Journal Overview
The Perkin&Will Research Journal documents research relating to the architectural and design practice. Architectural design requires immense amounts of information for inspiration, creation, and construction of buildings. Considerations for sustainability, innovation, and high-performance designs lead the way of our practice where research is an integral part of the process. The themes included in this journal illustrate types of projects and inquiries undertaken at Perkins&Will and capture research questions, methodologies, and results of these inquiries.
The Perkins&Will Research Journal is a peer-reviewed research journal dedicated to documenting and presenting practice-related research associated with buildings and their environments. The unique aspect of this journal is that it conveys practice-oriented research aimed at supporting our teams.
This is the 27th issue of the Perkins&Will Research Journal. We welcome contributions for future issues.
Research is a systematic investigation into existing knowledge to discover or revise facts or add to knowledge about a certain topic. In architectural design, we take an existing condition and improve upon it with our design solutions. During the design process, we constantly gather and evaluate information from different sources and apply it to solve our design problems, thus creating new information and knowledge.
An important part of the research process is documentation and communication. We are sharing the combined efforts and findings of Perkins&Will researchers and project teams within this journal.
Perkins&Will engages in the following areas of research:
nj Practice related research nj Resilience and sustainable design
nj Strategies for operational efficiency
nj Advanced building technology and performance nj Design process benchmarking nj Carbon and energy analysis
nj Organizational behavior
2 2023 ― Volume 15.01 Research Journal
Editorial
This issue of the Perkins&Will Research Journal includes three articles that delve into different research topics—research that aims to provide insights into the impact of daylighting within patient rooms in hospital settings, the development of a space program to address future pediatric care models, and a study to present the benefits of E-health and tele-health in hospitals in the United Kingdom.
“Investigating the Impact of Daylighting in Patient Rooms: Developing a Parametric Building Envelope in Healthcare Design" uses visualization tools and simulation modeling to evaluate the impact of building envelope design on daylighting within a patient room setting using parameters such as window-to-wall ratio and shading mechanisms. A wide range of building envelope options were evaluated for varying patient room orientations focusing on daylighting metrics and annual sunlight exposure received.
“Growing Pains: Modernization of Urban Pediatric Environments toward a Post-COVID Future” provides key insights into how pediatric micro-hospitals could be a possible future model of care to fill gaps in access, delivery, and quality of pediatric care environments with significant potential to address current and future capacity problems in conjunction with pediatric care.
“E-health & Tele-health: Potential Impacts on Space in Hospitals in the United Kingdom” is aimed at assessing the potential benefits of tele-health in addressing the needs of patients with respiratory illnesses who were most vulnerable during the pandemic and required extra precautions to prevent further infection while receiving care and treatment.
Kalpana Kuttaiah, Associate AIA, LEEDAP® BD+C
3
2 3 7 20 42 59 Contents Journal Overview Editorial 01: Investigating the Impact of Daylighting in Patient Rooms: Developing a Parametric Building Envelope in Healthcare Design Tanmay Anil Naik, OAA Intern Architect, LEED AP® BD+C Tarek Rakha, PhD 02: Growing Pains: Modernization of Urban Pediatric Environments Towards a Post-COVID Future Jamie Wiberg 03: E-health & Tele-health: Potential Impacts on Space in Hospitals in the United Kingdom Hala ElKhorazaty, WELL AP Asif Din, PhD, RIBA, BREEAM AP, LEED® Green Associate™, LFA Mark Rowe, RIBA, MRIAI, AECB Peer Reviewers Authors 60
6 2023 ― Volume 15.01 Research Journal
Investigating the Impact of Daylighting in Patient Rooms
Investigating the Impact of Daylighting in Patient Rooms: Developing a Parametric Building Envelope in Healthcare Design
Tanmay Anil Naik, OAA Intern Architect, LEED AP® BD+C, tanmay.naik@perkinswill.com
Tarek Rakha, PhD, rakha@design.gatech.edu
Abstract
In healthcare facilities, with the very nature of healing at its core, designing spaces with enhanced levels of human comfort is of prime importance. Daylighting in healthcare facilities has benefited the physiological and psychological well-being of patients receiving treatment. However, many decades of scientific and technological innovation in the field of electrical lighting have resulted in providing ambient daylighting losing its priority in the overall design process. This research evaluates the impact of building envelope design on daylighting within a patient room setting using parameters such as window-to-wall ratio, and shading mechanisms. By using optimization tools such as Colibri and visualization tools like Design Explorer, a wide range of building envelope options are evaluated for different orientations of patient rooms focusing on daylighting metrics like sDA (Spatial daylight autonomy) and ASE (Annual Sunlight exposure). An integral part of this research is assessing the impact of daylighting in varying sky conditions on the melanopic lux levels measured in EML (Equivalent melanopic lux) regulating the circadian rhythms of the patients by using the circadian lighting software ALFA. The results derived from this simulation-based framework would aid in creating a workflow for early-stage design of patient rooms in healthcare settings by focusing on daylighting.
Keywords: daylighting, building envelopes, circadian rhythms, melanopic lux
1.0 Introduction
Over the past several decades, a focus on daylight performance has impacted key decisions of architects and urban planners in designing and shaping the built environment. Apart from recording the changing times of the 24-hour daily cycle, daylighting also aided in understanding seasonal changes and variations. In terms of framing construction codes and regulations, it played a key role in facilitating micro-level changes such as building floor depths, the overall form of the building, and other fundamental parameters.1 However, technological advancements in electrical lighting, mechanical heating, ventilation and air conditioning (HVAC) in the mid-20th century resulted in development of buildings with deeper floor plates and resulted in
people spending close to 90 percent of their time indoors in a controlled environment which in the long run has severely impacted their overall health and well-being.1 The primary objective of daylighting is to minimize the dependence on electrical lighting during daytime hours, which also has an impact on the overall energy savings to some extent. Apart from providing visual comfort, daylighting plays a pivotal role in regulating the circadian clock of occupants thereby affecting their sleep, and wake cycles. In the context of the built environment, the building envelope plays a key role in regulating daylight access. Envelope parameters such as window-to-wall ratio, and shading mechanisms like louvers and fins define the intensity of incident
01
7
daylighting and illuminance within the interior spaces.2 These parameters differ for different building typologies and the nature of occupants. For example, the ‘daylight access’ requirements in habitable spaces such as residential homes, offices, schools, and healthcare institutions are different compared to warehouses, data centers, film studio floors, and industrial buildings. In healthcare design, daylight access is often considered as a vital factor impacting the overall health of patients and healthcare staff. There is significant research conducted in the past that established a relationship between daylight intensity and the average length of stay (LOS) periods. The higher the intensity of daylighting inside the patient rooms shorter is the length of stay (LOS) period.3 This article aims to establish a relationship between the building envelope and its impact on the circadian entrainment of the occupants within the interior-built environment of a healthcare setting. Through optimization of building envelope parameters like window-to-wall ratio and shading mechanisms, different permutations are analyzed using daylight and circadian lighting metrics to evaluate ambient daylight intensity levels and optimum occupant visual comfort. The outcome of this research would aid designers and planners in creating a simulation-based workflow to design patient rooms in healthcare settings with a focus on daylight access.
2.0 Literature Review
2.1 Daylight and Building Envelope Design
Building envelope design forms an integral part of establishing a connection of the interior built environment with its immediate context. Apart from energy usage, thermal comfort, and quality views it also impacts daylighting in a significant manner. There has been significant research conducted in the field of daylighting and its impact on the interior built environment. Jakubiec and Reinhart developed a plugin called DIVA for Rhino 3D that calculates daylight and thermal performance using Radiance/DAYSIM and EnergyPlus.⁴ To improve building performance, Motamedi and Liedl used daylight and energy as objective functions and skylight as a parameter.⁵ Fang and Cho proposed an optimization framework of the envelope of an office building focusing on building geometry, window and skylight dimensions and louver
length in three different climates (hot, mixed and cold)⁶ Ayman and Ahmed used optimization to evaluate the impact of louvers on daylight intensity on the southern façade of healthcare building.⁷ Based on previous studies as mentioned above, this research will further investigate the impact of daylight on the circadian entrainment of occupants through specific analysis nodes measuring EML.
2.2 Daylight in Healthcare Design:
The primary aim of healthcare facilities is to treat patients and improve human well-being. The therapeutic space's interior design is an important aspect of the environment's overall design quality. Previous research indicates therapeutic environments require a high level of adaptability, security, privacy, and relaxation. Users are dissatisfied due to a lack of attention to physical design and interior design in therapeutic areas.8 Lighting acts as one of the primary environmental factors in providing users with the right healing conditions.9 The hospital's patient rooms are crucial for patient observation and treatment. Daylighting and quality views can help patients recover more rapidly, reduce discomfort, and cut down on their length of stay (LOS). Keeping this in mind the external facade should be constructed to enhance daylighting and provide the best daylighting performance to aid in patient health care and comfort.10 Previous research indicates that daylight substantially impacts human health, both physically and psychologically.11 It also indicated the positive impact of daylight on the overall work performance of the healthcare staff.11 Recent research suggests that daylighting has an impact on the human circadian clock and the cognitive performance of patients recovering in a hospital.12 Research also indicates that our circadian rhythm is greatly influenced by lighting conditions. Extensive research on human circadian and sleep have derived two effects of light as follows: (1) melatonin suppression is a short-term reaction to light exposure and (2) the ability of light to change one's circadian phase.13
2.3 Lighting and Human Health:
Keeping in mind the delicate nature of 'treating a human body' within a healthcare context, it should be designed
8 2023 ― Volume 15.01 Research Journal
Investigating the Impact of Daylighting in Patient Rooms
with the highest level of physical, social, and symbolic comfort and care. Therefore, maintaining a bright environment within the healthcare setting becomes an integral part of the healing environment. During the day, light intensities can reach 100,000 lux in direct sunlight and 25,000 lux in full daylight. Closed rooms within the built environment have much lower intensities and conventional electrical lighting is only 500 lux or less.14 Over the years, light therapy has become more widely used as an additional treatment for a variety of medical disorders. For example, light not only improves mood in individuals with anorexia or bulimia nervosa but also aids in the treatment of disease-related symptoms.15 Light not only has antidepressant characteristics in agerelated depression, but it can also aid dementia patients to slow down their cognitive degeneration, according to other studies.16 Bright light therapy is relatively safe, and there is some evidence to support its use in the treatment of nonseasonal MDD (major depressive disorder); nonetheless, there is a paucity of data in this field.17
2.4 Circadian Lighting Metrics:
In a human body many physiological and behavioral rhythms in humans, such as the hormone levels, body temperature, and sleep-wake cycle, waver within a 24hour period.18 In humans, melanopsin-containing retinal ganglion cells—rather than rods or cones—are thought to primarily mediate circadian responses to light. Despite being primarily sensitive to blue light, melanopsin cells also get input from vision photoreceptors.19,20 These photosensitive retinal ganglion cells (ipRGC) are linked to the ‘circadian cycle’ which is also known as the common rest wake cycle.18 In practice, exposure to blue light may alter the hormone cycles of cortisol and melatonin, which control mental activity and sleep during the day.21 The melanopic lighting approach uses the composition spectral value of the light weighted irradiance to the cornea in relation to the unique spectral contents of the five different types of receptors to determine the suppression of melatonin.18 Through the calculation of irradiance, previous researchers were able to record the light exposures of each of the photoreceptors in the greater whole form as a power distribution spectral corneal.22 J.A Enezi in a previous research introduced the equivalent ∝ -optical illuminance concept E ∝ , where ∝ indicates the retinal photopigment for a given organism to calculate the values of the five types of illuminance.23
This was further developed by Lucas who created the EML (Equivalent Melanopic Lux) metric which is measured vertically at the height of the observers eye to calculate the equal lux melanopic.24 The WELL building standard 2023—L03 Circadian lighting design standard suggests minimum threshold EML levels for projects with enhanced daylight in the range of 120EML to 180EML.25
3.0 Research Methodology
3.1 Research Goal
The goal of this research is to understand the impact of daylighting design on regulating the circadian rhythms of occupants within a patient room setting using a simulation-based workflow that analyzes building envelope parameters like window-to-wall ratio and shading systems.
3.2 Research Objectives
The objectives of this research aim to cover a wide spectrum of topics related to access to daylighting with reference to building envelope parameters, external sky conditions and occupant visual comfort.
nj To evaluate opportunities to harness the daylight intensity potential within a patient room setting by incorporating strategies in the building envelope design.
nj To assess the potential of optimization of building envelope parameters such as window-to-wall ratio, and shading mechanisms in regulating daylight intensity within the interiors of a patient room and comparing it with baseline threshold metrics for sDA and EML.
nj To understand the impact of varying ‘sky conditions’ like clear and overcast sky on daylight intensity and the subsequent effect on melanopic lux levels.
3.3 Research Questions
This research attempts to address the following questions:
1. How can building envelope parameters facilitating daylighting in the interior built environment help in regulating the circadian rhythms of its occupants?
9
2. How can an occupant-centric approach be incorporated in daylighting simulation workflows to benefit the overall visual comfort within a healthcare setting?
3.4 Research Experiment
This research used a simulation-based workflow to evaluate the impact of daylight intensity in patient rooms of the acute stabilization unit level of the HMHI
crisis care centre facility in Salt Lake City, Utah. This level consists of 24 numbers of patient rooms around the perimeter of the floor plate and 4 numbers. of patient rooms were selected in each of the cardinal directions to address the impact of daylighting. A 3D base model for each of the existing patient rooms was developed using the proposed floor layouts of the facility. The simulation experiment is conducted in two stages analyzing building envelope performance and the subsequent impact on melanopic lux levels.
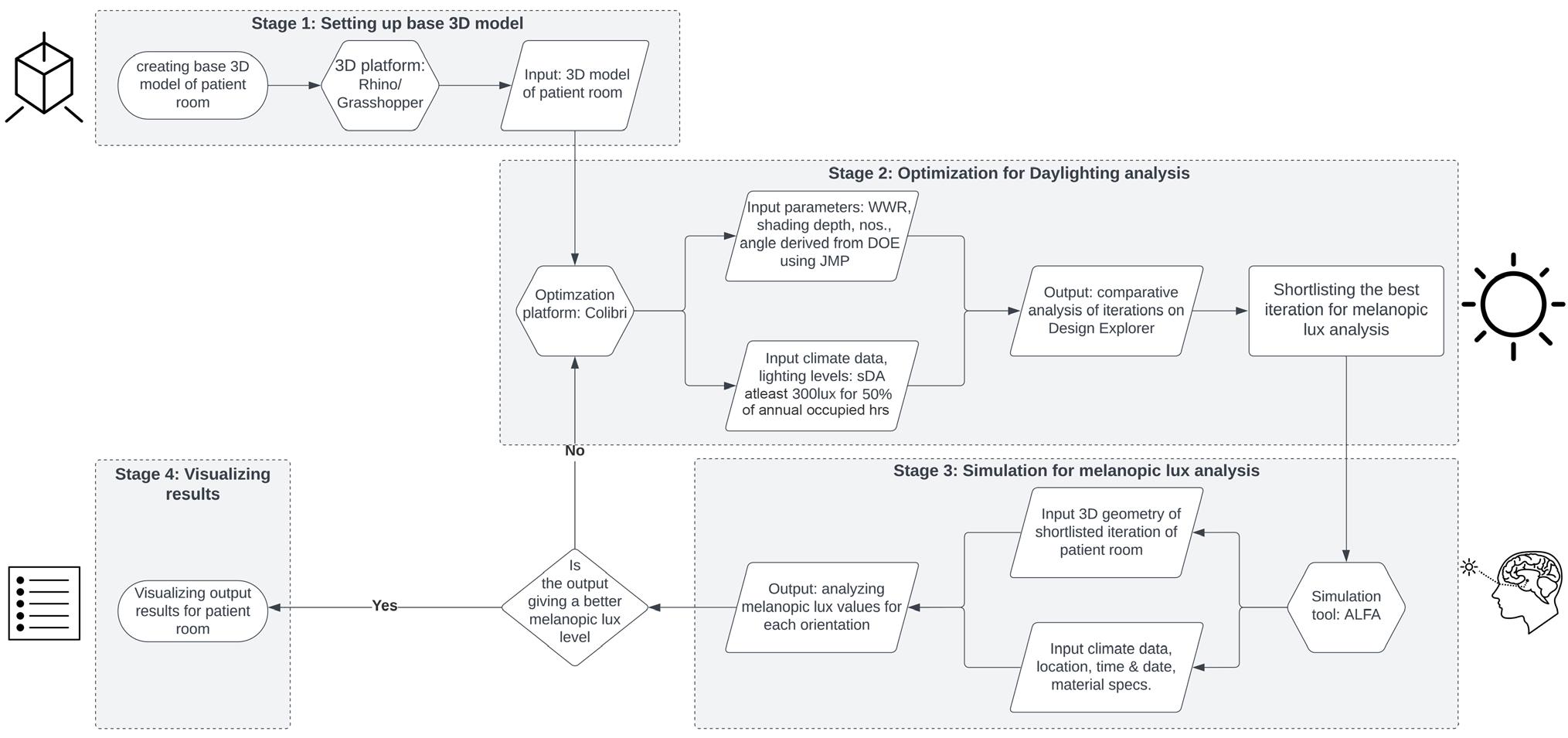
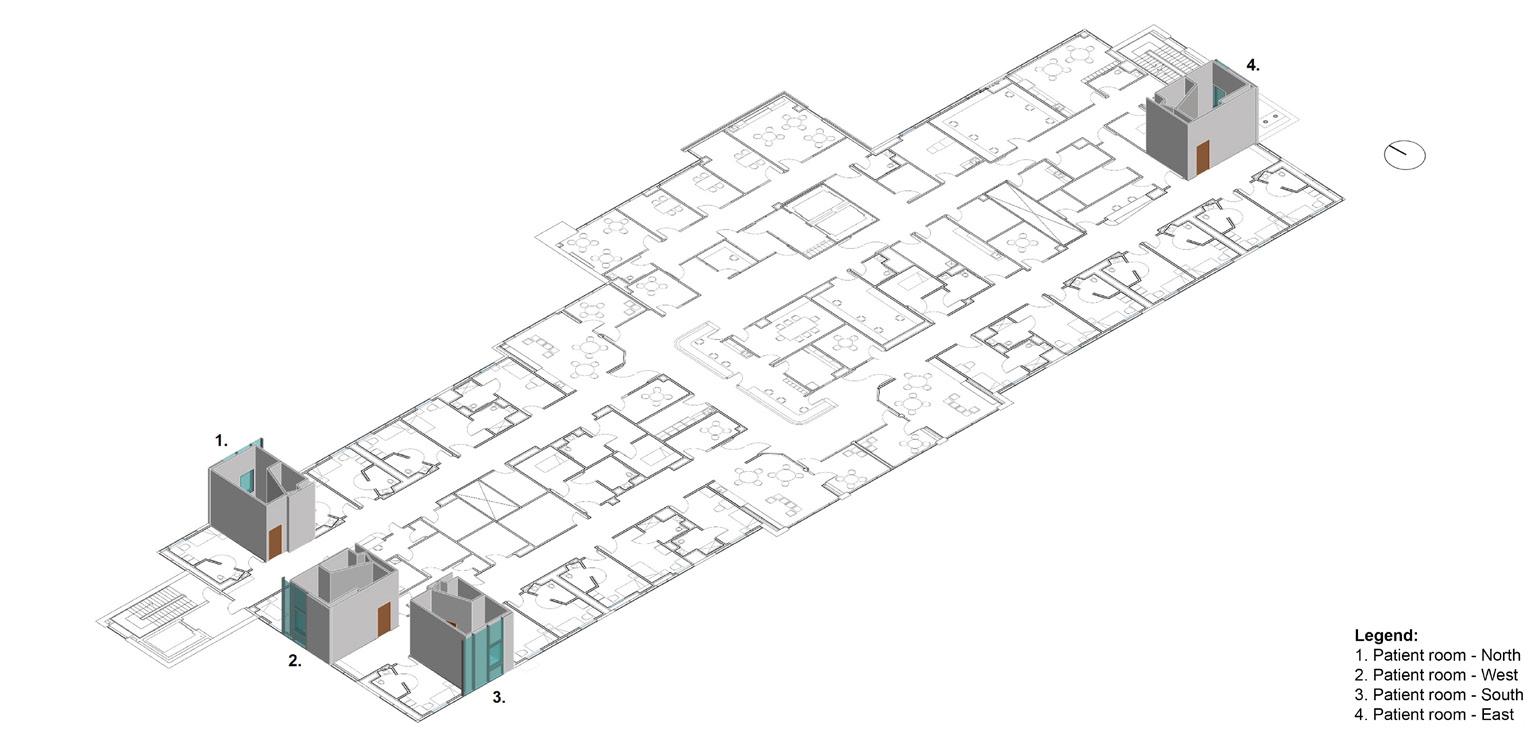 Figure 1: Simulation experiment framework.
Figure 1: Simulation experiment framework.
10 2023 ― Volume 15.01 Research Journal
Figure 2: 3D Isometric view of the Acute Stabilization Level in HMHI, Salt Lake City, Utah, USA.
Figure 1 gives an overview of the framework for the simulation experiment explaining the different stages. In stage 1 the shortlisted patient rooms in each orientation are modelled using Rhino 3D. Figure 2 indicates the base 3D isometric model of the shortlisted patient rooms in the cardinal directions. A parametric shoe-box model is developed using Grasshopper with the existing envelope conditions to conduct the daylighting analysis and evaluate sDA (spatial daylight autonomy) and ASE (Annual Sunlight Exposure) values. The VT or visible transmittance level of glass was considered as 0.4 based on the inputs received from FFKR architects and their vendors for this simulation.
Table 1 indicates the sDA and ASE values of existing patient rooms. Apart from the daylighting analysis, the melanopic lux levels at specific nodes within the patient room are recorded in clear and overcast sky conditions at 9:00 am. The simulation is carried out using ALFA— circadian lighting software. Specific analysis nodes are placed inside the patient room to capture melanopic lux
levels at the bed and chair. Table 2 gives an overview of the melanopic lux levels of the existing patient rooms. In Stage 2 a DOE or Design of experiment is developed using JMP—statistical analysis software. The DOE table mainly consists of iterations derived from a combination of input parameters like window-to-wall ratio, no. of louvers/fins, depth of lovers/fins, and angle of louvers/ fins. For the North and South orientations, a windowto-wall ratio range of 0.4 to 0.7 is considered whereas for East and West orientations a range of 0.2 to 0.5 is considered to reduce glare from daylighting. The VT value of glazing is considered as 0.65 for the simulation runs to facilitate higher daylighting levels inside the patient rooms. A total of 50 iterations are considered for each patient room orientation. The results are then analyzed in Design Explorer to select the optimum building envelope iteration for each orientation. A sensitivity analysis is carried out to understand the impact of different input building envelope parameters on the sDA and ASE values.
ORIENTATION s DA VALUE (%) ASE VALUE (%) North 26.39 0 South 63.23 46.55 East 42.41 20.22 West 36.74 27.71
Table 1: Existing Patient room’s sDA and ASE values.
ORIENTATION EML (BED) CLEAR SKY EML (BED) OVERCAST SKY EML (CHAIR) CLEAR SKY EML (CHAIR) OVERCAST SKY North 96 32 295 141 South 157 42 108 37 East 488 49 1514 169 West 125 50 183 79 11
Table 2: Existing Patient room’s melanopic lux levels.
Investigating the Impact of Daylighting in Patient Rooms

 Figure 3: Daylighting optimization results – Patient room North, louvers iteration.
Figure 3: Daylighting optimization results – Patient room North, louvers iteration.
12 2023 ― Volume 15.01 Research Journal
Figure 4: Comparative analysis of daylighting optimization results using Design Explorer.
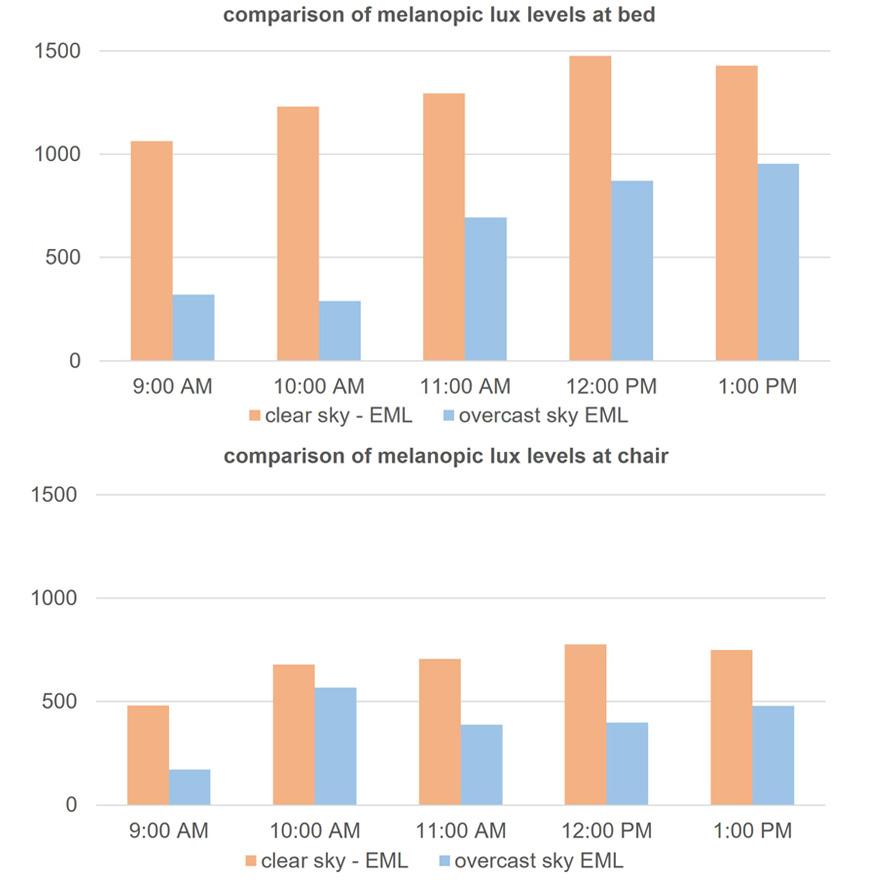
Figure 3 indicates a sample output derived from the daylighting optimization runs evaluating the sDA and ASE values for different iterations. Figure 4 gives an overview of the comparative analysis of the simulation runs of different iterations. Glare analysis of the shortlisted iterations derived from the optimization runs analyze the overall occupant comfort within the patient rooms. In Stage 3 the shortlisted iterations are further analyzed to understand the impact of daylighting on the melanopic lux levels. The shortlisted patient room iterations are modeled using Rhino and the simulation is carried out using ALFA. The necessary input parameters like climate data, date/time, and material finishes are added before running the simulations. To understand the performance of the building envelope, seasonal variations like the clear sky and overcast sky conditions are considered. Based on the climate data of Salt Lake City, Utah two days each from the summer and winter seasons are selected for the clear and overcast sky conditions, respectively. In terms of evaluating the melanopic lux levels at different times of the day, five separate time slots—9:00 am, 10:00 am, 11:00 am 12:00 pm, and 1:00 pm. are considered to understand the variations in the values. Like the existing patient rooms, the analysis nodes are set over the bed and chair to simulate the position of the occupant within the shortlisted iterations in each orientation.
4.0 Results
This section focuses on the results derived from the simulation experiment runs for the daylighting optimization and circadian rhythm analysis, respectively. For baseline threshold levels, the LEED v4.1—EQ— Daylight credit indicating an sDA for at least 55 percent of regularly occupied floor area within the perimeter area for healthcare projects and the WELLv2, Q3 2022 standard for living environments: 120-180 EML or equivalent melanopic lux for projects with enhanced daylight for living environments are considered as references. 25 The above-mentioned baseline levels are considered keeping in mind the application of this research and workflow in the schematic design phase of real time projects to evaluate optimum building envelope solutions.
4.1 Patient Room Orientation—North
Based on the results derived from the daylighting optimization simulations, it can be concluded that the fins iteration provides a better balance between the sDA and ASE values. The optimum fins iteration recorded sDA- 94.48 percent and ASE-2.61 percent. Glare analysis recorded imperceptible glare with DGP values of 0.32 and 0.23 for clear and overcast sky conditions.

