The Danger of Overlooking Diagnostic Test Results
Sioux Falls Goes Red for Women’s Heart Health
Spring Events to Put on the Calendar


The Danger of Overlooking Diagnostic Test Results
Sioux Falls Goes Red for Women’s Heart Health
Spring Events to Put on the Calendar

















20,000+
14,000+

The Advanced Pediatric Heart Failure & Transplant Program at Children’s Nebraska received full approval from the Centers for Medicare and Medicaid Services in November 2024, is active in the United Network for Organ Sharing system and is actively listing patients for heart transplantation. Led by surgical director Camille Hancock Friesen, MD, and medical director Jason Cole, MD, the program provides comprehensive care for children with heart failure, serving patient families in the region and beyond.
Children’s Advanced Pediatric Heart Failure & Transplant Program offers compassionate, familycentered care, ensuring patients and families are well-informed throughout the care process. The multidisciplinary team comprises specialists from various pediatric fields, including Cardiology, Cardiothoracic Surgery, Cardiac Critical Care, Anesthesiology, Nutrition, Child Life, Social Work, Pharmacy and more, with consultations available from other specialties. Care is provided in Children’s 32-bed, acuity-adaptable Cardiac Care Unit (CCU) in the state-of-the-art Hubbard Center for Children, where patients receive continuous, specialized monitoring and treatment.
Recently, Children’s Advanced Pediatric Heart Failure & Transplant team performed its first-ever placement of a durable mechanical circulatory support in the form of ventricular assist device (VAD), a significant milestone. The life-saving device can serve as a bridge to heart transplantation or, in some cases, act as a long-term solution for children with heart failure. The ability to offer

VAD implantations is a testament to Children’s commitment to providing the most advanced pediatric cardiac care.
Children’s Advanced Pediatric Heart Failure & Transplant Program is a major step in expanding access to care. Advanced pediatric cardiac therapies are available close to our patients’ and families’ homes. Patients and families traveling more than 90 miles outside Omaha can access the Carolyn Scott Rainbow House, a 56-room overnight guest house for a patient’s immediate family.

To learn more about Children’s Advanced Pediatric Heart Failure & Transplant program, visit ChildrensNebraska.org/HeartTransplant or scan the QR code. To refer a patient, call 402.955.4350.

Midwest Street Medicine’s Call to Compassion
■ By Alex
Strauss
PAGE 8
From treating wounds and managing chronic conditions to providing vaccinations and emergency interventions, Midwest Street Medicine is redefining healthcare access for the Sioux Falls community’s most vulnerable residents. Meet the physicians, nurses, and specialists volunteering their time and expertise to bridge critical gaps in care - and learn how you can get involved.
PAGE 6 | This Month Online
Exclusive online content plus how MED can help keep your office tidy
PAGE 11 | NO NEWS IS NOT GOOD NEWS: Overlooked Diagnostic Test Results
■ By Dr. Sue Sgambati
A gripping case study reveals how poor office communication around lab results led to a preventable emergency – learn five key strategies to protect your patients and practice.
PAGE 12 | NEWS & NOTES
The region’s first Baby Café, five years of a Monument/Mayo relationship, a perfect score for Brookings’ Birth Center and more headlines from across our region
PAGE 17 | USD School of Health
Sciences Success Spotlight: Jason Simon-Ressler
PAGE 18 | Beyond the Border: News from MED’s Multi-state Coverage Area
PAGE 20 | [Sponsored]
RN Case Manager Joyfully Helps Clients Find Long-Term Care
After 23 years in long-term care, this dedicated Sanford case manager shares why helping families navigate placement decisions has become her life’s most rewarding work.
PAGE 22 | Sioux Falls Community Unites for Women’s Heart Health at Annual Go Red Event
PAGE 23 | Upcoming 2025 Events
STEFFANIE LISTON-HOLTROP
VP Sales & Marketing
FROM US TO YOU
Welcome to the March issue of MED, where we’re exploring some remarkable healthcare initiatives making a difference across our region.
In our cover story, we take you inside Midwest Street Medicine, a grassroots movement bringing healthcare directly to some of our most vulnerable neighbors. What began with a chance encounter with a podcast has blossomed into a powerful model of community-based healthcare that’s changing lives across South Dakota.
Inside, you’ll find exciting developments in pediatric cardiac care from Children’s Nebraska, revealing new data on healthcare AI adoption, and valuable insights on patient safety from our friends at COPIC. Plus, we have our usual comprehensive roundup of news from across the region and a full calendar of upcoming spring and summer healthcare events.
All the best, —Alex & Steff
P.S. Don’t forget to check out our expanded digital content at MidwestMedicalEdition.com, where you’ll find even more regional healthcare news and resources.
Publisher / MED MAGAZINE, LLC
Sioux Falls, South Dakota
Vice President Sales & Marketing
STEFFANIE LISTON-HOLTROP
Editor in Chief / ALEX STRAUSS
Staff Writer / KIM LEE
Magazine Design / ANGELA CORBO GIER
Client Relationship Manager / BARBIE MUNOZ
605-366-1479
Steff@MidwestMedicalEdition.com
ALEX STRAUSS
Editor in Chief
605-759-3295
Alex@ MidwestMedicalEdition.com
WEBSITE
MidwestMedicalEdition.com
Digital Media Director / HYA AMURAO NEXT ISSUE
MAILING ADDRESS
PO Box 90646, Sioux Falls, SD 57109
10
10
Editorial contributions due March 5
Ads due March 10



Alarming new data from the American Heart Association reveals cardiovascular disease claims a life every 34 seconds in the U.S. While smoking rates decline, rising obesity emerges as the new critical health threat, contributing to 1,300 deaths daily.
Read the full analysis of the 2025 Heart Disease Statistics Report online.
With Medicaid payments increasing and construction costs stabilizing, hospitals are revisiting delayed capital projects.
A new analysis from the financial experts at Nebraska’s UMB Bank explores two key financing options — Hospital Revenue Bonds and USDA Direct Loans.
Learn how your facility can leverage these favorable market conditions for strategic growth in the full online article.



