Better Health









 By C ori U rban Special To The Republican
By C ori U rban Special To The Republican
For 30 years, Kathy Tobin, director of annual giving and events for the Baystate Health Foundation, has watched “the power of this community bathe breast cancer survivors in the pink rays of their love and support.”
Since it was founded in 1994, Rays of Hope has been committed to improving the breast health of people in local communities with quality and compassion. The event has grown from 500 to more than 20,000 participants and has raised more than $16.6 million, all of which supports patient care, services and research throughout Western Massachusetts.
This year’s 30th anniversary event, which takes place Oct. 22, offers three participation choices: an 8k run, a 2-mile handicap-accessible walk route or a 5-mile walk route, all beginning at Temple Beth El in Springfield and winding through Forest Park.
Temple Beth El will host a pre-walk action.
The stage program opens at 9:45 a.m. and will showcase survivors, community partners and Baystate Health medical staff. There will be a Rays of Hope store — 100 percent of proceeds support Rays of Hope. The Pink Hope Lounge for
survivors will feature community partner programs, survivor resources and exclusive survivor shirts available on a first-come, first-served basis. Along the walk route, local performers and sponsored water stops will keep participants entertained and hydrated.
The mission of Rays of Hope is to raise funds to improve the breast health of the people in local communities with quality and compassion in partnership with the Baystate Health Breast Network. By offering community education and outreach; providing coordinated, accessible, and medically advanced care at the initial stage of diagnosis and continuing through treatment and recovery; and supporting patients through the continuum of care, the needs of the whole person are acknowledged.
Rays of Hope also is committed to funding breast cancer research.
Last year, Rays of Hope raised more than $523,000, all of which remained local.
“Our goal this year is to surpass last year’s total so that we can continue to fund local breast cancer care, support and research for the people in western Massachusetts,” said Michelle Graci, manager of events for the Baystate Health Foundation.








Since its inception in 1994, Rays of Hope has been helping individuals in the fight against breast cancer. Through the Baystate Health Breast Network, Rays of Hope cares for the whole person from diagnosis and beyond. This is done by supporting research at the Rays of Hope Center for Breast Cancer Research, funding state-ofthe-art equipment, sponsoring breast health programs, outreach and education and supporting patients and survivors. Rays of Hope also provides grants for complementary therapies and cancer programs to its community partners throughout Western Massachusetts.
One in eight women and one in 100 men will develop breast cancer in their lifetimes, and it is estimated that there will be more than 290,000 cases diagnosed in 2023, noted Dr. Grace Makari-Judson, medical director at the D’Amour Center for Cancer Care and co-director of Rays of Hope Center for Breast Cancer Research.
Since 1994, significant progress has been made in diagnosis and treatment. “Many of these innovations were fast-tracked into our community thanks to Rays of Hope including minimally invasive biopsies instead of surgical biopsies, sentinel lymph node
biopsy rather than complete axillary dissection and seed localization instead of needle localization,” Makari-Judson said. “Increased uptake of genetic testing aids to identify individuals at highest risk and develop personalized strategies for risk reduction.”
Coordinated multidisciplinary teams have been assembled to address complexity of care and streamline and select best options for each individual patient. New drugs and new molecular tests are used to personalize care.
Chemotherapy is reserved for those who will benefit the most. Targeted treatments, such as the HER2 directed treatment, trastuzumab (Herceptin) and immunotherapy have revolutionized care in specific subsets of breast cancer, she added.
“Many of those with metastatic breast cancer live longer with better quality of life and may survive over five years thanks to many new treatment options. The best news: Since the 1990’s, mortality has declined by nearly 40 percent,” Makari-Judson said. She pointed out that studies show that screening mammography reduces risk of death from breast cancer in women ages 40 to 74: “Most recent recommendations suggest women at average risk

