The potential of artificial intelligence in health care comes with both groundbreaking advancements and critical challenges as PCOM alumni navigate an evolving landscape PAGE 14 Founders’ Day Tribute PAGE 24 Osteopathic Medicine in the AI Age































































































































































































































The potential of artificial intelligence in health care comes with both groundbreaking advancements and critical challenges as PCOM alumni navigate an evolving landscape PAGE 14 Founders’ Day Tribute PAGE 24 Osteopathic Medicine in the AI Age





























































































































































































































Join us in remembering Paul W. McGloin, former chairman of the Board of Trustees, posthumously awarded PCOM’s highest honor.
AI in Medicine: The Promise and the Paradox
Dive into the complex world of AI in medicine, where promise meets paradox. Discover how PCOM alumni from diverse fields are navigating this transformative frontier.
Explore how the osteopathic profession can lead the ethical integration of AI, leveraging datadriven advancements to enhance holistic, patientcentered care while upholding its core values.
5News
10 Field Notes
11 Office Hours and Second Opinion
12 Pulse Check
13 In Their Words
16United & Ignited
25Time Machine
26Shoutouts
27Class Notes
35Quick Takes
PCOM Georgia students hone their skills in the medical simulation lab, where hands-on training meets cutting-edge technology. As AI continues to evolve, it will enhance their didactic education and clinical practice—sharpening diagnostics, personalizing treatment and reshaping patient care.
























Dear Alumni and Friends:
Welcome to the newly refreshed Digest Magazine. In this issue, we’re excited to unveil a modernized format that strikes the perfect balance between professionalism and approachability. With thoughtfully curated sections—from in-depth explorations of critical trends to engaging alumni profiles—this updated structure is designed to both inform and inspire, reflecting the prestige of our institution and the achievements of our community.
At the heart of this issue is our feature story, “AI in Medicine: The Promise and the Paradox.” Artificial intelligence is transforming health care, offering unprecedented opportunities to advance medical education and improve patient outcomes, while also raising essential questions about ethics, equity and trust. This duality reflects our mission at PCOM: to embrace innovation that enhances both education and care, all while remaining committed to compassion and excellence.
This issue also invites us to reflect on our roots as we celebrate Founders’ Day. We pay special tribute to the late Paul W. McGloin, CPA, LLD (Hon.), a dedicated trustee and former chairman of the PCOM Board of Trustees. His leadership profoundly shaped the College’s trajectory and extended its reach, particularly into the southern United States.
I encourage you to explore this issue, engage with its stories, and join us in shaping the future of health care. Thank you for your ongoing connection to and support of PCOM.

Jay S. Feldstein, DO ’81
VOL. 86, NO. 1, USPS, 413-060
Digest Magazine is produced by the Office of Marketing and Communications under the direction of Wendy W. Romano, chief marketing and communications officer.
EDITOR
Jennifer Schaffer Leone, MA
PUBLICATION DESIGN
Abigail Harmon
CONTRIBUTORS
Gabrielle DePietro
Janice Fisher
Jamesia Harrison
Kristen Hopf
Brandon Lausch
Jennifer Schaffer Leone
Alexis Martina
Meghan McCall
Cindy B. Montgomery, PhD
Ally Wengel
PHOTOGRAPHY
Theo Anderson
Tara Bazilian Chang
Megan Chapman
Bruce Fairfield
William Griffith
Melissa Kelly
Theresa Regan
Anthony Stalcup
QUESTIONS OR COMMENTS
pcomcommunications@pcom.edu
CLASS NOTES OR ADDRESS CHANGES alumni@pcom.edu
Periodical postage is paid at Upper Darby, PA, and at additional mailing offices.

President and Chief Executive Officer



















































































































































Opinions expressed are not necessarily shared by the College or the editor.
© 2025 Philadelphia College of Osteopathic Medicine. All rights reserved.
A study of hundreds of people using medical marijuana reported “rapid and significant improvements” in healthrelated quality of life over the first three months, according to research led by Michelle R. Lent, PhD, a professor in PCOM’s School of Professional and Applied Psychology.
The study, published in the Journal of Cannabis Research, followed nearly 400 adults who were new to using medical marijuana to treat any of the more than 20 qualifying conditions in Pennsylvania. Study participants, with an average age of about 46 years, were most commonly prescribed medical marijuana to treat anxiety disorders or “severe chronic or intractable pain.” From baseline, respondents improved in all areas of health-related quality of life that researchers evaluated, including less

pain, more energy, and better emotional, social and physical functioning.
“Little is known about what happens to individuals who use cannabis products for medicinal purposes in regard to functioning and health,” said Dr. Lent, who is also director of psychosocial research for PCOM’s Medical Marijuana Research Program. “This study, one of the largest to date, captured how their lives and health status changed after using these
PCOM has completed $1 million renovations at its Cambria and Lancaster Avenue Healthcare Centers, transforming them into modern, accessible facilities for North and West Philadelphia communities. Upgrades include new flooring, wall coverings, lighting, furniture, enhanced exam rooms, conference areas, waiting rooms and staff lounges. Both centers now feature redesigned check-in/ check-out areas, updated bathrooms with gender-neutral options and new lab and immunization rooms. Additional improvements include advanced medical refrigeration and optimized storage solutions as well as the addition of quiet rooms for staff mindfulness breaks.
Medical directors Kristen Berry, DO ‘00, and Barbara Williams-Page, DO ‘92, noted patients’ enthusiasm and appreciation for the modernized spaces. Ryan Ford (DO ’25) highlighted the upgrades’ positive impact on efficiency and patient comfort. These centers continue to provide essential healthcare services—from family medicine to gynecology and psychology.
products. In the era of precision medicine, understanding which type of patient may benefit from which type of therapy is of high importance.”
Dr. Lent said it can be challenging for patients and providers to make decisions about whether to incorporate medical marijuana into treatment planning. Studies like these provide “evidence to support greater access to, and coverage of, medical cannabis treatments,” she said.

As part of PCOM’s wider commitment to advancing healthcare education in its local communities, the College was proud to partner with various higher education institutions throughout its footprint in 2024 to provide students with more pathways to achieving their medical degrees.
In the Philadelphia region, PCOM expanded clinical education through the creation of the Northeast Pennsylvania Clinical Consortium and through new and expanded partnerships with Jefferson Health New Jersey, Holy Redeemer Hospital and Meritus Health. It also launched collaborative academic programs with the Wistar Institute for a PhD in cancer biology and La Salle University to support forensic medicine.
In Georgia, the Physical Therapy Department has partnered with Gwinnett Ballet Theatre (GBT) for a three-year collaboration aimed at providing free physical therapy services to dancers. Under the supervision of licensed faculty, PT students will offer injury prevention resources, comprehensive screenings, and targeted interventions to improve strength, flexibility, endurance and balance. This partnership emphasizes early intervention to reduce injury severity and help dancers return to performance faster. GBT, Gwinnett County’s first performing nonprofit, is excited to provide dancers with high-quality care, supporting their long-term careers in the arts. The services will be offered onsite at GBT’s Suwannee location.
The University of Georgia (UGA), PCOM Georgia and PCOM South Georgia have established a partnership to provide a clear pathway for students graduating with a bachelor of science in pharmaceutical sciences to enter the DO program at PCOM. The agreement reserves up to three seats per year for qualified UGA students who meet specific academic criteria, including a competitive GPA and MCAT score. This partnership aims to create a new generation of medical professionals in Georgia, with mentorship and guidance throughout the application process.

In addition, PCOM South Georgia has joined Emory University in a five-year, $5 million initiative, funded by the U.S. Health Resources and Services Administration, to address the growing need for geriatric healthcare professionals. The Georgia Gear program, led by Emory’s Department of Family and Preventive Medicine, will offer training for physicians to care for Georgia’s aging population. As part of the program, PCOM South Georgia will provide third- and fourth-year osteopathic medical students with elective clinical rotations focused on geriatrics. This partnership is crucial, as Georgia’s senior population is projected to surpass the number of children by 2025, creating an increased demand for geriatric care.
Both partnerships aim to strengthen health care across the state by preparing students to meet the diverse needs of Georgia’s population.

formalizes a $5 million partnership with Emory University to enhance physician training focused on Georgia’s aging population.
Larry N. Finkelstein, DO ’87, a professor in PCOM’s Department of Family Medicine, has seen a lot in his nearly 40 years of practicing medicine, but he recently encountered a first. Thankful for his care, a longtime patient dedicated a book to him.
During an appointment, Arlene J. Surrency, who has seen Dr. Finkelstein as her primary care provider for more than 25 years, displayed three children’s books she had published, prompting Dr. Finkelstein to ask whether she had considered writing one to promote healthy lifestyles.
“That’s why I was inspired to write it,” Mrs. Surrency said of the book, titled Healthy Living Leads to a Healthy Me “When someone sees something in you, it makes a big difference. When Dr. Finkelstein looked at these three books, he saw something in them.”
Told through the story of Elijah, Mrs. Surrency’s youngest son, the 44-page book emphasizes the importance of diet, exercise and hygiene as some of the keys to good health. It includes this dedication page: “I want to give a ‘special thanks’ to my primary care physician, Larry Finkelstein, DO, for the excellent service he has provided me

through the years. Most of all, I want to thank him for inspiring me to write this book. Thank you, Dr. Finkelstein.”
Dr. Finkelstein said the dedication “reinforces that what I’m doing makes a difference.
“I’ve always known that I’ve had strong relationships with my patients and developed rapport with my patients, but here it is in black and white, in print—which is a first,” he said.

PCOM South Georgia led a collaborative rural health initiative at the recent Sunbelt Ag Expo at Spence Field in Moultrie. Visitors engaged with speakers on topics such as mental health and CPR training. They could also have their blood glucose or blood pressure checked as well as view demonstrations of cutting-edge medical technology. The initiative featured representatives from over 30 nonprofit organizations, underscoring PCOM South Georgia’s commitment to rural health care.
PCOM received the 2024 Higher Education Excellence in Diversity (HEED) Award from Insight into Diversity magazine, the oldest and largest diversity-focused publication in higher education. This marked PCOM’s 10th consecutive year receiving the national honor for its efforts in advancing health equity through the creation of educational programs, impactful advocacy efforts and meaningful community partnerships.