We don’t have room inside this publication to list all of the new physicians and other healthcare professionals that are joining facilities across our region. But you’ll find them all on our website. Come on over to meet your new colleagues and to let us know when someone new joins your clinic, hospital, or health system. We’d love to share the news with MED’s growing readership!
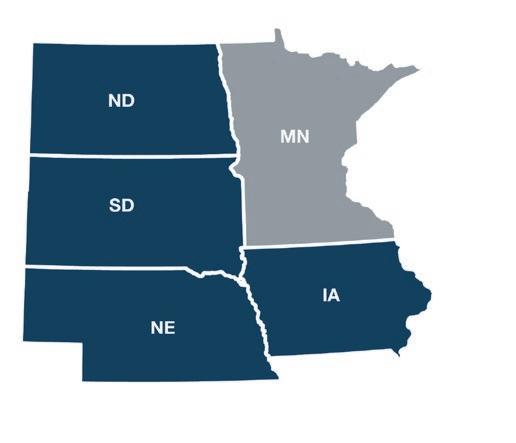
Did you know that MED provides region-specific news to thousands of subscribers in Iowa, Nebraska, and North Dakota, too? See page 18 for a preview of some of that content and select “News by Region” at the top of our website to see just the news YOU want!


Healthcare artificial intelligence adoption is gaining momentum among physicians, according to the American Medical Association’s latest Augmented Intelligence Research survey. The study, comparing data from August 2023 to November 2024, shows a significant shift in physician attitudes and implementation.
The percentage of physicians whose enthusiasm exceeds their concerns about health AI increased to 35% in 2024, up from 30% in 2023. More notably, physician adoption of AI tools has surged, with 66% of physicians reporting current AI use in their practice—a dramatic increase from 38% in 2023.
Administrative burden relief remains the top opportunity, cited by 57% of physicians. However, concerns persist around privacy, EHR integration, and liability issues. The survey identified key requirements for broader adoption, including designated feedback channels (88%), data privacy assurances (87%), and seamless EHR integration (84%).
“Physicians are increasingly intrigued by AI’s assistive role,” notes AMA Immediate Past President Jesse M. Ehrenfeld, MD, MPH. “But there remain unresolved concerns with design and potential flaws that could impact privacy, accuracy, and liability.”
The AMA continues to advocate for responsible AI development in healthcare, emphasizing patient safety as the paramount concern.
VISIT OUR WEBSITE for an in-depth analysis of the survey findings, including detailed breakdowns of physician concerns, adoption rates across specialties, and the AMA’s comprehensive principles for ethical AI implementation in healthcare.
If you are one of those MED print subscribers who can’t bear to part with a single issue “just in case”, we see you, we feel you, and we have your back! Now, you can easily access the entire year’s worth of MED Magazine right on our website. No need to hoard your back issues on the chance you’ll want to refer to something later. Just visit MidwestMedicalEdition.com/ med-magazine for direct links to the latest issues. And, to make sure you never miss your MED, subscribe to our bi-monthly digital newsletter and we’ll send each new digital issue directly to your Inbox!
(while you’re thinking about it) at MidwestMedicalEdition.com/ med-vip!









BY ALEX STRAUSS
people. Their mission—carried out twice weekly
for the last year-and-a-half—is to bring help and medical care directly to one of the most vulnerable populations in the state: people who live on the streets.
The story of Midwest Street Medicine began with a chance encounter, according to co-founder, and medical director Shannon Emry, MD, a pediatrician with Avera in Sioux Falls.
“I was actually just listening to a podcast about health and health equity and stumbled onto an episode about street medicine,” says Emry. “The concept just stole my heart.” That spark of inspiration led her to Dr. Melissa Dittberner (“Dr. Mo”), a professor of addiction counseling and prevention at USD, and together they launched Sioux Falls’ street medicine program in July 2023. Dittberner is now the executive director.
The statistics underline the urgency of Midwest Street Medicine’s mission: The mortality rate for unsheltered people is 10 times that of the general population. Even sheltered homeless people die at three times the rate of people with homes, and as many as three decades earlier.
From the beginning, the team took a uniquely patient-centered approach. “One of our mantras is that we ‘let the street build the program,’” says Dr. Emry, who spent the first few months handing out snacks and conducting needs assessments.
“You learn to meet people where they are at and ask them what they want from you,” says RN Diane Eide, case manager, grant support, and volunteer coordinator at Midwest Street Medicine. “We don’t ever tell people what to do. We leave them in control.”
Now, with those needs in mind, the team provides comprehensive care directly on the streets every Sunday and Monday morning from nine to noon. Medical interventions range from blood pressure checks and wound care to more complex challenges like help for addiction, mental health care, or medication management. They offer thiamine injections to prevent encephalopathy in individuals with significant alcohol use, administer flu and COVID vaccines, and conduct syphilis testing—particularly crucial given South Dakota’s highest-in-the-nation syphilis rate.


