The Prism Wellness and Community Center: A Model for Inclusive Design
 One of a series of white papers by Page professionals Lisa Ulibarri, LEED Green Associate and Hilary Bales, AIA, ACHA, EDAC
One of a series of white papers by Page professionals Lisa Ulibarri, LEED Green Associate and Hilary Bales, AIA, ACHA, EDAC

Think What’s Possible
Page is a powerfully imaginative and collaborative architecture and engineering firm: one that’s ready for today and designed for what comes next. We pair form with function, reason with emotion, and ideas with expert implementation. At Page, the potential of what’s possible is paired with the practicality of how to make it happen. Our purpose is designing places smarter, while improving the experiences of those who work, live, and learn in them. From thought to finish, Page experts—of all disciplines—see the big picture, figure the best way forward, and deliver solutions in inventive and amazing ways. Imagine that.
Visit our website at pagethink.com


Introduction
Healthcare is always looking to the future and learning from the past. With innovations in technology and research, continuous improvements are being made in safety, accuracy, efficiency, and patient experience. Even in the effort to make healthcare more accessible and patient-centered, however, there are populations that remain underserved due to financial, social, or legal barriers. One such population is the LGBTQIA+ community. Non-cisgender patients (individuals whose gender identity does not align with the sex they were assigned at birth) and those of different sexual orientations have not always been embraced within the larger community, healthcare, or the inclusive design initiative. Individuals still struggle to find accommodating, compassionate care in a safe and affirming environment. Unfortunately, stigma, prejudice, and misinformation are still creating barriers to care, acceptance, and access.
The Prism Wellness and Community Center is an imagined prototype clinic centered around specialized wellness and gender-affirming care to serve and give voice to those who may be under-represented. It is intended to provide a safe and inclusive environment that addresses and celebrates all parts (physical, emotional, and social) of the LGBTQIA+ culture and identity. The clinic itself is not affiliated with a health system, but the components and design concepts addressed in the prototype can stand alone or serve as a part of a larger wellness campus. The center is envisioned to embrace the holistic health and wellness of LGBTQIA+ patients and to encourage family support while providing education, wellness resources and open amenities for the larger community.
To fully appreciate the necessity and impact of the Prism Wellness and Community Center, it is essential to understand the broader context and underlying issues faced by the LGBTQIA+ community. This paper includes comprehensive background information and research to highlight the challenges of stigma and misinformation. By delving into these complexities, the importance of creating specialized, inclusive spaces becomes clearer. First, detailed background information is presented, followed by an in-depth discussion of the prototype and design considerations that address specific needs identified through the research.

