OF DIRECTORS RETREAT









August 2022: PMC was ranked by Forbes® as the #1 (Best-In-State) Hospital Employer in Kentucky.
May 2022: Pikeville Medical Center (PMC) has received the American College of Cardiology’s NCDR Chest Pain � MI Registry Platinum Performance Achievement Award for 2022.
February 2022: PMC Among Top in State and Nation in Six Areas of Medical Excellence and Patient Safety by CareChex/Quantros. Top 10% of Hospitals in the Nation for Medical Excellence:Hip Fracture Care, Top 10% of Hospitals in the Nation for Patient Safety: Heart Failure Treatment and Heart Attack Treatment, Top 10% of Hospitals in the State for Medical Excellence: Hip Fracture Care, Top 10% of Hospitals in the State for Patient Safety: Heart Failure Treatment and Heart Attack Treatment.
November 2021: PMC Employees, CEO Donovan Blackburn and Infectious Disease Specialist Dr. Fadi Al Akhrass recognized by Pikeville City Commission as Extra Mile Heroes as part of the “Extra Mile America” initiative
October 2021: Chest Pain Center reaccredited by the American College of Cardiology Accreditation Services, version 7; First hospital in Kentucky to be awarded this version of accreditation and the 5th in the nation
October 2021: Sleep Lab re-accreditation by American Academy of Sleep Medicine
September 2021: PMC recognized as co-business of the year by Southeast Kentucky Chamber of Commerce
August 2021: Joint Commission Re-Accreditation for Hospital and Home Care
August 2021: College of American Pathologists Accreditation for Lab services
July 2021: Geriatric Emergency Department Accreditation, level 3 Bronze by American College of Emergency Physicians
July 2021: Laboratory Services re accredited by College of American Pathologists
May 2021: Hospital and DME re-accreditation by Joint Commission (Deemed status)
May 2021: Pikeville Medical Center is a recipient of the 2021 Chest Pain MI Registry Platinum Performance Achievement Award, awarded by the National College of Cardiology
March 2021: Hip Fracture, Hip and Knee Replacement re-certification from Joint Commission
March 2021: Hospital License Renewal by Kentucky Office of Inspector General
February 2021: ACGME re-accredited PMC's Family Medicine Residency Program
February 2021: The Joint Commission re-certified PMC's Advanced Primary Stroke Center
February 2021: Utilization Review Accreditation Commission (URAC) accredited PMC's Outpatient pharmacy
November 2020: PMC was ranked by Forbes® as the #1 (Best-In-State) Hospital Employer in Kentucky.
October 2020: PMC was ranked as the #1 Hospital in Kentucky and in the top 100 in the nation for Heart and Vascular Care (CareChex by Quantros)
October 2020: PMC received the Gold Performance Award (Chest Pain/MI Registry) by the American College of Cardiology (NCDR)
July 2020: Pikeville Medical Primary Stroke Center received the American Heart Association/American Stroke Association's Get With The Guidelines® Stroke Gold Plus Quality Achievement Award with Target: Stroke Honor Roll.
June 2020: Comprehensive Pharmacy Services, the nation's largest pharmacy management organization, honored Pikeville Medical Center with the Pharmacy Site of the Year Award.

June 2020: Pikeville Medical Center's cardiac cath lab has received a Cardiac Cath Lab Percutaneous Coronary Intervention (PCI) Accreditation from the American College of Cardiology.
June 2020: Received Cardiac Cath Lab Certification from American College of Cardiology
January 2020: Pikeville Medical Center receives certification from the American Society of Clinical Oncology, Quality Oncology Physician Improvement (QOPI)
2020: Appalachian Valley Autism (AVA) Center received certification from International Board of Credentialing and Continuing Education Standards
January 2020 – 2019: Pikeville Medical Center was named a Top 100 Hospital in the Nation for Heart Attack Treatment and Number 1 in Kentucky for Vascular Surgery from Quantros Quality Check.
January 2020: American Academy of Sleep Medicine accreditation for Sleep Center (Main campus)
January 2020: Pikeville Medical Center receives certification from the American Society of Clinical Oncology, Quality Oncology Physician Improvement.
January 2019-2020: Pikeville Medical Center was named a Top 100 Hospital in the Nation for Heart Attack Treatment and Number 1 in Kentucky for Vascular Surgery from Quantros Quality Check.
PMC was awarded a Level IV Accreditation as a Chest Pain Center with PCI by the Society of Chest Pain Centers. This highly-acclaimed distinction made PMC one of the first five in the nation and the first hospital in Kentucky to earn this accreditation, meaning PMC can provide the whole continuum ofcareon-site,fromdiagnosticstoheartsurgeryprocedures.