Medical interventions can range from blood pressure checks, wound care, and vaccinations, to medication management, mental health care or addiction support. Sometimes, what’s needed most is a snack, fresh water, warm clothes, and kindness.
Volunteer groups can change from week to week and may include physicians, nurses, PAs, CHWs, pharmacists, addiction and peer support specialists and others.




The success of the program stems largely from the trust MSM has built with a population often wary of the healthcare system. “A history of trauma is universal among folks who are homeless,” says Dr. Emry. Understanding trauma’s role in healthcare avoidance has helped to shape the group’s care delivery model, which Dittberner describes as deeply responsive to individual needs.
“We always start by asking people what they need,” she says. “Whether that is medical care, mental health care, help with addiction, etc. If we see that they need gloves and a hat, or snacks, we’ll leave these with them, too.”
This kind of patient, human-centered approach appears to be paying off.
“We can get people to do more than anyone else in town,” says Eide. “For instance, maybe they need to go to the emergency room, but they’ve been reluctant to do it. We can get them there. Now, we have our regulars that recognize us from two blocks away and say, ‘Street Medicine’s here!’ And they get excited.”
co-founder and executive director, Melissa Dittberner, PhD
Supported by grants and donations, Midwest Street Medicine teams serve about 50 people on Sundays and about 30 on Mondays, with new operations launching in Aberdeen and Rapid City. In 2024 alone, they recorded over 600 medical visits in Sioux Falls, while providing countless others with food, supplies, and support. And the people receiving care are not the only ones impacted.
“I think we gain more than we give every single time we’re out there,” says Eide, a former ER nurse who says caring for people’s immediate needs “is like coming home”.
“This work has changed my life in so many ways,” agrees Dittberner. “The unhoused people in our community have taught me so many lessons about kindness and about giving back to others.”
As rewarding as it is, Emry says it is not easy and often requires a mindset shift for those in healthcare.
“We know that social determinants of health drive 85 percent of health outcomes, but we still just focus so hard on the medical piece because that’s what we are trained for, that’s what we know how to fix,” she says. “We struggle to wrap our arms around the social factors and how to help people with that piece. But we need to get better at that.” ❖
❱ MSM is in need of more prescribing physicians. Visit our website to find out how to get involved.
BY DR. SUE SGAMBATI
A primary care provider sees a patient acutely who is “not feeling well” in the morning. The exam is unremarkable and the provider orders a complete blood count (CBC) and chemistry panel. At 4:55pm, the lab calls to report a critical potassium level of 6.0. The provider has already left for the day and is not called. Due to the provider’s unpleasant demeanor and grumpiness, the staff rarely calls after hours. Later that night, the patient presents to the ED with syncope, cardiac arrhythmia, and a potassium level of 6.3.
Diagnostic test results are a critical component of patient care and the tests we order are increasing in numbers and complexity. Missed or delayed follow-up can lead to adverse outcomes, including delayed diagnoses, unnecessary complications, and potential medical liability claims.
To prevent these errors, medical providers must implement strategies to ensure that diagnostic test results, whether sent directly or forwarded to the office, are received, reviewed, and acted upon promptly.
National safety organizations, including the Joint Commission, the National Patient Safety Foundation (NPSF), and the Agency for Healthcare Research and Quality (AHRQ), provide valuable published guidance to help practices avoid these pitfalls.
1. Establish Clear Communication Protocols
One of the most effective ways to avoid missed results is to create standardized processes and a structured communication system for receiving and reviewing test outcomes. This should include documenting who is responsible for receiving, reviewing, and acting upon results.
2. Implement Electronic Health Record (EHR) Alerts
Leveraging technology can significantly improve the management of test results. The NPSF suggests the use of EHR alerts or notifications to flag pending results or abnormal findings. Automated alerts can trigger action by clinicians and staff, ensuring timely follow-up.
3. Ensure Test Results Are Tied to Clinical Workflow
Diagnostic test result management must be integrated into the clinical workflow. Practices should ensure that test results are reviewed by the ordering physician, ideally within a set timeframe, and that abnormal results prompt an immediate follow-up action.
4. Patient Notification Systems
Patient notification is critical to ensuring that diagnostic results are acted upon. Practices should have clear protocols for notifying patients of both normal and abnormal results.
5. Conduct Regular Audits
Regular audits of the test result management process can help identify potential gaps and areas for improvement.
Avoiding missed diagnostic test results requires a combination of clear protocols, technological tools, effective communication strategies, and ongoing monitoring. By following these best practices, medical providers can significantly reduce the risk of errors, improving patient safety and care outcomes.
Information in this article is for general education purposes and is not intended to establish practice guidelines or provide legal advice. ❖

Dr. Sue Sgambati is Senior Physician Risk Manager at COPIC

Avera Research Institute held its 2025 Maternal American Indian Rural Community Health (MARCH) Annual Summit on March 4. The MARCH Center of Excellence serves as a platform for collaboration between researchers, tribal nations, rural communities, and healthcare partners to address maternal mortality and morbidity. The summit featured keynote speaker Deb Kilday, Senior Advisor for Maternal and Infant Health at the U.S. Department of Health and Human Services. Other speakers included Avera Research Institute scientists, including Dr. Amy Elliott, Chief Clinical Research Officer, Avera Community Health Resource Workers and professors from the region.

