

MEDICAL STUDENTS MARK PATH FOR YOUTH
STUDENT HEALTH EMPOWERMENT CONFERENCE INSPIRES THE FUTURE OF MEDICINE
11 days after appendectomy, tests for acute abdominal pain revealed a
retained object
left inside the patient.
Surgical miscounts are considered never events because they are usually preventable by following established procedures.
ProAssurance offers risk assessments designed to help practices minimize errors by establishing and evaluating safety procedures and communication protocols.
With reliable procedures in place, our insureds are more likely to reduce errors in their medical practice, avoid claims, and make claims more defensible if they do occur.




PRESIDENT Neelesh Bangalore, MD
PRESIDENT ELECT Sujeeth Punnam, MD
TREASURER Stephen Tsang, MD
BOARD MEMBERS Cyrus Buhari, DO, Maggie Park, MD, Alain Flores, MD, Manreet Basra, MD, Sanjeev Goswami, MD, Kinnari Parikh, MD, Bhagya Nakka, MD, Sunny Philip, MD, and Ripudaman Munjal, MD
MEDICAL SOCIETY STAFF
EXECUTIVE DIRECTOR Lisa Richmond
MEMBERSHIP COORDINATOR Jessica Peluso
COMMITTEE CHAIRPERSONS
CMA AFFAIRS COMMITTEE Larry Frank, MD
DECISION MEDICINE Kwabena Adubofour, MD
MEDICAL EDUCATION PROGRAMS Kelly Savage, MD
SCHOLARSHIP LOAN FUND Gregg Jongeward, PhD
CMA HOUSE OF DELEGATES REPRESENTATIVES
James R. Halderman, MD, Raissa Hill, DO
Richelle Marasigan, DO, Ramin Manshadi, MD
Philip Edington, MD , Sujeeth Punnam, MD
Sunny Philip, MD, Ripudaman Munjal, MD
Stephen Tsang, MD
SAN JOAQUIN PHYSICIAN MAGAZINE
EDITOR Lisa Richmond
EDITORIAL COMMITTEE Lisa Richmond, Neelesh Bangalore, MD
MANAGING EDITOR Lisa Richmond
CREATIVE DIRECTOR Sherry Lavone Design
CONTRIBUTING WRITERS Jo Ann Kirby, Neelesh Bangalore, MD, Ankeeta Saseetharran, MPH, Rosaelena Menendez, MPH
THE SAN JOAQUIN PHYSICIAN MAGAZINE is produced by the San Joaquin Medical Society
SUGGESTIONS, story ideas are welcome and will be reviewed by the Editorial Committee.
PLEASE DIRECT ALL INQUIRIES AND SUBMISSIONS TO:
San Joaquin Physician Magazine 3031 W. March Lane, Suite 222W Stockton, CA 95219
Phone: (209) 952-5299 Fax: (209) 952-5298
E-mail Address: lisa@sjcms.org
MEDICAL SOCIETY OFFICE HOURS:
Monday through Friday 8:30am-4:30pm
Closed for Lunch between 12pm-1pm




As the seasons change, there’s no better time to upgrade your ride! At Mercedes-Benz of Stockton, we have a wide selection of Vans and Mercedes-Benz SUVs perfect for all your spring adventures whether it’s a weekend getaway, a road trip, or simply cruising in style.
From the versatile Sprinter Van to the luxurious GLC, GLE, and GLS SUVs, we have the perfect vehicle to match your lifestyle.
Visit us today and drive into spring with sophistication and performance. Your next Mercedes-Benz is waiting!



STRONGER TOGETHER
Our close partnership with the California Medical Association (CMA) is one of the key reasons SJMS has been so successful in supporting our members and advancing the practice of medicine in our region. In 2024, this partnership was especially significant as we worked together to secure historic Medi-Cal funding through a successful ballot measure.
In this issue, you’ll find a summary of the many victories achieved by the CMA—and by you—over the past year. It was a landmark year in which Governor Newsom signed all of CMA’s priority bills into law. Overall, 115 CMA-supported bills were enacted, while dozens of others were either successfully opposed or amended to address concerns important to physicians.
Looking ahead, this year's focus will be the implementation of Prop 35 funding, which will increase Medi-Cal reimbursements for primary care, specialty care, behavioral health, and emergency department services. In addition, funding will support clinics, family planning, ground emergency transportation, graduate medical education, and workforce development. Other key priorities include improving the practice environment—such as reducing administrative burdens, reforming prior authorization, and addressing physician wellness. We will also continue to advocate for the ethical oversight of AI technologies used by health plans in physician practices.
We encourage you to get involved! Whether you’re interested in leadership, advocacy, governance, or supporting local students with an interest in medicine through our Decision Medicine or Bridge to Medicine pipeline programs, there’s a place for you to make a difference. Keep an eye out for an email this Spring with opportunities to nominate yourself or others for open positions on our Board of Directors and the CMA House of Delegates.
Also, don’t miss the chance to join your colleagues for the CMA’s 51st Legislative Advocacy Day on Wednesday, April 9, in Sacramento. This event will bring together more than 400 physician and medical student leaders from across specialties and practice settings. Attendees will have the opportunity to meet with legislators and discuss priority healthcare issues. Register online at www.cmadocs.org or contact Lisa@sjcms.org
Finally, I hope you enjoy this issue’s feature on the Stockton Health Empowerment Conference, a student-led initiative by UC Davis Medical School aimed at bridging the educational gap for high school and community college students in Stockton.
Best Wishes,

LISA RICHMOND






Celebrating 60 years of excellence and unwavering commitment to businesses and families in California’s Central Valley and East Bay communities




May 21, 1965.