TheAmerican College of Cardiology (ACC) recognized PMC for its expertise and commitment to treating patients with chest pain. Based on rigorous onsite evaluation of the staff's ability to evaluate, diagnose and treat patients who may be experiencing a heart attack, PMC was awarded Chest Pain Center Accreditation with Primary Percutaneous Coronary Intervention (PCI).
The Society of Cardiovascular Patient Care (SCPC) awarded PMC with full Atrial Fibrillation Certification status for its commitment to quality patient care and meeting or exceeding a widesetofstringentcriteria.
The American College of Cardiology (ACOC) Accreditation Services awarded PMC for its demonstrated expertise and commitment in meeting or exceeding in the criteria for diagnostic catheterizations and percutaneous coronary intervention(PCI)procedures.

PMC is one of the nation's 225 hospitals to receive theAmerican College of Cardiology's (ACC) NCDR Chest Pain-MI Registry® PlatinumPerformanceAchievementAward. PMC was recognized for its commitment to provide a higher levelofcareforheartattackpatients.

While federal funding helped

rural hospitals
by Clarissa Donnelly-DeRoventhe
Many rural hospitals see more uninsured patients, more patients who are covered by Medicare or Medicaid, and fewer private insurance patients than urban hospitals do. Any changes to those federal programs can have a disproportionate impact on rural hospitals’ ability to stay financially afloat.



That’s the conclusion of the Center for Healthcare Quality and Payment Reform, whose recent study sees 500 hospitals at immediate risk for closing within two years and more than 300 others at high risk within five years. The grim assessment by the policy center found the problems spread across the country, and that the threats will persist even if the pandemic ends because rising costs are outrunning revenue.



 By: Ayla Ellison March 4th, 2022
By: Ayla Ellison March 4th, 2022
More than 500 rural hospitals in the U.S. are at immediate risk of closing because of financial losses and lack of financial reserves to sustain operations. Across the U.S., 892 hospitals — more than 40 percent of all rural hospitals in the country — are either at immediate or high risk of closure.




nurses
By: Marissa Plescia

 CFO REPORT
BY: NathanTucker September 15th, 2022
CFO REPORT
BY: NathanTucker September 15th, 2022
A new analysis from management consulting firm Kaufman, Hall & Associates indicates hospitals and health systems continue to face intense pressure on staff and resources while also dealing with rising expenses for supplies, drugs and equipment, and the workforce, according to a Sept. 15 special bulletin from the American Hospital Association


These trends are expected to continue through 2022, with hospitals and health systems losing billions of dollars. Left unaddressed, these challenges can jeopardize access to essential healthcare services for patients, according to the bulletin.
Challenges in the first half of 2022 tested healthcare organizations with the impact of COVID-19 surges, increased expenses, and a lack of relief funding for economically struggling institutions. https://www.beckershospitalreview.com/finance/2022-the-most-financiallydifficult-year-for-hospitals-health-systems-since-start-of-pandemic.html? origin=BHRE&utm_source=BHRE&utm_medium=email&utm_content= newsletter&oly_enc_id=6799J6353967F9A
 BY: NathanTucker
BY: NathanTucker
15th, 2022
a result, the most optimistic projections for 2022 indicate margins will be down 37 percent compared to pre-pandemic levels. More than half of hospitals are operating in the red, according to Kaufman, Hall & Associates, and forecasts for the remainder of 2022 indicate that margins could be down by 133 percent compared to pre-pandemic levels. More than half of hospitals — 53 percent — are projected to have negative margins for the rest of the year.
Furthermore, over two-thirds of hospitals

forecast to operate in the red, with expenses
2022, leading to an increase of $135 billion over 2021. Labor expenses are projected to increase by $86 billion, while non-labor expenses are projected to increase by $49 billion.
to increase


 BY:Ayla Ellison
BY:Ayla Ellison
21st, 2022
More than six dozen hospital CEOs have left their roles this year, according to a Sept. 21 Challenger, Gray & Christmas report. Six hospital CEOs left their positions in August, bringing the total number of departures to 77 for this year. Sixty-eight hospital CEOs left their roles in the first eight months of 2021.

