THE PROMISE OF WEARABLE TRACKERS AND APPS PLUS
HOW HEALTH DISPARITIES AFFECT PH CARE
NEW LUNGS SPUR POSSIBILITIES
When You Can’t Breathe, Nothing Else Matters


THE PROMISE OF WEARABLE TRACKERS AND APPS PLUS
HOW HEALTH DISPARITIES AFFECT PH CARE
NEW LUNGS SPUR POSSIBILITIES
When You Can’t Breathe, Nothing Else Matters

The Navigating PAH Pathways program offers free webinars created specifically for patients and caregivers, all led by a PAH Nurse and sponsored by Janssen.*
Hear an educational presentation from a PAH nurse on topics that may be important to you.
Understand more about the effects of PAH, the 3 key treatment pathways, and treatment goals.

























Discover how to have more informed conversations about PAH with your care community.
Knowledge. Understanding. Empowerment. Register today at PAHregister.com or call 1-888-370-8111
Webinars are available at various dates and times so you can register for one that best fits your schedule.
Your PAH healthcare team should always be your main source of information. This program is not intended to provide medical advice or address specific medical concerns.
All webinars are viewed on a computer; internet access required. PAH=pulmonary arterial hypertension.
*The speaker is a paid consultant presenting on behalf of Actelion, a Janssen Pharmaceutical Company, and must present information in compliance with FDA requirements applicable to Actelion, a Janssen Pharmaceutical Company.


6

26
29
30


32



Matt J. Granato
President & CEO
Linda Busche
Editor-in-Chief
Paula Maturana
Graphic Designer
Karen Smaalders
Vice President, Communications and Marketing
Naya Baharona, Debra Hines-Bruce, Danielle Clement, Angela Golden, Cash Harpp, Jeff Harpp, Haley Johnson, Daniel Layton, Zan Laughlin, Barb Linser, Elisa Lipnick, Debbie McCarthy, Zangi Miti, Melanie Padgett Powers, Mary Beth Ramsey, Abby Sickles, Jaeger Spratt, Sara Tyghter.
301-565-3004
PHAssociation.org
SUPPORT LINE
800-748-7274
We’re here to support anyone with a connection to PH. (Daytime, please.)
Submissions to Pathlight are welcome. Please email your articles, photos and queries to Communications@ PHAssociation.org.
1629 K St., Suite 300 Washington D.C., 20006
BILLING AND MAILING ADDRESS
8401 Colesville Road, Suite 200 Silver Spring, MD 20910
Officers
Tony Lahnston, chair
Traci Stewart, R.S.N., C.S.N, CHFN, chair elect
Matt Wall, treasurer
Nicole Creech, secretary
Colleen Brunetti, M.Ed., C.H.C, immediate past chair
Matt J. Granato, L.L.M., M.B.A, president and CEO, ex officio
Trustees
Todd Bull, M.D., Scientific Leadership Council chair elect
Murali Chakinala, M.D., FCCP, Scientific Leadership Council immediate past chair
Colleen Connor
Ramona Doyle, M.D., M.Sc.
Anna R. Hemnes, M.D., Scientific Leadership Council chair
Kimberly Jackson, R.N., B.S.N., PH Professional Network chair
Jesse Kohler Wenninger, Esq.
Mitch Koppelman, Ph.D.
Michelle Ferdinand Liu, M.D., M.P.H., FAAOA
Melissa Magness, M.S.N., APRN, CNP-AC, PH Professional Network chair elect
Monica M. Penaranda
Diane Ramirez
Doug Taylor
Delphine Yung, M.D, Accreditation and Registry Committee (PHCC) chair
Emeriti ex officio
C. Gregory Elliott, M.D., FCCP, MACP
Michael D. McGoon, M.D.
Edwin Simpson
Judith Simpson, R.N., Ed.S.
Honorary
Carl Hicks
President & CEO
Matt J. Granato, L.LM, M.B.A
Kimberly Jackson, R.N., B.S.N., chair
Cheri Abbott, R.N., CCRP
April Blakley, R.N., B.S.N.
Jessie Dunne, PharmD, BCPS, BCCP
Loida A. Johnson, CRNP
Tisha Kivett, R.N., B.S.N.
Melissa Magness, M.S.N., APRN, CNP-AC, chair-elect
Anna R. Hemnes, M.D., chair
Steven H. Abman, M.D.
William R. Auger, M.D.
Eric D. Austin, M.D., MSCI
Sonja Bartolome, M.D.
Todd M. Bull, M.D., chair-elect
Murali M. Chakinala, M.D., FCCP, immediate past chair
Kelly Chin, M.D.
Vinicio A. de Jesus Perez, M.D., FCCP
Teresa De Marco, M.D.
Ankit A. Desai, M.D., FACC, FAHA
Jeffrey Fineman, M.D.
Robert P. Frantz, M.D.
Mardi Gomberg-Maitland, M.D., M.Sc.
Daniel Grinnan, M.D.
Kristin B. Highland, M.D., MSCR
Tim Lahm, M.D.
Deborah J. Levine, M.D.
Wes McConnell, M.D.
Lana D. Melendres-Groves, M.D.
John J. Ryan, M.D., M.B., B.Ch., B.A.O.
Sandeep Sahay, M.D.
Oksana A. Shlobin, M.D., FCCP
Thenappan Thenappan, M.D.
Nidhy Varghese, M.D.
Corey E. Ventetuolo, M.D., M.S.
R. James White, M.D., Ph.D.
Timothy L. Williamson, M.D.
Distinguished Advisers
David B. Badesch, M.D.
Erika S. Berman Rosenzweig, M.D.
Bruce H. Brundage, M.D.
Richard Channick, M.D.
C. Gregory Elliott, M.D., FCCP, MACP
Karen A. Fagan, M.D.
Michael D. McGoon, M.D.
Vallerie V. McLaughlin, M.D.
John H. Newman, M.D.
Ron Oudiz, M.D.