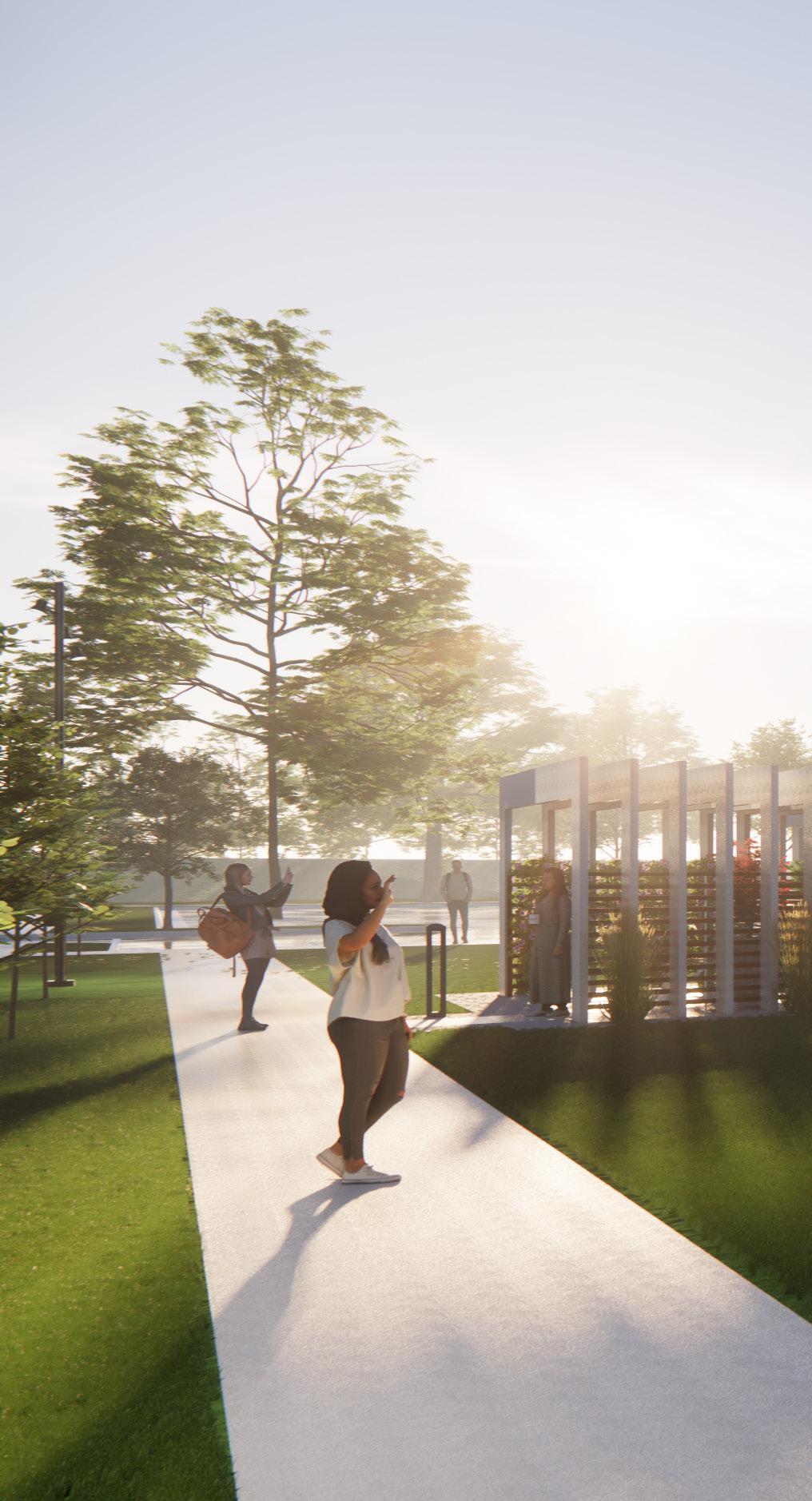
Prism Wellness and Community Center Main Entry
History of Exclusion
Throughout history, members of the Lesbian, Gay, Bisexual, Transgender, Queer/Questioning, Intersex and Asexual (LGBTQIA+) community have endured prejudice, hatred, and misunderstanding. Although there have been movements fighting for social justice, there continue to be issues that disproportionately affect the community, such as lack of access to healthcare, violence, social exclusion, and discrimination.
The LGBTQIA+ community comprises members varying by age, race, religion, and background. Several statistics support the need for specialized and gender-affirming healthcare community facilities. A Gallup study found that with each new generation, the percentage of LGBTQIA+ self-identifying people is increasing: 2.6% of Baby Boomers, 4.2% of Generation X (Gen X), 10.5% of Millennials, and 20.8% of Generation Z (Gen Z) are LGBT-identifying. These numbers may be lower than the actual percentages due to the stigma around publicly reporting non-cis/hetero identities. Gallup defines Gen Z as being born between 1997-2003, so anyone born after 2003 has not been included in the statistics (Gallup). Within those percentages of LGBT+ adults, 13.9% identify as lesbian, 20.7% as gay, 56.8% as bisexual, 10% as trans, and 4.3% as outside those four options (Gallup). 6.1% of current U.S. military personnel and an estimated one million veterans also identify as LGBT (Mahowald; Grant).
In addition to traditional primary and wellness care needs, members of the LGBTQIA+ community also have unique needs and health factors that disproportionately impact them. Many of these are exacerbated by the fact that in a 2017 poll, 18% of LGBTQ people say they have avoided medical care out of fear that they would face discrimination due to their identity (NPR). For example, members report a lower rate of mammography and Pap smear screening, higher rates of obesity, and poor cardiovascular health. Individuals facing increased psychosocial stressors are more than twice as likely to smoke. Many struggle with a higher rate of infertility, and reproductive and sexual performance issues. Other disparities include higher rates of HIV and other sexually transmitted infections that drive additional screening for certain cancers and sexual health-related education and treatment. Those receiving gender-affirming care require different surgical or hormone-based treatments, as well as specialty support for care management, and are affected by side effects throughout the course of their lives (National LGBT Health Education Center).
Mental health is just as important to address as physical health and wellness. Community members report higher rates of anxiety, stress, depression, eating disorders, and exposure to violence, bullying, and discrimination. According to the Trevor Project, 73% of LGBTQ youth in 2022 reported symptoms of anxiety and 58% reported symptoms of depression. Further, 45% of LGBTQ youth said they seriously considered suicide in the past year, with 14% attempting it. These statistics go hand in hand with 82% of LGBTQ youth wanting to receive mental healthcare, but 60% were not able to access it (Trevor Project). This shows that even with the availability of care, many in the LGBTQIA+ community are not able to use those resources. With the increasing limitations and bans on affirmative medical care, these percentages will likely continue to rise. Homelessness, substance abuse, and lack of social support also have a disproportionate impact.
LGBTQ People Avoiding Medical Care out of Fear of Discrimination NPR, 2017
4
0 5 10 15 20 25 73% 58% 45% 82% 60 0 5 10 15 20 25 73% 58% 45% 14 82% 60
Traditionalists Born before 1946 Baby Boomers Born 1946-1964 Generation X Born 1965-1980 Millennials Born 1981-1996 Generation Z Born 1997-2003
Americans’ Self-Identification as LGBT, by Generation Gallup, 2021
Reported Anxiety Reported Depression Seriously Considered Suicide 14% Attempted Suicide Wanted Mental Health Care 60% Unable to Receive Care 0 5 10 15 20 25 73% 58% 45% 14 82% 60 18% 0 5 10 15 20 25 73% 58% 45% 14 18% 0 5 10 15 20 25 73% 58% 18%
2022 National Survey on LGBTQ Youth Mental Health The Trevor Project
0 5 10 15 20 25 73% 58% 45% 14 82% 60 18%
Benchmarking
In the healthcare realm, there is a distinct lack of targeted education among the provider community (a median of five hours of clinical training), resulting in misinformation, bias, and insensitivity (National LGBT Health Education Center). Until 1987, homosexuality was listed as a “psychiatric disease” in the Diagnostic and Statistical Manual of Mental Disorders (DSM) (Bass, Nagy). Transgender status was also listed in the DSM as a “gender identity disorder” until 2013 when the wording was revised to a patient-centered term, “gender dysphoria,” to properly emphasize treatment targeting the distress of the dysphoria, not any assumed pathological origin (Russo). Today, many providers still do not know basic concepts or appropriate terminology to use when interacting with patients. Still, others lack experience with specialty care or fail to ask the right screening questions to address patients’ needs (Bass, Nagy). In many cases, specifically regarding reproductive and sexual health, preconceived gender and sexual lifestyle assumptions prevent patients from accessing their desired healthcare solutions (Wingo, Ingraham, Roberts). All these factors color how patients interact with health systems and may create continued barriers to trust and open dialogue with providers.
LGBTQIA+ specialty and gender-affirming clinics in the United States have a limited history. Some have found success within a larger hospital network and others have occupied standalone facilities. Each scenario has pros and cons, and program success, access, and support vary greatly. In our research to see how such clinics have operated, we have found a few that offer various services for a range of patient populations. The examples cited within this paper are not affiliated with our firm or design concepts and are provided here for reference.
One example is Outside In, a clinic in Portland, Oregon, that primarily serves youth and adolescents, offering primary care, gender-affirming hormone therapy, surgery referrals, wellness screenings, pharmacy services, behavioral health services, and advocacy for legal and financial aid. Additionally, they are a Federally Qualified Health Center, meaning they can serve adults and veterans. While the center’s primary goal is healthcare, part of its mission statement includes aiding unhoused individuals and the larger community through meal programs, syringe exchanges, housing programs, and job training. While Outside In offers more services than mentioned, the clinic clearly provides a holistic approach to health and wellness care beyond just medical support.
Another example is the Living with Change Center at Cincinnati Children’s Hospital in Cincinnati, Ohio, a clinic that is managed through the safety and resource net of a larger hospital network. Care is focused on clientele up to 24 years old and on individualized treatment plans based on medical interviews, physical exams, psychosocial consultations, and referrals. Treatment plans typically include in-depth looks at gender identity, age, puberty stage, risk and benefit analysis, treatment costs, and readiness for next steps. Physicians work with a team of healthcare providers to ensure patients get the best care possible. The center also offers information and resources for families and other healthcare professionals, such as addressing frequently asked questions and making best practice suggestions. While this clinic primarily looks at genderaffirming care through a medical lens, the team-oriented approach to care is consistent with other examples that look at healthcare from all angles.
The last example is the Resource Center in Dallas, Texas, which provides a range of healthcare, education, advocacy, and community services. The center’s healthcare component focuses on sexual health and wellness, primary care services, HIV/AIDs services, pre-exposure prophylaxis (PrEP), gender-affirming care, and behavioral health services. Community programs include group events, dances and socials, field trips, clubs, monthly mixers, and support groups. Educational opportunities are available through sex education, youth and student resources, and support from foundations and specialty population groups. Suicide hotlines, chat spaces, and outreach are part of the Resource Center’s advocacy program. The center has locations throughout Dallas, serving a large part of the LGBTQIA+ community.


