NALOXONE VENDING MACHINES
COACHING UNCOMMON
EMERGENCY CARE
PAMED LEGISLATIVE UPDATES


NALOXONE VENDING MACHINES
COACHING UNCOMMON
EMERGENCY CARE
PAMED LEGISLATIVE UPDATES


The Surgery Center of Allentown is a state-of-the-art ambulatory surgery center providing low-cost services and high-quality care since 2007.
Our services include: Colon and Rectal I Ear Nose and Throat I Opthalmology Orthopedics I Hand Now Offering Robotic Joint Replacement Surgery Sports Medicine I Pain Management I Plastic Surgery I Podiatry I Spine
Our board certified physicians are committed to providing the highest level of personal care in a safe and comfortable environment.




















We accept most major insurance plans, including Workers Compensation and High Deductible Health Plans.
To learn more about our surgery center and specialty physicians visit SCOAllentown.com or call 484.268.5232.
a 2024-2025 Best Ambulatory Surgery Center by U.S. News & World Report "Orthopedics & Spine"

Carol C. Dorey Real Estate, Inc.
Bucks County / Lehigh Valley, PA www.doreyrealestate.com / (610) 346-8800




A rare and beautiful example of a barn renovation, with re-imagined vaulted spaces blended with stunning new architectural details, sequestered on 90 acres. Offered for $4,500,000

Polished, with understated notes of elegant and luxurious, this custom crafted Tudor home & vineyard set on 55 acres is a master class in creating the perfect blend. Offered for $3,950,000
One of only a handful of Saucon Valley’s legacy properties, the house and grounds have been proudly cared for & recently updated with a stunning addition. Offered for $4,250,000

Renovated in 2021 and set on 3 private acres with views over pristine Cooks Creek, this stunning villa is a rare blend of 19th century touches & outstanding modern luxuries. Offered for $1,999,000


A verdant 2+ acre parcel in Bucks County is the setting for this stone home and Pennsylvania bank barn. 4 beds, 3 baths in the main house; finished barn offers 1.5 baths. Offered for $1,550,000
A private lane in peaceful Bridgeton Township is the setting for this lovingly cared for colonial surrounded by more than 10 acres of mature woodland Offered for $1,199,000


Augusta Manor
Brimming with natural light, Augusta Manor stands proudly on almost 2 acres in a picturesque neighborhood of custom-built homes, with 3,650 finished sq ft over 3 floors. Offered for $1,199,000

Kindred Knoll

Open fields & long-distance views comprise an extraordinary 22 acre setting for this midcentury ranch. Peaceful and rural, the property includes a pool & detached garage. Offered for $875,000

LEHIGH COUNTY MEDICAL SOCIETY
P.O. Box 8, East Texas, PA 18046 610-437-2288 | lcmedsoc.org
2024 LCMS BOARD OF DIRECTORS* Chaminie Wheeler, DO President
Kimberly Fugok, DO President Elect
Mary Stock, MD Vice President
Oscar A. Morffi, MD Treasurer
Charles J. Scagliotti, MD, FACS Secretary
Rajender S. Totlani, MD Immediate Past President
*effective February 1, 2024 - for two-year terms
CENSORS
Howard E. Hudson, Jr., MD
Edward F. Guarino, MD Gregory Wheeler, DO
TRUSTEES
Wayne E. Dubov, MD
Kenneth J. Toff, DO Alissa Romano, DO
EDITOR
David Griffiths Executive Officer


Welcome to the Winter edition of Lehigh County Health & Medicine. We hope you enjoy the many articles we have curated for you on topics ranging from Naloxone Vending Machines to the 2024 Legislative Wrap-Up from PAMED, to some very useful information on tick-borne illness for the upcoming spring, plus much more. We have two pieces on Point‐of‐care ultrasound (POCUS). One piece describes POCUS for pediatrics, and the other is a physician’s view from the ER and his experiences working with POCUS as well as coaching it.
With milder winters, we’re seeing insects become more prevalent. In the article Recognition, Diagnosis, and Treatment of Lyme Disease and Other Tick-borne Pathogens, physicians and other health care workers can learn more about this topic and be prepared for spring. We also hope to hold a CME on this topic.
Many families in Pennsylvania have been affected by the fact that 14 people die every day from an overdose. The City of Allentown’s Substance Use Task Force has been working tirelessly to address the opioid crisis. Learn more in the article Naloxone Vending Machines.
Are you getting sufficient information about how what is going on in Harrisburg is affecting medicine? Please read the 2024 Legislative Wrap-Up to learn more about such topics as Scope of Practice, Telemedicine, and Non-Competes.
Additionally, on the above topics, please join us on March 20th, 2025, to explore the Lehigh County Medical Society (LCMS) and the Pennsylvania Medical Society (PAMED). Discover why your participation is crucial for both you and your patients. We will delve into our legislative initiatives targeting key issues like scope of practice, venue shopping, and restrictive covenants. These challenges are pivotal in today’s healthcare environment, essential for safeguarding the integrity of our profession and the well-being of our patients.
We hope that you enjoy the magazine and find it both educational and relevant to your interests. If you are interested in back issues, or just want to read Lehigh County Health & Medicine online, please visit our website at https://lcmedsoc.org/our-publication. Thank you for reading.

