THE AURICLE



Dear valued readers,
Welcome to The Auricle’s January-March Edition, our first instalment fo 2023. We are absolutely delighted to share this publication with you an the creativity of the contributors featured in these pages.
In 2023, the MUMUS Publications team is hoping to create an engagin and informative editorial experience We hope that through The Auricle as well as our associated Writing and Visual Arts Competition, there w be an opportunity for students to learn, read and express their writin and visual art endeavours. Following on from the 2022 edition, th MUMUS Publications team hopes to present a quartly 'The Auricle' fo your reading pleasure
To introduce myself, I'm Yash, currently a 4C student completing my G rotation. Over the past 2 months, the MUMUS Publications team has been getting stuck into creating the M and Grad Guide for the incoming Year 1 and Year A students. As of late in my spare time, I’ve been trying out new recipes (with a great lack of success :P) and have recently started work in the disability support space
I hope you enjoy the upcoming publications that are to come this year, as we hope to share with you some regular segments in the Auricle that will be featured in each edition In the background, we ’ ve been in collaboration with many of our MUMUS Subcommittees to bring along interesting segments for our readers Between each edition, we will be featuring stories from within these pages by publishing them to our website and the MUMUS Facebook page in blog format. Please keep a careful eye out as there may also be new content published between editions
This year we'll be trying something a little new and interesting, through uploading our 'Humans of Medicine' interviews onto Spotify so that you as our readers can have a listen to what we cover in your own time - helping make those commutes to a from uni/placement all the more enjoyable. In house, we've dubbed our podcast 'The Ossicle'.
If you want to contribute to The Auricle, please get in touch with us! Details about the kind of submission we are looking for can be found at https://theauricle.org/contributing/ or if you have any questions, email us at publications@mumus.org or ypat0008@student.monash.edu
We hope you enjoy reading this first edition of 2023. There’s a whole lot to get stuck into!

Happy reading :)
Yash Patwardhan, MUMUS Publications Yash Patwardhan is currently a 4C Student completing his GP rotationEach edition of The Auricle, we interview a member of the Monash medical cohort who has been up to something interesting that they are willing to tell to readers of The Auricle. If you think you or someone you know would have an interesting story to share, please contact us!
CAN YOU TELL US ABOUT YOURSELF AND YOUR MONASH MEDICINE JOURNEY?
I'm in my final year right now, and it's been amazing As an international student, I didn't expect it to go so wonderfully. I started out in 2019, as this young, naive boy entering into medicine in Australia, which was really daunting initially, but the community here has been so lovely Although I had to go back for one and a half years during COVID, I still feel like Australia is my second home. I've loved it here, and am keen on staying here in the future...

WE UNDERSTAND THAT OVER THE SUMMER HOLIDAYS, YOU DID SOME TRAVELLING. CAN YOU TELL US MORE?
Over the summer holidays, I did a solo trip to the US and Canada! After a pretty intense fourth year, I wanted a break. One of the key things I've always wanted to do as a student was to travel and see how a different medical system works. I've come from Singapore, and I've got to see

Melbourne's medical system. So I applied to Yale in the US. To be fair, I'm not sure how I got it, but I am extremely lucky and grateful that I managed to get the opportunity. For me, I took it as a great excuse to travel down to the US and explore the place, while seeing the medical system which was tons of fun.
INCREDIBLE! CAN YOU TELL US MORE ABOUT WHAT BEING AT YALE MEDICAL SCHOOL WAS LIKE?
So it was throughout the whole of December. It was a 4 week program, where I went in every day for Monday to Friday. During my time, I was allocated to the cardiac surgery unit, which was quite intense. I was going in every day at 6AM, and coming back home at
6PM That being said, it was a great experience because I managed to scrub in for the majority of the surgeries. I got to see a lot of robotic surgeries, which frankly speaking, I've never seen much before in my placements in Australia.
First, prefacing that with four weeks of experience, my knowledge of the US medical syste is still limited, so all I say are anecdotal experiences from my registrar.
Starting from a local perspective (e.g. someone US-born, studying in the US), many of them get matched into a residency program right after medical school (e.g. cardiac surg or gen surg). In comparison, we get a lot more time to explore through our different specialities once we graduate. Although we do find it intense during medical school, we still are comparably relaxed as we get time to get involved in different committees and pursue our own individual interests.
