





Three years on from the final report of the Royal Commission into Aged Care Quality and Safety, the impact is still being felt.
The Government is well advanced in many of its initiatives, with new aged care standards, new aged care quality indicators, star ratings for residential aged care and a serious incident response scheme. A new aged care data and digital strategy was also launched earlier this month.
The importance of research to improve aged care was a key theme of the Aged Care Royal Commission. Research Australia played a lead role helping the Commission develop its research agenda and identify the researchers the Commissioners subsequently engaged to undertake research on its behalf, informing their findings and recommendations. Following on from the Royal Commission, the National Ageing Research Institute (NARI) is developing the Australian Ageing Well and Innovation Clearing House, and Flinders University is at the centre of the Aged Care Industry Research and Innovation Australia (ARIIA).
More remains to be done. This edition of INSPIRE highlights the significant work our members are undertaking in ageing research and innovation, with the objective of enabling older Australians to lead healthier and more fulfilled lives.
We also report on Research Australia’s most recent University Roundtable, our recent Parliamentary Friends of Health and Medical Research Event, and we profile one of our newest members, Women’s Health Road. I invite you to read on and learn more about the breadth and depth of research and innovation being undertaken in aged care.
The health and medical research sector never rests, and neither do we. As we do every time at this stage of the election cycle, Research Australia is convening our Preelection Summit on 8 October. The Summit will draw together the whole health and medical research and innovation sector, including the other sector peak bodies, to focus on the key things our sector needs from the next Government. These priorities come from the views of our membership, what you tell us you would like to see, as well as being informed by our advocacy across the broader ecosystem.
Asking what ordinary Australians think and expect of our Government and our sector is also important; our 2024 Opinion Poll gives us insight into a range of health and medical research and innovation related topics. Currently in development, the report of the Opinion Poll will be released later this year.
Last but not least, the 21st Research Australia Awards for health and medical research will be celebrated on 14 November, bringing policy makers, politicians and our fantastic research and innovation community together. Nominations are still open, so take the opportunity to recognise your colleagues by nominating them here
I look forward to celebrating with you!
Best wishes
Nadia and your Research Australia Team




The hidden issue of elder abuse and what is being done to tackle it The right to be heard
Events overview 18
Meaningful and purposeled engagement in residential aged care


Intergenerational programs

Hearing and vision care to optimise health, wellbeing and independent living for older people


Co-designing respectful and dignified care for older people

Unravelling the cycle of representations for pain in older adults to the emergency department: a predictive model

Future-focused research to optimise care for an ageing Australia




Publisher Research Australia Ltd
Art Direction
Matthew Ware p +61 403 844 763 e matt@objktive.com
For Advertising enquiries please contact the Research Australia office on p 02 9295 8546 or e admin@researchaustralia.org researchaustralia.org
INSPIRE ONLINE issuu.com/researchaustralia
INSPIRE is a publication of Research Australia Ltd ABN 28 095 324 379 384 Victoria Street Darlinghurst NSW 2010
Who can submit articles?
Any current member of Research Australia who would like to share a relevant story that affects their organisation including, philanthropic donations and their outcomes, research findings, and any other related health and medical research topic that affects the Australian population.
Submission guidelines & deadlines For information regarding how to submit and publishing deadlines visit the Research Australia website
Disclaimer
The opinions expressed in INSPIRE do not necessarily represent the views of Research Australia. Whilst every effort has been made to ensure accuracy, no responsibility can be accepted by Research Australia for omissions, typographical or inaccuracies that may have taken place after publication. All rights reserved.
The editorial material published in INSPIRE is copyright. No part of the editorial contents may be reproduced or copied in any form without the prior permission from Research Australia. © Research Australia 2024.







Research Australia has provided specialist consulting and advisory services for many years. Our consultancy services continue to expand each year, driven by our unique expertise, reputation for high quality work, and strong relationships to drive outcomes and influence system change.
Most recently we have worked with state and federal governments, patient groups, industry, hospitals, and aged care. Some of the consulting services Research Australia provides are:
Market scanning – detailed analysis of who is undertaking what research to inform project planning and ensure projects target the right health and medical research stakeholders.
Policy advice – on the funding streams, government policy landscape and political interests that impact your projects’ success.

Sector consultation – facilitating engagement with the health and medical research community and the consumers who can best inform approaches to health and medical research.
Grants guidance – evaluating and reviewing grants opportunities and funding programs. m +61 2 9295 8546
k admin@researchaustralia.org

On 29 May 2024, the Research Australia University RoundTable was held at Australian National University. Taking advantage of its location Australia’s capital, the two guest presenters were Mr Blair Comley PSM, Secretary of the Australian Government Department of Health and Aged Care Mr Simon Cleverley, Assistant Secretary of the Digital Health Branch at the Australian Government Department of Health and Aged Care.
Mr Comley spoke about Australian healthcare and the role of health and medical research, in improving health outcomes and the health system. He also discussed the upcoming consultation on the National HMR Strategy, and how it will link back to the broader narrative of reforming Australia’s health system and workforce.
Mr Simon Cleverley discussed the National Digital Health Blueprint and the corresponding Action plan and the role for research in supporting the Blueprint’s vision of ‘trusted, timely and accessible use of digital and data underpins a personalised and connected health and wellbeing experience for all Australians’.
Greg Mullins provided a summary of the recent Budget Update to the Roundtable and a review of recent policy changes.
The Roundtable was also the forum for the launch of Research Australia’s latest report, Clinician Researchers: Research Activating the Health System. The report highlights the breadth and variety of the clinician researcher role, by profiling more than 30 clinician researchers from across Australia, in a range of disciplines and roles at different stages of their career.
As well as highlighting the challenges and barriers, the report identifies what needs to change, including better integrated training for clinician researchers, and more dedicated positions that fund clinician researchers to undertake both research and clinical practice in a single role with one employer. The report is available on our website here.
The next University Roundtable is on 14 August, hosted by the University of Western Australia.
Research Australia’s Philanthropy round table met on 30 April 2024. Approximately 40 representatives from across the philanthropic sector, academia, medical research institutes, pharmaceutical companies, health systems and government met to discuss overcoming barriers to giving.
Jonathan Smithers CEO at Arthritis Australia and Sarah Thyssen, Head of Philanthropy, Development and Engagement at Crohn’s & Colitis Australia shared their experiences around barriers to giving and strategies to minimise these challenges. Of note was the importance of communication and engagement in being visible and promoting the work being done.
Greg Mullins, Head of Policy at Research Australia provided a summary of the most recent report from the Productivity Commission’s Philanthropy Inquiry. Bolstering confidence in charities by strengthening the ACNC; better, more available data; and streamlining regulation between jurisdictions to create a more national system were a few of the draft recommendations.
Finally, we heard from Dr Joseph Po, Health 10X Program Manager, UNSW Founders and Dr Karin Sitte, Trust & Grant Program Manager, Equity Trustees to provide a funders perspective around what they look for when reviewing applications

On 26 June, Research Australia, in partnership with our member, Australian biotechnology company Vaxxas, convened a policy roundtable of more than 70 health innovators, alongside government officials, to identify policy solutions to support the uptake of Australian health innovations here at home.
Australian health innovation represents 26% of all Australian R&D activity.1 Australia is leading the world in many health technologies but bringing them to market more quickly and efficiently is key to facilitating better commercial, economic and social outcomes for Australia and Australians.
Hosted by Research Australia member Australian National University, the roundtable examined existing barriers to commercialisation of medical products in Australia, including regulatory and reimbursement practices. It also explored a suite of policy options, including the current Health Technology Assessment Review and the role of Commonwealth, State and Territory government procurement in the $170 million per annum health market to support Australian enterprises to progress from R&D to market.
The policy roundtable was followed by a Parliamentary Friends of Health and Medical Research event, hosted by the Hon Milton Dick MP, Speaker of the House of Representatives. This event showcased just some of the healthcare innovations being developed by Australian companies. Co-Chairs Dr Mike Freelander MP, Dr David Gillespie MP and Dr Monique Ryan, spoke of their support for healthcare innovation. We were privileged to have the support of the Hon Mark Butler MP, Minister for Health and Aged Care and Senator the Hon Anne Ruston, Shadow Minister for Health and Aged Care demonstrating multi-partisan support for our sector.
Minister Butler spoke about the National Health and Medical Research and Innovation Strategy, currently under development. It is to be a truly national strategy, including the state and territory governments, to drive more effective health and medical research and innovation for the national benefit.
Research Australia looks forward to working with the sector and government to advance policy solutions to help drive Australian innovation and manufacturing and will build on these discussions in developing a policy platform ahead of the next Federal Election.






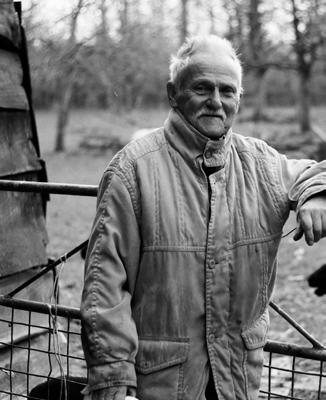
Elder abuse is widespread in Australia, and chronically underreported.
The National Ageing Research Institute’s Bianca Brijnath has spearheaded the No More Shame initiative to help healthcare professionals spot the signs and increase levels of reporting.
Almost 15% of older Australians experience elder abuse, defined as any act within a relationship where there is an expectation of trust, which results in harm to an older person.
Elder abuse takes on various forms, including physical, financial, social, sexual and psychological mistreatment, with psychological abuse being the most prevalent, affecting 11.7% of older people.
The impacts can be severe, with victims of elder abuse registering higher rates of depression, anxiety, fear, and stress; and mortality risk can increase by as much as 40%.
Elder abuse is predominantly perpetrated by family members, particularly adult children who account for 1 in 5 abusers. Intimate partners make up 10% of perpetrators, while partners of children account for 7%, grandchildren 4%, and friends and neighbours 12% and 7% respectively. These familial ties are at the heart of the issue – older people often feel shame around reporting, seeing the abuse as a negative reflection on their parenting and families. For groups who are already at greater risk of abuse – for example those with experience of homelessness and women living in non-urban areas –issues are compounded.
Beyond the shame associated with admitting abuse at the hands of a family member, there are often complicated power dynamics at play which contribute to underreporting.
Adult children may pressure older parents to transfer assets or lend money, using the threat of not being able to see their grandchildren.
There are also instances where the older person may have no idea they are the victim of abuse. A family member could be doing the weekly shop on a relative’s behalf, and pocketing some of the cash each week, for example. When people become more reliant on family members in their older years, there are increased opportunities for mistreatment.
Elder abuse is a complex topic and tied to a host of other issues. With that said, there are two standout factors that can be addressed now that will make a significant difference: improving services’ recognition and response to elder abuse.
Healthcare professionals are a trusted source of information and help for older people. As a result, older people are more likely to disclose abuse to these professionals, who in many instances they will see regularly and have built a relationship with.
However, as well as older people being reluctant to report instances of abuse, healthcare professionals often don’t know how to look for signs of abuse and don’t know what to do when disclosure happens. They need to be trained to spot the signs and empower older people to want to take action to stop the abuse.
When older people are ready to take action or intervention is essential, healthcare professionals can then facilitate a multidisciplinary response, including referrals to specialist professionals, who are able to give older people the help they need. They can offer wrap-around services including family mediation, financial and housing assistance to stop the abuse.
As part of my work for the National Ageing Research Institute (NARI), and alongside 10 public hospitals across



