

THE SURGICAL PATIENT – AN IMPORTANT AND UNDERMANAGED CAUSE OF MORBIDITY AND MORTALITY

• Hyponatraemia is the commonest electrolyte abnormality in hospitalised patients.1
• It is associated with increased morbidity, mortality and length of stay.2
• NICE have extensive guidance on the assessment and management of the condition 3
Plan: All surgical inpatients at a single centre, cross sectional analysis, 24 variables collected, 3 PDSA cycles over 6 months, compared to NICE guidance
• Aims: To identify whether an issue exists and how it is managed, comparing local standards to national guidance .
• To provide a framework for clinicians to improve care, reducing complications and length of hospital stay

• Methods: A cross sectional analysis of all surgical inpatients was performed. Laboratory findings and clinical notes were reviewed.
• The audit cycle was ran 3 times.
• Results were analysed after each intervention and compared with baseline data
•
% of Patients
% of Patients
15
Study: 0
10
5
20 Cycle 1 Cycle 2 Cycle 3
Treatment Commenced
% of Patients
Paired Osmolalities Sent 0 5 10 15 20 25 30 35 Cycle 1 Cycle 2 Cycle 3

Complications
% of patients
50



40
Do: New intervention each cycle 10
Documented Fluid Status Examination 0 5 10 15 20 25 30 35 Cycle 1 Cycle 2 Cycle 3
30
20
60 Cycle 1 Cycle 2 Cycle 3
• References: 1. Corona G, Giuliani C, Parenti G, Norello D, Verbalis JG, Forti G, et al. Moderate hyponatremia is associated with increased risk of mortality: Evidence from a meta-analysis. PLoS ONE. 2013;8(12).
• The improvements noted after each cycle were both additive and sustained.
.
• 2. Peri A, Thompson CJ, Verbalis JG (eds): Disorders of Fluid and Electrolyte Metabolism. Focus on Hyponatremia. Front Horm Res. Basel, Karger, 2019, vol 52, pp 36-48
• 3. CKS is only available in the UK [Internet]. NICE. National Institute of Health and Care Excellence; 2020 [cited 2022Oct13]. Available from: https://cks.nice.org.uk/topics/hypona traemia/management/management/
Key Messages: Hyponatraemia is a prevalent problem in this population.
• The changes we implemented improved patient care
National standards for investigation and management were better adhered to and complication rates were reduced.
IMPROVING PATIENT FLOW BETWEEN WHITEBOARD SYSTEMS
By Hannah Chow and Ben Langhorne,BACKGROUND

The current method of recording new referrals and inpatent under the care of Liaison Psychiatry uses Microsof (MS) Word. Each Word document records diferent informaton. One board for new referrals, one for inpatents, and one for closed patents.
The limitatons of this method include:
Only one user being able to edit the board at once Manual highlightng and formatng of boards
• Manual copy and paste of informaton between MS Word documents can lead to patents getng missed if triage becomes distracted between tasks
Aims:
To increase the accuracy of informaton being stored on the whiteboard system. We will measure this by asking staf for feedback on accuracy of the informaton being recorded using a Likert scale, and aim to improve upon this baseline value. This will improve patent safety since patents are less likely to be missed.
To improve accessibility of the whiteboard by increasing the number of users able to access the whiteboard at once from one to ten.

To improve staf communicaton using the whiteboard system by measuring current subjectve communicaton perceptons using a Likert scale and improving upon this baseline value.
• We achieved this on 30th November 2022.
CHALLENGES BEFORE LAUNCH
We encountered several challenges whilst trying to implement our inital whiteboard launch.
Our challenges included:
• Excel is not deemed secure enough for patents’ data, so can only use via MS teams
Current Trust IT policy did not allow us to build on existng programme therefore implemented code to move data between cells in Excel MS Teams was automatcally deleted
• The IT support team were unable to assist
• Only members added to MS team could access whiteboards
Manually saving copies of the whiteboard throughout the day
CHALLENGES AFTER LAUNCH
Our inital whiteboard launch was well received and worked well for a few days before it got accidently deleted by the team.
We identfed the following as reasons for this:
Although whiteboards were auto-saved, team were unsure how to restore it back to the latest version
• Difcultes with team members quickly adaptng to IT changes
Only members added to MS team could access whiteboards
• The 3 of us who created the new whiteboards were absent from the ofce at the tme of deleton so unable to help with restoraton
• There was no ‘help sheet’ to assist with guiding the team
with thanks to Sam Kirkwood.
IMPROVE
We took responsibility for this and made the following improvements:
We increased the numbers of staf who were able to add new members
• We created a step by step ‘help sheet’ with numbered steps. Each with a clear instructon of what the user needed to do and included an annotated screenshot at each stage
• We circulated this document to the wider team via email, uploaded it to be accessible on the main MS teams channel and printed it out for both the admin team and displayed a copy in the shared hot desking ofce