As American medical students have to match immediately, it can be quite daunting as they need to know what they want from day one. Many of them are doing research from the start of medical school That being said, the US medical students tend to be at a later stage of their life as they begin medicine as postgraduate students
From an overseas graduate perspective, I found out the pathway is not as straightforward as I thought it would be. If you wanted to apply to US, you would need to do a USMLE to match into residency, and that would be the baseline

as you can to help develop your cardiac unit before you can apply to the program and hopefully get in. On top of that, he was still disadvantaged compared to many local students given that he is a 'foreign' student.
Speaking to an international medical graduate (cardiac surgery research doctor), he shared that even after the USMLE, you would need a couple of years of publishing as many papers
It's very interesting the difference in training pathways and the involvement in clinical medicine For example, in Australia, even though you may be an unaccredited reg while applying for training program, that time is still spent doing 'clinical medicine' that would be relevant to when you are in the training program.
In comparison, in the US, when applying as a foreign graduate, you would be spending a few years doing research, and nothing clinical while you try to apply to the program. Once you get in, only then would you return to clinical medicine.
WHAT WERE YOUR MAJOR TAKEAWAYS COMPARED TO AUSTRALIA?
So it was quite straightforward. The majority of American Universities use a portal called the "Visiting Student Learning Opportunities". Unfortunately, Monash is not a part of the portal, and so it's hard to apply to many of the instituitions in America.
However, there are still a few that are outside of the portal, and that includes Yale, for which you apply straight to In June/July, I submitted a CV, a 250 word personal statement, and 2 academic references. Normally, you apply 6 months in advance of when you go, and so I was later selected for the December holidays period.
ANY ADVICE FOR YOUNG MEDICAL STUDENTS TRYING TO BALANCE STUDIES, WANTING TO DEVELOP THEMSELVES AS PEOPLE AND TICK THINGS OFF THEIR BUCKET LIST?


Just do the things you are passionate about. I genuinely believe that with us having recently moved towards a competency based grading system, there's such a beautiful avenue for us to get involved in things that you're passionate about. Jump into different projects, and put you're 100% into it and do the things you're passionate about
It doesn't have to be med related, it doesn't have to be for your CV, because in the end, everything will work out.
If you are keen on a particular speciality, or keen on getting ahead in life, it will 100% happen. But now is the best time to just experience everyhting that you love doingsport, music, now is the best time as a student. Once you've started working, you have a lot less time to do so, so just enjoy the journey.

"MANY OF THE PEOPLE I STAYED WITH WERE GERMANS, AND THEY REALLY KNOW HOW TO HAVE FUN"Keen to hear the whole interview in full? The full interview is available on our Spotify 'The Ossicle' podcast

Thesepastcoupleofyearsmerelyseemlikeablur.Atimewhenthedaysseemsolongyetayearseemsto disappearintheblinkofaneye.Wewakeupanddreadthecontinuationofamonotonousroutineasallthehours, daysandmonthsseemtoblendintoone
Arewestillin2020?
Orhavewemovedonto2021? Twenty…twenty…too? No...
Wearein2023.
Whenthepandemicbegan,adjustingtotheisolationwasdifficult.54%ofAustraliansreportedincreasedfeelings oflonelinessasrestrictionscameintoplaceandwewereconstrainedtotheconfinesofourhomes(Limet al 2020) Tocombattheriseofloneliness,anorganisationemergedtohelpthosewhostruggledinadaptingtothis ever-changingworld.ConversationinIsolation.Acharityledbyhealthstudentstohelppromotesocial connectionintheAustraliancommunityandfightlonelinessandisolation Itbeganin2020asasmallgroupof medicalstudentsfromMonashUniversitysetupaservicewherecommunitymemberscouldsignuptobe matchedwithadedicatedstudentvolunteertohaveregularchatsandgrowcompanionshipoverthephone. Simple,right?
Sincethenwe'vebeenamazedathowwe’vegrown,drivenbystudentsnationwidelookingforawaytomakea difference.Ourvolunteerscomefromarangeofclinicalbackgrounds(suchasmedicine,nursing,alliedhealth andmore)allaroundAustralia,butweallunderstandhowimportantsocialconnectednessistooverallhealthand well-being.Ourphoneserviceisstillgoingstrong,spearheadedbyourpassionatevolunteers.Manyofusspeak multiplelanguagesandcomefromdiverseculturalbackgroundsandwalksoflife.
