BENEFICIAL FOR MOM AND BABY Breast
PEARLS
THIS IS YOUR LANE
PAMED LEGISLATIVE UPDATES












PEARLS
THIS IS YOUR LANE
PAMED LEGISLATIVE UPDATES













Set amidst rich landscaping on 4.6 acres, this custom home was lovingly and thoughtfully built. The timeless design is bathed in light from oversized windows, skylights, and French doors to the private acreage beyond. Offered for $4,250,000

A house to live in, to entertain in, and to cherish, this classic colonial is a genteel blend of grace and subdued elegance, offering every detail befitting a home of this quality. 11,700 sq.ft. of living space over 3 floors. Offered for $7,950,000


Extraordinary finishes and meticulous care are the hallmarks of this outstanding Bethlehem home. Rarely does a property feature the attention to detail and upscale amenities at every turn as does Cross Creek Court. Offered for $1,295,000

A premier property located on Bethlehem’s coveted Main Street extension, this Georgian colonial dates back to the city’s earliest days. Moore Estate has been thoughfully restored and remodeled with wonderful updates. Offered for $1,250,000

back from the road on the banks of Monocacy Creek,
the luxuries of a modern home within the walls of a historic building. Multiple outbuildings on 5 acres offer lots of possiblity. Offered for $925,000



Mountain View
Surrounded by 5 acres of open fields, this circa 1855 barn was thoughtfully converted in 1999. Historic interior details were left intact, and the grounds include raised bed gardens and extensive plantings. Offered for $799,000

LEHIGH COUNTY MEDICAL SOCIETY P.O. Box 8, East Texas, PA 18046 610-437-2288 | lcmedsoc.org
2024 LCMS BOARD OF DIRECTORS*
Chaminie Wheeler, DO President
Kimberly Fugok, DO President Elect
Mary Stock, MD Vice President
Oscar A. Morffi, MD Treasurer
Charles J. Scagliotti, MD, FACS Secretary
Rajender S. Totlani, MD Immediate Past President
*effective February 1, 2024 - for two-year terms
CENSORS
Howard E. Hudson, Jr., MD
Edward F. Guarino, MD
TRUSTEES
Wayne E. Dubov, MD
Kenneth J. Toff, DO Alissa Romano, DO
EDITOR
David Griffiths Executive Officer
The opinions expressed in this publication are for general information only and are not intended to provide specific legal, medical or other advice or recommendations for any individuals. The placement of editorial opinions and paid advertising does not imply endorsement by the Lehigh County Medical Society.
All rights reserved. No portion of this publication may be reproduced electronically or in print without the expressed written consent of the publisher or editor.






Welcome to the summer issue of Lehigh County Health and Medicine. We are focusing on some seasonal health topics with articles we hope you will read, enjoy, and perhaps even be surprised by. Here are some highlights.
We have a great article on the importance of communication skills in the physician-patient relationship, so read “Communication Pearls Learned as an Emergency Room Physician.” The author shares some of what she learned from workshops on the relationship-centered communication program. Hopefully, our members will be interested in participating in a workshop like this.
August is National Breastfeeding Month, and you can learn more in the article “Breastfeeding: Beneficial for Mom and Baby.” The author provides information and education from the first decision of whether to breastfeed or not, and discusses the benefits.
We also want to introduce you to our 2023 Humaneness in Medicine Award recipient, Auguste Niyibizi, D.O. The Lehigh County Medical Society awards this annually to one or more Lehigh County medical residents or fellows who have best displayed the ideals of outstanding compassion in the delivery of care, respect for patients, their families, and health care colleagues, as well as demonstrated clinical excellence. Congratulations to Dr. Niyibizi.
We hope you enjoy this and past issues as we add to the conversation about how medicine and wellness can help us form strong communities in Lehigh County. If you are interested in back issues, or just want to read Lehigh County Health and Medicine online, please visit our website at https://lcmedsoc.org/our-publication
If you have ideas or suggestions for upcoming issues, please consider reaching out to us; our email address and phone number are on our website https://lcmedsoc.org/
Thank you for reading!
MADALYN SCHAEFGEN, MD, FAAFP, LEHIGH VALLEY PHYSICIAN GROUP AMBULATORY IMMUNIZATION CLINICAL LEAD AND VICE CHAIR OF PENNSYLVANIA IMMUNIZATION COALITION
VACCINE PREVENTABLE DISEASES ARE ON THE RISE.
As we recover from the COVID-19 pandemic, let us not forget that we still have more people dying from COVID than from influenza, and that most of these deaths can be prevented through vaccination. (COVID-19 illness, although declining, resulted in 132 deaths the week of June 8th.) Cases of pertussis, measles, Neisseria meningitidis, and hepatitis A illness are rising, resulting in outbreaks.
THERE IS A DECLINE IN ROUTINE VACCINATIONS SINCE THE PANDEMIC, WHICH HAS SPREAD FROM COVID-19 VACCINES TO ALL VACCINES.
The prior 3 school years (2019–20, 2021–22 and 202223), national coverage with state-required vaccines among kindergartners declined from 95% to approximately 93%. 2023-2024 school year was the first time that MMR vaccine coverage for PA kindergarteners went below 95%. Maintaining community immunity greater than 95% is necessary to reduce risk for vaccine preventable disease and to protect those whose immune systems are not as robust. Immunization is the most effective means of prevention.
VACCINES WORK.
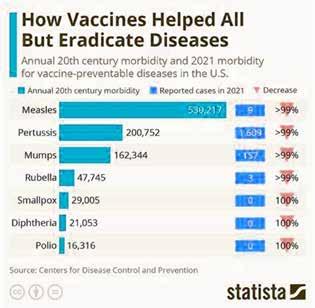


