

Welcome to the Climate Change edition of INSPIRE
This issue of INSPIRE is dedicated to looking at innovation in the health and medical research arena with respect to our changing climate.
We understand that there are a range of opinions on climate change that vary widely across different individuals, groups, and societies. We also know that there are a range of truly innovative and interesting health and medical research studies being undertaken. Even though these articles come from various institutions, and they tackle a wide range of themes, they have a few important factors in common. All these articles express an urgency to deal with an important issue that the authors are seeing and facing on a regular basis.
There are also concerns raised about the impact of economics, equity and justice for the individuals and communities who are facing these climate challenges and do not have the resources to adequately face, yet alone manage these issues.
There is, however, an optimism that runs through the articles. That by accepting the challenges we face, taking responsibility and using the technological tools at our disposal, we can find solutions for the current and future problems associated with climate change.
We believe that addressing the impacts of our changing climate requires interdisciplinary approaches that integrate health and medical research with public health, environmental science, government policy, and community engagement. Strategies include mitigating greenhouse gas emissions, adapting healthcare infrastructure and services to climate-related risks, enhancing surveillance and early warning systems for climate-related health threats, promoting sustainable development and resilience-building measures, and prioritising equity and social justice in climate action.
Yes, it’s a lot! In this issue of INSPIRE our members share their strategies and actions, from across the health and medical spectrum. HMRI, University of Queensland and The Telethon Kids Institute are just some of the members that discuss respiratory diseases and our changing climate.
Read about how the ANU and Bond University are tackling the impact on regional healthcare systems and
doctor numbers due to extreme weather events and our hotter climate. One of our new members, the National Centre for Farmer Health discuss that heat kills more Australian than other natural disasters! The University of Queensland examines the impact of mental health of Australians affected by climate change.
Be inspired by the initiatives outlined by Central Queensland University who discuss trauma informed disaster resilience approaches. The University of Technology and Western Sydney University discuss advances in healthy homes and finding natural and effective urban air conditioners.
And read about our first University Roundtable for 2024, and meet three new members who have joined the strong and active Research Australia alliance. In the Last Word hear from new NHMRC CEO, Professor Steve Wesselingh, who shares his views on combining “innovation, collaboration, and a steadfast commitment to public health” to “not only heal but also safeguard our planet for generations”.
We thank all our members for generously in sharing their awe “INSPIRE-ing” work with us. While we may come to the question of climate change with different opinions, we can all agree that work being undertaken in the health and medical research sector is pivotal to help us understand and tackle the changing of our climate. We hope that you enjoy reading this edition of INSPIRE.
Best wishes
Nadia and your Research Australi a Team
















Publisher Research Australia Ltd
Art Direction
Matthew Ware p +61 403 844 763 e matt@objktive.com
For Advertising enquiries please contact the Research Australia office on p 02 9295 8546 or e admin@researchaustralia.org researchaustralia.org
INSPIRE ONLINE issuu.com/researchaustralia
INSPIRE is a publication of Research Australia Ltd ABN 28 095 324 379 384 Victoria Street Darlinghurst NSW 2010
Who can submit articles?
Any current member of Research Australia who would like to share a relevant story that affects their organisation including, philanthropic donations and their outcomes, research findings, and any other related health and medical research topic that affects the Australian population.
Submission guidelines & deadlines
For information regarding how to submit and publishing deadlines visit the Research Australia website
Disclaimer
The opinions expressed in INSPIRE do not necessarily represent the views of Research Australia. Whilst every effort has been made to ensure accuracy, no responsibility can be accepted by Research Australia for omissions, typographical or inaccuracies that may have taken place after publication. All rights reserved.
The editorial material published in INSPIRE is copyright. No part of the editorial contents may be reproduced or copied in any form without the prior permission from Research Australia. © Research Australia 2020.
 My Twitter : @chriskere CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
My Twitter : @chriskere CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
Australian Health & Medical Research & Innovation

38 Changing the Climate: Addressing the Social, Economic and Cultural Factors Undermining Planetary Health

56 Reef research leads to new insights on climate change and wellbeing

58 Addressing the challenges of

40 Could climate-related exposures contribute to prolonged pregnancy?

48 Safeguarding children’s health in Australia amidst climate change TELETHON KIDS INSTITUTE

Children are disproportionately affected by sepsis: IT can help



Planetary Health education is about enabling students to take action 42
Nitrous Oxide leaks in hospitals – finding and fixing carbon hotspots in healthcare
HOSPITAL WESTMEAD

Providing evidence to guide public health messages during bushfires



Mood tracking study to help plan for mental health support


Understanding the impact of bushfires on people with asthma

Mitigating the mental health impacts of climate change

Setting
EVENTS OVERVIEW ROUNDTABLE ROUND UP
The Research Australia University Roundtable on 27 March was hosted by La Trobe University and was chaired by Professor Russell Gruen, Dean of the ANU College of Health and Medicine and Research Australia Director. It was attended by 40 representatives from 26 universities. 14 attended in person.
The day commenced with a tour of the La Trobe Institute for Molecular Science . LIMS brings multiple disciplines and research areas together in the one facility for teaching and research, with the aim of promoting collaboration. It contains research groups in life sciences, physical sciences, and applied sciences, and teaches undergraduate and graduate courses. The tour was led by Professor Patrick Humber, the Institute’s Director.
This was followed by a tour of the new Digital Innovation Hub at La Trobe University, with its Manager, Jeff Jones, and attendees were provided with the opportunity
to experience the virtual holographic virtual medical consultation under development at the DIH and an introduction to the DIH AI Catalyst.
After a networking lunch, Roundtable participants were welcomed by the Roundtable’s Chair, Professor Russell Gruen, Research Australia CEO, Nadia Levin and Professor Susan Dodds, La Trobe University’s Senior Deputy Vice-Chancellor and Vice-President (Research and Industry Engagement).
Greg Mullins, Head of Policy, gave a policy update, highlighting some of the initiatives currently under way.
Ahead of the report’s imminent public release, Associate Professor Darshini Ayton and Dr George Taiaroa provided the Roundtable with a preview of the findings of the national survey of Early and Mid-Career Academics in health and medical research. The report provides unique insights into the challenges facing EMCAs in our universities as well as some of the opportunities to better support them and advance their careers. The report is available here.



Professor Meg Morris provided a presentation on Latrobe University’s Academic and Research Collaborative in Health , with assistance from Professor Katherine Harding. Working with eight industry partners and across more than 90 individual healthcare sites, the ARCH brings together academics, health professionals, consumers, clinician researchers, students, health and social care agencies and policy makers skilled in the translation of interdisciplinary, consumer led, and industry focused research. Meg and Katherine gave several examples of the programs and interactions ARCH has with its partners across teaching research training and research, and explained that engagement with industry partners and public involvement underpins ARCH’s success.
It was a very stimulating and informative day, with very complimentary feedback from all participants.
The next Roundtable will be held on 29 May at the Australian National University.
On 14 August the Roundtable will be hosted by University of Western Australia; the first time a Roundtable will be held in WA. Flinders University will host the Roundtable on 20 November.




 CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
LIVING IN A HOT BOX
Sub-standard housing combines with energy insecurity to produce dangerously hot and often overcrowded living conditions in remote Northern Territory communities. Climate change is set to amplify this problem unless we act now.

People often ask Dr Simon Quilty * why he turned from medicine to housing to advocate Indigenous Australian health and wellbeing.
“I tell them it’s because housing drives health and social inequality,” says Quilty, “with climate change exacerbating every element of this inequality.”
Quilty has worked as a specialist physician in the Northern Territory for the last decade and has seen firsthand the impact that changing climate can have on health.
“Summers are no longer what they used to be here in the Northern Territory. They are incredibly hot and prolonged –everyone is very worried about the weather and its impact on community wellbeing.”
Illness during hot weather spikes. Research by Quilty and colleagues show remote communities in the Northern Territory experience higher rates of soft tissue infections, scabies, streptococcus, and staphylococcus during hotter months. They also found a statistically significant relationship between obstetric emergencies requiring retrieval services, as well negative maternal, foetal, and neonatal outcomes associated with prolonged exposure to very hot temperatures.
But the root of this problem extends beyond ongoing climate shock.
“I could walk you through Tennant Creek and you will be left with no doubt about what the issue is: housing,” says Quilty.

“The houses being built by the Northern Territory Government are appalling. There are no outdoor living spaces, they are not ventilated, and many of the older houses have little or no insulation. During hot weather these houses are as hot or hotter on the inside than on the outside if you don’t have the air conditioning on.”
This second-rate housing combined with power outages is a recipe for disaster according to Quilty. Energy insecurity is rife in outback communities – most houses are on prepaid power cards, and when credit runs out and air conditioners turn off, the houses are thermally unsafe for people.
Research by Quilty and co-author Indigenous Elder
Norman Frank found that nine out of ten homes in remote Northern Territory lost power in 2018, with seven out of ten disconnected more than ten times. When these homes are disconnected, families are forced to escape the heat by crowding into homes that still have power and thus air conditioning.
“You can have 20 or 30 people in a single dwelling, and these crowded conditions a breeding ground for disease manifestation. Streptococcus thrives and is the perfect conditions for rheumatic heart disease, for example.”
Without any substantial changes to housing policies to make them well-suited to local climate – and climate change, these problems will be amplified in the future.
Indeed, temperatures are set to rise further according to a report commissioned by the Northern Territory Government. By the middle of this century the number of days over 35°C will at least double in many places, and the number of days over 40°C will also increase considerably.
“We have healthcare professionals running public health campaigns about how to stay safe during heatwaves – but these people have got nowhere to go! Where are health professionals advocating for better housing?” says Quilty.
The solutions must start with designing and building houses that meet the minimum national standard of seven-star energy efficiency – which they currently do not.
Adopting solar photovoltaic (PV) in places like Tennant Creek, with over 200 sun days per year, is another obvious solution. Work by Quilty and colleagues shows
Indigenous Elder Norman Frank holding a model of a proposed Wilya Janta home, with Serena Morton, and Nicole Frank.
Photo: Simon Quilty.

that accessing solar PV significantly reduces household electricity expenditures. Furthermore, it reduces the frequency and duration of involuntary disconnection events.
Their preliminary analysis indicates that solar PV systems with an expected lifetime of up to 25 years on panels, and costing approximately $10,000, has a payback period of a little over seven years. However, bureaucratic barriers are curtailing the installation of solar PV.
“When Original Power first asked to put solar on Indigenous public housing they were told by bureaucrats it could not be presumed that remote houses had structurally sound roofs. We had to get in engineers, and then it took almost six months once the panels were installed for systems to be switched on. Housing even made Norman sign a waiver of responsibility for removing the panels if he vacated the property!”

With communities feeling forgotten by the Government on this issue, residents of Tennant Creek are championing a new collaboration that hopes to future proof their homes against climate change. Wilya Janta (‘standing strong’) plan to build culturally appropriate houses that can cope with dangerous summer heat. These houses will be solar-powered, wellinsulated, have shaded outdoor areas, and be water efficient.
As the climate crisis deepens, “there’s a lot of ecosystems that we cannot protect,” says Quilty.
“But we can protect human health by investing in houses that are highly thermally performing and resilient to climate shock.”
 Dr Simon Quilty
Dr Simon Quilty
Authors: Liz Drummond, Australian National University. Dr Simon Quilty has over 20 years’ experience in remote medicine and is currently undertaking a PhD at the Australian National University examining the relationship between environmental heat and wellbeing in the Northern Territory.
FINDING SHELTER IN THE STORM

The climate crisis, extreme weather resilience and people experiencing homelessness
As the climate crisis intensifies extreme weather events, the homeless community is increasingly at risk.
Their vulnerability to climate change is a combination of the physical impacts of extreme weather, and the social, economic, political, institutional, and technological inequalities which unevenly distribute these physical impacts (Every and Thompson, 2014; O’Brien et al., 2011).
People experiencing homelessness have developed skills for hot and cold weather. However, their adaptation conceals a myriad of hardships, including isolation (walking to services becomes impossible with a 20 kg backpack in the heat), mosquito bites from sleeping outdoors, food that spoils and losing medication because it cannot be kept cool or dry (Cusack et al., 2013; VCOSS 2016). For those who have been through extreme weather and disasters:
• 39 per cent of people lost their home (tents, temporary structures, safe sleeping spaces)
• 37 per cent experienced worsening or new mental health issues and of these, 30 per cent experienced trauma
For 16 per cent of people, an extreme weather event is a factor in their pathway to homelessness (Every and Richardson, 2018).
People experiencing homelessness are not well prepared physically or emotionally for protecting themselves from the economic, social and health effects of climate
change. They face significant challenges, particularly social isolation, mental health issues and limited funds to purchase emergency supplies (Every, Richardson & Osborn 2019; Edgington 2009).
A multi-level approach of government, services and community actions is required to build resilience for people who are homeless.
GOVERNMENT-LEVEL INTERVENTIONS
Homelessness services are already unable to meet demand (SCRGSP, 2024). This pressure on services is significantly worsened by disasters and extreme weather. It costs services up to $5,000 to respond to discrete weather events (like heatwaves or storms) and over $20,000 to assist people in more extensive weather events (floods and bushfires) (Every and Richardson, 2018).
As part of building resilience to climate change, government-level interventions are required. These include:
• accessible and affordable public housing which meets best practice climate adaptation standards
• thermal quality improvements in public housing
• reducing the cost of electricity to make running fridges, fans and air-conditioning affordable for everyone
• appropriately funding homelessness services to support service users before, during and after extreme weather
• publicly-funded mental health care for everyone.
(Edgington, 2009; Hanson-Easey, et al., 2017; Every, et al., 2018).
COMMUNITY-LEVEL INTERVENTIONS
As well as providing funding, housing and health care for people living in poverty, education about extreme weather and how to cope helps to improve resilience (Osborn et

al., 2019). Using trauma-informed principles (Mental Health Coordinating Council 2017; National Health Coalition to End Homelessness 2017; OASPR, 2012), together with survey and interview data from Australian homeless service providers and people with a lived experience of homelessness, Every and Richardson (2018) developed Trauma-Informed Climate Resilience Education principles to guide education programs.
Table 1: Trauma-Informed Climate Resilience Education principles and implementation.
Principles Implementation
Build safe relationships Employ trusted people, including peers with a lived experience of homelessness, to deliver extreme weather information.
Build relationships with emergency services organisations.
Co-create, collaborate and partner Resources reflect the shared knowledge of the homeless community and emergency services organisations.
Strengths-based Activities that assist people to identify, develop and use skills and knowledge to respond appropriately during extreme weather events.
Empowerment Develop plans and improve skills in relation to specific needs and specific hazards including knowledge of first aid.
Provide essential material resources Distribute weather-protection items via emergency kits like beanies, water bottles, sunscreen, mosquito repellent and tarpaulins to address the ongoing effects of poverty on people’s ability to respond safely.
Be inclusive, nondiscriminatory and non-judgmental
Acknowledge and respond to gender, age, sexuality, ethnicity, literacy standards and living circumstances that influence people’s ability to prepare, respond and recover from extreme events.

FROM RESILIENCE PRINCIPLES TO RESILIENCE PRACTICE
Out of the Storm was a community-led program which implemented this trauma-informed approach in Adelaide, South Australia. Homeless service users, emergency services, health providers and volunteer graphic designers co-designed posters, a city services map and emergency kits that reflected the needs of people experiencing homelessness in a changing climate. The program then employed people with a lived experience of homelessness as outreach workers. The team delivered 278 of these emergency kits and maps and had 466 conversations about extreme weather with other people in experiencing homelessness (Every, Pedler, Collyer-Braham, 2020).

The climate resilience education principles and their implementation in the Out of the Storm program outlined here not only enhanced disaster risk knowledge, but also addressed the exclusion, isolation and disempowerment experienced by people who are homeless. Together with desperately needed government-level interventions for funding, housing and health care, these community-level approaches can better protect vulnerable people. Additional References are available upon request.