The summer 2023 issue of Pathlight zeroes in on the important topic of managing pulmonary hypertension (PH). This issue provides great insight into new ideas and resources that will inspire caregivers and those with PH, giving them tools they can learn from and use.
From the great network of PHA support groups to a successful lung transplantation; from improving technology to assisting patients with monitoring their health; from accessible oxygen for all those in need; to inspirational research, this is an important issue for everyone in the PH world.
Our cover story talks about a topic familiar to almost anyone. We all know about wearable devices and fitness trackers, but now they could help people with PH monitor their health and increase their physical activity. Clinicians are actively pursuing how to use apps for clinical care, even though they aren’t yet widely used in this way.
Our volunteer spotlight focuses on Deborah HinesBruce, who teaches language arts to students with disabilities. She and her husband Gary, who also has PH, are working hard to re-energize the Dallas support group as the effects of the pandemic diminish.
A related story highlights the importance of building a strong support network. We talk to Boston resident Shannon O’Donnell, who didn’t know anyone else with PH until she joined a PHA Facebook support group, and eight others about their support networks.
For inspiration, read the amazing story of Elisa Lipnick. After a decade of living with PH, Elisa, 37, received a lung transplant. She shares how thankful she is for her donor and their family as well as her new ability to breathe.
This issue also focuses on another component vital to helping people with PH breathe: supplemental oxygen.
Unfortunately access to oxygen isn’t as readily available as it should be. Hear from the parent of a teen with PH, the teen and a woman with PH about the crucial need for better access to oxygen.
Last but not least, with the 15-year anniversary of the passing of my niece in September 2022, I can personally relate to our story about Debbie and Steve McCarthy of Belford, New Jersey. Debbie and Steven raise money for PH research in remembrance of their daughter Katie, who died 10 years ago. Katie was diagnosed at age 29 and died less than a year later. Kudos to Debbie and Steve for their remembrance of Katie and all they do to support research to find a cure for PH.
As we roll into the warmer temperatures, I reminisce about the 15-plus years that I have been involved with the Pulmonary Hypertension Association, all the wonderful people and friends that I have met along the way, and the inspiring stories I have heard. I am very thankful for the joy and learning that all of this has given me.
Thank you to all those folks in this organization that have inspired me to work hard to fulfill the PHA mission!
Have a great summer.
Tony Lahnston Chair, Pulmonary Hypertension Association Board of Trustees
As a special education teacher, DEBRA HINES-BRUCE teaches English, language arts and reading to students with learning disabilities. She and her husband Gary live in Little Elm, Texas. They have a combined family of four children and six grandchildren, ranging in age from 6 to 22. Debra is a member of the Pulmonary Hypertension Association (PHA) Support Group Leader Advisory Board.
BY DEBRA HINES-BRUCEIn June 2016, I attended my first PHA conference, where I met my amazing husband. Like me, he has pulmonary hypertension (PH) and was attending his first PH International PH Conference and Scientific Sessions. Neither of us had heard of PH before we were diagnosed.
The conference was just what I needed. I engaged with many people who understood what I was going through. There were many leaders in the PH field, who shared an abundance of information.
After a year of long-distance dating, I moved to Texas from California. Gary and I got married, and I joined him as co-leader of the Dallas Support Group. He had been the leader for two years prior. I became a volunteer because I knew the importance of giving back, and I think it is important to support others.
PH is the reason Gary and I met, but we have so much more together. Although being a patient and a caregiver has its ups and downs, I love taking care of my husband. And I have experienced many of the same difficulties he experiences from this illness.
Prior to COVID-19, our support group had over 40 members. We now have about 15 members who attend consistently. Last year, we held seven support group meetings. I am looking forward to seeing what the future holds as people are beginning to go out more.
I enjoy co-leading the support group with my husband; we feed off each other. I think our relationship strengthens
the group, and it gives hope to our singles. We have been told that we are an inspiration. Gary is quite the comedian, so there is always laughter at our meetings.
The most rewarding part of leading a PHA support group is seeing the smiles on the faces of the people who have been encouraged, comforted and inspired. I feel this way because it reveals to me that I am a light in this sometimes-dim community.
I am most proud of helping others in need, whether from providing a listening ear, offering insightful information or giving back to the PHA community.
I am inspired by the 10-plus-year survivors of pulmonary arterial hypertension (PAH). Whenever I am down or have concerns about this disease, I know I can reach out to one of them for comfort, inspiration or even knowledge about a particular medication or treatment. This is really a great community to be involved with.
My doctor told me about PHA support groups and conferences in 2016, not long after I was diagnosed. At the time, I was living in the Los Angeles area. When I went to my first meeting, I was embraced by a wonderful group of people who made me feel comfortable and removed some of my fears.
As many of you know, this can be a very scary diagnosis. My doctor advised me not to search Google (I did). She recommended I find a support group as soon as possible. I’m glad I did.
My diagnosis came in 2015, after a routine physical. My doctor noticed my heart was enlarged and sent me to the emergency room. After I was admitted to the hospital, I spent 10 days in ICU. The doctors discovered I had idiopathic PAH. I’d had no symptoms.


I thought I caused my PH because I wasn’t taking care of myself. Deep down, I knew that wasn’t true because I worked out daily and had recently lost 130 pounds.
Currently, I’m on IV therapy and two other medications, which has reduced many of my symptoms. I live a normal life. Gary was diagnosed in 2009, and his case is associated with COPD. His PH isn’t as severe as mine, and he is only on one medication.
We love our roles as PHA support group leaders. If you’re considering leading or starting a support group, step out on faith and do it! There are so many volunteers who would be willing to help you along the way.
Feeling inspired to support the PH community? PHA provides you with a toolkit to get started and helps each step of the way. Apply to become a PHA support group leader: PHAssociation.org/get-involved/volunteer.
‘PH is the reason Gary and I met, but we have so much more together. Although being a patient and a caregiver has its ups and downs, I love taking care of my husband. And I have experienced many of the same difficulties he experiences from this illness.’
Being informed about treating and managing your pulmonary hypertension (PH) is key to becoming an active member of your care team. The Pulmonary Hypertension Association (PHA) can equip you with resources to advocate for yourself through our PHA

Connects: PH Community Workshops, formerly known as PHA On the Road.
Our next PH Community Workshop heads to the New England region. Join us Saturday, July 29 in Burlington, Massachusetts, for this free, daylong event.
The workshop is a unique opportunity for people with PH of all ages, family members and caregivers to learn about PH, disease management, and research advancements. The workshop offers educational tracks and
PROGRAM DETAILS
Saturday, July 29
Boston Marriott Burlington Burlington, Massachusetts
peer support for adults and children with PH.
The event aims to provide valuable information and resources to help attendees navigate their PH, whether they’re newly diagnosed or long-term thrivers.

PHA is partnering with Brigham & Women’s and Boston Children’s Hospitals to present this free workshop. Presenters include health care professionals and other experts. All ages are welcome. Tweens and teens will learn about key lifestyle steps to help them transition from young adult to adult care. The workshop
offers opportunities to connect with other youths to help navigate life as a young adult with PH.
Parents of children with PH will learn about managing their children’s treatment and care from PH pediatricians and other experts. An onsite Kids Room will offer fun activities for children while parents learn and connect with each other.
Don’t miss this opportunity to join the PHA community in the Boston area. Visit PHAssociation.org/ PHworkshop to see the agenda and register.
The Pulmonary Hypertension Association offers several new videos through its free onlinelearning platform, PHA Classroom.

PHA Classroom is a collection of educational materials, including prerecorded webinars, printable handouts and informational videos. Resources range from PHA’s Empowered Patient Toolkit, guided exercise worksheets, and more. PHA Classroom materials are designed for people with PH, families, caregivers and health care professionals.
Newer materials in the collection include our new video series on pediatric PH. Michelle Sykes, M.D., Ph.D., a pediatric cardiologist specializing in PH at Kentucky Children's Hospital worked with PHA to create the series. Dr. Sykes discusses how pediatric PH is diagnosed and treated and the importance of finding a pediatric PH specialist for treatment and care.
Each of the eight videos in the series addresses a single issue so parents can find specific videos to address their children’s needs:
• Diagnosing Pulmonary Hypertension in a Pediatric Patient.
• Treating Pediatric Pulmonary Hypertension.
• Understanding the Signs and Symptoms of Pulmonary Hypertension in a Child.
• What Are the Types of Pediatric Pulmonary Hypertension?
• Managing Your Child’s Pediatric Pulmonary Hypertension.
• What Are the Differences Between Pediatric and Adult Pulmonary Hypertension?
• How To Talk to Your Child About Pulmonary Hypertension.
• The Importance of a Pediatric Pulmonary Hypertension Specialist.
PHA Classroom also is a valuable resource for health care professionals. PHA offers several videos to help physicians and patients understand the complexity of PH diagnoses. PH specialists can easily share the videos with their patients.
Watch these videos and other new releases at PHAssociation.org/ classroom.
Before Shannon O’Donnell joined a Pulmonary Hypertension Association (PHA) Facebook support group, she didn’t know anyone else with pulmonary hypertension (PH).
Shannon, of Boston, had joined PHA’s Young Adults with PH: Generation Hope Facebook group in 2013 to meet other people her age with PH. She later became a volunteer moderator.

Finding support is crucial when you or a loved one live with PH. PHA offers several options for peer support, including in-person meetings, online and hybrid meetings, Facebook groups, email PHriends and its toll-free patient and caregiver support line.
“Attending a support group is important because it gives everyone a chance to talk and help each other,” says Alberta Wright, a support group leader in Detroit, Michigan. “ We have the same illness, so we understand one another.” Support groups have helped Alberta get the support she needs as a patient and allow her to help others as a leader.
“I can express how I’m feeling,” she says. “I also listen to what has helped others and I take lifestyle tips from them.”
Similarly, Diane Ramirez, of the Piedmont area in North Carolina, says support groups are a great way to learn about PH from other patients just like you. “You can ask questions as often as needed and it’s a great way to make friends,” says Diane, a support group leader and a PHA Board of Trustees member.


Evelyn Mitchell, who leads a support group in Lexington, Kentucky, says, “It’s helpful being around other people who are like us and understand what we go through with symptoms, medications and side effects on a daily basis. It’s important to attend a support group meeting so you don’t become isolated.”

Many patients feel like they are fighting PH alone. “Sometimes they are,” says Monica Penaranda, a PHA board member and Greater Los Angeles PHA support group leader. She recommends people with PH go to support group meetings so they don’t feel alone and to learn from their peers.