Over250+communitymembers
400+volunteersintotalacrossarangeofdisciplines
In2022,wealsostartedamonthlynewsletter,‘CopinginIsolation’whereweopenuptheconversation surroundingmentalhealth.Ouraimistonormalisethestruggleswefacewithisolationandloneliness,sharethe experiencesofmanyandprovidecopingstrategiesandadvicetoourcommunitymembers
Weareslowlystartemergingfromourpandemicstrickenworld…intoanewworld.Thisnewworldwherewearein ahybridmodelofconnectingwithothersin-personanddigitallymeansthatwearestillincontactwithlesspeople thanbefore Itputsmanyatriskofstillfeelinglonelydespitetheliftingofrestrictions Despitethesechallenges,this newworldalsogiftsustheknowledgethatthetimewespendwithourfamilyandfriendsismeaningful,cherished andspecial.Thatthepeoplewhoremainclosetousduringtoughtimesareourbiggestsupporters.Thisnewworld hasrewardeduswithsmallmomentsofjoy;sharingamealatthedinnertable,goinggroceryshoppingwithouta mask,huggingourlovedones,andmypersonalfavourite:myGPsaying'Imissgivinglolliestochildrenaftertheir immunisationtostopthemfromcrying'.Thisnewworldhasreturnedtous,thethingsthatwemayhavetakenfor grantedinthepast,allowingustobefullygratefulforwhatwedohave
Moreover,thenewworldhastaughtussomethinginvaluable.Thedistinctionbetweensolitudeandloneliness. Solitudeisthephysicalstateofbeingalone Achoice
Lonelinessisapsychologicalstateassociatedwithnegativeemotionssuchasdepressionanddistress
Thepandemicwasnotachoice.Itwasforcedseclusion,onethatturnedintoisolationandbredloneliness. Thepandemichasputaspotlighttothebenefitsofsocialmedia Ithasallowedustoremainincontactwithothers and…Alas,themarvelsthatsocialmediabringstousinourtimeofneedcomesataprice:Thewonderful momentsofdistractionevolveintoboredomwithacertaindarknessshownusthedarksideofsocialmediawhen coupledwithboredom Themindlessscrolling Theunrealisticexpectations Thespreadingofmisinformation
In fact,asurvey(Beech,M2020)recordedabout50–70percentincreaseininternetuseduringtheCOVID-19 pandemicandofthat50percentofthetimewasspentengagingonsocialmediain2020.Itmayhavebeenthe onlywaytoremainconnectedtotheworld,butsocialmediacouldnevershouldnotreplacehumaninteraction
Belowarethreereasonsastowhyweneedtolearntoembracesolitude,despitethefearsofisolationasweare slowlyrecoveringfromtheeffectsofthepandemic
1.Beingaloneallowsustobetterinteractwithothers
JackFong,asociologiststatedthat‘Whenpeopletakethesemomentstoexploretheirsolitude’,notonlywillthey beforcedtoconfrontwhotheyare,theymightlearnalittlebitabouthowtoout-maneuversomeofthetoxicity thatsurroundstheirsocialsetting’.Itallowsustobuildconfidencemakingiteasiertomaintainourboundaries
2.Webecomeunshackledfromtheinfluenceofothers,freefromwhatothersmaythinkofus
Wecanallowourselvestobefreefromthepressuretosocialise.Theobligationstomakeplansandtobefreefrom theincessantanxietiesoflife.Eventhemostsocialhumanbeingsneedtimetodecompress.Toallowourselvesto discovernewinterestsandideaswithouttheworryofjudgementandopinionofothers
3.Whenwearefreefromtheconstantnoise,chatterandinput,wecancreatemeaningfuloutput.
Weliveinaworldfullofdistractions Aworldfilledwithconstantnoise There’sareasonwhyauthorsorartistsgoto acabininthewoodsorhidethemselvesinaprivatestudiotodowork.GeorgeOrwelltravelledtoaremoteisland towritehismostfamousandfinalwork‘1984'whichhedescribedtobe‘anextremelyun-get-atableplace’.
Socialisolationexistedbeforethepandemic,itwasexacerbatedduringthepandemicandcontinueseventoday
Soaswetransitionintothisnewnormal,wecangrievewhatwehavelost,butourorganisationcontinuestohold tightlyontowhatwestillhave Ourhumankindness Ourrenewedsenseofgratitude Ourpurposeandhope
So much can happen in a lap around the sun
365 days. 8760 hours.