13 Investigating the Impact of Daylighting in Patient Rooms
Figure 5: Patient room North, shortlisted iteration—Daylighting and Glare analysis.
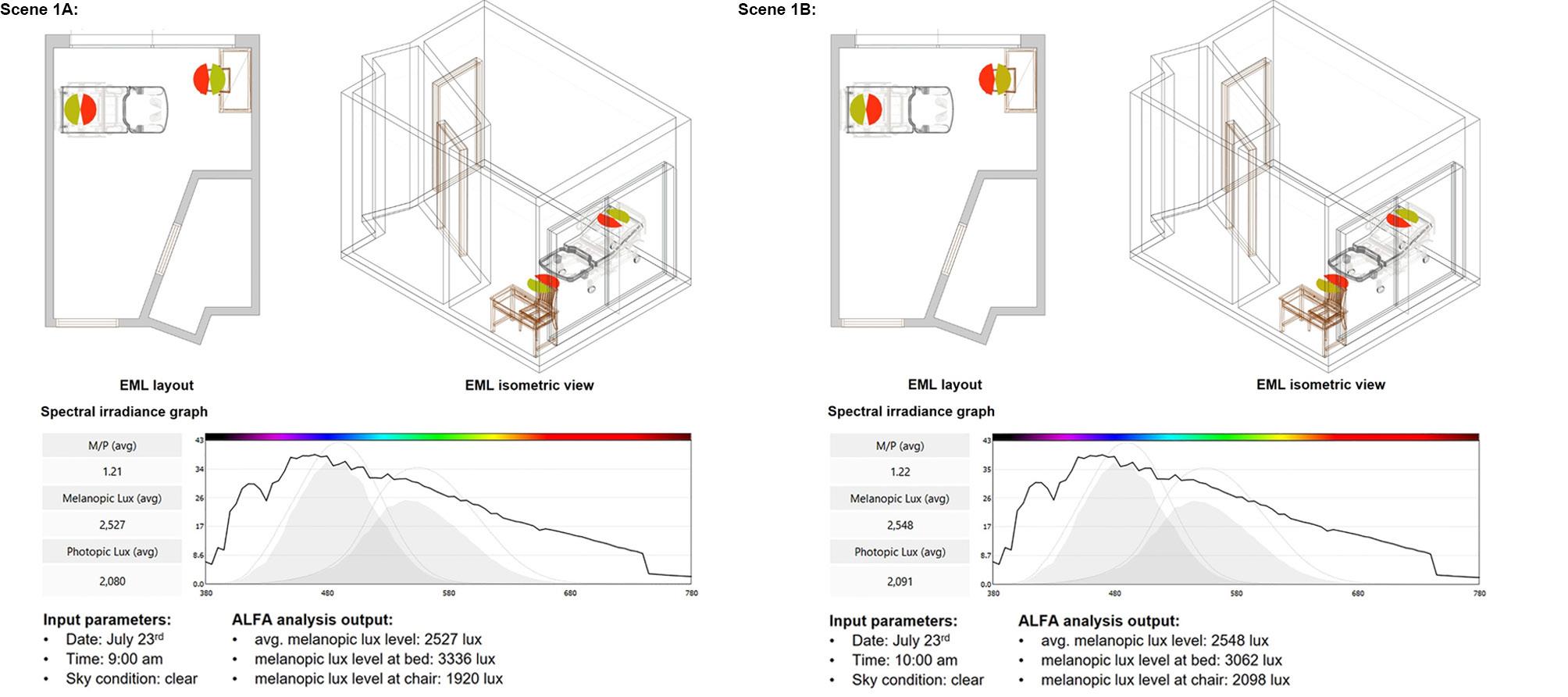
the shortlisted iteration under clear and overcast sky conditions between 9:00am and 1:00pm.
The melanopic lux levels recorded at the bed range between 1117–3374 lux for overcast to clear sky conditions, whereas for the chair the levels range between 764–2234 lux for overcast to clear sky conditions respectively. Figure 7 indicates the comparative analysis of melanopic lux levels recorded at bed and chair and highlights the variations across the levels with each passing hour for clear and overcast sky conditions.
 Figure 5 indicates an overview of the daylighting and glare analysis. The circadian rhythm analysis was conducted on
Figure 6 indicates a sample output of the melanopic lux levels.
Figure 6: Patient room North – melanopic lux analysis | July 23rd | clear sky condition | 9:00am and 10:00ams.
Figure 5 indicates an overview of the daylighting and glare analysis. The circadian rhythm analysis was conducted on
Figure 6 indicates a sample output of the melanopic lux levels.
Figure 6: Patient room North – melanopic lux analysis | July 23rd | clear sky condition | 9:00am and 10:00ams.
14 2023 ― Volume 15.01 Research Journal
Figure 7: Patient room North - melanopic lux levels.
4.2 Patient room orientation – South
The daylighting optimization results indicate the louvers iteration provides a better balance between sDA and ASE values. The optimum louvers iteration recorded sDA —89.49 percent and ASE—12.14 percent. Glare analysis recorded imperceptible glare with a DGP value of 0.28 for clear and overcast sky conditions. The circadian rhythm analysis recorded melanopic levels for the bed ranging between 283-1743 lux for overcast to clear sky conditions, whereas for the chair the levels range between 183-1012 lux for overcast to clear sky conditions, respectively. Figure 8 indicates the comparative analysis of melanopic lux levels recorded at bed and chair in the South orientation and highlights the variations across the levels with each passing hour for clear and overcast sky conditions.
4.3 Patient room orientation – East
From the daylighting optimization results it can be concluded that the louvers iteration provides a better balance between the sDA and ASE values. The optimum louver iteration recorded sDA—87.94 percent and ASE— 48.62 percent. Glare analysis recorded imperceptible glare with DGP values of 0.30 and 0.22 for clear and overcast sky conditions. The circadian rhythm analysis recorded melanopic levels for the bed ranging between 356-1939 lux for overcast to clear sky conditions, whereas for the chair the levels range between 203-1190 lux for overcast to clear sky conditions, respectively. Figure 9 indicates the comparative analysis of melanopic lux levels recorded at bed and chair in the East orientation and highlights the variations across the levels with each passing hour for clear and overcast sky conditions.
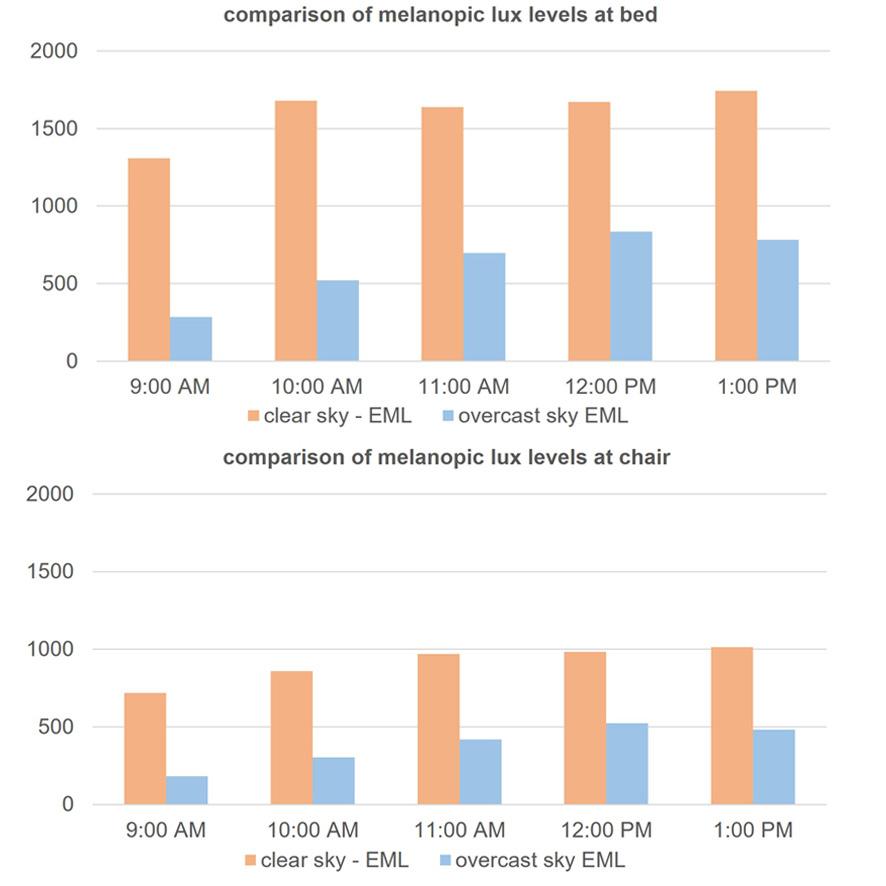
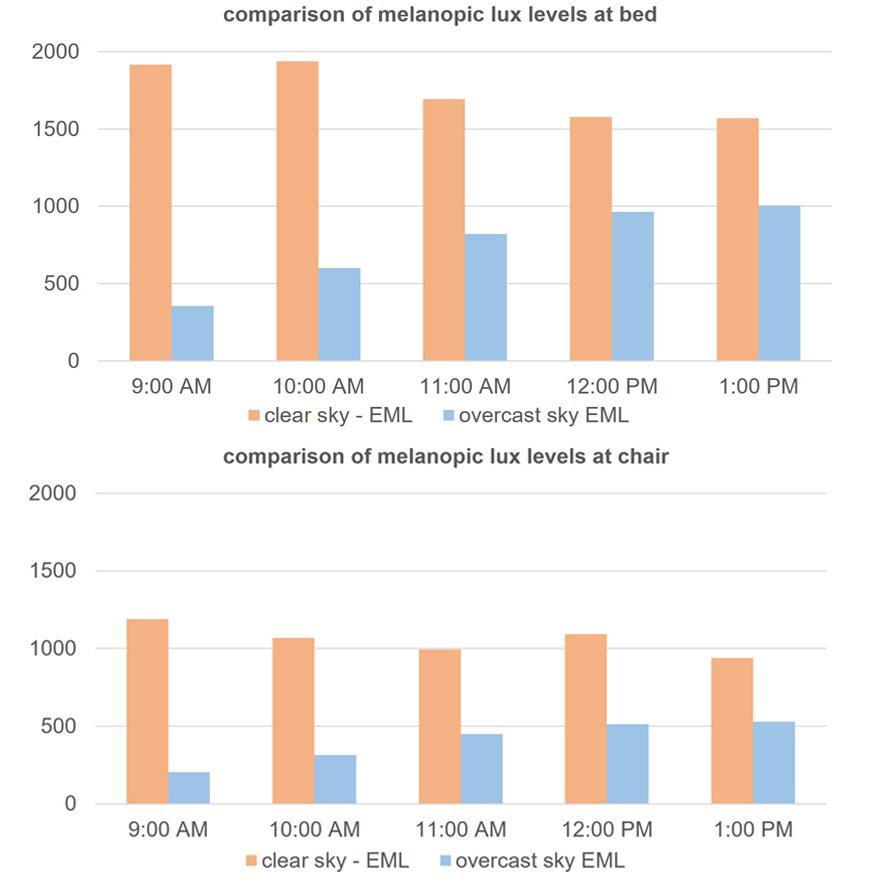 Figure 8: Patient room South - melanopic lux levels.
Figure 8: Patient room South - melanopic lux levels.
15 Investigating the Impact of Daylighting in Patient Rooms
Figure 9: Patient room East - melanopic lux levels.
4.4 Patient room orientation – West
From the daylighting optimization results it can be concluded that the louvers iteration provides a better balance between the sDA and ASE values. The optimum louver iteration recorded sDA—82.58 percent and ASE— 49.12 percent. Glare analysis recorded imperceptible glare with DGP values of 0.30 and 0.22 for clear and overcast sky conditions. The circadian rhythm analysis recorded melanopic levels for the bed ranging between 289-1476 lux for overcast to clear sky conditions, whereas for the chair the levels range between 171-776 lux for overcast to clear sky conditions, respectively. Figure 10 indicates the comparative analysis of melanopic lux levels recorded at bed and chair in the West orientation and highlights the variations across the levels with each passing hour for clear and overcast sky conditions.
5.0 Discussion
The optimization results provide an insight into the varying levels of permutations possible for the building envelope in regulating daylighting inside patient rooms. There is a significant impact of the envelope parameters like window-to-wall ratio and shading mechanisms on the sDA and ASE values. In terms of selecting the shading mechanisms, the DGP or Daylight Glare Probability value became a critical factor especially for the South, East, and West orientations. Apart from the primary envelope parameters, the visible transmittance (VT) value of the glass also played an important role in regulating the sDA and melanopic lux values. The VT level for the existing patient rooms is 40 percent which resulted in sDA levels below 50 percent for all orientations except South which recorded an sDA value of 63 percent owing to the longer façade of the building in a North-South orientation. An increase in the VT value of the glazing from 40 percent to 65 percent while conducting the optimization permutations resulted in a significant increase in the sDA values while balancing the ASE values by the virtue of shading mechanisms. The North and South orientations recorded sDA values of 94.35 percent and 89.49 percent, respectively. Although the East and West orientations recorded sDA values higher than 80 percent they also recorded higher ASE values than the North and South orientations. The circadian rhythm analysis of the patient rooms focused on a more occupant-centric approach by placing the analysis sensor nodes on the bed and chair. This resulted in the recording of melanopic lux levels anticipating patient behavior inside the room during daytime hours of 9:00 am to 1:00 pm on both clear and overcast sky conditions. A comparative analysis of the melanopic lux levels during the clear and overcast sky conditions resulted in evaluating the performance of the building envelope during varying climatic conditions. Whereas a comparative analysis of the values for the existing and optimized conditions indicates the percentage of increase in the sDA and melanopic lux levels for the different orientations.
16 2023 ― Volume 15.01 Research Journal
Figure 10: Patient room West - melanopic lux levels.
Investigating the Impact of Daylighting in Patient Rooms
Due to a paucity of data specific to healthcare environments, the baseline threshold levels set by LEED for sDA—55 percent and WELLv2, Q3 2022 standard for living environments: 120-180 EML or equivalent melanopic lux for projects with enhanced daylight are considered for the comparative analysis.25 From the above tables, it is evident that optimization of the building envelope in different orientations resulted in a significant gain in both sDA and melanopic lux values. The North orientation displayed the highest percentage of increase in values followed by the West orientation.
6.0 Limitations and Future Research
This research was conducted in a semi-arid temperate climate. There is a wide scope to explore other climate zones and subsequent daylighting scenarios. Owing to the building oriented along the north-south axis, intercardinal directions were not explored in this research. The proposed facility is in a semi-urban context with very few buildings located in distant blocks. Future research can explore the impact of dense urban contexts and rural contexts with vegetation on daylighting penetration. The opacity nature of the materials used in shading mechanisms can also be explored as a part of future research. Apart from ALFA, Lark spectral lighting tool can be used with its nine-channel method for daylit scenes and prediction of indoor daylight. Previous research highlighted that horizontal task-based illuminance metrics often overestimate the risk for glare as they do not consider the position of an occupant within the room. Whereas view-based metrics provide a more holistic overview considering the seating position, view orientation, distance from the window and daylight composition which has an impact on occupant
ORIENTATION s DA EXISTING s DA OPTIMIZED % INCREASE North 26.39 94.48 258.01 South 63.23 89.49 41.53 East 42.41 87.94 107.36 West 36.74 82.58 124.77
Table 3: Percentage increase in sDA values.
ORIENTATION EML (EXISTING) EML (OPTIMIZED) % INCREASE North 141 764 441.84 South 37 183 394.59 East 169 203 20.12 West 79 171 116.46
Table 7: Percentage increase in melanopic lux values at chair in overcast sky conditions at 9:00am.
ORIENTATION EML (EXISTING) EML (OPTIMIZED) % INCREASE North 96 3336 3375.00 South 157 1309 733.76 East 488 1915 292.42 West 125 1063 750.40
Table 4: Percentage increase in melanopic lux values at bed in clear sky conditions at 9:00am.
ORIENTATION EML (EXISTING) EML (OPTIMIZED) % INCREASE North 32 1117 3390.63 South 108 283 162.04 East 49 356 626.53 West 50 320 540.00
Table 5: Percentage increase in melanopic lux values at bed in overcast sky conditions at 9:00am.
ORIENTATION EML (EXISTING) EML (OPTIMIZED) % INCREASE North 295 1920 550.85 South 425 718 68.94 East 1512 1190 -21.30 West 183 482 163.39
Table 6: Percentage increase in melanopic lux values at chair in clear sky conditions at 9:00am.
17
health and comfort.26 Although this research adopted an occupant-centric approach to collect melanopic lux data, it is difficult to anticipate occupant comfort behavior inside a patient room owing to the nature of illness, immunity, and response to treatment levels. To better understand the impact of increased EML levels on patient health, the average length of stay (ALOS) period can be analyzed as a part of the post-occupancy evaluation study. Apart from patients, the scope of this research can also be expanded to the overall health and well-being of healthcare staff owing to the nature of their workloads within a healthcare setting. Future research can also be conducted in varying typologies such as workplace, education, recreational buildings to evaluate the impact of daylighting access on the overall visual comfort experience of the occupants.
7.0 Conclusion
The outcome of this research is to provide designers, planners, and healthcare staff with a simulation-based framework for designing healthcare environments with a focus on daylighting simulation. This research provided some valuable insights into the building envelope and its impact on the non-visual effects and circadian entrainment of occupants inside a patient room setting through daylighting access and intensity levels. Through an optimization model approach evaluating multiple scenarios focusing on window-to-wall ratios and shading mechanisms, this research indicated a potential scope to further investigate material specifications and economics in implementing such building envelope interventions in real time projects. Using specific analysis nodes within an interior built environment setting, the research also emphasizes the importance of furniture planning to provide optimum occupant visual comfort.
Acknowledgments
The authors gratefully acknowledge the support of the SimTigrate design lab at Georgia Institute of Technology and the valuable feedback from Ms. Jennifer Dubose, and Dr. Siobhan Rockcastle to author Tanmay Naik in enriching this research from various perspectives.
References
[1] Konis, K. (2019). A circadian design assist tool to evaluate daylight access in buildings for human biological lighting needs. Solar Energy, 449-458.
[2] Wong, I. L. (2017). A review of daylighting design and implementation in buildings. Renewable and Sustainable Energy Reviews, 959-968.
[3] Man Young Park, C.-G. C.-K. (2018). The Effects of Natural Daylight on Length of Hospital stay. Environmental Health Insights, 1-7.
[4] J.A. Jakubiec, C.F. Reinhart (2011). Diva 2.0: integrating daylight and thermal simulations using Rhinoceros 3D, Daysim and EnergyPlus. Proceedings of Building Simulation 2011, 2202-2209.
[5] S. Motamedi, P. Liedl (2017) Integrative algorithm to optimize skylights considering fully impacts of daylight on energy. Energy Build, 655-665.
[6] Y. Fang, S.Cho (2019) Design optimization of building geometry and fenestration for daylighting and energy performance, Sol. Energy, 191, 7-18.
[7] Ayman Wagdy, Ahmed Sherif, Hanan Sabry, Rasha Arafa, Islam Mashaly (2017) Daylighting simulation for the configuration of external sun-breakers on south oriented windows of hospital patient rooms under a clear desert sky, Solar Energy, Volume 149, 164-175.
[8] Husein Ali Husein, S. S. (2020). Impacts of Daylight on improving healing. Internal Transaction Journal of Engineering.
[9] Kellert, S. &. (2015). The practice of biophilic design. Retrieved from https://www.biophilic-design.com/
[10] Ahmed S, H. S. (2015). Daylighting in Hospital Patient Rooms: Parametric Workflow and Genetic Algorithms for an Optimum facade design. 14th Conference of International Building Performance Simulation Association. Hyderabad: IBPSA.
[11] Aripin, S. (2007). Healing Architecture: Daylight in hospital design. Conference on Sustainable Building Southeast Asia.
[12] Maria Englezou, A. M. (2020). Assessment of daylight performance and the impact of shading devices for typical in-patient rooms in healthcare facilities. Optimization-Driven Architectural Design (OPTARCH 2019), (pp. 277-285).
18 2023 ― Volume 15.01 Research Journal
Investigating the Impact of Daylighting in Patient Rooms
[13] Christine Blume, C. G. (2019). Effects of light on human circadian rhythms, sleep, and mood. Somnologie, 147-156.
[14] Manuel Spitschan, G. K. (2016, June 7). Variation of outdoor illumination as a function of solar elevation and light pollution. Retrieved from Scientific reports: https:// www.nature.com/articles/srep26756.
[15] BeauchampMT, L. J. (2016). A systematic review of bright light therapy for eating disorders. Retrieved from www.psychiatrist.com: https://www.psychiatrist.com/ pcc/eating/bright-light-therapy-for-eating-disorders/
[16] Ritsaert Lieverse, E. J. (2011). Bright light treatment in elderly patients with nonseaonal major depressive disorder: a randomized placebo-controlled trial. Arch Gen Psychiatry
[17] Mark A. Oldham, D. A. (2014). Use of Bright Light Therapy Among Psychiatrists in Massachusetts: An E-Mail Survey. Prim Care Companion CNS Disord.
[18] Busatto Nicola, Mora Dalla Tiziano, Peron Fabio, Romagnoni Piercarlo. (2020). Application of Different Circadian Lighting metrics in a health residence. Journal of Daylighting. DOI:10.15627/jd.2020.2
[19] R.L. Brown and P.R. Robinson (2004) MelanopsinShedding Light on the Elusive Circadian Photopigment, Chronobiol Int 189-204.
[20] J.L Ecker, O.N Dumitrescu, K.Y Wong, N.M Alam, S.K Chen, T LeGates, J.M. Renna, G.T Prusky, D.M. Berson and S. Hattar (2010) Melanopsin-expressing retinal ganglion-cell photoreceptors: cellular diversity and role in pattern vision, Neuron 76, 49-60.
[21] C.Lok (2011) Seeing without seeing, Nature 469, 285-285.
[22] L Bellia, F. Fragliasso, E. Stefanizzi, Sensori crcadiani per la caraterizza zione dell’ illuminazione, (2016)ENEA.
[23] J.A. Enezi, V. Revell, T. Brown, J Wynne, L Schlangen and R. Lucas, (2011) Journal of biological rhythms 26, 314-323.
[24] R.J. Lucas, S.N Pierson, D.M Berson, T.M Brown, H.M Cooper, C. A. Czeisler, M.G Figueiro, P.D Gamlin, S.W Lockley, J.B. O’Hagan, L.L Price, I. Provencio, D. J Skene and G.C Brainard (2014) Measuring and using light in the melanopsin age, Trends in Neurosciences 37, 1-9.
[25] WELL v2, Q1-Q2 2023, L03 Circadian lighting design, https://v2.wellcertified.com/en/wellv2/light/feature/3
[26] Rockcastle, Siobhan Francois; Ámundadóttir, María Lovísa; Andersen, Marilyne (2019). The Case of Occupant-Centric Daylight Analytics: a comparison of Horizontal Illumination and Immersive view. Proceedings Of Building Simulation 2019: 16Th Conference Of IBPSA. 1239-1246.
19
02
Growing Pains:
Modernization of Urban Pediatric Environments Towards a Post-COVID Future
Jamie Wiberg, jamie.wiberg@perkinswill.com
Abstract
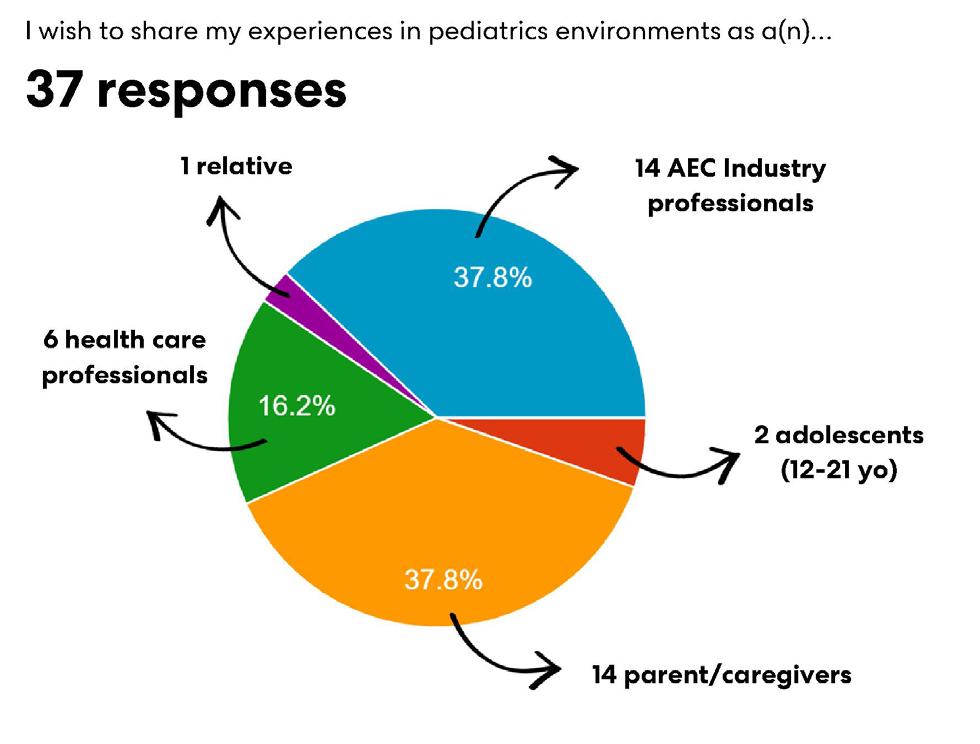
Pediatric care and the built environments that support it have been experiencing rapid disinvestment in the United States—regional and local pediatric units are being shut down throughout the country.1,2,3,4,5 There is an urgent need to rethink modern pediatric care models that include low-budget and equitable solutions to meet the growing needs of the population. This research provides key insights for micro-hospital development to fill gaps in access, delivery, and quality of pediatric care. Evidence and experience-based design methods were used to analyze the feasibility of pediatric micro-hospitals. A narrative literature review of 40 articles and three case studies were conducted to better understand the complexities of pediatric design and the micro-hospital model. Interviews with architecture, engineering, and construction (AECand healthcare professionals were conducted to better understand the current trends and best practices in pediatric care (N=10. A survey was conducted to capture perspectives of children (n=2, their parents and caregivers (n=15, health care providers (n=6, and AEC professionals (n=14about the current state and future potential for modernization of pediatric environments (N=37).
This research resulted in the development of a proposed model for a pediatric micro-hospital, conditions to operate in urban and suburban environments, and implementation tools for future development. Micro-hospitals for pediatric populations offer a patient-centered, economic, and sustainable solution to address the pediatric care crisis. Pediatric micro-hospitals as a future model of care have significant potential to address current and future capacity problems in pediatric care. An interdisciplinary design approach is necessary for successful implementation of future pediatric micro-hospital care models.
Keywords: micro-hospitals, inpatient, family-centered care, experience-based design
1.0 Introduction: The Pediatric Care Crisis
Prior to 2019, standalone pediatric hospitals and hospitals with pediatric intensive care units (PICUs) were growing. The American Academy of Pediatrics (AAP) and the Society of Critical Care Medicine (SCCM) updated their policy in 2019 on levels of critical care, reflecting the dramatic advancements in pediatric care and development of specialized PICUs. The COVID-19 pandemic regressed growth and accelerated disinvestment in pediatric care, notably several PICUs
were converted into adult ICUs. Children today are suffering physical and psychosocial challenges that previous generations have never encountered.
In November 2022, The American Academy of Pediatrics (AAP) and Children’s Hospital Association (CHA), representing the voices of 67,000 pediatric care professionals and 220 children’s hospitals, sent a letter to President Joseph Biden asking to declare an emergency
20 Research Journal 2023 ― Volume 15.01
to support a national response to a surge in pediatric respiratory illnesses and the ongoing children’s mental health crisis.4 The letter stressed significant capacity issues, longstanding underinvestment in Medicaid compared to Medicare and private insurance, and the disproportionate impact on historically under-resourced communities.
Pediatric subspecialty and surgical care have become increasingly regionalized to freestanding children’s hospitals and large academic centers. 5 While this regionalization has improved the outcomes for complex conditions, it has altered the landscape of availability and accessibility to pediatric health care across the nation (Figure 1).6
A 10-year study from 2008-2018 of 4,720 US hospitals concluded that pediatric inpatient units have decreased by 19.1 percent, pediatric inpatient unit beds decreased by 11.8 percent, and nearly one-quarter of US children experienced an increase in distance to their nearest pediatric inpatient unit.⁵ By contrast, pediatric inpatient unit beds and pediatric intensive care unit beds increased within children’s hospitals, thereby consolidating beds into a smaller number of locations. This shift represents a trend towards regionalization of pediatric care. The increasing concentration of PICU and inpatient beds
within children’s hospitals may be explained by factors such as the increased complexity of pediatric inpatient patients, and the growing demand for subspecialty services and PICU bed availability at these facilities.5 The United States is currently underprepared to handle volume surges in pediatric patients. Further closures of inpatient units will exacerbate healthcare system’s ability to adapt during times of crisis.
It is well understood that children are physically and developmentally different from adults. Similarly, pediatric populations have quite different spatial needs in healthcare settings compared to adult populations.⁷ However, medical solutions for adults are commonly retrofitted for children. This application is seeping into our built environments, where spatial solutions are considered without children at the forefront.
The country has been continuously disinvesting in pediatric care, and the pediatric health system has reached a breaking point manifested in physical voids throughout our communities. Our current built environments are not working towards protecting, healing, and growing our children. These ongoing problems in pediatric health care are evidence of an overwhelmed and outdated system. When there is another virus, pandemic, or unexpected condition, it will

 Figure 1: Map of continental US locating standalone pediatric hospitals. Map by author generated using GIS Data. Data sources listed on image.
Figure 1: Map of continental US locating standalone pediatric hospitals. Map by author generated using GIS Data. Data sources listed on image.
21 Growing Pains
Generated with GIS Data using ArcGIS Maps for Adobe Creative Cloud. Oak Ridge National Laboratory (ORNL); National Geospatial-Intelligence Agency (NGA) Homeland Security Infrastructure Program (HSIP) Team. | Missouri DNR, Esri, HERE, Garmin, FAO, NOAA, USGS, EPA, NPS
strain our pediatric health systems. The modernization of pediatric environments calls for design of a model that can be sustained, in times of normalcy and crisis, by supportive spaces for children, families, and providers.
2.0 Methodology
This research hypothesizes that the difficulties in access, delivery, and quality of pediatric care can be addressed through a new hospital model, a pediatric microhospital. The research framework included a literature review, survey, expert interviews, and case study analysis. The survey was conducted to capture user group perspectives, the current state, and future potential for modernization of pediatric environments. Conference proceedings on topics of micro-hospitals, pediatric design, and the future of healthcare real estate helped to support and inform this proposal. Data gathered from this research was analyzed to develop design guidelines, recommendations, and considerations for development of a pediatric micro-hospital model.
The primary research question explored was “Can micro-hospitals fill access, delivery, and quality gaps in pediatric care?” with the following secondary questions:
1. What are the types of growing pains in pediatric care?
2. How is a micro-hospital defined?
3. What are the unique considerations of a pediatric micro-hospital?
2.1 Literature Review
A narrative literature review of over 40 sources was conducted to inform current understanding of pediatric care systems, pediatric design, and micro-hospitals. Search databases and journals included the Journal of American Medical Association, American Academy of Pediatrics, the Center for Health Design, Health Environments Research and Design Journal, Google Scholar, PubMed, Research Gate, and other academic and professional journals. Keywords used in the search included “pediatrics,” “inpatient,” “access,” “hospital,” “size,” “scale,” “environments,” and “pediatric design.”
2.2 Survey
A primarily qualitative survey was designed to gather information on the pediatric experience from a diverse range of user group perspectives. User groups included children (6-11 years old), adolescents (12-21 years old), parents/caregivers, health care professionals, relatives of a child/adolescent, and AEC industry professionals. Newborns and infants (0-1 years old) were excluded from this study. Children ages 2-5 years old were also excluded from the children survey section, as it was assumed that any responses from that age range would be captured from the parent/caregiver response section. All survey respondents were provided the definition of micro-hospitals given in Section 3.2, purpose of the research, and survey context details. Survey sections for each user group maintained a constant set of questions, with additional unique questions based on the respective user group. The survey was designed with open-ended questions as well as some closed-ended scaled questions. The main purpose of the survey was to understand relationships between pediatric experiences and the built environment.
2.3 Expert Interviews
Semi-structured 30-minute to 1-hour virtual interviews of AEC and healthcare professionals were conducted to better understand current methods, policy, and spatial gaps in pediatric care. Seven healthcare AEC industry professionals, one micro-hospital systems healthcare administrator, and two clinician interviews were conducted (N=10). The AEC professionals interviewed are experienced in micro-hospital and similar scaled healthcare projects from architectural, financial, and strategy perspectives. Interviews followed a standardized set of questions, with additional unique questions based on every interviewee’s area of expertise.
2.4 Case Studies
Three projects designed by Perkins&Will were selected as case studies based on unique building scale of the facilities, community integration in urban contexts, and innovative design strategies.
22 2023 ― Volume 15.01 Research Journal
1. University of Chicago Medical Center Micro-Hospital and Cancer Center (UCMC)
2. New York-Presbyterian Komansky Children’s Hospital
3. Family Tree Clinic (FTC)
These facilities were analyzed at the macro-scale of community and hospital systems integration and microscale of medical planning of the individual hospitals. The case studies were further informed by expert interviews of the designers, medical planners, and project managers of the respective projects. The author also had the opportunity to attend a user group meeting for pediatric intensive care unit headwall mock-ups at New York Presbyterian Children’s Hospital of New York.
3.0 Results
3.1 Experience-Based Design
The following results from the qualitative survey, expert interviews, and case studies use evidence-based design paired with experience-based design approaches to analyze the feasibility of pediatric micro-hospitals. The sustainability of evidence-based design methods relies on the lived experiences of the users and the hospital.⁸
3.1.1 Survey Results
The survey yielded 37 responses across different user group experiences in pediatric environments (Figure 2). There was an insufficient amount of survey data from children and adolescent respondents to perform reliable analysis.
Negative aspects commonly mentioned from patient and family experiences in hospitals are identified below.
nj long wait times further contributing to children and family’s anxiety
nj few amenities for positive distractions
nj uncomfortable spaces
nj lack of sleeping accommodations
nj parents/caregivers feeling excluded from their child’s care
Two negative spatial analogies of the hospital feeling like a factory and a casino were made, referencing hospital induced delirium and lack of access to natural exterior elements.
Positive aspects and suggestions for improved spaces commonly mentioned from family experiences in hospitals are identified below.
nj calming pediatric graphics
nj child-friendly healthy food options
nj access to respite areas for children and caregivers
nj positive distractions
nj family accommodations in inpatient and waiting rooms
nj comfortable environments
nj children-focused spaces
nj improved facility maintenance
nj increased access to natural daylight in exam rooms and hallways
nj less visual clutter
nj improved wayfinding
nj varied/customizable furniture designed for a wide range of users
23 Growing Pains
Figure 2: Summary of survey respondents. Source: Author.

