10 minute read
Elderly care home nutrition
the North BedfordShire ‘PUffiNS’ ProjeCt
Bernice Chiswell Bsc hons Rd Bedford hospital nhs trust and north Beds Food First Project
Advertisement
Carol Ferdinandez msc Rn south Essex Partnership trust, lead tissue Viability nurse
Bernice is a Community dietitian with over 30 years’ experience. As well as leading part of the North Bedfordshire food first Project, she has interests in behaviour change, obesity and mS.
Carol has been a registered Nurse for 22 years, laterally specialising in tissue Viability with a keen interest in Pressure Ulcer Prevention work.
PuffiNs - aren’t they small black and white birds, often pictured with their brightly coloured beaks packed with sand eels? well, North bedfordshire is a long way from the coast, but we do have PuffiNs!
Our PUFFINS are Pressure Ulcer Food First INitiative Champions, and their ‘habitat’ is the elderly care homes in Bedford and surrounding areas.
The impetus for this project was generated by a desire to see an improvement in the detection and management of malnutrition in care homes for the elderly. At the same time, there are national and local initiatives to stop avoidable pressure ulcers (1). This is seen as a key objective for healthcare providers and commissioners in an effort to ensure provision of high quality, patient-centred care in line with the Department of Health’s ‘Operations Framework for the NHS in England’ 2012/13. Pressure ulcers are seen as an indicator of quality of care and, given that they are largely avoidable, Tissue Viability Nurses (TVNs) have long expressed concern (2). Some are questioning whether pressure ulcers could be construed as an act of nursing negligence (3).
NHS Midlands and East (previously the regional SHA cluster, compromising NHS East Midlands, NHS West Midlands and NHS East of England) set the goal to eliminate avoidable grade 2, 3 and 4 pressure ulcers by December 2012. BAPEN are involved in this ongoing work, looking at disseminating good practice and sharing the resources produced to support this goal (4).
Managing nutrition and hydration is a key aspect of pressure ulcer prevention (5). In view of this, we teamed up with the lead tissue viability nurse in Bedfordshire (South Essex Partnership Trust) who was also considering a champions programme in order to recruit, train and support champions who would be skilled to focus on both agendas. Studies indicate that provision of champions in addition to effective prevention practices leads to an improvement in patient outcomes with respect to pressure ulcers (6). This multidisciplinary approach of sharing knowledge and expertise enhanced engagement with the care homes. Together I believe we have achieved far more than we could have as separate teams, to promote evidence-based practice in the care homes.
The name PUFFINS came from the champions themselves, as did the title ‘Puffin Flyer’. (I wish we possessed such creative thinking!)
To qualify as a champion, the member of staff needs to be in a position to influence practices in their care home. It was necessary to have the care home management buy in to ensure commitment to change within their care homes, as it is known that practice is linked not only to knowledge, but to inherent beliefs and values (3) 3. We have chefs, senior carers, nurses and home managers who are PUFFINS. In all, 96 have been trained, with a further training course planned in March where a further 22 are booked (with a waiting list).
Once recruited, budding champions attend a one-day training course. This is presented in an interactive way to keep staff engaged and includes topics such as: the aetiology of pressure damage; the cost in terms of morbidity and mortality as well as financial; how to screen using Waterlow and action plans to prevent and managed pressure ulcers. The Food First approach is explained, together with MUST screening and nutrition
action plans. Change planning is included to allow the PUFFINS to apply the information to their care home setting and develop a detailed action plan for a realistic change they want to implement.
A pressure ulcer has been described as ‘localised injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear’ (EPUAP, 2014) (7).
There are graphic slides to increase awareness of the potential severity of pressure ulcers. The fact that 95 percent are preventable, places the onus on staff to screen residents and to take appropriate action to reduce risk. Staff are trained in the fivestep model for pressure ulcer prevention, known as SSKIN (8). • Surface: make sure your patients have the right support. • Skin inspection: early inspection means early detection. Show patients & carers what to look for. • Keep your patients moving. • Incontinence/moisture: your patients need to be clean and dry. • Nutrition/hydration: help patients have the right diet and plenty of fluids.
This has been shown to have an impact on prevention and ensure consistency of care (9). Through case studies they practice completing the Waterlow score. Focusing on malnutrition detection and prevention, and again using case studies, the Malnutrition Universal Screening tool is explained and practised (11). As both tools include weight and nutrition, but score in a different way, this can understandably prove confusing for staff. Food fortification is demonstrated, and the staff sample a homemade milk shake. Recipes are provided for high protein, high calorie shakes and desserts.
An educational resource folder is provided for each champion, including guidelines specifically aimed at care homes, presented in an easy-tounderstand format. This includes what should be done, how and when, including the rationale for each intervention.
It is known that education alone rarely makes a difference to practice and Moore (2010) concluded that often work-place challenges of lack of staff and time prevent staff from adhering to evidence based practice (12). Thus, it was important to ensure champions were utilised as drivers of change, acting as a clinical resource for colleagues. The final exercise of the training day is to support the champions to decide on one realistic change that they would like to implement in their care home, and to produce a detailed change plan to take this forward.
Up to 30 attend at a time. Sponsorship (from wound care companies for example) has enabled refreshments and lunch to be provided.