31,536,000 seconds. Seconds that began to tick away as sweat stung the man ’ s eyes like tiny vipers; the nape of his neck damp, as his consciousness ebbed away with the pungent, suffocating heat. His hands clutched ever so tightly onto his briefcase, eyes glazed with the watch face As if time had become his captor
He immersed himself into the sleek office chair, finding a moment’s respite. Unphased and unkempt, he slid his eyes to his side, beholding a cornucopia of highrise buildings which lay under the raging sun. Monoliths of grand cities spiralled towards the yellow inferno that moored itself in the blue. There were no more ambulances that erratically offloaded at the emergency bay. No more restless days being throttled awake by the chime of his pager at his perfectly square desk guarding the second ward.
Only brittle silence, a sense of zeal and eternity that gripped the earth And somehow his reflection blurred into the pane of glass at his periphery. He tried to look away.
But he simply couldn’t.
His slicked hair gave way to his sunken cheeks; carving deep crevices beneath his eyes. He was met with this sense of –
He couldn’t remember the last time he smiled.
“It’s been a while. Doctor.” His coworker vacantly stated, “Is Montreal treating you well?” She endeavoured to inject a tinge of interest into the conversation.
“The winter is unsympathetic here Work is a different kind of fun like life is all a movie but one where I’m not given the script and won’t know how it ends.”
His thoughts flitted as she nestled the badge within his hands. He held it against the sunlight that radiated from his desk. Threads of amber emanated from the steel, illuminating the emblem of his once-acquainted institution It was an insignia of their youth the wintry nights in Tokyo, the time they both gazed into each others’ eyes in the pottery studio on Copper Street The first time they splurged on their first taste of luxury three times a week for cocktails at the bar with their fake IDS. He held it close to his heart.
“Thank you. ”
“No emergencies this time. Right?” The grin lingered on her face, perhaps for seconds. And those five utterances struck a chord within his chest Gripped him like taut chains that did not release him at his will Did she remember when they were youthful and ravishing? When life seemed limitless? When it’d seem impossible for him to get a job in the city?
And as the day bled into the night, he cradled the phone, beguiled by the neon lights that surged from the screen in the Uber. His fingers undulated over the keypad as he was warped into oblivion – stultified by the flares of light that penetrated the darkness. The name sounded unfamiliar as it rolled off his tongue.
E - mer - gen - cy He squinted his eyes – soon met with a text
“Did u switch off the desktop when u left tonite? ta.”
Disgust coiled within his stomach. Would it have taken too much time and effort to key in an extra three letters to simply express her gratitude? Or to thank him in person?
For a moment, the silence was drowned out by his thoughts Because so little can happen in a lap around the sun.
So little progress. Choosing to remain complicit in a life that wasn’t for him. Money. Fame. The tantalising exterior of prestige. The illusory pursuit for consumerist ideals at the expense of everything he once cherished. Idolatry traits that became a facade. Traits that began to chip away at his humanity. And all that was left within him was this sense of bitterness. Resentment against himself Resentment that was – numbing Like an anaesthetic
Because when was the last time he found true joy in his work? When had he last felt awe or ambition? He evaded the clamour as he sauntered towards Central Station. An hour's walk was far more appealing than chaos, he deduced.
The piercing alarms cut through the murky depths of his trance. His ears pricked at the thunderous, yet sublime hum of engines. His periphery gravitated towards the curve of the vehicle and its vibrant facade, electric against the darkness He considered the ambulance He considered the thought of people being conveyed from one place to another, across towns, cities, borders Across hearts The thought of viewing this lonely world under the blanket of stars – arteries of light contouring the heart of the metropolis. Pinpricks of shattered light marking another house, another family. Another passion. Another patient. Another soul. He considered the mind behind the operating table. The workers who breathed life into the hospice, the hands that sculpted its brick bodice. A timeless euphoria.
He found himself eye-level with the worker adorned in fluorescent, noticing the stretcher poised on left cue
“I’ve done this before. Please. Let me help.”
“Can you grab me the salve?”
He remembered when his fingertips danced away at the microscope in front of his very presence – the four walls of that sterile room He remembered the sensation when his fingers graced the chrome perfection of the scalpel at hand And together, they began to vigorously bandage the man. Like a rhythm. Like a well-oiled machine.
This moment was only a fraction of a lap around the sun. Ten minutes perhaps.