5
Legislation in the U.S.
LGBTQIA+ and gender-affirming healthcare cannot adequately be discussed without mentioning the barriers being raised in current legislation. The Human Rights Campaign keeps an updated map of gender-affirming care bans in progress or passed in the United States at the state level. So far, 25 states have passed laws or policies that ban genderaffirming care (Human Rights Campaign). Three have blocked or put the bans on hold, while nine have ongoing litigation that challenges these bans.
More concerning is that while the map focuses on bans that affect youth 13 to17 years old, several states are considering bans on care up to 26 years of age. In the United States, about 39% of trans youth live in one of the 25 states that have bans in place. Almost 50% of trans youth will not be able to access proper care and support and of these, one-third will still be unable to receive publicly funded gender-affirming care, regardless of age.
One of the bans in question “restricts transgender minors from accessing puberty blockers and hormone therapies” and went into effect Sept. 1, 2023. This ban also mandates that any youth or adolescents currently receiving gender-affirming care be weaned from treatments. While this ban is new regarding legislative impact, the efforts to stop gender-affirming healthcare are not new. For example, in recent years, some specialty clinics that provided care to trans youth were forced to close. In one case, mounting pressure from state officials and activists resulted in close to 500 patients needing to seek help elsewhere (New York Times). The clinics had provided counseling, primary care, and hormone therapy to patients up to 21 years old since 2014 (New York Times). Several more states have adopted bans regardless of age. With neighboring states also banning care, some patients now must travel even further for gender-affirming health services.
Nationally, there is a federal policy that aims to “promote access to healthcare for LGBTQ+ people and … prohibit discrimination on the basis of sexual orientation and gender identity” (KFF). In May 2021, the Department of Health and Human Services’ Office for Civil Rights included gender identity and sexual orientation in its definition of sex discrimination under the Affordable Care Act. This was a reversal of a recently held policy that eliminated gender identity and sexual orientation from the definition. While this is a positive step for the LGBTQIA+ community, this policy only applies to health programs that receive federal financial assistance. In response to state directives to ban genderaffirming care, the Americans with Disabilities Act was updated to include guidance that care is mandated if gender dysphoria is qualified as a disability (KFF). The complications surrounding the ways in which patients can access genderaffirming care underscore that facilities dedicated to these types of services are vital to the American healthcare and social care system. Below is a map illustrating current laws regarding insurance discrimination concerning LGBTQIA+ care, including transgender exclusions to prohibit care (Movement Advancement Project).

Law prohibiting health insurance discrimination based on sexual orientation and gender identity. Transgender exclusions in health insurance service coverage prohibited.
Law prohibiting health insurance discrimination based on only gender identity. Transgender exclusions in health insurance service coverage prohibited.




No law providing LGBTQ inclusive insurance protections.
No law providing LGBTQ inclusive insurance protections. Transgender exclusions in health insurance service coverage prohibited.
Law explicitly permits insurers to refuse to cover gender-affirming care.
6
Many U.S. military veterans are members of the LGBTQIA+ community. During the 17 years “don’t ask, don’t tell” was in effect, an estimated 100,000 were discharged due to their sexual orientation, according to the VA. These “other than honorable” discharges directly impact the services and benefits they are eligible to receive. Although the repeal went into effect in 2011, many still maintain their discharge status. The fight for Transgender rights to serve continues.
Human Rights Campaign
Interview: Ms. P
To further understand the need for gender-affirming care, we interviewed Ms. P (pseudonym for anonymity), who, now in her seventies, has seen a great many changes in the growth of inclusivity, but also sees how far it still must go, especially in healthcare. Ms. P is a transgender woman (she/her) and a retired professional with academic and practical experience in counseling, ministry, and healthcare. Like many transgender individuals, she was acutely aware of her gender identity from a very young age but was unable to comprehend, embrace, or even begin to express this to an adult. It was not until 1981 that she first visited a psychologist after struggling with what was then termed Gender Identity Disorder (GID) and related issues of mental health. She has survived suicidality twice, during puberty and again as an adult, exacerbated by the humiliation of being outed within a professional and religious context. She started medical transition in 1993 and received gender-affirming surgery in 1996. Ms. P believes such services are life-extending per the individual needs and situational experiences of transgender persons. Since her transition, she has endured various unsupportive and disrespectful experiences during vulnerable moments of medical and social need. One instance she recounted was when she suffered a kidney stone and sought emergency medical care. During the physical exam, her attending emergency department physician hesitantly stopped short of her pelvis and “became physically repulsed,” she said, averting eye contact and backing away from her. She recalled that he told her that “[he’d] never treated someone like [her] before.” Following diagnostic imaging, she said the doctor only communicated with a thumbs-up gesture extended through a slightly opened door, not speaking directly to his patient again. (Ms. P, March 14, 2022).
When asked about how architectural design has impacted her life, Ms. P had many insights to share. One key area of discussion was bathrooms. She said bathrooms are particularly hard for those who are starting to transition or presenting differently. Recounting times of perceived tensions and anxiety, she mentioned that many occurred while sharing sink and mirror locations with onlookers. For a more inclusive design, she suggested sinks and mirrors be placed within stalls for more privacy. Another suggestion was to provide unisex, single-stall toilets as an option where possible. For larger multi-stall restrooms, other thoughts include eliminating urinals due to privacy and difficulty of use by many transitioning individuals, or to create floor-to-ceiling, fully private stalls.
Dressing areas and locker rooms are other areas where design can improve experience. Ms. P recalled when she was younger that male dressing areas, locker rooms, and showers were open and communal, which was extremely uncomfortable and only amplified the underlying dysphoria and the anxiety of being teased or worse. She encourages the use of private dressing rooms and individual shower stalls for everyone’s privacy and comfort. Areas where people may feel singled out or on display should be avoided. Gowned areas in healthcare facilities should be as private as possible, with smaller seating groups.
For supportive healthcare and social services, Ms. P recommends access to specialties such as aesthetic dermatology, urology, gynecology, internal medicine, endocrinology, cosmetic surgery, and behavioral health. Many of these impact transgender people differently than cis-gendered people. Additionally, inclusions such as education, family support, and social services are important to reduce stigmatization and fully support the needs of patients, clients, and family and friends.
Ms. P’s experiences with gender dysphoria and being acutely aware of perceptions, even before her transition, influenced how she hopes healthcare access and awareness can improve. It is important to her that everyone feels comfortable and supported in their environments and experiences.
7

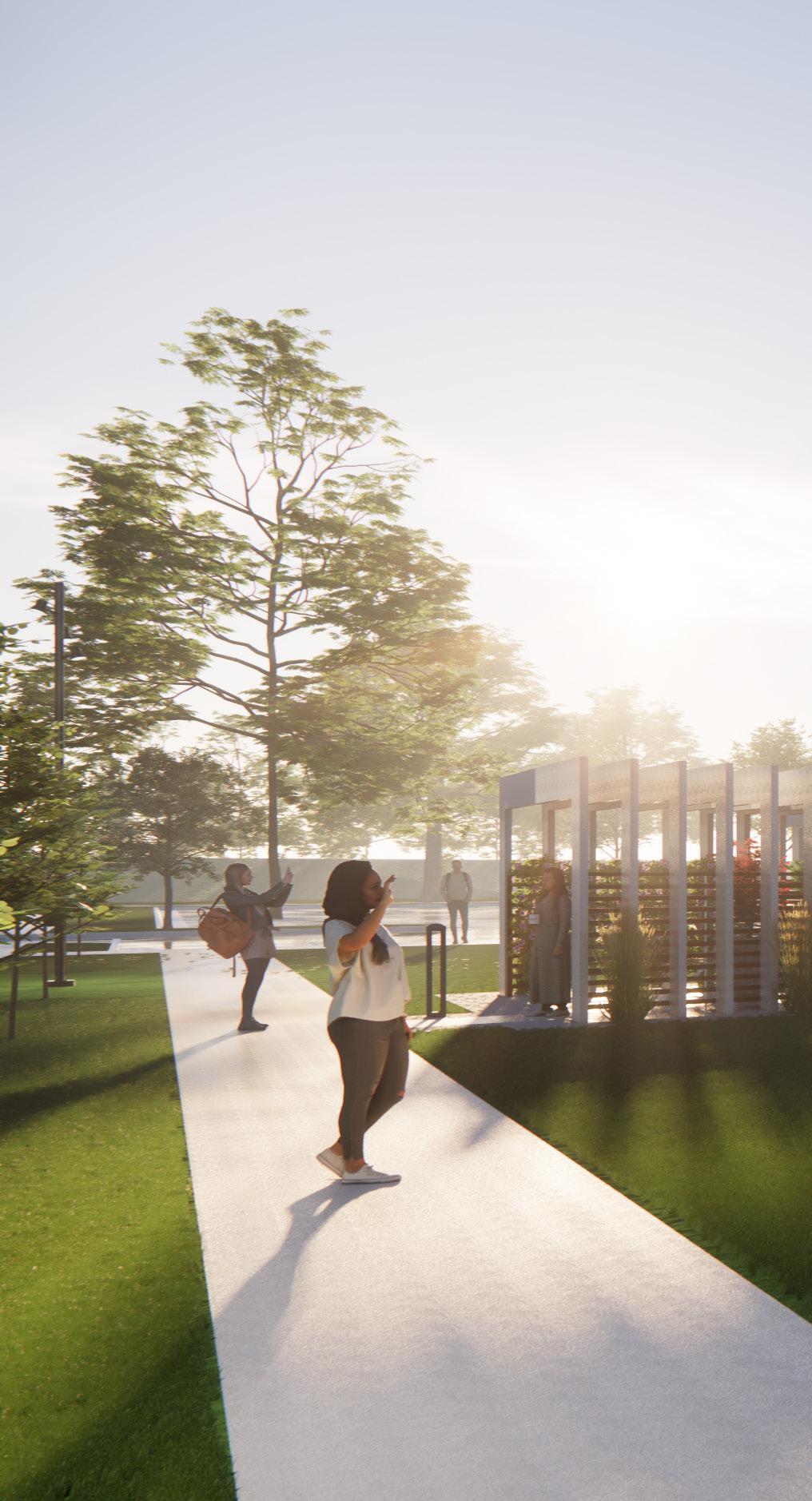
Prism Wellness and Community Center Main Entry and Community Patio

