
























11 days after appendectomy, tests for acute abdominal pain revealed a
left inside the patient.
Surgical miscounts are considered never events because they are usually preventable by following established procedures.
ProAssurance offers risk assessments designed to help practices minimize errors by establishing and evaluating safety procedures and communication protocols.
With reliable procedures in place, our insureds are more likely to reduce errors in their medical practice, avoid claims, and make claims more defensible if they do occur.




PRESIDENT Neelesh Bangalore, MD
PRESIDENT ELECT Sujeeth Punnam, MD
TREASURER Stephen Tsang, MD
BOARD MEMBERS Cyrus Buhari, DO, Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Sanjeev Goswami, MD, Kinnari Parikh, MD, Bhagya Nakka, MD, Sunny Philip, MD, and Ripudaman Munjal, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE Larry Frank, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Gregg Jongeward, PhD
CMA HOUSE OF DELEGATES REPRESENTATIVES
Robin Wong, MD, Lawrence R. Frank, MD
James R. Halderman, MD, Raissa Hill, DO
Richelle Marasigan, DO, Ramin Manshadi, MD
Philip Edington, MD , Sujeeth Punnam, MD
Sunny Philip, MD, Ripudaman Munjal, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Neelesh Bangalore, MD
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Neelesh Bangalore, MD, Maggie Park, MD, Cyrus Buhari, DO, and George M. Khoury, MD
THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO: San Joaquin Physician Magazine 3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS:
Monday through Friday 8:30am-4:30pm
Closed for Lunch between 12pm-1pm

As the San Joaquin Medical Society prepares for its 150th anniversary celebration, I began to explore the history that has shaped this esteemed organization since its founding in 1874. Delving into old albums, notebooks, and fragile artifacts dating back to the early 1900s, I found myself absorbed in the stories they told—stories of perseverance, adaptation, and a deep commitment to the medical community. Some of the minutes were beautifully written by hand, so intricate and detailed that they were sometimes difficult to decipher— not due to the illegibility often associated with “physician’s handwriting,” but because of the formal script typical of the era.

Without an official office, board meetings were held at various locations, including the Chamber of Commerce and physicians’ homes. These meetings, held on the second Friday of each month, began at 8:00 p.m. and often didn’t adjourn until well after 10:30 p.m., reflecting the dedication of those early members whose passion for the medical society kept them engaged, even as the hours stretched late into the evening. Meeting topics included the latest public health challenges, new diagnoses and treatment regimens, fee schedules, and ethical discussions.
In 1918, Dr. Margaret Symth made history as the first woman elected to serve as president of the San Joaquin Medical Society. A pioneering figure, she would later serve as the Superintendent of Stockton State Hospital. Her leadership during that era speaks to the remarkable fortitude and vision of this trailblazing woman. That same year, however, the society faced a financial crisis. With many members serving in World War I, dues went unpaid, and the organization’s funds were quickly depleted. After careful deliberation, the board made the difficult decision to impose a $2 assessment on each member to keep the society’s operations afloat. This bold move not only ensured the society’s survival but also highlighted the resilience and solidarity of the medical professionals who rallied together in the face of unprecedented challenges.
The rich history of the medical society is reflected in the portraits that line the walls of our boardroom. With each passing year, the collection of presidential portraits, beginning in 1903, continues to grow—a testament to the continuity of leadership that has steered the SJMS through decades of change. Suffice it to say, we may eventually run out of wall space—but that’s a problem for the future Executive Director to address.
As we move into the holiday season, I wish you abundant laughter, joy, and good cheer, as well as cherished time with those who mean the most to you. It has been an honor to lead the society for another year. I look forward to seeing you at our 150th Anniversary Celebration on December 12.
Happy Holidays,

Lisa Richmond



Neelesh Bangalore, MD is the current president of the San Joaquin Medical Society and practices at Stockton Hematology Oncology Medical Group
Let me start by congratulating San Joaquin Medical Society for turning 150 years in 2024. It has been wonderful to be the president during this time. There will be a celebration of this monumental event on December 12 which I am eagerly looking forward to. It reminds me of all the achievements of San Joaquin Medical Society. Especially, programs such as Bridge to Medicine, Decision Medicine, Scholarship Loan Fund as well as SJMS Alliance which offers through networking and social programs to support members as well as spouses of physicians. I am also reminded of all the advocacy that SJMS has been doing over many, many years.
One of the recent achievements related to activities of SJMS is the passage of Prop 35. As you may all know Prop 35 was resoundingly approved. It was voted yes by 67.5% of the Electorate. It is an investment in Medi-Cal services which will affect approximately 15 million Californians. This has been a concerted effort by CMA and a broad coalition, including SJMS. Many members, physician practices, healthcare facilities, as well as hospitals led the effort to promote education on this proposition. Clearly it was an excellent combined effort.
Prop 35 will protect and enhance our health care system for Medi-Cal patients and ALL Californians. Prop 35 will secure ongoing revenue by extending an existing tax on health insurance companies and dedicate these funds to protect and expand access to care. And it will prevent the state from redirecting these revenues for non-health care purposes.
The question is: who specifically benefits from the passage of Prop 35? Approximately 15 million Californians rely on Medi-Cal for health insurance coverage including more than 50% of all children of low-income families, seniors, and patients with disabilities. It has been tough for this group to see primary care doctors and specialists in a timely manner. Therefore, many times emergency rooms are used as a substitute for primary care services. By providing this much-needed dedicated funding we will hopefully see significant improvement in the usage of Emergency Room services, reimbursement to the doctors and clinics which will directly affect patient care positively. It would also
help to expand access to primary care services, specialty services, family-planning and mental health providers.
Prop 35 will protect and enhance our health care system for Medi-Cal patients and ALL Californians. Prop 35 will secure ongoing revenue by extending an existing tax on health insurance companies and dedicate these funds to protect and expand access to care.
The San Joaquin Medical Society will continue to be an advocate for the community as well as for physicians and healthcare clinics. Our goal is to address both sides of the issues. Community access to healthcare and appropriate reimbursement to physicians and clinics who spend significant time and effort to provide the needed care. In a way, SJMS is trying to be efficient in terms of getting the best out of healthcare dollars.

Job Fair & Mixer invites medical residents to envision a career in San Joaquin County
BY JO ANN KIRBY

After a long day of work, weary medical residents had a chance to unwind and check out employment opportunities at the San Joaquin Medical Society’s inaugural Job Fair & Mixer in September at Mercedes Benz of Stockton.
The new initiative is yet another way that SJMS is working to address a critical physician shortage in San Joaquin County. As it prepares to celebrate its 150th anniversary, the society’s rich history of community involvement includes programs to inspire local students to become physicians continues. Now, SJMS is reaching out to medical residents who are training in San Joaquin County to inform them of the myriad of employment opportunities that await them.
“We have residents here from St. Joe’s and San Joaquin General and our goal is to retain the residents in the county where they are training. Our hope is that they stay and practice medicine here,” Lisa Richmond, executive director of SJMS, said at the event, which also welcomed the society’s general membership. Afterwards, she said feedback from both vendors and attendees was positive.
The San Joaquin County has been deemed a medically underserved area for at least three decades. According to Congressional Rep. Josh Harder, who represents a portion of San Joaquin County and routinely introduces legislation to


and his office reports that there are 22% fewer primary-care physicians than the state average. Many of those who do practice are aging toward retirement.
“We’re focusing on trying to retain talent locally,” Dr. Neelesh Bangalore, president of the San Joaquin Medical Society, said. “It has been difficult to recruit doctors to our community. There is a big push to change that.”
Gill Primary Care had a booth at the event with staff who provided information about two physician openings at their growing practice, highlighting the urgent need that residents could fill. Residents were able to chat with Shanette Hagedorn, Gill Primary Care Manager, and Gill’s two primary care physicians, the Pennisi twins – Dr. Dominic Pennisi and Dr.
Vincent Pennisi, who said they were covering the equivalent of four practice by themselves and are looking for either two physicians to join them or one physician and a nurse practitioner.
Dr. Kwabena Adubofour was one of several SJMS members who attended the job fair and spoke with residents about their aspirations. He is a co-founder of the society’s Decision Medicine program, and he beamed with joy as Dr. Breanna Hernandez, who attended Edison and Stagg high schools in Stockton, said she was interested in staying local. “Of course you are,” he said, as if there were any other option for her. She is specializing in internal medicine. Dr. Adubofour applauded the job fair as an excellent way to expose new doctors to a myriad of positions in their field.
The residents who attended the event have bright futures ahead and would be ideal physicians for such a diverse community, with many of them speaking more than one language. Residents said that they have enjoyed their training here, so far and would consider the possibilities of practicing locally.
“The community here is so kind and welcoming, so I’m not ruling it out,” Dr. Duc-Huy Nguyen, a third-year family medicine resident who speaks Vietnamese and is getting better at Spanish, said. “I’m not sure where I want to practice. I’m from Sacramento and I have ten months left.”
Dr. Diego Marquez, who is from Chicago, said all of his medical school friends are from San Joaquin County and they were the ones who had encouraged him to do his residency here. Now, he’s thinking about sticking around. “I’m looking for something in emergency medicine primarily,” he said. “I will
be double boarded in two residencies – family medicine and emergency medicine.
Vendors said they enjoyed the opportunity to speak to the residents. Kelvin Amoah, a physician recruiting liaison with Hill Physicians Medical Group, said the main goal is “meeting the residents and letting them know we exist. If we aren’t the team for them, we point them in the right direction.”
In addition to meeting potential employers, attendees got to nosh on a buffet of appetizers and desserts, enjoy drinks and talk with colleagues about their day. Dr. Courtney Nguyen had started her workday at 6 a.m. and made it to the mixer by 7 p.m. She was grateful to be able to grab a bite to eat and put her name in the raffles for a chance to win prizes such as a Nespresso Vertuo machine, Air Pods, Uber Eats gift cards and more.
Sponsors of the event included Adventist Health, Art Godi Realtors, California Medical Association, Dignity Health St. Joseph’s Medical Center, Gill Primary Care, Hill Physicians Medical Group, ProAssurance, Sutter Health and The Permanente Medical Group. The San Joaquin Medical Society hopes to build on the success of the inaugural event and attract even more residents and vendors next year. As with its scholarship opportunities and programs such as Decision Medicine and Bridge to Medicine, the Job Fair & Mixer is another way SJMS is rising to the challenge of reversing desert conditions in local medicine.