And yet, so much was happening. It was as if liquid adrenaline seeped into every facet of his body As if this was the only way his body truly knew how to speak And as the wounded male was strapped onto the stretcher, his dusty black eyes grazed over the man ’ s body – noticing his dust-laden slacks and blood-stained suit – impetuously overdressed yet perfectly aligned with the occasion. And with all his might, he bared a smile before being hauled into the vehicle.
“Carpe diem”.
“What?”
The worker nodded to the suited-man in deep gratitude, her lips curving upwards
“Seize the day”.
Warmth radiated in his chest. As if the warmth was unleashed from a locked strongbox within him that has burst open – its contents rippling free in a desperate escape. A haloing glow enveloped the starlit night above Jasmine Liew is a current student
He beheld the crimson and magenta hues that caressed the illusion of two moons against the dying sun –resplendent with energy and colour. The Chancellor of the sky, its rays holding the tapestry of earth under its command – even at night. Holding the very essence of life under its authority.
He didn’t blink – didn’t realise the heat that emanated from the badge adorning his chest he gently rubbed at.
Tears swiftly trickled down his folds of skin. It was the most beautiful thing he had ever seen.
He considered the first time he stepped foot into the wards – and the last. He considered the menial click-clack of Cassandra’s shoes as she hovered by his desk to return last week’s payroll, their roving relationship, the sentiment – the ambulance travelling towards the infinite spanse of the horizon. He considered the ephemerality of life – what was of it a lap of the sun ago. All around him was magnificence.
Light, power, space and sun the beauty of it all.
Perinatal healthcare is plagued by various systemic and individual barriers both in low income countries (LIC) and high income countries (HIC).
Though barriers manifest differently based on varying health settings, perinatal health outcomes are hindered universally. It is imperative to identify and examine the current landscape to prime suggestions for the future to ensure satisfactory levels of safe, accessible healthcare during childbirth.
Perinatal financing is arguably the greatest hurdle in LIC. In Sub-Saharan Africa, Caesarean sections (C-section) cost families over 10% of their average yearly income, whilst vaginal births are deemed affordable, costing approximately 1% [1].

In up to 47% of Malian households in which the mother succumbs to obstetric complications, the family incurs “catastrophic” expenditures, threatening the household’s ability to meet its needs [2]. In the United States, a country without universal health coverage, over 2 million people fall into a ‘coverage gap’ in which they do not qualify for either publicly funded Medicaid insurance nor receive Marketplace coverage through their workplace [3]. Those finding themselves uninsured predominantly live in states which have not opted into the expanded
Medicaid program - these states also offer lower minimum wages, fewer social welfare programs, and laws against abortion, further challenging pregnant women. 1 in 3 uninsured women have untreated hypertension, a risk factor for preeclampsia, intrauterine growth restriction, and other serious perinatal complications [4].
Living in remote and disadvantaged areas predisposes women to poor health literacy, contributing to challenges understanding prenatal care. For example, 8.8% of Australian women smoked cigarettes during their first trimester with the vast majority of these women living in remote or disadvantaged areas [5]. Poor health literacy may also interfere with the ability of women to communicate with
healthcare providers, recognise when to access healthcare services, and make informed decisions throughout their pregnancies [5].
In an attempt to improve health literacy, the USA has developed the ‘Centering Pregnancy’ program (CPP), which is a model whereby a pregnant person receives group-based care from a primary healthcare worker, such as an obstetrician or a midwife, throughout the duration of their pregnancy. The benefits of CPP are mainly derived from its group setting design, as it provides a safe space that encourages sharing of experiences and learning. This model resulted in reduced rates of preterm birth, low birth weight and maternal depression, as well as increased satisfaction with prenatal care felt by patients [6].
Surabhi Shashishekara, Olivia Melone, Paige Allen, Natania D'Sa, Chloe Lay from the Women's Health Interest Society of Monash (WHISM)Most LIC operate under a two-tiered model of childbirth care whereby “low risk” pregnancies are directed to primary care facilities whilst the “high risk” pregnancies are referred to advanced obstetric and neonatal services [7]. As a result, between 33-50% of births from the highest maternal mortality countries occur in community clinics where there is little recourse to lifesaving services (e.g. surgical and transfusion services) should the need for them arise [7].