should start annual screening mammography at age 40. Women should undergo risk assessment and those at higher risk may consider starting earlier. There is no upper age limit for mammography, rather this should be decided based on an individual’s overall health.”
She recommends knowing one’s family history, not smoking, maintaining a healthy weight especially after menopause, limiting alcohol and exercising at least 120-150 minutes a week. For some women, risk-reducing medications might be recommended.
A breast cancer diagnosis is the beginning of a long, difficult and stressful journey.
“Rays of Hope surrounds survivors and those who care about them in a great big pink hug of support, Graci said.
“Together we look for ways to inspire hope for a cure and offer an opportunity to lighten the load through personal
and community experiences. We may don a pink tutu, wear funny hats or paint the city pink during a Springfield Thunderbirds game — it’s the Rays of Hope way of saying every moment matters.”
Rays of Hope began as a one-day event, raising $50,000. Now it has mobilized 20,000 participants, businesses and municipalities to form a year-round movement.
There is no fee to register for the 30th anniversary event on Oct. 22; however, participants are encouraged to set a fundraising goal to help support the mission.
To receive the collectible Rays of Hope T-shirt, participants must raise at least $50. T-shirts are only available on a first-come, first-served basis by picking them up the morning of the event.
“Looking out at the thousands who gather on that special Sunday morning every year, I witness shaved heads, crazy hats, smiles through tears,” Tobin said. “I receive hugs and give hugs to survivors joyous that they are back
for another year. I realize how lucky I am to be healthy, and I marvel at the strength of those doing battle. When those thousands of feet cross the finish line and we count the proceeds of their actions, I know that together we are making a difference by funding research, programs and opportunities — the experience gives me hope that we are making progress and we will one day find a cure.”
Registration is easy and convenient through the website baystatehealth.org/raysofhope. Participants can register as individuals, join a team or form a team.
In addition to the walk and run fundraising efforts, community members can organize their own supportive fundraising events. These events can range from setting up a lemonade stand to hosting a paint-and-sip party.
For more information call 413-794-8001 or visit Baystatehealth.org/ Raysofhope.

We’re BOTH survivors because of people like you who give HOPE here in western Massachusetts.
For 30 years you’ve come together to fund research, improve treatment and provide support to people diagnosed with breast cancer.
JOIN US SUNDAY, OCT 22 FOR A BIG PINK HUG!
Your fundraising will help get us over the finish line toward the cure.
BaystateHealth.org/RaysofHope
Presenting Sponsor

















Medical treatment, prayer, family support and a positive attitude all helped Melanie Roy of Agawam survive breast cancer.
ByC ori U rban Special To The Republican
She was diagnosed on Nov. 22, 2022, her 19th wedding anniversary; she began chemotherapy on Dec. 8.
Roy is grateful for the care she received at Mercy Medical Center’s Sister Caritas Cancer Center. She appreciated the positive attitude and confidence in the treatment plan of Dr. Sarah J. McPartland, medical director of the Center for Breast Health and Gynecologic Oncology at Mercy Medical Center. “Dr.
surgery performed influences the length of recovery. Women who undergo minimally invasive breast conserving surgery (lumpectomy) can expect to have discomfort at the operative site(s) for 1-2 weeks. “Most women do not have severe pain following this surgery, with discomfort managed with over-the-counter medications,” McPartland said.
in their lives. For the majority of women, however, adjusting to life after cancer can take months or years,” McPartland said.
The physical recovery from cancer treatment can be faster than the psychological recovery. Having a support system in place is important during this time; the type is varied and personal depending on the needs and resources of the patient but may include family, friends, a spiritual community or leaders, counselors or survivorship groups/ networks.
coordinated cancer therapies and patient education. “We strongly believe in empowering women to become active participants in their treatment planning and care,” McPartland said.
conserving surgery (lumpectomy) using radiation-free and wire-free magnetic-seed localization procedures, nipple sparing mastectomy, reverse axillary mapping and oncoplastic procedures.