We ofered the wider team a 1:1 run through of how to use MS teams and ensure they were comfortable with using it independently
• We ensured there was an allocated tme during the weekly team meetng to answer whiteboard Q&As
We also were able to show the team how to navigate the whiteboards physically via projector
CONCLUSION/ LESSONS LEARNT
• This project was a simple yet efectve way of improving an area of daily team frustraton
• We have learnt the importance of keeping the wider team involved, encouraging ongoing suggestons and actng promptly on feedback.
• This helped maintain the momentum for relaunching our improved whiteboards
New whiteboards preferred by the team due to real tme documentaton and improved accessibility
Next steps are to share the project with other teams who could beneft from these changes
CONTINUOUS IMPROVEMENT
Using the PDCA Model

SHORTEN THE TIME, SHORTEN THE PAIN
Ensuring first visit injection in booked patients



BACKGROUND
• Patients booked in for joint injections have had to be turned back on at least one visit, and re -booked into a future clinic.


• Prolonged pain and distress + Incurred commuting expenses = Poor patient satisfaction


• Wasted slots = Loss of NHS money and resources
• Time and resources of staff are also wasted, leading to gradual build up of frustration.
DIAGNOSTICS
AIM & MEASUREMENT DEFINITION

CHANGE IDEAS
PDSA cycles


RUN CHART
REFLECTIONS & LEARNING

• Modifying appointment letters made a huge improvement to outcome of joint injection clinics, further buttressing the importance of adequate communication with patients.








• Injection slots are now being better utilized, leading to patient and staff satisfaction.




• One change can make a huge difference
• Working with members of staff across various cadres, taught me a lot more about management and leadership.
Acknowledgements: Nicola Vanes, Emma Harvey, All Royal Wolverhampton
Rheumatology Staff
 Adeola Ajibade 1 , Latika Gupta1, Preet Singh1, Heather Shearer 2 , Stephanie Meddick-Dyson3, Nicola Davey2 1
Adeola Ajibade 1 , Latika Gupta1, Preet Singh1, Heather Shearer 2 , Stephanie Meddick-Dyson3, Nicola Davey2 1
Improving Compliance with Renal Cell Carcinoma Follow up Post Nephrectomy
Mrs Sophie Davies, Uro-oncology Cancer Nurse Specialist Mrs Karen Edwards, Uro-oncology Cancer Nurse Specialist Ms Kim Davenport, Consultant Urological SurgeonIntroduction
This project was performed within Urology after identifying deficiencies in patient follow up after kidney cancer surgery
Surveillance is recommended for at least 5 years following surgery to detect early recurrence or residual disease There is no consensus regarding the best schedule for surveillance scans with a number of different protocols offered nationally and internationally

In 2008, after an extensive literature search, a local protocol was designed based on patients’ being categorised into low, intermediate or high risk groups for recurrence

This protocol was validated in 2021 This data showed 66% of the high-risk group missed at least one scan and 48% missed 2 or more scans over the 5-year period Only 34% were compliant with protocol
Smart Aim
We aimed to improve protocol compliance by 30% over 12 months through colleague and patient education and involvement
Methods
Process mapping allowed us to understand why there was so much variation and allowed us to identify areas to improve

Risk allocation was added to the kidney specimen histology report This was discussed and documented in the MDT and added to the MDT outcome sheet
Patient involvement was encouraged through the use of specifically designed risk group patient information leaflets providing patients with a personalised plan for their follow up