VACCINE REFUSAL PUTS PEOPLE AT RISK.
Immunize.org has evidence-based references regarding decline in vaccination rates and rising rates of vaccine preventable diseases that you can find at https://www.immunize. org/wp-content/uploads/catg.d/p2069.pdf.
VACCINE EXEMPTIONS ARE ON THE RISE.
Vaccine exemption rates among kindergarteners has increased in 41 states, including Pennsylvania. Childhood immunization coverage levels are lower when non-medical exemptions to requirements are available, especially if they are easy to get. PA allows medical, religious and moral/ethical exemptions to vaccines. PA law requires certain immunizations, but does not require HPV nor MenB. HPV vaccine is extremely effective in preventing HPV-related cancers. Outbreaks of other vaccine-preventable diseases, such as measles, pertussis, and varicella, have been traced to pockets of unvaccinated children. And no one wants to lose a child to meningitis which can be prevented.
VACCINES HAVE BEEN AROUND SINCE THE 1700S , AND THEY CONTINUALLY CHANGE AS TECHNOLOGY AND VIRUSES CHANGE.
Vaccine changes are improvements. U.S. governmental reviews, approvals and monitoring of vaccines is robust. The vaccines go through rigorous testing prior to FDA approval, then have continued monitoring after approval through agencies including The Vaccine Adverse Event Reporting System (VAERS), The Vaccine Safety Datalink (VSD), V-safe, and The Clinical Immunization Safety Assessment (CISA) Project. The newer vaccines are more effective with no more associated risk.
ACIP is meeting on June 26-28 to review and vote on vaccines for RSV, DTaP/Hib/HepB (Vaxelis), COVID-19, influenza (including Avian influenza A H5N1), and pneumococcal (PCV21) vaccines. They will also review Chinkungunya, Dengue (both of which may become more important as travel and global temperatures increase) and MenABCWY. Look for the immunization schedule and schedule changes with guidance at https://www.cdc.gov/vaccines/ schedules/index.html and https://www.cdc.gov/ vaccines/schedules/hcp/schedule-changes.html.
1. THINK ABOUT DRIVERS FOR HESITANCY.
Health care information is found increasingly outside of the physician/clinician-patient relationship.
Misinformation/Disinformation has accelerated exponentially with social media.
Distrust/lack of confidence in vaccines has increased with the COVID-19 pandemic, vaccines.
Polarization regarding vaccines has occurred similar to polarization of the country.
Number of vaccines in the schedule has increased and changed.
Misperceptions and myths occur regarding
a. Low level of risk to disease (invulnerability)
b. Higher risk of adverse events than exists with the vaccine
c. Vaccine ingredients and harm (lack of knowledge)
Vulnerability (pandemic, pregnancy, mental illness, etc) to be persuaded by “fake news.”


2. REMEMBER THAT PEOPLE WANT WHAT’S BEST FOR THEMSELVES, THEIR CHILDREN, THEIR FAMILIES.
Treat all with empathy and compassion.
Avoid labeling patients or increasing their fears.
Listen and ask questions.
Provide choices. Offering options can reduce vaccine hesitancy.
Remind that a choice to not vaccinate is not a risk-free choice.
3. STRATEGIES TO USE FOR ALL YOUR PATIENTS.
Give a strong recommendation which is personalized to your patient.
a. Providers are a patient’s most trusted source of information on vaccines.
b. Research shows a patient who receives a strong recommendation from a provider is 4–5 times more likely to be vaccinated.
Presume they are interested in getting the vaccine.
Continued on page 8