McPartland was wonderful!
She explained everything that needed to be done, and she had such a positive attitude about my prognosis. She’s my angel,” said Roy, who prayed for strength, energy and courage every day.
She underwent chemotherapy prior to a lumpectomy to remove a small tumor and one lymph node. McParland performed the surgery and achieved “clear margins.”
The doctor usually begins talking to patients about survivorship six months after they have completed the “active” parts of treatment (surgery, chemotherapy, radiation). Sometimes women may still be receiving some type of maintenance treatment during this period, such as endocrine therapy or immunotherapy.
How quickly a patient recovers from breast cancer surgery is dependent on several factors. The type of
Women who undergo removal of their breast (mastectomy) usually have a longer period of recovery, during which time they may need to have more frequent bandage changes or have a drain in place to collect excess fluid. Recovery from mastectomy can take 3-4 weeks, sometimes longer. “More frequent appointments with the surgeon and care team are expected following mastectomy,” she said, adding that at home, women may initially need assistance with everyday activities, such as dressing and bathing. A visiting nurse can be arranged to provide care in the woman’s home when necessary. If breast reconstruction is performed, recovery can take three or more months.
“Women who have other serious medical conditions, such as diabetes or heart disease, as well as those that receive chemotherapy before or after surgery, often need a longer period to heal and regain fitness following surgery,” McPartland said.
Just as the journey through breast cancer diagnosis and treatment is different for every woman, so too is the journey through survivorship. Women navigate the transition from active cancer care to survivorship in many different ways. “For some women, the return to a ‘normal’ life occurs quickly, and they are happy to move on to the next chapter
“As cancer physicians, we encourage women to lead the healthiest life possible after cancer care,” McPartland said. This includes regular exercise, eating a healthy diet that is rich in fruits and vegetables and addressing chronic medical issues such as diabetes, high blood pressure or heart disease.
According to the doctor, there is growing evidence to suggest that healthy lifestyle choices can help to prevent both the development of a new cancer as well as cancer recurrence. Participating in exercise most days of the week (with a goal of at least 150 minutes per week) and eating a heart healthy diet that is low in saturated fats and sugars reduces the risk of breast cancer recurrence. Avoiding excessive alcohol and quitting smoking also reduce the risk of breast and other cancers.
During recovery, medical professionals actively screen for anxiety and depression during this period. “It is both understandable and common for women to experience some degree of anxiety regarding the potential for cancer recurrence,” the doctor said. “This can be exacerbated by routine testing such as blood work and mammograms. We encourage women to have an open dialogue with their cancer physicians about these concerns.”
Additional support from behavioral health counselors is sometimes recommended to help empower women about their health.
Roy said, Rebecca DeJesus Sleeper, the nurse who oversaw her chemotherapy treatment, always made her smile and feel comfortable. “Seeing and talking to her made the chemo treatments seem less difficult – and I’ll always be thankful for that,” she said.
The Center for Breast Health and Gynecologic Oncology at Mercy Medical Center is focused on providing personalized, state-ofthe-art care close to home. Services are provided by a multi-disciplinary team of cancer specialists and complementary support staff who focus on prompt diagnosis,
Mercy’s breast care program is the only one in Springfield accredited by both the National Accreditation Program for Breast Centers and the American College of Surgeons Commission on Cancer, assuring that Mercy meets the highest standards of care for patients with diseases of the breast. Breast surgeons utilize contemporary surgical techniques such as breast
Cancer support services that are available at the Center for Breast Health and Gynecologic Oncology include counseling, support groups, nutritionists, a lymphedema clinic, a recovery and rehabilitation program, physical and occupational therapists and certified mastectomy bra fitting and prosthesis.
“A patient is considered in remission from breast cancer



when they have completed all portions of their treatment plan which may include surgery, chemotherapy, radiation, endocrine (hormone) therapy and/or immunotherapy, and testing (such as lab work, X-rays) fails to show any evidence of cancer,” McPartland said. “Most patients who are treated for breast cancer will remain in remission.” However, any patient who has had breast cancer is at risk for cancer recurrence.
For more information go to trinityhealthofne.org and click on “Cancer Care.”





Cancer is a formidable disease that the World Health Organization reports is the leading cause of death worldwide. Figures vary, but organizations such as the WHO and the American Cancer Society estimate that around 9.5 million people die from cancer every year.
No type of cancer causes more deaths in women across the globe than breast cancer.
Though the five-year survival rate for breast cancer patients has increased by a significant margin in recent decades, a 2019 study published in The Asian Pacific Journal of Cancer Prevention reported a significant increase in breast cancer mortality rate in the 25-year period preceding the study. The researchers behind the study theorized that the spike in mortality rate could be due to an increase in incidence and prevalence of breast cancer.
Like all cancers, breast cancer cannot be prevented. However, various healthy habits could help women reduce their risk for the disease.
Avoid alcohol
The ACS reports that alcohol consumption is a clear risk factor for breast cancer. Risk increases with the amount of alcohol a woman consumes.
For example, a woman who consumes one alcoholic drink per day has a 7 to 10 percent higher risk of getting breast cancer than a woman who abstains from alcohol.
Drinking two to three drinks per day



could increase risk by around 20 percent.
Being overweight or obese increases breast cancer risk, particularly among postmenopausal women. According to the ACS, after menopause women get most of their estrogen from fat tissue.
Fat tissue increases estrogen levels in the body, which in turn increases a woman’s risk for breast cancer. Elevated levels of insulin in the body, which is common among individuals who are overweight, also has been linked to higher breast cancer risk. Establishing and maintaining a healthy weight cannot prevent breast cancer, but it can help women reduce their risk for the disease.
A sedentary lifestyle increases a person’s risk for various conditions and diseases. Women who live such a lifestyle are at elevated risk

for breast cancer. The ACS notes that sedentary behavior such as sitting, lying down, watching television, or engaging with screen-based forms of entertainment that do not require physical activity can increase breast cancer risk, especially for women who spend most of their work day sitting down. A more physically active lifestyle that includes routine exercise can help women reduce their breast cancer risk.
Eating right is another way for women to reduce their breast cancer risk. Vegetables, fiber-rich legumes such as beans and peas, fruits across the color spectrum, and whole grains are some components of a healthy, nutrient-rich diet that can help lower breast cancer risk. Women also can avoid certain foods, such as red and processed meats and refined grains, to lower their breast cancer risk.
Though there’s no guaranteed way to prevent breast cancer, women can embrace various healthy habits to lower their risk for the disease.