A prospective audit was then performed to assess compliance with protocol for all new patients post nephrectomy between November 2021 to October 2022
Data for 43 new patients post nephrectomy were reviewed 34/43 had their risk discussed in MDT with 31/43 documented on the outcome sheet (see figure 4)
The initial audit data was presented to urology and uro-radiology colleagues in November 2021 and an updated protocol based on new literature/practice agreed (figure 2) Laminated copies were distributed to colleagues and placed in clinics
Every patient should be scored with Mayo and UCLA systems at MDT & documented on MDT Outcome Sheet
Low risk Clinic at 6 wks – Explain histology, provide CNS details & appropriate Patient information sheet
CT Chest/Abdo/pelvis at 24 & 60 mths & Discharge if clear at 5 years
Risk of progression: 0.5% at 1 yr & 2% at 3 yrs (75% lung)
5yr recurrence free rate 10% (local data 2010-2014 4%)
Median time to recurrence 29 mths
Clinic at 6 wks – Explain histology, provide CNS details & appropriate Patient information sheet
Intermediate risk
Protocol compliance was 100% in the high-risk group, reducing to 66% for the intermediate-risk and 63% for the low-risk groups
Overall protocol compliance increased from 34% to 76% during the study time period (see figure 5 for monthly compliance from Nov 21 to Oct 22) The remaining patients had their scans planned earlier than indicated No scans were omitted
Figure 5 Monthly compliance with protocol from Nov 21 to Oct 22
CT Chest/Abdo/pelvis at 12, 24, 36 & 60 mths & Discharge at 5 years
Risk of progression: 20% at 3 yrs (42% lung occurs in Yr 1)
5yr recurrence rate 38% (local data 2010-2014 24%)
Median time recurrence 18-24 mths
High risk Clinic at 6 wks- Explain histology, provide CNS details & appropriate Patient information sheet
CT Chest/Abdo/pelvis at 6, 12, 24, 36, 48 & 60 mths
Consider CT Chest/Abdo/pelvis at 84 mths if patient PS 0-2 and age appropriate
Risk of progression 60% at 3 yrs – majority Yr 1, 68% local recurrence (60% in first 6/12)
Median time to recurrence 9-10 months
5yr recurrence rate 58% (local data 2010-2014 50%)
Few patients develop recurrence with longer follow-up
Lessons Learnt
To improve compliance, we had to engage all involved, from the patient to their surgeon, the cancer nurse specialist, histopathology and radiology colleagues Early involvement allowed us to achieve our aim in a relatively short time frame

Next Steps
Patient involvement and the use of an excel tracker file should improve compliance further Longer term, we are in discussion with radiology to allow bulk requesting of all surveillance scans required
Figure 2: Revised Surveillance Protocol Figure 4 MDT risk group discussion and documentation Figure 1: RCC Follow up Process MapAntimicrobial Stew ardship : Deprescribing Urinary Tract Infection (UTI) Antibiotic Prophylaxis at Ty’r Felin Surgery
W. Ul-Haq, N. Lewis, Dr. K. Hawkins, Dr. S. Greenfield, Dr. J. Sartori, Dr. N. Rice, Dr. J. Kerrigan, Dr. L. Newington, Dr. C.Smith, Dr. L. Heath and Dr. A. Rees-Evans
Ty’r Felin Surgery (TFS), Gorseinon, Swansea (2022)

Introduction
• The Welsh Government states that antimicrobial resistance (AMR) poses a significant threat to life as approximately 700,000 people die annually from infection globally1

• Long-term antibiotic prophylaxis is strongly associated with the development of AMR
• A study published in the BMJ has demonstrated that Methenamine Hippurate, a non-antibiotic prophylactic treatment, is appropriate for women with a history of recurrent episodes of UTIs2
• SBUHB guidelines recommend methenamine Hippurate as an antimicrobial sparing agent that can effectively prevent UTIs while reducing the use of antimicrobial use meeting Welsh Government targets3
• Therefore, a Quality Improvement Project was commenced to analyse current UTI prophylaxis prescribing at TFS against SBUHB guidelines.
Methodology
This study did not require ethics approval.
Search on Vision system (including trimethoprim, nitrofurantoin, nitrofurantoin MR and cefalexin) to identify patients currently prescribed UTI prophylaxis.
Exclusion criteria: pregnant women and patients <14 years old
Contemporaneous analysis of prescriptions using data collection form: drug choice, dosing, duration, renal function, MSU results.
Results compared against SBUHB UTI Prophylaxis Guidelines via MicroGuide App.

Individual patient cases discussed with relevant prescribers according to prudent healthcare principles (GP, Clinical Pharmacist), followed by patient telephone encounters to implement ongoing AMS in practice and discuss self-care measures (hydration, urge-initiated voiding etc.)
Results
Quarter ending June 2021
Discussion
• 54% of patients were successfully stopped or switched to methenamine, exceeding national targets set by WHC for this patient group 100% of patients remaining on prophylactic antibiotics are treated according to SBUHB Antimicrobial treatment guidelines.