To close out its 125th anniversary year, PCOM hosted staff, students, volunteers and community partners for a morning of service on December 5, where they assembled 500 Health Aid Kits—a more holistic and preventative take on first-aid kits.
The kits—sponsored by Independence Blue Cross—included wellness resources, a meditation playlist, a reusable canvas bag, and a $125 gift card to ShopRite or The Fresh Grocer for grocery support during the holiday season.
“It's all about making our communities healthy,” said PCOM President and CEO Jay S. Feldstein, DO ’81, during opening remarks. “That's our mission, and we're going to keep doing it for the next 125 years.”
Volunteers included teams from 6ABC, The Fresh Grocer, Independence Blue Cross’s Blue Crew, 160over90 and Image Ink, in addition to PCOM faculty, staff and students.
In the weeks following the event, PCOM distributed kits to community members across the city through PCOM’s Community Wellness Initiative (CWI), which fosters a culture of holistic health and well-being in surrounding neighborhoods.
“We are happy to empower people to purchase their own food that will be healthy and help them with their families," said Flo Byarms, director of PCOM’s CWI.
Among the recipients was Asia Stanford, a West Philadelphia resident who was one of the 75 patients across PCOM’s three community Healthcare Centers that received kits in December.
She has been coming to PCOM’s Lancaster Avenue Healthcare Center all her life for care. Her mother first brought her and, now as a mom to her own three children, she does the same. She said the $125 in grocery support is "very meaningful to me because I have a family I'm providing for this Christmas. It helps a lot."
Other community partners who joined with PCOM’s CWI to distribute kits included Methodist Services, Ward Emmanuel AME Church, City Councilmember Jamie Gauthier of the Third District and Overbrook West Neighbors (OWN).
On the Saturday before Christmas, PCOM volunteers and students visited Tustin Recreation Center in West Philadelphia to hand out 150 Health Aid Kits to the local community at its annual Toy Drive, organized by OWN, a community development

organization focused on enhancing commerce throughout the Upper Lancaster Avenue Business Corridor.
Paige Syndnor, a West Philadelphia native and single mother of three, was one of the many local residents who received kits at Tustin Recreation Center, a gift she said she would never forget.
“I have never received something like this in my life,” Ms. Syndnor shared upon receiving the Health Aid Kit. “Being a single mom is hard. I work every day and still struggle to provide for my kids, so this box really means so much to me and my family.”
Sharing in Ms. Syndnor’s sentiment was Stella Allen, a fellow West Philadelphia resident and grandmother of three, who became overwhelmed with emotion when opening her kit. “I’m completely floored by this, it is a true blessing from God,” she said in tears.
Last year, Mrs. Allen adopted her three grandchildren in hopes of giving them a better life and said it's because of the community’s support that she is able to make that happen. “I wanted to do right by them,” she shared. “They get good grades, have good morals and deserve to have a good Christmas, so I’m thankful I will be able to do that now.”
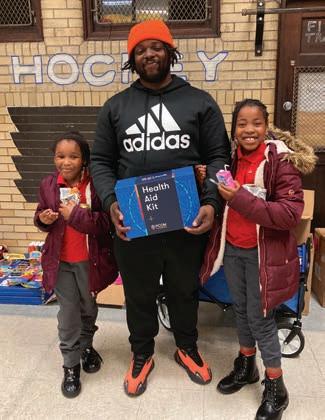
The month-long initiative was not only a perfect close to the College’s banner year, but also a demonstration of its continued commitment to advancing the health of diverse communities.
















The Health Aid Kit includes a $125 gift card to ShopRite or The Fresh Grocer, a canvas tote bag, sensory pop-it toy, band-aid magnets, wellness cards and a meditation playlist.
and








Empowering clinicians to combat gun violence through education, prevention strategies and vital community resources in urban healthcare settings
by Kristen Hopf

In recent years, Erik Langenau, DO, MS, MAPP ’23, chief academic technology officer and professor in the department of pediatrics at PCOM, observed a rise in gun violence among patients at PCOM’s Lancaster Avenue Healthcare Center in West Philadelphia. In response, his team launched a survey-based study to assess gun violence prevalence, improve clinicianpatient communication and evaluate awareness of community resources.
Between February and April 2024, PCOM students conducted verbal surveys with 428 patients visiting the College’s urban healthcare centers. Findings revealed that 64 percent of patients had been directly impacted by gun violence, often through personal loss or trauma.
“Gun violence is prevalent nationwide, but North and West Philadelphia are particularly affected,” Dr. Langenau said. “We must explore prevention strategies while offering services and mental health support. That’s the driving force behind this project.”
Dr. Langenau emphasized the need to rebuild community strength and belonging to combat the gun violence epidemic. His long-term goals include partnerships with anti-violence organizations and creating healthcare models to better support patients in need. He is seeking funding through recent grant proposals and awaiting a manuscript review of the study. To advance advocacy, Dr. Langenau has engaged with state leadership and is planning a community discussion on the impacts.

Gun deaths in big cities have surged by 65% over the past decade, with the sharpest increase occurring at the height of the COVID-19 pandemic.
1,600
Every year in Pennsylvania, gun violence claims 1,600 lives and leaves another 3,000 people wounded—averaging more than a dozen victims every single day.





College faculty share insights on the role of AI in health care, both in clinical practice and in educational contexts
by Jennifer Schaffer Leone







BRIAN BALIN, PHD WITH

A growing research consensus is emerging that infections may trigger or exacerbate neurological conditions
by Brandon Lausch
Amid greater public understanding that infections like SARS-CoV-2, which causes COVID-19, can result in neurological consequences such as brain fog, an international coalition of researchers is investigating how inflammation-causing infections can lead to Alzheimer’s disease and other dementias.
Brian J. Balin, PhD, director of PCOM’s Center for Chronic Disorders of Aging, is a founding member of the Alzheimer’s Pathobiome Initiative (AlzPI), which convened on PCOM’s campus last year to share findings of the pathogen hypothesis of Alzheimer’s disease, which is moving toward the scientific mainstream. Joining scientists at PCOM were colleagues from Columbia, Harvard, Oxford and more.
Bacteria, viruses, fungi and parasites are capable of entering the brain. Other microbes, such as those comprising the gut microbiome, may inflame the brain from a distance by triggering damaging immune responses. Several neurological conditions have been linked with microbial infections, but establishing a causal relationship has largely remained elusive.
“We want scientists globally to be more collaborative and consolidate efforts that standardize approaches in diagnosing infections when people have neurocognitive change,” Dr. Balin said.

HSIN-LIANG (OLIVER) CHEN, PHD, professor and chief library services officer at PCOM, chairs the College’s AI Governance Council, curating resources and shaping guidelines for AI’s role in healthcare education. “Generative AI offers immense potential for transforming education—enabling personalized learning, enhancing research and supporting clinical decision-making. Yet these advancements come with risks requiring careful consideration. We must maintain transparency, mitigate bias and safeguard academic integrity,” he said. “Our goal is to drive innovation that upholds College values while preparing students to thrive in an evolving healthcare landscape.”
SCOTT W. LOWE, PT, DPT, OCS, FAAOMPT, assistant professor of physical therapy at PCOM Georgia, recently published two papers on AI's role in physical therapy education. His findings indicate enthusiasm for AI's potential but highlight educator preparedness needs. He describes applications such as generating low-stakes quizzes and creating innovative classroom tools, citing a multimodal activity he piloted to teach normal human gait. “AI could address challenges such as providing timely feedback, offering varied explanations of complex concepts, and fostering new learning experiences,” said Dr. Lowe.


RUTH M. MAHER, PT, PHD, DPT, WCS, former chair of physical therapy at PCOM Georgia, led a study on AI's potential to enhance diagnostic efficiency. Alongside Jeanne Welch, PT, EdD, DPT, and Jennifer Wiley, PT, DHSc, DPT, she tested the Clarius Bladder AI (BLAI), a deep learning model automating bladder volume assessment, critical for managing lower urinary tract symptoms. “Our results revealed a high degree of accuracy between AI-generated and expert measurements, with performance metrics showing strong alignment. Recently FDA-approved, BLAI is now integrated into Clarius ultrasound units, streamlining bladder assessments for improved care,” said Dr. Maher.
ROBERT JASON WALKER, PHD, associate professor of physiology at PCOM South Georgia, presented research on AI and culinary medicine with Evan Curry (DO ’26), Emeka Ikeakanam (DO ’26) and Terrence McHugh (DO ’26) during Research Day. Their work explores how AI-powered tools help individuals overcome barriers to healthy cooking. “AI has the potential to revolutionize culinary medicine by providing personalized, accessible dietary recommendations,” explained Dr. Walker.
“Through machine learning, AI can tailor meal plans to specific health needs and guide nutritious choices, empowering individuals to take control of their health.”
A heartbeat of PCOM life—dynamic moments, shared connections and events—that bring our campuses to life



1. PCOM celebrated its 125th anniversary with the burial of a time capsule to be opened in 2099. The ceremony honored the institution's rich history and enduring commitment to shaping the future of healthcare education.
2. Andrea Mann, DO, dean and chief academic officer, osteopathic medicine program, PCOM Georgia, joins Corvin, a young boy with spina bifida and Chiari malformation, at the “Super Speaker” event, where he bravely shared his journey of living with complex medical conditions.
3. The Association of Black Cardiologists honored Evelyn Orusa (DO ’27) with its Dr. Richard Allen Williams Scholarship, which recognizes outstanding medical students who aspire to impact underserved communities.



4. The DO and Pharmacy classes of 2028 at PCOM, PCOM Georgia and PCOM South Georgia received their white coats, marking a significant moment in their journeys as aspiring healthcare professionals.
5. On October 29, PCOM South Georgia hosted “Pink Out Day,” where faculty, staff and students donned pink to show their support for those affected by breast cancer, especially Joanne M. Jones, MBA, chief of campus operations, and other members of the PCOM South Georgia family.
6. PCOM Georgia’s Physical Therapy Department provided demonstrations and health screenings at the Piedmont Park Fair.
2025 PCOM Alumni Association Certificate of Honor Recipient Paul Lapoint, DO ’90, served as president of the PCOM Alumni Association from 2022 to 2024. A board-certified orthopedic surgeon in Williamsville, New York, he is dedicated to mentoring future healthcare professionals and giving back to PCOM.
by Alexis Martina
Q: The PCOM Alumni Association underwent a restructuring while you served as president. Why do you think that was necessary, and how do you hope the association continues to evolve?
A: During my tenure as president, a key objective was to elevate the Alumni Association’s national presence and encourage deeper connections between alumni and PCOM. Traditionally, the association had been focused on DO alumni, and it was important to ensure that alumni from all degree programs had an equal platform to share their perspectives. We restructured to create a more inclusive community that values the unique insights of all alumni while supporting the success and growth of the College.
Q: You recently established the Lapoint Family Endowment for Student Wellness. What inspired you to give back to PCOM in this way?
A: PCOM gave me the foundation I needed to succeed in my career, and I feel a deep responsibility to give back and support the next generation of osteopathic physicians and healthcare professionals. Our didactic and clinical education is very challenging, and it is critical to have a strong support system. By creating this endowment, I hope to ensure that students always have access to mental health resources and the help they need to thrive. No one should feel like they’re falling through the cracks because of their circumstances. When you’re part of the PCOM family, you should feel confident that the College and its alumni are here to support you, every step of the way.
Q: As an orthopedic specialist, you’ve mentored PCOM residents and students. Why is this a priority to you?
A: It’s incredibly rewarding to watch students and residents grow and succeed, becoming exceptional physicians. My goal is to provide them with a strong foundation in orthopedic knowledge so they can confidently diagnose and treat basic

“PCOM gave me the foundation I needed to succeed in my career, and I feel a deep responsibility to give back.”
orthopedic issues. As physicians, we must commit to lifelong learning, and I emphasize this principle with both students and residents. When I look back at the mentors I had at PCOM and the influence they had on my development, I only hope that I can provide, in some small way, the same experience.