"
said AndrewHospitals continue to be hammered on the labor front Challenger, senior vice president of Challenger, Gray & Christmas. "The staff shortages, access-to-care concerns, legal issues, and resource management issues continue to create challenges for hospital leadership, and leaders themselves are not immune from the burnout felt at all levels.

September 21st,
Operating margins were up in June compared to May, but expenses remain at historic highs, leaving hospitals and health systems with cumulatively negative margins, according to Kaufman Hall.

Four things to know:
1. The median change in operating margin was up 30.8% in June over May, but down 49.3% from June 2021, according to the report released Aug. 1.
2. Hospitals are seeing improved volumes and reduced expenses monthover-month, but will likely end up with historically low margins for the remainder of the year, according to the report.
3. "Decreases in acuity, escalations in outpatient volume and easing costs in June show that hospitals are faring better month-over-month but are nowhere near pre-pandemic levels," the report stated.
4. Contract labor costs in June were down from May as demand wanes, but rising employee pay and additional labor pressures are keeping overall expenses high, according to the report. https://www.beckershospitalreview.com/finance/hospital-margins-still-in-red-halfway-through-2022kaufmann-hall-says.html?origin=BHRE&utm_source=BHRE&utm_medium=email&utm_content= newsletter&oly_enc_id=6799J6353967F9A
20th, 2022
Due to ongoing inflation and higher labor, supply and capital costs, nonprofit hospital margins

see further erosion, Fitch reported July 19
ongoing margin
a result of the
and materially higher inflation,
be compelled to attempt to secure much higher rate

their
to the report.
also facing similar
resulting in increased

 By: Marissa Plescia May 11th, 2022
By: Marissa Plescia May 11th, 2022
Kaufman Hall's most recent flash report showed that median hospital operating margins were negative for the first three months of 2022. The median hospital operating margin in March was -2.43 percent, up from -3.99 percent in February and -4.52 percent in January, according to the report.
"The pandemic made longstanding labor challenges in the healthcare sector much worse, making it far more expensive to care for hospitalized patients over the past two years," Erik Swanson, senior vice president of data and analytics at Kaufman Hall, said in a May 11 news release. "Skyrocketing labor costs, decreasing patient volume and lower revenues create a perfect storm for steep declines in profit margins. Hospitals now face a number of pressures to attract and retain affordable clinical staff, maintain patient safety, deliver quality services and increase their efficiency." https://www.beckershospitalreview.com/finance/a-perfect-storm-labor-expenses-rise-37from-pre-pandemic-levels-kaufman-hall-finds.html?origin=BHRE&utm_source=BHRE&utm_

 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT

 By: Marissa Plescia April 28th, 2022
By: Marissa Plescia April 28th, 2022
"Our operating results during the first quarter of 2022 reflect continued uncertainties related to the COVID-19 pandemic, as well cost as escalations related to the nationwide shortage of nurses and other clinical staff and support personnel," "As a result, our labor costsUHS said in the report. were higher than anticipated, and patient volumes at our behavioral healthcare facilities , which unfavorablywere lower than anticipated impacted our operating results during the first quarter of 2022." https://www.beckershospitalreview.com/finance/for-profit-health-systemsreport-financial-challenges-as-labor-expenses-soar.html

 By:Ayla Ellison July 28th, 2022
By:Ayla Ellison July 28th, 2022
Franklin, TN-based Community Health Systems, which operates 83 hospitals, saw revenues decrease in the second quarter of this year and ended the period with a net loss. "Our results in the second quarter were affected by challenging operating dynamics that included lower than anticipated volume, lower net revenue per adjusted admission, and significant contract labor costs driven by labor market and inflationary pressures," CHS CEO Tim Hingtgen said.
Looking at the first six months of this year, CHS reported a net loss of $327 million on revenues of $6.04 billion. In the first half of 2021, the company posted a net loss of $58 million on revenues of $6.02 billion.
newsletter&oly_enc_id=6799J6353967F9A



