2022 RUSH Department of Orthopedic Surgery


Donor Impact Report
Bone and Joint Care Celebrating 50 Years






Thanks to you, the bone and joint program at RUSH has much to celebrate in 2022.
This year marks the 50th anniversary of RUSH University and the formation of the Department of Orthopedic Surgery, which was led by the late Jorge Galante, MD, MDSc, when he was named as the first chairperson in 1972. The academic hub for all we do, our department has been a leader in revolutionizing orthopedic medicine through research and training generations of surgeons and scientists, many of whom still practice at RUSH and around the world.
In 2022 our team also celebrated another milestone: recognition as a top-10 orthopedics program in the nation by U.S. News & World Report for a 10th consecutive year, with RUSH earning the No. 5 spot. While many organizations evaluate specialties, these rankings are among the most well-recognized and respected in medicine. Two of the biggest factors driving this recognition are the superior outcomes our patients experience and RUSH’s reputation among thousands of orthopedic specialists surveyed.
Of course, we also celebrate you — our community of steadfast donors, supporters and friends. Thank you. Every day, your investment in RUSH’s bone and joint program empowers all we do to help people maintain or regain mobility and enjoy the activities they love without pain. The stories and research highlighted in this report are a snapshot of the work and achievements you have supported over the past year.
The William A. Hark – Susanne G. Swift Professor of Orthopedic Surgery Chairperson, Department of Orthopedic Surgery

Hip surgery wasn’t a present Mike Newman was expecting for his 40th birthday in 2014. But when the former professional soccer player’s persistent lower body pain became unbearable, he turned to sports medicine orthopedic surgeon Shane J. Nho, MD, MS, at RUSH.
“I wasn’t able to function on a day-to-day basis,” Newman recalled. Bewildered by the pain, he had a breakthrough when another former soccer player suggested it may be his hips. Newman soon found Nho and his team.
Imaging tests didn’t reveal arthritis in Newman’s left hip, but the ring of cartilage around the hip’s socket joint known as the labrum was torn. He also had femoroacetabular impingement syndrome, or FAIS, a hip abnormality that disproportionately affects younger, athletic people like Newman.
Nho’s team in the Section of Young Adult Hip Surgery at RUSH is an international trailblazer in studying and treating FAIS, a condition that didn’t even have a name 20 years ago. FAIS is diagnosed when a patient has a bony overgrowth on the ball or socket parts of the hip joint — or both. Evidence suggests that people who are physically active during adolescence may be more susceptible to painful FAIS, which is strongly associated with hip osteoarthritis later in life if left untreated.
Newman underwent a procedure — an arthroscopic surgical technique Nho and his collaborators helped pioneer at RUSH — to correct the FAIS and repair the labrum. A successful surgery and rehabilitation process for the left hip gave Newman confidence to address the right hip three years later, and he’s grateful he did.
“Now I’m able to play with my kids again,” said Newman, now 48, who has resumed his favorite athletic activities without pain.
Newman and his wife, Jaquelyn, established the Jaquelyn M. and Michael B. Newman Fund for Orthopedic Research in 2018 to fuel more innovation that will help others with similar orthopedic problems.
“Any time we’re investing in research, it requires tremendous resources — personnel, testing equipment, data analysis and so forth,” Nho said. “Thanks to Mike and Jaquelyn’s support, we have the largest data repository on patients with FAIS that we know of in the field.”
More than 3,500 consenting patients in the registry are followed over time, including Newman himself, with findings from the data that move the field forward. Nho’s team published nearly 50 peer-reviewed articles on this work in the past year alone.
“My experience as a patient opened my eyes,” Newman said. “Learning how emerging this field is and knowing what the surgery at RUSH has done for me is why we wanted to get involved and support this work. Dr. Nho changed my life. There are no two ways about it.”
“ I can do the things I want without restrictions. I’m the result of Dr. Nho’s work.
Scan the QR code or visit rush.edu/mikenewmanstory to read Mike’s full story and learn more about RUSH’s leading hip preservation research.