“We can share how we do things to help us in this journey,” Monica says. “We can also learn about new treatments and how to better advocate for ourselves. Support comes in many forms.”
Nancy Zeppa, who leads the group in Southern New Jersey, says meetings can connect attendees with valuable resources, such patient
‘You never know by sharing your journey or asking a question whom you may help.’
-NANCY ZEPPATop to bottom: Shannon O’Donnell, Alberta Wright, Monica Penaranda, Diane Ramirez, Jacqui Kanat. Opposite, clockwise: Joseph and Janet Harda, Nancy Zeppa, Jeri Nudell, Evelyn Mitchell.
referrals to doctors who helped them. “You never know by sharing your journey or asking a question whom you may help.”
Support groups can be lifelines, says Janet Harda of Thomasville, North Carolina. “Providing a place for people on the phone or online — to share feelings confidentially, make friends, get help navigating the health care system and your disease, and learn from others who have walked a similar path.”


Jacqui Kanat says going to support group meetings and meeting others with PH/PAH was beneficial. “I learned a lot from the various speakers and was encouraged by others with this rare disease.”

Another way to make in-person connections is through PHA events, such as its International PH Conference and Scientific Sessions and its PH Community Workshops. Jeri Nudell, a support volunteer from Peyton, Colorado, says in-person connections with peers changed her life.
“The very first PHA conference that I went to in Orlando, not one person looked at me like I was actively dying,” Jeri recalls. “What a huge boost for my self-esteem to be looked at for my contributions and my presence without people dissecting my health conditions. This was my first interaction with anybody else who had pulmonary hypertension. It was extremely emotional, but life-changing for me.”
PHA provides you with a toolkit to get started and helps each step of the way. Apply to become a PHA volunteer: PHAssociation.org/get-involved/volunteer.
PHA Support Groups. Support groups meet in person, online or hybrid (in person with virtual elements).
PHA Support Line. Call (800) 748-7274 to connect with a member of the PH community.
PHA Facebook groups. Social media can be a powerful tool for connection, but it can be challenging to know where to go or who to trust. PHA groups are trusted resources that we manage and are moderated by volunteers. Here are our Facebook groups:
• PHA Long-Term Thrivers.
• PHA Generation Hope: Young Adults.
• PHA PH Plus: Associated Conditions.
• PHA CTEPH (chronic thromboembolic PH).
• PHA Teens.
• PHA Parents of Kids with PH.
• PHA Caregivers.
• PHA Newly Diagnosed.
• PH & HHT: What’s the Connection?
PHA Email PHriends. Contact an experienced, trusted fellow patient or caregiver by email to get information, share stories or connect.


 BY ELISA LIPNICK
BY ELISA LIPNICK
In August 2010, I was diagnosed with systemic lupus erythematosus. When I was diagnosed, I knew nothing about lupus. So I found a good doctor and started treatments to help me feel better and manage my disease.
During the fall of 2011, I was working in retail management. I noticed that I became short of breath and my heart beat rapidly while I was working. Walking up the stairs became difficult too. I emailed my rheumatologist my symptoms, and he ordered blood work, CT scans and a chest X-ray. After my tests, my rheumatologist said I could have something called pulmonary hypertension (PH), a disease I had never heard of.
In January 2011, I changed insurance and had to find new doctors. At that point, I didn't have a confirmed PH diagnosis, and I was determined to get answers. I found a pulmonologist, but I had to wait a couple months to be seen.
I had my first appointment in May and a right heart catheterization in June. After the catheterization, I was
referred to another pulmonologist, Roblee Allen, M.D., at UC Davis Hospital in Sacramento.
From November 2011 to July 2012, my body was shutting down. My breathing and rapid heart rate were getting worse. I became shorter of breath at work, while working out, and going up the stairs. I had no energy and started experiencing bouts of dizziness.
In July 2012, I met Dr. Allen and received my official PH diagnosis. He went through everything I could expect with this new diagnosis with me and my mom. Without treatment,
he said I wouldn’t live more than three years, that I couldn’t get pregnant, and my life would be very different than before.
Significantly, he said he would be with me all the way on this new journey and started me on medication that day.
After starting Letairis and Revatio, I started to feel a little better. In November 2011, Dr. Allen asked me if I wanted to join a clinical drug trial. For the trial, I came in once a month
for a six-minute walk tests, EKGs and blood work. I was happy to be a part of the trial.
I started the trial in 2014. Two years after the trial ended, I found out I was on the placebo treatment. Luckily, I was able to start the real medicine, Uptravi. This medication continued to work well for me for a while.
By early 2013, I was feeling so well that I hired a personal trainer and started to work out three days a week. I loved being active and seeing my body get stronger. Being active was mentally and physically helpful.
In 2016, the Uptravi no longer worked for me. A right heart catheterization found that my pressures had gone up. I was taking Letairis and Adcirca at the time, but my doctor wanted to be more aggressive with my treatments.
In April 2017, I started subcutaneous Remodulin. The site pain was terrible, but I continued the treatment because I didn't have many choices. Being in pain from site changes made me depressed, and I stayed alone for years. It was hard to make plans because I never knew how I'd be feeling. Despite the site pain, the Remodulin worked well for me.

In November 2017, I got very sick and ended up in the hospital. The hospital staff performed many tests to figure out what was wrong with me but couldn’t figure out the cause of my illness. After rounds of testing, I underwent a lumbar puncture. After two weeks of treatment, I was released from the hospital.
I was told my lumbar puncture would continue to heal. But the wound didn’t heal properly, and I began leaking brain fluid.
On Jan. 11, 2018, I woke up in the hospital where I was undergoing a procedure to put staples in my head to secure the brain bleed. My mom said I had been “acting weird” that morning. I was scheduled for an appointment with a neurologist, but after he heard my mom’s explanation of my behavior, he sent an ambulance for me.
In the emergency room, the doctors performed a CT scan and found the brain bleed. I don’t remember much from the days before the brain bleed was discovered. After the surgery, I spent the next year and a half focused on healing my mind and body. It took me about three years to feel like myself again.
In 2020, COVID-19 hit, my doctor retired, and I met my new PH specialist, Namita Sood, M.D., FCCP. The pandemic affected everyone, but it was especially hard for those who were disabled. We faced more isolation and had to be extra cautious not to get sick. I did my best to stay away and stay healthy.
My health started to decline again in early 2021. I was having more shortness of breath, and my activity level went down. Every couple of months I had six-minute walk tests, pulmonary function tests, blood work and right heart catheterizations to monitor the progression of my PH.
I was lucky to get another wonderful doctor who worked hard to help me through my disease progression. Even when I switched
to Adempas, my health continued to decline. By October 2021, Dr. Sood and I began talking about transplant. Medicine just wasn't working for me anymore.
By January 2022, I could feel my oxygen drop every time I got up to walk. At my pulmonary appointment in February, Dr. Sood admitted me to the hospital for monitoring and to switch my Remodulin to IV Flolan. I started Flolan that night.

Soon after I was admitted, the team noticed my platelets were dropping. They started to run a battery of tests, including a bone marrow biopsy. I spent a month and a half in the hospital and made no progress. I was so frustrated that I had a breakdown in front of my doctor. At that time, we came up with a plan to move forward with transplant.
I originally planned to go to the University of California San Francisco Hospital for my transplant, but my doctor ultimately sent me to Stanford
Hospital. On Mar. 31, 2022, I got news there was a bed ready, and I transferred to Stanford that night. While I was at Stanford, the team started my transplant workup. Each day brought different tests, including CT scans, swallowing test, walk tests, right heart catheterization and tons of blood work.
On April 15, 2022, I was officially put on the transplant list. My lung allocation score was 35, which was low. However, Dr. Sood continued to advocate for my transplant by writing an exception letter to help get a higher score. After her letter, my score went from 35 to 53. My team decided that I should stay in the hospital until my new lungs became available.
My doctors at Stanford urged me to get as strong as possible before surgery. I began using elastic bands for my workouts. I also did a lot of walking and used a stationary bike twice a day.
While I was at Stanford, I kept thinking of my donor and their family, sending love and blessings. When people said they were praying for me, I said to pray for my donor and their family too. I felt so calm during the whole process; there was never a worry in my mind.
On May 16, 2022, my doctor came into my room, laughing. She said I had organs! My lungs were there, ready to change my life. As I was getting onto the operating table, my surgeon told me the lungs were perfect, and surgery was a go. I was so happy and ready.

The two days after my transplant are a bit of a blur for me. Thankfully, my family was there to tell me all that happened. My surgery was six hours, with one minimal complication. After surgery, my chest was left open because the surgeon needed to go back and fix a hole in my heart from 2018.
I don't know if anyone can prepare for the aftermath of lung transplant. When I fully came to consciousness and was aware of what was going on, I was so anxious. I thought I couldn’t breathe. I had to relearn to breathe on my own.

