
Transforming lives through innovation




As the new Chair and CEO of Health Innovation KSS, we are proud to present our first annual review. The 2023-24 year has been transformative, marked by significant changes and remarkable achievements.
Our organisation’s new name better reflects our role in supporting the development and spread of innovation across the health and care ecosystem. We’re delighted that we secured a fiveyear re-licensing, ensuring the continuity of our vital programs. This will allow us to continue delivering high-quality adoption and spread initiatives, rapid uptake of approved products, and close collaboration with Integrated Care Systems (ICSs).
Despite facing unprecedented challenges - the cost-of-living crisis, NHS workforce issues, political uncertainties, and ongoing system restructures - we’ve had an outstanding year.
Collectively, the Health Innovation Network contributed over £475M in inward investment to the economy, a 10% increase from the previous year.
This highlights the critical role of technology and the life sciences in driving economic prosperity, with Health Innovation KSS playing a significant part through our support of high-growth innovators, such as Leo Cancer Care.
We have continued to build strong partnerships with local ICSs, leading to impactful initiatives. For example:
• In Surrey, we’ve tackled health inequalities by improving access to cholesterol screening for underserved groups.
• In Kent and Medway, we have evaluated the impact of mental health practitioners in primary care.
• Our collaboration with NHS Sussex produced a comprehensive women’s health assessment, informing their 10-Year Implementation Plan.
Through our connection with the NIHR Applied Research Collaboration, we’ve advanced translational research in dementia, social care, primary health, and children and young people’s mental health. We’re particularly proud of our work coordinating the Kent, Surrey and Sussex Migrant Mental Health Community of Experience, addressing critical research gaps.
Patient safety remains at the core of our mission. Nationally, the Patient Safety Collaborative has prevented over 44,969 emergency admissions from care homes and supported a 75% reduction in traumatising restraint use across England’s Mental Health Trusts. We’ve also made significant strides in improving maternity care and enhancing medicines safety.

Internally, we’ve undergone leadership changes to better align with our ICS partners and local systems. We’ve invested in Equality, Diversity, and Inclusion (EDI) training and a cultural transformation journey, recognising its crucial role in the success of innovation, and our business case, as well as the learnings we can apply to the health and care systems we support through perspectives on health inequalities.

Looking ahead, we’re focusing on five cross-cutting themes: inclusion and equity, workforce transformation, patient safety, co-design, and environmental sustainability. These themes will guide our efforts as we continue to drive innovation and improvement in health and care services.
As part of a collaborative network of 15 innovation hubs across England, we’re committed to sharing best practices and amplifying our impact on a national scale. We believe this collaborative approach is key to achieving transformative change in our health and care system.
None of our achievements would have been possible without the dedication and hard work of our employees, partners, and stakeholders. We extend our thanks to everyone who has contributed to our success - commissioners, delivery partners, professionals, patients, and communities.
As we look to the future, we’re excited about the opportunities that lie ahead. We remain committed to driving innovation, improving patient care, and contributing to economic growth in the health sector.
Our focus on addressing health inequalities and improving patient outcomes will continue to guide our work. We’ve recently launched our ambitious two-year business plan, which sets out our renewed vision, strategic priorities and areas of growth for our organisation.
The challenges we face in the health and care sector are significant, but so too are the opportunities for positive change.
With your continued support and collaboration, we’re confident that Health Innovation KSS will play a crucial role in driving a healthier and more equitable society.
Thank you for your trust and partnership. We look forward to another year of transforming lives through innovation.


Jane Ollis Chair
Professor Hatim Abdulhussein CEO
Health Innovation Kent Surrey Sussex (KSS) is one of the 15 health innovation networks across England, established by NHS England in 2013

We are the health innovation adoption experts.
We transform lives through innovation by supporting health and social care teams to find, test and implement new solutions to the NHS’ greatest challenges, driving economic growth.
We tackle national problems, with local understanding. And local problems, with national expertise.
This drives economic prosperity and growth in all parts of the country, and ensure that everyone benefits from innovation
Health Innovation KSS covers the whole of Kent and Medway, Surrey and Sussex. Our impact comes from our ability to bring people, resources and organisations together, delivering benefits that could not be achieved alone.

46 projects/programmes completed by Health Innovation KSS jobs created nationally Over 500
11,827
£251,000 Our Innovation for Health Inequalities Programme (InHIP) in Surrey and Sussex could result in of cost savings over 5 years £475,820,793 funding leveraged across the national Health Innovation Network
1,300 health and care professionals received our monthly KSS ICB/ PCN lipid prescribing dashboard and monthly lipid management data newsletter
Nationally, over
100,000 patients have benefitted from the technologies supported by the MedTech Funding Mandate in 2023/24, generating £8.5million in estimated savings
50 employees
Nationally the health innovation network has worked with to support safe care and prevent over 44,969 emergency admissions care homes received equality, diversion and inclusion training and 4 employees became EDI champions
393 innovators supported in Kent, Surrey and Sussex
3,000 downloads Over of our My Choice booklet for dementia
My Choice
Through our MatNeo programme, we have saved up to of cerebral palsy nationally and prevented up to 1,198 lives 463 cases