BETH LOVE, OPIOID PREVENTION MANAGER ALLENTOWN HEALTH BUREAU
In the United States, over 720,000 people have lost their lives to overdose since 1999, when the opioid epidemic began. What started with increased prescriptions for pain management, rapidly accelerated illicit use following the expansion of the heroin and later fentanyl markets. Americans, already addicted to prescription medication, found themselves turning to harder, less regulated medication to cope with their addiction. According to the National Library of Medicine, in one study, about 80 percent of current heroin users reported that they began with prescription opioids. Therefore, the public health effects of prescription opioids and heroin (now fentanyl) are intertwined.
In Pennsylvania alone, 14 people die every day from an overdose – or one every 1.7 hours. Nationwide, 81,806 people died from prescription and illicit opioid overdoses in 2022, up from just over 21,000 in 2010.
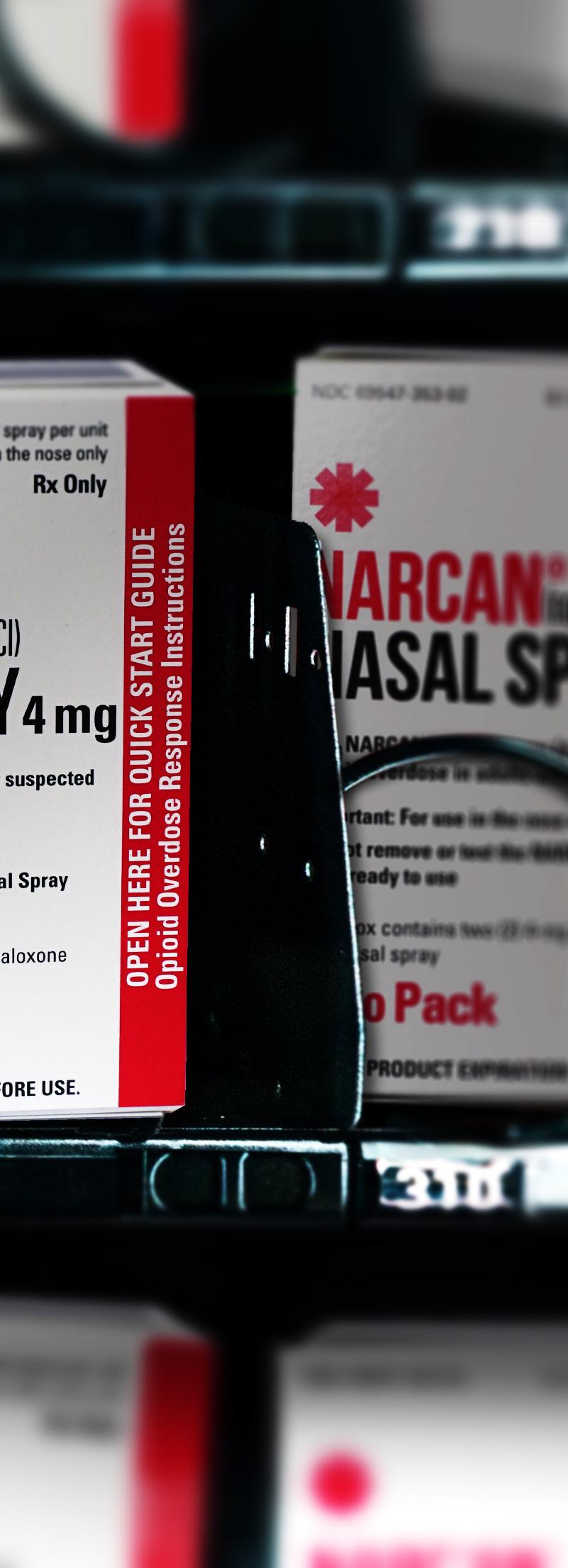
In an attempt to reverse the increase in overdoses, public health vending machines dispensing naloxone (brand name Narcan) were first introduced in Puerto Rico in 2009 and in the continental United States in 2017. Naloxone is a medication used to reverse or reduce the effects of opioids. In an acute opioid overdose, high levels of opioids affect the parts of the brain that regulate breathing. This respiratory depression leads to low oxygen levels (hypoxia) resulting in anoxic brain injury and eventually death.
Naloxone competes with opioids for the same receptors, reversing the depression on the brain and respiratory system. It’s the most efficient way to save people’s lives during an overdose occurrence, making fast access to this medication a necessity. Naloxone vending machines present a convenient and effective way to improve the use of naloxone by non-medical personnel dealing with an overdose emergency. There is no medical training needed to administer naloxone.
Vending machines for harm reduction have been successfully implemented in Australia, Taiwan, Mexico, Canada and several other nations as well as the United States. In one example from Hamilton County, OH, the introduction of 24/7 naloxone-filled vending machines led to a 10% decrease in overdose deaths in 2021, compared to a 15% rise nationally.
In response to opioid overdose deaths, these vending machines are appearing across Pennsylvania, including Philadelphia, Pittsburgh and Harrisburg. Often, these machines are located in emergency department lobbies, local libraries, and YMCAs. This strategy enhances public outreach, providing 24/7 access to life saving medication for people with substance use disorders or those who inadvertently encounter or consume opioids whether obtained illegally or through prescriptions.
In 2023, state and local governments received approximately $1.5 billion in settlement funds from companies that manufactured, sold, or distributed prescription painkillers, due to their role in fueling the opioid crisis. This money offers a lifeline to cities and counties battling addiction and overdose. In the city of Allentown, part of the opioid settlement fund is going towards the purchase of two vending
Ending this stigmatization is part of the push towards ending the opioid crisis – and that starts with better access to life saving medications. Every person is a valued member of our community, whose life matters – be it your child, spouse, co-worker or neighbor.

