
As much as they appreciate her service, Khan and Sheikh say it is their trusting relationship with Carlson that they value most.
“We tell her our goals and she figures out how to get it handled,” says Dr. Khan. “That is the best.”

Monument Health has begun construction on two new standalone urgent care locations in the Rapid City area. The first clinic will be in Box Elder, offering urgent and primary care services. A second location will open in Rapid Valley in Fall 2025. These additions will bring the total number of Monument Health urgent care centers to four in the Rapid City area. As a TRICARE Network Provider, Monument Health supports military personnel and their families with local care options


Howard, South Dakota-based Horizon Health hosted its annual Circle of Care Awards recognition event August 6 to recognize outstanding contributions by staff members and donors.
The Keeping Communities Well Award recognizes an outstanding clinical team that demonstrates excellence in quality, patient care, community involvement, and Horizon’s core values. This year’s award was presented to Howard Medical and Dental Teams.
The Team on a Mission Award recognizes an outstanding administrative/support team that takes initiative to improve the organization’s values, efficiency of services, and processes that continue to move the Horizon mission forward. The award was presented to both the Marketing and the Information Technology Team.
The Outstanding Philanthropic Corporation Award was presented to Rivers Edge Bank for outstanding commitment to Horizon initiatives through financial support and encouraging others to take leadership roles toward philanthropy and community involvement.
The Outstanding Philanthropist Award was presented to the family of Jim Burg posthumously. Jim was a longtime member of the Foundation board and lifelong public servant to South Dakota.
Dave Belde, PhD, has been appointed Chief Mission Officer for Avera Health. Belde brings 25 years of executive leadership experience in Catholic health care and mission-based leadership. He will provide strategic direction in integrating the mission, vision, and values of the Benedictine and Presentation Sisters into Avera’s Catholic health ministry. Belde’s responsibilities include formation, ecclesial relations, Catholic ministry identity, ethics, and workplace spirituality. He will begin his role on September 16.

Monument Health has begun construction on one of two new standalone urgent care locations planned for the Rapid City area. The first new location will be located near Liberty Plaza in Box Elder. Another clinic will open in Rapid Valley in Fall 2025. These additions will bring the total number of Monument Health urgent care centers to four in the Rapid City area.

Prairie Lakes Healthcare System has received a five-star quality rating from the Centers for Medicare & Medicaid Services for the second consecutive year. The rating, based on outcomes, patient experience, and processes, places PLHS among the top 8% of U.S. hospitals. PLHS is one of six South Dakota hospitals to receive this designation for 2024. The rating evaluates mortality, safety of care, readmission, patient experience, and timely and effective care.
PLHS has also received the American College of Cardiology’s NCDR Chest Pain – MI Registry Platinum Performance Achievement Award for the second consecutive year. The award recognizes the hospital’s commitment to implementing higher standards of care for heart attack patients. Prairie Lakes demonstrated sustained achievement in the Chest Pain - MI Registry for two consecutive years and performed at the highest level for specific performance measures.
In recognition of these recent achievements, PLHS has been named to Becker’s Hospital Review’s most recent 100 Great Community Hospitals list. Prairie Lakes was one of two South Dakota hospitals on the list.

LifeScape has announced that Nathan Koens, PA-C, has joined the Sanford Pediatric Physical Medicine and Rehabilitation Team and is now accepting patients. Koens holds a Physician Assistant degree from the University of South Dakota and has a background in athletic training, including a role as a baseball athletic trainer at North Dakota State University. He also has experience with 3D motion analysis in runners and has worked as an athletic trainer in an orthopedic walk-in clinic. Koens will focus on neuromusculoskeletal conditions in his pediatric rehabilitation practice.
Dakota Vascular recently celebrated its second anniversary. Over their first two years of operation in Sioux Falls, they have served more than 15,500 patients, performed more than 2,300 successful endovascular procedures, and performed more than 12,000 vascular ultrasounds.

