






DHShas released its first annual report on how the No Surprises Act is impacting health care markets, and the results are both surprising and expected.
Among the crucial findings are the decrease and concentration of out-of-network billing, both claims and the total amount associated with those claims; trends regarding changes in hospital ownership; and horizontal consolidation and pass-through costs to consumers
Join us as we analyze the findings and what they mean to the industry going forward We will also discuss the key factors that play a role in the DHS?evaluation of NSA and what they might mean for market trends, consolidation, and out-of-network billing.

Leading the series is CorroHealth?s resident subject matter expert, Barbara Johnson, BSN, RN ? Senior Revenue Consultant. As a registered nurse Johnson worked in emergency medicine before transitioning into nursing administration She entered the specialty of Revenue Integrity as a nurse auditor where she expanded her knowledge of coding and revenue cycle compliance through membership in AAPCand HFMA Today, she is CorroHealth?s leading subject matter expert on NSA.

You can cat ch up here!
CorroHealth?s ?No Surprises Act and Price Transparency, a New Monthly Series?was created to provide attendees with clarity around No Surprises Act, to answer questions, and get you on the best path for success The series also clarifies payers?increased role in the process, the status of impactful legislation, and the processes providers should follow to comply


Contact Your State's Account Executive.




Quest ion:
With PAMA moving reporting period to January - March, 2024, would you suggest we wait to report any data for any regulatory changes between now and then?

Answ er:

It is not yet possible to submit lab payment data to CMS, as the online reporting portal is not open and will not be opened until the reporting period begins.
Late last year, Congress delayed (for the fourth time) the reporting period for payment data collected in 2019 to the first quarter of 2024. Meanwhile, a bill titled the Saving Access to Laboratory Services Act (SALSA) has been re-introduced into both houses of Congress; the SALSA Act would substantially revise the reporting requirements going forward, and would eliminate reporting the 2019 data altogether The proposed legislation has been referred to congressional committees in both the House of Representatives and in the Senate ? but no hearings have been scheduled to discuss the proposed legislation We may not know the fate of the SALSA Act until the end of this Congressional session.

Our paper regarding the proposed SALSA Act is attached If it is not signed into law, Congress will have to decide whether to extend the reporting period yet again ? but 2019 data is less and less relevant to determine future rates of payment under the Clinical Lab Fee Schedule
CorroHealth will continue to report as information about the SALSA Act and/or the next data reporting period comes to light. Please keep reading our eJournal for future updates

On July 7, 2023, in light of the Supreme Court?s decision in American Hospital Association v. Becerra (142 S. Ct. 1896 (2022)) and the district court?s remand to the agency, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule outlining the proposed remedy for the 340B-acquired drug payment policy for Calendar Years 2018-2022.
CMSis publishing this proposed rule to remedy the payment rates the Court held were invalid Aspects of this proposed policy will affect nearly all hospitals paid under the OPPS