The
World
Health Organization reports that roughly 2.3 million women were diagnosed with breast cancer in 2020.
By the end of that year, there were nearly eight million women alive who had been diagnosed with the disease in the previous half decade.
A breast cancer diagnosis inevitably leads to questions about the disease. The bulk of those questions undoubtedly are asked by the millions of women who are diagnosed with breast cancer. But millions more individuals, including friends and family members of recently diagnosed women, may have
their own questions. Women can discuss the specifics of their diagnosis with their physicians. In the meantime, the following are some frequently asked questions and answers that can help anyone better understand this potentially deadly disease.
Cancer is a disease marked by the abnormal growth of cells that invade healthy cells in the body. Breast cancer is a form of the disease that begins in the cells of the breast. The National Breast Cancer Foundation notes that the cancer can then invade surrounding tissues or spread to other areas of the body.
The NBCF notes that exercise strengthens the immune system and women who commit to as little as three hours of physical activity per week can begin to reduce their risk for breast cancer. However, even routine exercise does not completely eliminate a woman’s risk of developing breast cancer.
Is there a link between diet and breast cancer?
The organization Susan G. Komen®, a nonprofit source of funding for the fight against breast cancer, reports that studies have shown eating fruits and vegetables may be linked to a lower risk for breast cancer, while consuming alcohol is linked to an increased risk for the disease. In addition, the NBCF reports that a high-fat diet increases breast cancer risk because fat triggers estrogen production that can fuel tumor growth.
Is there a link between oral contraceptives and breast cancer?
The NBCF reports that women who have been using birth control pills for more than five years are at an increased risk of developing breast cancer. However, the organization notes that risk is very small because modern birth control pills contain low amounts of hormones.






Can breastfeeding reduce breast cancer risk?
Breastfeeding and breast cancer are linked, though the NBCF notes that the role breastfeeding plays in lowering cancer risk depends on how long a woman breastfeeds. The World Cancer Research Fund International notes that evidence indicates that the greater number of months women continue breastfeeding, the greater the protection they have against breast cancer.
Is there a connection between stress and breast cancer?
The NBCF notes that researchers have found that traumatic events and losses can alter how the immune system functions, which can provide an opportunity for cancer cells to establish themselves within a person’s body. The NBCF urges women to identify ways to keep their stress levels in check.
Breast cancer education can be a valuable asset as women seek to reduce their risk for the disease.
 By K eith J O C onnor, Sr Special To The Republican
By K eith J O C onnor, Sr Special To The Republican
When it comes to treating most cancers today, specialists are quick to denounce the “one-size-fits-all” or “cookie cutter” approach that has vastly changed over the past several decades.
It was back on April 16, 1999, that a short article appeared in The Wall Street Journal entitled “New Era of Personalized Medicine: Targeting Drugs for Each Unique Genetic Profile,” which introduced to the public the new term “personalized medicine.”
“Decades ago, most patients with breast cancer received the same treatments. At that time, there really wasn’t a way for us to differentiate treatments for more effective outcomes based on a woman’s specific type of breast cancer,” said medical oncologist and breast specialist Dr. Prarthna Bhardwaj of the Baystate Regional Cancer Program.
But today, there is.
Personalized medicine, now more often referred to as precision medicine, is an innovative approach to the tailoring of medical (pharmacological) treatment. It is based on the individual characteristics of each patient by identifying the molecular fingerprints of various cancers and using them to divide cancer’s oncebroad categories into far more precise types and subtypes. It allows for medical care that “focuses on the right drug at the right dose at the right time for the right patient.”
“Modern science has allowed us to focus on improving outcomes for our patients.
Today, we are seeing women diagnosed with stage 4 breast cancer, who years ago would have an average life expectancy of months to now surviving for years with treatments that are improving the quality of life for many,” Dr. Bhardwaj said.
“Many of these new treatments began with patients who had advanced or stage 4 breast cancer. When oncologists started to see success in treating these patients with targeted therapies, what followed was incorporating them into treatment for patients with earlier stage cancers to achieve better outcomes for them as well,” she added.
The Baystate breast specialist noted that in precision breast cancer medicine, doctors are now aware that cancer results from a unique variation in an individual’s genetic makeup or genome. “We now know what proteins are being expressed in a patient’s particular type of breast cancer. Taking that a step further, we can perform sophisticated genetic testing on the tumor’s tissue, which is critical today for improved personalized medicine,” she said.
One of the earliest examples of putting precision medicine to work for breast cancer patients, and that served as an initial step in identifying different types of breast cancers, was the discovery in 1986 of the HER2 gene that promotes the rapid growth of cancer cells. HER2-positive breast cancers, which tend to be more aggressive than other types of breast cancer, account for about 15-20 percent of all breast cancer
diagnoses, where the breast tumor has high levels of the protein (also called receptors) known as HER2 which stands for human epidermal growth factor receptor 2.
“Researchers were able to identify in the 1990s a HER2 directed therapy, a humanized monoclonal antibody treatment called Herceptin (trastuzumab) that targets the HER2 protein by actually going inside these cancer cells and shutting them off, resulting in longer survival for those patients,” Dr. Bhardwaj said.
Herceptin paved the way for the development of additional pharmaceuticals that specifically target the HER2 gene, such as Kadcyla (ado-trastuzumab emtansine) and oral agents like Tykerb (lapatinib).
“Not all patients benefit from the same treatments,
and this is what inspired researchers to learn why. Breast cancers are routinely tested for hormone receptors, specifically estrogen and progesterone, as well as HER2 currently. There is a subset of women who have triple-negative breast cancer who do not express HER2, estrogen or progesterone, resulting in their not being able to be treated with therapies targeting these protein markers leaving them to rely on standard infusional chemotherapy,” Dr. Bhardwaj said.
“Triple-negative breast cancers are much more aggressive. However, they are immunologically active cancers, and that is where the concept of immunotherapy was introduced,” she added. Immunotherapy is a type of cancer treatment that involves