FOUNDERS’ DAY TRIBUTE:
POSTHUMOUSLY AWARDED PCOM’S HIGHEST HONOR, MR. MCGLOIN DEMONSTRATED VISIONARY LEADERSHIP THAT DEFINED A TRANSFORMATIVE ERA, EXTENDING THE COLLEGE’S REACH AND IMPACT.
by Jennifer Schaffer Leone
The passing of Paul W. McGloin, CPA, LLD (Hon.), on December 6, marked the loss of a visionary leader and an integral member of the PCOM family. As a dedicated trustee and former chairman of the PCOM Board of Trustees, Mr. McGloin made contributions that profoundly shaped the College’s trajectory and extended its reach, particularly into the southern United States.
Throughout his tenure on the Board of Trustees, including more than a decade as chairman, Mr. McGloin guided PCOM through pivotal moments in its history. Under his stewardship, the College achieved financial stability and strategic growth, highlighted by the establishment of PCOM Georgia in 2005. This expansion solidified the College’s mission of advancing healthcare education and delivery beyond its Philadelphia roots.
“Paul was a steward of integrity, objectivity and competence,” shared Jay S. Feldstein, DO ’81, president and chief executive officer, PCOM. “His professional acumen in business and finance ensured PCOM’s resilience, enabling us to navigate challenges and seize opportunities. His leadership was marked by a steady hand and a strategic mind, always driven by a deep commitment to PCOM’s mission.”
A graduate of Drexel University, Mr. McGloin began his career as an auditor for KPMG Peat Marwick before transitioning into banking, where he held executive leadership roles for more than three decades. His career spanned positions as division president, vice president, executive vice president and president at several banks, including First Union National Bank in Philadelphia and National Penn Bank. Following his professional retirement in 2011, he served on the board of the Almo Corporation.
In 1991, Mr. McGloin was elected to the PCOM Board of Trustees, where he served for 23 years. Upon his resignation in 2014, he was named Trustee Emeritus. Beyond PCOM, his dedication to community and civic engagement was evident in his involvement with the Foundation for Architecture and the Philadelphia Convention and Visitors Bureau.
In the early 2000s, as the healthcare market in the Northeast became increasingly saturated, Mr. McGloin, in partnership with the late President Matthew Schure, PhD, recognized the need for PCOM to expand its reach. This strategic vision aimed not only to address regional physician shortages but also to stabilize tuition by reducing reliance on state funding.
Suburban Atlanta was selected for the College’s first branch campus, which opened in 2005 with an inaugural class of 80 osteopathic medical students. PCOM Georgia was designed to address the state’s critical shortage of healthcare providers. By establishing a robust network of clinical rotations, internships and residencies, the cam-
pus significantly increased the likelihood that graduates would remain in the region, directly impacting healthcare disparities.
Mr. McGloin’s leadership spanned the tenure of two PCOM presidents—Leonard H. Finkelstein, DO ’59, and Dr. Schure. His ability to navigate challenges, foster collaboration and unite the Board of Trustees and College leadership under a shared vision was pivotal to PCOM’s growth.
“Paul’s enduring influence on PCOM is immeasurable,” said Dr. Feldstein. “He believed in our mission, our people and our potential to make a difference in the world. It is through his vision that we continue to thrive.”
At the time of his passing, Mr. McGloin was slated to receive the O.J. Snyder Memorial Medal, PCOM’s highest honor, during the 2025 Founders’ Day celebration. This prestigious award, named for PCOM’s co-founder and first president, Oscar John Snyder, DO, is now given posthumously in recognition of a man whose leadership and contributions set the foundation for PCOM to flourish well into its next chapter.
“Paul’s life reminds us that true leadership is not just about advancing an institution. It is about building a foundation for others to succeed,” said Dr. Feldstein. “His legacy will remain a guiding light as we continue to fulfill our mission.
“Our prayers are ever with his family—the cornerstone of his life. Mr. McGloin was deeply devoted to his family, and will be remembered as a loving husband to his wife, Bev, a proud father to his sons, and a doting grandfather. We thank them for sharing Paul with us.”
“Paul’s life reminds us that true leadership is not just about advancing an institution. It is about building a foundation for others to succeed.”
– Dr. Feldstein
by Meghan McCall



PCOM South Georgia’s A Night to Ignite Celebration raised an impressive $250,000 for United & Ignited, thanks to the generosity of Title Sponsor Colquitt Regional Medical Foundation and event attendees. Held on October 19, the event united PCOM and the local community to celebrate campaign progress and honor outstanding supporters with Ignite Awards. Proceeds will provide scholarships for students from Southwest Georgia.
PCOM presented Ignite Awards to honor those whose generosity, commitment, and passion for PCOM South Georgia has had a substantial impact on the institution. The recipients were Jim and Jill Matney, as well as Jeter Partners, LLC, owned by brothers Jimmy and Dan Jeter.
As the chief executive officer of Colquitt Regional Medical Center, Mr. Matney played a prominent role in improving healthcare quality in Colquitt County and throughout South Georgia. He was instrumental in helping PCOM establish the South Georgia campus. He and his wife, Jill, are dedicated supporters of their community, serving on several boards, and opening their home on numerous occasions to host events for PCOM South Georgia. Mrs. Matney also served on the Celebration Committee that planned A Night to Ignite, capitalizing on her network in the region.
Brothers Jimmy Jeter and Dan Jeter own Jeter Partners, LLC, a real estate partnership that develops owner-occupied commercial properties for office and professional use. Recognizing the need for additional medical facilities in the area, the Jeters developed 15 acres near Colquitt Regional Medical Center, which has grown to include nine medical offices. Through Jeter Partners, LLC, they acquired 130 acres of land in Moultrie and donated 30 acres of the tract to PCOM. It is on this land that PCOM South Georgia now sits.




by Meghan McCall

Over one year since its public launch in January 2024, the United & Ignited fundraising campaign continues to ignite remarkable support to accelerate academic excellence, expand experiential opportunities and enhance student experiences. The campaign continues to unite alumni, faculty, staff, friends and organizations in a common goal to successfully prepare and position PCOM students to be leaders in a competitive healthcare market.























































6,841 GIFTS MADE TO THE CAMPAIGN



$52,545,981 OF












Jeffrey Kingsley recently committed $250,000 to establish the Jeffrey K. Kingsley, DO ’01, Endowed Scholarship to relieve the tuition burden for DO students who had nontraditional paths to medical school.
“Some of the best physicians I ever met are those who were relatively nontraditional—individuals who came from disadvantaged backgrounds, who had work lives between high school and college or between college and medical school. Scholarships can dramatically enhance the ability for these individuals to become thriving physicians, and that’s a win for all of society,” says Dr. Kingsley.


“Students have such a voice in this campaign. My fellow members of student government and I were given opportunities to speak on how we wanted a recent donation to be used. This campaign is more than just a fundraiser. From scholarships to enhancing clinical sites, this is a tangible way to improve the daily lives of students as well as their time here at PCOM.”


THE POTENTIAL OF ARTIFICIAL INTELLIGENCE IN HEALTH CARE COMES WITH BOTH GROUNDBREAKING ADVANCEMENTS AND CRITICAL CHALLENGES, AS PCOM ALUMNI NAVIGATE THE EVOLVING LANDSCAPE
by Janice Fisher
“AI holds immense promise in transforming health care, but its potential will only be fully realized if its challenges are effectively managed.”
But don’t take our word for it. That’s how ChatGPT concluded its response to the prompt: “Provide an overview of the challenges and promise of AI in medicine today.”
The forms of AI that are on the threshold of entering every aspect of our lives go way beyond the generative version we know from ChatGPT and its kin, or the algorithms that process data from our wearable devices. Healthcare providers use AI-powered medical note-taking apps. AI chatbots and virtual assistants help with patient triage. Hospitals and health systems use AI to streamline administrative processes and improve scheduling. Robotic surgical systems rely on AI enhancements. AI may (or already does) reduce the cost and time of drug development, improve medical imaging and diagnostics, and spur advancements in genomics and precision medicine.
Turning to the challenges AI poses, it’s worth noting that new inventions and new technologies have often aroused as many fears as hopes. In a nutshell, though, the two strongest threads of concern are these: Will AI allow computers to make decisions for us, or even require them to do so? And will AI disrupt the labor market, taking jobs previously held by human workers?
In the following pages, three PCOM alumni in three very different settings offer a birds-eye view of how they work with AI and think about the challenges it poses.

BARBARA A. CROTHERS, DO ’86 , is chief scientist for AIxMed, a cytopathology software company. She is also associate professor of pathology, James H. Quillen Veterans Affairs Medical Center, Tennessee. Dr. Crothers has served as president and executive board member of the American Society of Cytopathology and as chair of the Cytopathology Committee at the College of American Pathologists.

JOHN POTTS, DO, RES ’00, FAAFP , is vice president and chief medical information officer at Main Line Health. Dr. Potts completed his family medicine internship and residency at PCOM after earning his medical degree from the Chicago College of Osteopathic Medicine of Midwestern University.

PRERAK ADHURIA, PHARMD ’17 , is a pharmacy solutions analyst at CaryHealth, which delivers personalized digital healthcare experiences at scale. His cross-functional role provides him with firsthand insights into the development/enhancement of products, interactions with team leads and their feedback to improve technology, and differences in patient outcomes via a digital pharmacy experience, health plans medical savings, and improved efficiencies for clinicians and providers. He is a licensed pharmacist in 17 states.




Barbara A. Crothers, DO ’86 , is chief scientist for AlxMed, a cytopathology software company based in Santa Clara, California, and Taipei, Taiwan. AlxMed’s niche is non-gynecologic cytology—all cytology other than Pap tests.
Cytopathology has thus far been an unmet need in digital pathology, Dr. Crothers explains, because unlike surgical pathology, which was “already dealing with two-dimensional images on a glass slide, tissue samples that are a couple of microns thick, and two or three layers of cells,” cytology requires much more scanning. “We compress what we call Z-layers into one image when we’re using a digital scanner, so that the pathologist doesn’t have to use a microscope to focus up and down—they’ll see all of the cell’s features in one flat image.”
AlxMed uses artificial intelligence to deal with the quantitative diagnostic criteria that pathologists have a hard time evaluating “because we’re subjective,” she explains. “For the most part, when we’re doing microscopic work, we’re visually evaluating the size of the nucleus and comparing it to the size of the cytoplasm. But we know that certain cancer cells, for example, have a high nuclear-to-cytoplasmic ratio. And there are some standardized nomenclature systems in cytology for certain body sites, like urine cytology, that specify what that nuclear-to-cytoplasmic ratio should be in


order to define that cell as a cancer cell or a potential cancer cell. The computer can do this very well when it’s trained with artificial intelligence.”
Software companies take a whole slide image and overlay it with AI training models that look at particular components on that slide, “in order to do tasks that pathologists do every day,” Dr. Crothers explains. “For example, we have to count the number of mitotic cells in a tumor by examining high-power fields. We know from studies that we’re not very good at it—we don’t get very good concordance, but it’s important. This can be done by AI very well and very quickly.
“More complicated is training the software that this particular cell is probably malignant, which we do by looking at the cell characteristics. In urine, sometimes you’re looking for a needle in a haystack. You may not have many abnormal urothelial carcinoma cells in a urine specimen, but AI can pick them up a lot quicker than any of us can looking at the slide, and it can also categorize them quickly. The software we’ve developed presents those cells to you on a screen as thumbnail images, with the statistics for each cell, so you know exactly what that cell’s characteristics are.”
The same model can be transformed slightly to fit other specimen types, such as thyroid specimens.

Down the line, says Dr. Crothers, “we’re going to be looking at lung and probably other systems, to create an entire suite of AI software modules.”
Much of AlxMed’s current research is in preparation for an FDA submission, since medical devices can be used in clinical practice only with FDA approval. “That hurdle is very high,” says Dr. Crothers, “and there’s only been one approved AI in cytology to date, just this past year. The FDA is very helpful in giving you guidance on what kind of data they’re looking for. An FDA validation study is usually a very large study that shows proof of concept and the device’s reliability in a medical setting.

