PG. 10 Maintaining Normalcy Through Cancer
Go after the life you want.
We are entrepreneurs, doctors, veterinarians and writers for page, stage and screen. We’re business leaders, educators and performers. We’re scientists, nurses and fashion leaders. We’re mold breakers and trend makers.
We are a small yet mighty community that nurtures and supports the potential in everyone who calls Stephens home.
Learn more at stephens.edu

Emily
Tveitnes,
Please submit comments or feedback to erin.wegner@boone.health or call 573.815.3217

1600 East Broadway Columbia, MO 65201 573.815.8000




For a FREE subscription, call 573.815.3392 or visit boone.health/my-boonehealth and click on the subscription link on the right side of the page.




Check us out on Facebook, Twitter, Instagram, Pinterest and YouTube. Follow us Table of Contents 10 12 2616 MANAGING EDITOR Erin Wegner Marketing & Communications Consultant I COPY EDITOR Jessica Park Communications Consultant II CONTRIBUTING WRITER Madison Loethen Digital Communications & Marketing Consultant II ADDITIONAL CONTRIBUTING WRITERS
Nusbaum, Lucy Shaffer, Jennifer
Hannah Williams, Jenny Workman 5 A Note from Troy 6 Hospital Headlines 10 Maintaining Normalcy Through Cancer 12 Better Sleep for Better Health 14 Hospice Supporting Families 16 Community Wellness 18 Screening Colonoscopy 20 Heart Healthy Soup 22 Breastfeeding a Newborn 24 Get to Know a BHC Doctor 25 Get to Know a BHC Nurse 26 Fueling Our Bodies 28 All Shook Up 30 Foundation News




Boone Health Status Report

“How are things at Boone?”
Whenever I’m asked this question, I pause. It’s not because this is a question that I don’t want to answer – Boone Health is an accountable organization, and we owe our community a clear picture of challenges as well as successes. It’s a question that requires more than a sentence to answer.

First, 2022 has been an exciting year for Boone Health. In our second year as an independent healthcare organization, we’ve opened new clinics, including Boone Health Plastic Surgery, and walk-in lab test collection sites in Centralia and Osage Beach. Boone Health Medical Group now includes over 100 primary care and specialty medical providers throughout mid-Missouri.
Through this time of growth and change, providing quality patient care has remained our top priority. I am proud of the incredible work that Boone employees and providers have done to retain our ranking as the #1 hospital in central Missouri by U.S. News and World Report for the eighth year in a row!
Like many hospitals across the nation, Boone Health has faced the challenges of the COVID-19 pandemic including labor and supply shortages. These effects don’t only impact healthcare – your favorite restaurant may have changed their hours or temporarily closed their dining room. You may have seen empty shelves at your favorite supermarket. You’ve likely paid more for products and services as prices are raised to stay on top of rising supply costs.
But hospitals can’t use similar approaches to respond to shortages. We can’t close our ICUs on Mondays. We can’t let our supply shelves in the Emergency Department go empty. And we can’t raise our prices to reflect increased expenses.
As a mission-driven organization, our priority in 2020 and 2021 was to protect and care for our community. When a hospital experiences surges of severely ill patients who need our help, stopping to analyze the costs of supplies, medicines, or personal protective equipment becomes less important than fulfilling our mission. As the clinical aspect of the pandemic winds down, we can now refocus our efforts on long-term sustainability.
Even with nationwide challenges, we are responsible for Boone Health’s success. We’ve developed and launched a comprehensive plan to achieve the financial performance required for a health system with our high standards. Over the last 3 months, we have seen a significant reduction in our
supply and agency staffing costs, thanks to our committed focus on recruiting new Boone Health employees, diligent negotiations with our suppliers, and innovative approaches to staffing and supply chains. These improvements reflect our staff’s commitment to ensuring that Boone Health continues to improve the health of the communities and people we serve.
Boone Health also remains strong because of your commitment. People don’t just say “I believe in Boone” – they live it. It’s why people continue to choose us to care for them and their families. It’s reflected in the compliments we get from patients and visitors about the care and compassion they experienced. It’s exemplified by our Employee and Leader of the Year and our employees’ years – sometimes decades – of committed service.
Another way individuals and organizations in our service area demonstrate their belief is through their support for the Boone Hospital Foundation. The Foundation funds programs at Boone which enhance patient care and promote community wellness, including specialized training and free health screenings. To learn more about how the Foundation makes Boone an even better place to work and to receive healthcare and how you can help, see page 30 in this issue of My Boone Health.
Thank you for believing in Boone!
Troy Greer CEO, Boone Hospital Center

A NOTE FROM TROY
Ed Clayton Joins Boone Health as CFO

Boone Health is proud to announce Edward J. Clayton, CPA, MBA as our next Chief Financial Officer.
Ed most recently served as the President and CEO of Phelps Health in Rolla, Mo., where he had previously served as Phelps Health Chief Operating Officer and Chief Financial Officer. Ed received his Bachelor of Science in Accounting at Southern Illinois University and his Master’s in Business Administration from Webster University in Rolla.
“My family and I are thrilled to join the Columbia community and experience all it has to offer,” says Ed. “For me personally, I couldn’t be more excited to be part of the Boone Health family, working with great colleagues to improve the health of people in mid-Missouri. I can’t wait to get started!”
Ed will be joined in Columbia by his wife Sharon and their four children – Tyler, 15; Logan, 12; Ashlynn, 9; and Kylie, 5.
Boone Health Osage Beach Opens with Lab Draw Clinic
On Wednesday, June 29, Boone Health cut the ribbon on both the remodeled Boone Health Primary Care clinic and a brand-new Lab Draw clinic in Osage Beach.

The 288-square foot lab has all new equipment and will be open to all patients, from Monday through Friday, 7 AM to 5 PM, with no appointments necessary.
Boone Health Announces New CNO
Boone Health is proud to announce Shannon Kuczynski, MSN-A, MHSA, RN, NE-BC as our next Chief Nursing Officer.

Shannon grew up in Columbia, attending David. H. Hickman High School before earning her degrees at the University of Kansas – Kansas City.
Shannon brings 28-years of nursing experience, 25 in leadership, having most recently served as Division Vice President, Service Lines and Divison Chief Nursing Informatics Officer for Hospital Corporation of America (HCA) in Overland Park, Kansas. While there, Shannon specialized in workflow optimization and transforming data into usable knowledge.
“I am excited to come back to Columbia and join a health system that is known for excellence in nursing,” says Shannon. “I look forward to getting to know the team and making a positive impact on our employees and patients.”
Shannon and her husband Gary have three children – Dash, 21; Jett, 18; and Thaddeus, 16. Shannon’s first day at Boone will be October 10.
6 BOONE HEALTH Fall 2022 HOSPITAL HEADLINES
Boone Health Trustee Jan Beckett Honored For Civic Leadership
Boone Health Trustee Jan Beckett was selected as Woman of The Year – Civic Leader by Greater Missouri Leadership Foundation.

As written by Greater Missouri: Through her years of community service and more than 50 years of involvement with healthcare, she has built meaningful relationships, fostered collaboration, she gives back freely and with commitment, all the while being an enthusiastic celebrant. She took the 2013 GMLC Challenge to heart and enriches the lives of women helping them broaden their perspectives which ultimately helps solve some of the critical issues facing our community and state.
Jan was a founding member and President of the Board of the Assistance League of Mid-Missouri; was a founding board member of the Vincent P. Gurucharri Foundation (providing aid to families of cancer patients); founder and continued supporter of the Columbia Public Schools Foundation; member of the Columbia Metro Rotary club and participates in their charitable activities including weekly readings to pre-school children at the Columbia Public Schools Early Childhood Learning Center; member and former Board Member of the Columbia Chamber of Commerce and past chair of the Ambassador program.
Jan has served on the Boone Hospital Board of Trustees since 2011 and is the current Secretary of the Board working tirelessly to keep high quality health care available to all citizens of the region. She is providing important leadership as they have gone through a monumental governance transition. Jan has never wavered and continually puts in whatever effort it takes to make this transition a success for future generations.
Boone Health Receives 5 AHA Achievement Awards
Boone Health has received five American Heart Association Get With The Guidelines and Mission: Lifeline achievement awards demonstrating commitment to following up-to-date research-based guidelines for the treatment of heart disease and stroke, ultimately leading to more lives saved, shorter recovery times and fewer re-admissions to the hospital.
Every 40 seconds, someone in the U.S. has a stroke or heart attack, and heart disease and stroke are the No. 1 and No. 5 causes of death in the United States, respectively. Studies show patients can recover better when providers consistently follow treatment guidelines.
Get With The Guidelines and Mission: Lifeline put the expertise of the American Heart Association and American Stroke Association to work for hospitals nationwide, helping ensure patient care is aligned with the latest evidence- and research-based guidelines. As a participant in both Mission: Lifeline and Get With The Guidelines programs, Boone Health qualified for the award by demonstrating how their organization has committed to improving quality care.
This year, Boone Health received the following achievement awards:
• Get With The Guidelines® - Stroke GOLD PLUS with Target: Stroke
• Get With The Guidelines® - Honor Roll and Target: Type 2 Diabetes Honor Roll

• Get With The Guidelines® - Heart Failure BRONZE
• Mission Lifeline® - STEMI Receiving Center – GOLD PLUS
• Mission Lifeline® - NSTEMI – GOLD