This Quality Improvement Project demonstrates the importance of the Pharmacy team within a GP practice in providing impartial prescribing analysis, and effective multi-disciplinary team decision making in delivering patient-centred care and co-production in practice; This project resulted in the implementation of new guidelines into current practice.
Limitations: future additional independent analysis of data required to remove variation and personal subjectivity.
Conclusion: following successful AMS campaign, 3 monthly UTI prophylaxis reviews are now embedded in practice to reduce potential of antibiotic resistance.
3.SBUHB. Recurrent (Symptomatic) lower UTIs in adult women [Internet]. MicroGuide Viewer - Web Viewer. [cited 2022Nov20]. Available from: https://viewer.rx-guidelines.com/SBUHB/Abx#content,9375c1aa-0afe-4002-aee99e64ac545a7d
Figure 2: Quality Improvement Project: UTI Antibiotic Stewardship Outcomes
• 0.1 % of practice population prescribed UTI prophylaxis (11 patients).
• 64% of prescriptions initiated in primary care.
• 3 patients (27%): antibiotic stopped;
• 2 patients (18%): antibiotic continued;
• 3 patients (27%): switched to methenamine;
• 3 patients (27%): switched to alternative antibiotic.
Variability in Predicted DLCO During Pre -operative Assessment Across a Lung Cancer Alliance
Dr Leah Argus1, Dr Matthew Evison1, Mr Felice Granato1PDSA Cycle 1







MFT Wythenshawe is sole thoracic surgical centre for Greater Manchester cancer alliance


- Referrals from 10 Trusts1
- ~500 lung cancer resections per annum1
International lung cancer guidelines place significant weight on predicted postoperative forced expiratory volume in 1 second (FEV1) and diffusion capacity of lungs for carbon monoxide (DLCO)2-5

Clinicians at surgical centre suspected PFT results differ across referring trusts

Introduction Aim
Reduce unnecessary repeat PFTs between at surgical centre by April ‘20
- Identify and quantify duplicate testing and PFT variability

- Identify source of variability
- Assess impact on lung cancer pathway times
Key Interventions
Adoption of Global Lung Initiative reference equations
Recommendations for standardised practice to regional cancer alliance
Local education
Limitations
Covid-19, cancer referrals & operating volumes
Service re-structuring & improvement

Lessons Learnt
P – Identify departmental perception of PFT variability
March 2019
D – Interview clinicians at surgical centre after Thoracic Surgical MDTs
S – Consensus perception that PFT results higher at surgical centre
A – Process map, retrospective data analysis proposed
PDSA Cycle 2
Figure
Standard of Practice for Surgical Referrals, and Processes Leading to Duplication of PFTs

April - June 2019
P – Quantify variability, identify source and impact on cancer pathway times
D – Retrospective review of surgical patients 2018-2019, interview with PFT lab
S – Significant variability in PFTs, especially % predicted DLCO, outdated llllll reference ranges in use (from 1993)
A – Implementation of recommended reference ranges at local lab
Results
763 patients had lung cancer resection

Trust merger, including two referring centres
IT re-structuring, reduced data availability
Significant differences in the PFT results across a cancer alliance
Has resulted in excessive duplicate PFTs
No impact on time to cancer treatment identified
‘Global Lung Initiative’ is the recommended reference equation

Importance of standardising assessment measures if centralising care
Consider impact on patient experience
12% had duplicate PFTs [n=91]
Median time from PFT at referring trust to surgery 52 days [IQR 37-73]
Table 1: Absolute and Percentage Difference in repat PFTs
PDSA Cycle 3
P – Assess attitudes to requesting repeat PFTs
Figure 2: Variability of % predicted DLCO between referring trusts and surgical centre