 Marissa Plescia May 12th, 2022
Marissa Plescia May 12th, 2022
The 22-hospital system had a net loss of $114.9 million in the three months ended March 31, compared to a net income of $28.3 million the previous year. This can be largely attributed to salaries and wages, which increased by 14.7 percent to $183 million in the third quarter this fiscal year from $159.5 million last year.
"COVID-19 hospitalizations, driven by the omicron variant, peaked at record levels in the third quarter with those inpatients requiring longer hospital stays," the system said in the report. "The omicron surge contributed to declines in other volume, while expenses continued to escalate due to widespread national labor shortages and global supply chain issues coupled with inflation on most other non-labor expenses.” https://www.beckershospitalreview.com/finance/ballad-health-reportsoperating-loss-of-37-3m.html#:~:text=Johnson%20City%2C%20Tenn. %2Dbased,according%20to%20its%20financial%20results


 By:Ayla Ellison August 30, 2022
By:Ayla Ellison August 30, 2022
"Nationwide labor shortages have created staffing challenges that have resulted in increased overtime costs and premium pay for employed caregivers as well as an increase in the utilization of agency nurses and other temporary personnel to meet the demand of patient activity," Cleveland Clinic said in an earnings release. "Supplies, pharmaceuticals and other nonlabor expenses have also increased due to recent inflationary trends and supply chain challenges."
Looking at the first six months of this year, Cleveland Clinic reported a net loss of $1.1 billion on revenue of $6.2 billion. In the same period a year earlier, the health system reported net income of $1.3 billion on revenue of $6 billion, according to the financial documents.


Clinic ended the second quarter of this year

operating income of $155 million,
$451 million
the same quarter
Clinic management

the
a
 By:Ayla Ellison
By:Ayla Ellison

 By:Ayla Ellison
By:Ayla Ellison
The 143-hospital system Ascension's operating expenses climbed to $7.34 billion in the first three months of 2022, up from $6.59 billion in the same period a year earlier. The increase was attributed to several factors, including higher salaries, wages and supply expenses.


 By:Ayla Ellison
By:Ayla Ellison
The 144-hospital system reported operating revenue of $27.98 billion in the year ended June 30, up from $27.24 billion a year earlier.
factoring in nonoperating items, Ascension reported a net loss of $1.8 billion for the 12 months ended June 30. A year earlier, the health system posted net income of $5.7 billion.

facing many
the U.S.
the

other health systems
than half of hospitals
53 percent
the rest of the year.
revenue was up, so w e r e A d v e n t H e a l t h ' s expenses. In the first quarter of 2022, AdventHealth saw its expenses grow to $3.72 billion, up from $3.23 billion recorded in the same period in 2021.


increased expense is primarily a result of elevated premium and contract labor costs and wage inflation resulting from workforce shortages

AdventHealth stated in its financial report. "The system continues to implement
plans to reduce turnover and temporary labor utilization.”

 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
 By:Alia Paavola May 16, 2022
By:Alia Paavola May 16, 2022

The 27-hospital system
In addition to seeing its revenue increase, Advocate Aurora saw its expenses rise nearly 11 percent to $3.56 billion in the three months ended March 31. Advocate Aurora attributed the expense increase to a boost in agency staffing and supply costs.
Overall, Advocate Aurora ended the first quarter of 2022 with a net loss of $253.23 million, driven by losses on nonoperating items. In particular, Advocate Aurora recorded an investment loss of $265.97 million in the first quarter of 2022. In the same period one year prior, Advocate Aurora saw investment gains of $295.73 million and a net income of $351.75 million.

The health system also saw expenses rise. Total operating expenses reached nearly $8.9 billion in the three months ended March 31, up from $8.3 billion in the same period a year earlier. Expenses tied to salaries and benefits increased from $4.2 billion in the third quarter of fiscal year 2021 to nearly $4.7 billion in the most recent quarter.

CommonSpirit closed out the third quarter of fiscal year 2022 with a net loss of $592 million. In the same period of 2021, the health system reported net income of $1.7 billion.