Health Innovation KSS has five underpinning themes that are seen throughout our work programmes and priorities. We are committed to developing and supporting best practice approaches in these areas.
We are committed to promoting health equity and creating a more inclusive health and care system, especially by ensuring socially excluded groups have a voice. We work to promote equity, amplify diverse voices, and tailor innovations to meet the needs of various populations affected by certain health issues. Collaboration with stakeholders who share this vision is vital for driving transformative and inclusive change.
The 2022 Women’s Health Strategy for England aims to improve women’s health over the next decade. In 2023, NHS Sussex partnered with Health Innovation KSS to conduct a baseline report and needs assessment around women’s health. The findings were used to inform the development of NHS Sussex’s Women’s Health 10-Year Implementation Plan.
A learning health system approach was used, focusing on local data, knowledge, evidence, and developing communities of practice. The voices and experiences of women from diverse communities and backgrounds were central to the report, including young carers, Arabic speaking women, women with disabilities or long-term health issues, women with ADHD or neurodiversity, women who have experienced
homelessness and trans, bisexual, non-binary and intersex (TBNI) communities.
Common barriers to health services for women included not feeling believed about health problems, lack of understanding around women’s health, lack of reliable information, misdiagnosis or underdiagnosis of issues like menopause, and difficulty accessing services with long mental health waiting times. Focus groups with underrepresented women and genderdiverse people highlighted these concerns.
Health Innovation KSS utilised their strong links to bring together National Institute for Health and Care Research (NIHR) Clinical Research Network (CRN), and Applied Research Collaboration (ARC) KSS, and Sussex-based academic institutions. Research partners collaborated to develop a KSS-wide women’s health research network, holding an event in November 2023 with over 100 delegates to discuss priorities.
We aim to use innovation to ease pressure faced by NHS and social care employees. We recognise there is growing demand for services due to ageing populations and more people living with chronic conditions. Transformative solutions and sustainable pathways can help to reduce the strain our workforce faces by creating more capacity for upskilling and releasing time to care.
Mental Health Practitioners (MHPs) were introduced in Kent and Medway primary care in April 2021, funded by the Additional Roles Reimbursement Scheme (ARRS) and ICB funding. MHPs are patient-facing mental health specialists aiming to improve access to mental health support, offering longer appointments, shared care plans, and appropriate signposting.
In late 2023, Health Innovation KSS commissioned Unity Insights to evaluate the impact and implementation of MHPs. The mixed-methods evaluation found that MHPs had a positive impact on patients, primary care workforce, and the wider system. They reduced GP burden, improved patient experience and outcomes, and were likely to
be resource efficient and generate a positive return on investment.
MHPs were generally satisfied with their roles, although some variation was observed across Primary Care Networks (PCNs) and experience levels. Kent and Medway NHS and Social Care Partnership Trust (KMPT) implemented a successful recruitment process and centralised management function, which helped minimise variation and implement best practices.
Recommendations for the future include continuing to recruit and retain MHPs, allocating dedicated resources for these activities, and engaging with PCNs that haven’t yet implemented MHPs. The evaluation also suggested providing more support, flexibility, and autonomy to MHPs to improve their experience. Further assessment is recommended to continue understanding the ongoing impact of this initiative.
The safety of patients and our communities is a priority that runs through all our work. Our Patient Safety Collaborative (PSC) works to support National Patient Safety Improvement Programme delivery and focuses on encouraging the spread and uptake of innovation.
Our PSC is making an impact by identifying and rolling out safer care initiatives within the NHS and industry, ensuring these are shared throughout the health and care system.
For more specific information about our work in patient safety, please see page 33.
Co-design focuses on involving patients and the public, especially marginalised or seldom-heard groups, in designing health and care interventions that impact their lives. This approach ensures interventions address pressing challenges and unmet needs by incorporating the perspectives and experiences of those directly affected.
Involving patients, carers, and communities is integral to all work at Health Innovation KSS, with ARC KSS Implementation Leads specialising in facilitating co-design processes. Codesign promotes patient-centred care, reduces health disparities, and fosters an inclusive system where individuals can shape services impacting their lives.
Connecting with young people digitally: Toolkit for innovators
Health Innovation KSS worked with YMCA Downslink Group and an NIHR ARC KSS PHD candidate to develop best practice guidelines for innovators working with children and young people. The checklist includes a selection of resources for innovators which are free to view and download. The expert guidance includes direction from industry partners but most importantly feedback from young people themselves who were instrumental in co-producing and designing the toolkit, providing blogs and practical advice to innovators.
Top tips for engagement and co-design: People living with dementia
This document provides best practice for involving people living with dementia in research projects. Involvement helps us to find answers and solutions that meet individuals needs and is likely to result in better quality and more relevant research and outputs.
The Health Innovation Network is a key enabler in achieving a net zero NHS. We provide the health and care system with innovation to support sustainability across the entire lifecycle, from the supply chain through to improved patient outcomes, through three strategic goals: becoming influencers in net zero, educating innovators and supporting our system partners.
Sustainable health and research events, organised by Health Innovation KSS in collaboration with Kent and Medway ICB, addressed the challenge of siloed knowledge and limited resources and funding in the sustainability space. To combat this, we have hosted a series of events focused on priority areas such as medicines, adaptation and behaviour change. These sessions resulted in improved knowledge, enhanced connections across the NHS, industry and academia, the sharing of best practices among staff and raising awareness of the climate crisis.

Funded by the Government’s Office for Life Sciences (OLS), we work to support health and care innovators to realise the potential of their innovations.
In 2023-24, we have made a significant contribution to economic growth through our targeted support of high growth innovators. Nationally, the Health Innovation Network collectively achieved a 10% increase in overall funding leveraged compared to the previous financial year.
This demonstrates the huge contribution that the technology and life and science industries can make to supporting economic prosperity. More than half of the national funding leveraged was obtained by 15 local health innovation networks, which shows the benefit of having 15 local organisations that are also connected nationally.
Our innovator offer and impact in 2023-24
We act as an innovation exchange to:
Identify need and communicate regional priorities
Signpost and support innovators
Validate in real-world settings
£475,820,793 funding leveraged 554 jobs created 554 jobs safeguarded
In 2023-24, Health Innovation KSS supported
393 to develop their ideas and solutions, ready for adoption and spread, and to understand and prove their value
companies
Adopt and spread innovations across the system
We adapt the support we provide to meet the needs and development stage of the innovation. For example, we help early-stage innovators refine value propositions, while latter-stage support may include business case development and real-world evaluations. The Real Birthing Company case study overleaf demonstrates our work with innovators ready for scale and adoption.
We work closely with funders, like the Small Business Research Initiative (SBRI) and Innovate UK, to provide themed calls that meet the most pressing needs of the NHS. In 2023-24, we supported nine innovation open calls, including those focusing on net zero and health inequalities and supported companies, trusts and universities across 25 bids.
Continued over >
We also partner closely with our ICSs and local providers to identify and understand regional needs and to find opportunities to address these challenges through innovations that are evidenced, accessible and sustainable.
Horizon scanning focuses on informing stakeholders about the innovations that are available with the potential to impact on specific challenges. This year, we’ve completed horizon scans in several areas including women’s health to support the Sussex Women’s Health Strategy, and endoscopy to support Kent and Medway Cancer Alliance with the development of Kent & Medway’s ‘Strategy for Endoscopy’.
More broadly, we have collaborated with other local health innovation networks and across the collective Network to broaden the spread and adoption of innovation. For example, our work supporting the Accelerating FemTech programme, led by Health Innovation Network in South London. This programme focused on supporting innovators to boost the development of technology solutions to address current challenges in women’s health.
Nuala Foley, Associate Director Commercial and Enterprise, said:

“I’m so proud of our work supporting innovators this year. Together, we’ve advanced great ideas for our health and care system. My team’s efforts have been outstanding, and we’re privileged to work with amazing companies and innovators from our region.
While economic growth matters, it’s the potential impact on people’s lives that drives us. We’re seeing more innovations that address both urgent healthcare needs and health inequalities, giving hope for inclusive innovation.”

Cross-cutting themes:
Quality Statement 22 (NICE, 2012) suggests antenatal care should be readily and easily accessible and the Core20PLUS5 approach (NHS England, 2021) aims to help reduce health inequalities within maternity settings.
The Real Birth Company aims to increase access to antenatal training through The Real Birth Workshop. The Real Birth Digital Workshop is a user friendly, animated, and easily accessible tool. It provides mothers-to-be with the essential support that they may not have otherwise received. To create the content, the project has involved service users, lived experience teams, as well as clinicians.
Health Innovation KSS has supported The Real Birth Company through evaluation design, market research within the KSS footprint and building intelligence to inform product design iterations, as well as support with their successful SBRI funding bid. The Real Birth Company won the award for Innovation in Helping Address Health Inequalities at the Innovate Awards 2023.
Health Innovation KSS commissioned evaluation partners, Unity Insights, to evaluate the Real Birth Workshop in East Kent Hospitals. The evaluation found that participants had high satisfaction levels and that 100% of staff suggested that patient care and outcomes had improved since using The Real Birth Workshop.
“This is such an awesome workshop about birth. I was not expecting it to be this helpful when I started, but I’m glad I decided to check it out. It has helped me greatly and I will definitely recommend it to other pregnant women. I feel so calm and confident as my labour approaches.”
“The Real Birth Company is immensely grateful to Health Innovation Kent Surrey Sussex for their support and collaboration over the past couple of years and especially their support for the real-world evaluation and SBRI Healthcare competitions around Maternity - with their support we found the processes easier to manage. Their commitment to innovation in healthcare has been instrumental in helping us advance our mission of providing equitable access to prenatal birth education and support.”
Zoe Wright, CEO and Founder, The Real Birth Company
Cross-cutting themes:
Cancer will impact one in two people [1] and one in four people will require radiotherapy for cancer in their lifetime [2]. Radiotherapy is a commonly used treatment to kill cancer cells and traditionally involves patients lying down to receive treatment. Traditional radiotherapy can 1) be costly, 2) take up a lot of space, 3) involve a lot of set-up time and 4) cause anxiety or discomfort for some patients [3].
Health Innovation KSS has been supporting an innovative Surreybased company that aims to change the way cancer therapy is delivered. Leo Cancer Care, based in Horley, makes upright radiotherapy products, including a proton beam therapy (PBT) device, with the potential to save the NHS millions of pounds and increase patient throughput. The company’s products use a unique upright positioning system alongside upright imaging modalities, which can be installed more quickly, at a lower cost, and take up a fraction of the space of traditional machines [4].

Health Innovation KSS’s long-term support for Leo Cancer Care has yielded significant results. Leveraging our organisation’s strength in industry networking, we facilitated crucial introductions between Leo Cancer Care and Macmillan Cancer Support, the UK’s leading cancer charity. Recently, Leo Cancer Care received a strategic impact investment from Macmillan Cancer Support, received as part of the Macmillan Innovation Impact Investment Portfolio.
We have supported Leo Cancer Care to commission evaluation and validation reports, leading to a cost-benefit analysis and budget impact model. We enabled Leo Cancer Care to showcase their product on The Health Innovation Network’s national stand at NHS ConfedExpo 2023 and 2024.
Our support also included detailed horizon scans, scoping discussions, market feedback from local Cancer Alliances, and strategic planning for NHS access. This multi-faceted approach demonstrates our ability to provide comprehensive support to leading innovators.
Stephen Towe, Leo Cancer Care said:
“Our partnership with Health Innovation KSS has provided tremendous support to build awareness of our solutions in the UK. With their support, we will aim to bring this new and innovative treatment option to patients in the NHS in the near future.”
Evaluation and validation reports found that Leo Cancer Care’s Marie™ system could lower the cost and waiting list backlog in the NHS and yield greater return on investment compared to existing NHS machinery for cancer treatment [4]. However, the potential impacts on the NHS are yet to be determined.
As well as transforming cancer care and providing potential cost savings to the NHS, Leo Cancer Care is also driving economic growth in our region.
• Since 2020, Leo Cancer Care has created 50+ UK jobs in our region and has generated ~£20M in total revenue.
• Leo Cancer Care has also secured £75,000,000 in private investment.