August -
September 2019
D – Interview clinicians at surgical centre after Thoracic Surgical MDTs
S – Consensus perception that repeat PFTs still commonly indicated
A – Presentation at surgical centre recommending cessation of duplicate testing; presentation at cancer alliance board recommending regional implementation of recommended reference ranges
Consider impact on trust resource use
Risk of "blind trust" in common tests
Importance of multi-modal surgical assessment processes including objective measures of functional capacity, that do not rely on single measures of reserve such as lung function
PDSA Cycle 4
P – Identify and quantify unnecessary duplicate PFTs
January -
D – Retrospective review of lung cancer resection patients 2022-2023
S – No unnecessary duplicate PFTs; duplicated only if DLCO missing
A – Present lessons learnt loco-regionally, re-assessment in 24 months
Results
142 patients had lung cancer resection
1.4% had duplicate PFTs [n=2]
Median time from PFT at referring trust to surgery 57 days [IQR 45-78] Not significantly different from PDSA Cycle 2
Table 2: Absolute and Percentage Difference in repat PFTs
March 2023 References
1:Home in Time for TeaImprovement in the number of discharges prior to 3pm using Quality Improvement methodology
Dr Anna Winfield , Dr Kate Guthrie- Leeds Teaching Hospital Trust
WHAT’S THE PROBLEM?
Hospitals are facing incredibly high levels of occupancy which creates a discord between the arrival of new admissions and the availability of beds.
When hospitals are operating at full capacity, late afternoon discharges can lead to admission delays and emergency department (ED) overcrowding1
Prolonged ED stays are associated with poor patient outcomes and decreased patient satisfaction2 . Also, a patient’s experience deteriorates if they wait most of the day to be discharged.
Focussing on discharging patients earlier in the day can contribute to greater flow through the hospital and greater patient satisfaction by being home in time for tea.
The Specialist and Internal Medicine (SIM) department was initially focussed on as they care for frail older patients who are at increased risk of harm with prolonged stays in ED and contains two admission wards. SIM were discharging 30% of their patients before 3pm
AIM
Leeds Teaching Hospitals NHS Trust aims to achieve 70% of discharges before 3pm in the next 12months

MEASURES
Outcome Measure: Weekly measurement of % of patients discharged by 3pm
Balance Measures: Monitor average length of stay of patients.
DIAGNOSING THE PROBLEM
Discharging a patient is a complex process which involves multiple professionals as demonstrated by the process map (see Figure 1).
Using the Pareto principle, the highest discharging wards were identified and worked with initially. To gain a greater understanding, a staff survey was conducted to identify perceived barriers to timely discharge. A deep dive into records was conducted to identify avoidable and unavoidable delayed discharges (see Figure 2).
Various team members were also given quality improvement training to help equip them with the skills to trial changes and learn from them. By analysing this data with the ward teams, potential interventions for improvement were identified and attempted (Figure 3).
PDSA CYCLES




Late completion of eMEDs
Pharmacy delay
Awaiting investigation
Transport not released
Follow up confusion
OUTCOME
As a result of multiple interventions, the SIM department achieved a step improvement of 12% for discharges before 3pm (See figure 4). This is the highest median ever achieved by the department and has been maintained despite increased pressures.
LESSONS LEARNT
v Not all changes lead to an improvement but important not to lose focus
v Complex systems require multiple improvement approaches
v Complex problems take time to understand and assess and needs to be individualised for teams
v Timely access to data is crucial
CONCLUSION

Achieving patient discharges earlier in the day is a complex problem which requires a multifocal approach with multidisciplinary professions. The interventions used were based on an in depth look at data and developing an understanding of perceived and actual barriers to timely discharge.
FUTURE PLANS
The process of understanding barriers to timely discharge and enabling staff to develop their own interventions has been spread through different departments throughout the hospital resulting in two step improvements in the number of discharges before 3pm.

OUTCOME- RUN CHART
 Figure 1: Process map of discharge process
Figure 2: Pie chart to represent avoidable causes for discharges after 3pm on a ward
Figure 1: Process map of discharge process
Figure 2: Pie chart to represent avoidable causes for discharges after 3pm on a ward
Improving Weekend Handovers for the On-Call Team
Claire Shadwell1 , Adnan Alnaser1 , Harsha Jayanna1 , Silviou Sabou1 1 Department of Neurosurgery and Spinal Surgery, Salford Care Organisation, Northern Care Alliance NHS Foundation Trust, UK
Background
Weekend ward rounds present a number of challenges to junior doctors. Reduced staffing levels, unfamiliar patients, and competing clinical priorities can influence quality of patient care. Within the tertiary neurosurgical department at Salford Royal Hospital, comprehensive handover documents form an essential tool to ensure safe and efficient ward rounds. This summary of a patient’s notes provides doctors with the salient information required as they are reviewed at the bedside. Unfortunately incomplete documentation is common and may contribute to failings in patient care.
Aims and Methods
Our aims for the project were two-fold:
1) Maximise completion of weekend handover documents
2) Improve the overall quality of handovers through standardising the information included
Plan
• Design a custom tool to allow us to collect both quantitative and qualitative data on the completion rates and quality of handover documents
• Collect our data over a single weekend to give us a snapshot of current practice
• Develop and instigate a change in the same month, then re-audit the data the following month to see if improvements have been made
Do
• Handover documents across the five main neurosurgical and spinal wards were audited across a single weekend
• For each patient on the ward weekend list, a score was allocated for the completion of an up-to-date handover document
• Further scores were given for the inclusion of concise patient summaries, specific weekend plans and key clinical information (weekend bloods, VTE, antibiotic, antiepileptic and steroid status)