While the two-tiered model of care seems efficient in theory, it is grounded by the assumption that risk stratification is reliable. In reality, 30% of pregnancies stratified as "low risk" translate to complications in HIC; this is further exacerbated in LIC as detection of antepartum risk factors is limited by poor quality antenatal care [8].
Furthermore, the model relies on having an effective emergency referral response to hospitals in the event of a complication during childbirth [9]. Intrapartum transport in high income countries itself is challenging and reserved for necessary cases, despite travelling on reliable roads in ambulances equipped with advanced life support. The ability to refer complicated births to a hospital in a LIC setting is increasingly more risky due to the poorer infrastructure [9].

While the two-tiered system worked to minimise the barrier of access previously, recent urbanisation and reductions in travel time has enabled LIC communities in Haiti, Malawi, Nepal and Tanzania to be within 2 hours of an advanced healthcare facilities, providing better access to hospitals and consequently less reliance on primary facilities [10].
Reforming the Landscape
De-tiering the current two-tier system and concentrating all obstetric and neonatal service advancements to fewer facilities allows for the development of high-delivery volume providers who are skilled in managing rare complications. Moreover, health system reform will naturally diminish the inequalities that currently exist as wealthier women bypass the twotiered system by acquiring higher quality care at an additional cost.
Redesigning the health system is a long term objective, however, there is scope for improving community care during the transition period. One such initiative is Malawi’s ‘Birthing Companions’ program (BCP) which incorporates volunteers from the community to provide emotional, verbal and practical aid during childbirth [11]. Non-healthcare specific supports and initiatives such as the BCP cements holistic care in primary facilities, providing a better maternal experience.
The private healthcare system of HIC is vulnerable to over medicalisation during childbirth, as seen in the rates of elective C-sections, which consequently hinders evidence based practice. Though the World Health Organisation (WHO) states that C-section rates should remain between 10-15% [12], it is 37% in Australia with 43-56% of planned C-sections before 39 weeks having no clinical indication [13]. Overmedicalisation of C-sections commonly leads to maternal complications (haemorrhage, excessive bleeding, endometritis, or wound infections, and newborn morbidities (impaired lung function metabolic issues, and immunosuppression) that can have longterm or life threatening consequences [14,15].
The increased C-section rates may be driven by poor health literacy regarding childbirth or coercion from the treating team for their own convenience or financial gain. In the United States, the elective caesarean section rate for African Americans is significantly higher at 36.8% compared to 32.7% for non-African Americans [16]. Although grossly over generalised, African-American women are more likely to have narrower and shallower pelvises which may complicate normal vaginal deliveries [17,18]. However, many obstetricians are prejudiced by this and push for women to elect for C-sections without individual assessment [18].
REFERENCES
MoriAT,BinyarukaP,HangomaP,RobberstadB,SandoyI.Patientandhealthsystemcostsofmanagingpregnancyandbirthrelatedcomplicationsinsub-SaharanAfrica:asystematicreview.HealthEconomicsReview.2020Dec;10:1-5. ArsenaultC,FournierP,PhilibertA,SissokoK,CoulibalyA,TourignyC,TraoréM,DumontA.Emergencyobstetriccarein Mali:catastrophicspendinganditsimpoverishingeffectsonhouseholds.BulletinoftheWorldHealthOrganization. 2013;91:207-16. GarfieldR,DamicoA,OrgeraK.Thecoveragegap:UninsuredpooradultsinstatesthatdonotexpandMedicaid.Peterson KFF-HealthSystemTracker.Disponívelem:.Acessoem.2020Jan14;29:1-1. https://everymothercounts.org/giving-birth-in-america/ (Liv2)AustralianInstituteofHealthandWelfare.NationalCoreMaternityIndicators[Internet].Canberra:AustralianInstituteof HealthandWelfare,2022[cited2023Mar.27].Availablefrom:https://www.aihw.gov.au/reports/mothers-babies/national-corematernity-indicators RisingS.CenteringPregnancyAnInterdisciplinaryModelofEmpowerment.JournalofNurse-Midwifery.1998Feb;43(1):46–54. LiuL,OzaS,HoganD,ChuYPerinJ,ZhuJ,LawnJE,CousensS,MathersC,BlackRE.Global,regional,andnational causesofunder-5mortalityin2000–15:anupdatedsystematicanalysiswithimplicationsfortheSustainableDevelopment Goals.TheLancet.2016Dec17;388(10063):3027-35. AoyamaK,DSouzaR,PintoR,RayJG,HillA,ScalesDC,LapinskySE,SeawardGR,HladunewichM,ShahPS,FowlerRA. Riskpredictionmodelsformaternalmortality:asystematicreviewandmeta-analysis.PLoSOne.2018Dec4;13(12):e0208563. Roder-DeWanSNimakoK,Twum-DansoNA,AmatyaA,LangerA,KrukM.Healthsystemredesignformaternalandnewborn survival:rethinkingcaremodelstoclosetheglobalequitygap.BMJGlobalHealth.2020Oct1;5(10):e002539. GageADCarnesF,BlossomJAluvaalaJ,AmatyaA,MahatK,MalataA,Roder-DeWanS,Twum-DansoN,YahyaT,Kruk ME.Inlow-andmiddle-incomecountries,isdeliveryinhigh-qualityobstetricfacilitiesgeographicallyfeasible?.HealthAffairs. 2019Sep1;38(9):1576-84. KungwimbaE,MalataA,MaluwaA,ChirwaE.Experiencesofwomenwiththesupporttheyreceivedfromtheirbirth companionsduringlabouranddeliveryinMalawi.Health.2013;05(01):45–52.