Increase your vaccine knowledge. If patients have questions about the vaccines, be sure that you AND YOUR STAFF have evidence-based answers! To prepare, see https:// www.cdc.gov/vaccines/hcp/conversations/ preparing-for-parent-vaccine-questions.html.
Have the vaccines available in the office (or refer out if needed).
Ask where they lie on the number continuum to accept a vaccine. (On a scale of 1 to 10, 10 being they are ready to get a vaccine, where are they? Look for the positive - Have them express why they did not pick a lower number.)
Ask open ended questions as to why they do not want to get a vaccine.
Actively listen to the concerns.
Affirm you hear what they are saying.
Request permission to share what you think. Know your patient. Highlight social norms. Use stories. Present facts.
If they are still unwilling, be patient and be sure to maintain the relationship to discuss another day.
CHANGE IS HARD BUT INEVITABLE.
Change increases emotions like anxiety. There are 2 ways to cope with change: escape (avoidance, feeling like a victim) and control (managing the change).
VACCINE HESITANCY IS NOT NEW.
Vaccine opposition/hesitancy has been around ever since the first vaccine was introduced by Jenner in 1796. Why is hesitancy increasing? Big changes over which we have no control (pandemic, climate change), changes in how we view the world (internet,
1. https://covid.cdc.gov/covid-data-tracker/#trends_weeklydeaths_select_00
2. Seid, Arlene, Torso Orkis, Lauren. PA Immunization Conference, Hershy, June 13, 2024
3. https://www.cdc.gov/mmwr/volumes/72/wr/mm7245a2.htm
4. http://dx.doi.org/10.15585/mmwr.mm7245a2
5. https://www.pacodeandbulletin.gov/Display/pacode?file=/secure/pacode/ data/028/chapter23/s23.84.html&d=reduce
6. https://www.pacodeandbulletin.gov/Display/pacode?file=/secure/pacode/ data/028/chapter23/s23.83.html&d=reduce
7. https://www.cdc.gov/vaccines/vpd/hpv/hcp/vaccines.html#:~:text=All%20 HPV%20vaccines%20have%20been,with%20the%20vaccine%20types%20at
8. https://www.who.int/news-room/spotlight/ history-of-vaccination/a-brief-history-of-vaccination
9. https://www.cdc.gov/vaccinesafety/index.html
10. https://www.cdc.gov/vaccines/acip/meetings/index.html
11. https://www.mindtools.com/amgqesi/coping-with-change
12. https://www.michigan.gov/-/media/Project/Websites/mdhhs/Folder3/ Folder36/Folder2/Folder136/Folder1/Folder236/Fall_Immunization_Conferences__building_vaccine_confidence_102018_Final_Marquette. pdf?rev=0874ee45607c43568e1d0cb6f9aef772
13. https://doi.org/10.1016/j.vaccine.2023.11.004
14. https://medicalxpress.com/news/2024-04-options-vaccine-hesitancy.html
15. JAMA Netw Open. 2022;5(12):e2246634. doi:10.1001/ jamanetworkopen.2022.46634
16. 2007 National Survey of Children’s Health. Factors associated with human papillomavirus vaccine-series initiation and health care provider recommendation in U.S. adolescent females. Vaccine 2012;30(20):3112-3118
social media), and the decline in prevalence of vaccine preventable diseases (due to prior vaccines and better health care).
ADDRESSING VACCINE HESITANCY.
Intention to vaccinate was consistently correlated with concerns about the disease, trust in health institutions, and previous vaccinations. How do we move from hesitancy to accepting vaccination?
EVERYONE DESERVES A SECOND CHANCE! BE AWARE OF THE VACCINE CATCH UP SCHEDULE. You can find it at https://www.cdc.gov/ vaccines/schedules/hcp/imz/catchup.html.
TRAVELING THIS SUMMER? Don’t forget vaccines at least 2 weeks prior to the trip. See https://wwwnc.cdc.gov/travel.
Vaccinate! You can save a life!