Australia; research partners in Victoria, Western Australia, New South Wales, and South Australia as well as the UK and Norway; policy and advocacy groups; and most importantly older people themselves including those with lived experience of elder abuse, I have designed a support model of care. The model includes:
• training for health care providers on elder abuse and how to screen for it
• a screening tool
• a site champion for more help and support.
This model is being implemented in sub-acute care in 10 public hospitals across Australia. We selected subacute care because vulnerable older people who are hospitalised, often spend a significant amount of time in this care setting. This time can be used to build trust and rapport and sub-acute health providers are therefore well placed to recognise and respond to signs of elder abuse and take action.
The goal of the study is to detect significant progress in participating health providers’ knowledge and their management of elder abuse; strengthen hospitals’ detection and multidisciplinary responses to elder abuse; and improve older people’s sense of safety, quality of life, and mental health.
Empathy, respect and putting older people at the centre is critical to tackling the widespread issue of elder abuse. The No More Shame trial is just the beginning, but through continuing to raise awareness and tackle the stigma associated with elder abuse, we can chip away at this destructive challenge.
Author: Professor Bianca Brijnath, Divisional Director of Social Gerontology at the National Ageing Research Institute (NARI).
Almost one million older Australians have a communication disorder that affects their ability to understand and to be understood. Communication is how we send and receive information. It occurs most often through speech, listening, reading and writing, but also through gesture, behaviour, facial expression and touch. Communication is integral to healthy and active ageing. It allows us to connect with other people, express our preferences and decisions, and critically, to tell others when something is wrong.
Many older Australians who receive aged care services have unmet communication needs, placing them at risk of poor health, adverse events, and even abuse and neglect.
With the support of a $2 million grant from the Medical Research Future Fund Dementia, Ageing, and Aged Care Mission, Associate Professor Sarah Wallace and her team from UQ’s Queensland Aphasia Research Centre are working to co-design, implement, and evaluate an interdisciplinary, multi-component intervention to support better communication in aged care.
“Communication is a human right and a human need. Our National Aged Care Quality Standards state that consumers must be supported to participate in assessment, care planning, decision making, feedback and complaints, irrespective of ability,” Associate Professor Wallace says.
“But it can be very difficult to express a decision, raise a concern or make a complaint when you have difficulty communicating. Through our research, we are working to ensure that all older Australians have a voice and that
aged care workers are equipped with the resources and training they need, to help raise this voice.”
Now in its second year, the five year ‘Conversations about Care’ project is using a method called ExperienceBased Co-Design to explore the experiences of people who receive and provide aged care services. To date, UQ post-doctoral researchers Dr Michelle King, Dr Asmita Manchha, Dr Zheng Ng and PhD candidate Bridget Burton have conducted 65 interviews in community and residential aged care services across metropolitan, regional and remote areas of Australia.
The insights gained from these interviews are informing the co-design of a multi-component intervention, comprising:
• A tool for profiling communication support needs,
• Web-based communication partner training for aged care workers,
• Picture-based resources to support conversations about care and
• Guidelines for “communication friendly” care planning, feedback and complaints resolution, and support for decision-making.
With the support of a UQ stipend, PhD candidate Bridget Burton has heard first-hand the difference that good communication can make to the lives of older Australians.
“My PhD focuses on understanding how aged care workers can best support diverse communication needs. I have travelled out to the Western Downs to meet with aged care recipients. I have learned how communication challenges affect not only the quality of care they receive, but also their ability to participate in decisions, and engage in feedback processes.”




Researchers, lived experience experts, and Government and Industry partners meet at the project planning day.
Broad and meaningful engagement with government, industry, and community partners is core to ensuring the co-designed intervention can be feasibly and sustainably implemented, at scale, across aged care settings. Project partners include: the Australian Government Aged Care Quality and Safety Commission, Wesley Mission Queensland, Southern Cross Care Queensland, the Older Person’s Advocacy Network, Dementia Australia, the Ethnic Communities Council of Queensland, Speech Pathology Australia, Audiology Australia and Southern Queensland Rural Health.
Consumer and community involvement is central to the research, and all aspects of the project are overseen by the Lived and Living Experience Advisory Group (LEAG), comprising a diverse group of older Australians and aged care service providers.
The final stage of the project will evaluate the feasibility of the intervention in a pilot cluster Randomised Control Trial (RCT). The pilot RCT will be conducted in collaboration with the UQ Clinical Trials Centre (CTC). Professor Nadine Foster is the Academic Director of the CTC, which has been created to provide end-to-end collaboration on high quality RCTs that make a difference to the health and wellbeing of Australians.
‘Conversations about Care’ is a first step towards better communication in aged care, however there is more
work to be done. Steps must be taken to improve the identification of communication support needs through changes to aged care funding tools. Best practice speech pathology services and interdisciplinary communication training must be embedded in aged care. Communication must feature in quality indicator programs, and the tools used to assess quality of care must be accessible to people with communication support needs.
“In order to ask for help with communication, you need to be able to ask. As older peoples’ communication support needs increase, the burden of ensuring good communication falls to us—as a society we have a responsibility to ensure that older people do not lose their voice,” says Associate Professor Wallace.
For more information on QARC and to find out how you can support QARC projects visit shrs.uq.edu.au/QARC
Author: Associate Professor Sarah Wallace is an NHMRC Emerging Leadership Fellow, Certified Practising Speech Pathologist, and a 2023 Queensland Young Tall Poppy. Sarah conducts her research within the Queensland Aphasia Research Centre. She works in partnership with people with lived experience, clinicians and community members to co-produce interventions, systems and standards that improve quality of care and outcomes.

By 2050, an estimated 3.5 million Australians are expected to access aged care services, and it is projected that Australia will face a shortage of more than 400,000 aged care workers.


University of New South Wales (UNSW) Ageing Futures Institute members are developing and evaluating approaches to care that can potentially alleviate this shortfall.
With over 420,000 people estimated to be currently living with dementia, and with cases estimated to more than double by 2050, the UNSW Ageing Futures Institute hosts several large programs of work on dementia diagnosis, prevention and care.
In a project led by Australian Research Council Laureate Fellow Professor Jill Bennett, a fully realised AI companion has been co-created with women living with dementia.
Called ‘Viv,’ the companion has been used as a teaching tool for professionals working with people with dementia as well as a companion for aged care residents in realtime.
In another project, Dr Claire O’Connor is working to understand how to implement reablement programs nationally for people living with dementia, working with community aged care providers.
CogDRisk is a free online risk tool developed by Institute Director Professor Kaarin Anstey that provides the user with an assessment of their dementia risk and a personalised report they can discuss with their GP. The tool provides an accessible way for individuals to take action in preventing or delaying the onset of dementia.

Lead of our theme People, Technology and Society, Professor Mari Velonaki has pioneered social robots and other sensor technology that incorporate immersive interactions with people. Social robots are increasingly being used in care settings to provide cognitive stimulation, companionship and to undertake practical tasks.
Scalable and cost-effective healthy ageing programs are also important to ensure those ageing in the community maintain independence into later life – empowering individuals while alleviating demands and resources from health and care systems.
Within our program of Inclusive Healthy Ageing, members have also developed digital health apps to improve healthy ageing. Professor Kim Delbaere’s ‘Standing Tall’ app provides tailored exercise programs for older adults that have been proven to reduce risk of falling.
TV shows like ABC’s award-winning “Old People’s Home For 4 Year Olds” brought together older people and preschool children to showcase the benefits of intergenerational programs.
In 2020 the Institute seed-funded The INTERGENERATION INTEGRATION project, which was led by Associate Professor Ruth Peters and included co-investigator Dr Stephanie Ward (a geriatrician on the show). The project provided a novel, evidence-based, user-friendly toolkit to support the development of community-based intergenerational integration programs tailored to local Australian communities.
There are also cultural considerations that need to be addressed to ensure optimal ageing for all.
Connection to country is a critical element for health and wellbeing for Aboriginal and Torres Strait Islander peoples.
However, in urban environments, such connections can be easily lost. This can especially be felt by older Aboriginal peoples – who through the Stolen Generation –were forcibly displaced and relocated to highly urbanised environments.

Dr Aryati Yashadhana co-designed and co-led a study with Yuwaalaraay cultural knowledge holder Ted Fields, that delivered a walaay (ceremonial camps in cultural landscapes) for older Aboriginal people who are survivors, family members or descendants of the Stolen Generation and explored how this impacts wellbeing and connection to place. The study highlighted the importance of connection to Country for older Aboriginal people living in urban areas.
PhD student Ms Yuchen Xie has also explored the challenges of aged care navigation from the consumer perspective using both national datasets and qualitative interviews with home-based aged care recipients and/ or their family carers, including those from culturally and linguistically diverse backgrounds.
While the above highlights some of the research work by our members, effectively addressing the complexities of population ageing requires further collaboration, innovative thinking and transformative solutions. To better prepare Australia for the future, the UNSW Ageing Futures Institute will continue its mission to “address the complex challenges and opportunities of population ageing through interdisciplinary research that takes a life-course perspective.”
Authors: Scientia Professor Kaarin Anstey is an ARC Laureate Fellow and Director of the UNSW Ageing Futures Institute. Scientia Professor Jill Bennett is an ARC Laureate Fellow and founding Director of the Big Anxiety Research Centre. Professor Mari Velonaki is Founder and Director of the Creative Robotics Lab. Professor Kim Delbaere is Senior Principal Research Scientist at Neuroscience Research Australia. Associate Professor Ruth Peters is Program Lead for Dementia, Global Brain Health Initiative at the George Institute. Dr Stephanie Ward is a geriatrician and clinical lead for the Australian Dementia Network Clinical Quality Registry.
Dr Aryati Yashadhana is a Research Fellow at the Centre for Primary Health Care and Equity, UNSW. Dr Claire O’Connor is a Senior Research Fellow in the School of Psychology, UNSW. Ms Yuchen Xie is a Research Associate at the Centre for Social Research in Health and the Social Policy Research Centre at UNSW.
An industry partnership to develop a new model of care applying principles of Montessori for dementia and ageing, dignity of risk, and strength-based person-centred care.
The delivery of evidence-based high-quality care in residential aged care [RAC] that meets the psycho-social needs of residents is an urgent priority in Australia and internationally [1-3]
Relevant principles of care include person-centred care [PCC], the right of older people to make decisions that involve positive risk (dignity of risk), meaningful purposeled engagement, and home-like environments.
These principles of care are enacted in government guidelines and regulations as they are well recognised to contribute to the quality of life [QoL] and well-being of RAC residents. However, despite Government mandates and recognised benefits, the principles have not been fully realised and adopted in RAC in Australia and internationally [1-7]
Concerns about the quality of care in RAC persist and residents experience low QoL [1-3], with few opportunities for meaningful engagement [1] . The RAC workforce continues to operate with a task-oriented approach rather than practising person-centredness [1-7]
Implementing the principles of PCC, dignity of risk, meaningful purpose-led engagement, and home-like environments in RAC to improve the quality of care is fraught with complexity.

Factors at the government, organisation, and RAC home levels, such as funding, education and training, policy/ regulation direction, accreditation standards, competing work demands, and culture influence how these principles are embedded at the RAC workforce level.
Hence, models of care that define and conceptualise how care is delivered, and move beyond single interventions by addressing the multi-level influencing factors occurring outside of the RAC workforce are required to improve the quality of care delivery and QoL of residents [8,9]
Informed by Human Factors and guided by Implementation Science, researchers from the Health and Social Care Unit – Monash University – are working in collaboration with aged care industry partners to develop, implement and evaluate an innovative model of care that leverages wellestablished approaches of Montessori for dementia and ageing, dignity-of-risk, strength-based person-centred care, and dementia-friendly environments.
Crucially, in developing the model of care, key stakeholders are being engaged, including RAC staff (all levels and roles), residents (living with and without dementia) and families. Further, an implementation framework has been developed,





also with the key stakeholders, to underpin the translation of the model to practice. The model of care incorporates the principles of Montessori for Dementia and Ageing.
Montessori is often understood as a method that was first designed by Dr Maria Montessori for children. However, recognising the specific contextual and individual characteristics of older people and the aged care sector, Montessori has been used for over two decades as a nonpharmaceutical approach to the care of older people [10,11]
Examples of methods used in Montessori align with those of PCC, Dignity-of-Risk, strength-based person-centred care, and dementia-friendly environments and hence have also been conceptualised with the model of care, such as individual-centred engagement in activities and care, support for independence and choice through prepared environments, the provision of meaningful work and opportunities to make contributions, and fostering abilities and engagement throughout daily interactions (not limited to activities) [10,14] .
These elements enrich the model of care and extend beyond a clinical care model that is unlikely to meet the needs of residents.
Our work to develop a model of care that defines practice and is underpinned by an operational framework is important.
RAC homes have a significant role to play in promoting and maintaining the health and well-being of residents. The progressive loss of physical and cognitive function means that most RAC residents rely on others to enact their preferences and for support to maintain their physical, cognitive, and social engagement in the home [7]
As populations age and the demand for RAC rapidly increases [15], there is an urgent need to support the RAC workforce with models of care that guide practice and are underpinned by practical implementation plans that ensure the translation of theory to practice.
Dr Marta Woolford is a postdoctoral research fellow in the Health and Social Care Unit at Monash University.
Associate Professor Darshini Ayton is the Deputy Head of the Health and Social Care Unit at the School of Public Health and Preventive Medicine and a National Health and Medical Research Council (NHMRC) emerging leader fellow (2021-2025).
Sock puppets designed by our children and adult participants at one of the intergenerational sessions.