Throughout our hospitals and clinics, Adventist Health physicians have the opportunity to help individuals live healthier, happier lives. Joining one of our facilities in Calaveras, San Joaquin or Tuolumne counties allows you to transform the health experience of the communities we serve through our unique focus on caring for the whole person — mind, body and spirit. As an Adventist Health physician, you will find a more fulfilling, inspiring career.
We are currently seeking primary care physicians, as well as physicians across various specialties such as: Cardiology, Dermatology, Endocrinology, Gastroenterology, Obstetrics & Gynecology, Orthopedic Surgery, Radiology, Wound Care, and Urology. If interested in learning more, visit AdventistHealth.org/Provider-Careers or email our Physician Recruitment team at PhyJobs@ah.org.
Join our dedicated team at Gill Primary Care, where we are seeking a skilled Primary Care Physician to provide compassionate medical care to our diverse patient population. We offer a supportive work environment with competitive compensation and benefits.
Responsibilities:
• Provide comprehensive primary care services to patients of all ages.
• Diagnose and treat acute and chronic illnesses.
• Perform routine check-ups, screenings, and vaccinations.
• Collaborate with specialists and healthcare professionals as needed.
Requirements:
• Medical degree (MD or DO) from an accredited medical school.
• Board certification in Internal Medicine or Family Medicine.
• Active medical license in California.
• Strong communication and interpersonal skills.
Benefits:
• Competitive salary with productivity incentives.
• Comprehensive benefits package including health, dental, and retirement plans.
• Malpractice coverage.
To Apply: Interested candidates should submit a resume/CV and cover letter to gillmed@sbcglobal.net

Hill Physicians Medical Group
Personalized care for every body!
Hill Physicians Medical Group is proud to provide top quality, highly rated medical care and services to meet the need of our members in San Joaquin County.
With 6,000 physicians – the largest network of independent doctors in Northern California – Hill Physicians patients have a diverse selection of primary care and specialty providers, backed up with pharmacy consultations, health educators, case management and outstanding customer service to advocate for our members.

Save time, check into our ER online.
We’re here with 24-hour emergency care. And, with our InQuicker, you can let us know you’re on your way.
When an emergency changes your plans, plan to get great care. Our experienced ER team is ready at any time to diagnose and treat a variety of emergency conditions, including life-threatening illnesses, injuries, broken bones, burns, stroke, heart conditions and more.
In addition, as part of Central Valley Doctors Health System, we can enhance patient-care coordination and provide access to additional specialized services and resources provided by Doctors Medical Center and Emanuel Medical Center.
When an emergency strikes, you can trust the ER team at Doctors Hospital of Manteca.

Doctors Hospital of Manteca Taps New CEO
We’re proud to announce our new Chief Executive Officer, Tina Burch, RN, MSN. Burch began her nursing career at DHM more than 33 years ago and has served as an asset to the hospital since, serving in various leadership roles.
To check in online, scan the code or visit DoctorsManteca.com/ER For life-threatening emergencies, call 911.

A note of gratitude from
George M. Khoury, MD
It was 33 years ago that I came to Stockton to join my father’s practice. The community welcomed me warmly and helped me acclimate to both Stockton and the practice of medicine.
The San Joaquin Medical Society (SJMS) was instrumental in guiding me as a young physician venturing into private practice, far removed from the hospital environment I had known for 12 years. In the 1980s and early 1990s, most practices in Stockton were private or small groups. Then came the era of Independent Practice Associations (IPAs), like Delta IPA and Medcore, followed by medical group foundations spearheaded by Kaiser, Gould Medical Group, and others. These groups emerged to help physicians navigate the complexities of medical practice regulations and insurance reimbursements. Every doctor was vying for their fair share of the healthcare dollar. Medicare and MediCal rates plummeted, affecting everyone, though some specialties were hit harder than others. The hospital systems and pharmaceutical industry initially faced less drastic cutbacks, but this changed over time, even as these giants found ways to mitigate the impact.
The Medical Society and California Medical Association (CMA) were invaluable in guiding me through this maze, offering best practice guidelines,

fiscal management advice, and support with malpractice and office employee issues. The SJMS not only supported my professional growth but also helped me connect with the medical community, fostering friendships and a sense of camaraderie. This support was crucial for my wife, Kari, who relocated from the East Coast and found a welcoming community and lasting friendships here.
The SJMS assisted me with health insurance for myself and my staff, malpractice insurance, corporate governance, and community involvement. My father encouraged me to join the medical society, leading me to serve on the membership committee, finance committee, and eventually the board, culminating in my role as president. The encouragement from the committee and board members was pivotal in my journey.
As a CMA member, I witnessed its societal and political roles. Serving as an alternate delegate, I became involved in local issues through the Delta IPA and the Health Plan of San Joaquin medical and pharmaceutical utilization committees, eventually joining their boards. Through these committees, I learned about our community’s chronic health issues and
disparities in access to care, nutrition, air pollution, and social inequities. Inspired by my colleagues, most notably Dr. Kwabena Adubofour, I joined their efforts to address these challenges. My background in Internal Medicine enabled me to engage in community health education through diabetes groups, churches, and the cancer society. I worked as a community liaison for the medical society, including the Asthma Coalition, Diabetes Commission, and Su Salud.
My most profound experience has been the establishment of the Decision Medicine program, which the Medical Society has wholeheartedly championed. The program was the brainchild of a discussion Dr. Adubofour, and I had while playing golf, as a means to increase the number of physicians who would be invested in returning to our community and eventually replace us. Seeing the excitement in the eyes of high school students as they went through the program and the fruition of some of these students becoming physicians and returning to their community is incredibly satisfying. Keep passing it forward.
The tumor conferences with local Hematology and Oncology specialists, Radiation Oncologists, and surgical specialists were invaluable learning experiences, enhancing my radiologic assessments. The feedback from pediatric physicians improved my ability to support our mutual patients. The medical community, including referring physicians and continuing education meetings at Dameron Hospital and St. Joseph’s Medical Center, has been instrumental in my growth.
I am profoundly grateful to the referring physicians who have supported our radiologic services over the years. I hope you continue to use our office, which provides stateof-the-art, affordable services with subspecialties in every radiologic field.
I am profoundly grateful to the referring physicians who have supported our radiologic services over the years.
I also served on the boards of DELTA IPA and the Health Plan of San Joaquin to ensure we were doing the right thing for physicians and patients. Over the years, I formed many acquaintances and friendships, learning from local physicians in specialties like orthopedics, endocrinology, ENT, oncology, pulmonary, and GI. I am deeply grateful for their contributions to my continued education, particularly Dr. Salamon, an excellent educator in orthopedics.
The art and science of medicine continue to evolve. One constant truth is that knowledge continuously changes. The radiology my father practiced transformed dramatically by the time I became a radiologist, with advancements in diagnosis, reduced radiation exposure, and the growing use of Artificial Intelligence (AI). The days of the Star Trek “Medical Tricorder” are not far off, with tools like glucose monitors and cardiac monitors now available on our cell phones. Telemedicine and teleradiology are advancing such that we can diagnose patients at the far ends of the world as well as in space.
While I will miss the ever-changing world of medicine, I am fortunate to be a potential patient with access to these remarkable advances.
Thank you all for your support and camaraderie over the years.

For the California Medical Association (CMA), the 2024 legislative year started out with an ominous beginning. In 2023, CMA successfully negotiated the largest investment in Medi-Cal in history, including billions to increase reimbursement rates, through an expansion of the Managed Care Organization (MCO) Tax. Utilizing the MCO Tax as a funding source meant that California could finally fund the Medi-Cal program and create true health equity without raising taxes on individuals or cutting other crucial programs. While some reimbursement rates were raised under the MCO Tax in 2024, the bulk of the new funding was allocated to increase rates starting in 2025.
In January 2024, however, Governor Newsom’s initial 2024-25 budget proposal estimated a budget deficit of $22.5 billion, a number that would grow to $68 billion by the May budget revision.
The governor’s revised budget proposal cut all of the proposed new Medi-Cal funding from the MCO Tax and swept the entirety of the tax, over $21 billion, into the state’s general fund coffers to cover normal operating expenses of the state.
This is why CMA led the charge to pass Proposition 35 this November. Voters overwhelmingly approved Prop 35, which will secure ongoing funding for Medi-Cal and dedicate these funds to protect and expand access to care for all Californians. And importantly, it prevents the state from redirecting these revenues for non-health care purposes.
The expansion of Medi-Cal over the last decade has resulted in some incredibly illuminating statistics that underpinned CMA’s determination for increased Medi-Cal investments:
+ Half of all babies in California are born through Medi-Cal.
+ The program now covers one-third of the state – almost 15 million people.
+ It is the largest state Medicaid program in the country, both in overall size and percentage of the population.
+ California lands near the bottom of Medicaid reimbursement rates nationally, ranking 40th, even though the cost of living and practicing in California is much higher than in many other states.
+ California has not raised Medi-Cal rates across the board since 2000, and in fact has cut them twice in the past 24 years. While some physicians received increases thanks to CMA-sponsored Prop 56 (2016), those increases were limited to supplemental payments for a short list of codes for physician services, dental care and family planning services.
While the battle for Medi-Cal funding has been CMA’s top priority this year, the association engaged on multiple fronts on behalf of the physician community.
In 2024, the California Legislature introduced a total of 2,124 bills. Of the bills that made it to Governor Newsom’s desk, 1,017 were signed and 189 were vetoed. The most common reason given by the governor for a veto over the past two legislative cycles was that the legislation would strain the budget. The second most common reason cited for a veto this year was a simple disagreement with the policy.
In the end, four of CMA’s priority bills made it to the governor’s desk and all four were signed.
CMA was also at the forefront of key legislative battles, ensuring that many bills that would have negatively impacted patients and the practice of medicine would not move forward through the legislative process.
CMA successfully defeated several pieces of legislation that would have jeopardized patient safety by creating an exemption to the ban on the corporate practice of medicine; imposed burdensome regulations on physician practices; heightened the risk of unnecessary lawsuits against physician practices; and legislated the practice of medicine.
CMA sponsored a bill on prior authorization and its intersection with the growing utilization of augmented intelligence (AI) in health care decision-making. SB 1120 (BECKER), the Physicians Make Decisions Act, prohibits a health plan from using AI for prior authorizations or utilization review unless a physician is overseeing the process. The bill passed out of the legislature and was signed by the Governor. It was one of the few bills on regulating AI that were signed by the Governor this year and it is likely to be replicated in many other states. CMA also sponsored SB 598 (SKINNER), which would have required health plans to institute a one-year prior authorization exemption for physicians who practice within the plan’s criteria 90% of the time. It would also have granted treating physicians the right to have their appeals of prior authorization denials conducted by a physician in the same or similar specialty. Unfortunately, this bill stalled over opposition from the administration. CMA subsequently worked with the administration to create a pilot program where prior authorization would be eliminated on a code-by-code basis as determined by the California Department of Managed Health Care (DMHC). CMA was successful in getting this language inserted into a bill that was amended out of Assembly appropriations Committee in August (SB 516, SKINNER). However, the new Assembly Health Chair, Mia Bonta, insisted on reporting requirements that would have increased administrative burdens on many physician practices, and we were forced to hold the bill this year.
CMA engaged on AB 3129 (WOOD), which would have granted the Attorney General new enforcement powers over private equity transactions of health care entities. CMA worked to ensure critical amendments were included in the bill that would strengthen the bar on the corporate practice of medicine and give the attorney general new powers to independently bring actions against violators. Additionally, CMA secured amendments that made the reporting thresholds consistent with those of the California Office of Health Care Affordability (OHCA). CMA initially started in a support if amended position, but moved to support after these amendments were taken.
The bill took hostile amendments out of Senate Appropriations committee, which exempted hospitals and physician groups who primarily provide dermatologic services. It remains a Sacramento-wide mystery as to who requested these amendments as they did temper CMA support. The bill did pass out of the legislature but was vetoed by the governor with the veto message claiming that OHCA already has sufficient powers to oversee private equity activity.