Boone.Health/My-Boone-Health 7
STEMI RECEIVING GOLD PLUS 2022 Mission: Li f e l ine®
Boone Health Celebrates New Plastic Surgery Clinic

Boone Health is proud to announce the opening of its Boone Health Plastic Surgery clinic.
The clinic is led by Giorgio Allegra, MD. Dr. Allegra joined Boone Health this spring. He is board certified in General and Plastic Surgery and is a member of the American Society of Plastic Surgeons. Dr. Allegra has practiced in Atlanta, Chicago, Dallas, New York, Dubai and Milan - bringing over 27 years of experience to mid-Missouri.
Also providing services is Family Nurse Practitioner Tiffany Carmichael, FNP-C. Before joining Boone Health Plastic Surgery, Tiffany worked at the Boone Health High Risk Breast Clinic.
Services provided by Dr. Allegra and Tiffany at Boone Health Plastic Surgery include breast reconstruction and augmentation, face lifts, body lifts, tummy tucks, body contouring, liposuction and fat augmentation.
Boone Hospital Center Ranked No. 1 Hospital In Mid-Missouri for Eighth Year In A Row

For the eighth year in a row, Boone Hospital Center was ranked the #1 hospital in mid-Missouri by U.S. News & World Report. It was ranked the #6 hospital in the state.
U.S. News & World Report also rated Boone Hospital Center “High Performing” in abdominal aortic aneurysm repair, aortic valve surgery, chronic obstructive pulmonary disease (COPD), colon cancer surgery, heart attack, heart bypass surgery, heart failure, hip fracture, hip replacement, kidney failure, and stroke.
The annual Best Hospitals rankings and ratings are designed to assist patients and their doctors in making informed
decisions about where to receive quality care for challenging health conditions or elective procedures.
For the 2022-2023 rankings and ratings, U.S. News evaluated more than 4,500 hospitals across 15 specialties and 20 procedures and conditions. In the 15 specialties, 164 hospitals were ranked in at least one specialty. State and metro area rankings reflect the highest performing hospitals in the area across multiple areas of care.
“The hospitals named to the U.S. News Honor Roll excel across numerous specialties and service lines,” said Ben Harder, chief of health analysis and managing editor at U.S. News. “When
The new clinic is 2,477 square feet and has a spa-like feeling. It has 3 exam rooms, 1 procedure room and 1 recovery room.
Boone Health Plastic Surgery is located at Broadway Medical Plaza 1, Suite 260. To schedule an appointment, call 573.815.5310.
patients and their medical professionals are considering their options for care, the rankings are designed to help them identify hospitals that are superior in the kind of care they may need.”
U.S. News evaluated each hospital’s performance using a variety of measures such as survival rates, complication rates, patient experience and level of nursing care. The Best Hospitals methodology factors in data from the Centers for Medicare & Medicaid Services, American Hospital Association, professional organizations and medical specialists.
8 BOONE HEALTH Fall 2022
Boone Health 2021 Employee & Leader of the Year
2021 Employee of the Year
Jordan Parks
Histotechnician, Laboratory Services
“I’m not sure there is a word that describes how helpful Jordan is,” wrote one of Jordan’s colleagues. Jordan was recognized for going the extra mile for Boone Health coworkers, physicians, and patients in ensuring timely and accurate laboratory test results. He has a reputation for his positive attitude, excellent communication skills, and kindness towards everyone.

2021 Leader of the Year
Kyndal Riffi e
Group Administrator, Boone Health Medical Group
Known throughout Boone Health as a team player and problem-solver, Kyndal was recognized for her commitment to her sta , professionalism, and willingness to step up when help is needed. In 2021, she played an instrumental role in setting up COVID vaccination clinics for employees and community members while simultaneously taking on an expanded role with Boone Health Medical Group’s specialty clinics.

Boone.Health/My-Boone-Health 9 HOSPITAL HEADLINES
Maintaining Normalcy
THROUGH CANCER
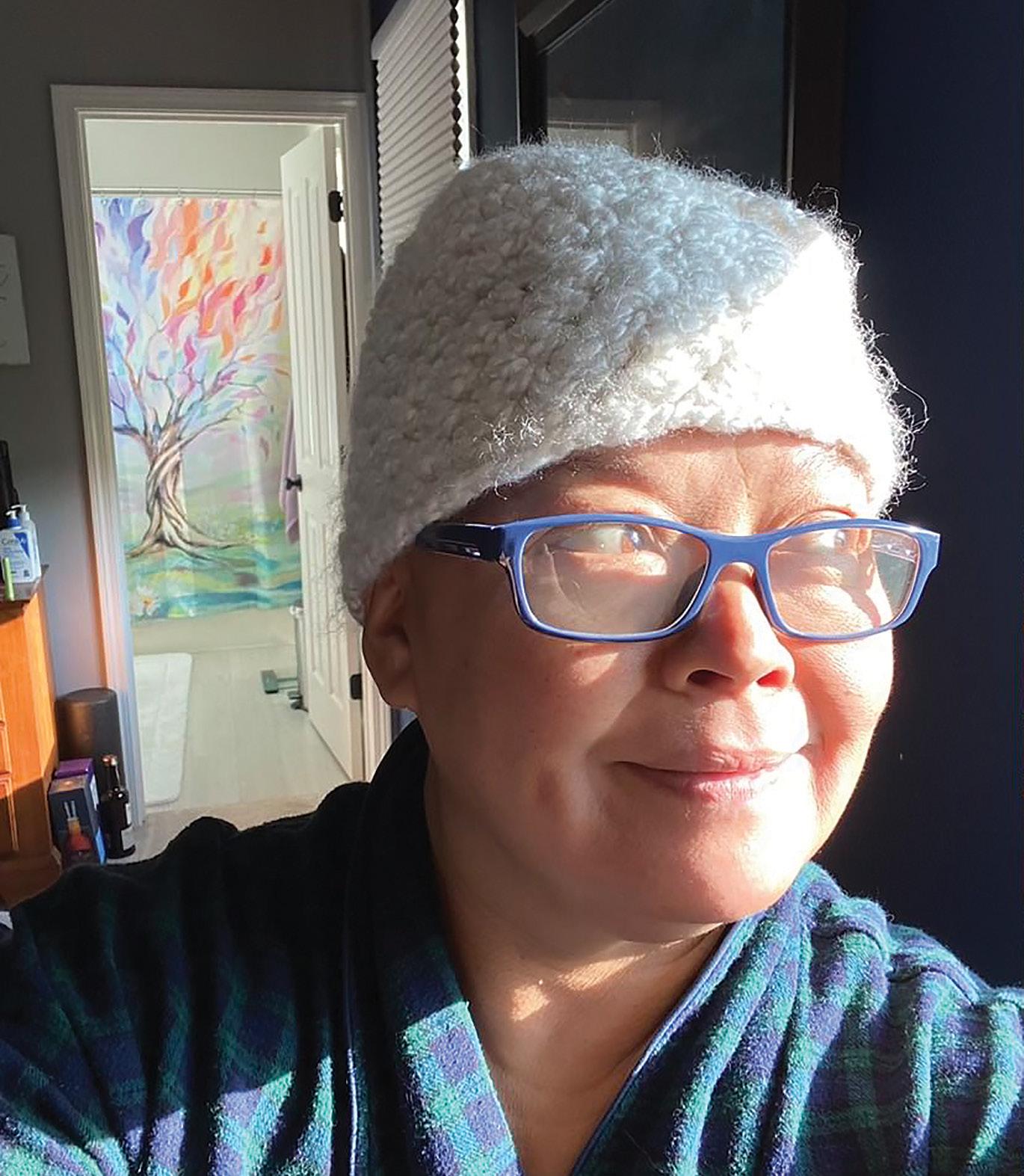
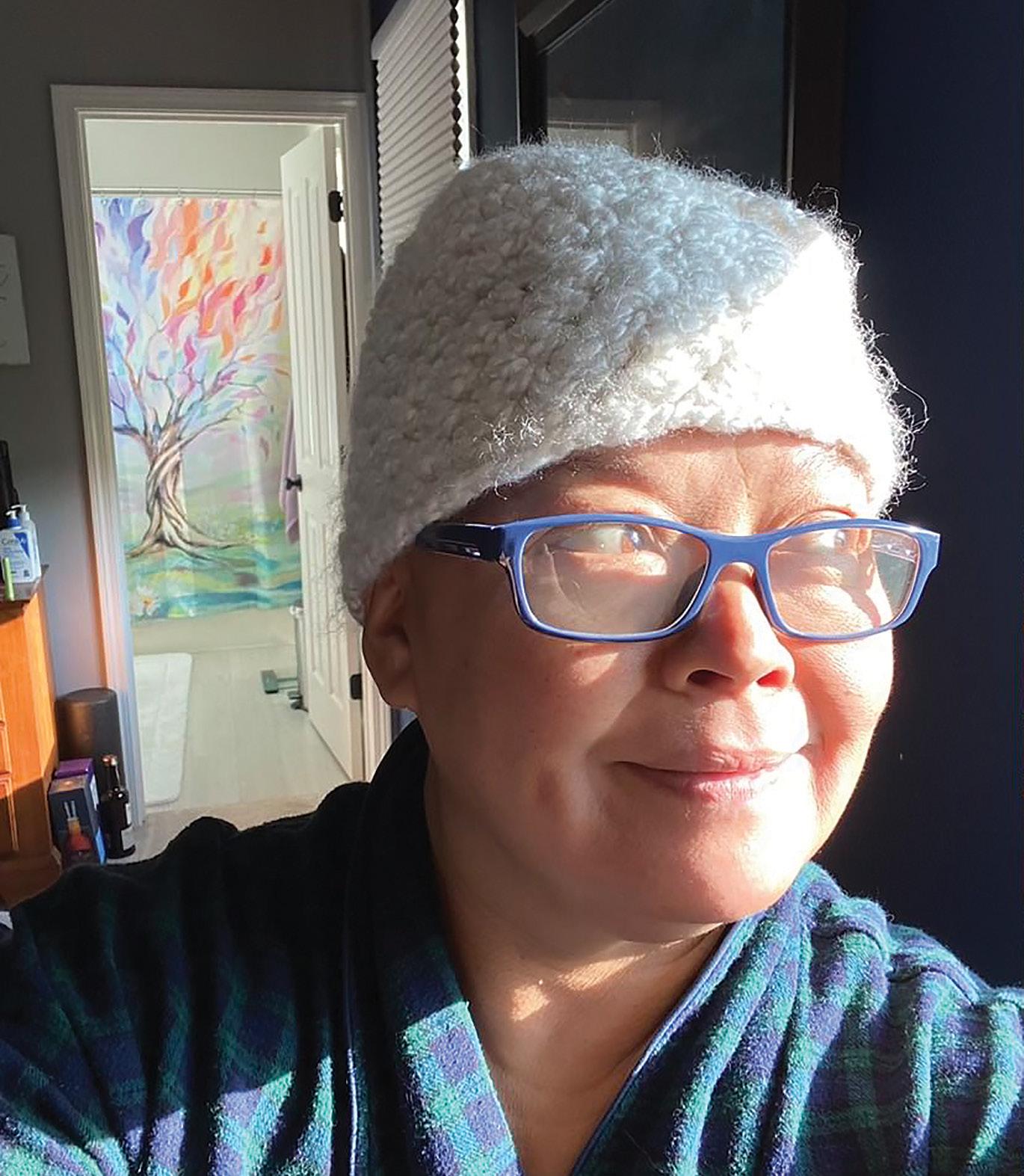
A Columbia mom’s breast cancer journey.
49 -year-old married mother of two Nancy Gillig remembers getting the call that changed her life. She had just undergone a routine mammogram at Boone Health’s Harris Breast Center when an abnormality was found. That led to her getting an ultrasound and then a biopsy.
“I got the call, and they told me I had cancer. They then started talking about next steps. It all felt surreal, but I knew I was going to do what I had to do to keep moving forward,” says Nancy.