For 10 years, I had breathed out of my mouth because of my PH. Now, I needed to breathe through my nose, which was difficult for me. But everyone around me was reassuring, so I eventually started breathing through my nose again.
I stayed in the heart and lung ICU for four days. I then moved to the heart and lung floor, where I underwent a swallowing test to ensure
I didn’t aspirate food or drink into my new lungs. After I got the hang of swallowing, it was time to walk.
When I got up to walk with physical therapist, I was so nervous. I hadn't been out of bed for almost two weeks, other than to practice getting in and out of a chair. My legs were shaky, but I was determined. I couldn’t go far, and I was very short of breath, but I did it. I was so proud of myself. Walking twice a day was my goal going forward.
A few days later, I got the news that I was ready to be discharged. I didn't get to go home, but I moved across the street from the hospital into patient housing. I needed to stay close for my twice-weekly blood work and X-rays.
After leaving the hospital, I discovered I had extra mucus in my lungs. I underwent bronchoscopies for a couple weeks until the mucus was gone. I also struggled with low white blood cell count. I was admitted a few
times for monitoring, but I haven’t had any infections so far. I continue to get bronchoscopies every two weeks.
In January, my doctors placed a custom 3D-printed stent in my left airway to help with some issues I was having. The stent has helped me feel a lot better, and my breathing has continued to improve. My doctors and I plan on keeping the stent in for a year to fix my airway. I have also experienced severe pain from gastroparesis, a condition that makes digesting food difficult. My gastrointestinal doctor and I are working to resolve the issue.
Making the decision to go forward with transplant wasn't easy, but I have no regrets. The experience has been wild, but I've had the best support system.
I have great days and days where I struggle. Through all of this, I keep pushing forward, and I always keep a positive outlook.
I'm so thankful for my donor and their family and loved ones. There are no words to express my full gratitude, but I hope to express it in my actions going forward. I plan on planting a tree in my garden and living a full and happy life thanks to my donor and their family.
I'm beyond elated that I no longer have to be attached to a medical pump. I truly feel free. PH changed my life for 10 years, and now I get to experience life with new lungs and a new outlook on my life.
Learn more about the lung transplant journey at PHAssociation.org/patients/ treatments/transplant.
Shavini Fernando, M.B.A., couldn’t go without her oxygen backpack and nasal cannula because she never knew when her oxygen levels might plummet without warning from pulmonary arterial hypertension (PAH). Suddenly, she couldn’t breathe and sometimes her heart stopped.

“I had to walk with the oxygen everywhere, and it’s heavy,” she said. “I was always having neck aches because the nerve would get compressed from the weight of the oxygen.”
A few years ago, Fernando began brainstorming on how she could live more freely, without being tethered to oxygen. She developed the idea of a wearable device that would continuously monitor a person’s SpO2, or oxygen saturation levels. She called it OxiWear.
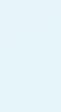
OxiWear is among the apps, wearables and fitness trackers that could help people with pulmonary hypertension (PH) monitor their health and increase their physical activity. However, the devices are not part of the “standard of care” for those with PH, meaning they aren’t included in the current widely used medical recommendations. Anyone who wants to use such devices should talk
over their plans with their health care provider.
“There’s obviously a lot of interest in developing this field, in understanding what we’re measuring and how to use it for clinical care of patients,” said pulmonologist Jasleen Minhas, M.D., MSCE, of the Hospital of the University of Pennsylvania. “But the field overall is very, very early in researching these things.”
Janssen Pharmaceuticals is among the companies developing digital tools to help physicians identify PH and assess risks for PAH.
People with PAH often go undiagnosed for two or three years after initial discussions about symptoms with their doctors, says Sean Studer, vice president, medical education, Janssen.
Echocardiograms are the most important noninvasive screening tool and should be used whenever PH is suspected, he says. However, a significant skill gap exists in assessing right heart parameters on echocardiograms to determine the probability of PH, which is an important step in the PAH diagnostic algorithm.
In 2019, Janssen developed EchoRight Pro, a free smart phone app, to address that skill gap. It uses case studies and gaming techniques to help cardiologists, pulmonologists and sonographers identify PH on echocardiograms. Users read case studies and view echocardiogram pictures, then answer questions about the likelihood of PH. The cases become more difficult to diagnose as users advance through increasing challenging stages.
“Improving these skills among physicians may help create urgency for earlier detection and diagnosis of PH, which are essential for informing treatment decisions and improving patient outcomes and quality of life,” Studer says.
The EchoRight Pro is the third version of the app, which started with 27 cases. The latest version has more than 94 case studies, based on feedback from health care professionals who asked for increasing challenging cases and left-heart phenotype cases.
Janssen also offers the DETECT Screening Tool for PAH-Ssc. It launched the app in 2013 for health care professionals who treat patients with connective tissue diseases. The tool uses a two-step algorithm developed and validated in a 2013 study by Janssen subsidiary Actelion.
Connective tissue disease is the second most common form of PAH in the United States and Europe, after idiopathic PAH. About one in five people with the most common connective tissue disease, systemic sclerosis, or scleroderma, develop PAH.
The app can help clinicians determine which patients need electrocardiography and ultimately
right heart catheterization to confirm scleroderma-related PAH. Clinicians can learn more and download the app to their iPhones or Android devices at suspectpahctd.com/DETECT.
“Mobile applications, game-type experiences and patient simulations can offer an engaging way to empower current and future health care professionals to practice clinical reasoning in educational settings,” he says. “That will help enable them to provide the best possible care for PH and PAH patients.”
Apps and gaming technology also enhance how people with PH learn about their disease, track test results, and assess their mental and physical health.
For example, United Therapeutics launched its PHPal App in 2019 to empower patients to better understand their disease and manage their symptoms, says Meredith Broderick, PharmD, J.D, senior director, medical affairs. The app is for anyone with PH, no matter what treatment they take, she emphasizes. UT designed the app to help patients feel more confident, hopeful and informed about their disease state.
“It’s information they can take back to their health care team, make informed decisions and be part … of the decision-making process,” Broderick says.
The app helps patients learn about PH in easily understandable language through a fun facts game. Other features allow patients to track six-minute walk distances, assess their functional class or manage their
mental wellness through breathing and yoga videos. The app also includes a journaling feature and podcasts.
UT continuously looks for ways to improve the user experience, seeking feedback through formal sessions in 2020 and 2021, as well as the app itself. When patients asked about dictation features because they didn’t like typing long notes about their symptoms and day-to-day changes on their phones, the app developers added voicerecording.
“It goes back to UT’s core mission to be able to give patients a hopeful, brighter future,” Broderick says. “We’ve heard through … the patient feedback on the app that they want to feel empowered. They want to be knowledgeable about their disease. They want to be informed about their disease. They want to feel confident about the decisions that are being made.”
Similarly,
Connect app allows people with PAH to track tests results, functional class
and data measured at home, such as weight and mood. The app provides education material to help patients understand their PH, as well as mindfulness exercises and recipes.
The app allows patients to log goals set with their doctors. Patients can share data about their health trends so their doctors can tweak or manage their care plans. The app keeps patients motivated to stay on track through messages from the app. Doctors connected to the Care4Today portal also can use the app to send motivating messages to patients.
For some patients, progression can happen quickly and without warning, so it’s important for people with PAH to actively monitor how they’re feeling, whether it’s through an app, a journal or other means, Studer says. It’s equally important to feel comfortable sharing that information with their care teams, he says.
“Technology has revolutionized patients’ ability to play an active role in their own health,” Studer says. “When a patient and their care provider are making collaborative, informed decisions … together, patients feel a greater sense of responsibility over managing their disease.

“Increased patient involvement could result in improved adherence to their treatment regimens and ultimately improve outcomes, which is critical for progressive diseases like PAH.”