A novel approach to protect against frailty, dementia and social isolation?
Social isolation in older people is a global public health concern. Research has shown that older people with good social relationships and who are actively connected to their communities tend to have better health outcomes, including better cognitive and physical health and are less susceptible to becoming frail.
In contrast, high levels of social isolation have been associated with increased mortality, reduced functional status, lower physical activity and greater sedentary time. More importantly, high levels of social isolation and low physical activity in the older population are associated with significantly higher risks of developing dementia or cognitive decline and transition to long-term care.
With age-related constraints such as poor health and mobility, driving cessation and living alone, many can find it challenging to maintain or build reliable positive social interactions and stay physically active in their later life. Given the complex issues surrounding social isolation and physical inactivity, there is an urgent need for a multidisciplinary approach to tackle this pressing problem.
Naturalistic, community-embedded intervention, such as intergenerational programs that provide opportunities for older adults to build positive social relationships and increase physical activity and cognitive engagement, are potentially the key to reducing the risk of many unwanted health consequences, including frailty and dementia. Intergenerational programs that bring together non-familial older people and children to engage in purposeful joint activities have shown additional potential benefits for older adults in improving their self-esteem, self-worth, perceived usefulness and reduced loneliness and anxiety. At the same time, preliminary research findings have shown potential gains for the children in their development, empathy and language skills. However, more robust research is needed to generate evidence on the impact of intergenerational programs on health outcomes in older adults and developmental outcomes in children. There is also a need to find the best approach to keeping these programs sustainable in the communities.
To address these gaps, Associate Professor Ruth Peters and her team from The George Institute for Global Health are now conducting The INTErGenerational Intervention to Reduce frallTY (INTEGRITY) trial across Sydney, New South Wales. The INTEGRITY trial is a waitlisted randomised clinical trial designed to investigate the outcomes of involving older adults and preschool children in structured, play-based intergenerational programs. INTEGRITY brings together around 10 older adults living in the community and 10 preschool children in each participating preschool, and they aim to run this program in up to 44 preschools in Sydney. Each group will participate in a 2-hour weekly session for 20 weeks at a local preschool led by experienced preschool educators.

“The intergenerational sessions provide older adults and preschoolers opportunities each week to engage in enjoyable activities, including games, arts & crafts, physical activity, cooking, dancing, music, singing, yoga, and a whole lot more. The activities we have designed not only benefit children but also older adults, supporting better health, well-being and social engagement, increased self-worth and promoting powerful community connections.” says Associate Professor Ruth Peters. She further adds that “many participants comment on how fast the 20 weeks goes and are always eager to continue their connection with the early childhood service”.
My Twitter : @chriskere

Participants who completed their 20-week intergenerational program have shared some of their wonderful experiences. “I was away last week, but I spent my whole Thursday morning wondering what the group was up to and which activities they were doing.” said one of the participants.”
Another participant shared “I have enjoyed it immensely and gained a lot from my days at the preschool. Everyone involved has been very friendly and the children were delightful. The programs presented by Rachelle (educator) challenged us in various ways each week and were enjoyed by children and adults alike. I hope the outcome of this study will be that older people can be welcomed into the preschool environment on a regular basis as I can see great benefits for all.”
With families often spread out and many older adults living alone, inviting older adults into a preschool setting, presents a unique opportunity to enhance social connectedness, reduce isolation and improve health outcomes whilst simultaneously offering opportunities for the growth and development of the children as well as providing an enjoyable experience for all involved. By encouraging meaningful connections between generations, we can potentially combat social isolation, reduce risk of frailty and dementia in older people and promote holistic well-being across communities.
This research is supported by the NHMRC Clinical Trials and Cohort Study Grant (GA259020)
Authors: Assoc Prof Ruth Peters is the program lead for Dementia, Global Brain Health Initiative at the George Institute and a Conjoint Associate Professor, Faculty of Medicine, at the University of New South Wales. Dr Mae Lim is a Research Fellow at The George Institute and a Conjoint Associate Lecturer at the University of New South Wales. She is also a Postdoctoral Fellow at Neuroscience Research Australia.
As we move through the stages of our lives, care, dignity, and respect is what we hope for ourselves and those we care about.



Australia’s ageing population is increasing the demand for aged care services and there is growing need and expectation to improve the experience of living in residential aged care.
The Royal Commission into Aged Care Quality and Safety’s 2021 Final Report described a ‘rights-based approach’, placing the needs and preferences of the older person at the centre of the aged care system1. Person-centred care emphasises personhood, respect, maximising choice and autonomy, physical and emotional comfort, relationships which nurture, and supportive physical environments2. Aged care policy has historically emphasised external regulation and monitoring to ensure safety and prevent poor quality care; person-centred care is part of a shifting focus towards resident quality of life, wellbeing and overall satisfaction.
Calvary Health Care’s new model of care is being implemented in residential aged care homes across Australia. Called PEARS, the model of care for older people was developed to clearly direct the way Calvary meets the needs of older people in its care. The evidence-based model is underpinned by the domains of Personhood, Environment, Activity, Relationships and Safe care (PEARS), of which each has a corresponding set of principles1. In partnership with Hunter Medical Research Institute, a qualitative evaluation of co-design as an implementation strategy for the PEARS model is underway, to be completed early next year.
Having staff and residents in the same room listening to each other, where they just listen, is a big achievement” (Key informant interviewee, June 2024)
Consistent with improving the quality of care and as a mechanism to enact person-centred approaches to aged care, in its Final Report the Royal Commission recommended:“priority [be] given to research and innovation that involves co-design with older people, their families and the aged care workforce”1
Co-design is an approach that focuses on involving end users in the design of services and has been used in a wide range of contexts. Co-design might be considered as much a way of thinking as a set of prescriptive steps1 and can take various forms across a collaboration continuum. It typically uses a staged process that adopts participatory and narrative methods to understand the experiences of receiving and delivering services, which then sees these same participants co-design improvements collaboratively3. It requires strong facilitation to engender key principles of equal partnership, openness, respect,
and empowerment, principles which are also central in delivering personhood and person-centred care
Calvary has commenced co-design initiatives for eight of its residential aged care homes across Australia. There is a nine-month timeline for the PEARS co-design process. Key is facilitating sessions between residents, carers, and staff to collaboratively ‘gather’ issues about living in the home, ‘understand’ or validate these issues, and develop co-designed workable solutions. The solutions evolve into an implementation plan, triaged according to feasibility, and the likelihood of having an overall positive impact on the quality of care for the residents.

Co-design has known challenges for organisations, including existing openness to change and knowledge of co-design, the need for specialised training and its time demands for staff. The inclusion of people with dementia and cognitive impairment in co-design activities is a further challenge. However, growing evidence points to novel methods of engagement for these residents, including ‘co-production’, where relationship building occurs through staff and residents working alongside each other in a common activity or goal1,2
• Increased opportunity for residents to be involved in decision making,
• Identification of high impact and low effort solutions – many of the actions resulting from co-design are simple, relatively inexpensive and easy to operationalise / implement, and
• Increased permission to contribute and a sense of empowerment for residents to have a say, and greater organisational accountability for follow-up.
To date, the PEARs model of care appears to be strengthening mutual equality, trust and respect among residents, carers, and staff at Calvary’s participating eight residential aged care homes. While not without its challenges, co-design is adaptable and iterative, with the potential for further integration and adoption to support care, dignity, and respect at all Calvary homes.
Authors: Karen Harrison, National Manager, Collaborative Care Redesign, Calvary Health Care. Dr Anthea Bill, Senior Health Economist, Hunter Medical Research Institute. Dr Tracey Tay, Chief Medical Advisor, Calvary Health Care. Dr Olivia Wynne, Health Economist, Hunter Medical Research Institute
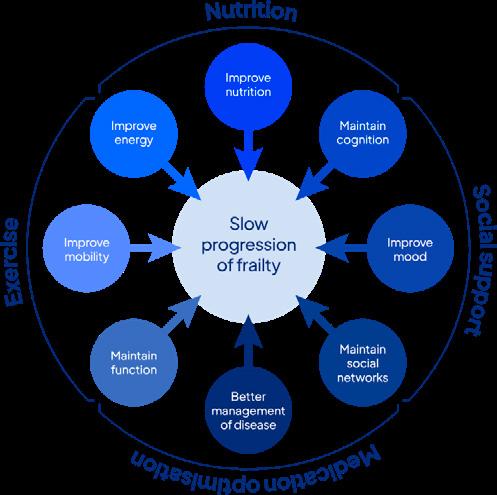
A comprehensive approach to combat frailty and enhance the quality of life for older Australians

Frailty is a state of vulnerability characterised by a loss of reserve across multiple physiological systems. In simple terms, someone who is frail is less able to “bounce back” after a stressor event — be it something minor like a urinary tract infection, or a more significant event like a fractured hip.
One way to think about frailty is that it increases an individual’s risk compared with others of the same age. In fact, studies have shown that a person’s frailty status is a better predictor of mortality than their chronological age.
Frailty can lead to impairments in physical function and mobility, as well as in mental and cognitive health — predominantly in older adults and people living with chronic diseases. With an ageing population, frailty is a major health concern, and it has become one of the most significant challenges to ‘ageing well’ in Australia.
To address this pressing issue, the Medical Research Future Fund (MRFF) has funded the establishment of the


recommendations for the four pillars. However, the approach to facilitate behaviour change will differ between the groups. Participants will be randomly assigned to either receive a self-directed program with online resources, or to receive the online program together with support from healthcare professionals. This will involve two sessions per week with an exercise professional, one dietitian assessment, and fortnightly/monthly sessions with a health coach.
It is already known that programs promoting good nutrition, regular exercise, optimisation of medicines, and social support networks can improve frailty. However, these programs are not routinely available, and when they are, people do not always participate.
Australian Frailty Network (AFN) under the initiative of Professor Ruth Hubbard at The University of Queensland’s Centre for Health Services Research. The AFN aims to deliver a national response to frailty by creating knowledge, implementing findings, and supporting training to improve outcomes for older Australians and their families and caregivers.
The AFN brings together consumers, healthcare professionals, multidisciplinary researchers, policymakers, and peak bodies to address this issue through a multipronged approach that focuses on preventing frailty and slowing its progression. Two years into its operation, research teams within the AFN have already obtained several large grants to improve the health, care, and quality of life for vulnerable Australians.
A core principle of the AFN is ensuring that all frailtyrelated initiatives are informed by the needs of people living with frailty, their families, and caregivers. This consumer-focused approach ensures that the research conducted is directly relevant and beneficial to those it aims to help.
One of the significant initiatives under the AFN is the FITTEST study. This multicomponent frailty program integrates exercise, nutrition, optimisation of medicines, and social connectedness, which are known as the ‘Four Pillars of Frailty Prevention and Management’. The study targets these pillars to provide a comprehensive approach to frailty management.
The FITTEST study is designed for people living in the community who are aged 65 years and older and have mild frailty. Participants will be randomised to either a supervised or self-directed intervention. Each intervention will be based on the latest evidence-based
The FITTEST study goes beyond assessing the impact of these interventions. It includes a rigorous process evaluation that seeks to identify the intervention’s barriers and enablers, as well as the mechanisms of its impact. By examining the mechanisms behind successful outcomes, we can identify key factors contributing to improved health and wellbeing among older Australians. Further, the FITTEST study and interventions have been designed with consumers, who have shaped the content and format of the online program, the role of the health coach and the outcomes measured.
We aspire to create a lasting legacy from the FITTEST study. Our goal is to widely implement this multidisciplinary intervention nationally and set a new standard of care for older Australians. By combining evidence-based practices with innovative approaches, we aim to change the approach to frailty management and enhance the quality of life for our ageing population.
The FITTEST study is a testament to the AFN’s commitment to transforming care through a holistic approach that prioritises the overall well-being of individuals.
For more information about the Australian Frailty Network, visit afn.org.au
Authors: Ida Tornvall, Project Manager, UQ Centre for Health Services Research and the Australian Frailty Network Professor Ruth Hubbard, Masonic Chair of Geriatric Medicine at the University of Queensland and Director of The Australian Frailty Network

Most people who have a stroke receive, at best, a combined six to eight weeks of acute and rehabilitation care in a public hospital setting.
Those in metropolitan areas, and occasionally those in regional communities, receive a further six weeks of rehabilitation therapies and support at home or in an outpatient setting. But what then?
Stroke is the leading cause of adult disability in the world, and despite immense progress in treating stroke, many people still live with the after-effects.
Dr Heidi Janssen is a physiotherapist and researcher working in the public health system delivering programs designed to prevent secondary stroke and promote selfmanagement of their recovery. She witnesses this shortfall in access to ongoing rehabilitation services firsthand.
It’s what drives her research agenda to find sciencebacked, sustainable ways to improve outcomes for people with stroke, especially if they live outside a major city.
“I am motivated to ensure all stroke survivors have the opportunity to access evidence-based recovery care because where people choose to live should not determine their quality of life after stroke.”
Dr Janssen explains people living with stroke in metropolitan areas receive relatively more comprehensive stroke care and recovery support compared to people living with stroke in regional, rural and remote areas.
Part of her solution to address this unmet need is to embed her ESTEEM Program into regional communities.
Dr Janssen’s ESTEEM (Exercising, Socialising and Thinking – an Environmental Enrichment Model in the community After Stroke) Program is currently running at Newcastle Mercy Services and is about to launch in Maitland, led by Maitland Community Care Services.