A couple days later both Nancy and her husband Brian found out they had Covid.
“We really weren’t that sick from Covid because we had our vaccines, so we spent our isolation making appointments and getting ready for the journey that was to come,” says Nancy.
Nancy and Brian reached out to several friends of theirs who had been going through their own cancer journey.
“So many people supported us through gifts, prayers, and kind words, but Brian was my number 1,” says Nancy.
Nancy was set up with Mark Tungesvik, MD at Missouri Cancer Associates (MCA) as her oncologist. He didn’t want to wait to meet, so their first appointment was via Zoom since she was still selfisolating.
“Nancy had a great attitude from the very beginning. She was very brave at the time of diagnosis as well as throughout treatment. Nancy is an inspiration to us all and we are grateful to have her within our MCA family,” says Dr. Tungesvik.
During the zoom appointment, they discussed her diagnosis and treatment plan. Nancy found out she had early-stage invasive breast cancer.
Nancy Gillig
10 BOONE HEALTH Fall 2022
“We developed Nancy’s treatment program based on her staging as well as markers that help us predict the need for chemotherapy. Since Nancy had positive lymph nodes at time of diagnosis as well as positive estrogen receptors and a negative HER2/neu status, she did qualify for an aggressive chemotherapy regimen prior to resection surgery,” says Dr. Tungesvik.
Nancy began chemotherapy right away.
“I made some friends in that chemo room at MCA. All the other patients and the staff were awesome,” says Nancy.
When she began losing her hair from the chemo, she had Brian shave her head.
“We were hanging out in our basement with our boys, and I had him get out the trimmer. We actually had some fun with it. We did a few different hairstyles and of course did a mohawk,” says Nancy.
Nancy was also given a wig from MCA which she found comforting to wear.
“That wig was great! It was so nice of them to provide that,” says Nancy.
Nancy says her main symptoms from the chemo were fatigue, nail reactions, and neuropathy. Neuropathy is a dysfunction of nerves that causes numbness, tingling, or pain. Nancy experienced the neuropathy mainly in her fingers. She was given a comfortable chair from Healing Chair of Columbia which helped her cope with her symptoms.
“That chair was the best!” says Nancy.
Nancy did 16 rounds of chemo. When the chemo was complete, the next step was a double mastectomy followed by radiation.
“I choose the double mastectomy because the odds were better, and it would completely get rid of the cancer,” says Nancy.
Her surgeons were General Surgeon Anne Petersen, MD and Plastic Surgeon Giorgio Allegra, MD.
“Nancy was the perfect candidate for this operation. She asked lots of questions about the surgical choices, and we had several discussions about the options for surgery as well as what her expectations should be for the recovery process,” says Dr. Petersen.

Nancy says she felt very confident after meeting with her doctors.
“Dr. Petersen was so kind and knowledgeable. I felt very comfortable with her doing the double mastectomy. Dr. Allegra was very likable and has lots of experience. It made me feel very confident going into surgery,” says Nancy.
Nancy’s surgery went well and both her breasts along with 7 lymph nodes were removed, 2 of which were cancer positive.
Dr. Allegra placed expanders that will allow for the placement of implants once her radiation is complete.
“I remember being in Dr. Allegra’s office and looking in the mirror thinking, wow I look good! Which is crazy because I had just had surgery,” says Nancy.
Dr. Allegra joined Boone Health in the spring of 2022 and opened Boone Plastic Surgery. He does both cosmetic and reconstructive surgeries.
“Nothing can be accomplished without the good synergy between all specialists of the interdisciplinary breast unit at Boone. Dedication, expertise and passion are all present with this group. Our new Boone Plastic Surgery service gave its humble contribution to yet another Boone Hospital Center of Excellence experience,” says Dr. Allegra.
Nancy completed her radiation and will have her surgery to replace the expanders with implants later this year.
“My focus has always been on maintaining normalcy where I can. That is so important when you are going through a journey like this. For me that means staying active, gardening, spending time with my family and friends,” says Nancy. By Madison Loethen
Nancy with her family on her last day of radiation
Boone.Health/My-Boone-Health 11
To learn more about Boone Plastic Surgery, visit boone.health/plasticsurgery or call 573.815.5310

Better Sleep for Better Health
 By Dr. Graham A. Colditz, Siteman Cancer Center
By Dr. Graham A. Colditz, Siteman Cancer Center