Tamme Davis, DO, has joined the Huron Regional Medical Center medical staff
and HRMC Physicians Clinic women’s health team as of July 8. Specializing in obstetric and postpartum care, complicated pregnancy, and general gynecological care, Davis will work with Rebekah Storm, DNP, and Dr. Nathan Loewen. Davis earned her degree from the University of North Texas Health Science Center and completed her residency at Tulane University. She recently relocated from Washington State.

Jordan Finck, DPM, began his role as HRMC’s first full-time podiatric surgeon on July 22. Finck specializes in foot and ankle injuries, arthritis, and diabetic wounds. He will provide podiatric care and perform surgeries at HRMC. Originally from Madison, South Dakota, Dr. Finck completed his podiatric medicine degree at Des Moines University and his residency at Intermountain Medical Center in Salt Lake City, Utah.

Huron Regional Medical Center has partnered with South Dakota State University Extension on a pilot project for diabetes prevention and education. HRMC received $15,000 in grant funding to utilize community health workers in leading the Better Choices, Better Health SD Diabetes Self-Management Program. The project aims to expand access to diabetes prevention and education across cultures, with plans to train additional facilitators to lead courses in Spanish.

The first BREATHE-SD respiratory care program students began classes for their professional year at three Northern Plains Health Network affiliate hospitals this summer: Huron Regional Medical Center, Madison Regional Health System, and Brookings Health System. The program is part of a $1.5 million Health Resources and Services Administration grant in partnership with South Dakota State University. Respiratory care is a high-need clinical care profession, especially in rural areas. The BREATHE-SD program aims to bring respiratory therapy education and public health opportunities to rural health facilities and the communities they serve.

Leonard Wonnenberg, PA-C, started with the HRMC allied health staff and HRMC Physicians Clinic on July 1. who brings over 12 years of experience from Horizon Health, will provide family and orthopedic care, assisting with surgeries and expanding HRMC’s orthopedic services. A native of Winner, South Dakota, Wonnenberg earned his Master of Science in Physician Assistant Studies from the University of South Dakota.

Pediatrician Sean Schooley, MD, also joined the HRMC Physicians Clinic in July. Schooley will provide comprehensive care for children in the clinic, emergency room, and hospital. He earned his medical degree from the University of Colorado and completed his residency at the Children’s Hospital of the King’s Daughters in Norfolk, Virginia. He recently moved to Huron with his family.
Spencer Hospital in Spencer, Iowa recently received a 5-Star rating from the Centers for Medicare & Medicaid Services, one of only 381 hospitals nationwide to earn this top rating. The hospital is the sole facility in northwest Iowa and one of seven statewide to achieve this distinction. Spencer Hospital was also named one of the country’s Top 20 Rural and Community Hospitals among about 800 mid-sized facilities, maintaining its place on the Top 100 list for nine consecutive years.

Review’s 100 Great Community Hospitals 2024 list. The recognition highlights Brookings Health’s recent honors, including being named a Top 20 Rural Community Hospital for the seventh time and receiving Performance Leadership Awards in quality, outcome, and patient perspective for seven consecutive years. Brookings Health has also been featured on Newsweek ’s list of World’s Best Hospitals for four consecutive years.


Isaac Gerdes has been appointed CEO of Pioneer Memorial Hospital & Health Services in Viborg, South Dakota. Gerdes brings experience in healthcare administration, having led various organizations through periods of growth and improvement. He previously served as CEO of Sanford Webster Medical Center and administrator of Bethesda Home. Gerdes joined Pioneer Memorial at the end of June. He succeeds Lindsey Hauger, who served the organization for nearly twelve years.

Pioneer Memorial Hospital and Health Services’ Laboratory has received a deficiency-free rating from the South Dakota Department of Health. The rating resulted from an evaluation of the laboratory’s compliance with quality and safety standards and Clinical Laboratory Improvement Amendments regulations. The laboratory team provides comprehensive clinical testing in Chemistry, Hematology, Immunology, and Microbiology, demonstrating commitment to high-quality patient care.