Study
• A total of 105 patients were included in the first audit, 85 in the second audit and 95 in the third audit
• The first audit established a baseline – on average 9/10 patients had an up-to-date handover document (88%)
• Overall quality was poor - the average handover scored half marks for details of admission and weekend plan (62% and 50% respectively)
• Around two thirds had correctly mentioned weekend bloods (62%); even fewer had correctly mentioned thromboprohylaxis (VTE), antibiotic, steroid and antiepileptic status (39%, 40%, 18% and 7% respectively)
Act
• We published our findings and raised awareness of the aims of the project through our departmental communications group
• We then promoted the use of a standardised template for writing handovers, which could easily be distributed to all of the ward teams via our electronic patient records system
Results
• Our first intervention lead to improvements in completion rates across almost all wards, however the biggest improvements were seen in the quality of information included, specifically mentioning of key medications
• Unfortunately these positive changes were not sustained on completion of the second cycle, highlighting the underlying issue of inconsistency in handover documentation from month to month
Graph 5: Percentage of handovers mentioning VTE status
Graph 7: Percentage of
Conclusions and Recommendations
• Completion rates of handovers can vary significantly from month to month. These documents are a vital tool for safe continuity of care out of hours, and we should therefore be striving for 100% completion every week. Continuing the project, perhaps with the introduction of a competition element between the different ward teams, may help to promote a culture of consistent handovers.
• The use of a template for handovers helps to both standardise and improve the quality of information included in written handovers, however uptake of this template was variable across the months and further work is needed to consider how we can embed usage of such a template.
Improving compliance to best medical therapy in post-operative carotid endarterectomy patients in Southmead Hospital
 Anthony A, O’Keeffe C, Shorten C, Watson L, Let KS, Beckitt T Department of Vascular Surgery North Bristol Trust
Anthony A, O’Keeffe C, Shorten C, Watson L, Let KS, Beckitt T Department of Vascular Surgery North Bristol Trust

• According to NASCET criteria (1,2), Carotid Endarterectomy (CEA) combined with Best Medical Therapy (BMT) is advised for symptomatic patients with 50-99% carotid stenosis to reduce the risk of major stroke.
• The European Society for Vascular Surgery (ESVS) suggests the implementation of dual antiplatelet therapy (DAPT) before surgery and lifelong use of single antiplatelet therapy (APT) as part of BMT after surgery (3).
• The purpose of this closed -loop audit is to evaluate and enhance our compliance with the use of BMT for patients undergoing CEA at North Bristol Trust (NBT).

Methods
• Fifty CEA patients were identified from the National Vascular Registry at NBT over a ten-month period from January to November 2022.
• Data was compared to NICE and ESVS Guidelines.

• After a first audit, three interventions were introduced, following presentation at the Vascular Clinical Governance Meeting.
• Compliance was reassessed in a second audit.
Results





• 50 patients total

• 100% compliance to BMT on discharge post intervention
• All Patients received statin on discharge
Discussion and Conclusion





Data Collection
Presentation
Our unit has enhanced compliance with the use of best medical therapy (BMT) after carotid endarterectomy through staff education and interventions in existing multi-disciplinary care tools. Moving forward, we aspire to achieve greater consistency among guidelines, which will enable better standardization of antiplatelet therapy for patients undergoing CEA.
1. NICE guideline [NG128] Stroke and transient ischaemic attack in over 16s: diagnosis and initial management https://www.nice.org.uk/guidance/ng128/chapter/Recommendations
2. North American Symptomatic Carotid Endarterectomy Trial Collaborators Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J med. 1991;325(7):445–453. doi: 10.1056/NEJM199108153250701.
3. Management of Atherosclerotic Carotid and Vertebral Artery Disease: 2017 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS) https://doi.org /10.1016/j.ejvs.2017.06.021
BEAT HF QiK Bringing Early Attention To Heart Failure
G. Bell, L. Smith, L. Moran, G. Bell, V. Cain, E Wiper, A Seed
Introduction
In 2019/20 , 5,322 people had been identified by NHS Blackpool and Fylde & Wyre (BF&W) Clinical Commissioning Group (CCG) practices as living with Heart Failure (HF).1 This equates to 1.5% of the BF&W’s total population compared with the National Average of 0.9%. Prevalence is in fact understood to be significantly higher than that recorded. Evidence for under reporting includes the fact that as many as 20% of patients identified as having HF during an admission were not registered with their GP. A patient that is not recognised as having HF by their GP practice is less likely to benefit from optimised care, surveillance and the support of specialist teams benefitting from

