







linkedin.com/company/healthinnovationwessex healthinnovationwessex.org.uk




Our impact in 2023-24
Finding and connecting innovators to health and care systems Developing, testing, and evaluating innovations in the real world











linkedin.com/company/healthinnovationwessex healthinnovationwessex.org.uk




Our impact in 2023-24
Finding and connecting innovators to health and care systems Developing, testing, and evaluating innovations in the real world


In 2023-24, we continued to work with our regional and national partners to improve health outcomes and support economic growth by transforming the way that health and care services find, test and implement evidence-based innovations.
This includes, as part of the Health Innovation Network, securing £475m of external funding secured by innovators, creating 554 jobs and safeguarding a further 755 during this 12 month period.
Our teams have helped to improve health and care across Hampshire, the Isle of Wight and Dorset during this time. Over 12000 referrals for further investigation were made as a result of the innovations we support to detect cancer at an earlier stage, with at least 576 cancers diagnosed. More than a thousand NHS staff received cancer education and training through our partnership with Wessex Cancer Alliance.
Almost 350 people in deprived communities who may struggle to access health services received blood pressure monitoring, and more than 33% were referred for further care. In Dorset, we contributed to 800 new patients being identified with familial hypercholesterolaemia, a genetic condition causing very high blood cholesterol levels which can lead to early heart disease if left untreated.
Over the last 12 months, we have grown and strengthened positive relationships with our local integrated care board (ICB) members and wider system partners.
These collaborative efforts have led to the co-production of delivery plans that address local health needs and align with the ICB Joint Forward Plans and integrated care partnership (ICP) strategies. Our system-wide work has garnered recognition by regional NHS England teams as a replicable model.
In 2023, we celebrated ten years since health innovation networks - formerly known as Academic Health Science Networks (AHSNs) - were established by NHS England. This important milestone was recognised with an announcement from NHS England and the government’s Office for Life Sciences confirming their intention to relicense for a further five year period as part of a £650m investment package to boost innovation within the UK’s life sciences sector. The welcome announcement is a testament to our collective impact and the way we have supported the development and spread of innovation across health and care services. Alongside the new licence came a clearer name for our network. Health Innovation Wessex continues to offer solutions to meet the challenges and priorities faced in health and care.
We also welcomed fresh leadership with Nicola Bent stepping into the role of CEO to drive us to achieve continued progress and prosperity. She is ably supported by her executive team, with a new Director of Innovation Adoption and Deputy CEO, and Director of Insight.
We know that innovation can transform lives. Alongside improving population health and patient care, innovation will help us to address health inequalities, reduce workforce pressures, deliver a net zero NHS by 2040, and provide value for money for the taxpayer. In a time of continued pressure and unprecedented demand on our health and care services, innovation has and will continue to contribute to healthier, longer lives for our communities.


Fiona Driscoll Chair Health Innovation Wessex Nicola Bent Chief Executive Officer Health Innovation Wessex
At Health Innovation Wessex we improve health, boost innovation, and support economic growth in our region’s life sciences and healthcare sector through the identification, adoption and spread of innovation.
We connect across the landscape of research, industry, commissioning provider trusts and the Wessex population, and bring together policy formulation and regulators, system design, operational frontline and stakeholder experience.
This role takes us across all parts of the NHS, local government, and other public agencies, into universities and the voluntary sector, and from entrepreneurial start-ups into established industry. By working across the system, we evaluate impact and create the conditions for innovation to benefit the people of Wessex.
and activities
Our national programmes are commissioned from NHS England (the Innovation, Research, Life Sciences and Strategy [IRLSS] group and the National Patient Safety Improvement Programme) and the Office for Life Sciences (OLS). The Wessex programmes are co-created to respond to the needs of our systems and delivered in partnership through our locality-focused delivery teams.
Finding and connecting innovators to health and care systems Developing, testing and evaluating innovations in the real world
Creating the conditions to innovate and bring about change 1 2 3 4
Adopting and spreading innovations
544 jobs created
£475m leveraged in grants and private investment
16 clients supported with evaluations
124 innovators received additional support 900 people in Dorset were surveyed about their experiences of using the FIT test to detect colorectal cancer
Up to 44 lives saved over the last 4 years due to improved outcomes for birthing parents and their babies
755 jobs safeguarded 1,094 NHS staff received cancer education and training through our partnership with Wessex Cancer Alliance
4,838 hours of support provided to innovators
75% of chief pharmacists piloting a new audit and assurance system (iQAAPS) reported that it made pharmacy aseptic services safer Our Innovation Exchange service helped 263 innovators
12,180 referrals made for further investigation as a result of the innovations we supported to detect early stage cancers
Over 80 people attended a genomics workshop hosted by HIW, Wessex Health Partners and the NHS Central and South Genomic Medicine Service Alliance
Maternity and neonatal coaching evaluated in 4 NHS trusts
We have helped our integrated care systems shape plans to meet their innovation priorities
1,349 views of our polypharmacy masterclass video
More than 200 women have accessed specialist perinatal trauma support
49 clinical staff trained to carry out structured medicines reviews for patients on long-term opioids for chronic noncancer pain
Cancer innovations assisted the diagnosis of at least 576 cancers, and helped to identify 12 people with pre-cancerous conditions that otherwise would not have been detected at an early stage
340 people attended outreach events in deprived communities for blood pressure monitoring; more than 33% were referred for further care
142 clinicians completed the Polypharmacy Action Learning Set (ALS) Foundation programme, with 5 accredited as ALS trainers
800 new Dorset patients identified as having familial hypercholesterolaemia

We help innovations reach health and social care faster to improve patient outcomes and value for the NHS, and to drive economic growth in the health and life sciences sector.
Finding and connecting innovators to health and care systems
We deliver end-to-end support for innovations in discovery, development or deployment. We support innovators from having a great idea through to successful launch and commercialisation.
Our tailored services include:
• Convening clinicians to advise on the current pathway and explore the potential value proposition
• Supporting innovators to find and win grant funding
• Providing both quantitative and qualitative market research
• Finding research partners to support clinical trials
• Helping innovators to navigate regulation and NHS standards
• Helping innovators to prepare for procurement opportunities.
We advise and develop evidence generation plans and undertake real world evaluations. We also advised innovators how to plan the adoption of their innovation and supported implementation in health and care settings.
“We came across a call for applications for technology support and that’s how we got talking - and we are on a fantastic journey together. Working with [HIW] and the rest of the team...you organised the health innovation surgery where I was able to test our commercial model with amazingly experienced senior people who do this day in and day out - they were critical friends and experts who encouraged us but also gave us constructive feedback. You helped us enable market insights; [...] we were working with clinicians but you also expanded that network for us. Writing applications for grants - all of those steps were refining my thinking and our concept. Working with Health Innovation Wessex gave us huge credential - to have you guys endorse us as an innovator has been amazingly important.”
Jyoti Sharma Founder, TaraCares Limited
Finding and connecting innovators to health and care systems
In 2023-24:
We supported 263 innovators to develop their ideas Of these, 124 innovators received further services
We provided 4,838 hours of support £475m funding was leveraged as part of the Health Innovation Network
Listen: In conversation with Jyoti Sharma, Founder and CEO of TaraCares Limited, a femtech AI startup: A healthcare innovator’s journey with Health Innovation Wessex