This proposed rule will have a 60-day comment period, which will end onSeptember 5, 2023 This fact sheet discusses the provisions of theproposedrule (CMS- 1793-P), which can be downloaded at
https://www federalregister gov/public-inspection/2023-14623/medicare-program-hospital -outpatient-prospective-payment-system-remedy-for-the-340b-acquired-drug CMSanticipates issuing the final rule before the Calendar Year (CY) 2024 Outpatient Prospective Payment System/Ambulatory Surgery Center (OPPS/ASC) final rule is published in Fall 2023.
Section 340B of the Public Health Service Act (340B) allows participating hospitals and other providers to purchase certain covered outpatient drugs or biologicals (hereinafter referred to collectively as ?drugs?) from manufacturers at discounted prices. Prior to 2018, the Medicare payment rate for Part B covered outpatient drugs provided in outpatient hospitals was generally the statutory default of average sales price (ASP) plus 6% In the CY2018 OPPS/ASC final rule that was finalized in 2017, CMSadjusted the payment rate for 340B drugs to ASP minus 22 5%to reflect more accurately the actual costs incurred by 340B hospitals when acquiring 340B drugs.
This rate applied from CY2018 through approximately the third quarter of CY2022. To comply with statutory budget neutrality requirements under the OPPS, CMSmade a corresponding increase to payments to all hospitals (340B hospitals and non-340B hospitals) for non-drug items and services, which was in effect from CY2018 through CY2022
On June 15, 2022, the Supreme Court unanimously ruled that the differential payment rates for 340B-acquired drugs were unlawful because, prior to implementing the rates, HHSfailed to conduct a survey of hospitals?acquisition costs under the relevant statute.
On September 28, 2022, the District Court for the District of Columbia vacated the differential payment rates for 340B-acquired drugs going forward As a result, all CY2022 claims for 340B-acquired drugs paid on or after September 28, 2022, were paid at the default rate (generally ASP plus 6%).
In the CY2023 OPPS/ASCfinal rule, CMSfinalized a general payment rate of ASPplus 6%for drugs acquired through the 340B Program, consistent with the agency?s policy for drugs not acquired through the 340B program As required by statute, CMSimplemented a 3.09% reduction to the payment rates for non-drug items and services to achieve budget neutrality for the 340B drug payment rate change for CY2023.
This budget neutrality change ensured the CY2023 OPPSconversion factor was equivalent to the conversion factor that would have been in place had the 340B drug payment policy never been implemented.
In the CY2023 OPPS/ASCfinal rule, CMSannounced that it would address the remedy for 340B drug payments from CY2018-2022 in future rulemaking prior to the release of the CY2024 OPPS/ASCproposed rule.
In the proposed rule, CMSis proposing to make an additional payment to affected providers for 340B-acquired drugs as a one-time lump sum payment. CMSestimates that for CY2018 through the approximate third quarter of 2022, certain OPPS340B providers received $10.5 billion less in 340B drug payments than they would have without the 340B policy.
CMS is proposing t o m ake an addit ional paym ent t o affect ed providers for 340B-acquired drugs as a one-t im e lum p sum paym ent .
However, many CY2022 340B drug claims have been processed, or reprocessed through standard claims processing, at the higher default payment rate since the 340B payment policy was vacated on September 27, 2022
As a result, affected 340B providers have already received from Medicare and beneficiaries $1 5 billion of the $10 5 billion that would otherwise have had to be remedied through these reprocessed claims For the remaining $9 billion owed to affected 340B providers for claims covering CYs 2018 through 2022, CMSis proposing to make a one-time lump-sum payment to each 340B-covered entity hospital that was paid less due to the now-invalidated policy. The proposed rule contains the calculations of the amounts owed to each of the approximately 1,600 affected 340B covered entity hospitals
Beneficiary copayments make up approximately 20%of the payments affected 340B covered entity hospitals did not receive due to the 340B payment policy Because CMSplans to structure the remedy as a lump-sum remedy payment, providers would not be able to bill beneficiaries for that cost sharing. To account for that fact and to ensure that affected 340B providers are put in as close to the same position as if the 340B payment policy had never existed, Medicare proposes to account for beneficiary cost sharing within the one-time lump sum payment to affected hospitals. Under this proposal, affected 340B covered entity hospitals may not bill beneficiaries for coinsurance on remedy payments.
As part of this proposed remedy, CMSproposes to maintain budget neutrality as required by statute As described above, CMSfinalized the 340B policy for CY2018 in 2017 in a budget neutral manner that included increasing payments for non-drug items and services; this payment increase was in effect from CY2018 through CY2022 CMSestimates that hospitals were paid $7.8 billion more for non-drug items and services during this time period than they would have been paid in the absence of the 340B payment policy Because CMSis now making additional payments to affected 340B covered entity hospitals to pay them what they would have been paid had the 340B policy never been implemented, CMSproposes to make a corresponding offset to maintain budget neutrality as if the 340B payment policy had never been in effect. To carry out this required $7.8 billion budget neutrality adjustment, CMSis proposing to reduce future non-drug item and service payments by adjusting the OPPS conversion factor by minus 0.5%starting in CY2025. CMSproposes to continue making this adjustment until the full $7 8 billion is offset, which CMSestimates to be 16 years
Quest ion:
We are having difficulty billing vaccines while the patient is admitted It is our understanding that it should get billed on a separate claim as a Part B charge to Medicare. Should it get billed as a 121 TOB?That will send the claim out on a swing bed NPI. Is this correct?

Answ er:
You are correct, report the covered preventive vaccine and administration charge on a separate claim, Type of Bill 12X, and reporting the date of discharge as the date of service, whether the patient is in a swing bed or is an acute care inpatient.

Our 2014 paper on this topic is attached; unfortunately, Medicare no longer offers a ?Quick Reference Information: Medicare Immunization Billing?document, but the information in the document is still valid.