People don’t seek orthopedic specialists when everything is A-OK. They come when they’re in pain — which they’ve often experienced for a long time. Innovations in bone and joint care continue to help more people regain a full, active life without pain. These innovations are fueled by research, including numerous efforts underway at RUSH to improve scientific knowledge about musculoskeletal pain and devise new ways to eliminate it.
For most people, pain goes away after recovery from surgery. But for some — varying estimates suggest 20% to even up to 50% of people — pain after surgery can linger for years or even a lifetime. RUSH bone and joint researchers led by Joshua J. Jacobs, MD, with collaborators in psychiatry and anesthesiology, are helping to lead a massive national research effort to find out why.
The Acute to Chronic Pain Signatures, or A2CPS, consortium brings together scientists from around the country to identify patterns that may explain why certain people experience chronic pain after surgery — and why some people are especially resilient to it. Of the 3,600 people enrolled in the first-of-its-kind study, half are consenting participants receiving a total knee replacement at RUSH. Brain imaging scans, blood tests, psychosocial evaluations and other tests — before surgery and six months after surgery — will assess hundreds of factors that may impact the development of chronic pain. Funded by the National Institutes of Health, the study’s data and resulting discoveries will be made available to scientists everywhere.
In recent years, RUSH physician-researchers, including Denis Nam, MD, MSc; Tad Gerlinger, MD; and Craig Della Valle, MD, have pioneered studies to bring scientific evidence to the fight against the nation’s opioid crisis. Their research has brought to light the surprising number of patients with hip and knee pain prescribed opioids for the non-operative treatment of arthritis, as well as safer prescribing patterns after surgery that prevent unused pills from getting into the wrong hands. This past year, Della Valle and his collaborators also found that patients taking even small doses of opioids
prior to knee replacement surgery had an increased risk of complications, including hospital readmissions and infections requiring revision surgery. Their findings from this analysis of more than 20,000 knee replacement patients were published in The Journal of Arthroplasty.
For decades, physicians and scientists had a difficult time identifying the precise origins of most patients’ low back pain, the most common disabling condition worldwide. New imaging tools like advanced MRI are changing that. A growing body of research pioneered by scientists including RUSH’s Dino Samartzis, DSc, points to subtle changes to the vertebral endplates — a layer of bone and cartilage between the spine’s vertebrae and its cushionlike discs — as a driver of low back pain. Now, through the RUSH Multi-Omics Spine Study, Samartzis is leading a study funded by the National Institutes of Health to find out why these changes occur and expand upon the new field of precision-based spine care.
In an initial group of 100 patients undergoing spinal surgery, the researchers are studying imaging, genetics, the gut microbiome, metabolism and inflammatory profiles as well as samples of spine tissue from consenting participants. Through artificial intelligence and other sophisticated techniques analyzing the vast amount of data, their hope is to identify biomarkers that are associated with changes in the spine. Such biomarkers will aid in predicting outcomes, refining patient management and identifying potential targets for future therapies. The multidisciplinary study brings together research labs from across and beyond RUSH, with the hope that results will set the stage for a much larger study with thousands of participants. Their initiative is the first in the world to examine spine health and disease from a multi-omics, big-data perspective with long-term outcomes.

