



































LINKS






























































ALUMNI IN
COUNTRIES





































































































Apart yet together, in isolating us the pandemic also served to unite us. is past year, alumni all over the world have welcomed RCSI into their lives, sharing stories and exchanging experiences. e quest to halt the devastation caused by COVID-19 sparked our desire to reach out to those who matter to us, personally and professionally, to address challenges together but also just to check in and connect, with this institution, with former classmates, and with peers and colleagues.
e capability to connect was eased by the new normal: the virtual revolution. Calls, meetings, consultations, discussions and events have become our daily life. We observed the global become personal. e ties that bind have never seemed so tight.
e last twelve months have brought fascinating stories of our alumni to life. We have discovered that our thriving global community (in 94 countries) is involved in many exciting endeavours, from oating doctors and ying doctors to the world of Formula One, to alumni working in isolated communities in Northern Canada, in rural Sierra Leone and in the Australian outback. ese far- ung alumni have become closer to the rest of us – just a screen away – as we gleaned insights into their very interesting lives.
With such a rich tapestry of alumni stories to choose from, we decided to make those stories a key feature of this, our annual RCSI Alumni Magazine. In the pages that follow, you can read about alumni all over the world in Going Places (page 8); about alumni whose careers have taken an unexpected twist in Tales of the Unexpected (page 18). You can discover how alumni coped with COVID-19 in the Irish Prison Service (page 44); and read about some memorable rotations experienced by alumni (page 51). Professor Clive Lee tells the truly remarkable story of the Anatomy Department (page 26); and on page 38 we reach back into the archives to explore the history of Sir Charles A Cameron, Dublin’s rst public health specialist, and for whom RCSI has named a new award, the Cameron Award, whose rst recipient is Dr Mike Ryan of the WHO.
Alumni voices are a key feature of the RCSI weekly eNews bulletins. Please do keep your details up to date and sign up on our website (www.rcsi.ie/alumni) to receive them. It’s a great way to keep connected with all things RCSI. We are creating, with alumni inspiration and help, more opportunities to connect. Alumni are involved in leading new innovations like the virtual 2020 Annual Gathering, the North American Engagement Series and virtual catch-ups and class calls. Please do get in touch with the Alumni Relations o ce if you would like more information on any of our activities.
e growing numbers of RCSI Alumni Instagram and Facebook followers show how much we value our sense of community at RCSI, past and present. We encourage alumni to stay in contact. We thank all those alumni who have shown incredible support to current students by mentoring, guest talks and via nancial support. Our particular thanks too, to the alumni panel, who contributed to the magazine, especially Dr Veer Gupta (Medicine, Class of 2012), Graham Widger (Physiotherapy, Class of 2015) and Dr Pui-Ying Iroh Tam (Medicine, Class of 2004).
It is true, however, that while we are all active online, there is no replacement for in-person connections. We look forward to a time when we all can meet again face-to-face. Until then, keep close.
AÍNE GIBBONS DIRECTOR OF DEVELOPMENT AND ALUMNI RELATIONS
Aíne Gibbons

PROTECTING YOUR DATA RCSI is committed to protecting your privacy. To enable you to receive invitations for reunions, events and scientific conferences and to continue to stay in touch with classmates, please keep us informed of any changes to your details. Update your information online at rcsi.ie/alumni, by email to alumni@rcsi.ie or by calling the Alumni Office directly on +353 (0) 1 402 2523.


08 GOING PLACES



Alumni in destinations all over the world 26 STORY OF ANATOMY The place, the people and the art
Professor

18 TALES OF THE UNEXPECTED When a traditional career route takes an unexpected turn ON OUR
The story of RCSI’s first Emeritus Professor Sir Charles A Cameron

For details, see page 15
Professor Moira O’Brien: a trailblazer
The Swan pub: the “Surgeons Local” 44 Class Call
Alumni check in 48 A Life’s Work
Alumnus Dr John Latham (Medicine, 1962) on a life well lived 51 Pride of Placements
Alumni recall their more memorable rotations
55 Alumni Volunteering
Giving back and helping out
RCSI ALUMNI MAGAZINE is published annually by the RCSI University of Medicine and Health Sciences. Issues are available online at rcsi.ie/alumni. Your comments, ideas, updates and letters are welcome. Contact Caoimhe Ní Néill, Alumni Relations Manager at RCSI, 123 St Stephen s Green, Dublin 2; telephone: +353 (0) 1 402 8682; email: caoimhenineill@rcsi.com.
RCSI ALUMNI MAGAZINE is POSTED ANNUALLY to alumni who we have listed on our database. To ensure you receive a copy, please PROVIDE YOUR CURRENT CONTACT DETAILS at rcsi.ie/alumni. RCSI ALUMNI MAGAZINE is produced by Gloss Publications Ltd, The Courtyard, 40 Main Street, Blackrock, Co Dublin. Copyright Gloss Publications. RCSI Editorial Board: Aíne Gibbons, Louise Loughran, Jane Butler, Paula Curtin, Stuart MacDougall and Caoimhe Ní Néill.
RCSI was founded by Royal Charter in 1784 as the national training and professional body for surgery. In 1978, RCSI became a recognised College of the National University of Ireland and in 2010, RCSI was granted by the State, the power to award its own degrees. In 2019, RCSI was granted University status and became RCSI University of Medicine and Health Sciences.




In June 2020, RCSI announced the election of Professor Ronan O’Connell as its new President, following the biennial Council Elections. Replacing outgoing President, Mr Kenneth Mealy, Professor O’Connell is Emeritus Professor of Surgery UCD and Consultant Surgeon at St Vincent’s University Hospital. An international leader in the field of colorectal surgery, he is also the incoming President of the European Surgical Association.

Professor Laura Viani, Consultant Otolaryngologist and Neurotologist at Beaumont Hospital and the Children’s University Hospital Temple Street was elected as the new Vice-President. She is Director and Professor of the National Cochlear Implant Programme and Hearing Research Centre.
Speaking on his appointment, Professor O’Connell said: “It is my great honour to be elected as President of RCSI. My presidency will be like no other in our 236-year history as the COVID-19 pandemic has presented our surgical community with unprecedented challenges that will shape the future of surgery for years to come.
“I am particularly conscious of supporting our surgical trainees whose training has been disrupted by the COVID-19 restrictions. RCSI will use the excellent facilities of the National Clinical and Surgical Skills Centre at 26 York Street to provide innovative ways of training to complement hospital experience.”

Professor Mark Shrime, co-author on the Lancet Commission on Global Surgery, was appointed O’Brien Chair of Global Surgery at RCSI in June 2020. Professor Shrime will lead the University’s Institute of Global Surgery in its work to address the provision of surgical care in low and middleincome countries.
The groundbreaking Lancet Commission Report, “Global Surgery 2030 ”, highlighted the stark and troubling deficit in the equity of surgical and anaesthesia care globally. Every year, an estimated 140 million people who needed surgical procedures
to save their lives or to prevent long-term disability did not get them and an estimated 81 million people who receive surgical care are impoverished by its costs.
Confirming his acceptance of the O’Brien Chair of Global Surgery, Professor Shrime said: “I am tremendously excited to join the stellar team at the RCSI Institute of Global Surgery. I look forward to building on the decade of innovation that the University has driven in global surgery to create a holistic, patient-centred, equity-driven approach to surgical systems strengthening.”
Announcing Professor Shrime’s appointment, RCSI Chief Executive, Professor Cathal Kelly said: “We are delighted to welcome Mark Shrime as the O’Brien Chair of Global Surgery at RCSI. For over ten years, we have pioneered and accelerated change to provide solutions to the surgical deficit, focusing on low and middle-income countries. It is our dedicated surgical focus, research capacity and sustainable partnership model that positions us well to make a significant and lasting impact on surgical access globally. I greatly look forward to seeing Professor Shrime and his team further expand and amplify this important work over the coming years.”
Ahead of the 2020/2021 academic year that began in September, RCSI teamed up with Croke Park Meetings & Events to create a unique satellite campus for medical students to continue their education safely, at the historic Dublin home of the GAA.
RCSI Orientation Day was held at Croke Park and three main learning spaces were created – two for teaching, with a third designated as a study space for students to use between classes. Over 650 students have used these facilities to continue their learning at a safe physical distance, as part of a six-day cycle through the campus.
In addition to being well connected to the RCSI city centre campus and the rest of Dublin, Croke Park is close to Beaumont Hospital, the main RCSI teaching hospital. This proximity of the new satellite campus to Beaumont allowed academics who work there to easily travel to deliver lectures.
Mark Dorman, Head of Stadium Business at Croke Park, confirmed the announcement, saying, “Croke Park is delighted to provide a range of safe, flexible spaces where RCSI can continue the educational experience of future doctors during these unprecedented times.”

Professor Lisa Mustone Alexander has been appointed Director of RCSI’s Physician Associate Programme. The Programme was launched in 2015, and its graduates have played a critical role during the COVID-19 crisis. They have worked across surgical and medical services, with a number staffing some of the hospital testing facilities.
There are now over 135,000 physician associates practising in the US, and the UK has more than 35 programmes graduating over 750 physician associates annually. As well as leading the development and delivery of the programme, Professor Alexander will play an important role in advocating for the recognition of physician associates in the Irish healthcare system and in promoting the value of the role to healthcare professionals.
“With the increasing demands on healthcare systems during the COVID-19 pandemic, educating and utilising physician associates is important now more than ever,” said Professor Alexander. “I look forward to working with my colleagues at RCSI and within the wider Irish medical community to grow and expand not only the RCSI Physician Associate Programme, but the profession throughout the country.”
Professor Alexander joins RCSI following four decades at the George Washington University School of Medicine and Health Sciences. She was among the fifth cohort of physician associates entering the George Washington programme in 1977 and went on to teach in the programme and twice serve as its director. From 2009 to 2010, as a Fulbright Senior Specialist to the Rwandan Ministry of Education, Professor Alexander led a feasibility study to determine whether a physician associate model could meet Rwanda’s extensive postgenocide health workforce needs.


A new painting inspired by the RCSI Graduates’ Declaration was officially unveiled last October. “I make these promises solemnly, freely and upon my honour”, created by Mary A Kelly, winner of the RCSI Art Award 2019 in association with The Irish Times and the Royal Hibernian Academy (RHA) Annual Exhibition, was commissioned by RCSI to capture and to honour the ritual of the white coat ceremony and the symbolism of the white coat. During the ceremony, students are invited to make a commitment to professionalism that mirrors the Graduates’ Declaration recited at their conferring day. The Declaration signals the responsibilities they must begin to undertake as future health professionals from the start of their academic training.
Aíne Gibbons, Director of Development and Chair of the RCSI Art Committee, said: “This year, our students are commencing their academic journeys at a time of great challenge and change, and also one of great opportunity. We are delighted to add this powerful painting to RCSI’s art collection. We hope this artwork will inspire generations of students, our future healthcare leaders, and returning alumni.”
Mary A Kelly’s work is widely collected and is included in both the Microsoft and Goldman Sachs collections. She commented: “The ethos of humanity at the core of the RCSI Declaration was the inspiration for this painting.”
RCSI
ranked joint second in the world for adherence to UN Sustainable Development Goal 3: “Good Health and Wellbeing”
RCSI has achieved Ireland’s highest position in the Times Higher Education (THE) University Impact Rankings 2021, coming joint second in the world for “Good Health and Wellbeing”, from a total of 871 institutions. These THE University Impact Rankings recognise universities around the world for their social and economic impact based on the United Nations’ 17 Sustainable Development Goals (SDGs). For its contribution to SDG 3, “Good Health and Wellbeing”, RCSI’s score increased from 90.8 in 2020 to 93.1 in 2021. In addition, according to the 2021 THE World University Rankings, RCSI has maintained its worldwide position in the #201-250 category and ranks second out of nine institutions in the Republic of Ireland. RCSI’s performance in this latest ranking is linked in particular to its continued strength in research with the impact of its publications in translational medicine and health sciences in areas including cancer, neuroscience, population health and surgical science and practice ranked highest in Ireland. RCSI continues to perform strongly in the area of international outlook, currently ranked 52nd in the world.

In November 2020, RCSI coordinated its virtual conferring ceremonies for the many nurses, health research scientists, pharmacists and physiotherapists graduating from the University.
Dr Mary D’Alton was awarded an honorary doctorate, in recognition of her position as Chair of the Department of Obstetrics and Gynecology, Willard C Rappleye Professor of Obstetrics and Gynecology Columbia University Medical Centre, USA, and her achievements throughout her career. In the course of her distinguished work in obstetrics and gynaecology, Dr D’Alton has focused on eliminating the gaps in women’s health, building and strengthening programmes in infertility, minimally invasive gynecologic surgery, gynecologic oncology, family planning, and integrated women’s health care.
RCSI awarded best-selling international author, inspirational speaker, TV presenter and charity campaigner, Ms Katie Piper, an honorary doctorate, for her achievements. The survivor of a horrific acid attack in 2008, which caused extensive damage to her face and blindness in one eye, Ms Piper set up the Katie Piper Foundation which supports survivors of burns, their families and carers and works alongside existing support networks. In 2019, the Foundation achieved a significant milestone, opening a rehabilitation centre in the UK that offers burn survivors the same treatment Ms Piper received in France.
Editor-in-chief of The Lancet since 1995, Dr Richard Horton, was also awarded an honorary doctorate. This year marks Dr Horton’s 25th year in charge of what has been described as “the world’s leading independent general medical journal”. In his most recent book COVID-19 Catastrophe: What’s Gone Wrong and How to Stop it Happening Again, Dr Horton explores the global response to the COVID-19 pandemic, calling it the “greatest science policy failure in a generation.”

The RCSI Institute of Global Surgery and global medical technology company, BD (Becton, Dickinson and Company), recently announced KidSURG, a joint initiative aimed at significantly improving paediatric surgical services across southern Malawi. Created in collaboration with leading Malawian paediatric surgeon, Professor Eric Borgstein, the KidSURG initiative will develop a paediatric surgical network in southern Malawi, to expand surgical access to eight million children. The initiative will also seek to develop and share optimal models for replicating this initiative in other countries. BD has donated $500,000 in cash and surgical products to support the initiative.


Leading healthcare simulation educator and scholar Professor Walter Eppich has been appointed Chair of Simulation at RCSI. Building on RCSI’s significant investment in simulation, Professor Eppich will lead the University’s interdisciplinary Centre of Simulation Education and Research (RCSI SIM) in informing the global growth in experiential simulation-based learning in healthcare and other training and education sectors. Professor Eppich, who joins RCSI from the Northwestern University Feinberg School of Medicine in Illinois, will also build the University’s capacity to improve patient safety and care through simulation which is embedded across RCSI’s curricula.

Professor Jan Illing has been appointed as Professor of Health Professions Education and Director of the Health Professions Education Centre. Professor Illing will build on RCSI’s strength in health professions education and advance the University’s health professions education research strategy. She will lead on the evaluation of RCSI’s new medical curriculum, support the development of interprofessional education at the University and build international research collaborations.
In April 2020, RCSI launched a fundraising appeal aimed at making protective face masks more comfortable to wear for intensive care staff providing care to COVID-19 patients.
The Comfort for Carers Appeal was a huge success, raising over €18,000 and funding multiple Wound Care Kits for intensive care staff.
According to Professor Zena Moore, Head of RCSI’s School of Nursing & Midwifery: “We are acutely aware of the skin abrasions and pressure ulcers experienced by ICU teams as a result of wearing PPE for prolonged periods on a daily basis. Each Wound Care Kit consists of a set of instructions, moisturiser, tape and wipes. These Wound Care Kits have been developed by the RCSI School of Nursing & Midwifery, as a preventative measure and the School captured data over a 12 week period to document the impact of the kits, with very positive results.”
Ms Helen Mohan FRCSI, was announced as the recipient of the second PROGRESS Women in Surgery Fellowship. Aimed at addressing the barriers to women medical graduates advancing in the surgical profession in Ireland, this prestigious RCSI bursary, funded by Johnson & Johnson Medical Devices Companies, promotes female participation in surgical training at Fellowship level.
Ms Mohan will now undertake a Fellowship in colorectal surgery at Peter MacCallum Cancer centre in Melbourne, Australia. This will focus on advanced colorectal cancer, including training in robotic surgery, peritonectomy and pelvic exenteration.

“ The Ways COVID-19 has Influenced Our Lives and United Medical Forces” was the theme of the address at the 88th Biological Society Inaugural Meeting, which took place virtually in January 2021. The Biological Society (BioSoc) is the oldest student society in RCSI, and the event was organised by students from the BioSoc Committee with assistance from the RCSI Student Services team. At the meeting, exiting Faculty President of the Biological Society, Professor Camilla Carroll (Class of 1985), passed the chain of office to the new Faculty President of the 2020-21 academic year, Professor Rory McConn Walsh.
The Widdess Lecture, “How Our Medical School has Adapted to Covid-19: Implications for the Future of Medical Education”, was delivered by Professor Arnold Hill, Head of the School of Medicine at RCSI, Professor and Chair of Surgery at RCSI, National Advisor for Surgical Oncology for the National Cancer Control Programme and President of the Surgical Research Society. Professor Samuel McConkey, Deputy Dean and Head of the Department of International Health and Tropical Medicine at RCSI, spoke about the COVID-19 vaccination programme. Dr Eoghan De Barra, Consultant in Infectious Diseases at Beaumont Hospital and Senior Lecturer at RCSI, delivered his address: “Discussing the COVID-19 Pandemic”. Dr Eoin Cleere, an intern at Beaumont Hospital and Class of 2020 alumnus of RCSI, gave insights into his experience as an intern during the pandemic.
The RCSI Bahrain campus was a very different experience for new and returning students and staff members this academic year, following the implementation of a host of processes and initiatives designed to combat the spread of COVID-19.
Among the new measures are a one-way system around the campus, plexiglass protection at student-facing contact points, extensive instructional signage to guide people and remind them of precautions, additional hand-sanitising stations, foot-operated door-opening devices, and enhanced cleaning processes.
Access to the campus has been closely managed and monitored in order to adhere to social distancing guidelines, with pre-planned
timetabling and seating arrangements limiting the total number of people on campus at any one time.
As part of the support programme implemented to assist in the safe return to campus, all international students were offered the opportunity to avail of a tailored group health insurance scheme with a flexible payment plan, while the University also offered to reimburse the cost of compulsory COVID-19 tests for those entering Bahrain to attend classes.
On the teaching side, part of the sports hall has been repurposed as additional clinical simulation space, equipped with new simulation equipment, while some lecture theatres and tutorial rooms have been upgraded to facilitate adequate online streaming.
With alumni in
94 countries, the RCSI diaspora
is truly global. Eight alumni tell us about where they live and work

PERTH, AUSTRALIA
ALISON MOLAMPHY
Physiotherapy, Class of 2015
After graduating, I worked in University Hospital Limerick for two years before coming to Perth in 2018. I had no job organised before I arrived, and it took a while to organise the paperwork side of things. I was here for two or three months before everything was approved for me to start working as a physiotherapist.

I work in private practice. I had originally thought I might work in a hospital as that was my experience in Ireland, but you have to be a permanent resident or citizen to work as a physiotherapist in a hospital in Western Australia; it’s di erent for doctors. e practice I work in is based in the Wembley suburb of Perth; we consider ourselves generalists. We have a mix of private and insurance patients, and we run specialist osteoporosis classes. We have a gym and a clinical pilates studio, and I am trained to deliver clinical pilates instruction. In private practice we have autonomy to refer for imaging, which is something I did not have at home when I worked in private practice, and many health insurance schemes cover preventative physiotherapy.
Perth is very beautiful, and can be very hot – it’s 37°C today! It’s very easy to live an active lifestyle, because of the dry, sunny weather. Because of the heat, people tend to be early risers, and things kick o early in the morning and nish early at night. If you are a er late nightlife, there are better places. It’s not uncommon for exercise classes to happen at ve in the morning, and I’m o en in work before 7am. Usually I work three early days, nishing at
“WE ENJOY THE LIFESTYLE SO MUCH.”
lunchtime, and some late days, nishing at 8–8.30pm. I o en work on Saturdays. Accommodation can be quite di cult to come by, and apartment living is not as prevalent outside of the city centre as on the east coast, so house shares are more common. Cost-wise, rents are comparable to Ireland, and cheaper than the eastern states, but eating and drinking is a bit more expensive. ere are lots of Irish doctors here, but not as many physios – there are more in Sydney and Melbourne.
Public transport connections in Perth aren’t as extensive in suburban areas as they are in the centre, as there has been a lot of development over the past decade and the train line has not been extended to reach sprawling suburbs. A car is the easiest way to get around if you are not living directly on the train line. e beaches are amazing and the shopping and restaurants are great. One of the amenities I love is the public barbecues for groups of families and friends. We try and go on trips as o en as possible – there are so many places to visit even just within Western Australia. When we came initially, we thought we would be here for a year or two and then return home, but we extended that because we enjoy the lifestyle so much and it’s one of the very few places in the world where you can live a relatively normal life during the pandemic. Now we have permanent residency so we have the option to stay, but we haven’t made a decision yet.
BETH WOLFE
Physiotherapy, Class of 2017
I’m from Cork originally and two weeks after graduation I moved to Vancouver for the summer to teach sailing at Jericho Beach. Initially I thought it was only going to be for a couple of months but very quickly I decided to stay and I’m still here four years later. I don’t have any immediate plans to go back to Ireland – the more I get settled here, the harder it is to leave. I really love it here but do see myself going back to Ireland at some point in the future.

Vancouver is not a very big city, it’s a similar size to Dublin. It is built on an outcrop of land surrounded by water. ere’s a huge seawall with a cycling and running track that wraps around the city which is absolutely beautiful. Most of the Irish in Vancouver live in an area called Kitsilano. I lived there for a while but I moved downtown to an area called Yaletown. You can see the mountains and the water from my apartment.
As a relatively junior physiotherapist it is easier to get work in a private practice here than it would be back in Ireland. In Ireland they won’t hire anyone to a clinic without a number of years’ experience, but here in Canada they train you up within the practice.
I rst got interested in physiotherapy as a career through a family friend who is a physiotherapist. He worked both with out-patients at a hospital in Cork and with sports teams so I got an insight into both types of work. And I experienced physio as a patient when I had sports injuries and I loved that. In university we spent more time on rotation in hospitals and I didn’t enjoy it as much – I didn’t feel as if I was making any di erence to patients because you have such a short time to see people. In hospital the focus is on getting people mobile enough to get them home, which is what you need to do in that situation, but in private practice sometimes I could get to work with people for a year or more and I feel more ful lled in terms of the type of work I am doing. at’s not to say I wouldn’t work in a hospital again, just that for now I prefer private practice.
It takes me 25 minutes to get to work on public transport, the buses are great. Vancouver is quite an expensive city, on a par with Dublin and Cork, but I am probably earning a bit more here than I would back home. e cost of housing here is through the roof and I have to say that is one consideration in terms of whether I will stay, because to a ord a nice house I think you would have to move quite a way out of the city.
At the moment I feel as if I work all the time. It’s shi work and I usually work ve days, including Saturday. In private practice you do have to work either early mornings or late into the evenings, and you don’t get paid for time o or holidays. Work/life balance can be tricky but I don’t mind it at the moment. My favourite time of year here is summer and the weather is so nice. I love sailing and going to the beach. Hiking and anything to do with the mountains is massive here, I had never really skied or snowboarded growing up, but here I’ve been going snowshoeing. ere are lots of great spots to explore within a couple of hours of the city. e worst thing about being in Vancouver is missing family: I was homesick when the borders closed, it felt so far away. I’m coming to terms with it now.