All NHS acute trusts have pharmacy aseptic units manufacturing bespoke injectable medicines such as chemotherapy agents. This high-risk work requires careful auditing by external specialists, which is time consuming for both the service and the auditor but is essential for maintaining quality and safety. Despite national standards, regional and hospital level variation was present across the audit process.
Health Innovation Wessex first met the Dorset-based CEO of Quiqsolutions at its Health Innovation Surgery in 2019, where it was shown the customisable audit tool. We provided support to extend the use of the audit tool to local GP practices and advised on routes to market such as procurement frameworks. In 2020, the tool was introduced to NHS Specialist Pharmacy Services (SPS) and we brokered early discussions to support bespoke creation of a cloud-based aseptic services auditing tool.
This tool, known as iQAAPS, was piloted in five hospital sites in Wales and 20 in England.
Our offer to conduct an independent evaluation of iQAAPS was a key factor in securing the contract to develop the system, as it de-risked this for both commissioner (NHS England) and the supplier. The Insight team at Health Innovation Wessex conducted a full evaluation of the value, impact, and challenges of iQAAPS for the auditing of high-risk clinical services.
Findings demonstrated better audits in less time, reducing risk to patients, improving productivity for hospital pharmacists, and providing national oversight of performance.
This independent evaluation supported full NHS commissioning and further spread of iQAAPS which, in April 2023, became a mandatory requirement for NHS audits in every aseptic pharmacy unit in Wales and England. It also generated a new income stream for Quiqsolutions, leading to multi-million pound investment from overseas.
Finding and connecting innovators to health and care systems
59% of high-risk pharmacy aseptic services
piloting iQAAPS said that it improved their quality audits
61% of services said that iQAAPS improved patient safety through greater compliance with quality standards and audit actions
75% of chief pharmacists and 44% of quality auditors reported that iQAAPS increased the awareness of quality assurance in aseptic units
Specialist pharmacists and auditors confirmed that the iQAAPS process had reduced their workload and released time
iQAAPs improved quality and risk management with oversight of audit outcomes and provided the first national dashboard

“The relationship and support from Health Innovation Wessex has been incredibly valuable in our journey; we would not be where we are today without it.”
Paul Kaye Business Development Director, Health & Care, Quiqsolutions
Perinatal trauma and loss impacts parents and families and affects their use of NHS services.
FLY Mama provide trauma-informed accessible and professional guidance to support the physical and emotional wellbeing of birthing people following perinatal trauma and loss. Modules provide content tailored to miscarriage, stillbirth, pregnancy after loss, and termination for medical reasons. FLY Mama’s specialist support during pregnancy and the postpartum period provides clinical information and access to physiotherapists, health coaches and holistic care to progress recovery.
We arranged market insights with midwives and our Local Maternity and Neonatal System (LMNS) Lead, and the innovator attended our four-day Wessex Health Innovation Programme. Course introductions with a lead
midwife resulted in a FLY Mama pilot at Hampshire Hospitals NHS Foundation Trust (HHFT) to support parents who have experienced birth trauma. The innovator attended an innovation surgery to further develop their commercial plans and value proposition. An evaluation surgery with the HIW Insight team enabled a review of the planned outcome measures and a focus on the process to demonstrate impact and benefits to parents.
Following the pilot’s success, additional licences were purchased to provide ongoing support. Based on the learning from the pilot, the Forget Me Not Children’s Hospice in Yorkshire used FLY Mama within their services for families experiencing baby loss. HIW’s Insight
team co-designed the logic model to evaluate the rollout at this site.
FLY Mama’s services also supported an employee programme for expectant/ new parents within a Welsh police force. Ahead of full deployment, HIW’s guidance enabled the co-founders to plan the rollout, the deployment in nonclinical provision, and follow up.
Throughout their innovation journey, FLY Mama received one-to-one mentoring from HIW, with successful grant applications made via our funding support service. These awards, including a £50,000 FAST START grant from Innovate UK, paid for additional product development.
Finding and connecting innovators to health and care systems
Over 200 women have been supported by FLY Mama via specialist charities, employee wellbeing programmes and as part of pilot projects in NHS maternity services
107 women accessed the FLY Mama platform to start a 12-month support programme through Hampshire Hospitals NHS Foundation Trust
8 support bundles were offered; Motherhood, Birth trauma recovery, Rainbow baby, Stillbirth and neonatal death, Termination for medical reasons, Pregnancy and baby loss (0-23 weeks), Life-limiting diagnosis during pregnancy and Postpartum

“Working with Health Innovation Wessex has been transformative for FLY Mama. The HIP course was fantastic, providing support and constructive feedback that turned our idea into a viable business model, helping us gain trust and contracts within the NHS and leading to two NHS trials to date.
Health Innovation Wessex’s expert advice and guidance have added credibility and trust to FLY Mama. Their evaluation surgery and implementation workshops have ensured the smooth running of our external partnerships.”
Michelle Norton-Hughes and Kelly Thistlethwaite Co-founders, FLY Mama

We provide independent expertise and capability in evaluation and implementation to support sustainable adoption of innovation. By doing so we help local health and care partners understand the impact of innovation on patients, staff and system activity.