Formed in Brentwood, CA, BAC first opened for business
Photos from left to right: Ron Berberian, President and Board Chairman; Dana Bockstahler, Board Vice Chairman and former CEO; Dante Tosetti, Chief Executive Officer; Jackie Verkuyl, Executive Vice President and Chief Operating Officer; Bill Trezza, Board Member and former CEO.
FRUSTRATIONS OF DEALING WITH INSURANCE COMPANIES

ABOUT THE AUTHOR
I have been practicing Hematology and Medical Oncology for 25 years. As a private practitioner it is becoming more and more difficult to do the best for our patients with the current insurance environment. Many insurance companies are making it very difficult for both practicing physicians and patients to provide and receive excellent medical care. Specifically, I am referring to denial of service and down-coding of physician charges.
DENIAL OF SERVICE
I am referring to the denial of service by various private for-profit insurance companies. The number of times we participate in peer-topeer discussions for denial of service has significantly increased over time. In very few cases denial is justified, however, in the majority of cases it is a medically appropriate need. In a few cases we do get approval but only after we spend a lot of time and energy discussing the situation with medical personnel at the insurance company. This contrasts with the patients who have Original Medicare as their primary insurance where such a problem does not exist.
The process of getting approval for a service is quite complicated. The most common example in oncology is a request for PET-CT imaging. Initially, when there is denial of coverage it is usually because of lack of information. After we provide additional information most often the service is still denied. At that point, there may be an option to do a peerto-peer call or it could be a flat denial without the option of an appeal. In the latter case we have filed complaints with the California Department of insurance. However, that has had limited success.
There are many factors that make the process complicated resulting in significant emotional and possibly financial stress for the patients.
Neelesh Bangalore, MD is the current president of the San Joaquin Medical Society and practices at Stockton Hematology Oncology Medical Group
First, insurance companies do not have the ability to customize. For example, in many of our cancer patients we request PET/CT imaging to stage malignancies because contrast enhanced CT imaging is unsafe due to chronic renal disease. In my experience, that factor has never been incorporated into the decision-making process. In the interest of time, I do get CT imaging without contrast just to meet the requirement of a prior “traditional imaging” request before PET-CT can be authorized. Clearly, it is a waste of time for the patient.
Second, the whole process is time-consuming and resource consuming. Once we receive a denial generally it means a peer-to-peer discussion. The process of getting to it is quite cumbersome. It is usually handled by a third party. Once a call is made my staff or I will have to mention the name of the patient, date of birth, name of the physician and reference number at least 2 times and most often 3 times before somebody is able to help us. It can take up to 15 minutes before anything meaningfully can happen. Out of frustration, many times we hang up the phone which is certainly not in the best interest of the patient. In this day and age of computerization and Apps I feel the process is still very archaic.
Third, many insurance companies have a requirement that every authorization request must go through the primary care physician. That causes significant delays. We do understand the need for centralization of care through the primary care physician. However, putting the burden of specialty care authorization request on the primary care physician is not fair to the primary care physician or the patient. It adds an extra step which is truly unnecessary.
Lastly, the share-of-cost and copayments for certain services are simply exorbitant. Even though the service is approved it is impossible for the patients to get the benefit because of inability to pay for such services. A good example would be an MRI scan, PET-CT scan or chemotherapy. It has caused significant financial stress to the point of financial ruin for many patients.
IMPACT OF DENIAL OF SERVICE
Patients who have conditions such as malignancies or chronic diseases that require multiple treatments on a regular basis may have a worsening outcome without timely care. It can lead to an increased overall mortality and morbidity. Our
experience with administration of chemotherapy and other Biologics is the time it takes from deciding to implementing a treatment is getting longer and longer. Many patients who are denied coverage for preventative services may rely on emergency services, leading to significant overcrowding and higher costs. In some situations where the service is not denied but still cannot move forward because of exorbitant out-ofpocket costs. In those situations, patients end up foregoing the treatments. Patients facing financial hardship due to denied claims may experience mental health issues. Low-income individuals, racial minorities, and people with disabilities are disproportionately impacted by denials, exacerbating health inequalities.
DEFAULT DOWN-CODING
Some insurance companies fail to understand the complexity of providing medical care. That is reflected by a default position of down coding of charges. For example, anytime there is a charge for 99214 level of service it is down coded to 99213. It is then upon us to provide adequate documentation, many times in paper form, to get that down coding reversed. It is flat out disrespecting the effort that we put into taking care of patients. When we confronted one of the insurance companies about this, the reply was “It is simply a standard practice to down-code”. They are completely unaware of the resources it takes to reverse a claim to the appropriate charge level.
In summary, I feel the insurance companies are rarely held accountable for their actions. However, I am feeling cautiously optimistic on one of CMA’s top priorities in 2025 which is to advocate for legislative changes that will alleviate the increase in prior authorization requirements and denials from health plans. They will be proposing separate legislative vehicles that will be advocated for as a legislative “package” to reform the prior authorization process relying on experience from physicians and groups. This will include in part, removing prior authorizations for services that are approved at a high rate, decreasing the amount of time the health plan must approve or deny a request and requiring appeals be reviewed by a physician of the same or similar specialty.
If you are not a member of SJMS/CMA , we encourage you to join us. As physicians, we must come together as a group to fight in the interest of our patients and our profession.
Recognized for Excellence
Heart & Vascular Institute
Designated heart attack and stroke receiving center.
Cancer Institute
San Joaquin County’s only nationally accredited cancer center.
Orthopedic & Spine Center
Certification of distinction for total hip and knee replacement from the Joint Commission.


















• Robotic-assisted surgery

We’re proud to announce our new Chief Executive Officer, Tina Burch, RN, MSN. Burch began her nursing career at DHM more than 33 years ago and has served as an asset to the hospital since, serving in various leadership roles.