DAVID ADAMS, MSIV, USF MORSANI COLLEGE OF MEDICINE, AND PATRICIA M. IRVINE, MD, FACULTY CONTENT ADVISOR
New mothers are faced with a myriad of decisions on a daily basis. One of the most important decisions is whether to breastfeed. This article endeavors to lay out the benefits of breastfeeding for both the mother and the child. The topics reviewed in this article are important for both mothers and healthcare providers to consider during the decision-making process. Ultimately, the choice to breastfeed or use an alternative method is a deeply personal decision. Children can grow and develop appropriately regardless of what method is employed. There are a multitude of factors that inform a mother’s choice on how to feed their child. It is
Continued on page 10



important to remember that at the end of the day, the best decision is the one that works for each individual and their child.
Babies will often show interest in feeding within the first few hours after being born. Skin-to-skin time immediately after birth, if feasible, is helpful to promote bonding and encourage the baby to begin feeding.1 Babies will feed about every two to three hours beginning at birth and continuing for the first few weeks. They will often set their own schedule, feeding much more frequently during some periods in what is referred to as “cluster feeding.” A typical feeding can be 10 to 15 minutes per breast, but babies will often feed entirely at one breast and be full. This is normal, but it is important to switch breasts each feeding if this is the case.2 The initial milk produced is called colostrum. It is rich in nutrients for a newborn and is often more thick and yellow. Transitional milk will begin being produced within the first few days, commonly known
The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months before solid foods are introduced. Breastfeeding, along with complementary foods, can be continued for up to two years and even longer if desired.
as the milk “coming in.” Within two weeks, mature milk will be produced displaying the more characteristic appearance of breast milk. Throughout these stages, breast milk changes in nutrient composition to adapt to the needs of the baby.3 The American Academy of Pediatrics recommends exclusive breastfeeding for the first six months before solid foods are introduced. Breastfeeding, along with complementary foods, can be
continued for up to two years and even longer if desired.4
Breastfeeding is not without its complexities though. The progression of milk supply varies among mothers and can be a cause for concern in newly breastfeeding mothers when they may feel there is not adequate production. While frustrating, if the baby is producing adequate wet diapers
and having appropriate changes in weight, there is no need to worry. Mothers rarely produce inadequate quantities of milk. If the nutrition of the baby does become an issue, it is perfectly reasonable to supplement with formula until milk production rises to the necessary levels. Breast milk production can be stimulated by frequent feedings or pumping to continue encouraging the body to produce.5 The baby’s ability to latch and feed properly can also impact this process. Some babies require extra help to learn this new skill, which is where lactation consultants and other support groups can be of great assistance to a new mother.2 While the journey to successful breastfeeding can be fraught with setbacks and challenges, the benefits to the mom and baby can be substantial.
MATERNAL BENEFITS
The maternal health benefits of breastfeeding are well documented. Breastfeeding has been shown to stimulate the release of the hormone oxytocin. This helps the uterus contract, which will decrease postpartum bleeding and expedite the return of the uterus to its normal size. Another popular benefit is that breastfeeding can help mothers return to their baseline weight more quickly.2 Breastfeeding can also reduce the risk of chronic diseases such as hypertension, diabetes, and rheumatoid arthritis while also reducing the risk of certain cancers such as breast and ovarian cancer.4 Outside of the health benefits for the mom, breastfeeding can improve bonding with their child and reduce the financial burden imposed by needing to purchase formula.6
The benefits of breastfeeding are extensive for children. One of the most important benefits is the passive immunity conferred to the child through maternal antibodies in breast milk. Children breastfed for three to six months had significant reductions in their rates of common childhood infections like otitis media, respiratory tract infections, and GI tract infections. Breastfed children also have decreased rates of chronic illnesses such as asthma, eczema, inflammatory bowel disease, and celiac disease.4 It has been shown
1
It stimulates the release of the hormone oxytocin, which helps the uterus contract which helps decrease postpartum bleeding.
2
It can help mothers return to their baseline weight more quickly.2
3
It can reduce the risk of chronic diseases such as hypertension, diabetes, and rheumatoid arthritis, as well as certain cancers such as breast and ovarian cancer.4
4
It can improve the bonding between mother and child.6
5
It can reduce the financial burden imposed by needing to purchase formula.6
that any amount of breastfeeding can lower the risk of sudden infant death syndrome.2 Studies analyzing the benefits of breastfeeding are ever evolving, with new potential benefits still being discovered. There is evidence that breastfeeding can reduce the risk of pediatric cancers, particularly acute lymphocytic leukemia and acute myelogenous leukemia.4 There is also evidence to suggest that breastfeeding can reduce lifelong rates of obesity, diabetes, and hypertension. Many of the discussed health benefits are directly correlated to the length of breastfeeding, with longer durations associated with more drastic reductions in risk. Particularly important are the first six months.6 As a good summary of the benefits of breastfeeding, a trial was conducted comparing 1,000 infants exclusively breastfed for three months versus 1,000 infants who were never breastfed. It was found that within the first year of life, the 1,000 infants who were never breastfed required over 2,000 more office visits, over 200 more days in the hospital, and over 600 more prescriptions. 7 The benefits of breastfeeding are clear, and breastfeeding should be encouraged for all children if their situation allows.
This article does not constitute medical advice and any questions or concerns relating to you or your baby’s health should be directed to your healthcare team.
1. https://www.stanfordchildrens.org/en/ topic/default?id=breastfeeding-getting-started-90-P02637
2. https://www.acog.org/womens-health/faqs/ breastfeeding-your-baby
3. https://wicbreastfeeding.fns.usda.gov/ phases-breast-milk#:~:text=You%20will%20 make%20transitional%20milk,to%20meet%20 your%20baby's%20needs.
4. https://www.aap.org/en/patient-care/ newborn-and-infant-nutrition/ newborn-and-infant-breastfeeding/
5. https://www.nationwidechildrens. org/conditions/health-library/ breastfeeding-and-delayed-milk-production
6. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC3508512/
7. https://pubmed.ncbi.nlm.nih.gov/10103324/
The Lehigh County Medical Society (LCMS) is pleased to announce that Auguste Niyibizi, D.O., is the recipient of its 2023 Humaneness in Medicine Award, which is given annually to one or more Lehigh County medical residents or fellows who have best displayed the ideals of outstanding compassion in the delivery of care, respect for patients, their families, and health care colleagues, as well as demonstrated clinical excellence.
Dr. Niyibizi is a chief resident in the family medicine residency at St. Luke’s Hospital. He also is the director of clinical operations at the student-led Interprofessional Care Center located in Allentown. Dr. Niyibizi was deeply involved with the formation, development and on-going staffing of the free healthcare clinic that offers comprehensive services to marginalized communities. His patients have embraced his approach, giving him a strong following.
Described as innovative, caring, compassionate and a leader, Dr. Niyibizi is known to deeply care for patients, and care for their whole person, not just a specific ailment. He often is found advocating for his patients with social workers, who can sometimes find additional support services for their often complex needs. Also known for his leadership, he is active in St. Luke’s Resident Organization, the network of Black physicians, and was elected by his peers as a chief resident for the current academic year.
LCMS is proud to have Dr. Niyibizi as the recipient of this important award.
Located in Allentown, PA, LCMS represents physicians of all specialties on local issues. In coordination with the Pennsylvania Medical Society, LCMS also works to address health issues at the state capitol.