Author: Dr Danielle Every is a senior lecturer at the Appleton Institute, Central Queensland University. Her research explores community experiences of bushfires, climate change and disasters, particularly with people experiencing homelessness.
THE VOICES AND THE HANDS
Indigenous leadership working with nonIndigenous allies on climate change and health

Aresearch team of Aboriginal, Torres Strait Islander and non-Indigenous scholars was asked to provide specialised advice on what the Australian Government can do to recognise and prioritise Aboriginal and Torres Strait Islander Peoples’ voices in future Intergovernmental Panel on Climate Change (IPCC) reports. In response, they went above and beyond to capture those voices.
When Dr Vinnitta Mosby, from the Meriam Nation in the Torres Strait Islands, joined the majority Indigenous team to inform the Australian Government on climate change research, she knew that the only way to do this appropriately was to be on Country in discussion with her community members.
“They want their voices heard rather than being collected in numbers. They say – we want proper talking; come and see what’s happening to us,” Dr Mosby reflected. In response, face-to-face conversation-based yarning approaches were undertaken whenever possible and ensured adequate time for gathering responses, knowing that some respondents also needed to seek permissions

from relevant community Elders to share Knowledge and data. Because, for far too long, information shared with outsiders was either misconstrued or mismanaged. This response contrasted with a tendency for ‘Western tick and flick’ quantitative survey methods.
INDIGENOUS KNOWLEDGE BRINGS HIGH VALUE CLIMATE CHANGE INFORMATION
Climate change is having, and will continue to have, a significant impact on the Country, culture, and health of Aboriginal and Torres Strait Islander Peoples. Experiences of climatic change over 65,000 years provide valuable and very diverse knowledge. These experiences are based on many years monitoring changes through locally specific

indicators, that require place-based mitigation and adaptation options for Australia.
Many communities living on Country are in areas exposed to extreme and changing climatic conditions, with threats to human, economic, cultural and social wellbeing exacerbated by climate change. Increasingly frequent and severe cyclones, rising sea levels, and extended heatwaves are just a few examples. These climatic conditions multiply existing vulnerabilities due to social disadvantage and the legacy of colonialisation. This ‘invisibility’ in government and Western-focused documentation persists through the follow-on consideration of priority areas and populations to which climate change policies, funding and monitoring are tailored.
LEADING GLOBAL BODY ON CLIMATE CHANGE HAS NEGLECTED INDIGENOUS VOICES
It was not until the fourth Intergovernmental Panel on Climate Change (IPCC) report in 2007 that the value of Indigenous Knowledges on responding to climate change was considered. However, although inclusion of Indigenous Knowledges within IPCC reports has increased over time, the latest report (AR6, 2022) did not include any Indigenous Lead Authors in the Australian chapter.
Indigenous scholars were invited to participate in the IPCC drafting and assessment process for the Australasian chapter as Contributing Authors but were not nominated by the Government, nor invited by the IPCC Bureau. Consequently, they did not have the same level of access to, or authority over, the whole chapter or report as the Lead Authors. The IPCC voices were not Indigenous voices.
WINDS OF CHANGE TOWARDS IPCC AR7
Multiple suggestions were made for inclusion of Aboriginal and Torres Strait Islander scholars and Knowledge holders in the IPCC. In response, the Australian Government commissioned advice ahead of the Assessment Report 7 planning that commenced in mid-2023.
The resulting research team of Aboriginal, Torres Strait Islander and non-Indigenous scholars (who were IPCC Lead Authors) were asked to provide specialised advice on what the Australian Government can do to recognise and prioritise Aboriginal and Torres Strait Islander Peoples’ voices in subsequent IPCC reports.
THE RIGHT PEOPLE TRUSTED FOR THE RIGHT TASK
The research team knew that their trust and access with potential respondents was likely to yield higher response rates and more detailed data. However, this is an engagement process that requires a mutual exchange from both parties, including anticipated engagement into the future.
Such responsibility was described by research team member, Adjunct Professor Sandra Creamer AM (Waanyi Kalkadoon), who said:
“Hear from the real and authentic voices. These ‘invisible people’ can be hard to access and the Government cannot reach them. But trusted Aboriginal people can reach them through their networks. Through having Indigenous peoples like us we are getting the right conversations, concerns and solutions that the government would not get otherwise. This is how effective consultation works.”

THE ‘PROMISE’ OF CONSULTATION ON CLIMATE CHANGE: THE START OF ENGAGEMENT
All research team members, especially Indigenous researchers, were committed to deliver on the promise of genuine consultation. As Adjunct Professor Creamer said:
“Our reputation is on the line. We are asking for survey responses, but this brings in cultural obligations, reciprocity and responsibilities.”
In response, a commitment to implementing actions following the research should be made. This was described by the team’s Associate Professor Bradley Moggridge (Kamilaroi), who reminded the Government:
It is important for Voices to be heard, but when does the action come back to the community?”
This call for a voice on climate change decisions came through in a powerful response from many Aboriginal respondents to the research team’s survey. Their direct words were considered by the team to highlight the extent of the challenge to be heard, and the experience, Knowledge, and human right to lead on climate action:
“There is limited recognition regarding Aboriginal and Torres Strait Islander Peoples other than relegating us to ‘vulnerable communities’ in the context of climate change. This disregards our over-65,000 years of sustainable practices and customary knowledge of the natural environment and thus our significant contribution to policy. Our People need a voice”.
Authors: Associate Professor Nina Lansbury (The University of Queensland), Dr Vinnitta Mosby (Meriam Nation, James Cook University), Adjunct Professor Sandra Creamer AM (Waanyi Kalkadoon, The University of Queensland), Professor Bradley Moggridge (Kamilaroi, University of Canberra), Lillian Ireland (Melukerdee), Professor Gretta Pecl (University of Tasmania) and Dr Geoff Evans (The University of Queensland)

IMPACTS OF CLIMATE CHANGE AND EXTREME WEATHER EVENTS ON HEALTH AND HEALTHCARE IN AUSTRALIAN COMMUNITIES AND BEYOND
Australia is vulnerable to a changing climate.
Snapshot taken by Dr Kazi Rahman from the Bureau of Meteorology website warning page just before the start of the storm on the evening 25 Dec 2023
One manifestation is extreme weather events which appear to be increasing in frequency and intensity, not only causing considerable infrastructural damage but also physical harm and emotional trauma.
On top of that, the ecosystem is changing which is resulting in additional direct and indirect impacts on health and healthcare. It is thus important to explore and measure the burden of the health impacts from climate change, particularly extreme weather events so that appropriate measures can be taken to support those affected and response measures can be planned and implemented in future events.
Under the umbrella of Planetary Health, Bond University Faculty of Health Sciences and Medicine (FHSM) is conducting research on the effects of climate change, particularly through extreme weather events on health and healthcare. The focus is both on Australian settings and communities and beyond, in the global context. Our research includes investigations through MD research projects and Healthcare Innovations program Capstone Projects.
We are currently developing research on the impacts of the 2023 Christmas night tornado like storm (see image –a snapshot taken by Dr Kazi Rahman from the Bureau of Meteorology website warning page just before the start of the storm on 25 Dec 2023 evening) on the physical and mental health and wellbeing of the Gold Coast residents. This exploration involves the public, particularly those who were impacted by the storm, and patients with chronic health conditions (e.g. kidney diseases) needing uninterrupted access to healthcare. This is important collaborative research led by us, a group of academics, clinicians and researchers at the FHSM at Bond University. We are also involving MD students and students from the Master of Healthcare Innovations program. We hope that the findings from the study will have useful programmatic implications and recommendations for the ongoing healthcare service delivery. The study will also feed into future research including quantitative estimation of the burden of the health problems at the population level.
A member of our Planetary Health research team at Bond University, Dr Kazi Rahman, has ongoing collaborative research on climate change and extreme weather events on health including vector-borne diseases in Australia, particularly in New South Wales (NSW) and North Queensland, and in other developing country settings in South-East Asia . Dr Rahman closely works with the industry, especially the Government agencies and programs evaluating the impact of climate change on health and health services in Australia. The recent extreme weather events, especially the floods, have resulted in significant impacts on the mental health and wellbeing of



the affected communities. The magnitude of this impact has been demonstrated in the investigations in Lismore, NSW, one of the most flood affected cities in Australia. Moreover, research on bushfires, air pollution and heath protection messaging in the affected communities, especially focusing on the North Coast of NSW which was affected significantly in 2019-20 bushfires has been ongoing involving primary data collection. A review on the topic has also been conducted and published. Finally, our researchers are investigating impacts of extreme weather events on One Health, which encompasses human health, animal health and the ecosystem. Identifying the interfaces of these three domains for a particular health issue and designing suitable interventions targeting them is crucial. Overall, the Planetary Health team at Bond University is multi-disciplinary, spanning across different programs and disciplines. We focus on various aspects of health impacted by the changing climate involving multiple research methods. We are conducting research to generate evidence as well as to support the implementation of the ongoing programs in Australia and in other country settings in the region. We have integrated Planetary Health research and education in our curriculum in different disciplines including Medicine and Healthcare Innovations within the Faculty of Health Sciences and Medicine at Bond University.
Author: Lead Researcher: Dr Kazi Rahman is an Associate Professor of Healthcare Innovations at the Faculty of Health Sciences and Medicine, Bond University, Gold Coast. Being a medical doctor he has post-graduate training in epidemiology and population health and has extensive research and teaching experience in epidemiology, with a particular focus on environmental determinants of health.
Co-researchers: Dr Thomas Titus is a Consultant Nephrologist with a strong focus on research and educations. He is an Associate Professor at the Faculty of Health Sciences and Medicine at Bond University. Professor Michelle McLean is a medical educator who has overseen the integration of Planetary Health in the Bond University medical curriculum.

SAFEGUARDING AT-RISK COMMUNITIES


Advancing heat-health warning systems for enhanced protection and resilience through a trans-disciplinary research approach.

Effective climate action demands research processes that Invite consumer engagement, embrace policy makers as partners, and integrate transdisciplinary values.
By embodying such processes, our Wellcome funded Ethos project (Extreme Heat and Older Persons) strives to develop and evaluate a heat-health early warning system that can overcome the limitations of existing populationbased early warning systems.
Heatwaves are recognised as the deadliest1 of all natural disasters in Australia. Their impact on increased mortality and morbidity, particularly for at-risk populations such as older persons or those living with multi-morbidities, translate to increased pressure on the healthcare system. Indeed, higher numbers of emergency department visits, hospital admissions, and ambulance callouts occur during heatwaves, with a meta-analysis of Australian research indicating a 10% increase in ambulance callouts on heatwave days compared to non-heatwave days2 .
Government and policy makers around the country have been working on increasing awareness of heatwaves, by implementing a nationally consistent warning system framework distributed via the Bureau of Meteorology (BOM). Associated heat-health messaging regarding risk and actions are delivered alongside this to communities across jurisdictions.
Though implementing these population-based, homogeneous systems fill an important void, their efficacy is limited by their inability to address personal heat-health threats, leaving some of our most at-risk populations (e.g., older persons), particularly vulnerable via their exposure to hot living conditions. Further, these systems make broad recommendations for cooling that are not always accessible, affordable, or acceptable to such populations3,4
Our research applies the well-established early warning systems framework 5 used in disaster management to protect older persons at home from extreme heat. We have worked with older adults as research affiliates and developed an in-home heat-health warning system that overcomes some of the common limitations of a population-based system by: a) measuring real-time inhome temperature and humidity, b) estimating personal

heat-health risk using available laboratory-based evidence and individual characteristics, and c) generating risk alerts and making cooling suggestions that are evidence based6 , and tailored to the individual’s access and acceptance (Figure 1).
By purposefully engaging with policy makers across the health and care sectors from its commencement, our project is exploring ways for this system to be embedded into in-home care systems targeting the most vulnerable, alongside its utility for other at-risk populations and further exploring its feasibility in low-middle income countries.
Using a trans-disciplinary approach underpinned by codesign principles, our ‘Extreme Heat and Older Persons’ (Ethos) project assists older persons through smart technology to remain at home safely and independently as extreme heat events increase in duration, intensity, and frequency7
Our research team is structured across three key themes - care systems and user experience, technology development, and extreme heat preparedness. Our extended team includes expertise spanning environmental health, epidemiology, nursing, thermophysiology, social work, gerontology, human-computer interaction, software development, environmental science, architecture, public health, health communication, and data science.
Our research processes and design relating to capacity development, co-leadership, transdisciplinary values, purposeful and structured user and policymaker engagement throughout the project’s lifecycle have attracted large funding by Wellcome; a valuesbased granting body promoting equity, environmental sustainability, and science-policy translation in their research programs.
Following Pineo et al’s transdisciplinary framework8, our project has progressed through the development and conceptualisation phases. In these phases the focus was developing a shared understanding of transdisciplinary, building the program logic and clear goals and indicators
of success, developing team processes including coleadership and team capacity development requirements, learning about each other’s disciplinary frames and evidence needs and building and engaging partnerships with users and stakeholders.
In addition, these early phases focused on developing a solid understanding of the multiple dimensions of the problem, identifying physical requirements for the early warning system, increasing heat-health awareness in older persons through the development of a series of short, animated videos 9 and utilising evidence to inform our system’s risk model, design, and implementation strategy.
This evidence was drawn from literature review, a statewide survey of older Queenslanders, group discussions involving a diverse group of stakeholders using the World Cafe method and ongoing engagement with our research affiliates (older adults and carers) whose community knowledge and lived experience continue to provide valuable insights into system design and implementation (Figure 1 depicting one of our design meetings with our research affiliates).
Now in the investigation phase, our system was trialled in 85 homes in Southeast Queensland over the summer of 2023-2024 when the region experienced multiple severe heat warnings. This phase 1 trial period provided critical at-home temperature and humidity data, heat-protection behaviour information, cooling preferences and behaviourrelated responses to warning prompts information. This phase also includes a continuation of partnership and user engagement including a focussed analysis of the feasibility of the developed system across a number of domains.
Across these three phases, structured team processes facilitating continuous co-learning and reflection and refinement have helped the team remain aligned to the research project goals while progressing and growing individually as researchers. These will continue as we move to the implementation phase of our research program. References can be supplied upon request
Figure 1: Schema of the Ethos at-home individualised heathealth early warning system




Author: Assoc Prof Shannon Rutherford has extensive experience in climate and health research, with a focus on understanding impact and adaptation processes in local, national and international contexts. Team and co-author acknowledgements: This project is co-led by Dr Aaron Bach and Dr Sebastian Binnewies and this short paper was co-authored by Ms Mehak Oberai. The team acknowledges the large multidisciplinary team involved from its inception (Grant: Rutherford, S., Binnewies, S., Bach, A., Tjondronegoro, Moyle W, Torrisi G, Nghiem S, Phung D, Zhang F, MacQuarrie S, Gabric A. Baker, S (2022) Individualised Heat-Health Early Warning Systems: a novel digital solution. This work was supported by Wellcome (224709/Z/21/Z: ‘Individualised heat-health early warning systems: A novel digital solution’.
Ms Mehak Oberai
FIRE, FLOODS AND INFECTIONS:
BLOOD SUPPLY AND CLIMATE CHANGE