“YOU CAN SEE THE MOUNTAINS AND THE WATER FROM MY APARTMENT.”

AKSHAY PADKI
I’m originally from India but I grew up mainly in China as my parents were based there for work and I did most of my schooling there, with my last three years of high school in Canada. In my nal year at RCSI, I applied for a job in Singapore as a back–up option, in case I didn’t get the job I wanted in Ireland a er graduation. I was o ered a medical job outside Dublin but I wanted a surgical job so I took up the position in Singapore instead, moving here in August 2015, straight a er graduation. I had never lived here but had visited several times, I knew what it was like.

I did my houseman year – the equivalent of intern year in Ireland – in Singapore. at consisted of three di erent postings: one medical, one surgical and one elective. You are graded on those postings and then you can apply for SHO postings in areas you are interested in, a er which you can apply for a specialist scheme, which is a direct pathway to consultancy. I am applying for the Orthopaedic Surgery Scheme which is quite competitive, but I hope to be accepted this year. ere are only ten to 15 spots a year.
I have worked at several di erent public hospitals including Changi Hospital in Eastern Singapore and the National University Hospital. I am now at Singapore General, the biggest hospital in the country. During the height of the COVID-19 pandemic, I helped at the National Centre of Infectious Disease as well.
Singapore is a small country and its healthcare system is very well-funded, e cient and quite advanced. It was a bit of a culture shock at rst, I was surprised how quickly things were done. I remember when I was in Ireland I would have had to take all the bloods myself and wheel the ECG cart around, but here it is more automated and nurse-led. at was both refreshing and interesting to see. Work/life balance here is de nitely less than in Ireland. Saturdays are still technically a half day, and sometimes I have clinics/OTs. On calls can be tiring as well and the following day you’re expected to continue your normal duties until around noon when you can go “post call”.
I’ve always been comfortable in big cities, and I enjoy living here but there is no beach near the city and although we have some parks there is not much access to large parks/nature trails. One of the biggest draws is the proximity to SE Asia, which is cheap and easy to get to. Prior to the pandemic, we would have gone on holiday somewhere every two months or so, to Bali, ailand, Cambodia or Vietnam. Singapore is one of the most expensive cities in the world – as a nonSingaporean doctor you get a housing allowance when you arrive, which helps. If you are looking to buy, the prices are astronomical so you are likely to be renting here longer than you might in other cities. Cars are expensive too, but food and day-to-day expenses are reasonable. Public transport is very e cient,
“THERE IS GREAT NIGHTLIFE HERE, IT IS A VERY VIBRANT CITY WITH LOTS OF YOUNG WORKING PROFESSIONALS.”

I usually take a taxi to work in the morning, which takes about 15 minutes, and get the MRT home, which takes about 40 minutes.
I did not originally intend to stay in Singapore, but I met my wife who is Singaporean and we are settled here now for the foreseeable future. ere were about 20 other Irish medical graduates who arrived here the same year I did and we meet up fairly frequently. We go out for drinks and dinner. ere is great nightlife here, it is a very vibrant city with lots of young working professionals. But now it’s less nightclubs and more going to cafés and walking the dog.


DR JEYSEN YOGARATNAM Medicine, Class of 1999
A er graduating from RCSI, I moved to the UK to pursue training in Cardiothoracic Surgery and completed a PhD. In 2008, while I was coming to the end of my training at the Royal Brompton Hospital in London, I began to realise that opportunities to progress my career in cardiac surgery were diminishing. Many of my more senior colleagues who had completed their cardiothoracic surgical training found it very challenging to secure consultant positions in the UK.

“WHEN WE MOVED HERE FROM THE EAST COAST, OUR HOUSE HALVED IN SIZE BUT OUR MORTGAGE DOUBLED!”
I was keen to explore opportunities outside academia in the area of biotech–based clinical research and joined a world class biotech organisation, Bristol Myers Squibb (BMS), in the UK to explore and pursue a new career as a clinical drug developer. at was 13 years ago and I have not looked back since! Within two years, I was promoted and BMS relocated me and my wife to Connecticut and later I secured a place at the Massachusetts Institute of Technology (MIT), Sloan School of Business, to pursue an MBA. While in Boston I worked with Vertex and following the completion of my MBA in 2015, my family, now including two children and a husky, decided to move to sunny California.
I transitioned to a more senior role as a drug developer at Janssen Pharmaceuticals (a Johnson & Johnson Company) in the Bay Area of San Francisco, USA. While working in the Bay Area, I have held increasingly senior roles as a drug developer at a number of di erent biotechs, leading the early clinical development activities of a number of di erent novel therapeutics in the areas of chronic hepatitis B, C and D and in uenza. In my current role at Aligos erapeutics, I was incredibly fortunate to be able to join the company while it was just a small private start-up biotech. In my role, I lead and advance the clinical development of many novel therapeutics through early clinical development that ultimately enabled the company to transition into a successful publicly traded biotech.
California is beautiful and the amazing weather is a huge attraction for my family. We live in a suburb of San Francisco, in the East Bay, called Danville. In this part of the Bay, it is possible for us to drive up to the slopes of Lake Tahoe for early morning skiing and still be able to drive back to the Bay Area beaches to catch the late a ernoon sun and waves. It also o ers some of the best US public schooling systems and recreational activities for our growing boys.
e San Francisco Bay Area is consistently ranked in the top two of the best biotech hubs in the world. As such it o ers ample professional opportunities for me to continue to grow as a drug developer. Furthermore, it has world class hospitals and healthcare systems that o er fantastic opportunities for my wife to grow her career as an intensive care nurse.
While the Bay Area of California is a fantastic area to raise a family, it is one of the most expensive places to live in the USA. When we moved here from the East Coast, our house halved in size but our mortgage doubled! Tra c is frequently awful in the Bay Area, though it has improved since the start of the COVID-19 pandemic. Prior to the pandemic, in order to avoid sitting in tra c for two hours or more, I used to leave the house at 5am each morning to travel the 50 miles to my o ce in South San Francisco. To avoid the evening tra c, I used to leave the o ce by 3pm.
e COVID-19 pandemic has brought a whole new way of balancing work and life that I would never have thought possible, showing that it is possible to be a successful biotech executive while working from home. It has brought us closer together as a family.
My wife and I became US citizens in 2018 and we love every part of contributing to our new home country. It has o ered our family opportunities beyond our expectations.
“I LOVE IT HERE. MALAWI IS KNOWN AS THE WARM HEART OF AFRICA, AND THE PEOPLE ARE WARM AND FRIENDLY; AND THE COUNTRY IS BEAUTIFUL.”


I’m originally from Hong Kong and did a rst degree in the US before going to RCSI for my medical degree. A er graduating, I stayed in Ireland for two years and, a er nishing my SHO posts, I went to the US for residency and fellowship. At the time I nished fellowship the plan was to move to Nigeria, but we ended up staying in the US and I got a faculty position in Minnesota in Paediatric Infectious Diseases, where I stayed for four years. roughout that time my interest in global health and working in sub-Saharan Africa never waned. I realised several years a er arriving in Minnesota that even though I was enjoying what I was doing there, it wasn’t the work that had inspired me to go into medicine in the rst place. I started looking around and found this position at a research institute in Malawi and came out here in 2016.
I am a senior scientist at a clinical research institute, the Malawi-Liverpool Wellcome Trust Clinical Research Programme; the parent institution and my employer is the Liverpool School of Tropical Medicine in the UK. I am based in Malawi fulltime and head the Paediatrics and Child Health Research Group. My work is a combination of clinical work, where I am a consultant paediatrician in the government hospital, and clinical research, which focuses on infections in children relevant to this setting. We see a lot of pneumonia, diarrhoeal disease and sepsis caused by bacteria that are resistant to our commonly used antibiotics. I recently led a multinational clinical trial evaluating a novel treatment of diarrhoea in HIV-infected patients, and currently am the local lead for a multicountry clinical trial evaluating empirical treatments for HIV–infected infants with severe pneumonia.
Before I came to live in Malawi, I had been to many other parts of Africa but not this country. I love it here. Malawi is known as the warm heart of Africa, and the people here are warm and friendly; and the country is beautiful. I have
lived in many cities around the world and I think what I have traded o in terms of urban activity, such as art galleries and museums, is made up for with a lot more outdoor activity and a better quality of life in many ways. With my family we go hiking, we visit waterfalls and wildlife reserves and Lake Malawi is just a couple of hours away.
Blantyre is the second largest city in Malawi, with an urban population of about a million. I live in a neighbourhood where I have my own plot of land, and a house with a huge garden overlooking a river. It’s a ten-minute drive to the hospital. ere are several international schools in the area, so my children have choices. My research is organised around my own schedule and can happen at all hours, but I enjoy it and the work is meaningful and interesting. One of the most satisfying aspects of my work is helping to develop the careers of the (currently twelve) junior researchers who I am supporting, from masters to PhD and postdoc level, in addition to the medical students, clinical o cers and registrars that I am teaching, supervising and mentoring.
It’s too early to say if I will make Malawi my permanent home. I would like to return to Hong Kong but this is looking increasingly unlikely as Hong Kong is going through political change; I could move to the UK or Europe; and my children were born in the US so they are US citizens. I haven’t yet decided which path to take next. I am in the process of certifying as a professional coach, and am coaching other physicians and academics as an executive/ leadership/ life coach. I help early/mid-career women who are trying to balance career and family and nd a way to create the life they were meant to live (reach out to me on LinkedIn).
It’s something I can do with anyone anywhere in the world. So I feel like a truly global citizen, because where I am located does not limit me in any way.

I am originally from Niger state, two hours away from Abuja, the capital of Nigeria, where I live now. I was away studying for eight years, I did A-levels in the UK before attending RCSI in Bahrain. I got married just before graduation and moved back to Nigeria in July 2019. I had been missing home and was happy to return.

It was not easy to nd a job here; there is no standardised recruitment process for internship. As a foreign medical graduate you have to enrol in a privately run training programme to prepare you for a licensing exam. When you pass, you are inducted into the Medical and Dental Council of Nigeria (MDCN) and you are given a provisional license to do a one-year internship, a er which you receive your permanent license from MDCN. Having the provisional license doesn’t guarantee an immediate intern place though, you have to apply to multiple places and it can take several months or even years to nd a job. ere are so many medical graduates and not enough spots, it’s a big issue and COVID-19 made everything worse. I sat for the licensing exam in November 2019 and got the results a week later but the induction ceremony did not happen until February. I got my license then and applied to hospitals immediately but was not called to an internship position until December. I was hanging around for months with no clear indication of when I was going to be called, and yet the National Hospital of Abuja, the main government hospital, where I currently work, was functioning without house o cers for several months. I was on maternity leave from January to April.

“I HOPE TO STAY IN ABUJA AND MAKE MY LIFE HERE, AND WOULD HOPE TO DO MY RESIDENCY IN THE SAME HOSPITAL.”
When I nish my internship, I have to apply to do a one-year service to the country with the National Youth Service Corps, which is compulsory for everyone under the age of 30. As a medical graduate I will do this in a clinical setting and a er the year I will sit an exam and then apply for residency. I hope to stay in Abuja and make my life here, and would hope to do my residency in the same hospital.
I had never lived in Abuja before but I have family here and used to visit o en. e population is around a million, it is nothing like Lagos, which is huge and very densely populated. It’s a busy city and getting busier, there are better job opportunities here than in other cities and the standard of living is good. Rents are high, there are lots of nice restaurants and we have a few malls. ere are some parks and lakes, which are nice for picnics with friends. I live a 20-minute drive from the hospital. e worst thing about Abuja is the tra c, but it’s not as bad as Lagos. Schools are expensive here, you have to pay a lot for good quality education and you have to plan for that.
DR KINAN ALRYAHI
Medicine (Bahrain), Class of 2017
My father is Palestinian, my mother is Bosnian and I grew up and went to school in Jordan. I went to RCSI Bahrain because it was close to home. I did my intern years in Jordan. When I was nished I wanted to get a place on an Ophthalmology Residency Programme. I thought I would go to the UK but my father, who is an ophthalmologist, wanted me to go to Sarajevo, where he studied. We had an on-and-o conversation for a while but I eventually decided to come to Sarajevo as I would get more hands-on experience here and the residency

programme is shorter and less competitive. My father and older brother have a private clinic here.
I arrived in Sarajevo in 2019 to start the four-year residency programme at the University Hospital. I had visited the city a few times before, and had a good sense of it. I get good hands-on experience with my father and brother in their private practice, where they do some pro bono surgeries for people who cannot a ord to pay. In the public hospital the machines tend to be quite old, but we get a lot of rare cases and diseases.
Between the hospital and the clinic I work 8am to 8pm every day, with one day o . Sarajevo is a small city where a lot of people know one another. People are very friendly and the cost of living is pretty low. If you want to go away, it’s easy to jump in the car and head to Croatia, Serbia, or Italy. I wouldn’t be here if there weren’t good restaurants! ere is a good social life. e university has delivered its medical programme in English for about six years so the school of medicine is growing and there are many international students. My plan is to stay in Sarajevo. My family hopes to expand the clinic into a hospital and start an Ophthalmology Residency Programme; that’s our aim. I’m excited to do that in Eastern Europe because there are not a lot of opportunities in the region and it will give more access for people who want to pursue a career in ophthalmology. It is a great goal for me.
Nursing (Bahrain), Class of 2015
I am originally from Bahrain, and a er I completed my degree I took a gap year in Austria, teaching high school students there about Middle Eastern Culture. When I returned to Bahrain I initially worked in the private sector and then took a job at the Ministry of Health working as a nurse in primary healthcare. en I was awarded a Fulbright scholarship o ered by the US Embassy in Bahrain and I moved to Idaho in 2020 to study for a master’s degree in public health. I work part-time in a public health department as a contact tracer for COVID-19.


I love it here in Boise. It is very safe and the people are friendly; it feels very family-centred. It’s a fast-growing city, as many people are moving here from



“SARAJEVO IS A SMALL CITY WHERE A LOT OF PEOPLE KNOW ONE ANOTHER.”

California because it is safer and cheaper. I live o campus in an apartment, it is very di erent to home but there are so many students here I have found it easy to make friends. Boise has everything you want in a small city – with mountains, parks, hiking trails and a river. I love the countryside and spending time with friends outdoors.
e scholarship gives me a monthly stipend but it’s quite expensive here –it’s a city on the rise and you can really feel it getting more expensive. At rst I used public transport but a er a few months I did my driving test and got a car, which makes it much easier to get around.
I have three classes per week, some in person and some online. e work takes me the whole week to prepare; working and studying is tough. It is a two-year course, a er which I have to go back to Bahrain and do something useful for my country. In Bahrain I plan to work as a public health professional. I am studying prevention and intervention and will be able to work on health promotion programmes. If I want to return to the US, I’ll have to wait two years before applying for residency. I’m not sure yet whether I will do that. ■

“BOISE HAS EVERYTHING YOU WANT... MOUNTAINS, PARKS, HIKING TRAILS AND A RIVER.”


e third annual RCSI Alumni Awards ceremony took place on 25 April. While the outstanding achievements of the six RCSI Alumni Awardees for 2021 could not be marked in person, the University honoured these global healthcare professionals in a virtual celebration attended by fellow alumni, faculty, family and friends
When the Alumni Awards 2020 became a casualty of restrictions imposed by the global pandemic, little did we expect that these same conditions would prevail in 2021. For the second year running, the University acknowledged its awardees virtually.
e Awardees, one from each of the six Schools, were chosen on the basis of their extraordinary accomplishments in their own eld that have contributed to patient welfare and the business of health care, and have also enhanced the reputation of the University globally.
Alumni from all over the world were invited to nominate classmates and peers. Written submissions were assessed by a panel of judges led by RCSI Chief Executive, Professor Cathal Kelly; Dean of RCSI, Professor Hannah McGee; Professor Arnold Hill (Medicine); Professor Suzanne McDonough (Physiotherapy); Professor Tracy Robson (Pharmacy and Biomolecular Sciences); Professor Zena Moore (Nursing and Midwifery); Professor Niamh Moran (Postgraduate Studies) and Eunan Friel (Institute of Leadership).
Aíne Gibbons, Director, Development and Alumni Relations, RCSI said: “We are extremely proud of the recipients of these special awards, our distinguished alumni who are united by their time spent at RCSI. eir enduring contributions to the betterment of human health are extraordinary. We look forward to receiving nominations for the 2022 Alumni awards and to being able to gather in person to honour another cohort of exceptional RCSI alumni.”

RCSI acknowledges the support and contribution from our Alumni Award sponsors
Rising Star Award, supported by Physiologix
Outstanding Clinician Award, supported by 3M
Ambassador Award, supported by Novartis

Research and Innovation Award, supported by HealthTech Ireland
Humanitarian & Community Award, supported by Medical Protection
Positive Global Impact Award, supported by Bon Secours Health System

MR STEPHEN O’ROURKE School of Physiotherapy

Stephen trained as an actor at e Samuel Beckett Centre, Trinity College Dublin, and worked as a professional actor and performer before entering the world of physiotherapy. After graduating from RCSI in 2014, he worked as a rotational Sta Grade Physiotherapist in Beaumont Hospital and in both vestibular and musculoskeletal private practice, pioneering Ireland’s rst Healthier Dancer Programme and Injury Screening Programme. He undertook research examining injury incidence and physical tness in aerial dance performers, with the support of RCSI and the Irish Aerial Creation Centre.
In 2016, Stephen became Company Physiotherapist for Riverdance and toured China, visiting 18 cities. In 2017, he went on to become Senior Physiotherapist at Franco Dragone’s e House of Dancing Water Show in Macau, looking a er more than 100 professional international performers, from former Olympic gymnasts to cli divers and elite motocross riders.
Stephen says he loved his time at RCSI, singling out one lecturer for special mention: “I began my physiotherapy studies as a graduate student with the intention to work in musculoskeletal medicine with performers. Louise Keating was assigned as my personal tutor. When I discovered she had previously worked and toured with Riverdance, I knew I was in the right place. Louise was and is a huge inspiration to me.” He says that RCSI set the standard for the quality of care he delivers to patients: “RCSI instilled a strong ethos of looking to evidence-based practice and international best practice in me. is has guided my physiotherapy practice throughout my career.”
Stephen says being selected for the Rising Star Alumni Award is a huge honour. “It is an encouragement to continue to strive for excellence and new heights in my future career.”

DR CLARE LEWIS
School of Nursing and Midwifery

Clare is Deputy Chief Nursing Officer in the Department of Health, supporting the Chief Nursing O cer with policy and strategic development, as well as clinical and operational expertise, to translate policy into practice.
Clare has over 20 years’ experience in advanced practice, working in both primary and secondary care settings and in areas of chronic disease management and older persons’ care. Clare worked across hospital and community, supporting GPs and the primary care team to provide rapid access to diagnostic nurse-led clinics, care at the front door (emergency department), in-patient consultation services and domiciliary care.
As part of her PhD research, she developed and tested Ireland’s rst Community Virtual Ward, which supports older persons with complex health and social care needs at home, thereby reducing unplanned hospital admissions and emergency department presentations. is model of care has been recognised nationally and internationally to improve integration and complex care provision in the community.
Clare says the education she received from RCSI in uenced her approach to policy and strategic development. “I start from the patient/service user, building care and services around them. RCSI prepared me by developing my knowledge and skills to lead on innovation, to critically analyse and synthesise evidence, translating it into practice, as well as teaching me conceptual models, frameworks and methodologies to develop and evaluate policy to advance practice. I am truly honoured to receive this award. I dedicate it to my husband Je , my sons Tristan and Adam and my late mother Margaret, who have been so supportive throughout my academic journey. I hope this award will inspire nurses and midwives in the future.”

MS LOUISA POWER School of Pharmacy and Biomolecular Sciences

Louisa, Chief Pharmacist for Pharmacy Services in the HSE Community Healthcare Mid West, graduated from RCSI in 2007. She has worked in both traditional and non-traditional pharmacy roles, always striving to promote the profession and ensure excellent pharmaceutical care. Her particular interest is in the role of the pharmacist in ensuring medication safety and medicines optimisation across all divisions of healthcare.
In her early career, Louisa took the opportunity to work in other healthcare systems before returning to Ireland to take up the post as the rst Medicines Management Inspector with the Health and Social Care Regulator in Ireland, forging a path for pharmacists to work in this area in the future.
Due to her family background in pharmacy, Louisa has always been passionate about the practice of community pharmacy. She was elected a member of the Council of the Pharmaceutical Society of Ireland and sits on the PSI Risk and Audit Committee. Louisa is part of the Peer Support Network with the Irish Institute of Pharmacy.
While a student at RCSI, Louisa says Professor Judith Strawbridge was a key inspiration. “She brought enthusiasm, positivity and energy to every lecture. Professor Strawbridge had the great skill of imparting a huge amount of knowledge in a manner that was easily understood and accessible for all students.” Professor Strawbridge also played a key role in Louisa’s decision to choose the path of hospital pharmacy on graduation. “I didn’t believe in myself but Professor Strawbridge’s belief that I could t into this world kept me pushing forward. is had a signi cant impact on me, as a young person, that a respected professional was so invested in my journey.” Receiving the award was a huge honour, she says: “I am proud to be a member of the RCSI family and to be recognised by my alma mater.”