Avera recently received five national Cancer Awareness Advertising Awards. Gold awards went to the Avera Race Against Cancer Mustang car wrap, lung cancer screening poster, and check yourself breast cancer flyer. Silver awards included breast cancer website banners and a blog on Avera.org/ Balance: “Expanded Cancer Care Options Translate to Hope for Both Urban, Rural Patients.” The Cancer Awareness Advertising Awards program is hosted by Creative Images, Inc., an internationally recognized firm that has specialized in strategic healthcare marketing for more than 30 years.
Avera McKennan Hospital & University Health Center’s Emergency Departments have been named a 2024 Human Experience (HX) Guardian of Excellence Award® winner by Press Ganey, placing them in the top 5% of healthcare providers nationwide for patient experience. The recognition applies to emergency departments at three locations: the main hospital campus and Avera Family Health Centers on Marion Road and at Dawley Farm. Press Ganey works with more than 41,000 healthcare facilities in its mission to reduce patient suffering and enhance caregiver resilience to improve the overall safety, quality and experience of care.

Monument Health is celebrating its five year anniversary as a member of the Mayo Clinic Care Network . Through this membership, Monument Health physicians and providers get special access to Mayo Clinic resources, knowledge and teams of specialists. As a member of the Mayo Clinic Care Network, Monument Health has access to: AskMayoExpert, a point-of-care tool offering concise clinical information on hundreds of medical conditions, eConsults, eBoards, and Health Care Consulting. Monument Health staff members can also use Mayo Clinic’s patient education materials, and access opportunities for professional development and CME opportunities.

Monument Health hosted its annual Community Health Summit during the Black Hills Stock Show & Rodeo at the end of January. The event, held at The Monument, included blood pressure checks, mental health assessments, prediabetes screenings, and cooking demonstrations in a teaching kitchen. New features this year included interactive displays of robotic-surgical systems and participation from specialists in orthopedics, audiology, and cardiovascular care. This year also included an expanded free community health booth thanks to new partnerships with the department of health and the American Heart Association, among others.

Justin Feeser, Manager at Monument Health Northern Hills Rehabilitation and Sports Medicine
Mark Nore, BHSU Director of Athletics, Shaun Skavang, BHSU Head Athletic Trainer, Thomas Worsley Monument Health President Spearfish & Hills Market
Monument Health has donated a state-of-the-art Therm-X compression and cryotherapy unit to Black Hills State University’s Athletic Training department. The portable unit is capable of delivering simultaneous static or oscillating compression with hot or cold therapy, significantly expanding treatment options for student-athletes. The equipment donation builds upon Monument Health’s previous support of local educational initiatives, including past contributions to Spearfish High School athletic programs.

The Monument Health Foundation funded the purchase of a new ultrasound machine for Sturgis Hospital through its Greatest Need Fund. The fund is supported by donations from caregivers, physicians, and community members. The purchase represents a decade of community investment in local healthcare initiatives. The Sturgis Hospital Greatest Need Fund is just one of the many ways Monument Health Foundation raises funds to develop programs, purchase cutting-edge medical equipment and expand facilities.

Dr. Tommy Ibrahim, CEO of Sanford Health Plan, delivered a keynote address at Columbia Business School’s 21st annual healthcare conference. Ibrahim discussed strategies for addressing rural healthcare challenges and innovations in care delivery. Sanford Health Plan serves 425,000 members across six states, focusing on expanding access to personalized care in rural communities. Ibrahim oversees the plan’s population health initiatives, value-based care programs, and managed-care product development. He also serves as an advisor to several healthcare technology and venture capital firms and is a graduate of Columbia Business School.
Sanford Health and Marshfield Clinic Health System, have completed their merger and are now one nonprofit integrated health system operating as Sanford Health. Marshfield Clinic Health System, now Marshfield Clinic region of Sanford Health, is an integrated health system serving Wisconsin and Michigan’s Upper Peninsula with more than 1,400 providers comprising 170 specialties. There are more than 60 Marshfield Clinic locations, 11 hospitals, Marshfield Children’s Hospital, Marshfield Clinic Research Institute, Security Health Plan and Marshfield Clinic Health System Foundation. Dr. Brian Hoerneman will lead the new Marshfield Clinic region.
proximity in living cells. His ongoing research program focuses on nuclear envelope structure and function, with implications for treating diseases including muscular dystrophy, cardiomyopathy, lipodystrophy, and progeria.

Becker’s Healthcare has named Jeremy Cauwels, M.D., chief medical officer at Sanford Health, to its list of 180 Chief Medical Officers to Know in 2025. Under Cauwels’ leadership, Sanford achieved significant safety improvements, including an 80% reduction in serious safety events at Sanford Bismarck and Bemidji facilities. As chief medical officer for the nation’s largest rural health system, Cauwels represents physician interests to the executive leadership team and board of trustees. He also chairs the quality cabinet, leads enterprise aspects of the medical staff and oversees the system’s graduate medical education program.

Whitney (Anderson) DeBoer, RN, of Orange City Area Health System in Orange City, Iowa, was the Sanford Health Network’s 3rd Quarter DAISY Award recipient. The patient family member who nominated DeBoer wrote, “She was the most compassionate, kindest, caring, relaxed, informative, diligent proactive nurse I have ever met.”