drugs that boost the body’s own immune system to recognize and attack cancer cells.
“Although several gene defects have been identified today that contribute to breast cancer, we don’t yet have treatments against all of them, but the good news is that more are slowly beginning to be introduced in the fight against breast cancer. One of the newest and fastest-growing types of anticancer drugs is antibody-drug conjugates (ADCs) like Enhertu (trastuzumab deruxtecan).
ADCs involve the targeting properties of monoclonal antibodies, which bind to a specific protein attached to those cells and then go on to release a chemotherapy drug, preferentially killing cancer cells but preserving the normal cells,” Dr. Bhardwaj said.
However, surgery remains an integral treatment for early-stage breast cancer. This can be in the form of a lumpectomy or mastectomy, depending on the tumor size and breast size. Precision medicine has opened the window to allow targeted medical therapy to help shrink larger tumors or to treat positive lymph nodes and allow for smaller surgeries with less surgical risks, such as lymphedema which is a chronic swelling of the arm. There may even be a day when surgery does not need to be part of a treatment plan, and clinical trials are ongoing looking for the appropriate cancer and patient scenarios to which this could apply.
Dr. Bhardwaj noted patients need to keep in mind that not every treatment option

works for every type of breast cancer. For that reason, it is important for patients to have open discussions with their healthcare team to learn and understand what their options are. The most optimal treatment for breast cancer today involves a multidisciplinary team like that found at Baystate Health involving surgeons, medical oncologists, radiation oncologists, pathologists, and radiologists.
“At Baystate Health, we are fortunate to have a robust breast cancer program with dedicated healthcare professionals who work in tandem to provide the most appropriate care for an individual,” Dr. Bhardwaj said.
“Any type of cancer diagnosis is a life-changing event for patients, and we are striving hard to make treatments more effective and less toxic. It is a privilege to be an oncologist guiding patients through their cancer journey as the field evolves in exciting ways,” she added.



Tuesday, October 10, 6-7 p.m. | with Dr. Folashade Ajegba
After getting a mammogram, it’s common to receive a callback which can be stressful and worrisome. Join Dr. Folashade Ajegba, Radiology at Baystate Health, for a discussion about mammography, what a radiologist is looking for, why you might get a callback, what happens next, and why the additional information you receive from a callback is a good thing.
Monday, October 16, 6-7 p.m. | with Dr. Jesse Casaubon
Treatment options for breast cancer can include surgery as part of the full treatment plan. Join Dr. Jesse Casaubon, Baystate Surgical Oncology & Breast Specialists, for a discussion about the options for a lumpectomy and a mastectomy, the potential differences, factors determining the surgery, surgical techniques, cosmetic results, and recovery.
Monday, October 30, 6-7 p.m. | with Dr. Prarthna Bhardwaj
The treatment of breast cancer has evolved from a “one size fits all” approach to “precision medicine.” This means we now can tailor medical treatment based on the genetic personality of an individual’s cancer. Join Dr. Prarthna Bhardwaj, Hematology/Oncology, Baystate Regional Cancer Program, for a discussion about how molecular testing impacts targeted treatments and the advances that have been made.



signed to help them accurately interpret mammograms. If the mammograms were flagged as suspicious, women were asked to come back for more tests.
In total, AI-supported screenings detected breast cancer in 244 women, compared to 203 in the standard screening group - a difference of 20 percent.


