

Drug Round Interruptions, Prince Philip Hospital
Sister Amber Bolt, Manager Ward 1, Sharon Jones QIST Practitioner & Eleanor Pearce QIST Facilitator
Background, Aims and Objectives

Ward 1 nurses were frequently being disturbed during medication rounds resulting in an increased risk of errors and patient harm. Our Improvement Project ran from 11/01/22 until 09/06/22. Our AIM was to reduce the amount of interruptions and errors. A data collection tool was designed to analyse the main causes and themes, 12 PDSA cycles were carried out and a wider culture change was embedded to help people refrain from making unimportant interruptions, give the nursing staff the confidence to say “no” when being interrupted unnecessarily and identify other members of staff who can be interrupted.

PDSA 2/ 10/02/22
Doctors to change the time of their morning ward round so as to not clash with the medication round. At the request of the ward manager doctors have changed their morning ward rounds to 9.30am from 10/02/22

Outcome Measures
Process Measures













Balance Measures
PDSA 3/ 14/02/22
Creation of posters and door handle signs agreed and developed
Delivered to the ward on week commencing 14/02/2022.
Avoid harm to patients by working together on the ward

Identify interruptions during medication rounds





Staff feedback regarding interruption reasons
PDSA 5/ 28/02/22
HCSW to begin observing medication rounds with new audit form.



The view ultimately is to give them a role as Safety Links.


PDSA 12/ 20/05/22
Ward manager meeting with staff to discuss the implementation of reminding staff members and patients that they are on a drug round when disturbed with the assurance that they will speak to them on completion. Also, ward manager to support staff in embedding new culture.
Reflection
The fact that it is the registered nurses responsibility to focus on medication rounds doesn’t mean that other members of staff don’t need to play their part. We learned that it is important for everybody to understand that medication rounds are protected time. This made the nurses feel less stressed and created a better team atmosphere.
We are embedding the cultural changes throughout the Health Board. by spreading and scaling this project across all wards in Prince Philip Hospital. We are also providing training to Newly qualified nurses, Junior Doctors and recently we have been recognised by Swansea University who now use our learning and presentation in their Business School & Nursing school as part of their Medication Safety lectures
Its ok to say “no” to drug round interruptions

QI Project Improves Safer Psychiatric Physical Health and Informed Prescribing
 Dr Bjørn Varder (CT1 Psychiatry), Emma Livesey (Advance Clinical Practitioner), Dr Sally Arnold (Consultant Perinatal Psychiatrist).
Dr Bjørn Varder (CT1 Psychiatry), Emma Livesey (Advance Clinical Practitioner), Dr Sally Arnold (Consultant Perinatal Psychiatrist).


Further improvements to the physical health board to make it more comprehensive with colour coding to improve physical health investigations further. .
Re-audit and review
Physical health review should be undertaken within 24 hours
Pre-intervention: 75% had a physical assessment within 6 hours of admission, 10% within 24 hours, and 15% with no assessment. Post implementation: All but 1 had a physical health assessment done within 6 hours of admission and the remaining 1 had an assessment done with 24 hours.
Recognising the importance of physical health and how we needed to improve.
Pre-audit, and implementation of a physical health board to recognise what interventions are needed.
ECG investigation
Pre-implementation: 15 patients had an ECG completed, 3 not completed and 1 patient who declined.
Post implementation: All patients had an ECG completed.
Blood monitoring for patients on antipsychotics.
Antipsychotic monitoring ensures safe prescribing. Data post intervention showed further scope for improvement, and now on the board there is a list of which blood tests required for antipsychotic monitoring

Contraception
All patient should have contraception discussed before discharge.
Pre-implementation 55% had a discussion regarding contraception.
Post-implementation: 85% had a discussion around contraception. Reason for not discussing was due to the patient being too psychiatrically unwell to engage. The board then changed to reflect discussions and contraception being in place.
Green (on contraception)

Yellow (discussion about contraception has taken place, but not on contraception yet)

Red (contraception discussion needed).