Climate change has many interconnected and complex consequences. The safety of the blood supply is one you may not have thought about.
As the world deals with the worsening effects of climate change, the complex interactions between shifting weather patterns, natural disasters, and infectious diseases are an increasing concern for the blood supply.
For more than 90 years Australian Red Cross Lifeblood (Lifeblood) has collected, processed, and distributed blood and plasma products to hospitals across Australia, ensuring a safe and stable supply for those in need. About 31,000 blood donations a week are needed, and all donations are subject to strict screening procedures to minimise the risk of transmitting infectious agents to patients. However, changing global conditions means that Lifeblood needs to maintain a careful watch on emerging threats to ensure a consistent and safe blood supply.
WHY DOES LIFEBLOOD CARE ABOUT CLIMATE CHANGE?
Although Lifeblood maintains one of the world’s safest blood supplies, some infections may be spread in blood transfusions and new diseases might arise or spread because of a changing climate. This necessitates ongoing vigilant surveillance and risk assessment. Significant natural disasters in Australia, such as floods and bushfires, also threaten blood supply’s safety and sustainability. For example, the recent, devastating 2022 floods caused widespread damage to areas in Queensland and New South Wales. Seven donor centres and mobile units in Queensland were affected, and the Lismore Donor Centre in New South Wales was closed due to flood damage for almost ten months. Floods and road closures lead to challenges in blood collection due to staff and donor accessibility issues.
CHALLENGES TO THE RESILIENCE OF THE BLOOD SUPPLY
Climate change affects the transmission of infectious diseases, such as vector-borne infections (e.g., Japanese encephalitis, dengue fever, West Nile virus). With changes


in climate, the vectors that spread diseases, such as mosquitoes, ticks, and migratory birds, are moving into new and expanded areas around the world. Human and animal behaviours also change in response to a changing environment. Consequently, the prevalence and geographical distribution of infections may change in ways that are hard to predict.
In the wake of escalating natural disasters, such as bushfires and floods, the resilience of the blood supply faces new challenges. Compromised infrastructure and logistical challenges, for example, challenge blood operators to meet the escalating demands amidst crises1.
Moreover, the aftermath of such disasters often catalyses the proliferation of infectious diseases (e.g., Ross River Virus transmission in hot weather after floods), which can reduce the number of healthy people able to donate.
WHAT DO WE DO AT LIFEBLOOD?
Lifeblood has comprehensive strategies to evaluate and mitigate the effects of emerging threats on blood safety where required. Strategies may include diversification of donor recruitment (ethnic groups and demographics), enhanced inventory management, emergency preparedness and responses, climateresilient infrastructure and transportation networks, public education and engagement, continuous monitoring and risk assessment, and a range of research projects investigating the possible impacts of climate change.
“We must continue to focus on being proactive. This means predicting risks, assessing them, and building the capacity to deal with them before they become major issues “said Dr. Viennet
A SUSTAINABLE, RESILIENT BLOOD SUPPLY AND RESEARCH GO HAND TO HAND
The outbreak of Japanese encephalitis (JE) on the Australian mainland in March 2022 is an example of an emerging threat to blood safety. Spread by mosquito species that have fed on infected waterbirds or pigs, the JE virus found new ground as increased rainfall, attributed to La Niña weather patterns since 2020, likely facilitated migratory bird movement between Papua New Guinea and northern Australia. Formerly confined to seasonal transmission in the Torres Strait and Far North


Queensland, the outbreak expanded to Victoria, New South Wales, Queensland, and South Australia, infecting over 80 piggeries and 45 infected cases, resulting, sadly, in seven fatalities since 1 January 20212
A combined response from Lifeblood, public health authorities and researchers in multiple states allowed for the assessment of the ongoing risk from the virus to the blood supply3
Lifeblood conducts a broad range of research studies where our wonderful donors have consented for us to


use data and donated samples to understand the human epidemiology of potential transfusion transmissible infections in Australia and inform a targeted strategy for blood safety4-6
Facing these challenges, predictive modelling and datadriven insights are important tools to ensure the safety of blood supply. Dr. Elvina Viennet, a Lifeblood Research Fellow, is dedicated to understanding and predicting how a changing climate, global change, and emerging threats, could affect the blood supply in the future. She uses advanced analytic tools to find vulnerable areas and potentially strengthen policy against new dangers.
Lifeblood researchers and specialists collaborate extensively, integrating climate change considerations into their comprehensive approach to ensure the safety and sustainability of our blood supply.
References available upon request.
Authors: Dr. Elvina Viennet, Research Fellow, Australian Red Cross Lifeblood, Brisbane, Australia; Dr. Alison Gould, National Leader Research Communication and Engagement, Australian Red Cross Lifeblood, Sydney, Australia
Acknowledgement: Professor David Irving, Director Research and Development, Australian Red Cross Lifeblood, Sydney, Australia; Dr Veronica Hoad, Public Health Physician, Australian Red Cross Lifeblood, Perth, Australia
CAPTURING THE EXPERIENCES OF HEAT ON HEALTH IN RURAL POPULATIONS

Near enough is not good enough when considering high heat events across Victoria. Recent research highlights why researching and understanding the local context matters.
HIGH HEAT AND HEAT-RELATED ILLNESS
Heat kills more Australians than any other natural disaster, and it also causes increased hospitalisations 1. A recent report by the Australian Institute of Health and Welfare 1 noted that of the 9,119 hospitalisations due to extreme weather between July 2012 and June 2022, heat was responsible for 7,014 admissions. Further, of the 677 injury deaths from extreme weather between July 2011 and June 2021, 293 were due to heat. Globally, 2023 was classified as the warmest year on record 2 and as the climate continues warming, more intense and prolonged periods of heat are predicted. Understanding heat-related illness and protecting those at greatest risk is required.
Western District Health Service, Hamilton. Dr Jessie Adams and Professor Susan BrumbyPrevious research in Australia has largely focused on metropolitan populations. Studies have reported increases in mortality and morbidity including increased ambulance callouts, Emergency Department presentations and hospital admissions. A recent study by Thomson and colleagues 3, used the Victorian Emergency Minimum Dataset (VEMD) and found increased morbidity during Victorian heat health alerts between 2010 and 2022. However, the VEMD uses data from larger Emergency Departments and subsequently misses approximately 35% of the data currently available via the governmentreported dataset 4, 5. Research directly focused on rural populations, has been minimal, despite having been recognised having high occupational risks and poorer health outcomes when compared to metropolitan populations.
HEAT-RELATED ILLNESS IN RURAL SOUTH-WEST VICTORIA
The National Centre for Farmer Health and Deakin University undertook research that aimed to examine the characteristics of heat-related illness in rural south-west Victoria using the Rural Acute Hospital Data Register (RAHDaR) 6. This database includes all presentations to the 10 emergency care facilities in south-west Victoria. Of these facilities, only two directly report to the VEMD.
The first stage of the project investigated presentations on days of high-heat (above the 95th temperature percentile) to the Emergency Departments and Urgent Care Centres in the RAHDaR database between 1 February 2017 and 31 January 2020 7
Interestingly, unlike previous metropolitan studies, the results demonstrated an overall reduction in presentations on days of high-heat.
There was a more prominent decrease in those from farming towns—individuals from farming towns were 17% less likely to present on days of high-heat than those from non-farming towns.
The most common presentation on both days of highheat and non-high heat were injuries, however, these also decreased on days of high-heat. Respiratory system illness increased in individuals from farming towns on days of high-heat, and circulatory system illness increased for both groups on days of high heat. Admissions to hospital of those from farming towns also increased on high-heat days, suggesting those presenting were more unwell.
A second stage of the study is currently being undertaken to examine characteristics of presentations between 2017 and 2023 to the emergency care facilities included in the


RAHDaR database during heatwaves (consecutive days of high-heat) as per the Bureau of Meteorology’s Excess Heat Factor classification identified approximately half of presentations during the heat events in south-west Victoria are to the emergency care facilities that are not required to report to the VEMD. This means half of all presentations in the area have been missed from any previous research or government reports.
IMPORTANT TO CONSIDER HEAT IN THE LOCAL CONTEXT
The results highlight the value of considering the effects of heat in a localised context, and also of considering how impacts vary across key populations in a region. Firstly, the identification of common presentation types to the emergency care facilities on days of high-heat can assist in healthcare service planning and resource allocation. On both high-heat and non-high heat days, injuries were the most common presentation to the emergency care facilities suggesting a greater focus on injury prevention overall. Further, healthcare services should prepare for increases in respiratory and circulatory system illness presentations. The reduction in overall presentations of days of high-heat may be due to awareness of risks around heat and subsequent behavioural adaption (e.g. self-pacing, increased rest periods, completing more strenuous activities in the cooler parts of the day and increased water consumption). As populations have varying characteristics and acclimatise to their local climate, the identification of trends in presentations during heat events in a localised context is important for both health services and municipal planning.
Over half of presentations during heat events in rural south-west Victoria are not reported into the VEMD, highlighting the importance of including smaller facilities in any state-based heat planning. Investigation of trends in regard to heat-related illness and understanding the who, what, when, where, how and why of presentations on days of high-heat and high-heat events must be at the very least regionalised to ensure they accurately inform the development of both future health service and municipal planning.
References are available upon request.
Authors: Dr Jessie Adams (Deakin University, National Centre for Farmer Health), Prof Susan Brumby (Deakin University, National Centre for Farmer Health), Elvira Hewson (SouthWest Healthcare), Dr Kate Kloot (School of Medicine, Deakin University), Assoc Prof. Tim Baker (School of Medicine, Deakin University).
E-DENGUE PROJECT
Digital tool to prevent dengue outbreaks in VietnamE-Dengue will provide timely warnings of dengue outbreaks to support local health departments to proactively deploy dengue preventive and control measures in the Mekong Delta.



My Twitter : @chriskere
Prior to 1970, only 9 countries in the world had experienced severe dengue epidemics. Deaths were rare, and years passed between major epidemics.
In the past 10 years, cases of dengue fever have soared, with the World Health Organisation estimating that more than half of the world’s population are now at risk of becoming infected.
Global warming is playing a significant role in creating favourable conditions for mosquito breeding, viral replication, and longer transmission seasons.
Dr Dung Phung is a Senior Lecturer in the School of Public Health at The University of Queensland and said Vietnam is one of the countries most vulnerable to climate change in South-East Asia and is suffering an increase in climatesensitive infectious diseases.
“Dengue is one of the leading causes of hospitalisation between May and October, which is the dengue transmission season. It is estimated that more than 2 million people become infected by dengue fever annually, with approximately 100 thousand people treated for the mosquito-borne illness in healthcare settings,” Dr Phung said.
“Symptoms include high fever, rash and muscle and joint pain. In severe cases there is serious bleeding and shock, which can be life-threatening. Those who are infected a second time develop a significantly higher severity of the disease.”
Dr Phung, who worked as a medical professional in Hanoi, has a very strong connection with the health sector in Vietnam and is passionate about decreasing the incidence and spread of the virus.
“Dengue incidence is now significant in some areas where it had not been a big problem in the past. For example, the dengue outbreaks have been observed in several mountainous areas in North Vietnam, where they have scantly had dengue cases before,” Dr Phung said.
“This creates a huge burden on the healthcare systems of Vietnam, particularly for crowded and overloaded hospitals where it is now more and more common to see multiple patients sharing one bed.”
Moved by Vietnam’s decades-long struggle with the virus and climate change, he has developed an early warning model for dengue outbreaks.
E-Dengue, as it’s known, uses a prediction model to help local communities and health centres mitigate outbreaks of the mosquito-borne disease in the Mekong Delta Region.
With the assistance of global charitable foundation
Wellcome Trust, Dr Phung has received an $8,445,649 grant to lead the project’s development across 13 provinces and 134 districts that are highly vulnerable to climate change between 2023 and 2027.
“Current dengue control measures are mostly reactive due to the absence of an early warning system tailored to the needs of the local health systems,” Dr Phung said.

“The E-Dengue tool will provide timely warnings of dengue outbreaks from the surveillance system that will support the local health departments and the community to proactively plan and deploy dengue preventive and control measures in high-risk areas.”
It is a global effort, with the 3-phase project attracting an internationally renowned team of researchers, technicians, and decision-makers.
“We are currently at phase 1 – building a climate-informed predictive model to accurately anticipate dengue incidence and outbreaks 2 months in advance at the district level,” Dr Phung said.
“Dengue is very sensitive to climatic factors including population density and water storage, so we are working closely with the YALE School of Public Health during this phase to develop and validate prediction models.”
Phase 2 will develop E-Dengue as an open-source software system that has a user-friendly mobile-app and web-based interface based on the prediction model determined in phase 1.
During phase 3, E-Dengue’s effectiveness and costefficiency will be evaluated through a community-based cluster-randomised controlled trial study, making it the first climate-driven emergency warning system to be thoroughly evaluated with a gold-standard method.
E-Dengue is expected to reduce dengue incidence and outbreaks by 25 per cent in comparison with the current reactive prevention practice.
“We are also working on ways to make the tool applicable in other regions that have similar environmental and social conditions,” Dr Phung explained, with information collected to be available on open-source software.
“I used to work as a health professional in a developing country, and I really want to find an effective solution to prevent dengue fever. My goal is that health departments input their own data and modify the E-Dengue tool for their own location.”
POWER IN THEIR HANDS
Providing consumers with planetary health ratings for packaged foods and beverages

Australians now have access to a novel Planetary Health Rating System and accompanying app that provide information on the environmental impact of more than 60,000 packaged foods.
AN URGENT PROBLEM
The food system contributes around one-third of global greenhouse gas emissions. A formal statement from the recent United Nations COP28 climate conference noted that transformation of the global food system is essential for meeting the 2030 warming target specified in the Paris Agreement. However, governments have yet to make meaningful changes in this domain.
Transformation strategies for a more sustainable food system include both supply side (e.g., improving agricultural efficiency) and demand side solutions (e.g., encouraging consumers to change what they eat). However, changing individual diets is typically inefficient and difficult, and macro-level approaches are needed instead to achieve major shifts in diets at the population level. An example of such an approach is to display user-friendly sustainability information on food labels to enable consumers to compare products and make climate-friendly choices. As evidenced by front-of-pack nutrition labels , labelling can both encourage changes in consumers’ choices and trigger reformulation activities by food producers as they seek to maintain or increase market share.
Sustainability information provided to consumers must be trustworthy to be effective. The Australian

Competition and Consumer Commission (ACCC) has identified ‘greenwashing’ in the Australian food market as a substantial problem requiring comprehensive action. This situation is expected to worsen as consumers become more aware of environmental issues, making sustainability-related claims an attractive option for brand owners. The proliferation of unsubstantiated claims can do more harm than good by misleading consumers and creating an uneven playing field in the market. Consumers need and want a reliable method of assessing the sustainability of the foods and beverages they purchase.
A NOVEL PLANETARY HEALTH RATING FOR PACKAGED FOODS AND BEVERAGES
Information is emerging about which general food groups (e.g., vegetables vs meat) are more or less sustainable. This information has yet to become widely known among the general public and can be of limited value when consumers are selecting packaged foods that contain multiple ingredients. Until very recently, there has been no simple way for consumers to estimate the likely environmental impacts of specific products.
To address this issue, the Healthy Food, Healthy Planet, Healthy People NHMRC Centre of Research Excellence, based at The George Institute for Global Health, has developed a Planetary Health Rating System for packaged food products. The rating represents an estimate of the greenhouse gas emissions attributable to the production of individual products. The estimate is calculated in four


steps: (i) a mathematical optimisation technique is applied to estimate the quantity of each ingredient using the product’s ingredient list and nutrient information, (ii) data from life cycle assessments (LCA) are used to provide estimates of the amount of greenhouse gas emissions associated with different Australian ingredients, (iii) the LCA data are applied to the ingredient information for each product, with the outcome modified to account for greenhouse gas emissions resulting from processing and transport, and (iv) the planetary health score is converted to a star rating system.
Consistent with the Health Star Rating in use in Australia, the Planetary Health Rating is in the form of a 10-point scale ranging from half a star to 5 stars. The more stars a product receives, the lower the greenhouse gas emissions associated with its production. To further enhance interpretation, the star ratings are colour coded from green through to red.
Australian consumers can now access Planetary Health Ratings for more than 60,000 products via a free, userfriendly app called ecoSwitch that is available from the App Store and Google Play. Using ecoSwitch, consumers can scan a product’s barcode and access ratings for it and a list of similar product alternatives with lower greenhouse gas emissions.
Further information is also provided on the item’s country-of-origin, NOVA level of processing classification, sustainability claims, and Health Star Rating. In the short to medium term, the Planetary Health Rating algorithm will be upgraded to include an additional 13 indicators




covering diverse environmental issues such as land and water use and pollution.
In conclusion, it is becoming increasingly clear that governments are moving too slowly to undertake the scale of food system transformation required to avert catastrophic climate change. In the absence of timely, decisive policy action, it is critically important to empower consumers to make more sustainable food choices by providing relevant information at the point of sale. The research-informed ecoSwitch and its underlying Planetary Health Rating System represent important and timely tools to assist consumers in making more sustainable everyday food choices. In addition, these tools can prompt government and industry action by identifying the most and least environmentally friendly options across the Australian packaged food supply, and everything in between.
Authors: Simone Pettigrew is Director of Food Policy at The George Institute for Global Health and a Professorial Fellow in the School of Population Health at The University of New South Wales. Fraser Taylor is Managing Director of FoodSwitch at the George Institute for Global Health. Michalis Hadjikakou is Senior Lecturer in Environmental Science and Sustainability in the School of Life and Environmental Sciences at Deakin University.
BUILDING A VILLAGE TO COMBAT THE THREAT OF CLIMATE CHANGE
Professor Craig Munns calls for a united approach to addressing the disproportionate effect of climate change on the health and wellbeing of children.