“We’re excited to support such an innovative company to achieve its ambitions. It’s a delight to work with innovators from our region and to watch their ideas flourish. Leo Cancer Care has the potential to make an enormous contribution to our health and care system, patients living with cancer, and our local economy.”
Nuala Foley, Associate Director, Commercial and Enterprise
References
[1] NHS Cancer Overview. Available at: https://www.nhs.uk/conditions/cancer/
[2] Analysis suggests one in two people will get cancer in their lifetime. (Source: Ahmad AS, OrmistonSmith N, Sasieni PD. Trends in the lifetime risk of developing cancer in Great Britain: comparison of risk for those born from 1930 to 1960. Br J Cancer 2015; 112: 943-7. doi: 10.1038/bjc.2014.606.) Further analysis suggests around half of people who get cancer should receive radiotherapy as part of their treatment according to standard clinical guidelines. (Source: Delaney G, Jacob S, Featherstone C et al. The role of radiotherapy in cancer treatment: estimating optimal utilization from a review of evidencebased clinical guidelines. Cancer 2005; 104: 1129-37. Doi: 10.1002/cncr.21324. Erratum in: Cancer
2006;107: 660. PMID: 16080176.) Taken together, this results in the estimate that around one in four people will require radiotherapy for cancer in their lifetime.
[3] Forbes E, Baker AL, Britton B et al. Non-pharmacological approaches to procedural anxiety reduction for patients undergoing radiotherapy for cancer: systematic review protocol. BMJ Open 2020; 10: e035155. doi: 10.1136/bmjopen-2019-035155. PMID: 33039983; PMCID: PMC7549444
[4] Health Innovation KSS and Unity Insights. Health Economic Modelling – Proton Therapy. Available at: Health Economic Modelling - Proton Therapy - Unity Insights
[5] S. Boisbouvier, A. Boucaud, R. Tanguy, V. Grégoire (2022) Upright patient positioning for pelvic radiotherapy treatments https://doi.org/10.1016/j.tipsro.2022.11.003

Innovation is needed across all areas of the health and care system. The key programmes we delivered in 2023-24 spanned multiple disease areas and focus areas. From patient safety, cardiovascular disease and polypharmacy to addressing health inequalities, all 45 programmes and projects in 2023-24 were delivered to the highest quality by our expert teams. Our programmes are commissioned by national and local partners, including National Health Service England, the Accelerated Access Collaborative, the Office for Life Sciences, our local ICBs/ICSs in KSS, universities and the life sciences industry, plus others. We deliver our programmes in partnership with a range of stakeholders including citizens, NHS and academic organisations, local authorities, the third sector and industry.
In 2023-24, key highlights that are included in our review this year are:

“What a remarkable year 2023-24 has been. I’m immensely proud of our team’s achievements. Working alongside our regional partners, we continue to deliver impactful projects that enhance the health and care of roughly 4.7 million people in our area.
We collaborate with local integrated care systems and national partners to drive innovation and improve population health across numerous diseases and focus areas.”
“This report offers a snapshot of some of our work, but it’s by no means an exhaustive account of all we’ve accomplished. Our dedication to supporting and scaling the best healthcare innovations remains steadfast, and we look forward to building on our partnerships and programmes of work in the coming year.”
Lisa James, COO, Health Innovation KSS
There is more information about all of our programmes included on our website.
Cross-cutting themes:
challenge
Cardiovascular disease (CVD) affects around seven million people in the UK, costing £7.8 billion annually. If not properly managed, CVD can lead to disability or death. Despite effective management options, low detection rates and limited awareness hinder optimal care. Two thirds of at-risk individuals are undertreated, with greater disparities in deprived areas. In our region, people from underserved communities can struggle to access screening and treatment, leading to urgent health inequalities.

NHS England’s Innovation for Healthcare Inequalities Programme (InHIP) aims to address local healthcare inequalities experienced by deprived and other under-served populations in line with NHS England’s Core20PLUS5 approach.
We supported our local integrated care systems (ICSs) to deliver projects that focussed on increasing cholesterol / familial hypercholesterolaemia screening, and access to, and adoption of, evidence-based innovations for CVD in underserved populations. For example, this included females aged 40-69, ethnic minority groups (including Traveller communities) and those living amongst the 20% most deprived areas in England.
The overall aim of the projects was to support early identification of CVD risk factors to reduce the risk of developing CVD and associated complications, as well as addressing local healthcare inequalities.
We worked with Unity Insights to undertake independent evaluations of each project to establish effectiveness of reaching target communities.
More details on the specific projects undertaken in each of our ICBs are included overleaf.
In Surrey and Sussex, independent evaluations found both projects were effective at reaching underserved populations by bringing screening and treatment closer to patients in the community.
In Surrey, the project was effective in increasing engagement with ethnic minorities, under 40s and Core20 groups. Meanwhile in Sussex, the project was effective at reaching the target Core20PLUS populations. In particular, females aged between 40-69 made up 39% of the total population sample.
In Sussex, Core20PLUS groups combined received a medical intervention at a greater rate than the overall population, demonstrating its effectiveness at treating people in Core20PLUS groups. In Surrey, the project supported 240 patients with health indicators of a CVD condition to receive health education, and a further 135 patients were sent on for further care, which may lead to better outcomes for these individuals. More work needs to be done to reach ethnic minority groups, Gypsy Roma Travellers, those with severe mental illness, and people living with HIV.
Taken together, cost savings of around £251,000 over 5 years could be achieved across Surrey and Sussex by improving access and early management.
Findings from Kent are not yet available as the evaluation is underway.
While these projects target small sample sizes, if scaled in future, they have the potential to address health inequalities in KSS, reducing mortality and morbidity associated with CVD and save money for the health and care system.
Additionally, health literacy will be improved amongst vulnerable communities and people’s trust will improve in the ability of healthcare providers to meaningfully develop relationships to support positive health outcomes.