Contraception
Discussed During Admission? (PreIntervention)
A closed-loop audit on venous thromboprophylaxis prescriptions in an acute general hospital
 Jun Yu Chen, Mustafa Kareem and Danujan
Jun Yu Chen, Mustafa Kareem and Danujan
INTRODUCTION:
Venous thromboembolism (VTE) occurs secondary to deep vein thromboses within the leg. It classically presents as acute leg swelling, pain and breathlessness and is the leading cause of preventable deaths in hospitals.(1) COVID-19 infections are associated with an increase in VTE underlying the increased importance of VTE risk assessment.(2)
AIM:
To objectively review the adherence to venous thromboembolism prophylaxis prescriptions in an acute general hospital.
METHODS:
Following two previous plan, do, study and act (PDSA) cycles conducted in July and December 2021, two further cycles were conducted in March 2022 (Cycle 3) and April 2022 (Cycle 4).

Act:
Cycle 3 - presented findings at departmental meeting and displayed posters
Cycle 4 - added a section on VTE into induction handbook and discuss assessment and reassessment at departmental induction
hospitalisation
VTE is the #1 cause of preventable
Every 37 seconds, someone in the VTE risk assessment is quick and

VTE risk assessment is a quick and effective tool to reduce

Regular VTE reminders are essential to ensure consistent

UHMB Cross-Bay VTE Audit 2022
Background and Aims
Methodology and Standards
first dose administered within 14 hours of admission
100% of patients had VTE prophylaxis/management reviewed on the first consultant review Additional areas were reviewed after discussion in audit meetings in previous cycles: Patent's’ receipt of verbal and written information about thromboprophyalxis If patients were to be discharged on extended VTE prophylaxis with low molecular weight heparin, was appropriate information and training given? If the patient was SARS-CoV-2 positive, was the modified regimen for thromboprophylaxis given?
Results (October 2022 cycle)
65% compliance of
Action Plan


Conclusions
Clear improvement has been demonstrated in compliance against NICE and local guidelines.

However we have room for improvement in administration of enoxaparin within 14 hours of admission, PTWR/consultant review of VTE prophylaxis, and provision of verbal and written patient information regarding VTE

Audit of Medicines Reconciliation timings for General Surgery admissions
Robert Hwang, Scott Crosbie, Marianne Gazet, Suzana Anjum, Charlotte AllanIntroduction
• Medicines reconciliation is the process of recording and prescribing patients’ regular medications upon a change in care setting such as hospital admission (1). NICE states that this should be completed within 24 hours of admission.
• Timely completion of medicines reconciliation allows the healthcare professional to continue the patient’s regular treatments while applying any modifications made necessary by the acute presentation, such as preventing any interactions with newly prescribed medications.
Aims
• To evaluate Royal London Hospital General Surgical department compliance with the NICE guideline of completion of medicines reconciliation within 24 hours of admission.
Methods
Intervention:
• Written correspondence to all members of the team emphasising medicines reconciliation
• Tickbox column added to handover sheet
• First cycle: Patients on the General Surgical take list between 05/12/22 and 18/12/22 (n=61).



• Exclusion: <18 years old, <24 hours admission.
Re audit:
• Performed using the same methodology between 20/02/23 and 03/02/23 (n= 46).
Results
• First-cycle : 62.3% meeting the target
• Second-cycle results: 74.0% meeting the target
• Overall improvement of 18.7%
Conclusion
• Visual reminders and increased awareness enhance the team’s ability to meet National targets for Medicines Reconciliations.
References & Acknowledgements
1) National Institute for Health and Care Excellence (NICE), Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes. 4th March 2015.
2) World Health Organization (WHO). Standard Operating Protocol for Medication Reconciliation. Version 3. Many thanks to the Royal London Hospital General Surgery department for their support in this project.