The parent/caregiver respondents noted light, air quality, sound and noise levels, patient room layout, and family proximity to the hospital were the most important spatial considerations affecting experiences in a pediatric setting. Healthcare professionals noted lighting, surface qualities, patient room layout, proximity to equipment, workstations, and patient rooms as the most important spatial considerations affecting their ability to perform. Across all user groups, outdoor spaces/gardens, clinician recharge spaces, playscapes, and community spaces were chosen as the highest impact spaces desired in pediatric environments (Figure 3). Other unique pediatric spaces noted include adaptive playgrounds, sensory rooms, flexible-use spaces, spaces to accommodate counseling services, support groups and group therapy, multigenerational spaces, pediatric behavioral health dedicated spaces, wellness spaces for meditation and yoga, and age-range adaptable spaces.
Qualities and characteristics desired in future pediatric spaces include the incorporation of latest technology, playfulness, modern, clean, and easy to maintain, positive distractions, emotionally, educationally, and socially enriching, transparency, child-friendly, warm, humane, empowering, supportive, and bright (Figure 4).
Overall, parents/caregivers, AEC professionals, and health professionals view pediatric micro-hospitals as a promising future model of care. Respondents mentioned that since patients need larger support systems, having
a smaller hospital nearby could lessen the burden on parents and families who visit. They also mentioned the need for micro-hospitals to be created as a network system to best fill gaps in underserved areas, located
Figure 4: What does your future children’s hospital look like? Source: Survey Respondent.
24 2023 ― Volume 15.01 Research Journal
Figure 3: Survey insights: Spatial impact across user groups in pediatric environments. Source: Author.
within communities but not too far from each other or a major hub. Modern telemedicine capabilities can help to create a robust healthcare model with access to top-rated clinicians or services. Micro-hospitals have greater ability to engage with the site and outdoor environments. The pandemic has prompted the growth of “hospital at home” or concierge healthcare, which could be developed with micro-hospitals to further integrate systems. Current local conditions have pediatric patients relying solely on the local children's hospital for all types of specialized pediatric care. Microhospitals could relieve the stress on local hospitals by being able to treat patients with less severe injuries and illnesses. The primary concern for pediatric microhospitals noted challenges around staffing, this is addressed in Section 3.3.2.
3.1.2 Case Studies
University of Chicago Medical Center Micro-Hospital and Cancer Center
Project Location: Crown Point, Indiana
Client: University of Chicago Medicine
Size: 115,000 square feet
Project Completion: In Progress
Program: Micro-Hospital, Medical Offices, Ambulatory Surgery Center, Ancillary Services, Cancer Center
Macro: The University of Chicago Medical Center (UCMC) Micro-Hospital and Cancer Center is one of Perkins&Will’s first micro-hospital projects (Figure 5). Situated in northern Indiana, the hospital designates an inpatient hospital presence within the community, serving the neighborhood. It maintains the identity and quality of care associated with UChicago Medicine,
 Figure 5: University of Chicago Medical Center Micro-Hospital and Cancer Center. Source: Perkins&Will.
Figure 5: University of Chicago Medical Center Micro-Hospital and Cancer Center. Source: Perkins&Will.
25 Growing Pains
expanding into a sister region beyond Chicagoland. An emerging practice associated with micro-hospitals to address capital challenges is new partnerships between the healthcare real estate developers and healthcare systems. The stakeholders arranged a long-term leaseback agreement, where UChicago pays interest to the developers to lease out the micro-hospital until a set period in which they will own and operate the building long-term.
Micro: The micro-hospital occupies 15,000 square feet and is physically connected to a larger medical facility. The micro-hospital has access to the main hospital’s imaging and diagnostic services and an ambulatory care center. It is operated and staffed by a third party who specializes in micro-hospital operations, to provide the unique cross-training required for staff at this scale of operations. This system is designed to be staff efficient with minimized overhead costs. The micro-hospital faced regulatory and operational challenges, with complexities in outpatient versus inpatient hospital licensure. Operational licensing of micro-hospitals requires careful review by the authority having jurisdiction, as they are the first of their kind in many cases.
Innovative Design Strategies:
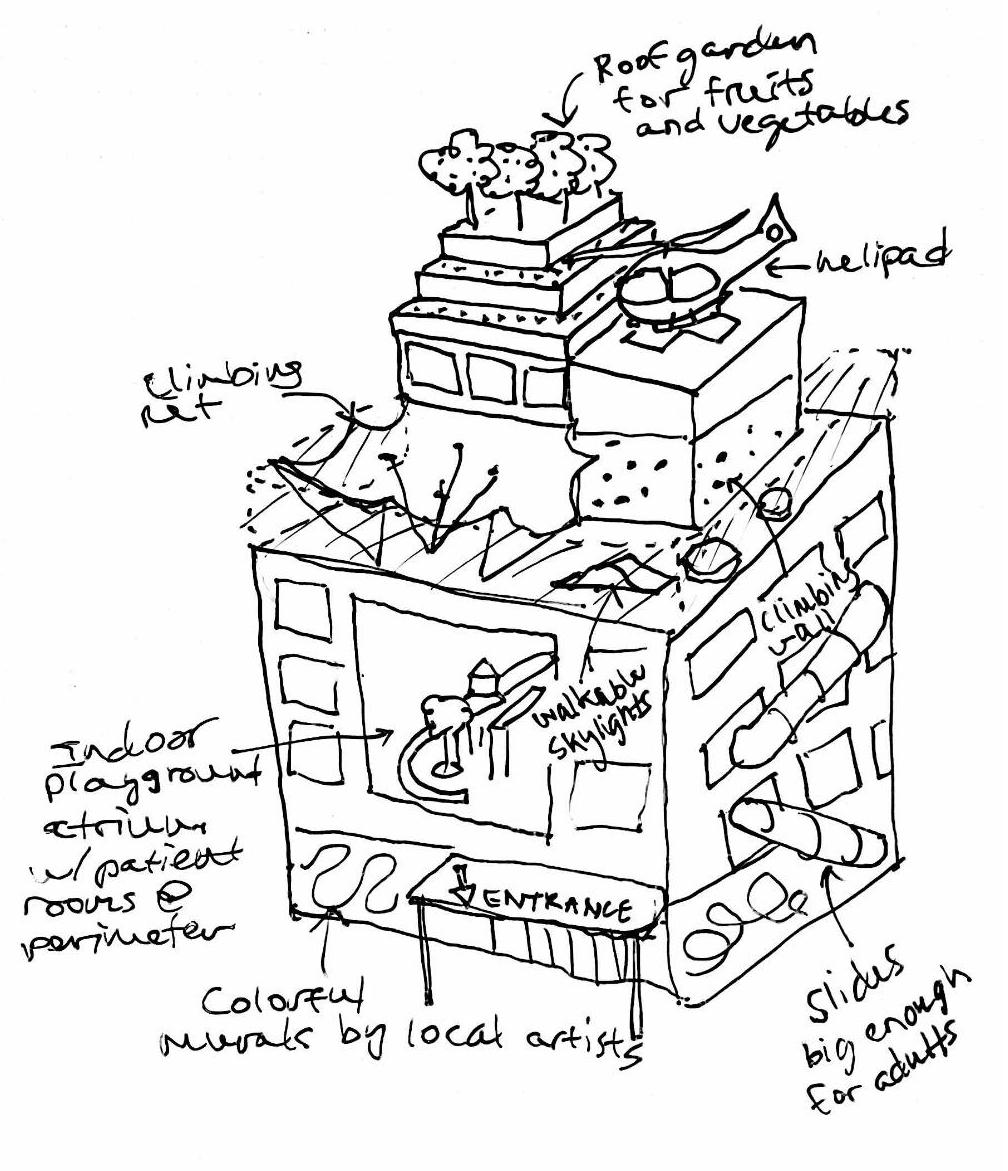
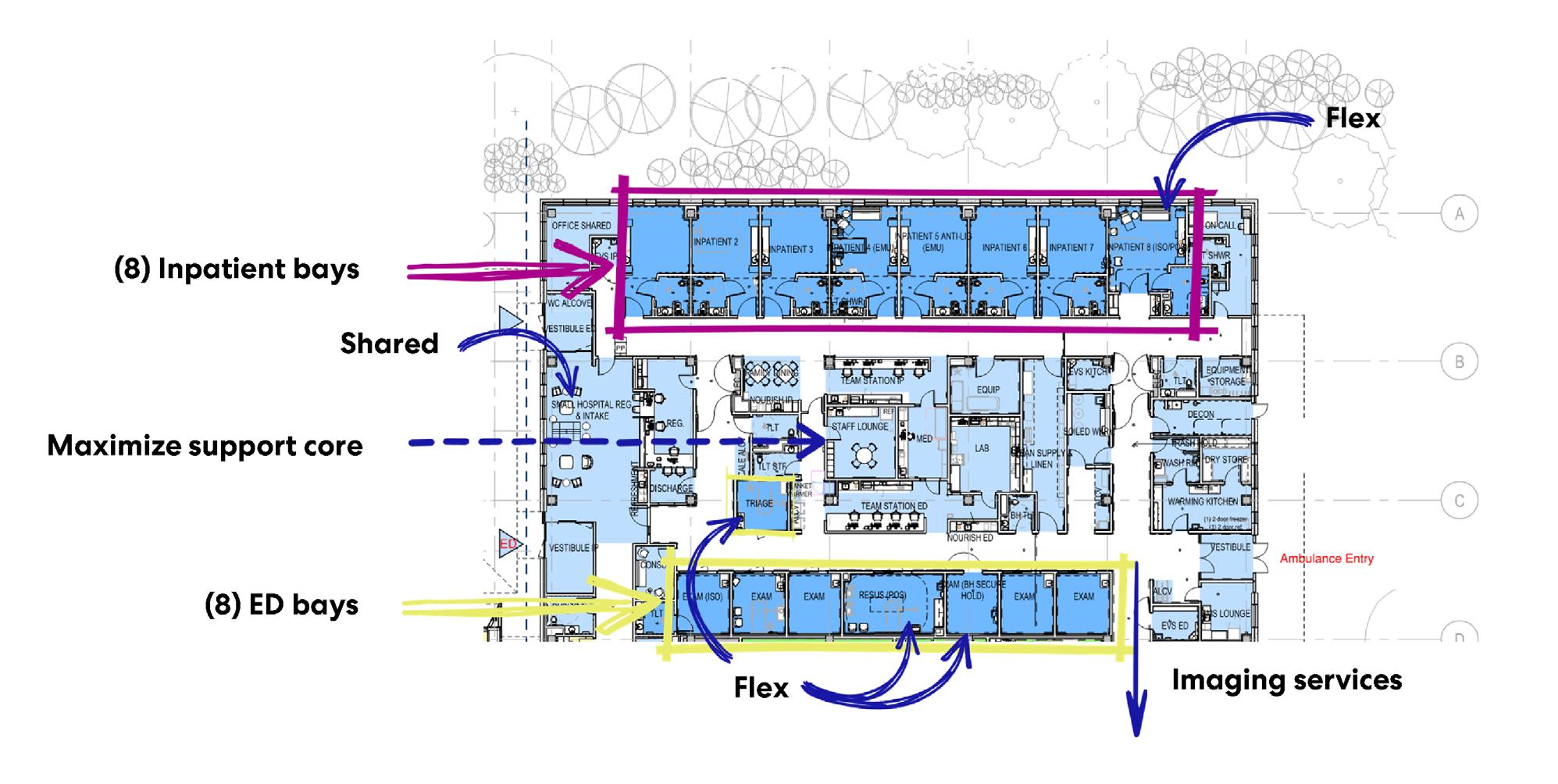
UCMC used a designbuild project delivery model. UCMC set precedence for a unique delivery model that expedites the time from a project award to admission of the hospital’s very first patient, with a total project timeline of 2.5-3 years. In design-build project delivery, the designer and contractor work together from the beginning, as one team, providing unified project recommendations to fit the owner’s budget and schedule.9 Design-build creates an inherent culture of collaboration, the kind of problem-solving and innovation needed to shape the future of micro-hospitals. The weekly owner, architect, contractor meetings from the beginning were greatly beneficial to maintain design and budget alignment. A major client concern was around inflation, as the project was in the middle of historic construction material inflation peaks, causing drastic budget changes in just a few months. A progressive timeline in the AEC industry can improve accessibility to the types of time-sensitive healthcare environments that need it most. In addition, the design of UCMC implemented important space saving strategies, incorporating multi-purpose and flex spaces wherever possible (Figure 6).
26 2023 ― Volume 15.01 Research Journal
Figure 6: Space saving strategies incorporated in the UCMC Micro-Hospital. Source: Author.
New York-Presbyterian Komansky Children’s Hospital
Project Location: New York City, New York
Client: New York Presbyterian Hospital
Size: 35,000 square feet
Project Completion: In Progress
Program: Pediatric Intensive Care Unit, Pediatric Surgical Suite
Macro: The earliest versions of New York Presbyterian Hospital dates to the 1770s and have since grown and modernized alongside New York City. Komansky Children’s Hospital is one of eight children’s hospitals throughout New York City, serving approximately 1.8 children across Manhattan, Brooklyn, the Bronx, Queens, Staten Island, and surrounding areas. It is a Level One Trauma Center and regional burn center. It has consistently ranked as one of the nation’s best children’s hospitals, and many other New York Hospitals are also among the best in the country. The site functions as one of six New York-Presbyterian campuses in New York City. The hospital site spans two city blocks and one avenue.
Micro: Komansky Children’s Hospital is located within Weill Cornell Medical Center. The pediatric acute care unit is on level 6 and pediatric surgical services are on level 7. There are 109 beds in the unit.
Innovative Design Strategies: This case study offers insight into medical planning priorities in limited space contexts and ways to integrate comforting elements into the patient experience. The PICU patient rooms in this unit are smaller than average patient rooms that would be designed today. Due to the space constraints of renovating an existing building in New York City, maximization of every square foot matters. The design strategy took inspiration from the surrounding city contexts – the building is situated with views that overlook the East River, city gardens, and historic Upper East Side brownstones (Figure 7). The interior color palette was inspired by the three unique gradients of blues, greens, and browns. Each wing of the unit incorporates familiar city elements of subways, skyscrapers, and brownstones as wayfinding elements.
 Figure 7: Komansky Children’s Hospital Waiting. Source: Perkins&Will.
Figure 7: Komansky Children’s Hospital Waiting. Source: Perkins&Will.
27
Growing Pains
Family Tree Clinic
Project Location: Minneapolis, Minnesota
Client: Family Tree Clinic
Size: 17,000 square feet
Project Completion: 2021
Program: Family Health and Reproductive Services
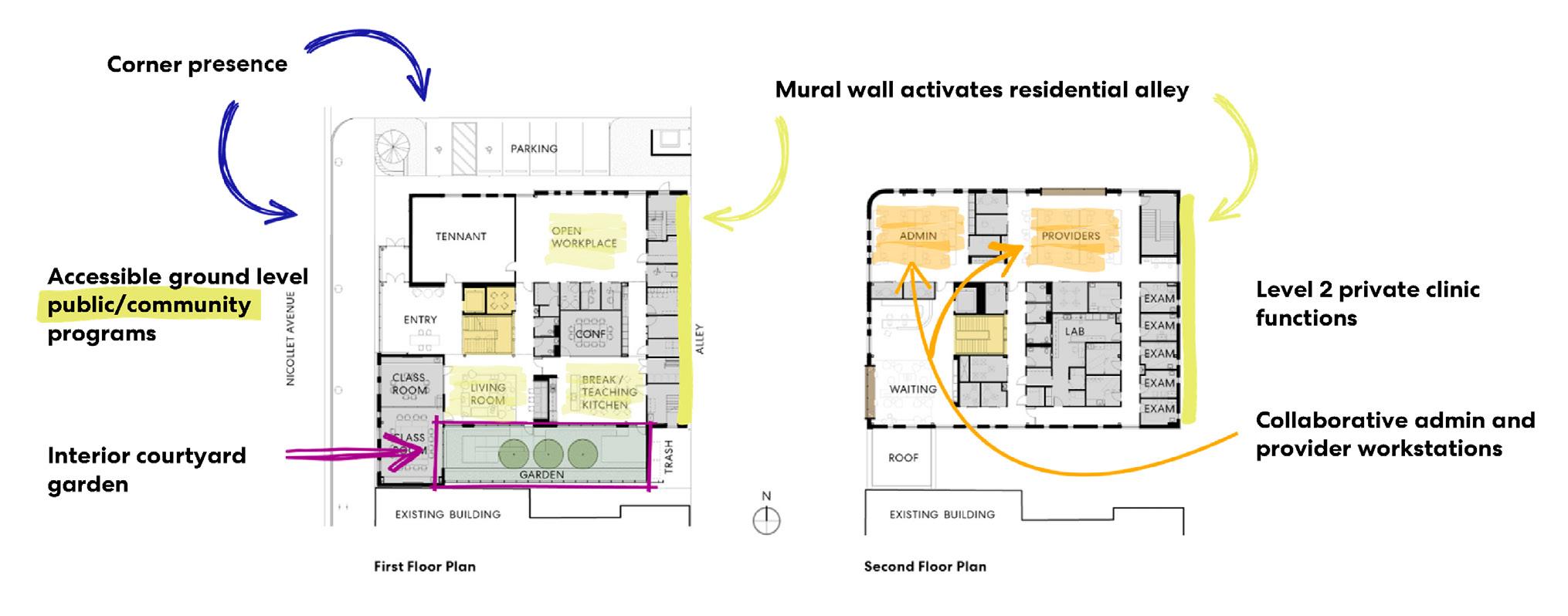
Macro: The Family Tree Clinic (FTC) is a leading example of social impact work at Perkins&Will (Figure 8). FTC is a space that provides hope, respite, and specialized care for the LQBTQIA+ community in Minneapolis and the
surrounding neighborhoods. Family Tree Clinic is a nonprofit organization with the mission to provide health care that uplifts patients through education, accessibility, and understanding. As a community clinic, FTC focuses its healthcare services on providing the best care for uninsured, underinsured, working poor, high-risk, and vulnerable populations. FTC has expanded to pediatric care serving an additional 10,000 patients per year.
Micro: Clinic accessibility is critical. FTC is strategically embedded within the community and is accessible by three mass transit lines, bike share, and two