DR EVA BUNK School of Postgraduate Studies

Eva studied Biology at Westfälische WilhelmsUniversität Münster, Germany before undertaking postgraduate studies in the Department of Physiology and Medical Physics at RCSI.
e title of her PhD thesis was “E ect of Gene Knockout and NMDA Receptor Modulation on Cell Survival and Neuronal Stem Cell Fate in in vitro and in vivo Models of Excitotoxicity”. Having studied adult neural stem cells in mice brains at RCSI for so long, she became curious about how this could be of bene t for humans and how she could be involved in these processes.
A er graduating from RCSI, she took a decision to return to Westfälische Wilhelms-Universität Münster to study medicine with the aim of becoming a neurosurgeon. Eva is now a resident physician at the clinic for neurosurgery in Münster, and her research interest has shi ed towards brain tumour treatment. Her research has been published in various academic journals and she has presented her work at a number of international conferences.
Eva says that RCSI taught her to never give up on ideas, research interests and long-term goals, even when nothing seems to work and experiments don’t show the hoped-for results. “My years at RCSI proved to me that there will always be a colleague to speak to or a discussion to have that will give you a new perspective so you can move on with your work.”
anks to her degree from RCSI, Eva was able to work in research during her medical studies. “I was able to work and support myself, thanks to this experience. is award means a lot to me. It demonstrates how hard work will be recognised and honoured when the time is right and it always pays to give the best you can. It brings back very good memories of RCSI, the good friends I made and the beautiful country I was able to live in for that time.”

DR BENJAMIN
LA BROT School of Medicine

Ben, founder and CEO of Floating Doctors, is a Southern Californian, who from childhood, has had a deep connection with the ocean, spending countless hours on (or under) the water o the coast of Southern California.
Ben is the President of RemoteCare Education. providing training for clinicians to practice international medical relief. He is Professor of Global Medicine at the Keck School of Medicine UCLA, and a Clinical Professor at University of California, Irvine Medical School, and an FDA Compliance Advisor for Roche Pharmaceuticals.
A er graduating, Ben worked in the Irish healthcare system before private medical mission work in developing countries led him to combine his love of the sea and medicine. He founded the Floating Doctors in 2009, to bring medical services to remote rural communities. In 2010, he led the rst Floating Doctors mission to Haiti.
“Everything I have done in my career is the result of having gone to RCSI. One of my Norwegian classmates suggested I visit East Africa. It was on that trip I decided to pursue a career in international medicine. At RCSI, we were trained in a public healthcare setting with conscientiousness about resources. I had been told that the clinical skills emphasised at RCSI would be extraordinary: that turned out to be true. I will forever be indebted to RCSI. e collective level of excellence pushes you to do well; RCSI alumni go on to do some pretty extraordinary things.
“I feel incredibly humbled and grateful to have been able to add anything at all to the long list of amazing accomplishments by RCSI alumni over the past 200-plus years. Of course, now I feel like I have a lot to live up to, so I’m going to consider everything we’ve done so far just the warm-up for our ambitions in the years to come!”


In 2007, Subashnie graduated from RCSI with an MSc in Healthcare Management and in 2014, received a PhD from Edinburgh Business School. She is President of the American College of Healthcare Executives, and the Director of Accreditation, Enterprise Quality and Patient Safety at the Cleveland Clinic, Ohio, USA. Since acquiring her BSc in Physiotherapy from the University of the Witwatersrand, South Africa, in 2007, her research on reducing the knowledge gap in healthcare quality and patient safety has been recognised internationally. In 2017, Subashnie received the Harvard Medical School Certi cate in Safety, Quality and Informatics Leadership (SQIL). Subashnie developed a robust analytical methodology to evaluate the impact of quality interventions, such as accreditation. is has been replicated in healthcare environments around the world, including Denmark, Brazil, Saudi Arabia, Hungary, Turkey, Australia, Jordan, Rwanda, United Kingdom, and the US. In addition to her role at Cleveland Clinic, Subashnie is an International Consultant with the Joint Commission and a speaker at international conferences.
“A truly remarkable aspect of RCSI, apart from the superb education, is that RCSI is for life,” says Subashnie. Subashnie recalls Professor Ciaran O’Boyle’s lectures at RCSI and his ability to make the complex, simple. She remembers how she later encountered Professor O’Boyle when he was appointed as an external examiner in Edinburgh, where Subashnie was completing her PhD: “He provided exceptional academic guidance, read my entire thesis, adding notes in the margin as to how it could be improved, and gave excellent feedback. is made me realise that I am still very much a part of RCSI, even 14 years a er graduation. RCSI has this incredible ability to connect students and graduates across the world.”
When a traditionally routed career path takes a twist anything can happen. Six alumni share their distinctive stories




Aer graduation, like most of my classmates, I headed to Beaumont for my intern year followed by two years as an SHO, with some “out” rotations in Letterkenny and Cavan. During that time I spent quite a bit of time in the emergency department and decided that was the area in which I wanted to specialise. I was planning to go to Chicago to train and then someone suggested Australia. Almost overnight it suddenly seemed an option worth thinking about – with a very similar health system to Ireland but better weather. I arrived in 2001, with the intention of staying only as long as it took to get my Fellowship sorted out, be appointed as a Consultant and then go home. at plan completely fell apart and I’m still here.
My rst job was in Liverpool Hospital, New South Wales and I did all my emergency training there, with a couple of “out” rotations. I completed my Fellowship in 2008 and a second in intensive care in 2010. en I moved to the job I hold now in Wollongong Hospital, an hour south of Sydney, where I’m an Intensive Care Consultant.
When I was a medical student on elective in Malaysia, I had the opportunity to tag along with the medical team at a motorsport event. I spent the day hanging out in a rubber plantation, avoiding snakes, eating roti and curry, watching fast cars at what I think was probably a stage of the Asia Paci c rally. It was pretty good, and back in Ireland I started to do the same at Mondello Park, a few forest rallies and at the Donegal rally, hanging out with the paramedics and occasionally getting paid 50 quid. At that stage I’d started to watch Formula One – I knew I would never be a driver but to be involved in some capacity became a thing I thought I would like to do. Once I got
settled in Australia I got online and tracked down the doctor for the stage of the World Rally Championship held in Perth and asked if I could join in, and I’ve been involved here ever since.
I’ve now spent the best part of 20 years being a Medical O cer for everything from club motorsport events to international events and long distance endurance events. For the last couple of years I’ve been Deputy Chief Medical O cer for both the Formula One in Melbourne and the World Rally event in Co s Harbour. I usually do between six and twelve events each year, including at my local track Sydney Motorsport Park in Eastern Creek. ere have been fewer events due to COVID-19 but they are coming back now, although with fewer spectators.
Motorsport has changed a lot over the years. When I started, I was going to a lot more incidents, with a wider range of injuries and illness, but there has been a lot of engineering work done on the safety features of the cars, as well as on helmets, re suppression systems, and driver conditioning. At the top tiers of motorsport, competitors now have a much better chance of walking away from a big crash without major injury than any time previously, though the gap between having no injury and not walking away at all is much narrower. ere is a wider range of potential for injury at the lower tiers where the cars can be older or the safety equipment less well developed.
More recently, for relaxation outside of work and motorsport, I play the drums in a band with some friends – some of whom are medics. We don’t have a name yet but we have been practising for the last six months and we’re getting to the point of thinking we might take the next step and play in front of a few people. I’m not sure if my kids think this is a good idea, though.
“AT THE TOP TIERS OF MOTORSPORT, COMPETITORS NOW HAVE A MUCH BETTER CHANCE OF WALKING AWAY FROM A BIG CRASH WITHOUT MAJOR INJURY THAN ANY TIME PREVIOUSLY.”

After graduating from RCSI, I stayed in Ireland to specialise in Anaesthesia, training mainly in Dublin. In 1994 I went to Toronto to sub-specialise in General Cardiac Anaesthesiology and in 1996 took up a post as Consultant Anaesthetist at Kings College Hospital. While I was in London, I met my husband, Christopher Roberts, and in 2007 we returned home to Sierra Leone, a er the war.

I took up a position as Head of Intensive Care at Connaught Hospital. ere is a shortage of anaesthetists here and one of my priorities has been to support and develop a pre-existing training programme for nurse-anaesthetists to provide anaesthesia services in rural Sierra Leone, which is particularly vital for women, who are at risk of greater morbidity and sometimes mortality. e programme to train nurse-anaesthetists is on pause at the moment as we are trying to move from a diploma to a degree course. I am busy putting together a new curriculum to start in October 2021, alongside a curriculum to train critical care nurses, as we don’t have a course here and currently we have to send people away to train in Ghana and Nigeria. We hope to take on ten nurse-anaesthetists who have graduated from the present diploma course, and eight to ten critical care nurses. In the rst semester there will be some commonality between the two courses, and then we will send them out for further training. With my colleague Dr Eric Vreede from e Netherlands, who I rst met at our post graduation ceremony in 1994 at RCSI, we are also preparing three residents in anaesthesia for their Primary exams in April. As well as my work in anaesthesia and medical education, I have, together with my husband Chris, founded a business, Morvigor Sierra Leone, making tea from the leaves of the moringa plant. I rst heard of it by chance, as it is
used in East Africa as a natural method of water puri cation. e leaves are full of vitamins, minerals and antioxidants and help to prevent malnutrition, which is still endemic here especially in the underves. We also prepare tea infusions and powders that we are exporting to the US and UK. ey are in all the supermarkets here too and going quite well, children take it as a nutritional supplement. It’s not a big business but it is growing!
“THE MORINGA PLANT... LEAVES ARE FULL OF VITAMINS, MINERALS AND ANTIOXIDANTS AND HELP TO PREVENT MALNUTRITION.”
I am a very busy person but having good people around me to help is key; once you have good people you try to train your staff and it’s a continuous process in which you play a supervisory role. I go examining for the West Africa College of Surgeons twice each year in Nigeria and Ghana, but I don’t do on-call from the hospital any more, only from home. My husband takes care of a lot of the business side of things. Outside of this I have a full social life, and am involved in my church – you can’t help but be involved when you are back here. It is good to do good.

“WE ALSO SEE A LOT OF GEOTHERMAL BURNS FROM HOT POOLS.”
Deirdre Seoighe was on maternity leave with her three-month old son, Ruadhán in 2019, when New Zealand’s Whakaari/White Island volcano erupted with 47 people on the island. Some died instantly, while others were injured, many su ering severe burns. e nal death toll was 22 people.

Aer graduating, I did the BST and then SpR training in plastics. I worked as a locum consultant in Galway, then lived in New York and came to the National Burns Unit at Middlemore in Auckland for Fellowship in 2016. I was appointed to a permanent consultant position in Hamilton, in the Waikato region, in 2017. I moved for love – I’m married to Joe Baker, an Orthopaedic and Spinal Surgeon, who’s from New Zealand.
I love the burns side of plastics. e patients tend to be from poorer socioeconomic groups and many have lifelong injuries. ey have to live with the impact and rami cations of those, I nd it awe-inspiring the way they get on with life, maybe not quite as before but with a great deal of courage.
Waikato where I work is the biggest hospital in New Zealand, it’s a busy Level One trauma centre serving a population of nearly one million. e Taupo Volcanic Zone lies within our catchment area, this includes several active volcanoes. We also see a lot of geothermal burns from hot pools. I y to Gisborne on the east coast of New Zealand every fourth week and do an operating list and a clinic. We provide a service over a huge area, much of it quite remote so many major traumas are choppered in to us.
Ruadhán turned three months on the day of the volcano. I was taking the older kids to their singing lesson and my husband texted to say there had been a volcanic eruption. I rang in to work, and they said they were expecting casualties and one of the consultants in the ED said, “I think you need to come in.” I wasn’t due back from maternity leave for another four or ve months and was still breast-feeding. I hadn’t bothered introducing a bottle so I couldn’t leave Ruadhán with anyone else because he’d starve. I le the other kids with the babysitter and I went in. We didn’t know what we
were expecting but we were ready and waiting. Someone took the baby from me and said she would let me know when he cried; Waikato is one of these places where they just cope.
Initially we took eight patients, all with serious injuries. We didn’t know their names, ages or nationalities. We operated on all eight that night, nishing at four in the morning. I went home with the baby and came back in for seven the next morning. e hospital management gave Joe leave at short notice to balance my coming in o leave.
e thing about burn injuries is they are very labour intensive. You need a big team in theatre, and the temperature needs to be turned up to 36°C so it’s very hard on sta . You want to do the work quickly and e ciently so the patients don’t lose heat or blood. And you have to operate and do changes of dressings every second day for each patient.
I am the only dedicated burns surgeon but we have six other plastic surgeons. e hospital decided I would oversee the clinical management of these patients. It’s very hard as a surgeon not to be hands-on – your instinct and training is to just get in there and do it all yourself. We had three theatres running at a time, and operated every day for two weeks solid. For four or ve days we had eight patients, then two Australians were airli ed out, two went up to Middlemore, and two unfortunately died. We were le with two, but even two meant operating every day for two weeks. You can only chip away at burns until they heal. ose last two patients stayed for months. ere is really good social medicine in New Zealand, so if you are in an accident all your treatment is covered until you are fully treated. I kept operating until all the burns were o and the new skin was on. We achieved that on Christmas Eve and I went home to Ireland on 26 December. It was a real team e ort with so many people from di erent areas of the hospital helping out.


At school, I was con icted by my love for maths and all things analytical versus a huge interest in science and the humanities (my English teacher told me I was an “unusual case” – I think it was a compliment!). My career started when I joined Irish Life as a trainee actuary when I was 17 and I quali ed as an actuary there. I practised as an actuary for about 15 years, with a break to take a degree in mathematics at Oxford University. is work was largely focused on the nancial services industry. It was a great experience but for me there was something missing so I re-evaluated and decided to return to complete graduate entry medicine in RCSI. I graduated in 2014. I absolutely loved studying medicine for four years and bene ted from the wisdom of some great teachers and mentors. In fact, a er I completed my intern year in Beaumont Hospital, I went back as a clinical lecturer in Connolly Hospital, Blanchardstown, largely focused on lecturing the second year of the GEM programme.
When I was in RCSI I didn’t really know where I was going to end up and that was part of the excitement and intrigue of the journey. I had a huge interest in medical oncology, and working with Professor Liam Grogan and the medical oncology team in Beaumont Hospital was the highlight of my clinical career. I spent some time hoping to pursue a career in medical oncology. However, I was always aware that I had a complementary skill set and wondered about the possibility of combining my two professional lives. I am passionate about medicine – especially innovation in medicine – and healthcare, but I also love turning my mind to complex problems. e determining factor in the direction of my journey was the fact that I had my son in nal med and once I had completed BST, it became apparent to me both from a lifestyle and nancial perspective that it would be impossible to pursue my medical oncology dream. It was a very di cult decision – medical training pathways are typically traditionally routed and don’t easily allow for family life, especially at the early stages. I know that progress is being made in this area and I was supported in my clinical journey as much as was possible within the constraints of the system. Both Professors Seamus Sreenan and John McDermott in Connolly Hospital Blanchardstown were particularly supportive.
In 2018, I took on a new role and challenge with EY’s consulting practice. I hoped to combine my two professional lives. It is fair to say that this has been more than realised.
“THE COMBINATION OF BEING AN ACTUARY AND A DOCTOR HELPS ME TO BE A LEADER IN THIS AREA.”
I work in the eld of health analytics. is essentially relies on mathematical modelling of any and all relevant variables from the whole system to individual patient level factors. We are all familiar these days, for example, with some of the epidemiological concepts that drive the pandemic. My role for the last year or so has been to largely support an understanding of the practical implications of these factors for the demand and provision of healthcare in this country – from both a COVID-19 and non-COVID-19 perspective. ese are complex and largely novel challenges and I hope and believe my ability to combine deep analytical rigour with clinical understanding and insights have helped some of our key decision makers. e work is fascinating.
e work is essentially an evidence-based approach to planning which helps inform strategic and operational planning. It is signi cantly actuarial in nature, which the health domain hasn’t adopted extensively in the past; its value is more appreciated now. ere is a huge opportunity for the advancement of health analytics due to the accelerant factor of the pandemic. e opportunity to optimise population and individual health outcomes is rst and foremost, but this sort of evidence based approach is more far-reaching. We can save taxpayers’ money by embedding premium quality quantitative analysis of expected outcomes as part of the planning cycle and basing decisions on this.
I greatly enjoy the technical aspects of the work. I am also passionate about its communication to key stakeholders. One of the main challenges of my work is to translate complex concepts into simple messages – to me the work is only as good as this step and I work hard to try to ensure that the messaging does justice to the insights generated. e work may be complex, but the messages delivered are best if they can be distilled simply.
e work is specialised and the combination of being an actuary and a doctor helps me to be a leader in this area. None of us ever wanted this to happen, but a pandemic of this nature was a mathematical certainty given how we exist on this planet. It will happen again and it is likely that it won’t be another hundred years. Hopefully we will have learnt valuable lessons this time round – both in terms of future prevention and management.
I miss patient contact and in some ways this has been accentuated by the pandemic, knowing the stress and strain on my clinical colleagues. Ideally in the distant future, I would like to think I can return to some degree of this. However, I love what I do now – I am absolutely passionate about the opportunity for health that this type of work presents. It certainly gives me purpose in getting out of bed every morning.


PhD in Chemistry from the National University of Ireland, PhD, BSc. FRSE, FRSC, CChem, FICI, FCSFS, FFireInv, Professor of Forensic Science, University of
Iwas one of the rst chemistry PhD students at RCSI, arriving in the College in 1989 a er an undergraduate degree in applied science (chemistry and mathematics) at DIT Kevin Street.
My doctorate was in the eld of bioinorganic chemistry. I worked under Professor Kevin Nolan and a second supervisor from UCD. e area was interesting to me because it was connected with medicinal applications, something in which I had a side-interest.
Towards the end of my research, I spent a year working for a Trinity spinout company involved in environmental monitoring and in 1994 applied to Strathclyde University in Glasgow for a lecturing post in the forensic science unit. My parents were the rst private practice consultant re investigators in Ireland, so I grew up having an understanding of the importance of forensic science.
My initial contract was for two years, but I am still in Scotland nearly 30 years later, having worked my way up the academic ladder here, attaining my Professorship in 2011, the rst female Professor in natural sciences in Strathclyde’s history.
In 2014, I moved to the University of Dundee where I am the University’s Professor of Forensic Science, and within 18 months had, with my colleague Professor Dame Sue Black, landed the biggest grant ever awarded (£10m) to forensic science in academia in the UK. What I do now is lead the Leverhulme Research Centre for Forensic Science, which is unusual in that it is funded to undertake disruptive research, to look at the whole ecosystem of forensic science and see where a profound disruption needs to occur in order to shi the culture, focus or mindset of that ecosystem to a better place. For the rst time, we have brought scientists, law enforcement, legal colleagues and the judiciary together to discuss openly the challenges we have all faced in ensuring that evidence presented in the courts is robust and scienti c.
In particular there are concerns about the scienti c robustness of feature comparison evidence where we are trying to link people to ngermarks, bullets to guns, shoes to shoe prints or tools to tool marks. Most of these comparisons are undertaken subjectively rather than through objective veri able measurements with known uncertainties, and this has caused concern about the scienti c validity of that evidence when presented in court. e Leverhulme Research Centre for Forensic Science endeavours to tackle these issues by creating opportunities for senior members of the judiciary and legal practitioners from both defence and prosecution sides to meet with forensic and other scientists, as well as representatives of law enforcement
and the public, to explore what advances in science can do to help address the challenges in relation to evidence being put before the courts and nd solutions.
“WE FACILITATE CONVERSATIONS BETWEEN JUDGES AND SCIENTISTS.”
We facilitate conversations between judges and scientists that don’t take place in a courtroom but in a space where we can all speak freely and discuss each other’s needs and challenges, and work out what research needs to be done to raise the level of science underpinning the evidence that may be admitted to the courts. It enables frontline practitioners to work with academic researchers to tease out what exactly is the challenge around a particular evidence type and how to work collectively to address that challenge.
While it is not my core job, I also undertake forensic casework for both prosecution and defence in relation to re investigation and clandestine drug manufacture, my speci c areas of expertise, and also give expert testimony in court and at public enquiries.
We have now secured an additional £15m of funding commencing in 2024 to fund JustTech, the world’s rst institute for innovation for forensic science, which will take the output of academic researchers and translate it into operational practice. It’s a translation engine but also a space where we can be adventurous, try things and fail safely so as ultimately to develop and implement technologies that are really t for purpose when they go into the operational context.
ese days my teaching load is small, as I manage a sta and postgraduate student complement of 42. e thing that is most enjoyable is watching how sta who have come into the Centre, with diverse backgrounds from social science to computing and the natural sciences, have developed together as an interdisciplinary team working on everything from public engagement to the development of research in new psychoactive drugs, the use of virtual reality in forensic casework and understanding transfer and persistence of DNA. With our tech and administrative sta we all work together like one big family. It is a pleasure to see them understanding each other’s areas of expertise and also to witness their willingness to help each other. Doing interdisciplinary research is really hard as it is di cult to get people to see the perspective of others, so it is great to see now there is no fear of getting stuck in and facilitating these open discussions.
VETERINARIAN
Prior to RCSI, I quali ed as a vet in UCD and worked in the UK and Ireland. My time in Surgeons was one of the best periods in my life – great sta , great classmates from all over the world and great craic.
A er graduating from RCSI, I interned in Drogheda, which was run by a religious order, the Medical Missionaries of Mary, who operated several hospitals in Africa. In 1988, I volunteered to work in a very rural area in Tanzania for two years where the order ran a busy hospital and mother and baby clinics in 22 villages in the district. e hospital was the last stop for patients and there was no referral so whatever came in had to be dealt with. e HIV epidemic had started and at the time there was no antiretroviral therapy so a diagnosis of HIV/AIDS was an inevitable death sentence.
When I returned from Tanzania I worked in the UK. I got a bit of a shock as a er working in Kabanga I thought I could do anything, but all my peers had acquired Memberships and Fellowships and proceeded up the medical career ladder. But I was lucky and got a few breaks.

I started o as an SHO, enrolled in a public health training programme, and worked in public health departments in Kent and Berkshire. I did a Masters as a Research Registrar in the Hammersmith Hospital on the molecular epidemiology of infectious diseases. From there I went to work in the UK Communicable Disease Surveillance Centre on the Public Health Laboratory Services laboratory campus in Colindale, London. Initially I was working in the HIV/AIDS Division and I did my Membership of the Faculty of Public Health Medicine while there.
was Scottish wanted to go home, and I got the job as his locum, which tee’d me up to get the fulltime position a year later.
e BSE epidemic undermined consumer con dence in the entire food supply and triggered global reforms on the oversight of the food chain. I was involved in working groups in the UK engaged in setting up an independent food agency, the Food Standards Agency. In Ireland the BSE epidemic was causing a double problem in that, in addition to undermining consumer con dence, our beef exports were collapsing. Ireland wanted to set up its own food safety agency, but there were di culties in deciding whether it should fall under the aegis of the Department of Agriculture or Department of Health. Each had di erent views as to what kind of a CEO was required, but a compromise would be a vet and a doctor. I was headhunted for the job and returned to Ireland a er eleven years away.
Setting up and running the Food Safety Authority was a brilliant job and I met and worked with fantastic people from the public service and the food industry, and in the Government. A er my ve-year term as CEO I got a position as Chairman of the newly formed European Food Safety Authority (EFSA), initially headquartered in Brussels, and then moved to Parma in Italy, where I ate my fair share of Parma ham and Parmesan cheese. One interesting assignment was being on the food safety committee for the Beijing Olympic Games which involved many trips to China. I am still on the International Scienti c Advisory Committee of the Chinese National Centre for Food Safety and Risk Assessment.