Cross-cutting themes:
As more people live longer with multiple long-term health conditions, the number of medicines they take often increases. Managing multiple medicine regimes can create a significant burden for the patient and it may cause them harm. More broadly, problematic polypharmacy can be costly for the healthcare system, and wasted medicines have a negative impact on the environment.
In Kent Surrey and Sussex, we are working with ICSs and ICBs to deliver the three pillars of the national polypharmacy programme, including:
Pillar one: Securing attendance from stakeholders at national learning events focusing on using data to understand Primary Care Network (PCN) risks and prioritise patients for a Structured Medication Review.
About the Polypharmacy programme
The Health Innovation Network national polypharmacy programme is creating clinical, multi-stakeholder communities of practice across England, focusing on addressing problematic polypharmacy within local areas.
There are three pillars of activity:
Pillar one: Population Health Management
Pillar two: Education and Training
Pillar three: Public Behaviour Change.
Pillar two: Delivery of Polypharmacy Action Learning Sets (ALSs) and local communities of practice to upskill the primary care workforce to be more confident about stopping unnecessary medicines.
Pillar three: Sharing a suite of patient-facing resources to change public perceptions of a “pill for every ill” and encourage patients to open up about medicines.

Between 2022-24, we have:
• Held 10 Communities of Practice across KSS with a total of 460 participants attending.
• Sponsored five local stakeholders to become polypharmacy trainers by attending national evidence-based polypharmacy Action Learning Sets (ALS).
• The KSS polypharmacy trainers have delivered two local bespoke polypharmacy training sessions, showing how knowledge is being shared across our region.
• 309 attendees at NHSBSA Polypharmacy Prescribing Comparators Webinars in KSS between April 22 – March 24
• 64 ALSs delegates in KSS between April 2022–March 2024
- Including 14 attendees representing from Primary Care Networks serving the most deprived 20% of the national population
Longer-term this programme has the potential to:
• Reduce patient risk of harm from medicines.
• Reduce medicine waste and the associated carbon impact of wasted medicines.
• Empower patients to self-manage their own health and care where clinically appropriate by providing access to medicine information they can trust.
• Improve patient and healthcare professional (HCP) experience and build HCP confidence to provide a better quality of care.
• Reducing health inequalities by focusing on most deprived areas in England.
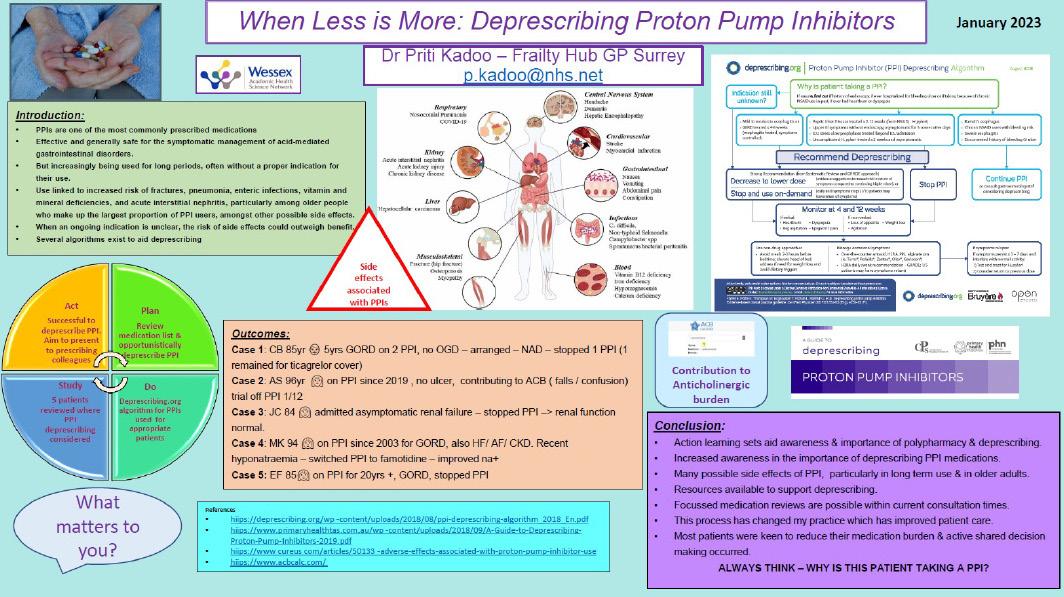
Quality improvement project poster summary completed by a delegate who attended the national evidence-based polypharmacy Action Learning Sets (ALS). Source: When Less is MoreDeprescribing Proton Pump Inhibitors by Dr Priti Kadoo – Frailty Hub GP Surrey.
Cross-cutting themes:
Cardiovascular disease (CVD) is the biggest cause of avoidable mortality in England. Intrinsically linked to health inequalities, for many people, lack of awareness, detection and treatment can result in longterm disability. The early detection and treatment of CVD can help patients live longer, healthier lives.
High cholesterol is a top contributor to risk of CVD death and increasing access to lipid lowering therapies to optimise lipid management is an effective way to reduce the risk of death or disability caused by cardiac events.

As part of our CVD Prevention portfolio, the Lipid and Familial Hypercholesterolaemia (FH) programme takes a Population Health Management (PHM) approach. This involves improving the cardiovascular health of target populations by using data to inform planning and delivery of lipid optimisation care. Our targeted approach allows us to achieve the best possible outcomes. This is supported by engagement, development of education/resources and local collaboration.
The KSS Lipids and FH programme is Primary Care led and Secondary Care supported to integrate services and the NICE-endorsed lipid pathway, aiming to:
• Improve lipid detection and optimisation, upskill Primary Care to detect, triage and manage appropriate patients and increase prescribing to impact on patient outcomes.
• Establish a Lipid and FH Steering Group to drive the programme to improve patient care and outcomes with lipid experts from secondary care supporting, guiding, and educating Primary Care.
• Support and upskill primary care clinicians further with dedicated clinical leadership support, Lipids Community of Practice, education series, access to lipid specialists, resources, lipids data reports and patient experience feedback.
In the first year of the Lipids and FH programme, all 109 PCNs in KSS had adopted the NICE-endorsed Lipid Management Pathway.
1,300 health and care professionals received our monthly KSS ICB/PCN lipid prescribing dashboard and monthly lipid management data newsletter, which featured data sourced from Open Prescribing and CVDPREVENT.
The CVDPREVENT Audit data analysis for England, which includes Kent and Medway, Surrey Heartlands and Sussex ICB, spanning June 2022 to December 2023, presents a detailed picture of the management of cardiovascular disease and related risk factors.
The data for people with known CVD treated to NICE-recommended lipid management thresholds, showed that all three KSS ICBs had a greater percentage increase from September 2023 to December 2023 than England.
Across KSS, we have achieved a steady and sustained increase in prescribing of all the new cholesterol-reducing drugs that are important additional tools for managing cardiovascular disease. We have also seen an increased clinical awareness of the NICE-endorsed lipids management pathway.
We have successfully continued to collaborate with, support and upskill clinicians. Our reach and engagement with stakeholders have increased every year:
• We maintain a CVD mailing list of 1359 people from across the South East.
• We are growing a CVD Central Community of Practice on FutureNHS - Updated with the latest guidance, resources and slides/recordings of events and webinars.
• CVD Central Inbox: kssahsn.cvdprevention@nhs.net
• CVD Central website