“The device doesn’t make the diagnosis, the pathologist does. We have extensive quality assurance programs in pathology, and we’re checking each other all the time. But we could rely on AI to help check us as well, instead of needing another set of human eyes—maybe have AI do a lot of that backend quality assurance work that we do every day.”
In that case, will pathologists lose their jobs?
“I saw this same concern arise with the advent of automated Pap tests,” says Dr. Crothers. “Screening guidelines changed; test volumes dropped, and automation reduced the time required for screening Pap tests. We thought cytotechnologists, who screened most of the Pap tests, would lose their jobs. But meanwhile, there was an unmet need in the lab for small biopsy, fine-needle aspiration specimen quality evaluation because of the implementation of robotics and new methods of collecting specimens and cells. We needed cytotechnologists to go to these procedures to evaluate the adequacy of these specimens. Very few cytotechnologists lost their jobs.”
What’s more, she points out, “there continues to be a decline in the number of individuals who are doing cytotechnology. Schools are not putting out enough technologists to meet the need, and the shortage is worldwide. The same is true for pathology, and honestly, the same is true for medicine. We’re at a crisis point; we don’t have enough individuals to do the work. AI could free us up from some of the time-consuming manual tasks.”
Besides her involvement in AlxMed’s research studies, Dr. Crothers is responsible for developing the training materials and for training investigators and future customers on the use of the software. “If I’m involved in the process,” she says, “I can help to fine-tune how it will be helpful to pathologists in their day-to-day practices.”
As chief medical information officer at Main Line Health, John Potts, DO, RES ’00, FAAFP , is responsible for facilitating the electronic medical record (EMR) strategy, implementation, optimization and data analytics for users throughout the Main Line Health Network. This means ensuring that people have the technology they need in their roles and the knowledge to use it—and AI increasingly is central to that technology.
About the concern that AI is going to take people’s jobs, Dr. Potts says, “AI offloads tasks, whether from a physician, nurse, medical assistant or medical biller. I suppose if you offload enough tasks for someone’s specific role, you might be able to repurpose them to a different role. But I don’t see artificial intelligence replacing people. In fact, as baby boomers get older, and sicker, and Gen X is starting to head into the retirement years, we don’t have enough of Gen Z coming out of schools to replace folks that are retiring. We can’t hire our way out of this.”
An example of AI providing diagnostic assistance is Main Line Health’s use of a platform that reviews CAT scans to not only look for large vessel strokes, but to “immediately alert our stroke team by phone to go see that patient, and it tells them where that patient is,” says Dr. Potts. “It also alerts our radiologists and prioritizes that film to be read immediately. If the patient truly is having a stroke, then we can begin treatment right away. And that’s allowed us to decrease our times to treatment for the appropriate patients.” Besides neurology, the platform is being used in cardiology and pulmonology.
Clinician assistance can take the form of AI generating replies to questions on patient portals. It turns out that “AI is far more verbose than our clinicians,” says Dr. Potts. “Studies have shown that patients often like the AI replies—‘Look how much time the doctor spent writing back to me’— but a long reply might encourage a patient to keep asking more questions over the portal as opposed to coming in for a visit. That’s always been a feature of having patient portals, of course, but we had to work with our AI and prompt training to dial down the length of the replies.”
What’s more, the clinicians might say that a reply doesn’t capture their “voice.” Dr. Potts recalls, “We once had a patient call the office to ask, ‘Is the doctor feeling okay? Their reply to me doesn’t sound like them.’ The AI we use is a generic model—a HIPPA-compliant version of GPT4. Training AI so it can mimic clinicians is extremely expensive and very challenging. But companies are pursuing this, and our development team is working on it as well, so that the AI would train off a model that would be tailored to individual clinicians.”
Whether you’re a mid-size health system like Main Line Health or a larger network, says Dr. Potts, the key question is “how do you scale whatever you’re bringing to the clinical side. For example, we’re looking to create an innovation room—a patient room that brings in all the new technologies to see how they work with the other equipment, what the workflows are like. We want to bring in doctors and nurses to test innovations and determine if they’re ready for rollout on a broad scale.”
Dr. Potts predicts that the hospital is going to radically change in the next three years for patients and for staff and become a “smart hospital room.”
“Technologies using cameras can take a patient’s vital signs, contactless—pulse rate, heart rate, temperature, and we’re told that blood pressure is coming in the near future. A nurse or care tech won’t have to interrupt the patient, whether they’re with family during the day or sleeping at night. No one will have to manually enter those vital sign numbers into the EMR.
“AI in that same camera can detect whether the patient is a fall risk, and if so, alert somebody on the floor. It can show us if a patient is at risk for developing pressure ulcers, or is smoking in the room and at risk of causing a fire, or if somebody has brought a weapon into the room. There’s lots of use cases for AI in the room, not only for the patient, but for the hospital staff as well.”
Dr. Potts points out that every specialty can benefit from AI. “Think dermatology, for example. AI models can do as well as a person looking at a lesion to determine if it’s malignant or not. Precision medicine and human genomics—they’re sequencing patients’ DNA and then loading it back into the EMR. AI can look at a humongous amount of data and help predict for us what cancer treatments are the best options for a particular patient based on their genomics. That is really exciting, and that day is coming.”
Dr. Adhuria is currently the project manager for all CaryHealth conferences—for the pharmaceuticals industry, for payers, for providers—related to Clair: Clinical AI Reference, a tool focused on fast, precise information retrieval. Besides attending some of these conferences, he vets them and determines how the team will reach out to attendees. Clair, which is designed for quick lookups of medical guidelines, evidence-based practices and other clinical data without extensive patient-specific integration, gives users answers within seconds, says Dr. Adhuria, rather than the minutes needed by other resources.
Clair’s answers are geared toward whoever’s asking it a question. The app allows retail pharmacists, physicians and other professionals who see patients throughout the day to answer patient questions right away, face-to-face, rather than making an extra trip to look something up. “A professional can ask Clair about a medication’s effects on blood pressure or drug interactions,” explains Dr. Adhuria. “But a lay person could ask Clair if it’s OK to be taking three medications together. Meanwhile, the admin team could ask about ICD-10 codes for billing purposes.”
Some people think of AI as “an engine out there that does its own thing,” Dr. Adhuria says, “but with proper guardrails and monitoring, it makes people’s jobs easier, allowing them to focus on the patient’s needs.” Dr. Adhuria especially loves to connect with students, and at a recent conference of the Academy of Managed Care Pharmacy, “I got to see students’ reactions,” he says, “and it was blowing their minds.”
As a pharmacy solutions analyst at CaryHealth, Prerak Adhuria, PharmD ’17 , explains, “I’ve been working very closely with marketing sales as well as development enhancements of products within our company that use AI—improving our tech and seeing the patient outcomes in the digital pharmacy experience—as well on the patient side and on the health plan side, so payers and health systems can make better decisions. My role is essentially to be a bridge that supports the C-suite, connecting my pharmacy background with the technology background I’m learning and then tying it all together.”
OneDash, another CaryHealth offering, is a population health tool: an AI-driven clinical automation platform designed to identify and automate the closure of care gaps. A plan can, for example, immediately see if any patients with diabetes are not on a statin, or pull all patients in a particular age range that have been taking a particular medication over the past three months. Previously, that might take the health plan a couple of weeks. Now, says Dr. Adhuria, “the turnaround is 10 or 20 minutes. And that allows decisions to happen faster.” Automations save time, too, not only by sending faxes to doctors’ offices but by making AI-assisted calls to patients “that sound like a normal conversation,” says Dr. Adhuria. He notes that a health plan in the DC/Maryland/Virginia area has recently been able to see financial savings, improved patient outcomes and increased patient adherence rates.
“A doctor can do their job,” he continues, “without having to handle prior authorizations submitted by pharmacies, without having to reach out to
the insurance company. It was a mess, and now all this is automated. Doctors love this because now they can spend more time taking care of patients; pharmacists love this because now they can talk to patients who come to the pharmacy to get their prescription.”
Before he graduated from PCOM, Dr. Adhuria worked for almost a decade as a technician and intern with CVS. After he graduated, he did independent pharmacy work “in a small town, with a very small patient base—home care, assisted living services, packing medications in a bubble pack, delivering those medications at 8:00 PM if I had to. I knew people had no other means of getting what they needed, and I thought, ‘There has to be a better way.’”Next, working with a mail order retail pharmacy, he learned “how to improve on efficiencies and get 100 percent of our medications out every day without sacrificing quality. So I went from delivering medication myself to someone’s house to being able to ensure they could have it mailed to them before their medications run out.”
Now, with CaryHealth, Dr. Adhuria works with a digital pharmacy that is licensed in 50 states and “offers phenomenal patient experience. Whether you need to refill a medication, or discontinue a medication, or want to check on something, you can just do it from your mobile app.”








Ravi David Yarid, DO, assistant professor of osteopathic manipulative medicine at PCOM Georgia and a member of the American Osteopathic Information Association’s Digital Health Innovation Steering Committee, provides insight into AI’s impact on osteopathic medicine.
Healthcare Data as a Major Asset
AI thrives on data, which holds immense potential in medicine. AI can help uncover correlations and trends in treatment efficacy; it can personalize medical education, and even provide deeper insights into osteopathic manipulative medicine (OMM).
AI’s Role in Healthcare Data Utilization
AI-driven predictive modeling enhances disease prevention strategies, while personalized treatment plans can be optimized in real-time with up-to-the-minute evidence-based medicine. Additionally, AI holds promise for expanding osteopathic care into rural and underserved areas, addressing disparities in healthcare access.
Ownership and Responsibility
The osteopathic profession must ensure that healthcare data remains controlled by those who generate it. By preventing corporate monopolization, the osteopathic profession can establish an ethical framework that ensures AI benefits all stakeholders, rather than prioritizing profit over care.
Bridging AI and Osteopathic Medicine
Much of today’s AI-driven healthcare development is corporate-led, often sidelining the patient-first, holistic approach central to osteopathic medicine. The profession can ensure alignment and growth from its foundational philosophy by developing its own AI models rooted in osteopathic principles and practices.




















Need for an Osteopathic AI Governance Model




An AI governance framework that focuses on transparency, accountability and patient-centered solutions is essential. This model should ensure compliance with data security regulations while fostering innovation that aligns with osteopathic values.
Osteopathy’s Opportunity to Lead Digital Health
AI-powered training tools, decision-support systems and patient engagement platforms can transform osteopathic education and practice. Early integration of AI into osteopathic medical schools can set the standard for responsible AI use in medicine.
THE FUTURE OF AI IN OSTEOPATHIC MEDICINE
AI as a Force Multiplier for DOs
Rather than replacing hands-on osteopathic care, AI can enhance it. AI-driven diagnostics and predictive insights can improve treatment precision, while AI-assisted education can provide customized learning experiences for students, allowing faculty to focus on knowledge comprehension and provider skill training.
Developing AI-Driven Healthcare Systems
AI-powered research can unlock new insights into the efficacy of OMM, identifying patterns that further validate osteopathic approaches. Integrating AI into medical education can foster the next generation of DOs equipped with advanced analytical tools.
Osteopathic medicine has always prioritized treating the whole person. With appropriate and responsible integration, AI enhancement of medical education and practice will position osteopathic medicine as the gold standard in ethical, data-driven health care. Now is the time for osteopathic leaders to guide AI’s development, ensuring it serves the profession’s mission of advancing education, research and patient care for the betterment of all.






