Our Insight team provides independence and rigour in generating evidence about the impact and implementation of innovation across local, regional, and national systems. We employ creative approaches to test and verify innovation and create clear, engaging narratives to support behaviour change. We help learning health systems to improve by building capability in generating and using insights from innovation adoption within real world settings.
In 2023-24, we worked with our Industry and Innovation team to develop a real world evaluation programme providing evaluation support to our members in Wessex, with interest received from diverse clinical areas such as mental health, oncology, women’s health, and point of care testing. In 2023 we also launched a competition, funded by the Office for Life Sciences and open to innovators from all areas of England. Applicants came from a wide range of clinical areas and real world evaluations were awarded to projects in neurology and equipment decontamination.
We work with organisations to develop evaluation frameworks or surveys which they can use with their staff teams, patients, focus groups or integrate into their operational processes to improve delivery and stakeholder experience. We co-designed and produced with four organisations during 2023-24, including the production of a qualitative survey to capture user experience of endoscopy AI innovations within University Hospitals Dorset, and an evaluation framework for Fluid Motion Theatre which provides innovative creative activities to deliver early mental health and wellbeing support for children and young people.
The insight team also completed 12 evaluations at a local and national level across healthcare, academia and the voluntary and community sector. We began nine new evaluations, including CVD Prevention Innovation for Healthcare Inequalities Programme (InHIP2), the national Transforming Wound Care (TWC) programme, and the maternity triage service in Southampton, Hampshire, Isle of Wight and Portsmouth (SHIP).
We also enable organisations to better understand the readiness of their workforce and the existence of the conditions needed to enable effective innovation adoption. We supported systems in their strategic decision making through the application of our Attitudes Towards Innovation Survey (ATIS) tool.
12 evaluations were completed for clients in 2023-24
4 co-designed frameworks and surveys completed to support staff and user experience of innovation
9 evaluations were externally commissioned and started in year, continuing into 2024-25
2
large scale/long term evaluations continued during the
year (Dorset Innovation Hub and Alternatives to
Crisis)
Health Innovation Wessex was commissioned to evaluate a coaching programme designed to support Maternity and Neonatal Safety Improvement Programme preterm optimisation activity in the south of England. This evaluation was conducted in conjunction with the South East Leadership Academy, Health Education England and the Southampton, Hampshire, Isle of Wight and Portsmouth Local Maternity and Neonatal System. Four NHS trusts received the quality improvement coaching for eight to ten clinicians working in multidisciplinary maternity and neonatal teams.
The coaching was provided for six months. The evaluation was commissioned to help demonstrate the effectiveness and impact of the coaching programme. It engaged with 35 clinicians who took part in the initiative. The evaluation report has been shared with national colleagues and local partners. Consequently, there is appetite to spread the approach wider.

“Thank you for sharing a really comprehensive evaluation. I have found the pre and post measure really powerful across both Patient Safety Index and G3 team working surveys.”
Rebekah Giffney
Chartered Psychologist
Four NHS trusts each received six months’ QI coaching for eight to ten clinicians working in maternity and neonatal teams
Our evaluation engaged with 35 clinicians
100% of staff spoke highly of the coaching programme; it was reported to be educational, useful and they enjoyed developing skills with their colleagues
All four NHS trusts reported the coaching positively impacted on their team and on the objectives and processes
Staff felt more understood and listened to by their colleagues, and collectively supported to achieve team objectives. Staff felt that there was less conflict in their team following the coaching programme
All units saw a positive change in overall Patient Safety Index score, which indicates the coaching is valuable regardless of the context and culture of the maternity and neonatal unit
The impact of the programme has created appetite from the NHS England maternity and neonatal transformation programme leads to spread the coaching initiative to other NHS trusts
NHS England’s Innovation for Healthcare Inequalities Programme aims to address local healthcare inequalities experienced by deprived and other under-served populations. The collaboration between NHS England and Health Innovation Network teams, in partnership with integrated care systems, focused on five clinical areas of priority: maternity, mental health, respiratory, cancer diagnosis and cardiovascular disease, with the overall aim of improving access to the latest health technologies and medicines.
CVD causes one death every three minutes in the UK, with those in the most deprived areas four times more likely to die. 40% of people with hypertension in the UK are undiagnosed, and blood pressure monitoring is key. CVD is the single biggest area where the health service can save lives over the next ten years through targeted approaches to reduce health inequalities.
“It’s quite an easy experience, much better than having the pumping up of your arm for your blood pressure. So, she said that mine was a bit high, to have it checked again, and I could either to go to the doctors or come back here, so I said, oh, I’d rather come back here.”
Penny Thornhill Wellbeing Cafe
The aim of the programme was to increase clinical checks for hypertension and atrial fibrillation by engaging with local at-risk populations at communitybased events across the most deprived areas of Southampton and Portsmouth. At the events, participants were offered a blood pressure prediction via a device for measuring vital signs called Lifelight (manufactured by xim Ltd). Lifelight uses a smart device
Developing, testing, and evaluating innovations in the real world
with camera to measure pulse and respiration rate and applies an algorithm to predict blood pressure levels. Participants were then measured using a manual cuff and escalated for further blood pressure monitoring if required.
The evaluation assessed the approach to using two diagnostic methods from the perspective of the public attending the community testing events, healthcare staff and trusted community leaders, as well as outcomes on access to testing, diagnosis and clinical pathways. The findings informed future HIOW ICS strategic decisions related to health inequalities and access to healthcare.
Watch BBC South Today’s report about our innovative outreach sessions

340 people attended five community outreach events 123 people attending the events were identified for escalated care after having their blood pressure monitored
HIOW ICB has successfully bid for £57,000 additional funding to expand the CVD project to a further five primary care networks (PCNs) as a result of this evaluation, and we have been invited to provide evaluation support Best practice outcomes were shared with the Dorset CVD team to spread learning. The approach has helped shape the design of Hampshire and Isle of Wight Women’s Health Hubs

We enable health and care systems to understand, adopt and spread proven innovation through applying tested tools and frameworks. Through co-production and delivery, we act on key priorities to sustain innovative solutions, deliver sustainable change, and ensure positive outcomes for the workforce and people across Wessex.

We support our local health and care systems to adopt innovation, including
• new care pathways
• devices, digital technologies
• diagnostic technologies, and
• novel workforce practices.
We also help them to benefit from inward investment and economic growth.
When ICBs were formed in 2022, Health Innovation Wessex was commissioned to support integrated care systems to translate research findings, real world evidence and innovation into practice.
Throughout 2023-24 we worked closely with the integrated care boards (ICBs) to co-design delivery plans aligned to their local priorities.
Improving outcomes in population health and healthcare
Tackling inequalities in outcomes, experience and access
Enhancing productivity and value for money
Helping the NHS support broader social and economic development