We may not think about sleeping as a healthy behavior like we would exercising or eating a healthy diet, but we probably should.
Sleep can play a key role in health and wellness, and studies show that many of us just aren’t getting enough of it.
“Short sleep and poor-quality sleep are linked to increased risk of depression, obesity, diabetes, hypertension, heart disease and some cancers,” said Yikyung Park, associate professor in the Division of Public Health Sciences at Washington University School of Medicine in St. Louis. “A lack of sleep also weakens immune function, making you vulnerable to common infections such as the common cold.”
How can sleep problems have such a wide-ranging effect on health?
For one, they can disrupt the circadian rhythm, our natural “body clock” that controls all biological functions in a 24hour period, Park said. That disruption can lead to many different reactions in the body that can increase the risk of certain diseases and conditions.
Less directly, sleep problems can also simply make it harder for us to make choices that are good for our health. Lack of sleep can impact decision-making, energy levels and a number of other factors that can make us more likely to stay on the couch rather than get outside for a walk, or choose a fast food meal over making something healthier at home.
About a third of U.S. adults are short sleepers, getting fewer than seven hours of sleep a night. But it’s an issue more
common in some groups than others. “There is a significant disparity in sleep duration by race and ethnicity, and income,” Park said. “Short sleep is a particularly important problem for African Americans, multiracial non-Hispanics, American Indians/Alaska Natives and Native Hawaiians/Pacific Islanders – as well as those with lower incomes.” A range of issues can contribute to these differences, including stress, discrimination, job schedules and neighborhood conditions that can make it harder to get good quality sleep.
It’s recommended that most adults get about seven to eight hours of sleep each day. But what counts as healthy amounts of sleep can vary.
“For some people, six hours of sleep a day is enough, but others may need nine hours. And although it’s important to get enough sleep, sleep quality is also crucial,” Park said.
While some of the factors that impact the quality and length of sleep are out of our direct control, there are simple approaches we can take to improve the chances of getting good sleep regularly. As a first step, Park recommends we:
• Put away electronic devices such as smartphones, tablets and TVs at least 30 minutes before bed
• Have a routine sleep schedule – that is, go to bed and wake up at the same time – every day
• Avoid large meals within a couple hours of bedtime
• Avoid caffeinated beverages and alcoholic drinks before bed
• Get regular physical activity, though not close to bed time
In our busy, round-the-clock world, these changes can be an adjustment. But you don’t need to tackle them all at once. Pick just one to start, and then go from there. Small changes build on each other. And like other healthy behaviors, improving the quality of sleep is something well worth the effort and can provide a real boost to health and well-being.
And that may just help you rest a bit easier.
It’s your health. Take control.
Dr. Graham A. Colditz, associate director of prevention and control at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, is an internationally recognized leader in cancer prevention and the creator of YourDiseaseRisk.com, a free, personalized tool for helping people reduce the risk of cancer and other chronic diseases. An epidemiologist and public health expert, he has a long-standing interest in the preventable causes of disease. Colditz has a medical degree from The University of Queensland and a master’s and doctoral degrees in public health from Harvard University’s T.H. Chan School of Public Health.
Boone.Health/My-Boone-Health 13
HOSPICE FAMILIES Supporting
Boone Health Hospice supported the Cox family through end of life care.
Nothing can truly prepare you for the loss of a loved one, but the Cox family will tell you the Boone Health Home Care & Hospice team offered the support they needed during that difficult time.
85-year-old Connie Cox was diagnosed with a Glioblastoma in April 2021 and given a 6-month life expectancy. The Cox family was heartbroken and gathered around Connie to support her.
Connie underwent surgery, radiation and chemotherapy in hopes of adding time to her life, but she and her family ultimately decided to cease treatment and focus on her comfort. That is when the family was first introduced to Boone Health Hospice services.
 The Cox family. From left to right: Mark, Melanie, Jerry, Connie and Marty
The Cox family. From left to right: Mark, Melanie, Jerry, Connie and Marty
14 BOONE HEALTH Fall 2022
“Jacqueline came out and spoke with us, and we were so impressed. We talked about mom’s end of life goals, and she helped us process what was going on,” says Connie’s son Mark Cox.
Jacqueline also explained to the family all that the Hospice team would be doing to assist them. The team is composed of nurses, social workers, chaplains, aids, and volunteers all working together.
“Decisions at end of life can be difficult and Hospice is there to guide patients and families, drawing upon years of hospice experience,” says Boone Home Care & Hospice Clinical Manager Jacqueline Fernald, RN.
Boone Hospice is also able to provide specialized equipment such as hospital beds, bedside commodes, wheelchairs and personal care supplies to the patients at no additional cost.
“Our mom was a very strong woman, but she was willing to accept the care and help from the hospice team. My mom loved her whole support team - Melissa, Jacque, Dee, Destiny, Elizabeth, and Ken,” says Mark.
After 4 months of Connie being cared for at home, the Cox family and hospice team felt it was time to move Connie into a care facility.
“We were so comforted that Boone Hospice would still be with us even after she was moved,” says Mark.
Boone Hospice is able to assist when patients are moved to a care facility by advocating for the patient and family, addressing personal care and comfort, and offering bereavement support.
“We all know that patients and families worry when having to consider moving from their home to a care facility. It is a very difficult decision, so Hospice is there to ease the process,” says Jacqueline.
When Connie’s time came, Boone Hospice was with the Cox family for support.

“They walked us through everything. They encouraged us to keep talking to her and touch her saying she could still hear and feel us. They handled everything with such love and care,” says Mark.
When Connie passed, her Boone Hospice aide Melissa prepared her for the funeral home.

Boone Hospice is continuing to provide care to the Cox family through its bereavement program. Hospice continues to provide bereavement services for 12 months following the patient’s death.
“They still call and check on us and offer support. They’ll pray with us. They’re such a wonderful group of people,” says Mark.
The Cox family was so touched by the program that they gave a generous donation to the Boone Hospital Foundation so that the program could continue to help other families.
“The hospice team offered wonderful support, both medically and emotionally to my mother. They preserved her dignity, and we will always be grateful,” says Mark. By Madison Loethen
To donate to the Foundation, visit boone.health/foundation or call 573.815.2800
 Connie and Jerry on their 66th Anniversary on July 31, 2021.
Connie at a St. Louis Cardinals baseball game in 2020.
Connie and Jerry on their 66th Anniversary on July 31, 2021.
Connie at a St. Louis Cardinals baseball game in 2020.
Boone.Health/My-Boone-Health 15
To learn more about Home Care and Hospice, visit boone.health/home-care-and-hospice or call 573.815.0555
 Jenny L. Workman, Community Wellness Manager & Charles Kitchen, Mobile Health Unit driver.
Jenny L. Workman, Community Wellness Manager & Charles Kitchen, Mobile Health Unit driver.
Introducing Boone Health COMMUNITY WELLNESS
Boone Health Community Wellness is our outreach program which supports health and wellness programs and screenings for mid-Missouri companies, communities in our service area, and Boone Health employees.

In the 2000s, Boone Hospital Center established a community outreach program called WELLAWARE that provided community health screenings, health fairs, and wellness challenges for staff, and corporate and community partners. The COVID-19 pandemic had put a stop to our community outreach as we focused our efforts on prevention and vaccination, but it also gave us the opportunity, particularly during our transition to an independent health care organization, to revisit our purpose and programs and start with a new name and mission as Community Wellness.
Community Wellness provides programs similar to WELLAWARE, but with a new emphasis on promoting overall well-being and wellness. We help people find overall wellness by promoting 8 dimension of wellness: physical, intellectual, emotional, social, spiritual, vocational, financial, and environmental.

We’ve also adjusted our goal to provide education and resources to fit the needs of our population. For example, we encourage people to find a medical home with a primary care provider. A medical home is associated with improved health outcomes including fewer emergency
room visits, hospitalizations, and delaying or going without care. Having a medical home leads to more preventative care, including yearly wellness exams and other recommended preventive care.
Community Wellness continues to work with our corporate partners in midMissouri to provide wellness screenings, programs and initiatives tailored to their employees’ specific needs.
Wellness programs benefit employees, their organizations, and communities. Wellness programs can reduce absenteeism in the workplace because employees who work at companies invested in their well-being are less likely to get sick, overwhelmed, or feel unappreciated. They are also better equipped to handle stress at work and are less likely to call in sick.
A strong wellness program also helps employees feel cared about and seen. If people know their employer is invested in helping them achieve personal and health goals, they are more likely to be personally invested in helping their organization be successful.
Our Community Wellness team includes program manager Jenny L. Workman; program coordinator Lisa Todd; Mobile Health Unit driver Charles Kitchen; and a team of part-time nurses: nurse coordinator Brenda Wilson; Lucy Shaffer, Elaine Samuel, Sharilyn Reedy, Cheryl Currie and Phyliss Golden. We also collaborate with registered nurses, exercise
physiologists, and clinicians from various Boone Health departments for community and corporate screenings, flu vaccines, and wellness programs and education.
Partnerships with various community organizations, including health departments, allows us to provide resources and education to community members. The Mobile Health Unit, funded by Boone Hospital Foundation, helps Community Wellness bring our wide array of wellness services to communities throughout our 26-county service area. By Jenny L. Workman, Community Wellness Manager
For more information on Community Wellness, including upcoming screenings and corporate programs, please visit
Boone.Health/My-Boone-Health 17
WHAT YOU NEED TO KNOW ABOUT
Screening for Colorectal Cancer
The age for a colonoscopy screening was previously recommended to happen when you turned 50. After an increase of patients diagnosed with colon cancer in people younger than 50, the recommended age for a screening colonoscopy was lowered to 45.