The Washington Post
Artificial intelligence can detect breast cancer in mammograms as effectively as experienced radiologists, according to a new study that some experts are calling a game changer for the field of oncology. The emerging technology could cut radiologists’ workload by about half, freeing them for more advanced diagnostic work, the study found.
The preliminary analysis of a long-term trial of 80,000 women in Sweden, published Tuesday in the journal Lancet Oncology, showed that AI readings of mammograms actually detected 20 percent more cases of breast cancer than the “standard” reading by two radiologists. The AI assessments were verified by one or two radiologists, depending on the patient’s risk profile.
This led the researchers to conclude that using AI in mammography screening is a “safe” way to help cut patient waiting times and reduce the pressure on radiologists amid a global workforce shortage.
It may be a while before mammograms will be read by a machine - as the authors and other experts have warned that AI models need to be trained and tested more before they can be deployed in health-care settings.
Still, the findings are “breathtaking,” wrote Nereo Segnan and Antonio Ponti, experts affiliated with the Center for Epidemiology and Cancer Prevention in Turin, Italy, who were not involved in the analysis.
In an article accompanying the release of the study, they suggest that integrating AI in screening procedures could ultimately “reduce breast cancer mortality” by making

sure breast cancer is identified sooner, when it is more treatable. This would be a huge win, given that breast cancer is the “world’s most prevalent cancer,” according to the World Health Organization.
The analysis is “game changing,” Robert O’Connor, director of Ireland’s National Clinical Trials Office (NCTO), wrote on X, formerly known as Twitter. It shows that AI could help triage mammograms according to cancer risk and identify breast cancer in those mammograms at a higher rate than radiologists with at least a couple of years of experience.
Using machine learning to try to improve medical diagnostics is not new, but it has accelerated in recent years with advancements in artificial intelligence.
The findings from this study are in line with emerging research showing that AI could

413.525.6062
www.petes-sweets.com

Whelp humans identify cancer earlier or more accurately, possibly leading to better outcomes for patients. The study is the first randomized controlled trial to investigate the use of AI in mammography screening, according to its authors.
The trial recruited 80,020 women from 40 to 80 years old who had mammograms in Sweden between April 2021 and July 2022. Half of them were randomly assigned to have their mammograms read by a commercially available AI model and by one or two radiologists, depending on the risk score on a scale of 1 to 10 that the AI assigned them in an initial screening. The other half had their mammograms assessed by two radiologists, the “standard” in Europe, according to the authors.
The AI model also supplied radiologists with information from the initial screening de-
Improving the rates at which breast cancers are caught is crucial because early-stage breast cancers are increasingly treatable.
The disease killed at least 685,000 women worldwide in 2020, according to the WHO. In the United States, the average woman has a 13 percent chance of developing breast cancer in her lifetime - and a roughly 2.5 percent chance of dying of the disease, the American Cancer Society says.
In the study, AI-supported screenings didn’t lead to higher rates of false positives.
The authors didn’t measure the time it took radiologists to do the readings, but assuming a rate of about 50 readings per hour per radiologist, they calculated that it would have taken one radiologist 4 to 6 months less to read the mammograms in the AI test group compared to the mammograms in the standard screening group.
James O’Connor, a professor of radiology at the Institute of Cancer Research in London, said that integrating AI into breast cancer screenings could have a huge impact on the day-to-day work of people in his field.
If AI-supported screenings could be implemented “across different jurisdictions [and] populations,” and be “accepted by patients and by regulators as well as health-care professionals, then this does have the potential to save a lot of time, and this could help with shortages in workflow,” he said. But questions remain around implementation, he said, particularly because countries have different regu-
lations regarding AI diagnostics, and some patients may not agree to the use of AI in the course of their medical care.
James O’Connor said the idea that artificial intelligence would ever replace radiologists is “nonsense.” In the hospital where he works, as well as many others around the world, there is a shortage of experienced radiologists and an increasing pile of scans to be read. Instead, he says that the right AI model, if well-implemented, could help radiologists focus on tougher cases to diagnose and on other types of scans.
“Usually, if you can replace something with AI, it was probably not the best use of human time anyway,” he said.
Kristina Lang, the lead author of the study, said in a news release that the interim safety results are “promising” but “not enough on their own to confirm that AI is ready to be implemented in mammography screening.”
One concern arising from the study is that, in detecting more cancers, the AI-supported screening may also over-diagnose or catch cancers that represent a low risk to patients.
In the study, screenings done with the help of AI detected more “in situ” cancers - cancerous cells that haven’t yet spread and may turn out to be low-grade. As the authors point out, this could lead patients and doctors to over-treat something that isn’t necessarily a threat - including through mastectomies, or the surgical removal of one or both breasts.
Another limitation of the study is that it did not collect data on the race and ethnicity of patients, so it cannot determine if the AI-supported screenings are better at identifying cancers in particular groups over others.
“Breast cancer can present slightly differently in [different] ethnicities and at different ages so validation in more countries will be vital,” wrote the NCTO’s Robert O’Connor.
e at Pete’s Sweets are excited to bring back our cupcake decorating event. The “Pink Party” will be Friday, Oct. 20, 2023 at Pete’s Sweets in East Longmeadow. 20+ breast cancer survivors and family members, as well as Pete’s staff, will help decorate 500+ pink cupcakes that will be given out in the Pink Hope Survivors’ Lounge at this year's 30th annual Rays of Hope – Walk & Run Toward the Cure of Breast Cancer. Supplies have been donated by other local businesses including: Arnold's Meats, Center Square Grill, Pip Printing, Party World, And Many More. This will be our 5th "Batch" of donated cupcakes to the Rays of Hope event. This will be our first "Pink Party" since before covid and we are so happy to have our friends back in the kitchen to help with this incredible event. This is our way to give back to the community in the sweetest way we know how.