The ESTEEM Program sees participants engage in the following activities twice a week for 10-weeks: 30 minutes of physio-led ‘huffy puffy’ exercise (fitness and strength), then 30 mins of socialisation over morning tea, followed by 90 mins of either dance or art. This also gives carers a regular break from caring duties.
“Most rehab is very goal focused and tends to place more emphasis on what someone can’t do – what do we need to fix? The ESTEEM Program is equally focused on improving stroke recovery and maximise independence but does so with a large emphasis on celebrating achievements in novel activities participants have never tried before but which they can master,” says Dr Janssen.
The plan now is to prove the feasibility and sustainability of the ESTEEM Program being delivered by NGOs all over the Hunter New England region.
“Public health doesn’t really fund maintenance after a stroke. It reacts to acute episodes but there’s limited ability to keep going. For most people, once they finish in the public health system, any further rehabilitation or recovery activities must be self-funded. For many people, such funds are very limited or unavailable.
“The National Stroke Guidelines recommend that stroke survivors have access to ongoing support from peers and support for self-management of recovery. This is important given our increasing awareness of how much social isolation contributes to poor health outcomes including poor heart health, poor mental health and an earlier death,” says Dr Janssen.
“Our goal is to set up ways that people with stroke can participate in the ESTEEM Program using existing funding systems provided by either the Government (e.g., Home Care Packages and NDIS), the primary care and/or private health sectors. A win/win for both participants and the community.”
The feedback from the preliminary evaluation of the ESTEEM Program has been overwhelmingly positive.
Many participants reported better emotional health, quality of life and that they could do more.
• “I just had a damn good time.”
• “…you’ve got exercise of the brain as well as the body so it’s really good…good for you…it’s a relaxed atmosphere…”
• “…without this program… I wouldn’t have [been] exercising and got myself, it’s great, I’ve straightened myself up.”
• “…there should be something like that, that we can go to forever because the social side is...is absolutely wonderful.”
The hope is to find an NGO provider as a partner to ensure people living with stroke in the Manning Region can have the ESTEEM Program experience as well.

The second part of Dr Janssen’s mission to bring better stroke recovery services to regional areas is being achieved in partnership with the Gomeroi/Gamilaraay communities through the Yarning Up After Stroke Project. Community Elders, people with lived experience and other members of the Aboriginal community are leading the way in how to partner with the community in a culturally responsive and safe manner.
Established in Tamworth with the Gomeroi/Gamilaraay community, the concept is to provide culturally safe supports to people with stroke through a ‘navigator’ role; a person who is well-respected by the Aboriginal community and works with Aboriginal stroke survivors and their families to support interactions with the doctors and allied health professionals.
The Community and Dr Janssen are currently refining this role with community members and will then evaluate how well this ‘navigator’ approach strengthens the health and wellbeing of Aboriginal and/or Torres Strait Islander people living with stroke in regional communities.
“It’s possible that this model may be wanted and needed by other communities in other regional areas. Chances are it will look a little different, depending on where it’s located. It is important that any approach to strengthen recovery in a culturally responsive way considers the issues and wants and needs of each individual community.
“A stroke is a life changing event. Access to activities and support that we know support better physical and emotional recovery, and that maintain relationships and ensure people return back to participate in their community, should be available to all - irrespective of their postcode and their cultural background,” says Dr Janssen.
For further information, click here and here Community Led Project - Yarning up After Stroke
Author: Professor Heidi Janssen is a physiotherapist and Hunter Medical Research Institute researcher who is passionate about ensuring people living with stroke receive rehabilitation and post-stroke management that works, and that people are given the opportunity to recover as best as they can after their stroke.
SENSEcog: Hearing and vision support to improve the quality of life for older adults

For older people, undetected hearing and vision problems are detrimental to communication, social connections, participating in hobbies and independent living.
Professor Piers Dawes from The University of Queensland’s School of Health and Rehabilitation Sciences is leading a research program to better identify and support the hearing and vision needs of older people. The UQ team is working with people who have hearing and vision difficulties, aged care staff, families, and hearing and vision professionals to develop a program called SENSEcog.
The program will provide home-delivered sensory support to people living independently at home, as well as support for people in residential aged care settings. Care staff will also be able to access tools they need to support people with hearing as well as vision impairments.
More than 70 per cent of people receiving home care and 90 per cent of people living in residential aged care settings have hearing and/or vision impairments.
For people receiving home care, untreated hearing and vision impairments increase the likelihood of transitioning to residential aged care. In residential aged care, many residents do not get the help they need for hearing or vision impairments, limiting their ability to communicate, engage in activities and socialise. For people living with dementia, hearing and vision impairments exacerbate the impact of symptoms, increasing disorientation, communication difficulties, and responsive behaviours.
According to the Royal Commission into Aged Care Quality and Safety Care, Dignity and Respect report, people in aged care settings do not receive regular hearing and vision checks, and there are no clear links between aged care and hearing and vision services.2
Hearing and vision impairments make living independently much more difficult. Home care provided by professional carers can help older adults continue living independently at home, yet current home care packages do not include sensory support. The SENSECog Home Care project aims to identify and provide effective and timely treatments for hearing and vision impairments.
The project involves adapting a home-based sensory support intervention developed with people living with dementia and their families by Professor Dawes and colleagues in Europe3.
The intervention is tailored to individual sensory needs and delivered in people’s own homes by a trained Sensory Therapist over several visits. The program includes identifying hearing and vision problems, optimising hearing and vision by correcting sensory impairments, and supporting home modifications or use of other assistive devices. This intervention will be implemented through three home care provider organisations: Ballycara, Bolton Clarke, and Wesley Mission Queensland.
Challenges in identifying and supporting the hearing and vision needs of people in residential care settings are substantial. Hearing and vision problems are not obvious, and functional difficulties due to a treatable hearing or vision problem might be misinterpreted as being due to dementia. People may not have hearing or vision checks, and care staff lack knowledge about the impact of hearing

or vision problems and how to support people with sensory needs (e.g., changing hearing aid batteries).
To address these factors, we worked with aged care residents and family members, aged care staff, and hearing and vision professionals to understand the challenges and co-design a hearing and vision support intervention for residential care settings.

The intervention will upskill staff to support residents with hearing and vision difficulties, including integrating sensory support into daily responsibilities and placing visual reminders about these tasks in residents’ rooms.
Staff will also receive training to support communication by reducing background noise, speaking clearer, nearer, and slower; and to support visual communication by making text brighter, bigger, and bolder. The intervention includes setting up a sensory support station in residents’ rooms where all personal hearing and vision devices and related items are labelled and stored.
‘Sensory champions’ will be identified to provide leadership and support for their colleagues in assisting residents with hearing or vision needs. Champions will identify the hearing and vision needs and preferences of individual residents, provide information about hearing and vision services and arrange referrals to hearing and vision specialists and GPs when needed.
The effectiveness of both home and residential aged care SENSEcog hearing/vision interventions will be assessed by evaluating the impact on the quality of life of people living with hearing or vision problems. For the home care project, we will also evaluate whether the intervention helps people live independently in their own homes rather than moving to residential care.
Hearing and vision interventions are effective, low cost, low risk and strongly desired by older people. If we can do a better job at detection and intervention for sensory impairments, we could make a meaningful difference to the lives of older Australians, enabling people to live independently, fostering well-being, dignity, and quality of life.
The research program is supported by a Medical Research Future Fund.
Author: Professor Piers Dawes is Director of the Centre for Hearing Research at The University of Queensland, and Professor of Audiology at the University of Manchester.

UNRAVELLING THE CYCLE OF REPRESENTATIONS FOR PAIN IN OLDER

In the past decade, Dr Carla Sunner dedicated significant time to caring for older patients in the emergency department (ED), witnessing firsthand the unique challenges faced by older people in this setting. As part of her role, Carla conducted audits to explore the factors contributing to frequent ED visits among older patients, finding the most common reason was pain.
Pain management presents a complex challenge in older adults. This complexity arises from their increased likelihood of experiencing many different health issues at the same time. The presence of chronic health conditions, which affect over a third of older patients in the ED, 2 can make it difficult to detect underlying issues. Further complicating the situation are communication barriers such as vision and hearing deficits and psychosocial factors such as isolation.1
These factors can exacerbate depressive symptoms and cognitive impairment, making pain management even more difficult. Failure to identify and address all the issues which may be contributing to the pain during the initial evaluation could result in unresolved pain and subsequent return visits to the ED.
Unplanned ED re-presentations have a significant impact on individuals and the health care system. A representation can be disruptive and burdensome for older patients, and associated with unnecessary risks such as psychological distress, iatrogenic complications such as delirium, falls, medication errors, pressure injuries and even death.2
Discharge planning involves the development of a personalised plan to ensure the smooth transition of a patient from a hospital to home. Appropriate discharge planning can avoid complications after discharge from hospital, avoid errors with medications and may help prevent re-presentations.
Medications such as opioids for example are known to significantly increase the risk of ED re-presentations.1 Clear communication for patients that present to ED for reasons of pain can further improve pain management strategies for older patients, reducing the need for return visits to the ED. Efforts to reduce avoidable ED re-presentations have far-reaching benefits, including improved health outcomes, enhanced patient safety, and increased healthcare system efficiency.3
References to be supplied upon request.

Driven by curiosity and a desire to improve patient outcomes, Carla convened a research team to delve deeper into understanding pain re-presentations for older people to ED. To address this, the research team developed the project Re-presentation to the Emergency Department for reasons of Pain with Older People (REDPOP) project to address the following questions: What proportion of older people re-present for pain? What are the characteristics of those who re-present for painrelated issues?
To answer these questions, the research team will examine medical record data from EDs across the Hunter New England Local Health District (HNELHD) of New South Wales. This medical record audit is the first, imperative step in building an evidence-base to understand representations to ED for pain among older people.
The research team also aims to create a more concrete framework for pain management in older adults to explore a predictive model for pain.
A predictive model has the potential to guide patients’ pain-related issues, leading to improved quality of life and overall wellbeing for older adults. This routinely collected medical record data allows us to examine factors, including patient demographics, medical history, psychological and physiological measures, to develop such a model.
The HNELHD serves 920,370 people across rural and urban areas and a sample from this population will provide significant insights into the issues of pain re-presentations for older people. RED-POP lays the groundwork for future research that will inform practice change in healthcare utilisation among older people, leading to cost-saving measures, optimised resource allocation, and the development of health policies and clinical guidelines tailored to the older population’s pain management needs.
Author: Dr Carla Sunner is an early-career researcher and lecturer working at the University of Newcastle.
Professor David Komander, with the 2023 GSK Award for Research Excellence trophy, and the Ubiquitin Signaling division at WEHI.