The California Medical Association (CMA) works tirelessly to ensure the physicians of California have the support they need to deliver the highest quality of care to the people of California. Here's a look back at what we've accomplished this year!
Wins at the Ballot Box: Rate increase for physicians, improved access to care for patients and more
+ Prop 35: 57 of 58 counties voted yes to approve Proposition 35, a historic investment in Medi-Cal that provides the first across the board rate increase for physicians in more than 20 years and dedicates funding to improve access to care for the millions of seniors, children, low-income families and people with disabilities in our state.
+ Prop 1: Expanded funding for mental health and addiction treatment, including investments in the health care workforce.
+ Measure C: Protected physician practices from huge tax and fee increases by defeating Measure C in Sacramento.
Codifying Physician Priorities: Supporting physician mental health, ensuring protections against AI, and more
+ Governor Newsom signed all of CMA’s priority bills that made it to his desk: a bill to ensure artificial intelligence does not take the place of physicians, legislation giving health care workers new tools to support victims of domestic violence and human trafficking, a legislative change to the medical board’s licensure application that will reduce mental health stigma for physicians, and a new law that will provide parity in the penalty for violence committed against health care workers in emergency departments.
+ A banner legislative year, with 115 CMA supported bills signed into law, 24 opposed bills stopped and 23 problematic bills successfully amended.
+ Successfully advocated for significant prior authorization reforms for Medicaid and Medicare Advantage plans to speed up treatment and save physician practices billions of dollars.
Fighting for Physicians: Reducing administrative burdens, helping keep practices open and more
+ Supported physician practices during a devastating cyberattack that resulted in nationwide outages that threatened the viability of physician practices. CMA successfully advocated for advance payments and interest-free financial resources to keep practice doors open.
+ Stepped in to stop a Blue Shield modifier 25 policy that would have significantly reduced reimbursement for E/M services and created a disincentive for physicians to provide efficient care for unscheduled services.
+ Worked with Aetna to get California physicians excluded from its emergency services review policy, which would have increased costs for physicians and created delays for patients in crisis.
+ Filed a lawsuit against DMHC for failing to enforce California’s prompt payment regulations in implementing SB 510, which resulted in significant delays and reductions in reimbursements.
Supporting the Physician Workforce: Funding GME and investing in the physician pipeline
+ Awarded $25,170,000 through Physicians for a Healthy California to 142 GME programs to train 184 residents in underserved communities, increasing the physician pipeline.
+ Awarded $72,500,000 in CalHealthCares educational loan repayments to 297 physicians and dentists who provide care to Medi-Cal patients.
+ Graduated 190 CalHealthCares cohort 1 awardees, after completing five years of service to underserved communities in California, with 90% saying they intend to continue serving Medi-Cal patients.
+ Delivered dynamic, quality medical education to nearly 15,000 physicians and health care providers via CMA’s monthly Virtual Grand Rounds.
Protecting Practice Viability: Helping physicians get paid
+ Recouped more than $2.1 million from payors on behalf of physician members, protecting the viability of independent physician practices.
+ Returned $53 million in Medicare shared savings back to physician practices through CMA’s Physician Services Organization’s partnership with Aledade.
+ Stopped federal legislation that would have cut Medicare physician payments by $100 million a year.
Together We Are Stronger: Increasing the power of physician voices
+ Saw record membership growth in 2024 , boasting a 25% increase and making CMA the largest state medical association in the country.
+ Successfully supported dozens of candidates for state and federal office who share CMA’s philosophy and vision of the future of health care and medical practice.
ٙ Five California physicians elected to state and federal office.
ٙ 28 of 32 CALPAC-supported candidates in targeted races won their bids for state and federal office.
Our success this year and every year wouldn’t have been possible without the dedication and commitment of the physicians of California. Thank you to all of our CMA members for your unwavering support of the medical profession and your dedication to the health and well-being of our communities.
For more details, see cmadocs.org/year-in-review.



J
T HURSDAY, D ECEMBER 12, 2024
M agical Cocktail Reception 6:00pm | Dinner 7:15pm S tockton Golf & Country Club










TROLLING MAGIC, A PHOTO BOOTH, AND MORE!


J oin us for an Enchanting Evening featuring strolling magic, a photo booth, and more!
T HURSDAY, D ECEMBER 12, 2024
M agical Cocktail Reception 6:00pm | Dinner 7:15pm S tockton Golf & Country Club





HOSTED THURSDAY,DECEMBER THANK YOU TO EVERYONE





THURSDAY,DECEMBER 12,2024
EVERYONE FOR ATTENDING



IN THE NEWS

Gill Family Receives Key to The City
In December, then Stockton Mayor Kevin Lincoln presented Drs. Jasbir and Param Gill with a Key to the City. They were recognized as pioneering physicians and business leaders who embody the American Dream and the spirit of Stockton. Their first- generation success story resonates with the values of the diverse and growing city.
“The Gill Family has been a cornerstone of quality healthcare delivery in our community for decades,” said Mayor Kevin Lincoln. “Their invaluable contributions have not only transformed the healthcare landscape in Stockton but have also uplifted countless families through their compassion and dedication. It was my distinct honor to recognize their profound impact on the City of Stockton and the greater community.”
Providing staff, physicians, and patients with relevant & up to date information
Stockton Welcomes Central Valley Vein and Wound Center
Central Valley Vein and Wound Centers is expanding its specialized care to Stockton, offering advanced treatment for chronic wounds and vascular conditions. Led by Dr. Leo Fong, a board-certified vascular surgeon with over 25 years of experience, the center provides comprehensive care for patients suffering from nonhealing wounds, venous insufficiency, and other vascular issues.

Dr. Fong and his team are committed to improving patient outcomes through evidence-based treatments, including minimally invasive vein procedures and advanced wound care therapies. With a focus on accessibility, the Stockton location offers urgent appointments and accepts most insurance plans, including Medi-Cal.
By bringing expert wound and vein care to Stockton, Central Valley Vein and Wound Center aims to enhance quality of life for patients while reducing the need for hospital visits.
For more information, visit cvveinandwound.com or call (559) 721-4910.
Gill Family
Leo Fong, MD
The California Medical Association will host its 51st annual Legislative Advocacy Day on April 9, 2025, in Sacramento
CMA’s Legislative Advocacy Day consistently brings together more than 400 of physician and medical student leaders from all specialties and modes of practice. Attendees will have the opportunity to meet with legislators on priority health care issues.
Attendees can expect to get hands-on experience and learn the nuts and bolts of advocating for their patients and profession.
• Join your physician, medical student and resident colleagues at the Sheraton Grand Sacramento Hotel.
• Attendees will have the opportunity to meet and lobby legislators on priority health care issues and learn how to become an advocate for your patients and colleagues.
• Registered attendees will receive a webinar training on legislation and policy affecting the practice of medicine.
• Register online at www.cmadocs.org/eventregistration/sessionaltcd/LEGDAY25 or email Lisa@sjcms.org.
St. Joseph’s Medical Center Appoints
David P. Ziolkowski
as New President
St. Joseph’s Medical Center is pleased to announce the appointment of David P. Ziolkowski as its new President and Chief Executive Officer, effective February 10, 2025. Mr. Ziolkowski succeeds Don Wiley who retired in November 2024 after a 34-year career at St. Joseph’s Medical Center.
Mr. Ziolkowski brings more than 20 years of healthcare leadership experience, by his success in improving organizational efficiency, strengthening financial performance, enhancing patient care quality, and building meaningful connections within the community. Most recently, Mr. Ziolkowski served as Chief Executive Officer at Tenet’s Carondelet St. Mary’s