MICHELLE CARRARO, D.O., F.A.C.E.P.
Ibelieve communication is the key component in any relationship, especially the patient-provider relationship. I had the wonderful opportunity to refine my communication skills to become a more effective and more efficient communicator. I am a facilitator in a program called the relationship-centered communication program at Lehigh Valley Health Network.
Continued on page 14
This workshop has not only enriched my relationships with my patients, but also with my co-workers, family, and friends.
This course has been shown to not only save providers time but also ensure better control and more effective management of chronic conditions such as hypertension and diabetes. In addition, the more a provider is able to effectively communicate and show empathy, the more patients have relayed improved pain control. The goal of the program is to have all colleagues attend this course to not only enrich the relationships between providers and patients, but also amongst colleagues. This course also improves team collaboration and reduces burnout. Improved communication has been shown to reduce medical error and enhance trust within patients. I feel due to this course not only are my patients and co-workers more satisfied and happier, but myself as well. Despite an increasingly busy emergency department, I find myself finishing my charts daily, having to be called back into rooms less, and overall extremely happy with
my career. I believe this is largely due to the tools in this program.
Several colleagues and I have gone through more than sixty hours of training to facilitate this workshop. In addition, multiple other colleagues are certified to provide individualized coaching sessions after a colleague experiences a session. This session is a requirement and provides CME and an additional monetary bonus for completing the course. Each session lasts about 7 hours and includes lectures and small group activities. The course is broken down into 3 sections for an encounter: the beginning, relationship-centered, and ending. The beginning focuses on creating rapport, eliciting the list of the patient’s issues, and negotiating the agenda. The relationship-centered section focuses on opening the conversation, exploring the personal story and naming emotions, and responding with empathy. The ending focuses on how to share information in an ART (Ask, Respond, Tell) format, ask for Teach-Back, and intentionally close a visit. After the course, a 1:1 coaching
session is set up where a coach follows the provider during 2-3 patient encounters and gives live positive feedback on how the skills are being applied.
For me, this course allowed me to be more organized and thoughtful about my communication. Many of these recommendations we do every day, but this course allows you to be more mindful and intentional with them. For example, the initial greeting of a patient and everyone in the room is the first valuable impression. Taking a few seconds to ensure comfort with a blanket or turning the lights down displays care and engages trust. Creating a rapport with a patient, even if it’s a few seconds of complimenting their nails, goes a long way to make a patient feel comfortable. In addition, sitting down and noting interruptions may occur but ensuring you will give the patient your undivided attention immediately afterwards shows you are “in the moment.” Addressing any communication barriers is vital for the experience. Offering an interpreter, turning down the TV, or closing
the door all are examples to ensure the best environment.
In this course, we are encouraged to obtain the entire list of problems that a patient has. While this may seem like the list will go on forever, most patients truly do not have more than a few items they are concerned about. I have found keeping this open communication allows patients to verbally express their concerns and makes patients feel more at ease. While I may not be able to address all of their concerns during one emergency department visit, we can discuss and negotiate a plan for the visit and ensure follow up where needed. For example, a patient may be concerned about their chronic knee pain, but I am more concerned about their extremely elevated blood sugar. This course gave me the tools to negotiate the visit to address their top ailment while addressing my top concern for the patient. And while I may not be able to cure their chronic knee pain, perhaps I can give some relief and close follow up. In addition, ensuring an open dialogue and obtaining this list has saved me many times. For example, asking a patient “what else?” invited a patient’s wife to relay he has been complaining of headaches and his personality was off. These additional “list items” allowed me to ultimately diagnosis a patient with a brain mass who was otherwise there just for an upper respiratory infection.
Empathy is another aspect I have learned to enhance and is a key component in any patient-provider interaction. There are many ways to show empathy during a visit from beginning to end. There are facial, verbal, and even physical gestures such as a hand on a shoulder, which truly enhances the patient’s experience and again ensures trust. Many colleagues ask how we can show empathy during a critical situation such as a stroke alert. There are always a few seconds to place a hand on the patient’s shoulder or give verbal reassurance. For example, I say often “A lot will happen in the next few minutes but we are all here for you and will take great care of you!”
This course has been show to not only save providers time but also ensure better control and more effective management of chronic conditions such as hypertension and diabetes.
While we purposefully start a patient encounter, it is recommended to purposefully close the encounter. One method is through something called ART Loops (Ask, Respond, Tell). While this may take me a few extra minutes, it ultimately saves time in the end with decreased calls or return visits to the emergency department. And there have been many times where I “ask a question” to start the conversation at the end of the visit and the patient knows everything about the diagnosis, treatment, and follow up which actually saves me time!
In addition, the teach-back method allows myself to visualize areas where I may not have communicated an important detail and ensures true understanding of a diagnosis, plan, and follow up. For example, an important detail about directions for a certain medication may have been missed on my part when the patient relays the plan back through the teach-back method.
Overall this course not only enriches and allows more effective, empathetic communication between patients and colleagues, but also enhances relationships between colleagues and I am grateful that I had this extra training.
ADAM GARBER, EXECUTIVE DIRECTOR OF CEASEFIREPA EDUCATION FUND
It was November of 2018. In response to a new position paper by the American College of Physicians outlining a public health approach to preventing firearm deaths and injuries, the National Rifle Association scolded doctors to “stay in their lane.”
Maybe you remember what happened next.
An outpouring of frustration and exhaustion from physicians made clear that “this is our lane.” They started a movement that continues to grow five years later.
The toll of gun violence on our society is staggering. But as a healthcare provider, you see the impact much more up-close than most.
The emergency physician stabilizing a gunshot victim who’s about to bleed out. The surgeon sewing up a bullet wound. The psychiatrist tending to the mental trauma of a non-fatal shooting victim. The pediatrician counseling gun-owning parents about secure storage. The physiatrist rehabilitating a patient who lost the ability to walk.
Or the perfectly understandable, ever-present fear of workplace violence – already acute in healthcare settings – worsened by the growing ubiquity of firearms. Like the retaliatory incident last summer where over 50 shots were fired at three people standing directly in front of Temple University Hospital’s ER. You could hardly be blamed for wondering: “Could I end up being a gunshot wound patient myself?”
This epidemic is personal to you and the patients you are dedicated to healing. This is your lane.