As technology evolves beyond mobile apps, developers and entrepreneurs are investigating wearable health trackers.
OxiWear, worn on the ear, provides continuous SpO2 monitoring. It
Tracks health measures, provides medication and appointment reminders and motivating messages. Free in the App Store from Janssen. pahriskassessment.com/care4today
Ear-wearable oxygen saturation tracker. The device bundle, which includes a charger and mobile app, is $500. Monthly payment plans are available, and people with PH can use the code PH20 to get 20% off. oxiwear.fitness
Education PH content, PHacts game, track health measures and six-minute walk, record metrics to review with care team. Free in the App Store by United Therapeutics. phpal-app.com

Janssen app to help health care professionals assess PAH risk in patients with systemic sclerosis. suspectpahctd.com/DETECT

Janssen app to teach health care professionals to identify signs of PH. echoright.com/united-states
vibrates when oxygen levels decrease and tracks oxygen levels in an accompanying mobile app. While OxiWear undergoes the Food and Drug Administration’s medical device approval process, Fernando is marketing it as a fitness app. Elite athletes use it to measure their oxygen levels during exercise to evaluate and tweak their performance. Those living and exercising at high altitudes also have shown interest in the device. High altitude affects pulmonary arteries and lung function and can cause Group 3 PH.
Fernando has been wearing her own OxiWear on her ear since mid-2022. She keeps her oxygen backpack nearby but no longer wears it all the time. Now, she feels confident in running quick errands, like grabbing lunch during the workday, while leaving her oxygen behind.
As research continues, apps and wearables that track activity levels and health measures might offer those with PH ways to easily keep updated on their health, ultimately improving quality of life.
“What we’re able to do with technology continues to grow,” says pulmonologist Daniel Lachant, D.O., an assistant professor of medicine at the University of Rochester Medical Center. “Finding a way to incorporate it into pulmonary hypertension care will help to improve outcomes and assessments and complement things like telemedicine, which provides a great service to our patients.”
Several pulmonary hypertension (PH) researchers are studying how wearable devices and fitness trackers could improve health monitoring.
In two related studies, researchers are using Fitbits, which are wearable fitness watches, to evaluate how physical activity changes the quality of life among people with PH. Both studies are enrolling now and don’t require in-person visits.
In the Mobile Health Intervention in PAH (MOVE PAH) Study, participants with pulmonary arterial hypertension wear a Fitbit provided by the researchers for 28 weeks. Some will receive daily encouraging text messages about fitness. At the end of the period, they will take an at-home six-minute walk test and fill out a survey about quality of life, according to cardiologist Evan Brittain, M.D., MSCI, associate professor of medicine at Vanderbilt University Medical Center in Nashville.
Dr. Brittain and his team are recruiting participants through the Pulmonary Hypertension Association Registry. MOVE PAH study is a longer and larger study than its initial pilot study, which showed that those who received the text messages averaged 1,300 more steps in the final 12th week. Those who didn’t receive the texts didn’t improve their step count.
Dr. Brittain also is looking at how physical activity changes over time. In a related study, participants will wear a Fitbit for 12 weeks a year for four years. Adults with any cause of PH and no recent hospitalizations are eligible.

“One of the major limitations of most activity studies in general — PH or otherwise — is very short monitoring periods,” Dr. Brittain said. “[Many studies are] basically measuring activity for seven days and then seeing what happens many years later, without any information about what happens with activity in between those times. We think that extending the observation period to three months, and doing it year after year will be a really valuable look at what the natural history of physical activity is.”
Similarly, pulmonologist Jasleen Minhas, M.D., MSCE, of the Hospital of the University of Pennsylvania is studying what various activity levels mean for those with PH. Without longitudinal studies, researchers can’t assume that low activity levels mean more severe disease, she says.

In a 2021 study, Dr. Minhas and colleagues at seven sites enrolled 55 people with PAH in the PHANTOM (Pulmonary Hypertension and Anastrozole) randomized controlled trial. Each participant wore an accelerometer for seven days, then
underwent a six-minute walk test and echocardiography and completed a quality-of-life survey.
“We saw that patients spend up to 80% of their time being sedentary and are active only 20% of their day,” Dr. Minhas said. “Activity counts were associated with disease severity and health-related quality of life, so patients that had worse disease based on echocardiographic measures had lower activity levels, and then those with lower activity levels had worse clinical metrics, such as a lower six-minute walk test and lower health-related quality of life.”
This type of information guides treatment, so it’s important to continue to invest in further studies that track physical activity and disease activity over time, she said. Their ongoing study, ACTiPH, aims to bridge some of these gaps.
In 2020 and 2021, pulmonologist Daniel Lachant, D.O., an assistant professor of medicine at the University of Rochester Medical Center, studied whether patients could safely do sixminute walk tests at home. Because of
the pandemic, many people with PH couldn’t perform their regular six-minute walk tests in their doctors’ offices.
Dr. Lachant recruited 20 people with stable PAH to wear small chest-based accelerometers and electrocardiogram heart rate monitors, the MC10 BioStamp nPoint, while performing two six-minute walk tests in clinic and at least two at home. The participants mapped out short walking courses, typically 30-40 feet, in their houses. An app provided instructions on how to perform the test and included a six-minute timer.
The study results showed that walk distances were slightly lower in the home setting. By incorporating the heart rate data, cardiac effort (the number of heart beats used during the
test divided by walk distance) showed a very similar number to what was seen in the clinic. The initial feasibility study was completed between October 2020 and April 2021.
Dr. Lachant is now validating his initial findings in a larger study. In the current study, 100 patients are using chest monitors for six-minute walks at home four times in one year.
“What’s exciting about this, instead of somebody having this measurement checked every three months like we do routinely, somebody could do this once a week or every month to get a better sense of whether they are improving,” Dr. Lachant said. “It allows for more frequent observations.”
A goal in PH treatment is to reach the low-risk level, and the at-home walk
might be able to help with this.
“With a more frequent walk, you can get more observations to assess whether somebody is responding to a drug, or do we need to be more aggressive sooner, instead of waiting for clinic appointments that just happen to fall three or six months later,” Dr. Lachant says.
By incorporating the heart rate, it provides a more frequent “safety check,” letting clinicians know whether a patient’s heart is growing more stressed, he says. In addition, perhaps a person’s walk distance isn’t improving but the number of heartbeats during the walk is decreasing. “That tells us that they’re actually responding to therapy, which is equally important,” he says.
Researchers seek participants for the following studies:
Mobile Health Intervention in PAH (MOVE PAH) Study
Goal: Clinical trial to test the effect of increasing physical activity on quality of life and six-minute walk distance. No in-person visits required; participants will wear Fitbits for 28 weeks; randomized to receive daily encouraging text messages or to usual care.
Eligibility: Adults with idiopathic, heritable, connective tissueassociated PAH, or simple congenital heart disease PAH, who are on stable therapy. Contact: alisha.lindsey@vumc.org.
Activity Monitoring in Pulmonary Hypertension
Goal: To understand how physical activity changes over time and its association with PH severity and quality of life. No in-person visits required; participants will wear a Fitbit for 12 weeks a year for four years.
Eligibility: Adults with any cause of PAH with no recent hospitalizations. Contact: Email alisha.lindsey@vumc.org.
Physical Activity in Pulmonary Hypertension (ACTiPH)
Goal: Monitor physical activity in a large population of PAH patients in the U.S. to determine if certain
types of activity are particularly beneficial. Participants will wear an ActiGraph device for seven days after each regularly scheduled PH clinic visit for four years.
Eligibility: Adults with PAH or chronic thromboembolic pulmonary hypertension who are treated at Pulmonary Hypertension Association-accredited PH Care Centers and enrolled in the PHA Registry. Contact your PHCC physician during your regularly scheduled clinic visit for information.


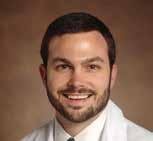
The Pulmonary Hypertension Association brings together more than 400 health care professionals every two years for its Pulmonary Hypertension Professional Network Symposium. The professionals have various specialties, experience levels and disciplines, but they all care for people with pulmonary hypertension (PH).
Attendees include nurses and nurse practitioners, physicians, researchers, physician assistants, pharmacists, respiratory therapists, social workers from clinics, universities and pharmaceutical companies.
The Sept. 28-30 event, themed “PHoundation for a Brighter Future,” will have something to offer everyone on your PH care team. Attendees can participate in person in Arlington, Virginia, or online.
One session in particular will focus on how to bring all of these experts together to provide the best care for people with PH. During the session,
“Foundation of a Successful Care Team,” speakers from four PHAaccredited PH Care Centers will define how they develop, expand and support their multidisciplinary care team models.
Speakers Michael Eggert, M.D., FCCP; Elise Whalen, M.S.N., APRN, FNP-C, CPN; Melisa Wilson, D.N.P., APRN, ACNP, BC; and Diahann Wilcox, D.N.P., APRN will explore strategies to resolve common challenges as a team and how to provide quality patient care while also caring for their team members’ wellbeing.