machines dispensing naloxone along with other public health supplies. Participants can discretely input their PIN (usually their zip code) and receive supplies along with information about local resources free of charge. It’s hoped that the increased anonymity and free access will reduce overdose deaths, improve availability and achieve overall acceptance of these machines.
The City of Allentown’s Substance Use Task Force has worked diligently to combat the opioid crisis. Its primary focus is to decrease the dangers of overdose and overdose fatalities. Effective strategies include raising awareness through education, stakeholder involvement, and community connection. Stigma remains a major factor preventing people from seeking help. Individuals who may have begun with a prescription medication before turning to illicit opioids or who unintentionally became addicted may fear the label “drug addict” with all the social repercussions that come with it. As one study demonstrated, stigmatizing attitudes change depending on whether a person received the opioids from a friend as opposed to a doctor, despite both situations ending with equal outcome. Ending this stigmatization is part of the push towards ending the opioid crisis – and that starts with better access to life saving medications. Every person is a valued member of our community, whose life matters – be it your child, spouse, co-worker or neighbor.
According to the National Institute on Drug Abuse, Substance Use Disorders are chronic but treatable medical conditions. Yet, the discrimination and stigma that people face can further deepen the challenges to arrest addiction. People feel more alienated, alone, and without hope, fueling addictive behavior. It is often one of the main reasons why they don’t seek care.
Carla Sofronski, executive director of the Pennsylvania Harm Reduction Network, argues, “Some still perceive harm reduction as a means of enabling drug use. Rather than endorsing drug use, it offers critical interventions aimed at preserving life and lowering risk.” With more people dying of overdose, it could prove a much-needed lifeline for people in need of a second chance.
For more information about the city of Allentown’s initiatives addressing the opioid crisis, or if you have any questions regarding naloxone vending machines or are interested in hosting one at your business, please contact the Allentown Health Bureau’s Injury Prevention Program at 610-437-7760 or via email at injuryprevention@allentownpa.gov.
The 2023-2024 Pennsylvania Legislative Session began with the House Democrats taking a one-seat majority for the first time in over a decade. We also saw the election of Arvind Venkat, MD, the first physician elected to the State House since 1961.
2024 brought some consistency back to the Pennsylvania General Assembly’s 2023-2024 Session. While 2023 was fraught with resignations, special elections, and the constant question of who held the majority in the State House, 2024 saw more legislative functioning than what we saw in the year before.

This year PAMED saw movement on legislative proposals that impacted medicine, including bills that PAMED had as legislative priorities. These include, but are not necessarily limited, to the following in no order:
One area to highlight is PAMED’s continued vigorous opposition to bills that would expand the scope of practice to non-physician providers throughout the Commonwealth. Senate Bill 25 (Bartolotta) and House Bill 1825 (Guenst), bills that would allow for the independent practice of Nurse Practitioners, were both reintroduced. At the time of this writing Senate Bill 25 passed out of the Senate Consumer Affairs and Professional Licensure Committee and is awaiting final consideration from the PA Senate, while HB 1825 has received no action. HB 2037 (Bullock) was introduced, which would allow pharmacists to vaccinate children down to the age of three, and we expect a Senate companion bill to be introduced in the near future. We have also seen a push to allow psychologists to prescribe medications in HB 1000 (Frankel), which we oppose. PAMED, and our physician specialty partners, will continue to advocate for physician-led team-based care.
The Pennsylvania Senate recently considered Senate Bill 739 (Vogel), legislation which would require health insurers to cover and pay for health care services provided via telemedicine. Senate Bill 739 passed the PA Senate with a vote of 49-1 and then passed the PA House with a vote of 194-8. The bill was then signed by Governor Shapiro.
Another advocacy priority for the Pennsylvania Medical Society
is Restrictive Covenant legislation. As directed by the PAMED House of Delegates, we continue to discuss the issue of noncompete agreements in physician contracts with a number of legislators. Interest in this area seems to be growing as lawmakers learn more about how these contractual agreements negatively impact patient access and continuity of care. Rep. Dan Frankel (D-Allegheny) previously introduced House Bill 1633, a proposal that would outright ban the use of non-compete agreements in all physician employment contracts.
On April 17th, the Pennsylvania House of Representatives passed House Bill 1633, by a vote of 150-50. The bill had previously passed out of the House Health Committee on March 27th with a vote of 21-4. The bill was amended in the Health Committee to include a rural exemption, which PAMED had previously agreed to in previous sessions. PAMED did pursue an amendment on the House floor, sponsored by Representative Torren Ecker, that would exempt private practices from the prohibition. The amendment did fail with a vote of 99-102. House Bill 1633 then passed both the House and Senate and in July was signed into law by Governor Shapiro. PAMED has been at the forefront of restrictive covenant legislation and supported HB 1633’s advancement.
While PAMED was supportive of House Bill 1633 advancing out of the Senate HHS Committee, we strongly expressed our concerns that the bill did not go far enough. The Senate Committee amended the bill to allow non-compete clauses when the length is no more than one year, and the physician is not dismissed by their employer. HB 1633 also provides for a patient to be notified should their provider leave the hospital, or health system, the physician is employed by. The final element of HB 1633 provides for a study to be conducted by the Pennsylvania Health Care Cost Containment Council, 3 years after this legislation takes effect.
AMY SLENKER, MD