CMA and the California Academy of Eye Physicians and Surgeons (CAEPS) jumped into early action this year to stop a bill (AB 1570, LOW) that would have authorized optometrists to perform six new procedures using lasers and scalpels in and around the eye with minimal training, at a great risk to patient safety. It is not hard to see why this bill was a bad idea. Thanks to the grassroots efforts of CMA physicians, we were successful in holding this bill on the suspense file in the Appropriations Committee, ensuring it would not move forward in the legislature.
SB 1451 (ASHBY) was a Business and Professions omnibus bill that required CMA to advocate for and against different pieces of the bill. CMA was successful in including title transparency language that prevents anyone other than an MD or DO from using the term “doctor or other like terms” in a medical setting where the patient would believe that licensee was a physician. Combined with our badge requirements, California has some of the strongest title transparency laws in the nation.
The bill included CMA-opposed changes to the Nurse Practitioner Practice Act that loosen training requirements for independent practice. CMA was successful in obtaining an amendment that requires all clinical experience required for independent practice to occur entirely within California, preventing the bill from creating a back door nursing licensing compact for nurse practitioners.
CMA partnered with the California Society of Anesthesiologists in opposing AB 2526 (GIPSON), which would have allowed nurse anesthetists to prescribe and administer sedation independently in dental offices. This bill was successfully held in Assembly Appropriations Committee.
CMA also successfully collaborated with Senator Lena Gonzalez, the author of SB 1131 , to remove problematic provisions from the bill that would have significantly expanded the scope of practice for physician assistants, by allowing them to independently bill in the Medi-Cal program.
CMA supported a number of public health measures this year. CMA worked with the California Attorney General on AB 3128 (WOOD) to close loopholes to the flavored tobacco ban that tobacco companies were exploiting.
We worked closely with Asssemblymember Hart’s office on AB 1866 , which requires oil companies to accelerate the plugging and cleanup of idle wells, which pose health and safety threats to the surrounding communities.
CMA sponsored SB 963 (ASHBY), which requires emergency departments to deploy anonymous identification systems to help health care workers intervene and provide resources to victims of domestic violence and human trafficking in a safe, confidential and timely manner. Signed into law by the governor, SB 963 will allow emergency room staff to connect victims of trafficking to services and break the cycle of abuse.
CMA also successfully defeated SB 1250 (NGUYEN), which threatened to undermine the effectiveness of California’s newborn genetic screening program. The bill aimed to transition the program from a patient opt-out to an opt-in system. Requiring parents to proactively opt in to the program would have risked a significant decline in participation, hampering research and other scientific efforts. Such a shift would have jeopardized the early detection of life-threatening genetic conditions in newborns, leaving countless infants vulnerable. CMA preserved the integrity of this vital screening program, ensuring that it continues to safeguard the health and well-being of California’s youngest patients.


Governor Gavin Newsom signed CMA-sponsored AB 977 (RODRIGUEZ) to protect health care workers while at work in emergency departments. Previously, assaults against health care workers inside an emergency department carried lesser penalties than assaults committed outside an emergency department. AB 977 will ensure that health care workers are not treated differently simply because they work in a hospital emergency department.
Another important bill CMA successfully sponsored was AB 2164 (BERMAN), which prohibits physician licensure applications from requiring the disclosure of personal medical information that does not impact their ability to practice medicine, helping reduce the stigma around mental health support for physicians.
CMA successfully stopped AB 2960 (LEE), which sought to legislate the practice of medicine by mandating yearly syphilis testing in all primary care clinics and hospital emergency departments for every sexually active patient aged 15 and older, whether it was clinically indicated or not. While the bill may have been well-intentioned, it posed a significant overreach by interfering with the trusted relationship between physicians and their patients and would have unnecessarily raised the cost of care.
Unfortunately, one bill CMA opposed, SB 607 (PORTANTINO) did pass and was signed by the governor. Current law requires physician to have discussions with minor patients for whom they are prescribing opioids about the risks of addiction and overdose associated with such drugs. This bill extends that requirement to all patients. CMA is currently working on potential clean up language centered around liability and the administrative burden this expanded requirement creates.
+ 2,124 bills introduced in the State Legislature. CMA tracked 537 (25%)
+ 400 members attended CMA’s 50th Annual Legislative Advocacy Day with 88 legislative offices visited.
+ 3300+ grassroots messages sent by members to their legislators on CMA priority issues.
+ 4 sponsored bills signed into law.
+ 115 supported bills signed into law.
+ 24 opposed bills stopped.
+ 23 problematic bills successfully amended.
+ 3 dangerous bills to expand non-physician scope stopped.
+ 5 California physicians elected to state and federal office.

+ 88% of CALPAC-supported candidates were successful in their election bids.
For more details on may of the key bills that CMA was involved with in 2024, visit cmadocs.org/legwrap24.
Doctors Hospital of Manteca Announces New CEO
Tina Burch, RN, MSN, is the new Chief Executive Officer (CEO) of Doctors Hospital of Manteca (DHM) after being confirmed by the hospital’s Governing Board today.

Burch, RN, MSN
“Tina has been an asset to DHM for over 33 years and her work in supporting CEO duties during my interim role made it clear that she is the best person for this position,” said Jay Krishnaswamy, CEO for Central Valley Doctors Health System (CVDHS).
Krishnaswamy has been interim CEO, in addition to being CEO of CVDHS and Doctors Medical Center in Modesto, since January of this year.
“It is an honor to take on this role at Doctors Hospital of Manteca,” said Ms. Burch. “I am grateful and enthused for the opportunity to continue to serve the community as a leader at DHM, and to enhance the quality, compassionate care that DHM provides. I love being a part of this community and all the great work of the DHM team.”
Ms. Burch will continue to serve as Chief Nursing Officer,
Providing staff, physicians, and patients with relevant & up to date information
which she has done since May 2021. She previously served as Director of Clinical Quality Improvement/Patient Safety before moving into Administration. Ms. Burch began her nursing career with DHM in 1991 and her roles have included Critical Care Services Director, Sepsis/ Stroke/Dialysis Coordinator, and Clinical Manager of Inpatient Nursing Services.
Ms. Burch earned a Bachelor of Science in Nursing from California State University at Stanislaus and a Master of Science in Nursing from Grand Canyon University. Her honors over the years include Employee of the Year and Tenet Hero.
Doctors Hospital of Manteca and San Joaquin County Conduct Full-Scale Drill for Hypothetical Chemical Attack or Incident
Doctors Hospital of Manteca, part of Central Valley Doctors Health System, and San Joaquin County

conducted a full-scale exercise for a hypothetical chemical attack, such as in Japan in the 1990s, in the week leading up to Labor Day. While volunteer actors pretended to be part of a nerve agent exposure, possibly as part of a terrorist attack, physicians, nurses and County officials drilled on processes for patient treatment, including CHEMPACK antidote deployment, as well as staff and public safety. Six different television stations from Sacramento ran 17 segments that educated 346,168 viewers in English and Spanish.

Along with the newly renovated Emergency Department (ED) and new flooring throughout, visitors to Doctors Hospital of Manteca will notice new signs that increase visibility of the location and directions to the ED entrance. The signs are the most visible parts of what is an overall investment by Tenet Health into Doctors Hospital of Manteca to advance with the communities it serves.
Health Lodi Memorial Named Surgery Center of Excellence for Robotic Surgery, Orthopedic Surgery, Minimally Invasive Surgery, and Gynecology
Adventist Health Lodi Memorial has recently been accredited as a Surgery Center of Excellence in Robotic Surgery, Orthopedic Surgery, Minimally Invasive Surgery and Gynecology by the Surgical Review Corporation (SRC). This prestigious recognition underscores the hospital’s commitment to delivering high-quality surgical care and its dedication to utilizing the most advanced technologies and surgical techniques.
These accreditations highlight the exceptional skill
of the surgical team and the comprehensive, patientcentered approach at Adventist Health Lodi Memorial, which ensure the highest standards of safety and patient outcomes for the San Joaquin community.