On June 7, members of DO classes ending in 0 and 5 will gather to celebrate to reconnect and reminisce about their times spent at PCOM at the 2025 Philadelphia Reunion Celebration. The luncheon will take place at La Collina restaurant in Bala Cynwyd, Pennsylvania, and will honor the 50th reunion class of 1975, as well as the 55th, 60th, 65th, and 70th reunion classes of 1970, 1965, 1960, and 1955. A full schedule and registration will be available in March—join us for a special luncheon celebrating your milestone reunion.

POP CULTURE
Song of the Year: “Love Will Keep Us Together” by Captain and Tennille Movies Released: One Flew Over the Cuckoo's Nest, Barry Lyndon, Jaws
Super Bowl Champions: Pittsburgh Steelers



A classic view of

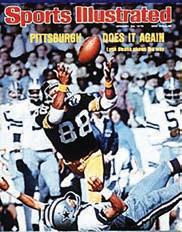
PCOM’s first-ever Medicine Cup ice hockey game saw the student team defeat the faculty 12-10, but with an enthusiastic crowd of 800 and nearly $2,000 raised for the student loan fund, all were winners in a night of fun and fundraising.


On June 1, the 156 members of

PCOM welcomed two distinguished military trailblazers as keynote speakers at its Military Medicine Symposium, hosted by the student division of the Association of Military Osteopathic Physicians and Surgeons. U.S. Army Surgeon General Lieutenant General Mary Krueger Izaguirre, DO ’95, and Retired Lieutenant General Ronald Ray Blanck, DO ’67, former U.S. Army Surgeon General and Vietnam battalion surgeon, shared their invaluable experiences and insights, inspiring military medical professionals from across the nation.
With more than 5,000 osteopathic physicians, physician assistants, pharmacists, physical therapists and behavioral health professionals serving in the U.S. Armed Forces—many of whom are PCOM alumni—the College remains a cornerstone of military medicine. Currently, 50 DO students are recipients of Armed Forces Scholarships, proudly representing the Air Force, Army, Navy and National Health Service Corps.
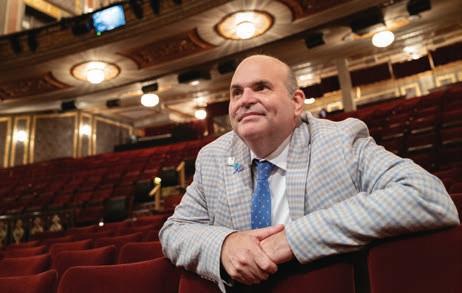
PCOM celebrates Jason Kindt, DO ’99, who accepted a 2024 Tony Honor for Excellence in Theatre on behalf of the Entertainment Community Fund and Mount Sinai Doctors’ Samuel J. Friedman Health Center for the Performing Arts. As medical director of the Friedman Center, Dr. Kindt leads a facility dedicated to providing primary and specialty care tailored to New York City’s vibrant theater and performing arts community. Congratulations to Dr. Kindt for this extraordinary recognition of his work at the intersection of medicine and the arts!
1966
Ralph E. Fishkin, DO, Bala Cynwyd, PA, recently celebrated his 84th birthday and is continuing to practice part-time in his home office. Dr. Fishkin is a personal and supervising analyst at the Psychoanalytic Center of Philadelphia. He also acts as a reviewer for the Journal of the American Psychoanalytic Association and the International Journal of Applied Psychoanalytic Studies
1968
Richard L. Gordon, DO, Voorhees, NJ, is a hematology and oncology specialist at Comprehensive Cancer and Hematology Specialists in Voorhees.
1970
John W. Becher, DO, Newtown Square, PA, was featured in the article “Doctors Weigh In on Full Moon Superstition


in Hospitals: Everybody Talks about the Bewitching Hour” in the New York Post (April 22, 2024). Dr. Becher discussed his experience with the folk tale—and how he sees an increase in patient volumes during a full moon.
Darryl A. Robbins, DO, Westerville, OH, was featured in the CityScene article “The Uncertain Book Club” (July 1, 2024), which spotlighted his innovative book club for children aged 8–14. Founded in 2020 after his retirement from a 45-year career in pediatric medicine, the club encourages young readers to explore diverse reading styles and levels.
1973
Stuart D. Levy, DO, West Chester, PA, is enjoying retirement after 40 years of psychiatry practice.




Okatie, SC, recently ended his term on the PCOM Board of Trustees. At his final meeting, he was presented with a certificate of appreciation for 21 years of dedicated service to PCOM and the Board.
1975
James E. Hoffman, DO, Cape Girardeau, MO, was featured in the Southeast Missourian article “Faces of Southeast Missouri: Dr. Jim Hoffman” (August 15, 2024). The piece detailed Dr. Hoffman’s inspiring journey into medicine and his ongoing medical missionary work around the globe. A retired pediatrician, he continues to support communities by focusing on prevention and education through his medical expertise.
Edward H. Yob, DO, Broken Arrow, OK, was featured in The DO article “Meet the DO Who Served in the White House Medical Unit During the Reagan Administration” (July 31, 2024). Dr. Yob broke new ground for DOs on that service. He also served as personal physician to former Vice President George H. W. Bush and assistant physician to former President Ronald Reagan.
Ted S. Eisenberg, DO, Philadelphia, PA, wrote the foreword and contributed two chapters to Manual of Cosmetic Medicine and Surgery: Volume 2 Breast Reshaping, a new textbook published by Springer International. One chapter details Dr. Eisenberg’s I.D.E.A.L. Breast Lift, a staple-first technique that can be combined with breast augmentation. The other highlights his innovative, lessinvasive method for correcting tuberous breasts using saline implants in a single-stage procedure. Dr. Eisenberg is a Philadelphia-based plastic surgeon specializing exclusively in cosmetic breast surgery. Cecilia M. Smith, DO, Reading, PA, was appointed associate dean of the Tower Health Regional Campus of Drexel University College of Medicine. Dr. Smith served
as chair of the Department of Medicine at Reading Hospital for 18 years until her transition to associate dean.
Thomas A. Haffey, DO, Roseland, FL, joined the staff of Sebastian River Medical Center in Roseland as a cardiologist.
Richard B. Russell, Jr., DO, Pine Grove, PA, was honored at the dedication of the new Lehigh Valley Physicians Group Family Medicine building in recognition of his 40 years of service in medicine. Dr. Russell was presented with two plaques commemorating his dedication to health care in the Pine Grove community.
1979
Andrew J. Gelman, DO, Palm Beach Gardens, FL, transitioned from clinical orthopedic surgery to a focus on musculoskeletal forensics. He is a certified medical-legal evaluator and a fellow of the International Academy of Independent Medical Evaluators.
William B. Swallow, DO, MS/ FM ’20, Dingmans Ferry, PA, was installed as the 113th president of the Pennsylvania Osteopathic Medical Association (POMA), the statewide organization representing doctors of osteopathic medicine. Before his election as president, Dr. Swallow served as a trustee for POMA’s District 5 and chaired multiple committees. He also represents POMA as a delegate to the American Osteopathic Association House of Delegates.
1980
Nicholas O. Biasotto, DO, Wilmington, DE, is president of the New Castle County Physician Organization in Delaware. He also hosts the Health
Care Reality podcast for the Medical Society of Delaware. Previously, Dr. Biasotto served as president of the Medical Society of Delaware and as medical director of ChristianaCare’s Wound Care and Hyperbaric Oxygen Center in Wilmington.
David A. Bitonte, DO, MBA, MPH, Uniontown, OH, was honored with the 2024 Ohio Osteopathic Association Board of Trustees Award at the Ohio Osteopathic Symposium in April in Columbus.
Gerald V. Klim, DO, Lexington, KY, retired from the University of Kentucky College of Medicine after 36 years in the Department of Physical Medicine and Rehabilitation.
Alice Gertrude McCormick, DO, Phoenix, AZ, received the 2024 Distinguished Service Award from the Arizona Osteopathic Medical Association. This award honors a physician or non-physician who has significantly contributed to improving the community and promoting osteopathic medicine, donated their time to improve mankind and/or has volunteered their time to the community or association.
Kathleen M. Tylman, DO, Pompano Beach, FL, retired after a distinguished career in internal medicine. She is proud of her two successful children and several grandchildren.
Bruce A. Feinberg, DO, Atlanta, GA, launched the Weekly Check-Up Podcast after 13 years of hosting the healthcare radio show The Weekly Check-Up on 99.5. In the podcast, Dr. Feinberg offers the community the latest health information and a platform to share their views on health and medicine. He is the president and chief executive officer of Georgia Cancer Specialists in Atlanta.
1983
Beth A. Loss-Higgins, DO, York, PA, retired from family practice in 2022 after 36 years in private practice alongside her husband, Ken Higgins, DO ’83.
Joan Sureck Naidorf, DO, Alexandria, VA, was featured on the Nurse Keith Show (March 29, 2024), where she discussed “Let’s Change How We Think About Difficult Patients.” Dr. Naidorf shared her insights from working in the emergency room and explored how medical professionals can reevaluate their approach to patient care. She is an author and a retired emergency medicine physician.
Kenneth E. Wood, DO, Hershey, PA, was appointed vice dean for clinical affairs and professor of medicine at Penn State University College of Medicine. He also serves as executive vice president and chief medical officer for the Penn State Health System.
1985
Robert Hostoffer, Jr., DO, Cleveland, OH, was honored with the 2024 American Osteopathic Foundation Lifetime Achievement Award. This prestigious award recognizes individuals who have made significant contributions to the osteopathic profession throughout their careers. A leader at the local, state and national levels, Dr. Hostoffer has served as president of the Ohio Osteopathic Association, American College of Osteopathic Pediatricians, Cleveland Academy of Osteopathic Medicine, and Cleveland Allergy Society. He currently serves on the American Osteopathic Association Board of Trustees.
1987
Michael A. Becker, DO, MS, Blue Bell, PA, associate dean of clinical education, PCOM,