 Professor
Craig Munns
Professor
Craig Munns
They say it takes a village to raise a child, but Professor Craig Munns from The University of Queensland’s Child Health Research Centre (CHRC) contends the environment of that village is just as important as the people.
“The environmental determinants of health and wellbeing are only starting to be fully appreciated with their complex interplay impacting on all aspects of a child’s life,” Professor Munns said.
“Whether it is the natural environment the child is in, the microbial environment a child is exposed to, the built environment they interact with, the psychosocial environment in which a child is embedded or the digital environment we have built for the child – the different environmental determinants have a huge impact on the short and long-term health and wellbeing of that child.”
“These environments interact with each other, so a significant change in one, impacts all. There is one environmental factor that is looming as a major threat,” he said.
A LOOMING THREAT
That looming threat is climate change and the impact it is likely to have on children.
“Climate change will disproportionately affect our children more than any other group in society, so we must act to lessen the impacts of it,” Professor Munns said.
“Climate change is an enormous existential threat to the wellbeing of children and young adults. The American Academy of Paediatrics has highlighted that ‘climate change poses threats to human health, safety, and security, and children are uniquely vulnerable to these threats’1. We have to think not only about children but of our children’s children, who will also be the ones who have to fix the problems that we leave them.”
Professor Munns said the challenge of climate change is far too big for any one group or organisation to address by themselves.
He said it’s a responsibility that falls upon bigger collectives.
“The Child Health Research Centre is doing our bit and working to bring together experts across The University of Queensland and the wider community to address climate change and the impacts it is having on child and youth wellbeing. It will take collective action to truly make a difference,” he said.
And it is doing more than just a bit, with several projects in the arena with researchers investigating relationships between environmental exposures and child health.
“CHRC is a World Health Organisation Collaborating Centre for Children’s Health and Environment, so we’re leading the way not just locally, but also within our region.
1 Climate Change (aap.org)

“We’ve got Professor James Scott, who’s the Professor of Child and Adolescent Mental Health and he’s doing research looking at the impact of climate change on the mental health of children and young people.
“We’ve also got programs like The Children’s Health and Environment Program (CHEP), that is led by Professor Peter Sly and Professor Paul Jagals. CHEP has wonderful researchers such as Dr Dwan Vilcins who is undertaking ground-breaking research on bush fire smoke and breathing disorders in children.”

Professor Munns said a whole of community response is required to battle the effects of climate change on children.
“To truly get a holistic response to the impact of climate change, we need to look at these different environmental impacts on wellbeing with a whole community approach across universities, government, industry and community to ensure that we’re addressing this enormous issue.”
IT’S A FIGHT THAT’S GOING TO REQUIRE THE GLOBAL VILLAGE
Professor Munns said a reimagining of the approach we are taking is required when it comes to climate change.
“We need to talk about reimagining the system that we all work in because it is the current system that has led us to the crisis we are facing, so now we need to think and act differently to find and enact the solutions needed to address the problem,” he said.
The CHRC has 15 research groups that investigate three broad priority areas: brain and mind; population, environment, and health; and personalised prevention and care.
There are dozens of active projects spanning childhood brain injury, cystic fibrosis, allergies, cancers, diabetes, allergy, immunology, bone health, physical activity and more.
The engine room of the CHRC is its diverse and growing research base of over 90 medical, allied health, nursing and scientific staff, more than 50 higher degree research students, and 250 academic title holders (full-time clinicians within the hospital system who contribute to teaching and research).
“All of these initiatives and people are employed to do one thing: to help children, youth and families thrive,” Professor Munns said.
“And so, we must all do our part in battling what’s being described as the biggest threat to children, climate change with global warming.”
Author: Professor Craig Munns, University of QueenslandENERGY EFFICIENCY
IMPROVEMENTS IN HOMES PROVIDE LONG-TERM FINANCIAL, ENVIRONMENTAL AND HEALTH BENEFITS
A ground-breaking study has shown the impact that improved thermal comfort can have on quality of life, physical health and mental wellbeing.

Much of Australia’s housing stock is ill equipped to cope with climate change. In Victoria alone, there are more than 1.3 million houses built before 1991 with an average below 2 stars for energy efficiency. For the people living in these homes, this means that winter brings not only cold indoor temperatures and high energy bills, but also risks to health.
Cold weather increases the risk of illness and death from lung and heart problems, falls and poor mental health. The elderly and people with chronic conditions, in particular, experience worse health outcomes if the temperature in their houses falls below 18°C, which is the World Health Organization threshold minimum indoor
temperature required to protect the health of general populations during cold seasons.
Previous research has suggested that improving thermal comfort in homes will lead to better health outcomes. Yet retrofitting older houses to improve energy efficiency can be too expensive for lower income homeowners – often those who are the most vulnerable to the health impacts of climate change.
The Victorian Healthy Homes program was an Australianfirst randomised controlled trial managed by Sustainability Victoria and evaluated by UTS Institute for Sustainable Futures (ISF) and Centre for Health Economics Research and Evaluation (CHERE) that sought to understand how thermal comfort and energy efficiency upgrades affect


the health, comfort and financial situation of low-income Victorians with a health or social care need.
The Program offered free thermal comfort energy efficiency upgrades to 1,000 households across western Melbourne and the Goulburn Valley during three winters from 2018–2020.
The average age of the participants was 76, and in all houses at least one person had a chronic health condition such as cardiovascular or respiratory disease. Their homes were assessed and they were provided minor home upgrades such as insulation, draught sealing, reverse cycle air conditioning or gas heater replacement, and internal window coverings, at an average cost per household of $2809.
Over three consecutive winters, the study measured changes in residential energy efficiency, energy use, thermal comfort, healthcare use and costs and selfreported quality of life.
The study found that indoor temperature was significantly increased during winter in houses that had received the upgrades. Householders reported feeling warmer, and data showed significantly lower gas use, contributing to both lower energy bills and fewer greenhouse gas emissions. People also said having a warm home increased their social connectedness.
“I wouldn’t have family come and visit me in winter because my house was too cold,” said one of the study participants, Heather.
“Here I am, I’m sitting under a split system with visitors, so how good is that? In the middle of winter. So this is great, I’ve got my life back.”
For the first time, the study also measured health and wellbeing outcomes and cost effectiveness of the energy efficiency upgrades.
We collected self-reported ratings of health and wellbeing and respiratory symptoms at baseline and after the home upgrades. We combined this with data on healthcare utilisation including hospital admissions, emergency department attendances (provided by the Centre for Victorian Data Linkage), GP visits, specialist visits and use of prescription medicines (data provided by Services Australia)

Our evaluation found that the Program was associated with significant benefits in health. It showed participants who received the home upgrades experienced reduced breathlessness and improved quality of life, with mental health and social care improvements.
The households that received the upgrades saved $887 per person in the healthcare system over the winter period with this being a cost-saving predominantly to the Federal government in reduced Medicare services. A cost-benefit analysis showed that the upgrade would be cost saving within three years and would create a net saving of more than $4,783 over 10 years in both energy and health expenditure.
Cost savings were heavily weighted towards healthcare. For every $1 saved in energy, more than $10 was saved in health.
This study has gained local and international attention, including from the recently released National Health and Climate Strategy and the UK’s Pathfinder Initiative, and its findings are being considered by state and federal governments in Australia.
The Hon Dr Andrew Leigh MP, a long-standing advocate for randomised control trials, has referenced Healthy Homes as a good example in his advocacy for the Federal Government to evaluate its own programs.
This research confirms the value and importance of investment in improving winter warmth through energy efficiency upgrades for the environment, the economy and for people’s physical and mental health, especially with the rapidly changing climate.
Author: Dr Katie Page is a Senior Research Fellow at the Centre for Health Economics Research and Evaluation (CHERE) at the University of Technology Sydney. Professor Rosalie Viney is Director of the Centre for Health Economics Research and Evaluation at UTS. Kerryn Wilmot leads smart cities and healthy urban environment research programs at the UTS Institute for Sustainable Futures.
GREEN AI FOR EFFECTIVE CLIMATE ADAPTATION
Machine Learning algorithms and a digital twin are used at Sydney Olympic Park to maximise the Park Cool Island Effect and demonstrate how public green infrastructure can be turned into natural air-conditioning systems for climate change adaptation and greater public wellbeing.

 Professor Sebastian Pfautsch
Professor Sebastian Pfautsch

Australia is the driest and hottest permanently inhabited continent, facing annual heatwaves more deadly than all other natural disasters combined, AdaptNSW (2023) reports.
Urban areas, home to over 85% of Australia’s population (Worldbank), exacerbate heat events as concrete, buildings, and asphalt absorb, retain and reemit heat, making cities at least 1-3°C warmer when compared to nearby reference sites covered in vegetation. With the Bureau of Meteorology and CSIRO forecasting hotter, drier summers ahead, particularly impacting urban spaces, the role of green spaces in cooling cities, enhancing health, wellbeing, and ecology becomes crucial.
As cities densify and expand, the preservation and expansion of quality green spaces are imperative. The areas encompassing vegetation are increasingly acknowledged for their essential role in cooling urban areas naturally, through air and surface temperature reduction, alongside providing health and wellbeing benefits, and overall social advantages . However, these increasingly essential areas are threatened by drought and rising temperatures. Addressing these challenges, Professor Sebastian Pfautsch of Western Sydney University has spearheaded the Smart Irrigation Management for Parks and Cool Towns (SIMP@CT) project. This initiative unites 12 partners from academia, government, and the private sector to combat urban heat, water scarcity, and the necessity for quality public green space using smart technology.
Implemented in Sydney’s Bicentennial Park, a beloved 42-hectare space attracting over a million visitors annually, SIMP@CT aims to create a green, cool oasis promoting health and social equity. The project employs Ground to Cloud technology, integrating over 200 LoRaWAN soil moisture and temperature sensors and 7 weather stations, streaming live data to the park’s digital twin. The system also ingests location-specific weather forecasts and turbocharges existing data streams by comparing anticipated and delivered water volumes which further assists in quality control of irrigation scheduling and fault detection of the irrigation hardware. An online dashboard helps people know where the coolest and warmest areas are so they can factor microclimate conditions in when planning their run, bike ride or picnic. The first detailed analyses have shown that air temperature in the irrigated park can be 7°C cooler compared to the nearby commercial and entertainment centre (see p.314 ff in these Proceedings).
The impact of SIMP@CT has been remarkable, delivering environmental, economic, and social benefits. On the utilities side, SIMP@CT provides savings in energy

consumption and pumping costs due to increased distribution efficiencies. At the same time SIMP@CT provides the aforementioned real-time information to park visitors and local residents to better locate ‘cool zones’. Arguably this provides for ‘avoided public health costs’ - given the increased social connection that occurs in public green spaces and improved outcomes for both mental and physical health where people can access live information on their nearby zones of thermal comfort.
Financially, the project has demonstrated substantial payback. An analysis revealed a net present value ranging from $9.72 to $12.44 million, and a benefit-cost ratio of 2.62-3.07, suggesting that for every dollar invested, more than $3 are returned. The Cost Benefit Analysis by the NSW Government has estimated that the improved park microclimate could generate savings of $2,260,000 every year from reduced heat-induced deaths and $32,600 from reduced heat-induced hospitalisation.
Australia is taking notice. In 2023, SIMP@CT received state and national awards and was a finalist in the World Smart Cities Awards competition. Receiving awards from the Internet of Things Association Australia (IOTAA) for ‘Best Research Project’ and ‘IoT for Good’ and two Innovation AUS 2023 Awards for Excellence, including the ‘People’s Choice’ award signifies that the industry clearly sees merit in our solution to cool cities. The project team also won a prestigious Banksia Foundation Sustainability Award, trailblazing the pathway for innovation around urban green infrastructure and its capacity to cool our cities during increasingly hotter summers.
Continuing to push the boundaries of innovation, the team has been focused on scalability. The digital architecture of the project was design to easily scale up or down. Being so flexible and web-based makes it possible to adopt the SIMP@CT technology for any irrigated greenspace like golf courses, sport fields or botanic gardens in Australia and overseas. This represents a unique approach that turns green spaces into effective cooling assets in a warming word, making SIMP@CT a pioneering solution in utilizing urban green infrastructure to combat the effects of increasingly warmer summers. The team continues its work and hope to set a new standard for climate resilience in urban planning and green space management. For more information reach out to the project team by clicking here
Authors: Professor Sebastian Pfautsch, Urban Transformations Research Centre, WSU
Professor Robert Gorkin – Translational Health Research Institute, WSU
CHANGING THE CLIMATE: ADDRESSING THE SOCIAL, ECONOMIC AND CULTURAL FACTORS UNDERMINING PLANETARY HEALTH
Human disruptions to Earth’s natural systems in the Anthropocene, including climate change and largescale biodiversity losses, are directly damaging to all life, including our own.

Rising rates of disease distress, and despair are inextricably linked with degradation and destruction of ecosystems at all scales, including unhealthy socio-political ecosystems. This requires urgent, deep structural changes in how we live—to the social, economic, and spiritual “climate” underpinning destructive human values, attitudes, and behaviors.
Planetary Health is a solutions-oriented, transdisciplinary field and social movement focused on analysing and addressing the impacts of human disruptions to Earth’s natural systems on human health and all life on Earth.
Solutions depend on understanding the complex interdependence across systems, and the “relationship
Constellation Project: Inspiring social and environmental change through imagination and connected planetary consciousness (Image with permission: credit: Greg Rakozy)
crisis” between humans and the natural world. Addressing worldviews and value systems as root causes of social and ecological injustice is key to a planetary health agenda. It is critical to break the cycle of anxiety, despair, cynicism and polarisation associated with the crisis narratives of the climate agenda.
The Constellation Project addresses the mounting calls for a “spiritual and cultural transformation” to tackle these challenges, which requires more integrated approaches to research and policy, and educational frameworks that promote emotional intelligence, moral wisdom, and cultural competency. This is an initiative of the Planetary Health Alliance (PHA), a global consortium of over 400 universities, non-governmental organizations, and
government entities committed to understanding and addressing environmental change and its health impacts.
The Project provides a visionary space to weave new stories and emergent ways of being for a new era of planetary consciousness. At this critical moment in history, we seek to ignite and reimagine more intentional spiritual relationships with ourselves, others, and the natural world—recognising that so many challenges in the Anthropocene ultimately stem from erosion of these emotional connections. We are networking communities of care for diverse voices from all disciplines, geographies, and traditions to contribute to a more ethical stance and an earth-based spirituality. Through a range of scholarly activities, research, artistic works, contemplative practices, and regular conversations, we seek to inspire worldviews that enable flourishing— not merely by reactively challenging old paradigms, but by proactively creating hopeful stories of new ways of inter-being with ourselves, each other and the planet.
There are several key interrelated themes underpinning the current and proposed activities of the Constellation Project. These are intended to influence both academic discourse and social movements by promoting holistic approaches and “reverence for life” to accelerate meaningful cultural change and sustainable actions.
Narrative co-creation for cultural change: Narratives shape human reality and have the power to shift the worldviews, values, attitudes, and behaviors for individual, collective and systems change. More optimistic and mutualistic narratives improve social cohesion, engagement, and collaborative action towards environmental and collective well-being.
Cultural capacities, awareness, and inner development: Individual empowerment through selfdevelopment is a key factor in collective capacity for equitable, ethical, sustainable social transformation. Promoting self-awareness and the skills, virtues, and character strengths to tackle challenges is key in motivating behaviors for the common good. Creating environments that support competence and capacity also
 David Webb
David Webb



promotes purpose, happiness, hope, and engagement in social and environmental actions.
Enriching worldviews through diverse perspectives: We encourage convergence of scientific discovery and spiritual knowledge for expanded worldviews that are enriched by Indigenous and diverse faith perspectives. In an era of political polarization, we seek inclusiveness to synthesize and harmonize positive goals and common universal values for a shift in consciousness.
Connectedness, coherence, and community: Meaningful relationships with other people and nature promote a sense of belonging, compassion, care, and “unitive” awareness of the interdependence of all life. Emotional connections, inspired by awe and wonder, encourage actions for co-beneficial solutions that align with nature.
Creative emergence: New paradigms depend on imagination and creativity. The expressive arts enhance intercultural and intergenerational learning, deepening emotional connection and motivating change by integrating intellectual and heart-centered approaches.
These efforts provide new research and advocacy opportunities for social and environmental justice and human flourishing. By promoting these capacities in a culture of collaboration through our global networks, we aim to contribute to quantum social change—in ways that cannot be achieved by logic and advances in technology alone.
Authors: Susan Prescott MD, PhD, FRACP (Professor of Planetary Health, Medical School, University of Western Australia; Director of Planetary Health at the Nova Institute; Lead, Constellation Project, Planetary Health Alliance). David Webb PhD. Associate Professor (Regenerative Business and Planetary Health), Business School, University of Western Australia.
COULD CLIMATERELATED EXPOSURES CONTRIBUTE TO PROLONGED PREGNANCY?