Surface of a damaged mitochondrium as seen by Parkin. An anchored PINK1 molecule (light pink, centre) attracts Parkin (purple) to the surface, and Parkin assembles ubiquitin chains (orange ballson-a-string) to mitochondrial complexes and pores (green) to signal damage and initiate destruction of the mitochondrium.

Ubiquitin is a small protein found in human cells, that can modify other proteins in a variety of ways. It performs important functions within the body, including the destruction of proteins, also known as the ‘kiss of death’ process1, transporting proteins to a different place in the cell or generating new interactions between proteins. 2 Due to the significance of these processes, defects in ubiquitin signaling are at the heart of a range of conditions, including cancer, rare inflammatory diseases, and Parkinson’s disease.
My scientific focus has been on the fascinating world of ubiquitination for almost two decades. Since uncovering the key principles in ubiquitin chain assembly and disassembly, I was determined to better understand how this can lead to translational outcomes and new therapy discovery projects.
We may be far off from fully discovering the potential of ubiquitination but this keeps fueling my research interest, which more recently has turned to early onset Parkinson’s disease, and two proteins called PINK1 and Parkin.
Parkinson’s disease is a neurodegenerative disease of the brain. There are estimated to be more than 200,000 people currently living with Parkinson’s disease in Australia, with one-in-five being diagnosed before the age of 50.3 The disease is characterised by major motor difficulties, such as tremor, rigid muscles and slowness of movement.
Early onset Parkinson’s can be caused by genetic mutations that alter the function of key proteins. In 2021, we produced a ‘live action’ view of PINK1, which showed how the protein progresses from when it is initially made, to being activated and functional, giving us powerful insights into how Parkinson’s disease develops. This breakthrough discovery of PINK1 and Parkin-mediated degradation processes basically showed us how we can ‘switch on’ proteins, paving the way to developing therapeutic agents for this incurable disease.
Our work on PINK1 and Parkin at the Ubiquitin Signaling division formed a powerful spark to establish the Parkinson’s Disease Research Centre at WEHI. The centre works highly collaboratively with like minded researchers and movement disorder clinicians, and consults with the Parkinson's community to better understand the needs of those living with Parkinson's and to guide research.
We are really getting out of the academic mindset and moving towards more translatable outcomes, which is

My Twitter : @chriskere
a necessary step to achieve improvements in health outcomes for patients. I am grateful to have fantastic collaborators working alongside me, including Professors Grant Dewson, Michael Lazarou, postdocs Sylvie Calligari and Tobias Schneider, and former PhD student Dr Zhong Yan Gan.
“Parkinson’s incidence is increasing faster than other neurological disorders. Importantly, there are no drugs that can stop disease progression,” says Professor Grant Dewson, lab head within the Ubiquitin Signaling division at WEHI and head of the Parkinson’s Disease Research Centre.

“David’s research has provided key insights into this and the role of PINK1 and Parkin in this highly complex disease. These proteins are the focus of international drug discovery efforts to stop or slow the progression of Parkinson’s and David’s research has unlocked this potential.”
As we face an ageing population, we should be joining forces to accelerate and support research into ageingrelated diseases. It’s our common race against time. While a degree of healthy competition is necessary, we need to embrace partnerships between research organisations and with industry.
I have been honoured to receive recognition for achievements in ubiquitin research, most recently becoming a Fellow of the Royal Society and of the Australian Academy of Science, and receiving the 2023 GSK Award for Research Excellence. This provided my team and I with access to eminent scientists and enhanced our opportunities for collaboration, as well as financial support needed to take our research to next level to build new methods for measuring ubiquitin modifications.
It takes a community to solve the most difficult scientific challenges. At WEHI, we are lucky to have seven collaborative research centres that unite brightest minds with multi-disciplinary expertise and advanced technologies to accelerate scientific successes that can help people live longer and healthier lives.
The innovation and research in ageing-related processes has come a long way but it hasn’t really become any less complex. While we can anticipate that we will continue improving our understanding of ageing-related diseases, it is through multi-disciplinary collaborations, gaining fundamental knowledge, and sharing these insights, that we can solve multi-faceted and complex problems.
Komander,

The genuine engagement of people living with dementia is essential to create authentic Dementia Friendly Communities
People living with dementia have a desire to remain living in their own home 2 . A recent project explored the global movement of Dementia Friendly Communities (DFC)1.
A DFC aims to address barriers so people with dementia can stay living in their home and community for as long as possible. A foundational principle for DFCs is the need to have people living with dementia leading initiatives. Yet, local committees in Southeast Queensland struggled to engage and effectively involve people living with dementia.
This micro-ethnographic case study used participant observation, semi-structured interviews and fieldnotes to conduct an in-depth inquiry into the micro-processes and practices of two DFC committees. The research question was: How do people experience the implementation of DFC principles and micro-processes in locally based DFC committees?
Two committees were observed between September 2019 to January 2020. Both committees hosted monthly meetings. The Service Provider-led committee had 20-30
attendees, whilst the Volunteer-led committee had nine regular attendees. Committees had aspirational goals but were faced with real-world systemic barriers, showing glaring gaps in current practice. Key barriers experienced locally were associated with engagement, power sharing and leadership. For example, the positioning of people living with dementia as passive clients or valued contributing members of committees then shaped how power was retained, controlled or shared. Another associated barrier was the competing market-driven priorities of organisations; priorities which sometimes took precedence over the engagement of people living with dementia to the detriment of their experiences.
Inclusive processes are needed to facilitate the engagement of people living with dementia. Necessary considerations for DFCs include the location of meetings, the number of people in meetings and multisectoral collaboration1. People living with dementia and their carers need to be included in the planning process to ensure that meeting locations and times are practical and accessible. Having a large number of people in DFC meetings can


limit participation by people living with dementia as it can be difficult to follow the conversation. A smaller number of people in an informal setting fosters greater engagement with people living with dementia and family carers.
Effective DFC meetings can be more time intensive to facilitate but authentic inclusion increases the effectiveness of the DFC. Taking time to engage and support people living with dementia and their carers in the process facilitates their active engagement which provides richer insights into DFC actions and is an opportunity to empower people living with dementia.
By sharing power with people living with dementia, meaningful inclusion can occur and potentially lead to co-leadership and leadership roles for people living with dementia, as seen in one case study where a person living with dementia was chair of the DFC committee1 This example directly challenges misconceptions and assumptions about the ability of people living with dementia, creating a counter narrative that further challenges discourse and practice.


People living with dementia have demonstrated their interest and ability to participate in DFCs and associated research, but flexible, individual approaches are necessary to facilitate this1. Authentic engagement is necessary to truly privilege the voices of people living with dementia to uphold the mantra, Nothing About Us Without Us.
Author: Caroline Grogan is a Research Fellow in the Health Services Research Team at Wesley Research Institute. She has over ten years of practice experience in aged care community services in community development and codesign. She currently leads the Older People, Aged Care and Dementia Research Program at Wesley Research Institute. She is passionate about amplifying the voices of people with lived experience in research and service design.

PRESENTATIONS IN ACUTE AGED PSYCHIATRY, BARRIERS TO DISCHARGE AND IMPLICATIONS FOR SOCIAL WORK PRACTICE IN DISCHARGE PLANNING.

The Royal Commissions into Mental Health services1 and into the Aged Care system in Victoria 2 , emphasised the need for patient centred care with psychosocial support.
However, the findings from the Royal Commission into Aged Care highlighted the shortcomings in providing adequate care and treatment of aged care residents’ mental health. There is a significant increase of patients with dementia and health care challenges such as Behavioural and Psychological Symptoms of Dementia (BPSD) who require admission to an aged psychiatry unit for acute intervention.3 Our goal was to assess barriers to discharge from acute publicly funded beds and inform social work practice in older adult psychiatric services.
It is estimated the global population of people living with dementia will quadruple to 81 million people by 2040.4 In 2018 there were an estimated 219,000 Australians with dementia, a 12.7% increase since 2015.5 The prevalence of dementia and mental health disorders is increasing amongst the population of people living in a Residential Aged Care Facility (RACF).6,7 Older persons diagnosed with mental health and cognitive impairments, including dementia and BPSD, often require specialist care in RACF to support needs such as affective, psychotic, and aggressive behaviours.8
Up to 100 patients with a primary or secondary diagnosis of dementia over a two-year time frame (November 2019-November 2021) were admitted at an Older Mental Health unit located in Melbourne, Australia. The datamining investigation consisted of a retrospective audit of 100 patient files, with 122 hospital admissions with 16 of the 100 patients having multiple presentations. Any identifying features were removed. This research was conducted over the COVID-19 pandemic period which has an indirect effect on people with dementia due to delay reduction in medical diagnosis, treatment and preventative care.3
Of the 100 patients admitted to the unit, 60% were male with an average age of 78.3 years (with an age range of 57 to 92 years); female average age was 79.4 years (age range of 65 – 95 years). 78 patients had no previous history of mental illness and were admitted to a psychiatric unit for the first time; 33 patients had a co-morbidity of depression (a common comorbidity associated with dementia). Patients who experienced the longest length of stay had a diagnosis of BPSD, agitation and aggression. The most common barriers to discharge of long stay patients were: 23% had no appropriate discharge destination, 8% involved family conflict and 47% experienced medical instability. The average length
of social work (SW) involvement was 28.2 days, however 3 patients with BPSD had the longest length of stay and recorded an average of 333 days of SW input. The majority of short stay and medium stay patients were discharged to funded supported accommodation.
Most of the presentations of patients with dementia were from RACF. One of the main barriers to discharge from the acute unit was male patients presenting with high levels of agitation and aggression, and sexual disinhibition which impacted on discharge planning. The study found that the majority of patients had no prior contact with community mental health services which would support and prevent unnecessary hospital presentations. There were challenges in sourcing the most appropriate discharge destination for patients with complex BPSD. SW roles involve the coordination of family or care planning meetings with relevant stakeholders which support a patient's transition from hospital.9 Thorough discharge planning from the treating team and SW input often helps with preventing readmissions back to hospital.9,10

It is notable that most of the sample had no history of a mental illness. BPSD and aggression with agitated behaviours are overwhelmingly the greatest barriers to discharge from Older Adult Mental Health inpatient units for people with dementia with projected increase in these types of presentations in the future. Early engagement of the Older Adults Community Mental Health services can potentially reduce mental health admissions and associated costs with inpatient stay. Higher levels of coordination, communication, and consultation by the SW in the Older Adult inpatient unit are required to ensure the patients are discharged to a safe and sustainable discharge destination. The SW in collaboration with the treating team is heavily involved in supporting the patient and their family/carers in establishing the most suitable discharge destination. There is a need to help improve patient, carer, and family experiences through navigation of a complex health care system and reduce the length of stay in acute psychogeriatric care. This research helps to inform SW practice with discharge planning, increase patient flow, maximise use of limited public health resources and support future workforce planning on an organisational level.
Authors: Jenny Kats, Senior Social Worker at Monash Health Margaret Deitz: Clinical Educator, social worker in the mental Health program at Monash Health Dr Marcelo Maghidman: Senior Lecturer - MSW Course Director, Fellow Higher Education Academy (FHEA),Social Work,Monash University

CHAI project is a strategic initiative of the Healthy Minds Research Program of the Hunter Medical Research Institute.
It aims to address the fact that most people who engage with healthy ageing information are highly educated, health literate and come from relatively affluent backgrounds.
“When we give public talks, we are generally preaching to the converted. If we want to make a difference, we need to go out and proactively connect with broader sectors of the community.”
“At a time when there is increasing scepticism about science, people are more likely to engage with health information coming from people who look like them and sound like them,” says Professor Frini Karayanidis.
“So, we need to work with community leaders to get health messages across.”
“Some people say, ‘You can’t teach an old dog new tricks’, but from a healthy ageing and dementia standpoint, we know that there are many modifiable risk factors, and that lifestyle choices in mid-late life can have a profound impact on preventing or slowing down the onset of dementia,” she says.
The Australian Government’s recent Intergenerational report stated the number of people aged over 65years will



double and the number of people aged over 85 will triple in coming years.
Professor Karayanidis says it is important not only to connect with older people, but also with people in their 20s, 30s and 40s, when the biggest long-term benefits can arise.
“Dementia has a 20 – 30 year incubation period. If you look after your heart, brain, social life and drink in moderation, as well as exercise and eat a good diet, you can reduce your risk of developing the disease.
“Cognitive decline doesn’t happen because of ageing, per se. It is linked to the cumulative effects of many lifestyle factors, as well as a person’s genetic risk,” says Professor Karayanidis.
In order to get this message out to a broader audience, CHAI aims to establish community-based ‘hubs’ – dropin facilities for people of all ages to receive personalised information, assessment and guidance to make evidencebased lifestyle choices that promote healthy ageing.
CHAI hubs will be situated in familiar environments like shopping centres and community facilities and use a trainthe-trainer model to facilitate learning through interactions with peers, as well as trained professionals.
A pilot hub will run from July to September 2024 at the Belmont Café, a joint initiative of Hunter Ageing Alliance and Home Instead Newcastle, attracting older people to trial social and creative activities while learning about healthy ageing.
The vision for this program is that it could be run in a selfsustaining way around the country.
“It could be like a Telstra shop. A place where you can pop in and ask questions and be directed to the services and information you need,” says Professor Karayanidis.
This ‘shop’ would provide access to lifestyle and creative arts workshops and run in partnership with organisations like Dementia Australia.
“The idea is to introduce people to appropriate activities early, and encourage lifelong engagement,” says Professor Karayanidis.
“The hubs will be run by community leaders and supported by student placement clinics, offering students an authentic experience to practice their skills – it is a win/ win from that perspective. They will provide a free, easily accessible place for everyone to access information about healthy lifestyles, ageing and dementia,” says Professor Karayanidis.
Another pilot hub will soon be launch together with researchers from Sunshine Coast University. These will assess the feasibility and acceptability of CHAI hubs and support progress to an implementation trial.


