
3 minute read
Stem Cells and Miscarriage: What is the Correlation?
BIOLOGY
Stem Cells and Miscarriage: What is the Correlation?
Advertisement
Emily Clark
A miscarriage can be defined as the loss of a pregnancy within the first 23 weeks. Around 10 to 20% of pregnant women will suffer a miscarriage [1]. Recurrent miscarriages, where a woman suffers 3 or more consecutive miscarriages, affect one in 100 women. A recent study in the University of Warwick has discovered a link between a lack of highly proliferative mesenchymal stem cells (hPMCs) in the lining of the womb and the likelihood of a woman suffering from recurrent miscarriages [2].
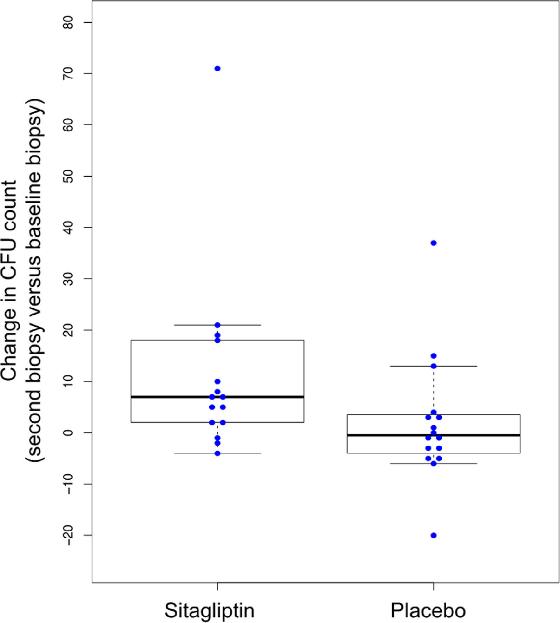
During the second half of the menstrual cycle, the endometrium (womb lining) responds to increased levels of progesterone by remodelling itself so it is ready for the short period of time when an embryo can be implanted. This process is called decidualisation and it depends on the differentiation of endometrial stromal cells into specialised decidual cells [3]. During this time, lots of highly proliferative mesenchymal stem cells (hPMCs) are directed to the endometrium due to their important role in aiding the endometrial remodelling as well as maintaining the placentaas explained later in this article.
The study in Warwick aimed to find out where these hPMCs were differentiating from and how exactly they worked. In the study, tissues were taken from the lining of the womb of 183 women and analysed closely. The results showed that fewer hPMCs were found in the group of women suffering from recurrent miscarriage compared to those in the control group and these results suggest that there is a correlation between the hPMCs and recurrent miscarriage [4]. Dr Brosens, the professor who led the research at Warwick, said they had found that the “hPMCs are derived from circulating bone marrow-derived stem cells and recruited into the lining of the womb at the time of embryo implantation” [1].
Diagram showing the decidualisation process and how highly proliferative mesenchymal stem cells aid with this.
BIOLOGY
Lots of hPMCs are needed in the endometrium during conception as they play a vital role in assisting the rapid growth of the placenta. With a depleted number of these stem cells, as found in women suffering from recurrent miscarriages, there are not enough cells being produced in the placenta to allow it to grow adequately and this also affects and interrupts the interaction between the lining of the uterus and the placenta which can lead to miscarriage [5]. Overall, a lack of these stem cells means that the endometrium has worse conditions to support the embryo and there is also extra stress placed on the specialised decidual cells (which could breakdown the lining and also cause miscarriage) [6].
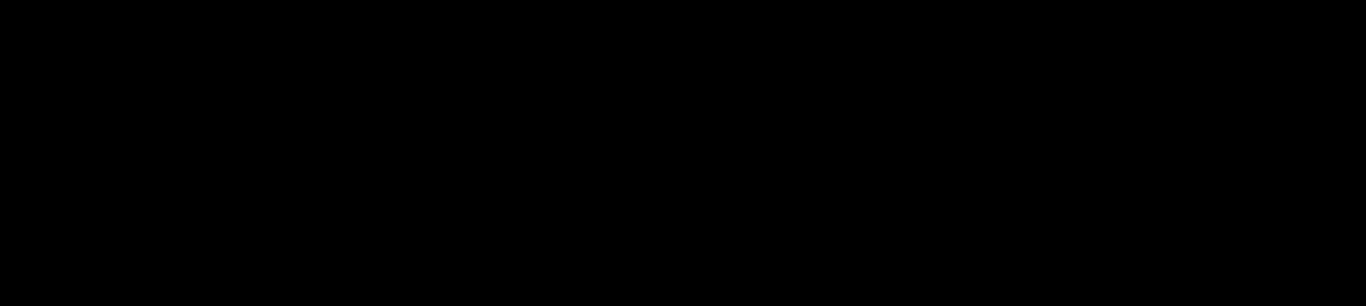
Using information from these trials, scientists are now researching ways of preventing recurrent miscarriages through increasing the number of hPMCs in the endometrium by either physically inserting more in, or encouraging the differentiation of more hPMCs. There is a trial currently happening that is investigating the use of Sitagliptin, a drug used for diabetes, in preventing miscarriage. When an enzyme, called DPP4, is too active, it can stop the stem cells from being directed to the endometrium which could explain why there is a lack of hPMCs in the endometrium in certain women. The sitagliptin drug acts as a DPP4 inhibitor and therefore allows the stem cells to reach the endometrium as normal and perhaps prevent miscarriage [7]. An initial trial for this drug went ahead at the start of 2020 where 38 women suffering from recurrent miscarriages were given the sitagliptin drug or a placebo. The results showed that the number of stem cells in the endometrium increased by 68% after taking the sitagliptin whilst there was no increase with the placebo [7]. The number of stressed decidual cells also decreased by 50%. A further clinical trial will be happening for this drug over the course of the next year and will hopefully be able to prevent thousands of recurrent miscarriages.
Overall, this information from the Warwick study has provided crucial information about how miscarriages are caused and has therefore prompted the research and further trials of treatments that will help to prevent recurrent miscarriages.
Results from the sitagliptin trial showing that there was a bigger change in the CFU count when using the Sitagliptin compared to barely any change when using the placebo. A CFU count shows the ability of the stem cells to proliferate and differentiate in this sample.
BIOLOGY
Sources :
1. https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptomscauses/syc-20354298 2. https://warwick.ac.uk/newsandevents/pressreleases/stem_cell_depletion 3. https://stemcellsjournals.onlinelibrary.wiley.com/doi/full/10.1002/stem.3367 4. https://www.sciencedaily.com/releases/2016/03/160307211055.htm 5. https://sydneynewstoday.com/diabetes-drugs-may-help-women-with-repeated-miscarriagesstudies-miscarriage/110800/ 6. https://www.thepharmaletter.com/article/diabetes-drug-could-lead-to-new-treatment-forrecurrent-miscarriage 7. https://www.tommys.org/research/research-topics/miscarriage-research/can-sitagliptin-helpincrease-stem-cells-wombs-women-who-have-suffered-recurrent-miscarriages