Hospital, where he improved the hospital’s finances, increased patient satisfaction, and enhanced overall performance of the hospital.
Mr. Ziolkowski stated, “I am honored and excited to join the team at St. Joseph’s Medical Center. I look forward to working with the dedicated staff, physicians, and community partners to build upon the hospital’s legacy of providing exceptional care.”
St. Joseph’s Medical Center Celebrates Third Year as One of America’s 250 Best Hospitals
St. Joseph’s Medical Center has been named one of America’s 250 Best Hospitals for 2025, according to new research released by Healthgrades, the #1 site Americans use when searching for a doctor or hospital. This achievement reflects St. Joseph’s unwavering commitment to exceptional patient care and puts the organization in the top 5% of hospitals nationwide for overall clinical performance. SJMC is celebrating its third consecutive distinction of being named one of Healthgrades America’s 250 Best Hospitals (20232025) and has received Healthgrades America’s 100 Best Hospitals for Critical Care™ for four years in a row (2022-2025), reflecting St. Joseph’s commitment to exceptional patient care.
In addition to this recognition for overall clinical care, SJMC is the recipient of numerous accolades related to its exceptional patient outcomes in key service areas, including Coronary Interventional Procedures, Chronic Obstructive Pulmonary Disease, Treatment of Bowel Obstruction, Treatment for Sepsis, and Treatment of Pulmonary Embolism. These achievements further underscore the organization’s dedication to clinical excellence, placing SJMC among the upper echelon of hospitals nationwide.
David P. Ziolkowski
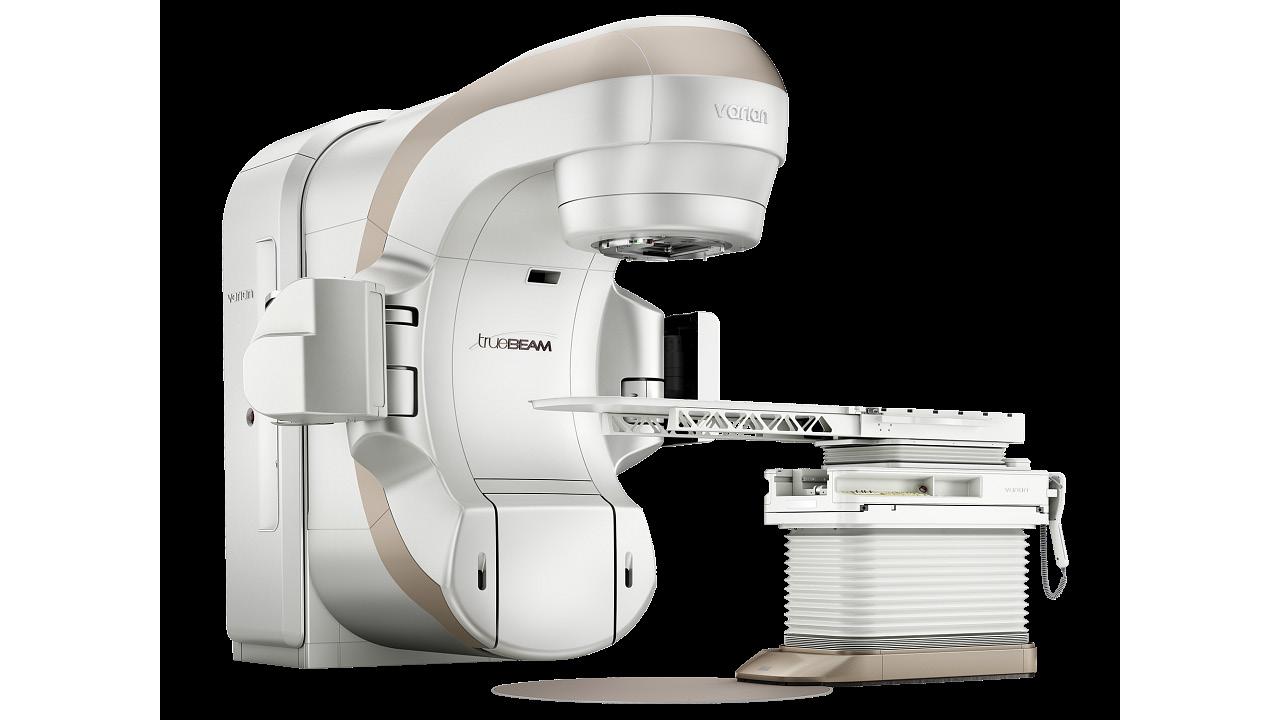
The most advanced cancer-fighting technology, closer to home.
Now at St. Joseph’s Cancer Institute, the TrueBeam Linear Accelerator combines imaging, radiation beam delivery and sophisticated motion management to accurately and precisely target tumors with speed.
The TrueBeam provides breakthrough technologies that allow our experts to treat more challenging cancers with precisely targeted, highly concentrated doses of radiation, given in less time, and with less impact on healthy tissue.
Learn more at dignityhealth.org/stockton/cancercare





St. Joseph’s Medical Center Employees Donate over 1,400 Toys to Children in Need
Dignity Health St. Joseph’s Medical Center (SJMC) held their annual Adopt-a-Child toy drive on December 12th, with 1,403 toys and 20 bikes collected for local children. For more than 40 years, employees at SJMC have donated gifts to local children through the annual event that is organized and carried out entirely by employee volunteers.
Through partnering with nonprofits such as Child Abuse Prevention Council, Human Services Agency, PREVAIL, Children’s Home of Stockton, and Stockton Shelter for the Homeless, the toys will be distributed to over 500 local children in the San Joaquin community prior to Christmas.
“We continued to be blown away by the generosity of the staff at St. Joseph’s Medical Center,” said Vice President and Chief Philanthropy Officer, Julie Kay Eckardt-Cantrall. “The hospital was founded on the mission of serving the greater community, and I am proud that 125 years later, we continue that legacy of giving back.”
St. Joseph’s Medical Center Celebrates 125 Years Since Opening Doors to Stockton Community
On December 20th, Dignity Health St. Joseph’s Medical Center hosted a special anniversary in celebration of the opening of the doors to St. Joseph’s
Home and Hospital 125 years ago, on December 21, 1899. Hospital leadership, staff, physicians, donors and dignitaries came together for a ceremonial ribbon cutting at the Medical Center’s Main Lobby, followed by an open house hosted by the St. Joseph’s Foundation of San Joaquin.
“Having the opportunity to celebrate this milestone with our staff, donors and greater Stockton community is truly remarkable,” said B.J. Predum, Central Valley Market President and Interim President of St. Joseph’s Medical Center. “We are grateful for the community’s continued support and are proud of the accomplishments we have achieved over the past 125 years which allow us to provide the highest quality care to our local population.”