And you also have a unique level of credibility and trust that makes your voice especially powerful in the public discussion about how we can drive down the incidence of gun violence and make our communities safer and healthier.
That’s why CeaseFirePA Education Fund, the Commonwealth’s leading gun violence prevention organization, is partnering with medical professional organizations, hospitals, and public health institutions across Pennsylvania to foster a space where healthcare providers can come together to educate the public and policymakers, and advocate for systemic change through a public health lens. We’re helping to lay the foundation and chart the course for “your lane” to lead to tangible changes in the public’s understanding of the gun violence crisis, and concrete reforms in Harrisburg that save lives and mitigate harm.
Gun violence is a public health crisis. We hear that said all the time. But what does it really mean?
It’s simple: we should use an empirical approach to understanding the drivers of firearm injury and death at a population-level, and then marshal the best evidence available to design and enact systemic, upstream reforms that address these causes and prevent harm and mortality.
And the harm is massive and widespread.
Gun violence took the lives of more than 1,900 Pennsylvanians in 2022, the latest year for which complete data is available. Another 3,500 survived a gunshot, but suffer physical, psychological, and emotional trauma. For context, this level of death and injury is
roughly equivalent to the number of people who die from kidney disease and flu/pneumonia combined each year in Pennsylvania.
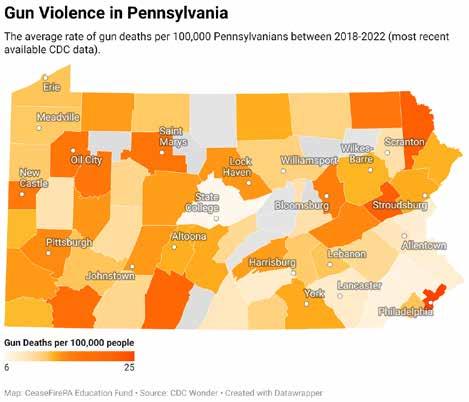
No part of our Commonwealth is left unscathed.
Contrary to popular understanding, the majority of gun deaths in Pennsylvania are suicides. This “silent killer” (compared to the high-profile nature of other gun deaths) disproportionately impacts rural counties, which on average have a 37% higher firearm death rate than urban counties.
The toll of firearm suicide also has a disproportionate impact on rural children, who are four times more likely to die by gun suicide compared to children in urban areas.
More broadly, gun violence poses a direct threat to the health and wellbeing of kids everywhere. In 2020, firearms became the top cause of death for children and teenagers in the United States, overtaking car accidents, according to the American Academy of Pediatrics. This is especially visible in unintentional shootings, which every year kill one-two dozen Pennsylanians – often
children who access unsecured weapons that are improperly stored by irresponsible gun-owning adults.
And of course, community-based gun violence ravages Pennsylvania’s cities, with the impact concentrated among Black and Brown communities. Due to a confluence of social determinants of health, Black Pennsylvanians are 21 times more likely to be killed with a gun than white Pennsylvanians. Every shooting has second-order effects: children living near a shooting are twice as likely to visit an Emergency Room for mental health concerns.
Over 800 Pennsylvanians of all ages and backgrounds died from this type of community-based gun violence in 2022. And while 2023 did bring a 21% reduction in Philadelphia’s gun homicides, the impact on public health is still far too severe.
Mass shootings, while statistically much less common than community-based violence or gun suicide, are an especially visceral symbol of the constant feeling of unease that Pennsylvanians have now sadly become enured to. The recent shooting at a SEPTA
bus stop that injured eight has reignited fears that violence can hit anywhere, at any time. Pennsylvania averages roughly 10 mass shootings per year, defining mass shootings as four or more people injured or killed, not including the shooter. The inability to go to the store or send your kids to school without the nagging fear of mass violence is an indication that health and safety systems are not working.
And finally, domestic violence is a threat in every community across Pennsylvania, made significantly worse by the presence of firearms. The cause of death in 67% of domestic violence fatalities in Pennsylvania is a firearm. Abusers are five times more likely to kill their partner if they have access to a gun.
This bleak picture adds up to a Pennsylvanian being shot every two hours, on average.
While of course this is a human tragedy –one that physicians are left on the front-lines to address – it’s also an enormous financial burden on the healthcare system. One study found $1.57 billion in annual hospital costs alone from gun violence, which is likely an undercount that does not include physician and other costs. This is money spent treating the symptoms of a crisis that could surely be better used to improve health and wellbeing if we can address the root cause of gun violence: unfettered access to deadly weapons.

Dr. Arvind Venkat, an Emergency Physician and now a first-term State Representative, speaks on the front steps of the State Capitol at CeaseFirePA’s 2023 “March For Our Lives: PA Advocacy Day.” Photo Credit: Michael Mason
And you have a uniquely powerful ability to help do just that.
The credibility and trust that your white coat, blue scrubs, and medical expertise affords you gives your voice a heightened impact when it comes to shifting the perspective of the public and decisionmakers, and mobilizing others to push for systemic change.
As a physician, you have a powerful opportunity to serve your patients in a new way, outside of a medical setting, to advocate for an environment that is more conducive to their health and safety, and that would free up the healthcare system to focus on other pressing public health issues. One might even argue that given your Hippocratic Oath to “improve the public health,” you have an obligation to get involved, even in a small way.
CeaseFirePA invites you to join us in this work, with two easy actions you can take:
1. Sign-up to join the “This is Our Lane” public health gun violence prevention coalition, a statewide network we’re building to give doctors, nurses, and other medical professionals opportunities to speak out for policy change.
2. Attend “End Gun Violence: PA Advocacy Day” in Harrisburg on Tuesday, May 7, 2024. Stand with us and dozens of other healthcare professionals for a rally at the State Capitol and engage state lawmakers on pending legislation.
The evidence is clear that states with stronger gun laws have less gun violence. And the good news is that research shows there are a number of effective policy prescriptions immediately available.
Among the many policies for which CeaseFirePA advocates, four core priorities form our Common Agenda to End Gun Violence:
1. Safe Storage to require that firearm owners secure their firearms when not in use. This has been shown to prevent

school shootings, unintentional shootings, and suicides, especially by preventing children from accessing weapons.
2. Lost and Stolen Gun Reporting to prevent firearms from being illegally trafficked into communities for use in community violence.
3. Extreme Risk Protection Orders (ERPOs) to provide family members and law enforcement a tool to temporarily restrict access to firearms to prevent firearm suicides, mass shootings, and domestic violence killings.
4. Closing the loophole in PA’s background check system and enacting universal background checks will prevent violent felons and other dangerous individuals from accessing long guns including military-style, semi-automatic rifles.
One of the first things learned in medical school, nursing school, or other public health institutions, is that preventing disease and harm is better for the individual – and often cheaper – than reacting after the fact to treat the symptoms and injuries.
These policies are society-wide preventative care. And working together, we can get them passed into state law, and save lives.
About the Author: Adam Garber is the Executive Director of CeaseFirePA Education Fund and lives in Philadelphia. CeaseFirePA’s mission is to organize with communities closest to the issue of gun violence, hold those in power accountable, and maximize the strengths of every member in its broad coalition — understanding that the strongest work is work done by many. Learn more at CeaseFirePA.org.
This article was originally published in the Spring 2024 edition of Philadelphia Medicine magazine. It has been updated.