Creating greater research impact by facilitating authentic engagement of older people in service and community design.
In 2023 there were an estimated 411,100 people living with dementia and was the second leading cause of burden of disease in Australia1. There are approximately 140,900 unpaid primary carers providing 60 or more hours a week of care1.The formal services and support they both receive does not meet their collective and individual needs.
The Royal Commission into Aged Care Quality and Safety highlighted the need for a new rights-based aged care act to “ensure the focus of the aged care system is on the needs of the individual, regardless of their location, background and life experiences, and their choice and preferences”2. Another key recommendation was to focus on the preferences and needs of older people to drive the delivery of services4. To do this, older people need to be actively engaged and supported to be heard.
Our Health Services Research Team at Wesley Research Institute utilises evidence-based methods for authentic research participation and championing the importance of consumer voice in health services research. Our important research helps to ensure health and aged care services are accessible and suitable for older people.
Wesley Research Institute recently conducted an explorative research project in collaboration with BlueCare investigating the perspectives and wishes of people living with dementia and family carers to inform their dementia in-home respite service. Family carers are more likely to experience low wellbeing, high financial stress and psychological distress compared to other Australians 3 . Respite offers support for family carers to have a break from their caring role, while a trained staff member provides care to the person living with dementia. This can take place at a day respite centre, cottage respite, nursing home or in the client’s home. In 2018, 23% of carers of people living with dementia reported the need for more respite care1
Wesley Research Institute partnered with BlueCare to understand the preferences and needs of clients to inform the model of care delivered. The Institute’s independence from BlueCare meant participants could speak openly without perceived or actual repercussions. Inclusive practical steps were vital to ensure safe and authentic

participation. Researchers offered transport assistance if needed and were flexible to meet participants how, when and where they prefer, offering to talk face to face, over the phone or in their home or at the BlueCare community centre. Extended time frames for interviews and focus groups were embedded into the process. This allowed participants to have time to ask any questions, become more comfortable with the team and allow participants to take breaks.
Two researchers attended focus groups to create a safe, welcoming and relaxed environment, be able to provide support to any who became upset- without stopping the session- and enhance the facilitation of the group. Morning tea was provided, and the room was set up so everyone could sit around shared tables, further contributing to a relaxed and friendly space. Participant information forms used picture communication symbols and simplified accessible plain language. Forms were provided to participants before the focus group and again in hardcopy on the day. Each section of the form was talked through with participants, making sure they understood and were comfortable in proceeding. The two researchers were attentive to any incongruent verbal and nonverbal behaviour.
Recommendations from the project were shared with participants in a one-page document. Participants were called to talk through the results and seek their preference for receiving the document- mail or email. Results and recommendations were presented and shared with BlueCare executive leadership to inform the adaptation of the model of care before wider implementation across BlueCare. Findings are currently under review for publication in an academic journal.
Author: Caroline Grogan is a Research Fellow in the Health Services Research Team at Wesley Research Institute. She has over ten years of practice experience in aged care community services in community development and codesign. She currently leads the Older People, Aged Care and Dementia Research Program at Wesley Research Institute. She is passionate about amplifying the voices of people with lived experience in research and service design.
Unravelling the link between postmenopausal bleeding and genitourinary syndrome of menopause

Postmenopausal bleeding (PMB) is a concerning symptom that requires timely medical attention. While PMB can be an indicator of serious conditions such as endometrial cancer, it is more frequently associated with Genitourinary Syndrome of menopause (GSM).
GSM is a collection of symptoms affecting the genitourinary tract due to decreased estrogen levels, affecting over half of post-menopausal women, these include:
• Vaginal dryness
• Vulval Itching and irritation
• Pain during intercourse (dyspareunia)
• Urinary symptoms such as urgency, frequency, incontinence and recurrent infections
• Postmenopausal bleeding
The decline in estrogen results in thinning and inflammation of the vaginal walls, leading to the symptoms. Unlike other menopausal symptoms that may resolve over time, GSM often persists and can worsen longer term, significantly impacting the quality of life of post-menopausal women. Estrogen, which can be given topically is an effective management of symptoms.
The average age of menopause is 51. Postmenopausal bleeding (PMB) refers to any vaginal bleeding that occurs more than 12 months after the final menstrual period. This does not include the scheduled or regular withdrawal bleed some women get when using Menopause Hormone Therapy (MHT).
While PMB is often a result of benign conditions like GSM, it can also indicate underlying endometrial hyperplasia or

cancer. Therefore, PMB management requires prompt and thorough evaluation to rule out malignancy and address underlying conditions.
Statistically, only around 10% of women with PMB have underlying endometrial carcinoma, however, over 90% of women diagnosed with an endometrial malignancy will present with PMB. The lifetime risk for a woman is 1:44 for endometrial cancer and risk increases with age, nulliparity, obesity, use of unopposed oestrogen, polycystic ovary syndrome, Type 2 diabetes mellitus and family history of gynaecologic malignancy.
PMB is often attributed to the uterus, but the bleeding may also arise from the urethra, vulva, vagina, cervix, or rectum. The most common cause of postmenopausal bleeding is genitourinary atrophy, accounting for 60% of PMB cases. The irony of the PMB aetiology is that it can have too little estrogen (atrophy) or too much (unopposed estrogen) as an underlying problem.
An endometrial thickness of ≤4mm on transvaginal gynaecological ultrasound has a 99% negative predictive value for malignancy.
An endometrial biopsy should be performed in women who have a greater endometrial thickness, or ongoing PMB, a suspicion of polyp or Inadequate visualisation of the endometrium in imaging studies due to fibroids for example.
The Women’s Health Road Abnormal Uterine Bleeding Hub (WHR AUB Hub) offers a ‘one stop’ hybrid care service that includes GP and gynaecology reviews, diagnostic ultrasound, menopause service with pelvic floor physio and urogynaecology on site sessions using enhanced digital technology including AI scribe.
The AUB Hub at Women’s Health Road employs a comprehensive approach to diagnosing PMB, ensuring that any underlying conditions such as GSM are accurately identified.
As we can undertake a diagnostic transvaginal ultrasound at WHR, after a comprehensive history and examination facilitated by the ability to take and store pictures in a sophisticated outpatient gynaecological set up, it is relatively easy to triage GSM based PMB episode from the women who will benefit from operative work up including a hysteroscopy and endometrial biopsy.
The quality of life of women with GSM and PMB is much improved with vaginal moisturisers, lubricants and most importantly topical estrogen to minimise other symptoms that can be long term (for 50%) of aging women, unlike the vasomotor symptoms that typically tend to cluster around
the perimenopause and just after, then with time tend to reduce. GSM does not usually ‘go away’ spontaneously.
This is particularly a problem in patients with a history of breast cancer and it is important to support this cohort of women, to minimise their GSM based symptoms but also recognise that there can be an additional risk factor for endometrial cancer for example for women on tamoxifen.

As far as unscheduled bleeding in women on MHT, this is the main reason women stop using it, so there are benefits from an MDT menopause management service with a co-located AUB hub as there is momentum to support majority of women (with no underlying hyperplasia or malignancy) to safely remain on MHT after work up of the PMB. This is a topical space with the current parliamentary enquiry into menopause and does make us wonder that if GSM was better recognised and more women accessed hormonal and other support would that reduce PMB rates as well as better QOL for women?
PMB occurs in women who have not had a menstrual period for 12 consecutive months. While PMB can be a symptom of benign conditions like endometrial atrophy, it may also indicate serious issues such as endometrial hyperplasia or cancer. Early diagnosis and intervention are crucial for effective management and improved patient outcomes.
Postmenopausal bleeding, often associated with genitourinary syndrome of menopause, requires thorough evaluation and personalised management to ensure women’s health and well-being. The AUB Management Hub at Women’s Health Road offers comprehensive diagnostic services and tailored treatment options, emphasising early intervention and effective management strategies to address GSM and its associated symptoms. GSM significantly impacts sexual health, comfort, and overall quality of life. Our research advocates for improved diagnostic approaches and personalised treatment plans to address the complex needs of women experiencing PMB and GSM. By fostering awareness and education, we can enhance women’s health and well-being in the postmenopausal phase of life.
Authors: Dr. Talat Uppal is a Gynaecologist and Director of Women’s Health Road in Sydney. Dr Megan Young is a GP with an interest in menopause management, digital and public health. Mariah Amjad is Media Manager at WHR and works with AI in healthcare.