28 2023 ― Volume 15.01 Research Journal
Figure 8: (Left to Right) Family Tree Clinic waiting, staircase, and (below) Mural wall. Source: Perkins&Will.
major interstates. The clinic itself is situated along a retail corridor representing a safe, inviting, and familiar presence. The clinic intentionally maintains neighborhood familiarity through its two-story smallscale design and brick materiality. On a similar scale to a micro-hospital, this facility successfully showcases what a two-story micro-hospital could look like.
Innovative Design Strategies: This project is an example of how healthcare organizations, AEC firms, and community partnerships can redefine the roles of medical buildings in the communities as hubs for physical and social well-being. This exceptional level of community collaboration is important for micro-hospital integration in neighborhoods. Facility community involvement such as listening sessions and parent classes helps address health disparities at the home and neighborhood levels. It is critical to design the space within healthcare facilities for community engagement to grow (Figure 8). The clinic embodies inclusive and universal design principles through researched color palettes, diverse seating arrangements, and representation of body types with local art and imagery within the clinic. These are effective tools to accommodate a range of patient ages and can help bridge design for the wide age range of pediatric spaces. The organization seeks to hire and train individuals within the community for medical roles, which helps provide a stake and personal investment into the care of the facility. The clinic also implements a courtyard garden along one façade, allowing relief
from the existing building and more surface area for daylight and views.
3.2 Analysis of the Micro-Hospital for Pediatrics
Micro-hospitals are an evolving concept in healthcare and AEC industries. There is limited research on the topic of micro-hospitals. State Departments of Health are beginning to establish local classifications and guidelines for micro-hospitals.10 Generally, microhospitals can be defined as small-scale, inpatient facilities with an average of 8-10 beds that range from 15,000 to 50,000 square feet. They are licensed hospitals that operate 24/7 care offering a set of core services, including inpatient care, emergency medical care, laboratories and lab services, diagnostic imaging, pharmacy services, and additional services based on local needs.11,12,13,14 Micro-hospitals are intended to fill access gaps in underserved communities and provide a local alternative of care closer to home. Micro-hospitals have been constructed in approximately 20 US states and are expected to continue in growth.13
While all micro-hospitals operate with a core set of services, they are highly customizable to meet the needs of local patient populations, and for healthcare organizations to target new or growing markets. Additional services included in some micro-hospitals are primary care, outpatient rehabilitation, outpatient
29 Growing Pains
Figure 9: Community Integration Strategies Incorporated in the Family Tree Clinic. Source: Author.
surgery, specialty care, wellness services, and women’s services.11 The micro-hospital model has not yet been explored for pediatric populations.
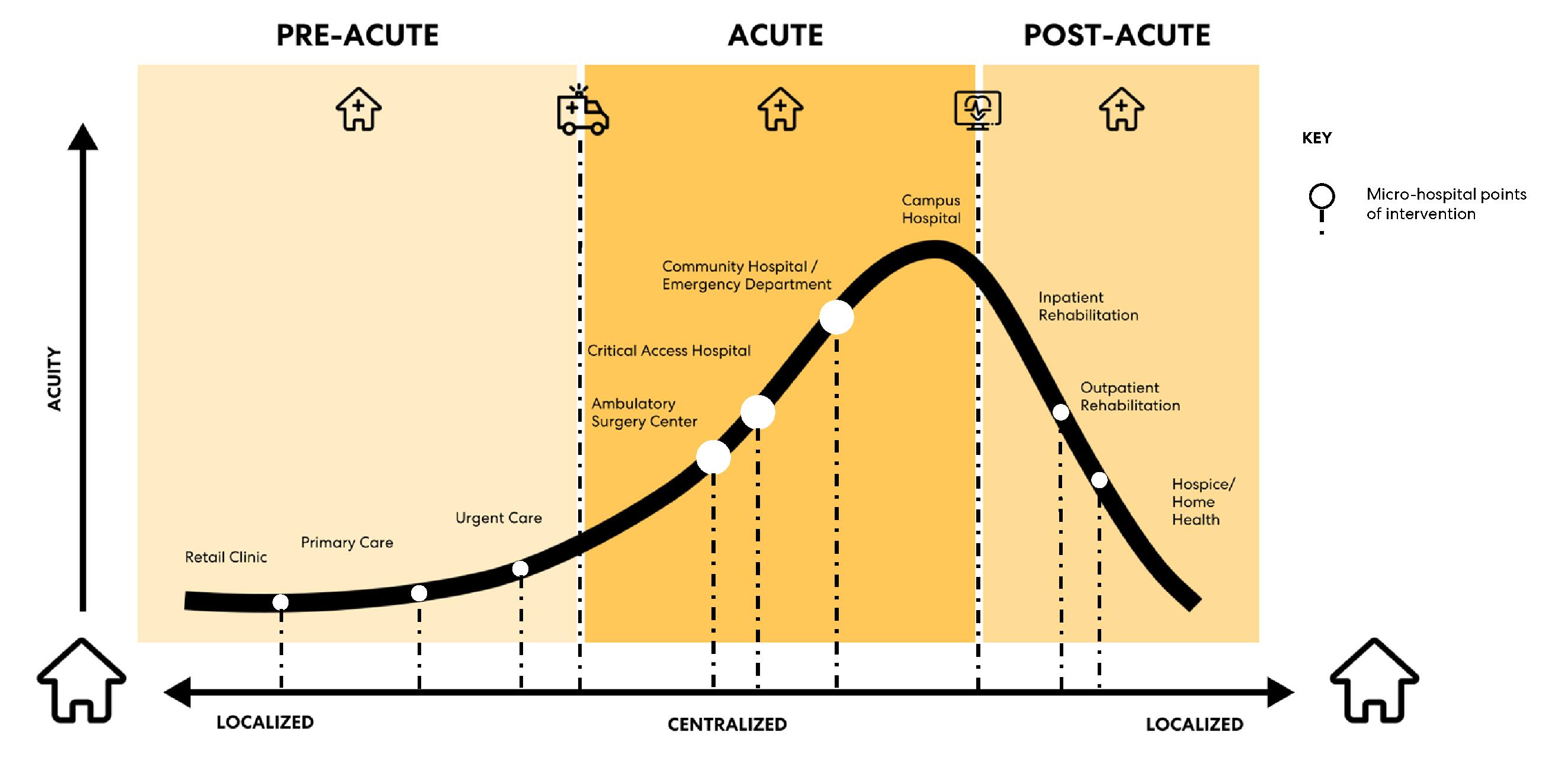
Pediatric micro-hospitals as a future model of care have significant potential to address current and future capacity problems in pediatric care (Figure 10). Pediatric healthcare facilities are at risk of volume surges and limited bed capacity with increasing regionalization of services.6,15 Tertiary and large academic pediatric referral centers in urban areas are especially at risk.6,16 Volume surges and bed capacity problems can be mitigated by offloading lower acuity pediatric patients from Level I hospitals into micro-hospitals.
Micro-hospital settings work well for low-acuity patients, who may need inpatient overnight stays for 1-3 nights but are at low risk of needing transfers to tertiary centers. Most micro-hospitals are designated as Level IV-V Trauma Centers equipped to provide evaluation, stabilization,
and diagnostic capabilities for injured patients before transfer to a higher-level trauma center. Interviewed healthcare professionals mentioned patient populations that are low complexity, need simple outpatient procedures or treatment, and may benefit in smaller hospital settings as potential patient populations. Some patient populations suitable for integration in a pediatric micro-hospital model may include behavioral health patients, rehabilitation patients, patients with simple orthopedic conditions, and patients with respiratory illnesses.5,6,17
Most existing micro-hospitals have been established through joint venture partnerships between microhospital developers and hospital systems.18 Patient transfer agreements must be established between the micro-hospital and tertiary hospital should a patient admitted at a micro-hospital become more acute beyond the hospital’s capabilities,
30 2023 ― Volume 15.01 Research Journal
Figure 10: Micro-Hospitals Across the Healthcare Continuum. Visually adapted from Emerus.
3.2.1 The Benefits of Small Hospitals for Small Patients
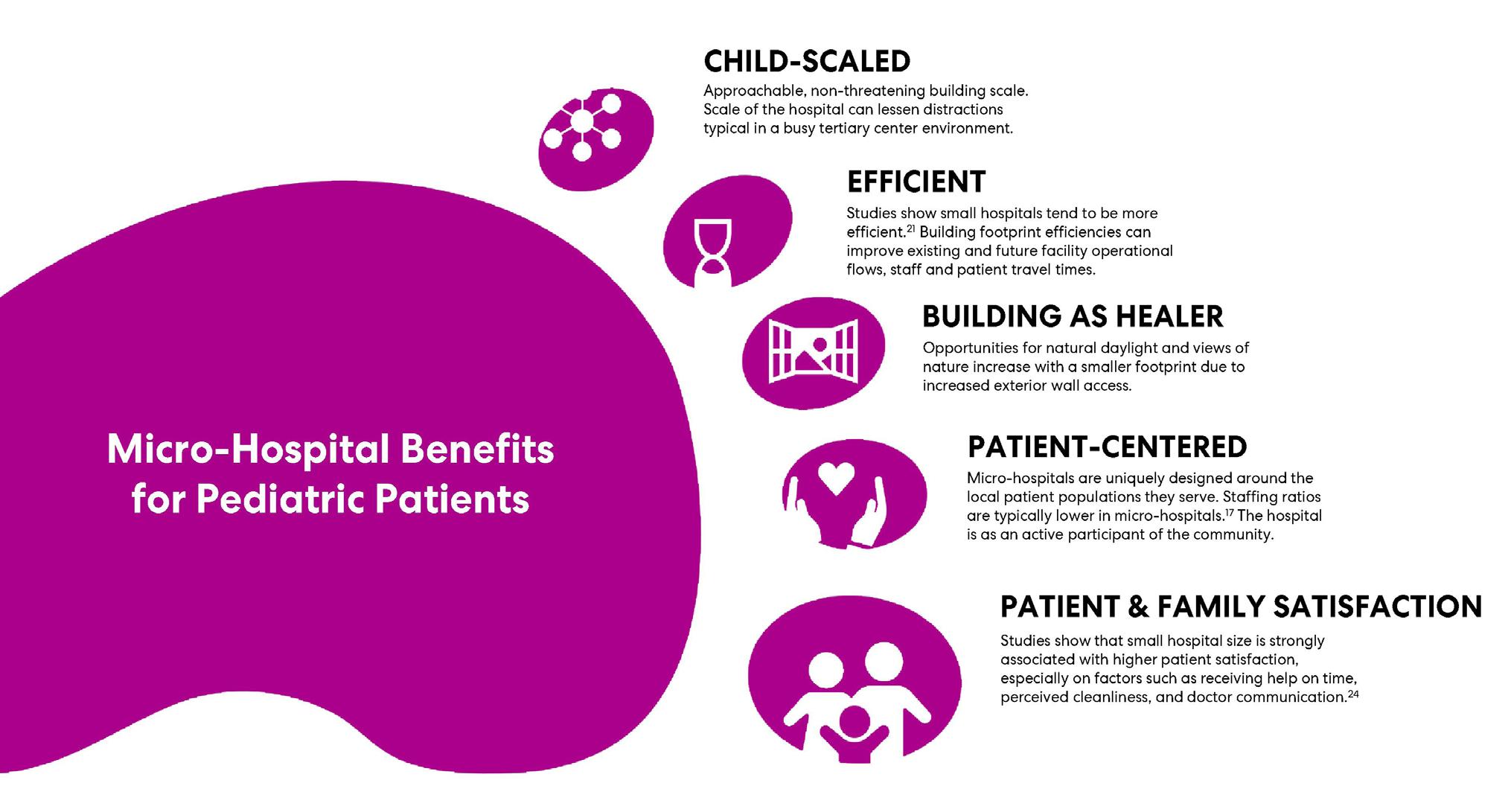
A critical advantage of a micro-hospital is its unique relationship to scale, both in its positioning across geographies and physical size of the facility. Possible advantages of a pediatric micro-hospital model were summarized based on survey responses, literature review, and expert interviews (Figure 11).
A micro-hospital is a child-scaled, approachable, and non-threatening building scale. The small scale of the hospital can lessen distractions typical in a busy tertiary center environment. Less support staff is needed with fewer patients, lessening the total noise levels and visual distractions for child patients. Noise, even at normal to moderate levels, was associated with physiological and psychological stress and poorer cognitive functioning. Crowding, both spatial and social, was associated with poorer cognitive, physiological, and behavioral functioning.19 Survey respondents commonly mentioned approachability, familiarity, and comfort as positive qualities from hospital experiences.
Studies show small hospitals tend to be more efficient.20,21 Building footprint efficiencies can improve existing and future facility operational flows, staff, and patient travel times.
Opportunities for natural daylight and views of nature increase with a smaller footprint due to increased exterior wall access. Natural daylight and views of nature have been widely studied and proven to impact shorter patient stays, improve patient satisfaction, and improve patient outcomes.22
Micro-hospitals are uniquely designed around the local patient populations they serve. Interviewees noted staffing ratios are typically lower in micro-hospitals than in large hospitals. Patient and family-centered care becomes easier to prioritize with lower overall patient volumes. Micro-hospitals have potential to improve compassion as a central construct to quality of pediatric healthcare.23
Small hospital size is strongly associated with higher patient satisfaction, especially on factors such as receiving help on time, perceived cleanliness, and doctor communication. 24 Patient satisfaction is an important and commonly used indicator to measure the quality of health care systems. Patient satisfaction affects clinical outcomes, patient retention, and medical malpractice risk.
31 Growing Pains
Figure 11: The Benefits of Small Hospitals for Small Patients. Source: Author.
3.2.2 Addressing the Concerns
Possible disadvantages and concerns of a pediatric micro-hospital model were summarized based on survey responses, literature review, and expert interviews. The primary concern mentioned by survey respondents and interviewees was the ability to adequately staff a pediatric micro-hospital given the existing staff shortages. One method to address the existing healthcare staff shortages is through cross-training. 25 Cross-training staff will become increasingly valuable within micro-hospital models. 25,26,27,28,29 The millennial generation of nursing professionals seek growth development opportunities with blended roles and leadership development opportunities. Cross-training is a strategic approach for enhancing nurse satisfaction and retention. 26 Implementation of cross-training in pediatric hospitalist roles in a combined pediatric emergency department (ED) and inpatient unit was associated with improved financial outcomes, increased ED patient satisfaction, and decreased throughout times.30 Effective cross-training promotes professional development, team workflows and dynamics, wellbeing, and reduces staffing costs.25,26,27,28,29
Another concern mentioned was around maintaining staff proficiencies with low micro-hospital patient volumes. Rotating staff scheduling between the affiliated tertiary hospital and the micro-hospital can provide continuity in both staff competency and standards of care.
Another concern of pediatric micro-hospitals is in achieving successful integration with tertiary hospitals. Telehealth support infrastructure within micro-hospitals can provide cost effective and convenient consultation between micro-hospital and tertiary center providers.31 Advancements in telemedicine technology can enable access to specialists 24/7 from micro-hospital settings. Telehealth can also be integrated with micro-hospital patients in the medical home model as a means of further improving access, quality, and cost in pediatric care.32
The long-term economic implications of micro-hospitals are unknown. The following section outlines some of the financial considerations of a pediatric micro-hospital.
3.3 The Business Case for Pediatric Micro-Hospitals
Micro-hospitals are an emerging market. Investment in specialized micro-hospitals for pediatric populations may be an economic and innovative solution to address the pediatric care crisis. Strategic facility site selection, careful assessment of pediatric patient populations, integration with existing facility operations, and collaborative interdisciplinary design solutions will have a critical role in the financial success of a pediatric micro-hospital.
1. Strategic Community Growth: Micro-hospitals build a community health-minded approach. Offensive or defensive growth strategies can introduce healthcare networks into new communities.
2. Service: The quality of services for children and their families can improve with patient-centered care being a primary focus in micro-hospitals.
3. Speed to Market: Design to micro-hospital opening times is 2-3 years total, which is shorter than typical hospital development timelines. This may help deliver care more quickly to medically underserved areas.
4. Low Relative Upfront Costs: The design and construction costs of a micro-hospital range from $7 million to $30 million, which is considerably less expensive than $112 million for the national average cost of a large hospital development.33,34 A pediatric micro-hospital can offer a low-cost growth opportunity for pediatric health systems that may need expansion but have limited funding.
5. Lower Facility Operations and Maintenance Costs: The small facility footprint reduces the overall energy loads of electricity, natural gas, fuel oil, and district heat required to operate the hospital.35 The embodied and operational carbon of the building can be reduced by the micro-hospital footprint efficiencies. Smaller facilities may require less sophisticated heating, ventilation, and air conditioning systems with shorter ductwork runs due to the small scale, zoning proximities, and more compact service areas.
6. Lower Overhead Costs: Staffing models with crosstraining can lower long-term overhead costs of operating the facility.
32 2023 ― Volume 15.01 Research Journal
7. Operational Efficiencies: Door-to-doctor times, staff, patient, and logistics travel times are improved with shorter travel distances.14,21
8. Higher Patient and Staff Satisfaction: Microhospitals provide higher patient satisfaction than large hospitals, driving patient loyalty.
9. Diversified Real Estate Portfolio: A small footprint provides flexibility in site selection and diversifies healthcare system’s real estate.
10. Opportunity for Innovation: Implementation of a new physical model will require adjustments to operational models, posing an opportunity for healthcare systems to reevaluate existing staffing, resource allocation, technology, and even care models, to find ways to improve.36
4.0 Framework for the Pediatric Hospital Model
The knowledge acquired from Sections 3.2 and 3.3 has informed the framework developed below.
4.1 Pediatric Micro-Hospital Program Guidelines
Since micro-hospitals are largely defined by their scale, it is important to identify the minimum size a pediatric micro-hospital can be. Program guidelines were developed, based on Facilities Guidelines Institute (FGI) Guidelines, to be used as a starting point for facilities and design professionals to better understand the services and minimum functional requirements of a pediatric micro-hospital. Pediatric Micro-Hospital Program Guidelines can be found in Table 1. Additional program identified through the survey, interviews, and literature to improve patient and staff experience is notated with an asterisk. This program accounts for eight pediatric inpatient and eight emergency department beds. This program can be scaled up to meet specific hospital needs. Pediatric design guidelines conflict with size. Pediatric spaces oftentimes have higher space requirements than that of adult populations because there must be appropriate accommodation space for the child and their family.37 So the challenge is: how do we design child-scale hospitals that think big?
Room / Space Name QtyUnit Area (SF)Net Area (SF) Space Consolidation / Notes REGISTRATION & MAIN WAITING Public / Registration Patient/Family Drop-Off/Pick-Up 1 - - Outside Entry Vestibule, Inpatient 1 120 120 Entry Vestibule, ED 1 160 160 Entry Vestibule, Staff 1 160 160 Alcove, Wheelchair Storage 1 40 40Part of ED vestibule Alcove, Stroller/Carrier Storage 1 40 40Part of inpatient vestibule Security 1 120 120 Registration Admission/Discharge 1 360 360Collocated, 3 positions for intake and 1 for discharge Imaging Check-In 2 10 20Includes imaging and blood draw registration Waiting, Inpatient 1 120 1208 seats Waiting, ED 1 120 1208 seats Waiting, Imaging/Blood Draw 1 120 1208 seats Waiting, Family 1 200 200Distribute to waiting areas Consult, Family 1 100 100 Toilet, Family 2 70 140 Refreshment Alcove 1 30 30 *Telemedicine Services 1 100 100 *Community / Multi-Purpose Conference 1 200 200 *Convenience/Retail Small 1 150 150 *Courtyard/Garden 1 - -Outside PEDIATRIC INPATIENT UNIT Patient Care Areas Inpatient Room 7 270 1890 Toilet Shower, Inpatient 7 60 420 Inpatient Room, Isolation 1 290 290Doubles as patient of size (POS) room Ante/PPE Alcove 1 40 40 Toilet Shower, Inpatient 1 70 70 Department / Functional Area 33
Table 1: Pediatric Micro-Hospital Space Program Guidelines.
Growing Pains
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Room / Space Name QtyUnit Area (SF)Net Area (SF) Space Consolidation / Notes REGISTRATION & MAIN WAITING Public / Registration Patient/Family Drop-Off/Pick-Up 1 - - Outside Entry Vestibule, Inpatient 1 120 120 Entry Vestibule, ED 1 160 160 Entry Vestibule, Staff 1 160 160 Alcove, Wheelchair Storage 1 40 40Part of ED vestibule Alcove, Stroller/Carrier Storage 1 40 40Part of inpatient vestibule Security 1 120 120 Registration Admission/Discharge 1 360 360Collocated, 3 positions for intake and 1 for discharge Imaging Check-In 2 10 20Includes imaging and blood draw registration Waiting, Inpatient 1 120 1208 seats Waiting, ED 1 120 1208 seats Waiting, Imaging/Blood Draw 1 120 1208 seats Waiting, Family 1 200 200Distribute to waiting areas Consult, Family 1 100 100 Toilet, Family 2 70 140 Refreshment Alcove 1 30 30 *Telemedicine Services 1 100 100 *Community / Multi-Purpose Conference 1 200 200 *Convenience/Retail Small 1 150 150 *Courtyard/Garden 1 - -Outside PEDIATRIC INPATIENT UNIT Patient Care Areas Inpatient Room 7 270 1890 Toilet Shower, Inpatient 7 60 420 Inpatient Room, Isolation 1 290 290Doubles as patient of size (POS) room Ante/PPE Alcove 1 40 40 Toilet Shower, Inpatient 1 70 70 Play Space 1 80 80 Storage, Toys 1 20 20Locate within play space Family Lounge/Dining 1 150 150 Locate by team station, nourishment, and play space *Linen Services 1 60 60 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Clean Supply/Linen Room 1 310 310 Medication Room 1 160 160 Nourishment Alcove 1 50 50 Soiled Utility 1 140 140 Storage, Equipment 2 180 360 (1) Shared with inpatient and ED (1) Pediatric bed and other equipment storage Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Staff & Administration Support Areas Shared Office, General 2 170 340 (1) Shared with inpatient, ED, & imaging (1) Shared with child life, OT/PT, & other support services Lounge, Staff 1 200 200 Lockers, Staff 1 30 30 Locate within lounge Toilet, Staff 1 60 60 PEDIATRIC EMERGENCY DEPARTMENT Patient Care Areas ED Triage 1 120 120 Doubles as ED treatment room ED Resuscitation 1 280 280 Doubles as POS treatment room Department / Functional Area Entry Vestibule, Inpatient 1 120 120 Entry Vestibule, ED 1 160 160 Entry Vestibule, Staff 1 160 160 Alcove, Wheelchair Storage 1 40 40Part of ED vestibule Alcove, Stroller/Carrier Storage 1 40 40Part of inpatient vestibule Security 1 120 120 Registration Admission/Discharge 1 360 360Collocated, 3 positions for intake and 1 for discharge Imaging Check-In 2 10 20Includes imaging and blood draw registration Waiting, Inpatient 1 120 1208 seats Waiting, ED 1 120 1208 seats Waiting, Imaging/Blood Draw 1 120 1208 seats Waiting, Family 1 200 200Distribute to waiting areas Consult, Family 1 100 100 Toilet, Family 2 70 140 Refreshment Alcove 1 30 30 *Telemedicine Services 1 100 100 *Community / Multi-Purpose Conference 1 200 200 *Convenience/Retail Small 1 150 150 *Courtyard/Garden 1 - -Outside PEDIATRIC INPATIENT UNIT Patient Care Areas Inpatient Room 7 270 1890 Toilet Shower, Inpatient 7 60 420 Inpatient Room, Isolation 290 290Doubles as patient of size (POS) room Ante/PPE Alcove 40 40 Toilet Shower, Inpatient 70 70 Play Space 80 80 Storage, Toys 20 20Locate within play space Family Lounge/Dining 1 150 150 Locate by team station, nourishment, and play space *Linen Services 1 60 60 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Clean Supply/Linen Room 1 310 310 Medication Room 1 160 160 Nourishment Alcove 1 50 50 Soiled Utility 1 140 140 Storage, Equipment 2 180 360 (1) Shared with inpatient and ED (1) Pediatric bed and other equipment storage Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Staff & Administration Support Areas Shared Office, General 2 170 340 (1) Shared with inpatient, ED, & imaging (1) Shared with child life, OT/PT, & other support services Lounge, Staff 1 200 200 Lockers, Staff 1 30 30 Locate within lounge Toilet, Staff 1 60 60 PEDIATRIC EMERGENCY DEPARTMENT Patient Care Areas ED Triage 1 120 120 Doubles as ED treatment room ED Resuscitation 1 280 280 Doubles as POS treatment room ED Treatment 5 150 750 One doubles as a behavioral health holding room ED Treatment Isolation 1 150 150 Ante Room, Isolation - 40Toilet, Patient 1 60 60 Toilet, Patient 2 60 120 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Alcove, Scale 1 20 20 Alcove, Pediatric Scale 1 20 20 Clean Supply/Linen Room - 120 -Shared with Inpatient Medication Room - 120 -Shared with Inpatient Nourishment Alcove - 50 -Shared with Inpatient Soiled Utility - 140 -Shared with Inpatient Storage, Equipment - 180 -Shared with Inpatient Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Ambulance Vestibule 34 2023 ― Volume 15.01 Research Journal
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Room / Space Name QtyUnit Area (SF)Net Area (SF) Space Consolidation / Notes REGISTRATION & MAIN WAITING Public / Registration Patient/Family Drop-Off/Pick-Up 1 - - Outside Entry Vestibule, Inpatient 1 120 120 Entry Vestibule, ED 1 160 160 Entry Vestibule, Staff 1 160 160 Alcove, Wheelchair Storage 1 40 40Part of ED vestibule Alcove, Stroller/Carrier Storage 1 40 40Part of inpatient vestibule Security 1 120 120 Registration Admission/Discharge 1 360 360Collocated, 3 positions for intake and 1 for discharge Imaging Check-In 2 10 20Includes imaging and blood draw registration Waiting, Inpatient 1 120 1208 seats Waiting, ED 1 120 1208 seats Waiting, Imaging/Blood Draw 1 120 1208 seats Waiting, Family 1 200 200Distribute to waiting areas Consult, Family 1 100 100 Toilet, Family 2 70 140 Refreshment Alcove 1 30 30 *Telemedicine Services 1 100 100 *Community / Multi-Purpose Conference 1 200 200 *Convenience/Retail Small 1 150 150 *Courtyard/Garden 1 - -Outside PEDIATRIC INPATIENT UNIT Patient Care Areas Inpatient Room 7 270 1890 Toilet Shower, Inpatient 7 60 420 Inpatient Room, Isolation 1 290 290Doubles as patient of size (POS) room Ante/PPE Alcove 1 40 40 Toilet Shower, Inpatient 1 70 70 Play Space 1 80 80 Storage, Toys 1 20 20Locate within play space Family Lounge/Dining 1 150 150 Locate by team station, nourishment, and play space *Linen Services 1 60 60 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Clean Supply/Linen Room 1 310 310 Medication Room 1 160 160 Nourishment Alcove 1 50 50 Soiled Utility 1 140 140 Storage, Equipment 2 180 360 (1) Shared with inpatient and ED (1) Pediatric bed and other equipment storage Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Staff & Administration Support Areas Shared Office, General 2 170 340 (1) Shared with inpatient, ED, & imaging (1) Shared with child life, OT/PT, & other support services Lounge, Staff 1 200 200 Lockers, Staff 1 30 30 Locate within lounge Toilet, Staff 1 60 60 PEDIATRIC EMERGENCY DEPARTMENT Patient Care Areas ED Triage 1 120 120 Doubles as ED treatment room ED Resuscitation 1 280 280 Doubles as POS treatment room Department / Functional Area PEDIATRIC EMERGENCY DEPARTMENT Patient Care Areas ED Triage 1 120 120 Doubles as ED treatment room ED Resuscitation 1 280 280 Doubles as POS treatment room ED Treatment 5 150 750 One doubles as a behavioral health holding room ED Treatment Isolation 1 150 150 Ante Room, Isolation - 40Toilet, Patient 1 60 60 Toilet, Patient 2 60 120 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Alcove, Scale 1 20 20 Alcove, Pediatric Scale 1 20 20 Clean Supply/Linen Room - 120 -Shared with Inpatient Medication Room - 120 -Shared with Inpatient Nourishment Alcove - 50 -Shared with Inpatient Soiled Utility - 140 -Shared with Inpatient Storage, Equipment - 180 -Shared with Inpatient Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Ambulance Vestibule 1 100 100 Decontamination Shower Room 1 160 160 Located on ambulance drop-off side Staff and Administration Support Areas Office, General - 100 -Shared with Inpatient Conference Room - 200 -Shared with public/main waiting Lounge, Staff - 200 -Shared with Inpatient Lockers, Staff - 30 -Shared with Inpatient Toilet, Staff 1 60 60 EMS Lounge 1 140 140 Can be used as a staff wellness room Physician On-Call Room 1 160 160 Can be used as workroom Toilet, Shower 1 70 70 IMAGING SERVICES Patient Care Areas Radiography/Fluoroscopy 1 400 400 Alcove, Imaging 1 40 40 Mobile imaging X-Ray 1 380 380 Patient Dressing 1 40 40 MRI 1 450 450 Control 1 130 130 Equipment Room 1 40 40 Patient Dressing 1 40 40 CT 1 450 450 Control 1 130 130 Equipment Room 1 40 40 Patient Dressing - 40 -Shared PET 1 450 450 Control 1 130 130 Equipment Room 1 40 40 Patient Dressing - 40 -Shared Pediatric Injection Room 1 100 100 IV Patient Hold Bay 1 70 70 Toilet, Patient 1 60 60 Clinical Support Areas 1 20 20 1 20 20 1 20 20 1 100 100 1 50 50 Alcove, Linen Alcove, Sink and Contrast Storage Alcove, Crash Cart Clean Supply Soiled Holding Environmental Services/Housekeeping Closet 1 60 60 Staff and Administration Support Areas Office, General - 100 -Shared with Inpatient Conference Room - 200 -Shared with public/main waiting Lounge, Staff - 200 -Shared with Inpatient Lab/Blood Draw Registration & Waiting - - Shared with Imaging Intake & Waiting Blood Draw Stations 2 50 100 Recliners with one large enough for stretcher Toilet, Patient 1 60 60 Includes specimen pass-thru Shared Staff Workstation 1 100 100 4 positions Lab 1 400 400 35 Growing Pains
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
4.2 Feasibility for Pediatric Micro-Hospitals in Urban Settings—New York City
The opportunities presented for pediatric microhospitals in an urban setting such as New York City are unique. New York City was home to Dr. Abraham Jacobi, who distinguished pediatrics in the 1860s as a unique field of medicine and is widely considered to be the father of pediatrics.
New York City was an early epicenter of COVID19 infections in 2019, with overwhelmed pediatric emergency departments. 38 The ongoing impacts of COVID-19 on New York City hospital systems are still seen today, with threatened pediatric hospital capacity during 2022.1,16 NYC Health + Hospitals is the largest healthcare delivery system in the United States, consisting of a network of hospitals at all scales from community hospitals to home care services.39 New York City is an ideal testbed for micro-hospital innovation due to its characteristics of being high density, diverse with all types of patient populations, being a historic city
with limited space, and a mindset of space as a precious commodity and resource. This criterion sets prime grounds for a model such as a micro-hospital to be integrated into existing healthcare infrastructures. One particular benefit of locating micro-hospitals in urban areas is the potential for direct connection, proximity, and integration into large academic hospitals. The
 Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Figure 12: A Micro-Hospital on a New York City Block. Source: Author.
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Figure 12: A Micro-Hospital on a New York City Block. Source: Author.
QtyUnit Area (SF)Net Area (SF)
REGISTRATION & MAIN WAITING Public / Registration Patient/Family Drop-Off/Pick-Up 1 - - Outside Entry Vestibule, Inpatient 1 120 120 Entry Vestibule, ED 1 160 160 Entry Vestibule, Staff 1 160 160 Alcove, Wheelchair Storage 1 40 40Part of ED vestibule Alcove, Stroller/Carrier Storage 1 40 40Part of inpatient vestibule Security 1 120 120 Registration Admission/Discharge 1 360 360Collocated, 3 positions for intake and 1 for discharge Imaging Check-In 2 10 20Includes imaging and blood draw registration Waiting, Inpatient 1 120 1208 seats Waiting, ED 1 120 1208 seats Waiting, Imaging/Blood Draw 1 120 1208 seats Waiting, Family 1 200 200Distribute to waiting areas Consult, Family 1 100 100 Toilet, Family 2 70 140 Refreshment Alcove 1 30 30 *Telemedicine Services 1 100 100 *Community / Multi-Purpose Conference 1 200 200 *Convenience/Retail Small 1 150 150 *Courtyard/Garden 1 - -Outside PEDIATRIC INPATIENT UNIT Patient Care Areas Inpatient Room 7 270 1890 Toilet Shower, Inpatient 7 60 420 Inpatient Room, Isolation 1 290 290Doubles as patient of size (POS) room Ante/PPE Alcove 1 40 40 Toilet Shower, Inpatient 1 70 70 Play Space 1 80 80 Storage, Toys 1 20 20Locate within play space Family Lounge/Dining 1 150 150 Locate by team station, nourishment, and play space *Linen Services 1 60 60 Clinical Support Areas Team Station 1 200 200 Alcove, Equipment 1 20 20 Locate within team station Alcove, Code Cart 1 20 20 Locate within team station Handwash Station 1 10 10 Locate within team station Alcove, Printing 1 10 10 Locate within team station Clean Supply/Linen Room 1 310 310 Medication Room 1 160 160 Nourishment Alcove 1 50 50 Soiled Utility 1 140 140 Storage, Equipment 2 180 360 (1) Shared with inpatient and ED (1) Pediatric bed and other equipment storage Alcove, Equipment 1 50 50 Storage, Medical Gas Cylinder - 50 -Shared with med gas manifold room Environmental Services/Housekeeping Closet 1 60 60 Staff & Administration Support Areas Shared Office, General 2 170 340 (1) Shared with inpatient, ED, & imaging (1) Shared with child life, OT/PT, & other support services Lounge, Staff 1 200 200 Lockers, Staff 1 30 30 Locate within lounge Toilet, Staff 1 60 60 PEDIATRIC EMERGENCY DEPARTMENT Patient Care Areas ED Triage 1 120 120 Doubles as ED treatment room ED Resuscitation 1 280 280 Doubles as POS treatment room Department / Functional Area Control 1 130 130 Equipment Room 1 40 40 Patient Dressing - 40 -Shared Pediatric Injection Room 1 100 100 IV Patient Hold Bay 1 70 70 Toilet, Patient 1 60 60 Clinical Support Areas 1 20 20 1 20 20 1 20 20 1 100 100 1 50 50 Alcove, Linen Alcove, Sink and Contrast Storage Alcove, Crash Cart Clean Supply Soiled Holding Environmental Services/Housekeeping Closet 1 60 60 Staff and Administration Support Areas Office, General - 100 -Shared with Inpatient Conference Room - 200 -Shared with public/main waiting Lounge, Staff - 200 -Shared with Inpatient Lab/Blood Draw Registration & Waiting - - Shared with Imaging Intake & Waiting Blood Draw Stations 2 50 100 Recliners with one large enough for stretcher Toilet, Patient 1 60 60 Includes specimen pass-thru Shared Staff Workstation 1 100 100 4 positions Lab 1 400 400 HOSPITAL SUPPORT SERVICES Clinical Shared Nourishment Warming Kitchen 1 200 200 Dish Washing Room 1 80 80 Accessed from warming kitchen Dry Storage 1 100 100 Accessed from warming kitchen Trash Holding 1 10 10 Materials Management Receiving and Breakdown 1 200 Bulk Storage 1 100 Building Support Electrical Closet -Accounted for in tip-up factor Electrical Room -Accounted for in tip-up factor Telecom Room -Accounted for in tip-up factor HVAC -Accounted for in tip-up factor Total Net Area (DGSF): 14230 Tip-up Factor: 1.35 Circulation, mechanical, electrical, structure Total BGSF: 19211 36 2023 ― Volume 15.01 Research Journal
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.) Room / Space
Name
Space Consolidation / Notes
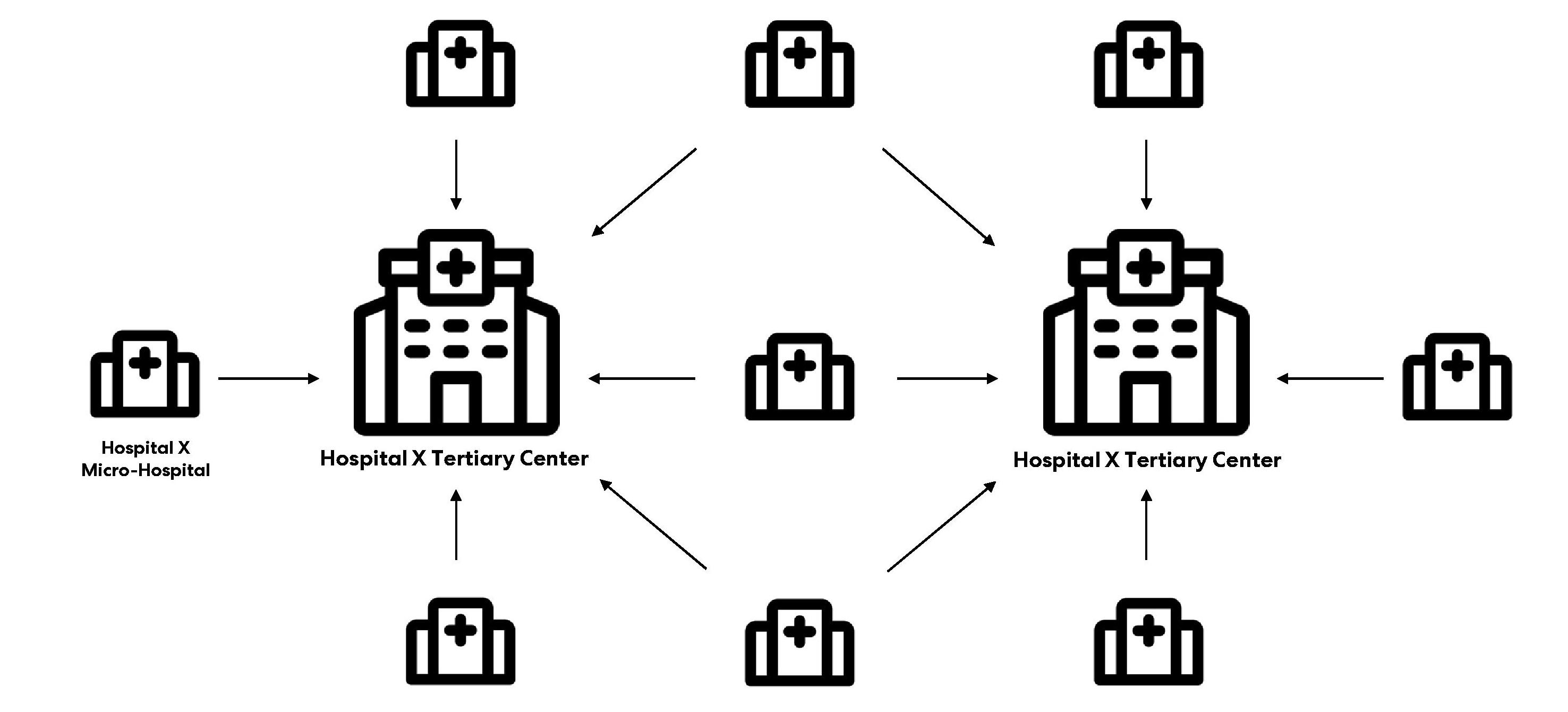
small-scale micro-hospital footprint is well-suited for integration in the New York City block, offering corner visibility, land efficiency, and the possibility to be sited in non-traditional neighborhood settings (Figure 12).
To understand micro-hospitals, it is important to define critical access hospitals (CAHs). Rural health disparities and barriers to healthcare access have been addressed through critical access hospitals (CAHs), which provide care to residents in rural communities. CAHs are designated by individual States based on strict criteria. Important criteria to be designated a CAH are to be located more than 35 miles from the nearest hospital, maintain no more than 25 beds for inpatient or swingbed services, maintain 24-hour emergency care services seven days a week, and maintain an annual average length of start of 96 hours or less for inpatient care, among other criteria.40 Operationally, micro-hospitals are very similar to critical access hospitals. CAHs are also similar in size to micro-hospitals, with micro-hospitals being on the smaller scale of CAHs. Federal and state regulatory standards for micro-hospitals have not been developed to the extent of CAHs.
Access gaps and medically underserved areas for pediatric populations are also present in urban settings. A hub-and-spoke model of care for micro-hospital development can provide care close to home in a
child’s neighborhood and provide access in areas with limited resources for pediatric care (Figure 13). Microhospitals should be planned as a network of facilities operating under the same hospital system as the nearest tertiary center.
From conference proceedings mentioned in Section 2, New York City healthcare real estate developers, AEC professionals, and healthcare facilities foresee microhospital development growth in New York City over the next decade. Provision of zoning and other regulations can also allow for micro-hospital operation at ground and first levels of buildings with mixed uses above, to maximize the square footage and offset high land costs. In areas with overall lower building heights and more residential settings, such as Upper Manhattan, a one or two-story micro-hospital would integrate well with the existing neighborhood fabric.
4.3 Recommendations: Architects as Advocates for Equity in Pediatric Spaces
Architects are active liaisons between governments, hospital systems, and developers to facilitate future visions and advocate for the spatial needs of children and their families. The regulatory environment around micro-hospitals is vague and inconsistent across federal,
Growing Pains 37
Figure 13: Hub-and-Spoke micro-hospital development model. Source: Author
state, and local levels. Certificate of Need laws pose additional barriers to micro-hospital implementation in several states.14 In the FGI Guidelines, there are design guideline sections for inpatient and outpatient hospitals that can be cross-referenced, but there is not a dedicated section for micro-hospitals. As microhospital development continues, specific FGI Guidelines addressing complexities of micro-hospital design should be considered.
There is potential for architects as space planners to push back on traditional facility operations models through the unique adjacencies that micro-hospitals can create. Micro-hospital models can challenge medical staff to rethink their current ways of practicing and collaborate with other team members to design more efficient workflows. Multisite practicing and telehealth infrastructure will be critical in tying pediatric microhospitals into the larger health systems.15,32 Based on interviews, the recommended project delivery model for micro-hospitals is design-build for its flexibility, interdisciplinary design team, and innovative framework. As micro-hospitals grow into parts of healthcare systems, it is important to create a unified identity with consistent branding throughout the primary campus hospital to the micro-hospitals to be easily recognizable. There is unique opportunity for micro-hospitals to be designed as part of the neighborhood fabric, integrated near local markets, homes, and familiar places to children. The pediatric micro-hospital should become an active participant in the community where it is sited, with a focus on psychosocially supportive spaces.41
5.0 Limitations and Future Studies
There were several limitations to the survey, case studies, and interviews. The qualitative survey conducted captured the pediatric experience and perspectives from various user groups. As such, there are inherent biases in the survey structure, order, and question wording that could have affected survey responses. The small participant population in child and adolescent responses resulted in an inconclusive analysis from the child and adolescent perspectives. Future studies must include representation from the actual patient populations being designed for. The case studies were limited to one architectural firm’s projects. The interview data was limited to the number of interviewees.
Future studies should include quantitative research on pediatric patients, their families, and clinicians in small versus large-scale hospital settings to evaluate measurable outcomes, such as pre- and post-occupancy evaluations for children’s hospitals and micro-hospitals. Additional incorporations for micro-hospitals, such as the need for psychosocially supportive spaces within pediatric hospitals, among others, require a broad disciplinary research approach.41
There is limited academic literature available on microhospitals because it is a new concept. Most microhospital data in this study came from white papers, news articles, and industry data. Future studies should include pre- and post-occupancy evaluations of micro-hospitals and literature review of academic research once it is available.
This research focused on pediatric care and microhospitals in urban settings. In addition, there is a need to validate pediatric micro-hospital hypotheses once there are physical prototypes in urban settings. Future studies should be conducted on the feasibility of pediatric micro-hospitals in rural settings.
There is minimal research on the effects of decentralized pediatric care in US contexts. There is also minimal research that compares regionalization versus decentralization of pediatric medicine as health care methods.15
Lastly, preliminary research was conducted on general pediatric patient populations who may be best suited for this type of model. More case studies are needed on specific pediatric patient populations who are best suited based on local hospital catchment area demographics.
6.0 Conclusions
Micro-hospitals are an emerging concept in the AEC and hospital industries. Investment in specialized microhospitals for pediatric populations may be a patientcentered, economic, and innovative solution to address the pediatric care crisis. New York City is a well-suited urban setting for a micro-hospital model to be integrated into existing healthcare infrastructures. Pediatric microhospital solutions may provide relief to overwhelmed tertiary pediatric hospitals by creating space in larger
38 2023 ― Volume 15.01 Research Journal
hospitals through relocation of lower acuity patients into micro-hospitals. An interdisciplinary design approach is necessary for successful implementation of pediatric micro-hospital care models. Micro-hospitals are an opportunity for architects to advocate for equity in pediatric spaces.
Acknowledgments
I would like to express my sincere gratitude to Kalpana Kuttaiah, Laura Morris, Ryan Ramsey, Tatiana Escobar, Dr. Than Huynh, Dr. Andrew Stadler, the New York City Studio, and the previous cohort of healthcare fellows for supporting this research. I would also like to thank every individual interviewed and every individual that shared their insights and touching experiences in the research survey. I am especially grateful for the support and opportunity provided by the E. Todd Wheeler Health Fellowship at Perkins&Will.
References
[1] The New York Times, (2022). “As Hospitals Close Children’s Units, Where Does That Leave Lachlan?” Retrieved on November 5, 2022 from https://www. nytimes.com/2022/10/11/health/pediatric-closureshospitals.html.
[2] VonAchen, P., et al, (2021). “Closure of Licensed Pediatric Beds in Health Care Markets Within Illinois.” Academic Pediatrics
[3] Liang, T., et al, (2022). “Pediatric emergency care in New York City during the COVID-19 pandemic shutdown and reopening periods.” Am J Emerg Med
[4] American Academy of Pediatrics, (2022). “Pediatric Health Care Organizations Call for National Response on RSV and Flu Surge.” Retrieved on January 3, 2023 from https://www.aap.org/en/news-room/news-releases/ aap/2022/pediatric-health-care-organizations-callfor-national-response-on-rsv-and-flu-surge/.
[5] Kushing, A., et al, (2021). “Availability of Pediatric Inpatient Services in the United States.” Pediatrics, Vol. 148, No. 1.
[6] Kushing, A., et al, (2020). “Trends in Regionalization of Emergency Care for Common Pediatric Conditions.” Pediatrics, Vol. 145, No. 4.
[7] Blumberg, R., (2006). “Design Issues in Hospitals, The Adolescent Client,” Environment and Behavior, Vol. 38, No. 3.
[8] Bock, E., et al (2021). “Literature Review: EvidenceBased Outcomes and Perceptions of the Built Environment in Pediatric Hospital Facilities,” Journal of Pediatric Nursing, Vol. 61, pp. 42-50.
[9] (2023) “What is Design-Build?” Design Build Institute of America.
[10] Pennsylvania Department of Health, (2022). Updated Micro-Hospital Guidance. Pennsylvania Department of Health.
[11] The Advisory Board, (2018). “How Micro-Hospitals Impact System Strategy,” Report, Retrieved on November 7, 2022 from https://www.advisory.com/Blog/2018/01/ micro-hospitals.
[12] The Advisory Board, (2018). “How to Know Whether a Micro-Hospital is the Right Investment,” Report, Retrieved on November 7, 2022 from https://www.advisory.com/ Blog/2018/09/micro-hospital.
[13] U.S. News & World Report, (2017). “Micro-Hospitals Provide Health Care Closer to Home,” Retrieved on September 8, 2022 from https://www.usnews.com/ news/healthcare-of-tomorrow/articles/2017-04-24/ micro-hospitals-offer-an-alternative-health-caremodel-for-local-communities.
[14] Industry Dive, (2018). “Health Systems Increasingly Think Small. At the Micro Level,” Retrieved on October 20, 2022 from https://www.healthcaredive.com/news/ health-systems-increasingly-think-small-at-the-microlevel/527235/.
[15] Lorch, S., et al (2010). “The Regionalization of Pediatric Health Care,” Pediatrics, Vol. 126, No. 6, pp. 1182-1190.
39 Growing Pains
[16] Gothamist, (2022). “Is NYC Running Out of Children’s Hospital Beds? State Officials Won’t Say,” Retrieved on January 4, 2023 from https://gothamist.com/news/ is-nyc-running-out-of-childrens-hospital-beds-stateofficials-wont-say.
[17] Frush, B., (2022). “Moral Distress Amid the Pediatric Behavioral Health Crisis: A Call to Action.” Pediatrics, Vol. 12, No. 8.
[18] Emerus, (2020). “What Are Micro-Hospitals?” Retrieved on October 2, 2022 from https://www.emerus. com/understand-what-are-micro-hospitals/.
[19] Sherman, S., et al (2011). “Quantifying the Relationship Among Hospital Design, Satisfaction, and Psychosocial Functioning in a Pediatric HematologyOncology Inpatient Unit,” Health Environments Research & Design Journal, Vol. 4, No. 4, pp. 34-59.
[20] Ray, K., et al, (2018). “Access to High PediatricReadiness Emergency Care in the United States.” J Pediatr.
[21] Giancotti, M., et al (2017). “Efficiency and Optimal Size of Hospitals: Results of A Systematic Search,” Plos One
[22] Ulrich, R., (1984). “View Through a Window May Influence Recovery from Surgery,” Science, Vol. 224, No. 4647, pp. 420-421.
[23} Sinclair, S., et al (2020). “Compassion in Pediatric Healthcare: A Scoping Review,” Journal of Pediatric Nursing, Vol. 51, pp. 57-66.
[24] McFarland, D., et al, (2017) “Does Hospital Size Affect Patient Satisfaction?” Quality Management in Healthcare, Vol. 26, No. 4.
[25] Paul, J., et al (2014). “Modeling the Benefits of Cross-Training to Address the Nursing Shortage,” Int. J. Production Economics, Vol. 150, pp. 83-95.
[26] Galuska, L., et al (2022). “Strategies to Stay: Role Enrichment Models for Retaining Millennial Nurses,” Nurse Admin Q, Vol. 47, No. 1, pp. 64-71.
[27] Hedges, A., et al (2019). “Effects of Cross-Training on Medical Teams’ Teamwork and Collaboration: Use of Simulation,” Pharmacy, Vol. 7, No. 13, pp. 1-10.
[28] Inman, R., et al (2005). “Cross-Training Hospital Nurses to Reduce Staffing Costs,” Health Care Manage Rev, Vol. 30, No. 2.
[29] Potaka, Osborne, L., Reducing OR Delays: Cross Training and Frontline Engagement Improves Patient Flow in a Tertiary Pediatric Hospital,” Journal of PeriAnasthesia Nursing, Vol. 32, No. 4, pp. e34.
[30] Krugman, S., et al, (2007). “Redefining the Community Pediatric Hospitalist: The Combined Pediatric ED/Inpatient Unit,” Pediatric Emergency Care, Vol 23, No. 1.
[31] Stefano, G., et al (2018). “The Micro-Hospital: 5G Telemedicine-Based Care,” Medical Science Monitor Basic Research, Vol. 24, pp. 103-104.
[32] Curfman, A., et al (2022). “Telehealth: Opportunities to Improve Access, Quality, and Cost in Pediatric Care,” Pediatrics, Vol. 149, No. 3, pp. 1-12.
[33] Fixr, (2022). “How Much Does it Cost to Build a Hospital?” Retrieved on February 15, 2023 from https:// www.fixr.com/costs/build-hospital.
[34] Statistica, (2022). “Average construction costs of general hospitals in the United States from 4th quarter 2021 to 3rd quarter 2022, by city” Retrieved on February 20, 2023 from https://www.statista.com/statistics/830405/ construction-costs-of-general-hospitals-in-us-cities/.
[35] U.S. Energy Information Administration (2012). “Energy Characteristics and Energy Consumed in Large Hospital Buildings in the United States in 2007” Commercial Buildings Energy Consumption Survey, Retrieved on February 7, 2023 from https://www.eia. gov/consumption/commercial/reports/2007/largehospital.php.
[36] Slosberg, M., et al (2018). “Transitioning to a New Facility: The Crucial Role of Employee Engagement,” Journal of Healthcare Management, Vol. 63, No. 1.
[37] Facilities Guidelines Institute, (2022). “FGI Guidelines for Design and Construction of Hospitals,” 2022 edition.
[38] Brown, K., et al, (2021).” Access to Optimal Emergency Care for Children.” Pediatrics, Vol. 147, No. 5.
[39] NYC Health + Hospitals, (2022). “Community Health Needs Assessment 2022,” Retrieved on February 18, 2023 Retrieved from https://hhinternet.blob.core.windows. net/uploads/2022/07/community-health-needsasssessment-2022.pdf.
40 2023 ― Volume 15.01 Research Journal
[40] Centers for Medicare and Medicaid Services, (2021). “Critical Access Hospitals,” Retrieved on January 4, 2023 from https://www.cms.gov/ Medicare/Provider-Enrollment-and-Certification/ CertificationandComplianc/CAHs.
[41] McLaughlan, R., (2018). “Psychosocially Supportive Design: The Case for Greater Attention to Social Space Within the Pediatric Hospital,” Health Environments Research & Design Journal, Vol. 11, No. 2, pp. 151-162.
41 Growing Pains
E-health & Tele-health:
Potential Impacts on Space in Hospitals in the United Kingdom
Hala ElKhorazaty, WELL AP, hala.elkhorazaty@perkinswill.com
Asif Din, PhD, RIBA, BREEAM AP, LEED® Green Associate™, LFA, asif.din@perkinswill.com
Mark Rowe, RIBA, MRIAI, AECB, mark.rowe@perkinswill.com
Abstract
This study was carried out during the 2020 COVID pandemic. It aimed to assess the potential benefits of tele-health in addressing the needs of patients with respiratory illnesses who were most vulnerable during the pandemic and require extra precaution to prevent their infection.
A proposed solution to tackling one of the hospital's many challenges during the pandemic was the practice of Electronic Health (E-health) with advances such as tele-health. Tele-health has been found to be effective in supporting patients who are engaged in self-care, improving quality of care, and reducing medical costs for the NHS. As well as relieving hospitals from significant pressure in providing care for minor health problems and the unnecessary admission of people with one or more long-term conditions.
This study uses data from two hospitals; Airedale NHS Foundation Trust that has a tele-medicine program established for the past 9 years and St George’s University Hospital London that has recently utilized tele-health to decrease patient admissions. These case studies assess the extent to which the reduction of centralized healthcare and the retention of main treatment services can provide better care for patients, reduce build budget, and allow enhanced staff facilities reducing staff fatigue and burnout on existing sites.
A comparison between the admitted patient care records between 2018 and 2020 demonstrates an overall reduction in hospital admissions for non-COVID related diseases. The Hospital Episode statistics (HES) identifies a reduction of length of stay using the data recorded from April 2020 to December 2020 compared to that of June 2018 to March 2019 through interventions of E-health services.
Finally, by reviewing the Provisional Monthly HES for Admitted Patient Care for long term patients with chronic respiratory illnesses (COPD), the study shows the impact in the length of the period of care (EPIORDER), and method of admission (ADMIMETH) recorded by the two hospitals.
Designers can contribute to the existing structure of the hospital and re-imagine a new hospital that can better benefit from the wider rollout of E-health & Tele-health. Through the identification of new practices that would benefit most from the application of E-health; the results show a potential 30% overall reduction of a hospital’s current real estate programme. A decrease in required space for outpatient consultations and reduce hospital beds.. Furthermore, by adding an additional 5% space to support the technology and infrastructure needed for the new functions, and an additional 5% to increase clinical staff productivity by providing better focus on their wellbeing and increasing respite areas. This results in a net reduction of 20% in floor area with an enhanced architectural programme to support this new technological and cultural shift.
Keywords: E-health, Tele-health, virtual healthcare, COVID-19, chronic respiratory illnesses
03
42 2023 ― Volume 15.01 Research Journal
1.0 Introduction
During the COVID-19 health crisis, healthcare systems were required to adjust the way they triage, evaluate, and care for patients using methods that do not rely on in-person services. In order to reduce patient surges on facilities as well as protect staff exposure to ill persons; new treatment approaches had to be adopted. These approaches safely preserve patients’ experience of care while maintaining a safe environment for essential workers in the NHS. Previous studies have shown that Tele-health services help provide necessary care to patients while minimizing the transmission risk of SARSCoV-2, the virus that causes COVID-19, to healthcare personnel (HCP) and patients.1
While the idea of remote healthcare or tele-health technology is not considered new, healthcare professionals typically use these approaches to be able to connect with patients in faraway regions. In situations where medical services are scarce, telehealth was considered the only viable option to support recent hospital activity and provide care for patients in a timely manner. The widespread effects of tele-health become evident during the peaks of the pandemic with demand for most of the population to stay home. This has directed the larger healthcare system towards a dynamic shift from an in-person care model to a more remote-based system of care.
Many studies have shown that, even before the spread of the COVID-19 pandemic, recent years have witnessed an increased interest in tele-health services.² Statistical evidence revealed an increased preference for telehealth systems by both healthcare professionals and patients when delivering acute, chronic, primary and specialty care.³ There are also some indications that tele-health can improve patient health outcomes.4
This study aims to address the effects of the adoption of the E-health system on the architectural programme and design of a hospital. It also addresses the need for a sustainable way of providing health care to an ageing population without the recourse of centralised care. As both patients and healthcare professionals are becoming more technology savvy, it would be appropriate to use this platform to expand healthcare provision. By understanding the aspects of care that E-health system could affect most, this study aims to explore the potential reduction of these aspects within
the architectural programme by creating more effective planning data that can accurately mirror the dynamic shift of healthcare to a home or remote based model of care. The aim is to sustain the provision of the essential services needed to the population and patients, whilst preserving the NHS staff from work fatigue and stress due to the surges of hospital visits as the demands for services continues to rise.⁵
2.0 Background
2.1 E-health and Tele-health
E-health defines a system in which Information Technology drives the flow of data from patients to healthcare workers. The concept of E-health systems can be traced back to the 1960s under multiple labels including “computers in healthcare”, “medical informatics”, “health informatics”, “tele-medicine” and “health tele-matics”. E-health was considered a “revolution.”6 Two main common notions emerge from all these labels; the first is “improving healthcare through the use of ICT” and the second is to seek to “create ambient intelligence for healthcare professionals”. The E-health system had the promise to deliver healthcare knowledge across multiple clinical boundaries and create “responsive healthcare tailored to the needs of the citizen.”⁶
The emergence of E-health conjures an association with tele-expertise and more specifically tele-medicine. Where one of the five key applications of tele-medicine was a focus on prevention, diagnosis and collaborative practice. 6,7,8 The main differentiator between telemedicine and E-health is that tele-medicine may place a larger emphasis on the application of certain IT technologies in the system of care referred to as Technology enhanced care systems (TECS). This can support new technological development for healthcare such as virtual e-hospital, tele-surgery, tele-conferencing, and remote electronic clinical consultation.6,7,8
E-health takes into consideration the wider perspective of sharing clinical information and services, supporting a wider range of patient care services without dependencies on specific technologies. Silber (2004)
E-health & Tele-health 43
suggests that outcomes of E-health can be used in multiple contexts including patient management and “electronic messaging between the hospital and other healthcare actors for communication of clinical and administrative data, and tele-medicine and second opinions, in any specialty.”6
Although E-health has had many definitions over the decades, and many authors have used it in its more general form defining healthcare services related to the internet, the definition that strikes the most interest in the context of this study is Eysenbach’s definition.
Eysenbach (2001) 9 viewed e-health as "a new way of working, an attitude, and a commitment for networked, global thinking, to improve healthcare locally, regionally, and worldwide by using information and communication technology". According to this definition, a system of care is not confined by any geographical boundaries and has the potential to create a more personalized system of care not central to the confines of a hospital but shared, ever evolving and enhances collaboration.
For the better progress of E-health services, Silber (2004)⁶ also defines a more collaborative approach stating that clinical staff would have the ability to “engage in informal networking with colleagues in other countries”6 an aspect that could support healthcare systems to prevent widespread diseases in the near future as well as collaborate more effectively on prevention methods. One of the common modalities of tele-health care is the CDC modality 2020, as shown in Table 1.
2.1.1 Modalities of Care Using Tele-health
Synchronous: This includes real-time telephone or live audio-video interaction typically with a patient using a smartphone, tablet, or computer. In some cases, peripheral medical equipment (e.g., digital stethoscopes, otoscopes, ultrasounds) can be used by another HCP (e.g., nurse, medical assistant) physically with the patient, while the consulting medical provider conducts a remote evaluation.
Asynchronous: This includes “store and forward” technology where messages, images, or data are collected at one point in time and interpreted or responded to later. Patient portals can facilitate this type of communication between provider and patient through secure messaging.
Remote patient monitoring: This allows direct transmission of a patient’s clinical measurements from a distance (may or may not be in real time) to their healthcare provider.
44 2023 ― Volume 15.01 Research Journal
USING TELE-HEALTH TO EXPAND ACCESS TO ESSENTIAL HEALTH SERVICES
DURING THE COVID-19 PANDEMIC. 2020 TELE-HEALTH SERVICES CAN BE USED TO
• Tele-health services can facilitate public health mitigation strategies during this pandemic by increasing social distancing. These services can be a safer option for HCP and patients by reducing potential infectious exposures. They can reduce the strain on healthcare systems by minimizing the surge of patient demand on facilities and reduce the use of PPE by healthcare providers.
• Maintaining continuity of care to the extent possible can avoid additional negative consequences from delayed preventive, chronic, or routine care. Remote access to healthcare services may increase participation for those who are medically or socially vulnerable or who do not have ready access to providers. Remote access can also help preserve the patient-provider relationship at times when an in-person visit is not practical or feasible.
• Screen patients who may have symptoms of COVID-19 and refer as appropriate
• Provide low-risk urgent care for non-COVID-19 conditions, identify those persons who may need additional medical consultation or assessment, and refer as appropriate
• Access primary care providers and specialists, including mental and behavioural health, for chronic health conditions and medication management
• Provide coaching and support for patients managing chronic health conditions, including weight management and nutrition counselling
• Participate in physical therapy, occupational therapy, and other modalities as a hybrid approach to in-person care for optimal health
• Monitor clinical signs of certain chronic medical conditions (e.g., blood pressure, blood glucose, other remote assessments)
• Engage in case management for patients who have difficulty accessing care (e.g., those who live in very rural settings, older adults, those with limited mobility)
• Follow up with patients after hospitalization
• Deliver advance care planning and counselling to patients and caregivers to document preferences if a life-threatening event or medical crisis occurs
• Provide non-emergent care to residents in long term care facilities
• Provide education and training for HCP through peerto-peer professional medical consultations (Inpatient or outpatient) that are not locally available, particularly in rural areas.
Table 1: CDC report: Using Tele-health to Expand Access to Essential Health Services during the COVID-19.
45 E-health & Tele-health
2.2 Financial Benefits of E-health
Healthcare systems worldwide face organisational and financial challenges due to increasing number of people with chronic conditions, increasing costs, and ageing population (NRC 2001).10 The continuous debate on whether healthcare systems will be financially sustainable in the future remains a constant concern. Although financial sustainability has often been referred to as “the ability of governments to pay” (WHO, 2009), nevertheless, financial sustainability also refers to the affordability of health services for everyone. Recent studies have shown that shifting the financial burden of health service to the population usually creates an even more problematic outcome. In the USA, at least 30% of Americans suffered from debt due to healthrelated services.11
E-health services offer a potential solution to these challenges through supporting patients who are engaged in self-care, improving quality of care, and reducing medical costs.12 In 2012 Uppsala in Sweden launched an E-health system that allowed patients to access their electronic health data online. Although the service received strong criticism from HCP at the time, the patient accessible electronic health records (PAEHRS) received great praise from patients and was received
very positively. Patients were allowed to freely access, comprehend, and engage in their health issues. The effects also showed that a vast majority appreciated more timely access to their results and a reduction of patient visits to HCP and a more content approach to their treatments.12 S. Barello (2015) 12 states that “an E-Health service like PAEHR is an important first step towards patient participation. The support of patient participation in their own care through PAEHR outweighs the potential harm”
In the United Kingdom, Technology Enabled Care Services (TECS)13 programme focuses on providing tactical tools and solutions to healthcare providers across the nation that can enable them to progress their healthcare facilities with new technology that supports both HCP and patients. Recently, TECS researchers showed substantial evidence for positive impact for shifting some care services to a Tele-health platform. TECS researchers found that E-health can reduce hospital admission by 45%, Accident and Emergency (A&E) attendance services by 60%, overall bed days by 50% and stay length in hospital among Chronic Obstructive Pulmonary Disease (COPD) patients by 9% (NHS Official, TECS Case study 02, Airedale Hospital).14
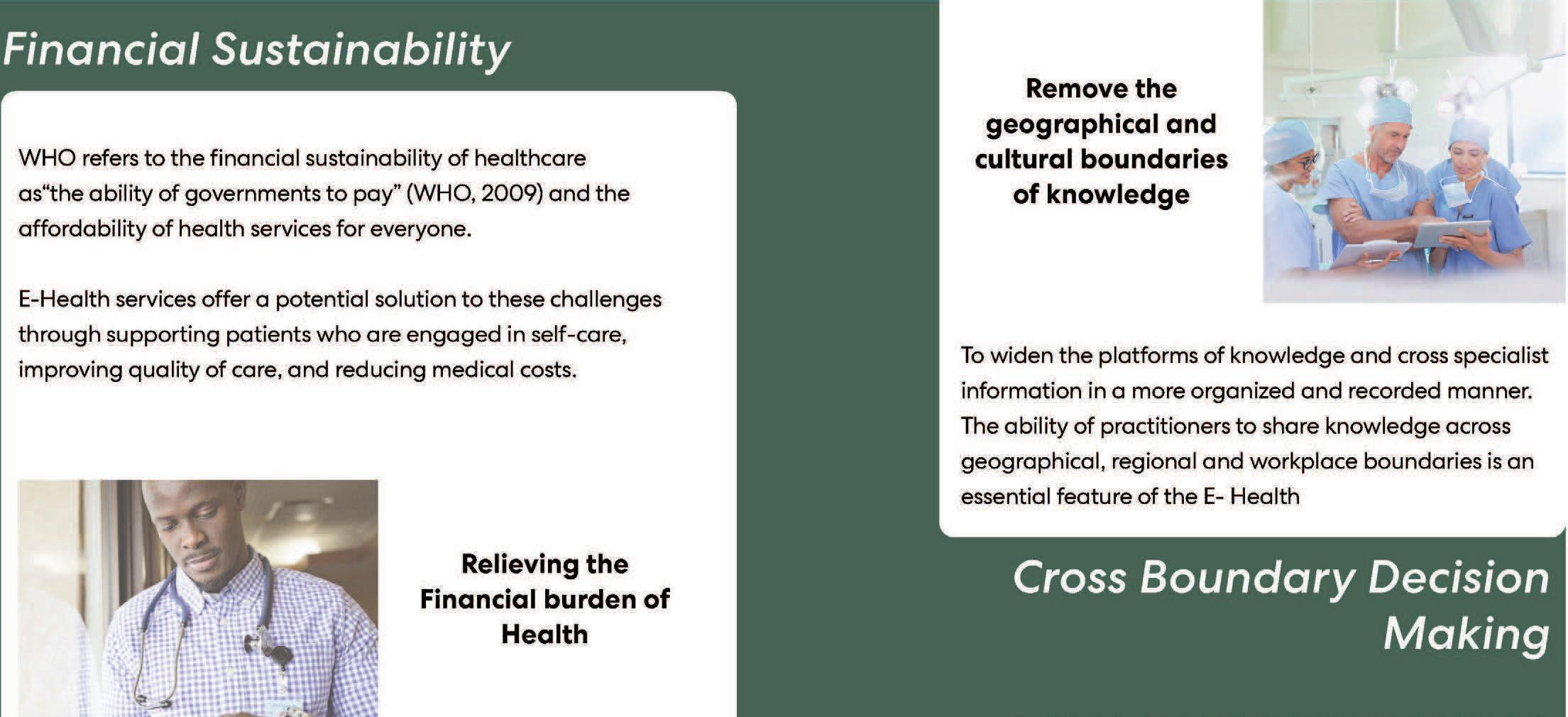
46 2023 ― Volume 15.01 Research Journal
Figure 1: Shows two main factors affecting the need for E-health.
2.3 Cross-Boundary Decision Making
Anya (2012)15 explores recent concepts in the “network sociality” which generated a remarkable shift in the way people access information and base their decisions15. These recent advances create a new perspective of information exchange or a “flat world” (Friedman, 2005).15 This has led to professionals from all sectors to increase collaboration and leverage collective intelligence, harnessing expert opinion across organisational, regional and workgroup boundaries for better decision support.16
This shift provoked designers to re-think work environments and re-imaging the future “ways of working.” 17,18,19,20 Healthcare being at the forefront of this as the basis of exchange of knowledge is in the form of “the second opinion” is considered a necessity in practice.21 In healthcare systems, care providers engage in “Problem based” “conversational encounters”22 between clinicians using clinical based research, clinical reviews and published administrative guidelines, creating a team-based approach to reviewing the case in hand that results in a care plan and workflow that typically engages in referrals to other care specialist. This can result in multiple decision support activities that are interactive and may incur in an informal manner.23
E-health has the potential to widen the platforms of knowledge and cross specialist information in a more organized and recorded manner. The ability of practitioners to share knowledge across geographical, regional and workplace boundaries is an essential feature of the E-health.15 This can be adapted and interpreted separately within the user-based context of work and region. E-health can support local decision making based on a wider and more timely form of information flow across the globe.
2.4 User-Centered Approach to Healthcare
In 2004 Moody and colleagues (2004) 24 addressed the acceptance and preferences of nurses when asked about their experience with E-health systems. The results showed positive attitudes towards the E-health system and a large percentage of nurses saw a positive impact
of E-health directly affecting patient care. “EHR use was more of a help than hindrance to care” was reported by 81% of the respondents. Furthermore, 75% of the nurses in the study thought EHR had improved documentation, while 64% indicated they believed the EHR system had not decreased the nursing workload. In general, nurses thought that in time, the EHR system would have a positive effect on improving patient care.24
A review of studies conducted over the period 1991-2001 by van der Meijden and colleagues (2003) 25 revealed a relatively high user satisfaction with the patient care information systems, 25 However, some studies have indicated some limitation in the patient care information systems. Darbyshire (2004) 26 recorded fewer positive experiences with the application of the EHR. In his study, nurses recorded increased in “digital disappointment rather than electronic efficiencies” in using the system for research purposes.26
3.0 Methodology
This study uses data from two hospitals; Airedale NHS Foundation Trust that has a tele-medicine program established for the past 9 years and St George’s University Hospital London that has recently utilized tele-health to decrease patient admissions. A comparison between the admitted patient care records between 2018 and 2020 demonstrates an overall reduction in hospital admissions for non-COVID related diseases. The HES (Hospital Episode statistics) identified a reduction of length of stay using the data recorded from April 2020 to December 2020 compared to that of June 2018 to March 2019 through interventions of E-health services.
By reviewing the Provisional Monthly HES for Admitted Patient Care for long term patients with chronic respiratory illnesses (COPD), the study shows the impact in the length of the period of care (EPIORDER), and method of admission (ADMIMETH) recorded by the two hospitals. A limitation to this study was that the study period was short (8 months) and largely around a single chronic disease, COPD. This would need a longer period of study in multiple areas of long term or frequent use of hospital beds.
47 E-health & Tele-health
4.0
Assessment of Architectural Needs
To present a comprehensive approach to the spatial and infra-structural needs and requirements of E-health systems in the architectural programmes of hospitals, Mukhiya (2019) 27 reviewed the flow of information systems across the clinical and patients’ interactions with the system is required.
Figure 2 illustrates the links and user systems of E-health connected to the central cloud “internet backbone” that is supported by an increase in allowance for a better equipped data centre within the confines of the hospital.
The content types created by E-health system can be outlined as the following: Data (i.e. in the form of files, e.g. a word document, images information, deferred transmission of sampled information such as ECG and video etc.). Video (e.g. in the form of live casting, and more generally, all real time data streams obtained from real time multidimensional sampled signals). 27 Audio (including speech, ECG, and more generally, all
real time data obtained from real time single dimension sampled signals). Image (i.e. a specialist form of data file generally of large size, e.g. high-resolution digital photograph), deferred ECG, deferred video, etc. (DTR/E-HEALTH-0002).27
Planning E-Health strategies for healthcare providers or a nationwide healthcare system within the architectural framework is one of the most critical aspects when starting programmes or initiatives for E-health and tele-medicine implementation. When reviewing a recent project designed by Perkins&Will we can use the structure as a basis of design for a dynamic and progressive institute for E-health services. Nicklaus Children’s Tele-health Center in Miami, Florida added a Tele-health services wing to accommodate the increase in demand for tele-health services as well as facilitate the hospitals outreach programme to service patients in remote regions where access to advanced medical advice is scarce.
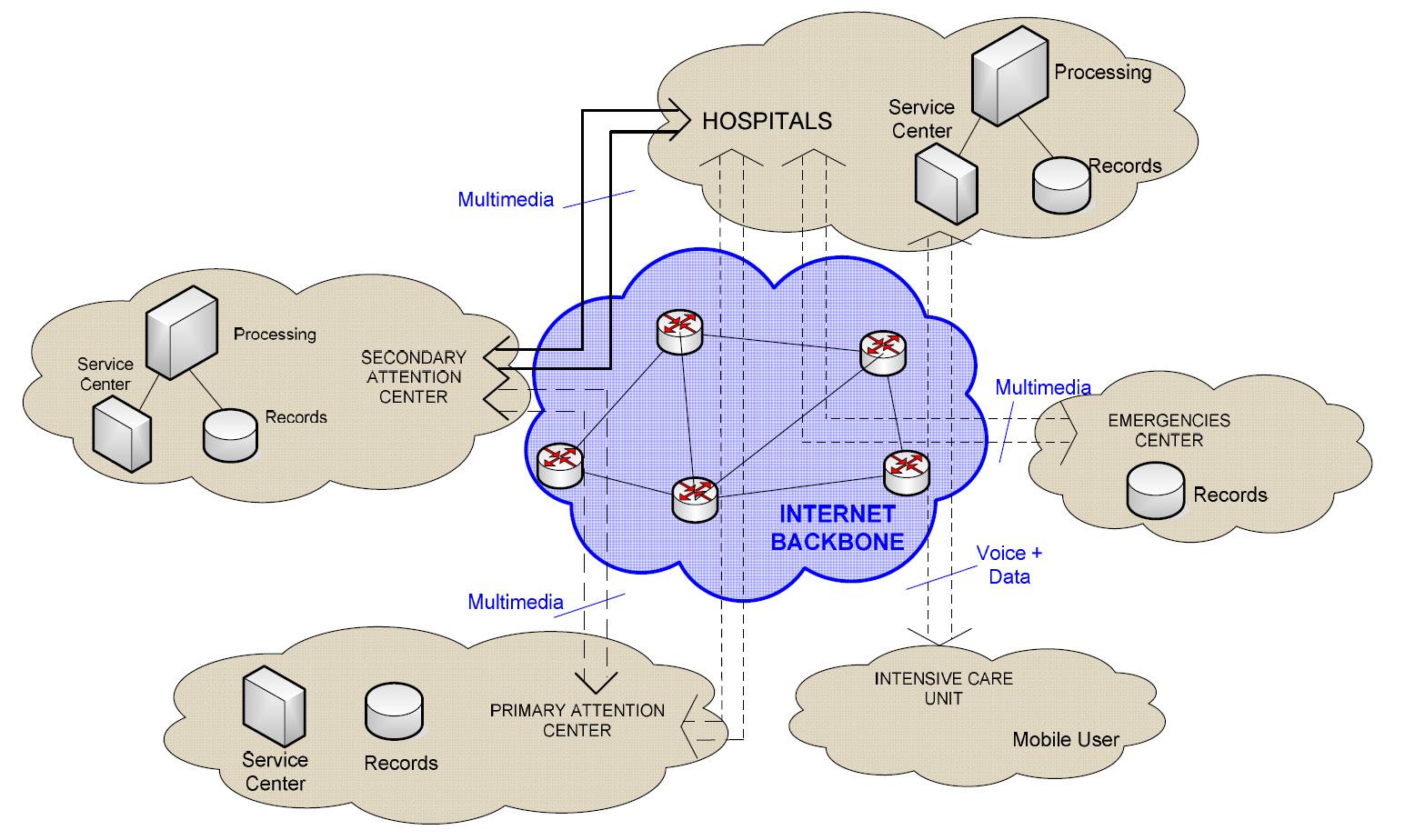
48 2023 ― Volume 15.01 Research Journal
Figure 2: Illustrating links and users to the E-health system. Source: ETSI TR 102 764 V1.1.1 (2009-02) technical report.
The Figure 3 shows a view inside one of the individual consulting rooms at the tele-health center, conveying the decreased spatial needs of the system when considering more routine and traditional patient consultation rooms. In order to sensitize the work environment that has the greatest potential to be affected by the new E-health systems, working practices must be evaluated as a fundamental part of this study. The identification of working practices and systems that have the potential to rely almost entirely on E-health services is still challenging. Recent studies have shown the potential effects of adapting the E-health model on certain areas of the care practice. When reviewing clinical practices, it is important to take into consideration human views and interaction with the system. Clinicians view themselves as “experts” in their fields, being aware of the most recent research and having the most local based “tactics,” they
may not necessarily believe in a “rule-based” computers to make major recommendations. 28 Therefore, when planning out an E-health system, it is important to maintain a partial traditional view in the working practice, allowing clinicians the freedom to address some of the less common cases and review them in a face-toface context to assess the situation more accurately. This can result in a percentage of every practice having a structured E-health system with a tele-medicine center to be utilized more regularly, decreasing the pressure and surges of patients entering hospitals with common issues and allowing more space and time for clinicians to review the less common illnesses. This reduction in consultation space can allow the facility to expand on collaborative, team based working environments for clinicians to review cases together in a less siloed manner.