Local Dorset ICB Agreed Priorities
Cardiovascular Disease (CVD)
National Patient Safety Programme
Five delivery areas based on NHS Patient Safety Strategy priorities
Rollout of named medtech, supported by national policy
National Cardiovascular Disease Programme
National Health Inequalities Programme
National MedTech Funding Mandate Programme Regional Polypharmacy
Blood Pressure Optimisation (BPO), Familial Hypercholesterolaemia (FH), Lipid Management
InHIP CVD project (hypertension identification) Faecal Immunochemical Testing (FIT) project Admission Avoidance, Virtual Wards and Technology Place-based Partnerships
Cross-cutting themes
Priority area being patients aged 75 and over taking NSAIDs and medicines known to increase risk of AKI
Workforce, Environmental Sustainability, Patient Partners & Community Conversations, Digital, and Health inequalities
Regional Early Cancer Diagnosis Programme
Insight (Evaluation) Economic Growth
Delivering real world evaluations to support impact assessment and a learning health system
Faster adoption of innovations to improve early diagnosis Signposting
Understanding need Real world validation Spreading innovation
“The support, leadership, advice and insights HIW have provided have been absolutely paramount in driving forward the Dorset Women’s Health Programme. We’re extremely lucky to be working with them, and hugely benefit from their skills and expertise. The programme should be a huge success due to our joint working and the skills they bring.”
Helen Crook Programme Manager - Transformation Delivery, NHS Dorset
“The work with Women’s Health Hubs has helped bring some clarity and focus, creating a set of priorities that have harnessed the ideas and enthusiasm of our clinicians and user groups. Your willingness to be present, involved and help lead has been great.”
Paul Johnson Chief Medical Officer, NHS Dorset
Local HIOW
ICB Agreed Priorities
National Patient Safety Programme
National MedTech Funding Mandate Programme
National Cardiovascular Disease Programme
National Health Inequalities Programme
Regional Early Cancer Diagnosis Programme
Mental health and wellbeing
Frailty, Virtual Wards and Technology Polypharmacy
Five delivery areas based on NHS Patient Safety Strategy priorities
Rollout of named medtech, supported by national policy
Blood Pressure Optimisation (BPO), Familial Hypercholesterolaemia (FH), Lipid Management
InHIP CVD project (hypertension identification) Health inequalities cross-cutting through all workstreams
Faster adoption of innovations to improve early diagnosis
Cross-cutting themes
Workforce, Environmental Sustainability, Patient Partners & Community Conversations, Digital, and Health inequalities
Insight (Evaluation)
Delivering real world evaluations to support impact assessment and a learning health system
Economic Growth
Understanding need
Signposting
Real world validation Spreading innovation
Cross-cutting themes
“We have worked hard to establish a successful partnership in 2023-24 and focused on delivering programmes of work to support our virtual ward development, provision of mental health services for children and young people, and reducing problematic polypharmacy.
These workstreams have a clear alignment with our system transformation efforts and priorities for our population, weaving together the national and regional work which Health Innovation Wessex is commissioned to deliver locally, alongside the priority areas described in our Joint Forward Plan.
Our agreed programme of work supports Hampshire and Isle of Wight’s strategic priorities. We look forward to continuing to collaborate with Health Innovation Wessex in the achievement of these objectives.”
Dr Lara Alloway Chief Medical Officer, Hampshire and Isle of Wight Integrated Care Board
As one of 15 regional collaboratives in England, Wessex Patient Safety Collaborative (PSC) improves patient safety and reduce avoidable patient harm by working with staff and patients across Wessex to achieve the objectives set out in the NHS Patient Safety Strategy.
We use quality improvement (QI), networking and scale-up methods to deliver projects within five priority areas:
• Managing Deterioration
• System Safety
• Medicines Safety
• Mental Health, Learning Disability and Autism
• Maternity and Neonatal.
Patient safety is integral to quality care and patient experience - it focuses on maximising the things that go right and minimising the things that go wrong for people experiencing healthcare. Our PSC can identify and roll out safer care initiatives within the NHS and industry, ensuring these are shared across our local health and care system.
We support this work with three objectives:
• to develop QI capability
• to encourage patient, family, and carer involvement in improvement, and
• to facilitate the development of a positive safety culture.
‘You have encouraged and supported Beechwood so much, and without you we would not have had the confidence to get involved in a QI project, which led us on to being recognised and winning awards.’
Elaine Gomez Ward Manager
Our collaborative comprises all the NHS providers and commissioners across the Wessex region, including hospitals, mental health and community organisations, the ambulance service and primary care. It brings together local patients and healthcare staff, all driven by a shared vision to bring about system-wide improvements to ensure the safety and wellbeing of people in the care of our health services.
To support systems to test and spread effective safety interventions and strategies, learn from excellence and continuously improve
National PS Improvement Priorities 2023-24
Workstreams 2023-24
Mental Health, Learning Disability and Autism System Safety
Improving chronic non-cancer pain management by reducing high-risk opioid prescribing
Reducing restrictive practice
Pre-term optimisation Managing maternal and neonatal deterioration

Managing Deterioration: This national programme was paused in June 2023. We co-produced an additional communication video with care homes to help staff to frame conversations, escalate clinical concerns and improve patient care.
System Safety: We have co-facilitated workshops and communities of practice at both ICB and regional level to ease the transition to the Patient Safety Incident Response Framework (PSIRF). This sets out the NHS approach to developing and maintaining effective systems and processes for responding to patient safety incidents for the purpose of learning and improvement.
Medicines Safety: We held an opioid prescribing masterclass attended by 49 delegates including GPs, pharmacists and pharmacy technicians. Following positive feedback this is being repeated in 2024-25 and written into the local ICB incentives scheme.
Mental Health, Learning Disability and Autism: Individual support to 17 wards has resulted in a number of local improvements to reducing restrictive practice, preventing suicide and self-harm, and embedding sexual safety standards.
Up to 44 lives were saved over the last four years due to improved outcomes for people giving birth and their babies
49 primary care clinical staff trained in how to carry out structured medicines reviews for patients who have been taking long term opioids for chronic non-cancer pain
4 in-patient mental health units have reduced restrictive practice due to support from our mental health safety programme
Over 2m views of our managing deterioration programme RESTORE2 videos produced to help carers and clinicians recognise when someone is becoming unwell
Maternity and Neonatal: We hosted our first in-person event in over four years to share regional quality improvement projects and national programme updates with matneo staff. 97% of attendees said the initiative met or exceeded their expectations and 100% said they would attend future events.
“If the Wessex Opioid Working Group had not been established, I think I would have thrown in the towel because prior to that it was so hard to get anyone to take notice of the work needed to be done to tackle this.”
Pain Medicines Management Pharmacist, Southampton Locality


Polypharmacy and overprescribing have been highlighted by the Department of Health and Social Care and NHS England as a concern especially in older people. Studies have shown that up to 16% of unplanned admissions to hospital are due to adverse drug reactions with polypharmacy being a major cause of these admissions to hospital.
Over one million people in England take ten or more medicines and over 400,000 of those people are aged 75 and over.
In Wessex, almost 40,000 people take ten or more medicines. 18,000 of them are aged 75 or over, and 6,500 are aged 85 or over.
The Health Innovation Network Polypharmacy programme aims to help local systems to:
• identify patients deemed to be at the greatest risk from harm from polypharmacy (Pillar 1)
• upskill the primary care workforce to carry our high-quality structured medication reviews to reduce unnecessary prescribing (Pillar 2)
• support patients to share their issues, concerns, and expectations about their medicines, especially in their later years. (Pillar 3)
1340 views of our polypharmacy masterclass videos
275 local clinicians attended four of our national polypharmacy masterclasses
142 local clinicians completed the Action Learning Set Foundation (ALSF) programme with 5 local clinicians accredited as ALS trainers
73 local clinicians from a range of disciplines joined our polypharmacy communities of practice
“Really fantastic learning. Felt very fortunate to hear from experts in the field that established evidence for what we do and why we do it.”
Masterclass delegate

Cardiovascular disease (CVD) is a leading cause of illness and death in England, with high blood pressure and high cholesterol leading risk factors. We prioritised the early detection and effective management of CVD to prevent life changing events such as stroke and heart attack, and to reduce the incidence of premature death.
Key elements of the programme focused on:
• detecting hypertension and optimising blood pressure
• lipid (cholesterol) services and treatment, and
• the identification of familial hypercholesterolemia (FH).
Treatment of high blood pressure (hypertension) substantially lowers the risk of cardiovascular disease, but around 30% of people with high blood pressure are unaware of their condition. Around 50% of people with established CVD also have high blood pressure, but many are either on no treatment or treatment that could be improved.