Diplomate in the European College of Veterinary Public Health Professor of Public Health UCD
“WE HAVE BEEN OPERATING A BUSY CONTACT TRACING CENTRE FOR THE HSE SINCE THE START OF THE PANDEMIC.”
Next I went to work in the Field Investigation Service where we investigated many very interesting outbreaks from TB to legionella and cryptosporidiosis, and numerous foodborne outbreaks. It was a great learning environment and I had the opportunity to go for training to the CDC in Atlanta. We had a great bunch of epidemiologists and molecular scientists in the Centre in London at this time; Dr Mike Ryan, who is now in the WHO, was there with me.
I got another one of my lucky breaks when the head of the Gastrointestinal Division, who was younger than me, took a job in Scotland as his wife, who
A er my EFSA adventure, I got a part-time job in UCD covering for the late Dan Collins, the Professor of Veterinary Public Health, who had retired. Subsequently a job came up in the School of Medicine. UCD is full of young people who are positive and optimistic; they have an infectious enthusiasm and I get energy from them. One Health is my area and I teach medical, veterinary, agriculture and food safety students and, with my colleagues in the School of Public Health, I run the Masters in Public Health Programme. Dr Ronan Glynn, the acting CMO, is one of our star alumni. I am involved in the Public Health and One Health programmes in the RCSI/UCD satellite campus in Penang, where I spend a few enjoyable weeks each year.
With my colleague Professor Mary Codd, we have been operating a busy contact tracing centre for the HSE since the start of the pandemic. Initially it was manned by volunteers and now we have progressed to having contract sta . Many of our graduates make up the core team and they are doing great work assisting the public health doctors in the HSE, investigating webs of transmission and tracking variants of concern.
My main hobbies are shing and horse riding and I spent four years as the Chairperson of Horse Sports Ireland, the governing body of equestrian sport in Ireland. I breed a few horses and I have one I ride daily to keep me sane. ■

For visiting alumni, the unique aroma in the Anatomy room at RCSI stimulates the limbic system, and brings memories ooding back. Above the skeletons, dissections and models, hangs a collection of artworks, donated by students and visiting artists.
Professor of Anatomy, Clive Lee recounts the remarkable story of Anatomy at RCSI
The Department of Anatomy is almost as old as the College, with the rst Professor appointed in 1785. Twenty-nine Professors and 236 years later, it remains the oldest chair of anatomy in continuous existence in Ireland. Professor John Halahan began by teaching from his own premises, but in 1789, a two-storey house adjoining Mercer’s Hospital was purchased for the Schools of Anatomy and Surgery. e theatre, museum and preparation room were on the upper oor, with the dissecting room on the ground oor, enlarged in 1796, and there was ready access to Goat Alley for the discreet delivery and removal of cadavers.
Halahan was also the Professor of Anatomy to the Hibernian Society of Artists and, from 1789, held the RCSI Chair jointly with William Hartigan. Hartigan was notable for carrying a pair of kittens in the pockets of his great-coat and, along with William Lawless, wrote A Syllabus of a Course of Lectures on Anatomy and Physiology in 1796, comprising 103 lectures delivered between October and April. Hartigan treated the fatally injured Lord Edward Fitzgerald in 1798, while Lawless ed to France to join Napoleon’s army and was expelled by the College. His successor, Richard Dease, was even less fortunate, as he died of septicaemia acquired while demonstrating anatomy in 1819. In 1824, a similar fate befell the Curator of the Museum, John Shekleton, and it was not until 1867, and the
discoveries of antisepsis by Lister, and formaldehyde by von Hofmann, that dissection became safe.
One RCSI student in the 1790s was not impressed by the systems-based teaching approach. Hartigan and Lawless’s syllabus began with osteology followed by myology, angiology, neurology, respiration, digestion, secretion and the urinary organs, and nally generation. It was, the student later wrote, like attempting to: “explain the mechanism of a watch, by taking it to pieces, and giving a separate description of every particular wheel and spring without a erwards attempting to show by what contrivance the one moves the other … the student who has been shown the venous, arterial and nervous systems of the arm, does not know how each of them lies with respect to each other.”
This is student feedback, but it was written when Abraham Colles was already in the Chair, having been the rst graduate so appointed in 1804. Colles’ book of 1811, A Treatise on Surgical Anatomy, also provided the solution – to teach anatomy topographically, region by region: “to describe the relative position of the parts and to point out the subservience of anatomical knowledge to surgical practice”.
In 1810, the College moved to St Stephen’s Green, and the plans for the dissecting room were altered during building due to “the great increase in pupils”. In 1812, the construction of “extensive” dissecting rooms was underway, and this is now the south aisle of the Anatomy Room, the remaining top-lit aisles being added in 1891-2. In 1826, when the Chair was jointly held by Colles and Charles Hawkes Todd, 224 pupils attended. e Lancet described the behaviour of the students at one of Colles’ packed teaching sessions: “But the bell rings – Mr C’s carriage is at the gate – the benches ll – confusion in all its fantastic forms of juvenile levity prevails throughout the scene. e whole artillery of confectionery, from canister lozenges to the heavy grape-shot of spice nuts, is ying on all sides – while other aspirants for anarchical reputation eagerly contend for the aromatic ammunition. On another side some musical amateur amuses the audience with the fashionable song or quadrille of the day. us everyone contributes something to increase the scene of unphilosophical tumult. Here, I must cease – the folding doors open – and in hurries Mr C – with a slip of paper, twisted round his index nger – a simultaneous burst of applause greets his welcome entry, but modestly declining the honour intended him, he instantly proceeds, without even returning the salute, ‘Gentlemen, at our last meeting’ …”
A student of this period was Dominic Corrigan, of aortic incompetence fame, who later published this account of body snatching, “Reminiscences of a Medical student Prior to the Passing of the Anatomy Act”, in the BMJ: “We moved with our hands the recently deposited clay and stones which covered the head and shoulders of the co n –
no more was uncovered; then a rope about three or four feet long was let down, and the grapple, an iron hook with the end attened out attached to the rope, was inserted under the edge of the co n-lid. e student then pulled on the rope until the lid of the co n cracked across. e other end of the rope was now inserted around the neck of the dead, and the whole body was then drawn upwards and carried across the churchyard to some convenient situation … awaiting the car that was to convey it to some dissecting theatre.”
HARTIGAN WAS NOTABLE FOR CARRYING A PAIR OF KITTENS IN THE POCKETS OF HIS GREAT-COAT ...
e Anatomy Act of 1832 provided for bodies to be obtained legally and stopped the practice of body snatching. By today’s standards, dissection of human remains without the explicit consent of the person themselves, or their next-of-kin, is unacceptable. Robert Harrison, who published e Dublin Dissector, and Arthur Jacob, who described the layer of rods and cones in the retina, were both appointed in 1827. Jacob served for 40 years and was the “uncompromising champion” of the RCSI Medical School. In 1844, he addressed the new students: “ is College, although called a College of Surgeons, is, as you all know, just as much a College of Physicians. We have the same corps of professors, or even a larger one; we require the same course of medical studies, or even a more extended one; and we examine as carefully on medical subjects as they do in the schools of medicine. In fact, this is a College of Medicine and Surgery, and the Diploma you receive from it is universally accepted as evidence of your tness to practice every branch of the healing art.”
In 1837, a Chair of Descriptive Anatomy was founded and its occupants included John McDonnell, who used ether anaesthesia only ten weeks a er its introduction in Mass General, and Sir William ornley Stoker, brother of the author Bram. Bram Stoker’s composition notes for Dracula show that he consulted his elder brother about the medical scenes in his novel. Stoker collected antiques, furniture and objets d’art. Oliver St John Gogarty quotes the author George Moore, who examined a Chippendale chair and inquired: “A cancer, Sir ornley, or a gallstone?” in reference to Stoker’s habit of buying “a museum piece” a er carrying out a major operation. e rst fulltime professor was Daniel Cunningham, who went on to write Cunningham’s Manual of Practical Anatomy, the successor to e Dublin Dissector. He was followed by Alexander Fraser who wrote a pioneering neurosurgery text Guide to Operations on the Brain. e departures of Edward Dillon Mapother and Stoker in


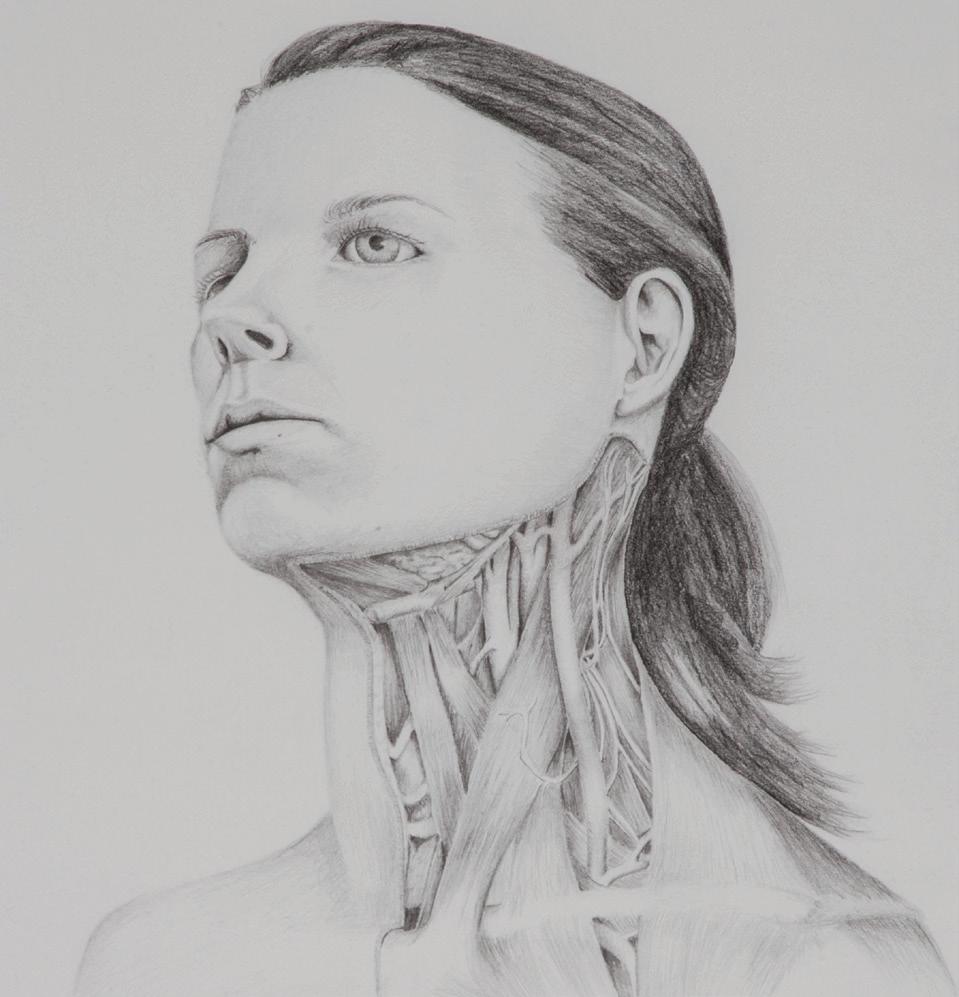


1889, and the amalgamation with the Ledwich and Carmichael medical schools, led to the establishment of the Chair of Anatomy rst held by Frederick Nixon and Francis Heuston.
THE RIFLE RANGE WAS IN THE BASEMENT, BESIDE THE EMBALMING ROOM.
Auckland Campbell Geddes was the rst Professor of Anatomy as we know it. A Boer War veteran appointed in 1909, he introduced a number of reforms, literally cleaning up the Department. He founded the RCSI O cer Training Corps at the students’ request – the ri e range was in the basement, beside the embalming room. Geddes brie y served as Dean, before resigning to take the chair at Magill University in Montreal in 1913. An extraordinary career saw him serve as Brigadier General and Director of Recruiting in the War O ce (1916-17), MP for Basingstoke (1917-20), Minister of Reconstruction (1919) and President of the Board of Trade (1919-20). He was appointed British Ambassador to the United States (1920-24), Chairman of the Rio Tinto Company (1924-47) and was elevated to the peerage as Baron Geddes of Rolvenden in the County of Kent in 1942.
Evelyn John Evatt served from 1913-1947, with a break for active service in the Great War, earning the DSO at Gallipoli. Evatt enjoyed teaching in the Anatomy Room, regarding it as “a fountain of perpetual youth” and among his students who won the Stoney Memorial Gold Medal were two future Registrars, H O’Flanagan (1936) and WAL MacGowan (1945). e 1st Med prize medal was subsequently named a er Evatt, and he appointed Billy White as Technician, a role Billy held up to the 1980s.
In 1947, Evatt was succeeded by a surgeon, AK Henry, who had served in the army medical corps of the Serbian, British and French armies in the Great War, being made a Chevalier de la Légion d’Honneur for his services to France. He
was Professor of Surgery in Cairo and at the Postgraduate Medical School at Hammersmith and wrote the classic applied anatomy text, Extensile Exposure Applied to Limb Surgery. He instituted the College canteen, which was named a er him on two occasions in di erent locations, the rst in the basement of 123 St Stephen’s Green and the second on the First Floor of the 1970s building, beside the Exam Hall. He was also a patron of the boxing club and a ring was erected between the pillars of the Anatomy Room. Henry recognised the unique teaching talents of Tom Garry, who had disagreed with the examiners in UCG and came to live in York Street. Garry’s aphorisms were legendary – the appendix as an organ of no xed abode – and most of the mnemonics used in the Anatomy Room – 1,3,5,7, 9,10, 11 for the spleen – are linked with this original Surgeon Prosector.
Gilbert Marshall Irvine, another military man, succeeded Henry in 1959. According to Terry Byrne, he would stand on the landing overlooking the Anatomy Room, shout “Byrne”, and Terry would be expected to come running. On the day of Terry’s retirement 48 years later, we tried this out again – he enjoyed the joke. Irvine was joined, and then succeeded by Brendan Rooney in 1969. Academics Jim Doyle, brother of Stephen, Moira O’Brien and Anne Legge taught during this period, assisted by Technicians Terry Byrne, Peter Kellaghan (recently retired after 47 years) and Eric Clarke. Following Dr Legge’s tragic death in a car accident, graduate and Fellow, Krikor Erzingatzian, returned to


the Department. Surgeon Prosectors, including Jock O’Hanrahan and Michael McCormack, and more youthful Demonstrators, taught in the Anatomy Room. ‘Card Signings’ were major events. Over time, these have evolved from the signing of a card con rming that a region had been satisfactorily dissected, to a tutorial where the student identi es structures and answers questions on the area they have been studying in the presence of their peers – then it is their classmate’s turn, so they learn from each other. Student feedback indicates that they regarded such ‘Card Signings’ with trepidation at the time, but look back fondly on them as they learn a lot, become skilled at thinking on their feet and appreciate that they helped keep them up to date. at said, some graduates still complain about getting a B on the orax.
e appointment of Stanley Monkhouse in 1988 coincided with an almost complete change of teaching sta . Harold Browne, Seán Hanson, Max Ryan and later Kamal Sayed joined as Surgeon Prosectors and Pat Felle and myself as Lecturers. Stanley’s approach was straightforward – what do medical students need to know and what is the best way to teach them? He transformed the anatomy curriculum with his Blue and Pink books and text books on Cranial Nerves and Clinical Anatomy, and histology online. New lecturing sta included Skantha Kandiah, Gloria Meredith, Tom Farrell and Alice McGarvey. Stanley introduced our Service of anksgiving for those who so generously donate their remains for medical teaching and research. It is held every two years and is an opportunity for our sta and students to meet and thank the families of our donors. Stanley was a very successful Vice-Dean, and brie y Professor of Physiology, before returning home to England and ordination as an Anglican priest.

When I took over in 2002, the aim was to continue the successful teaching programme, but changes in surgical training had made Anatomy Demonstratorships unattractive to surgical trainees. e answer was to recruit more Surgeon Prosectors including Dan Kelly, Eddie Guiney, Brian Lane, Ray Fitzgerald, Paul Farrell, Arthur Tanner, Frank Keane, Henry Osborne, Alec Blayney, Freddie Wood, Bill Quinlan, Frank Thompson, Jim Griffin, Michael Earley, Parnell Keeling, David Charles, Catherine Riordan, Tom Gorey, Patricia Eadie and Cara Connolly, now a Clinical Lecturer. They have
received excellent technical support from John O’Brien, Vincent McDonagh, Katie Reeve-Arnold, Bob Dalchan, Andrew Lynch and Patrick Conlon. In the Division of Biology, Peter Sta ord supported Alec Elliott, Brendan Kavanagh and Jacqueline Daly. Brendan, Tom Farrell, Alice McGarvey, Jane Holland, Cathal Kearney, Emmet ompson and Oran Kennedy have all won President’s Teaching Awards, while Tom, Oran, Cara Connolly and myself have won national Teaching Hero Awards.
Student course books now cover the entire rainbow and everything from Postgraduate Courses in Surgical Anatomy to Physician Associate Studies. Two students, Jamil Ahmad and Matthew Inwood, created dissection videos and this was extended by Farhad Kheradmand to create an online Dissection Guide. Valerie Morris followed suit with an online Surface Anatomy Guide – try Googling ‘RCSI Surface Anatomy videos’. Central to this were Anil Kokaram, an Oscar-winning engineer from TCD, and artists Mick O’Dea and Una Sealy from the Royal Hibernian Academy.
Fergal O’Brien was the rst engineer appointed to the Department. He had done his PhD in bone biomechanics with us before embarking on a Fulbright to MIT. On his return, he set up the Tissue Engineering Research Group, and its alumni Garry Du y, Cathal Kearney, Oran Kennedy, Caroline Curtin, Aamir Hameed, Ciara Murphy, Olga Piskareva, Claire Conway, Shane Browne and Fabio Quondamatteo have successfully combined teaching and tissue engineering research. Fergal now has a personal chair and is RCSI’s Director

of Research and Innovation. e importance of both teaching and research is re ected in our 2019 renaming as the Department of Anatomy & Regenerative Medicine. We have been very fortunate to have excellent administrative support provided by our Department Secretaries, from Margaret McCarthy and Annette Sweeney, Sinead Byrne, Mary Brennan and Amanda Campbell to Lorraine Harte and Laraine O’Brien.
In all of this, we have tried to keep the interests of our students paramount, to ensure that they can learn the anatomy that is essential for clinical practice. e unique and priceless gi of the human body from the donor provides a source of knowledge that is the foundation of medical education and research. A former President of RCPI, John Donohoe, used to say that students remember their teachers with great clarity and varying degrees of a ection. To this I add that teachers remember their students with great a ection and varying degrees of clarity. So if you are in Dublin, do drop in to say hello. We’ll bring you into the Anatomy Room, where the unique aroma will stimulate the limbic system and bring the memories ooding back. From the dado rail down, all will be familiar – skeletons, dissections and models – but above hangs our collection of artworks, donated by our students and visiting artists, some of which are shown here. We look forward to welcoming you. ■


RECENT HIGHLIGHTS


In 2021, the success of RCSI researchers re ects the contribution that scientists make to our society and economy
Researchers at RCSI are leading a new €3m study to investigate the real-world effects of the newest cystic fibrosis (CF) medications as they become available for people with CF. The research will look at how a new triple combination CF drug, Kaftrio, will affect people in their day-to-day lives, rather than in controlled clinical trial conditions. Kaftrio (known as TriKafta in the US) is a successor to Orkambi.
The project, called RECOVER, has been awarded €2.85m from the Cystic Fibrosis Foundation (US), €112,000 from the Cystic Fibrosis Trust (UK) and €100,000 from Cystic Fibrosis Ireland (CFI). Professor Paul McNally, Associate Professor of Paediatrics at RCSI, Respiratory Consultant in Children’s Health Ireland and lead researcher on the RECOVER study said: “Clinical trials occur under very controlled conditions and exclude many sick people with CF. ‘Realworld’ studies are essential to confirm the trial findings and examine in-depth effects on the everyday lives of all people with cystic fibrosis.” The Irish research team is collaborating with researchers in 16 clinical and university sites in the UK, Europe and North America. Philip Watt, CEO, CFI said: “Cystic Fibrosis Ireland is proud to support this major research study.”
A new research study from RCSI and CHI Temple Street will examine if Ireland’s COVID-19 restrictions will result in an increase in allergies in infants born since March 2020. The study will investigate whether the lower rates of viral infections and improved air quality which resulted from the lockdown are going to make allergic conditions more or less common in children born to families who have experienced social distancing and isolation. Identifying non-acute consequences of COVID-19 is now a global research priority.
Professor of Paediatrics at RCSI, Jonathan Hourihane, who is leading the study that will involve 1,000 infants born in Ireland between March and May 2020, said: “The lockdown presented a unique opportunity to examine the early origins of often lifelong diseases that constitute a major health and social burden in Ireland.”
Allergic diseases like eczema, asthma, hay fever and food allergy



that have become more common over the last 30 years, are thought to result from decreased exposure to infections due to smaller family sizes, the introduction of effective immunisations against the most serious infections, and community focus on hygiene. This is called the “Hygiene Hypothesis”. Air quality, which has also worsened in industrialised nations over the last 30 years, also affects allergic conditions.
Professor Hourihane said: “After birth, a baby’s immune system soon focuses on the new challenges that life outside the womb brings, including fighting infections and responding to immunisations. We want to see children playing on the floor, getting dirty, and being exposed to lots of people in lots of environments. The outcome of this is usually a stronger immune system.”
The study received funding from the Clemens Von Pirquet Foundation, a European allergy charity, and the Temple Street Foundation.