Menopause is a major milestone for female reproductive aging, and something the majority of women will experience. As a woman begins transitioning to menopause, rapidly changing hormone levels and reductions in oestrogen contribute toward a myriad of unpleasant symptoms including hot flushes, hair loss, vaginal dryness, and sleep disruption 1
The most common complaints from women during menopause are hot flushes and night sweats; described as a sudden wave of heat that feels most intense over the face or chest and is often accompanied by profuse sweating.
Although the physiology behind these symptoms are not fully understood, previous studies have suggested reductions in vascular function of systemic arteries may play a role 2. Similarly, reductions in oestrogen levels seen during the transition to menopause have also been linked to elevated vascular disease risk 3 .
Dr Jenna Taylor imaging the diameter and blood velocity of the right brachial artery using ultrasound.
Indeed, studies have reported that greater frequency and severity of hot flushes may be linked to adverse cardiovascular disease risk factors 4. This makes sense when you consider what “reductions in vascular function” look like. Reductions in vascular function otherwise known as endothelial function present as an inability for blood vessels to precisely regulate everything from temperature, blood flow, oxygenation, and nutrient delivery to its target organs. Ultimately, disruptions in the body’s ability to control the blood vessels that supply the heart and brain can potentially lead to an increased risk of cardiovascular disease and cognitive impairment.
Vascular function can be assessed using ultrasound to measure changes in blood velocity and vessel diameter, in response to vasodilatory stimuli such as breathing higher concentrations of carbon dioxide, exercise, or cuff-induced ischemia 5,6. In health, optimal blood vessel function results in a prompt and marked change in vessel diameter following the stimulus, while in disease the time it takes to elicit a change may be delayed or the actual response might be attenuated.
Recently, using regular exercise as a means of reducing menopausal symptoms and vascular disease risk has been gaining popularity. Exercise has been shown to
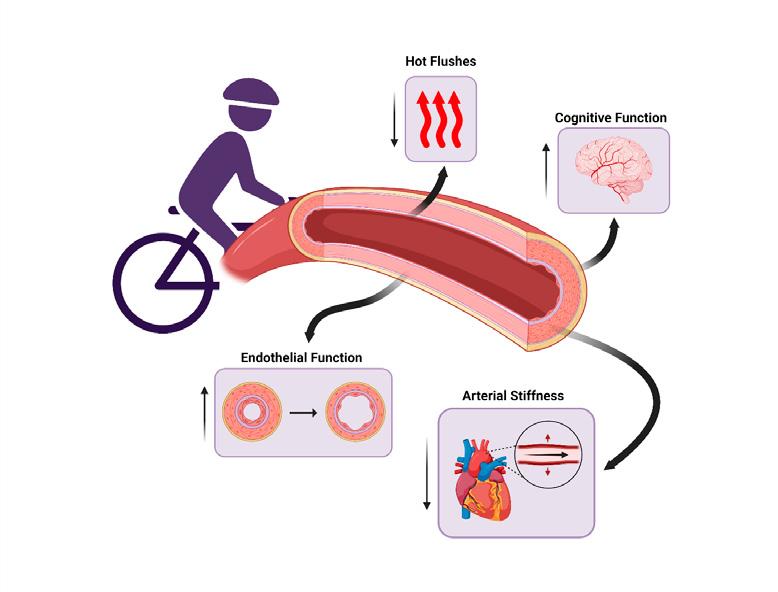
reduce hot flush frequency 7 and arterial stiffness 8, and promote endothelial function 9 and brain health10
Currently, the World Health Organization recommends at least 150-300 minutes of moderate-intensity aerobic activity or 75-150 minutes of vigorous aerobic activity weekly. In addition, it is recommended to partake in at least two or more days of strength/resistance training weekly11
High-intensity interval training (HIIT), involving periods of high-intensity exercise interspersed with periods of recovery, has become a very popular and time efficient method to reach weekly aerobic exercise targets. Another common method is moderate-intensity continuous training where exercise is performed at a lower intensity with no rest periods, although this requires additional time commitment to reach weekly exercise target.
However, during menopause, reduced oestrogen levels can affect how women adapt to exercise and modulate the degree of improvement they experience12. Prior to menopause or early during the menopause transition referred to as perimenopause, regular aerobic exercise can reliably improve several indicators of vascular health. This is because oestrogen levels are still high; compared to oestrogen levels seen after menopause referred to as postmenopause. Subsequently, as a woman enters postmenopause, these improvements become less reliable, often requiring some form of hormone supplementation to garner the full gamut of benefits8
That’s not to say all hope is lost...even without hormone supplementation, physically active postmenopausal women were able to improve markers of arterial stiffness significantly compared with their physically inactive counterparts 8
To gain the greatest benefits, it’s recommended to begin exercising early and often, though its certainly never too late to start.


However, that still leaves the question, what is the optimal exercise prescription? Studies have shown repeatedly that HIIT has outperformed moderate-intensity continuous training when it comes to improvements in vascular function13. Although on the surface it appears HIIT is the clear winner, its unclear how moderate-intensity “interval” training MIIT would compare. More specifically, is it the higher intensity or the periodic ‘interval’ nature of the exercise that plays a role in the greater improvements.
Our research group will conduct a randomised controlled trial to understand how the role of exercise training intensity contributes to improvements in vascular health, hot flushes, and cerebral blood flow during menopause. Late perimenopausal women will be allocated to either a work matched HIIT or MIIT group, or into a control group.
We will assess both systemic and cerebral vascular function using ultrasound-based techniques before and after the 12-week exercise intervention or control period.
Our findings will enable practitioners to understand how to prescribe targeted exercise interventions to improve vascular health and menopausal symptoms for women throughout menopause transition and beyond.
For more information, please reach out to the UQ Centre for Research on Exercise, Physical Activity and Health team.
Authors: Conan Shing is a PhD student at the University of Queensland, in the School of Human Movement and Nutrition Sciences. Dr Jenna Taylor is an Accredited Exercise Physiologist and Lecturer in Clinical Exercise Physiology within the School of Human Movement and Nutrition Sciences at the University of Queensland. Dr Taylor is the Director of the Centre for Research on Exercise, Physical Activity, and Health (CRExPAH), and Head of the Physiology and Ultrasound Laboratory in Science and Exercise (PULSE).
Parkinson’s disease is a chronic, progressive and degenerative neurological condition.

It’s estimated to affect more than 200,000 Australians, with a further 38 diagnosed daily. These stats are set to increase, with the prevalence of Parkinson’s increasing faster than other diseases of ageing, and expected to double by 2040.
Given an estimated 80% of people living with Parkinson’s are over 50, this makes it a crucial area of focus for health and medical research to improve healthy ageing in Australia.
SLOWING AND STOPPING
PROGRESSION IS AN URGENT GOAL
Many people will be aware of the movement-related symptoms of Parkinson’s such as tremor, muscle rigidity and challenges with balance. However, the disease has a wide range of symptoms, many of which are lesserknown and poorly understood. These include cognitive impairment, depression and anxiety, sleep difficulties,
loss of smell, issues with swallowing and speech, and vision problems. It’s a disease that has a serious impact on quality of life, and as people get older, this impact only increases.
Parkinson’s is also a notably idiosyncratic condition. Not everyone will experience the same symptoms, and the order in which symptoms appear and progress also varies. Perhaps for this reason, much of the research, and available treatments, have focused on addressing the symptoms.
Yet many of those living with Parkinson’s will experience severe ups and downs within the same day, depending on medication ‘on’ and ‘off’ times. Emma, living with both Parkinson’s and multiple sclerosis, says, “My life is forever up and down, left and right – entirely unpredictable. It can go very right or very wrong in a minute.”
At Shake It Up, we recognise how critical it is that research is targeted at slowing and stopping the progression of
the disease, to improve quality of life; not just for those diagnosed, but for their loved ones too.
As people living with Parkinson’s age, they can become increasingly dependent on carers to remain in the home. When the disease progresses, there are often high rates of hospital admissions, and the person may be moved to a residential facility for more advanced care. This means the burden of the disease weighs on caregivers, the health and human services workforce, society, and government.
Research, clinical trials, and drug treatments in development must focus on ways to stop the disease in its tracks, slow the progression over time, and ultimately, find a cure.
There is significant progress being made. In April last year, an international coalition of scientists made an enormous


leap forward in the understanding of Parkinson’s, with the discovery of the α-synuclein seeding amplification assay (αSyn-SAA), which can detect the presence of abnormal alpha-synuclein - not just in those diagnosed with Parkinson’s, but also in those at a high risk of developing it.
This discovery opens a brand-new chapter for research, with the hope that in the future, those newly diagnosed with Parkinson’s will never advance to full-blown symptoms. In Australia, many of our most innovative researchers are getting closer to solving crucial parts of the Parkinson’s puzzle, to ensure that, as the prevalence of the disease grows, the impact on those living with it is lessened.
A study conducted by Professor Carolyn Sue AM, at NeuRA, is investigating whether overexpressing a Nix protein using gene therapy could stop the progression of Parkinson’s. “We are really looking at a way to provide a new, reliable, sustainable source of energy for the brain cells that die in Parkinson’s disease,” Professor Sue told The Australian.
The Australian Parkinson’s Genetics Study (APGS), led by Associate Professor Miguel Rentería at QIMR Berghofer Institute for Medical Research, is a nation-wide effort to learn more about what causes Parkinson’s and why its rate of progression is so individual. This is vital for our understanding of Parkinson’s and the development of new therapies to prevent progression of the disease.
At Shake It Up, we fund only the most globally competitive, innovative and non-redundant research projects, like these, to slow, stop and cure the disease. For people living with Parkinson’s, and their loved ones, the sooner this becomes a reality, the better.
“Slowing, stopping and curing Parkinson’s would mean the world to me. No, actually, it would mean the universe!”, says Emma. “It would mean I could run, laugh and play all the time with my two young girls and fulfil my ambition to be a Yoga teacher. My body wouldn’t be shutting down at 9 p.m.”
Author: Vicki Miller, CEO, Shake It Up Australia
With the release of fresh data from its 45 and Up Study, the Sax Institute is inviting researchers and policymakers to collaborate in building new data platforms that will improve our understanding of transitions to aged care, disability and cognitive decline.

By 2050, millions more Australians will need aged care or support for a disability, and the number of Australians with dementia will have tripled.
To meet these and other challenges facing our ageing population, it is critically important for public health researchers and decision makers to have access to timely, high-quality information about the way older people use health services and their experiences with age-related and other disabilities.
For almost 20 years, the Sax Institute’s 45 and Up Study – one of the world’s largest ongoing studies of healthy ageing – has been fulfilling that role, collecting a huge trove of information on the health and wellbeing of more than a quarter of a million older Australians and providing it to researchers. The 45 and Up Study has already been used by more than 800 researchers and provided data for over 500 research papers, many of which have informed health and prevention strategies and helped plan health services in Australia and across the globe.
Every five years, we send Study participants a survey of more than 100 questions to identify health and lifestyle changes. A fourth round of surveys is currently underway and will add major value to what is already a globally significant asset. This latest survey has a special focus on transitions to aged care, disability and cognitive decline, and although survey collection will continue into next year, we are making available data from the first 17,000 Australians to support timely and relevant research.
This will include extensive data about participants’ use of community aged care, including what services were received at home, out-of-pocket costs for aged care services and any barriers to accessing care. With the recent Royal Commission into Aged Care Quality and Safety ushering in new reforms, data from the 45 and Up Study, coupled with linked administrative data, has the potential to measure the impact of some of these changes.
The impact of disabilities and cognitive decline on older Australians is also being explored for the first time in




this survey. There are new questions on participants’ disabilities and the services received for them, including funding from the National Disability Insurance Scheme (NDIS). Participants are also asked about memory loss and if they’ve had a diagnosis of cognitive impairment, dementia or Alzheimer’s.
Some of the initial data from the Study’s latest survey demonstrates the challenges ahead for health service planning. For example, we found that almost a fifth of older Australians have avoided or delayed accessing healthcare services recently due to cost, and 8% are not getting all the aged care that they need. The psychological wellbeing of older Australians is also highlighted in the data, with around 30% of participants reporting loneliness, and over 10% reporting low levels of social interaction.
A key advantage of using 45 and Up Study data is that all participants have consented to linkage of their surveys with other health datasets. That means the new data we are making available can be linked not only with previous surveys, but also with hospital and emergency
department admissions records, cancer registries, Medicare and prescription data, immunisation data, death data and more. Altogether, this forms a unique national asset with the capability of yielding powerful insights into how our aged care and disability services are addressing the needs of older Australians.
Given the importance of policy issues around aged care, disability and dementia in our community, our aim at the Sax Institute is to establish strong, long-term collaborations to strengthen the evidence base and inform changes to policy and practice. We are at the beginning of an exciting new wave of data for the Study that will allow researchers to marshal crucial evidence that can guide efforts to improve health and wellbeing through bettertargeted policies and services.
Learn more about the Sax Institute’s 45 and Up Study here
To find out more about working with the 45 and Up Study, contact Dr Greer Dawson, Deputy Director of Research and Partnerships, at 45andUp.Research@saxinstitute.org.au

Australia’s aged care system has faced intense scrutiny over recent years, culminating in the Royal Commission into Aged Care Quality and Safety.
The Commission’s final report laid bare the systemic issues plaguing the sector, highlighting an urgent need for reform. Among its 148 recommendations, a significant focus was placed on enhancing digital health and data utilisation to improve care quality, transparency, and outcomes.
The Royal Commission underscored several key areas where digital health and data innovations could drive transformative change. These included:
• Enhanced Data Collection and Sharing Real-time
• Monitoring and Reporting
• Personalised Care Planning
• Informed Decision-Making
Addressing these needs head-on are initiatives such as the Aged Care Data Compare and Aged Care Explainer projects. Digital Health Cooperative Research Centre
(DHCRC) research endeavors are poised to revolutionise how data is utilised in the aged care sector, aligning closely with the Royal Commission’s recommendations.
The Aged Care Data Compare project is an ambitious initiative aimed at developing a comprehensive benchmarking system for aged care providers. By collating and analysing a wide array of data points,from clinical outcomes to operational efficiency, the project seeks to establish robust benchmarks that can guide providers in enhancing care quality.
Care Data Compare aims to create an interoperable platform where data from different sources can be integrated and compared. This directly addresses the Commission’s call for a unified data system, facilitating better information sharing and coordination among stakeholders.
Real-time Monitoring: The benchmarking system will employ real-time data analytics to monitor care standards

continuously. Providers can receive instant feedback on their performance, enabling them to address issues promptly and maintain high-quality care.
Transparency and Accountability: By making benchmark data accessible, the project promotes transparency. Providers, regulators, and families can easily compare performance across different facilities, resulting in greater accountability and better-informed decision-making.
Improved Care Outcomes: Through data-driven insights, the project will help providers identify best practices and areas for improvement. This continuous learning loop is vital for enhancing overall care standards and achieving better outcomes for residents.
The Aged Care Explainer project focuses on making aged care data more accessible and understandable for all stakeholders. By translating complex data into comprehensible information, it empowers residents, families, and care providers to make informed decisions.