Prototype: Design Narrative
Our design team has explored the creation of an inclusive prototype facility that promotes the physical and mental health and wellness of the LGBTQIA+ community and works to reduce stigma and judgment within society. We hope the concepts presented will provide insight for consideration to ultimately reduce barriers to care and stimulate solutions for inclusive design. We have researched and studied the existing care sites previously discussed, held interviews with multiple members of the LGBTQIA+ community, and used research-based design principles to create a multi-faceted facility that celebrates the culture and identity of those it will serve. This prototype demonstrates a model that can apply to various locations and is adaptable to specific community needs.
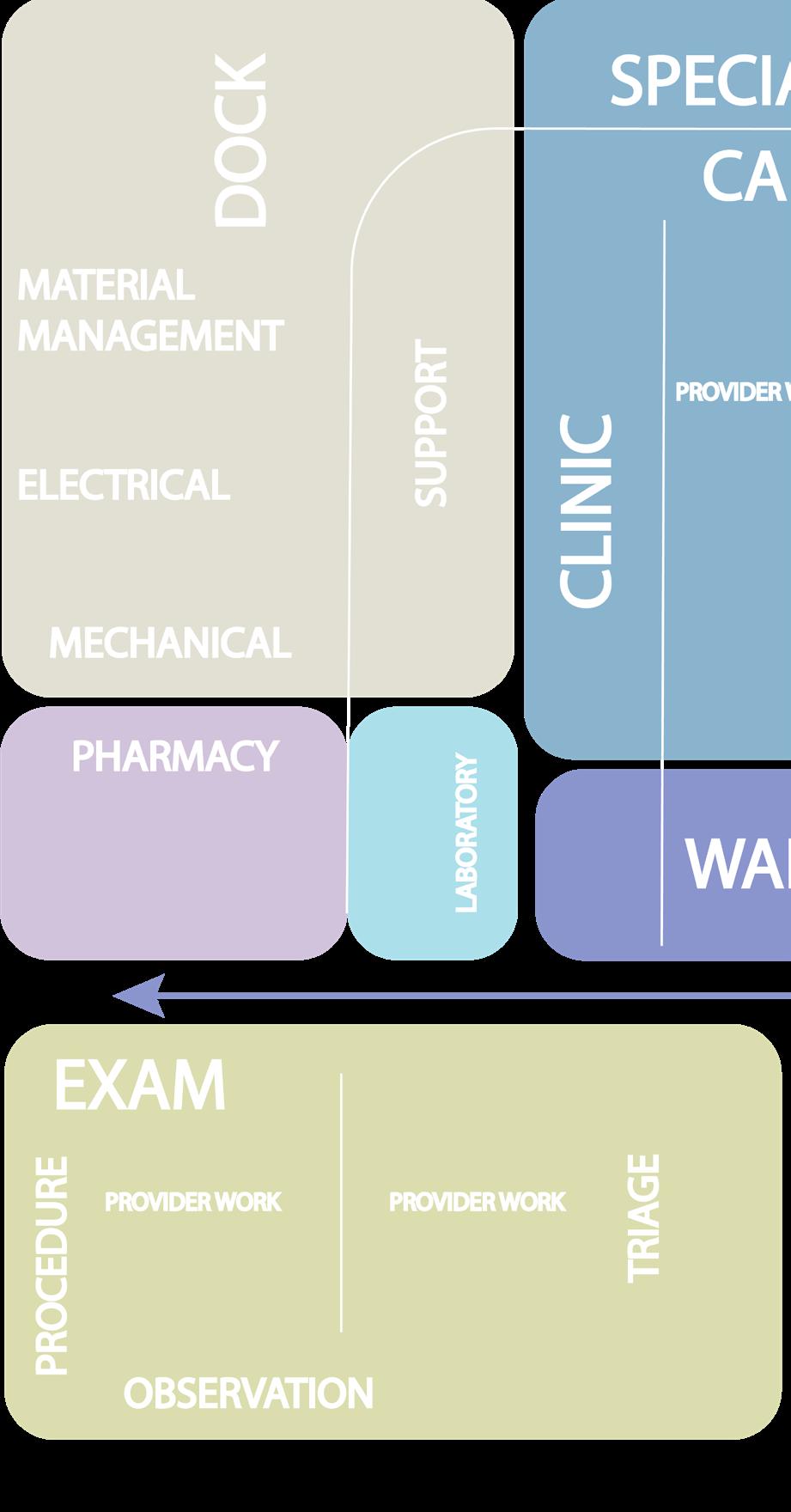
The Prism Wellness and Community Center concept is a single-story, 57,000 SF space that includes clinics, a micro lab, a retail pharmacy, urgent care, advocacy offices, a center for the unhoused, a café, retail, and education. Other amenities of note are the behavioral health crisis and observation area, community room, safe lounge, education center, salon, and outdoor activity spaces.
PRISM WELLNESS AND COMMUNITY CENTER
Primary Care/Patient Centered Medical Home
Specialty Care
▪ Urology
▪ Breast Care
▪ Gynecology
▪ Dermatology
▪ Fertility
▪ Voice and Speech Therapy
▪ HIV/AIDS Care
▪ Medication Support
▪ Cosmetic Surgery
Behavioral Health
Administration
Advocacy Support
▪ Adoption Services
▪ Social Work
▪ Legal Counseling
Unhoused Center
Urgent Care and Crisis Care
LaboratoryPharmacy (Drive Thru)
Education
Support Services
Patient, Staff and Community Amenities
9
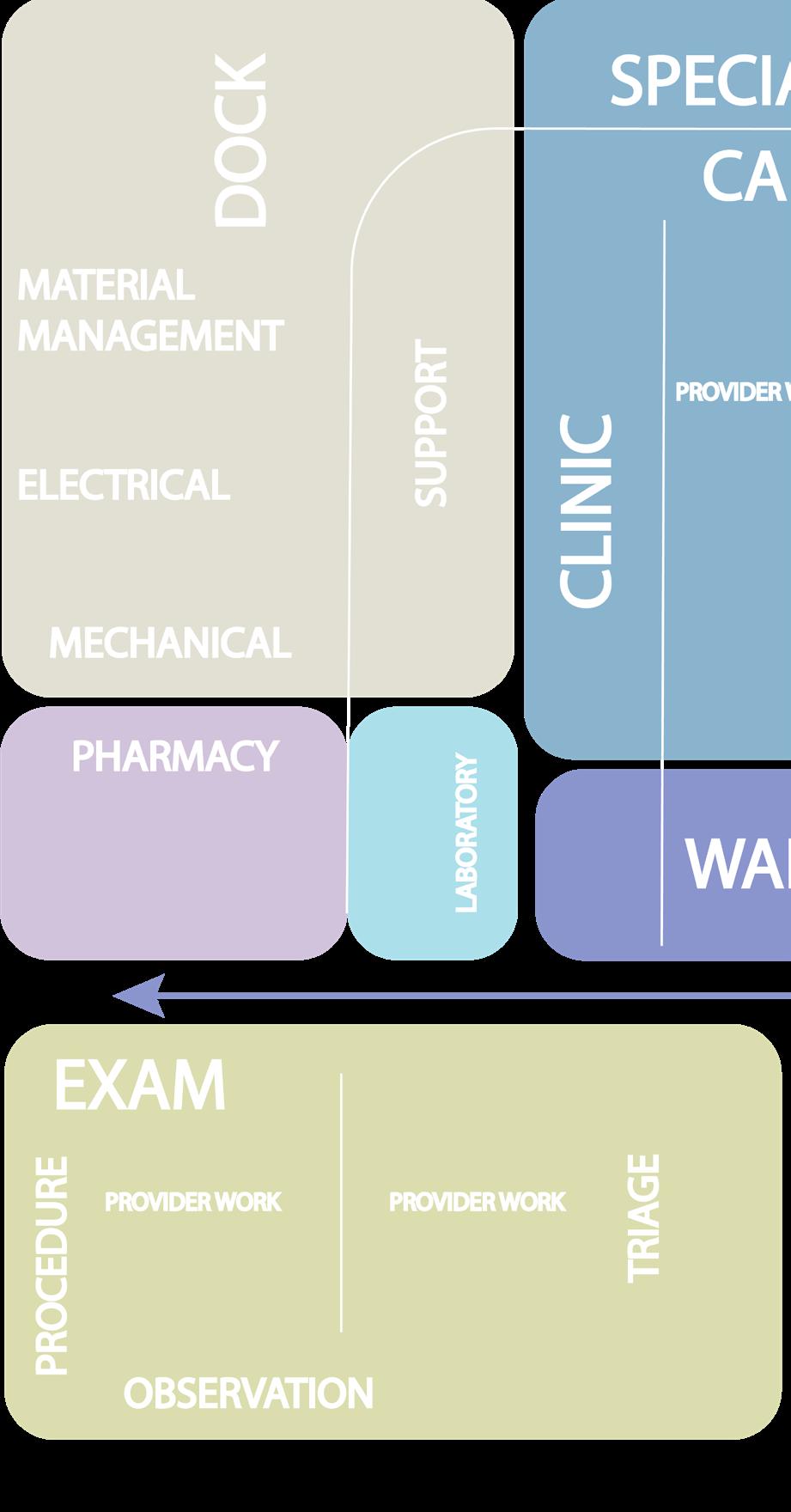
The prototype’s main clinic modules are primary care, behavioral health, specialty care, and Urgent or Crisis Care. The healthcare clinics are modular and surround a collaborative care teamwork area. Each has direct access to clinical support, ancillary services, and staff respite space. Other features such as outdoor seating, operable walls, and public access points allow for wider community engagement.
The Primary Care Clinic addresses general wellness and treatments for common illnesses for all ages. Exam rooms are private and surround a central multi-disciplinary work area for staff to collaborate. Rooms are equipped to include telehealth services and can easily be adapted for other uses. The clinic module allows for flexibility within and between departments with consistent locations of common support spaces. As healthcare needs in the community grow and change, the module allows for equipment and furniture to be moved or replaced without needing to remodel or redesign rooms. The racetrack format is also part of the module and creates intuitive wayfinding and optimal locations for staff work areas.
The Behavioral Health Clinic provides general mental and emotional wellness for all ages with additional resources for substance abuse and short-term outpatient care. Provider offices and exam rooms are oriented for safety and egress. Educational classrooms and a central group room are available for learning, group and family therapy, and other care activities, such as art and expressive therapy.
The Specialty Care Clinic provides auxiliary services in conjunction with primary and behavioral health that impact this patient population uniquely throughout their lives. Urology, breast care, gynecology, dermatology, fertility, voice/speech therapy, and HIV/AIDs care are offered within the clinic to serve patients better and more conveniently. By co-locating these services, staff can collaborate closely with other providers in caring for the whole person’s specific needs and sensitivities.
The Urgent and Crisis Care Clinic will serve as a medical triage and treatment option for the larger community. Since mental health is an important consideration, observation, behavioral health, and crisis stabilization are also provided. Provisions to ensure mental and physical safety, such as options for communal and private rooms and direct sightlines to staff work areas, are carefully considered in the design. Testing for substance abuse can be done within the urgent care clinic with convenient access to the micro lab and retail pharmacy.
In addition to the care clinics mentioned above, ancillary support services such as a small lab and drive-through retail pharmacy can fulfill basic pointof-care testing and medication distribution in a more private and sensitive manner. A consult room will allow pharmacists to have private discussions with patients and family members about any new or changing medications or dosages. Personal items, sexual health protection, and unique vaccinations and medications for the LGBTQIA+ community can also be addressed. Other services in The Prism Wellness and Community Center concept include administration, community education, social services, advocacy services, and an unhoused housing assistance and outreach center. The intention is to provide services tailored to supporting clients and attending to the physical, emotional, and social needs of everyone.
DEPARTMENT LEGEND