Lyme disease is the most common vector-borne disease in the United States. Approximately 90% of all cases in the US are reported from fifteen high-incidence areas, including the state of Pennsylvania (1). As we head into the spring, it is important to be aware of the common clinical manifestations of Lyme disease and other tick-borne illnesses.
There are multiple species of ticks in Pennsylvania, including the black-legged tick (Ixodes scapularis), the American dog tick (Dermacentor variablis), and the Lone Star tick (Amblyomma Americanum). The black-legged tick is the vector of Borrelia burgdorferi, the pathogen that causes Lyme disease, and it may also transmit Anaplasma phagocytophilum (human granulocytic anaplasmosis), Babesia microti, and Powassan virus.
The black-legged tick has a 2-year life cycle and goes through three stages, larva, nymph, and adult. Infected nymphs will take a blood meal in the spring or summer and are the primary vector of Lyme disease. The nymphal ticks are highly effective at transmitting infection because they are small (<2 mm) and are more likely to go undetected for the required period to transmit infection (≥ 36 hours) as compared to an adult female (2). Adult females may also transmit infection and they may seek a blood meal during the colder months, thus accounting for scattered cases outside of the spring and summer months (3). The rate of Borrelia burgdorferi infection in the black-legged tick in Pennsylvania is reported to be as high as 47% in some studies (4).
The incubation period between the tick bite and the onset of infection is 1-2 weeks (range 3 to 30 days). Early localized disease is the first manifestation and usually presents with an erythema migrans (EM) rash which occurs in 80% of patients. Some patients may have associated fatigue, fever, headache, and myalgias (5). EM rashes occur at the site of the tick bite, are not painful, and are usually found in the groin, axilla, waist, back, or legs. Central clearing may develop slowly over days to weeks and the EM rash may rarely have a necrotic or vesicular center (6). Clinicians should have a heightened awareness of EM in a patient who presents with a circular rash in the spring or summer months.
Patients may go on to develop early disseminated disease which can manifest as multiple EM lesions, cranial nerve palsies (classically, a facial nerve palsy), lymphocytic meningitis, and carditis with heart block. Late Lyme disease may occur weeks to months later as an arthritis in up to 10% of untreated patients, and usually presents as a large joint monoarticular effusion (6-8).
Post-treatment Lyme disease syndrome (PTLDS) may develop in 5-15% of patients. Criteria for this syndrome include a prior history of treated Lyme disease with stabilization of the objective
manifestations of Lyme disease and the onset and persistence of fatigue, musculoskeletal pain, and cognitive difficulties for at least 6 months after completion of therapy (7).
A two-tier testing strategy is recommended by the CDC and is both sensitive and specific when used appropriately in patients with symptoms consistent with Lyme disease (7). This strategy typically starts with an enzyme-linked immunosorbent assay (ELISA) which detects the presence of Borrelia burgdorferi antibodies or antigens, followed by either a confirmatory Western blot or a second ELISA test with different targets. For patients with suspected Lyme arthritis, PCR testing of the synovial fluid may be helpful in addition to serologic testing. For patients with neurologic symptoms, such as meningitis or encephalitis, CSF studies should be considered in addition to serologic testing, and testing is usually guided by an Infectious Diseases specialist.
False-positive IgM testing is common (including on Western blot testing) and therefore, isolated IgM positivity is not sufficient to make a diagnosis of Lyme disease in patients with symptoms for greater than 4 weeks (9, 10). Testing is not recommended in patients who present with a single EM lesion due to the potential
continued on next page