We shared assets from across the Health Innovation Network, including UCLP’s Proactive Care Framework for hypertension, to help primary care networks prioritise which patients to see first and to provide the best care and management of patients with high blood pressure.
In Hampshire and the Isle of Wight, the Innovation for Healthcare Inequalities Programme (InHIP) improved access to CVD health checks in areas of greatest deprivation, through five community outreach events targeted at people who don’t normally engage with healthcare services to get their blood pressure checked. Introducing the use of vital signs technology that provides cuff-free blood pressure and heart rate monitoring to complement conventional measurement, 123 people from the 350 attendees at the outreach sessions were referred for further care. Adopting and spreading
“Really brilliant idea. A lot of people that we see would never set foot in a GP surgery, they find it quite intimidating but happy to come somewhere like this, somewhere less clinical.”
Organiser, Horizon Wellbeing Hub Pod Launch

“There are loads of barriers aren’t there to making an appointment, having the courage to go in, the worry about what you might find. And particularly with blood pressure, if it’s all being taken in a really relaxed environment we’re pulling out the best in people. So I think if we can take any services to where people are at, it reduces the barriers, it makes it more straightforward, and that has to be a good thing.”
Astrid Vaswani Minister, Thornhill Baptist Church

We supported local health systems to optimise lipid management to prevent cardiovascular disease. Working with industry (Sanofi and Amgen) we mapped secondary care lipid management services across Wessex, providing a system-developed options appraisal and recommendations to improve how patients access and receive diagnosis and treatment.
We also supported local systems to implement and evaluate innovative technology such as OMRON to enable the transfer of data into clinical systems.
Familial hypercholesterolaemia (FH) is an inherited condition which leads to exceptionally high cholesterol levels, often two to four times those of the general population. It is estimated that one in 250 people may have FH in the UK but fewer than 10% of these people have been diagnosed, and are at increased risk of heart attack or stroke.
We focused on increasing the number of patients identified and treated for FH through diagnosis in primary care. We mapped the Dorset genetic referral pathway to understand where improvements could be made and innovation introduced; and provided education and training in FH identification to over 350 healthcare staff. We also helped primary care networks to implement the UCLP Proactive Care Framework, a toolkit for management of FH.
By April 2024, 800 new patients in Dorset with FH had been identified, and 82% of primary care networks in our region had made at least one order for the novel cholesterol-lowering treatment, Inclisiran.

800 new patients in Dorset identified as having familial hypercholesterolaemia
Over 350 people have attended educational events delivered or supported by Health Innovation Wessex
82% of primary care networks across Wessex made at least one order for the new cholesterol-lowering treatment, Inclisiran
Delivery of our InHIP programme via community outreach was featured on BBC regional news - Revolutionising access to health checks in Hampshire
241 people trained in familial hypercholesterolaemia and lipid management across Dorset, Hampshire and the Isle of Wight
NHS Dorset wanted to use health economics to demonstrate the value of digital intervention and to apply this knowledge across their system. Health Innovation Wessex was asked to deliver a webinar which would provide local system staff with a basic understanding around health economics, the role of the National Institute for Health and Care Excellence (NICE), and the ICB’s strategic and commissioning priorities.
The NICE Technology Appraisals team presented ‘An Introduction to Health Economics’. The webinar, hosted in November 2023, was attended by 52 delegates from across Dorset, Oxford, and Hampshire and the Isle of Wight as part of HIW’s support to integrated care systems to use cost effective analysis to help evidence impact and value of service transformation. The session started with debunking myths related to health economics before demonstrating how best to assess cost effectiveness in healthcare.
Participants were surveyed preand post-session to measure their knowledge of health economics, its relevance to their job role, and their confidence in using cost effective analysis. Feedback was overwhelmingly positive in terms of enjoying the content and increasing their levels of understanding of health economics, demonstrating a 50% increase in knowledge amongst the delegates.
Watch the health economics webinar
“I think that today demonstrated clearly that all ICS will need support in this, and that webinar will be sought after across all areas!
Thank you again for being so listening to my ask and doing a great job in smashing the answer so we can take all disciplines on this adventure.”
Crystal Dennis Deputy Director – Digital & Technology, NHS Dorset
Training delivered to 52 delegates Attended by senior leaders, heads of department, commissioners and evaluation specialists
50% increase in knowledge following the session of those surveyed

Since 2020, Health Innovation Wessex has collaborated with Wessex Cancer Alliance (WCA) to deliver a cancer innovation programme to identify and support the adoption and spread of innovations in Wessex. The programme enables teams to achieve the ambitions of the NHS England Long Term Plan by:
• building links with local, regional and national teams involved in the diagnosis of cancer and the implementation of innovations
• developing relationships with cancer Clinical Advisory Groups across Wessex
• gathering insight to understand which cancers would benefit the most from early diagnosis and map any unmet needs against available and proven innovations
• using the HIW cancer innovation horizon scan to identify tested and proven innovations adopted by other health innovation network/ Cancer Alliance teams that may benefit local need
• working with WCA and local cancer leads to establish spread and adoption plan of cancer innovations – including plans on how to identify suitable early adopters, innovation scale up across other relevant teams and longer-term sustainability of innovation adoption
• supporting and enabling the spread and adoption of nationally approved innovations.
“The biggest lesson I’ve learned with any innovation and adoption is that it’s not something you can do as one person, you can’t do it in isolation of others. There is a need to find the right people to help you and that might be different people for different projects, as we all have our different strengths, experiences of how certain parts of the project would work.”
Anna Wykes Programme Manager for Cancer Care, Health Innovation Wessex
£880,000 in funding won to support two new pilots benefiting 12,621 patients
1,094 NHS staff have received training and education via the pilots
Development and chairing of a national community of practice
12,180 referrals for further investigation were made as a result of the innovations we support to detect early stage cancers
Cancer innovations assisted the diagnosis of at least 576 cancers, and helped to identify 12 people with precancerous conditions that otherwise would not have been detected at an early stage
Listen to the Wessex Cancer Innovation Programme podcast