The Auricle January-March 2023 13
'accidental poetry found in the colossal library of electronic medical records'
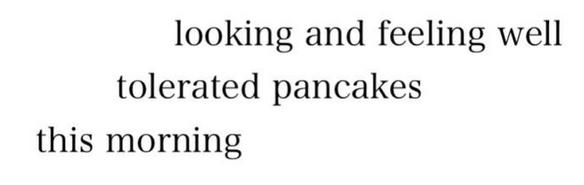
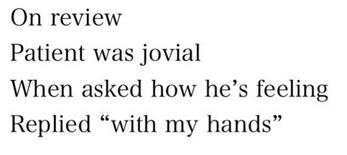
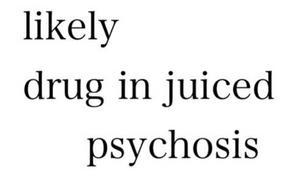
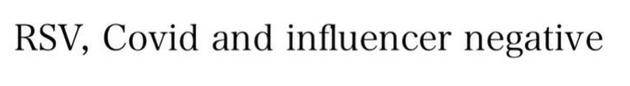




compilation of posts from Monash Med's favourite IG account


Some people do it for the free choccy milk, some people do it for the free strawberry milk (not really a valid reason), some for the great feeling they get afterwards, and Kavin does it for the compliments he gets on his veins. Where is this utopia with free food, compliments and good vibes you ’ re wondering? It’s a blood donation centre! Kavin and I, as the 2023 Monash Vampire Cup coordinators are spreading the word about how good donating blood is. We both love it, and we ’ re hoping more people like you will grow to love it too!
Kavin first donated blood in 2022 and since then has donated blood 6 times! I found out about blood donation in 2021 through the Vampire Cup (blood donation competition between medical schools all around Australia), and have been back twice more since then. We both decided to get involved in the competition this year because we think donating blood is super fun and important!!
Everyone knows that blood donation is essential, but we didn’t realise how vital it is until we got involved this year The demand is HUGE, and the current blood donors are not able to keep up with the need for blood products. This is where we can help! Every year for 8 weeks around the time of April, the Vampire Cup starts. This is a critical period in terms of blood donations because stocks are beginning to fall, and less people donate during the winter months. Lifeblood relies on Monash students and our friends and family members during this time, to keep enough blood available for people who need it!
Kavin and I have a few goals for this years competition With your help, we want to create a new cohort of lifelong blood donors. Regular donors can donate blood every 12 weeks, and plasma every 2 weeks. It’s a good habit to get into, taking only about an hour out of your day every time you donate, and potentially saving three lives! We are hoping to make people realise this is a habit they can incorporate into their lives, while making a massive difference to people who need blood! Last year was a mammoth effort from the Monash students (362 donations!) but this year we reckon we can top it For the Vampire Cup 2023 we are hoping to get 1.5 times the donations we made last year (=543 donations). Hopefully, with this number of donations we can take out the top spot and beat the smug JCU med students :)
We’d love to get you involved in blood donating, so check out our ‘Monash AMSA Vampire Cup 2023’ facebook page for more blood donation updates, or www lifeblood com au for awesome info and resources! Get around it!
- Ella and Kavin (2023 Vampire Cup coordinators)