Informed Decision-Making: support the Commission’s recommendation for accessible data. By simplifying data presentation, they ensure that stakeholders have the information they need to make wellinformed decisions about care options.

Personalised Care Planning: By providing clear insights into individual health metrics and care plans, the projects enable more personalised and effective care planning. Families can better understand the care needs and preferences of their loved ones, facilitating tailored care solutions.
Enhanced Communication: Clear and understandable data fosters better communication between care providers, residents, and families. This aligns with the Commission’s emphasis on the importance of effective communication in delivering quality care.
Empowerment through Knowledge: Knowledge is power, and the Aged Care Explainer project aims to empower all stakeholders with the knowledge they need to advocate for better care. This empowerment is a critical component of the broader effort to reform the aged care system.
The integration of digital health and data innovations in aged care is not just about technology; it’s about fundamentally reshaping the way care is delivered, monitored, and experienced. The Royal Commission’s recommendations provide a clear blueprint for this transformation, and initiatives such as the DHCRC’s Aged Care Data Compare and Aged Care Explainer are crucial in turning that vision into reality.
These projects exemplify how targeted research and innovation can address systemic issues, driving improvements in care quality, transparency, and outcomes. By harnessing the power of data, we can ensure that Australia’s aged care system is equipped to meet the challenges of today and tomorrow, delivering the high-quality care that our elderly population deserves.
With continued collaboration between researchers, policymakers, and care providers, together, we can build a more robust, transparent, and compassionate aged care system—one that not only meets the needs identified by the Royal Commission but exceeds the expectations of all Australians.
Author: Annette Schmiede, Digital Health CRC CEO



The Australian Research Data Commons (ARDC) drives development of world-class national digital research infrastructure that gives Australian researchers competitive advantage through data and supports research impact.
As Australia’s leading facility for research data infrastructure, we facilitate access to research data sets and tools from academia, industry and government for all Australian researchers.
We run programs and offer services that ensure Australian researchers are internationally competitive by having access to high-quality data assets, platforms, infrastructure, policies, people and training. Collective effort is needed to solve society’s greatest health challenges. Through our national and international partnerships, we provide and coordinate consistent approaches to data findability, secure access, data integration, and advanced analytics. Our infrastructure enables leading-edge, nationalscale research that makes a difference to people’s quality of life and healthcare.
The ARDC is enabled by the Australian Government’s National Collaborative Research Infrastructure Strategy (NCRIS).
The ARDC builds on past experience working in partnership to deliver digital research infrastructure for health and medical researchers, which has culminated in a wide range of datasets, free tools and upskilling materials.

In the ageing sector for example, the ARDC has supported projects including the Dementias Platform Australia (DPAU), a secure platform for sharing dementia data to take ageing research global.
The ARDC People Research Data Commons (People RDC) is delivering national-scale data infrastructure for health research and translation.
Researchers, innovators and policymakers seek to improve health outcomes for society, which requires data and digital platforms that span multiple layers of government, health service operations, health research studies, institutes, facilities and the private sector.
The People RDC is addressing some of Australia’s core digital health research challenges:
• FAIR Assets - Findable, Accessible, Interoperable, Re-usable data for health research
• Secure Data Access - Trusted research environments and data governance
• Data Integration - Data standards, common data models, ontologies, and vocabularies
• Advanced Analytics - Modelling, Machine Learning, Natural Language Processing, and Large Language Models applied to sensitive health data.
ARDC looks forward to supporting Research Australia members with our infrastructure and enabling them to shape our directions into the future.
Register your interest in the People RDC Visit ardc.edu.au
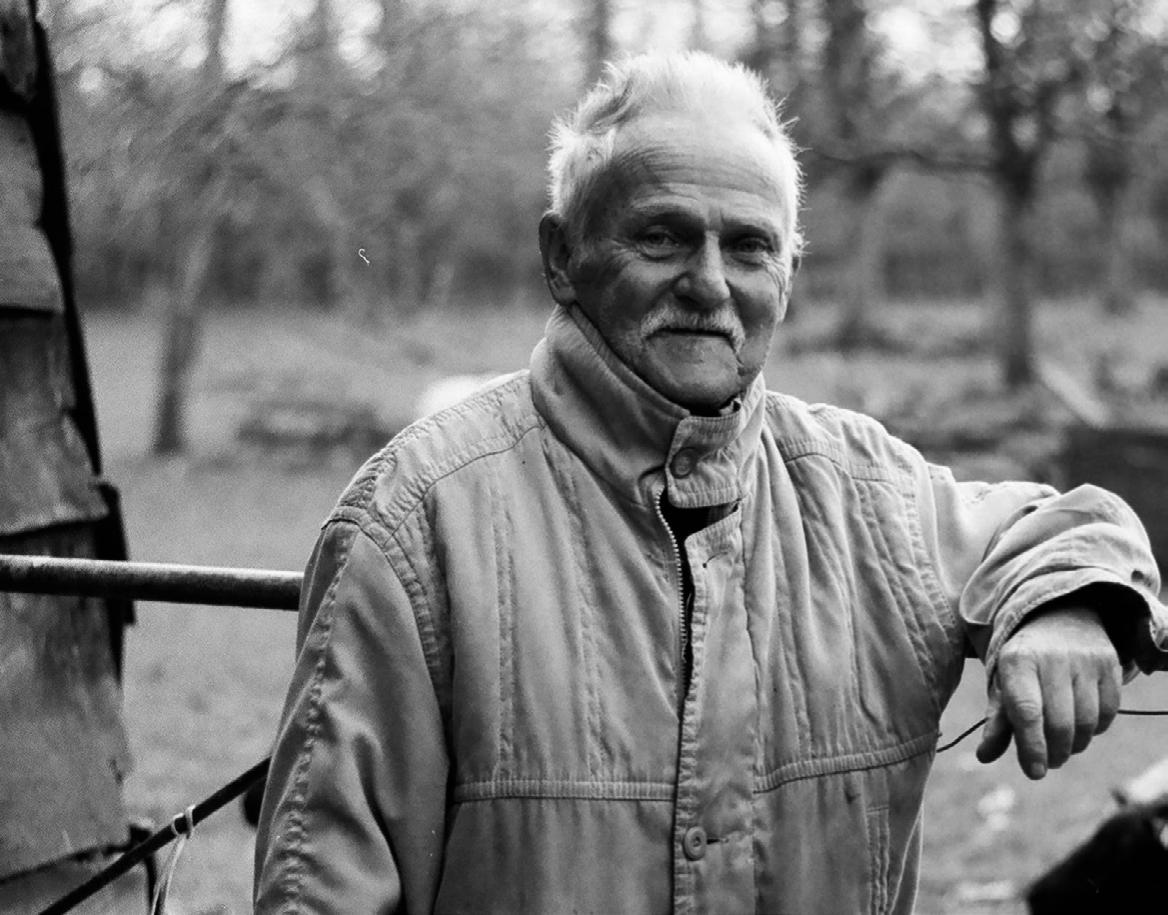
Eli Lilly and Company (Lilly) is a medicines company, headquartered in the United States, with a strong focus on bold science and innovative treatments for some of the world’s most challenging medical conditions.
Alongside breakthrough medicines in diabetes, obesity, oncology and immunology, Lilly has a strong commitment to neuroscience, including more than 35 years of research into Alzheimer’s disease.
Lilly’s President and General Manager in Australia, Tori Brown, shares her thoughts on the role of science and research in addressing dementia and helping society to age well.
Did you know that dementia is the leading cause of death for women in Australia, and the second leading cause of death overall? This statistic is shocking, but what’s even more alarming is that there doesn’t seem to be enough awareness or urgency to address dementia as a society.
Globally, attention on healthy ageing is increasing. In Australia, as is in most developed countries, our overall population is ageing and is expected to continue doing so for decades to come. Australians over 65 years will make up more than 19% of the population by 2030, and 25% by 2071, compared to 17% in 2022.1 This shift has major structural implications for our economy and society.
To maintain a healthy society, we must focus on ageing well: maintaining health, independence, connection and purpose as we age, whilst ensuring high quality care is available when it is needed. The cost of not having this focus is too high. Apart from increasing health and aged care costs, and negative impacts on quality of life and workforce, ageing “poorly” can place a large emotional and physical burden on families and caregivers, and force people to reduce or give up work to care for their loved
ones, further impacting productivity. Factoring in the dementia significantly increases these impacts.
Dementia is a debilitating and fatal disease that is most common in people over 65 years of age. While ageing increases the risk of dementia, dementia is not a normal part of ageing. In Australia, there are around 421,000 people that have dementia and 1.6 million carers, and these numbers are growing.2
Alzheimer’s disease is the leading cause of dementia, contributing to up to 70% of cases, so it goes without saying that reducing the impact and prevalence of Alzheimer’s disease is a crucial part of a healthy ageing agenda and essential to health system and economic sustainability worldwide. A 2022 report by the University of Canberra’s National Centre for Social and Economic Modelling (NATSEM) found that cases of Alzheimer’s disease are expected to nearly double in Australia by 2041 and will cost our national economy $26.6 billion annually.3
Research into Alzheimer’s disease has been underway for over a century. Collectively, there has been progress, but it has been slow and until now has not translated into meaningful options for people living with Alzheimer’s disease.
Now, for the first time, we are seeing real scientific advancement and a once in a generation opportunity to change the paradigm for people living with Alzheimer’s disease. Lilly alone has invested more than US$8 billion into Alzheimer’s disease research over the last 35 years, US$5 billion in the past decade. The combined research and action from industry, academia and charities is now starting to deliver new treatments that can delay Alzheimer’s disease progression, and there is a strong and promising pipeline of research sitting behind them. Alongside medicines innovation, there are new developments in early detection, nutrition and lifestyle interventions that can collectively help tackle this disease. It is entirely possible, and our hope, that in 10 years’ time, timely detection, accurate diagnosis, appropriate treatment and ultimately prevention of Alzheimer’s disease could be a reality – offering a different trajectory for the over 55 million people living with Alzheimer’s disease around the world.4
The challenge – and the opportunity – is to translate scientific research into practice in Australia in a timely way that reflects the urgency of tackling this disease. We cannot settle for waiting the average of 14 years to
2 www.dementia.org.au
3 National Centre for Social and Economic Modelling (2022) The Economic and Society Cost of Alzheimer’s Disease in Australia, 2021-2041, Canberra
4 Dementia statistics | Alzheimer’s Disease International (ADI) (alzint. org)



translate this research into routine clinical practice. 5 Enabling Australians to age well means making Alzheimer’s disease and dementia a social, health and political priority. It requires collective vision and partnership across government, health and aged care, patients and carers, industry and researchers to build a model of prevention, early detection, diagnosis and treatment, and to provide fast and affordable access to new treatments as they emerge in a way that is safe and equitable. It requires investment in infrastructure and workforce. And it requires a health technology assessment process in Australia that is contemporary and properly reflects the impact of Alzheimer’s disease on caregivers and aspects of life beyond the health sector in its valuation – without this, we risk disadvantaging older people when it comes to accessing medicines.
Australia has the opportunity to lead the way in how it responds to innovation in Alzheimer’s disease and dementia more broadly, creating an environment that fosters learning and rapid translation for the benefit of people living with Alzheimer’s disease, their loved ones, and society more broadly. Lilly is ready to play its part and partner with others across the ecosystem to make this a reality in Australia. Let’s not miss this opportunity.
5 Advancing Translation of Clinical Research Into Practice and Population Health Impact Through Implementation Science (mayoclinicproceedings.org)
Author: Tori Brown, President & General Manager, Eli Lilly