ADVOCACY
BUILDING SUPPORT
CAFE
EDUCATION
UNHOUSED CENTER
LABORATORY
LOBBY
MENTAL HEALTH CLINIC
OFFICE
PHARMACY
PRIMARY CARE CLINIC
RETAIL
SITE
SPECIALTY CLINIC
URGENT CARE
10

Neighborhood and Built Environment Health and Healthcare Social and Community Context Education Economic Stability
Adapted from Healthy People 2020
11
Prototype Clinic Services based on Social Determinants of Health

12
Prototype: Floor Plan
ADVOCACY
BUILDING SUPPORT
CAFE
EDUCATION
UNHOUSED CENTER

LABORATORY
LOBBY
MENTAL HEALTH CLINIC
OFFICE
PHARMACY

PRIMARY CARE CLINIC
RETAIL
SITE
SPECIALTY CLINIC
URGENT CARE

13
DEPARTMENT LEGEND
Prototype: Site Plan
Outdoor Social Spaces for Patient, Staff and Community Interaction
Service Entry and Loading Dock
Staff Parking
Private and Accessible Drive-Through Pharmacy with Exterior Community Access
Urgent Care | Crisis Care with Exterior Community Access
Patient and Public Parking

14
Outdoor Labyrinth for Meditation
Outdoor Pavilions for Respite and Reflection
Outdoor Lawn for Community and Therapy Activities
Administrative Suite with Private Exterior Access
Staff Parking
Center for the Unhoused with Private Exterior Access
Savoy Salon and Boutique Offering Affirmation
Consultant Services and Specialty Items
Kiki Cafe with Exterior Community Access

Community Dog Park and Service Animal Support
Bike Racks
Public Transportation Access
15
Prototype: Design Considerations
In addition to the services needed to support health and wellness care of the LGBTQIA+ community, four key themes emerged in the design of the prototype: affirmation and celebration of culture; reduction of stigma; privacy, safety, and accessibility; and community connectivity.