St. Joseph’s Foundation of San Joaquin brings life-saving equipment to expectant mothers and children
Thanks to philanthropic efforts, St. Joseph’s Foundation of San Joaquin has provided funding for pediatric-focused equipment such as glidescopes, handheld ultrasounds, and fetal monitors.
“St. Joseph’s maternity ward sees a high volume of high-risk mothers who have received no or little prenatal care, increasing the need for emergency C-sections,” said Amy Fry, Director of Family Birth Center at St. Joseph’s. “It is no exaggeration to say that this gift will save lives and improve outcomes for
SJMC Employees Donate over 1,400 Toys
SJMC Celebrates 125 Years
IN THE NEWS

Life-saving equipment
mothers and babies alike.”
This new equipment is an example of how philanthropy works quietly in the background, leveraging gratitude to supply what other funding sources cannot consistently deliver.

Introducing Dan Vongtama, MD, radiation oncologist with Dignity Health Medical Group –Stockton
We are pleased to introduce Dr. Dan Vongtama, a boardcertified radiation oncologist dedicated to
Providing staff, physicians, and patients with relevant & up to date information
providing compassionate, patient-centered care with clear communication. Dr. Vongtama treats cancer using advanced techniques, including stereotactic body radiotherapy and electron beam therapy. His expertise ensures patients receive the most effective and personalized treatment plans. He is affiliated with St. Joseph’s Medical Center and brings extensive experience and a compassionate approach to his practice.

San Joaquin General Hospital Proudly Welcomes Dr. Zamip Patel
Dr. Zamip Patel is a highly respected Urologist and Andrology/Male Infertility specialist. With fellowship training in Andrology at the University of Illinois and residency at Mount Sinai School of Medicine
in New York, Dr. Patel is a recognized leader in male reproductive health.
Over the years, Dr. Patel has received several prestigious awards for his contributions to the field, and his leadership extends to crucial roles such as Chief of Staff at Advent Health East Orlando.
His practice focuses on General Urology, Urologic Cancers, and Male Infertility, with a particular
Dan Vongtama, MD
Dr. Zamip Patel
Marike Zwienenberg, M.D.
Enhanced referrals, closer to home

The UC Davis Pediatric Neurosurgery program is proud to offer minimally invasive and endoscopic interventions for disorders of the brain and peripheral nervous system. Our level I Children’s Surgery Center is equipped with image-guided surgical navigation, brain mapping and intraoperative imaging to ensure optimal outcomes, and is among few fetal treatment centers nationwide to perform in utero repair of spina bifida. Your referred patients and their families benefit from the academic expertise of nationally ranked UC Davis Children’s Hospital, plus the convenience of care closer to home and lodging on our Sacramento campus.
Our physician referral liaisons are here to help navigate referrals and:
■ Facilitate access to our secure EMR system, PhysicianConnect
■ Assist with UC Davis Health clinical trials and telemedicine
■ Keep you abreast of new services, providers and research programs
■ Arrange meetings, webinars, and share details about CME and events
Connect with your local Physician Referral Liaison: Joaquin Muñoz 916-878-7301
joamunoz@ucdavis.edu
IN THE NEWS
passion for microsurgical techniques and the pathology of male reproductive organs.
As a thought leader and innovator, Dr. Patel’s research is dedicated to improving the function, surgery, and treatment of male reproductive organs and gametes. We’re proud that Dr. Patel’s expertise is making a difference in the lives of so many, and we look forward to his continued impact in the years to come!
San Joaquin General Hospital First in Northern California to Adapt Groundbreaking Medical Technologies
New surgical robot and automated laboratory to provide improved health outcomes
San Joaquin General Hospital (SJGH) has acquired two groundbreaking medical technologies, including the Intuitive da Vinci 5 dual console surgical robot and Abbott’s Total Lab Automation.
SJGH is the first teaching facility in Northern California to offer the da Vinci 5 dual console technology, providing an unprecedented patient and Residency experience. The da Vinci 5 succeeds the da Vinci Xi, which has performed over 1,000 noninvasive surgeries at SJGH since its acquisition in 2017.
Adding Abbott’s Total Lab Automation will ensure that the downtime is kept to a minimum so clinicians will receive the laboratory results they need to make informed decisions. The automation system is the first in the U.S. for clinical labs featuring this smart CAR technology, which allows samples in self-
Providing staff, physicians, and patients with relevant & up to date information

propelled cars to travel throughout the track without a belt. Smart CAR technology streamlines operations so labs can provide quick, accurate results and deliver the best care to patients. Lab worker safety is improved by minimizing contact with patients’ blood samples and preventing exposure to biomedical waste.
“The acquisition of both da Vinci 5 and Abbott’s Total Lab Automation guarantees that the patients of SJGH will have access to the most advanced medicine available,” said SJGH Chief Executive Officer Rick Castro. “Our commitment to health equity means that every patient in the San Joaquin community, regardless of socioeconomic status, has equal access to these cutting-edge technologies.”
da Vinci 5 Dual Console