As medical care grows in precision and personalization, Marta Batus, MD; Alan Blank, MD, MS; Steven Gitelis, MD, and their collaborators are analyzing sarcomas down to the molecule to develop the best treatment approaches for their patients. The team of RUSH collaborators recently published the results of a study in which they performed comprehensive molecular profiling with next-generation sequencing on 136 bone and soft tissue sarcomas. This technique helps clinicians discover genetic mutations in the tumor that may provide insight into therapeutics most likely to be effective.
The information gained from this profiling — one of the largest studies of its kind in sarcoma — revealed about 47% of patients had a mutation considered “actionable,”
meaning it could be directly targeted by an approved or investigational therapy. Treatment plans for a subset of patients were changed based on the tumor profiling, and three of those patients with advanced cancers experienced a measurable clinical benefit (defined as the absence of new metastatic lesions and no significant growth in the size of the primary tumor for six months after the change). While further research is needed for physician-scientists to fully refine precision oncology care capabilities for sarcomas, the results of this study show that evaluating each patient’s tumor at the molecular level can support better treatment plans — especially for those with late-stage or recurrent sarcomas.
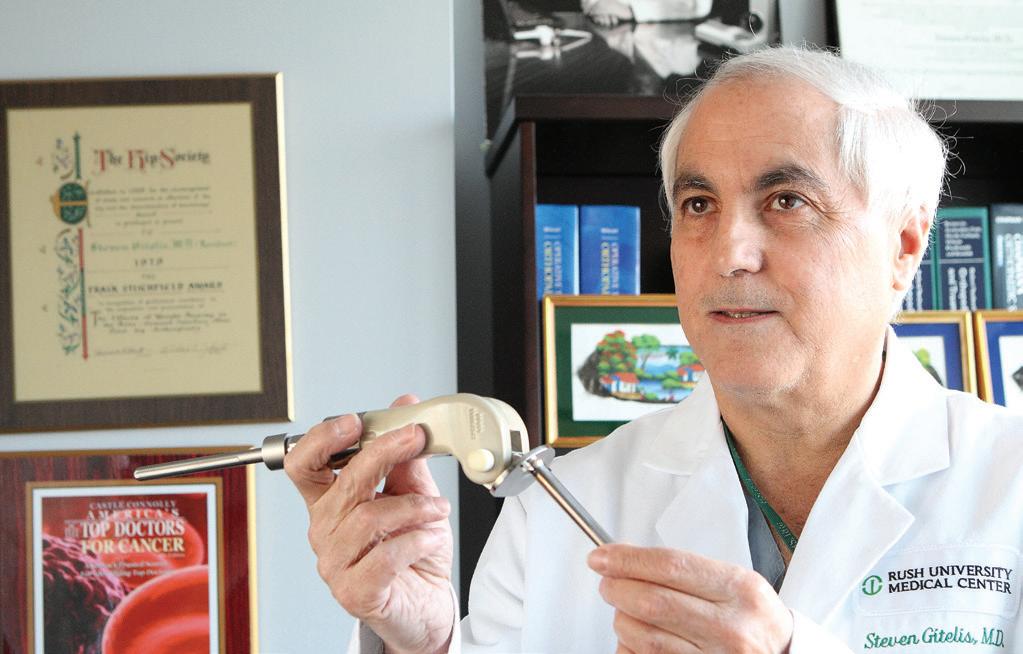
Celebrating 50 Years of Steven Gitelis’ Excellence in Orthopedic Cancer Care
In 2022, RUSH celebrated the 50-year career milestone of internationally recognized orthopedic surgeon Steven Gitelis, MD . When Gitelis began his career in medicine, the only treatment for osteosarcoma — the most common form of bone cancer — was amputation of the affected limb. The prognosis for today’s patients has improved dramatically, thanks in large part to Gitelis’ impressive contributions to orthopedic oncology.
Gitelis pioneered surgical resection and reconstruction methods known as limb-salvage techniques to improve the treatment of sarcomas, making amputation a rare, last resort. He helped popularize arthroplasties (surgeries to restore the function of a joint) and allografts (bone transplant operations) and even launched the Chicago area’s first bone bank to store donor tissue. Beginning in the 1980s, he became one of only a handful of orthopedic surgeons in the nation performing bone transplants.
Gitelis has directed the Section of Orthopedic Oncology at RUSH University Medical Center since 1984, turning RUSH into an international destination for sarcoma care, research and training. He has published more than 200 scientific articles, mentored hundreds of resident physicians and fellows, and lectured at institutions worldwide.
A groundbreaking ultrasound imaging device created by RUSH experts is employing the power of artificial intelligence to improve the accuracy of minimally invasive lumbar spine surgeries. SonoVision was developed by Kern Singh, MD , and his colleagues and informed by years of research and clinical expertise. The device is placed on top of the psoas muscle during lateral interbody fusion procedures, which treat degenerative disc disease through coin-sized incisions, circumventing damage to back muscles. The device uses machine-learning algorithms to provide real-time soft tissue imaging to help surgeons avoid damaging nerves and blood vessels without having to make large incisions. These visualizations help surgeons accurately determine the safest and most effective surgical route to the disc space.
In ongoing clinical trials at RUSH and medical centers around the country, the device has so far proved highly successful in identifying these important anatomical structures and preventing serious complications. As a result, the use of this device is also linked to shorter operative times. Through machine learning, SonoVision’s accuracy will continue to improve as it is utilized with more patients.