Colorectal cancer is the fourth most common cancer, with poorer outcomes affecting those living in communities with higher social deprivation. While the use of the NICE-approved faecal immunochemical test (FIT) is one way of supporting earlier detection, uptake remains low in some communities, particularly those in areas of deprivation.
Health Innovation Wessex (HIW) supported the Dorset ICS Cancer Programme to engage with people across the county to understand their awareness and experiences of using FIT.
This included a survey to the Dorset public and those less likely to complete a test (people experiencing homelessness, learning disability, fishermen, farmers, and construction workers) to gather insight and identify interventions that would support uptake from people with suspected colorectal cancer.
Instructional videos and standardised patient information were then tested through a second public survey and directly with the Core20PLUS5* groups to understand if they would encourage people to complete a test.
A clinical decision support tool, C the Signs, was also implemented across all Dorset primary care networks (PCNs) to enable teams to track and monitor patient uptake of FIT. This improvement to the pathway contributed to over 3500 referrals requested for further investigation, and 36 cancers detected.
Outcomes of this work were independently evaluated by HIW.
We engaged with over 900 members of the public
C the Signs was implemented in all 73 practices across all 18 primary care networks in Dorset
Work started with Mast Ltd to change the transparency of the packaging for completed kits following patient feedback that it was embarrassing to return these in person. This update is anticipated to benefit patients across England
Funding of £292,000 was received from NHS England and Wessex Cancer Alliance, with industry providing £30,000 in-kind for evaluation

“This project is a great example of the power public engagement can have on influencing how we make diagnostic tests more accessible.”
Anna Wykes Programme Manager for
Cancer
Care, Health Innovation Wessex
The frailty virtual wards and technology enabled care project was co-developed with Hampshire and Isle of Wight Integrated Care Board (ICB) as part of their 2023-24 delivery plan and aligned with the following ICB priorities - frailty and virtual wards; system working; productivity; and efficiency and developing models of care.
This project has supplemented information on the ICB’s readiness to innovation adoption of wearables and provided identification of the key issues/ opportunities and next steps for scaling of technology enabled care on virtual wards.
The aim of the project was for the ICB to understand innovation challenges in implementing technology enabled care (wearables) in frailty virtual wards using the following techniques:
• a Rapid Insight event – to undertake a rapid cycle of engagement, data collection, analysis and feedback to capture and analyse the lessons from adopting innovation.
• an Attitudes Towards Innovation Survey (ATIS) - to measure the attitudes towards innovation of staff working in health and social care.
• clinician feedback – to gain their feedback on the selected innovations.
• patient/carer feedback - to gain their feedback on the selected innovations.
• observations of the ICB implementing the project, as well as how clinical colleagues implemented locally.
38 attendees from across the integrated care system contributed to a Rapid Insight event to learn from local experiences of innovation
4 face-to face training sessions observed, and 12 virtual check-ins attended with clinical teams to build our relationships
21 respondents provided valuable insight of innovation readiness within the ICB and local providers through the ATIS survey
2 reports co-produced, detailing 11 recommendations to further enhance innovation adoption across the ICS

“Our work with Health Innovation Wessex is aligned and purposeful. We are learning together how to most effectively deploy Health Innovation Wessex to maximise impact for both them and NHS partners and the wider system. During 2023-24 we have been sharing and consolidating communications, governance and ways of working aligned to key priorities to support Health Innovation Wessex working effectively within the system. The Health Innovation Wessex team have been highly supportive, responsive and constructive in our shared endeavor to identify areas of focus aligned to our strategic objectives.”
Frances Wiseman Director of Insight and Improvement, Hampshire and Isle of Wight ICB

Health Innovation Wessex aims to create the conditions to encourage the discovery, development, and deployment of innovative solutions to address current and future system challenges.

The NHS has a long history of innovation which has transformed patients’ lives and brought huge benefits to society and the UK economy.
Innovation is now more important than ever, but it is not without its challenges within the wider health innovation ecosystem. There is a need for all partners in the life sciences ecosystem to align efforts more closely and to support this in ensuring innovations can go further, faster in the future.
NHS England, working with the Innovation, Research, Life Sciences and Strategy (IRLSS) team has engaged national innovation partners, local systems, industry, and research charities to develop a clear blueprint for how the NHS and social care can best support and benefit from a strong life sciences ecosystem.
The Learning by Doing workstream was led by Roland Sinker (Chief Executive, Cambridge University Hospitals NHS Foundation Trust), Professor Gary Ford (Chief Executive Officer, Health Innovation Oxford & Thames Valley) and Dr Sam Roberts (Chief Executive, National Institute for Health and Care Excellence [NICE]).
Creating the conditions to innovate and bring about change
The aim of this workstream was to rapidly generate insights from the health innovation ecosystem, including those from NHS organisations, academia, industry, and patients/public.
The Innovation, Research, Life Sciences and Strategy (IRLSS) team and NHS England, along with Health Innovation Wessex, Health Innovation South West, and Health Innovation West of England, delivered a series of three Learning Collaboratives between November 2023 and February 2024 to generate insights with local system partners, representatives from the Health Innovation Network, Industry, and implementation leads from the regional NIHR Applied Research Collaboratives.
“For the Innovation Ecosystem Programme to be impactful, its emerging hypotheses and ideas need to be tested robustly with a range of key stakeholders.
The Health Innovation Wessex Rapid Insight and Learning Collaborative methodology for facilitating this testing has proven invaluable, generating rich insights and learning to refine key Innovation Ecosystem Programme outputs.”
Dr Samantha
Roberts
Chief Executive,
National Institute of Health and Care Excellence (NICE)
132 attendees across three Learning Collaboratives which explored practical ideas and recommendations to overcoming innovation adoption barriers
Delivered a national rapid insight event, summary analysis and report detailing the resonance of 9 innovation adoption hypotheses
Reported 4 primary recommendations for national consideration alongside 6 national and 4 local enabling activities which will feed into the overarching Innovation Ecosystem Programme and policy
People working in health and care interact with innovations in a variety of ways, yet the health and care workforce is not systematically supported to adopt innovations, which can be a complex process.
Health Innovation Wessex (HIW) on behalf of the Health Innovation Network worked with NHS England’s Innovation, Research, Life Sciences, and Strategy (IRLSS) team to develop a suite of educational resources to equip the NHS, social care and voluntary sector workforce with the knowledge and skills needed to successfully adopt innovations within their team, service or system – at an awareness level.
People require support to increase their capacity, capability and confidence to use innovations to meet their needs and the needs of their patients, service users and communities. However, currently there is no standard programme for innovation adoption training (practical skills development) or education (theoretical knowledge development). NHS England and partners are therefore developing an innovation adoption programme to support local and regional systems through a range of education and training offers for different audiences.
To support this ambition, in early 2023 we worked with NHS England and partners to conduct webinars with stakeholders from across the health and care workforce to understand what their learning needs were in terms of innovation adoption. This enabled the refinement of topic areas that could fit into an innovation adoption ‘awareness level package’.
The aim of this phase was to build on the work undertaken by HIW and the IRLSS in Phase 1 and to focus on:
• an evaluation of the 60 curated resources from Phase 1
• the development of a self-assessment framework for individuals to use the curated resources
• the creation and curation of a suite of communication materials to promote the resource
• the facilitation of two face-to-face events.