49 E-health & Tele-health
Figure 3: Nicklaus Children’s Tele-health Center, Miami, Florida Photo looking inside the individual consulting rooms at the Tele-health Center.
5.0 Evidence Based Approach
5.1 Analysis
Statistical data show the effectiveness of an elaborate E-health system on patients and HCP. The new telehealth system became a main channel connecting patients to their care services in an effective and timely manner. HCPs will need time to adjust as well to the new system, but the longer-term effects presented in the Ariedale case study prove the positive implications of the system and its widespread usage to cover more patients remotely than a typical Trust.
A recent study launched by the NHS to investigate the potential outcomes of TECS14 has been the basis of some post analysis assumptions, the study reviewed the activity in Airedale NHS foundation trust and showed the results of utilizing a secured two- or multi-way system to contact study focused its results to address the needs of patients with Chronic Obstructive Pulmonary Disease (COPD) a lung disease that was considered one of the “at risk” cases during COVID. This presented a higher motivation to fully utilize the service and can allow a healthier base to study the effects of implementing a widespread E-health system for healthcare in a post covid world. The results showed (Figure 4) that at home patients with COPD had a 45% reduction in hospital admissions, 60% reduction in A&E attendances, 50% reduction in overall bed days and 9% reduction in length of stay. Nursing and residential care home results show 35% reduction in hospital admissions, 59% reduction in total use of bed days and 53% reduction of use of A&E.14
For example, a comparison using data from public NHSx datasets was also assessed for St. George University Hospital for the two period pre and post applying the E-health in the hospital namely 2018 and 2020. 29 The comparison showed a reduction in hospital admissions by at least 4% with a reduction of 31% in mean waiting time. At contrast, the average bed case increased by 8% indicating that only serious cases are admitted to the hospital. This was accompanied with The HES (Hospital Episode statistics)30,31 was also used to support this study (Figure 5), identifying a reduction of length of stay in hospital beds using the data recorded from April 2020 to December 2020 compared to that of June 2018 to March 2019 through interventions of E-health services.