Colorectal cancer is the 2nd leading cause of cancer deaths among cancers that affect both men and women. Symptoms usually do not appear until the disease has spread.
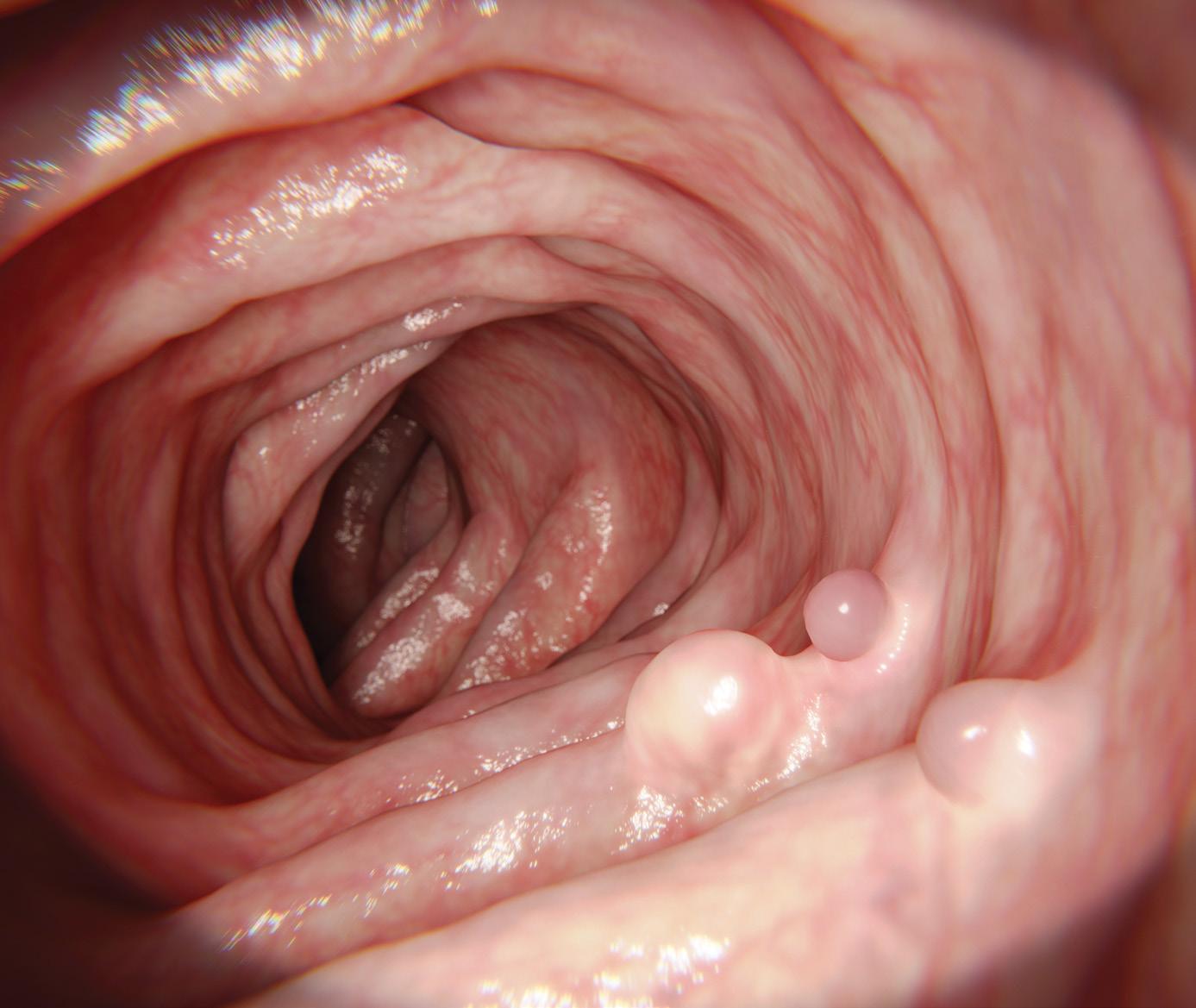
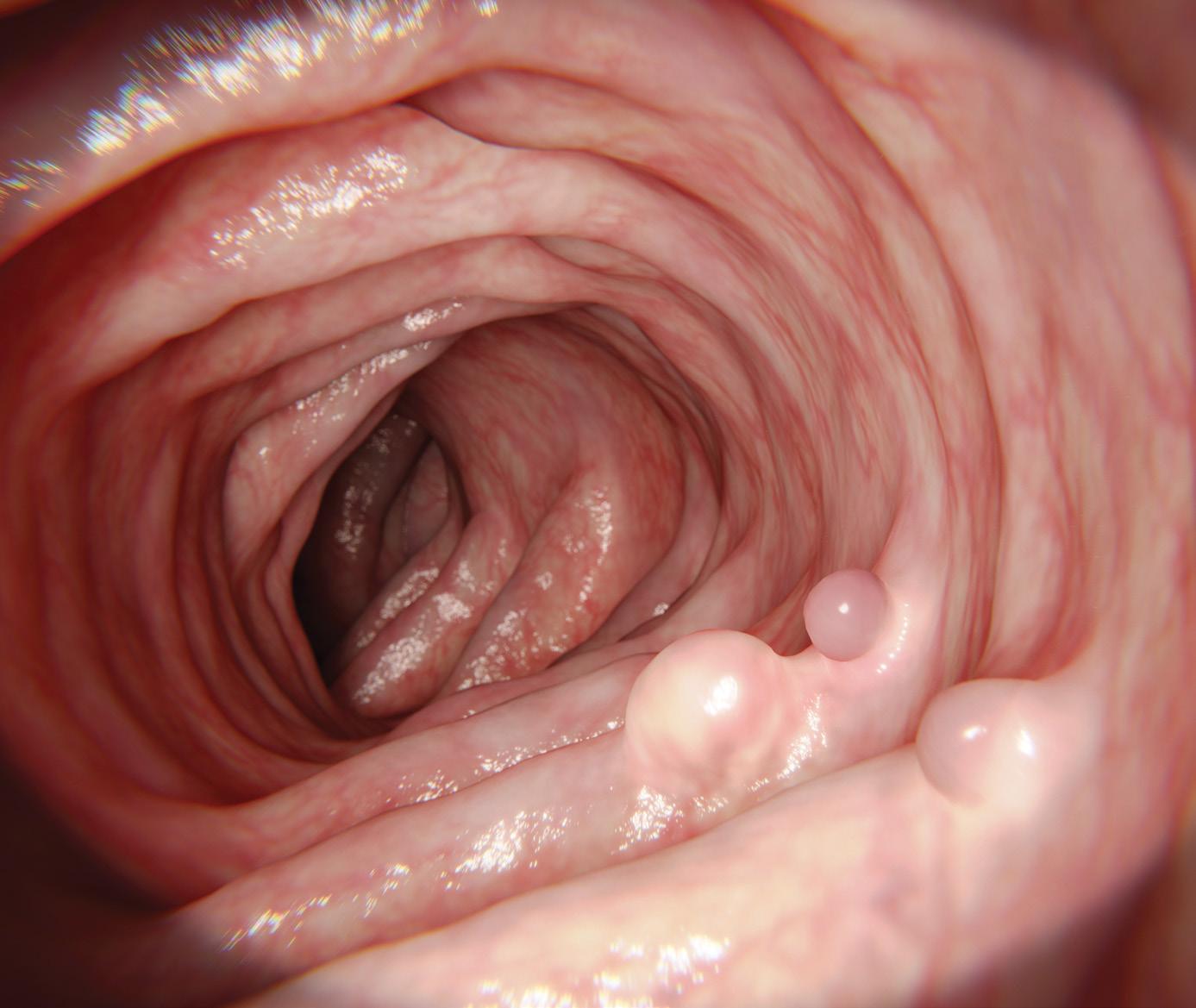
What is a Polyp?
A small growth in the colon is called a polyp. Colon cancer usually originates from the growth of polyps. Small polyps do not cause pain and can grow undetected without symptoms. The best way to detect and remove polyps is by having a screening colonoscopy. A well prepped colonoscopy is also the only way to remove a polyp.
What is a Screening Colonoscopy?
The screening procedure is called a colonoscopy. This is the only way to detect if there are any polyp growths in a colon. These screenings are important, because they can detect a problem early when it is most curable. A colonoscopy is a safe procedure that is performed with sedation.
18 BOONE HEALTH Fall 2022
When is it time to begin screening?
• If you have no family history of colon cancer
• If you have no symptoms
• Age 45
• A screening colonoscopy should be performed sooner if you have symptoms of rectal bleeding, have had a change in bowel habits or if you have a family history of colon cancer. Consult your physician if they do.

What happens if I don’t get a screening colonoscopy but there could be polyps in my colon?
A polyp can be safely removed during a screening colonoscopy. If a polyp is not removed, and is allowed to continue to grow, it has a potential of turning cancerous. By getting a colonoscopy, you are detecting and removing polyps before they can become cancer.
Risk Factors You Cannot Control
• Genetics
• History of polyps
• Inflammatory bowel disease
• Age
• History of colon, breast or ovarian cancer
Risk Factors You Can Control
• Obesity
• Inadequate Exercise
• Tobacco Use
• Alcohol consumption beyond recommendations
What can I do to help myself?
• Diet and good physical health
• Diet can play a role to decrease colon cancer: Eat foods high in fiber and low in fat and limit red meat and processed foods.
• Good physical health and exercise can decrease the risk of colon cancer up to 24%. American Cancer Society recommends 30 minutes 5 days a week.
A polyp is a small growth on the colon.
A camera is used to safely check the colon for small growths.

“With other types of screenings, you can see, feel and touch what you’re evaluating. Like breast cancer. You can’t do a self evaluation for your colon like you can do for your breasts. You can’t feel a polyp. And if you have a polyp, your symptoms may occur after a polyp has progressed too far.
A screening colonoscopy is such an important screening because it actually gets inside the colon with a camera visually looking for small growths. We’ve made such good progress over the last 25 years and that is why colon
cancer is decreasing. Because we’re catching it and finding polyps so much earlier!” says Lucy Shaffer, Certified Gastroenterology RN.
Scheduling a colonoscopy requires a referring physician. If you need to find a provider, please visit www. boone.health/primary care. If you have a physician and want to schedule a screening colonoscopy, you can call your provider and request one be sent to Boone Hospital Scheduling.
By Lucy Shaffer, CGRN
Boone.Health/My-Boone-Health 19
A
By Jennifer Tveitnes, RD, LD

Hamburger Soup
Heart Healthy
For a recipe to be considered heart healthy, it should be low in saturated fat, low in sodium, and high in fiber. A few easy changes to this Hamburger Soup recipe made it more suitable for a heart healthy diet.