On October 31, 2024, the Lodi Memorial Hospital Foundation completed a purchase of the Lodi Outpatient Surgery Center and donated it to Adventist Health Lodi Memorial hospital. The hospital has leased the 9,000 square-foot facility for years from the ownership group, consisting of several physicians. The center was developed in 1984 by a group of physicians whose practices were impacted when the hospital operating room schedules became overwhelmed, so they decided to build an outpatient surgery facility, originally for their exclusive use. As the doctors retired, AHLM was eventually able to lease the entire facility for its own use.
Wayne Craig, President of the LMH Foundation, stated, “ For years we have purchased critical medical equipment for the hospital to expand services or update to the latest technology, but when this opportunity came up, and after consulting with the hospital, our Board determined this would be an excellent way to support expansion of surgical services in the community and give the hospital full ownership to not only save leasing costs, but more importantly to give them the opportunity to develop and use the facility to meet future care demands.”
Currently, nearly 7000 surgeries are performed each year at AHLM. The Lodi Outpatient Surgery Center will add capacity to significantly increase total surgeries, reduce elective surgery wait times and expand services lines,
In his 34 years at St. Joseph’s, President and CEO Donald J. Wiley has played an instrumental role in the opening of the Heart Center, the Patient Pavilion, launch of our Graduate Medical Education program, groundbreaking partnership with Kaiser Permanente, and expansion of the Neonatal Intensive Care Unit and Emergency Room spaces.





Together with St. Joseph’s Foundation of San Joaquin, St. Joseph’s has brought a new Linear Accelerator to the Medical Center, expanded specialized care, and earned national recognition for our commitment to patient care and safety.
Thank you, Don, for being a trailblazer in improving the health of the San Joaquin community - congratulations on your retirement!









beginning with Gastroenterology in 2025. “We continue to be blessed by the Lodi Memorial Hospital Foundation, and their loyal donors, who make it possible to advance our hospital and to continually improve healthcare in our community,” said Brooke McCollough, AHLM President. “We are grateful for their legacy of commitment to the community by raising over $20 million for the hospital since 2008.”
Chief of Surgery, Dr. Kevin Hilton, stated, “We are grateful that AHLM continuously upgrades to the latest surgical technology that enables us to provide the best care for our patients, resulting in better outcomes and, often, quicker recoveries.”
Adventist Health Lodi Memorial to be the first hospital in Northern California to receive the da Vinci 5 Robotic Surgical System
Adventist Health Lodi Memorial will be the first hospital in San Joaquin County and surrounding Northern California areas to acquire the latest da Vinci 5 Robotic Surgical System.
Slated to arrive before end of year, the da Vinci 5 was approved by the U.S. Food and Drug Administration in March 2024 and was developed by Intuitive, a global leader in minimally invasive care and the pioneer of robotic surgery.
Adventist Health Lodi Memorial is excited to be able to provide this state-of-the-art robotic surgery technology to the community. The da Vinci 5 system will complement the hospital’s current da Vinci Xi system, which has been in use for nearly ten years. The Lodi Memorial Hospital Foundation played in integral role in the purchase of this state-of-the-art robotic system.
With additional upgrades and enhancements to the already well-established robotic platform, da Vinci 5 has the potential to continue expanding access for patients, as well as to improve outcomes. The system will also help make surgery more efficient for care teams that include physicians and hospital staff. Da Vinci 5 enhancements include:
Improved accuracy and precision: Da Vinci 5’s design and engineering enhancements, including new surgeon
controllers and powerful vibration and tremor controls, make it the smoothest and most precise system Intuitive has developed to date.
First-of-its-kind force-sensing technology: In preclinical trials with surgeons at all experience levels, da Vinci’s Force Feedback technology demonstrated up to 43 percent less force exerted on tissue, which may result to less trauma on tissue. This may also translate to quicker recovery times.
Expanded computing power and advanced data capabilities: Da Vinci 5 has more than 10,000 times the computing power of da Vinci Xi. This enables innovative new system capabilities and advanced digital experiences, including integration with Intuitive’s My Intuitive app, SimNow (virtual reality simulator), Case Insights (computational observer) and Intuitive Hub (edge computing system).
Lodi Memorial is accredited as a Surgery Center of Excellence in Robotic Surgery by the Surgical Review Corporation (SRC). An accreditation of this level indicates that Adventist Health Lodi Memorial’s Robotics program excels at patient safety, fewer complications, and overall improvement of patient outcomes. SRC accredits the top hospitals and ambulatory surgical centers in the world, and this reaffirms the excellence of the hospital’s program. While there are a number of trained robotics surgeons across the General Surgery and OB/GYN specialties using Adventist Health Lodi Memorial’s current system, surgeons actively participating in their Robotic Surgery Center of Excellence program include Dr. Param Gill, Dr. Sukhmine Nedopil, Dr. Tarig Samarkandy, and Dr. John Lee.
Adventist Health Lodi Memorial anticipates that the da Vinci System 5 will provide the hospital with the capacity to perform an additional 400 robotic surgical cases annually. Running both systems concurrently will help Lodi Memorial significantly increase their overall surgical case volume for consistent organizational growth and financial stability.
Adventist Health Lodi Memorial and the Lodi Memorial Hospital Foundation are thrilled for this important investment in the community that will give residents access to the highest levels of surgical excellence right here in San Joaquin County.
St. Joseph’s Medical Center Achieves Seven Specialty Care Honors From Healthgrades
Dignity Health St. Joseph’s Medical Center has achieved numerous accolades for clinical excellence from Healthgrades, the #1 site Americans use when searching for a doctor or hospital. Among St. Joseph’s Medical Center’s distinctions are two Specialty Excellence Awards, placing the hospital among the nation’s top 10% for Coronary Interventional Procedures and Critical Care. SJMC was also rated five stars for five services, including Coronary Interventional Procedures, Chronic Obstructive Pulmonary Disease, Treatment of Bowel Obstruction, Treatment for Sepsis, and Treatment of Pulmonary Embolism.
“We are especially proud of this year’s specialty recognitions, which exemplify St. Joseph’s commitment to high quality care and dedication to the health of the San Joaquin community,” said Donald J. Wiley, President and CEO, St. Joseph’s Medical Center. “In addition to being placed among the top 10% of hospitals nationwide for clinical performance, these specialty recognitions place us in an elite group that provides nationally-ranked care in areas such as Cardiology and Critical Care.”
St. Joseph’s Medical Center Holds Blessing of the Rigs for
Dignity Health St. Joseph’s Medical Center held their third annual Blessing of the Rigs & Responders event on Monday, October 28th, in recognition of National First Responders Day. SJMC offered a county-wide invitation to all city and county fire, police, sheriff and highway patrol departments, and county ambulance companies to attend. Festivities entailed an interfaith blessing of vehicles
Providing staff, physicians, and patients with relevant & up to date information

and first responders, which also included specialty units and motorcycles.
Nearly 90 first responders attended, with Chaplains from the Spiritual Services Department performing the blessings for the first responders and their respective rigs. In addition to the blessing, each first responder received lunch and a token to show appreciation from SJMC, in addition to having the opportunity to enter a raffle, with prizes donated by local businesses.
Through the power of philanthropy, St. Joseph’s Foundation of San Joaquin brought a Trios Surgical Table to St. Joseph’s Medical Center, advancing care for local spine surgery patients. The table allows for enhanced patient positioning, support, and stabilization. St. Joseph’s performs over 275 spinal surgeries each year, and through increased technology such as the Trios Surgical Table, those needing advanced operations are able to stay local


UC Davis Health is an extraordinary place to grow your career. You’ll experience being part of an academic medical center that’s committed to advancing pioneering research, promoting a sense of belonging through an inclusive work environment, and fostering continuous learning to develop health care leaders.

Join our team as we strive to provide world-class care in the Northern California region. Offering a competitive compensation and benefits package, flexible schedules, access to wellness programs, and more.
for both surgery and recovery.
“It allows us to do advanced surgeries at St. Joseph’s,” said Dr. Gary Alegre, Orthopedic Spine Surgeon. “If [we] didn’t have it, those surgeries wouldn’t happen at all. It’s an essential everyday item.”
Kaiser Permanente’s Medicare Health Plan in California Tied for Highest Rating in the State
Kaiser Permanente’s Medicare health plan in California is rated among the best in the state for providing highquality, seamless care, and outstanding service to its 1.4 million Medicare Advantage members.
This year, the Kaiser Permanente Medicare health plan in California received 4.5 out of 5 stars, according to the Centers for Medicare & Medicaid Services (CMS) 2025 Star Ratings. In addition, the Kaiser Permanente Medicare health plan in California is tied for the highest star rating in the state.
Providing staff, physicians, and patients with relevant & up to date information
“These ratings demonstrate our commitment to providing high-quality care and exceptional service to all of our Northern California members, including our Medicare Advantage members,” said Carrie Owen Plietz, FACHE, president of Kaiser Permanente’s Northern California region. “Kaiser Permanente is routinely recognized as being among the nation’s best for improving the health and well-being of our members and patients.”
The Kaiser Permanente Medicare health plan in California has been highly rated – with mostly 4.5 and 5-star ratings – for the past 15 years.
“Our clinicians work together across all specialties to ensure personalized, high-quality care for our patients,” said Maria Ansari, MD, FACC, CEO and executive director of The Permanente Medical Group. “The CMS Star Ratings, along with our nation-leading NCQA ratings, demonstrate the commitment of our physicians and care teams to provide all of our patients with the exceptional and compassionate care they need to live long, healthy lives.”
Office space available now to be leased for medical/dental/medically relevant professional office. The space is 1367 square feet for immediate occupancy in the established Medical Doctor’s Complex, Weber Ranch Professional Park at East March Lane, with 7 rooms and waiting area. Call now (209) 951-8830.

















For over 100 years, San Joaquin General Hospital has been more than a place of healin g— it’s a lifeline to our communit y. From advancing medical education to unwavering compassion, our legacy reflects a deep commitment to every individual we serve. We remai n devoted to advancing medical excellence and fostering a healthier, stronger community for all of San Joaquin County.





