After the session, attendees will leave with tools to support or develop their own PH programs, including tips to leverage shared resources and make connections to build or maintain a program. Panelists will share their own experiences on succession planning, training, policies and procedures, and many more practical aspects of working with a multidisciplinary PH team.
Other educational breakout sessions will focus on a range of topics, including how to use case studies to manage patients, tips for discussing risk assessments with patients, and genetic counseling for pediatric patients and their families.
Another reason to bring your whole team is the research poster hall, which features some of the latest scientific advancements in PH. On Friday night, attendees can meet the researchers, network and discuss the research. Virtual attendees can participate in fireside-style chats with authors over Zoom.
Register now and invite all of your colleagues to attend, either in person or online. Visit PHAssociation.org/ symposium to learn more.
The Pulmonary Hypertension Association (PHA) welcomes health care professionals back to Capitol Hill for PH Professional Network (PHPN) Symposium Advocacy Day on Thursday, Sept. 28.
Be sure to arrive in time for this eye-opening opportunity to join your colleagues in person and advocate on behalf of your patients.
After PHPN Advocacy Day 2021, Diahann Wilcox, DNP, APRN-BC, at UConn Health’s Pulmonary, Critical Care and Sleep Medicine Department, shared why Advocacy Day is important to her.



“I know PH. I know my patients. I have witnessed the frustration of navigating through a complex health care system that sometimes did not make sense. Who better to advocate for my patients than me?”
Kristine Ritenour, RN coordinator for the PH program at Medical University of South Carolina said, “This is another way to spread awareness of PH. Our lawmakers can't do anything to help us if they don't know how. And PHA gives us the tools to get the conversation started with specific asks that can ultimately benefit our patients.”
When you participate in Advocacy Day, you have the opportunity to make a difference in the lives of your patients in a fun, supportive environment. No advocacy experience is needed, as in-person training and talking points are provided. PHA will schedule the
legislative visits and assign attendees to small groups based on legislative district, including a PHA staff person or experienced advocate in each group.
“The experience can be profound,” says Rebecca Fenton, R.N., clinical nurse coordinator at NYU Langone Health. “We have unbelievable stories. It's worth taking the time off.”
Of her first Advocacy Day in 2017, Diahann was a bit nervous. “But the staff at PHA prepared me to speak about legislation pertaining to PH and provided a script of what to say to the legislative staff. Plus, I was partnered with other PHPN members from my New England region for support.”
Legislators listen when medical professionals bring their unique perspectives to Capitol Hill and voice their patients’ concerns. Join PHA in educating more than 80 new lawmakers about critical treatment access challenges facing the PH community.
“When I met with the legislative staffers, I spoke of who I was, where I was from, and why I was there. I know PH, the legislators and their staff don’t.
This was my opportunity to tell the PH story and why my congressman should support legislation that impacted patients with PH whom they represent,” Diahann says.
“Since that first PHPN Advocacy Day, I have felt empowered to reach out to my legislators about all kinds of issues that affect the people I take care of. But I still feel the frustration of my patients and colleagues. Our work is not done; I encourage you to take that extra day at Symposium and advocate,” she urges.
Jeanette Merrill-Henry, RCP, RRT-NPS, PH coordinator at LLUMC, adds, “Engaging our local representatives in Washington, D.C., and placing a human touch on impactful legislation is one of the best opportunities we have to speak up for the patients and families who cannot speak for themselves. The more voices and faces we can put toward an issue the more we can accomplish together.”
Check the Advocacy Day box on your Symposium registration form to join us. Visit Symposium.PHAssociation.org/ Advocacy-Day.
Like many 16-year-olds, Cash Harpp goes to school and loves playing video games. However, he needs continuous high-flow oxygen to get through his school day.

Cash, who was diagnosed with pulmonary hypertension (PH) in 2015, has needed supplemental oxygen since elementary school. Throughout his childhood, he’s had to use compressed oxygen tanks, called e-tanks. The heavy green canisters need their own wheeled cart to move them around, so Cash pulls the equipment behind him as he navigates the halls of his school. Pulling the oxygen is particularly difficult because Cash has the use of only one hand.
The Harpp family of Indianapolis, Indiana, has faced many struggles related to Cash’s supplemental oxygen needs. Their story is typical of others who don’t have access to the most appropriate type of oxygen for their needs.
Supplemental oxygen is a vital component of treatment for many people with PH. Limited forms of oxygen are available to people who struggle with the physical demands of heavy oxygen canisters.
Although liquid oxygen offers the highest degree of mobility and highest quality of life for those with high-flow oxygen needs, many oxygen suppliers no longer provide it. This
lack of options limits PH patients’ engagement in everyday activities and sometimes leaves them homebound when they might otherwise be able to work or go to school.
The Pulmonary Hypertension Association (PHA) recognizes the importance of appropriate oxygen delivery and is working with other patient organizations to secure oxygen access reform. [See sidebar, Page 28.] Oxygen access reform will help patients who lack recourse when medical equipment suppliers are
unresponsive about problems with oxygen equipment. PHA seeks to ensure accountability and prioritize patient-centered care related to oxygen supply.
The Harpps are acutely aware of the need for reform. At the beginning of 2022, the family finally secured a portable oxygen concentrator. Now Cash can wear the oxygen concentrator on his back, significantly improving his quality of life.
“Cash has more energy after school, and he actually wants to go out to eat with the family now that he has the portable concentrator,” dad Jeff Harpp says. “With the e-tank it was too difficult for him to go out to the store; he didn’t want to do things with us outside of the house.”
However, challenges remain: The machine has a two-hour battery life, so Cash must plan his schedule around access to a wall outlet several times a day. And Jeff has had an infuriating battle trying to keep his son’s portable oxygen concentrator running.
Almost as soon as the equipment arrived, it stopped working. It took the family months to get a technician to look at it and tell them the battery was faulty. Just a few weeks after the replacement battery was installed, the machine again stopped working. That time the problem was with the column that converts air into medical grade oxygen. After 10 months of reaching
out with minimal response, multiple delays, and poor communication from their equipment supplier Lincare, Jeff finally secured the replacement part in February 2023.

“I can’t calculate the number of hours I tried to get a response,” Jeff says. “I still hear the hold music in my sleep. It has never taken fewer than 45 minutes for me to reach someone at Lincare.”
Jeff waited more than a month to hear from Lincare after filing a complaint. The response didn’t address his concerns. “The ability to complain
is made so difficult that people are discouraged from reaching out. It’s shameful.”
Another person affected by liquid oxygen shortages is Barbara Linser of Cincinnati. Barb, who has lived with PH for 22 years, had a relatively active life, thanks to the liquid oxygen treatment her doctor prescribed.
Her lifestyle changed when Lincare stopped delivering liquid oxygen without notice and began providing e-tanks in March 2021.
Liquid oxygen tanks are light enough to be strapped to the back so patients don’t have to carry them by hand. They hold a sufficient volume of oxygen to provide a continuous flow for six to eight hours so Barb can breathe easily while walking. E-tanks are heavier and hold a smaller volume of oxygen, so they sustain her for only a fraction of the time.
The forced transition to the cumbersome e-tanks caused a steep decline in Barb’s quality of life. She now struggles with routine errands and her travel is limited.
“Before I lost the liquid oxygen system, I could play with my grandkids

‘I can’t calculate the number of hours I tried to get a response. I still hear the hold music in my sleep.’
JEFF HARPP
freely and move around easily,” Barb says. “After that time, I have not even been able to see them as much. I am unable to get to many of their games and other activities like concerts, plays and grandparents day at their school. It breaks my heart.”
In August 2022, Barb’s youngest son got married. Although she attended his wedding, she couldn’t have the mother-son dance she had been looking forward to because of the difficulty of maneuvering her e-tank.
“The amount of hassle with this oxygen option is so much, moving it in and out of the car, running out of the canisters. The whole day is full of hassle.
The new limitations have caused Barb to become depressed. At a medical visit shortly after losing access to liquid oxygen, Barb’s PH specialist said, “I’ve never seen you this bad.”
Her mood isn’t the only thing that has declined. The next pulmonary function test Barb took after losing access to liquid oxygen showed a significant downturn, and it has since remained at that level.

