Publisher:
Graphic & Art Design: Valor Design, Inc.
Website & Logo Design:
























Publisher:
Graphic & Art Design: Valor Design, Inc.
Website & Logo Design:
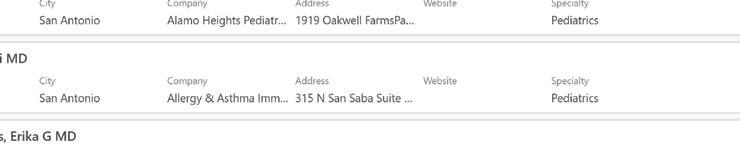
TOTAL TIME: Prep: 15 min. Bake: 15 min.
YIELD: 12 servings.
INGREDIENTS
For The Pizzas:
• 6 whole deli rolls or French bread, sliced
• Jar of marinara or pizza sauce
• 2 lb. shredded mozzarella cheese
• Grated parmesan cheese, to taste
Topping Suggestions:
This is where making pizza is fun for the kids, let them add their own toppings to individualize their own pizza
• Pepperoni slices
• Canadian bacon slices
• Pineapple chunks, fresh or canned
• Roma tomatoes, sliced
• Sliced black olives
• Goat cheese
• Sliced bell peppers
• Pepperoncini
• Jalapeño slices
• Sliced red onion
• Ground Sausage
DIRECTIONS
1) Preheat the oven to 375°.
2) For the pizza: Slice rolls in half and lay them, cut side up, on a large baking sheet.
3) Top each half with a generous portion marinara or pizza sauce. Next, top with a generous amount of grated mozzarella and parmesan cheese, if you'd like.
4) choice of optional toppings.
5) Once all assembled, put the pan in the oven on the lowest rack for 8 to 10 minutes.
6) Remove and serve immediately! You can cut the pizzas in half right across the middle so there are mini French bread pizzas for everyone.









Your child probably spends a lot of time with their doctors and therapists.
And we spend a lot of time on their medical care too. We manage those appointments. We talk to health insurance companies about getting things covered. And we work hard in general to make sure our children’s medical teams work well for them.
As your child becomes an adult, their medical care will also change. Doctors who work with children will be replaced by doctors who work with adults. Waivers and health insurance programs designed for children will be replaced by waivers and insurance programs designed for adults. And, legally, your child will be responsible for managing all of their medical care when they turn 18 unless you put protections in place to share decisions or make decisions for them.
Over time, we can help our children learn to take charge of some or all of their medical care themselves, teaching them to talk to the doctor about their symptoms, showing them how to schedule visits, and making sure the doctor talks to our child during the appointment. It’s a lot to adjust to. Here are some facts, ideas, and tips we’ve gathered from other parents to help you and your child go through this change.
One of the biggest parts of a medical transition is the shift in who the doctor expects to talk to. When you have a baby or younger child, doctors expect you, as a parent, to tell them what that child needs. But doctors who work with adults are used to talking to their patients directly.
We realize that not all children will be able to take over management of their own health care. You can read over the list of specific skills your child will need, like managing insurance and payment, describing symptoms, and knowing what to do in an emergency.
And, if you start early, you can prepare your child step-by-step to be ready for as much of their own care as they’re able to manage. Here are some ideas to help your child get ready:
• Have your child greet the doctor at the start of each visit.
• Encourage your child to tell you if something hurts or is bothering them. Then have your child practice telling this to the doctor. Making a script, writing a list, or role-playing before you go to the doctor might help your child be more comfortable.