for a false negative result early in infection (11). If the etiology of the skin lesion is not clear, testing may be performed, but a negative test result should be repeated in 2 weeks. Repeating serologic testing is generally not helpful in patients with prior Lyme disease, since antibodies to both IgM and IgG can persist for years which can make the diagnosis of reinfection challenging (12). Most experts do not recommend testing of ticks, since the results do not reliably predict clinical infection. Additionally, testing is not recommended in patients with non-specific symptoms such as fatigue, musculoskeletal pain, and headache due to the likelihood of a false positive result that will lead to unnecessary treatment (13).
Doxycycline is the treatment of choice for Lyme disease for nonpregnant adults and children > 8 years of age (7). Amoxicillin or cefuroxime are the preferred medications for pregnant persons. Amoxicillin is an acceptable choice in children < 8 years of age if there is no concern for neurologic involvement. If there is concern for neurologic involvement, the American Academy of Pediatrics supports the use of doxycycline for children < 8 years of age when administered for ≤ 21 days (14).
Several studies have shown that oral doxycycline is an excellent choice for neurologic and late Lyme disease (such as Lyme arthritis) (15). Symptomatic patients with carditis should be started on intravenous ceftriaxone but can be quickly transitioned to oral doxycycline once there is a response to therapy. For patients with PTLDS, there is no evidence that persistent symptoms represent ongoing infection, or that repeated or prolonged antibiotics provide any benefit to patients (16).
Patients with Lyme disease may be coinfected with other agents transmitted by the black-legged tick, such as Babesia microti or Anaplasma phagocytophilum (which causes human granulocytic anaplasmosis). The proportion of black-legged ticks coinfected with babesiosis or anaplasmosis in the United States range from 1 to 5% (17). Clinicians should maintain a high degree of suspicion for coinfection, particularly in patients with persistent symptoms or lab abnormalities such as anemia, leukopenia, thrombocytopenia, elevated bilirubin, or elevated transaminases (18, 19). Patients with suspected coinfection should undergo a work-up with a peripheral blood smear, Anaplasma blood polymerase chain reaction (PCR), and Babesia blood PCR testing. Acute and convalescent serologic testing has limited use in diagnosis but can be considered for confirmation of prior infection. Anaplasma phagocytophilum can be adequately treated with doxycycline for a 7-day course and Babesia infection should be treated with azithromycin plus atovaquone or clindamycin plus quinine for 7 to 10 days (18, 19).
PREVENTION OF TICK-BORNE ILLNESSES
Repellents that continue DEET (N,N-Diethyl-meta-toluamide) offer protection if applied to skin and clothing. Additionally,
permethrin is an effective deterrent that can be applied to clothing. When venturing into wooded or brushy areas, long-sleeved shirts and long pants should be worn and self-examination should be performed after spending time outdoors. If an embedded tick is encountered, it should be removed with fine tweezers by the head. Antibiotic prophylaxis with doxycycline can be considered for nonpregnant adults and children who have an Ixodes scapularis tick attached for an estimated ≥ 36 hours and when prophylaxis can be given within 72 hours of tick removal (20).
Dr. Slenker is the Chief of the Division of Infectious Diseases at Lehigh Valley Health Network and a passionate advocate for quality improvement, patient safety, and appropriate test utilization.
1. Kugeler KJ, Earley A, Mead PS, Hinckley AF. Surveillance for Lyme Disease After Implementation of a Revised Case Definition – Unites States, 2022. MMWR Morb Mortal Wkly Rep 2024;73:118-123. http://dx.doi.org/10.15585/mmwr.mm7306a1.
2. Hojgaard A, Eisen RJ, Piesman J. Transmission dynamics of Borrelia burgdorferi s.s during the key third day of feeding by nymphal Ixodes scapularis (Acari: Ixodidae). J Med Entomol. 2008 Jul;45(4):732-6. doi: 10.1603/0022-2585(2008)45[732:TDOBBS]2.0.CO;2. PMID: 18714875.
3. Piesman J, Schneider BS, Zeidner NS. Use of quantitative PCR to measure density of Borrelia burgdorferi in the midgut and salivary glands of feeding tick vectors. J Clin Microbiol. 2001 Nov;39(11):4145-8. doi: 10.1128/JCM.39.11.4145-4148.2001. PMID: 11682544; PMCID: PMC88501.
4. M. L. Hutchinson, M. D. Strohecker, T. W. Simmons, A. D. Kyle, M. W. Helwig, Prevalence Rates of Borrelia burgdorferi (Spirochaetales: Spirochaetaceae), Anaplasma phagocytophilum (Rickettsiales: Anaplasmataceae), and Babesia microti (Piroplasmida: Babesiidae) in Host-Seeking Ixodes scapularis(Acari: Ixodidae) from Pennsylvania, Journal of Medical Entomology, Volume 52, Issue 4, July 2015, Pages 693–698, https://doi.org/10.1093/jme/tjv037.
5. Nadelman RB, Nowakowski J, Forseter G, Goldberg NS, Bittker S, Cooper D, Aguero-Rosenfeld M, Wormser GP. The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. Am J Med. 1996 May;100(5):502-8. doi: 10.1016/s00029343(95)99915-9. PMID: 8644761.
6. Smith RP, Schoen RT, Rahn DW, Sikand VK, Nowakowski J, Parenti DL, Holman MS, Persing DH, Steere AC. Clinical characteristics and treatment outcome of early Lyme disease in patients with microbiologically confirmed erythema migrans. Ann Intern Med. 2002 Mar 19;136(6):421-8. doi: 10.7326/0003-4819-136-6200203190-00005. PMID: 11900494.
7. Lantos PM, Rumbaugh J, Bockenstedt LK, Falck-Ytter YT, AgueroRosenfeld ME, Auwaerter PG, Baldwin K, Bannuru RR, Belani KK, Bowie WR, Branda JA, Clifford DB, DiMario FJ, Halperin JJ, Krause PJ, Lavergne V, Liang MH, Meissner HC, Nigrovic LE,
Nocton JJJ, Osani MC, Pruitt AA, Rips J, Rosenfeld LE, Savoy ML, Sood SK, Steere AC, Strle F, Sundel R, Tsao J, Vaysbrot EE, Wormser GP, Zemel LS. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease. Clin Infect Dis. 2021 Jan 23;72(1):e1-e48. doi: 10.1093/cid/ciaa1215. PMID: 33417672.
8. Halperin JJ. Nervous system Lyme disease. Handb Clin Neurol. 2014;121:1473-83. doi: 10.1016/B978-0-7020-4088-7.00099-7. PMID: 24365431.
9. Branda JA, Steere AC. Laboratory Diagnosis of Lyme Borreliosis. Clin Microbiol Rev. 2021 Jan 27;34(2):e00018-19. doi: 10.1128/ CMR.00018-19. PMID: 33504503; PMCID: PMC7849240.
10. Seriburi V, Ndukwe N, Chang Z, Cox ME, Wormser GP. High frequency of false positive IgM immunoblots for Borrelia burgdorferi in clinical practice. Clin Microbiol Infect. 2012 Dec;18(12):123640. doi: 10.1111/j.1469-0691.2011.03749.x. Epub 2012 Feb 28. PMID: 22369185.
11. Moore A, Nelson C, Molins C, Mead P, Schriefer M. Current Guidelines, Common Clinical Pitfalls, and Future Directions for Laboratory Diagnosis of Lyme Disease, United States. Emerg Infect Dis. 2016 Jul;22(7):1169–77. doi: 10.3201/eid2207.151694. PMID: 27314832; PMCID: PMC4918152.
12. Kalish, RA, McHugh, G, Granquist, J, Shea, B, Ruthazer, R, Steere, AC. Persistence of immunoglobulin M or immunoglobulin G antibody responses to Borrelia burgdorferi 10-20 years after active Lyme disease. Clin Infect Dis 2001;33:780-785.
13. Markowicz M, Kivaranovic D, Stanek G. Testing patients with non-specific symptoms for antibodies against Borrelia burgdorferi sensu lato does not provide useful clinical information about their aetiology. Clin Microbiol Infect. 2015 Dec;21(12):1098-103. doi: 10.1016/j. cmi.2015.08.005. Epub 2015 Aug 29. PMID: 26321669.
14. Kimberlin, D. W., Brady, M. T., Jackson, M. A., Long, S. S., & American Academy of Pediatrics. (2021). Borrelia Infections other than Lyme disease. Red Book, 2024.
15. Ljøstad U, Skogvoll E, Eikeland R, Midgard R, Skarpaas T, Berg A, Mygland A. Oral doxycycline versus intravenous ceftriaxone
for European Lyme neuroborreliosis: a multicentre, non-inferiority, double-blind, randomised trial. Lancet Neurol. 2008 Aug;7(8):6905. doi: 10.1016/S1474-4422(08)70119-4. Epub 2008 Jun 21. Erratum in: Lancet Neurol. 2008 Aug;7(8):675. PMID: 18567539.
16. Krupp LB, Hyman LG, Grimson R, Coyle PK, Melville P, Ahnn S, Dattwyler R, Chandler B. Study and treatment of post Lyme disease (STOP-LD): a randomized double masked clinical trial. Neurology. 2003 Jun 24;60(12):1923-30. doi: 10.1212/01. wnl.0000071227.23769.9e. PMID: 12821734.
17. Hersh MH, Ostfeld RS, McHenry DJ, Tibbetts M, Brunner JL, et al. (2014) Co-Infection of Blacklegged Ticks with Babesia microti and Borrelia burgdorferi Is Higher than Expected and Acquired from Small Mammal Hosts. PLOS ONE 9(6): e99348. https://doi.org/10.1371/ journal.pone.0099348.
18. Biggs HM, Behravesh CB, Bradley KK, Dahlgren FS, Drexler NA, Dumler JS, Folk SM, Kato CY, Lash RR, Levin ML, Massung RF, Nadelman RB, Nicholson WL, Paddock CD, Pritt BS, Traeger MS. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis - United States. MMWR Recomm Rep. 2016 May 13;65(2):1-44. doi: 10.15585/mmwr.rr6502a1. PMID: 27172113.
19. Krause PJ, Auwaerter PG, Bannuru RR, Branda JA, Falck-Ytter YT, Lantos PM, Lavergne V, Meissner HC, Osani MC, Rips JG, Sood SK, Vannier E, Vaysbrot EE, Wormser GP. Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA): 2020 Guideline on Diagnosis and Management of Babesiosis. Clin Infect Dis. 2021 Jan 27;72(2):185-189. doi: 10.1093/cid/ciab050. PMID: 33501959.
20. Nadelman RB, Nowakowski J, Fish D, Falco RC, Freeman K, McKenna D, Welch P, Marcus R, Agüero-Rosenfeld ME, Dennis DT, Wormser GP; Tick Bite Study Group. Prophylaxis with singledose doxycycline for the prevention of Lyme disease after an Ixodes scapularis tick bite. N Engl J Med. 2001 Jul 12;345(2):79-84. doi: 10.1056/NEJM200107123450201. PMID: 11450675.