16
Prism Wellness and Community Center Savoy Salon and Boutique

Affirmation and Celebration of Culture
Identity is a basic human need. Our experiences, our history, and our values shape us. Our physical and emotional expression of that identity is inherent in our health and well-being. A person’s health is optimally maintained when physical, mental, and social care are congruent across all demographics. Holistic personal care is driven by a head-to-toe, outside-in approach to wellness care. It is not enough to address basic physical ailments. It is critical the facility is designed to not only acknowledge and accept the LGBTQIA+ community, but to celebrate and affirm its members and culture.
Features using bold color and light act as wayfinding elements inside and outside, reflecting the iconic rainbow, a well-known symbol of pride for the LGBTQIA+ community since 1978. In the main lobby, a dynamic history wall depicts culturally and socially significant gender, sexual, and romantic minority (GSRM) movements that have occurred throughout the years. Fabrics and artwork chosen from celebrated LGBTQIA+ artists are featured throughout, reflecting serenity, healing, and inclusivity. Display space is provided to highlight patients’ artwork created as a part of treatment.
The Savoy Salon and Store, named after the historically significant ballroom known for its LGBTQIA+ community gatherings during the Harlem Renaissance, provides hair and nail services; a clothing shop with specialty items such as bindings and wigs and educational services offered with the express purpose of addressing the exterior portion of gender-affirming care. Supporting the ability to express oneself freely will contribute to overall health and identity. Retail services are co-located in one large area divided by a welcome and check-in desk. Nail technicians and hair stylists will function as they would at any salon, while the retail clothing and bookstore will have affirmation consultants to help clientele with different presentations and resources. The dressing area has single rooms with floorto-ceiling panels and integral mirrors for those who prefer privacy. Others may prefer to embrace their identity expression and strut. Large mirrors and a fashion runway lead out to the retail space to celebrate the individuality and uniqueness of each client. These amenities are available from within the PRISM building and from the street to allow for after-clinic-hours operations, if desired, and to serve the greater community.
17
Reduction of Stigma
The element of stigma must be addressed to create positive change in acceptance and access within the GSRM community and the community at large. The first step to connection is education. Learning about one another will foster understanding and the desire to come together. Strategies to reduce stigma hinge on education and outreach within and outside of the LGBTQIA+ community to combat misinformation and prejudice.
Spaces that foster and support education are distributed throughout the clinic. Two large classrooms are provided in the main lobby for activities such as afterschool programs, family classes, GED classes, sex education, first responder/law enforcement training programs, etc. These are expandable to cater to different groups. The community room is large enough to host conferences, parties, and events to increase understanding and engage public support of important causes. It features an operable wall, allowing events to open onto the entry courtyard. The Savoy Salon and Store contains books and educational materials. Additional locations for reading material and personal interaction opportunities are located throughout, encouraging curiosity and inclusivity in lieu of separation and judgment.
To address the disproportionate rate of homelessness within this group, an unhoused center is provided for those who need help finding resources for hygiene, weather-appropriate clothing, or counseling. Locations for personal belonging storage and service animal relief are present. The center has public access from the exterior to encourage use, and is disconnected from the healthcare clinic, quelling fears of overpayment or medical insurance issues. It functions purely as a space of support and advocacy.
Similarly, an office suite dedicated to advocacy services is available for community use. Because of ever-changing laws and bans, procedures and services easily accessible for some in the community may be increasingly complicated. Offices dedicated to legal counseling, social services, adoption consulting, financial aid services, case management, and insurance counseling are provided to help with possible obstacles.

18

19
Prism Wellness and Community Center Lobby and LGBTQIA+ History Wall

Door opens away from table
Controllable
Lighting Options
Privacy Curtain
Tele-health
Capable
Exam table foot oriented away from door