 By L indsey B ever
By L indsey B ever
The Washington Post
Most cancers in the United States are found in people age 65 and older, but a new study shows a concerning trend: Cancer among younger Americans, particularly women, is on the rise, with gastrointestinal, endocrine and breast cancers climbing at the fastest rates.
A study published in JAMA Network Open showed that while cancers among older adults have declined, cancers among people younger than 50 have increased slightly overall, with the largest increases among those age 30 to 39.
“This is a population that has had less focus in cancer research and their numbers are getting bigger, so it’s important to do more research to understand why this is happening,” said Paul Oberstein, director of the Gastrointestinal Medical Oncology Program at NYU Langone’s Perlmutter Cancer Center, who was not involved in the study.
If some younger people have an increased risk of cancer, as
they age, the concern is that their cancer risk may propagate, Oberstein said. “If we don’t understand what’s causing this risk and we can’t do something to change it, we’re afraid that as time goes on, it’s going to become a bigger and bigger challenge.”
There is not a clear explanation why cancer is rising among younger people, but experts say there are several possible reasons behind the trend, including rising obesity rates and lifestyle factors such as drinking alcohol, smoking, poor sleep and being sedentary. Environmental factors, including exposure to pollutants and carcinogenic chemicals, also likely play a role.
The researchers analyzed data from more than 560,000 patients in the United States diagnosed between 2010 and 2019 with early-onset cancerdefined as cancers that affected people younger than 50.
They found that, overall, early-onset cancer diagnoses rose by nearly 1 percent during the study period to 56,468 patients, up from 56,051 patients in 2010. The trend was most pronounced




in the 30 to 39 age group, with cases increasing about 19 percent.
There were significant increases in certain types of cancer. Breast cancer, for instance, accounted for the highest number of cancer cases in younger people, and increased about 8 percent over the 10-year period, said Daniel Huang, assistant professor at the National University of Singapore and a transplant hepatologist at the National University Hospital, who is the senior author of the study.
Gastrointestinal cancers, including the colon, appendix and bile duct, were fewer in number but increased about 15 percent during that timemaking it the fastest-growing type of cancer among younger people, he said.
The differences between men and women were striking. The number of early-onset cancers in women increased by 4.4 percent during the study period; among men