Lafayette Hill, PA, medical director of student wellness at PCOM, is pleased to announce the birth of his grandson, Maxwell Harrison. Maxwell is the son of Jamie Finkelstein and Dan McGrath, the great-grandson of Marylyn and the late PCOM President Leonard Finkelstein, DO ’59, and the great-nephew of Robert Finkelstein, DO ’90, Lisa Finkelstein, DO ’87, and Marc Domsky, DO ’86. Dr. Finkelstein also coauthored a research study titled “Utilization of Telemedicine to Supervise Medical Students in the Post-Acute/ Long-Term Care Setting,” published in the Journal of the American Medical Directors Association (August 3, 2024).
was the 2024 recipient of the Osteopathic Family Medicine Educator of the Year Award presented by the American College of Osteopathic Family Physicians.
Anthony B. Furey, DO, Wilmington, DE, authored an article for Women’s Journal titled “Improving Heart Failure Treatment at Cardiology Physicians, PA.” In the article, Dr. Furey discussed the severity and signs of congestive heart failure and emphasized the Cardiology Physicians Heart Failure Clinic in Newark as a key resource for treatment.
Suzanne L. Huffnagle, DO, Drexel Hill, PA, was honored with the Distinguished Service Award at the American Osteo-
pathic College of Anesthesiologists (AOCA) annual conference in St. Pete Beach, FL. A longtime member of the AOCA, Dr. Huffnagle has served on multiple committees and on the Board of Governors for the past six years. She is a professor of anesthesiology with a subspecialty in obstetric anesthesia and practices at Thomas Jefferson University Hospital in Philadelphia.
John F. Perri, DO, Chula Vista, CA, is the director of sleep medicine at the Naval Medical Center in San Diego. Dr. Perri also completed the master’s program in engineering for healthcare systems at Lehigh University.
Mark D. Beyer, DO, Muncy, PA, joined UPMC as an emergency medicine physician in Muncy.
Marla DePolo Golden, DO, Moultrie, GA, dean of the Osteopathic Medicine Program at PCOM South Georgia, was selected as one of 32 participants for the inaugural cohort of the American Association of Colleges of Osteopathic Medicine Graduate Medical Education Development Fellowship. Dr. Golden also participated in a debate on Florida’s recreational marijuana proposal, Amendment 3, on WJCT News 89.9 on October 22, 2024.
John A. Avallone, DO, Somers Point, NJ, joined Shore Physicians Group in Somers Point as an orthopedic surgeon. A. Roby Lal, DO, Galesburg, IL, joined Third Order of Saint Francis Healthcare in Galesburg as a radiation oncologist. Gregory McDonald, DO, Philadelphia, PA, chair of Forensic Medicine and Pathology at PCOM, was featured in the Pittsburgh Post-Gazette in an article titled “Why Forensic Pathologist Shortage Matters for Allegheny County and Across the Country” (April 22, 2024). In the article, Dr. McDonald discussed the challenges posed by a lack of funding and a shortage of forensic pathologists, which hinder the timely resolution of cases.
George J. Papanicolaou, DO, Byfield, MA, was featured on the Doctors Pharmacy podcast (April 15, 2024) to discuss “How to Recover from IBD without Surgery & Medication.” Dr. Papanicolaou shared insights on functional medicine approaches that help reduce symptoms of inflammatory bowel disease, focusing on solutions beyond medications and surgery.
1990
Steven F. Gitler, DO, Cherry Hill, NJ, retired after 31 years in practice. Dr. Gitler spent 24 years in private family practice and the last eight years in urgent care. In retirement, he enjoys spending time with his wife and daughter and runs an online collectibles business, frequently participating in estate sales, auctions and thrift shop visits to find items to resell.
Peter J. Dourdoufis, DO, Stratham, NH, has been appointed chief of cardiology at Portsmouth Regional Hospital. In addition to his new role, Dr. Dourdoufis serves as director of the hospital’s non-invasive cardiology program and is a member of the core faculty for its internal medicine residency program, which is accredited by the Accreditation Council for Graduate Medical Education.
David A. Doyle, DO, New York, NY, is a forensic psychiatrist at Manhattan Psychiatric Center.
Timothy Horsky, DO, Bedford, PA, joined WindberCare Surgical Associates & Bariatrics in Windber as a general surgeon. Dr. Horsky also joined the medical staff and general surgery practice at Chan Soon-Shiong Medical Center in Windber.
Noi Walkenstein, DO, Philadelphia, PA, joined Roxborough Memorial Hospital’s Family Medicine Practice as an internal medicine physician.
1992
Richard Thomas Jermyn, DO, Lititz, PA, was appointed dean of Rowan-Virtua School of Osteopathic Medicine. Dr. Jermyn assumes the role after overseeing the academic, research and clinical affairs of the school in an interim capacity for the past year. During Dr. Jermyn’s time as interim dean, the school enjoyed growth in both enrollment and research activity/funding.
Henry C. Novroski, DO, Shavertown, PA, joined The Wright Center for Community Health in Tunkhannock as a primary care physician. Brian Keith Steele, DO, Pittsford, NY, was featured in Medical Economics in an article titled “The Case for Transitioning to Value-Based Care” (July 24, 2024). Dr. Steele discussed key topics such as cost savings, physician burnout, quality improvement, and the future of value-based care, emphasizing how a successful transition can benefit healthcare organizations. Dr. Steele is the chief medical officer for Collaborative Health Systems in White Plains.
Anne B. Whalen McGinn, DO, Ewing, NJ, joined Capital Health Primary Care in Ewing.
Kelly Lynn Abbrescia, DO, Middletown, DE, was named regional vice president of the South Division at US Acute Care Solutions, the nation’s largest physician-owned emergency and inpatient medicine practice. Prior to this role, she served as the medical director at Carteret Health Care in Morehead City, North Carolina, and has held various leadership positions throughout her career.
Lt. Col. Stephanie Roell Fugate, DO, Fairfax Station, VA, was recommissioned to the U.S. Army Reserves after a 20-year hiatus. The ceremony, held at the Pentagon, was presided over by Lt. Gen. Mary K. Izaguirre, DO ’95, Surgeon General of the U.S. Army.

Carmel, IN, published an Amazon best-selling medical textbook, The Comprehensive Physicians’ Guide to the Management of PANS and PANDAS The textbook is based on Dr. Antoine’s approach to treating this type of autoimmune encephalitis and has become the standard of care for the treatment of these conditions.
Their long-standing friendship and professional connection added a meaningful depth to the proceedings.
1996
Nicole Marie Alu, DO, Salisbury, NJ, joined TidalHealth Family Medicine Practice in Salisbury as a family medicine physician.
James Frederick Frommer, DO, Duncansville, PA, opened Quantum HealthCare Services LLC in Duncansville as a solo osteopathic physician offering osteopathic manual medicine, regenerative medicine, extracorporeal shock wave therapy, IV nutrition, and functional medicine.
1997
Marc Aaron Greenstein, DO, Atlanta, GA, was named a Top Doc by Atlanta Magazine (July 8, 2024). Dr. Greenstein is a urologist with Advanced Urology in Atlanta.
Gretta A. Gross, DO, York Haven, PA, was appointed executive vice president for assessment and chief assessment officer of the National Board of Osteopathic Medical Examiners (NBOME). In this role, she will lead major NBOME testing departments and develop strategies to guide the innovation of current and future assessment tools. Dr. Gross previously served as vice president for clinical skills testing at NBOME from 2018 to 2021.
Mia Lynne Julia VanEken, DO, Chandler, AZ, joined East Valley Women for Women in Queen Creek as an obstetrician/gynecologist.
1998
Sheila F. Hockman, DO, Honesdale, PA, joined Wayne Memorial Community Health Centers in Honesdale as an obstetrician/gynecologist.
James Vincent Lieb, DO, State College, PA, joined Penn Highlands Oncology/Hematology
located in Huntingdon, Tyrone and State College.
Thomas Donald Scott, DO, Danville, PA, has expanded services and is accepting new patients at the UPMC Outpatient Center in Lewisburg. Dr. Scott is an interventional cardiologist with UPMC Heart and Vascular.
1999
William Edward McElmoyle, DO, Ewing, NJ, joined Capital Health Primary Care in Ewing. Kerry Marquez Scott, DO, Meridian, MS, hosted a community cooking class at Rouses in Gulfport, where he educated participants on healthier eating habits. Dr. Scott is a culinary medicine specialist at Memorial Health.
2000
Jill Marie Eckert, DO, Hershey, PA, assumed the role of chair of the Department of Anesthesiology and Perioperative Medicine at Penn State Health in August, after serving as interim chair since 2022. Dr. Eckert began her career at Penn State Milton S. Hershey Medical Center as an anesthesiology resident and served as chief resident. She then completed a chronic pain medicine fellowship before joining Penn State as a faculty member.
George John Gurdock, DO, West Palm Beach, FL, is the TeamHealth system medical director of emergency medicine for the Palm Beach Health Network emergency departments in West Palm Beach.
2001
Lori A. Alfonse, DO, Zionsville, PA, is featured in the article, “Breast Cancer Surgeon Lori Alfonse, DO, Sees the Future of Health Care in Her Hometown,” published by Lehigh Valley Health Network (LVHN) (October 5, 2024). Dr. Alfonse is a breast cancer surgeon at LVHN.
Kelly A. Felix, MS/PA, Rehoboth Beach, DE, recently rejoined Beebe Healthcare as a physician assistant in the hospital’s cardiac catheterization lab.
Carl R. Hoegerl, DO, Forest, VA, was appointed president of the Virginia Osteopathic Medical Association in April. Dr. Hoegerl’s term will run through spring 2026.
2002
Adnan Allan, DO, Macungie, PA, was appointed division chief of the Inpatient Pediatric Unit at St. Luke’s Children’s Hospital. In this role, he is responsible for overseeing the clinical and administrative functions of the unit, as well as supporting its growth and development.
William Craig Leach, Jr., DO, Lake Geneva, WI, joined Mercyhealth Hospital and Medical Center in Lake Geneva as an obstetrician and gynecologist. Michael Ernest Srulevich, DO, Wynnewood, PA, medical director, Physician Assistant Program, PCOM, co-authored a research study titled “Utilization of Telemedicine to Supervise Medical Students in the Post-Acute/ Long-Term Care Setting,” published in the Journal of the American Medical Directors Association (August 3, 2024).
Gregory Andrew Ambuske, DO, Broomfield, CO, joined Heart of the Rockies Regional Medical Center in South Park as a primary care physician.
Alex Diamond, DO, Nashville, TN, was named chair of the National Federation of State High School Association’s Sports Medicine Advisory Committee. Dr. Diamond is a professor of orthopedic surgery, pediatrics and neurological surgery at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
Tochi Margaret Okwuosa, DO, Naperville, IL, authored an article for blackdoctor.org titled “What Black Cancer Patients Should Know About Heart Damage After Treatment” (August 2, 2024). In the article, Dr. Okwuosa explored the connections between cancer treatment and the risk of cardiovascular issues. She is a professor and the director of the Cardio-Oncology Program at Rush University Medical Center in Chicago.
Tamika Lashunda Perry, DO, Dallas, TX, was featured as a “Superb Woman” by Metro News on August 20, 2024. She is a family physician at WellMed Medical Management, Optum Inc., USMD, Uptown Health & Wellness Center, and Redbird Community Clinic.
Cathleen Marie Brown, DO, North Wales, PA, was named medical director of Winona, a leading menopause telehealth company based in Austin, Texas. In this role, she serves as the company’s spokesperson and regularly contributes to the Winona Medical Journal, sharing her expertise in women’s health and menopause care.
Henry Gaihong Luu, DO, Middletown, CT, was appointed medical director at PursueCare, LLC, in Middletown. Leslie Alexandriana Saltzman, DO, Brooklyn, NY, authored an article for Ovia Health titled “What I Wish Every Person Knew About the Postpartum Period: A Physician’s Perspective” (September 18, 2024). In the article, she shares her insights on the postpartum experience from both a physician’s and a mother’s perspective, aiming to raise awareness of the importance of supportive postpartum care.
2005
Brian Anthony Acunto, DO, Brigantine, NJ, is an emer-
gency medicine physician at AtlantiCare Regional Medical Center in Atlantic City.
Benjamin Robert Kuhn, DO, Mount Pleasant, SC, is a pediatric gastroenterologist at MUSC Children’s Health in Mount Pleasant.
2006
Nicol E. Joseph, DO, RES ’06, Sicklerville, NJ, program director, Geriatric Fellowship, PCOM, co-authored a research study titled “Utilization of Telemedicine to Supervise Medical Students in the Post-Acute/Long-Term Care Setting” published in the Journal of the American Medical Directors Association (August 3, 2024).
Darrin Richard Mangiacarne, DO, Pompano Beach, FL, was sworn in as president of the American Osteopathic Academy of Addiction Medicine at the Osteopathic Medical Education Conference in September 2024.
Patrick M. Parker, DO, Valdosta, GA, joined SGMC Health in Valdosta as an urologist.
Ashlee Linn Smith, DO, Honeoye Falls, NY, was named medical director of perioperative services at Highland Hospital in Rochester.
Brad M. Taicher, DO, MBA, Washington, DC, joined Children’s National Hospital as chief of the division of anesthesiology, pain and perioperative medicine.
Renee Allen Caslow, DO, Marietta, OH, is a full-time provider at Akron Children’s Pediatrics—Belpre.
Stephen Gerard Tiley, DO, Savannah, GA, joined Low Country Cancer Care in Savannah as an oncologist/ hematologist.
Jennifer L. Alvarado, MS/FM, Riverton, NJ, was recognized as Outstanding Teacher of
the Year for New Jersey by the National Association of Biology Teachers. She was featured in an article in the Sun Newspapers titled “This Award Reinforces Why I Became a Teacher” (September 4, 2024). Ms. Alvarado is a biology teacher at Cinnaminson High School.
Emily Lynn Bray, DO, Philadelphia, PA, was promoted to psychiatry residency program director at Jefferson Einstein Philadelphia Hospital. In May 2024, Dr. Bray welcomed a son, Hugo.
Tamika Mozina Carter, DO, Huntington Park, CA, was featured in an article in Switching Fashion titled “Tamika M. Carter, DO, the Multi-Talented Internist Making Waves in Healthcare and Beyond” (May 16, 2024). The article highlighted her work as a physician, as well as her ventures in travel, culinary arts, and fashion. Dr. Carter is the CEO of Travel Medicine Culinary Arts LLC, where she combines her passion for travel and medicine to promote wellness and cultural exploration. She is also the owner of Kaleidoscope Sprinkles, a creative venture blending her love for baking and fashion. Dr. Carter practices as an internist at AltaMed Health Services in Huntington Park.
Monique A. Gary, MS/ Biomed ’05, DO, Perkasie, PA, authored an article for Clinical Leader titled “$100M in Government Funding Helps, But What Can Really Be Done about Trial Diversity?” (April 18, 2024), in which she discussed the importance of diversity in clinical research trials. Dr. Gary was also featured in the Philadelphia Inquirer in an article titled “This Breast Cancer Surgeon Traded City Life for a Farm, Where Her Patients Gathered for Her Fifth Wellness Retreat”
(October 16, 2024). The article focused on Still Rise Farm, Dr. Gary’s farm in Upper Bucks County, PA, where she hosts wellness retreats for breast cancer survivors and patients. Dr. Gary is the medical director of the cancer program and director of the breast program at Grand View Health/Penn Cancer Network in Sellersville.
Peter Arthur Burke, Jr., DO, Newark, DE, is the medical director of the kidney transplant program at ChristianaCare in Wilmington.
Chadd Kenneth Kraus, DO, Allentown, PA, was elected to the 2024-2025 Board of Directors for the American College of Emergency Physicians. Dr. Kraus is an emergency physician and vice chair, research, in the Department of Emergency and Hospital Medicine at Lehigh Valley Health Network.
Lida Fatemi, DO, Albuquerque, NM, was featured in Bloom in an article titled “Doctor’s Orders: Why Sleep Matters for Your Mental Health” (April 26, 2024). In the article, she discusses strategies for improving sleep habits and the crucial connection between sleep and mental health.
Sheedeh Madani, MS/ Biomed, Bryn Mawr, PA, was featured in the September 2024 issue of SuburbanLife in an article titled “Creating Happy Smiles for Every Child.” The article highlighted her pediatric dentistry practice, Bala Kids Dentistry in Bala Cynwyd.
Ebonie E. Vincent, MS/ Biomed, Valley Village, CA, was featured in an ABC News article titled “What to Look for in Slip-On Shoes, According to Experts” (May 2, 2024). In the article, Ms. Vincent shared
expert tips and recommendations for selecting the best slip-on shoes for any occasion.
2012
Kimberley Arthur Maxwell, DO, McChord, WA, was promoted to the rank of Lieutenant Colonel in the United States Army in June 2024, after serving as the inaugural 1st Multi-Domain Task Force Surgeon. She was also selected for a second residency in psychiatry at Walter Reed National Military Medical Center in Bethesda.
Joseph Thomas McDermott III, DO, Chambersburg, PA, is a family medicine physician at Keystone Family Medicine in Chambersburg.
Daniel Douglas McNeill, DO, Trappe, PA, joined Good Shepherd Rehabilitation as the medical director of Good Shepherd Rehabilitation Hospital.
Lisa M. Nail, MS/CCHP, Harleysville, PA, graduated from Fairleigh Dickinson University’s Postdoctoral Master’s of Clinical Psychopharmacology program in February 2024. That same month, she opened her private practice, Attune & Bloom Psychology PLLC, which specializes in compounded and intergenerational trauma, complex health, women’s health and life transitions. Dr. Nail offers telehealth-based individual, relationship and family psychological services across all PsyPact states (currently 40+ states). She also provides mentorship and clinical services to other medical and counseling professionals.
2013
Scott David Glassman, PsyD, Cherry Hill, NJ, director of the Master of Applied Positive Psychology Program at PCOM, delivered a lecture on October 22, 2024, at Temple Health titled “How to Be a Good Lis-