Improving documentation and teamwork in an oncological emergency




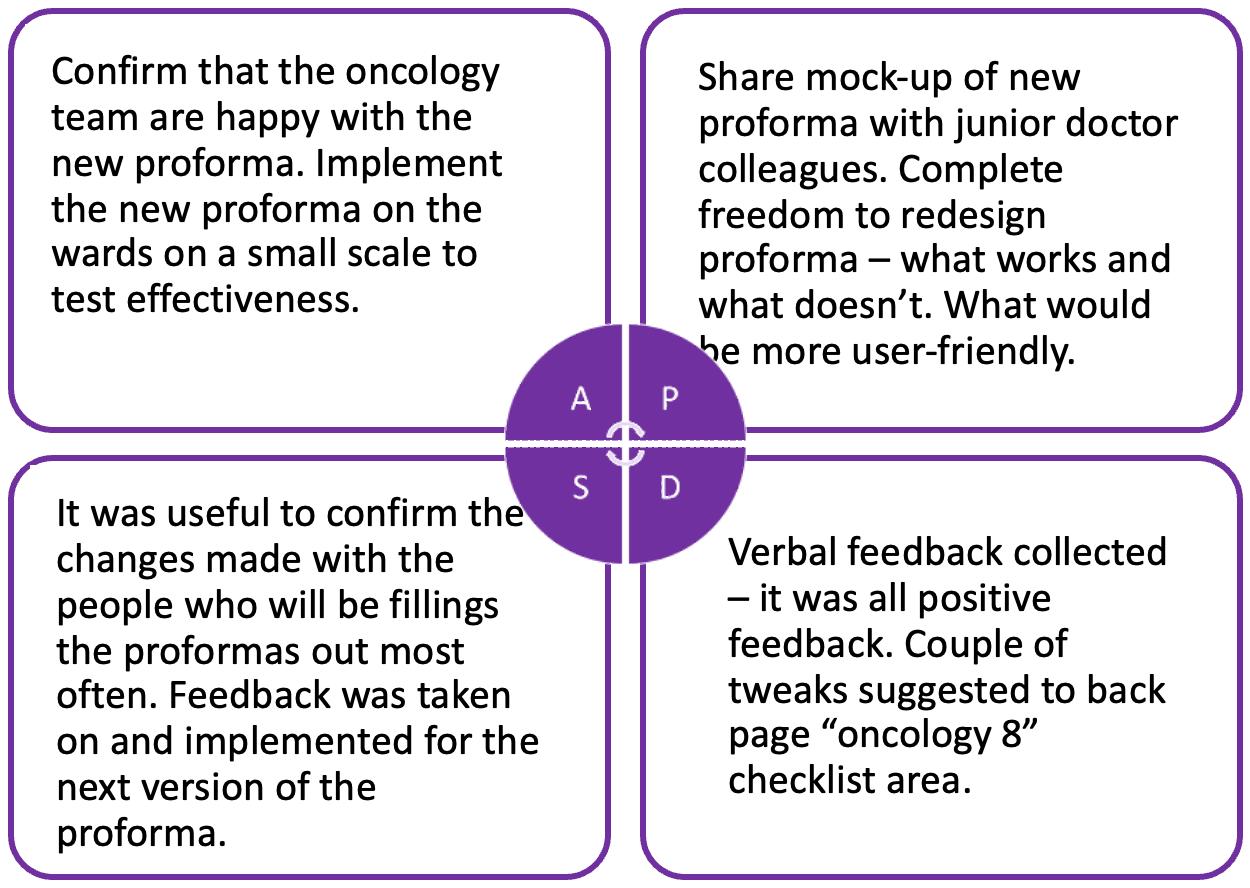









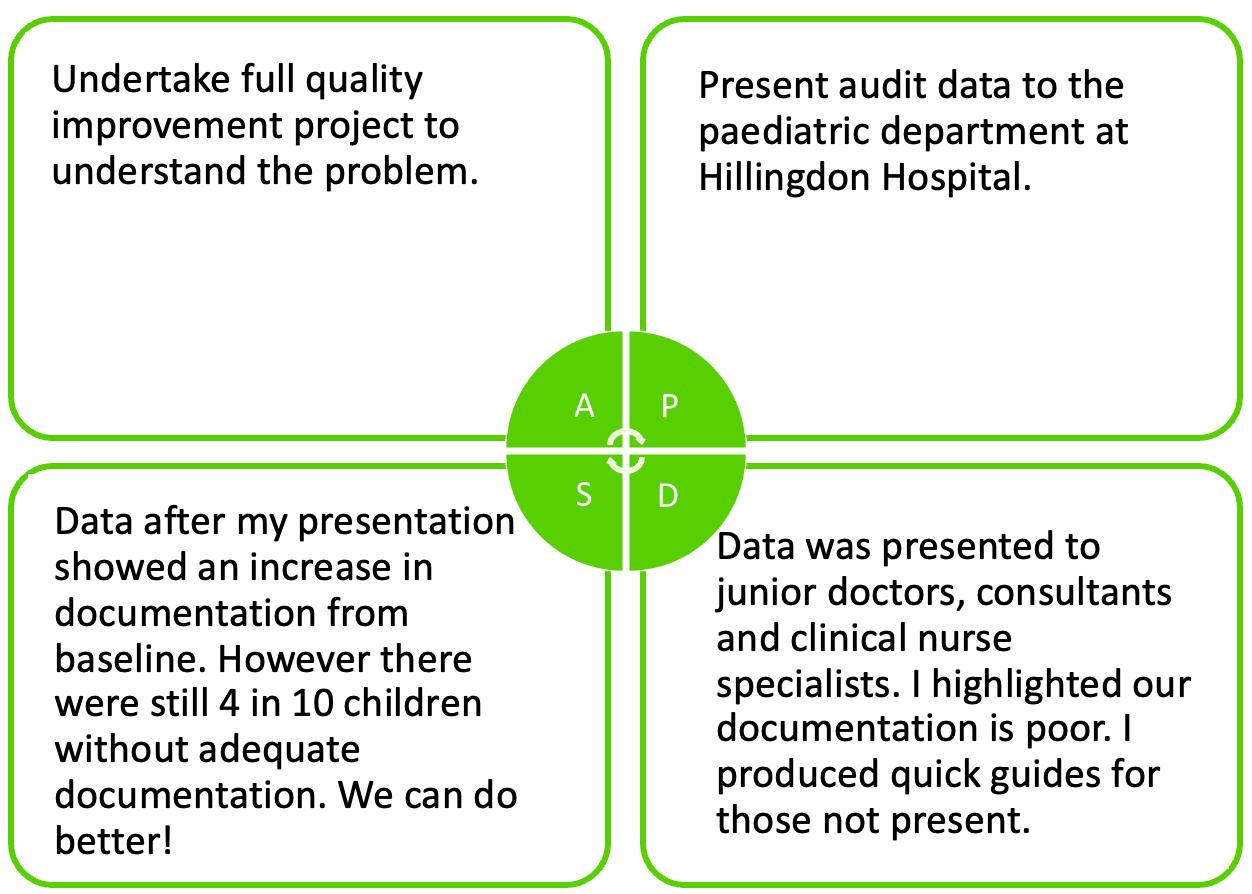

















Polly Outram Hillingdon Hospital


Authors: Bonnett, MH; Bacon, S; Mullins, J; Westcott, C
Clinical Transformation of an adult VTE Risk Assessment form
Why?
NICE and the VTE Exemplar Centres guidelines advises:
• 95% of patients should be risk assessed for:
• Venous thromboembolism (VTE) risk

• Bleeding risk
Internal Trust audits of VTE Risk Assessment compliance shows a range of completion as low as 70%.
Aim
1. Create a single standardised digital VTE Risk Assessment