Palliative
Pediatric
California voters have overwhelmingly approved Proposition 35, a historic investment in Medi-Cal, which serves 15 million Californians.
“California voters have realized a once-in-a-generation opportunity to build a health care system that works for all Californians,” said Shannon Udovic-Constant, M.D., president of the California Medical Association (CMA). “For too long, equitable access to health care has trailed behind growing eligibility and benefits provided by MediCal.
“With the passage of Proposition 35, we are ensuring Medi-Cal receives the dedicated funding it needs to serve the millions of seniors, children, low-income families and people with disabilities in our state. Going forward we will be able to hire more physicians, first responders, paramedics and other health care workers to address the worker shortage and ensure Californians aren’t having to wait hours in the emergency room or months to get an appointment with a physician. And once the new law is implemented, doctors, hospitals, clinics and health centers will have much needed stability to serve the patients in their communities.
“This would not have been possible without the advocacy of our physician members and our more than 400 coalition partners. Our victory tonight is a testament to what we can
in resounding vote, expanding health care access for 15 Million Californians
accomplish when we come together to work for the thing that matters most: our patients. While there is much to celebrate, we realize this is just the beginning. CMA will continue to work with stakeholders and the state to realize the vision of Prop 35, and I am excited to move forward together.”

CMA co-chaired the coalition that put Proposition 35 before the voters in order to provide a dedicated, ongoing source of funding to increase access to health care. The passage of Prop 35 is particularly important to improve access to health care for the nearly 15 million Californians, including half of the state’s children, who are covered by Medi-Cal. Prop 35 also will grow the health care workforce in California, which will improve access to care for all Californians.






















BY JO ANN KIRBY
The San Joaquin Medical society is celebrating its 150th anniversary! It’s hard to imagine what it was like practicing medicine in San Joaquin County when the San Joaquin Medical Society, with a charter from the California Medical Association, was formed for the betterment of the area’s fledgling medical community. At the time, the Southern Pacific Railroad had just launched, the Gold Rush was winding down, and the area’s economy was fueled by agriculture and manufacturing.
In 1874, the county was already home to San Joaquin General Hospital and Stockton State Hospital, California' s first psychiatric hospital. Most businesses, including doctor ' s offices and drugstores, could be found on Center Street. At the time, diseases such as tuberculosis were prevalent. Physicians were beginning to embrace the importance of hygiene to stem infection and stop the spread of diseases. The field of osteopathy was developed that year. As the CMA encouraged county societies to form,
IN 1874, THE COUNTY WAS ALREADY HOME TO SAN JOAQUIN GENERAL HOSPITAL AND STOCKTON STATE HOSPITAL, CALIFORNIA›S FIRST PSYCHIATRIC HOSPITAL.




they began offering medical malpractice insurance to member physicians. Across the state, members would form the first disciplinary and licensing terms, build medical schools and publish the state ' s first annual medical journal, which would become a monthly publication in 1901.
San Joaquin Medical Society ' s oldest living past president, Dr. Earl Taylor says he imagined the pioneer doctors found membership to serve practical and social purposes, as he did many years later when he joined.
Dr. Taylor, a surgeon who is

DR. TAYLOR, A SURGEON WHO IS STILL ASSISTING IN THE OPERATING ROOM, FOUND MEMBERSHIP USEFUL IN INTRODUCING HIMSELF TO COLLEAGUES IN THE PROFESSION WHEN HE JOINED IN 1967.
still assisting in the operating room, found membership useful in introducing himself to colleagues in the profession when he joined in 1967. " If you were new, networking was so important. You wanted to let everyone know you were here and accepting referrals. You had a chance to meet, chit chat, drink and have some congeniality," he said. " We met every month or every other month back then."
“The primary mission of the San Joaquin Medical Society ' s that has remained unchanged over the years is to promote the science and



TOP: Richelle Marasigan, DO, Thomas McKenzie, MD, Robert Lawrence, MD, Jasbir Gill, MD, Raissa Hill, DO
MIDDLE: John Zeiter, MD, Patricia Hatton, MD, George Khoury, MD, Cyrus Buhari, DO, Shale Imeson, MD, Hyma Jasti, MD, Kwabena Adubofour, MD
BOTTOM: Lawrence Frank, MD, Jack Funamura, MD, Ramin Manshadi, MD, James Halderman, MD, Robin Wong, MD, Earl Taylor, MD, Hosahalli Padmesh, MD, Jack Gilliland, MD
NOT PICTURED: Peter Salamon, MD, Gerald Bock, MD, F. Karl Gregorius, MD, Patrick Synder, MD, Sandon K. Saffier, MD, John Olowoyeye, MD, Dale Bishop, MD, Marvin Singleton, MD, Javad Jamshidi, MD, Raghunath Reddy, MD, and R. Grant Mellor, MD
art of medicine. SJMS is committed to protecting public health and supporting physicians in delivering high-quality care while advocating for community health needs,” Lisa Richmond, executive director of SJMS, said. “This mission emphasizes professional development and ethical practice. By upholding this mission, SJMS remains a vital resource for physicians, fostering collaboration and advocacy in a changing healthcare landscape.”
The SJMS formed a Women’s Auxiliary in 1931 to welcome families of physicians. Known in more recent years as the Alliance, the group helped ease the transition into San Joaquin County life for doctors’ families who were new to the area. They offered tips on the best neighborhoods, schools, and most importantly offered friendship. Today, the Alliance is open to the families of physicians, residents in training and medical students. The Auxiliary was deeply involved in helping the community. During World
War II, members collected used clothing, fundraised and knitted for the Red Cross. In the 1960s and 70s, they collected used medical equipment and sample drugs for charity and became involved in health education. In 1972, they even presented San Joaquin General Hospital with a dialysis machine. Physicians could depend on the SJMS to help them with a variety of practical issues. The Bureau of Medical Economics was launched in 1953 to offer practical services including billing, an answering service and even pager rentals. There was even a travel service. In keeping with its mission, members were crucial in helping form what was the county’s first blood bank in the late 1950s with two members joining the blood bank’s first board of directors. The Scholarship Loan Fund was formed in the 1960s to assist medical students with loans, and was later expanded to include nurses, nurse practitioners and physician assistants.



SJMS could always be counted on to inform its members about issues that impacted them such as the malpractice insurance crisis in 1975, health care reform in the mid-1990s and later the Affordable Care Act. The SJMS opened its office in Brookside in 1995, where it remains and where it hosts its board meetings.
Decision Medicine, a hugely successful program, began in 2001 to encourage rising high school students to pursue an education in medicine. DM continues to grow and Bridge to Medicine, which added mentoring for high school and college students, began in 2018. Both programs are efforts to grow local physicians who come back and serve in San Joaquin County’s underserved communities, which desperately need medical professionals.
As the medical landscape changes, the SJMS steps up to challenge. “The medical society has adapted to the evolving landscape of medicine, particularly in response to the corporatization of healthcare, by implementing initiatives to support its diverse membership,” Richmond said. “Recognizing the distinct challenges faced by solo/small practitioners versus large medical groups, SJMS offers tailored benefits like leadership and professional development, networking and educational opportunities as well as member discounts and payor assistance.” Through the larger network of the California Medical Association, SJMS actively represents the interests of organized medicine at both the local and state levels, ensuring that the voices of all modes of practice are heard in policy discussions.
Dr. Bangalore says the society’s longevity can also be attributed to the fact that physicians still want to get together, share their thoughts and come to consensus. It continues to provide networking opportunities. The society maintains a membership directory, which it distributes to members and sells to businesses and organizations. It honors members with an event celebrating Young Physician and Lifetime Achievement Award recipients, as well as an annual holiday party.
Today, the society is leading the effort to connect with young students and help them pursue an education in medicine while encouraging them to come back and launch careers in their hometowns.
“THE ONLY WAY THINGS CAN CHANGE IN MEDICINE IS TO BE PART OF A PLATFORM THAT HELPS YOU TO DO THAT.”
- DR. NEELESH BANGALORE
“SJMS is committed to addressing the physician shortage by developing local talent through pipeline programs like Decision Medicine and Bridge to Medicine, which encourages students to pursue medical careers and return to their communities,” Richmond said. “Additionally, with the growth of local graduate medical education programs, SJMS is focused on retaining residents to practice in the area.”
This year, it held its first job fair, providing medical residents with the opportunity to network with peers and regional employers. Around 30 residents signed up for the event where they enjoyed drinks, appetizers, conversation and introductions to local employers.

Dr. Neelesh Bangalore, president of the SJMS board of directors, says membership in the SJMS and CMA is relevant and can be transformative.
“The only way things can change in medicine is to be part of a platform that helps you to do that,” the oncologist said. “SJMS tries to be current in terms of understanding the local, regional and national issues that look out for both doctors and their patients.”
Dr. Bangalore encourages membership in the SJMS for a successful future. “I have to congratulate the management team at SJMS. They are always aware of all the current issues we face,” he said. Through active advocacy, he said, physicians are able to practice in a less stressful environment and take care of their patients.
Members will get to celebrate the society’s success at Cheers to 150 Years! The gala celebration will take place December 12 at the Stockton Golf & Country Club. It will be an enchanting evening featuring a strolling magician, photo booth and more.