To make this recipe low in saturated fat…
• Swap ground beef for lean ground turkey
• Use a naturally low fat cheese as a topping
To make this recipe low in sodium…
• Use a no-salt-added canned tomatoes
• Use a no-salt-added canned broth
• Use a small amount of reduced sodium soy sauce
• Add a modest amount of salt
To make this recipe high in fiber…
• Incorporate a lot of vegetables!
INGREDIENTS
• 1lb 93/7 ground turkey
• 2 stalks celery, diced
• 1 clove garlic, minced
• 1 (14.5oz) can no-salt-added diced tomatoes
• 3C no-salt-added beef broth
• 1 whole yellow bell pepper, seeded and diced
• 1 whole red bell pepper, seeded and diced
• 1 whole green bell pepper, seeded and diced
• 3 large carrots, peeled and sliced
• 5 baby red potatoes, cut into quarters
• ½ tsp each kosher salt, black pepper
• 1 tbsp Italian seasoning
• 1 tbsp reduced-sodium soy sauce
• Mozzarella cheese, shredded, for serving
INSTRUCTIONS
1. In a large pan over medium-high heat, brown the meat with the celery and garlic. Drain.
2. Add the meat mixture into a large slow cooker with the rest of the ingredients.
3. Cook on high for 4-6 hours, or until potatoes are softened. Serve with cheese.
Recipe adapted from www.thepioneerwoman.com
Boone.Health/My-Boone-Health 21
BY EMILY NUSBAUM, RN, IBCLC, BOONE FAMILY BIRTHPLACE

22 BOONE HEALTH Fall 2022 BRINGING UP BOONE BABIES WHAT’S NORMAL?
BREASTFEEDING A NEWBORN
Breastfeeding is a normal and natural part of delivering a baby. Our bodies produce breastmilk as a result of hormones and continue to produce as our babies nurse. New parents are often surprised to learn that breastfeeding can be confusing or hard – shouldn’t things that are normal and natural be easy? Not necessarily! So, what is normal for a newborn?
WHAT’S THE BEST WAY TO START BREASTFEEDING?
Skin to skin: When a baby is born, the best place to transition to the outside world is on their mother’s chest, skin to skin. Ideally, they will stay there for 2 or more hours. The baby may begin to show signs of hunger by opening their mouth, turning their head from side to side (a behavior called rooting), and putting their hand in their mouth. A baby can latch on the breast right away or they may need time to figure it out. Babies can breastfeed for a few minutes or for an hour. Often babies are awake and active for the first hour or two before they get sleepy.
HOW OFTEN SHOULD MY NEWBORN FEED?
8 to 12 times in 24 hours:
Babies need to eat 8 to 12 times in 24 hours to get the nutrients they need – and breasts need stimulation at the same time to get the message they need to continue producing milk.
It’s best and most effective to feed your baby when they show signs of hunger like opening their mouth, putting their hands in their mouth, and rooting. If your baby hasn’t eaten for 2 to 3 hours, undress your baby and change their diaper. Hold your baby skin to skin again so they can feel, hear and smell you, and they may begin to show hunger signs.
Sometimes a baby who had a great first breastfeed will go into a sleepy state and will not wake for a feeding until a few hours later. Babies don’t have to be wide awake to eat, but they do need to be awake enough to participate. Try to wake your baby by undressing him, changing his diaper and holding him skin to skin. If your baby won’t wake for feeding, then you can hand-express milk.
WHAT IS COLOSTRUM AND WHY IS IT IMPORTANT? Colostrum is the first milk your breast produce. It’s produced in smaller quantities than mature milk and is full of amazing nutrients for babies. Colostrum is also the best possible substance to make up your baby’s gut microbiome for a healthy gut. But sometimes it’s necessary for newborns to get formula as a supplement.
If your baby has low blood sugar, high bilirubin, or is losing too much weight (7 to 10% of their birth weight), your pediatrician or nurse may suggest using formula –but that shouldn’t stop you from breastfeeding, too. If your baby needs supplemental nutrition, it’s recommended that you still put your baby to the breast or use a pump or hand expression to stimulate the breast. Firstdroplets. com has helpful information, including videos, on how to hand-express and the importance of stimulating the breast to give your baby as much colostrum as possible in their first few days of life.
In the first few days of life, a healthy, full-term newborn will get approximately 2 to 10 milliliters (mL) –about ½ to 2 teaspoons – of colostrum at a feeding. If your baby has medical issues or is preterm, their needs may be different. Your baby’s doctor will discuss these needs with you.
If you set an alarm to wake or remind you to feed your baby, they can go for a longer stretch at night without eating, but not longer than 4 hours. You can begin to observe your baby’s pattern after a few days.
By day 3 of your baby’s life, they should eat 10-30 mL – about 2 teaspoons to 2 tablespoons – per feeding and by day 10 up to 1.5 ounces or 3 tablespoons. (Since we can’t precisely measure how much breastmilk a baby receives while nursing, these are estimates.)
HOW DO I KNOW MY BABY IS GETTING ENOUGH?
Wet and dirty diapers: You can make sure your baby is getting enough at feedings but counting how many times they eat, their weight, and how many wet and dirty diapers they have each day:
• Day 1: Your baby should have at least 1 wet diaper and 1 stool in the first 24 hours.
• Day 2: 2 wet and 2 dirty diapers
• Day 3: 3 wet and 3 dirty diapers changing from black meconium to brown
• Day 4: 4 wet and 2 to 3 dirty diapers with a yellow, seedy consistency
• Day 5: 5 wet and 1 to 5 dirty diapers
• Day 6 and beyond: At least 6 wet diapers and 1 to 6 stools each day
WHAT IF I’M STILL UNSURE?
If your baby has 8 to 12 feedings a day, the expected amount of wet and dirty diapers, and is not losing too much weight when she is weighed in the hospital or your pediatrician’s office, rest assured that you are doing what you can to ensure your baby gets the nutrition they need. If you have any questions or concerns, call your pediatrician’s office or lactation consultant.
DID YOU KNOW?
Boone Health Labor and Delivery provides lactation consultant support to new mothers while in the hospital and after returning home. For more information, call 573.815.6290.
Boone.Health/My-Boone-Health 23
Timur Gusov, MD

Endocrinology, Boone Health Diabetes & Endocrinology
Imoved to Columbia, Mo. from Brooklyn, Ny. in 2017 after completing my internal medicine training. I was a hospitalist at the University Hospital for 3 years. I loved my job, but I was missing my true passion – endocrinology. With support from my family, I decided to pursue this specialty and completed a fellowship in endocrinology at the University of Missouri. My wife is also a physician, and we have two adorable children.
Why did you get into the health care field? My mother was an exceptional physician who was dearly loved and respected by her patients and community. She was my role model, and I followed in her footsteps to pursue medicine.
What interested you in your specialty? Endocrinology is a very diverse field. You must master a much broader range of organs than other specialties. You get to take care of complex diseases and make a huge impact on your patients’ quality of life. Endocrinology covers conditions from fertility, treating chronic wounds, cosmetics, prevention of deadly complications from a metabolic syndrome to much more.
What is the most rewarding part of your job? The most rewarding part of my job is significantly improving my patients’ quality of life, changing lives, and treating diseases that as little as 100 years ago were a death sentence, not a diagnosis. Contemporary technologies help us better understand and treat diabetes – and now we can even do so remotely.
What is the most challenging aspect of your job? The most challenging aspect in clinic settings is time constraints. A patient isn’t just a list of medical problems and medications. It takes time to understand their clinical situations, and review and analyze laboratory results and radiologic data. A newly diagnosed patient requires time to understand the disease process and you need to work with them to develop a treatment plan together.
What do you see changing in health care in the next 5 to 10 years? I foresee an increase in use of technologies even more, including devices that will monitor vital information and send the data to your doctor.
What advice would you give someone looking to become a doctor? Follow your passion. Being a physician is
one of the greatest privileges. You not only get to alleviate pain and suffering but help people live healthier lives. You have the ability to change the lives of so many people for the better, but it also comes with responsibilities.
What do you enjoy doing outside of work? I enjoy spending time with my family, playing piano, biking, and playing tennis.
What advice would you give to someone who is going to be a patient in a hospital for a period of time? Being admitted to hospital is one of the most difficult times in a person’s life – and we understand that. Have faith in your team. We are working hard to help you feel better and get you back home to your loved ones.
Scan the QR Code to checkout Dr. Gusov’s musical talents!
24 BOONE HEALTH Fall 2022
GETTING TO KNOW A BHC DOCTOR
Pearl Lariosa, MBA, BSN RN, CMSRN Surgical Specialties
Iwas born and raised in Cebu, Philippines.
After receiving my Bachelor’s in Mathematics, I was a research analyst for 2 years. Working with nurses during a research study led to a change of heart – I pursued nursing and graduated in 1988. 2022 will be my 34th year as a nurse.