It can be difficult to imagine why oxygen wouldn’t be readily available to those with lung disease. With Medicare’s increasing focus on curtailing costs, suppliers often choose to substitute less expensive alternatives, replacing supplies of liquid oxygen with heavy tanks that are hard to move and hold less. That creates problems for oxygen users who find it increasingly difficult to participate in family and community activities that extend beyond medical clinics and home.
The oxygen access problem became so widespread that more than two dozen health care organizations including PHA came together this year to call for legislative reform. Since access to portable, accessible and readily available oxygen translates to a better quality of life, Barb and the Cash Harpp family are just two among thousands of patients with lung disease signing petitions. “It’s hard enough with this disease, and this [lack of access] makes it harder, not easier,” Barb says.
If you or someone you care for have challenges with receiving or using oxygen, whether you have a home concentrator, e-tank or liquid oxygen, let us know.
The Pulmonary Hypertension Association (PHA) needs your help to bring the pulmonary hypertension community’s voice to Congress and demand reform to address the challenges associated with supplemental oxygen. Your stories make PHA a more powerful and effective advocate for the community.

Visit PHA’s Advocacy Action Center at PHAssociation.org/ advocate, and use our message template to tell your legislators how access to supplemental oxygen has affected your life.
Reach out to PHA Advocacy and Treatment Access Program Manager Jaeger Spratt to share your experience and learn more about PHA’s advocacy efforts. Email Advocacy@PHAssociation. org or call 301-565-3004 x758.
‘Before I lost the liquid oxygen system, I could play with my grandkids freely and move around easily. After that time, I have not even been able to see them as much.’
BARB LINSER
May marked the end of federal measures to extend public health care benefits during the COVID-19 pandemic. That means many people will no longer receive health care benefits that were available during the pandemic.
Although COVID-19 continues to affect people three years after the World Health Organization declared a pandemic, the public health emergency expired May 11. Find out how this might affect your health care coverage or benefits:
As of April 1, states had the option to begin disenrolling people no longer eligible for Medicaid coverage. The Families First Coronavirus Response Act enacted in 2020 ensured that no one who received Medicaid coverage during the pandemic could lose it without personally opting out. The law required state Medicaid programs to continuously enroll them throughout the emergency period, regardless of changes in eligibility.
States have up to 14 months to redetermine eligibility and disenroll those no longer eligible. Some states will take the full 14 months, while others are disenrolling beneficiaries much more quickly.
The Georgetown University Health Policy Institute tracks how states are handing Medicaid disenrollment.
Find your state: ccf.georgetown. edu/2022/09/06/state-unwindingtracker.
Take these steps to retain your insurance coverage:
• Update contact information. Log into your account online or call your state Medicaid program to ensure Medicaid has your current contact information. Find the phone number for your state Medicaid program: medicaid.gov/about-us/beneficiaryresources.
• Watch your mail. The process and timetable for disenrolling people no longer eligible for Medicaid differs by state. Always promptly open communications from Medicaid.
• Complete re-enrollment forms. If you receive a re-enrollment form from Medicaid, complete and return it promptly. If you lose your Medicaid coverage because you don’t return the form in time, you will have to re-apply.
• Explore other insurance options if disenrolled. The health insurance marketplace has a special enrollment period for those no longer eligible for Medicaid or CHIP because of the expired pandemic measures. Visit healthcare.gov to learn more.

With the end of the public health emergency, Medicare and Medicare Advantage plans no longer must provide free, home-based COVID-19
testing and treatment. Many private insurance plans will stop providing free COVID tests at the same time. For those on Medicaid, at-home tests will be covered at no cost through September 2024.
However, COVID-19 vaccines will remain free to all people regardless of insurance coverage as long as the supply of federally purchased vaccines lasts.
Thanks to the advocacy work of PHA and other organizations, flexibilities introduced during the pandemic for Medicare’s telehealth benefits will remain in place until Dec. 31, 2024.
QUESTIONS? Contact PHA’s treatment access program at 301-565-3004 x758 or email Insurance@PHAssociation.org. Visit PHAassociation.org/ patients/insuranceand-treatment-access for more information.
Our Kathryn Ann McCarthy was born prematurely in January 1983. She was a 2-pound, 10-ounce little preemie and hydrocephalic.

after her PH diagnosis. Through these relationships we found PHA. Although it was too late for Katie, PHA provided much needed support to our family after Katie’s death.
BY DEBBIE MCCARTHYKatie had her first ventriculoatrial shunt surgery when she reached 4 pounds. The shunt was inserted to transfer cerebrospinal fluid from the cerebral ventricle to the right atrium. Katie had some motor skill issues, but she lived a normal life despite needing procedures when the shunt failed.
In August 2012, Katie’s doctors found her lungs were challenged and affected by primary pulmonary hypertension, now known as pulmonary arterial hypertension (PAH). Katie was 29.
Despite a strong fight by pulmonologists from Newark Beth Israel and UPenn Medical Center, the disease took our Katie at age 30 on April 30, 2013.
Katie’s experience brought our family to the world of the Pulmonary Hypertension Association (PHA), the need to draw attention to the littleknown disease of PH, and the impact it has on all lives both young and old.
We worked closely with the multitude of doctors and treatment personnel who administered the lifesaving drugs that sustained Katie
Our friends and family formed our first PHA O2breathe walk in May 2015. Our sMiles for Katie team participated in this fundraiser at the South Street Seaport New York City wearing our new yellow team t-shirts.

We walked again in June 2016 in the same event in NYC and a similar event in October 2016 at the Philadelphia Zoo. Our last walk in June 2017 unfortunately was the final PHA walk in New York City.
We continued to raise awareness locally and raised more than $10,000 for O2breathe in Katie’s honor.
Proudly, the sMiles for Katie team is made of Katie’s sisters, Sarah Miltner, Molly Eagelton and Emma McCarthy, along with other family members and close friends who share in the mission and love of Katie’s memory.
In 2016, we knew we needed to do more to help fundraise for PHA and bring more awareness of PH to the public. sMiles for Katie Inc. was born as a non-profit 501(c)(3) public charity in Belford, New Jersey.
With this tax- exempt charity, we were able to start our own
DEBBIE AND STEVE MCCARTHY of Belford, New Jersey, shared this remembrance of their daughter, Katie.Above: Katie's family attends a 2016 PHA fundraiser in New York City. Opposite: Katie’s family at a 2016 PHA fundraising walk in Philadelphia. Debbie is seventh from right and Steve is sixth from right.
PHundraising events. We also started a “smilesforkatie.org” website and Facebook page to provide information on our events and on PH support.
This was the next step towards our vision to bring awareness to PH while honoring Katie’s memory. The mission of sMiles for Katie is dedicated to bringing awareness to PH and financial support to the Pulmonary Hypertension Association. PHA’s efforts to develop lifesaving drugs and find a cure for this disease brings hope to all who suffer from this deadly but little-known disease. All proceeds go to Pulmonary Hypertension Association and to advocate in our area.
sMiles for Katie’s first PHamily PHun Phundraiser was held on May 7, 2016. Donations of food, baskets,
raffles and music brought us all together.
Since then, we have had several more fundraising events for PHA. In seven years, we have raised and donated approximately $71,00 to PHA in honor of our Katie.

As a special thank you, the Middletown Mayor Tony Perry and the township committee proclaimed April 30, 2022, as Pulmonary Hypertension Awareness Day in Middletown Township in memory of Kathryn Ann “Katie” McCarthy.
If sMiles for Katie can help save one life by bringing awareness to this little-known disease and financial support for researchers and doctors who work tirelessly to develop better medicines to treat PH, then we know
Katie’s memory has helped achieve those goals.
Learn about free bereavement resources at PHAssociation.org/ bereavement. Memorialize your loved one through a one-time gift of cash or other assets. Or consider making a recurring donation. Visit PHAssociation.org/ donate/information.
Where you live, your socioeconomic status and your race/ethnicity can impede your access to fair, affordable and appropriate pulmonary hypertension (PH) treatment. To explore how social determinants affect care disparities, Pathlight interviewed program directors and coordinators from Pulmonary Hypertension Association-accredited PH Care Centers.
One example of a health disparity is underrepresentation of minority populations in PH registry data. Multiple factors play into this disparity, including language barriers and distrust of healthcare providers among minority communities, says Vinicio de Jesus Perez, M.D., a PH physician at Stanford University. A potential solution would be to offer registry consent forms in several languages. For example, the PHA Registry offers forms in Spanish or English. Forms for other PH registries might be in only English.