KIMBERLY LEGG CORBA, DO
As physicians, it seems that every time we turn around, there is some kind of issue or change happening in the medical profession. Full implementation of the Affordable Care Act has helped millions of Americans get the health insurance coverage they needed, yet I believe it opened Pandora’s Box on many levels.
Don’t get me wrong; change is good. Everything changes. We can’t stop change. But when some changes, ultimately, interfere with the physician’s primary responsibility, which is to ensure that the care and safety of patients is the highest priority, then we have an “issue.”
Or call it a problem, if you’d like.
Who drives change in the medical profession? Doctors? Nurses? Hospital administrators? Insurance companies? Vertically integrated health systems? Big Pharma? PBMs? GPOs? Med mal lawyers/ companies? Lawmakers? Judges?
Yes, yes, and yes some more.
Do these groups know what is best for the sanctity of the patientphysician relationship and our ability to care for the health of those who TRUST us? With their lives?
Yes, to those who practice the art and science of medicine. A big No to the rest.
Do physicians interfere with the aforementioned groups’ abilities to perform their jobs?
Nope.
My generation of physicians has lived through the changes, issues, and problems (PCOM class of ’93) and…they continue. I will reiterate, some have been good. Many haven’t worked out so well for us and our patients.
Our current environment requires physicians to pay more attention to policy than ever before.
Policy? Laws? Regulations? Politicians? I don’t know how to read a House or Senate bill! Do you? Civics courses were painfully boring and blow-off classes anyway to keep GPAs high…
Now wait a minute, you mean we must leave our office/hospital and cut into time caring for sick people to educate our elected officials here in Pennsylvania about changes, issues, and problems which can arise from legislation they propose for healthcare and medical practices? About our profession? About bills that make NO sense?
You mean I need to drive to Harrisburg? How long will THAT take? Gas and tolls and parking? What do you mean only the staffer will talk to me? What is a staffer? Oh, those are staffers. They look about the age of my daughter or son…and why do they act like they own the place?
Can’t we just send an email and get back to taking care of our patients? I mean, teaching a bunch of elected officials about how health care works in the real world isn’t really in my job description, is it?
Physicians need help here. But who can help us with this admittedly important task? Thankfully, there IS a powerful entity, that supports not only physicians, but the patients we serve.
The changes, issues, and problems I mentioned above are just a few of the compelling reasons for why physicians need to belong to an organization that protects the interests of doctors and patients. Being part of an organization that guarantees representation with those who create and implement state laws and regulations affecting the delivery of medical care patients is more important now than ever, as both the science and delivery of healthcare become more and more complex.
In our Commonwealth, such a group exists at the local level in almost every one of Pennsylvania’s 67 counties.
In our neck of the woods it is the Lehigh County Medical Society (https://lcmedsoc.org/), which not only publishes this magazine, it has also provided support to our county’s physicians and patients since 1852.
At the state level it is the Pennsylvania Medical Society (https:// www.pamedsoc.org/), which has served Pennsylvania’s physicians and patients for over 175 years.
Currently, there are three pressing issues/problems that currently affect or stand to affect our duty to care for patients in the Commonwealth: restrictive covenants, scope of practice, and venue shopping.
It is empowering to have a strong county and state medical society to provide the support to engage, fight, and win these battles, because individually, or as small groups, physicians simply don’t have the time or financial resources to do so.
Lehigh County Medical Society and the Pennsylvania Medical Society have all of those things, coupled with the expertise to effectively educate those who are making regulatory and legislative decisions which impact the practice of medicine and the delivery of health care in our Commonwealth.
As physicians, we need to focus on patient care, which is hard enough in the current environment. That’s not to say we shouldn’t help our professional organizations make our cases when necessary, but an important part of supporting them in their effort to support us is simply being a member of our medical societies at the local and state levels.
As a member of LCMS and PAMED, you have the security of knowing that these organizations have your back, hear our voices, and are formidable advocates for physicians and patients. But they need YOUR support and your membership to be as effective as possible. Please join both today.
More details about restrictive covenants, scope of practice, and venue shopping appear elsewhere in this issue and will appear in future issues, including my own insights, so please watch for that in the next issue.

Join us on March 20th to learn more about the Lehigh County Medical Society (LCMS) and the Pennsylvania Medical Society (PAMED)—and discover why your involvement matters directly to you and your patients.
We’ll discuss our ongoing legislative efforts to address critical issues such as scope of practice, venue shopping, and restrictive covenants. In today’s healthcare landscape, these battles are essential to protect the integrity of our profession and the well-being of our patients.
LCMS and PAMED provide the resources, representation, and advocacy needed to fight these challenges. As physicians, we can focus on patient care, knowing these organizations have our backs, hear our voices, and work tirelessly for physicians and patients alike.
Don’t miss this opportunity to learn how you can make a difference by joining our efforts!
If you are interested in this meeting, please scan the QR code below for more information.