BACKGROUND
Prolonged pregnancy or late-term to post-term births (born at ≥ 41 gestational weeks) has received far less attention than preterm birth (born at < 37 gestational weeks).1,2 About 4-14% of singleton pregnancies worldwide end up in prolonged pregnancy, which leads to both child and maternal mortality and morbidity.1,3,4 Management of prolonged pregnancy can result in provider-initiated interventions such as labour induction or caesarean section, which themselves have also been implicated with subsequent maternal complications and adverse perinatal and child health outcomes.1,3,5 To date, there are no clear recommendations for effective treatment or preventive measures, and the causes of prolonged pregnancy have not been fully elucidated.3,4 Climate-related exposures offer a new avenue of enquiry.
Anthropogenic climate-related factors such as ambient air pollution and extreme temperatures have been linked to various adverse pregnancy outcomes.6,7 Climate-related exposures disrupt the mother-placenta-fetus physiology such as imbalanced hormonal and inflammatory activities which could either shorten the gestation, resulting in preterm birth 6,7 or lengthen it, resulting in prolonged pregnancy. 3,4 There is well-documented evidence of the association between climate-related exposures and preterm birth,6,7 but the link to prolonged pregnancy has not been explored. We investigated this link and identified vulnerable populations to inform timely interventions and understanding of biological mechanisms.


METHODS
We derived small-area level (Statistical area level 1, SA1) monthly fine particulate matter air pollution (PM2.5) and biothermal (Universal Thermal Climate Index, UTCI) exposures from three months preconception to the end of pregnancy for 393,384 singleton pregnancies between 1st January 2000 and 31st December 2015 in Western Australia that did not end in preterm birth. We estimated the covariate-adjusted odds of prolonged pregnancy (≥ 41 gestational weeks) due to maternal PM2.5 and UTCI exposures by applying a novel and robust statistical modelling framework that accounted for both the timing and intensity of past exposures. Adjustment was made for infant sex, maternal age, race or ethnicity, marital status, smoking status, parity, remoteness, socioeconomic status, and year and season of conception.
RESULTS
Of the included births, 47,380 (12%) were prolonged pregnancies. The average PM2.5 and UTCI exposures were 8.1µg/m3 and 14.5 ℃, respectively. Every 1 µg/m3 PM2.5 increment was associated with increased odds of prolonged pregnancy which increased from six months of pregnancy closer to birth. Compared to the median (14.2 ℃), both low and high UTCI exposures were associated with higher odds of prolonged pregnancy (Figure). The odds of prolonged pregnancy for cumulative exposures from three months preconception to nine months

pregnancy was 6% (95% CI 5%, 7%) higher for each 1 µg/ m3 increase in PM2.5 exposure and 8% (95% CI 2%, 14%) and 30% (95% CI 23%, 38%) higher for low (1st centile) and high (99th centile) UTCI exposures relative to the median, respectively. Disparate effects of the exposures were found in some subpopulations such as male births, and mothers who were urban residents, nulliparous, aged ≥ 35 years, and with complicated pregnancies.
DISCUSSION AND CONCLUSION
This is the first study to demonstrate that climaterelated exposures such as ambient air pollution and extreme biothermal exposures could contribute to the prolongation of pregnancy and vary by sociodemographic vulnerability. Air pollution and extreme biothermal (cold or heat) exposures can slow hormonal and inflammatory processes, leading to elongation of gestation. 3,6,7 The 12% prolonged pregnancy could be underestimated as a significant proportion of pregnancies that would have ended up as prolonged pregnancies might be either induced or delivered by caesarean section. Given the increasing anthropogenic climate change with associated health effects and the serious health effects of prolonged pregnancy on both mother and child,1,3,4 our findings on this neglected topic require further investigation and attention.
References to be supplied upon request

Authors: Sylvester D. Nyadanu*1,2 , Gizachew A. Tessema1,3 , Jennifer Dunne, 1,3 Aditi Roy,1 Gavin Pereira*1,3,4
1 Curtin School of Population Health, Curtin University, Perth, Kent Street, Bentley, Western Australia 6102, Australia.
2 Healthy Environments and Lives (HEAL) National Research Network, Australia
3 enAble Institute, Curtin University, Perth, Kent Street, Bentley, Western Australia 6102, Australia
4 WHO Collaborating Centre for Climate Change and Health Impact Assessment. Faculty of Health Science, Curtin University, WA, Australia.
From left to right: Assoc. Prof. Gizachew A. Tessema, Dr. Sylvester D. Nyadanu, Dr. Jennifer Dunne, Dr. Aditi Roy, and Prof. Gavin Pereira Figure. Monthly adjusted odd ratios (aOR) of prolonged pregnancy for exposures over three months preconception to nine months of pregnancy at low and high biothermal exposure (Universal Thermal Climate Index) relative the median exposure of 14.2 ˚C.
NITROUS OXIDE LEAKS IN HOSPITALS – FINDING AND FIXING CARBON HOTSPOTS IN HEALTHCARE
Overseas data suggests leakage is a major issue in nitrous oxide pipelines in hospitals. Given nitrous oxide is a potent greenhouse gas, fixing these leaks is a priority. We built a novel hospital-level nitrous oxide monitoring system to measure and help fix these leaks.



Nitrous Oxide, or laughing gas, has been used for more than 150 years for analgesia and sedation in medicine and dentistry (as well as a recreational drug of abuse).
It is well tolerated, with manageable side effects, but it is a potent greenhouse gas, and global efforts are underway to reduce its usage in a range of areas from agriculture to medicine. It is estimated that 1 litre of nitrous oxide has the same global warming potential as 0.5kg of CO
A big hospital can use more than 1 million litres a year, with a carbon footprint of 500 tons CO2e. Across a whole healthcare service nitrous oxide can be responsible for up to 3-5% of the total carbon footprint. In modern hospitals, pipelines are used to supply oxygen, medical air, and nitrous oxide from a central reservoir, to wherever they are needed, but it has been shown recently in the UK’s National Health Service that nitrous oxide pipelines can leak between 75-95% of the gas they carry.


Individual hospitals find it difficult to measure the size of this leak during normal operations, with special testing required that interferes with clinical practice. In this project, we designed and built a custom-made hospital level flow meter to precisely measure nitrous oxide flows at our large children’s hospital, to quantify how much was leaking, and what patterns of flow were associated with day-to-day operations.
There were several specific requirements that we needed to fulfill.
1. The ability to measure flow accurately and precisely across a wide range of possible flow rates. It was particularly important to accurately measure the lower range of flows, as this would help us quantify the size of any leakage.
2. Have a good time resolution to enable us to detect changes in flows every minute.
3. Placement at the actual source of nitrous oxide for the hospital, to try and capture all sources of leak.
4. Data storage and transfer capabilities to speed up analysis and interventions.
Emerson Corporation were engaged to help build the flowmeter system.
This project is in its early stages, and these results are preliminary.
Figure 1 shows the nitrous oxide flow over a weeklong period, and one can clearly see the peaks associated with clinical use, almost all being during normal working hours, and the low level, constant flow visible during the early morning hours. This represents leakage from the pipelines and distribution points in the hospital. We then calculate the average minimum flow rates during times of zero clinical use and extrapolate that over the full period to get total nitrous leakage volume. The total nitrous used
is calculated from the area under the whole graph. Total nitrous leakage divided by total nitrous used given us a leakage percentage of approximately 50% for this period.
Because almost all hospitals cannot accurately monitor total nitrous oxide flows, and because the gas is relatively inexpensive (a few tens of thousands dollars for a large hospital over a year), high leak rates have gone unnoticed. More recently, various techniques including discrepancies between purchased versus used nitrous, static pressure testing, and individual anaesthesia machine data have been used to get some idea of the leak fraction.
Our project has identified an approximately 50% leak of nitrous oxide at our institution over the period of monitoring, and we are now in the process of identifying the locations of that leakage, together with preventative maintenance that includes regular checking of outlets, joints, manifolds and other areas where leaks may occur. To aid in this leak localization process, we are combining data from a custom anaesthesia database that tracks all gas usage in the anaesthesia department on a minutely basis, with the whole of hospital nitrous oxide flow data. This data science focussed approach substantially aids in identifying where individual administrations of nitrous oxide come from, and will make the identification of leaks and the future maintenance of the pipeline system a lot easier.
This leak represents around 500 tons of CO 2e 0.5-1% of the carbon footprint of an average large hospital, and addressing these leaks, together with better management of clinical use of nitrous oxide, are part of the many steps we need to take to reduce the carbon footprint of healthcare.
Author: Associate Professor Justin J Skowno, Paediatric Anaesthetist and Director of Anaesthesia Research, Children’s Hospital at Westmead.PLANETARY HEALTH EDUCATION IS ABOUT ENABLING STUDENTS TO TAKE ACTION

With Australia vulnerable to triple planetary crises, universities need to graduate health professionals who are ecoethical leaders and planetary stewards. Several health professional educators in the Faculty of Health Sciences and Medicine at Bond University have been integrating Planetary Health into curricula or providing frameworks to enable action.
Australia is vulnerable to the triple planetary crises of a changing climate, biodiversity loss and pollution in all its forms. The wildfires, floods and severe weather of the last few years are evidence of a changing climate, due largely to the burning of fossil fuels.
Not only must all health professional graduates be wellprepared for the impacts of adverse weather events, but as they are highly trusted by the public, they are wellpositioned to be the eco-ethical leaders who personally and professionally can drive the urgent and just transition required for a more sustainable future for all of Earth’s inhabitants. With Australia’s healthcare system having a large environmental footprint (i.e. a big four global per capita carbon emitter, accounting for 7% of Australia’s carbon emissions),1 the health professionals we graduate should be resource and planetary stewards in their professional and personal lives.

INTEGRATING PLANETARY HEALTH INTO MEDICINE AT BOND UNIVERSITY BEFORE IT WAS AN ACCREDITATION REQUIREMENT
Led by Professor Michelle McLean, the integration of Planetary Health (PH) in the Bond Medical Program began in 2018, with the introduction of a second-year assignment underpinned by the 2030 United Nations Sustainable Development Goals (SDGs), with a focus on SDG 13 (Climate Action). Our recent article in Frontiers in Public Health provides a five-year (2018-2022) summary of the ‘Products’ (planned action) created by teams of students for their identified planetary problem.2 Actions included innovative healthcare interventions, policy documents relating to rising temperatures and vector-borne diseases, a proposal to transition to electric ambulances and green points for environmental volunteer work.
The medical curriculum-wide integration began in earnest in 2019. It begins in the second week of the first semester with an Introduction to Planetary Health and includes concepts such as planetary boundaries, global environmental changes, SDGs, Indigenous ways of knowing, being and doing, e.g. natural resource stewardship. This is immediately followed by the Ecobiopsychosocial model of health and well-being, framed by a strong sustainability model (as opposed to the weak triple bottom line SDG model) of concentric circles with the outermost circle representing the environmental and ecological determinants of health. The first-year health promotion sessions are framed through a PH lens in that a healthy lifestyle that includes active transport and sustainable, healthy diets not only reduce the incidence of chronic disease but also lower the impact on the healthcare system (i.e. fewer resources used and reduced emission and waste) which ultimately benefits the planet. The second-year Social Justice session transitioned to Ecological Justice and has recently been revised to include Planetary and Earth System Justice. In the final year, General Practice students explore how healthcare can become more environmentally sustainable. In addition, a PH Masters subject is offered as an MD professional development project.
The revised Australian Medical Council Primary Medical Education Standards (and Outcomes) released in late 2023 now require all medical programmes to include climate change, environmental determinants of health, sustainability, and planetary sciences in their curricula. The Bond University Medical Program is thus in a good position to report on its progress in July 2024.
INTEGRATING PLANETARY HEALTH IN OTHER HEALTH DISCIPLINES
In Biomedical Science, Associate Professor Christian Moro and Ms Charlotte Phelps have been looking at innovative ways of integrating PH in an introductory



Physiology subject without overloading an already busy curriculum.3 In the first iteration, a ‘Did you know?’ PH ‘fact’ aligned with the weekly topic was included, linked to a relevant SDG.3 Examples include how body temperature can be regulated in a warming world and how agriculture can sustainably provide healthy food.4 The next delivery iteration followed a design-based research framework to include facilitated tutorial discussions around the PH ‘fact’.
In Nutrition and Dietetics, PH considerations span both the health and food sectors and so dietitians are wellplaced to be eco-ethical leaders for a positive way forward. Dr Kristen MacKenzie-Shalders has been advancing educational scholarship around environmental sustainability and PH within the discipline. She recently led a rapid review that explored frameworks for PH education 5 and, with several Australian dietitians and nutrition professionals, she also led the development of a pathway to personal, population and planetary health for the profession 6 . This framework is currently being converted into a toolkit for practitioners, funded by the International Confederation of Dietetic Associations. Kristen has also published on food service sustainability which has been integrated into learning and teaching in that domain.
References to be supplied upon request.
Authors: Professor Michelle McLean, Bond University.
Associate Professor Christian Moro, Biomedical Sciences and Medicine at Bond University
Ms Charlotte Phelps, Senior Teaching Fellow in the Bond University Medical Program. Dr Kristen MacKenzie-Schalders, dietitian, educator and advocate for pro-environmental change.
Top to bottom:UNDERSTANDING THE IMPACT OF BUSHFIRES ON PEOPLE WITH ASTHMA

Hunter Medical Research Institute’s Asthma and Breathing Research Program started intently focusing on bushfire smoke – otherwise known as landscape fire smoke - after the devastating bushfires in 2019 and 2020.
Program leader, Professor Vanessa McDonald, says, “Over the past three years, our researchers have rapidly expanded our work to better understand how landscape fire smoke is impacting people with asthma.
We’ve conducted surveys on quality of life, mental health and symptoms and found that people with severe asthma had real concerns about access to medication during bushfire events. Furthermore, pregnant women were worried about their babies’ health, and breastfeeding mothers were unsure whether it was safe to breastfeed during the bushfires.”
NEW BUSHFIRE SMOKE RESEARCH
Asthma and Breathing researchers evaluated toxins in breastmilk from mothers who were exposed to landscape fire smoke and found that two polycyclic aromatic hydrocarbons (PAH) – pyrene and fluoranthene – were detected. Despite this detection, the levels weren’t beyond a concerning limit.
Another interesting result from the group’s research was that they were able to match up particulate matter levels in the air with participants’ geolocation.
“We found that asthma symptoms persisted after the fires, with both acute and persistent symptoms. People with asthma who were exposed to landscape fire smoke and therefore increased particulate matter, also experienced laryngeal hypersensitivity for up to three months after the fires ended. This causes breathlessness, coughing and strain on the voice,” says Professor McDonald. Those with laryngeal hypersensitivity also had poorer asthma control, and more health care utilisation.
Surveys also identified that people with asthma were implementing some but not all personal mitigation strategies to deal with bushfire smoke, and only about half accessed information about mitigation strategies.
The research team joined forces with the Thoracic Society of Australia and New Zealand and Asthma Australia, the country’s peak professional and consumer bodies for asthma. Together with the TSANZ, Professor McDonald published the Australia, New Zealand position statement to guide clinicians who treat people with asthma who are at risk of exposure to landscape fire. The team also developed community focused infographics in collaboration with Asthma Australia, to provide credible and consistent evidenced based recommendations for people with asthma and the community.
“There are few randomised controlled studies of mitigation strategies,” says Professor McDonald. “This is why we’re looking at things like air purifiers, HEPA filters, masks and staying indoors. We have applied for funding to conduct a RCT on the use of HEPA filters in homes of people with asthma during landscape fire events.”
WHERE TO NEXT?
Professor McDonald says that while it’s well known that landscape fire events can increase the risk of hospitalisation and sometimes death for people with asthma, there’s still plenty that’s not well understood in this area.