Researchers from RCSI have discovered that testing the levels of certain proteins in blood samples can predict whether a person at risk of psychosis is likely to develop a psychotic disorder years later. Blood samples taken from people at clinical high risk of psychosis were analysed and individuals followed up for several years to see who did and did not develop a psychotic disorder. Scientists found patterns of proteins in the early blood samples could predict who did and did not develop a psychotic disorder at follow-up. The most accurate test correctly identified those who would go on to develop a psychotic disorder in 93% of high-risk cases, and it correctly identified those who would not in 80% of cases.
RCSI was granted €1.3m from Wellcome to further develop this blood test. The grant will enable researchers to determine if this test is similarly accurate at predicting who will develop a psychotic disorder from other international groups of clinical high risk individuals. The ultimate goal is to develop a commercially available test for use in clinical practice so people can be treated earlier and more effectively. The work builds on a patent previously filed by the researchers, and this grant marks a key step in commercialising the test.
“Wellcome’s support will enable us to further expand our research and directly benefit patients,” said Professor David Cotter, Professor of Molecular Psychiatry at RCSI, Consultant Psychiatrist in Beaumont Hospital, Dublin and investigator at FutureNeuro, the SFI research centre for chronic and rare neurological diseases. “We would like to prevent psychotic disorders, but that requires being able to accurately identify who is most at risk. This grant will allow us to study these markers in other people at high risk of psychosis to confirm our previous findings.”
“I would like to congratulate Professor Cotter and his team and thank Wellcome for awarding RCSI this grant,” said Professor Fergal O’Brien, Director of Research and Innovation at RCSI. “The funding will be instrumental in carrying out a core mission of RCSI research – translating research from the laboratory directly to the patient. I look forward to seeing this research forge new paths in psychiatric care.”
The grant comes from Wellcome’s Psychosis Flagship developing novel, targeted interventions for psychosis. On this project, RCSI will collaborate with researchers from the UCD Conway Institute and from Cardiff University, among others.
Scientists have found that air pollution in winter is associated with more hospitalisations for all strokes in Dublin. The study, led by researchers from RCSI, is published in Cerebrovascular Diseases.
After accounting for other variables, researchers found there was a statistically significant rise in the number of hospitalisations for strokes in Dublin zero to two days after a rise in air pollution. The study marks the first time there has been a link demonstrated between short-term air pollution and stroke in Ireland.
“Every year, more than 10,000 people in Ireland have a stroke. Our research adds evidence that there needs to be a national ban on solid fuel burning to help in our efforts to reduce this number,” said Dr Colm Byrne,

the study’s lead author and clinical lecturer in the RCSI Department of Geriatric and Stroke Medicine.
The research was carried out by researchers from RCSI; Dr Colm Byrne, Professors Kathleen Bennett, Anne Hickey and David Williams in collaboration with Dr Paul Kavanagh from the Health Intelligence Unit in the HSE, and Professors Brian Broderick and Margaret O’Mahony from Trinity College Dublin.
28 COLLABORATIVE AGREEMENTS WITH INDUSTRY IN 2020 RCSI research impact in 2020
70% INNOVATION ACTIVE
2.7M Research PIs
4.5M INDUSTRY FUNDING FOR RESEARCH IN 2020 ENABLED RESEARCH COMMERCIALISATION FUNDING IN 2020
2,831 COLLABORATING INSTITUTIONS 2015 - 2019*
123 COLLABORATING COUNTRIES
51% PUBLICATIONS 2015 – 2019 OPEN ACCESS*
15 NE W INVENTIONS DISCLOSED
10 COMMERCIAL AGREEMENTS IN 2020
4,192 SCOPUS INDEXED PUBLICATIONS 2015 – 2019*
1,436 PUBMED INDEXED ARTICLES IN 2020
A study has found that adolescents who frequently use cannabis may experience a decline in intelligence quotient (IQ) over time. The paper, led by researchers at RCSI, is published in Psychological Medicin e. The results revealed that there was a decline of approximately two IQ points over time in those who use cannabis frequently compared to those who didn’t use cannabis.“Previous research tells us that young people who use cannabis frequently have worse outcomes in life than their peers and are at increased risk for serious mental illnesses like schizophrenia,” commented senior author on the paper Professor Mary Cannon, Professor of Psychiatric Epidemiology and Youth Mental Health, RCSI. The study was carried out by researchers from the Department of Psychiatry, RCSI and Beaumont Hospital, Dublin. The research was funded by a YouLead Collaborative Doctoral Award from the Health Research Board (Ireland) and a European Research Council Consolidator Award.

Professor Fergal O’Brien was announced as the winner of the Science Foundation Ireland (SFI) Industry Partnership Award 2020 in recognition of a successful collaboration with Integra LifeSciences on biomaterials spanning more than 15 years. The award was one of eight categories announced at the 2020 SFI Awards by Minister for Further and Higher Education, Research, Innovation and Science, Simon Harris TD at the annual SFI Science Summit.
Professor O’Brien, who is Professor of Bioengineering and Regenerative Medicine, Director for Research and Innovation and Head of Tissue Engineering Research Group at RCSI, brought his extensive experience to bear in leading this longstanding SFI Centre for Advanced Materials and Bioengineering Research (AMBER) partnership in collaboration with Integra LifeSciences. Since 2017, the collaboration with Integra has grown to a €1m-plus SFI AMBER co-funded spoke project led by Professors Fergal O’Brien
and Conor Buckley (TCD). This project has successfully developed two unique peripheral nerve repair technologies, both of which have proven highly effective in repairing damaged nerves in pre-clinical trials. These technologies have been protected by three patent filings and transferred to the company under appropriate commercialisation agreements.
Professor Mark Ferguson, Director General of SFI and Chief Scientific Adviser to the Government of Ireland, congratulated the award winners, saying: “I am delighted to congratulate this year’s award winners on their inspiring success and dedication. The SFI Awards recognise the expansive contribution that scientists make to our society and economy. Working closely together, the Irish research community continues to be impactful, inspirational and world-leading.” Professor Cathal Kelly, RCSI Chief Executive, congratulated Professor Fergal O’Brien on the notable award.
Researchers at RCSI have discovered a molecule, BAS-2, that can selectively kill cells in triple negative breast cancer; up to 70% of patients with this form of breast cancer develop resistance to treatment.
“Our aim now is to develop the small molecule into a more drug-like compound and to assess if we can harness the new function for potentially improved treatment of patients,” said Dr Tríona Ní Chonghaile, the study’s corresponding author and an RCSI lecturer in Physiology and Medical Physics.
To better understand how the molecule killed the cells, the researchers confirmed that it inhibited an enzyme called HDAC6. Using state-of-the art mass spectrometry, the researchers identified, for the first time, that HDAC6 plays a key role in altering energy in these cancer cells.
The work was funded by the Wellcome Trust Seed Award, L’Oréal-UNESCO For Women in Science Programme and SFI’s Frontiers for the Future Programme. In addition to those from RCSI, the work was carried out by researchers from the UCD Conway Institute of Biomedical and Biomolecular Sciences, NYU Langone Medical Center, Penn State University, the Koch Institute for Integrative Cancer Research at MIT and the Dana-Farber Cancer Institute at Harvard Medical School. With the help of RCSI’s Office of Research and Innovation, the researchers have submitted a patent around this work and are seeking industry partners to further develop this treatment.

RCSI and FutureNeuro, the SFI centre for neurological diseases at RCSI, were recognised at the Irish Pharma Industry Awards for their pioneering contributions to epilepsy research and development. A team led by Professor David Henshall and FutureNeuro Funded Investigator Dr Cristina Reschke earned the Research and Development Award for pioneering microRNA therapeutics for the treatment of epilepsy and their sustained industry engagement and commercialisation of this research.
MicroRNAs play a key role in regulating the production of proteins in the body. The researchers found that a certain microRNA is abnormally high in people with epilepsy. Through pre-clinical testing, they have determined that drugs that silence these microRNAs can reduce seizures.
Treatments such as this have entered into clinical trials for other diseases; however, this is the first microRNA-based therapy under advanced development for epilepsy treatment. If it is successful, it would be a groundbreaking treatment for those with epilepsy who do not benefit from current medications.
“Epilepsy can be a debilitating disease, with seizures interrupting everyday life for some patients,” said Professor Henshall, RCSI Professor of Molecular Physiology and Neuroscience and Director of FutureNeuro. “Seizures in 30% to 40% of patients with epilepsy fail to respond to anti-epileptic drugs or other treatments. If we are able to further this research to a successful treatment of the disease, it would improve patients’ quality of life immeasurably.”

By combining genomic testing and next generation sequencing technology, a new partnership led by RCSI researchers aims to advance predictive tests for multiple myeloma (MM), the second most common blood cancer in Ireland. The study will be carried out at Beaumont Hospital Dublin and run through the Blood Cancer Network Ireland with several other cancer hospitals in Ireland participating. It represents a collaboration between RCSI and SkylineDx with funding support from Amgen; Celgene, a Bristol Myers Squibb company; and Janssen.
Multiple myeloma is a cancer of plasma cells in the bone marrow that normally produce antibodies to help fight infection. Approximately 250 patients are diagnosed with this condition in Ireland every year. Globally the incidence of this disease is rising, due to population growth, an ageing world population and a rise in age-specific incidence rates. Patients often require multidisciplinary medical input and myeloma drugs are amongst the highest-cost therapies worldwide. Due to improvements in new treatments for MM, the outlook for patients has greatly improved. However, MM is still considered an incurable disease, with the majority of patients following a relapsing course and requiring further treatment to keep the disease at bay.

Predicting the course of the disease and guiding treatment choice in newly diagnosed patients is one of the major challenges in this regard. Newly developed tests over the last number of years are helping to do this and one such example is Minimal Residual Disease (MRD). This is a test performed on the patients DNA at diagnosis by Next Generation Sequencing (NGS), which can detect if there are trace amounts of the cancer remaining in a patient after treatment. Another test that can help to predict patients outcomes has been developed by SkylineDx, which uses a novel gene expression based test to guide prognosis called the ‘MMprofiler’.
At Beaumont and RCSI, in collaboration with SkylineDx, scientists have implemented these novel gene-based tests for the testing of MM patients in order to guide prognosis. This test called “ MMprofiler with SKY92 ” establishes if patients have a high risk of relapsing and has been increasingly adopted in global clinical trials as a more predictive and robuster marker than older tests like fluorescence in-situ hybridization. This study aims to combine these two highly predictive modalities to provide a personalised medicine approach for patients.
“If our study can definitively determine which patients will benefit from certain treatments, and when, it will provide clinicians with invaluable information that will lead to better outcomes for patients with MM,” said Professor Siobhán Glavey, Honorary Senior Lecturer at RCSI, Consultant Haematologist at Beaumont Hospital and the project’s Principal Investigator.
The Health Board Research (HRB) Impact Award 2021 was awarded to Professor Gerry McElvaney in recognition of his outstanding contribution to research. Throughout his career, Professor McElvaney proactively integrated research into policy and practice. His work focused on a specific genetic disorder called alpha 1 anti-trypsin deficiency (AATD) that leads to an increased risk of developing lung complications such as chronic obstructive pulmonary disease (COPD), which accounts for 5% of all deaths globally and is the second most common cause of lung-related deaths in Ireland. Presenting the award, Dr Mairéad O’Driscoll, Chief Executive at the HRB said: “Professor McElvaney has been applying research evidence to affect positive change in health, care and practice both here in Ireland and on a global scale.” Accepting the HRB Impact Award, Professor McElvaney said: “It is wonderful to see the outcomes of research materialise into real benefits for patients and the public and how the efforts to translate these findings have visibly improved people’s lives. People are at the centre of this work.”
RCSI Professors Gerry McElvaney and Ger Curley are leading a randomised double blind placebo controlled clinical trial of alpha-1-antitrypsin (a protein produced by the liver which normally acts to protect the lungs from the destructive actions of common illnesses) to treat critically ill patients mechanically ventilated in ICU with COVID-19 associated Acute Respiratory Distress Syndrome.
“A greater understanding of how the body’s inflammatory mechanisms are impacted upon by COVID-19 could open the door to several potential therapies including antiviral medications and targeted immune-modulators such as alpha-1antitrypsin,” says Professor McElvaney.
Professor Curley explains that “We know many
Science technology company 3M has awarded a significant research grant of €420,000 to RCSI, part of a $5m initiative to support research programmes with a focus on treatments and vaccine development for COVID-19.
RCSI CEO Professor Cathal Kelly said: “RCSI’s success in securing funding in this international competition is testament to the quality of the research being driven by our principal investigators.”
The research will focus on two specific areas of interest – the formation of micro blood clots within the lung and the ability of a repurposed drug to slow or stop the virus from causing severe damage leading to sepsis/septic shock. A team of RCSI researchers at the Irish Centre for Vascular Biology at St James’s Hospital, Dublin, led by Professor James O’Donnell, demonstrated that COVID-19 is associated with a unique type of blood clotting disorder that is primarily focused within the lung and which undoubtedly contributes to high levels of patient mortality. This new project will investigate the mechanisms through which COVID-19 triggers the formation of
COVID-19 patients in ICU develop severe inflammation throughout the body with a disproportionately high rate of progression to acute respiratory distress syndrome, acute renal failure, shock and heart arrhythmia.”
Professor Curley says that the most unanticipated differentiating factor between patients with stable and severe disease is not the degree of increase in inflammatory proteins, but rather the relative decrease in levels of an anti-inflammatory protein which indicates that the patients’ anti-inflammatory mechanisms are failing. “This suggests that a therapy which augments the body’s own inflammation-resolving mechanisms might have a positive impact. We are confident that this clinical trial will demonstrate the potential for alpha-1 to improve the outcomes for patients with the most

these micro-clots so that more effective treatments can be developed, particularly for those patients in highrisk groups.
The second study, led by Professor Steven Kerrigan will investigate a new approach to prevent the novel Severe Acute Respiratory Syndrome coronavirus-2 (SARS-CoV-2) that causes COVID-19-recognising human cells.
This project builds on pre-clinical research carried out by Professor Kerrigan’s team, supported by the Enterprise Ireland Commercialisation Fund. Plans to advance these findings into human clinical trials through an RCSI spin-out company, called Inthelia Therapeutics, are currently underway.

severe COVID-19-induced respiratory difficulties.”
This first Investigational Medicine Product trial to be approved in Ireland to test a therapy to treat COVID-19 is sponsored by RCSI and coordinated by the RCSI Clinical Research Centre. Beaumont Hospital is the first site to recruit patients. The study is supported by Grifols, a Barcelona-based multinational healthcare company.
RCSI researchers have developed a score that can accurately predict which patients will develop a severe form of COVID-19. The measurement, called the Dublin-Boston score, enables clinicians to make more informed decisions when identifying patients who may benefit from therapies, such as steroids, and admission to the ICU. Until this study, published in The Lance t, no COVID-19-specific prognostic scores were available to guide clinical decisionmaking. The blood test works by measuring the levels of two molecules that send messages to the body’s immune system and control inflammation. One of these molecules, interleukin (IL)-6, is pro-inflammatory, and a different one, called IL-10, is anti-inflammatory. The levels of both are altered in severe COVID-19 patients. Based on the changes in the ratio of these two molecules over time, the researchers developed a point system where each 1-point increase was associated with a 5.6 times increased odds for a more severe outcome. “The Dublin-Boston score is easily calculated and can be applied to all hospitalised COVID-19 patients,” said RCSI Professor of Medicine Gerry McElvaney, the study’s senior author and a consultant in Beaumont Hospital.
New research has found that elevated levels of a marker in the blood, von Willebrand factor propeptide, is linked to more severe disease and poorer outcomes for hospitalised patients with COVID-19. The findings may help to stratify those at high risk of severe thrombotic and respiratory complications. The study, led by researchers from RCSI, is published in the current edition of the British Journal of Haematology Professor James O’Donnell, Director of the Irish Centre for Vascular Biology (ICVB), RCSI and Consultant Haematologist in the National Coagulation Centre in St James’s Hospital, said: “ The mechanisms through which COVID-19 triggers the formation of these micro-clots has been puzzling doctors; this research helps us to more clearly understand these mechanisms.” Dr Jamie O’ Sullivan, StAR Research Lecturer at the ICVB and co-senior author on the paper, said: “ This study provides further insight into sustained damage to the cells lining the blood vessels in patients with severe COVID-19 and how this may contribute to thrombotic complications.”
MAKING A DIFFERENCE FOR OTHERS IN AN INCREDIBLY SPECIAL WAY

In a conversation recently with Aíne Gibbons, she asked me to share my thoughts as to why I made enduring provisions for RCSI in my will –hopefully to be activated only in the far future! It is bittersweet for me to write about my legacy intentions for the Alumni Magazine – I would much rather explain my reasoning to you in person.
My a ection for the College, for Ireland, for my classmates and many friends, is certainly the genesis. As I age, I care less how maudlin that might sound. Much of what I have achieved throughout my career is in substantial part due to the gamble that the College took on a character like me years ago.
e person I am today (for better or worse) was much moulded by my years and experiences in Dublin.
As we all know, there are a million good causes – I have chaired foundations, completed mission trips, swung a hammer, and still there is more pain than there are resources in this world. Why do I support RCSI rather than some other institution or cause? I do so not for some print or plaster immortality –Herodotus pointed out that none of us are known for who we really were past three generations… there are much more practical reasons – the desire to do something e ective, to make an impact on future generations of students, and above all the performance record of the College.
e College bears the imprint of O’Flanagan, MacGowan, O’Malley, Horgan, Kelly, and so many others. e culture and infrastructure they have built has demonstrably expanded and improved healthcare in Ireland and across the world. Consistency, leadership, and vision – that is a pretty good performance record. Along with my fellow alumni, I am part of the legacy that these individuals have created and that is something to be very proud of. I stand in the shadow of great women and men, but by including RCSI in my will I hope to also stand on their shoulders and support the College’s future ambitions.
Sometimes it is easier to establish credibility with some distance over time and in geography. From forty years and four thousand miles away, RCSI has established that credibility with me!
I hope you will give thought to joining me in considering RCSI in your legacy plans.
Dr Richard Nora, Class of 1980
If you would like further information on legacy giving please call Aíne Gibbons, Director of Development on +353 (1) 402 5189, or email ainegibbons@rcsi.ie
With an understanding of the online zeitgeist, RCSI alumni and faculty are building quite a following…
DR EOIN KELLEHER MEDICINE, 2014
@EOINKELLEHERCARTOONS
Theme: Cartoons 2,408 followers
Some RCSI alumni inject humour into their followers’ and friends’ newsfeeds. Dr Eoin Kelleher has a popular Instagram page featuring droll comics, at the moment mostly on the theme of the international vaccination race, or dubious developments in pandemic news. A master of the medical pun, his cartoons offer followers a much-needed laugh.

DR ADRI-ANNA ALOIA
MEDICINE, BAHRAIN, 2019
@FOUNDATIONOFIMG
Theme: Professional advice 503 followers
The Foundation of IMG page, founded by Dr Adri-Anna Aloia, is an extension of the non-profit organisation by the same name that offers personal, career and financial support to medical graduates around the world. The page prompts followers to consider their basic needs: “Have you made sure you are sleeping enough hours this week?” or “Have you set a study schedule?” Followers also have access to stories from fellow member graduates, and online events such as career talks.
DR VEER PUSHPAK GUPTA
MEDICINE, 2012
@DR_VEERPGUPTA
Theme: News 4,902 followers
RCSI alumnus, NHS physician Dr Veer Pushpak Gupta is an informative and interactive presence on social media, and features regularly on global news programmes on radio and television. His Instagram page links to a list of articles and video interviews that demonstrate his responsiveness to the topics of the day including, of course, the pandemic. From NDTV India to Radio Canada, Dr Gupta’s professional updates transcend global boundaries.


DR ADANNA STEINACKER
MEDICINE, 2015
@ADANNADAVID_FAM
Theme: Family Lifestyle 327K subscribers
Dr Adanna Steinacker is a doctor, entrepreneur and public speaker. Her YouTube channel which she runs with her German tech consultant husband David Steinacker has over 327,000 subscribers. She posts videos that reveal their approach to modern family challenges, and how they commemorate milestones. Videos of their three wedding celebrations – one a traditional Nigerian gathering, one a German civil wedding, and one a typical Irish church ceremonyamassed over 2.2m views.

DR JT O’SHEA
MEDICINE, 2004
@DRFITNESSMUM
Theme: Fitness 484 followers
Healthy living and fitness is a goal for all RCSI alumni, but achieving it can prove a challenge for busy healthcare professionals. Dr Juliah Tbarani O’Shea, founder of the Likha Aesthetic Clinic, motivates followers to do their best with limited time, sharing her approach to fitness on Instagram with videos and posts of her at-home workouts.

Theme: Leadership 4,197 followers While in-person lectures, talks and conferences have been postponed in the past year, RCSI leaders with a gift for public speaking can still inspire online. Professor Mark Shrime, O’Brien Chair of Global Surgery at RCSI, is followed by 4,197 Twitter users for his sharp insightful messages on current topics relevant to his audience. Key to amassing such a following is the ability to present a view on an urgent topic quickly, clearly, wittily and with personality. Professor Shrime demonstrates a great understanding of the platform’s rapidly changing tides.

Theme: Health 4,527 followers
Best known to viewers of RTE’s Operation Transformation series, where she led contestants to better health, Dr Sumi Dunne is a GP, and a lecturer in clinical medicine at RCSI. The Co Laois-based mother of four’s Twitter account reflects her busy life in frontline general practice while homeschooling, and caring for her elderly father. She is always on-topic; subjects such as the COVID-19 catastrophe in India, healthcare racism and women’s health all feature.

@SUSANMSMITH
Theme: COVID-19 research 3,194 followers Research professionals who tweet frequently do their followers a service, providing quick, succinct and reliable updates. GP and Professor of Primary Care Medicine at Mercer’s Medical Centre, Professor Smith’s Twitter account is a source for information relating to current research on the COVID-19 pandemic, and its consequences for society.

@DR.PHOTO2
Theme: Photography 102 followers Best known for his work on the condition named after him, Habba Syndrome, gastroenterologist Dr Saad F Habba serves as President of the Gastro-Surgi Center of New Jersey, has a private practice in Summit, New Jersey and is an attending at Overlook Medical Center. His Instagram, @dr.photo2, showcases his love of photography with his own elegant and emotive shots, often in black and white.

@TWISTEDDOODLES
Theme: Cartoons 88K followers
Dr Maria Boyle’s innovative illustration page is full of stylised sketch-and-caption cleverness. Often her posts seem wide-eyed and whimsical –traits not usually associated with a scientific mind – and are always witty. As a cartoonist for the New Scientist, Dr Boyle keeps her finger firmly on the global pulse with sketches reflecting the mundanity of lockdown life and its frustrations, others offer insight into the life of a scientist. Her huge following reflects her talent to draw in audiences with lighthearted honesty.