TAYLOR WEJKSZNER, DO, AND TASHA DESAI, DO

Point‐of‐care ultrasound (POCUS) has been established in the practice of emergency medicine for over two decades, but more recently, its use has expanded into the practice of pediatric emergency medicine (PEM). It encompasses a wide range of applications in children, and allows for a real-time, radiation free and non-invasive approach. As POCUS evolves as a standard tool for the care of children, there is a need for pediatric residency programs to create training programs, as few POCUS training resources exist.
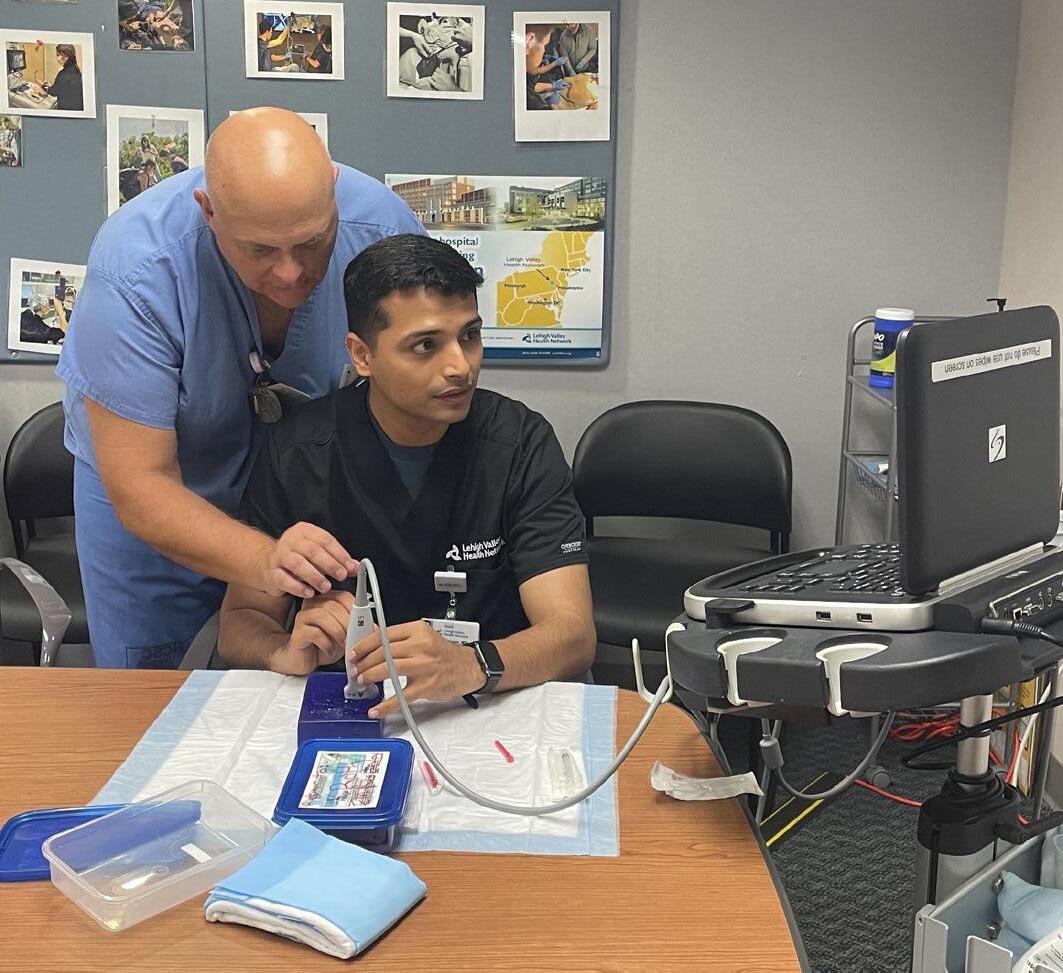
In collaboration with Dr. Schultz, Dr. Desai, and Dr. Wejkszner, the first Pediatric POCUS simulation workshop was held for Pediatric Residents at the LVHN Center for Healthcare Education Simulation. Residents completed didiatics and live scanning.
The goal of the Pediatric Residency POCUS curriculum is to create a multi-part lecture series throughout the year for residents interested in learning their skills.
Look forward to a combined POCUS/Global Health Event to discuss POCUS use in resource limited areas with Dr. Raab before he leaves for The Gambia in April 2025.

Cardiac scanning - use the smallest footprint, close to the sternum with superficial depth. Find ways to soothe the child at an age-appropriate level: bottles for babies, distraction with a favorite show for older kids, etc. Let them lay on their parents for comfort and have them bend their knees or roll them onto their left side.
Soft tissue - Water baths, when applicable, are great for skin/ soft tissue exams, whether you are evaluating for foreign bodies or infection. Quality images can be obtained, without causing pain from probe pressure. Plastic basins work great – check out our residents practicing with water baths in foil trays above!
This article was originally published in Sounds Effects: The Newsletter of the DOHEM POCUS Division.