 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT

 By:Ayla Ellison September 23, 2022
By:Ayla Ellison September 23, 2022
CommonSpirit recorded an operating loss of $1.3 billion in the 12-month period ended June 30, compared to an operating income of $998 million a year earlier. "This continues to be a very challenging time for health systems, especially nonprofit health systems like CommonSpirit where a majority of patients are Medicare and Medicaid beneficiaries, " CommonSpirit CFO Dan Morissette said in an earnings release. "As an integrated organization with a broad footprint, we've been able to take many steps to reduce costs and grow revenue. But it's clear we need to do more to improve performance. We will remain focused on growth in the new health care landscape, finding additional cost savings, and lowering contract labor costs while reducing turnover and improving retention by doing even more to support our teams.“
CommonSpirit is facing many of the same financial pressures as other health systems across the U.S. https://www.beckershospitalreview.com/finance/commonspirit-posts-1-3b -annual-operating-loss.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
 By: Marissa Plescia April 29th, 2022
By: Marissa Plescia April 29th, 2022
The system's expenses climbed 16.4 percent, to $1.96 billion, for the first quarter of 2022, compared to $1.68 billion for the same period last year. Salaries, wages and benefits represent a large portion of IU Health's expenses, at $1.14 billion for the first quarter this year, a 25.1 percent increase from the same period last year at $914.37 million.
"We continue to work through the labor shortage by investing in our workforce, particularly patient-facing roles, to ensure we can meet patient demand," Jenni Alvey, senior vice president and CFO of IU Health, said in a news release from the health system. "Additional workforce investments are expected throughout 2022. These investments are made in order to provide the best possible clinical care and to improve the health and well-being of Indiana. The challenges from the pandemic again show the critical need for hospital systems to maintain a strong financial position to be able to manage unforeseen operating challenges and continue serving the patients who depend on us."
https://www.beckershospitalreview.com/finance/iu-health-reports-358mnet-loss-as-labor-expenses-climb-25.html?origin=BHRE&utm_source= BHRE&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A

 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT

 By:Ayla Ellison August 8, 2022
By:Ayla Ellison August 8, 2022
August 8, 2022
Much like the entire health care industry, we continue to address deferred care while navigating COVID-19 surges and associated expenses," Kathy Lancaster, Kaiser executive vice president and CFO, said in an Aug. 5 earnings release. "Kaiser Permanente's integrated model of providing both care and coverage enables us to meet these challenges as demonstrated by our moderate increase in year-over-year operating expenses for the second quarter.“
After factoring in a nonoperating loss of $1.4 billion, Kaiser reported a net loss of $1.3 billion for the second quarter of this year, compared to net income of $2.97 billion in the same period last year loss was. Kaiser said the largely attributable to market conditions. https://www.beckershospitalreview.com/finance/kaiser-posts-1-4b-lossin-q2.html?origin=BHRE&utm_source=BHRE&utm_medium=email& utm_content=newsletter&oly_enc_id=6799J6353967F9A


Mass General Brigham
staffing,
Mass General Brigham
By:Alia Paavolathe expense increase to the use of
facilitate workforce retention,

the severe
to navigate the
General







 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT

 By:Ayla Ellison
By:Ayla Ellison
16, 2022
Providence CFO Greg Hoffman said in the earnings release. "But it has become even more imperative today as health systems across the country face a new reality. "Having served the Western U.S. for more than 165 years, Providence has lived through other economic downturns, past pandemics, and periods of political and social unrest. With the steps we are taking to respond to the times, we will continue supporting caregivers and serving our communities throughout these challenging times, with the mission of Providence enduring for generations to come," Providence President and CEO Rod Hochman

 By:Ayla Ellison
By:Ayla Ellison
the second quarter
 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT

 By:Ayla Ellison
By:Ayla Ellison
20, 2022
89 hospital system, Trinity Health's operating expenses for the first nine months of fiscal year 2022 increased by 4.8 percent year over year to $15.12 billion. The increase was attributed to a $679.8 million increase in labor costs. Contract labor expenses increased 154.2 percent during the nine-month period.
After factoring in investments
non-operating items, Trinity posted net income of $43 million for the first nine months of fiscal year 2022, down from $3.19 billion in the same period
year earlier.
 By:Alia Paavola
By:Alia Paavola
Duvall, who serves as president and CEO of both hospitals, said the layoffs occurred because the hospitals are feeling the financial effects of inflation and a decrease in COVID-19 hospitalizations. Specifically, Mr. Duvall said the

up by 30 percent because of inflation
the
by 2.7 percent.







 HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT
HOSPITAL CFO REPORT: FINANCIAL MANAGEMENT


health system
By:Ayla Ellison September


Several hospitals are scaling back services for a variety of reasons, including financial challenges and staffing issues.
By:Ayla Ellison1. ShorePoint Health Venice (Fla.) is no longer offering emergency services. The 312-bed hospital, part of Franklin, Tenn.-based Community Health Systems, permanently closed its emergency department on Aug. 29 before ending other services. ShorePoint Health said the hospital will close on Sept. 22.
2. Cleveland-based University Hospitals is scaling back care at two hospitals and consolidating services. The health system ended inpatient, surgical and emergency services at UH Bedford (Ohio) Medical Center and UH Richmond Medical Center in Richmond Heights, Ohio, on Aug. 12. The health system attributed the changes to a staffing shortage.
3. HCA Florida Oak Hill Hospital in Brooksville, Fla., announced in August that it closed its inpatient pediatric unit. The hospital cited several reasons for the closure, including the shift to outpatient pediatric treatments and remote monitoring.