• Ask your child to come up with at least 1 question to ask the doctor on each visit. Write or record the questions ahead of time to bring with you. If your child uses a communication device, just enter their questions into it before you go.
• Teach your child about their medical needs. As you do something for them, explain why you are doing it. Ask them to start explaining these things back to you.
• Show your child their care notebook and your filing systems so that they know where things are and what to keep track of. Ask them to help you read over paperwork, organize it, and more –as much as they can do.
• Take them with you to the pharmacy and show them how to use call-in or online refill systems. Have them ask for their own prescription when you pick it up. You can role-play this beforehand. And, if your child uses a communication device, enter these questions into it before you go.
• Have your child start helping you fill out their medical forms and schedule doctor’s visits. This might be you reading the questions to them and talking about the answers as you write them. Or having them listen in as you call and schedule a visit. Many doctor’s offices are now putting forms and appointment requests on their websites, so you and your child can just use a computer at home.
You don’t have to manage these big changes alone. If you are using the medical home model, the core medical team your child has been seeing can help your child get ready for this transition. Even though they might be transitioning out of being your child’s main team, they can help make the move to a new medical home smoother.
(Continued on page 15)

For our complete list of resources go online to www.ExceptionalKidsTexas.com
Apara Autism Centers
844-272-7223
1922 Dry Creek Way Suite 2-101 info@AparaAutism.com www.AparaAutism.com
◆Autism Treatment Center
210-590-2107
15911 Nacogdoches Rd Building 2 www.atcoftexas.org
Bloom Behavior & Educational Solutions
210-643-1119
1850 Lockhill Selma Suite 106 www.bloom-aba.net
Cole Academy - ABA Solutions
210-891-0800
1202 E Sonterra, Blvd 6, Suite 609 info@colehealth.com colehealth.com
Cole Academy - ABA Solutions
830-420-6200
6051 FM 3009, Suite 215 info@colehealth.com colehealth.com
Mindcolor Autism
833-646-3222
8507 Culebra Rd Suite 101 info@mindcolorautism www.mindcolorautism.com
LifeSpan Home Health
877-434-3153
6243 IH-10 W Suite 375 www.lifespantx.com
Pg 2
◆Donate◆
ADAPTIVE SPORTS (COMPETITIVE & RECREATIONAL)
◆Kinetic Kids
210-748-5860
11931 Starcrest Dr info@kinetickidstx.org www.kinetickidstx.org
◆Pathways Youth & Family Services
210-733-7117
1919 NW Loop 410 Suite 201 www.pathway.org
◆Artvango Therapeutic Services Inc.
210-387-2218
3201 Cherry Ridge Suite B202 artvangosa@gmail.com artvango.org
◆Artvango Therapeutic Services Inc.
210-387-2218
3201 Cherry Ridge Suite B202 artvangosa@gmail.com artvango.org



For our complete list of resources go online to www.ExceptionalKidsTexas.com
uDonateu
Catholic Charities
210-377-1133
San Fernando Community Center 231 W Commerce
uDeaf Interpreter Services, Inc. 210-545-2946
15600 San Pedro Ave #302 info@deaf-interpreter.com www.Deaf-Interpreter.com
uEpilepsy Foundation Central & South Texas 210-653-5353
8601 Village Dr, Suite 220 staff@efcst.org www.efcst.org
Achievers Center for Education
210-690-7307
5084 De Zavala Rd www.aceschool.org
uEpilepsy Foundation Central & South Texas 210-653-5353
8601 Village Dr, Suite 220 staff@efcst.org www.efcst.org
uFACT Institute, Inc. 210-267-9134
13032 Nacogdoches Rd #207 life@factinstituteinc.com www.factinstituteinc.com
uThe Winston School of San Antonio 210-615-6544
8565 Ewing Halsell Dr www.winston-sa.org
Catholic Charities 210-293-1009
202 W. French Place www.ccaosa.org
uPathways Youth & Family Services 210-733-7117
1919 NW Loop 410 Suite 201 www.pathway.org
Crisis Intervention (Foster Care Only)
1-866-912-6283 (press *)
1919 NW Loop 410 Suite 201 www.pathway.org
www.unitedwaysatx.org
2-1-1 Texas is a free, anonymous social service hotline available 24 hours a day, 7 days a week, 365 days a year.
Alamo Local Authority
Intellectual & Disability Services (IDD)
Phone: (210) 832-5020 Fax: 1-866-689-1843
2700 NE Loop 410 Suite 101 iddservices@aacog.com http://www.aacog.com
City of San Antonio - Utility Assistance 210-207-7830
uDown Syndrome Association of South Texas 1127 Patricia info@dsastx.org www.dsastx.org