the number declined by nearly 5 percent. The increases seen among younger women were likely driven by the rise in cancers of the breast and uterus.
Although the total numbers were small, the biggest increases in cancer among younger people by race were seen in Asian or Pacific Islanders (32 percent) and Hispanic patients (28 percent). Cases among younger Black patients slightly declined, falling by about 5 percent. It’s not clear if the decline is meaningful or if cases are underdiagnosed.
Overall, younger people diagnosed with cancer still represent a relatively small portion of overall cancer cases, but the increases are nonetheless concerning.
“It’s an important trend, especially important if it continues, but it is a small part of what’s going on in oncology,” said Otis Brawley, an oncologist at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins. The study did not examine cancer stages, so it’s unclear from the data whether the early-onset cancers developed earlier or were simply
being diagnosed earlier in the course of the disease, experts explained.
Most cancer risk factors are based on studies of predominantly older adults, but studies are being designed to help understand how certain exposures in earlier life may impact cancer risk in later life, said Hyuna Sung, senior principal scientist and cancer epidemiologist at the American Cancer Society.
Studies such as the one in JAMA, she said, “motivate new studies to help identify risk factors that may be able to explain these trends.”
Other research has shown a trend toward younger diagnosis in colorectal cancer. One in five new cases of colorectal cancer in the United States occur in people younger than 55 - a rate that has about doubled over the past three decades, according to a concerning recent report from the American Cancer Society. In 2018, the American
Cancer Society updated its colorectal cancer screening guidelines, lowering the age to start screening for those at average risk from age 50 to 45.
Experts say trends such as those seen in the new study should be closely monitored as they may influence other screening recommendations, including those for breast cancer.
“As we continue to do better at identifying people who are at higher risk at younger ages, we really need to adjust our screening practices as well,” said Jennifer Litton, a breast medical oncologist at the University of Texas MD Anderson Cancer Center.
An estimated 1.9 million new cancer cases are diagnosed each year in the United States. In some cases, there are no screening tests for certain cancers, and when there are, the tests are often not recommended for young people who are at average risk.
One of the most important things people can do to minimize their risk, Brawley said, is to manage body weight, exercise, limit alcohol consumption and avoid smoking.













Individuals can experience a whirlwind of emotion upon being diagnosed with cancer.
No one ever expects to receive such a diagnosis, so the moment a physician delivers such news can be emotional and compromise a person’s ability to focus. Once those emotions settle down and individuals resolve to overcome the disease, they typically have a lot of questions.
One of the questions doctors will attempt to answer is which subtype of cancer a person has. For example, when doctors initially deliver a breast cancer diagnosis, they may explain that further testing will be necessary to determine precisely which type of breast cancer an individual has. Identifying the subtype of breast cancer helps doctors choose the most effective course of treatment, but it’s understandable if patients and their families become confused during the process.
The following rundown can help breast cancer patients understand this crucial next step after diagnosis.
The American Cancer Society notes that breast cancer type is determined by the specific cells in the breast that become cancer. The Mayo Clinic reports that a medical team will use a tissue sample from a patient’s breast biopsy or, for patients who have already undergone surgery, the tumor to identify the cancer type.
What are the types of breast cancer I might be diagnosed with?
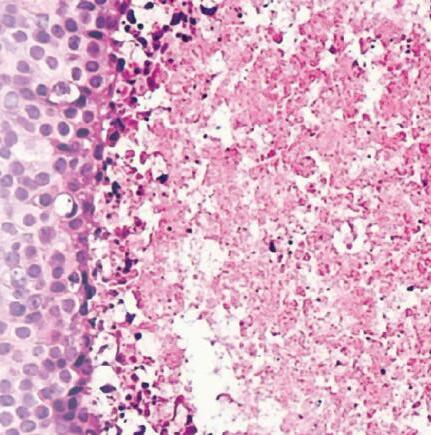
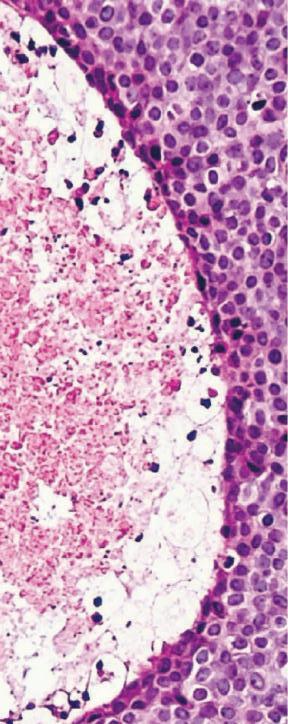
There are many types of breast cancer, but some are more common than others. Invasive and non-invasive (also referred to as Carcinoma in situ) are the two main subtypes of breast cancer.
According to the University of Pittsburgh Medical Center, the most common types of invasive breast cancer are invasive ductal carcinoma, which affects the inner lining of the milk ducts, and invasive


lobular carcinoma, which originates from the glands that produce milk.
The UPMC reports that the most common in situ types are ductal carcinoma in situ, which is cancer that remains within the milk ducts, and lobular carcinoma in situ, which does not often develop into breast cancer though it is considered a risk factor for an invasive form of the disease.

The ACS notes that triple-negative breast cancer is an aggressive form of breast cancer that accounts for roughly 15 percent of all breast cancers. Triple-negative breast cancer can be difficult to treat.


Less common types of breast cancer, each of which account for between 1 and 3 percent of diagnoses in a given year, include Paget disease of the breast, angiosarcoma and phyllodes tumor.
A breast cancer diagnosis marks the beginning of a sometimes lengthy but often successful journey that has ended in full recovery for millions of women across the globe. More information about the various types of breast cancer can be found at cancer.org.


