“What our group is looking at now is the impact of bushfire smoke exposure during pregnancy and whether this is associated with epigenetic changes in the offspring.
There is evidence that exposure over time can lead to new diagnoses of asthma in both adults and children.
“Following the Hazelwood Mine fires in Victoria, for example, there was an increased incidence of physician diagnosed new asthma and children in that area reported higher levels of both asthma and respiratory infections,” says Professor McDonald.
Poor air quality – whether it’s from bushfire smoke, pollution from gas appliances, woodfire smoke from cooking and heating, moulds or things like exposure to cigarette smoke or vape smoke in the home – all have negative effects on respiratory health.
For people with asthma, things like dust mites, pollen, animal dander and cockroach faeces all play a role too, and then there’s the environmental impact of the inhalers themselves.
The Asthma and Breathing team is dedicated to finding answers; not just to inform care guidelines and mitigation strategies for people with asthma, but also to hopefully minimise the number of new cases of asthma that emerge as bushfires become more common.
“At the intersection of environmental health, our initiatives provide a comprehensive understanding of the broader

impact on respiratory well-being, contributing significantly to the development of a resilient and sustainable future,” says Professor McDonald.
“If you can’t breathe, you can’t do anything. Issues around air quality affect everyone so it’s really important that the general community, as well as people with asthma, know what to do when there’s smoke around,” she says.
 Author: Professor Vanessa McDonald
Professor Vanessa McDonald
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
Author: Professor Vanessa McDonald
Professor Vanessa McDonald
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
CHRISTOPHE KEREBEL
SAFEGUARDING CHILDREN’S HEALTH IN AUSTRALIA AMIDST CLIMATE CHANGE
The ever-growing spectre of climate change poses a substantial threat to the health of the most vulnerable members of society: our children.
While the impact of climate change on human health has been explored in various studies, there has been a notable lack of comprehensive assessments focusing on the magnitude of health effects children face.
In an effort to bridge this gap, researchers from the Wal-yan Respiratory Research Centre, The University of Western Australia and Flinders University, in collaboration with Population Matters, co-authored a systematic review and meta-analysis to unravel the intricate relationships between climate change and the health of children globally.
A first of its kind, the study identified a range of significant relationships between climate change and child health.
The most alarming revelation was the 60% increase in the average risk of preterm birth due to exposure to temperature extremes.
Additionally, respiratory diseases, mortality, and morbidity were found to be significantly influenced by climate changes, albeit to a lesser extent than preterm birth.
The impact of different air pollutants on health outcomes was smaller compared to temperature effects, but nonetheless, most pollutant studies indicated at least a weak effect.

The study’s lead author Dr Lewis Weeda, a researcher with the Wal-yan Respiratory Research Centre and The University of Western Australia, said the study showed that children were already affected by climate change, with health problems set to increase as climate change worsened.
“Increased preterm birth, more respiratory disease, higher mortality, and more children in hospital are but a few of the health problems societies will face as climate change worsens,” Dr Weeda said.
“Some health outcomes, such as preterm birth, will result in lifelong complications and costs.
“Several studies have shown that diseases that are affected by climate change, such as preterm birth and asthma, can incur significant financial costs to the health sector. For example, the cost of wildfire-associated smoke on asthma has been estimated to as much as US$1.5 billion due to a single fire season in the future. Another study estimated a single case of childhood asthma could cost up to US$23,500.
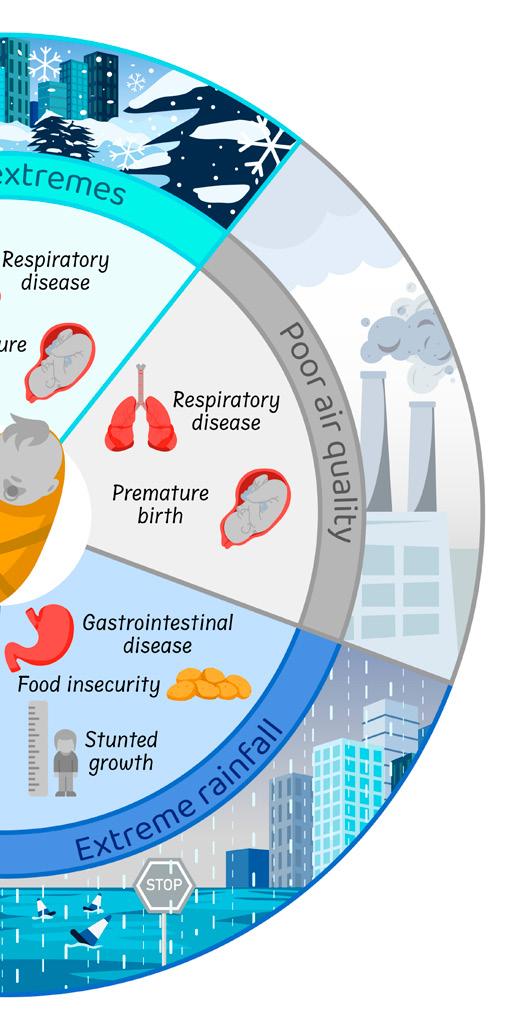



“The identified protective factors serve as a foundation for designing interventions that not only mitigate the health risks posed by climate change but also enhance the overall resilience of communities.”
The insights gleaned from this review are actively shaping several projects within the Wal-yan Respiratory Research Centre - a powerhouse partnership between Telethon Kids Institute, Perth Children’s Hospital and Perth Children’s Hospital Foundation.
Geospatial studies are under way across Australia, with a specific focus on Western Australian children and in particular Aboriginal children, to identify realistic solutions and mediating factors.
Among the factors being explored are public education of the health risks caused by climate change, promotion of personal behaviours to reduce environmental exposures, reviewing of health-service planning and allocation of resources to cope with the increases in climate-related hospital presentations, and upgrades in public housing to protect children from climate threats.
Relationships between climate change and child health
“Given that climate influences childhood disease, the social and financial costs will continue to rise as climate change worsens, placing increasing pressure on families and health services.”
Despite the grim findings, the team’s research also uncovered key protective factors against climate-related child health threats.
Economic stability and strength, access to quality healthcare, adequate infrastructure, and food security emerged as critical factors.
However, the susceptibility of these protective factors to local geographical, climate, and socio-economic conditions highlighted the need for targeted interventions tailored to specific communities.
Dr Weeda said the quantification of the magnitude of expected health increases in children is paramount for effective planning and mitigation strategies.
“Our findings underscore the urgency of addressing climate change to safeguard the health of current and future generations,” he said.
These initiatives aim to offer tangible, community-specific strategies to mitigate the adverse impacts of climate change on children’s health.
Dr Weeda said that without proactive measures, the social, financial, and health costs would escalate, leaving our children at increasingly higher risk.
“As we face the future, the imperative is clear: take action now to protect the health of the most vulnerable among us.”
The Science of the Total Environment paper is titled ‘How climate change degrades child health: A systematic review and meta-analysis’ and is available HERE . Dr Weeda is a doctor at Royal Perth Hospital who has an interest in environmental health and, specifically, how climate change can influence child health. He has been working at The University of Western Australia and with the Future Child Health research team at the Wal-yan Respiratory Research Centre, located at Telethon Kids Institute, since 2021. He believes an understanding of the determinants of health should inform clinical practice and policy to improve the long-term health of all people.
Author: Jacqui Caldwell, Communications. Specialist Telethon Kids, Wal-yan Respiratory Research Centre
PROVIDING EVIDENCE TO GUIDE PUBLIC HEALTH MESSAGES DURING BUSHFIRES
Bushfires are a national concern, especially in the face of climate change. The EMBER project aims to provide scientific evidence to support public health messages during bushfires.
Firestick farming, bushfire moons and capital cities enveloped in hazardous smoke haze. Australian summers have always been synonymous with scorching hot weather, planned burns and ferocious bushfires.
However, despite their increasing frequency, Australians are typically unaware of the health impact of inhaling bushfire smoke and how to minimise their exposure during bushfire smoke events.
The EMBER Study aims to address this knowledge gap, by undertaking an environmental assessment of bushfires and hazard reduction burns to understand pollutant profiles of smoke. This would provide scientific evidence to support policy decisions.
Environmental epidemiologist, Dr Dwan Vilcins from The University of Queensland Child Health Research Centre, is leading the study that will explore the respiratory and biological health effects of bushfire smoke on children, adults and firefighters.
“Smoke from bushfires and hazard-reducing burns, collectively known as bushfire smoke, is toxic and poses a significant threat to human health,” Dr Vilcins said.
“This project uses low-cost monitors to assess air quality during bushfires and hazard reduction burns in the outdoor air, penetration of smoke into the home, and measure biomarkers of smoke exposure measurable in urine. From this data we can build a complete picture of exposure from source to internal body systems and the resulting health effects.”
Collection of household dust samples, analysis of housing materials, house heating and cooling methods and how often people open their windows will also be examined. The hands-on project follows a successful pilot study of eight households across Southeast Queensland.
“Australia is unique globally because hazard reduction burns are well-regulated. We are working closely with local Councils and community groups so we can mobilise teams quickly to measure baseline health of participants before scheduled burns,” explained Dr Vilcins.
“This is a very difficult study to undertake, and we want to gather and analyse as much data as possible over the next 3 years so we can understand what bushfire smoke does to the body.”
The EMBER study is funded by the National Health and Medical Research Council and The Thoracic Society of Australia and New Zealand. EMBER will use drone technology from the United States Environmental Protection Agency to study particulate matter and other atmospheric toxicants released from the bushfires in real time.
The teams will also study charcoal from the bushfires, soil, and vegetation.
Dr Vilcins and her team are particularly keen to understand the impact of bushfire smoke exposure on children’s lungs.
“Airways are smaller in children, especially young children, and children also breathe more air per kilogram of body weight compared with adults, and therefore inhale more polluted air relative to their size,” Dr Vilcins said.
“Children’s detoxification systems are still developing, so environmental toxins take longer to effectively clear from their bodies.”
Researchers hypothesise that children’s behaviour and habits may also expose them to more environmental toxins than adults. For example, they tend to spend more time outdoors and ingest soil, dust and dirt as part of explorative play.
Recruiting participants for the study has proved the biggest challenge for the team.
“Prescribed burns and bushfires are unpredictable and weather dependent, so having a large contact list of participants is critical for the study,” Dr Vilcins said.
“Given this we are actively looking for volunteers to register their interest in participating, with a preference for families with children aged between 5 and 18.”
Households that sign up will be asked to monitor the air quality in their home so the team can understand if it worsens during bushfire smoke events.
“The study is open to everyone because we don’t know who the vulnerable will be. We know that people with



asthma will be vulnerable, but we want a broad sample of people so we can ascertain if there are any other vulnerable people or groups in our community.”
Results are expected to inform more effective public health advice.
“The Australian Government provides a set of recommendations to minimise risk during bushfire smoke, but we don’t know how many people implement those guidelines and if they implement them correctly,” Dr Vilcins said.
“Paediatric respiratory physicians on the team will also use results to improve clinical health recommendations. For example, could we be making better recommendations on what advice to give children or adults after bushfire smoke exposure?”.
As an early-career researcher, Dr Vilcins said attracting funding for the study is a personal achievement.
“I fell in love with this area while completing my Masters of Public Health because it brings together my passion for the environment and my passion for helping people,” Dr Vilcins said.
“Children will be more vulnerable than adults to the impacts of climate change and we need to have good data on the biological effects of bushfire exposure to inform public policy.”

 Author: Dr Dwan Vilcins, University of Queensland
Author: Dr Dwan Vilcins, University of Queensland

MOOD TRACKING STUDY TO HELP PLAN FOR MENTAL HEALTH SUPPORT

Healthy Minds researchers Dr Dara Sampson and Dr Louise Thornton from Hunter Medical Research Institute are launching a mood tracking app called the MindPulse Program to gather real-time data on people’s mental health.
With five simple questions, the researchers are hoping to understand the impact of a range of factors, including climate change and severe weather-related news and events, on people’s mental health.
Study co-lead, Dr Sampson, says that climate change intersects with mental health in the sense that the poorest and most disadvantaged groups in society tend to be the most affected.
Dr Sampson says, “Impacts of climate change are not being felt uniformly, with those people with least economic power being disproportionally affected. In recognition of the intersectional disadvantage climate change is exacerbating, real-time data on mental wellbeing is vital in order to provide a ‘snapshot’ of issues of concern across different locations and priority populations.
The MindPulse Program will launch in the Hunter region first and, contingent on funding, will hopefully roll out nationally.
The data from the app will be assessed to see what impacts people the most, whether it’s severe weather events like heat waves, storms, bushfires or floods, or
secondary impacts of climate change like increased food prices and energy bills.
“Similar to tools used to track outbreaks of flu, the MindPulse Program will revolutionise the way Australia collects and utilises mental health and wellbeing information,” says Dr Sampson.
The data that is collected will enable healthcare providers, researchers and government agencies to mobilise interventions and support, thereby challenging individual approaches and reshaping the mental health policy landscape.
GIVING A VOICE TO REGIONAL AUSTRALIA
Dr Sampson’s research group has considerable experience using digital tools in the mental health space. The team launched Eclipse, a digital support tool for people recovering from drug and alcohol addiction.
In the same way digital tools can provide an ‘always on’ service to people everywhere, Dr Sampson says that things like the MindPulse Program are able to provide information on mental health sentiment in regional, rural, and remote areas that are notoriously underserviced by mental health services.
“There’s a real service delivery issue because there’s high staff turnover in these areas,” says Dr Sampson.
People who live and rely on the land for the livelihoods have always been among the first to feel the brunt of natural disasters when crops get wiped out or herds are decimated.
“By engaging consumers as researchers that are contributing to a data set, people feel as though they have voice and a purpose.
“One of the main challenges of climate change is that it can feel so big. What can one person do? Climate change is one of the most politicised things in the last 20 years. There are still people, including politicians, that are saying climate change is not real. This creates a lot of doubt and uncertainty, as well as a lot of inaction, for people. Sometimes when things feel overwhelming it can be hard to know what to do to make a change,” says Dr Sampson.
THE GOAL OF STAGE ONE
The goal of the first phase of the project is to get enough information to meet an academic and practitioner level of acceptability.
“The next step will be to ask how we can use that data to shape services delivery and inform policy,” says Dr Sampson.
“Once we know what the needs are, we can work out how to service these cohorts of people.”




