
5 minute read
Is There a General Connection between Obesity and Genetics?
BIOLOGY
Is There a General Connection between Obesity and Genetics?
Advertisement
Tash Spungin
To define obesity, or to be overweight, means having abnormal or excessive fat accumulating in the body, presenting a risk to health in many different ways. When we look at the importance of genes in the body. we know that genes give the body instructions for responding to changes in its environment - both internal and external. This means that we can immediately associate genetics with body weight and food consumption, as our body may be ‘genetically engineered’ to respond with a fast or slow metabolism, with excess weight gained from eating certain foods, and we may even have the obesity-associated gene… FTO The obesity-associated gene -what is it? It is a protein which has an amino acid sequence made to demethylate -remove a methyl group -from DNA. Studies suggest that the levels of this gene -known as the FTO gene -can decrease during fasting periods and they can increase during feeding. The variation in FTO levels result in decreased expression or activity of the gene. This might provide a signal that promotes obesity. Similarly, variants of the FTO gene risk having an obesity-triggering allele. A study focused on 38,759 Europeans aged 7 and upwards and whether they had variants of the FTO obesity risk allele. It was found that carriers of one copy of the allele weighed on average 1.2 kilograms more than people with no copies, with all other conditions kept the same. Carriers of two copies weighed 3 kilograms more. This shows how even the simplest of mutations and variations of the genetic makeup can cause life-altering shifts in one’s body, especially in obesity which can be detrimental mentally, as well as physically [1].
Variants of the FTO gene can have many affects on the body, one of which is obesity.
Bardet-Biedl Syndrome (BBS) Bardet-Biedl syndrome is a human genetic disorder that affects many body systems. It is an autosomal recessive disorder, meaning that the sufferer inherits two mutated genes, one from each parent. A sufferer of BBS will have specific proteins that can cause vision loss, varying degrees of learning disabilities, and kidney abnormalities which can make the disease fatal. Another dangerous symptom is obesity, since the disorder can disturb appetite-regulating hormones. Abnormal weight gain typically begins in the early childhood stages and can continue into the rest of the patients’ lives [2]. The issue with such a threatening aspect of having BBS is
BIOLOGY
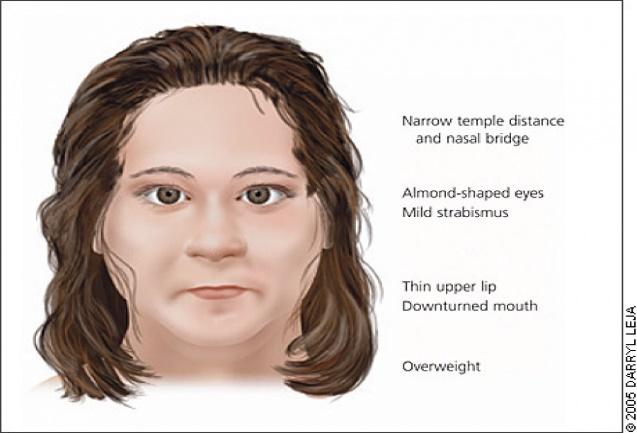
that obesity is not just one disease - it encourages endless damage to the body. Obesity increases the risk of type 2 diabetes, hypercholesterolemia, atherosclerosis and high blood pressure. Within the UK, around 1 in 160,000 people have BBS, which adds to the worrying danger of the estimated 28% obese UK adults.[3][4] Prader-Willi Syndrome (PWS) Another genetic disorder that can prove a lifetime of struggle with obesity is Prader-Willi syndrome. PWS is caused by a loss of specific genes on chromosome 15. It starts in childhood and newborns may present with weak muscles, poor feeding and slow development. Those affected become constantly hungry, leading to obesity and type 2 diabetes. There is a noticeable physical difference since sufferers often having a narrow forehead, small hands and feet and can be short in height too, alongside the impact of obesity. Most sufferers, as adults, are unable to have children.
About 74% of cases occur when part of chromosome 15 from the father is deleted. In another 25% of cases, the affected person has two copies of the maternal chromosome 15 and lacks the paternal copy. They end up with no working copies of certain genes. PWS is not generally inherited, but rather the genetic changes happen during the formation of the gametes or in early development. Unfortunately, the disease affects between 1 in 10,000 to 30,000 people worldwide.
Treatment Both diseases have no cure. However, the symptoms can be managed. BBS patients can be provided with vision aids and mobility training, they can have speech therapy and special education and monitored hormone levels. It is assumed that patients can have a kidney transplant to manage BBS, but the immunosuppressants taken afterwards can contribute to obesity, making it very risky. In PWS, new-borns can be supported with feeding tubes, strict food supervision from age three, and they will often have an exercise program. Growth hormone therapy can improve outcomes too. Life expectancy is limited with PWS, as there is a 75% mortality rate for 42 year olds with the disease. This is worsened when food intake and exercise activity is not managed appropriately since weight levels can become dangerously high and there is a higher chance of having heart issues [5][6]. When their quality of life is also low, due to inability to lead a fully-independent life even as an adult, PWS patients may be impacted in all areas of their lives. BBS also gives a high mortality rate, but with the development of both genetic technology and treatments, it is hoped that life expectancy for sufferers of both diseases will improve over time. Conclusion It is readily apparent from this that obesity can affect anyone, no matter the speed of your metabolism, the amount of exercise one does, or other factors in your life. This is because the slightest genetic mutations and variations of proteins from proteins that we all have can trigger such a great effect on the body. Whilst the chances are so low for both these types of variations like seen in FTO and genetic disorders such as BBS and PWS, it is essential that we are aware of these signs, and that we know the right ways to take care of our bodies with sufficient exercise and careful monitoring of our food intake.
Facial features presented with Prader-Willi Syndrome.
Sources:
1. https://en.wikipedia.org/wiki/FTO_gene 2. https://en.wikipedia.org/wiki/Bardet–Biedl_syndrome
BIOLOGY
3. https://rarediseases.info.nih.gov/diseases/6866/bardet-biedl-syndrome 4. https://medlineplus.gov/genetics/condition/bardet-biedl-syndrome/ 5. https://en.wikipedia.org/wiki/Prader–Willi_syndrome 6. https://www.nhs.uk/conditions/prader-willi-syndrome/ 7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770999/