4. Hazel Crest, Ill.-based Advocate South Suburban Hospital ended labor and delivery services on Aug. 1. The hospital cited a decline in births as the reason for the change in obstetric services, with a 40 percent decrease since 2015.
5. Davis Regional Medical Center in Statesville, N.C., plans to eliminate most patient services by the end of the year as it transitions to a specialty hospital focused on inpatient behavioral healthcare. The hospital closed its emergency department on Aug. 24.
6. Grand Blanc, Mich.-based Ascension Genesys Hospital will no longer offer inpatient pediatric care after September. The hospital's decision was made based on a decline in pediatric inpatient care numbers, difficulty providing different types and levels of treatment, and close proximity with other https://www.beckershospitalreview.com/care-coordination/17-hospitalsscaling-back-care.html?origin=BHRE&utm_source=BHRE&utm_medium =email&utm_content=newsletter&oly_enc_id=6799J6353967F9A

7. Palomar Medical Center in Poway, Calif., will close its 17-bed geriatric psychiatric space on or before Oct. 31.
8. Williamston, N.C.-based Martin General Hospital closed its intensive care unit on Aug. 1. The hospital said nursing staff shortages are the primary reason for the closure.
9. Huntington, W.Va.-based St. Mary's Medical Center will cease obstetrics services on Nov. 18. The obstetrics unit will transition to a medical/surgical department with a focus on women's health.
10. McLaren St. Luke's Hospital in Maumee, Ohio, is ending labor and delivery services. The hospital will end labor and delivery services between Aug. 31 and Sept. 30.
11. Chippenham Hospital in Richmond, Va., will close its neonatal intensive care unit on Nov. 1.
12. Jefferson, Iowa-based Greene County Medical Center will close its long-term care department by Sept. 28. During a public meeting in July, the hospital's board of trustees unanimously decided that keeping the department open was not cost effective considering the age of the facility and construction expenses.

13. Hicksville, Ohio-based Community Memorial Hospital will close its obstetrics department and end labor and delivery services in September.
14. Raleigh, N.C.-based UNC Health Rex closed its pediatric unit on Aug. 31. The hospital plans to convert the pediatric beds into adult beds.
15. Gallup, N.M.-based Rehoboth McKinley Christian Hospital closed its labor and delivery unit on Aug. 3.
16. Southeast Iowa Regional Medical Center in Burlington closed its skilled care unit and limited patient bed capacity in three additional units following a $40 million operating cost loss.
17. Honesdale, Pa.-based Wayne Memorial Hospital will end outpatient oncology care after its sole oncologist's last day on Sept. 30.


 By:Ayla Ellison
By:Ayla Ellison
 By: Kelly Gooch July 25, 2022
By: Kelly Gooch July 25, 2022

Hospitals and health systems across the U.S. have faced workforce challenges from staffing shortages throughout the COVID-19 pandemic. Now, as COVID-19

are rising, driven largely by the
to struggle with these
July 25.

 By: Molly Gamble May 12, 2022
By: Molly Gamble May 12, 2022
The United States could see a deficit of 200,000 to 450,000 registered nurses available for direct patient care by 2025, a 10 to 20 percent gap that places great demand on the nurse graduate pipeline over the next three years.
make up for the 10 to 20 percent gap, the United States would need to more than double the number of new graduates entering and staying in the nursing workforce every year for the next three years straight. For this to occur, the number of nurse educators would also need to increase.