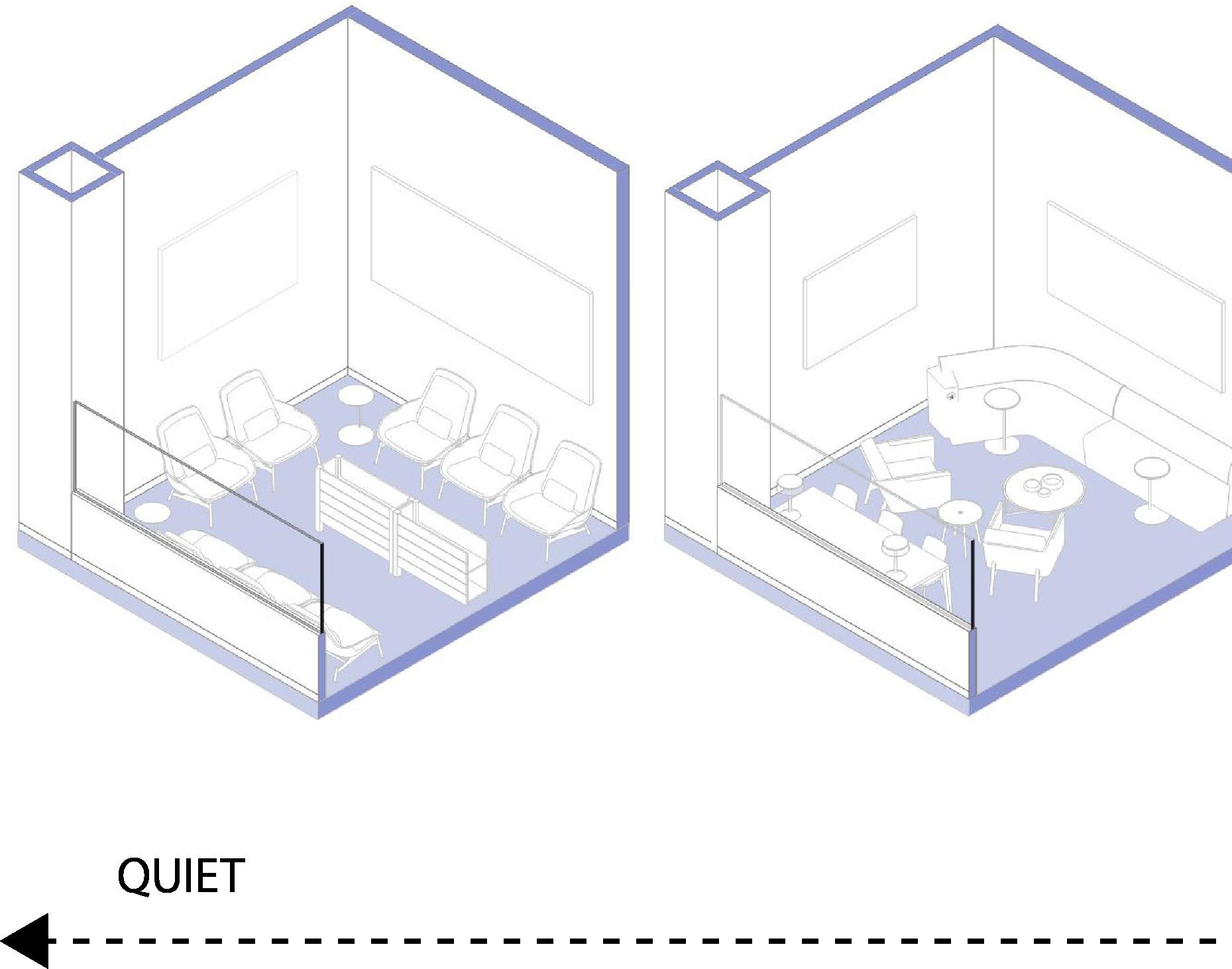
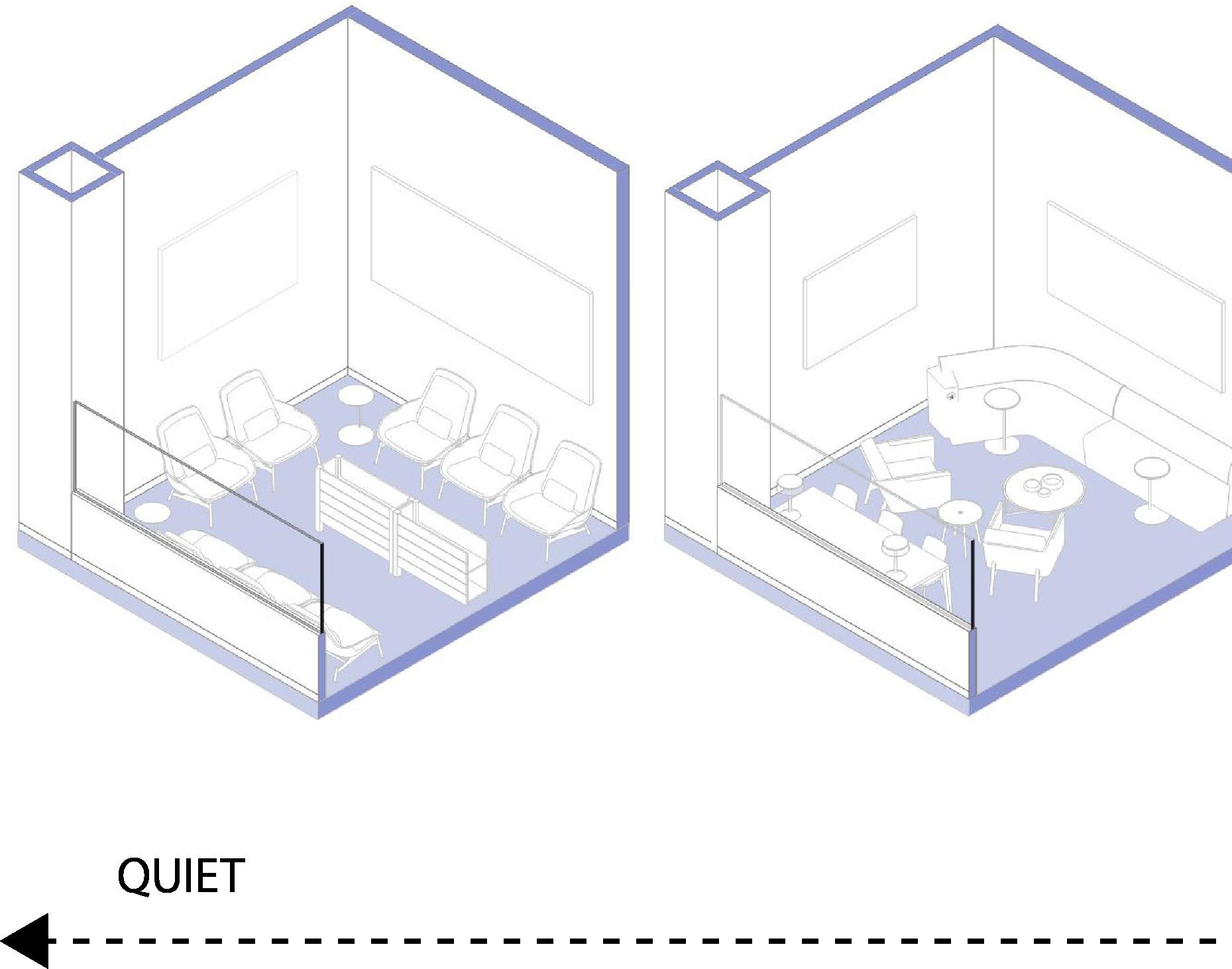
WAITING ROOM FEATURES
▪ Controllable Lighting Options
▪ Varied Size and Style of Seating Clusters
▪ Options that Protect the Back
▪ Translucent Panels for Visibility and Privacy
▪ Moments of High, Medium and Low Stimulation
▪ Variety of Spacial Volume for Choice
▪ Opportunities for Artwork, Education and Positive Distraction
▪ Adaptable Multipurpose Furnishings
▪ Operable Partitions for Flexibility
▪ Wayfinding Elements
▪ Autonomy of Choice in Environment
20 EXAM ROOM GENDER NEUTRAL TOILETS
WAITING ROOM VARIETY
Walls instead of Stalls
Individual Mirrors
Hangers for Bags
Physical Accessability
Doors for Privacy
Toilets instead of Urinals
Privacy, Safety and Accessibility

Three critical considerations within this community are privacy, safety, and accessibility. These needs are not always met for the GSRM group, which can have a tremendous impact on health and wellbeing. Auditory and visual privacy is extremely important to maintain, as people should trust that their conversations and health information are protected. A breach of this trust can be detrimental to one’s care experience. For example, exam, treatment, and intake spaces are acoustically treated to prevent sound transmission. All exam and consult rooms are private. Exam tables are turned so the foot faces away from the doors, which open away from the table, and are surrounded by privacy curtains. Visual privacy is prioritized in restrooms and changing rooms. Private toilets within the departments are unisex and meet physical accessibility standards, with only staff or patient identification to distinguish them. In the public toilets in the lobby, stalls are removed in favor of toilet rooms with doors and walls. No urinals are provided in the facility. The dressing rooms within the retail store are private rooms with individual mirrors and the option to use a larger, shared mirror. Waiting rooms vary in size, scale, and openness to allow for patient choice.
For some, safety is a more pressing need. Those who have been exposed to violence or abuse may prefer the visibility of staff and their surroundings to feel safe. A variety of spaces project a place of safety and inclusion. The reception desk in the entry is prominently displayed for observation and assistance. An adjacent open lounge provides an area for positive distraction within eye and earshot of staff. The front façade of the building allows visibility to public transportation and waiting and parking areas. Safety precautions extend to staff, as well. Considerations for mental and behavioral health design apply, such as avoiding dead-end hallways, orienting offices for staff to be able to quickly escape, the inclusion of panic buttons, and access control. Ideally, security features are well integrated into the architecture, yet provide occupants reassurance.