Peyton McWethy, RN, became the tenth recipient of Huron Regional Medical Center’s DAISY Award, earning recognition for his exceptional emergency department care. The award, established in memory of J. Patrick Barnes, acknowledges nurses who demonstrate outstanding patient care and compassion. McWethy was nominated by a patient who praised his respectful

In an effort to encourage literacy in children and foster a love for reading, HRMC Physicians Clinic and New Life Clinic in Huron, have joined the nationwide Reach Out and Read program. This initiative, aimed at promoting early childhood literacy, empowers healthcare providers to integrate books and reading into pediatric care. The program is simple yet powerful: during routine well-child visits, Sean Schooley, MD, pediatrician, and all family practitioners give children between the ages of 6 months and 5 years a brand-new book to take home. Simultaneously, providers offer guidance to parents about the importance of reading aloud to their children from an early age.
HRMC Physicians Clinic introduced Convenient Care services in January. Designed to meet unexpected health needs, Convenient Care is open from 7:00 to 9:00 a.m. Monday-Friday with walk-in care for minor illness and injury. The new service is a response to needs identified through Huron Rising 2.0 community surveys. The program accepts insurance and serves both established and new patients, aiming to provide accessible care before work and school hours.

Prairie Lakes Healthcare System has opened Watertown’s first Baby Café, providing weekly breastfeeding support in the Maternal Child Health family lounge. The program, available Tuesdays from 10:00 a.m. to 1:00 p.m., offers free access to certified lactation professionals and peer support. The facility is staffed by one International Board-Certified Lactation Consultant and two Certified Lactation Counselors, serving families regardless of delivery location.
Prairie Lakes Healthcare System will establish a presence in the new Castlewood Wellness Depot, offering primary care services two half-days weekly and rehabilitation services twice weekly to the Castlewood, South Dakota community. The Castlewood City Council approved the proposal by PLHS to lease medical office space in the Wellness Depot building. Opening in April 2025, the clinic will feature laboratory capabilities and walk-in appointments. The expansion represents PLHS’s strategic initiative to enhance healthcare accessibility in rural communities.

Prairie Lakes Healthcare System (PLHS) presented a $50,000 donation to the “Sam Off the Streets” campaign, spearheaded by Watertown Cares to support operational costs for 612 Flats, an emergency housing facility in Watertown which also provides case management for those experiencing homelessness. The donation included $25,000 in matching funds and an additional $25,000 contribution. The campaign featured Watertown Cares Board Member Sam Mooney camping in a tent for 36 hours, raising awareness about homelessness. Thanks to overwhelming community support, the campaign exceeded its goals raising more than $110,000 for Watertown Cares.

Brookings Health System’s New Beginnings Birth Center has achieved its third perfect score of 100 on the CDC’s Maternity Practices in Infant Nutrition and Care survey, surpassing regional averages by 21 points and national averages by 18 points. Hospitals that participate in the mPINC survey are rated on six care dimensions: immediate postpartum care, rooming-in policies, feeding practices, parent education programs, discharge support systems, and institutional management protocols. According to the CDC, institutional changes in maternity care practices effectively increase breastfeeding initiation and duration rates.

Our local rheumatology team will help evaluate, diagnose, and treat patients with a variety of rheumatologic conditions from our South Sioux City location.

Four outstanding Brookings Health System nurses have become the inaugural recipients of the hospital’s first DAISY Awards, recognizing their outstanding contributions to patient care. Home Health and Hospice nurse Shelly Deknikker was nominated for her problem-solving abilities and dedication to meeting patient needs. Obstetrics nurses Savannah Price, Sara Klug, and Nancy DeBoer were jointly nominated for their supportive care during complicated deliveries. Recipients received certificates, commemorative pins, and a sculpture called, A Healer’s Touch, hand-carved by artists of the
Tribe in Zimbabwe.

• Rheumatoid arthritis
• Lupus
• Psoriatic arthritis
• Gout
• Scleroderma
• Sjogren’s disease
• Other rheumatologic conditions
DELANEY-NELSON, MD Internal Medicine and Rheumatology



201 E 4th St | Suite 202 South Sioux City, NE

child welfare related law will have the opportunity to learn from local and national experts on April 3. The fourth annual Legal Workshop presented by the South Dakota Unified Judicial System, University of South Dakota Knudson School of Law, and Center for the Prevention of Child Maltreatment will take place at the Muenster University Center in Vermillion. This year’s workshop will feature two topics: Indian Child Welfare Act and Representation of Immigrants and Refugees. While the workshop is free, registration is required. Visit MidwestMedicalEdition.com/Events to learn more.


Make-A-Wish
South Dakota & Montana has announced a record-breaking $115,466 in net proceeds from its annual Northeast South Dakota Make-A-Wish Dinner and Auction held in November. This is the 32nd year for the Watertown event. It showcased powerful testimonials from local wish recipients and their families, who talked about the transformative impact that granted wishes had on their medical journeys. This year’s dinner and auction has already been scheduled for November 7, 2025.

A year after the South Dakota Health Department restructured its community health services, statistics and personal stories indicate that it’s been a big success. Public Health Nurses administered over 1,700 more immunizations in the first year after restructuring than the previous year. They credit more efficient practices like automated text reminders and strategic outreach efforts, which have minimized missed vaccination opportunities and fostered more engaged patients. The reorganization also enhanced WIC services efficiency through paraprofessionals, reduced operational costs by 20%, and strengthened the First 1,000 Days initiative focusing on maternal health and early childhood development.