JESSY FOSTER, DEPUTY DIRECTOR OF POLICY AND PARTNERSHIPS PENNSYLVANIA HEALTH ACCESS NETWORK

Medical debt is not rare. A trip to the emergency room for a car accident or medical crisis, a planned surgery, or even the birth of a child can mean hundreds to thousands in unexpected medical bills that most Pennsylvanians simply can’t afford to pay, leading to widespread medical debt. Moreover, medical debt can present in ways beyond a hospital collections bill. According to a 2023 study by Altarum1, 1 in 3 Pennsylvanians are struggling to pay their medical bills, reporting that they were reported to a collections agency (15%), used up all or most of their savings (11%), had to sacrifice paying for basic necessities like food, heat or housing (11%), racked up large amounts of credit card debt (9%), borrowed money, took out a loan, or got another mortgage on their house (8%), or were placed on a payment plan (7%).
According to the same study, 1 in 4 reported having bills that are overdue (i.e. they are in medical debt). Since 2015, the costs of seeking hospital-based care have increased as much as 31% nationally, growing more than four times faster than most workers’ paychecks2. A Kaiser Family Foundation report3 found that 1 in 7 people with medical debt said they’ve been denied access to a hospital, doctor, or other provider because of unpaid bills.
This means the levels of medical debt are very high, and many who aren’t in debt are
achieving that by forgoing basic necessities, taking out loans or second mortgages, or using up their savings. At the Pennsylvania Health Access Network (PHAN), we have been talking with people from across the state over the last year about their experiences accessing healthcare, and how medical debt has impacted them. Through petitions, surveys, focus groups, and one-on-one conversations, many Pennsylvanians shared with us examples of the financial and health impacts on their lives.
Seniors shared that because of a medical expense in years prior, their retirement savings were wiped out, forcing them to continue working despite their age and declining health. Other families noted that even though they are insured, high deductible plans with high copays mean they are still left to shoulder most of the bill, meaning thousands in out-of-pocket costs. Patients are forced to choose whether or not to pursue recommended care, some sharing how they put off care for years out of fear they would get a medical bill they could not afford, and now face the long-term impacts to their health and well-being as conditions have deteriorated. Despite the availability of financial assistance programs directly from hospitals, few patients report any knowledge about these programs. Often, patients are instead referred to long-term payment plans, that do not take into account limited fixed incomes or ongoing health needs. Lack of
information about resources was even greater among immigrant and limited-English-proficient communities.
In September, PHAN joined national partners for a Day of Action in Washington, DC where patients shared their personal stories directly with members of the Biden Administration. Shortly after, we have seen federal policymakers begin to take action. The Biden Administration announced support for the Consumer Financial Protection Bureau, which has launched a new rulemaking process to prevent medical debt from impacting credit scores4. Their proposal would help remove medical bills from consumers’ credit reports, stop creditors from relying on medical bills for underwriting decisions, and stop coercive collection practices.
While this is a great first step, we continue to push for state level measures. Medical debt can be prevented before a patient ever receives a medical bill, and the programs to prevent medical debt already exist. The vast majority (91%) of Pennsylvania hospitals are tax-exempt, and therefore required by law to create and publicize financial assistance programs that provide free or discounted care to eligible patients. Yet, many patients are not aware of these programs, meaning that the bills they receive for medical care do
Continued on page 20

not reflect the discounts they should receive. HB78 would provide relief and reduce predatory practices by collection agencies for Pennsylvanians already experiencing medical debt. More importantly, it will prevent medical debt altogether by
• Creating a single, uniform application for financial assistance
• Screening more people for eligibility for health coverage
• Providing information about available financial assistance and coverage in an easy to understand format
• Requiring clear, direct notices right on bills that assistance is available
HB78 passed the PA House twice on a bipartisan basis, once as a standalone bill and once as part of the fiscal code bill, HB1300.
At the time this article is being written, we are disappointed to say the language was not included in the budget code bill passed by the Senate, but the fight does not stop here. We will continue to advocate for these common-sense patient protections through the stand-alone version of the bill and the governor’s budget address in the new year. We continue to hear from Pennsylvanians about their experiences and will seek to monitor enforcement and additional patient protections.
PHAN has created a petition for physicians and healthcare providers to sign on to show support for action on medical debt and share anecdotes about how they have seen medical debt impact their patients’ lives, to show policymakers the need for meaningful change: https:// pahealth.salsalabs.org/hb78providersignon. If you have questions or want to get involved in PHAN’s work to prevent medical debt, reach out to jessica@pahealthaccess.org.
1 Altarum Healthcare Value Hub: Pennsylvania Survey Respondents Struggle to Afford High Health Care Costs; Worry about Affording Health Care in the Future; Support Government Action Across Party Lines
2 Families USA: Bleeding Americans Dry: The Role of Big Hospital Corporations in Driving Our Nation’s Health Care Affordability and Quality Crisis
3 Kaiser Family Foundation: Health Care Debt In the US: The Broad Consequences of Medical and Dental Bills
4 Consumer Finance Protection Bureau: CFPB Kicks Off Rulemaking to Remove Medical Bills from Credit Reports
This article was originally published in the Spring 2024 edition of Philadelphia Medicine magazine. It has been updated.