IN THE NEWS
Kaiser Permanente Modesto and Manteca Hospitals Among the Safest in the Nation
Kaiser Permanente’s Modesto and Manteca hospitals earn an “A” for limiting patient injuries, reducing medical errors, and preventing infections, according to The Leapfrog Group
Kaiser Permanente’s Modesto and Manteca hospitals are being recognized as among the safest in the nation for patient care, according to The Leapfrog Group’s biannual Hospital Safety Grades report.
Leapfrog reviews hospital clinical data and assigns hospitals grades based on approximately two dozen safety measures that analyze patient injuries, medical and medication errors, and infections. Kaiser Permanente’s Modesto and Manteca hospitals are recognized with an “A” grade for patient safety.
This fall, 14 Kaiser Permanente hospitals in Northern California received A grades from Leapfrog, including: Antioch, Fresno, Manteca, Modesto, Oakland, Roseville, San Francisco, San Jose, San Leandro, San Rafael, Santa Clara, Santa Rosa, South Sacramento, and South San Francisco.
“Our dedicated care teams place patient safety at the forefront of everything they do,” said Sanjay Marwaha, MD, Kaiser Pe rmanente Central Valley physician in chief. “We take pride in serving our community and ensuring we are meeting the diverse needs of our members and patients while providing them with the safest care possible.”
Providing staff, physicians, and patients with relevant & up to date information
The Leapfrog Group assigns letter grades to nearly 3,000 hospitals throughout the United States. The grades are updated twice annually, in the fall and spring.
More than 60% of Kaiser Permanente Northern California hospitals received an A grade. In California overall, only about 30% of the state’s hospitals earned this top grade.
Doctors Hospital of Manteca Achieves Level 3 Geriatric Emergency Department Accreditation
The Emergency Department at Doctors Hospital of Manteca (DHM) was recently informed by the American College of Emergency Physicians (ACEP) that it has achieved Level 3 Geriatric Emergency Department Accreditation (GEDA). The GEDA program confirms that DHM personnel are trained to implement processes to elevate the care of seniors and includes a Physician Champion and a Nurse Champion. ACEP, along with the Society for Academic Emergency Medicine, Emergency Nurses Association, and American Geriatrics Society, developed the geriatric ED guidelines, recommending measures for the accreditation, that includes ensuring availability of geriatric-friendly equipment, specialized staff, and routine screening for vulnerabilities such as delirium, dementia, and fall risk.
Doctors Hospital of Manteca Now Providing CKRT
The ICU at Doctors Hospital of Manteca (DHM) has implemented Continuous Kidney Replacement Therapy (CKRT), is a form of continuous dialysis treatment that provides continuous removal of fluids, electrolytes, and waste products from the blood when the kidneys are not functioning properly. Unlike regular dialysis, which takes 3-4 hours, continuous dialysis – as the name suggests – processes 24 hours a day, and the reason it is increasingly used in intensive care units that it is gentler on the body than traditional dialysis. It is a complicated therapy that requires special expertise on the part of physicians and nurses to implement properly and it is used until patients start showing signs of their own kidneys recovering, or until their blood pressure allows for traditional dialysis.
Aquablation Therapy Program for Enlarged Prostate Implemented at Doctors Hospital of Manteca
The Operating Rooms at Doctors Hospital of Manteca now feature Aquablation, a treatment for benign prostatic hyperplasia (BPH), commonly referred to as an enlarged prostate. This minimally invasive procedure, under the direction of Dr. Prithipal Sethi and Dr. Kisseng Hsieh, uses a robotically guided camera and ultrasound imaging to

map the prostate. The individualized map is used to guide a high-pressure, heat-free water jet to destroy and remove excess prostate tissue. Although this is a relatively new procedure, multiple five-year studies, including one published in the Journal of Urology, have shown safety and efficacy standards are met or surpassed and sustained benefits for patients.
Office Space Available for Lease
Office space available now to be leased for medical/ dental/medically relevant professional office. The space is 1367 square feet for immediate occupancy in the established Medical Doctor’s Complex, Weber Ranch Professional Park at East March Lane, with 7 rooms and waiting area. Call now (209) 951-8830.
We are excited to announce our annual membership dinner, where we will honor the recipients of the Young Physician and Lifetime Achievement Awards (recipients to be determined). Please mark your calendars for Sunday, June 8, at the Stockton Golf & Country Club. We look forward to celebrating with you!
Doctors Hospital of Manteca

MEDICAL STUDENTS MARK PATH FOR YOUTH
STUDENT HEALTH EMPOWERMENT CONFERENCE INSPIRES THE FUTURE OF MEDICINE
BY JO ANN KIRBY
The path to a career as a physician can be a long and arduous journey but one conference has students guiding students. With a theme of “You: The Future of Health Care,” the Stockton Health Empowerment Conference (SHEC) took place February 8 at San Joaquin Delta College. The daylong program featured six rotations of three to four workshops with titles such as “Medical Schools, The Nuts & Bolts of Getting In,” and even “Stitching Basics: Suturing 101.” The 11th annual event was launched in 2015 by a group of UC Davis medical students who were concerned over a lack of educational resources in Stockton and surrounding areas for high school and junior college students.
“Stockton is home to amazing individuals who are committed to making a difference. Your presence here today speaks volumes about your unwavering commitment to health care , to service and to the community we are building together,” Jose Aguilar, a first-year medical student at UC Davis who was born and raised in Stockton, said in welcoming attendees to the conference. “You are the changemakers, the visionaries, the ones who will shape the next era of innovation, compassion and excellence in the health care field.” >>

STOCKTON HEALTH EMPOWERMENT
CONFERENCE SPONSORS
GOLD SPONSOR
KAISER PERMANENTE
BRONZE SPONSORS
CALIFORNIA URGENT CARE
DELTA EYE MEDICAL GROUP
FOOD 4 LESS
PASSION PLANNER
SAN JOAQUIN DELTA COLLEGE
SAN JOAQUIN MEDICAL SOCIETY
SMART & FINAL
UC DAVIS SCHOOL OF MEDICINE
UC DAVIS SCHOOL OF MEDICINE, OFFICE OF STUDENT & RESIDENT DIVERSITY
THANK YOU FOR YOUR SUPPORT!
SHEC’s roots are strong and its purpose resonates with the students who help keep it going. To make a difference, a group of UC Davis Medical School students decided to start a conference that would introduce students to the networking and resources they would need to succeed. It is an effort to empower, motivate, and provide information about health professions to students from disadvantaged backgrounds where families might be supportive but unfamiliar with the pathways to health professions. The conference’s speakers, panel discussions and workshops are all attempts to encourage conversations about longterm goals, college admissions, financial aid, health profession careers, educational achievement, community service, research, and connections to help make a difference. SHEC’s ultimate goal is to equip students with the skills necessary to navigate the pursuit of higher education and become health leaders in the area’s medically underserved communities.
SHEC 2025 was organized by six second-year UC Davis medical students who co-chaired the event and were assisted by a committee of seven first-year UC Davis medical students including D’Angelo Martinez, who is a
Decision Medicine alumni and Stockton native who attended SHEC when he was in college. A volunteer committee of ten others also helped with the big task of producing the day-long program. This year’s organizers had the added responsibility of securing everything needed for an in-person conference for 150 students. The return to an in-person conference was applauded by organizers. Since Covid, it had been an online event. “It felt absolutely amazing to hold this conference in person again. Being part of something that can have such a positive impact on the youth means so much to me, especially as someone who was once inspired by this exact conference and similar programs,” Martinez said.
“ WE CAME TO CHECK IT OUT AND SEE WHAT DIFFERENT CAREERS ARE POSSIBLE. BOTH OUR OLDER SIBLINGS ARE STUDYING PHARMACY AT UNIVERSITY OF THE PACIFIC, SO THERE ARE HIGH EXPECTATIONS . ” - SEDRA ANNOUS
Aguilar urged the students to “ask questions, share your thoughts and participate, “adding that SHEC is designed to provide invaluable networking opportunities. Aguilar’s welcome remarks were followed by a keynote address presented by Dr. Kwabena Adubofour, an internal medicine physician at Community Medical Centers, an Associate Program Director for St. Joseph’s Residency Program and co-founder of Decision Medicine. Dr. Adubofour outlined all of the programs available to encourage and support young people who are interested in medical professions. Citing the work of the San Joaquin Medical Society’s Decision Medicine and Bridge to Medicine programs, he encouraged attendees to pursue their passion for medicine and return to work in their communities. “Wouldn’t you rather come home and sleep in your own bed at your parents’ house. They can babysit your kids for you. No, seriously, do you know how much child care costs?” he asked to laughter from the audience, which included high school students, college students and parents.
Many of those in attendance were eager to learn and some even took studious notes. “We came to check it out and see what different careers are possible. Both our older siblings are studying pharmacy at University of the Pacific, so there are high expectations,” Sedra Annous, a junior at Stockton Middle College, said. Sedra and her sister Jenna, a freshman at Bear Creek High School in Stockton, said they were also hoping to learn more about the pathways to medical school.
Multiple 45-minute workshops were divided up into rotations throughout the day. At a Professional Career Panel, the Annous sisters heard from a dentist, an EMT, a family medicine physician and a certified physician assistant. Dr. Fareen Baloch, the dentist, attended University of the Pacific’s