Lighthouse Autism Center held an open house in early February to celebrate the expansion of its services into South Sioux City, Nebraska. The new South Sioux City Autism Center is set to serve up to 25 families and employ 35 staff members, offering comprehensive services including ABA Therapy, Speech Therapy, autism diagnostic testing, and pre-academic learning. The facility features the proprietary Lighthouse Fusion® program, integrating speech therapy into daily activities through collaboration between certified behavior analysts, speech-language pathologists, and other therapists.

MercyOne hospitals marked Congenital Heart Defect Awareness Week by providing red hats to all its February newborns. The initiative highlights the hospital’s comprehensive approach to early detection and treatment of congenital heart defects, the most common birth defect nationwide. Dr. Neil Mandsager of MercyOne Perinatal Center emphasized the importance of immediate screening and intervention to optimize outcomes for affected infants.
❱ Intrigued by something you’ve read here? Want to go deeper? Read the full versions of these and other recent news items on our website.
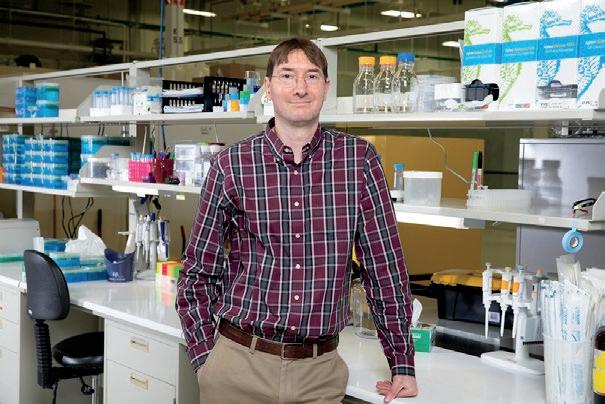
Jason Simon-Ressler
Degree: Master of Public Health (In Progress), BS in Kinesiology/Sports Management
Current Position: Child Health Coordinator, Title 5 Program, South Dakota State Health Department

Although he could not have known it at the time, Jason SimonRessler’s path to a career in public health began with a high school research paper on childhood obesity. Later, while playing football for USD and pursuing his Bachelor of Science in Kinesiology and Sports Management, he remembered that experience and began to think more broadly about health impact.
“I started thinking more ‘big picture’ about public health,” says Simon-Ressler. “My goal became ‘how could I support more chronic disease prevention?’ Public health was an avenue I felt would help me have more impact.”
That realization led him to add psychology and public health minors to his undergraduate studies, laying the groundwork for a future Master of Public Health degree. Then, during the summer of his junior year, Simon-Ressler secured a CDC undergraduate public health traineeship at Johns Hopkins in Baltimore, an opportunity that proved pivotal.
When he returned to South Dakota later that summer, he worked with the Sioux Falls Health Department through USD’s Center for Disabilities as part of the same program. “This gave me the opportunity to train in leadership and public health alongside some great multidisciplinary talent,” he says. “That really did solidify my idea of going into public health and continuing with a graduate degree.”
Now wrapping up his Master of Public Health degree at the USD School of Health Sciences while working full-time at the South Dakota State Health Department, Simon-Ressler says he especially appreciates the program’s practical applications. “Just about every class that I take, I can immediately translate the lesson into my job,” he says. “When you can immediately apply what you’re learning to your career, it’s easy to see the value.”
For Simon-Ressler, the fact that USD’s MPH program is offered online, is fully accredited, and costs less than many other programs made it an easy choice to continue his education there. “I don’t think I could have done it had I gone to any other university,” he says. “It wasn’t easy but it was manageable. I could see that it was going to work for me.”
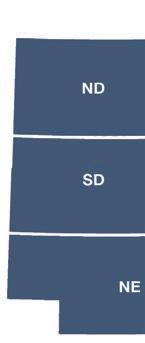
In addition to MED Magazine in South Dakota, MED also curates and shares medical community news with 13,000+ digital subscribers in North Dakota, Nebraska, and Iowa. We periodically print some of the most notable news items from our wider coverage area.
Stoddard Cancer Center Offers New Targeted
Des Moines, IA— UnityPoint Health–John Stoddard Cancer Center has become the first in Iowa to treat a patient with GammaTile Therapy, an innovative approach to combating brain tumors while preserving healthy tissue. This FDA-cleared, Surgically Targeted Radiation Therapy (STaRT) is made possible in Central Iowa through a collaboration between Stoddard Cancer Center radiation oncologists and Scott Seaman, MD, neurosurgeon with The Iowa Clinic.
“GammaTile therapy involves implanting postagestamp-sized tiles embedded with radiation sources into the brain during the final minutes of tumor removal surgery,” says Dr. Seaman. “The radiation immediately begins targeting tumor cells in the area where the tumor is most likely to recur.”
Aggressive brain tumors tend to be resistant to traditional treatments and have a high recurrence rate. The previous standard of care for patients with operable brain tumors was surgical removal of the tumor followed by adjuvant therapy, including radiation and chemotherapy. Traditional radiation is delivered in as many as 30 treatments extending over a period of several weeks.

Omaha, NE — The final beam is now in place on the CORE (Center of Research Excellence) building, located in the EDGE District west of the University of Nebraska Medical Center.
“GammaTile Therapy reduces the need for prolonged radiation schedules, delivering treatment in a single surgical procedure,” says Samuel Schroeder, MD, radiation oncologist at Stoddard Cancer Center. “It’s a highly targeted approach that minimizes side effects, allowing patients to maintain their quality of life.”