CVDP009CHOL (Secondary Prevention)
Percentage of patients aged 18 and over with GP recorded CVD

19
CVD Specialists recruited to the KSS Bank of Specialists to deliver education sessions
10
Lipid Specialists recruited to deliver education sessions & KSS Virtual Lipids MDT Clinics to PCNs

Cross-cutting themes:
The MedTech Funding Mandate (MTFM), launched in April 2021 by NHSE, aims to ensure patients and the NHS benefit from clinically effective and cost saving medical technologies faster and more equitably. The policy supports devices, diagnostics or digital products that are effective, cost-effective and affordable to the NHS. Selected technologies are National Institute for Health and Care Excellence (NICE) recommended and meet the criteria to save costs and resources and make a return on investment within three years.

Four technologies designed to address Benign Prostate Hypoplasia (BPH) as less invasive day case interventions, in contrast to traditional surgery involving overnight stays for patients
• UroLift (NICE guidance MTG58)
• GreenLight (NICE guidance MTG29)
• Rezum: (NICE guidance MTG49)
• PLASMA: (NICE guidance MTG53)
XprESS multi-sinus dilation system: a sterile, single-use device for treating chronic sinusitis. (NICE guidance MTG30)
Thopaz+: a portable digital chest drain system that provides regulated negative pressure close to the patient’s chest and continuously monitors and records air leak and fluid drainage. (NICE guidance MTG37)
Spectra Optia: an apheresis and cell collection platform for the treatment of sickle cell disease. (NICE guidance MTG28)
The introduction of AposHealth for knee osteoarthritis in 2024-25 - Health Innovation KSS are the Health Innovation Network national product leads for this. (news article)
• Patients and the NHS in KSS don’t always have quick and equitable access to clinically effective and cost saving medical technologies.
• NHS providers don’t always know which technologies to adopt, and often are unsure about the potential savings when investing in new technologies.
• We are commissioned by NHSE to support the policy, though identifying local need, brokering conversations between suppliers and commissioners and removing obstacles to adoption, whilst feeding back any clinical or logistical challenges that arise in this process to suppliers and NHSE.
• Most trusts in KSS continue to have patients benefitting from graduated technologies including placental growth factor basedtesting (PlGF), gammaCore, SecurAcath, and Heartflow.
• We have seen a significant increase interest in the innovations to treat Benign Prostate Hyperplasia with four new product adoptions across Kent Surrey and Sussex.
• Nationally, over 100,000 patients have benefitted from the technologies supported by the MedTech Funding Mandate in 2023/24, generating £8.5 million in estimated savings.

AposHealth’s innovator journey to date
Apos received CE regulatory approval as a Class 1 medical device
Submission of Apos as an innovation to the NHS Innovation Service, NICE and AHSN Network
April: NICE publishes MTG76 recommending Apos as a cost saving option for patients that choose not to undergo joint replacement surgery
First NHS Services established with Mid Essex, Bedfordshire and Greenwich CCGs. Patients that are eligable for surgery but choose not to have surgery

Jan: NICE publishes MIB284 naming Apos as potential alternative joint replacement surgery
May: Publication of 2yr NHS outcomes
May: Apos selected as the first new technology supported under the Med Tech Funding Mandate Policy for 2024/25
July: Publication of 3yr and 5yr NHS outcomes
AposHealth is an innovative treatment that helps people with knee, lower back and hip pain live well by improving their gait.

“We
are delighted to have supported Apos Health from early on in their innovator journey and are looking forward to continuing this support as they become part of the MTFM national programme.”
Julian O’Kelly, Innovation Manager, Health Innovation KSS
As the national product lead for AposHealth, Health Innovation KSS has raised awareness of the product and its national MTFM backing through various 2023-24 activities: presenting at NHSE webinars, developing toolkits, engaging stakeholders including voluntary sector and clinical leads, and securing Apos’ inclusion on the NHSE/Versus knee osteoarthritis patient decision tool. Our preparatory work with key stakeholders for AposHealth, including a thorough sustainability review, means we are well placed to drive uptake of this product in the coming year.


As a Patient Safety Collaborative (PSC), we play an important role in delivering the National Patient Safety Improvement Programme (NatPatSIP). The aim of the NatPatSIP is to support systems to test and spread effective safety interventions and strategies, learn from excellence and continuously improve. Our work focuses on five key areas:
Preventing and managing deterioration across systems
Patient Safety Incident Response Framework (PSIRF) implementation Managing maternal and neonatal deterioration and pre-term optimisation
Medicines safety Mental health
Overleaf is a case study of our work in Medicines Safety, which details the type of interventions we deliver and the associated impact through the PSC in KSS.