Dugoni School of Dentistry and said she chose the profession for its work/life balance. She encouraged students to reach out to her @toothfareen on Instagram. They also heard from Vy Pham, who immigrated from Vietnam to the United States when she was in middle school.
Pham says she values her profession as a physician assistant because she feels like she is bridging a gap between vulnerable patients and the health care system. To further help out in her community,
she spends her free time volunteering as a translator.
“ HEARING THE ORIGINS, STRUGGLES AND PERSEVERANCE FROM THESE INDIVIDUALS ARE BOTH INSPIRING AND HIGHLY RELATABLE,” - DR. DAVID ARAIZA

The personal histories that health care professionals shared during panel discussions are important for students to hear, Dr. David Araiza said. “As a volunteer, organizer and participant in these conferences, the most powerful and memorable sessions in my opinion have always been the stories of medical students, doctors and other professionals,” said Dr. Araiza, who is a family medicine physician with Community Medical Centers. He helped organize the 3rd SHEC when he was a medical school student at UC Davis and has participated as a guest speaker. “Hearing the origins, struggles and perseverance from these individuals are both inspiring and highly relatable,” he said.
One of the workshop presenters was Dr. Amir Assadi-Rad, a biology professor at San Joaquin Delta College and the co-author of “The Nuts and Bolts of Getting Into Medical

School.” During his presentation, students avidly took notes while he gave them helpful studying tips. He has been involved with SHEC since it began, first as an attendee and then as a presenter. “I am very thankful for the UC Davis medical students who come to Stockton to put together this conference,” he said, adding that it can’t be easy to organize with all the demands of medical school. “They work very hard. We owe them our greatest appreciation.”
Dr. Assad-Rad’s presentation was packed with valuable advice. “Are they pursuing it out of genuine passion, or are there external motivations driving their decision? Medicine is a demanding profession and students should be certain that becoming a doctor is their own heartfelt choice — one that excites them every morning,” he said. “Once they are confident that medicine is the right path, they must prioritize their academic performance. Strong grades are essential
and it can be difficult to recover from a weak academic record. A solid GPA is the foundation of a competitive application.”
Participants also enjoyed a lunch and a vendor fair where they could learn about opportunities including the San Joaquin Medical’s Society’s Decision Medicine Program. “This conference is giving us a lot to think about,” Jenna Annous said.
“I’m learning a lot.” That’s just the sort of feedback that organizers say makes SHEC valuable. “Coming from an underserved background, I understand the additional hardships and lack of resources that many in Stockton face. At the same time, our community needs more health care providers and this conference aims to inspire attendees to see themselves as future leaders in medicine,” Martinez said. “I believe in every student and feel they all have the potential to reach their dreams. I love this city and where I come from, so it was truly touching to hear students say that we helped spark their interest in medicine and that they left the conference feeling inspired.”




BUILDING HEALTHIER FUTURES:
EMPOWERING SAN JOAQUIN COUNTY THROUGH HEALTH AND COLLABORATION
BY NADEJA STEAGER
The Community Health Leadership Council San Joaquin (CHLC) has been steadfast in promoting public health and connecting healthcare, policymakers, education, business, and stakeholder communities in San Joaquin County to cultivate a culture of trust and develop strategic alliances and regional collaborations. >>