In February, a group of ten Pennsylvania Medical Society (PAMED) members attended the AMA’s National Advocacy Conference in Washington, D.C. This year the PAMED physicians had meetings with legislators or staff from 14 offices of the PA congressional delegation, including Congressman Dan Meuser and Congressman Glenn Thompson. Among the issues and legislation discussed was the critical need to reverse the Medicare physician payment cuts that took effect on Jan. 1, 2024, and the importance of increasing the number of graduate medical education training slots.
Continued on page 22

As part of the National Advocacy Conference, PAMED Board Member Michael Suk, MD, led a panel discussion about the impact of Medicare cuts to rural health care. As part of the panel, Dr. Suk was joined by PAMED Board Vice Chair Lorraine Rosamilia, MD, who demonstrated the need for Medicare reform to ensure that those in rural settings can continue to receive important care in their communities.
In Pennsylvania, PAMED participated in a hearing on challenges surrounding rural health care for the Senate Majority Policy Committee and a joint hearing with the House Professional Licensure Committee and the House Health Committee on improving access to health care. Former PAMED Board of Trustee David Csikos, MD, was among the panel to testify on challenges to rural health care.
With the legislature quiet the beginning of this year, the PAMED Government Relations team was on the move, visiting different districts in Pennsylvania. They were recently part of a legislative forum held by the Lycoming County Medical Society with Senator Yaw, Rep. Jamie Flick and Rep. Joe Hamm. There they discussed legislation on noncompete agreements and POLST.
PAMED has seen notable movement on three key issues:
Amending Medical Practice Act (Senate Bill 559 & Senate Bill 560) – On March 18, the PA Senate passed Senate Bill 559 and Senate Bill 560 to amend the Medical Practice Act and the Osteopathic Medical Practice Act regarding athletic trainers. The legislation would allow athletic trainers to perform certain specified procedures with the direction of a licensed physician and pursuant to a written protocol.
The bills would also amend the definition of a “physically active person” to include anyone that participates in an individual or team sport, an athletic competition, a performing art, a recreational activity, or a military exercise. The bills have now been referred to the House Professional Licensure Committee for consideration in the House.
Telemedicine Service Insurance Coverage (House Bill 1512) – On March 25, the PA House Insurance Committee considered House Bill 1512, legislation which would require health insurers to cover and pay for health care services provided via telemedicine. Unfortunately, the legislation does not address the issue in a comprehensive manner and only covers the insurance question.
PAMED has been engaged in negotiations over several legislative sessions regarding telemedicine and fully supports Senate Bill 739, a more comprehensive telemedicine bill currently waiting consideration in the Senate Appropriations Committee.
PAMED informed the House Insurance Committee that it supports moving House Bill 1512 forward in the legislative process to continue momentum on this issue, but we continue to press for an amendment
encompassing the already-negotiated comprehensive provisions contained in Senate Bill 739.
(House Bill 1633) – On March 27, the PA House Health Committee overwhelmingly approved House Bill 1633, legislation which would prohibit all non-compete agreements in employment contracts for health care practitioners. PAMED supports significantly restricting the geographic reach and duration of a hospital or health system’s non-compete agreements, but we also believe legislation on this issue needs to recognize the needs and concerns of small independent physician practices that require protection against predatory poaching of established community physicians.
PAMED is working with the prime sponsor and Committee Chairman to develop an acceptable amendment that balances these concerns. We have communicated to the Committee we support moving House Bill 1633 forward in the legislative process as we continue our negotiations on final language.
This year is an election year! To see a full list of important dates for the 2024 Pennsylvania elections, visit vote.pa.gov/About-Elections/Pages/Upcoming-Elections.aspx.
PAMED members are encouraged to meet with and develop relationships with their local state representatives and state senators. Building these relationships helps PAMED achieve the legislative goals for physicians and patient care.
Contributions can be made here: pamedsoc.org/laws-advocacy/PAMPAC.
For more information about any of the items mentioned above, please visit the Advocacy Section of PAMED’s web site at www.pamedsoc.org/advocacy

SUMMER NEW AND RE-INSTATED MEMBERS APPLICATIONS RECEIVED FOR REINSTATEMENT:
Thomas J. Amadio, DO Resident - Emergency Medicine
Joseph C. Bognet, DO Family Medicine
Arthur David Hoffman, MD Internal Medicine
Firas Ido, MD
Pulmonary & Critical Care Medicine (Internal Medicine)
Courtney Janowski,MD
Resident - General Surgery
Yaman Mo'ath Husni Jarrar, MD
Resident - Internal Medicine
Jay M. Kadhiwala, MD, MBA
Resident - Family Practice
Sierra Marie Kirsch, DO Resident - Emergency Medicine
Daniel K. Meyer, MD Internal Medicine
Tarannum Tuhin Mohammadi, MD Resident – Neurology
Rakin Muhtadi, MD Resident - Emergency Medicine
Connor Murphy, DO Resident - Emergency Medicine
John Sagrati, DO Resident - Pathology
Christopher P. Wayock MD - Obstetrics/Gynecology
Maria Cristina Erazo, MD Internal Medicine
Neil H. Feldman, DO Allergy and Immunology
Mal R. Homan, MD
Endocrinology, Diabetes & Metabolism (Internal Medicine)
Jason Edward Kaplan, DO Cardiovascular Disease (Internal Medicine)
Thomas E. Leet, MD
Pediatric Radiology (Radiology-Diagnostic)
Pratik Mayank Parikh, DO Emergency Medicine
Anthony Rainey, MD
Neuromuscular Medicine (Neurology)
Haseeb Siddique, MD Internal Medicine
When you have the best employees in the country, it is easy to become a Top Workplace
We are #StLukesProud to be recognized ONCE AGAIN as a Top Workplace health care organization locally, regionally, and nationally.
Our employees deserve this recognition as our most valued asset. As an employer of choice, St. Luke’s prioritizes the health and well-being of our employees so they are able to provide the highest quality care and services to our patients. This honor highlights St. Luke’s as an employer who listens to, cares for, and supports its employees.