Cross-cutting themes:
Opioids are effective at relieving acute pain and for managing pain at the end of life. However, there is little evidence that this class of medicines is helpful for managing longer-term pain (chronic pain). Despite this, until recently, clinicians had been widely prescribing opioids for chronic pain treatment. Opioids have a serious risk of addiction, especially with long-term use.
NHSE has been supporting local health and care providers to reduce inappropriate prescribing of high-strength painkillers, like opioids, where they may no longer be the most clinically appropriate treatment for patients – and in some cases can become harmful without intervention.
The Medicines Safety programme aims to reduce avoidable harm from medicines, especially from opioids, and improve chronic pain care. Our team have worked closely with ICSs and stakeholders to deliver meaningful change.
We have developed tailored support for each Integrated Care System in our region to help them to address their specific challenges in opioid overprescribing and managing chronic pain.
In 2023-24, Sussex Health and Care partnership secured new funding to expand a successful opioid deprescribing service from East to West Sussex. The service focuses on supporting prescribers to safely taper opioid use in collaboration with patients and their carers. Health Innovation KSS facilitated this expansion by connecting acute pain teams, secondary care pain teams, and social prescribers, enabling a more integrated approach to patient care.
The East Sussex service has demonstrated positive impacts on patients’ quality of life, including improved social interactions, increased ability to complete tasks, improved sleep, etc. By extending this service to West Sussex, the partnership aims to improve chronic pain management for a wider population and potentially address health inequalities by offering alternative approaches to long-term pain management across the region.
Recovery College is a training resource for anyone interested in managing their mental health recovery in Surrey and north east Hampshire, developed by Surrey and Borders Partnership NHS Foundation Trust. Courses cover a wide range of topics including understanding conditions, skills and wellbeing and creative recovery.
In Surrey Heartlands, Health Innovation KSS continued our work with Recovery College and pain specialist group to develop a chronic pain course on pacing and movement for patients, carers, and families. The course aims to promote supported self-management for patients, and to remove overreliance on traditional medical pathways. The course is available in an online and in person format. Since its launch, the course has been well received by attendees and there is a waiting list for virtual courses.
National impact
Across England, through this programme, we have...
Kent and Medway is at the start of its journey to reduce opioid prescribing. Our work in 2023-24 focused on delivering system mapping workshops to understand the pain services operating at a local level. These workshops convened a wide range of stakeholders include primary, secondary, and out of hours care, public health teams, the voluntary, community and social enterprise sector (VCSE), as well as those working in the health and justice system.
Workshops focused on gathering intelligence, understanding key issues, and gaining momentum. A cohesive action plan on how to move forward was developed as a result of the insights gathered at the workshops. This action plan will help to ‘connect the dots’ between different services and enable a deeper understanding of the complexities of the service offering already in place.
Kate Toms, Programme Manager for Medicines Safety Programme at Health Innovation KSS said:

518 saved lives
4,676 prevented moderate harms
9,552 halved the risk of death for pain sufferers
“2023-24 has been another impactful year for the medicines safety programme across our region. Our work has helped to remove disconnect between stakeholders and enabled prescribers to work with their patients to explore alternative ways of managing chronic pain, outside of traditional medical prescribing. It’s really encouraging to see our region’s strong appetite to work more closely together to find innovative ways to address these challenges. Our work in 2024-25 will focus on supporting systems to adopt these programmes sustainably in the longerterm as we enter the last year of our programme”.

Health Innovation KSS has a close working relationship with the National Institute for Health and Care Research (NIHR) Applied Research Collaboration Kent, Surrey and Sussex (ARC KSS).
ARC KSS is one of 15 ARCs across England, part of a £135 million investment by the NIHR to improve the health and care of patients and the public. ARC KSS brings together NHS trusts, local authorities, universities, communities and other partners to develop and implement innovative translational research to improve health and social care for patients and families in the south east.
Health Innovation KSS’s unique Implementation Leads are embedded within the organisation and focus on translating ARC KSS research into practice. Our four research themes in 2023-24 included: dementia, social care, primary and community health, and children and young people’s mental health. All of our work focuses on addressing health inequalities, which cuts across life stages, places and conditions.
In 2023-24, we implemented and disseminated over 30 impactful projects across these themes. Examples include evaluating and upskilling services on how best to discharge patients using the Discharge to Assess pathway (funded as part of the NHS Insights Prioritisation Programme (NIPP)), measuring the impact of a whole school and college approach to mental health (a project that has influenced national policy), and evaluating and implementing the mental health practitioner role in Kent and Medway. Overleaf are two case studies that showcase how we translate research into action, and co-design solutions to meet the needs of people living in our communities.

Cross-cutting themes:
Migrants may face mental health challenges due to their experiences and difficulties accessing appropriate support. We wanted to help health and care staff to better understand the mental health concerns of migrants, especially those from at-risk groups, including unaccompanied asylum-seeking children.
Health Innovation KSS has been co-ordinating a Kent, Surrey and Sussex Migrant Mental Health Community of Experience (CoE), which has involved sharing research and identifying research gaps, hearing from lived experience experts, and mapping data and service/interventions. A key priority identified by practitioners and clinicians in this CoE was the need for intercultural awareness training.
We worked in partnership with Nafsiyat Intercultural Therapy Centre to deliver therapeutic intercultural training (funded by Health Education England) and reflective sessions, and to develop an intercultural training toolkit for the wider workforce (currently being developed).
The training model was evaluated by ARC KSS.
• The training included six online and face-to-face sessions with reflective practices between December 23 and March 24.
• 109 stakeholders including those providing services for care leavers, police, housing providers, schools and mental health trusts attended the training.
• The ARC KSS evaluation showed high ratings of acceptability, appropriateness and feasibility and demonstrated changing perspectives, development of knowledge and increased understanding.
• This training supports clinicians and practitioners to understand how culture impacts mental health, and as a result, professionals will be able to better support patients to overcome stigma and seek the services that they need. More information can be found here.
• We are exploring opportunities to scale the programme across the South East.
Cross-cutting themes:
People living with dementia (PLWD) need access to trusted information immediately following diagnosis and throughout their journey to enable them to adapt and live well with dementia. However, service providers and PLWD told us they didn’t have access to this vital information provided in one place.
My choice is an evidence-based information resource for PLWD. It was developed by Health Innovation KSS and ARC KSS through a rigorous process involving a literature review, content simplification and co-design with PLWD, dementia support workers and caregivers. As part of their feedback, PLWD highlighted important areas to include like hearing and /vision and accessing additional care, as well as advising us to make sure content was simple to ensure wide accessibility.
The resource covers a comprehensive range of topics to support living well with dementia, such as nutrition, mental health, cognitive activities, supporting technology, and planning for the future.
• Both the workforce (72-100%) and people living with dementia and their carers (100%) found the ‘my choice booklet’ relevant, easy to understand and helpful. Most reviewers (>72%) learnt something new and intended to adopt some of its evidence-based recommendations.
• There have been over 3,000 downloads since launch.
• My choice is the first tool of its kind designed to help people to live well with dementia. It’s in the early stages of rollout so further evaluation will be needed to assess its wider impact, including on helping people towards planning for the future.