Finally, the assessment of HES29 datasets as well as the (EPIORDER), and method of admission (ADMIMETH) recorded by the two hospitals; provide an indication of a decrease in the required space needed for outpatient consultation, a decrease in need of Hospital beds due to the reduced days of stay and a more efficient A&E ward that can accommodate emergency interventions in a timely manner without and protecting the NHS staff from any additional stress factors.

5.2 Assessment
By assessing the decrease in average hospital visits for St. Georges during the year 2020 (Figure 6) we can equate a decreased need of the current outpatient and diagnostic programme by 4% when studying COPD
Figure 4: Analysis outcome from NHS TECS study for COPD patients.
50 2023 ― Volume 15.01 Research Journal
Figure 5: Analysis outcome HES datasets 2018 - 2020 for COPD patients.
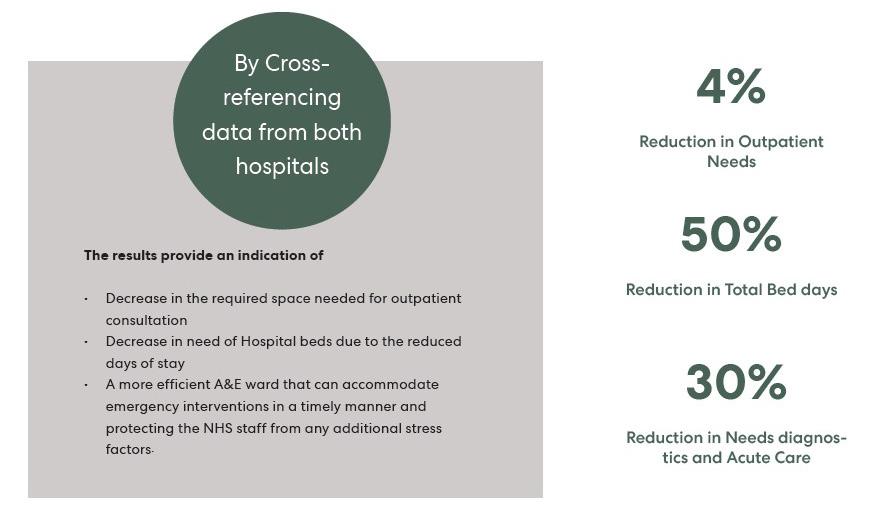
patients. A decrease in number of total bed stays by 50%. This allows them to cross reference the data taken from Airedale’s long-term E-health plan which shows an overall reduction of space needed for diagnostics and acute care by 30%.
Through the identification of new practices that would benefit most from the application of E-health; the results show a potential 30% overall reduction of a hospital’s current real estate programme. Furthermore, by adding an additional 5% space to support the technology and infrastructure needed for the new functions, and an additional 5% to increase clinical staff productivity by providing better focus on their wellbeing and increasing respite areas. This results in a net reduction of 20% in floor area with an enhanced architectural programme to support this new technological and cultural shift.
6.0 The New Operational Framework
In this section we have addressed the more holistic effects of E-health on the hospital operational, governance and real estate programme with an emphasis on the flexibility and adaptability of the design.
6.1 Project Governance
An effective E-health system is the starting point that can essentially prepare the hospital and lead the way to a more effective Smart healthcare system. E-health allows the potential spread of the hospital functions to multiple decentralized units. This allows a larger focus of the services to support a patient centric approach. This new decentralized system can better allow the flow of information data sharing with other contributors to support this system and new way of working.
This new system would require a new and adaptable governance structure at both the “integration Joint Board” and the “NHS Board” level that can provide assurance around the new way of working and extends support of front-line decision making.33 This new way of working would NHS “Long Term Plan” published in 2019 that addresses the need for a wider outreach programme without exhausting the NHS resources.
Other factors that need to be addressed would be managerial support for financial governance, service sustainability and a long-term view, staff governance and service planning. Factors directly affecting staff support should cover triage, clinical assessment and patient clerking, senior medical review, diagnostics and
51 E-health & Tele-health
Figure 6: Assessment outcome.
prescribing, care and support and review including the daily ward round or multidisciplinary team meeting as well as clear accountability for preventing and responding to risks, adverse events and performance reporting and a supportive culture for innovation that allows testing, adaptation, and development.
6.2 Flexibility and Sustainability
Real estate flexibility has been a main topic of discussion for many reasons, it allows future proofing of a site, creates a more adaptable space, and has a great impact on sustainability. As the NHS is continuously renovating many existing hospital trusts, future flexibility has become eminent to ensure the success of the existing and new hospitals.
E-health can support this need by allowing the trust to be able to serve a larger span of patients without any transportation needs, this enhances waiting times as mentioned earlier, with a reduction in waiting times by 31% but more importantly; reduces patient travel to the hospital without affecting the Trust’s catchment area.42
As for the built real estate programme, a 20-50% reduction on out-patient facilities would allow more floor space to become an adaptable/ flexible shell surrounding the hospital. This flexible space can be utilized in many ways including community spaces, educational pavilions and potential crisis relief areas that would not affect the hospitals core services.
As the NHS aims of creating a zero-carbon estate.43 thicker insulation and building fabric upgrades can be accommodated within existing buildings through reduced demand of facilities. This has the potential to reduce conditioning loads by 90% through the adoption of Passivhaus methodologies.44 New buildings could use the enhanced building specification which would increase the cost of buildings in the region of 10%, this would be more than compensated in the reduction in the overall floorplate required.41
The zero-carbon roadmap requires a range of different aspects and factors to be considered. E-health must be seen as an enabler to use the budgets which would have been traditionally spent within the hospital estate. These can be reinvested in research and development to achieve zero carbon hospitals. Given long real estate timescales.
6.3 Hospital Operations
When addressing the effects of an E-health system on the hospital operations, local governments are usually the main sponsors. They are deeply involved in influencing the objectives and outcomes of the system and direct the programme to embed effectively toward a smarter application within the hospital operations framework. Hospital operators play a crucial role in ensuring the effectiveness of the new functions as well as leading the staff through the significant transformation required. Hospital operators have effective foresight and experience in how the hospitals may operate in the future due to their strong connection to the role and functions of the existing hospital.
The following are some guidelines that can be highly effective in assimilating hospital operators to their new roles:
1. Support the Vision for the new hospital and its connection to a smart and sustainable eco-system. Rather than accepting a new programme and way of work, hospital operators can be selective of the services that would best affect the needs of the hospital the operators can start by identifying the diagnostic and treatment services that other entities cannot provide, and then determine how their hospital can efficiently deliver those services with a high level of quality.
2. Identify and Define “Smart Use Cases” by basing the assumptions in place operations and needs of the existing hospital.
3. Enhance the innovative environment by continually engaging with staff to understand patient needs, hospital operators can continuously affect the innovative solutions to adapt in a way that improves patient outcomes.
4. Invest in Staff by adding continuous education programmes and allowing innovative and new ideas to directly affect the flexible spaces within the hospital. Most clinical staff do not have the strong design language to support change in their environment, but by supporting them with new ways to communicate their needs, the hospital operations will progress effectively.
52 2023 ― Volume 15.01 Research Journal
5. Set up similar collaborations with government agencies, opinion leaders, and industry unions to encourage the staff to think about healthcare delivery in broader terms.
6.4 Impact
E-health systems have the potential to curate an entirely different experience for the patient, from their ability to receive care from the comfort of their homes or wherever they may need, as well as better accommodate their need.
The effects of E-health contribute to lower numbers of patients receiving care in the hospital building itself allowing a better and more curated experience for those in need of services in the hospital.
HCPs can accommodate and ease patient stress by connecting with their patients from the moment they are in need of care to the moment they are able to meet with them and have the needed face to face interaction for tests and diagnostics. This relieves patient stress and answers their needs more effectively. E-health also allows patients to freely access their medical case and history via an app or other online user-friendly tools.
To bring this to life, below is a vision, a description of a day in the life of a patient receiving care in the hospital building:
1. Before treatment: patients have access to remote sensing devices that can record blood pressure levels in real time. The device is connected to a network that uploads patient data to communicate with staff, they can then support the patient remotely in the case of emergency or refer the patient to a specialist that can better support his/her case.
2. Upon arrival: the patient verifies his/her identity with an RFID card that is connected the patient data. The IT system can then direct the patient where to go and all information needed to help the patient conform with the needed specialist.
3. After administering treatment: Patient data is then uploaded to the cloud platform, allowing real time assessment by the patient’s physician. A report is then created where the patient can easily access remotely to see the results.
4. Follow up: the patient can see their online test results and via an app, the patient will be sent reminders about medication adherence and notifications about upcoming care, rehabilitation services, and insurance matters. The hospital also uses a tele-health platform to regularly assess the progress of the patient’s recovery and provide consultations as needed.42,43 A couple ground-breaking examples of progressive E-health and smart systems
Some examples are Samsung medical centre in South Korea and the Cleveland Clinic Abu Dhabi (CCAD) where digital apps are used as part of the treatment to enhance the patient experience before admission. Patients can use the apps to communicate with the medical staff and finish all admission procedures. During their hospital stay, patients can use smart pads to access detailed clinical information and daily treatment plans, and to order food and other services. At discharge, CCAD uses mobile apps to send drug prescriptions to patients’ local pharmacies and to allow patients to confirm discharge times and check their bills.
Another application of E-health has been used to support diagnostics, E-health creates a large, connected platform creating a deep neural network. This potential arises from data analytics of this platform that could support early diagnostics and interventions. Statistical analysis of worldwide reports can support the progress of research in healthcare and medicine. Data analytics can also include procedure times, patient transports and hospital bed needs, resulting in a more lean and effective system, this can also reduce idle time between procedures.33,34
6.5 Potential Re-structure of Real Estate Programme
E-health requires a smart ecosystem to thrive and be fully utilized. Application of E-health has the potential to reduce the current real estate programme by an overall 20% by creating a more efficient and flexible hospital design. The results from analysing the data recovered from the NHS TECS programme shows a lower need of hospital beds, outpatient diagnostics and smaller more efficient A&E service centre. This can decrease real estate programme by 30%, but for the additional services needed to accommodate the smart infrastructure, the
53 E-health & Tele-health

tele-health unit (5% additional) and a larger focus on respite for staff (5% additional). The total reduction needed is 30% with 10% additional services. Further research is needed to investigate the potential effects on each department of care and how they could best benefit from the services provided.
The NHS is already on the path of developing the healthcare system, with the government investing in multiple new hospitals as well as re-furbishing exiting hospital trusts, a new vision must be directed to design and build a more effective healthcare system. This includes:
- Create an overarching vision: Rather than the focus on building large centralized systems of care, a new guidance needs to be administered that can support the new decentralized vision, with a greater emphasis on the IT infrastructure of the new institutions that can support future innovations. This enables stakeholders
to have a more effective role in envisioning the new system of care.
- Launch a more evolved platform to integrate care services: HCPs must be capable of sharing the appropriate data either operational or functional on a larger platform that supports their needs. We have seen a large progress in some trusts taking initiatives to create their own E-health systems, but a larger connection is needed between all facilities to inform HCPs of the better ways of working.
- The Smart healthcare Service Ecosystem: healthcare like any operational system must be viewed in the lens of a smart adaptable ecosystem. This requires a series of supporting mechanisms to ensure effective information dissemination. This can also help align stakeholders with a more united vision.
54 2023 ― Volume 15.01 Research Journal
Figure 7: Importance of respite areas for staff to relieve occupational stress.
6.6 Effects on Staff
The increasing number of care services needed has exhausted the NHS and has created an intense and stressful experience for all HCPs. Although healthcare is usually considered an intense experience for all occupants, patients and families, staff experience major psychological and physical effects during diagnostic procedures, caregiving, and care receiving.35
Multiple advocates on sustainable design have addressed this matter including the Green Guide for Health Care recommend that designers of healthcare facilities provide "places of respite" where occupants of the facility may go to recharge and refocus. WELL is also piloting a new study that focuses on all occupants within the healthcare facility, leading designers to create better physical aspects for staff including studies on daylight, rest, and psychological wellbeing.
E-health has the potential to support this on an even more effective level, as discussed earlier, some effects can lead to a more flexible environment where staff can easily adapt different spaces to accommodate different procedures. This will allow more efficient programming of space and free additional space for staff support and collaboration.
Lower numbers of patients receiving care in the hospital will allow staff to be able to focus better on the patient cases that require hospital visits. The flexible spaces can support teamwork when more than one specialist is involved in diagnostics and treatments as well as create a more effective training/learning experience.36
Respite areas can also be accommodated more comfortably and in better positions in the hospital grounds where the staff can get better exposure to natural daylight and quieter rest areas away from main circulation spaces. Well-designed and programmed places of respite are crucial in "defining a supportive, high performance healing environment with proven effects on patient, family, physician, and staff well-being and improved clinical outcomes."37
7.0 Conclusion
Integrating E-health and smart building solutions within the hospital system must be seen in a holistic, smart, and interdisciplinary manner. The innovations mentioned in this research do not require sole focus on smart IT solutions, rather, it is a holistic, deeply embedded process that requires engagement and active participation of
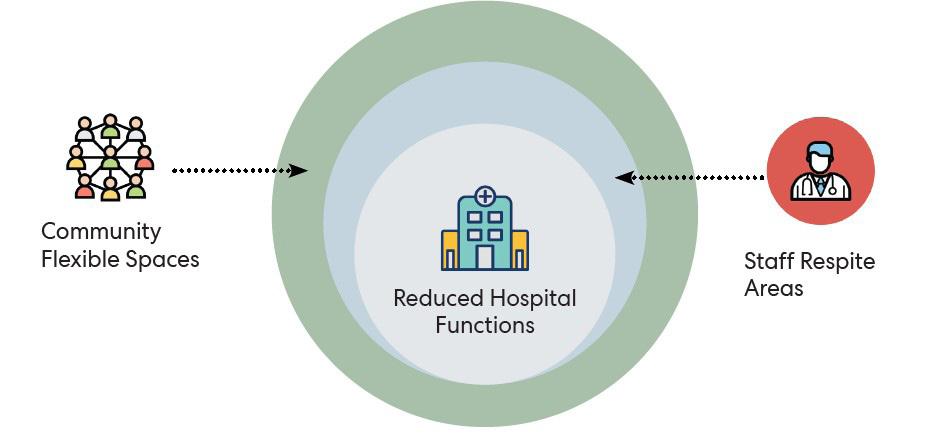
55 E-health & Tele-health
Figure 8: Layering effect of the flexible buffer space around the hospitals and its possibilities.
all HCPs and the community within the framework as well as ongoing collaboration to fully utilize E-health. Problems can be detected rapidly, and solutions can be studied, piloted, and rolled out more effectively. This way E-health can support clinical processes, quality of care, and patient experience keep improving on a continuing basis, yet costs are kept under control.
A few direct benefits for the NHS include the reduction of real estate programmes with maintaining the care services and increasing the number of patients receiving care by one trust, as well as the smart solutions that can be implemented in the hospital to support both staff and patient.
The reduced real estate programme can be looked at as an opportunity to create a flexible layer of space surrounding the hospital. This space can be curated and flexibly change to support the needs of staff, change into an isolated location for pandemic/ natural disaster relief, serve educational programmes, engage the community, and ultimately create a more positive experience for the society.
Potential outcomes of the design that can be further investigated (Figure 8).
• 20% Reduction of conditioned area specifically for outpatient consultations and reduce hospital beds.
• 5% technology hub that can enhance the hospital functions and service the tele-health centre.
• 5% increased staff respite areas.
• Reduction in new build cost with 30% reduction in programme.
• Supports retrofit more by using more space in a loose fit arrangement for a variety of needs.
• Reduction in patient travelling time, and congestion parking, time saved.
• Creation of flexible buffer space that is mothballed for emergencies.
• Ability to slim down deep plans to allow more daylight and increase recovery times.
• Allow more use of buffer spaces to modify climate rather than expensive retrofit with super insulation.
• Reduce burnout and occupational stresses as an outcome of the already congested hospitals.
• Work from home options for HCPs to reduce occupational context.
NHS studies show promising growth indications to its digital services, but the importance is implementing strong vision and planning initiatives that can foresee the larger effects on the community. Designers have a strong role in this, it is no longer sufficient to have a fast design response when procurement takes more time to implement than the need of the design solution. We are in a time that is shifting rapidly to a smart online platform; therefore, design should reflect the ability to change rapidly as well as an enhanced degree of flexibility within the healthcare system. In conclusion an eye must be kept on the holistic progress of the built design and E-health platforms for, without proper investment and vision, the danger is that expectations and reality may never meet.
References
[1] Ronnie, J., Using Telehealth to Expand Access to Essential Health Services during the COVID-19 Pandemic.
[2] Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with tele-health videoconferencing as a mode of service delivery in managing patients’ health. PloS One. 2019;14(8). https:// pubmed.ncbi.nlm.nih.gov/31469865/external icon
[3] Bashshur, R., Doarn, C.R., Frenk, J.M., Kvedar, J.C. and Woolliscroft, J.O., 2020. Telemedicine and the COVID-19 pandemic, lessons for the future.
[4] Hall, L.H., Johnson, J., Watt, I., Tsipa, A. and O’Connor, D.B., 2016. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PloS one, 11(7), p.e0159015.
[5] Martins, C., Godycki-Cwirko, M., Heleno, B. and Brodersen, J., 2019. Quaternary prevention: an evidencebased concept aiming to protect patients from medical harm. The British Journal of General Practice, 69(689), p.614.
[6] Kind, T. and Silber, T.J., 2004. Ethical issues in pediatric e-health. Clinical pediatrics, 43(7), pp.593-599.
[7] Perednia, D.A. and Allen, A., 1995. Telemedicine technology and clinical applications. JAMA, 273(6), pp.483-488.
56 2023 ― Volume 15.01 Research Journal
[8] Househ, M., Kushniruk, A., Maclure, M., Carleton, B. and Cloutier, D., 2009. A case study examining the impacts of conferencing technologies in distributed healthcare groups.
[9] Eysenbach, G., 2001. What is e-health. Journal of Medical Internet Research, 3(2), p.e20.
[10] Lutz, W., Sanderson, W. and Scherbov, S., 2001. The end of world population growth. Nature, 412(6846), pp.543-545.
[11] Mutchler, J.E., Burr, J.A., Massagli, M.P. and Pienta, A., 1999. Work transitions and health in later life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 54(5), pp.S252-S261.
[12] Serena Barello, Stefano Triberti, Guendalina Graffigna, Chiara Libreri, Silvia Serino, Judith Hibbard, Giuseppe Riva Front Psychol. 2015; 6: 2013. Published online 2016 Jan 8. doi: 10.3389/fpsyg.2015.02013
PMCID: PMC4705444
[13] Hamblin, K., 2020. Technology and social care in a digital world: challenges and opportunities in the UK. Journal of Enabling Technologies.
[14] England, N.H.S., TECS CASE STUDY 002: Using Telemedicine to reduce hospital admissions [Internet]. London: England NHS; 2014 [updated 2014 Dec; cited 2020 Mar 12].
[15] Anya, O., 2012. Practice-centred e-health system design for cross-boundary clinical decision support (Doctoral dissertation, University of Liverpool).
[16] Brézillon, P. and Araujo, R., 2005. Reinforcing shared context to improve collaboration. Revue des Sciences et Technologies de l'Information-Série RIA: Revue d'Intelligence Artificielle, 19(3), pp.537-556.
[17] Sellen, A. J., Murphy, R. and Shaw, K. (2002) How knowledge workers use the Web, CHI'2002, 4(1), ACM Press, 227-234.
[18] Nof, S. (2003) Design of Effective E-Work: Review of Models, Tools, and Emerging Challenges, Production Planning and Control, 14(8), 681-703.
[19] Fernando, T. (ed.) (2003) A Strategic Roadmap for Defining Distributed Engineering Workspaces of the Future, IST-2001-38346, Report on Future Workspaces Challenges, European Commission, Brussels.
[20] Schaffers, H., Brodt, T., Pallot, M. and Prinz, W. (eds.) 2006, The Future Workspace: Perspectives on Mobile and Collaborative Working, The MOSAIC Consortium, The Netherlands, Telematica Instituut
[21] Abidi, S. S. R. (2006) Healthcare Knowledge Sharing: Purpose, Practices and Prospects. In Healthcare Knowledge Management: Issues, Advances and Successes, In R. K. Bali and A. Dwivedi (eds.), Springer, 65-86.
[22] Vyas, D. (2011) Designing for Awareness: An Experience focused HCI Perspective, PhD Dissertation, University of Twente, The Netherlands.
[23] Whittaker, S., Frohlich, D. and Daly-Jones, O. (1994) Informal Workplace Communication: What is it like and how might we support it? Human Factors in Computing Systems, Boston, ACM Press, 131-137.
[24] Moody, L.E., Slocumb, E., Berg, B. and Jackson, D., 2004. Electronic health records documentation in nursing: nurses' perceptions, attitudes, and preferences. CIN: Computers, Informatics, Nursing, 22(6), pp.337-344.
[25] Van Der Meijden, M.J., Tange, H.J., Troost, J. and Hasman, A., 2003. Determinants of success of inpatient clinical information systems: a literature review. Journal of the American Medical Informatics Association, 10(3), pp.235-243.
[26] Darbyshire, P., 2004. ‘Rage against the machine?’: nurses’ and midwives’ experiences of using Computerized Patient Information Systems for clinical information. Journal of Clinical Nursing, 13(1), pp.17-25.
[27] Mukhiya, S.K., Rabbi, F., Pun, K.I. and Lamo, Y., 2019, May. An architectural design for self-reporting e-health systems. In 2019 IEEE/ACM 1st International Workshop on Software Engineering for Healthcare (SEH) (pp. 1-8). IEEE.
[28] Greenes, R.A., 2007. A brief history of clinical decision support: technical, social, cultural, economic, and governmental perspectives. In Clinical Decision Support (pp. 31-77). Academic Press, p. xiii.
[29] Data set, Part of NHS Outcomes Framework Indicators - December 2020 Supplementary Release 4b Patient experience of hospital care
[30] Data set, Publication, Part of Hospital Admitted Patient Care ActivityHospital Admitted Patient Care Activity 2018-19
57 E-health & Tele-health
[31] Data set, Publication, Part of Hospital Admitted Patient Care ActivityHospital Admitted Patient Care Activity 2019-20.
[32] Chen, B., Baur, A., Stepniak, M. and Wang, J., 2019. Finding the future of care provision: The role of smart hospitals. McKinsey & Company. Disponível em: https://www. mckinsey. com/industries/healthcaresystemsandservices/our-insights/finding-the-future-ofcareprovision-the-role-of-smart-hospitals.
[33] Johnston, E.E., Martinez, I., Currie, E., Brock, K.E. and Wolfe, J., 2020. Hospital or home? Where should children die and how do we make that a reality? Journal of Pain and Symptom Management, 60(1), pp.106-115.
[34] Chen, C.C. and Chang, Y.F., 2013. Smart healthcare environment: design with RFID technology and performance evaluation. Journal of Medical and Biological Engineering, 33(4), pp.427-432.
[35] Graham, Lisa M., and Curtis Fain. 2007. "“Places of Respite”: Designing Healing Experiences for Staff, Patients, and Visitors in Healthcare Facilities." The International Journal of the Humanities: Annual Review 5 (4): 211-216. doi:10.18848/1447-9508/CGP/v05i04/42088.
[36] Jones, C.B.C.B. and Gates, M., 2007. The costs and benefits of nurse turnover: A business case for nurse retention. The Online Journal of Issues in Nursing, 12(3).
[37] Graham, L. and Fain, C., 2007. " Places of Respite": Designing Healing Experiences for Staff, Patients, and Visitors in Healthcare Facilities. International Journal of the Humanities, 5(4).
[38] American Medical Association, 2020. AMA Digital Health Research: Physician’s motivation and requirements for adopting digital health—adoption and attitudinal shifts from 2016 to 2019.
[39] Babbu, A.H., 2016. Flexibility”: A key concept in Hospital Design. International Journal of Application or Innovation in Engineering & Management, 5(5), pp.24-28.
[40] Rosen, J.M., Adams, L.V., Geiling, J., Curtis, K.M., Mosher, R.E., Ball, P.A., Grigg, E.B., Hebert, K.A., Grodan, J.R., Jurmain, J.C. and Loucks, C., 2021. Tele-health's New Horizon: Providing Smart Hospital-Level Care in the Home. Tele-medicine and e-Health.
[41] Thomas, L., 2010. Flexibility & adaptability in hospital design & construction. DEA, 4530, p.18.
[42] Thomson, S., Foubister, T., Figueras, J., Kutzin, J., Permanand, G., Bryndová, L. and World Health Organization, 2009. Addressing financial sustainability in health systems.
[43] Jennings, N. and Rao, M., 2020. Towards a carbon neutral NHS.
[44] Fiest, M.D., Sharp, C.A., Mason, R.L. and Buckingham, J.P., 2008. Determination of PEMS measurement allowance for gaseous emissions regulated under the heavy-duty diesel engine in-use testing program. Final Report Prepared by Southwest Research Institute, San Antonio, TX, EPA. Contract No. EP-C-05e018, February. http://www. epa. gov/otaq/regs/hd-hwy/ inuse/420r08005. pdf.
58 2023 ― Volume 15.01 Research Journal
Peer Reviewers
Elizabeth Brinkley Innova Group
Dr. Mahsa Farid Mohajer Stantec
Dr. Thomas Nicholas NHS Trust
Dr. Siobhan Rockcastle University of Oregon
Dr. Mardelle Shepley Cornell University
Dr. Shyam Singham NHS Trust
59
Authors