Creation of a self-assessment capabilities framework which includes 12 principles
Designed an offline navigational tool for the 60 resources based on 12 guiding principles
A suite of communications assets which support the promotion of innovation adoption. Including copy for campaigns, case studies, graphics and images, and a 90 second animation
Extensive materials and resources for innovation adoption events
Creating the conditions to innovate and bring about change
Allied health professional support worker evaluation framework
Hampshire and Isle of Wight Integrated Care Board (HIOW ICB) Allied Health Professional (AHP) Faculty intended to build on national strategies such as The Allied Health Professions (AHP) Strategy for England: AHPs Deliver, which was developed to provide strategic direction to AHPs to maximise their contribution to improving health outcomes. The strategy represents the whole AHP community: support workers, assistant practitioners, registered professionals, pre-registration apprentices, and students. In 2022, a co-produced AHP Support Worker Development Strategy was developed by the HIOW ICB AHP Faculty.
The need for an evaluation of this strategy was recognised as a priority to ensure the commitments in the strategy were being achieved. HIOW ICB AHP Faculty approached Health Innovation Wessex in February 2023 for support with this evaluation.
The overall project aim, commissioned by Health Education England South East was to co-produce an evaluation framework which could be implemented independently by HIOW ICB AHP Faculty to measure how the three-year AHP Support Worker Development Strategy had been delivered.
During 2023-24 we provided an exemplar of how to analyse survey data, develop conclusions from survey data, and demonstrate how these conclusions could inform future planning when applied to 181 AHP support worker surveys which the faculty had undertaken.
Alongside the HIW exemplar report, we also developed an evaluation framework and two bespoke co-produced data collection tools.

We produced a framework for the HIOW AHP Faculty to measure how its three-year development strategy had been delivered We provided an exemplar report demonstrating how to analyse the data and conclusions from 181 staff surveys, and use the learning to support AHP development further
The co-production sessions enabled ICB AHP staff to develop data collection and analysis capabilities beyond HIW involvement

“I think that the work that you are doing is brilliant. I hope that you will agree with me when I say it would be great to share the results across all South East region AHP Faculties, perhaps by presenting at one of the Regional AHP Faculties Network meetings.”
NHS England South East regional office
Our Industry and Innovation team organise training events, programmes and masterclasses to support health and care innovators along their development journey. These opportunities enable the innovator to learn from experts in their field, network with other innovators, and help them to develop their innovation and establish the foundations of a robust and credible business model to meet NHS and healthcare needs.
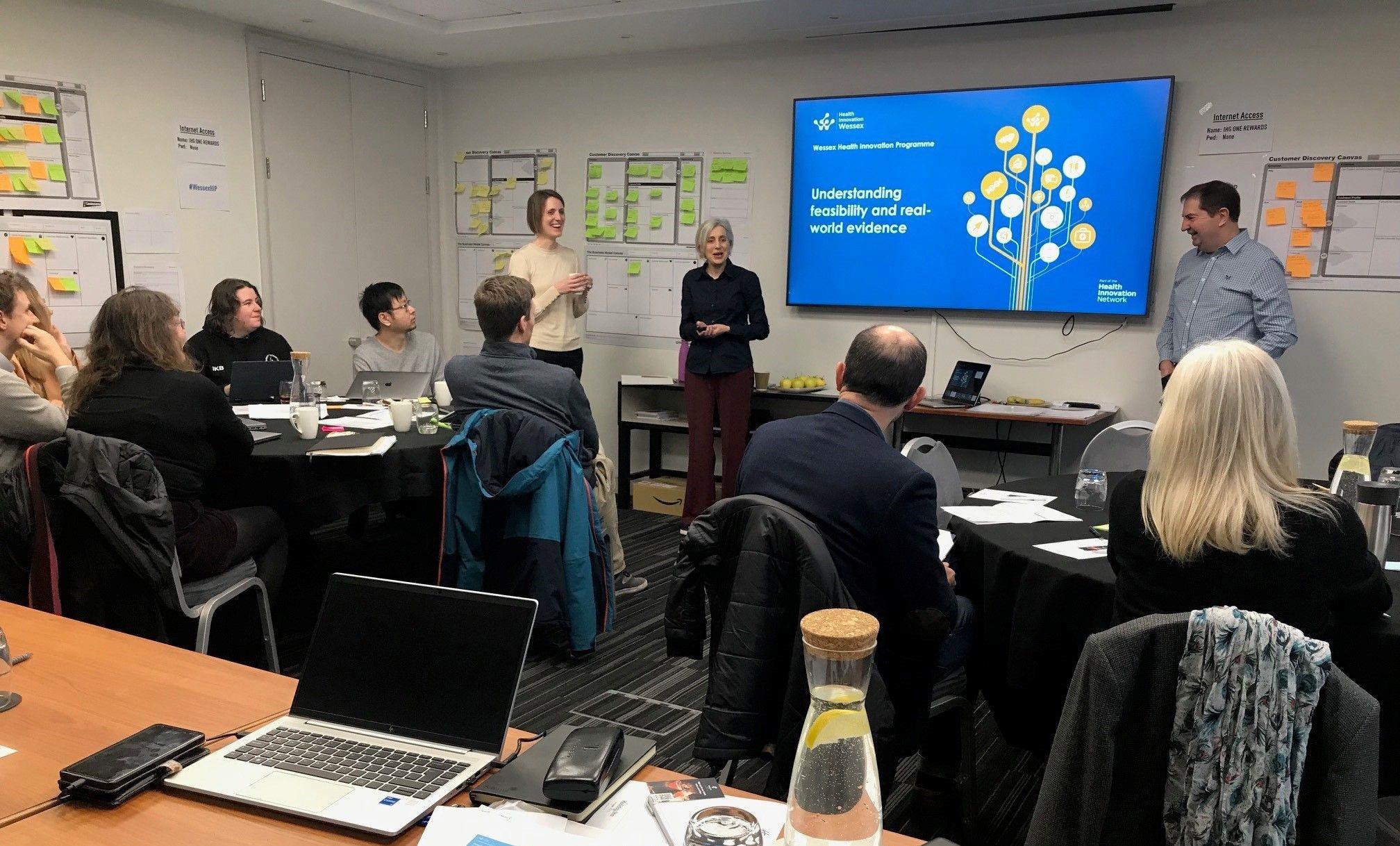
We delivered the interactive Wessex Health Innovation Programme (HIP) four-day course to 12 innovators, in partnership with the University of Southampton (Catalyst). The HIP was designed to help innovators test the validity of their business model and equip them with effective tools to explain the value of their proposition to potential funders and future customers in the NHS and healthcare sector. The course is designed for innovators and entrepreneurs from clinical, academic or commercial organisations engaged in developing healthcare-related products or services from early stage to market ready that could have a positive impact and deliver benefits to the NHS and social care organisations.
Creating the conditions to innovate and bring about change
In 2023-24, 158 delegates attended our innovator masterclasses on a range of topics including:
• grant writing
• medical device regulation
• building knowledge transfer
• evaluation – what is it and why do it?
“Excellent, insightful, and collaborative.”
“The breadth of the coverage from idea to adoption was excellent. The knowledge was very well transferred.”
Delegates from the Wessex Health Innovation Programme four-day accelerator course
158 delegates attended our innovator masterclasses during 2023-24
43 delegates attended the grant writing masterclass with 60% from innovation companies and 20% from the University of Southampton
31 delegates attended the medical device regulation masterclass with 55% from innovation companies and 29% from the University of Southampton
58 delegates attended the building knowledge transfer masterclass with 88% of attendees coming from universities
26 delegates attended the evaluation masterclass with 80% currently developing an innovation
Health Innovation Wessex is one of 15 founding partners drawn from health, research and academia to establish Wessex Health Partners, a strategic partnership formed to:
• improve the region’s collective ability to tackle the greatest challenges facing the Wessex health and care system
• generate greater collaborative and interdisciplinary research and speed the development and adoption of innovation at scale.
This mandate to collaborate has seen Health Innovation Wessex connect regularly during 2023-24 with Dorset
universities (Bournemouth University and AECC University College - now Health Sciences University), Wessex Health Partners and the NIHR Applied Research Collaboration Wessex (NIHR ARC Wessex) to support research into practice, including areas such as the Women’s Health Hub, Children and Young People – Healthy Weight, and avoidant restrictive food intake disorder (ARFID). These partnerships are important for enhancing discovery into practice, strengthening connections and sharing learning across our region.
HIW was invited by WHP to join the Clean Air South Network with local system partners, including the University of Southampton Sustainability and Resilience Institute, to address the region’s health inequity issues linked to poor air quality.