The researchers are currently finalising the questions for the app through their Expert Advisory Group to be loaded into the prototype.
Then they will recruit the first round of participants to create the first mental health snapshot looking at general wellbeing.
Once this is done, Dr Sampson and her team will start adding questions about the environment and other structural things like the impact of Reserve Bank of Australia interest rates rises, housing prices, rental market prices, the cost of groceries, electricity and gas.
“What impacts people crosses over into climate change,” says Dr Sampson,
“What happens if we move away from fossil fuels? This is a big thing for the Hunter region as there will be job losses. Climate change affects everything from jobs right through to food security right through to land security.
“The annual cost of mental health to the economy is $220 billion. This is through a loss of productivity as well as the cost to our under-resourced health system,” says Dr Sampson.
“As climate change gathers pace, there will be increased debate about whether we should adopt mitigation strategies or adaptation strategies.
“The recommendations are that the biggest polluters will attract the biggest penalties to level the playing field for poorer countries that are impacted more but pollute less.
“Australia is going to be high on the list of the big polluters so the penalties could be steep. That financial impact will ripple through the economy and, once again, hit the poorest, most disadvantaged people the hardest,” says Dr Sampson.
Author: Emma Castle – HMRI Media, PR & Content SpecialistMITIGATING THE MENTAL HEALTH IMPACTS OF CLIMATE CHANGE

Associate Professor Fiona Charlson’s research is at the forefront of efforts to understand and address the mental health impacts of climate change.
Associate Professor Fiona Charlson was attending the World Health Organisation (WHO) Mental Health forum in Geneva in 2019 when she realised more research was needed to measure the impact of climate change on mental health.
“I had been a public mental health researcher collaborating with WHO for several years and I was asked to speak at a breakout session on mental health in disasters because
Left to right - Dr Suhailah Ali, A/Prof Fiona Charlson, Ms Kisani Upward, Prof Jemaima Tiatia Siau.the Black Summer bushfires had just broken out in Australia,” Dr Charlson said.
“I realised research and policy was not up to speed in this space at all – we really didn’t understand the mental health impacts of increasing frequency and intensity of disasters as a result of climate change. I also realised I wasn’t going to address challenging global mental health research questions with my skillset alone; and that I needed to form a multidisciplinary team for research collaboration.”
On her return to Brisbane, Dr Charlson established the world’s first mental health and climate change network at The University of Queensland to understand and address the mental health impacts of climate change.
“Australia is a country that has always experienced natural disasters, and we have always had a mental health response. But these are not one-off events anymore and we don’t know if the myriad of mental health interventions that exist work in today’s climate change context,” Dr Charlson said.
“Take the floods in Lismore for example, we now have populations that are displaced – people lost their homes; they were mentally and physically exhausted and they didn’t have time to recover before the next flood.”
Shifting climate patterns also lead to food and water insecurity, social unrest, forced migration, disruption to healthcare access and other challenges that destabilise the conditions needed to protect mental health and care for those with mental illness.
“The mental health impacts of climate change are on a spectrum, but there is increasing evidence of depression, anxiety, and PTSD. There is also evidence of mental health-related hospitalisations and deaths associated with heatwaves,” Dr Charlson said.
“Climate anxiety is also on the rise and young people, in particular, are acutely aware of climate change and they are seeing media reports and feel anxious about what the future looks like.”
Despite the prevalence of extreme weather events, Australia does not have a standardised way of measuring the impact of climate change on mental health.
“This is something I know policymakers want, but we are still in the process of working out a methodology to measure mental health impacts,” Dr Charlson explained.
“Some potential ways might be using existing health surveys and then linking those to weather data and climate hazards; or analysing health data records in relation to particular weather events.”
Dr Charlson worked with the Federal Government on the National Health and Climate Strategy, released in December 2023, and said it’s a progressive document.

“This new strategy is one of very few in the world – the only one in the world I know of – that actively tackles mental health and climate change,” Dr Charlson said.
“It’s a really bold document that provides a whole-ofgovernment approach to address the health and wellbeing impacts of climate change and the contribution of the health system to climate change.”

Worldwide, communities are also coming together to develop a global research agenda to understand and respond to the deep interconnections between climate change and mental health.
Dr Charlson serves as the Oceania Regional Community Convenor for Connecting Climate Minds; an international community of practice that brings together climate and mental health communities in research, practice and lived experience.
“Connecting Climate Minds is a global project coming to a close soon, and we have undertaken considerable consultation in the Oceania region over the past 12 months to identify priority research areas,” Dr Charlson said.
“180 research topics emerged from our consultation, and we had the pleasure of launching our Regional Research and Action Agenda at a global event in March 2024.”
Longer-term, Dr Charlson believes a lot of solutions for addressing climate change mental health challenges will come from within the community.
“First Nations peoples, for example, have been trying to tell us how to manage our environment for a long time, but we keep ignoring that advice,” Dr Charlson said.
“Mental health is a Western concept, and we need to challenge fundamentals on how we conceptualise mental health for many cultures, who see mental health as a holistic concept that is intrinsically linked to land, water, culture, spirituality, ancestry, family and community.”
Exploring the development of community-based interventions to mitigate the mental health impacts of climate change is also a research focus for Dr Charlson.
“Communities typically know the best way to deal with extreme weather events, and I think there needs to be a shift from the current response of ramping up specialised mental health services to developing community-based support systems informed by local knowledge,” Dr Charlson said.
“For example, trained community-led groups could potentially provide basic psychological support – this approach has been advocated for decades in other countries and I think there is potential for those models to be trialled here.”

REEF RESEARCH LEADS TO NEW INSIGHTS ON CLIMATE CHANGE AND WELLBEING
Community-based research shows that losing places, ecosystems and species we love can lead to ecological grief, but taking action on climate change can benefit mental health and wellbeing.


Researchers at UQ are exploring the impact on communities living near the Great Barrier Reef and identify ways to support their long-term wellbeing.
Climate change is now a leading threat to physical and mental health and wellbeing, affecting a growing number of communities across the world. Climate change can reduce our quality of life, including emotional and social wellbeing, but it does so in complex ways that are only just starting to be understood.
Now, research at The University of Queensland is exploring how eco-emotions associated with climate change and loss of biodiversity, such as eco-anxiety and ecological grief, influence our wellbeing.
Dr Claudia Benham, an Australian Research Council Discovery Early Career Research Award fellow at UQ, is exploring how climate change affects our emotional wellbeing through eco-emotions such as ecological grief.
Dr Benham works with communities to understand their links to the places they live in, and love, and how the impacts of climate change contribute to their ecoemotions and affect wellbeing.
UNDERSTANDING ECOLOGICAL GRIEF
Ecological grief refers to a sense of loss related to losing places, ecosystems or species of importance to us. Dr Benham’s research has shown that ecological grief happens when places we love and value decline
The first stage of research, a global literature review, identified how ecological grief arises in communities across the world, suggesting that it is linked to our attachments to places, ecosystems and species, and how these contribute to who we are.
The literature review also showed that social inequities contribute to ecological grief, suggesting that future policy solutions need to address both socio-economic and environmental dimensions of climate change.
When communities are empowered to tackle the source of environmental losses, or are confident that they are being addressed, ecological grief is less likely to occur.
WORKING WITH COMMUNITIES
Over the next two years, Dr Benham’s research will explore how the emotional wellbeing of communities near Australia’s iconic Great Barrier Reef is affected by climate change.
Coral reefs are among the ecosystems most exposed to climate change , and they support livelihoods and community wellbeing for an estimated one billion people worldwide. The Great Barrier Reef is undergoing a mass bleaching event for the fifth time in eight years
Decline in coral reef ecosystems directly impacts the wellbeing of local communities who depend on them



Understanding how changes to reefs, such as coral bleaching, affect local communities and different social groups, including the young and elderly, Indigenous peoples and people of diverse genders, is critical to longterm community wellbeing.
This research asks the question: What happens to our emotional wellbeing when places we love are affected by climate change, and what can we do about it?
It will also explore how novel forms of governance and decision making, centred on place-based deliberation and ‘kitchen table’ conversations can help communities cope with climate change and lead to empowerment.
By understanding how environmental losses affect local communities, we can motivate action on climate change while also helping to support communities already experiencing its effects.
DEVELOPING INTERDISCIPLINARY SOLUTIONS
Complex challenges like climate change require interdisciplinary research and solutions.
Place-based research on climate change and wellbeing plays an important role in understanding how these challenges play out at the local scale, and how solutions can be tailored to individual contexts, helping to identify supports that work for each community.
Ultimately, though, taking action on climate change is the only way to reduce ecological grief associated with losing places, ecosystems and species we love. By highlighting the impacts of climate change on mental health and wellbeing, this research suggests that tackling climate change has broad benefits for the wellbeing of people, as well as the environment.
Author: Dr Claudia Benham, The University of QueenslandADDRESSING THE CHALLENGES OF RARE DISEASES

The
Rare Disease Awareness, Education, Support,
and
Training
(RArEST) Project is a partnership between the national peak body for Australians living with a rare disease, Rare Voices Australia, and researchers from three universities.
Together with the rare disease community, the RArEST Project is co-producing resources to support the implementation of the Australian Government’s National Strategic Action Plan for Rare Diseases.
Imagine there was a health condition that impacted 2 million Australians, including an estimated 400,000 children. A condition responsible for over a quarter of neonatal intensive care unit (NICU) admissions, and where 30% of children with the condition survive less than 5 years. Imagine it was difficult to diagnose, with many individuals seeing six or more physicians and receiving at least one misdiagnosis across at least 5 years before a correct diagnosis was made. Imagine the condition was poorly understood and, for over 95% of individuals, there was no curative treatment available.
There is no such single condition. However, if you consider the over 7,000 different rare diseases collectively, these statistics describe the situation for the estimated 2 million Australians living with rare disease.1,2 A rare disease is defined as a condition affecting less than 5 in 10,000 people. Though each rare disease is unique,
there are many shared challenges for people living with rare disease. The rarity of these conditions means there is a lack of societal and clinical awareness, resulting in diagnostic delays, insufficient societal supports, underfunded research, and paucity of investment in therapeutic development. 3,4 This disparity creates a greater health inequality, characterised by poor health outcomes, increased stress, mental health challenges, and significant financial burdens.1,3 These challenges are internationally acknowledged, with global efforts leading to the United Nations recently adopting a resolution to address the needs of people living with rare diseases, emphasising the need for inclusive policies, effective data sharing, and strengthened health care systems.5
THE RAREST PROJECT
The rare disease community’s systemic advocacy has long driven policy change across the world. In Australia, rare disease organisations, through the national peak body for Australians living with a rare disease, Rare Voices Australia (RVA), co-designed the Australian Government’s National Strategic Action Plan for Rare Diseases (the Action Plan) alongside other key stakeholders in the rare
disease sector.6 This plan, supported by all major political parties, was officially adopted by the Federal Government in 2020. As part of the collaborative implementation of the Action Plan, the Department of Health and Aged Care funded the Rare Disease Awareness, Education, Support, and Training (RArEST) Project, a collaborative initiative between three universities and RVA. This three-year project, due for completion in June 2024, has been codesigning a suite of resources to empower and support people living with rare disease, clinicians, and advocacy groups. The project closely links to other national rare disease projects including the Rare Awareness Rare Education (RARE) Portal and the RARE Helpline
The RArEST Project has the same overall goal as the Action Plan – the best possible health and wellbeing outcomes for Australians living with a rare disease. The term “people living with a rare disease” includes individuals diagnosed with a rare condition as well as those with a suspected rare condition or an undiagnosed disease. The term also includes the families and carers of these individuals, recognising that a rare disease can have impacts on the whole family unit. Across three streams, the RArEST Project has focussed on support for individuals and families through mental health resources; education for health professionals about rare disease, including the recently released National Recommendations for Rare Disease Health Care7; and improving capacity for systemic advocacy.
PRIORITISING LIVED EXPERIENCE
The participation of individuals living with rare diseases across all three streams has ensured that the project remains focussed and driven by the real needs of this diverse community. In addition to the lived experience of advocates at RVA, the project team brought together a remunerated consumer reference panel comprised of 12 people with lived experience of rare disease. This group has proven critical to the project – their insights and perspectives have shaped the direction of the project’s outputs at every stage and have enriched the resources with the authentic voice of the rare disease community.
CROSS-SECTORAL COLLABORATION
As an innovative partnership between advocacy organisations, academics, and clinicians, the RArEST Project aims to strengthen the support framework for people living with rare disease by emphasising the collective approach to education, resource development, advocacy, and policymaking. This approach has been central to the networks and resources developed throughout the project (see Box 1). By taking a “disease-agnostic” approach, the collective strengths of the rare disease community can be harnessed, with awareness efforts not being fragmented between the diverse range of conditions, but focussed

on approaches that support people regardless of which condition they have. Bringing stakeholders together has enabled knowledge translation that recognises diverse perspectives across a complex system. References are available upon request.

NETWORKS AND RESOURCE
BEING PRODUCED BY THE RAREST PROJECT
Mental health and wellbeing
• Mental Health First Aid Training and support resources for rare disease organisation leaders
• Rare disease training for mental health professionals
• Co-designed mental health and wellbeing resources for the rare disease community
Clinician education
• ‘Rare Disease 101 Australia’ eLearning course for health professionals, hosted on the international Medics4RareDiseases website
• Two series of a Rare Disease Project ECHO® Community of Clinical Learning Practice
• National Recommendations for Rare Disease Health Care7
• Lyfe Languages Rare Diseases Module
Advocacy capacity building
• Australian Rare Disease Organisations Community of Practice
• Multistakeholder Toolkit to support systemic advocacy
• System simulation workshops
Authors: The RArEST Project authors and collaboration includes: Dr Elizabeth Emma Palmer, Prof Adam Jaffé, Prof Michelle Farrar, Dr Lauren McKnight, Natalie Roberts, Krista Recsei, and A/Prof Chinthaka Balasooriya, from the University of New South Wales; Nicole Millis, Louise Healy, Dr Falak Helwani, Isabella Hixon, and Sarah Cannata from Rare Voices Australia; Prof Yvonne Zurynski and Christina Rojas from Macquarie University, Prof Gareth Baynam, Sue Baker, Sian Gannon, and Kaila Stevens from the University of Western Australia and the Rare Care Centre, Perth Children’s Hospital; and Rani Ong and Yarlalu Thomas from Lyfe Languages.
CHILDREN ARE DISPROPORTIONATELY AFFECTED BY SEPSIS: IT CAN HELP

In the first 12 months of life, children are disproportionately affected by sepsis and are at most risk of death from the condition.
Despite increased awareness and clinical initiatives, sepsis remains a growing health problem that impacts very young children more than others. Tailored health information systems may be able to help.
Sepsis is a life-threatening condition and a significant cause of death and disability in Australia and across the world. The earlier sepsis is detected, the faster treatment can be initiated, increasing the change of survival. Over the last 20 years, the use of IT in healthcare has rapidly advanced and is now aiding in sepsis care. Computerised clinical decision support (CCDS) systems, with integrated sepsis detection tools, support clinicians to identify and manage sepsis patients as timely treatment, such as antimicrobial therapy, fluid resuscitation and vasopressor use, save lives.
However, while CCDS systems have been implemented widely, there is little evidence of how effective they are for paediatric and neonatal patients compared to adult patients, despite the high burden of sepsis in this vulnerable population.
Associate Professor Ling Li from the Australian Institute of Health Innovation, Macquarie University, has led two
studies providing new evidence to support the case for improving detection among paediatrics. The nation-wide longitudinal sepsis epidemiology study, the first of its kind undertaken in Australia, reported the incidence and mortality of sepsis based on 24 million hospitalisations in 739 Australian hospitals over 5 years. This showed children under one year were disproportionately at risk of sepsis and had poor outcomes. A later scoping review investigating CCDS systems, and published in JMIR Medical Informatics, revealed a dearth of evidence for use with very young patients. The study highlighted the need for a consensus definition for paediatric and neonatal sepsis and further research on the usability and cost effectiveness of CCDS systems in these settings.
A key problem for paediatric sepsis is that many aspects of clinical practice currently rely on expert consensus and evidence from adult sepsis. Together, both studies highlight that for CCDS systems to deliver the results specific for neonatal and paediatric patients, they cannot be clones of systems used for adults but must be developed with specific criteria for children.
The case for developing CCDS systems fit for purpose is urgent. Children under the age of one are at the highest risk from sepsis. Of those that survive paediatric or neonatal sepsis, they often live with resulting physical disability or neurological impairment and have a poorer health-quality of life than children who have not had sepsis.
Associate Professor Li’s research showed that for every 100,000 children under one year of age in hospital in Australia, almost 7,000 have a sepsis diagnosis and more

males are diagnosed than females. Children under one who underwent surgery were more likely to have sepsis than their peers in hospital who did not have surgery.
Children under one in very remote areas or from low socio-economic backgrounds are particularly at risk of sepsis requiring hospitalisation. Being from an Aboriginal or Torres Strait Islander (ATSI) background was not associated with a greater risk for children under one, but the older ATSI children (>1 year old) were more likely to have sepsis than non-ATSI children.
Importantly, children are most likely to be hospitalised with something other than sepsis as the primary diagnosis. Sepsis is often a secondary diagnosis perhaps pointing to a delay in identifying sepsis or barriers to being able to classify symptoms under an existing sepsis clinical code.
During the study period, hospitalisations for sepsis increased for children under one, however mortality rates remained much the same. This is attributed to a welcome increase in awareness within the clinical and general population of the risk of sepsis, leading to earlier interventions. Public awareness campaigns and clinical training (particularly by the Australian Commission on Quality and Safety in Health Care) have both contributed to improved recognition, earlier treatment and better documentation.
This is welcome news but there remains much to be done to improve detection and care for neonatal and paediatric patients. Paediatric specific CCDS systems can play a critical part.
CCDS systems rely on embedded data and clinical guidelines. Unfortunately, while there is currently no

formal definition for neonatal sepsis, and the definition for paediatric sepsis is very broad covering children up to 18 years old, their effectiveness is hamstrung. The enormous diversity and variability of how children at different ages present with sepsis needs to be studied more closely and used to develop new consensus guidelines and criteria for CCDS systems. It is much more than adjusting the thresholds for monitoring vital signs.
All CCDS systems, and especially those for neonatal and paediatric settings, need to consider useability requirements. Careful calibration of CCDS systems is required for instance to reduce false alarms and alert fatigue where clinicians become overwhelmed by and then overlook alerts.