Tanmay Anil Naik
Tanmay is based in the Toronto studio of Perkins&Will. He has numerous years of experience in the AEC industry from India working as a Project Architect on a wide range of architecture and interior design projects. With a passion and keen interest in sustainability, he has recently completed his Master of Science Architecture degree in High Performance buildings from the Georgia Institute of Technology, USA.
Tarek Rakha
Dr. Rakha is an architect, building scientist and educator. He is an Assistant Professor of Architecture at Georgia Tech, and Faculty at the High-Performance Building (HPB) Lab. His research and teaching aims to transform climate-responsive and sustainable architectural design decisions to advance racially and socially just solutions using robotics, sensing, modeling, machine learning, and Artificial Intelligence.
Jamie Wiberg
Jamie is a designer at Perkins&Will in our New York Studio. She joined the firm as an E. Todd Wheeler Health Fellow and now contributes to healthcare design and planning projects. She received her dual Master of Architecture and Construction Engineering and Management degrees at the University of Michigan Ann Arbor.
01 01
60 2023 ― Volume 15.01 Research Journal
02
Hala is a Living Design Champion & Senior Interior Project Designer with over 13 years of experience and a tenure at Perkins&Will that spans the globe. Hala brings thoughtful design ideas and a diverse & multidisciplinary interest in wellness. She is a leader in Perkins&Will’s healthy materials research. Driven by the recent pandemic, she has become a key researcher and pioneer for reducing the carbon footprint within interior design projects.

Dr. Din is the Director of Regenerative Design in the London studio of Perkins&Will. He has been involved in environmental low energy buildings and supply chains for over 20 years, including Passivhaus and Zero Energy Developments. He has focused his work and research on the healthcare typology in order to achieve zero-carbon in this facility type. His contributions have changed design practices at Perkins&Will to include a more multivalent approach.

Mark is a practice leader in the London studio of Perkins&Will. His professional experience spans multiple healthcare projects. As we move into a post-pandemic future, he is particularly interested in how we can create wider resilience across our built environment beyond the specifics of COVID. Keen to share his broad experience and knowledge, Mark teaches, reviews, and currently chairs the NLA Expert Panel for Healthcare.
 Hala ElKhorazaty
03
Mark Rowe
Asif Din
03
Hala ElKhorazaty
03
Mark Rowe
Asif Din
03
61
03
This piece is printed on Mohawk sustainable paper which is manufactured entirely with Green-e certificate wind-generated electricity.
Through its “Green Initiative” Program, Phase 3 Media offers recycled and windpowered paper stocks, recycles all of its own post-production waste, emails all client invoices, and uses environmentally friendly, nontoxic cleaning supplies, additionally Phase 3 Media donates 5% of all sales from its recycled product lines to Trees Atlanta.
9 781734 488159 90000> ISBN 978-1-7344881-5-9
2023 Perkins&Will. All Rights Reserved. For more information, please send an email to pwresearch@perkinswill.com
©

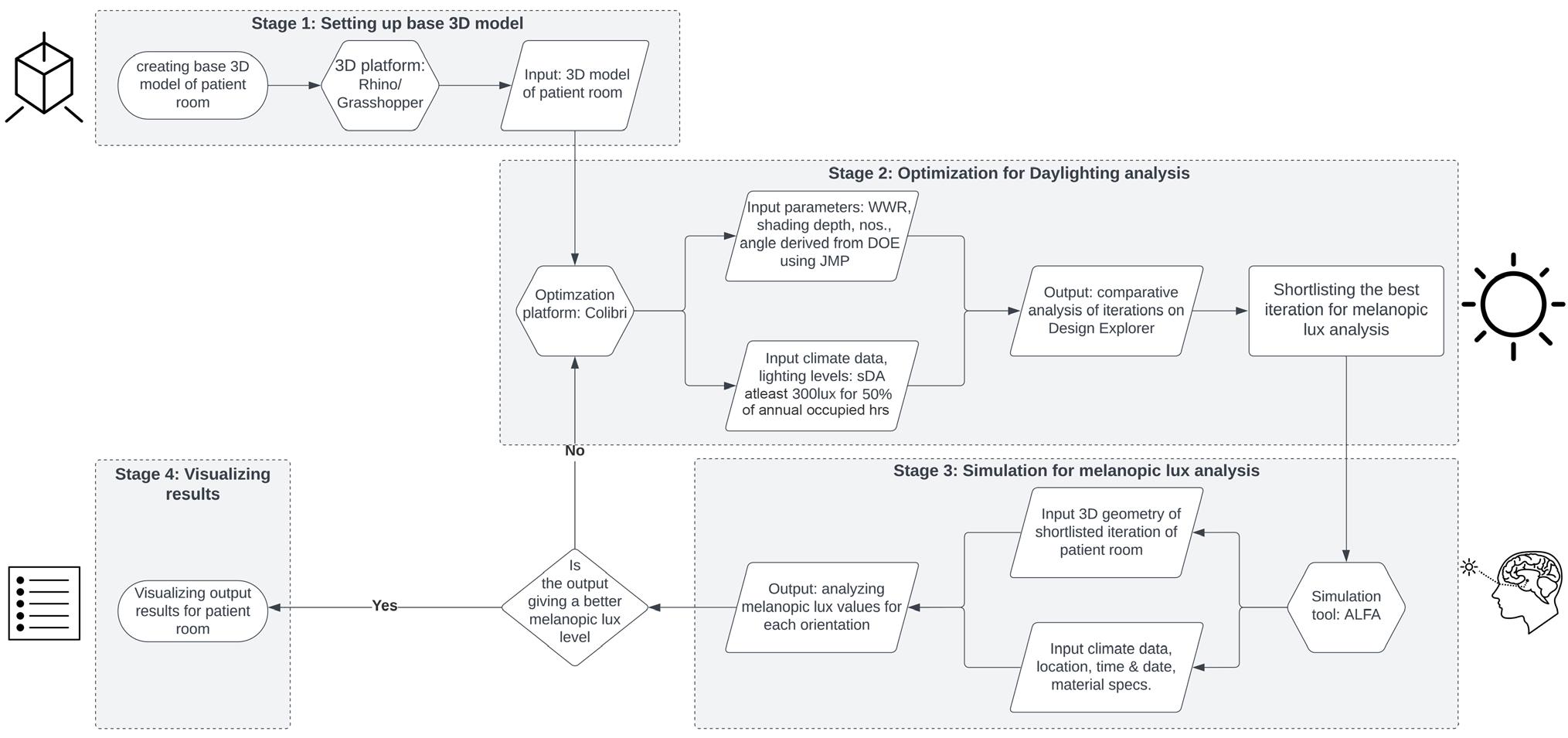
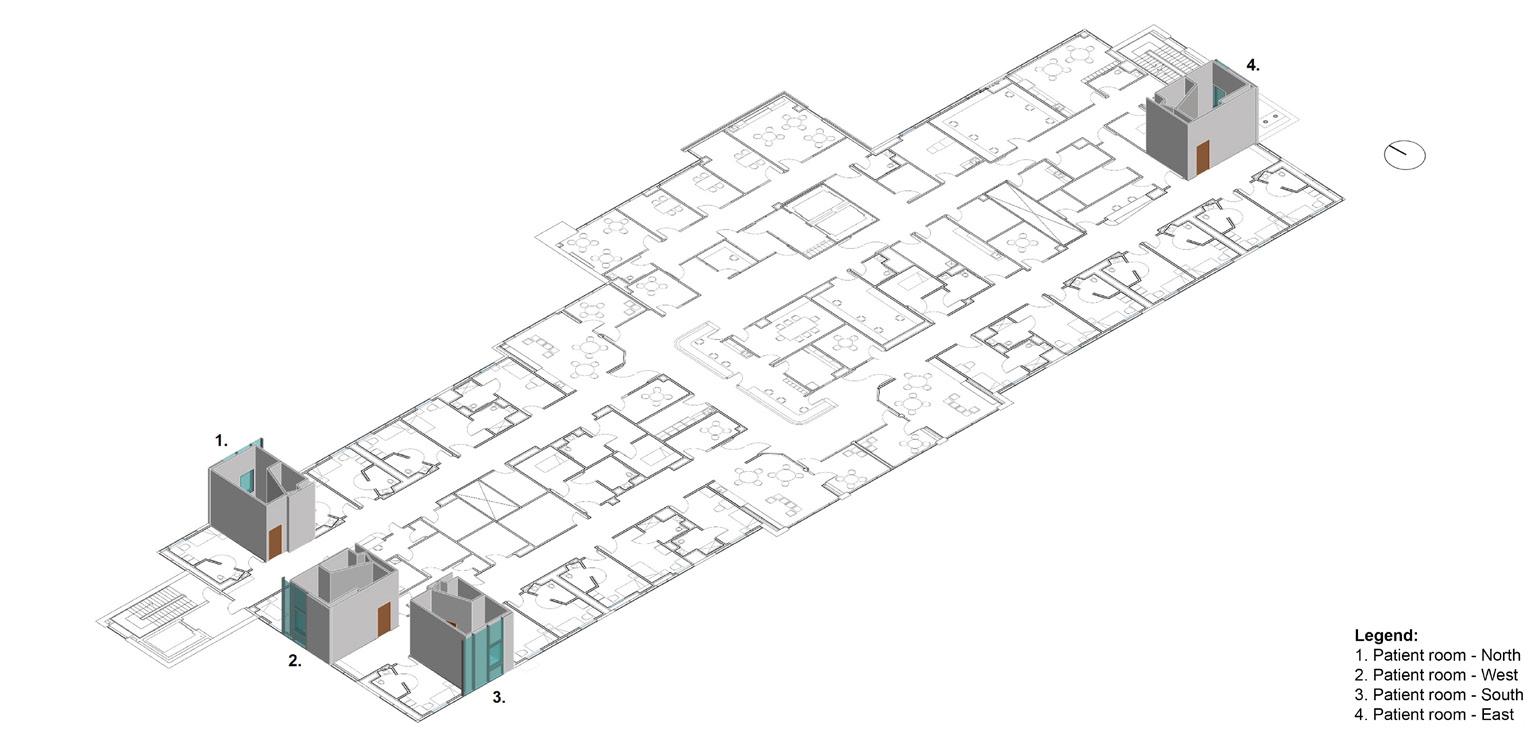 Figure 1: Simulation experiment framework.
Figure 1: Simulation experiment framework.

 Figure 3: Daylighting optimization results – Patient room North, louvers iteration.
Figure 3: Daylighting optimization results – Patient room North, louvers iteration.

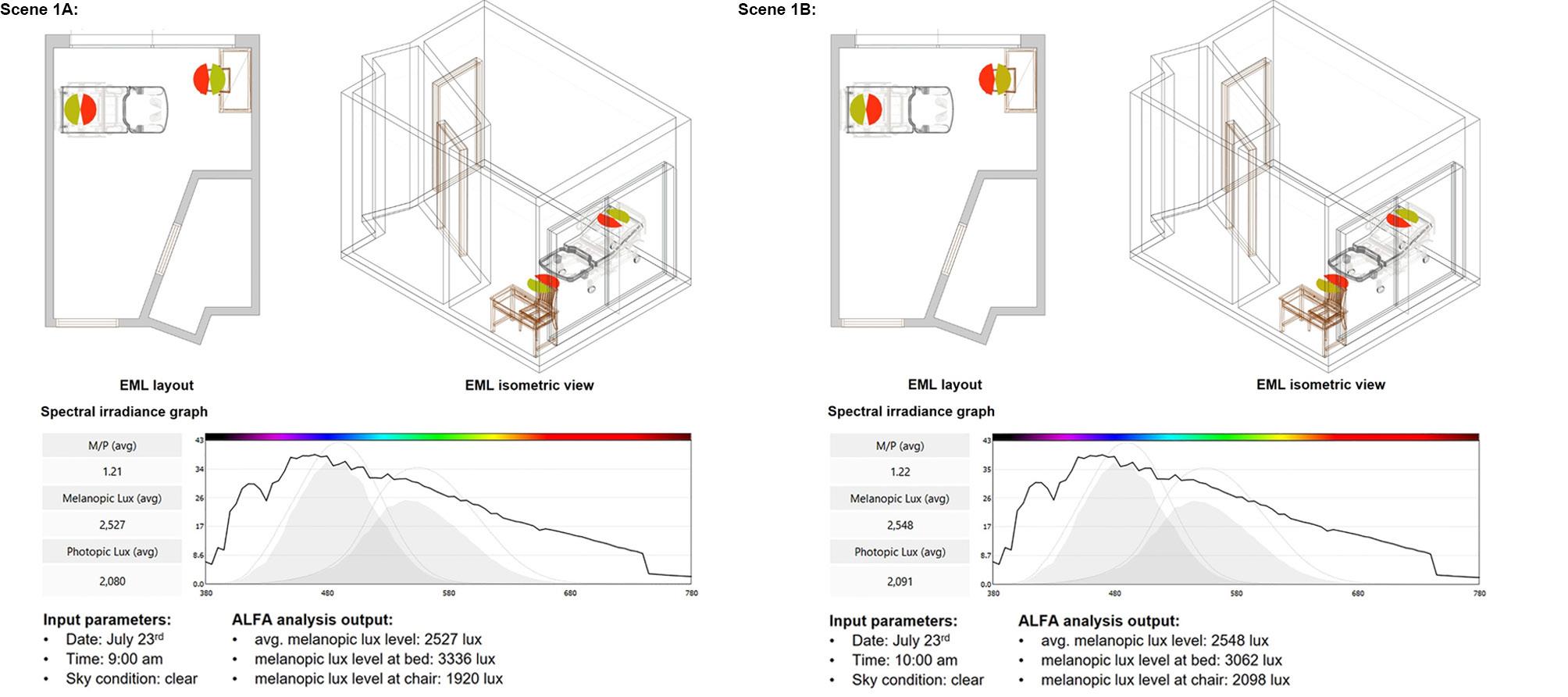
 Figure 5 indicates an overview of the daylighting and glare analysis. The circadian rhythm analysis was conducted on
Figure 6 indicates a sample output of the melanopic lux levels.
Figure 6: Patient room North – melanopic lux analysis | July 23rd | clear sky condition | 9:00am and 10:00ams.
Figure 5 indicates an overview of the daylighting and glare analysis. The circadian rhythm analysis was conducted on
Figure 6 indicates a sample output of the melanopic lux levels.
Figure 6: Patient room North – melanopic lux analysis | July 23rd | clear sky condition | 9:00am and 10:00ams.
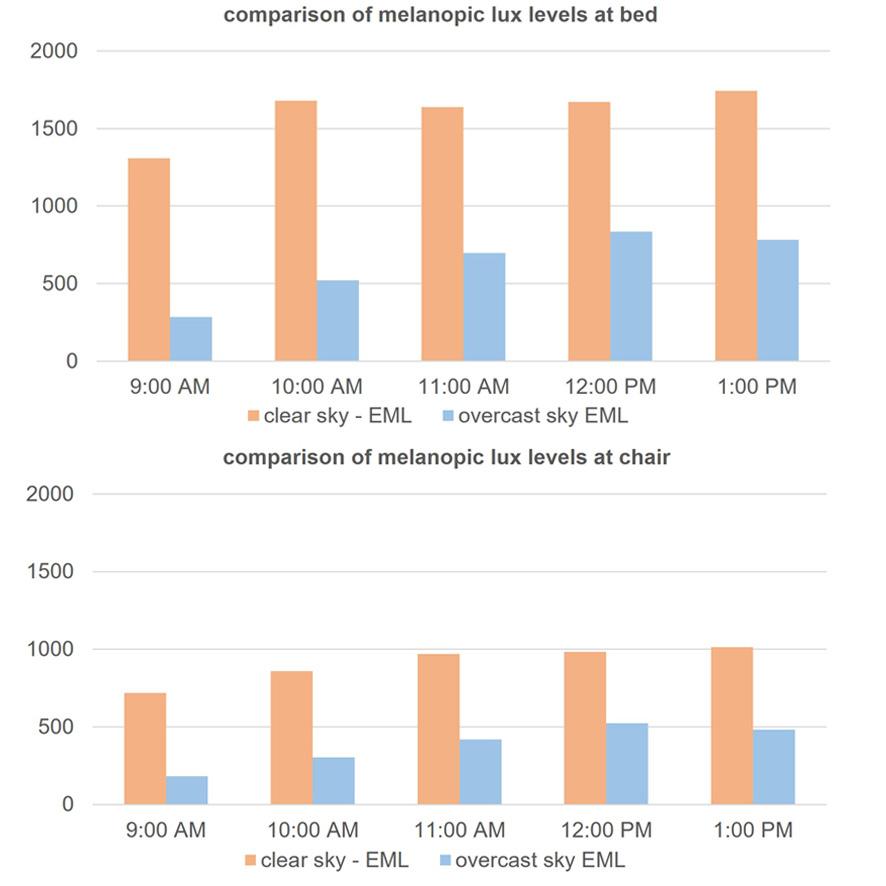
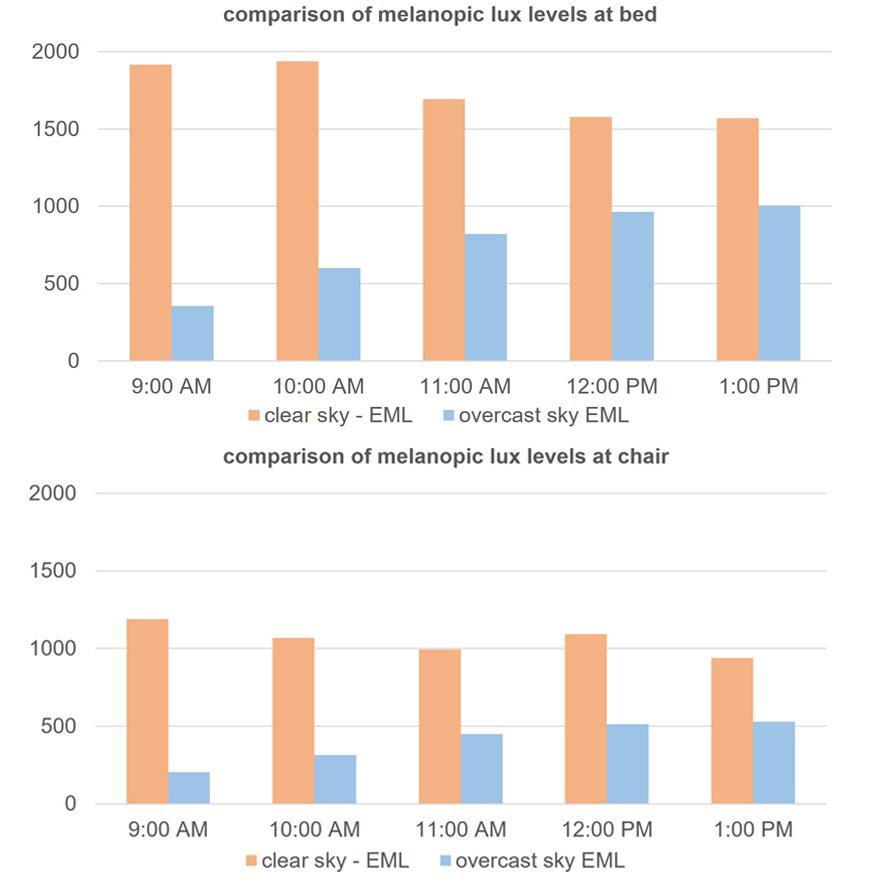 Figure 8: Patient room South - melanopic lux levels.
Figure 8: Patient room South - melanopic lux levels.
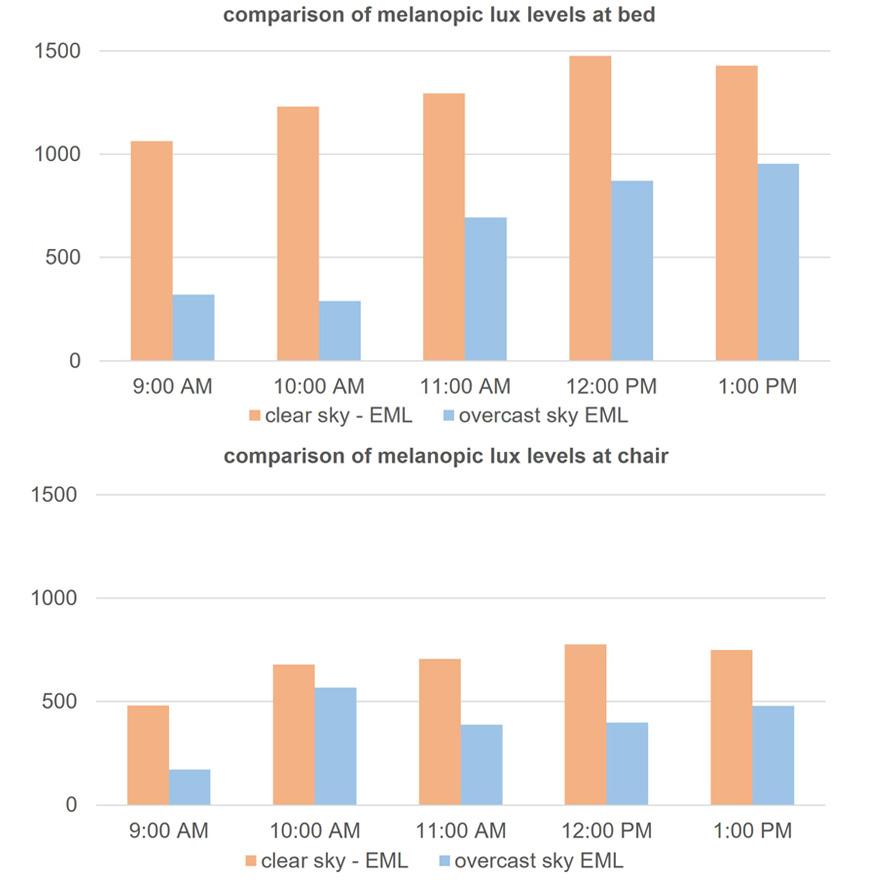

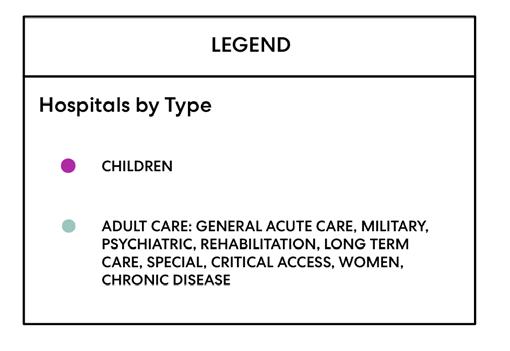 Figure 1: Map of continental US locating standalone pediatric hospitals. Map by author generated using GIS Data. Data sources listed on image.
Figure 1: Map of continental US locating standalone pediatric hospitals. Map by author generated using GIS Data. Data sources listed on image.
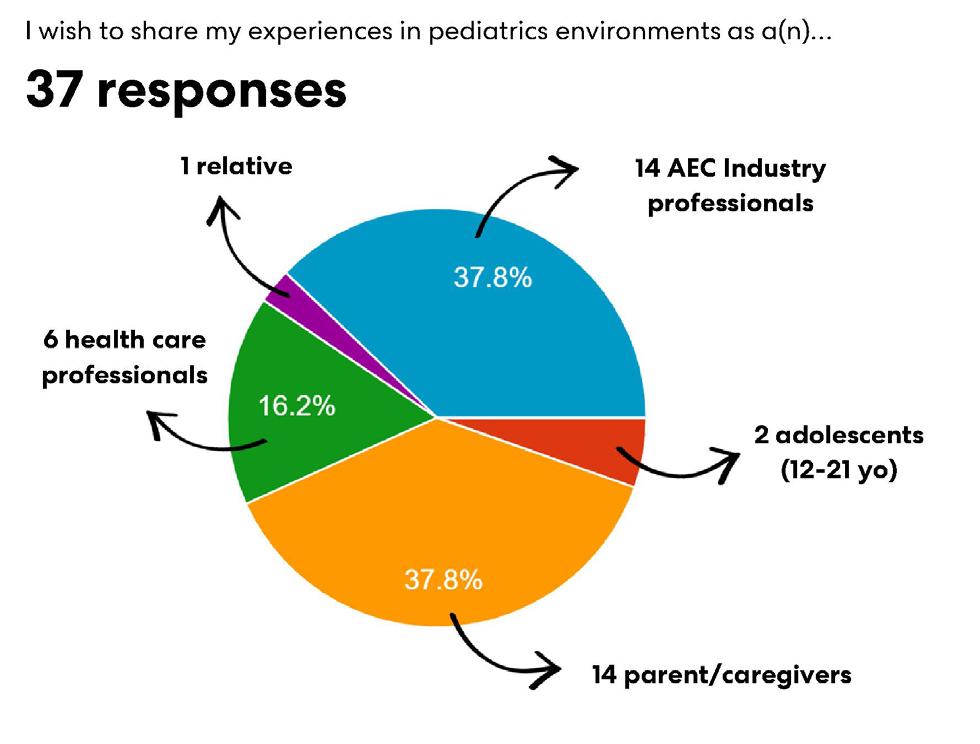