21
Accessibility, in any type of design, is more than just physical compliance. Accessibility means providing as many resources as possible to cast the widest outreach net. It means accommodating many kinds of patient populations, cultures, languages, and abilities -- even those who don’t step through the door. Everyone is treated with the same dignity, equitable accommodation, and mutual respect.
Examples of accessibility can be seen in the drive-through pharmacy and urgent care. The retail pharmacy serves clientele already in the building, but to expand the accessibility of pick-up and drop-off services, a drivethrough was added. This allows patients to pick up prescriptions or basic medical supplies conveniently, and physically disabled or recovering patients to remain in their cars. Urgent care is an accessible resource open to patients of the facility and the larger community. It serves as an alternative to emergency centers for anyone who needs triage or crisis care services without an overnight stay. Additionally, urgent care can function independently from the rest of the facility and stay open after hours if needed. Other elements include clear wayfinding not solely dependent on written language, avoiding high-contrast flooring for those with poor eyesight, providing active and passive environments for choice, language support, and a hygiene center with a shower and washer and dryer. Healthcare is constantly seeking to grow and adapt within and outside the hospital doors and the LGBTQIA+ community has been historically left out of those benefits. To bridge the gap, healthcare services must be available to everyone, regardless of their identity.

22

23
Prism Wellness and Community Center Drive-Through Pharmacy
Community Connectivity
A connection to the community is essential for not only LGBTQIA+ individuals but also for the communities in which they live. The PRISM model does not look to exclude non-members. In contrast, it aims to be an open and supportive environment for everyone to come together collectively. Many of the amenities provided are intended to be available outside the clinic’s normal business hours. At the entry, the communal front porch offers seating and play. The community room wall can open out onto the patio for social events. The Kiki Café, a common slang term for “gathering with friends for chit-chat,” and lounge provide safe areas for daily activity, interaction, and engagement in a supportive and welcoming environment. The Savoy Salon and Store have exterior public access allowing anyone to enter, similar to other retailers.
As we know from evidence-based design research, access to nature and daylight are critical to healthy and therapeutic environments. Outside of the building, ample green spaces are provided for activity and respite. An enclosed bus shelter is nearby for public transportation access. A walking path encourages movement and physical wellness. These elements are intended to be used by neighborhood members as well, reducing stigma through shared experiences and education. In addition to public and patient amenities, an outdoor respite area for staff is available near a secure private entry. From the inside out and outside in, the facility is designed to embrace the LGBTQIA+ and neighboring communities.

“The AIDS crisis in the 1980’s and 1990’s shined a light on how illness can affect the queer community uniquely, but diverse people need diverse healthcare to address every aspect of LGBTQIA+ wellness.”
- Lisa Ulibarri
24

 Prism Wellness and Community Center
Outdoor Social Space
Prism Wellness and Community Center Outdoor Labyrinth and Pavilions
Prism Wellness and Community Center
Outdoor Social Space
Prism Wellness and Community Center Outdoor Labyrinth and Pavilions
Advocacy
With the current climate surrounding the LGBTQIA+ community and gender-affirming care, advocacy has become key in battling misinformation and ensuring that healthcare is available for all. Many medical organizations support and recognize the necessity for more resources and appropriate care. Organizations including the American Academy of Pediatrics, American Heart Association, American Medical Association, World Medical Association, and American Public Health Association have maintained that specialized and gender-affirming healthcare is real and saves lives (Transgender Legal Defense & Education Fund). Local advocacy groups are a way to find resources and connect to providers that can help, especially in states enforcing bans. In Texas, The Resource Center has its own advocacy team that works within the Dallas Independent School District, the city of Dallas, and Dallas County to educate and inform on topics and programs that impact the LGBTQIA+ community. They promote upcoming projects, such as a new LGBTQIA+ affirming senior housing complex, that will expand the network of resources they provide. Larger organizations such as the Gay, Lesbian & Straight Education Network (or GLSEN), National Center for Transgender Equality, the Trevor Project, and Out Youth work within different facets of cities and states to protect access to holistic and affirming care.
Conclusion
Specialized and gender-affirming healthcare is in its infancy. As more people try to find patient-centered care, the demand for design that is supportive and accepting of LGBTQIA+ people will grow. While there are a few clinics around the United States that cater to the specific needs of the LGBTQIA+ community, there continue to be barriers for easily accessible care in many states. The need to address health from a full-body wellness and community-supported approach is gaining popularity, especially with the continued rise of behavioral health concerns in youth and adults. As Ms. P said, architectural design has a significant impact on the perception of a safe and welcoming environment and there are many ways we can improve. Through holistic personal care, thoughtful and empathetic design elements, accessibility, privacy, and community connection, design professionals can create an inclusive, affirming facility that educates and advocates for the LGBTQIA+ community.

Prism
Main
Wellness and Community Center
Entry and Open Lounge
Research Links
▪ https://outsidein.org/
▪ https://www.cincinnatichildrens.org/service/t/transgender
▪ https://myresourcecenter.org/
▪ https://www.hrc.org/resources/attacks-on-gender-affirming-care-by-state-map
▪ https://www.texastribune.org/2023/06/02/texas-gender-affirming-care-ban/
▪ https://www.nytimes.com/2022/03/08/health/texas-transgender-clinic-genecis-abbott.html
▪ https://www.kff.org/other/issue-brief/youth-access-to-gender-affirming-care-the-federal-and-state-policy-landscape/
▪ https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx
▪ https://www.thetrevorproject.org/survey-2022/
▪ https://transhealthproject.org/resources/medical-organization-statements/
▪ https://www.rxsaver.com/blog/10-organizations-supporting-transgender-and-gender-non-conforming-communities
▪ https://www.ncbi.nlm.nih.gov/books/NBK563176/#article-125326.s3
▪ https://legacy.npr.org/documents/2017/nov/npr-discrimination-lgbtq-final.pdf
▪ https://www.scientificamerican.com/article/where-transgender-is-no-longer-a-diagnosis/
▪ https://aspe.hhs.gov/sites/default/files/2021-07/lgbt-health-ib.pdf
▪ https://www.whijournal.com/article/S1049-3867(17)30599-6/abstract#articleInformation
▪ https://www.lgbtqiahealtheducation.org/publication/understanding-health-needs-lgbt-people/
▪ https://health.mil/Military-Health-Topics/Centers-of-Excellence/Psychological-Health-Center-of-Excellence/CliniciansCorner-Blog/LGBTQ-Pride-Month-Serving-All-Who-Serve
▪ https://www.americanprogress.org/article/lgbtq-military-members-and-veterans-face-economic-housing-and-healthinsecurities/
▪ https://www.lgbtmap.org/equality-maps/healthcare_laws_and_policies
Acknowledgements
AUTHORS


EXTERIOR DESIGN


INTERIOR DESIGN


27
Lisa Ulibarri LEED Green Associate
Hilary Bales AIA, ACHA, EDAC
Ricardo Muñoz AIA
Eric Enriquez
Aimee Burmaster-Hicks IIDA
Sarah Trinh LEED Green Associate
pagethink.com
 One of a series of white papers by Page professionals Lisa Ulibarri, LEED Green Associate and Hilary Bales, AIA, ACHA, EDAC
One of a series of white papers by Page professionals Lisa Ulibarri, LEED Green Associate and Hilary Bales, AIA, ACHA, EDAC

































 Prism Wellness and Community Center
Outdoor Social Space
Prism Wellness and Community Center Outdoor Labyrinth and Pavilions
Prism Wellness and Community Center
Outdoor Social Space
Prism Wellness and Community Center Outdoor Labyrinth and Pavilions






