




Quest ion:
If a patient comes in for a medication check, do you code the visit with a primary of Z76 0 even if no medication is refilled, a Z51.89 or Dx's they touched base on in the visit with the correct E/M level?

Answ er:
Report ICD-10 CM code Z76 0 (Encounter for Issue of repeat prescription), when the reason for the encounter was to refill a prescription, even if the encounter did not result in a refill
Please refer to ICD-10-CM® Official Guidelines for Coding and Reporting FY2023 IVG which states:List first the ICD-10-CM® code for the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the services provided ?The Official Coding Guidelines are available in the PARA Data Editor Calculator as shown below. Please also refer to the PARA Dat a Edit or ICD-10 CM description.

Quest ion:
We are planning to initiate the IDRprocess with a payer after the open negotiation was unsuccessful Remit from payer is showing the patient's responsibility at $4500 (coinsurance and deductible amounts). Is it appropriate to send patient statement while we are in the IDR process?It is their cost share amount per the payer so just wanting to make sure we are good to bill patient while we wait for the IDRprocess to make a decision which I am hearing is quite back logged.

Answ er:

Yes, the patient can be billed for any cost sharing amounts while the account is in arbitration

We encourage you to confirm that the $4,500 patient liability was accurately applied by the plan as required by the NSA.
In general, for emergency services furnished by a non-participating provider or a non-participating emergency facility, and for non-emergency services furnished by nonparticipating providers with respect to a visit to a participating health care facility, cost sharing is calculated as if the total amount that would have been charged for the services by a participating emergency facility or participating provider were equal to the recognized amount for the services
If an All-Payer Model Agreement or specified state law applies, the plan or issuer must calculate cost sharing for out-of-network services that are subject to the No Surprises Act (based on the amount determined by the All-Payer Model Agreement or specified state law.

If an All-Payer Model Agreement or specified state law does not apply cost sharing is determined based on the lesser of the billed charge or the Qualifying Payment Amount as calculated by the median contracted rate
When the recognized amount is the QPA, plans and issuers must provide the following information with an initial payment or notice of denial of payment:
(1) the QPA for each item or service involved;
(2) if the QPA is based on a downcoded service code or modifier, a statement from the plan or issuer explaining that the service code or modifier billed by the provider, facility, or provider or air ambulance services was downcoded; an explanation of why the claim was downcoded, including a description of which service codes or modifiers were altered, added, or removed, if any; and the amount that would have been the QPA had the service code or modifier not been downcoded;
(3) a statement to certify that the plan or issuer has determined that the QPA applies for the purposes of the recognized amount (or, in the case of air ambulance services, for calculating the participant?s, beneficiary?s, or enrollee?s cost sharing), and that each QPA was determined in compliance with the methodology established in the July 2021 interim final rules
(4) a statement that if the provider or facility, as applicable, wishes to initiate a 30- business-day open negotiation period for purposes of determining the amount of total payment, the provider or facility may contact the appropriate person or office to initiate open negotiation, and that if the 30-business-day open negotiation period does not result in a determination, generally, the provider or facility may initiate the Federal IDRprocess within 4 days after the end of the open negotiation period; and
(5) contact information, including a telephone number and email address, for the appropriate person or office to initiate open negotiations for purposes of determining an amount of payment (including cost sharing) for such item or service

The attached document includes the list of Remittance Advice Remark Codes which may be used by plans to communicate how cost sharing was calculated under the No Surprises Act. The other document helps determine the applicability for the Federal IDRprocess