2. Provide safe up to date clinical decision support (Fig 2.)
3. Improve completion compliance to meet national 4. improve patient choice faith and non 5. Improve patient 6. Support clinical teams to decommission paper forms


7. Future proof for future changes


Clinically led Transformation
Audit
Clinically led transformation:
The informatics team followed a cycle of transformation (Fig 1.) to design and implement a solution within the constraints of the system


Collaboration and engagement with:
• key stakeholders

• users
• Patients
Project Results










75% of the paper forms do not follow BNF & Trust guidance for pharmacological thromboprophylaxis. 0% of forms mention Fondaparinux as an alternative not containing animal
Feedback gathered & reviewed Collaboratively design the next iteration of the form. Roll out to more trust areas - Target compliance 95%

Launch digital VTE Risk assessment form, and flow board compliance indicator. Target compliance of 95%. Results Compliance of 88-91% (baseline improvement 18%).
Current and future state process maps (Fig. 3). A draft VTE Risk Assessment form was collaboratively designed
Review of all paper VTE Risk Assessments in use. Analyse the findings (Fig. 4,5,6). Make recommendation for change
THE USE OF A PATIENT PARTICIPATION SURVEY TO IMPROVE PATIENT EXPERIENCE IN A PAEDIATRIC EMERGENCY DEPARTMENT
 Dominic Ayi Gyimah Jordan Evans Michael Fox Cardiff and vale University health board Paediatric emergency department
Dominic Ayi Gyimah Jordan Evans Michael Fox Cardiff and vale University health board Paediatric emergency department
 Dominic.gyimah@wales.nhs.uk
Dominic.gyimah@wales.nhs.uk
Introduction
• Feedback on patient experience can help improve patient choice, self care and shared decision-making
• It is not always clear how to best collect and use feedback and the reality of implementation may be complex and yields suboptimal evidence of impact.
• Our aim was to improve the collection, analysis and utility of patient feedback that will inform improvement to patient experience in a Paediatric Emergency Department
Methods
• A team of stakeholders including the Patient Experience Team, Paediatric ED doctors, nurses and project managers was formed
• Patient-facing feedback posters were produced with QR codes to an online anonymous feedback survey (available in Welsh and English)
• Following initially low numbers of responses staff were provided with QR business cards for patients to scan on discharge and an iPad with the survey provided
• Later patients were all given the QR code cards to take away.
• Results were collated, anonymised, and then thematically analysed Pareto analysis was used to determine the most frequent compliments and complaints. The cumulative percentage line in the Pareto chart helped to analyse the effect of each category


Outcomes
The feedback collected resulted in:
• At baseline, we had an average of 5 survey responses per week.
• Following distribution of staff QR business cards and patient QR code cards, survey responses increased to 313 over the study period.

• Pareto analysis revealed attitude and relationship with staff, timeliness and communication accounted for 80% of feedback
• Other feedback related to the built environment and physiological needs such as improving the child -friendly environment and access to food and water.
• The provision of food and drink to patients in the paediatric emergency department
• Improved seating for breastfeeding mothers
• New flooring and child-friendly decoration of the department
Labelling X-ray compatible operating tables in Urology
Background
Insertion of a double-J (DJ) ureteric stent requires intra-operative fluoroscopy to confirm the position of the stent. Therefore, it is essential that the operating table is radiolucent; a factor, sometimes overlooked, leading to unnecessary interruptions during the surgery, and potentially a threat to patient safety.
Aim
To devise a fool-proof method of identification of X-ray transparent operating tables.
PDSA 1
Plan/Do: To document instances where a radiopaque operating table was used during the insertion of a DJ stent.