I emigrated to the U.S. in 1990 and was hired by New York City Health and Hospitals Corporation under an H-1B Professional/Skilled Worker Visa and worked in one of the biggest trauma centers in Brooklyn for 5 years.
My husband is a physical therapist who came here under the same working visa. We decided to move to Jefferson City, Mo. and call it our home away from home – and for the new family we started, home! Our two children were born in Jefferson City and went to St. Peter’s Interparish School and Helias Catholic High School. Both are University of Missouri alumni. My son earned a degree in Mechanical Engineering, and my daughter earned hers in Health Science, Pre-Med.
My nursing journey has been a rewarding one. When I relocated from New York to Jefferson City, where I worked at St. Mary’s, I found it challenging to meet new people while raising a new family with no relatives nearby. My husband and I became each other’s support system. As we settled in and became familiar with the area, we gradually felt at home. While the kids were at school, I decided to pursue my MBA. After graduation, I became a nursing instructor for the Practical Nursing Program. I taught at Nichols Career Center with the Jefferson City Public School District for 10 years. I stayed on for 4 years when the program transferred to State Technical College of Missouri, then joined Boone Health in December 2017.
Why did I choose to work at Boone? Why not Boone? This is the best place to work.
My daughter saw a Boone commercial on TV and said, “Mom, how would you describe Boone in one word?” Without hesitation, I said “Diversity.”
The moment you enter Boone, you meet people of different ages, walks of life, emotions, and backgrounds. Where there is diversity, there is progress. The culmination of differences shows both moving and learning from each other instead of stagnation. In our different units, you see employees of different backgrounds, and experiences working together to provide safe and excellent care to patients, their families, and other members of the Boone community.
I continue to be a teacher – I just moved my classroom to the nursing floor where everything is real and hands on. You can hear lung sounds and heartbeats. You turn patients, provide skin care, distribute medications, and monitor vital signs. You talk to patients, physicians, and care team members face-to face. In my opinion, learning has no walls, you can learn anytime and anywhere.
My advice to new nurses is to be resilient. Be like flowing water – if you encounter a stone along the way, go around or above the stone. But never stop, and keep moving forward, even at a slow pace, you are moving.
Also, strive to a better person than you were yesterday. Even if you learn something small today or repeat yourself to perfect a skill, you are doing something to better yourself.
It is also easy for us busy nurses to forget to take care of ourselves. A healthy nurse takes care of their personal health, safety, and wellness, and lives life to their fullest capacity. A healthy nurse is a better role model, educator, and advocate for themselves, for the family, for the community, for the work environment, and, most importantly, for the patient.
Boone.Health/My-Boone-Health 25 GETTING TO KNOW A BHC NURSE

FUELING OUR BODIES
When it comes to kids and sports, many parents are unsure how to best fuel their young athletes. Kids often arrive to practice or games under fueled or improperly fueled after being given inappropriate or unnecessary foods.

When striving for peak performance during sports, hydration is crucial. It is important to stay hydrated throughout the entire day for optimal performance. There are many options for beverages, but water is the best for hydration. Kids only need sports drinks during intense activity lasting an hour or more. Fruit juices and sugarsweetened beverages are not recommended.
When it comes to food, low-fiber, low-fat foods are the best choice immediately before and during a sporting activity. Simple, nutritious carbohydrates give your athlete easily accessible energy. Foods higher in fat or fiber take longer to digest, so their energy isn’t accessible to your child’s body during the activity and could also cause upset stomachs.

CHOOSE:
• Low-fiber granola bars
• Pretzels

• Graham crackers
• Fruit
• Dry cereal
• Fat-free yogurt
• 1% or skim milk
AVOID:
• Pastries (doughnuts, muffins, etc.)
• Desserts
• Vegetables
• Bacon
• Fried foods
• High-fat dairy products
How do we put all of this together to properly fuel for games and practices? Here’s an easy sample menu:
BEFORE: Water and apple slices
Immediately after a practice or game, foods high in fiber and protein are important. High fiber foods provide carbohydrates to replete your kid’s glycogen – or energy stores– and will help slow digestion and stabilize blood sugar. The body easily absorbs protein in the first hour after exercise – eating foods high in protein shortly after exercise is the best way to repair and build muscles.
Sugary, low-fiber snacks are often provided to teams after their games but don’t provide much fiber or protein and are not the best choices for growing athletes.
CHOOSE:
• Whole grains
• Lean cuts of meat
• Fish
• Vegetables
• Milk
• Fruits
AVOID:
• Sugary snacks
• Fatty meats
• Foods low in fiber
DURING: Water and pretzels or saltines
AFTER: Water and a lean burger on whole-wheat bun with small baked sweet potato By Jennifer Tveitnes, RD, LD

Boone.Health/My-Boone-Health 27
For more information on Nutrition Counseling, visit boone.health/nutrition or call 573-815.3870
All Shook Up
What to Expect After a Concussion
Your niece collided with an opponent at a soccer game. Your friend was rear-ended on the Business Loop. You fell from a ladder and hit your head. What do the three of you have in common?
Probably a concussion!
A concussion is a mild traumatic brain injury that temporarily affects the brain’s function. This can be caused by any impact or jolt to the head. And you don’t have to hit your head to sustain a concussion – a sudden stop, like in a car accident, can cause your soft brain to hit the hard skull encasing it, resulting in a concussion.

People at risk include athletes, older adults who have fallen, military personnel exposed to a blast, victims of violence and anyone involved in a car accident.
Immediate signs you have a concussion can include loss of consciousness, nausea or vomiting, confusion, clumsiness and difficulty remembering recent events. Seek medical care if you feel these symptoms or observe them in a loved one. X-rays, MRIs and CT scans won’t show a concussion; however, your provider can assess you for concussion symptoms and check your head and neck for other injuries.
Symptoms may change in the days following a head injury, including:
• Headache
• Sensitivity to light or sound
• Feeling more tired than usual
• Imbalance
• Dizziness
• Blurred vision with head movement
• Neck pain
• Thinking and memory changes
• Mood or behavior changes
28 BOONE HEALTH Fall 2022
If you’ve been diagnosed with a concussion, keep in mind that your brain has sustained an injury. Just like a pulled muscle, it needs a combination of rest and symptom-limited activity and exercise to recover. For the first 24 hours or so, rest and take it easy, then try to gradually return to your normal activities. High-quality, adequate sleep is important as you recover. You should also avoid activities that put you at risk of falling or hitting your head. A second head injury can significantly complicate recovery.
A return to activity will vary for each individual. Generally, you should let your symptoms guide your activity level. If you go to work and, after one hour of focusing on your computer screen, your symptoms return or worsen, it’s time to take a break. You may need to sit or lie down in a dark, quiet room for your symptoms to go away. When you feel better, try returning to the activity. If your symptoms get worse again, take another break or consider stopping for the day. This may require your workplace
or school to make accommodations, but don’t hesitate to advocate for yourself. After all, what’s more important than your brain?
Work and exercise aren’t the only things that can stress your recovering brain. Phone time, video games, reading, driving and household chores can also bring on symptoms. These should be gradually increased over several days or weeks until you can tolerate your normal activities.
If you are still dealing with concussion symptoms after a week, it’s time to seek help. Your provider can refer you to physical therapy for treatment. Boone Therapy has three physical therapists trained to treat concussions and dizziness. Thanks to the generous support of the Boone Foundation, Rachel, Nicole and Hannah are American Institute of Balancecertified in Vestibular and Concussion Rehabilitation – and we’d love to help you get back on track.
At your first visit, we will test your eyes, balance, tolerance to physical activity
Vestibular therapists, Hannah Williams, PT, DPT, Rachel Beanland, PT, DPT and Nicole Tunink, PT, DPT standing in front of a visually busy background, which they use to challenge dizzy patients.