This paper offers concise guidance on coding and coverage changes which apply to hospitals following the end of the Public Health Emergency on May 11, 2023
After the PHE, Medicare will require all COVID-19 and related testing that is performed by a laboratory to be ordered by a physician or non-physician practitioner.
Temporary COVID Test Codes U0003, U0004, U0005 will no longer be reimbursed by Medicare (and presumably other payors) after the end of the PHEon May 11, 2023. Most providers report HCPCS87635 (INFECTIOUSAGENT DETECTION BYNUCLEICACID (DNA ORRNA); SEVEREACUTERESPIRATORYSYNDROMECORONAVIRUS2 (SARS-COV-2) (CORONAVIRUS DISEASE[COVID-19]), AMPLIFIED PROBETECHNIQUE), but there are a number of other HCPCS codes which may represent alternate means of COVID-19 testing
May be covered at the discretion of the Medicare Administrative Contractor Commercial plan coverage may vary.
Nasal swab specimen collection for COVID testing will no longer be eligible for separate reimbursement While reporting HCPCSC9803 (HOSPITAL OUTPATIENT CLINICVISIT SPECIMEN COLLECTION FORSEVEREACUTERESPIRATORYSYNDROMECORONAVIRUS2 (SARS-COV-2) (CORONAVIRUSDISEASE[COVID-19]), ANYSPECIMEN SOURCE) is not expected to cause claim rejections, it will not be reimbursed after 5/11/2023
Will continue to be covered, but the cost will carry patient liability for the usual Medicare deductible and coinsurance. Commercial plan coverage may vary. (There are currently no COVID-19 monoclonal antibodies approved or authorized for use against the dominant strains of COVID-19 in the United States.)
Will no longer relieve patients of financial liability for evaluation and management charges when a practitioner orders a COVID test after 5/11/2023; patients will be responsible for the ordinary deductible and coinsurance obligations for problem-focused evaluation and management services.
Telem edicine
Delivered by billing professionals (not facilities) will continue to be an option for Medicare beneficiaries subject to Medicare?s ?List of Telehealth Services for Calendar Year 2023 " Professional fees for telehealth services will continue to be paid at the non-facility rate under the Medicare Physician Fee Schedule However, telehealth equipment must be HIPAA compliant after 5/11/2023
(Telehealth originating facility fee) should no longer be reported on a facility fee claim for supporting a facility-based physician or non-physician practitioner performing a telemedicine service Hospitals may report Q3014 only if the patient comes to the facility to utilize HIPAA-compliant telehealth equipment while a distant site practitioner performs a telemedicine visit.
During the PHE, HHSissued a temporary notice to allow covered providers to use popular non-public facing communications apps to deliver telehealth during the COVID-19 PHE, such as Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, Zoom, and Skype After 5/11/2023, telehealth equipment must utilize HIPAA-secure technology, and a Business Associates Agreement must be in place with the technology provider.
Will no longer be covered by Medicare (except certain mental health or substance abuse disorder treatment reported with HCPCSC7900 ? C7902 ) Some facilities took advantage of a PHEwaiver which allowed the hospital to bill for certain therapies (such as physical, occupational, speech, medical nutrition, or diabetes self-management training) over remote communications technology to patients in the home setting. This flexibility ends on May 11, 2023. (Although physical and occupational therapistsin privatepracticemayoffer servicesvia telehealth after the PHEends, hospitalswill no longer bepermitted to bill for remotefacility servicesdelivered via communicationstechnology.)
Medicare?s waiver of the 3-day qualifying inpatient stay as a prerequisite for Medicare coverage of a Skilled Nursing Facility or Swing Bed care will end; coverage of skilled care/swing bed stays will again require the pre-qualifying 3-day stay All new SNFstays beginning on or after 5/12/2023 will require a qualifying hospital stay before Medicare coverage.
The CARESAct provided a 20% add-on payment to IPPSDRG reimbursement for treating COVID-19 inpatients (ICD-10 diagnosis codes U07 1 or B97 27) will end for inpatients discharged after May 11, 2023. However, the new COVID-19 treatments add-on payments (NCTAP), which increase payment when specific treatments such as convalescent plasma and remdesivir are reported within the ICD-10 codes on an inpatient claim, will continue through September 30, 2023.
Will continue to be covered in full without cost by Medicare. Medicare Advantage members and commercial health plans subject to the Affordable Care Act will continue to cover COVID vaccinations without cost, provided that the beneficiary receives care at an in-network provider. Check with the individual plan for details of coverage.
Medicare beneficiaries will no longer be entitled to receive 8 home COVID tests per month per household Commercial plan coverage may vary
For more information, please visit Medicare?s FAQ document at: https://www cms gov/files/document/frequently-asked-questions-cms-waivers-flexibilitiesand -end-covid-19-public-health-emergency.pdf