Dakota Dermatology has opened a new outreach site at Harmony Hill in Watertown. Dr. Carmen Schwartz, a board-certified dermatologist, will provide care at the new location on Mondays. Services include skin cancer screenings, acne treatment, mole checks, and treatment for rashes and psoriasis.
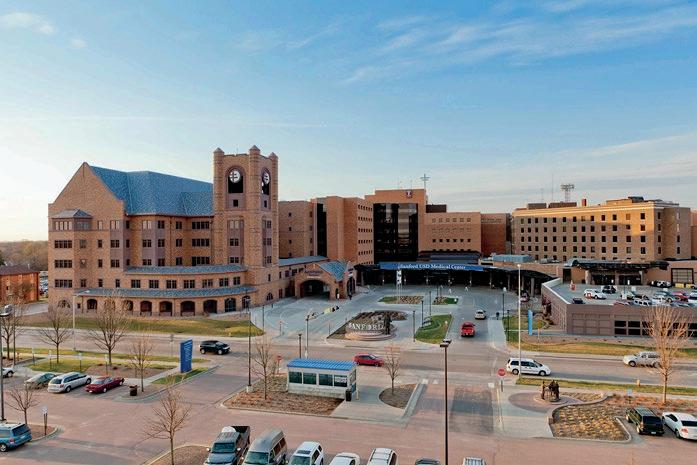
Sanford USD Medical Center has been recognized in Newsweek ’s Best Hospitals 2024 rankings. It’s the only South Dakota hospital named in America’s Best Cardiac, Children’s, and Neurological Hospitals categories. Sanford also made the lists for Best Cancer Hospitals and Pediatric Endocrinology. Rankings are based on nationwide surveys of healthcare professionals and patient experiences, plus hospital quality metrics. Sanford USD Medical Center was previously named South Dakota’s top hospital by U.S. News & World Report
Sanford USD Medical Center has also received the American College of Cardiology’s NCDR Chest Pain – MI Registry Platinum Performance Achievement Award for 2024. It’s one of 259 hospitals nationwide to receive this honor, recognizing sustained achievement in heart attack patient care for 2022 and 2023. The award acknowledges Sanford’s adherence to clinical guidelines and quality improvement efforts. The Chest Pain – MI Registry promotes guideline-based care for heart attack patients, aiming to improve outcomes for the estimated 800,000 Americans who suffer heart attacks annually.
Nicole Freeman, Ed.S, BCBA Degree: Applied Behavior Analyst Certificate
Current Position:
Secondary Autism Integration Specialist, Sioux Falls School District

Teacher and Board Certified Behavior Analyst Nicole Freeman knew early in her career that she wanted to work with students with autism, behavior or learning disabilities. After earning her undergraduate degree in K-12 Special Education, she went on to pursue first an MA as a Specialist of Disabilities and then an Ed.S in Special Education Administration at USD.
“I had a great experience in both of those programs, but I always felt as though there was something missing,” says Freeman.
It turns out that what was “missing” for Freeman was Applied Behavior Analysis, a therapy based on the science of learning and behavior. When the University of South Dakota School of Health Sciences started its ABA graduate certificate program in (2021), Freeman was excited to join a multidisciplinary group of professionals in the first cohort.
“Our classes were 100 percent in person so we really got a lot of hands-on experience,” says Freeman, who still keeps in touch with people from her cohort. “Even now, I know at least six professionals out in the community that I could reach out to if I had a question.”
Beyond the relationships she formed, Freeman says the ABA certificate program, which is now a Master’s level program (MS in Health Sciences with a specialization in Applied Behavior Analysis), equipped her with everything she needs to support students at the highest level.
“Not only did they teach us everything we needed to know to pass the board exam, but we also learned how to really be effective in the community,” says Freeman, currently the Secondary Autism Integration Specialist for the Sioux Falls School District. Next year, she will be a full-time Behavior Analyst working with any student with behavioral or learning challenges.
“Almost everything that we do is applying the behavioral principles that we learned in the program,” says Freeman.
Sanford USD Medical Center received the American Heart Association’s Get With The Guidelines – Heart Failure Gold quality achievement award for improving outcomes for heart failure patients. Sanford USD Medical Center was also recognized on the Target: Heart Failure Honor Roll and received the Target: Type 2 Diabetes Honor Roll award for providing up-to-date care for patients with Type 2 diabetes hospitalized due to heart disease or stroke.