The California Medical Association (CMA) recently convened its 153rd annual House of Delegates (HOD) meeting in Sacramento. More than 800 California physicians and medical students gathered to debate and establish broad policy on current major issues that have been determined to be the most important issues affecting members, the association and the practice of medicine.
The association also installed its new officers, including new CMA President Shannon UdovicConstant, M.D., a board-certified general pediatrician practicing in San Francisco. The major issues the delegates focused on this year were:
Maternal Health Equity, Obstetric Deserts and Reproductive Health: California is facing an alarming and accelerating trend of hospital maternity ward closures. These
closures come as California is dealing with a maternal mortality crisis, with pregnancyrelated deaths reaching a 10-year high in 2020. CMA’s physician delegates set policies related to maternal health equity, specifically areas such as maternal mental health, the OB-GYN workforce, and support for struggling hospitals in rural and underserved communities.
Rural Health: There are perennial concerns about access to care and health disparities that exist for rural communities, yet CMA had little policy specific to strengthening rural health care infrastructure. CMA delegates set policy to address gaps in existing CMA policy, with a focus on developing a workforce specially trained to practice in rural communities, bolstering financial resources available to rural health care providers, and safeguarding the services available to each community.
San Francisco pediatrician Shannon UdovicConstant, M.D., was installed as the new CMA president at the association’s annual House of Delegates in Sacramento.
Dr. Udovic-Constant – a passionate advocate for policies to improve the health of children and communities – addressed the hundreds of physician delegates and health care stakeholders, outlining her vision for the largest state medical association in the country representing more than 50,000 California doctors.
“I am invigorated to have the opportunity to advocate side by side with my physician colleagues to improve the medical profession and the health of our patients and communities,” said Dr. Udovic-Constant. “Physicians must be the architects of the future of health care, and CMA is positioned to lead the state in this evolution and provide a model for the country.”
Dr. Udovic-Constant is the 156th president of CMA and fifth woman to hold the position. She previously served as chair and vice chair of the CMA Board of Trustees. She is also a former President of the San Francisco Medical Society (now the San Francisco Marin Medical Society) and served on The Permanente Medical Group Board for 12 years.
Dr. Udovic-Constant has also been the chair of the CMA Political Action Committee (CALPAC) Independent Expenditure Committee and part of CMA’s Justice, Equity, Diversity and Inclusion Technical Advisory Committee (TAC) and Firearm Violence Prevention TAC. She has also served on CMA’s Council on Legislation and currently serves on the CMA delegation to the American Medical Association.



San Luis Obispo pediatrician René Bravo, M.D., was selected by the delegates as CMA president-elect. He will serve on the executive committee in that role for one year, and will be installed at the conclusion of next year’s annual meeting.
“The model of finding agreement from differences of opinion in order to meet the goals of a group is my guide, and it will help me as president of CMA serve the physicians of California,” said Dr. Bravo. “What strikes me most is what we can accomplish as doctors when we all agree to unify and work with shared purpose in crafting that common understanding. As physicians striving to improve health care for all Californians, our unity is our strength.”
Dr. Bravo is a primary care pediatrician who has been serving families and children on the Central Coast for 38 years. He is the founder and President of Bravo Pediatrics, a five-physician single specialty group practice where he was the managing partner before recently retiring.
Dr. Bravo is also past president of the San Luis Obispo County Medical Society (now the Central Coast Medical Association), where he also served on its Governing Board and chaired the Physician Wellness Committee for 10 years.
At CMA, he has served as District V Trustee and on the boards of CALPAC and the CMA Foundation (now Physicians for a Healthy California). He is a longtime delegate to the CMA House of Delegates, and has chaired many CMA committees in his 42 years of membership.
“I am honored to have been chosen as the new CMA president-elect. In this new role, I will represent all physicians and all practice modes with a focus on the real economic and personal needs of the physicians, all while prioritizing our patients,” said Dr. Bravo. “Our unity is our strength, and together we can strive to deliver the highest quality, science-based health care to all Californians.”
The full 2024-2025 CMA Executive Committee includes:

Shannon Udovic-Constant, M.D. President

Sergio R. Flores, M.D. Chair, Board of Trustees

Jack Chou, M.D. Speaker of the House

Tanya W. Spirtos, M.D. Immediate Past President

René Bravo, M.D. President-Elect

Eric Hansen, D.O. Vice-Chair, Board of Trustees

George Fouras, M.D. Vice-Speaker of the House
Read more about all of our CMA officers at cmadocs.org/executive-committee.









To view more pictures, visit our Flickr page: bit.ly/3OzxSCN
During the CMA House of Delegates, hundreds of physicians participated in a grassroots text bank reaching out to more than 1.1 million California voters about the importance of Prop 35. Grassroots efforts like this were integral to our landslide victory – with voters overwhelmingly approving an historic investment in Medi-Cal.
“California voters have realized a once-in-ageneration opportunity to build a health care system that works for all Californians," said CMA President Shannon Udovic-Constant, M.D. "For too long, equitable access to health care has trailed behind growing eligibility and benefits provided by Medi-Cal."
"With the passage of Proposition 35, we are ensuring Medi-Cal receives the dedicated funding it needs to serve the millions of seniors, children, low-income families and people with disabilities in our state. This would not have been possible without the advocacy of our physician members and our more than 400 coalition partners.
CMA co-chaired the coalition that put Prop 35 before the voters to provide a dedicated, ongoing source of funding to increase access to health care. The passage of Prop 35 is particularly important to improve access to health care for the nearly 15 million Californians, including half of the state’s children, who are covered by Medi-Cal. Prop 35 also will grow the health care workforce in California, which will improve access to care for all Californians.
Even though HOD might be over, there are plenty of ways to stay involved and advocate for your patients and your profession throughout the year. CMA and its county medical societies provide many avenues to get involved, including opportunities to volunteer; serve on a committee, council or board; and shape the future of the medical profession.
For more information, visit cmadocs.org/opportunities.




The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.
Dignity Health St. Joseph’s Medical Center recently graduated residents from its Anesthesia, Emergency Medicine, Family Medicine, and Internal Medicine Residency Programs. Among the graduates were four Anesthesia residents, who were part of an inaugural cohort split between two postgraduates from 2021. Additionally, St. Joseph’s Psychiatry Residency Program marked a milestone with one resident graduating early to pursue fellowship training in New England. Out of the 31 graduates, nine will continue their training in fellowships, with three remaining at St. Joseph’s for fellowships in Cardiology, Simulation, and Ultrasound. The other six graduates will complete fellowships in Child and Adolescent Psychiatry, Critical Care Medicine, Pediatric Anesthesia Critical Care Medicine, and Sports Medicine at various institutions. Twenty graduates will practice in California, including five who will remain locally and four in the Greater Sacramento Valley. St. Joseph’s is committed to retaining its residents to promote a healthier future for both the community and the Greater Central Valley. As one-chapter closes, another begins. St. Joseph’s values its trainees and recognizes the positive impact they have on the community-centered mission.



Ask us about our Forgivable Loan Program

Join a dynamic group of clinicians at one of Kaiser Permanente’s state-of-the-art facilities in California’s Central Valley and be part of our innovative team of physicians. A new, cutting-edge medical o ce building is coming in Spring 2026! Whether you're an experienced physician with extensive training and clinical expertise or a new clinician who is interested in receiving excellent on-the-job training and clinical support/mentorship, you will find all this and more with our team in the Central Valley and enjoy quality of living at its best. Work for one of the largest employers in the area and a leader in the health care industry!
Our Central Valley locations o er:
• State-of-the-art Robotic Surgery (DaVinci Xi Surgical Robot)
• Physician Leadership Academy to accelerate the development of our future emerging leaders
• 4.5 out of 5 stars for our CMS Medicare Stars Rating
• Joint Commission Accredited Primary Stroke Center
• Nationally Accredited Programs for Cancer Care:
- Commission on Cancer
- National Accreditation Program for Breast Centers
Extraordinary benefits:
• Competitive compensation and benefits package, including comprehensive vision, medical, and dental
• Interest Free Home Loan Program up to $250,000 (approval required)
• Relocation Assistance up to $10,000 (approval required)
• PSLF Eligible Employer
• Malpractice and Tail Insurance
• Life Insurance
• Optional Long-Term Care Insurance
• Paid holidays, sick leave, and education leave
• Shareholder track
• Three retirement plans, including a pension plan and 401(k)
A few reasons to consider a practice with TPMG:
• Unmatched practice support with opportunity for flexible schedules.
• We can focus on providing excellent patient care without managing overhead and billing. No RVUs!
• We demonstrate our commitment to a culture of equity, inclusion, and diversity by hiring physicians who reflect and celebrate the diversity of people and cultures. We practice in an environment with patients at the center and deliver culturally responsive and compassionate care to our member populations.
• Multi-specialty collaboration with a mission-driven integrated health care delivery model.
• An outstanding electronic medical record system that allows flexibility in patient management
• We have a very rich and comprehensive Physician Health & Wellness Program
• We are Physician-led and develop our own leaders.
• Professional development opportunities in teaching, research, mentorship, physician leadership, and community service.
To learn more about these opportunities, wage ranges, and to apply, please visit: https://northerncalifornia.permanente.org
For more information on our opportunities, please email TPMG-CVL-PhysicianRecruitment@kp.org or MDRecruitment.tpmg@kp.org

Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
December 11th, 2024: 11:00AM to 1:00PM
Join us for our annual Medicare Update workshop for physicians and office staff. This 2 hour seminar will cover relevant information about current, future and proposed changes for the coming year!
Cheryl Bradley- Associate Director of CMA’s Center for Economic Services

March 12th, 2025: 11:00AM to 1:00PM “2025
Discover how to navigate complex employment law changes and stay on track for a successful year. This will help businesses navigate California’s challenging employment and labor laws.
Jamie Bossuat, a shareholder and employment lawyer at Kroloff will present an update on the most pressing issues in employment law and will offer practical suggestions for reducing liability. Issues will include recent changes in wage and hour requirements, updates to leave of absence laws, and current litigation trends.
Medi-Cal Rx to reinstate prior auth requirements for pediatric claims
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
In March 2022, the California Department of Health Care Services (DHCS) suspended MediCal Rx prior auth requirements to ensure patients maintained timely access to pharmacy benefits. While previous phases of the Medi-Cal Rx transition plan restored prior auth requirements for patients 22 and older, claim edits and prior auth requirements remained suspended for all Medi-Cal Rx covered pharmacy claims for members 21 years of age and younger. Effective January 31, 2025, Medi-Cal Rx will reinstate claim edits and prior authorization requirements for patients 21 years of age and younger on January 31, 2025, as part of a planned “pediatric integration.”
As part of this pediatric integration, Medi-Cal Rx will also implement the California Children’s Services (CCS) Panel Authority policy, which will give certain CCS Panel Providers prescribing authority for a limited list of medications and supplies under a set of utilization management policies.
Recognizing the training and experience required by CCS Panel Providers to care for pediatric members with complex medical conditions, the CCS Panel Authority policy will apply to prior auth requests for select drugs, enteral nutrition products and medical supplies.
In January, Medi-Cal Rx will host weekly webinars about the pediatric integration to support stakeholder readiness.
Physicians have until December 31, 2024, to update their Medicare participation status for 2025, with any changes going into effect on January 1, 2025. This deadline is crucial for those reevaluating their participation due to the looming payment cuts reflected in the 2025 physician fee schedule announced by the Centers for Medicare and Medicaid Services.
Unless Congress intervenes, the 2025 physician fee schedule will cut Medicare physician payments by 2.8%. However, there is hope that Congress will act to prevent this cut by the end of the year. A bipartisan group of U.S. Representatives have introduced the Medicare Patient Access and Practice Stabilization Act of 2024 (HR 10073) to stabilize physician practices and improve patient access to care. The bill would stop the impending 2.8% Medicare physician payment cut in 2025 and provide a partial inflation update – 50% of the Medicare Economic Index for one year in 2025 – to help address inflationary increases in medical practice costs. Under HR 10073, the total Medicare physician payment increase for 2025 would be 4.73%.
As always, physicians have three choices regarding Medicare: Be a participating provider; be a nonparticipating provider; or opt out of Medicare entirely. Details on each of the three participations options are as follows:
A participating physician must accept Medicareallowed charges as payment in full for all Medicare patients. A participating provider receives 5% more reimbursement than a non-participating provider.