Further, research is also required to demonstrate the cost effectiveness of implementing CCDS systems in paediatric and neonatal settings. Given the enormous burden to the health system of death and disability from sepsis, investment in fit for purpose CCDS systems, that have the potential to improve outcomes for children, may prove economically beneficial and a wise use of resources.
With early detection the key for surviving sepsis, and the potential for paediatric specific CCDS systems to make a difference, Associate Professor Li’s program of research clearly identifies the next steps toward lessening the impact of this serious condition among babies and children, while also reducing the burden on the health system.


Authors: Ling Li is Associate Professor at the Australian Institute of Health Innovation, Macquarie University, leading the Health Analytics and Patient Safety research stream. Chrissy Clay is Media and Outreach Consultant for the Australian Institute of Health Innovation.
OLD AND NEW KNOWLEDGE COMBINE TO TACKLE CLIMATE CHANGE HEAD ON
A national research network grounded in Aboriginal and Torres Strait Islander knowledge and wisdom is working to help protect Australians from the health impacts of climate change. We look at progress so far within the Western Australian node, led by Associate Professor Brad Farrant from Telethon Kids Institute.

As authorities seek to address the growing challenges caused by climate change –regarded as the biggest global health threat of the 21st century – a transformative national network has emerged to ensure the voices of those most affected are central in planning and decision making.
Under the $10 million, NHMRC-funded Healthy Environments and Lives (HEAL) Network, collaborative communities of practice are being formed all over Australia to identify and catalyse health research to provide the evidence, capability and tools needed to address these issues.
Put together by researchers working with people from all walks of life – and in recognition of the fact that Indigenous people are among the groups most impacted by climate change – the network aims to weave Indigenous knowledge and science with together western science to address climate-related challenges including urban health,
bushfires, air, soil and water pollution, food security, biosecurity, heatwaves, and other extreme events.
Led by Professor Sotiris Vardoulakis at the University of Canberra but with multiple nodes across the country, HEAL comprises hundreds of people across Australia, including multidisciplinary researchers from dozens of tertiary and other institutions, community members, policymakers, and service providers.
The WA node includes researchers from Telethon Kids Institute, The University of Western Australia, Curtin University, Edith Cowan University, and Murdoch University. Led by Telethon Kids Institute’s Associate Professor Brad Farrant, the node is working to set up six communities of practice across the State.
“The idea is to bring all the community and other core stakeholders together in a conversation to actually work out how we’re going to best face and deal with what’s

happening already and what’s coming towards us with climate and other environmental change,” Associate Professor Farrant says.
“It’s a bit of a platform from which we can enable good conversations to do good work the right way with community, and then we’ve got to go and make sure we can get the resources to do it.”
That good work includes providing robust scientific evidence to underpin structural policy and practice changes that support long-term solutions.
In WA Dr Farrant is co-leading much of this work with Yamatji Elder Aunty Mara West – Chair of the HEAL WA Aboriginal Steering Group and a cultural governance advisor at Telethon Kids – to ensure Aboriginal wisdom and knowledge are at the forefront of discussions, projects and solutions.
“That’s the reason I’ve joined the HEAL Network –because it actually recognises and respectfully weaves together Aboriginal science with mainstream science,” Dr West says.
“This is so important, especially for our mob out in communities, but it’s been missing from the equation for a long time and I personally think that’s why the gap is widening instead of closing. The fact HEAL does this is why it’s so different from so many other programs out there.”
HEAL has been funded by the NHMRC for five years but Associate Professor Farrant and Dr West say that funding – spread across the different nodes – cannot, by itself, sustain all the work needed. Already the WA node has sourced important supplementary funding from organisations like the Stan Perron Charitable Foundation to help set up the State’s communities of practice properly.
“The importance of the original HEAL funding is it has given us some sort of starting point,” Dr Farrant said.
“This needs to be seen as groundwork that’s setting up the collaboration, relationships, and trust that are required, but there’s a real need for future funding to keep the momentum going and deliver in meaningful ways.”
Dr West says this is essential to overcome the distrust

often felt within communities who have become used to being promised a voice, or effective programs, only to have them de-funded.
“HEAL WA and our Aboriginal Steering Group have taken off in a big way – we’ve had the kind of response from the community we didn’t think we would have,” she says.
“A lot of people out there really want this sort of information and want to be involved in projects that can make a huge difference to communities, but building trust, and consulting and co-designing projects properly takes time. To have long-term benefits you have to have longterm funding, otherwise you just leave the communities high and dry.”

Conversations held under the HEAL WA banner so far have included a focus on appropriate language, with Dr Farrant saying the phrase ‘climate change’ can be a barrier due to politicisation of the conversation.
“If you start yarning instead to mob in particular about changes to Country, they are all seeing that and they’re really concerned about those changes and what they can mean culturally,” he says.
Priorities to emerge from community conversations under the HEAL WA banner so far include concerns about water availability and quality, protection from heatwaves, and a desire to see the expansion of Aboriginal Ranger programs.
“These are the people who are going out on and looking after Country, who have first-hand experience of the changes that are happening out there,” Dr West says. “They’re really concerned, especially the young people, because Country is changing so dramatically.
“The Ranger program is one of the very few programs the youth are really wanting to be part of – it’s so important that we support it in any shape or form that we can.”






CHANGING THE NARRATIVE
Ovarian Cancer Research Foundation (OCRF) is Australia’s largest independent funder of ovarian cancer medical research. Ovarian cancer is one of the most lethal cancers with a five-year survival rate that has barely changed in 50 years, languishing at under 50%. It is also chronically underfunded. Addressing health disparity and funding inequity in cancer research is fundamental to achieving higher survival rates for ovarian cancer.
The OCRF plans to change this narrative and improve outcomes for ovarian cancer patients now, and in the future, through raising awareness, advocacy, and funding innovative research.
The OCRF galvanises community efforts to generate critical funds for research, investing over $17 million since 2014. OCRF funds are 100% raised by the Australian community: dedicated corporate partners as well as mothers, fathers, sisters, brothers, sons and daughters, other family and friends, stepping up to raise urgently needed money for this important cause.
Guided by an International Scientific Advisory Committee and Consumer Panel, OCRF funding
targets four key areas: prevention, early detection, better treatments and managing recurrence. Investments focus on support for early- and midcareer ovarian cancer scientists, via the annual OCRF National Research Grants Scheme.
OCRF is a strong voice for collective action — advocating alongside others in the sector, major partners, and the community, to improve outcomes for ovarian cancer patients now, and for future generations.
Since 2014, the OCRF has funded 35 researchers in 20 medical research institutes across Australia and New Zealand, with vital initiatives including:
• dedicated specialist ovarian cancer research scientists
• critical studies in early detection research
• development of new technologies that promise more targeted treatment options to improve quality and length of life
• collection and management of ovarian cancer tissue samples for research
Three recent grants totaling $2.1 million will support Australian researchers investigating an early detection approach; a vaccine treatment option, and a drug combination treatment to target a rare subtype of the disease.
Together, we will overcome ovarian cancer.
CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
NEW MEMBERS



CENTRAL QUEENSLAND UNIVERSITY’S APPLETON RESEARCH INSTITUTE
The Appleton Institute at CQUniversity engages in applied and industry-led research projects that focus on improving individual, organisational, occupational and community health, safety and resilience.
Appleton’s work focusses on:
• the interactions between work patterns and practices for safer and healthier workplaces,
• design, implementation and evaluation of interventions to support wellbeing and resilience, and
• optimising health-related behaviours to benefit physical and mental health.
The Appleton Institute combines excellence in research, teaching and community engagement across a range of basic and applied research areas including behavioural health (sleep, physical activity, sedentary behaviour and nutrition), human factors and operational readiness (occupational health and safety, risk management, complex systems, rostering and shiftwork), and resilience and wellbeing, particularly in the regions.
The Appleton Institute is made up of four research Groups and Clusters.
HUMAN FACTORS AND OPERATIONAL READINESS GROUP
This Group has a focus on safety, performance and wellbeing in the workplace, to support individuals, industries and communities. At the core of our research is relationship between people and technologies, tools, environments, and systems. In partnership with industry and community groups, our program of work considers short, mid and long-term
physical and psychological health, as well as social, occupational and domestic impacts of nonstandard patterns of work.

PHYSICAL ACTIVITY RESEARCH GROUP
This research Group aims to advance the science of physical activity and related health behaviours, such as diet/nutrition, sedentary behaviour, weight loss/ maintenance and sleep. We develop and evaluate innovative intervention strategies to improve health behaviours at an individual and population level, both in healthy populations (e.g., children, elderly) and populations with health conditions (e.g., people with diabetes, cardiovascular disease, depression).
SLEEP AND BIOLOGICAL RHYTHMS GROUP
The Appleton Institute has a world-class sleep research facility at CQUniversity’s Adelaide Campus where this group conducts a range of basic and applied research projects related to the sleep/ wake and circadian systems of children and adults. We examine the effects of sleep loss and circadian disruption on cognitive function, accident risk, physical health, and mental well-being; we develop, implement, and evaluate tools, procedures, and systems to minimise fatigue risk in safety-critical workplaces; and we collaborate with industry and government stakeholders to inform policy and practice regarding safe hours of work.
CLUSTER FOR RESILIENCE AND WELLBEING
This Cluster provides leadership and expertise in resilience and wellbeing research from the individual, occupational, and community levels, including a focus on regional and rural issues. Our goal is to undertake research within the communities we serve, to improve the resilience and wellbeing of all Australians. The Cluster works with our partners to undertake applied and translational research in different settings to develop practical solutions to the challenges facing Australian communities.
The Appleton Institute actively engages with the health industry, forming partnerships to facilitate research collaborations, knowledge exchange, and innovation implementation.
CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL
NEW MEMBERS




SHAKE IT UP AUSTRALIA FOUNDATION



Shake It Up Australia Foundation is a notfor-profit organisation established in 2011. In partnership with The Michael J. Fox Foundation for Parkinson’s Research (MJFF) we promote and fund Parkinson’s research in Australia.
Founded by entrepreneur Clyde Campbell AM after he was diagnosed with Parkinson’s at the age of 44, Shake It Up Australia’s mission is to accelerate innovative research and treatments to slow, stop and cure Parkinson’s disease (PD). Together with MJFF, we are the largest nongovernment funders of Parkinson’s research across multiple institutes in Australia. Our funding model ensures efficiency, eliminates redundancy, and embraces international collaboration in the quest for a cure. 100% of all donations we receive are directed to innovative medical research right here in Australia, and every research project is assessed and validated by an expert panel of scientists at MJFF.
Recent research projects we have funded include:
• The Australian Parkinson’s Genetics Study at QIMR Berghofer Medical Research Institute, which aims to crack the genetic code of PD and contribute towards the largest global study of Parkinson’s genetics ever undertaken.
• Upgrading and expanding a world-class clinical trials hub at The Alfred Hospital, to create a blueprint for a nation-wide, best practice Parkinson’s clinical trials unit.
• Nix gene therapy research at NeuRA, which aims to develop a new gene therapy to increase Nix expression in the brain cells of patients with PD and slow the progression of the disease.
To date, Shake It Up has funded 79 research projects at 23 research institutes to the value of $30.7 million.
CHRISTOPHE KEREBEL CHRISTOPHE KEREBEL CHRISTOPHE KEREBELTHE LAST WORD SETTING HIGH STANDARDS OF INTEGRITY AND SCIENTIFIC RIGOUR

As the nation’s leading expert body in health and medical research, National Health and Medical Research Council (NHMRC) sets high standards of integrity and scientific rigour and champions the pursuit of better health outcomes for all Australians.
NHMRC is a statutory authority of the Australian Government responsible for funding high quality research to build capacity, support researchers, encouraging the translation of research into better health outcomes and promoting the highest ethical standards.
As the new CEO of NHMRC, Professor Steve Wesselingh reflects on the important role of health and medical research for addressing the challenges posed by our rapidly changing climate.
Climate change is one of the most pressing threats to human health and wellbeing globally. In this era of
environmental uncertainty, NHMRC is passionate about fostering innovation that not only advances healthcare but also enhances environmental resilience against climaterelated health risks.
The escalation of global warming presents unparalleled practical and ethical challenges to the health sector worldwide that demand immediate action. Understanding the intricate relationship between climate change and public health is paramount—from the rising temperatures to extreme weather events, the impacts will be extreme and far reaching.
At NHMRC, we are actively prioritising research into climate-related health risks, aiming for a comprehensive understanding of emerging threats and consequently, a national resilience to environmental change.
Since 2010, NHMRC has funded and supported more than $31 million on various grants relating to climate change.
A major health priority for NHMRC is strengthening resilience to emerging health threats and emergencies, including environmental change, pandemics, and antimicrobial resistance.
We aim to achieve this by enhancing research capacity and capability, and funding research that will improve Australia’s preparedness and responsiveness to human health threats from changing environmental conditions and extreme weather events.

We are forging partnerships with international research institutions, sharing knowledge, and collectively working towards innovative solutions that transcend borders. By prioritising research that not only identifies health risks but also empowers communities with the tools and knowledge to adapt and thrive, NHMRC is contributing to a healthier, more resilient future.
A few years ago, the Healthy Environments and Lives (HEAL) National Research Network was formed to provide a catalytic stimulus to improve Australia’s current capability and capacity in human health and environmental change research, by supporting a single, multidisciplinary, nationally focused, collaborative network of researchers across Australia.
The network, supported by a $10 million NHMRC grant, was established to help understand the complex interaction between primary, secondary, and tertiary health effects of environmental and climate change, systematically assess health risks, develop mitigation and adaptation plans, and estimate the cost-benefit of strategies addressing the impact of environmental change on human health.
NHMRC intends to invest a further $5 million through a forthcoming Targeted Call for Research (TCR) that will invite research proposals on climate-related health impacts and effective interventions to improve health outcomes that identify key areas of vulnerability and effective interventions to improve health outcomes and



reduce health inequities in Australia. I also welcome the government’s first National Health and Climate Strategy, which was published in December 2023. This strategy outlines priorities for the next 5 years to address the health and wellbeing impacts of climate change, focusing on building healthy, climate-resilient communities and a sustainable, high-quality, net-zero health system.
We will also work alongside many stakeholders who will play important roles in implementing this strategy. For example, the Australian Centre for Disease Control (CDC) who will work with us to protect Australia from public health threats and improve the health of all Australians.
The interim CDC is part of the Department of Health and Aged Care and is growing in a phased approach, with an initial focus on improvements in preparing for public health emergencies, improving the national public health surveillance system and building capability in One Health and health security.
The health and medical research sector can significantly contribute to achieving these objectives by conducting rigorous research to understand the complex interplay between climate change and human health, developing innovative solutions and technologies to mitigate adverse effects, and collaborating with stakeholders to implement evidence-based interventions that protect public health amidst a changing climate.
Through innovation, collaboration, and a steadfast commitment to public health, NHMRC envisions a future where healthcare not only heals but also safeguards our planet for generations to come.
Author: Professor Steve Wesselingh, CEO, NHMRC