For our complete list of resources go online to www.ExceptionalKidsTexas.com
uEpilepsy Foundation Central & South Texas
210-653-5353
8601 Village Dr, Suite 220 staff@efcst.org www.efcst.org
Hill Country MHDD Centers
358 Landa Street, Suite 300, New Braunfels 888-315-3277
http://www.hillcountry.org
Kerr County MH Center
955 Water Street, Kerrville 888-445-5232
http://www.hillcountry.org
Project Warm - Bexar County Dept of Community Assistance
210-335-3666
Salvation Army
210-226-2291
226 Nolan St
San Antonio Food Bank
210-337-3663
5200 Old Hwy 90 West
Society of St. Vincent de Paul
210-225-7837
WIC Program
210-207-4906
The Law Offices of Carol Bertsch, PC Pg 13 210-672-1034
8703 Broadway
www.assistingseniors.com
LOCAL IDD AUTHORITY (LIDDA) FOR BEXAR COUNTY
AACOG IDD Services - Alamo Area Council of Governments: Intellectual & Developmental Disabilities Services
210-832-5020
2700 NE Loop 410 Suite 101
https://www.aacog.com/66/Intellectual-Developmental-Disability-Se
uDonateu
uEpilepsy Foundation Central & South Texas 210-653-5353
8601 Village Dr, Suite 220 staff@efcst.org www.efcst.org
CDS in Texas Pg 2 210-798-3779
Toll Free 866-675-7331 www.cdstexas.com
CLASS - Medically Dependent Children's Program 877-438-5658
DBMD-Deaf/Blind Multiple Disabilities Program 877-438-5658
Disability Services of the Southwest
210-798-0123
6243 IH-10 West Suite 114
www.dsswtx.org
HCS - Home & Community-Based Services Program 210-832-5020
MDCP - Medically Dependent Children's Program 877-438-5658
LifeSpan Home Health Pg 2
877-434-3153
6243 IH-10 W Suite 375 www.lifespantx.com
Texas Home Living Waiver 210-832-5020

For our complete list of resources go online to www.ExceptionalKidsTexas.com
American Red Cross 210-224-5151
Cerebral Palsy Foundation ucp.org 210-520-1686
uEpilepsy Foundation 24/7 Helpline 1-800-332-1000 (en espanol 1-866-748-8008) www.epilepsy.com
Muscular Dystrophy Association (MDA) 800-572-1717
National Alliance for Mental Illness (NAMI), SA 210-734-3349
National Down Syndrome Society 800-221-4602 www.ndss.org
Scleroderma Foundation www.Sclerodema.org
Spinal Bifida Association Texas Chapter 972-238-8755
Williams Syndrome 800-806-1871
www.Williams-syndrome.org
uAutism Treatment Center
210-590-2107
15911 Nacogdoches Rd, Building 2 www.atcoftexas.org
CHCS-ECI (Early Childhood Intervention)
Specializing in Infants & Toddlers, Birth to 36 Months Easy to refer, no medical referral needed
Call 210-261-3300 or visit www.chcs-eci.org
Medicaid, CHIP, Private, all insurances accepted Sliding scale available
Cole Pediatric Therapy 210-891-0800

uDonateu
1202 E Sonterra, Blvd 6, Suite 609 info@colehealth.com colehealth.com
Cole Pediatric Therapy
830-420-6200
6051 FM 3009, Suite 215 info@colehealth.com colehealth.com
San Rafael Healthcare Inc
14 210-255-1466
4203 Gardendale St #C105 www.sanrafaelhealthcare.com
111
4502
2027
275 W Campbell Rd, Richardson
San
210-255-1466
4203 Gardendale St #C105
www.sanrafaelhealthcare.com
CHCS-ECI (Early Childhood Intervention)
Specializing in Infants & Toddlers, Birth to 36 Months
Easy to refer, no medical referral needed Call 210-261-3300 or visit www.chcs-eci.org
Medicaid, CHIP, Private, all insurances accepted Sliding scale available