Here?s an excerpt (at right top) from the Medicare Claims Processing Manual, Chapter 18 ? Preventive and Screening Services:
https://www cms gov/regulations-and-guidance/ guidance/manuals/downloads/clm104c18pdf pdf
Transitional Care Management (TCM) services play a crucial role in ensuring smooth and successful care transitions for patients moving from an inpatient hospital setting to their home or a community-based care facility. These services focus on coordinating and managing the patient's healthcare following a critical period after discharge. The aim of TCM is to reduce complications, improve outcomes, and enhance patient satisfaction Proper coordination and management of patients during the immediate post-discharge period may also reduce readmissions
KeyComponentsof TCM:
- Face-to-Face Visit
Following a patient's discharge from an inpatient hospital stay, a face-to-face visit is conducted within 7 or 14 days, depending on the complexity of the medical decision-making involved. During this visit, the physician evaluates the patient's medical condition, reviews the discharge summary, reconciles medications, and develops a comprehensive care plan.
- Communication and Care Coordination:
TCM services involve substantial communication and coordination between the physician, patient, and other healthcare providers This includes arranging necessary follow-up appointments, collaborating with specialists, and facilitating communication between the hospital and post-discharge care settings
An important aspect of TCM is reconciling and managing medications during the transition This involves reviewing the patient's medication list, addressing discrepancies, providing education on medication usage, and addressing any potential adverse effects or interactions

The physician, in collaboration with the patient and other members of the healthcare team, develops a comprehensive care plan tailored to the patient's specific needs and goals This plan includes instructions for follow-up care, self-management strategies, and coordination of additional services.
It is important to ensure accurate coding and documentation to support the services provided Here are some key considerations:
- Eligibility: TCM services are typically eligible for Medicare reimbursement Ensure that the patient meets the specific criteria set by Medicare or other payers for TCM services, including a face-to-face visit within the specified timeframes
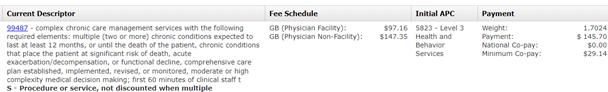
- Documentation: Accurate and detailed documentation is essential to support the medical necessity of TCM services. Documentation must include the complexity of medical decision-making, the coordination efforts involved, medication reconciliation, and the development of a comprehensive care plan Reimbursement: TCM services are typically reimbursed separately from the Evaluation and Management (E/M) services provided during the face-to-face visit Ensure that the appropriate TCM codes are billed separately from any E/M codes to avoid duplication of services See CorroHealth TCM, CCM, RPM, PCM Table.
- Reimbursement: TCM services are typically reimbursed separately from the Evaluation and Management (E/M) services provided during the face-to-face visit Ensure that the appropriate TCM codes are billed separately from any E/M codes to avoid duplication of services See CorroHealth TCM, CCM, RPM, PCM Table
- Reporting:
- Transitional Care Codes 99495 (TCM? within 14 calendar days of discharge) or 99496 (TCM? within 7 days of discharge) may be reported by the same practitioner during the 30-day TCM service period as Chronic Care Management codes 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)
- An RHCand FQHCmay bill TCM services and general care services for the same patient during the same service period if they are reported following the requirements for the code(s) billed.
- Shared or Incident-to-Billing: When performed in a clinic setting, some TCM services may be billed under the supervising physician or as incident-to-services. Understand the billing guidelines applicable to the practice and ensure compliance with the relevant regulations
- Consent: Obtain written consent from the patient for TCM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements.
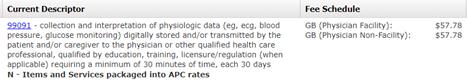
Remote Physiologic (or Patient) Monitoring (RPM) services have emerged as a powerful tool in healthcare, enabling the continuous monitoring of patients?health status and providing timely interventions RPM is a collection and analysis of physiologic data transmitted from the patient electronically to the healthcare provider for assessment RPM allows real-time opportunities for assessment and the ability to view trends over periods of time.
KeyComponentsof RPM:
- Remote Monitoring Devices:

RPM services rely on the use of remote monitoring devices that collect and transmit patient health data. These devices can include blood pressure monitors, glucose meters, pulse oximeters, weight scales, and wearable devices The data collected from these devices is securely transmitted to healthcare providers, allowing for continuous monitoring and assessment
- Data Transmission and Analysis:
RPM services involve the transmission of patient data from remote monitoring devices to healthcare providers or a designated monitoring center. Healthcare professionals review and analyze the data to identify trends, deviations, or any potential health concerns This allows for early intervention and proactive management of the patient's condition
- Care Coordination and Interventions: RPM services enable healthcare providers to coordinate care effectively and provide timely interventions. They can communicate with patients remotely, provide education on self-management, adjust treatment plans as needed, and address any concerns or questions raised by patients The goal is to optimize patient care and improve health outcomes