, Merrick, NY, was interviewed by Whispering Stories about her book, Theodore Bearkins Lost His Blue Sunglasses, released on September 16, 2023. In the interview, she shared insights into why she wrote the book and her journey to becoming a writer.
tener: A Path to Building Trust, Empathy, and Connection.”
In the lecture, Dr. Glassman outlined four listening strategies designed to transform one-sided conversations and reduce the likelihood of conflict in communication.
Julie A. Radico, MS/Psy ’08, PsyD ’13, Croydon, PA, published You Will Get Through This: A Mental Health Toolkit— Help for Depression, Anxiety, Grief, and More (2024). The book serves as an all-in-one guide to managing mental health, offering researchbacked strategies to address daily challenges such as depression, anxiety, panic disorder, ADHD and insomnia. Dr. Radico is a board-certified clinical health psychologist and the owner of Radico Psychological and Consultation Services, LLC.
family and geriatric medicine in Grand Rapids.
Kamina Richardson, MS/ODL, Wilmington, DE, was appointed to the board of directors for the Beautiful Brown Girls Foundation. The Beautiful Brown Girls Foundation is committed to incorporating the eight dimensions of wellness into the lives of Black women and providing accessible tools and resources that support everyday wellness.
Ms. Richardson is the assistant director of the nursing department at Temple University.
Dane Richardson Scantling, DO, Canton, MA, was awarded the C. James Carrico, MD, FACS, Faculty Research Fellowship by the American College of Surgeons for his study on trauma and critical care. The two-year, $80,000 award will support his project, Improving Equity and Access to Trauma Care for Victims of Firearm Violence. Dr. Scantling is an assistant professor of surgery at Boston University Chobanian & Avedisian School of Medicine.
Joy Leigh Ishii Zarandy, DO, Duluth, GA, assistant dean of clinical education, PCOM Georgia, received the Rocovich Research Grant, which recognizes a practicing DO or osteopathic medical student working to advance the profession through research that explores the biomechanical, biomedical, or clinical aspects of osteopathic manipulative treatment. Dr. Zarandy was selected based on her innovative research project that focuses on the development and utilization of 3D printed spinal models.
2014
Afriyie Makel Randle, DO, RES ’14, Caledonia, MI, is the owner of the private practice Gray Reign Medical, where she continues to practice
2015
Leah Mickelson Macklin, DO, Duluth, GA, recently launched a “Walk with a Doc” group to encourage community members, students, medical personnel, and physicians to get outdoors and engage in physical activity. Dr. Macklin is a lifestyle medicine and family medicine specialist at Family Practice Center in Johns Creek.
Michael Anthony Minni, DO, Philadelphia, PA, was featured in Suburban Life in an article titled “Satisfying an Urgent Need” (April 2024). In the article, Dr. Minni discussed Roxborough Urgent Care in Philadelphia and highlighted the vital role urgent care plays in serving the community’s healthcare needs.
LeeAnn Mie Tanaka, DO, Philadelphia, PA, was featured in an article for Healio titled “Health Care Providers Excited about Convenient, Safe OTC Birth Control Pill” (April 17, 2024). In the article, Dr. Tanaka discussed the benefits of Opill and offered insights into how it differs from other contraceptive options.
Kelsey Renee Thrush, DO, Washington, DC, has accepted a position as an obstetrics/ gynecology hospitalist at Meritus Medical Center in Hagerstown, Maryland.
Chad M. Weinhold, PharmD, Waynesboro, VA, obtained board certification in oncology pharmacy. Dr. Weinhold practices as an oncology clinical pharmacy specialist at the Phillips Cancer Center at Sentara Martha Jefferson Hospital in Charlottesville.
Laura Elizabeth Poskitt, DO, Lancaster, PA, presented a program titled “A Conversation with the Clinic for Special Children” at Fairmount Homes. As the medical director of the Clinic for Special Children, Dr. Poskitt shared insights into the clinic’s mission, the populations it serves, its approach to care, and the positive impact it has on the community.
Michael Bruce Roberts, PsyD, Woodstown, NJ, director of institutional research, PCOM, co-authored a research study titled “Utilization of Telemedicine to Supervise Medical Students in the Post-Acute/LongTerm Care Setting” published in the Journal of the American Medical Directors Association (August 3, 2024).
2016
Paige E. Black, DO, West Orange, NJ, delivered the keynote speech at the Tyrone Area High School 2024 Commencement Ceremony in Tyrone, Pennsylvania. Dr. Black works as a physician at Goreyb Children’s Hospital at Morristown Medical Center, where her expertise lies in
evaluating, caring for and managing hospitalized children from birth to age 21.
Brian Jeffrey Kramer, DO, Ithaca, NY, joined Northeast Pediatrics and Adolescent Medicine after graduating from residency at Carilion Clinic in Roanoke, Virginia, in 2019. Dr. Kramer became a partner in the practice in January 2021. He currently serves as the chairman of the Pediatrics Department at Cayuga Medical Center in Ithaca.
Nicole Sara Ruth, DO, New York, NY, was interviewed by Marie Clare for an article titled “The 14 Best Pore Minimizers for Smooth Skin, According to Dermatologists” (August 29, 2024).
Eric A. Bradley, DO, Mount Pleasant, PA, joined West Virginia University Medicine Uniontown Hospital as a sports medicine physician.
Edmond John Douglas Fenton, DO, Thomasville, GA, joined Archbold Memorial as an emergency medicine physician.
Petros Koutsogiannis, DO, Laurinburg, NC, joined OrthoCarolina in Laurinburg as a spine surgeon.
Richard A. Francesco, MS/ Biomed ’14, DO ’19, Clayton, NJ, joined the 94WIP Morning Show (October 14, 2024) to discuss the Eagles’ injuries from their week six win over the Browns, focusing on a hamstring injury sustained by offensive lineman Jordan Mailata. Dr. Francesco is a primary care sports medicine physician, board certified in both family medicine and sports medicine.
Samantha J. Giangrande, PsyD, Philadelphia, PA, received the Arthur W. Melton Early Achievement Award during the American Psychological Association
conference held in August. Dr. Giangrande is a submarine psychologist for the Submarine Readiness Squadron 32.
Samuel Alexander Schadt, DO, Coopersburg, PA, participated in the 2024 American-European Congress of Ophthalmic Surgery in July. Dr. Schadt was one of 20 eye surgeons selected from throughout the United States for the opportunity.
Farrah Rink Thompson, DO, Florence, SC, joined McLeod Regional Medical Center in Florence as a critical care specialist.
Jesse Eugene Thompson, DO, Florence, SC, joined McLeod Regional Medical Center in Florence as a hospitalist.
Shane Thomas Bealer, DO, Middletown, NY, joined Crystal Run Healthcare in Middletown as a sports medicine physician.
Julia Therese Boyle, PsyD, Paoli, PA, recently obtained her specialty board certification in clinical geropsychology from the American Board of Professional Psychologists. Dr. Boyle also holds a specialty board certification in behavioral sleep medicine (Diplomate of Behavioral Sleep Medicine), obtained in 2022. Dr. Boyle is the first psychologist to hold both specialty board certifications simultaneously.
Mary R. Festa, DO, RES ’20, was inducted as a fellow of the College of Physicians of Philadelphia.
Jude Leo Opoku-Agyeman, DO, RES ’20, Philadelphia, PA, has been recognized by the Philadelphia Inquirer as a city favorite for both cosmetic surgery and liposuction. An award-winning, board-certified Black plastic and reconstructive surgeon, Dr. OpokuAgyeman is the founder of Opoku Plastic Surgery and performs major surgeries for
high-profile clientele from around the world.
Timothy Charles Shuey, DO, Coal Township, PA, is a cardiology fellow at Geisinger Medical Center in Danville.
Mark Milo Ujevich, DO, Aliquippa, PA, joined UPMC as an emergency medicine physician in Muncy.
2021
Aysha Azam, DO, Somerville, NJ, joined the faculty at Somerset Family Practice at Robert Wood Johnson University Hospital Somerset.
Shelby E. Comeaux, MS/ Biomed ’17, DO, Suwanee, GA, is pursuing a cardiology fellowship at the Medical College of Georgia in Augusta.
Charles R. Cosby, MS/Biomed ’17, DO, Harlem, GA, joined Northeast Georgia Physicians Group Toccoa Clinic as a family medicine physician. Devaki Ashwini Dravid, DO, Maysville, KY, is a resident at PrimaryPlus, the first residency program in northeast Kentucky.
Shalonda Griffin, PsyD, Willingboro, NJ, serves as a clinical psychologist in the U.S. Army, providing critical mental health care to those who serve in the armed forces. Dr. Griffin shares that it has been a profound experience, allowing her to support service members through challenges both on and off the battlefield and around the world.
Kelsey Kreyche, DO, Philadelphia, PA, is working as a hospitalist at Penn State University and at Hospital Loma de Luz in Balfate, Honduras.
Lauren Melley, DO (RES ’26), Ambler, PA, won the 2024 Pennsylvania Academy of Otolaryngology Resident Conchal Bowl (ENT Jeopardy competition) in Hershey. As a resident in the PCOM Otolaryngology Program, she competed against otolaryngology residents in programs from across Pennsylvania.
Paulina E. Rudy, DO, Milford, DE, joined Bayhealth Primary Care in Milford as a primary care physician.
Sierra Armbrust, DO, Rome, GA, was named chief resident of the Atrium Health Floyd Medical Center Family Medicine Residency Program.
Paul J. Carango, MS/Biomed, Newtown Square, PA, coauthored a research study titled “Utilization of Telemedicine to Supervise Medical Students in the Post-Acute/LongTerm Care Setting” published in the Journal of the American Medical Directors Association (August 3, 2024).
Stacey Chazin, MS/ODL, Voorhees,NJ, was interviewed for an article in the Jewish Community Voice titled “Introvert Coach Helping Professionals Embrace Innate Talents” (April 17, 2024). As a certified MyersBriggs Type Indicator practitioner, Ms. Chazin works with introverts through one-on-one programs and workshops, helping them thrive in the workplace by unlocking their voice and leading from a place of self-acceptance. Megan Johnson, DO, Georgetown, TX, qualified for the semifinals of American Ninja Warrior with her husband, Kyle Soderman. Dr. Johnson is a doctor and captain in the U.S. Army in Austin.
Ryan Francis Moncman, DO, RES ’22, Fort Lauderdale, FL, joined Holy Cross Health in Fort Lauderdale as a neurosurgeon.
Anna A. Staskiewicz, MS/ Biomed, Lawrenceville, GA, published research in the Scientific Reports journal titled “Temperature-Dependent Iron Motion in Extremophile Rubredoxins—No Need for Corresponding States?” (May 28, 2024).
2023
Shelby Flowers, DO, Moultrie, GA, was featured in the Moultrie Observer’s “Resident Spotlight” (May 2024).
Dr. Flowers is a resident at the Georgia South Family Medicine Residency Program at Colquitt Regional Medical Center.
Keith Woodward Gramling, Jr., DO, Saint Petersburg, FL, was featured in the Moultrie Observer’s “Resident Spotlight” (September 10, 2024).
Dr. Gramling is a resident at Colquitt Regional Medical Center’s Georgia South Psychiatry Residency Program.