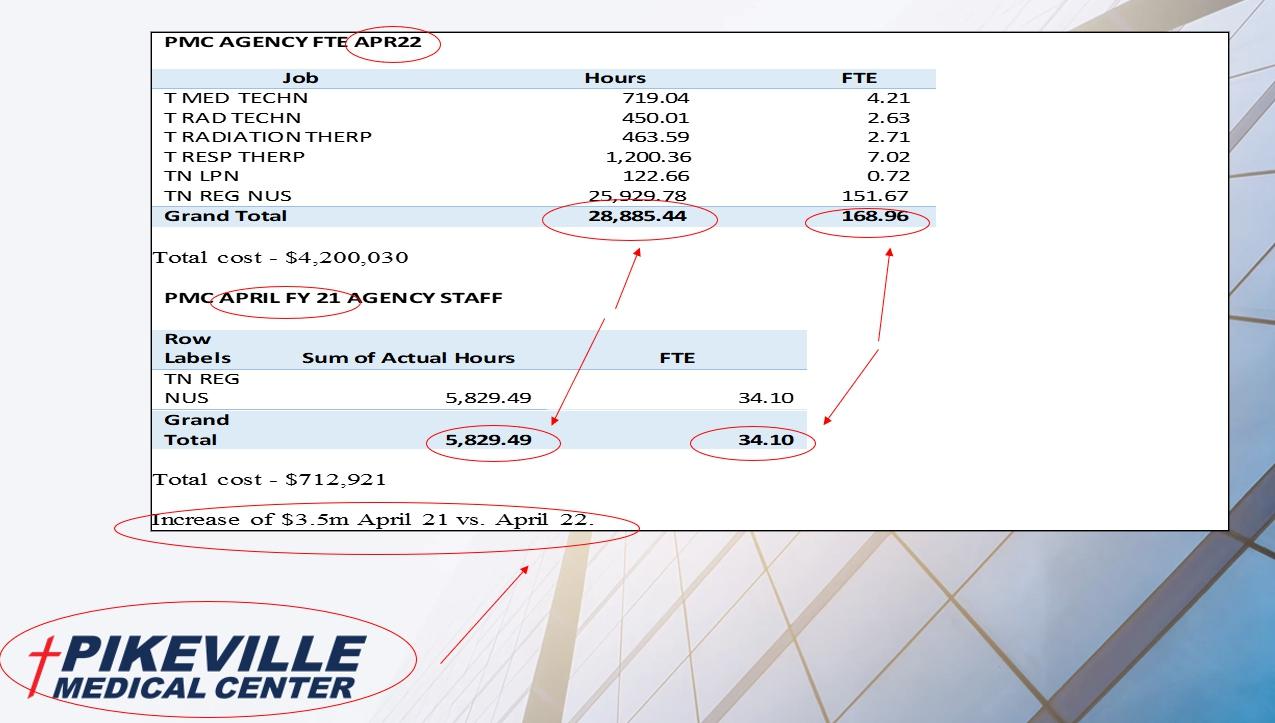
with 6 months to still go in the year projecting over a 1 Billion increase


Results would be: - We shut down services - We shut down beds in a �me of need and growth. Remember our volumes are up. - Reduce the need for other services like lab, environmental, tes�ng and more. - Thus reducing the demand for staff - We reduce services and capacity for our market and pa�ents. Hospitals, including PMC have taken the posi�on to take care of our markets and our staff.








https://www.youtube.com/watch?v=1NNzn0MPm30











https://www.northcarolinahealthnews.org/2022/05/17/billions-in-federal-fundsmay-make-rural-hospitals-look-more-stable-than-they-really-are/ https://www.bloomberg.com/news/articles/2022-03-09/heartland-hospitalsface-wipeout-with-800-at-risk-of-shutdown
https://www.beckershospitalreview.com/finance/892-hospitals-at-risk-ofclosure-state-by-state.html
https://www.beckershospitalreview.com/finance/one-third-of-hospitalsoperating-with-negative-margins-6-other-things-to-know.html?origin= BHRSUN&utm_source=BHRSUN&utm_medium=email&utm_content= newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/a-long-road-ahead-hospitaloperating-margins-negative-for-3rd-month.html?origin=BHRE&utm_source= BHRE&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/2022-the-most-financiallydifficult-year-for-hospitals-health-systems-since-start-of-pandemic.html? origin=BHRE&utm_source=BHRE&utm_medium=email&utm_content= newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/hospital-management-administration /more-hospital-ceos-exit-as-labor-challenges-persist.html?origin=BHRE&utm _source=BHRE&utm_medium=email&utm_content=newsletter&oly_enc_id= 6799J6353967F9A
https://www.beckershospitalreview.com/finance/hospital-margins-still-in-redhalfway-through-2022-kaufmann-hall-says.html?origin=BHRE&utm_source= BHRE&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/inflation-to-erode-nonprofithospital-margins-fitch-reports.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/a-perfect-storm-laborexpenses-rise-37-from-pre-pandemic-levels-kaufman-hall-finds.html?origin =BHRE&utm_source=BHRE&utm_medium=email&utm_content=newsletter &oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/iu-health-reports-358mnet-loss-as-labor-expenses-climb-25.html?origin=BHRE&utm_source= BHRE&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/kaiser-posts-1-4b-lossin-q2.html?origin=BHRE&utm_source=BHRE&utm_medium=email& utm_content=newsletter&oly_enc_id=6799J6353967F9A