We recognise our workforce is our greatest asset. Our team is made up of nearly 50 clinical and non-clinical experts from across multiple sectors. We have extensive knowledge and experience in Health and Social Care, Academia, Life Science and Research.
In 2023-24, we have welcomed several new team members, and said goodbye to some of our longest-serving colleagues. Now our new leadership team is in place, we are excited about what lies ahead, and are looking forward to building on the important groundwork completed by our departing colleagues.
During the past year, we have continued to invest in training, new systems, tools and processes. This work will continue in to 2024-26.
We are led by a Board made up of a Chair, non-executive, and executive directors. Our CEO is supported by our executive management group (EMG), who continue to oversee delivery activity, reporting to the Board. Recently, we have reconfigured our EMG structure so that the roles align more closely with our partners in the health and care system. Day to day delivery of our portfolios and programmes is led by our Senior Leadership Team (SLT). We also have in house enabling functions which include finance, HR and communications.
As an employer, we recognise EDI as crucial for helping employees feel valued and able to be themselves at work. Given EDI’s central priority, we started enhancing employee knowledge in 2023, investing in EDI training as part of a broader cultural transformation programme. This includes upskilling teams on understanding and responding to inequalities. We are enthusiastic about embedding EDI principles in all our delivery work in the coming year.


Our achievements this year mean we are well positioned for an exciting 2024-25.
With our new licence agreement in place, we can focus on continuing to deliver high quality national and local programmes. Our new business plan sets out our organisation’s strategic priorities for 2024-26.
We are excited to work even more closely with our local Integrated Care Systems (ICSs) and wider partners and help them to deliver on their regional priorities. We are also exploring new strategic partnerships that sit outside nationally commissioned services. These are projects that benefit our local systems and communities and are in areas of our growing expertise, for example, digital, data and AI and women’s health.
50%
These are our core services available to all stakeholders at no cost as part of nationally commissioned services. For example, our Patient Safety Collaborative and MedTech Funding Mandate.
50%
This support focuses on the specific services available to ICSs and wider parters at no extra cost, where requirement aligns with local priority or unmet need, dependent on resource availability. For example, Children and Young People’s Mental Health.
This work focuses on strategic partnerships with national and local stakeholders for ‘paid for’ services that sit outside of nationally commissioned services. These projects and partnerships focus on our cross-cutting themes and priorities.
Our
model: This is our structured approach to enabling the widespread adoption of
Our focus areas have been developed based upon national policy and regional alignment of needs, matched to our internal strengths and experience.
We deliver these portfolios across primary, secondary, tertiary and community care settings, with a view that innovations will eventually support people to access care closer to home.

Our overall portfolio includes our full range of national programmes (OLS, Patient Safety, AAC) but the areas below are where we see our work growing due to our expertise and strong track record.
These are new focus areas where our partners have expressed an increased interest. We will be establishing these programmes of work throughout our two-year business plan.
Secure Data Environments (SDEs) are secure data storage and access platforms, enabling approved researchers to analyse NHS health and social care data regionally. Kent, Medway and Sussex (KMS) have received NHS England funding to implement an SDE, part of a national interoperable network.
SDEs have numerous benefits for all stakeholders. For instance, we will likely see an increase in clinical trials via high-quality data and a clear accredited access process. SDEs should enable a better understanding of health and care inequalities, and growth in research participation from hard-to-reach groups. Other benefits may include faster access to new, more personalised treatments, and improved health, access, and experience outcomes.
Health Innovation KSS has been involved in the KMS SDE from its inception. Our support will continue in the coming financial year and will include leading the co-design of research environments, including for user research and medicines information, supporting with reporting and governance, setting up a citizens panel, and ongoing clinical and SME support as needed. We’re delighted to be involved in such an important project for our region

Health Innovation KSS has been selected by NHS England as a key delivery partner for implementing Martha’s Rule. ‘Martha’s Rule’ gives patients and their families round-the-clock access to a rapid review from an independent critical care team if they are worried about their own or a loved one’s condition. Work to support the delivery of Martha’s Rule builds on existing managing deterioration activity being delivered in our region by the KSS Patient Safety Collaborative as part of the national NHS Patient Safety Strategy
Health Innovation KSS is helping to drive Sussex Integrated Care System’s (Sussex ICS) ambitious agenda to address health inequalities through the lens of equity. Our collaborative efforts with Sussex ICS involve co-delivering the Sussex Population Health Academy, which aims to develop workforce skills and capacity in tackling health inequalities. One element of this is the Health Equity Fellowship, a capability building programme that is open to all employees across the ICS to apply to. The second element is our system-wide training, consisting of a series of webinars to provide foundational training on fundamental principles of population health, which are open for anyone across the ICS and beyond to attend.
enquiries@healthinnovation-kss.com
www.healthinnovation-kss.com
www.linkedin.com/company/health-innovation-kss
www.youtube.com/@HealthInnov_KSS