The Good Samaritan Society is expanding its senior services in Rapid City by renovating the former St. Martin Monastery on the Good Samaritan Society – St. Martin Village campus. The project will add 22 assisted living units and 10 memory care units. Currently serving nearly 1,000 seniors in the Black Hills region, the expanded facility will offer priority access to higher levels of care. Construction is expected to be completed and open to residents next Spring.
Sanford Health will host its 3rd annual Summit on the Future of Rural Health Care on October 29 in Sioux Falls. The event will feature speakers including former FDA Commissioner Scott Gottlieb, MD, and leaders from various healthcare organizations. Discussions will focus on harnessing technology and AI in healthcare, expanding access to care, and improving the consumer experience. The summit aims to challenge the status quo and explore new strategies for transforming care delivery in rural America.
Sanford Health has opened its new Medical Building 1 on the hospital campus in Sioux Falls. The first four floors of the five-story building feature 400 parking spaces for employees and staff. The fifth floor houses the Sanford Center for Digestive Health. The 45,000-square-foot Center includes 10 procedure rooms and 40 pre- and post-procedure rooms, with clinic space adjacent to procedure areas. The center also features the first GI fellowship program in the Dakotas, a three-year program for Internal Medicine residents.
❱ Intrigued by something you’ve read here? Want to go deeper? Read the full versions of these and other recent news items on our website.
Sanford Health has been ranked No. 1 in the Government & Non-Profit employers category on Military Friendly Brands’ annual list. The organization offers programs for military and veteran employees, including continuation of benefits and differential pay during deployment. Sanford Health has expanded support through partnerships with the Department of Defense SkillBridge Program and the Military Spouses Employment Program. Veterans applying for jobs at Sanford Health are automatically given screening interviews.

Sanford Health has introduced ImagineYou, a no-cost genetic screening research study in partnership with Helix. The study screens for conditions with increased risk for certain cancers and heart diseases, including familial hypercholesterolemia, hereditary breast and ovarian cancer syndrome, and Lynch syndrome. Participants showing increased risk will receive free genetic counseling. The study aims to help patients and care teams identify potential risk factors and plan for healthier futures.
MercyOne has reached a three-year agreement with UnitedHealthcare, ensuring continued in-network access to MercyOne hospitals, doctors, and specialists for patients covered by UnitedHealthcare Medicare Advantage plans. The agreement allows MercyOne to maintain delivery of high-quality, affordable care and invest in staff, treatments, and health programs, protecting access to care for patients.

The University of South Dakota School of Health Sciences has launched an accelerated RN to Bachelor of Science in Nursing (BSN) program. Working registered nurses can complete the degree in 16 months through eight-week course rotations. The program offers an affordable and flexible way for RNs to earn a BSN degree, with courses available online. Tuition reimbursement is available for enrolled students.

OCTOBER is National Pork month. This is a time when we celebrate the hard-working men and women who work in the pork industry and encourage our consumers to put pork on their plate. We were able to interview Registered Dietitian Nutritionist Charlotte Rommereim to tell us more about the powerhouse that is Pork.
Charlotte Rommereim was raised on a family farm near Alcester, SD, where she showed pigs and cattle and did food and nutrition 4-H projects 4-H. As the youngest girl, Charlotte helped prepare meals for her family, which is where her love of cooking began. Wanting to learn more about food science and nutrition, Charlotte attended SDSU and pursued a degree in nutrition and dietetics. She now lives and works in rural communities as a consultant dietitian to health care facilities in South Dakota and Iowa. With her unique perspective as a dietitian with a lifetime on a family farm, Charlotte Rommereim has been a resource for agriculture organizations in communication to consumers and health professionals. Charlotte shares her expertise in agriculture and its impact on food choices in speaking engagements, media interviews and farm tours. She also encourages conversations about how food is raised and speaks from her perspective of living “farm to fork.”
Let’s take a dive into pork. Lean pork is a nutrient-dense, high-quality source of all-natural