such as walking, vestibular or inner ear system, and neck movement. We will also ask you about your symptoms and goals. You’ll receive targeted exercises and guidance to help your brain recover and allow full return to your favorite activities. Over the course of a few weeks, we’ll guide you through progressed activities to decrease your symptoms and recover normal function.
The good news is that, even though a concussion is a brain injury and should be taken very seriously, the prognosis is good. Most people with concussions make a complete recovery. By Hannah Williams, PT, DPT, Physical Therapist at Boone Therapy
Boone.Health/My-Boone-Health 29
For more information on Therapy Services, visit boone.health/therapy-services or call 573-815-3868
A BIG Difference for Patients
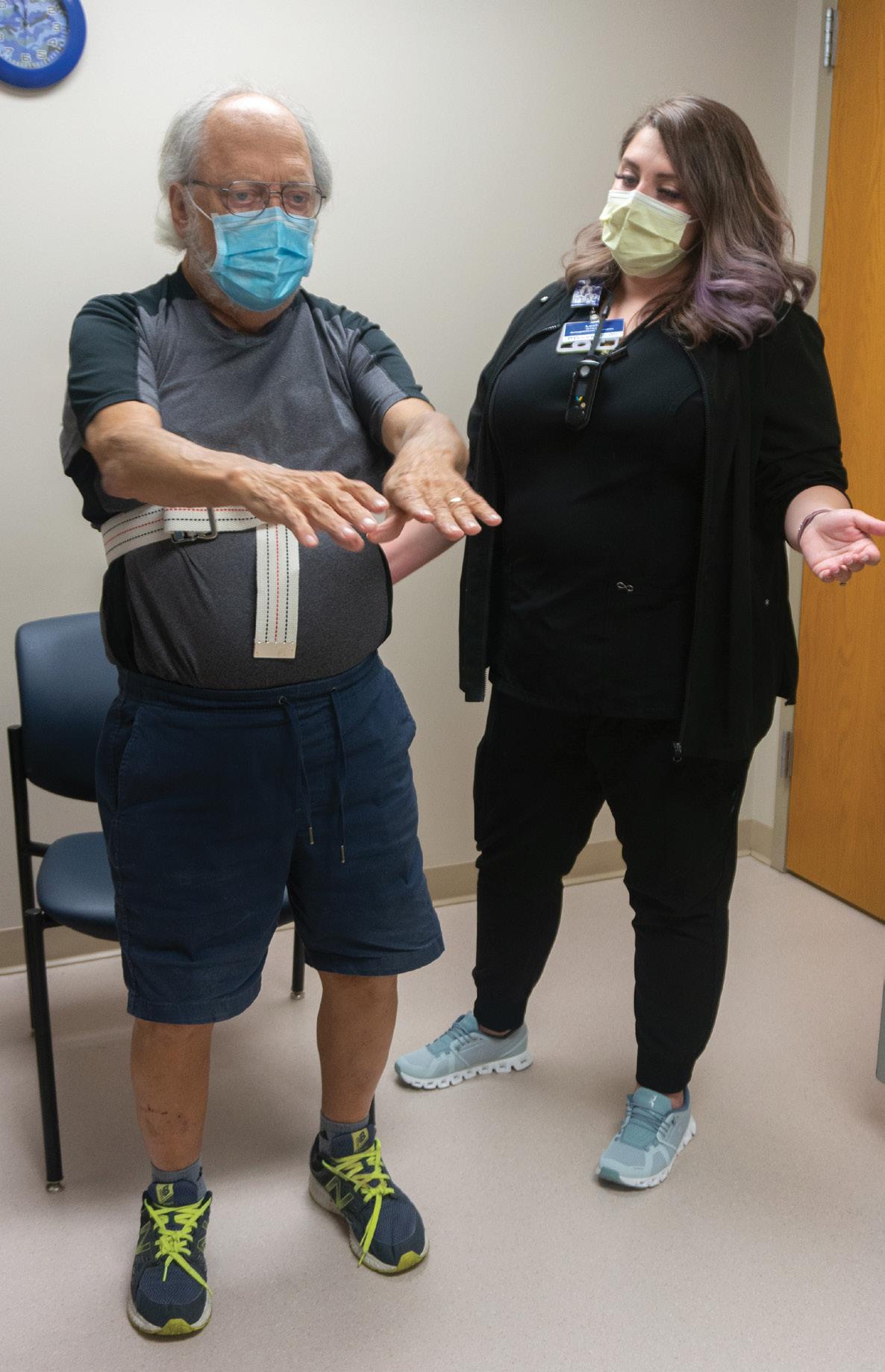
When Occupational Therapist Leah Botkin, MSOT, OTR/L, wanted to make Boone an even better place to receive healthcare, she thought BIG.
Specifically, LSVT-BIG, an evidencebased treatment program that trains people who have Parkinson’s disease or other neurological conditions to improve their mobility and functional independence. People with Parkinson’s typically move with smaller and slower gestures or actions, which can interfere with the activities of daily life, such as moving around the house or getting dressed. These movements can also affect balance, increasing a person’s risk for falls and injuries.
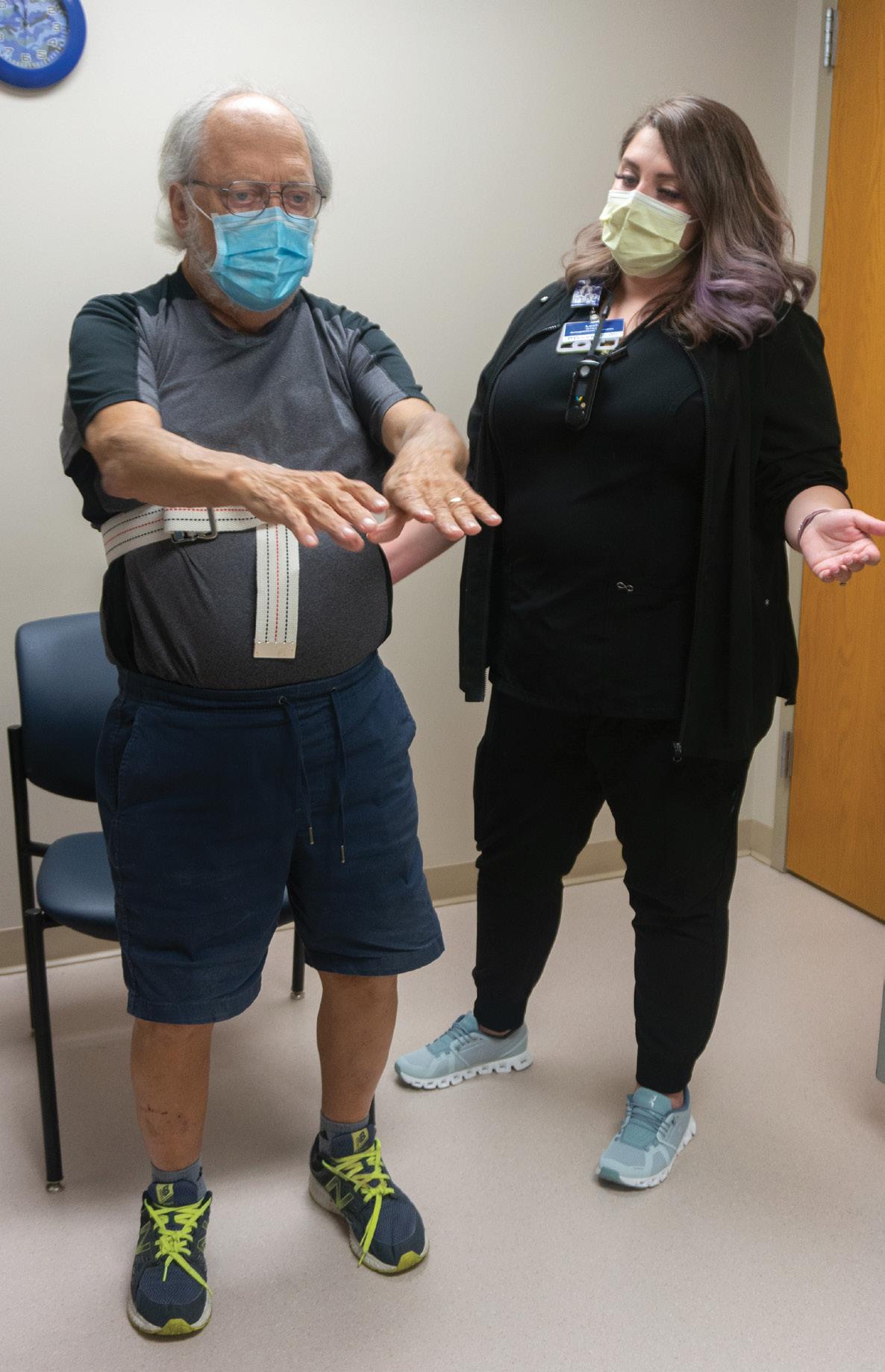

Leah knew that having physical or occupational therapists with LSVT-BIG training and certification could benefit patients with neurological conditions, including stroke and multiple sclerosis, so she approached the Boone Hospital Foundation.
The Foundation uses support from individuals, families, and community organizations to directly improve Boone Health’s patient care services and outreach programs, including staff education to provide enhanced patient care. These programs and enhancements are proposed by Boone’s healthcare professionals. Leah provided clinical evidence showing that LSVT-BIG has had positive impacts on participants’ movement and mobility. The Foundation reviewed and approved her request.
Leah Botkin, MSOT, OTR/L works with patient Woodie McElduff on LSVT-Big exercises
30 BOONE HEALTH Fall 2022 FOUNDATION NEWS
“The Boone Hospital Foundation funded this program because we believe that having more physical and occupational therapists with LSVTBIG certifications can help us better serve our community and increase our patients’ safety and quality of life,” explains Barb Danuser, Boone Hospital Foundation Executive Director. “We proudly support our caregivers seeking and achieving further education, so they have more knowledge and skills to help our patients!”
The treatment is an intensive course of one-on-one sessions, modified to

suit each patient’s individual needs and goals. For one month, a patient works with the therapist for four onehour sessions a week for four weeks, for a total of 16 hours. At the end of the session, Leah assigns her patients homework and carryover exercises that will recalibrate their movements so they can continue to make bigger movements at home.
She adds, “I like to tell my patients that, with this program, we’re going to retrain your brain to make bigger, more quality movements, to help you live life BIG!”
2022
CALENDAR OF EVENTS
OCTOBER 28
Boone Hospital Foundation Annual Gala

NOVEMBER 30-DECEMBER 1 Scrubs on Site Sale at Boone Hospital Center
DECEMBER 14 & 15
Linen Sale at Boone Hospital Center
DECEMBER 2022 COMO Gives Campaign
Boone.Health/My-Boone-Health 31

Boone Hospital Center 1600 East Broadway Columbia, MO 65201 573-815-8000 NONPROFIT U.S. POSTAGE PAID COLUMBIA, MO PERMIT 286

































 The Cox family. From left to right: Mark, Melanie, Jerry, Connie and Marty
The Cox family. From left to right: Mark, Melanie, Jerry, Connie and Marty

 Connie and Jerry on their 66th Anniversary on July 31, 2021.
Connie at a St. Louis Cardinals baseball game in 2020.
Connie and Jerry on their 66th Anniversary on July 31, 2021.
Connie at a St. Louis Cardinals baseball game in 2020.
 Jenny L. Workman, Community Wellness Manager & Charles Kitchen, Mobile Health Unit driver.
Jenny L. Workman, Community Wellness Manager & Charles Kitchen, Mobile Health Unit driver.