Philadelphia, PA, married her high school sweetheart, Luke Winnicki, who supported her throughout her pre-med and medical school career, in March 2024.
Atlanta, GA, joined Encompass Rehab Hospital as a physical therapist in McDonough. Dr. Wood married Miles Mitchell on May 4, 2024.
as of January 28, 2025
Joseph A. Ackil, DO’67, Southborough, MA, October 18, 2024
Albert R. Amalfitano, DO ’57, Amston, CT, September 5, 2024
Harvey V. Apple, DO ’73, Atlanta, GA, December 16, 2023
Ryan Beneby, PharmD ’21, Jacksonville, FL, June 30, 2024
David Clyde Call, DO’98, Birmingham, AL, October 19, 2024
Vincent A. Ciambotti, DO ’68, Sharon, PA, April 20, 2024
J. Paul Clymer, DO ’68, Lititz, PA, November 30, 2024
Robert B. Cohen, DO ’61, Cherry Hill, NJ, July 16, 2024
Kenneth Doroski, DO ’81, Wayne, PA, November 21, 2024
Kenneth Ellis, DO ’78, Naples, FL, August 21, 2024
Leonard R. Fina, DO ’57, Morgantown, PA, October 5, 2023
Howard L. Hausher, DO ’54, Philadelphia, PA, June 21, 2024
SuAnn Holt, RN ’58, Clearwater, FL, July 20, 2024
Elizabeth B. Hughes Promish, DO ’60, Margate City, NJ, February 10, 2024
Edwin A. Jensen, DO ’70, Cherry Hill, NJ, June 28, 2024
Nicholas J. Juele, DO ’79, Mount Laurel, NJ, October 27, 2024
Florence Hagadish Kashlak, RN ’50, Tamaqua, PA, July 2, 2024
Gary L. Kaufmann, DO ’77, Richboro, PA, July 13, 2023
Richard A. Kiszonas, DO ’58, Miami, FL, February 9, 2024
Edward Klein, DO, RES ’01, North Dartmouth, MA, January 2, 2025
Joseph R. Klos, DO ’77, Saint Augustine, FL, April 10, 2024
Evelyn C. Lerch, RN ’52, Clearwater, FL, August 19, 2024
Philip H. Lewis, DO ’54, Pittsboro, NC, May 22, 2023
Joseph A. Lozito, Jr., DO ’77, Wayne, NJ, November 21, 2024
Richard Duncan Lynch, DO ’66, San Antonio, TX, April 3, 2024
Steven Warren Moll, DO ’95, Sequim, WA, April 25, 2024
John C. Munshower, DO ’91, Wayne, PA, June 10, 2024
Murray Pine, DO ’61, Maplewood, NJ, March 30, 2024
J. Chase Rand, DO ’62, Raymond, ME, January 5, 2025
I. Philip Reese, DO ’75, Leesburg, GA, May 31, 2024
Amy P. Ringer, PharmD ’24, Cartersville, GA, January 15, 2025
Marjorie Love Roth, DO ’59, Allentown, PA, January 22, 2025
C. Richard Sharbaugh, DO ’77, Wilmington, DE, May 24, 2024
Stanford A. Shor, DO ’64, Garnet Valley, PA, December 28, 2024
Douglas K. Shumway, DO ’57, Middleville, MI, February 6, 2019
David M. Spratt, DO ’75, Warminster, PA, January 1, 2025
William C. Stettler, DO ’53, Ann Arbor, MI, January 26, 2021
John S. Stevens, Jr., DO ’73, Allentown, PA, June 2, 2024
Margaret M. Still, DO ’91, Winfield, PA, July 24, 2024
John L. Thomas, DO ’73, Long Beach, CA, July 22, 2024
Albert Joseph Tuono, DO ’92, Deming, NM, March 25, 2024
John W. Welsh, DO ’69, Linwood, NJ, August 22, 2024
Daniel David Wert, Jr., DO ’77, Lititz, PA, July 7, 2024
Terrence L. Wogan, DO ’77, Gulf Shores, AL, March 31, 2024
by Jennifer Schaffer Leone
“Artificial intelligence is integrated into our daily work as medical resident physicians, enhancing efficiency and precision. Tools like Dragon Medical improve documentation, while Epic Hyperspace EMR leverages AI for smarter workflows. In the operating room, AI aids surgical planning by generating 3D models from CT scans for complex trauma or head and neck reconstructive cases and provides real-time feedback during procedures like sinus surgery. Recently, we utilized AI to map a juvenile nasopharyngeal angiofibroma from pre-operative CT imaging, guiding the excision of a tumor intra-operatively with precision. … As its capabilities expand, AI is poised to play an increasing role in otolaryngology (my specialty) and in medicine as a whole.”


“My journey into AI began at the intersection of engineering and medicine, where I witnessed firsthand the transformative potential of machine learning in healthcare. As a machine learning research fellow specializing in intraocular lens and refractive surgery at McGill University in Montreal, Canada, I developed a deep learning platform aimed at enhancing the precision of toric intraocular lens surgeries by predicting total corneal astigmatism. By relying on streamlined variables—age and anterior corneal measurements and a neural network trained with a dataset of over 19,000 eyes—the model has the potential to enhance surgical planning and outcomes. Now as a DO student, what excites me is how AI aligns with osteopathic medicine’s core philosophy: treating the whole person. AI’s ability to analyze multiple interconnected factors simultaneously mirrors our holistic approach to patient care. In the next decade, I envision AI supporting clinicians across specialties: streamlining workflows, improving precision in procedures and enhancing decision-making. It will be a tool that empowers, rather than replaces, the physician’s role. Critically, AI tools like my platform democratize access to advanced medical technologies, operating entirely through a web browser and removing barriers of cost or hardware. As we thoughtfully develop these tools, AI will play a transformative role in optimizing patient outcomes and advancing health care globally.”
“MedMatrix is an AI-powered learning tool that has significantly enhanced my study habits at PCOM Georgia. It generates customized study resources from course lectures, including flashcards, review sheets and practice questions with varying difficulty levels. I especially appreciate the infinite question bank that tailors content to specific courses and Step and COMLEX exams, keeping me organized and focused. This tool fosters collaboration by allowing peers to work through shared questions, promoting verbalizing and teaching concepts to deepen understanding. MedMatrix also helps me think critically, make connections between topics and prepare for real clinical challenges.”