Another way to enroll people from more diverse backgrounds is for PH coordinators to use translators when introducing a PH registry, Dr. de Jesus Perez suggests. More community outreach efforts could raise awareness about PH and open clinical studies, he says.
Geography is another major factor in care access. Lynn Brown,
M.D., Ph.D., associate program director at Intermountain Medical

Center in Murray, Utah, notes that PH Care Centers are scarce on the West Coast. Her center often cares for people who live miles from paved roads. For those patients, Dr. Brown’s care team depends on local care providers to be partners in first-line care. Those care providers might be qualified to perform some tests, such as six-minute walk tests or right heart catheterizations, but they might not have the resources to do them. That means people who need catheterizations or other procedures requiring PH specialist care must travel long distances.
But traveling up to hundreds of miles may not be an option, depending on income and other socioeconomic factors. Jennalyn Mayeux, D.N.P., PH coordinator at the University of Utah, says some patients qualify for hundreds of thousands of dollars in approved medical therapies, but they don’t have housing security. Some might not have access to a bathroom, which is problematic for people who need diuretics. Others might not have access
to healthful, affordable food that won’t worsen their conditions.
Drs. Brown and Mayeux noted that telehealth and virtual patient visits have become essential in reaching people affected by geographic and socioeconomic challenges. But those patients also would benefit from financial aid for transportation, Dr. de Jesus Perez says. Dr. Mayeux agrees, adding that insurers for patients living in rural communities should be required to reimburse for transport or cover telehealth visits for access to PH Care Centers.
Learn how socioeconomic, racial and ethnic disparities affect PH diagnosis and treatment in this 2021 article from Advances in Pulmonary Hypertension, PHA’s free quarterly journal. Visit meridian. allenpress.com/aph/issue/21/2.
Pulmonary Hypertension Association has changed the date for PHA 2024 International PH Conference and Scientific Sessions. The conference is now set for Aug. 15-18, 2024, at the JW Marriott in Indianapolis. The new date allows the Scientific Sessions to focus on new guidance and findings from the seventh World Symposium on Pulmonary Hypertension (PH) in Barcelona, Spain. PHA 2024 will offer the latest information about PH research, treatment and disease-management, as well as networking events, support group meetings and celebrations. Health care professionals can earn continuing education credit for attending sessions and abstract presentations. General sessions bring together patients and health care professionals for inspirational, informative presentations of interest to the entire PH community. PHAssociation.org/PHA-conference.

Pulmonary Hypertension Association (PHA) members have a new way to manage their membership dues and get discounted rates. PHA is now offering multi-year membership enrollment, which means you can sign up for several years at once. The more years you enroll, the greater your discount will be:
• Two years: 7% discount
• Three years: 10% discount
• Four years: 15% discount
People with PH, caregivers or family members who have financial difficulties can request free general membership. Call 301565-3004 or visit PHAssociation.org/join.
Morethan 200 people participated in the Pulmonary Hypertension Association (PHA)’s Southern California O2breathe Walk. The April 15 event in Long Beach, California, raised more than $17,000, almost double the 2022 total. Mo’s Silver Jubilee was the top team, raising $3,100. The second highest fundraising team was PHENOMENAL Cayla, followed by Moni’s PHight 2 Breathe. Monica Sanchez was the top individual donor, raising $1470, with Monica Penaranda following closely with $1,150. Newly diagnosed patient Sarah Currie arrived for her first walk with an in-person donation of $1,100.

■ PHA Events
■ National O2breathe Events Community Fundraising Events
JULY
JULY 20
Paddle the Gallup Ann Arbor, Michigan PHAevents.org/paddle2023
JULY 22
PH Warrior Walk
Claremont, New Hampshire PHAevents.org/phwarrior2023
JULY 29
PH Community Workshop
Burlington, Massachusetts
JULY 30
Boston O2breathe Walk
Boston PHAevents.org/boston2023
AUG. 12
AUGUST
Northern California O2breathe Walk San Francisco PHAevents.org/nocal2023
AUG. 26
Philadelphia O2breathe Walk Philadelphia PHAevents.org/philly2023
AUG. 27
PH in the Park Denver PHAevents.org/ phinthepark2023
SEPT. 9
Chicago O2breathe Walk and 5K Chicago PHAevents.org/chicago2023
SEPT. 16
Glowing for Kassie Lawrenceburg, Tennessee PHAevents.org/ glowingforkassie2023
SEPT. 28-30
PHPN Symposium
Arlington, Virginia
PH Awareness Month
NOV. 4 Monrovia Fun Run Monrovia, California
See our calendar at PHAssociation.org/events.
QUESTIONS?
Contact us at 240-485-0762 or events@PHAssociation.org.
Since the Pulmonary Hypertension Association (PHA) began publishing Pathlight, “Passages” has provided a place to memorialize people with pulmonary hypertension who pass away. PHA extends its sympathy to the families and friends of these individuals and rededicates itself to its mission in their memory.
Patricia Ashburn
Linda S. Clark
Jimmie L. Crapps
Madlyn A. Cullen
Sandra Devine
Rudolph Dunn
Paul E. Glover
Eileen N. Herbst
Ann Mattson
Susan Matulewicz
Charles McCormack
Jeannette M. Morrill
Nancy Mory
Susan Rae
Patricia V. Sanabria
Loretta Shufford
Suanne Tuomi
Anne Wingate
To honor those who have included PHA in their estate plans or whose legacies have been realized, PHA created the Legacy of Hope Society. PHA is pleased to recognize the following members:
Laura* and Rino*
Aldrighetti*
Alice A. Arnott*
Sandra A. Awood*
Dauna L. Bauer*
Sylvia M. Becherer*
Joan F. BennettSchenecker*
Kris L. Best
Gloria G. Blodgett*
Dorothy E. Bradley*
Mary M. Brady*
R. J. Braun
Roberta F. Browning* and Lee A. Broadbent
Rita and Bruce Brundage
Colleen Brunetti
Stephen Carter-Hicks
Colleen and Shawn Connor
Jane P.* and Harold P. Cooper
James F. Corbett*
Nicole M. Creech
Laura H. D'Anna
Charles W. DeVier, III*
Linda M. Feibel*
Barbara T. Gamer
Stacey Gausling*
Franklin D. Gillespie*
Jeffery S. Hall*
Tammy A.* and Dean S. Hazen
Mary Jan Hicks
Carl Hicks, Jr.
Phyllis M. Hill*
Jackie Holt
Richard L. Horrocks
Constance G. Ives*
Terri L. Jakuboski*
Stanley T. Jusinski
Laura J. Kelly*
James Kenney
Jessie Kohler-Wenninger
Terri L. Kopp*
Debbie L. and Mitchell
Koppelman
Frank D. Koppelman*
Dee* and Walter Kruger*
Mary Jo* and Thomas Linnen*
Sally Maddox*
Bonnie and Michael D. McGoon
Joseph W. Mihuc*
Linda Miles*
Karen S. Moody
Larry D. Moody
Pamela R. Morris
Marjorie D. Mott*
Joyce L. Mowrer*
Pamela and Timothy O'Connor
Dorothy M.* and Harry J. Olson*
Theresa "Terry" E. (Cavanaugh) O'Reilly*
Rita and Guy Orth
Patricia R.* and Gerald D. Paton*
Cynthia and John R. Pickles
Jean D. Pitcher*
Carol L. Powell*
Frances A. Price
Carol J. Posner* and Marc Priore
Susan Tess Rae
Diane Ramirez
Dorothy A. Ryan
James Ryan*
Louise C.* and Gene P.* Salvucci
Judith and Edwin L. Simpson
Kelley Skumautz
Joanne Sperando
Marcia and Jack Stibbs
Helena M. Strauch*
Douglas R. Taylor
Frank A. Tobac*
Martha and Carlos Torres
Deborah J. and Roger K. Towle
Carol B. Ungar
Carol E. Vreim
Daniel R. Walsh*
Andrea and Stephen L. White
The accuracy of this list is important to us. Please contact the PHA office at 301-565-3004 x746 or Passages@PHAssociation.org to share the name of your recently deceased loved one or report an error or omission. Your donations in memory of others, in honor of others and in support of our mission mean so much to the entire PH community, and we thank you.
Gloria J. Lang*
Marie* and Ronald J. Levendoski
* deceased members
If you haven’t notified us of your intended gift, email us at development@PHAssociation.org so we can acknowledge your generosity.