The approximately 180,000-square-foot, $105 million building, which is owned by UNMC, is poised to be a pivotal cornerstone in propelling innovative biomedical research. It will support lab-based research in critical areas (microbiology, physiology, pathology, genetics, life sciences, light chemistry), as well as computer-based research.
The shelled research floors are designed to provide essential lab and office environments, promoting collaboration among startup founders, industry leaders, UNMC faculty, scientists, and inventors at the EDGE District campus. The CORE facility will also house incubator lab space tailored for bioscience startups in discovery and development phases. This space will be outfitted with vital features and shared equipment to facilitate safe experimentation and expedite research endeavors.
“As the EDGE District positions itself as a dynamic hub for health-focused scientific discovery and entrepreneurship, the CORE building will play an important role” says H. Dele Davies, UNMC interim chancellor. “Our goal is to foster groundbreaking discoveries that thrive here in Nebraska, driving education, economic growth and advancements in health care.”
The new building is set to open in 2026.

North Platte, NE — Great Plains Health is now the seventh hospital in Nebraska to be recognized as a Pediatric Ready Hospital by the Nebraska Emergency Medical Services for Children Committee, marking a significant milestone for pediatric emergency care in the North Platte region.
This achievement is particularly significant as approximately 90% of children needing emergency care are first treated at local community emergency departments.
To earn this designation, Great Plains Health met rigorous standards in several key areas, including staff qualifications and training, quality improvement measures, pediatric-specific policies, continuing education programs, specialized equipment and supplies, and a commitment to ongoing process refinement.
“Having the right equipment, protocols, and training in place for pediatric emergencies can make a critical difference in outcomes,” said Dr. James Smith, emergency physician at Great Plains Health. “Our team has worked diligently to implement these pediatric-ready standards, ensuring we’re prepared when children need emergency care.”
Grand Forks, ND — Altru’s highly anticipated new hospital is now open in Grand Forks. Under construction since 2019 and paused during the pandemic, the state-of-the-art facility spans 552,000 square feet with seven floors above ground.
The new hospital boasts a variety of enhancements and features aimed at improving patient outcomes and satisfaction including advanced technologist and design, a calmer atmosphere with all private patient rooms, an abundance of windows, and a dedicated spiritual center.
The hospital features 226 licensed beds, a 16-bed observation unit, 12 operating rooms, and 4 catheterization labs. It is also equipped with an integrated interventional radiology (IR) and computed tomography (CT) machine, a sophisticated imaging suite, and advanced infection control systems designed to convert entire wings into negative pressure environments.
Once the move to the new hospital is complete, the process of decommissioning and demolishing the old hospital will begin. Upon completion, the patient/guest


parking lot and water retention pond will be built in its place.
In the coming years, Altru will continue transforming the campus into a “Hospital in a Park,” further enhancing the serene, healing environment, while also ensuring sufficient parking and access to the facility.
The cost estimate for the new hospital and related facility renovations, including the new Altru Behavioral Health Center, is $500 million.
❱ Interested in more news from MED’s wider coverage area? Select your preferred regional newsletters on our website.
SPONSORED ]

FOR MANY individuals and their families, finding placement in a long-term care center is a difficult and exhausting process. Having the help of a dedicated RN case manager in these scenarios can be an immense blessing for them.
RN case managers, like Brenda Holm of Good Samaritan Society, understand the system and the struggles these families face. And for people like Brenda, filling the role is more than a job — it’s a satisfying way to serve others.
BRENDA’S DECADES OF WORK IN LONG-TERM CARE
Brenda has spent most of her working life in long-term care, and she credits a lot of her
success to her previous roles in the organization.
“I’ve done a little bit of everything, from floor nurse to minimum data set coordinator,” said Brenda. “I started out with long-term care at Sanford Health, and then later joined a joint venture between Sanford Health and Good Samaritan Society called Prospera before they decided to fully combine in 2017. I’m still a part of the same organization after 23 years.”
Starting out as an RN gave Brenda a good perspective on what it means to provide care. She has always believed it’s crucial to develop a trusting relationship with patients and their families so they can reach their shared goal.
“One of the things I like the
most about my job is visiting with the potential resident and their family members,” said Brenda. “I love hearing their voices go from unsure to joyful and relieved. It’s my job to be a source of positivity for them, and by the end of conversations we end up forming a friendly bond with each other.”
These relationship-building moments encourage Brenda, and they help her approach the other aspects of her job with renewed energy.
HOW BRENDA HELPS PEOPLE GET THE CARE THEY NEED
Navigating the world of longterm care is no small task.
It requires diligence and a lot of specialized knowledge
to understand the process and effectively communicate with regulators, officials and providers.
As an RN case manager for four Good Samaritan Society locations in the Bismarck-Mandan area of North Dakota, Brenda helps people in need find a safe long-term care solution. Because of the complexities of each case, her work can be difficult, but Brenda doesn’t like to back away from a challenge.
“Our clients come from a lot of care settings, whether it’s in acute care, at home, or in another facility,” said Brenda. “Sometimes they are unsure of what the next step is going to be for them and how they’re going to get care. Our job is to help meet the needs of these applicants and their families, to resolve their medical issues, and to improve their quality of life.”
Many families struggle to provide care to their loved ones, especially if their loved one has a lot of care needs or lives a long distance away from their family. Long-term care can bring an amazing sense of relief to the entire family, but overcoming the access barriers can be tough. Those barriers motivate Brenda to do everything she can to help her clients.
“I like helping people in their moment of need,” said Brenda. “Family members often act as caretakers, so if I can help them find a safe place for their loved one to live, I can help them just be a family member again. It gives me a great amount of satisfaction knowing we can help those people.”
Having a dynamic and supportive team to work alongside is a huge benefit at any job, but when it comes to working in
long-term care, it’s a necessity.
Sanford Health and Good Samar itan Society, Brenda has worked with outstanding coworkers who value her input and help her with anything she needs.