A recent policy announced by commercial healthcare payer The Cigna Group, which mandates the submission of office notes along with claims for specific evaluation and management (E/M) CPT® codes and modifier 25, is causing significant concerns among physicians and healthcare professional organizations. The American Medical Association (AMA) recently released a statement about their concerns surrounding this policy.
https://www.ama-assn.org/practice-management/cpt/cigna-s-modifier-25-policyburdens-doctors-and-deters-prompt-care

In March, the Cigna Group announced that effective May 25, 2023, they would reinstate their policy requiring submission of office notes with all claims including E/M codes 99212, 99213, 99214 and 99215 and modifier 25 when a minor procedure is billed on the same claim. Payment will be denied if medical records are not submitted to support the claim.
https://static.cigna.com/assets/chcp/secure/pdf/resourceLibrary/clinReimPolsModifiers/ Notifications/Modifier 25 Significant Separately Identifiable Evaluation and Management pdf

Last month, physician organizations co-signed a letter to Cigna CEO David Cordani, stating that this policy poses a significant and unnecessary burden on physician practices and negatively impacts patient care.


Cigna has not provided any rationale for the policy and has not offered any evidence of overuse or unnecessary application of modifier 25. The AMA recently released a CPT® Assistant supplement entitled ?Reporting Modifier 25?which outlines various scenarios modifier 25 is appropriate:

Adding to physicians?concern regarding this policy is that Cigna has stated they will only review approximately 10%of the documentation submitted Furthermore, the payer has offered only two options for submitting the required medical records when reporting modifier 25: the rarely used method of fax, and a HIPPA non-compliant, unsecured email address.
The various physician organizations have approached Cigna to collaborate in distributing educational materials and joining forces for training initiatives
1 The person hired t o do t he Palliat ive Care is a Nurse Pract it ioner Is t hat is a billable service?
Answ er: Services of a Nurse Practitioner are billable as professional fees, provided of course that the services billed are medically necessary and the nurse practitioner is properly enrolled with the payer.
2. Our Nurse Pract it ioner w ill be seeing bot h inpat ient s and out pat ient s in t he hospit al She m ay also be seeing pat ient s in t heir hom es
Be sure the NPis enrolled with Medicare and included under your medical group NPI with an 855B form (or on PECOS) no more than 30 days prior to the date on which the NPwill begin seeing patients.
The NPmust also update the NP?s individual Medicare enrollment (855I/PECOS) to add locations of service which include the facility and patient home visits. NPservices billed as professional fees will be reimbursed at 85%of the Medicare physician fee schedule (CAH Method II note: nurse practitioner services in the outpatient hospital setting must be billed with modifier -GFappended to the CPT® code on the UB/837i.)
Verify that the appropriate E/M codes are available with in the chargemaster, and ensure that the appropriate Place of Service codes are also reportable Typical professional fee codes would include, but not be limited to the following:
Out pat ient visit s in the clinic or hospital setting: 99202- 99215
Inpat ient s ? 99221- 99223
Hom e or dom iciliary visit s ? 99341- 99350
Typical Place of Service codes:
21 ? Hospit al Inpat ient
22 ? Hospit al Out pat ient
12 - Hom e
13 ? Assist ed Living Facilit y
3 Are t here any guidelines for Palliat ive Care program s?
Answ er: The National Coalition for Hospice and Palliative Care offers a guideline at the link here: https://www nationalcoalitionhpc org/ncp/


On April 18, 2023, the FDA authorized an amendment to the Emergency Use Authorization (EUA) for COVID-19 bivalent vaccines for all patients ages 6 months and older. Monovalent COVID-19 vaccines offered through Pfizer-BioNTech and Moderna are no longer authorized in the United States
Coronavirus (COVID-19) Update: FDA Authorizes Changes to Simplify Use of Bivalent mRNACOVID-19 Vaccines
The amended EUA provides the following information:
- Patients who had a monovalent COVID-19 vaccine only may receive one bivalent vaccine
- Unvaccinated patients may receive one bivalent vaccine
- Most patients who have already had one dose of bivalent are considered fully vaccinated at this time. The FDA may revise this decision after the FDA Advisory Committee meeting in June
Exceptions to this include:
- Patients aged 65 or older ? may receive an additional bivalent vaccine at least four months following the first
- Patients with immunocompromised conditions ? may receive an additional bivalent vaccine at least two months following the first with additional doses as determined by the healthcare provider The FDA states there are additional considerations for patients aged 6 months ? 4 years
The FDA offers additional recommendations for children ages 6 months through 5 years depending upon previous COVID-19 vaccination administrations
CorroHealt h invit es you t o check out t he m lnconnect s page available from t he Cent ers For Medicare and Medicaid (CMS). It 's chock full of new s and inform at ion, t raining opport unit ies, event s and m ore! Each w eek PARA w ill bring you t he lat est new s and links t o available resources. Click each link for t he PDF!