Study: In September 2022, there were 2 instances of radiopaque operating tables being used. The error was discovered midprocedure after the patient had been intubated. Patients were then shifted onto the correct trolley. No injuries or complications were reported, and the procedures were completed successfully
Act: Design and display visual aids on operating tables to correctly identify radio-compatibility.
Conclusion
PDSA 2
Plan/Do: To measure the change in practice after implementation of change
Study: In the month of October 2022, there were no instances of a radiopaque operating table being used for DJ stenting procedures.
Future action: To apply appropriate stickers on all operating tables. To educate new members of the team about the importance of confirming use of X-ray compatible operating tables.
Prominent labelling of operating tables, identifying X-ray compatibility, is a simple yet effective method of minimising errors related to incorrectly using Xray-incompatible tables for procedures requiring intraoperative fluoroscopy.

 Arman Z Chacko, Eng K Ong Royal Devon University Healthcare Trust, Barnstaple, North Devon
Arman Z Chacko, Eng K Ong Royal Devon University Healthcare Trust, Barnstaple, North Devon
AUTHORS: DR ROWENA GNANAPRAGASAM AND DR FAHAD

INTRODUCTION
• Patients need to be informed if a condition impacts their ability to drive to ensure their safety
• Between January to March 2022 , only 3 % of Cardiology patients at King George Hospital, Ilford received driving advice on discharge
• The DVLA’s guidance on driving advice for cardiovascular conditions is over 20 A 4 pages and is not easily digestible

• We created a concise A 4 page poster containing driving advice for Acute Coronary Syndrome ( ACS ) and Heart Failure (HF) and investigated whether this increased the proportion of patients receiving driving advice

METHODS
Study design and participants
• This was a single - centre study based on the ward at King George Hospital, Ilford
• Inclusion criteria :
o Diagnosis of ACS or HF
o Aged 18 years or older
o The patient had to be able to understand English
• Primary outcome : Whether the poster increased the proportion of patients receiving driving advice
• Secondary outcome : Whether the poster improved the confidence of doctors giving advice
Initial survey
• A survey of the junior doctors found that:
PDSA Cycle 1
• We created an A 4 poster containing DVLA guidance and displayed copies in the doctors’ office between 15 th April to 13 th May 2022
• The discharge summaries (N= 50 ) were audited over this time
RESULTS
Primary Outcome
• Between January to March 2022 , only 3 % of Cardiology patients (N= 101 ) at King George Hospital, Ilford received driving advice on discharge
Secondary Survey
• A survey distributed to junior doctors found that 2 factors hindered them giving advice :
o Uncertainty of NYHA class (80 %)
o Time pressures (20 %)
• They suggested that clear designation of NYHA class would reduce uncertainty and an online poster would allow them to copy information into the summary increasing efficiency
PDSA Cycle 2
• Between 21 st June to 12 th July 2022 , the heart failure nursing team designated the NYHA class of each patient in the notes and a pdf of the poster was distributed to the junior doctors
• The discharge summaries (N= 29 ) were audited over this time
• Between April to July 2022 99 patients were recruited into the study
• The physical poster led to a 13 - percentage point (pp) increase in patients receiving advice ( 16 % of patients)

• The online poster and designation of NYHA class led to an 37 pp increase in patients receiving driving advice compared to the number prior to the study ; where 40 % of patients received advice
• 24 % of patients received advice over the study period
Secondary Outcome
• By the end of study, 100 % doctors felt confident giving advice
DISCUSSION
• Prior to this study, King George Hospital was not consistently providing information to patients on the Cardiology ward and only 3 % received driving advice
• The physical copy of the driving advice poster increased the proportion of patients receiving advice to 16 %
• An online copy of the poster and designation of NYHA class improved efficiency of doctors and increased the proportion of patients receiving advice to 40 %
• The poster also improved the confidence of doctors in providing advice to 100 %
• Overall, the study suggests that this poster may increase the proportion of patients receiving advice on discharge and help to ensure patient safety
• A larger sample size and longer investigation period would provide more accurate analysis
CONCLUSION
• The poster increased the proportion of patients receiving advice increased from 3 % to 40 %
• The poster increased the confidence of doctors in giving advice