For our complete list of resources go online to www.ExceptionalKidsTexas.com
PHYSICAL THERAPY
Cole Academy - ABA Solutions 210-891-0800
1202 E Sonterra, Blvd 6, Suite 609 info@colehealth.com colehealth.com
Cole Academy - ABA Solutions 830-420-6200
6051 FM3004, Suite 215 info@colehealth.com colehealth.com
San Rafael Healthcare Inc Pg 14
210-255-1466
4203 Gardendale St #C105 www.sanrafaelhealthcare.com
San Antonio Parks and Recreation Department 210-207-3018
SCHOOLS
uThe Winston School of San Antonio 210-615-6544
8565 Ewing Halsell Dr www.winston-sa.org
uFact Institute Inc 210-267-9134
13032 Nacogdoches #207 life@factinstituteinc.com www.factinstituteinc.com
MC Educational Advocacy & Consulting LLC 210-901-9695
maryc@mceac.info www.mcedac.com
uMarbridge Foundation 512-282-1144
2310 Bliss Spillar Road, Manchaca TX info@marbridge.org Marbridge.org
uAutism Treatment Center 210-590-2107
uDonateu
15911 Nacogdoches Rd, Building 2 www.atcoftexas.org
CHCS-ECI (Early Childhood Intervention)
Specializing in Infants & Toddlers, Birth to 36 Months Easy to refer, no medical referral needed Call 210-261-3300 or visit www.chcs-eci.org Medicaid, CHIP, Private, all insurances accepted Sliding scale available
Cole Pediatric Therapy 210-891-0800
1202 E Sonterra, Blvd 6, Suite 609 info@colehealth.com colehealth.com
Cole Pediatric Therapy 830-420-6200
6051 FM 3009, Suite 215 info@colehealth.com colehealth.com
San Rafael Healthcare Inc Pg 14 210-255-1466
4203 Gardendale St #C105 www.sanrafaelhealthcare.com
Customer Service Line (Ombudsman) 877-787-8999 www.hhsc.state.tx.us
Department of Assistive & Rehabilitative Services NOW Texas Work Force www.twc.state.tx.us
North Field Office
210-561-8600
12000 Network Blvd #210
West Field Office 210-522-8010
5309 Wurzbach, Suite 102
Northeast Field Office 210-590-5740
10303 Nacogdoches
South Field Office 210-927-8300
1011 Ada St

We are here for the messy parts.
We do supplemental needs trusts. We can help you plan.



According to the US Census Bureau, over 27% of the U.S. population is under some form of disability. Many of these people rely on means-tested public bene ts (i.e., bene ts with nancial hardship requirements), and the number of Americans living with disabilities is expected to increase as the population ages. e need for specialized planning for these individuals is rapidly growing.
One issue faced by many persons living with disabilities arises when they come into a sum of money from an inheritance or lawsuit/settlement.
ese new assets can often cause them to lose vitally important means-tested bene ts. A supplemental needs trust (SNT) is a tool used to preserve governmental bene ts while providing a source of funds that provide for supplemental needs not covered by government assistance. is includes a wide array of goods/services, from adaptive aids and caregiver expenses to transportation and even vacations. An SNT allows these funds, managed by another person (the “trustee”), to be made available to the individual living with disabilities while not being treated as a resource that would otherwise disqualify them from public bene ts.
Parents including supplemental needs trusts in their wills can allow a child living with disabilities
to inherit assets without losing necessary bene ts like SSI and Medicaid. is type of SNT is called a “third party SNT” because it is funded by the assets of someone other than the person living with disabilities. If certain key requirements are met, the person living with disabilities can even create a “self-settled” SNT using their own funds. However, self-settled SNT’s must have a provision to pay back the State for bene ts received during that person’s lifetime, while third-party SNT’s are not required to have a “pay-back provision” -- so using the right type of trust is key.
It is best to consult with an attorney specializing in elder or disability law to ensure that a new SNT is appropriate for each individual’s unique circumstances. But supplemental needs trusts provide persons living with disabilities and their loved ones a wonderful opportunity to improve quality of life while maintaining eligibility for public bene ts.
Brennen Boze AttorneyLaw O ces of Carol Bertsch
8703 Broadway
San Antonio, TX 78217
Ph: 210.892.4555 Fax: 210.892.4505
bboze@assistingseniors.com