Medicare’s limiting charges do not apply to these contracts, but Medicare does specify that these contracts contain certain terms. When a physician enters into a private contract with a Medicare beneficiary, both the physician and patient agree not to bill Medicare for services provided under the contract. Validated opt-out affidavits automatically renew two years after the effective date.



Physicians who want to change their participation status for 2025 must submit a signed Medicare Participating Physician or Supplier Agreement (CMS-460) to Noridian, California’s Medicare contractor, postmarked by December 31, 2024. While participation agreements will automatically renew each year, you will need to complete a new participation agreement if there is a name or EIN (tax identification number) change.

Stockton 11/26
Ripon 12/2
Manteca 12/3
Escalon 12/3
Lodi 12/5
Rio Vista 12/7
Lockeford 12/7
Tracy 12/10
There is also information on physicians’ Medicare participation options in California Medical Association (CMA) health law library document #7209, “Medicare Participation (and Nonparticipation) Options.” Health law library documents are free to CMA members at cmadocs.org/health-law-library. Nonmembers can purchase documents for $3 per page.
Noridian is hosting a Provider Enrollment Basics and Overview webinar that will provide information about provider enrollment and how the process works. The free webinar will be Wednesday, December 11, at 11 am Pacific Time. Click here to register.







More information on open enrollment is also available on the Noridian website.
Questions? Contact CMA’s Medicare specialist Cheryl Bradley at (916) 551-2862 or cbradley@cmadocs.org.
























BY MAGGIE PARK, MD
Highly Pathogenic Avian Influenza (HPAI), caused by the H5N1subtype of the influenza A virus, was first detected in dairy herds in Texas in March 2024, subsequently spreading to multiple states. It began appearing in dairy farms in the Central Valley region of California in August. The response to this situation is being led at both the federal and state levels, with both human health and animal health sectors involved, including the Centers for Disease Control and Prevention (CDC), the California Department of Public Health (CDPH), the U.S. Department of Agriculture (USDA) and the California Department of Food and Agriculture (CDFA). San Joaquin County Public Health Services (PHS) is encouraging all healthcare providers to remain vigilant for signs and symptoms of possible H5N1 infections.
Also known as “bird flu”, HPAI is a contagious viral disease that is widespread in wild birds. It is transmitted from wild birds to other birds, domestic poultry, and mammals through direct or indirect contact with mucus, saliva, and feces. It is labeled “highly pathogenic” due to its severity in poultry, causing a fatal respiratory illness in chickens. The H5N1 strain has been around for over 25 years, mostly existing in wild birds as a reservoir, with wild birds being able to carry the disease while showing no signs of illness. In 1996-1997, infections in domestic waterfowl with H5N1 led to 860 human infections in China and Hong Kong, with a 50% death rate. The current circulating clade of H5N1, called clade 2.3.4.4b, had spillover from wild birds in North America and Eurasia to mammals such as foxes, skunks, bears, bobcats, and raccoons, starting in 2021.


In 2022-2023, the virus caused mass mortality in sea mammals, such as sea lions in Peru and elephant seals in Argentina. H5N1 clade 2.3.4.4b was first detected in the United States in 2022 in commercial and backyard poultry flocks, and infections in poultry have required the depopulation of entire flocks. Now, in 2024, the outbreak involves infected milking cows, posing an elevated risk to humans, especially those working on dairy farms, with transmission presumably occurring via direct contact with sick cows or raw cow milk.
Animal and human cases are being closely monitored, and the total number of outbreaks is continually updated. As of the week of November 18, the numbers are as follows:
• 549 dairy herds across 15 states have confirmed outbreaks
• 1,219 poultry flocks (commercial and backyard) with outbreaks in 49 states, affecting 108 million birds
• 336 affected dairies in California
• 53 human cases in the United States in 2024, 27 from California
• 10,604 wild bird detections across 51 jurisdictions in the U.S.
• 1 commercial poultry flock, no dairies and no human cases in San Joaquin County thus far. H5N1 detections have occurred in San Joaquin County wastewater.
The risk to the general public remains low at this time. Farmworkers who interact with dairy cows or poultry, or who handle raw dairy products, as well as wildlife workers, have
a greater risk of infection. There has been no detection of person-to-person spread. The consumption of pasteurized milk and dairy products is considered to be safe, as pasteurization inactivates the virus.
Clinical manifestations of influenza A (H5N1) clade 2.3.4.4b in humans can range from asymptomatic to severe. Symptoms may include:
• Eye redness or discharge
• Fever, Chills
• Cough
• Sore throat
• Runny or stuffy nose
• Diarrhea and/or vomiting
• Muscle or body aches
• Fatigue
• Trouble breathing
• Seizures
All human influenza A (H5N1) cases reported in the U.S. to date have had mild illness, with many limited to conjunctivitis only. All have been treated with oseltamivir (Tamiflu), and the CDC has issued EUI (Emergency Use Instructions) for the use of oseltamivir to decrease severity of illness.
PHS is encouraging the public to avoid being in proximity to sick and dead animals and avoid consuming raw milk and related raw dairy products. The public is also advised to avoid touching surfaces or materials contaminated with saliva, mucous, or animal feces from wild or domestic birds or other animals with confirmed or suspected bird flu virus.
With 72 dairy farms, San Joaquin County has been identified as one of the top 10 counties in California at risk for H5N1, and PHS has accepted 400 influenza vaccine doses to be specifically administered to at-risk farmworkers. Although the seasonal flu vaccine does not offer protection against H5N1, the goal is to keep workers healthy, decrease the risk of being infected with
both H5N1 and seasonal flu at the same time, and decrease the burden on the healthcare system during respiratory virus season.
Dairy and poultry farm operators can order and receive PPE (personal protective equipment) at no cost from CDPH. This includes hundreds of N95 masks, gloves, face shields, goggles and bouffant caps that have been provided to local farms. PHS has created and distributed a flyer to farmworkers that teaches the proper donning and doffing of PPE. Our social media pages offer education to the public on H5N1 and safe dairy product consumption. As we reach out to farms through our flu vaccination efforts, are distributing informational packets in English and Spanish for employers and employees.
• Consider a diagnosis of HPAI in patients with relevant exposure history who are exhibiting signs or symptoms of acute respiratory illness or conjunctivitis
• Collect clinical specimens as soon as possible: a nasopharyngeal swab and a nasal swab combined with an oropharyngeal swab; include a conjunctival swab if the patient has conjunctivitis
• Start oseltamivir early, within 48 hours of symptom onset. Do not delay while awaiting test results
• Offer oseltamivir to close contacts of symptomatic confirmed cases according to risk of exposure
• Notify SJCPHS Disease Control and Prevention Program of any suspect cases by calling (209)468-3822. Testing of specimens for H5N1 should be done in the public health laboratory.
CDC H5 Bird Flu Current Situation https://www.cdc.gov/bird-flu/situation-summary/
CDC HPAI Interim Recommendations for Clinicians https://www.cdc.gov/bird-flu/prevention/hpai-interim-recommendations.html
USDA Detections of Highly Pathogenic Avian Influenza https://www.aphis.usda.gov/livestock-poultry-disease/avian/avian-influenza/hpaidetections
CDPH Bird Flu page https://www.cdph.ca.gov/Programs/CID/DCDC/pages/Bird-Flu.aspx Emergency Use Instructions for Oseltamivir https://www.cdc.gov/bird-flu/hcp/emergency-use-oseltamivir/index. html#:~:text=What%20to%20know,A%20viruses%20with%20pandemic%20 potential.
Heart & Vascular Institute
Designated heart attack and stroke receiving center
Cancer Institute
San Joaquin County’s only nationally accredited cancer center
Orthopedic & Spine Center
Certification of distinction for total hip and knee replacement from the Joint Commission
.