ment. There’s so much teamwork,” said Brenda. “When I’m having a tough day, I know I can reach out to my coworkers for support, and on other days I get to pay it forward and help them, even if it isn’t related to work.”
Her team is great at what they do, and a lot of this success comes from their manager who serves as a voice of reason and key motivator.
“She has been such a great career builder for me,” said Brenda. “I want to stay here because we have great resources that help us be the best we can be.”
Above all, Brenda is extremely grateful for Good Samaritan
thankful I work for this organization, and I think my job is just awesome. God has blessed me beyond belief.”
Careers at the Good Samaritan Society have excellent pay, comprehensive benefits, and above all, the opportunity to serve residents and clients. If you’re looking for a rewarding career with plenty of room to grow, start exploring our open positions today at sanfordcareers. com/good-samaritan-society. ❖

BY ALEX STRAUSS
THE AMERICAN HEART ASSOCIATION’S 2025 Sioux Fa lls Go Red for Women Experience transformed the Sioux Falls Convention Center into a sea of red on January 31st, as more than 400 community leaders and healthcare professionals gathered to support women’s cardiovascular health.
The event, which aimed to raise $160,000 for critical research and education, balanced sobering statistics with messages of hope and resilience. The highlight of the program came from featured survivor Johanna Lippert, who shared her powerful post-stroke journey, offering fellow survivors and healthcare providers alike a testament to the importance of comprehensive stroke care and rehabilitation.

National data underscores the urgency of the Go Red mission. Despite being the leading cause of death among women, cardiovascular disease awareness remains critically low, with only 44% of women recognizing this threat to their health.
Even more concerning for healthcare providers is the persistent gender gap in clinical research — as of 2020, women represented only 38% of cardiovascular clinical trial participants, despite facing unique cardiovascular challenges throughout their lives.
There is also a troubling gender disparity in emergency response situations. A 2017 study revealed that women in cardiac arrest are significantly less likely to receive bystander CPR in public settings — 39% compared to 45% for men — resulting in 23% lower survival odds for women.
Regional healthcare sponsors of Go Red included Sanford Health, Avera Health, Dakota Vascular, and Encompass Health. MED continued its tradition of sponsoring a table at the event. MED co-founder Steffanie Holtrop sits on the Go Red board.
Healthcare professionals interested in learning more about the initiative or getting involved can visit www.heart.org/ SiouxFallsGoRed for additional information and resources. ❖
March 12
9:30 am–2:00 pm
IHA Hospital Day on the Hill
Location: Airport Holiday Inn, Des Moines, IA
April 1 – 2
8:00 am–5:00 pm
2025 Public Health Conference of Iowa
Location: Airport Holiday Inn, Des Moines, IA
April 3
9:00 am–4:00 pm
4th Annual Legal Workshop on Child Welfare Law
Location: USD MUC Ballroom, Vermillion, SD
April 4
6:30 pm - 10:00 pm
Pioneer Memorial Foundation Extravaganza
Location: Viborg Community Center, Viborg, SD
April 8–9
8:00 am–5:00 pm
SDAHO Post-Acute Partners in Care Conference
Location: Sioux Falls, SD
April 24
8:30 am–4:00 pm
Castle of Care Symposium: Trauma, Emergency and Critical Care 2025
Location: Sanford Center, Sioux Falls, SD
April 24 – 25
8:00 am–5:00 pm
Iowa Healthcare Leaders Association (IHLA) Spring Conference
Location: Renaissance Des Moines Savery Hotel, Des Moines, IA
May 13–14
8:00 am–5:00 pm
2025 Avera PACE Conference and Tradeshow
Location: Sioux Falls Convention Center, Sioux Falls, SD
May 20
4:00 pm–5:00 pm
2025 Avera Lung Conference
Location: Sioux Falls, SD
May 31
9:00 am–1:00 pm
National Cancer Survivors Day
Location: Monument Health Cancer Institute
June 17 – 19
8:00 am–5:00 pm
2025 Dakota Conference on Rural and Public Health
Location: Bismarck Event Center, Bismarck, ND
June 25 – 26
8:00 am–5:00 pm
SDAHO Rural Health Leaders Conference
Location: Drifter’s Event Center, Fort Pierre, SD
September 11 – 12
8:00 am–5:00 pm
Iowa Healthcare Leaders Association (IHLA) Fall Conference
Location: Hilton Garden Inn, West Des Moines, IA
Save the Dates:
September 24 – 26
8:00 am–5:00 pm
99th Annual SDAHO Convention
Location: Sioux Falls, SD
October 16
8:00 am–5:00 pm
11th Annual SD Health Link Fall Forum
Location: Sioux Falls Convention Center, Sioux Falls, SD
VISIT MIDWESTMEDICALEDITION.COM/EVENTS FOR MORE INFORMATION ON ANY OF THESE UPCOMING EVENTS AND TO SUBMIT YOUR OWN.