Initial Assessment
A review of national data highlighted that:
• 80% of patients with HF are not identified until the point of non-elective admission
• 40% of those patients having reported symptoms to their GP in the 5 years prior
• 90% having seen a clinician in Primary Care within the previous 12 months
A review of local data from the Trust highlighted that:
• In 2019/20, there were 740 emergency hospital admissions with HF
• Patients admitted had an average length of stay of 12 days
• In 2019/20, at any one time, 25 beds were occupied by a patient with decompensated HF
• In 2020/21 that had risen to 35 beds
Once a patient from BF&W is registered with the HF Team, the care they receive is associated with a lower admission rate than most CCGs in the country (6th & 10th of 106). With these figures in mind, it was suggested that earlier, elective, diagnosis would greatly improve patient care, reduce admission rate and burden on beds at a time of significant pressure.
The project team decided that every heart failure admission, without prior escalation to the HF team via an elective or non urgent route, should be viewed as a potential patient harm. A missed opportunity.

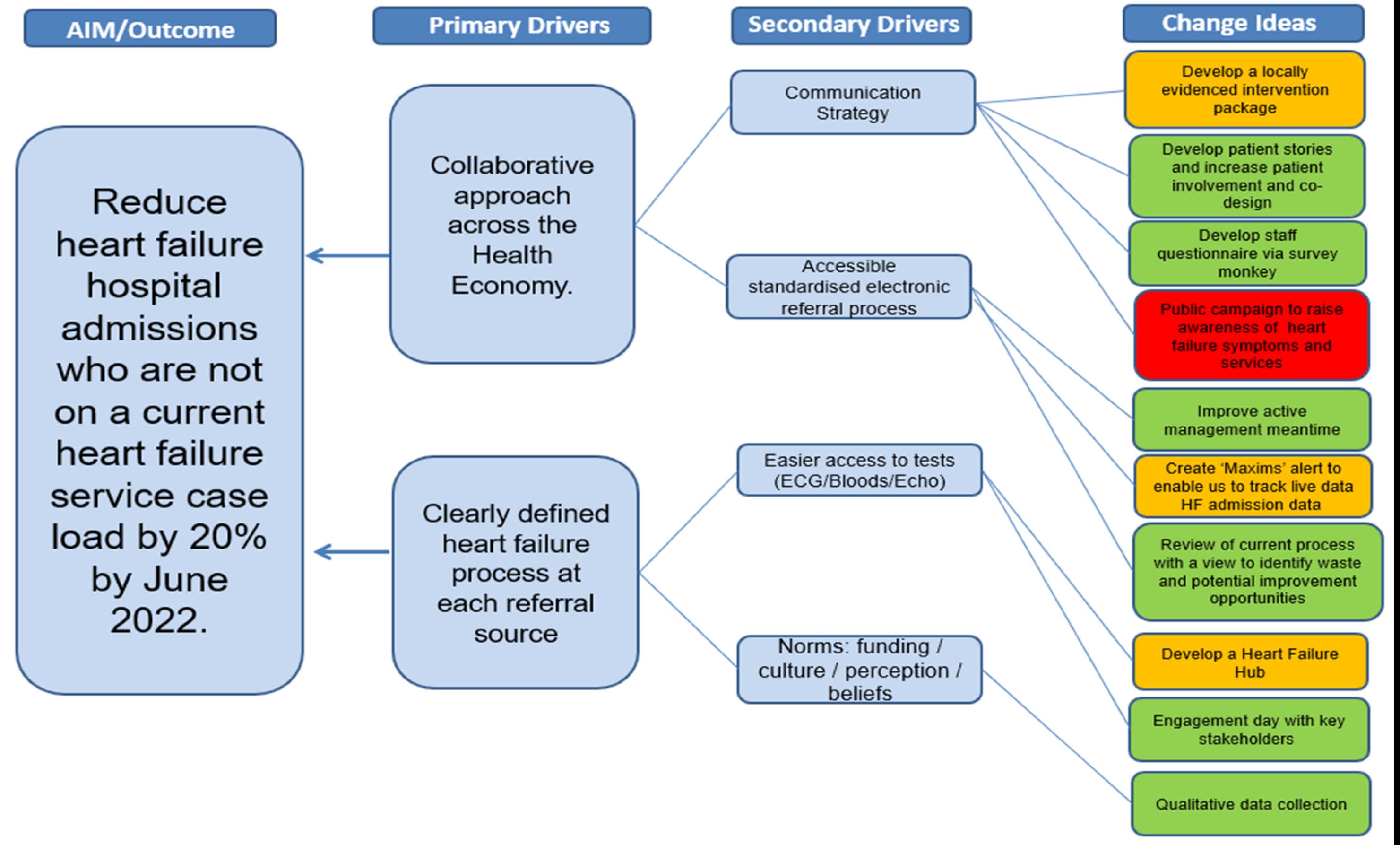
Aim & Driver Diagram
What matters to you
Throughout the project patient views & experiences were considered. Patient survey results indicated that:
• 50% visited their GP about HF on multiple occasions
• 50% reported that their GP had not discussed their referral to the HF team 75% reported symptoms for up to 3 months prior to seeking support from GP
• 75% reported staying alive as what mattered to them
• We will continue to ask patients: ‘What matters to you?’
Method
Baseline data in relation to our aim reported that in the six months prior to the project initiation, 65% of patients facing non elective admission had not been referred to the HF team more electively, they were not on the active caseload of the HF team.