@IMG.MARVELS
Theme: Careers advice 2,046 followers YouTube has proved a popular platform for medical graduates. IMG.Marvels was cofounded by 2019 alumna Dr Malvika Bhatia and features medical graduates who have secured jobs in the UK. Videos feature recent graduates who discuss their own routes to securing their first job after graduation, and give valuable tips to fellow alumni on the job hunt.

is year RCSI inaugurated the Cameron Award to commemorate the centenary of the death of the leading public health doctor in Victorian Dublin and former president of RCSI, Sir Charles A Cameron (1830-1921). Mary O’Doherty, Librarian, Heritage Collections RCSI, introduces this man of Science, Letters and the Arts
RCSI University of Medicine and Health Sciences is commemorating Sir Charles Alexander Cameron, the centenary of whose death occurred on 27 February 2021. An international gure in Public Health, he held numerous o ces in academic institutions and in RCSI.
Charles Alexander Cameron was born in Dublin on 16 July 1830, son of Ewen Cameron and Bridget Smith. Ewen Cameron, born in Inverness in 1787, a captain in the 42nd Regiment, retired aged 28 in 1815 due to injury. A mention by Charles “My mother, Belinda Smith, was born in the County of Cavan in the year 1793 and died in 1867” prompted RCSI to commission research by the genealogical company Eneclann, who found records of Charles’ birth, baptism and of his parents’ marriage. Bridget Smith was from Virginia, Co Cavan, but the fact that Charles renamed her Belinda may not have been a hankering for gentility. Records traced by Eneclann show that Charles was born before his parents married: being born out of wedlock would have had serious implications for his future. e Cameron family, Charles and an older brother and sister, lived in various locations in Dublin in the 1830s. Due to his father Ewen’s poor health, the family moved to Guernsey in the Channel Islands in 1844. Ewen died soon a erwards and the family could no longer a ord to establish Charles in a military life. Instead he took an apprenticeship with an apothecary.
CHEMIST FIRST AND FOREMOST

in geology from the Director of the Geological Survey Ireland. Already the family breadwinner at 19, Cameron deliberated on the most congenial way of making an income. “A large proportion of my income has been derived from my knowledge of medicine, hygiene, chemistry and physics; a much smaller proportion from journalistic and editorial work and lecturing on popular subjects.”
LECTURESHIPS IN CHEMISTRY
Cameron delivered his opening lecture to the Dublin Chemical Society on 13 December 1852 in its lecture room in Dublin’s Capel Street. Accounts of Cameron’s lectures appeared in the newspapers, and made him known. His rst appointment in a medical school was a result of those reports. Dr Edward Hamilton, whom he never met, wrote to Cameron in 1856, o ering him the Professorship of Chemistry and Natural Philosophy in the Dublin School of Medicine, which he accepted. In the following year Cameron was similarly o ered the Lectureship in Chemistry in the Original School of Medicine. us began Cameron’s lifelong association with many of the rival private medical schools in Dublin. He wrote a valuable account of them 30 years later.
Charles began his working life in 1846 aged 16, in the laboratory of Bewley & Evans, Apothecaries & Chemists, 3-4 Sackville Street Lower, Dublin. Here he acquired a good knowledge of pharmaceutical chemistry, which he subsequently found very useful. He read books on chemistry, physics, geology and medicine. He attended lectures at the Royal Dublin Society and received instruction
Cameron went to Germany in 1854 where he graduated with the degrees PhD and MD. His encounter with Baron von Liebig proved highly signi cant throughout Cameron’s career. Von Liebig, known as the ‘Father of Fertilisers’, “made signi cant contributions to the analysis of organic compounds, the organisation of laboratory-based chemistry education, and the application of chemistry to biology (biochemistry) and agriculture.” Cameron states that von Liebig’s writings inspired his love for science. Aspects of chemistry established by von Liebig became perennial topics of Cameron’s research: the application of chemistry to agriculture; the analysis of manures; the fertilising value of
the sewage of Dublin. Cameron published his own seven-page bibliography. Von Liebig’s in uence can be seen in the titles of his publications and also in that Chemico-Agriculture is one of the six headings into which he divides his original papers. He lists 17 of his papers in this section. ere are 18 papers listed under Chemistry and 15 under Hygiene.
e Corporation of Dublin appointed Cameron Public Analyst in 1862. In this role he examined all that a ected the health of the citizens: water, soil, milk, meat, food, alcohol and drugs. According to his ndings, he could proceed, in keeping with the Law. e adulteration of food and drink was widespread in the 19th century, causing illness and death. He records progress: “… e Anti-adulteration Act of 1872 worked in Dublin for ten years, and was the means of putting an end to the practice of adulterating many of the articles of food in common use. A very large number of convictions for the sale of adulterated articles were obtained in Dublin. At rst it was found that bread, our, tea, co ee, mustard, sweetmeats, and milk were largely adulterated. Now, with the exception of milk, it would be di cult to nd an adulterated article in Dublin.”
Cameron investigated the spread of human and animal diseases from milk and meat, and his work contributed to the debate on germs and disease. Filthy slaughterhouses were closed and replaced by a new abattoir. He analysed samples taken from wells, pumps, and rivers from all over Ireland to prove that the water people used was the source of various infectious diseases such as cholera and typhoid fever. “ e poison in the wells was derived from the foul drainage of the soil, tainted with the matters thrown out from the bodies of the sick. One of the most active agents in spreading epidemic and endemic diseases amongst crowded centres of population was impure potable water.” Cameron reported on malpractice in “ e quality of the drugs in, and the system of supplying them to, workhouse hospitals and dispensaries”, 1880.

On 16 October 1862, in St Mary’s Church of Ireland in Donnybrook, Dr Charles A Cameron married Lucie Frances McNamara, the only daughter of a Dublin solicitor. Charles and Lucie had eight children. On 28 November 1883, Lucie, his beloved wife and companion died of heart disease at the very young age of 45.At the age of 53, Charles Cameron was le a widower with seven children ranging in age from 16 years to a one year old. (William, their second son, died from scarlet fever in June 1875 aged seven). Lucie’s death deeply a ected Charles. His eldest son, Charles John, or Charlie as he was known, served in the army with the Enniskillen Fusiliers, the 3rd Battalion of the Royal Dublin Fusiliers and the 3rd Battalion of the Cameron Highlanders. He le for South Africa as captain in the 4th Battalion of the Dublin Fusiliers in March 1902. Charlie died in a boating accident on the river Shannon on 3 January 1913, aged 47.
Edwin Douglas, third son, worked in the Corporation laboratories as his father’s assistant.
A sportsman, he was Captain of Bective Rangers football club in Donnybrook. He contracted pulmonary tuberculosis and died on 7 April 1895, aged 27.
Lucie, elder daughter, born 1869, married John Denison Gerrard (Denny). Denny was appointed Resident Magistrate for Co Mayo where they lived.
Helena Margaret, younger daughter, born 1871, married Rupert Stanley, Professor of Electrical Engineering in Belfast Technical Institution, in 1903. ey lived in Belfast, and had three sons, Rupert, Vivian and Mervyn, who brought Sir Charles great happiness.
In 1874, Professor Cameron, who had held the Chair of Public Health at RCSI since 1868, was appointed Medical Officer of Health for Dublin.
Being a Chemist, Sanitarian, Public Analyst, and Medical Officer of Health generated synergies, which he ably tapped. He understood the connection between dirt and disease. Campaigns to rid Dublin of its infested slums and to provide houses with water and sanitation brought measureable benefit to public health. Cameron received a knighthood for this. Measures adopted by Cameron to counteract the great flu pandemic of 1918-19 were strikingly similar to the measures in the current pandemic.
Ernest Stuart, fourth son, born 1873, was also a Chemical Analyst with his father in Dublin Corporation. Devoted to music, he studied in Paris, and gave singing lessons in the family home on Raglan Road. He died in 1949, aged 76.
Mervyn Wing eld, h son, born 1875, contracted phthisis. A er several trips to warmer climates, he died in 1898.

Ewen Henry, sixth and youngest son, born 1882, was a tea planter in Ceylon. He joined the 3rd Battalion of the Royal Dublin Fusiliers as a lieutenant. Troubled by losses in the War, Ewen shot himself on the train between Greystones and Newcastle on 27 August 1915: “ is terrible blow will leave the little of life le to me joyless.” Sir Charles’ diary, 27 August 1915.
Sir Charles was most sociable. He was a member of clubs and societies in Dublin and London. An inveterate opera and theatre-goer he was friend and correspondent of leading actors and singers. He loved to host parties and to dine out, and did so at every opportunity as his diaries and memoirs show. He believed that dining out in company made for a longer life, which as a nonagenarian he proved. Initiated into the Society of Masons in 1858, he took Office in Grand Lodge, the Order’s governing body, in 1870, becoming Deputy Grand Master in 1911. In congenial company it was as if he could temporarily forget the many loved ones he lost.
In November 1919, at the age of 89, Sir Charles resigned from the RCSI Chairs of Chemistry and of Public Health due to ill-health. e President and Council entertained him to dinner on Saturday 2nd November. Sir Charles had been connected with the College and Schools for over 60 years.

Sir Charles Cameron died on 27 February 1921. His funeral took place on 2 March 1921 in St Bartholomew’s Church, Clyde Road and he was laid to rest in Mount Jerome cemetery. Sir William Ireland de Courcy Wheeler and other RCSI Members of Council followed the funeral procession preceded by the College mace bearer.
“I think that his heart was greatly bound up in the old College,” wrote Ernest, only survivor of Sir Charles’ six sons, in a letter to the Registrar a er his father’s death.
Any consideration of Victorian Dublin, its people and development, inevitably involves Sir Charles Cameron. e range of his activities as Medical O cer of Health, Public Analyst and Sanitarian led to his widespread in uence throughout the city. His specialist knowledge and his relentless drive to improve the City and its citizens’ lives are evident to this day. From slum clearance to the building of new houses, from lth-ridden yards to homes with toilets and
THE RANGE OF HIS ACTIVITIES ... LED TO HIS WIDESPREAD INFLUENCE.
running water, cleanliness reduced disease. ese developments can be traced in the landscape and are recorded in the annual reports on public health.
Sir Charles also le us his writings, both professional and personal. e data he recorded illuminate aspects of life, death, disease and its remedy. e development and his contribution to the emerging specialty of Public Health are all there.
He is immortalised in James Joyce’s Ulysses: e annual dinner, you know. Boiled shirt a air. e lord mayor was there, Val Dillon it was, and Sir Charles Cameron and Dan Dawson spoke and there was music.
RCSI inaugurated the Cameron Award for Population Health to honour Sir Charles A Cameron on the centenary of his death. e Award, “Bunsen’s Flame” by Jason Ellis, brings us back to Cameron’s pioneering work as a chemist. His laboratory experiments, many original, produced irrefutable evidence of the causes of death and disease. Chemistry remains the key to all Cameron’s evidence-based research whose application improved public health. Robert Bunsen (1811-1899), contemporary with Cameron (18301921), was a chemist of far-reaching importance whose discoveries form the basis of many modern scienti c developments. at Sir Charles continues to be celebrated 100 years since his death, is yet another measure of the man. ■ e Cameron archive, which contains the information and illustrations in this piece, is in the RCSI Heritage Collections and available to researchers at www.RCSI.com/Cameron.
The inaugural Sir Charles A Cameron Award for Population Health was presented to Dr Mike Ryan at a virtual ceremony hosted by RCSI

Dr Mike Ryan, Executive Director of the World Health Organization (WHO) Health Emergencies Programme, has been awarded the inaugural Sir Charles A Cameron Award for Population Health Advocacy by RCSI, in recognition of his global leadership during the COVID-19 pandemic.
Dr Ryan currently leads the WHO team responsible for the international response to COVID-19 and he has been at the forefront of managing acute risks to global health for 25 years. He rst joined WHO in 1996, with the newly established unit to respond to emerging and epidemic disease threats.

Dr Ryan has been a leader in the ght against COVID-19 and, emulating Charles Cameron, has been a powerful advocate for a “one global family” response to the pandemic and equity in the distribution of vaccines.
Accepting the award, Dr Ryan said: “ e link between Sir Charles Cameron and the pandemic we are living through is entirely relevant. He shows us why it is so important to stand up as advocates for the underpinning determinants of health. is award is a huge personal honour for me. I accept it on behalf of Irish people working at home and abroad in the spirit of Cameron.”
e annual
Distinguished
Graduate Award 2020 was presented to Professor Moira O’Brien
Every year the President and Committee of the Association of Medical & Dental Graduates at RCSI invite nominations for the Distinguished Graduate Award. is award, established in 1988, honours a graduate who has made an outstanding contribution to the improvement of health care through education, research, humanitarian aid or patient care.
e 2020 recipient is Professor Moira O’Brien (Medicine, 1956). Professor O’Brien was presented with the Distinguished Graduate Award by President of the Association, Dr Antonia Lehane, at a virtual ceremony. In her citation, Dr Mary Archer (Medicine, 1977) praised Professor O’Brien, stating that her “undergraduate successes and interests were an indication of the illustrious postgraduate pathway” Professor O’Brien would follow.
Professor Moira O’Brien was born in Malaysia and quali ed in Medicine from RCSI Dublin, in 1956. She sat the entrance exam at the age of 15, was awarded a scholarship, and commenced her studies just a er her 16th birthday. is remarkable achievement was in some ways attributable, according to Professor O’Brien, to the challenges she had already faced in her young life. Her parents, both medics, were based in Kuantan. Her father worked with the British Colonial Medical Services. He was the Chief Medical O cer at the hospital in Kuantan, on the east coast, before the war. Moira, at four years of age, was sent to boarding school with her older sister since there were no international schools in the area. When the Japanese landed, her father fetched the girls from their boarding school and she and her mother, who was ve months pregnant, and siblings (three sisters and a brother) le Malaysia, getting the last safe passage out of Singapore to Australia (“subsequent sailings were all bombed,” she recalls). ey were e ectively refugees, as they could only bring the clothes they were wearing. Her father remained in Singapore, as
he felt obligated to assist those le behind. He was captured by the Japanese and, while a prisoner, was assigned to be the doctor in charge of the civilian camp. His faith (he had become a Catholic so he could marry Moira’s mother) helped him to survive and for three and a half years his family in Australia did not know if he was alive.
Friends of her parents helped them to get settled in Sydney, and the Loreto nuns schooled the siblings free of charge. When Moira was twelve, the family returned to Ireland. As a student at RCSI, she excelled academically, and her many awards included First Place and Medal in Topographical Anatomy and Second Place in Systemic Anatomy. She was also awarded First Place and a Medal in Obstetrics and Gynaecology (1956) and remarkably, she was appointed as a demonstrator in anatomy and physiology, while still a student.
With her clear understanding of physiology and in-depth knowledge of anatomy, it was perhaps inevitable that she would blaze the trail for Sports Medicine, both in Ireland and abroad.
A er graduation, Professor O'Brien worked in Dublin, Manchester, and She eld, before returning to Dublin in 1959 to take up a position as a lecturer and then Reader in Anatomy at RCSI. Those fortunate enough to come through card-signings in her time were forever grateful, albeit in dread at the time, as she has always stated that “Medicine is a licence to kill, which is why it is so important that everyone knows the basics of Anatomy”.
In 1980 she founded the Irish Sports Medicine Association. She was Medical O cer for the Irish Olympic teams in 1980 (Moscow), 1984 (Los Angeles) and 1988 (Seoul). Significantly, she a liated Ireland to the northwest chapter of FIMS (Federation International Medicine Sportive) and was extremely active on FIMS Executive from 1981–1993.
In 1984, she transferred her skills to Trinity College when appointed Professor of Anatomy (the rst female appointment to the medical faculty ). In 1984 she set up a Human Performance Laboratory to monitor the tness, performance, and progress of elite athletes. In 1990, Professor O’Brien established a Masters in Sports Medicine (the rst in Ireland and the UK). Her research brought to light problems with bone health, which prompted her to set up the Irish Osteoporosis Society in 1996. She set up the rst Osteoporosis clinic in Ireland.
Professor O’Brien has had many accolades bestowed upon her, among them, Honorary Fellow of European College of Sports Science;
Professor Moira O’Brien, LRCPSI, MRCPI, LM, MA, FRCPI, FTCD, FFSEM, FFSEM (UK), FECSS.


Hon. Dip. Sp. Med., RCS Edinburgh; The 7th Annual Samuel Haughton Medal; Senior Fellow FSEM UK; Hon. Fellow FSEM UK; Roger Bannister Lifetime Achievement Award; FSEM Outstanding Contribution to Sports and Exercise Medicine; Lifetime Achievement Award in 2021 Irish Healthcare Awards. She is Emeritus Professor of Anatomy at Trinity College Dublin.
In 2003, Professor Moira O’Brien was a founder Fellow of the Faculty of Sports and Exercise Medicine of RCSI and RCPI. Her commitment to the Faculty is second to none, serving on Council, organising committees for annual conferences, assessing research papers and judging posters and clinical presentations.
In 2018, her former student, Dr William Blakemore (Class of 1979), established the Moira O’Brien Sport Scholarship in her name, which she awards annually. Professor O’Brien is very proud of this tribute from a past pupil. “I was so lucky to be able to teach, to try to bring out the best in students and to do my clinical work and research too.” A principled leader, she believes in hard work, standing up for what is right, and helping others. “ e patient has to come rst.” She continues to receive letters from former students and follows their careers. She remains very active, working as a consultant in the A dea clinic in Dundrum, Dublin, and promoting awareness of osteoporosis, highlighting its risks, promoting screening and the treatment of it.
e Association is privileged to have Professor O’Brien as a member and was honoured to o er her the Distinguished Graduate Award for 2020 and delighted at her acceptance. We thank her for her immeasurable, enriching contributions to the medical profession. ■
e “local” of choice for students, professors, consultants and faculty, e Swan has earned its place as an extension of the RCSI campus.
Antonia Hart describes the famous pub’s history, and its plans for the future
There’s been a licensed premises on the corner of York Street and Aungier Street for the 350 years since the streets were laid out, and for many years before that. It’s been called e Sign of the Swan, e White Swan, and now e Swan, a er the culverted river which ows north through Rathmines, under Ranelagh Gardens, and on to the Aviva Stadium, the Dodder and the open air. e Swan we know today is largely Victorian. While Victorian pubs feel quintessentially Dublin, only a precious few remain. As well as e Swan, authentic city stalwarts are e Palace, Toners, Doheny & Nesbitt’s, Grogan’s, Slattery’s, Bowe’s, Kehoe’s, Ryan’s, and e Long Hall. Every pub has its character. e Swan is a Victorian pub, a Dublin pub, a rugby pub, and, inevitably, given its location, a Surgeons pub. RCSI has always peopled the place, and not just on memorable big nights out. e Swan has always been an everyday meeting-place for students, professors, demonstrators, consultants, and administrative sta . It even earned the

The building dates back to the 1800s, the interior to 1897. The facade is pockmarked with bullet holes from the Civil War.
nickname LT4, an honorary lecture theatre and extension of the RCSI campus, which is certainly how many will remember it. Current owner Ronan Lynch says the presence of the student body, in particular, brought a very particular combination of vibrancy and intimacy to the pub. ere are standout memories of the Fridays when results were published, of pub crawls, of boat races, of fancydress races around Stephen’s Green, and endless more workaday memories too, of clocking-o pints, co ees for the exhausted, sandwiches bolted at lunchtime, and a table for two, in the corner.
The connection to RCSI is something Lynch values hugely. e student body changes year a er year, but tends to feature bright, driven people who work hard, come under pressure, and need space to let o steam over their degree years, years in which they also mature and develop. e zzing energy of the students seems to have been always manageable, although naturally Lynch has instigated the occasional quiet chat with an overenthusiastic reveller, just as he saw his father do. But Lynch’s guiding principle actually came from his grandmother, who told him to
Seán

run his pub as if he were having a party in his front room. It’s been a successful approach, as thousands of alumni, not just in Ireland, but around the world, know. e Swan easily topped a recent Instagram poll of RCSI alumni, to be voted the best night out in Dublin.
Lynch’s grandmother wasn’t the rst strong woman in e Swan’s history. Anne Sleator ran it in the latter half of the 19th century, also operating it for many years as a hotel. Before the century turned, the premises, which by now included 56, 57 and 58 York Street, was taken over by the O’Reilly brothers, wine and spirit merchants who also had premises at 11 North Wall Quay.
omas O’Reilly re tted the bar in 1897, and did it so beautifully that much of it remains today, including the original mahogany ttings and bar with traditional granite countertop, there to keep your drink deliciously cool. Dark wood is o set by the pale oor of footworn mosaic, including a swan on the threshold. Light re ects from the bevelled glazing of the original cashier’s kiosk, and the polished brass of the Victorian beer pumps.
IT HAS WITNESSED ARMED REBELLION AND CIVIL WAR.
O’Reilly’s revamped Swan was always busy. It was a good source of local employment, too, needing at least 20 sta , between porters on every door, the cashier, people to wash every glass and bottle by hand, and hand-bottle or hand-pump beer. Whiskey and beer came in casks, all bottled and labelled on site. Power’s was traditionally drunk by Catholics, and Jameson by Protestants. In a more ecumenical spirit, both are now owned by one company. On top of all this work, omas O’Reilly kept a white bull terrier, and
exhibited birds. He regularly sold Yorkshire canaries: “winners at several shows; best strain procurable”, though occasionally “cheap to clear”. e chat over the cool granite counter must have covered birds, dogs, and other animals, and surely included some predictable Dublin digs about the owner of e Swan having a canary. But ill-health meant that in June 1909, O’Reilly sold all his birds and cages, and in July he sold e Swan itself, to John Maher of Kingstown, who printed spanking new stationery headed ‘John Maher, Select Family Grocer, Tea & Wine Importer and Bonder’, with a sketch of the pub.
It was Maher’s Swan which Volunteers occupied during the Rising, and where anti-Treaty forces holed up during the Civil War. e façade still bears the scars of gun re, and John Maher’s claim for compensation a er 1916 detailed interior damage too, to the porch door, a glass case in the shop, and mahogany shop ttings. e plate-glass mirror in the private bar was also shattered by bullets.
Ronan Lynch’s family became involved in 1937. Ronan’s grandfather, John Lynch, had been running a grocery store in America, but got into “a tangle” with an Italian man who had tried to rob him. John Lynch had to hotfoot it out of New York, and made for Dublin and a job at Sheehan’s of Chatham Street (another Dublin pub that has been owned by three generations of one family), until he bought e Swan in 1937. He brought his family up on the upper oors, until his death in 1979. e pub passed to his son, the legendary rugby player Seán Lynch, and during his ownership e Swan became established as a rugby pub through and through. Seán played on the only Lions team ever to win a series against the All Blacks, and ran the place concurrently with his international rugby career. His framed jerseys, a bronze bust and other memorabilia are now on display in the pub.