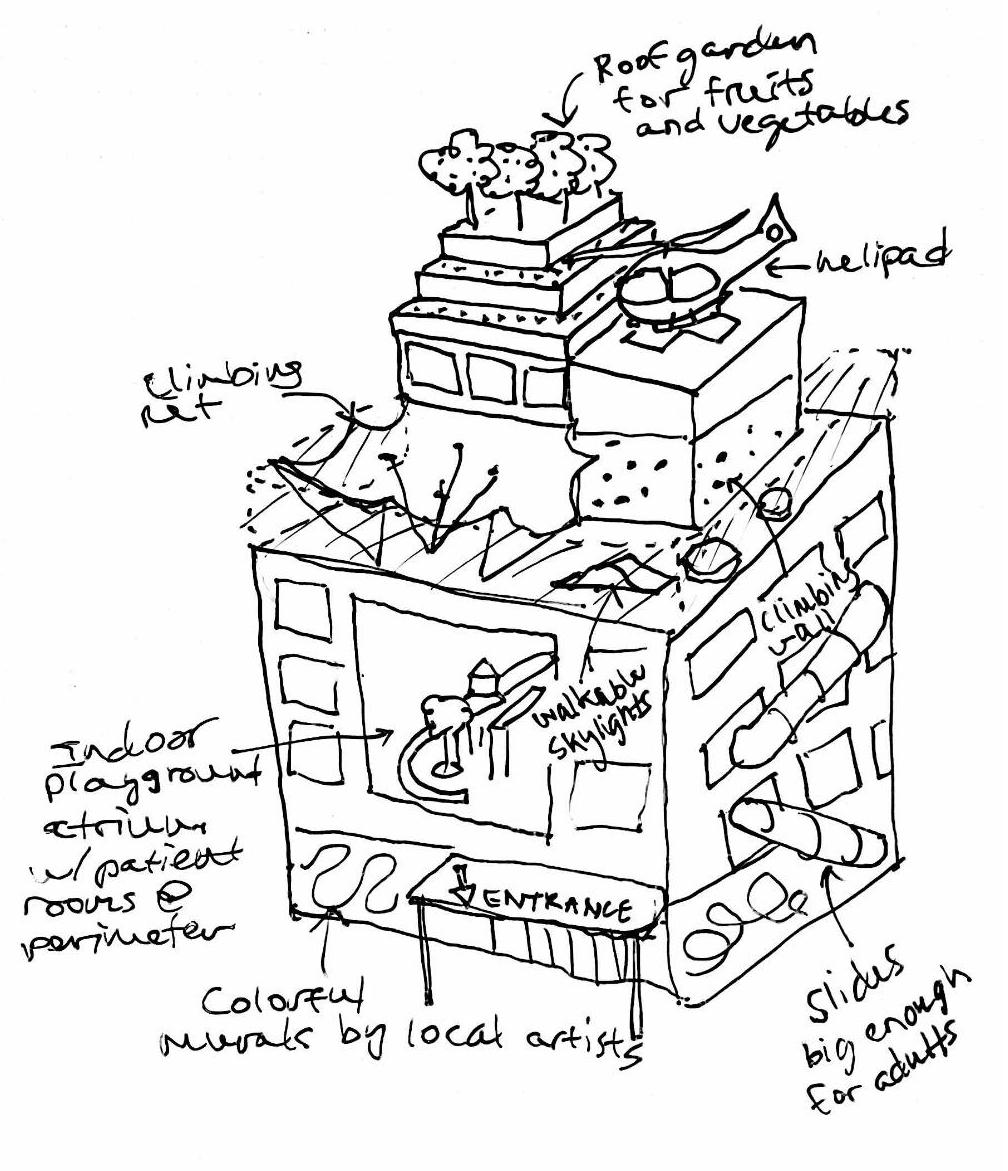
 Figure 5: University of Chicago Medical Center Micro-Hospital and Cancer Center. Source: Perkins&Will.
Figure 5: University of Chicago Medical Center Micro-Hospital and Cancer Center. Source: Perkins&Will.
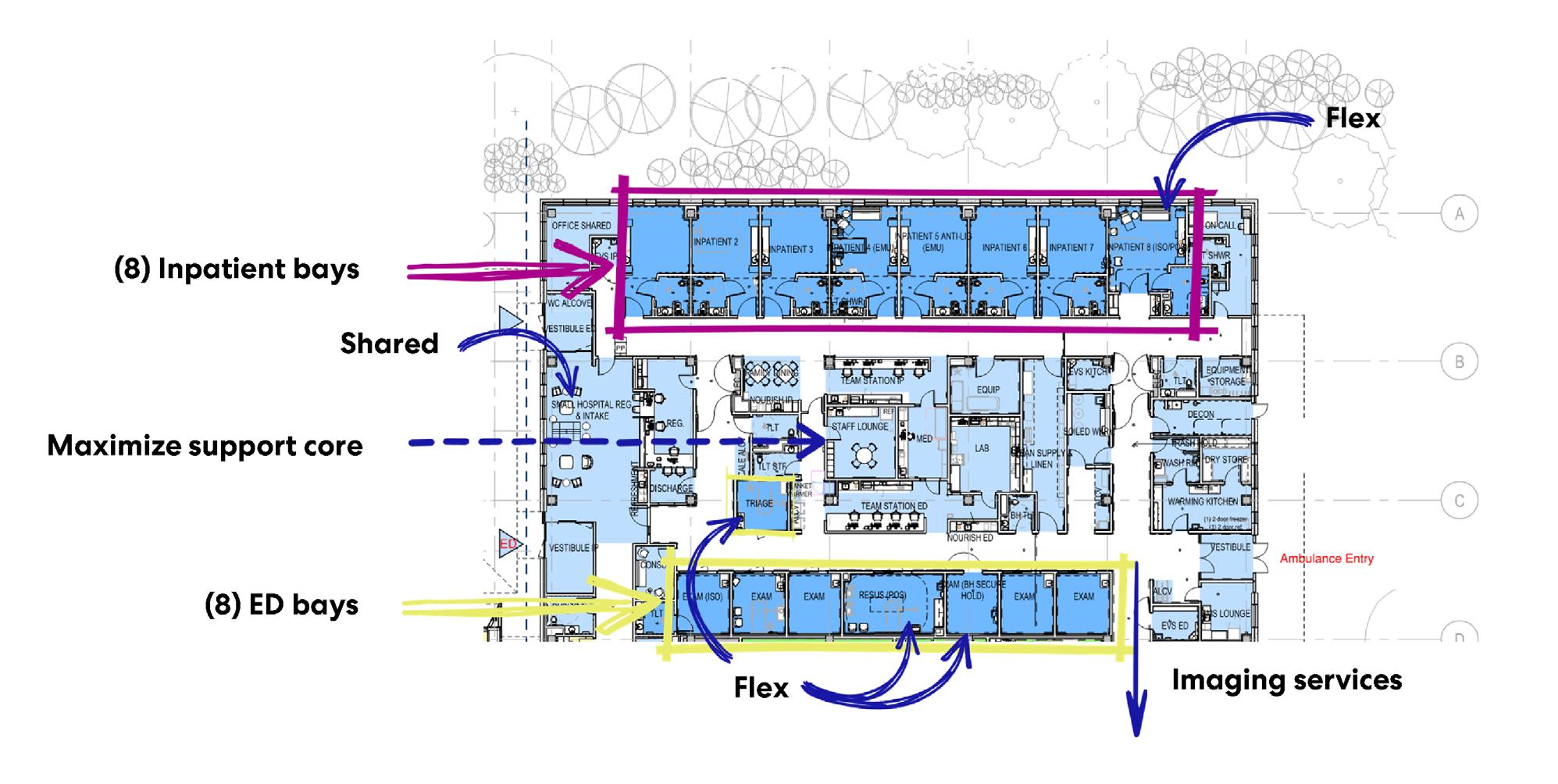
 Figure 7: Komansky Children’s Hospital Waiting. Source: Perkins&Will.
Figure 7: Komansky Children’s Hospital Waiting. Source: Perkins&Will.

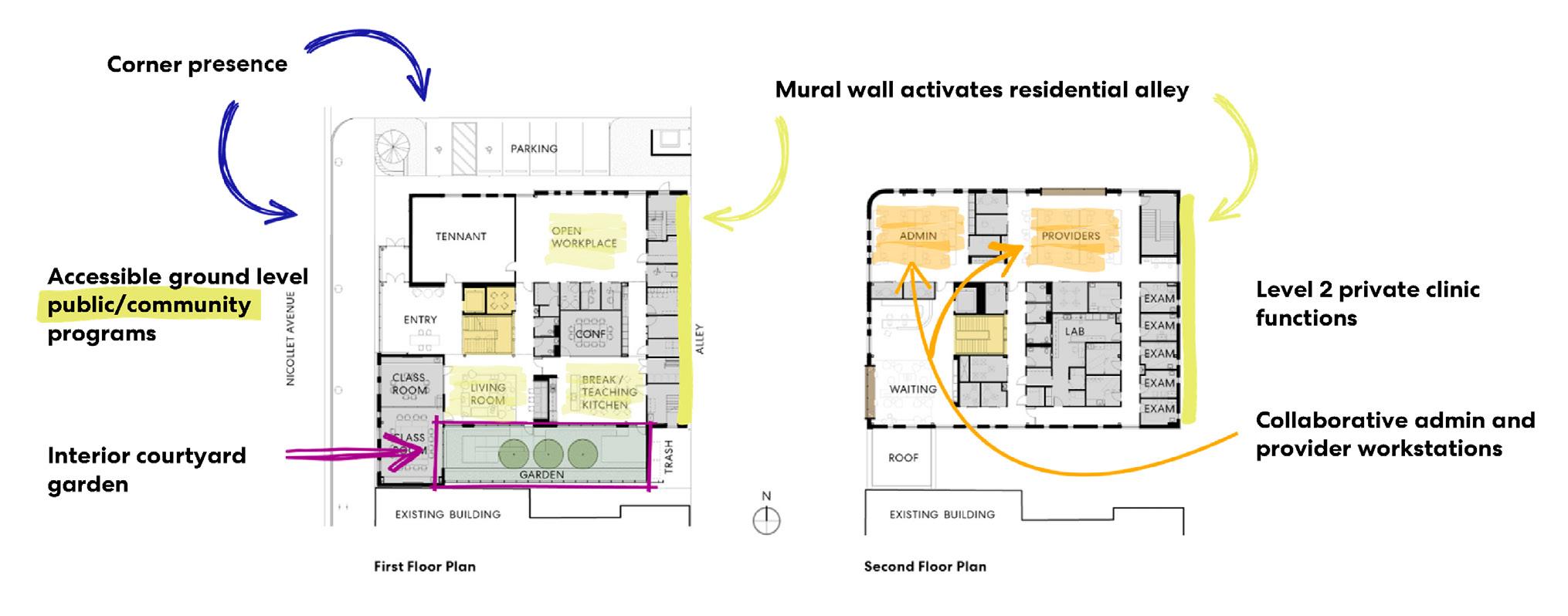
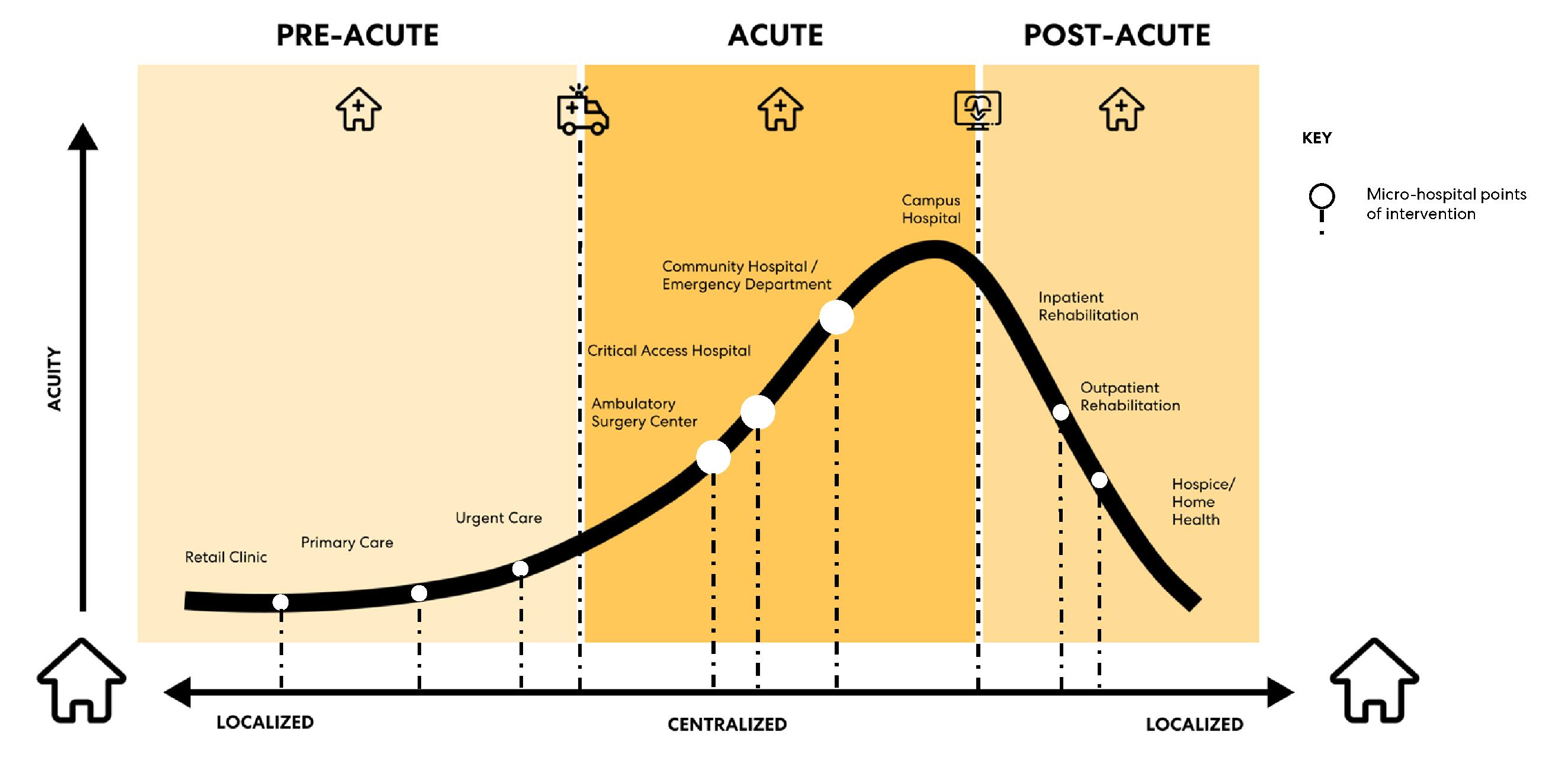
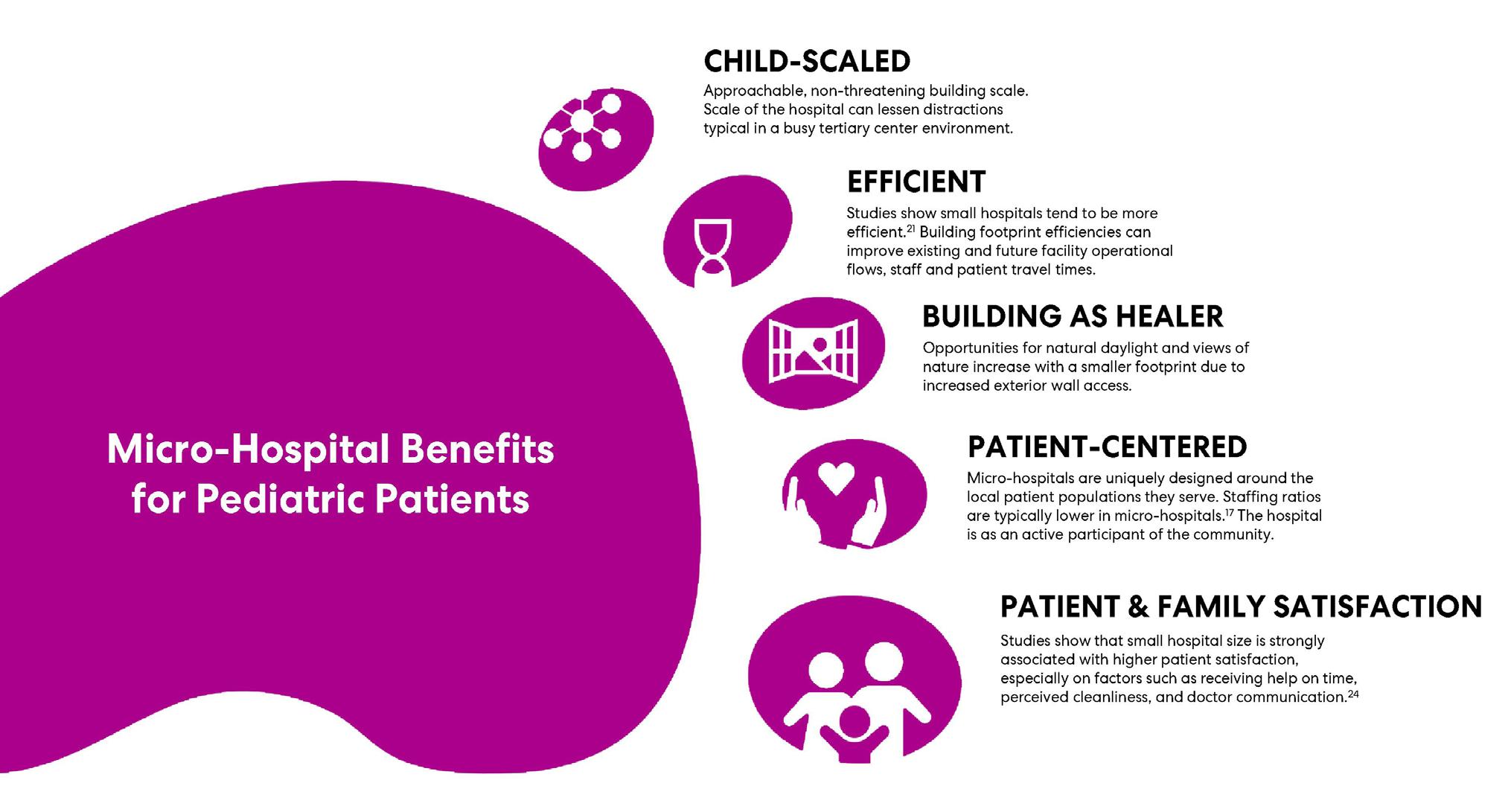
 Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Figure 12: A Micro-Hospital on a New York City Block. Source: Author.
Table 1: Pediatric Micro-Hospital Space Program Guidelines. (Continued.)
Figure 12: A Micro-Hospital on a New York City Block. Source: Author.
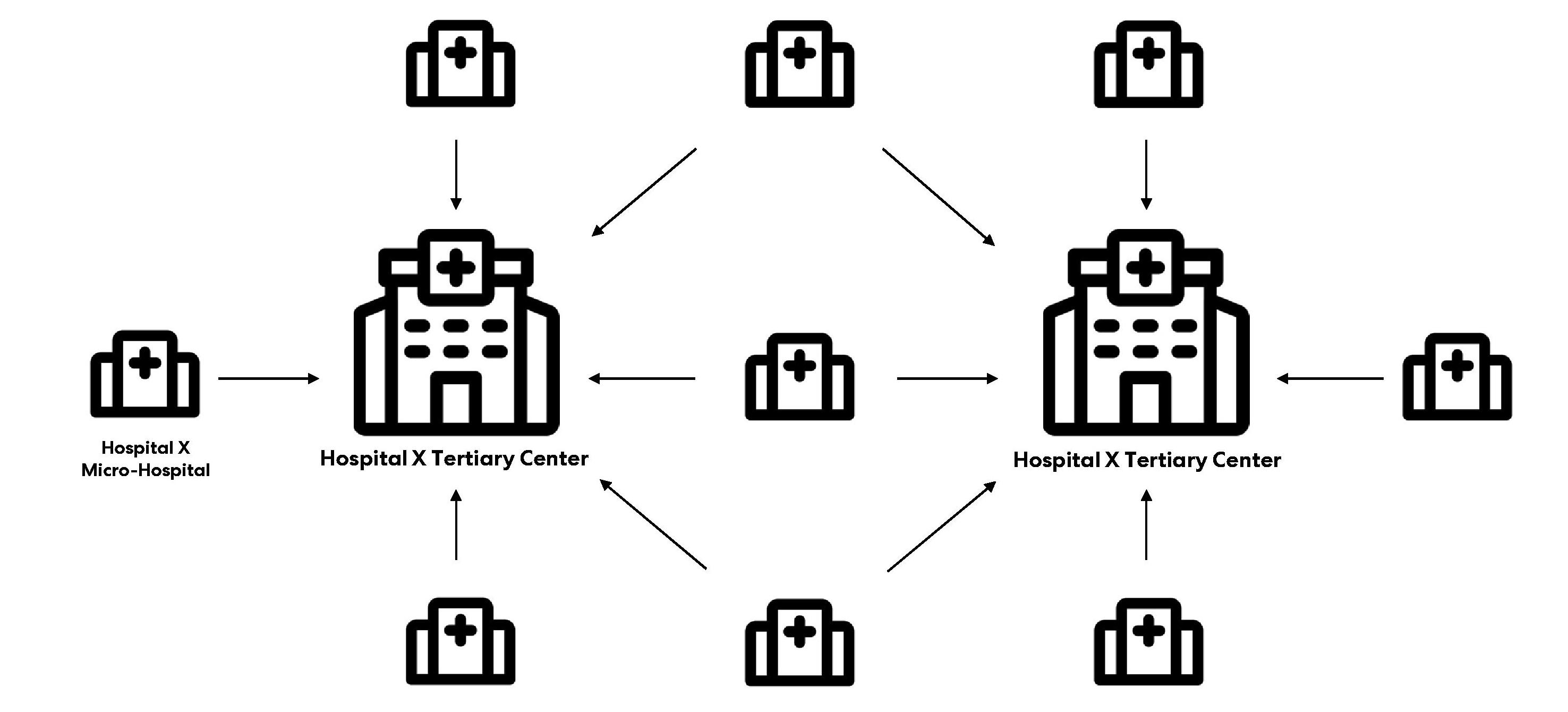
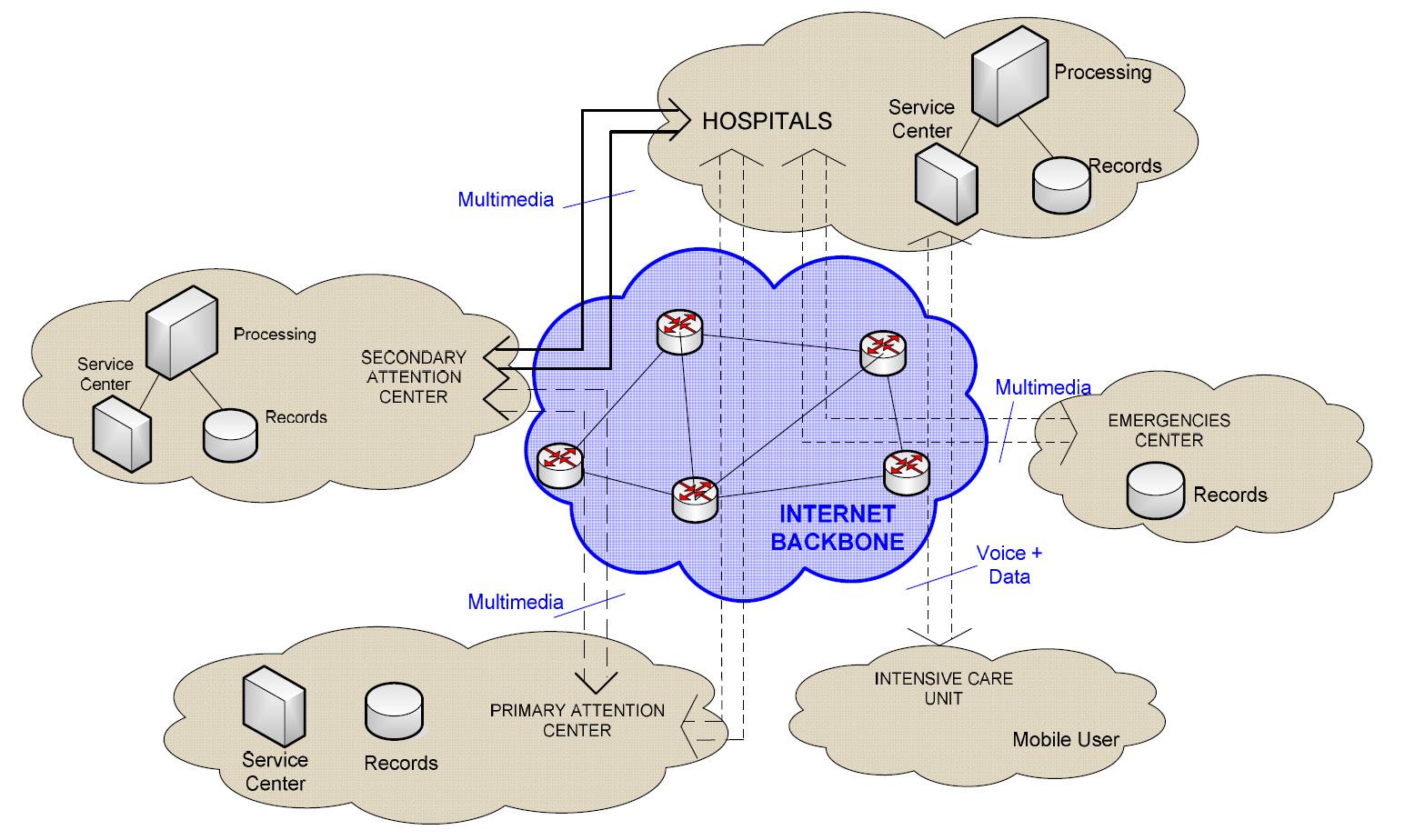



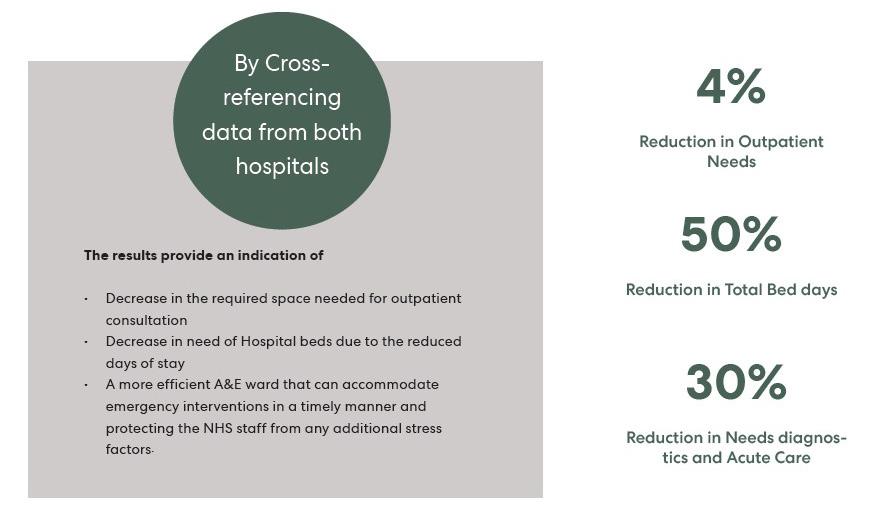

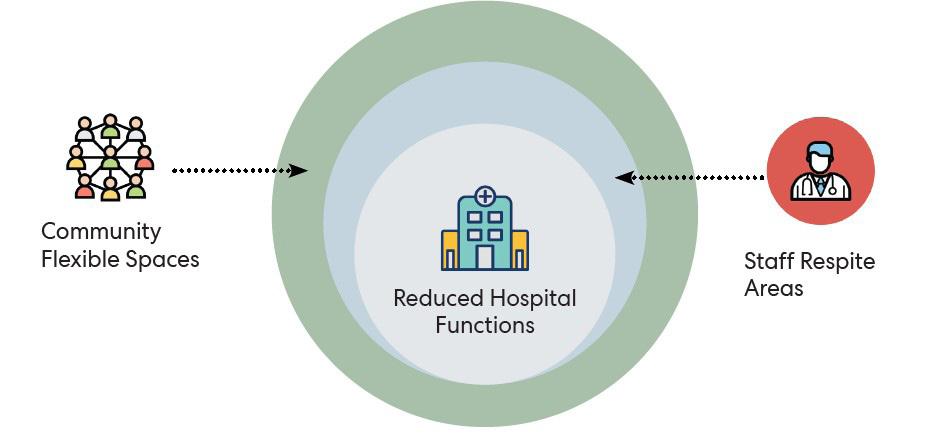





 Hala ElKhorazaty
03
Mark Rowe
Asif Din
03
Hala ElKhorazaty
03
Mark Rowe
Asif Din
03