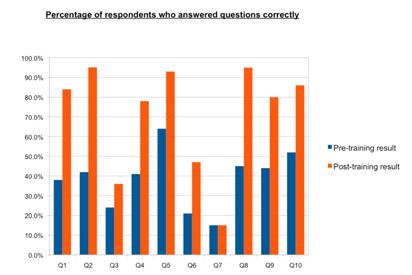
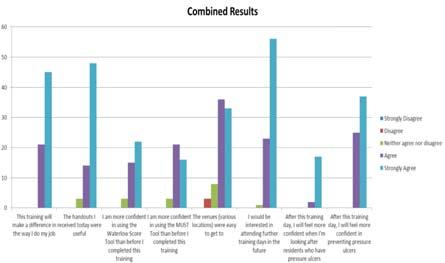
A questionnaire is completed pre- and posttraining, and this demonstrates an increase in knowledge from attending the day.
The questionnaire includes 10 questions relating to the causes of pressure ulcer, screening for pressure ulcer risk, equipment and procedures for pressure ulcer reduction, MUST screening, nutrition care plans, dehydration, food fortification, etc. This training has received positive feedback.
PREssuRE ulCER inCidEnCE and EFFECtiVEnEss oF thE PRogRammE As well as positive evaluation in terms of increased knowledge and enthusiasm, we were keen to see if pressure ulcer incidence was decreased in care homes with PUFFINS. Based on April to December 2014 figures, of elderly care homes with zero to one pressure ulcer alerts, 83 percent had one or more PUFFIN compared to homes with two or more pressure ulcers where only 59 percent had Puffins in place (Total number of homes: 46).
tEstimonial FRom a CaRE homE managER I thought you would appreciate some feedback from the two Puffin sessions we have attended and how it has impacted on the residents’ wellbeing in our care home.
The first session was so informative. It really made us consider if we’re doing enough to promote pressure care and enhanced nutritional support to our vulnerable residents living with dementia in our day-to-day care planning.
We came back and arranged for two cork boards to be erected to display information that we had obtained on the day to cascade information, as well as sharing with the senior staff. We also looked at the pressure relieving equipment to see if it was fit for purpose and whether cushions, for example, fitted correctly into the existing seats so as to not compromise the purpose of the cushion. Soap was replaced with gentle emollients to wash ‘at risk’ skin and has shown to be much kinder and less drying.
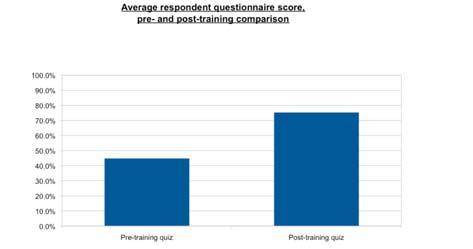
Figure 2
Figure 3
We have also had a meeting with our District Nursing Team who are more than willing to provide pressure relieving equipment to any of our Residents with a BMI of 20 or below as a preventative measure. From our point of view, this is a significant cultural shift in that the District Nursing Team are now working with us to be proactive rather than reactive.
Nutritionally, we have tried the recipe suggestions in the Food First information to fortify foods (we were pleased the cooks needed little prompting!) and we think about increasing protein for residents with poor appetite. We are very grateful for the support you have shown us and look forward to a continued partnership as PUFFIN champions.
PuFFins Fly-ER After the training, our fully fledged PUFFINS are eligible to receive their copy of PUFFINs FLY-ER, a two-page monthly publication with sound bites of information presented in a fun way - word searches, anagrams, fast facts, photos, recipes, etc. Topics covered include nutrition and hydration week events, examples of good practice from local care homes, chair based exercises, importance of protein and good dietary sources and assisting residents to eat.
The aim is for staff to look at the flyer in their break times, maybe find a tip to put into practice, but more importantly to keep the importance of good nutrition and pressure ulcer prevention on the agenda for them and their care home.
PuFFin quaRtERly mEEtings Ongoing support is provided by two-hour quarterly meetings. Topics covered have ranged from meeting the nutritional needs of residents with dementia, managing constipation, textured modified diets and use of soaking solutions for dysphagia, identifying and reducing shear and friction, use of safety cross, case studies using Waterlow and MUST, and discussing appropriate action plans.
thE ChallEngEs • Keeping staff engaged when there are many demands on their time. • Staff changes in the care home. • Working across two health trusts (Bedford Hospital NHS Trust and South Essex Partnership
Trust) with a range of private companies (care
home providers). • Making time in our busy workloads to continue proactive regular input.
ouR nExt stEPs We are conscious of the need to continue auditing the project in order to demonstrate value and to refine it to meet the needs of the staff attending and promote the well-being of the residents. We are currently contacting care home managers and staff who have been trained as PUFFINS to complete a survey monkey questionnaire. This will ask for examples of changes made in response to the training and assess further training needs. We are also in the process of getting badges for the PUFFINS to enhance their recognition in the care homes as champions.
ouR toP tiPs FoR ChamPion PRojECts • Team up with colleagues for a multidisciplinary approach. Care home staff are busy people, so will not be able to allocate separate champions for different facets of their work. • Identify allies - the Care Standards and Review team in the social services department have been a great support. (Teams in your area may well have different titles). • Recruit champions who will be proactive and have a role in their care home which will enable them to influence practice. • Telephone contact can promote attendance. Generally our quarterly meetings will receive perhaps five bookings in response to the advertising flyer. A proactive telephone call two weeks ahead of the event will increase attendance to 15 to 20. • Homes are keen to demonstrate their good practice to CQC, other care homes and perspective residents and their families, so providing the opportunity to demonstrate a proactive approach can gain their engagement. • Having regular contact both written (providing ongoing information on relevant topics and examples of good practice) and face to face (support group) help to keep champions engaged, motivated and keen to try new ideas. • Audit of results is essential to measure success and can help secure funding.