e Swan has served customers for centuries. It served them when the streets of the capital were unpaved, when water was so universally undrinkable that Dubliners quenched their thirst with beer. It has witnessed armed rebellion and civil war. Now, a er a historic and di cult enforced closure, Lynch will relish reopening. e elegant glazed Victorian partitions along the bar could have been designed for social distancing, and in some sense, perhaps, they were. ere are changes coming. Lynch is preparing beautiful hotel rooms on the upper oors, so that, for the rst time in almost a hundred years, e Swan will once again o er accommodation. Its city centre rooms, with their original replaces, intricate plasterwork, and shutters on their pretty sash windows, are going to be just the ticket for anyone looking to reconnect with Dublin. ■
At RCSI, we love to hear news about your career achievements and information about you and your life a er University. Find out what some of your classmates have been doing
■ DR KRISTL TOMLIN (MEDICINE, 2010) In ten years since graduation, Dr Kristl Tomlin completed her fellowship in Paediatric and Adolescent Gynaecology (PAG) before joining the University of South Carolina. Most recently, she has been promoted to the Department Head in Pediatric and Adolescent Gynaecology at the University of South Carolina, where she also holds the title of Clinical Assistant Professor in the Departments of Obs/Gyn and Pediatrics.
■ MS MUMI HOSSAIN (PHYSIOTHERAPY, 2011)
Congratulations to Mumi Hossain and her new husband Ruairi, who got married during lockdown (with a smaller than planned guest list due to restrictions) and had a wonderful day of celebration.
■ DR ALAA MUSHTAHA (INSTITUTE OF LEADERSHIP, 2012)
Dr Alaa Mushtaha recently began his career in academia, at the University of Balamand, Dubai (UoBD) as Assistant Professor of Healthcare Management. Dr Mushtaha has many years’ experience in multi-national commercial companies in the healthcare area and is excited to share his experience with students.
■ MS VICKI O’REILLY (INSTITUTE OF LEADERSHIP, 2016)
Congratulations to Vicki O’Reilly, who in early 2021 was promoted to the Head of Quality, Compliance and Regulatory A airs for Sisk Healthcare in Ireland.
■ DR EMAN AL-FARAJ (INSTITUTE OF LEADERSHIP, 2016)
Dr Eman Al-Faraj was delighted to be able to present her project as part of the International Forum on Quality and Safety in Healthcare in Glasgow in March 2019. She was also recognised by the BMJ for her work in peer reviewing.
■ DR HUSSAIN KHIMJI (MEDICINE, 2017) Congratulations to Dr Hussain Khimji, who was recently awarded the 2020/21 RS Grainger Award by the University of Calgary, whilst in the Family Medicine Residency Program. e award recognises good academic standing, solid clinical performance as well as compassion and leadership in practice amongst peers.
■ DR STEPHEN KEELAN (MEDICINE, 2018) Congratulations to Dr Stephen Keelan, who has recently been awarded an IRC grant as part of the Government of Ireland Postgraduate Scholarship Programme. e grant will fund his PhD in brain metastatic breast cancer under the supervision of Professors Hill and Young from RCSI Department of Surgery.







ORLAGH FINN (NURSING MANAGEMENT, 2017; MSC 2019)
CHIEF NURSE OFFICER, IRISH PRISON SERVICE
“In recent times, we have been saturated with national COVID-19 strategy and policies, mainly focusing on challenges in the HSE, nursing homes and wider society. But what if your setting was a prison? What if adhering to national policy on COVID-19 restrictions meant further restrictions of liberties for a population already deprived of their actual liberty – albeit in accordance with the law?
ENDA KELLY, National Nurse Manager of the Irish Prison Service (IPS) in conjunction with the Chief Nurse Officers (CNOs) and the National Infection Control Team assess, plan and implement national policy in a fair and humane manner to the prisoners in their care. CNO
URSULA NORTON and all IPS CNOs have guided their respective prison teams in preparedness measures from the beginning of the pandemic.
Nurse Officer (NO) CECELIA CONWAY, among others, led donningand-doffing training for nurses and discipline staff in a West Dublin prison, ensuring that all IPS staff had a standard for PPE usage. This was replicated in every prison.
All prisons established isolation units and nursing staff ensured that all infection control measures were introduced and implemented. Targeted swabbing was identified as the cornerstone in detection of COVID-19 in newly committed prisoners. This strategy was staffintensive and laborious but it was a crucial tool in the IPS early detection strategy. SHANE CLAFFEY was integral in the swabbing “train the trainer” role to enable the wider team to assist in the early detection of COVID-19. Contact tracing fed into early isolation and prevention of the spread of COVID-19, a vital component of the successful strategies implemented by the IPS.
SIOBHAN COTTER is a Lead Nurse on the Mobile Vaccination Team who will administer the COVID-19 vaccinations in adherence to the Government priority groupings. Meanwhile NO COLETTE FARRELL continues smoking-cessation education with prisoners, an important initiative given the respiratory complications that could present in the smoking population. NOs JAY ROSALIM and SALLY ABAGHA, among others, continue planning for the roll-out of prisoner vaccinations.
Managing prisoners’ mental health is a challenge throughout this pandemic. NO DENNIS BOTHA , among many others across the
■ DR ALHASAN ALHEBSHI (MEDICINE, 2018)
Dr Alhasan Alhebshi’s application to general surgery in one of Saudi Arabia’s largest hospitals in Jeddah has been accepted. He has also been working on three research projects, and he got married, all within the last year.
■ DR KATIE DUNLEAVY (MEDICINE, 2018)
Congratulations to Dr Katie Dunleavy, who will begin her fellowship in Gastroenterology with the Mayo Clinic in Minnesota.

prison service, has made concerted efforts to increase observation and vigilance towards vulnerable prisoners and ensure that they maintain contact with mental health services during this stressful time. I lead as COVID-19 vaccination roll-out Project Manager, linking in with the respective disciplines to ensure IT compliance, staff training and preparedness in administrative processes in line with the HSE. CNO ROSIE GATELY and the CPR instructors ensure mandatory training is maintained throughout the pandemic. Each CNO leads from the front in preparedness measures, detecting any threat of COVID-19 with proven systems to their credit, isolating positive cases and evaluating their practice regularly. While the pandemic has been challenging, all prison staff overcame every obstacle and remain resilient, pragmatic and hopeful.”
All nurses mentioned in this article are RCSI alumni.


■ MR CHRISTIAN JABER (INSTITUTE OF LEADERSHIP, 2007)
Congratulations to Christian Jaber who in late 2019 married Marie Murray. ey are delighted to announce they are now expecting a little bundle of joy to add to the family.
■ DR PAUL DHILLON (MEDICINE, 2009) Congratulations to Dr Paul Dhillon and his wife Sarah who welcomed a new member of the Dhillon family. Ruairí joins Darragh, Sarah and Paul to complete the family.
■ DR MOHAMMED AL MALIKI (INSTITUTE OF LEADERSHIP, 2009)
Congratulations to Dr Al Maliki, who has had a distinguished career as a Paediatric Specialist for the past 20 years and has now established his own private healthcare consultancy company, called Right Path Consultancy, in Bahrain. With learnings from his studies at RCSI, the consultancy will use technology at its heart to improve the quality and safety of patient care.
■ PROFESSOR MURIEL SODDEN (MEDICINE, 1982) Professor Muriel Sodden recently partnered with a jeweller in Townsville, Queensland, Australia to produce a beautiful ring-holding locket, called Fonya, which keeps your rings safe on your person while at work.
■ PROFESSOR JOHN FENTON (MEDICINE, 1984) Congratulations to Professor John Fenton,who as President of the board of European Union of Medical Specialists in Otorhinolaryngology (UEMS-ORL), has successfully published and had their training standards and logbook recognised by EU Medical Associations for the rst time.
■ DR MIKE GAYA (MEDICINE, 1970) In collaboration with the Lions Club of Quatre Bornes (his hometown), Mike has been involved in introducing vision screening to primary school children, coordinating voluntary donations to help fund eye tests and glasses.
■ PROFESSOR AUBREY MORRISON (MEDICINE, 1970) Congratulations to Professor Aubrey Morrison, MBBS, MACP, FASN, who was the recipient of the 2020 Barnes-Jewish Hospital Missouri medical sta association Lifetime Achievement Award. Professor Morrison recently retired from the Nephrology department at BJM Hospital a er 45 years of distinguished service with the hospital.
■ DR ROLF KIRSCHNER (MEDICINE, 1971) Congratulations to Dr Rolf Kirschner, who has been invited to become an Honorary Fellow of the Royal College of Obstetrics and Gynaecology in London, based on his work in the specialty in Norway and across Europe.
■ DR DEVI MODUN (MEDICINE, 1975) Happy retirement to Dr Devi Modun, who is looking forward to relaxing a er 35 years of dedicated medical service in her native Mauritius.
■ DR ROY KWONG (MEDICINE, 1979) Dr Roy Kwong continues to serve his community in Hong Kong, holding on average 100 consultations a day in clinics.








■ DR DAVID BARNES (MEDICINE, 1965)
Living by the mantra “age is just a number”, Dr David Barnes continues to work at the age of 83 and saw it as his privilege to be one of the rst responders during the COVID-19 pandemic in the USA. His third book, COVID-19 for Children and Others, will be published soon and will be dedicated to his good friend and RCSI classmate, Dr Eng Seem Cheam, who sadly passed away in 2021.
DR JOHN BYRNE (MEDICINE, 2000)
“I graduated from RCSI in 2000. After completing my vascular/general surgery training in Ireland, I completed a fellowship in vascular/ endovascular surgery at the University of Toronto. Since 2013, Canada has been home for my wife, three children and I.
Canada has many descendants of the first inhabitants of North America, including First Nations, Inuit and Métis. In modern-day Canada, many of these communities are isolated and have limited access to healthcare and other resources. This makes them particularly vulnerable to COVID-19. Many of these communities are only reachable by boat or plane.
The Canadian government prioritised these vulnerable communities for COVID-19 vaccinations. In Ontario, Operation Remote Immunity was run by the Ontario Air Ambulance Service with the help of local health authorities. Over a 6-8 week period, the goal
■ DR DERMOT REYNOLDS (MEDICINE, 1958)
Now retired and living in Minnesota, Dr Reynolds practiced urology there for many years, having trained at the Mayo Clinic. His last visit to Ireland was three years ago, for a 50-year reunion at RCSI. He has lovely memories including attending births in homes, in the 1950s. “If the mothers weren’t quite ready, we would be asked to stay for a cup of tea!”
was to reach as many people as possible. When the call for volunteers went out, my privileged position as an Irish immigrant made very welcome in Canada made me jump at the opportunity.
I was a member of a team of paramedics, physicians and nurses that joined healthcare workers from the local Weeneebayko Area Health



Authority. We travelled by plane daily and covered two communities on Hudson’s Bay in Northern Ontario, Kashachewan and Attawapiskat. In winter, these communities can be accessed by a treacherous ice-road (not for the faint of heart), but the remainder of the year they are only accessible by plane and boat. These communities are some of the larger First Nations communities with populations of approximately 2,000 people each. They have extremely limited access to healthcare and the other benefits of modern life the rest of us take for granted.
There were significant operational challenges. Unable to stay on the reservations, we flew in daily, bringing everything we needed to set up a mobile vaccination clinic. The vaccines were carefully transported in custom cooler boxes. There were challenges of cold weather (temperatures of -26°C or -15°F) and aborted landings.
With the help of a First Nations liaison and community elders, we managed to spread a positive message and with our small team vaccinated 1,200 people in five days. I am glad I had the opportunity to play a small part in this operation to vaccinate an at-risk community.” ■
Dr John Latham, Class of 1962, has had a long life of adventure. As well as practicing medicine for 40 years and raising a family, he’s tried every mode of travel, from plane to train to automobile – as well as troop ship and motorbike – and is still travelling solo around Australia. Resourcefulness and resilience were values taught at RCSI, he says
r John Latham, (Class of 1962) was born in England and has lived in Naracoorte, 336km south east of Adelaide in South Western Australia, an area associated with sheep and wheat farming, not far from Coonawarra, the famous winegrowing region, for 54 years. His beloved wife Jean died in February 2020; his ve children live in Australia. Now 89 and retired, he looks back on his long and varied medical career, which began in England.
Dr Latham’s father was a pharmacist, and the family lived over the chemist shop in Horwich, a small railway town in Lancashire, until he was four years old, when the family moved to Bolton to live with Dr Latham’s grandmother, a “short, stout lady with rheumaticky knees”, in a large, terraced house.
He was seven when the War started. As his school was commandeered as a gas decontamination centre for two years, lessons took place in the dining room at home, where the schoolteacher taught the three Latham children and other local children. “At ten, I went to the local grammar school,” says Dr Latham. Because he was a pharmacist, a protected occupation, his father was not called up. He joined the police force and as he had a car, which was rare, was attached to a socalled “mobile company”. “He actually went to help out at the blitz in Manchester and the blitz in Liverpool, taking with him as many loaves of bread as he could t in the back of his car, as those a ected wouldn’t have any food.” e idea of medicine as a career, helping and healing
people, was strongly encouraged. “I suspect myself and my brother were brainwashed into that sort of stu from a very young age,” laughs Dr Latham. Indeed, both were destined to become doctors, John in Australia, Harry on Vancouver Island in Canada.
Before that, there was military service. Harry was exempt –a keen gymnast, he had su ered a fall and failed his medical. He applied to She eld University and got in, leapfrogging his older brother John. “I applied for urgent entry to the army so that I could do my service and then apply to medical school.”
Entry to the army involved aptitude tests which determined that Dr Latham would go to the school of radiography at the Royal Herbert Hospital in Woolwich, South East London, in order to become an army radiographer. “A er basic training in Aldershot, for several weeks, I was doing fatigues, working in the kitchen, sweeping snow, lling in time. And then they gave me a railway warrant to go to Woolwich, to begin my radiography course. I arrived there at four o’clock in the a ernoon having le Aldershot at 8.30 in the morning, only to nd that that was the day that the course had started. I had to do fatigues again. Back to shovelling coal!”
Two months later, his medical journey began in earnest. In a way, the delay was serendipitous. “If I’d gone a day earlier, I would have been sent to Hong Kong. During the Korean war, Hong Kong was the place where serious cases were looked a er by the British army. But a er my training, I ended up in Chester, south of Liverpool, only 85 miles from home. I had a motorbike, so I rode back and forth.”


For his interview at Liverpool University, Dr Latham got dressed in a suit and took a bus. e bus deposited him on the wrong side of the river. “ en I got another bus, which took me to the university and the interview where they asked me things like, ‘What newspaper do you read?’ Well, I didn’t get into Liverpool, but I did get into Bristol. So I went to Bristol for three years. e Minister of Health in Britain during the War years had decided that the UK was producing too many doctors. ey tightened up the examinations. I got honours in physiology but failed anatomy, which is not really surprising when you consider the size of Greys Anatomy.”
Dr Latham wasn’t permitted to retake the exam. “A colleague of my father, an alumnus of RCSI, said he would write a letter of introduction to the College, and I was accepted. So in 1956, I took the B&I ferry from Liverpool to Dublin, then a taxi, to the College. I wouldn’t say I was terri ed, but I was fairly stressed! I stayed for two nights at the Salvation Army Hostel, then armed with an address from the o ce at the College, went to a guesthouse in Pembroke Park in Ballsbridge, which was full of students from various countries. I lived there most of the time I was at RCSI.”
Dr Latham had already met his wife Jean while at university in Bristol. “I had some friends who were evangelical Christians and they took me to a relay of a Billy Graham event in London, in central Bristol. at was a life-changing day for me. Two months later I was baptised in a little chapel in Cli on, a suburb of Bristol. I met Jean at an evangelical event. We had one of the longest courtships, about seven years; she stayed in England while I was at RCSI. We got married in 1961. I should have actually graduated in 1961 too – I’d done the exams in September but still had one more to go, so I graduated in 1962.”
Dr Latham enjoyed his time at RCSI and one of his professors stood out as the model of the caring physician. “I was doing my rotation at e Richmond hospital and had the good fortune to be taught by and observe John Lonergan, a neurosurgeon. I was terribly impressed by his humility and the way that he interacted with the patients. It was incredibly impressive to me and even now, the memory brings tears to my eyes. Neurosurgery is so dangerous, so stressful, takes such a long time. It had a huge impact on me.”
A er graduating, Dr Latham worked in England, “doing house jobs, six months in obstetrics, and so on”, at e Bolton District General Hospital. He took his diploma in obstetrics and gynaecology at St George’s in London. “I was very impressed with the college, the coat of arms, marble oors, impressive chandeliers.” A few weeks later he received a letter. “It said, ‘we are pleased to inform you that you passed the exam. When we receive your cheque for 50 guineas, we will be pleased to include you in the passed list’. e exam cost 200 guineas, but you had to pay 50 guineas on top of that to get to get the o cial bit of paper. at was why they had impressive chandeliers.”
A er that, Wolverhampton and three years in general practice. “It was boring. All I could do was write prescriptions and sick certs. During that time I trained in Anaesthetics at Wolverhampton Royal In rmary, with a man who had been in the Royal Navy and who had worked in Australia. At the time –this would have been 1967 – there was a little magazine circulating called e Practitioner, with details of medical postings abroad –South America, South Africa, New Zealand, Australia. I applied to a large practice of 15 doctors in a town in New South Wales and my application was accepted.”



But war – and transport issues – intervened again, this time the Six Day War between Israel and Egypt, and it was not possible to travel to Australia. e trip was delayed. “Our furniture had been packed up and loaded on a steamer, and thanks to the war, was now stuck in the
Finally Dr Latham, his wife Jean and three children (two more would be born in Australia) boarded an old troop ship, and started their long journey by sea. It would take them around the Cape of Good Hope. “On the boat, we met another doctor with his wife and children who were going to Mount Gambier, a hundred kilometres from where I live now. ey were Australian but had been working in England; Phillip was an Orthopedic Surgeon.”
“RCSI HAD AN ENORMOUS IMPACT ON MY CAREER. WE WERE TAUGHT TO FACE THINGS AS THEY AROSE, TO DECIDE WHAT TO DO.”
Another fortuitous event. Dr Latham’s job had fallen through, because of the delay. “Phillip said: ‘Here’s a telephone number. Place called Naracoorte in South Australia. ere might be a job there. Talk to Dr Campbell.’ I made contact; they told me to come as a locum for three months, a er which I would have to nd something else. But another Englishman in the practice, who had worked all over the world, said, ‘I’ve been here nearly three years in Naracoorte, the longest I’ve ever been anywhere. It’s time I moved on’. I had a job.”
Practicing medicine in Naracoorte was a far cry from the monotony of general practice in Wolverhampton. “ ere were ve doctors in the practice and between us we ran the hospital which had 112 beds. You might see a patient in the morning, then send him over to the hospital, and a er a discussion with the theatre sister and whoever was going to administer the anaesthetic, he would be operated on that a ernoon. Senior partner John Smith was a surgeon, experienced in major trauma – road tra c accidents and industrial accidents – and he could do everything. I did less of the surgery, but I was good at fractures and obstetrics. Other things we would usually save for John

Smith, and we would always tell him if we were doing an appendix. Once, one of the doctors who was keen on obstetrics and could do caesarean sections, said he was going to do an appendix. e patient had a temperature and tenderness in the abdomen. But when we operated, the fellow didn’t have an appendix, nothing there. John Smith came in to have a look said, ‘Tell Sister, we’ll write up the notes later. Try and nd out what’s wrong with him’. We deduced it might be typhoid. John Smith said, ‘We had better write in the notes that we removed his appendix, because if he ever gets an attack of this again and goes to the hospital in the city or something, they’ll say, ‘Oh that country bumpkin practice didn’t know what they were doing’’.”


when Elizabeth and I drove down to Killarney. When we got back to Dublin on the evening of May 17, the tra c was terrible. It was, I supposed, rush hour, about ve o’clock. We could hear sirens, ambulances, re engines. ree bombs had gone o and there was chaos.” e Lathams had arrived in Dublin on the evening of the Dublin Bombings, when the UVF planted three bombs, killing 23 people.
“ e second time, in the 1990s, I went to an alumni meeting at RCSI. And then the third time was in 2012, which was the 50th reunion. I wasn’t really sure whether I should call myself Class of 1961 or 1962, but it’s too long a journey to make two years’ running!”
When Dr Latham was 63, the indemnity insurance for obstetrics increased. “We decided it was time for me to stop doing obstetrics but I felt it as a blow, thinking, I’m never going to get a telephone call at three in the morning saying there’s a foot on view and a breech birth in progress.”
For 25 years, Dr Latham had been doing medicals for pilots in the local aeroclub. “In Wolverhampton, I had seen people learning to y little Piper Cubs. I remember thinking I would get around to doing that some day. So decided to learn to y. I got my private pilot’s license at 64. I learned to y in a Piper, and graduated to a Super Decathlon, the sort used for aerobatics. Not that I did much of that, though I can do a loop,” he laughs. “I wasn’t a Flying Doctor, I was a doctor who ew, mostly for pleasure. If I was travelling for work, it was o en quicker to drive! I had to drive to the aerodrome, open the gate, the hangar doors, walk around the plane to check it, start the engine, warm up the oil a bit before I took o . When I arrived at the destination aerodrome, ve kilometres from the hospital, someone would have to pick me up.”
Dr Latham’s wife Jean died in February last year. e last six years of her life, Dr Latham was her carer, with the support of his children. Dr Latham still travels into the outback in his Toyota van, into the Northern Territory, along the old stock routes, where tin sheds and a rudimentary shop provide the only creature comfort. Solitude and the outdoor life suit him. On his shortwave radio he calls in to report where he is and what his plans are for the next day, so that his family don’t worry about him.
Dr Latham has returned to RCSI three times since 1962, the rst time in May 1974. “I brought my daughter Elizabeth, who was about twelve. ere was a meeting of anaesthetists I conned my way into. I remember some car trouble
RCSI, says Dr Latham, prepared him well for the unpredictable medical life of rural Australia. “RCSI had an enormous impact on my career. Firstly, there are students from all over the world. Secondly, we were taught to face things as they arose, to decide what to do. You didn’t wait for someone else to make the call.
“I remember, shortly a er I arrived in Australia, John Smith was in Adelaide for a surgeons’ meeting. At picnic races nearby, a fellow who had been drinking insisted on getting on his horse. He was thrown and was unconscious. e ambulance came in. I was ready to intervene surgically. e theatre sister was readying the instruments. Happily his condition improved.
“Each year, we had a small number of infants with acute epiglottitis croup who needed intubation. Putting in a nasotracheal tube was always stressful with the infant in danger and the epiglottis so enlarged that there is no view of the larynx, we just have to go blind. We saved every single one. On one occasion, a mother didn’t like the tube so she pulled it out. I was doing an ENT list in theatre and managed to intubate in Recovery where there was a spare Boyles machine.”
He was on one occasion giving a lecture when a nurse approached and said, “Oh, I remember you. I had a patient I was worried about because he was getting so breathless. You said, ‘I’ll be back in a minute’. You dived into the hospital and returned to stab him in the chest, put in a tube and connect an intercostal drain”. e patient began to breathe again. at was John Latham, thinking on his feet. “I had really done, the wrong thing. I should have said, Oh, yes, he’s very sick’, and sent him to the casualty department.
“We have a good health system in Australia. Like many, it has its drawbacks, but by and large, it’s a very positive one. You are charged what we call a common fee, but you actually get back 85%. Spend 100 dollars on healthcare, you really spend 15. Much less expensive than maintaining your car,” says Dr Latham. ■
Clinical placements are o en the rst real-life experience of patient interactions for students. We asked alumni to re ect on their most memorable stints