Our Director of Insight is also Implementation Lead for NIHR ARC Wessex, the arm of NIHR applying research to address immediate issues facing health and social care, and bringing research evidence into practice and training. We work closely together to share and implement knowledge, and to optimise the impact of findings and innovations from applied health research.
178 people attended the NIHR ARC Wessex Annual Stakeholder event in June 2023. Jointly hosted with HIW, it presented an opportunity to celebrate research and innovation which addresses health inequalities in our region.
In June 2023, the jointly-resourced NHS Insight Prioritisation Programme (NIPP), reported on use, applicability and acceptability of digital remote monitoring for people living with frailty in the community. This work described implications for policy and practice in relation to frailty care pathways and virtual wards.
The team also developed a webbased implementation toolkit for practitioners and researchers to inform implementation planning.
During 2023-24 ARC Wessex and HIW produced an accessible Workforce Evaluation Toolkit for system partners which was co-designed with stakeholders. The proof of concept is ready for testing in 2024-25.
We co-designed a survey to identify ‘adoption-ready’ research outputs or innovations from across the ARC community, to introduce candidate projects to our systems that are aligned with their priorities. The survey will be conducted in 2024-25.
In 2023 HIW supported several university events, including the Responsible Innovation in Health Technology showcase hosted by the University of Southampton with the University of Portsmouth, UKRI and Empact Ventures.
We also designed a one-day intellectual property (IP) workshop, in partnership with the University of Southampton, aimed predominantly at university staff to introduce the requirements, challenges and opportunities associated with IP created through academic and clinical research and development.
The event was attended by 40 people and due to its success, will run again in 2024-25.

In November 2023, Health Innovation Wessex, Wessex Health Partners (WHP), and the NHS Central and South Genomic Medicine Service Alliance jointly hosted a workshop which brought together more than 80 people from the NHS, universities, and the local research and innovation ecosystem to review the government’s ten-year ambition to make the UK the most advanced genomic healthcare system in the world.
The focus of the day was to reflect on the delivery of the UK’s 2020 genomic strategy three years on and discuss its impact on many areas of health and care, including screening, risk and prevention; diagnosis, targeted therapies and treatment; patient and public engagement; workforce; and industry partnerships.
Attendees joined ten sessions throughout the day, with presentations and talks covering different topics, from pharmacogenomics within stroke services to screening for newborns.
Professor Dame Sue Hill, Chief Scientific Officer for NHS England and Senior Responsible Officer for Genomics in the NHS, delivered the keynote speech outlining the current genomic landscape. The workshop concluded with an expert panel discussion focused on the future of genomics and next steps for Wessex.
Watch speakers and delegates reflect on the Wessex genomics workshop
“The opportunities for our region brought about by the UK’s genomics strategy are big – a Wessex excelling in education, genomics research, and health and care delivery would benefit local patients, local populations, our workforce, our universities, our industry partnerships, and the taxpayer. With sustained system-level commitment, we know these benefits can be realised.”
Nicola Bent Chief Executive Officer, Health Innovation Wessex

“There was incredible goodwill in the room and commitment to work together across our geography to bring the power of the whole of Wessex to bear on adopting and adapting the new genomics to benefit the healthcare of our population. This makes it a great Wessex story – a Wessex story of success and a Wessex story of future opportunities.”
Professor William Rosenberg Chair, Wessex Health Partners
Health innovation networks transform lives through innovation by supporting health and social care teams to find, test and implement new solutions at scale to the NHS’ greatest challenges. We are the health innovation adoption experts.
Health Innovation Wessex is a partnership organisation. We bring together the NHS, health and social care providers, universities, industry, community groups and voluntary organisations, helping to generate economic benefits and improve health outcomes.
We champion the value of convening and collaborating, evaluating impact and creating the conditions for innovation to flourish, and bringing fresh energy and inspired thinking to benefit the population of Wessex and beyond.
How can we help you?
If you’d like to get in touch with the Health Innovation Wessex team, please email us at enquiries@hiwessex.net or call the main office on 023 8202 0840. Follow us on LinkedIn
Sign up for our monthly Wessex Wire newsletter here to receive the latest news and regional updates.