Thursday, May 11, 2023
New s
-
CMSRoundup (May 5, 2023)
- Medicare Ground Ambulance Data Collection System: Report Information
Com pliance
- Bill Correctly: Power Mobility Devices Repairs
MLN Mat t ers®Art icles
- Clinical Laboratory Fee Schedule & Laboratory Services Reasonable Charge
Payment: Quarterly Update
- Home Dialysis Payment Adjustment & Performance Payment Adjustment for ESRD Treatment Choices Model: Updated Process
Publicat ions
- Billing Medicare Part B for Insulin with New Limits on Patient Monthly
Coinsurance ? Revised
- Expanded Home Health Value-Based Purchasing Model: Updated Measure
Calculation Resources
Therew ereTWELVEnew or revised Transmittalsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.












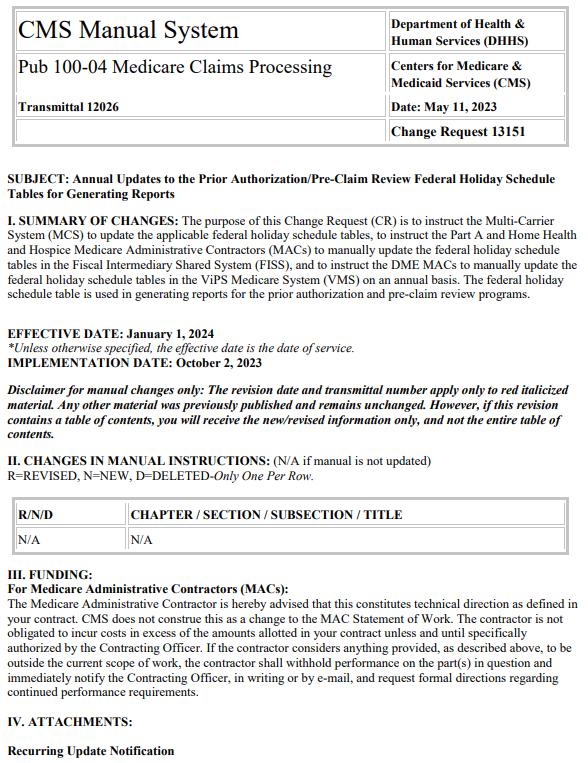
Therew as1new or revised MedLearnsreleased thisw eek.
To go to thefull Transmittal document simply click on thescreen shot or thelink.



Theprecedingmaterialsare for instructional purposesonly. Theinformation ispresented "as-is"and to thebest of CorroHealth'sknowledgeisaccurateat thetimeof distribution. However, due to the ever-changinglegal/regulatory landscape, thisinformation issubject to modification asstatutes, laws, regulations, and/or other updatesbecome available. Nothingherein constitutes, isintended to constitute, or should berelied on aslegal advice. CorroHealth expresslydisclaimsanyresponsibilityfor anydirect or consequential damagesrelated in anywayto anything contained in thematerials, which areprovided on an "as-is"basisand should beindependentlyverified before beingapplied. You expresslyaccept and agree to thisabsoluteand unqualified disclaimer of liability. The information in thisdocument isconfidential and proprietaryto CorroHealth and isintended onlyfor thenamed recipient. No part of thisdocument maybereproduced or distributed without expresspermission. Permission to reproduceor transmit in anyform or byanymeanselectronicor mechanical, includingpresenting, photocopying, recording, and broadcasting, or byanyinformation storageand retrieval system must beobtained in writingfrom CorroHealth. Request for permission should bedirected to Info@Corrohealth.com.