The sound of Michael Jackson’s “Thriller” fading in and out of RUSH’s Motion Analysis Lab may be mistaken for a dance party, but it is actually a unique and fascinating new research project. Researchers are investigating the power of music to help people with orthopedic and neurological conditions understand how movement impacts their physical function. The use of audio to convey information is known as sonification, and a multidisciplinary team of RUSH researchers led by Markus A. Wimmer, PhD, have been investigating how it may improve health outcomes, like pain and quality of life, for patients with conditions like osteoarthritis, lower limb fractures, knee instability and Parkinson’s disease.
The researchers invented a system that provides continuous, real-time auditory feedback to patients about their walking patterns by using the information transmitted by wireless pressure-sensing shoe inserts, also developed with the expertise of RUSH researchers. When a person’s walking patterns are ideal, music plays clearly at full volume, but when a person puts too much pressure on certain areas of the foot, which contributes to joint pain, the music becomes muffled. Physicians also use this data to monitor patients’ engagement with treatment plans. The team is partnering with Loyola University Chicago’s Department of Computer Science to develop a mobile application for this system so patients can use this impactful training technology at home for daily tasks and on the go.
The Cartilage Restoration Center at RUSH — established in 1997 as one of the first of its kind in the nation — specializes in repairing or replacing patients’ injured cartilage before more advanced deterioration occurs. Led by Brian J. Cole, MD, MBA, and Adam B. Yanke, MD, PhD, the center is a trailblazer in the research and development of treatments that aim to slow the progression of osteoarthritis and delay or prevent the need for joint replacement. From biomechanics and biochemistry to computer modeling and clinical outcomes studies, the team is a powerhouse for clinical trials and research — publishing dozens of studies in the past year to propel the field forward and improve patient care.
Among their ongoing studies, Cole’s team is detailing the results of RUSH’s meniscal allograft transplantation, or MAT, surgeries, used to replace damaged or missing knee cartilage. The research focuses on revision MAT, long-term outcomes following MAT after 10 years and adolescent outcomes following MAT after five years. This research aims to spur improvements to these treatments to shorten healing times and improve mobility. Yanke’s team is building on findings that the use of biologic treatments — cells, blood components, cartilage and other natural substances that replace or harness the body’s own power to slow or stop inflammation — administered immediately after a joint injury could mitigate the development of arthritis. These studies may inform the treatment of knee injuries in young, active people moving forward.

Top-ranked orthopedics program in Illinois by U.S. News & World Report

54 attending physicians with faculty appointments at RUSH, including 12 recognized as “Top Doctors” by Chicago magazine
#5
RUSH orthopedic program’s national ranking by U.S. News & World Report , our 10th-straight year in the top 10 29
research faculty, more than any other Chicago-area university
At RUSH, we understand the burdens of pain and firmly believe no one should have to live with them. The progress we are making in our labs, informed by the care we provide in our clinics, is made possible by your investment. You are helping us work toward a future free from pain. Thank you for your ongoing belief in our work.
$125.1 million in research awards at RUSH University from the National Institutes of Health and other external funders, benefiting dozens of bone and joint investigators
To support the Department of Orthopedic Surgery at RUSH, visit rushgiving.com/orthodept or contact: Derek Lambert Executive Director of Development (312) 942-6289 derek_lambert@rush.edu