BY CYRUS BUHARI, DO
On September 24th, 2024 Richard (Rip) Waters passed away at his home after a normal day’s work. We shared so many similarities having grown up in Stockton and returned with our families to practice in our home community.
I came to know him best when St. Joseph’s Medical Center established the (Transcatheter Aortic Valve Replacement) TAVR program. Jim Morrissey, Amod Tendulkar, Joanne Marks, April Randall, and the two of us were tasked with bringing this new procedure and technology. Over a period of several months Rip and I traveled to Munich, Germany as well as several other cities in the US to get our training and certification. We became friends in addition to being colleagues. Our first TAVR was performed on the father of one of my childhood friends in June of 2016.
From then on, every Thursday morning for the past 8 years prior to his death (with some exceptions for vacations or meetings that interfered) we would sit together in a room of cardiac surgeons, cardiologists, nurses, trainees, and medical device company technicians discussing patients and then getting up to go perform the TAVRs. Besides Jim Morrissey and Joanne Marks, many of the other members of the team have left and new ones have come onboard. We were the only constants; there together every Thursday… Our TAVR day. I tended to be the more jovial, yet technical one in the group and he was always steady-handed and thoughtful in his approach. He was very cerebral in his deliberations about each patient and the best course forward for them. His approach was always methodical, leaving as little to chance as possible. On rare occasions all the planning, thought,

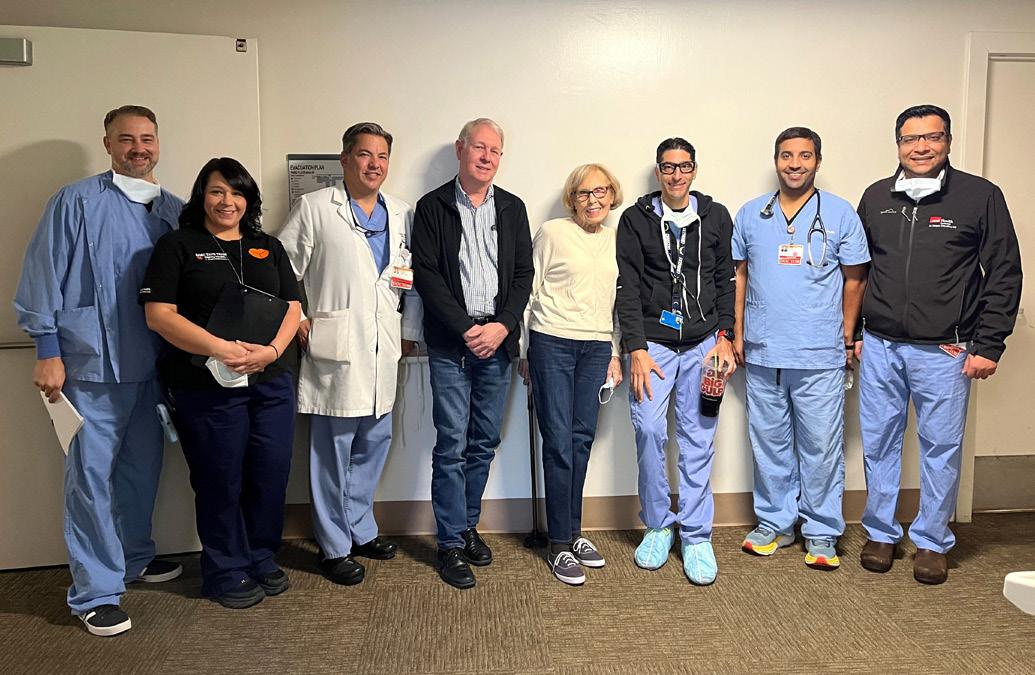
and technical success would not be enough, and patients would not make it. Each death or complication affected all of us, but we moved forward learning lessons along the way. When discussions were finished regarding patients, we would talk about our wives and our children. Ella and Reed were older than my boys so I would bounce parenting ideas off him, and he would get my opinion on things related to his kids. Although we laughed and smiled about many things in every discussion, he was never happier than when he would talk about his family. I listened attentively to his stories about college tours, and which places his kids liked best. He always made the most of any vacation or time off of work. He enjoyed his travels with his family and couldn’t stop telling us about the planning or how it was when he got back. To me, a hike in the Grand Canyon sounded like torture, but he was so excited about the opportunity.
The TAVR program and its success was personal for both of us, and it consumed much of our time. However, we both were also engaged in other programs in our community’s healthcare. He was Chair of the Cardiovascular Department at St. Joseph’s and served on the Medical Executive Committee. All things cardiology flowed through him in Stockton, and he was excellent as a leader. He was a member of the Board of Directors for the San Joaquin Medical Society’s Scholarship Loan Fund. He had been a beneficiary of the fund and felt a desire to contribute back to the SLF and guide its improvement in such a way that it would encourage recipients to return and practice in San Joaquin County.
Anyone who ever served on any board or committee with him knew his approach to even the most unpleasant tasks was fair-minded, even-handed, and very well thought out. He never made rash decisions. Even in our group of cardiologists he never played favorites; and despite our close relationship, he never hesitated to tell me where I was wrong. (These were rare occasions of course). After his passing I began to realize how close we were and how outside of his own partners I was probably his closest friend at work.
His most recent exploit was driving to Boulder, Colorado in a fully packed Jeep with Reed. We were concerned about the strength of the car and the potential for needing to call a helicopter to rescue them both. We knew that Erica would be sweating bullets the entire time. Thankfully the Jeep made it, and the mission was a success. On September 24th we sat alone and talked about many things both work related, and family related. That night he passed away suddenly and unexpectedly.
Richard Waters was a great son, brother, husband, uncle, and father. He was all of that long before becoming a fixture of our medical community and an integral part of our community’s leadership. He will be always loved and sorely missed by his entire family. He was our colleague and partner at work and his voice and smile are missed every day. He is a role model to follow for all of us.
But above all of that for me… I will miss my friend Rip. We love you and have fun on your next adventure brother.
August 14, 1971 – September 24, 2024
We are heartbroken to announce the passing of Rip Waters on September 24th, 2024. Rip was born in Reno, NV to Richard and Joanne Waters. He is survived by his loving wife Erica, and their children Ella (20) and Reed (19). He is also survived by his mother, Joanne Waters, brothers Robert (Sara) Waters and Randall (Janée) Waters, sister-in-law Lindsay (Scott) Horner, nieces and nephews Tucker, Claire, Kellen, Isabella, Alexandre, Grant and Gavin, and parents-in-law, Leon and Denise Reed. He was preceded in death by his beloved father and namesake, Richard E. Waters.
Rip moved to Stockton, California as a toddler, and was always proud to call Stockton his hometown. He grew up in the neighborhood surrounding UOP, attending local public schools, and forging friendships that lasted a lifetime. He attended Amos Alonzo Stagg HS, where he served as student body president, and graduated as valedictorian of the Class of 1989.
Rip was a brilliant student, and continued his academic pursuits, seeking excellence at all times. He graduated from Stanford in 1993 with a BA in Economics. After college, he spent a year traveling and serving as a medical volunteer in Peru, then continued on to Vanderbilt Medical School, receiving his MD in 1998. He completed internal medicine residency at Johns Hopkins Hospital in 2001, and cardiovascular fellowship at Duke University Hospital in 2005.
After completing his training, he returned home to Stockton, where he sought to always provide outstanding cardiology care to the community. He joined Stockton Cardiology Medical Group in 2005 and was a partner there for the remainder of his career. He was a dedicated clinician and loved to hear every person’s story.
He also worked at St. Joseph’s Hospital, where he served in many leadership roles. He was most proud of being part of the structural heart team, which brought non-invasive heart valve replacement (TAVR) to Stockton.
Though Rip valued his job as a cardiologist, his most cherished and gifted roles were as a husband, father, son,
brother and friend. He met Erica on a rafting trip just prior to their first day at Vanderbilt and their love for one another grew alongside their knowledge. They were married in 2001 and pursued their dreams and goals together from that day on. Although Rip received many accolades throughout his career, he considered Ella and Reed his greatest achievements. He loved them fiercely and was proud of them always. Rip was a great son, big brother, and uncle. He valued family connections and traditions above all. Rip was a dedicated and loyal friend to so many. At every stage, he made a large group of friends whom he held close for the remainder of his life.

Rip was serious about his commitments, but when the work was done, he definitely knew how to have a good time. He loved to gather with family and friends, and always enjoyed sitting around a full table, preferably with a Giants game on in the background. He appreciated a great martini (or two) and would craft a cocktail for you with love and attention to detail. He was always happiest outdoors. He preferred outdoor meals and was a master of the grill. As the original Waterboy1, he loved to be in the water and was a talented swimmer and water polo player. He loved to waterski and later enjoyed driving the boat and teaching the kids to ski. Rip especially loved the mountains. He was an expert skier and an avid hiker. His ideal day was spent on the slopes with his favorite ski companions, Ella and Reed. Though it was far too short, Rip’s life was always full of love.
SJMS
THIS FALL! ...and even more on the way.
Nuvpreet Bhandal, MD
Orthopaedic Sports Medicine
815 S. Fairmont Ave
Lodi, CA 95240
University of Missouri- Kansas City, 2015
Darbi Invergo, DO
Neurological Surgery
2209 N. California Street
Stockton, CA 95204
Chicago College of Osteopathic Medicine, 2008
Hely Shah, MD
Hematology Oncology
2626 N California Street, Ste B

Stockton, CA 95204
University of Alberta Faculty of Medicine, 2018
Ravleen Grewal, MD
Hematology Oncology
2626 N California Street, Ste L
Stockton, CA 95204
Saba University School of Medicine, 2018



✓ Over 11 billion accounts have been compromised – Has yours?
✓ Is your phone bill higher than you would like? Does your phone system allow you to work from anywhere?
✓ Have you conducted you r Risk Assessment yet? Call Mark Williams @ 209-623-1023 or email mark@ce-technology.com
San Joaquin Medical Society
3031 W. March Lane, Suite 222W
Stockton, California 95219-6568
RETURN SERVICE REQUESTED
Health Plan is creating health equity by investing in programs that improve access to care for our members and people who qualify for Medi-Cal. Health Plan is engaging our contracted providers to increase capacity through our provider recruitment grants and expanding our healthcare workforce by partnering with local schools to support students who are interested in medical careers.
Health Plan recently awarded 36 students with $104,000 in scholarships through our Health Careers Scholarship Program. Congratulations to our future physicians, specialists, registered nurses, pharmacists, and mental health professionals!


In September, through a partnership with CSU Stanislaus - Stockton Campus, Health Plan celebrated our first cohort of Community Health Workers (CHW). The CHW benefit is part of California’s Advancing and Innovating Medi-Cal initiative. A CHW’s role is to provide important liaison services between providers and their patient’s and promote advocacy for timely, coordinated care. Through our training and recruitment grants, our community has added 30 newly trained CHW’s ready to join your practice!
Do You Have Staff Who Can Benefit From CHW Training?
Join one of the upcoming virtual information sessions:
Session 1: 5:00-6:00 pm
Session 2: 6:00-7:00 pm
English Wednesday, November 13 Tuesday, November 19
Spanish Thursday, November 14
Thursday, November 21
The next CHW program begins January 2025!
Zoom URL: https://csustan.zoom.us/ j/89662510213