A change idea was agreed; to have this data reported live informing the HF team of the impact of their interventions. A new Maxims tool that allowed ‘tagging’ of HF patients according to their HF service status, would facilitate live data reporting to our aim and also support a future ‘virtual ward’ vision. Due to the need for IT development this data was to be reported as live run chart by August 2022
Analyses of the available data, adjusted for population size, helped to confirm that some practices had high numbers of elective referral and/ or non-elective admission.
With the help of funnel plots, a common not special cause for the issue was agreed and the need to focus on process and system barriers to improvement highlighted.
Various tools were used including: process maps, the ‘last 10 patient’ tool, qualitative interviews & surveys with service users and colleagues. Pareto analysis was used at different stages, E.g. to identify key stakeholders to work with, such as high frequency referrer GP practices.


Results & Lessons Learned
Data reports an encouraging increase in diagnostic referral via elective routes (figure 1)
The increase may be associated with a plateau and then fall in the post-covid admission rates 3 months thereafter (figure 2), sustained increase in admission rate is reported in other centres (admission rate acting as proxy measure pending live data reporting to our aim)
• The HF team are monitoring balancing measures and find areas of concern;
• Data has shown an increase in ‘elective’ referrals to Community team - an elective admission avoided means additional pressure on community teams with an increase in ‘urgent’ referrals
• The hospital team are referring fewer hospital discharges to the Community team due to the increase in waiting times – they are therefore carrying the burden of an increased OP caseload and less able to deliver specialist care to inpatients.

• LOS is reduced (figure 3) a recognised marker of less specialist supervision of inpatient care
• Increased SHMI/ HSMR, an increase in mortality associated with admission has caused serious concern, we have since refocused the in-hospital service and seen a recovery. However, it is noted that the data may also reflect a change in patient cohort as a result of the less critically unwell patients more often avoiding admission

Learning so far has included:

• Electronic systems can be used more effectively to help with improvement projects ; evidencing impact and maintaining improvements
• Implementing an e- triage process for HFDC referrals can provide more efficient care for patients; ACP clinical time (155 min/week) and administrative time (107 min/week) saved, protecting time for patient care. (figure 4)

• Efficient triage encourages timely feedback to referrer encouraging appropriate referral practices E-processing uses less paper and saves money
Next steps
As the current service is not adequately resourced to manage an electively referred high risk population alongside the demands of the non elective population, such ambitious service improvements may need to be delivered at a pace that protects those already dependent on our service
Continuous data monitoring, ideally sighted by service users (referrers) and Trust leadership, is essential to help maintain service improvements and ensure further progress with organisational support
• The HF team will continue to work with the Trust’s Directorate, Division and Exec team to invest in our communitybased service in line with NHSE priorities or accept a significant increase in admissions, readmissions and mortality risk for our patients (business case with options appraisal)
• Gain business intelligence support for a HF service dashboard
Deliver 1⁰ care network workshops
• Relaunch twitter account and develop comms strategy
• Use a ‘planned experimentation’ approach to care for HF patients at highest risk of admission