SERVINGS: 24
AUTHOR: Catherine McCord
PREP TIME: 15 minutes
TOTAL TIME: 15 minutes
Ingredients
1/2 cup whipped light cream cheese
2 teaspoons strawberry preserves
1 quart large strawberries (about 24)
48 mini chocolate chips
blueberries
raspberries
blackberries
pineapples, cut into small shapes
toothpicks
Instructions
1. In a small bowl, stir together the cream cheese and preserves. Spoon the mixture into a plastic sandwich bag and snip off one corner to create a mini piping bag.
2. Slice off the top or bottom of each strawberry to create a flat surface so that the strawberry will stand on it's own.

3. Slice a small notch out of the strawberry near the top and fill the notch with the cream cheese mixture.
4. Press 2 mini chocolate chips into the cream cheese to create eyes.
5. Press 1 or 2 toothpicks into the top of the strawberries and skewer with the remaining berries and pineapples to create antenna.
Here are some of the steps:
• Have a meeting with your child and their primary medical team to talk only about medical transition. You can do this as early as your child’s 14th birthday.
• Talk about each of the skills that your child will need to take part in adult health care. These include explaining their medical needs, knowing what to do in case of a medical emergency, being able to fill a prescription, managing health insurance, and getting themselves to a doctor’s visit, among other things. Make a plan to target the skills your family is going to work on first, and then later. Use it to figure out where your child will need extra help.
• Go through the list of your child’s doctors, therapists, and specialists to see which ones also work with adults. Work with your child and your medical team to decide who is going to replace the doctors that have to change.
• Work together to create a timeline for changing each of these doctors. The timeline might depend on your child’s abilities and what medical care skills they’ve developed.
• When it's time to transfer to a new doctor, ask your current medical team to be part of the process. See if there is a nurse coordinator who can gather the information from your current team and come to a meeting with your new team to share recommendations. They should also send along any files, records, or other background that will help the new doctor learn about your child's medical history.
Just because you start working on this plan when your child is 14 years old doesn’t mean you have to get the whole plan together overnight – or even in a year. Transition is a process, and creating a good plan is a process too. It will need to be updated as your child grows and changes in their teens.
Many of us have been through the switch to a new doctor. But, in the transition time, there are a few things you can do to find the right doctor and make things go more smoothly.
• Connect with other parents to find adult doctors in your area who work well with adults with disabilities or special health care needs.
• Think about your own doctors. Would they work well with your child?
• Ask for recommendations from your child’s doctors. Maybe they also work with adults or have

someone in their practice who does.
• Make a short 1- or 2-page summary of your child’s medical history that you can hand to any new doctors.
• Include your child. Have them help you find or interview some of the doctors.
• Think about making the transition a little early, before you absolutely have to, so you have enough time to get help if you run into any problems.
Group or private health insurance plans will let your child stay on your plan until they turn 26 years old – or longer, depending on their disability or special health care need. This gives you and your child time to figure out how they will get their own insurance coverage. Here are some ways to get insurance.
• Private insurance: The Affordable Care Act makes sure that everyone can get private health insurance, despite any pre-existing conditions.
• Employer-provided insurance: If your child is employed, they may be able to get insurance through their employer.
• Staying on your insurance: Depending on your child’s disability or special health care need, they can stay on your plan, even when they turn 26 years old. Talk to your insurance provider to see how to keep your child on your plan. Contact your health insurance company one year before your child turns 26 to see if the coverage can continue.
• Medicaid: Based on your child’s income, they might be able to get insurance coverage through Medicaid. At age 18, Medicaid only looks at your child’s income instead of the family income.
• Medicare: If your child receives Social Security Disability Insurance (SSDI) benefits, they can get insurance coverage through Medicare after they have SSDI benefits for 24 months.