https://www.beckershospitalreview.com/finance/mass-general-brighamposts-867m-quarterly-net-loss.html?origin=BHRSUN&utm_source= BHRSUN&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/mass-general-brighamposts-949m-quarterly-net-loss.html?origin=BHRSUN&utm_source= BHRSUN&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/providence-s-operating -loss-hits-510m-in-q1.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A








https://www.beckershospitalreview.com/finance/providence-s-operatingloss-grows-to-934m-as-it-shrinks-leadership-team.html?origin=BHRE &utm_source=BHRE&utm_medium=email&utm_content=newsletter& oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/sutter-health-posts51m-operating-loss-in-q2.html?origin=BHRE&utm_source=BHRE &utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/trinity-health-s-operatingincome-slips-79-as-labor-costs-soar.html?origin=BHRE&utm_source= BHRE&utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/citing-inflation-2-new-york -hospitals-lay-off-4-of-staff.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/10-hospitals-laying-offworkers-0802.html?origin=BHRSUN&utm_source=BHRSUN&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/9-hospitals-laying-offworkers.html?origin=BHRE&utm_source=BHRE&utm_medium=email &utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/for-profit-health-systemsreport-financial-challenges-as-labor-expenses-soar.html











https://www.beckershospitalreview.com/finance/chs-posts-326m-loss-in-q2. html?origin=BHRE&utm_source=BHRE&utm_medium=email&utm_content= newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/ballad-health-reportsoperating-loss-of-37-3m.html#:~:text=Johnson%20City%2C%20Tenn. %2Dbased,according%20to%20its%20financial%20results
https://www.beckershospitalreview.com/finance/cleveland-clinic-reports1b-loss-in-first-half-of-this-year.html?origin=BHRE&utm_source=BHRE& utm_medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/mayo-clinic-operating-income -slips-66-in-q2.html?origin=BHRE&utm_source=BHRE&utm_medium=email& utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/ascension-posts-884mquarterly-loss.html?origin=BHRE&utm_source=BHRE&utm_medium= email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/ascension-reports-1-8bannual-loss.html?origin=BHRE&utm_source=BHRE&utm_medium=email &utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/adventhealth-posts-4177m-loss-in-q1.html?origin=BHRE&utm_source=BHRE&utm_medium= email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/advocate-aurora-posts253m-net-loss-in-q1.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/commonspirit-posts-591m -quarterly-loss.html?origin=BHRE&utm_source=BHRE&utm_medium= email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/commonspirit-posts-1-3b -annual-operating-loss.html?origin=BHRE&utm_source=BHRE&utm_ medium=email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/finance/ohio-hospital-to-lay-off-978 -employees.html?origin=BHRE&utm_source=BHRE&utm_medium=email &utm_content=newsletter&oly_enc_id=6799J6353967F9A

https://www.beckershospitalreview.com/care-coordination/13-hospitalscutting-services-0804.html?origin=BHRSUN&utm_source=BHRSUN &utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
https://www.beckershospitalreview.com/care-coordination/17-hospitalsscaling-back-care.html?origin=BHRE&utm_source=BHRE&utm_medium =email&utm_content=newsletter&oly_enc_id=6799J6353967F9A






https://www.beckershospitalreview.com/care-coordination/hospitalscutting-services-over-staffing-shortages-2.html?origin=BHRE&utm_ source=BHRE&utm_medium=email&utm_content=newsletter&oly_ enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/workforce/hospitals-rob-peterto-pay-paul.html?origin=BHRE&utm_source=BHRE&utm_medium= email&utm_content=newsletter&oly_enc_id=6799J6353967F9A
https://www.beckershospitalreview.com/workforce/us-faces-deficit-of450-000-nurses-by-2025.html?origin=BHRE&utm_source=BHRE& utm_medium=email&utm_content=newsletter&oly_enc_ id=6799J6353967F9A