MB BCH BAO, BSc Resident in Internal Medicine, The Christ Hospital, Cincinnati
“I have two very clear memories of clinical placements with GPs. During my rst one in Dublin, the GP gave me a lot of autonomy seeing patients and drawing bloods, while always being close by, so I felt safe and well–supervised. It was more than being a y on the wall. My next placement was in Roscommon which was completely di erent. I was quite nervous arriving o the train in this sleepy little town, wheeling my suitcase and everyone looking to see who it was. ere were a lot of patients who hadn’t seen a GP in quite a long time or even followed up from previous appointments, whereas in Dublin, people were coming in for minor issues like sni es and a sore throat. I enjoyed the contrast between the two.
“One of my most memorable placements was Obstetrics and Gynaecology in e National Maternity Hospital. It was a tough one as I had my rst week of nights on labour and delivery, witnessing a number of emergencies. is was an eye–opening and challenging experience, which made me seriously consider this specialty as a career.
“Some placements were not as ful lling because of the team
“When I started in RCSI as a mature student, I had that extra bit of life experience that I hoped would help me to transition to my new life in the physio world. e class was a mix of other mature students as well as those coming through from pre–med; there was a nice balance to the group.
“My experiences with clinical placements were generally very positive. You were given responsibility very early on to manage your own patients and be responsible for their care. is was daunting at rst but soon became a rewarding challenge as it gave us a clear insight into our future career. Many students, myself included, may have entered the course thinking that we might end up in certain areas such as sports, private practice or hospital-based. e range of placements opened our eyes and minds to the varied roles available to physiotherapists.
“Placements could also be challenging. Having had numerous injuries over the years, I was used to being treated by physios in out-patient departments and private clinics. As a result, I found
dynamic and how interactive – or not – the consultant would be. I had a couple of placements in Dublin hospitals where the teams were just too busy, and the consultant didn’t have time to teach. Sometimes you felt that you were in the way; it’s di cult being a student, wanting to learn and trying to put yourself forward, when a team is not particularly receptive to you being there. I had to keep reminding myself not to be biased, it wasn’t the specialty, but the particular team that you were working with.
“As a female medical student, there were a few times where I experienced more exclusionary behaviour from male consultants, compared to my male peers. is was not a continuous problem but it was something that other female colleagues also experienced and that is now a topic for discussion globally in medicine.
“Having recently graduated, my clinical experiences are still fresh in my mind and it’s something I keep at the forefront when I am teaching medical students. I want to provide a positive and challenging learning environment that will help shape future doctors just as others did for me. My time in RCSI ew by and I cannot wait for the day I can come back and visit again.”
myself much more comfortable in these settings. e wards were a more intense prospect as the patients were more acutely unwell and required greater attention. is a orded a wonderful opportunity to practice the more caring side of our role as physios, with more time to get to know your patients while also helping them to regain their mobility and strength. I was fortunate enough to get experience in ICU and neonatal units, observe open heart surgery and work in A&E and paediatrics. is varied caseload was invaluable and I loved learning the roles of the MDT in patient care.
“Since graduating from RCSI in 2015, I have worked in private practice and pitchside with sports teams, as well as lecturing. I opened my own clinic last year and, COVID-19 permitting, I would love to accept students in on placements to observe and get them excited about a career in physiotherapy. My role gives me a great balance between treating patients, running classes, working with teams and most importantly, spending time with my wife and three kids.”


MB BCh BAO Resident in Paediatrics, Cincinnati Children’s Hospital
Starting fellowship at the The Hospital for Sick Children (SickKids) Toronto in summer 2021
“We started doing clinical placements a day a week in rst year and so we had a little taste of them by the time we started doing longer fulltime placements in third year. I think that helped eliminate the fear of the unknown, but even though I had had a little experience I was still nervous. Part of me was excited about getting into the meat and potatoes of medicine, but I worried that I might not be good enough or stick out like a sore thumb, so there were a lot of mixed emotions.
“Two placements really stand out for me. e rst was one of my rotations in Waterford. I was nervous going into it; I didn’t know what to expect. Would it be really dramatic, like the movies? Would I be able to interact well with the patients, some of whom had conditions that made their ability to communicate more di cult?
“ e teachers, especially Professor Mulcahy, helped me learn how to communicate with patients. at placement taught me
“I came to RCSI from Trinidad and Tobago at the age of 21 via an art history degree in NYU. I have great memories of clinical placements – all good. Psychiatry in St Luke’s, Kilkenny was particularly eyeopening in terms of interaction with the patients. I remember one patient with cannabis–induced schizophrenia who was in his early twenties, the same as us. Because I grew up in the Caribbean, seeing cannabis used was not a big eye-opener, but I had never seen the real psychotic e ects before.
“We were allowed to take histories in pairs and were included in round table discussions and team meetings in the Department during our time there. In the end I didn’t wish to pursue Psychiatry as a career, but I have carried a lot of what I learned into my dayto-day work as a Specialist in Occupational Medicine.
“On surgical placements, I remember standing around in theatre quite a bit. At the time, female medical students didn’t seem to get

MSc Neuroscience MB, Bch BAO LRCP&SI
Assistant Registrar General Surgery Jahra Hospital, Kuwait
one of the most important things in medicine, which is that most patients just want to be heard. You might not always get a straightforward history out of talking to someone for half an hour, but you can still learn a lot.
“I was able to take that learning with me to my other rotations. I also did a placement in a family GP practice in Drogheda which let me see what it is like to have a practice in a small town with patients of all ages, and I liked that very much too. My paediatrics placement con rmed for me that it was the area I wanted to pursue. In each clinical placement, the best teachers were always the ones who made me look at things in a di erent way.
“I did many placements in Waterford and it became like a second home to me. I love it there, it’s such a beautiful place. I ended up becoming friends with people outside my core group because of being on away placements with them. Being thrown together made you look outside your own bubble.”
as much attention as the males – it was a bit of a boys’ club. A er a great placement at the Eye and Ear I gave ENT serious consideration as I enjoyed learning about inner ear surgery. I remember being told by a surgeon that if I wanted to have a family one day I should probably not pursue a career in surgery. Back then, women who wanted to pursue surgery had to be very determined; I think the landscape has changed quite a bit since.
“I enjoyed the whole experience of medical school. I had a blast on all my placements. We all helped each other study and at our tenyear reunion we were all really wistful about our time in university. e whole social aspect of placements – sharing accommodation, learning and doing activities together – helped us all build better friendships. When I was an SHO and Registrar I did some teaching in Beaumont Hospital and I enjoyed that too. I hope to continue to teach in my current role in the University Hospital Limerick.”
DR HUSAIN ARIAN MEDICINE CLASS OF 2017
“ e rst day of a new placement always felt like the rst day of kindergarten, and I still feel the same starting each new rotation. My very rst placement was at Cappagh Hospital. It was in January and I remember arriving at St Stephen’s Green from where I was living in Sandyford to meet up with my classmates to share a taxi out to Cappagh. It was 5.30am in the morning and it was still dark. I was all over the place when it came to taking histories at the beginning, I had no system and was dealing with the challenge that English was my second language. Looking back I have made huge progress since then, taking histories is second nature now.
“I did a few placements in Waterford and got to know the city, it reminded me of Kuwait but with a di erent climate. I liked it very much. One placement was in Mullingar in November, and I decided to commute from Dublin. It rained a lot and I kept getting very wet. And I did my GP placement with a practice in Ennis in February. I fell asleep on the early morning train from Heuston and woke up in Cork, I went back to Limerick Junction

FRCPI (FOM). Specialist Occupational Health Physician, University Hospital Limerick. Acting Head of the Occupational Health Department Mid–West
to get on another train to Ennis but the tracks were ooded and I had to go by bus. I didn’t arrive in Ennis until 1.30pm. It’s funny, I remember less about the actual placements than I do about the weather.
“I remember two teachers in particular from placements. Dr Emer Henry in Waterford, taught us inclusively and pushed us out of our comfort zones; she taught us how to interact with patients.
“IT’S FUNNY, I REMEMBER LESS ABOUT THE ACTUAL PLACEMENTS THAN I DO ABOUT THE WEATHER.”
Professor James Paul O’Neill in Beaumont was an amazing teacher of clinical skills and now when I help teaching interns. I try to support them in the same way I was supported by Professor O’Neill; he’s my role model when it comes to teaching.”
“I remember my rst clinical placement was in Beaumont – that was the rst time we had interaction with patients. In 2002 in Ireland, they had a rm base system. e consultant had one team; everyone went on the ward round every morning, which provided continuity of care. It’s not the same in the UK, where I am based now.
“My Obstetrics and Gynaecology placement in Holles Street was one of the best. We were a group of about ten students, all on placement for eight weeks. We had one tutor, Dr Cathy Burke, with us for the whole time. She was very enthusiastic and involved us in lots of procedures. I remember scrubbing in on a C–section and delivering a baby via a normal delivery when she was on the night shi supervising. I still remember the baby’s name: Richard. at placement started me on the path in Obstetrics and Gynaecology.
“My clinical placement in Cavan was also memorable. We had a buddy system, and I did all my placements with my friend from

MB BCH BAO, Gastroenterology Specialist, Archbold Medical Center, Thomasville, Georgia
Cyprus, Evgenios Neofytou. He is now a researcher at Stanford University in the US. I was in Cavan, for a medicine and surgery placement, with him and another classmate of ours, for two months. We rented a car and stayed in a B&B, which was a ve–minute drive from the hospital. e doctors in Cavan hospital were very friendly. ey used to go out for drinks every ursday, and they took us with them.
“I had some of the best times of my life on placement; I had no bad experiences. I had good friends from Cyprus around me –we’d study together, go out together and make lifelong friends from all over the world.
“ e academic side of my job involves clinical lecturing and supervision. I have about eight students working with me on various projects and in the lab. I believe it’s very important to be enthusiastic and to really inspire students in what you are doing.”
“ e move from classroom to hospital was a moment we all awaited eagerly. Of course we were all anxious, and this was especially true as we were part of the rst graduating class from RCSI Bahrain. ere was a de nite sense of apprehension.
“Each clinical placement was unique. Whether it was medical or surgical, every patient encounter reminded us of the privilege of being in the medical eld and of becoming physicians. To me the ones that were most memorable were the placements where you truly felt like part of the team.
“Not all clinical placements go smoothly. Consultants, residents, and fellow medical students have di erent personalities. You have to gure out the team dynamics and decide on the best approach. ere are those who micromanage, and others who give you too much freedom. ere are those who are very interested in teaching
“I fondly remember all my clinical rotations, both in Dublin, at Beaumont Hospital and James Connolly Memorial Hospital, as well as in Drogheda and Kilkenny. Each had a di erent avour and added tremendous value to our ongoing clinical education and learning.
“ e Dublin hospitals had a di erent dynamic. ey were larger, with higher patient ow, and gave us a chance to interact with a multitude of clinical specialties. e peripheral hospitals, on the other hand, o ered us the opportunity to interact more closely with the in-patient teams, becoming adept at various procedures such as placing IV lines or performing lumbar punctures.
“I was blessed to meet many wonderful clinicians, with Professors Seamus Sreenan and Sam McConkey being two that had a tremendous impact on shaping my career. e clinical rotations were truly exciting, because in the pre-clinical years, one cannot wait to get started on the oor. ere is something magical about the rst time you put on a white coat and a stethoscope

LRCP&SI, MBBCh, BAO (NUI), MSc(Dist), AFHEA, MRCOG, PhD. NIHR Clinical Lecturer, sub-specialising in Maternal & Fetal Medicine, King’s College London
and others who are not at all. As long as you perform your duties and understand you are there to learn, it all works out.
“My most memorable placement was the cardiology elective at Emory University Hospital in Atlanta, Georgia. Since my goal was to complete my training in the USA I had to gure out how to go about applying for and getting approval to complete a clinical elective in a di erent country. Professor Kevin O’Malley, RCSI Bahrain President at that time, helped by introducing me to an RCSI Dublin alumnus who had been practising there. Dr Gerard McGorisk (Class of 1988) helped facilitate my visit and I had the privilege of working with him and other attendings during my time there. I had the opportunity to be an active member of the cardiology consult service and to get rst-hand experience of the practice of medicine in a di erent country and culture.”
around your neck – it instills a sense of gratitude at being given a chance to be part of this profession. To this day, when I put on my stethoscope, I get a similar feeling.
“I remember looking up to the interns, the SHOs, the Registrars and the Consultants and wondering, ‘Am I ever going to get there?’ I was very fortunate to have been part of a number of wonderful teams who took me under their wing and taught me to stand on my own two feet in an o en challenging environment. I never felt out of place. We tried to help by doing some of their work and in turn they would teach us when they had a free moment. It was a matter of nding one’s balance within the team.
“Overall, my pre-clinical and clinical training in Ireland gave me a solid practical foundation and clinical acumen. e focus on clinical examination and bedside teaching has stood me in good stead and still does to this day, when I teach my residents and fellows. I will forever be grateful for the opportunity to have studied in Ireland, and will remain eternally thankful to all those who helped me become the physician that I am today.”

Allegheny Health Network (AHN)

MB BCh MRCPsych
FRCPI, Consultant
Forensic Psychiatrist,
National Forensic Mental Health Service
“Seeing medicine in practice was inspiring and clinical placements were a great opportunity to get to know classmates better.
“One of my favourite placements was General Surgery in University Hospital Waterford – there was an excellent tutor there.
e sunny south east lived up to its name and I got to live with my best friend, Siún, and her family in the Comeragh mountains at weekends. I also enjoyed a placement in e Coombe. It was the rst time I felt included in the patient experience beyond history-taking – staying late and sitting with women during labour. An inspiring neonatologist, the late Dr Helen Mulcahy, stood out. She took the time to teach and include medical students,
“My rst observational placement was in Beaumont at the beginning of second year. I worried that I was in the way but my senior was lovely. I thought, ‘I can do this.’
“Over the course of my degree I did further clinical placements. Temple Street was fantastic, I adored it. I had just come back from the RCSI Christina Noble programme in Vietnam and was really interested in paediatrics. I found it quite emotional though and the placement opened my eyes to the realities of paediatrics. It de nitely changed my perspective. I had great teaching there from Zita McAllister, my senior. In nal year you get your own

MB BCH BAO, GP Registrar, Royal College of General Practitioners, London, UK
even remembering our names, which was a rare thing. Some consultants on placements could be dismissive. ere was also sexism at times. Students and junior doctors are more assertive now and that’s a good thing. It is certainly di cult at times to include students during a busy clinic but the onus is on the medical team to ensure they become, however brie y, part of the team.
“Funnily, my Psychiatry placement was lacking. It was when the emphasis began on home treatment in Psychiatry and there were no in-patients in the unit. e doctors were fantastic but the rotation lacked clinical exposure.”
caseload, so you are very much utilised as a physio, it is a very hands-on method of teaching. All my experiences were positive. e emotional connection with patients was something that I hadn’t considered previously, I didn’t think about how bringing your work home would a ect you. In one hospital I worked with the acute respiratory surgical team in ICU, where all patients are treated twice a day. I found that tough, particularly when I was with a patient when they died. I never thought that would happen to me as a physio. Peer support is huge in that situation, you really rely on your classmates.”
“My very rst placement in Cork turned out to be one of my best. For six weeks I went to Dr Don Co ey’s GP practice in the Salvation Army on Merchant’s Quay, where he treats the underprivileged and homeless, focusing on their welfare and wellbeing, and runs a TB clinic every week.
“It had a huge impact on me in terms of opening my mind to the scope of general practice, which is o en not considered a ‘specialist specialty’. It would be di cult for the patients Dr Co ey was seeing to be seen by a doctor in a hospital. He was able to treat them with care and develop a one-on-one rapport. I think being a GP gives you that ability to connect with your patients,
“I had some amazing clinical placements while I was at RCSI Bahrain. I struggled, lost my patience and made lots of mistakes, but I am a better nurse today because of all that. Each new clinical placement was like an expedition, and each day unpredictable, with new patients, new personalities and new information to learn.
“For one placement, I was assigned to the neurological ward, taking care of patients who had su ered a stroke. For the rst time in my life I understood the e ort that goes into getting these patients from bedridden to ambulatory on discharge. e rst time I observed a patient’s death and had to communicate with the family was hard and I remember it to this day.
“I remember one mentor from a surgical placement. I liked her way of organising everything. She made a folder for us students

BSc (Honours) Physiotherapy, RCSI Physiotherapist, Reform Physiotherapy and Pilates
to know the inside out of their illness and social situation and to give holistic care. ere is not the same continuity of care in a hospital setting.
“A er graduating from RCSI I worked in Singapore for a couple of years in di erent specialties, then at the UN in New York in a non-clinical role. I missed the connection with patients and kept thinking back to that rst placement in Cork. I realised that what I really wanted to do is have my own clinic and give my patients holistic care. I started GP training in London in 2018 and am in my nal year now. If it weren’t for Dr Co ey and the placement in Cork I would never have thought of going the GP route.”
to explain everything and every single day she used to assess the patient’s environment and make everything clean and tidy. She prepared patients’ medication in a very organised way. I learned a lot from her. How included you were depended on the team.
“I remember one placement on a female medical ward. A patient with Alzheimer’s Disease was described by the nurses as aggressive and uncontrolled. ey were trying to insert a peripheral line but she became agitated. No one from her family was present. I tried to communicate with her about her love of cooking and from that conversation, she became calm and the task was achieved successfully. Nursing is not just about giving medication and following the doctors’ orders. Communication, monitoring and observation can change and save patients’ lives.” ■

Every year RCSI students bene t from the hundreds of alumni who give generously of their time to support and advise, mentor and inform – and this is very much appreciated. If you would like to volunteer, here are some ways you could be of great help
• Register as a student mentor
• Offer to secure a clinical elective for a student/s
• Participate as a guest speaker in Student Society/Club events
• Provide advice through career talks
• Become a member of an organising group for alumni events
• Advise and assist with publications for alumni, including this Magazine!
We are very grateful to all alumni who helped over the past year. These alumni are just some who contributed in different ways:
DR JAVED MACHIKAN (Medicine, Class of 2020) joined other alumni panellists to speak to students about internship pathways in Ireland as part of an event organised by the Leadership and Management in Healthcare Student Society.
SIMON GALLIGAN (Physiotherapy, Class of 2017) shared his insights with 33 final-year Physiotherapy students as part of a virtual discussion about managing the transition from student life to being a working professional.
DR JOAN NOELKER (Medicine, Class of 2010) A registered mentor since 2012, Dr Noelker participated in a review of the Mentor Network and continued to provide advice and guidance via the platform throughout the year.
DR BEN LA BROT (Medicine, Class of 2006) mentored an RCSI final-year medical student during an unforgettable two-month immersive clinical elective with Floating Doctors, where the student played a critical role in providing essential healthcare to indigenous populations in the Bocas del Toro province of Panama.
DR EMMA MEAGHER (Medicine, Class of 1987) and PROFESSOR NOEL WILLIAMS (Medicine, Class of 1981) The married duo volunteered to become members of the alumni group which is organising the North American Alumni Engagement Series.
PROFESSOR MICHELLE F MAGEE (Medicine, Class of 1982) delivered a workshop on preparing personal statements as part of the Professional Identity Webinar Series organised by RCSI’s Careers Team.








IF YOU ARE INTERESTED IN VOLUNTEERING, PLEASE MAKE SURE TO REGISTER IN OUR UPCOMING AUTUMN RECRUITMENT DRIVE OR EMAIL THE ALUMNI TEAM DIRECTLY AT ALUMNI@RCSI.IE THANK YOU!



Over the past 12 months RCSI alumni and friends have donated €362,000 to support student programmes across the University.




RCSI has committed to ensuring that COVID-19 and its impact will not prevent students from gaining the world-class educational experience that RCSI prides itself on. In light of these unprecedented times, we launched #RCSItogether for Our Students’ Future Campaign and doubled funding for the Student Hardship Fund. Gifts from alumni ensure that students are supported to continue their path to become healthcare professionals.
34
In 2020, generous alumni funded 34 students across the Aim High, Consilio Manuque, Kiran Pathak, International Medicine and Moira O’Brien sports scholarships. Your support is enabling them to achieve their ambition and have a positive impact on patient lives in the years to come.
€18K
During the early days of the pandemic, RCSI alumni and friends raised over €18,000 as part of an emergency appeal to provide protective Wound Care Kits for intensive care staff providing care to COVID-19 patients.
14

In 2020, 14 students were given the opportunity to enrich their training by gaining valuable experience in leading teaching hospitals worldwide.
1,500
Over 1,500 RCSI students, who stayed in Dublin throughout the holiday period, were supported through the RCSI #FestiveNightIn appeal. The initiative saw students receive a festive stocking filled with cheerful treats and goodies to help sprinkle some Christmas magic and bring a little respite during the holiday season.
In addition… last year 123 members of our alumni community registered to become mentors for RCSI students, providing guidance and advice throughout their studies. Thank you for your support!
If you would like to provide your support to the RCSI_Tomorrow campaign, you can do so by visiting www.rcsi.com/support-us/give-now or call Paul in the Alumni Office on +353 (0) 1 402 2729 or email alumnioffice@rcsi.ie






