protein. Fresh pork is packed with protein, providing 47% of the recommended Daily Value with 20 grams of protein per 3-ounce serving. Pork is a carrier food, helping consumers add more under-consumed food groups like vegetables and whole grains and nutrients like choline, iron, and potassium. Researchers believe that when pork is on the plate, over 2.5 million children and 5.7 million adults meet their potassium recommendations daily. Fresh pork is a nutritional powerhouse that contributes to health and well-being at various life stages. Fresh pork is one of the lowest cost ways to get the daily recommended amount of protein.
You may ask, what cuts are lean? Eight cuts of pork meet FDA’s guidelines for “lean,” including pork tenderloin, sirloin pork chop, sirloin pork roast, New York pork chop, 96% lean ground pork,
New York pork roast, porterhouse pork chop, and ribeye pork chop. Many cuts of pork are lean and often there may be a misconception that all pork is high in fat. Pig farmers like Charlotte’s family have worked through genetics and nutrition to raise leaner pigs for the consumer. Compared to 30 years ago, pork today has about 16% less fat and 27% less saturated fat. In fact, a pork sirloin chop, sirloin roast and tenderloin all bear the Heart-check Mark from the American Heart Association, indicating they are part of a hearthealthy diet.
Charlotte’s favorite cut of pork is the tenderloin, which happens to be the leanest cut. Pork is a savory protein with a delicious natural flavor that can be accentuated by using your favorite marinades, rubs, sauces, and cooking methods. By seasoning pork with herbs and spices to boost flavor, you also cut back on fat and salt. Preparing a pork tenderloin on the grill or roasting it in the oven is a quick, easy evening meal that easily pairs with grains, fruits and vegetables to make a nutritious meal. A cooking temperature of 145° F for pork cuts such as chops, roasts and tenderloins with a 3-minute rest time is a safe final internal cooking temperature that keeps your pork juicy and flavorful for a spectacular eating experience.
Charlotte wants everyone to know that South Dakota pig farmers are committed to providing the consumer with tasty, nutritious pork in a sustainable way. ❖
September 5
12:00 pm–4:30 pm
September 6
7:40 am–5:00 pm
Imagenetics
ImaGENE Precision Medicine Summit
LOCATION
Sanford Imagenetics & Sanford Center, Sioux Falls
September 18 and 19
8:00 am–5:00 pm
South Dakota Statewide Trauma Conference
LOCATION
Highland Conference Center, Mitchell, SD
September 24–26
South Dakota Health Care Association Annual Fall Convention
LOCATION
Ramkota Hotel, Sioux Falls
September 25–27
8:00 am–5:00 pm
Mayo Clinic Neurology in Clinical Practice
LOCATION
Westin Chicago River North - Chicago, Illinois or Livestream
September 25–27
98th Annual SDAHO Convention
LOCATION
Holiday Inn Rapid City Downtown
September 27
8:00 am–4:00 pm
CNOS Orthopaedic Symposium
LOCATION
Holiday Inn Express and Suites, Dakota Dunes, SD
October 3 and 4
2024 APIC
South Dakota Annual Conference
(formerly SD Infection Control Conference)
LOCATION
USD Sioux Falls Campus or Virtual
October 4
8:00 am–4:30 pm
25th Annual Avera Cancer Institute Oncology Symposium
LOCATION
The District, Sioux Falls
October 17
7:30 am–5:00 pm
Monument Health Cardiovascular Disease and Wellness Symposium
LOCATION The Monument, Rapid City
October 21 and 22
8:00 am–5:00 pm Transforming Community and Rural Healthcare ‘24: Inspiring Partnerships and Scaling Collaborative Impact
LOCATION
Mayo Civic Center, Rochester, MN
October 25
8:00 am–4:00 pm
CNOS Occupational Medicine Symposium
LOCATION
Holiday Inn Express and Suites, Dakota Dunes, SD

The Monument, Rapid City Oct. 17, 2024 7:30 a.m. – 5 p.m.
Snacks and lunch provided
CME/CE credits available
A day-long symposium offering a practical approach to advances in cardiovascular care and technology, new preventative strategies and the latest wellness information.
For additional information visit: monument.health/cardiovascularsymposium
In-Person and Virtual Options Available