Consent: Obtain written consent from the patient for RPM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements
- Eligibility: RPM services are typically eligible for reimbursement from Medicare and some private payers Ensure that the patient meets the specific eligibility criteria defined by the payer, which may include having chronic conditions that require ongoing monitoring and management.
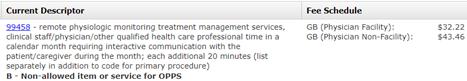
- Time-Based Billing: RPM services are billed based on the total time spent on care management activities during a calendar month This includes the time spent by clinical staff, physicians, or other qualified healthcare professionals in monitoring, reviewing data, and providing interventions. See CorroHealth TCM, CCM, RPM, PCM Table for more information
- Documentation: Accurate documentation is crucial to support the medical necessity of RPM services Document the time spent on care management activities, including review and analysis of data, patient interactions, and interventions provided. Additionally, maintain records of the types of monitoring devices used and the patient's consent for remote monitoring
- Reporting services:
Most RPM services will be billed under service codes 99453/99454 and time-based codes 99457/99458
99453 (remote monitoring of physiologic parameter? .initial setup and patient education on use of equipment) may only be billed one time per patient
A provider may only bill 99454 (remote monitoring of physiologic parameters) one time per month regardless of how many devices are monitored. Reporting 99454 requires transmission and reading performed at least 16 days during the month
99458 (remote physiologic monitoring treatment management services? each additional 20 minutes) may be reported up to two times per month (once at 40 minutes, next at 60 minutes) after 99457 (remote physiologic monitoring treatment management services? each first 20 minutes) has been billed RPM codes may be reported during the same service period as CCM (99487-99490), TCM (99495-99496)

- Communication and Interactivity: To bill for RPM services, there must be interactive communication between the patient or caregiver and the healthcare provider This may include phone calls, video visits, or secure messaging platforms. Ensure that these interactions are properly documented.
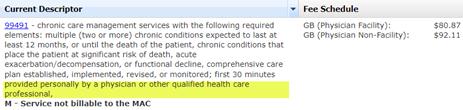
Chronic Care Management (CCM) services play a vital role in providing comprehensive and coordinated care for patients with chronic conditions These services aim to improve patient outcomes, enhance patient engagement, and reduce healthcare costs associated with managing chronic illnesses.
KeyComponentsof CCM:
- Care Planning and Coordination: CCM services involve the development of a personalized care plan tailored to the patient's chronic conditions. This plan encompasses an assessment of the patient's health needs, the establishment of goals, and the coordination of care across multiple healthcare providers Care coordination may include regular communication, scheduling appointments, and sharing health information to ensure a seamless healthcare experience
- Communication and Remote Patient Monitoring (RPM):
Effective communication between healthcare providers and patients is crucial for successful chronic disease management CCM services often involve regular telephone or electronic communication between the patient and the healthcare team Additionally, the use of remote patient monitoring devices, such as blood pressure monitors or glucose meters, can provide valuable data to assess the patient's condition remotely
- Medication Management:
Ensuring proper medication management is essential in chronic care CCM services may include medication reconciliation, monitoring adherence, and providing education to patients about their prescribed medications This component helps optimize medication regimens, minimize adverse effects, and improve treatment outcomes.