KEVIN R. ROTH, DO

Ilove my job! Are there tough days in the ED? You bet, but close your eyes and think how many times during a shift, a week of shifts, or a year, how many lives you have affected practicing as an emergency clinician? What would have happened if you were not there to intervene on the patient’s behalf?
The other fraction of my job is coaching emergency clinicians. Whether it be fellows, residents, nurses, or students, it is gratifying to see those who took some coaching to heart and incorporated your techniques into their own practice of medicine. While teaching the causes of metabolic acidosis is important, that knowledge can be gained through the web or “cheat sheet.” You’ve just got to embrace mudpiles.
Enter POCUS. It bridges the gap between the two things I love, caring for patients and coaching.
Let’s talk about coaching POCUS. It is labor intensive as there is no “cheat sheet” when it comes to performing this procedure. It
takes repetitive and consistent coaching and use to become competent in obtaining an image for you to interpret. There are reference materials to compare basic normal vs abnormal images but, subtle, dynamic findings are tough to find in a book or webinar, especially in the heat of battle we experience in the ED. POCUS learning takes some effort but, the gains in patient care have been measured.
Yes, POCUS has been studied extensively as to speed and accuracy of diagnosis. While we do not practice anecdotal medicine, just how many cases of right heart strain, retinal detachment, or achieving vascular access in that patient that “has no veins” do we need to discuss to make anyone realize that maybe, just maybe, POCUS should be the standard of care for all those practicing medicine.
Those above-mentioned direct effects have unquestioned value. I would argue that in the areas of patient satisfaction, providing those that are underserved access to more advanced care on the front lines, and cost savings may equal that value.
continued on next page
Teaching a patient with chest pain or palpitations that their heart appears normal and showing them the images builds a relationship and trust quickly. This can ease a patient’s anxiety and fears.
How about the case of that 16 y.o. basketball player that experiences syncope on the court? It can be the difference discharging with confidence or diagnosing HOCM almost immediately.
Providing access to care is part of our business and POCUS provides many patients who cannot access care, advantages they may never know until it is too late.
My least favorite case is to find the dilated cardiomyopathy on the patient with clear lungs that states, “I’ve had asthma for years” but, the inhaler and steroids “don’t work too well.”
Let’s “spend” a little time talking about cost. If you diagnose 1 retinal detachment in 30 seconds and make 1 phone call to ophthalmology to arrange care, how much money is saved as compared to non-performance/diagnosis of that retinal detachment?
Let’s get out our calculators. No POCUS but visual field deficit on exam. How much does a CTA cost? An MRI? Admission to the hospital? Neurology consult? Iatrogenic complication? What number did you calculate?
Committees are formed, meetings are held, and the same question is always asked. How do we do better? I have some answers.
POCUS early is better. POCUS often is better.
Advancing POCUS teaching and education is better.
All these statements come together to form this answer. You want better, POCUS is the answer. You want to stand out and provide uncommon care, POCUS is the answer.
Have a great day,
KR
This article was originally published in Sounds Effects: The Newsletter of the DOHEM POCUS Division.




WINTER NEW AND RE-INSTATED MEMBERS
Syed Ali Aown, MD Resident - Internal Medicine
Dimitry Belogorodsky, DO Sports Medicine (Family Medicine)
Emily Catherine Bilyk, DO Family Medicine
Joseph A. Candio, MD Internal Medicine
Michael Jay Gehman, DO Infectious Disease (Internal Medicine)
Victor David Gonzalez Benitez, MD Family Medicine
Kaveh Kousari, MD Urology
Chris Allyn Lycette, MD Neurological Surgery
Mia Mattioli, MD Internal Medicine
Chelsea Mary Nemeth, MD Obstetrics & Gynecology
Sarah Raab Medical Student, Philadelphia College of Osteopathic Medicine
Leyland A. Robinson, DO Family Medicine
Ramchandani Santosh, MD Resident - Internal Medicine
Muhammad Shehryar, MD Resident - Internal Medicine
Phillip Shwae, MD Psychiatry
Frank Jeremy Tamarkin, MD Urology
Hazel Alvaran Tuazon, MD Obstetrics & Gynecology
Elizabeth Lauren Andrews, MD Psychiatry
Kevin Connor Eddinger, MD Resident - General Surgery
Meredith Johnson, MD Neurology/Diagnostic Radiology/Neuroradiology
Henry Lam, DO Resident - Gastroenterology (Internal Medicine)
Kayla Walker Long, DO Emergency Medicine












At MADJ, we specialize in helping medical practices and health systems of all sizes thrive in competitive landscapes. From small beginnings to significant success, our tailored strategies have transformed healthcare providers into community cornerstones.

Participating in St. Luke’s University Health Network’s community health research program, DNA Answers, is quick, easy, and at no cost to you. You’ll learn about your genetic risk for certain cancers and heart disease, for which actions may be taken to help prevent, delay, or reduce symptoms. You may share your results with any healthcare provider at any facility for consultation or care. These insights can help you and your healthcare provider make more informed and proactive care decisions for you and your family. Health insurance is not required to participate.
Participating in St. Luke’s University Health Network’s community health research program, DNA Answers, is quick, easy, and at no cost to you. You’ll learn about your genetic risk for certain cancers and heart disease, for which actions may be taken to help prevent, delay, or reduce symptoms. You may share your results with any healthcare provider at any facility for consultation or care. These insights can help you and your healthcare provider make more informed and proactive care decisions for you and your family. Health insurance is not required to participate.
Participating in St. Luke’s University Health Network’s community health research program, DNA Answers, is quick, easy, and at no cost to you. You’ll learn about your genetic risk for certain cancers and heart disease, for which actions may be taken to help prevent, delay, or reduce symptoms. You may share your results with any healthcare provider at any facility for consultation or care. These insights can help you and your healthcare provider make more informed and proactive care decisions for you and your family. Health insurance is not required to participate.
If you participate, you also have the opportunity to learn about your ancestry and other traits like, caffeine sensitivity, sleep patterns and more.
If you participate, you also have the opportunity to learn about your ancestry and other traits like, caffeine sensitivity, sleep patterns and more.
If you participate, you also have the opportunity to learn about your ancestry and other traits like, caffeine sensitivity, sleep patterns and more.
Your voluntary participation supports research that could lead to new discoveries for improving healthcare for your community and generations to come.
Your voluntary participation supports research that could lead to new discoveries for improving healthcare for your community and generations to come.
Your voluntary participation supports research that could lead to new discoveries for improving healthcare for your community and generations to come.