CCM services aim to provide patients with increased access to care and enhance continuity. This includes same-day or next-day appointments for urgent needs, extended office hours, and 24/7 access to healthcare providers for urgent issues
Timely access to care helps manage exacerbations, address concerns, and prevent unnecessary emergency department visits.
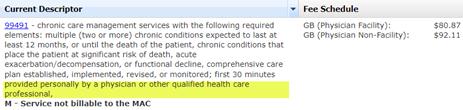
- Eligibility: CCM services are typically eligible for Medicare reimbursement. Ensure that the patient meets the specific criteria outlined by Medicare or other payers for CCM services, such as having two or more chronic conditions that are expected to last at least 12 months An initiating visit is required for patients who have not seen the billing practitioner within the past 12 months
- Time-Based Billing: CCM services are billed based on the total time spent on care management activities during a calendar month. This includes both the time spent by the physician or other qualified healthcare professional and the clinical staff. CCM services are not typically face-to-face but require a minimum of 20 minutes of services before billing. See CorroHealth TCM, CCM, RPM, PCM Table for more information.
- Documentation: Accurate and detailed documentation is crucial to support the medical necessity of CCM services. Document the time spent on care management activities, details of care coordination efforts, medication management, and patient communication
- Reporting Services:
- CCM initial visit may be a Face-to-face evaluation and management visit, an Annual Wellness Visit (AWV), or an Initial Preventative Physical Exam (IPPE) for a patient the billing practitioner has not seen in the previous 12 months The practitioner must discuss the CCM with the patient If the initiating visit requires a comprehensive assessment and care planning, G0506 (Comprehensive assessment of and care planning by the physician or other qualified health care practitioner for patients requiring CCM services (billed separately from monthly care management services) (Add-on code, list separately in addition to primary service) may be billed as part of the initiating visit
- Both complex and non-complex CCM services cannot be reported for the same patient during the same calendar month 99491 (CCM? multiple? first 30 minutes provided personally by a physician or other healthcare professional) may not be reported in the same calendar month as 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)
- Time included in a CCM service cannot be counted towards other billed time-based codes
- Transitional Care Codes 99495 (TCM? within 14 calendar days of discharge) or 99496 (TCM? within 7 days of discharge) may be reported by the same practitioner during the 30-day TCM service period as Chronic Care Management codes 99487 (CCM? multiple? first 60 minutes of clinical staff time directed by a physician or other qualified healthcare professional), 99489 (CCM? multiple? first 30 minutes of clinical staff time directed by a physician or other qualified healthcare professional) or 99490 (CCM? multiple? first 20 minutes of clinical staff time directed by a physician or other qualified healthcare professional)
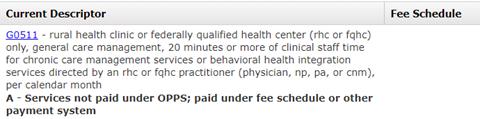
- RHCs & FQHCs may report general care management once per month using G0511 for 20 minutes or more of clinical staff time devoted to TCM, CCM, PCM, chronic pain management (CPM) or Behavioral Health Integration (BHI) services provided by a qualified healthcare professional
- Consent:
Obtain written consent from the patient for CCM services, explaining the scope and nature of the services, that only one practitioner (per month) may furnish and bill the CCM services The patient should be notified of cost-sharing requirements

Principal Care Management (PCM) services are designed to furnish care to CCM patients who may have one or more chronic conditions with a focus on improving a single high-risk condition. PCM services involve the coordination and management of a patient's healthcare needs across multiple providers, ensuring continuity and seamless transitions between different care settings
KeyComponentsof PCM:
- Care Coordination:
PCM services involve coordinating and integrating healthcare services across different providers and settings. This includes facilitating communication between healthcare professionals, scheduling appointments, arranging necessary tests or procedures, and ensuring the timely exchange of medical information Effective care coordination enhances patient safety, reduces duplicative tests or treatments, and promotes the delivery of appropriate and timely care
- Patient Education and Self-Management Support:

PCM services emphasize patient education and self-management support to empower patients in managing their health conditions This component includes providing education on medication adherence, lifestyle modifications, symptom management, and self-monitoring techniques. By equipping patients with the knowledge and skills to actively participate in their own care, PCM services promote better health outcomes and improved quality of life
- Care Plan Development and Review:
PCM services involve the development and regular review of a comprehensive care plan tailored to the patient's specific needs and goals. The care plan includes a summary of the patient's health conditions, treatment goals, medication list, and recommended interventions. Regular review and updates to the care plan ensure that it remains relevant and aligned with the patient's evolving healthcare needs.
- Medication Management:
Effective medication management is a critical aspect of patient care management PCM services include medication reconciliation, assessment of medication adherence, monitoring for potential drug interactions or side effects, and providing education to patients on proper medication use. Optimizing medication regimens improves patient safety, reduces adverse events, and enhances treatment effectiveness
- Consent:
Obtain written consent from the patient for PCM services, explaining the scope and nature of the services, as well as any associated cost-sharing requirements.
- Eligibility: PCM services are typically eligible for reimbursement from Medicare and some private payers. Ensure that the patient meets the specific eligibility criteria defined by the payer, which may include having chronic conditions that require ongoing care management.
- Time-Based Billing: PCM services are billed based on the total time spent on care management activities during a calendar month. This includes both the time spent by clinical staff and the physician or other qualified healthcare professional PCM services require a minimum of 30 minutes before billing. See CorroHealth TCM, CCM, RPM, PCM Table for more information.
- Documentation: Accurate and detailed documentation is crucial to support the medical necessity of PCM services. Document the time spent on care management activities, care coordination efforts, patient education, medication management, and care plan development or review.
- Reporting Services:
- 99497 (advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate) is a stand-alone billable RHCvisit
- Shared or Incident-to-Billing: When performed in a clinic setting, some PCM services may be billed under the supervising physician or as incident-to-services Understand the billing guidelines applicable to the practice and ensure compliance with the relevant regulations
CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, July 6, 2023
New s
- CY2024 Home Health Prospective Payment System Proposed Rule
- HHSAnnounces Actions to Lower Health Care Costs and Allow Medicare to Negotiate Lower Drug Prices
- CMSRoundup (June 30, 2023)
- Skilled Nursing Facility: COVID-19 Enforcement Discretion for Pharmacy
Billing Ended June 30
- Medicare Providers: Deadlines for Joining an Accountable Care Organization
- Help People with Disabilities Get the Care They Need
MLN Mat t ers®Art icles
- Corrections to Home Health Claims Edits
Publicat ions
-
Medicare & Mental Health Coverage ? Revised
From Our Federal Part ners
- Wildfire Smoke Exposure Poses Threat to At-Risk Populations
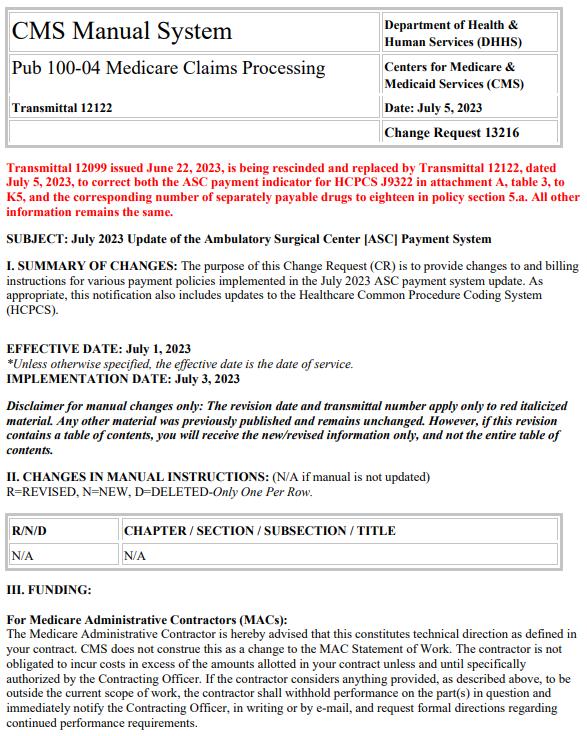
Therew asONEnew or revised Transmittal released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.

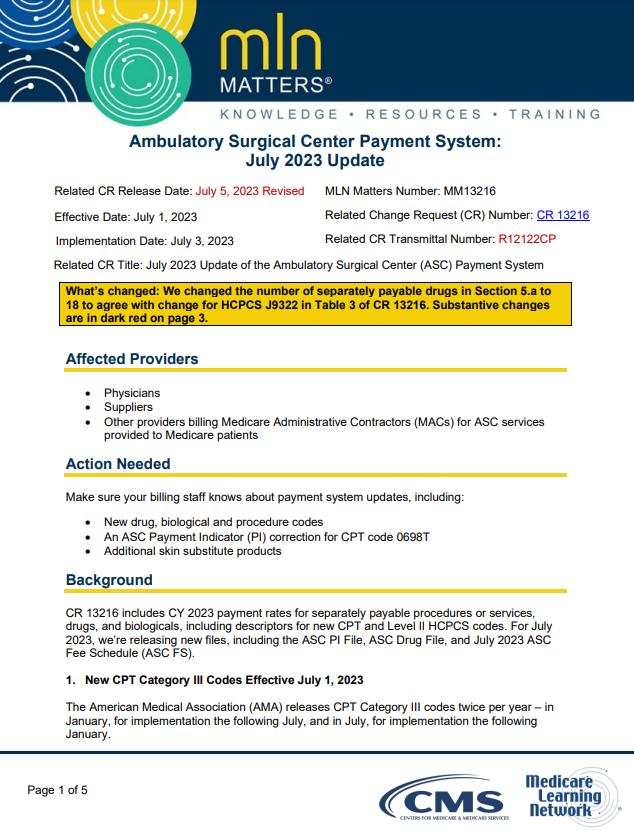
Therew asONEnew or revised MedLearn released thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.




Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.