AND COLLABORATION
PATHWAYS TO

Through annual community health convenings, the CHLC inspires and supports innovative solutions to lessen negative impacts on the communities we mutually serve.
As health challenges grow more complex, forums like this serve as vital spaces where health professionals, government, and community can unite, exchange knowledge, spark collaboration, and equip each other with practical resources to navigate the oftentimes difficult path toward better health.
The Council’s 24th Annual Community Health Forum held on November 15, 2024, at the Robert J. Cabral Agricultural Center, exemplified this collaborative mission through its empowering theme:
PATHWAYS TO WELLNESS: TIPS, TOOLS AND HACKS
The forum offered something for everyone; health and wellness education, interactivity, and tools to help get on the path to better whole health and improved quality of life.
Brian Jensen, the Master of Ceremonies and Regional Vice President of the Hospital Council Northern and Central California, ushered attendees into a vibrant morning
of education, energy, and empowerment. He exhorted, “Today is about equipping each of us with something, some change that we can implement in our own lives for the sake of our own health.”
The session commenced with striking facts about the state of health in San Joaquin County. “When you look at fifth through ninth graders, you’ll find that one in two of them is overweight,” stated forum Key Speaker, Dr. Anitra Williams, DNP, CCRN, PHN, HACP, Vice President and Chief Nurse Executive Officer, Dignity Health, St. Joseph’s Medical Center. A personal story highlighted the preventable and critical long-term consequence of dialysis due to neglecting selfcare. Attendees explored how barriers and social challenges influence the decision-making process around self-care and Dr. Williams elaborated on how socioeconomic status, access to quality healthcare, education, and neighborhood environments directly affect health disparities within communities. She noted, “When you look at the root cause of most illness... you begin to find modifiable behaviors. You can start to incorporate those things into your lives. And you can change the trajectory of your health and wellness.” Attendees were left with a thought-provoking message as Dr. Williams emphasized that in caring for ourselves, we are better equipped to support and care for one another.
HEALTH IN ACTION
From there, attendees stepped into a whirlwind of specialized workshops to delve deeper into various health
TO WELLNESS
issues. Mental health experts addressed the rising rates of anxiety and depression and led sessions that encouraged open dialogues to overcoming stigma, building support networks, and developing coping strategies. Participants had live healthy food preparation demonstrations and learned ways to identify healthy foods and foster healthier eating habits in a world that often prioritizes convenience over nutrition.
Other workshops included key topics like Chronic Conditions; Obesity, High Blood Pressure, Diabetes, and heart disease; these preventable illnesses are all key drivers of poor health in this region. Living Active and Physical Activity stations demonstrated different movements and techniques we can do throughout the busy day, even at our desks. They also shared how these small tweaks directly impact and support heart health. Stress Reduction and Social Wellness were also key topics showcased at this year’s forum and the workshops were full of energy and activity.
insights, practical tools, and a renewed sense of purpose, the forum empowered attendees to begin and take charge of their health and wellness journeys.
The sense of collaboration was reinforced by the CHLC’s commitment to ensuring that the work done during the forum extends beyond the event itself. Attendees were encouraged to form lasting partnerships and continue sharing resources, knowledge, and best practices in their settings.
As the forum concluded, it was clear that the Pathways to Wellness theme resonated deeply with everyone present. The event offered more than just an opportunity to learn—it was a call for collaboration and action.
The Community Health Leadership Council deeply appreciates the longstanding relationship with Health Careers Academy (HCA) and the collaborative efforts with HCA students to deliver exceptional personalized experiences at the forums. The CHLC offers students valuable opportunities to engage with real-time health strategies and connect with prominent community leaders.
An exciting feature at this forum, courtesy of Adventist Health, Lodi Memorial Hospital, was the selection of bitesized delicious “superfoods” like oriental chicken salad, baked chickpeas, chia pudding, and more, which forumgoers sampled between workshops. Participants were also given recipes to recreate them.
As the forum concluded, it was clear that the Pathways to Wellness theme resonated deeply with everyone present. The event offered more than just an opportunity to learn— it was a call for collaboration and action. By educating and equipping individuals and organizations with valuable
Altogether, the 24th Annual Community Health Forum was a resounding success, showcasing that through knowledge-sharing and collaboration, coupled with practical health and well-being tools, pathways to wellness can be accessible for all. Attendees left inspired and excited, equipped with tangible practices and toolkits they could immediately incorporate into their lives.

t o P h y s i c i a n s f o r 2 0 2 5
The California Legislature passed many new laws in 2024 affecting health care. In particular, there was a strong focus on health care coverage, drug prescribing, public health, workforce, and office safety issues. On the following pages you will find a summary of most significant new health laws of interest to physicians.
ALLIED HEALTH PROFESSIONALS
A B 2 7 3 0 ( L
Existing law defines when a physician assistant or nurse is a qualified health care professional authorized to conduct sexual assault forensic medical examination (SAFME) and treatment, including a requirement that the provider work in consultation with a physician and surgeon . This law removes the requirement that the consulting physician and surgeon be a practitioner who conducts SAFME examination or treatment, and replaces it with requirement that the consulting physician and surgeon be currently licensed. Also adds certified nurse-midwives to the list of qualified healthcare professionals, provided they work in consultation with a currently licensed physician and surgeon
Authorizes a pharmacist to furnish up to a 90 -day course of preexposure prophylaxis (PrEP), or preexposure prophylaxis (PEP) beyond a 90 -day course. Allows pharmacists to furnish PrEP beyond 90day limit if patient receives specified testing and follow up care consistent with CDC guidelines, including HIV, renal function, hepatitis B, hepatitis C, sexually transmitted diseases, and pregnancy for individuals of childbearing capacity. Requires health plans and health insurers to cover all PrEP and PEP furnish ed by a pharmacist, and all related pharmacist services and testing ordered by a pharmacist.
B 1
Prohibits anyone other than a licensed physician and surgeon from using “doctor,” “physician,” “Dr.,” “M.D.,” “D.O.,” or any other terms or letters implying the person is a physician, in a health care setting Extends pharmacist test-to-treat authority for COVID to January 1, 2026. For purposes of advance practice nurse practitioner certification under AB 890 (2020), prohibits limiting NP’s clinical experience to a single category of practice; allows an NP with at least 3 full-time equivalent years or 4,600 hours of direct patient care within the past 5 years to be deemed to have met the transition-to-practice requirements Eliminates requirement for NPs practicing independently to inform patients of their right to see a physician or to use specific phrases to communicate their non -physician status to Spanish language speakers. Adjusts the initial licensure period for resident physicians and surgeons to 26 months for those licensed after January 1, 2025. For residents who have not completed at least 36 months of approved training at initial renewal, allows licensee to renew if e nrolled in approved training program at time of renewal (only applicable to phys ician and surgeon licenses first issued on or after Jan. 1, 2022).

CLINICAL LABORATORIES
CMA Position: Support
Allows pathologists to remotely review digital materials (such as lab data, results, and images) under a clinical laboratory’s primary Clinical Laboratory Improvement Amendments (CLIA) certificate, without requiring separate licenses or registrations for the remote locations ; contingent on the State Department of Public Health determining that the authorization conforms to federal law by Jan uary 1, 2026, in consultation with the federal Centers for Medicare and Medicaid Service
CONSENT
CMA Position: Support
Authorizes a dependent child of the juvenile court who is 16 years of age or older to consent to receive medications for opioid use disorder from a licensed narcotic treatment program as replacement narcotic therapy without the consent of their parent, guardian, person standing in loco p arentis, or social worker, and without a court order to the extent permitted by federal law.
DRUG PRESCRIBING AND DISPENSING
Removes fenfluramine from list of Schedule IV –controlled substances under the California Uniform Controlled Substances Act, in alignment with federal Controlled Substances Act , under which fenfluramine was descheduled in 2022. Removes fenfluramine from list of controlled substances that are a crime to possess or sell As a result of the state descheduling, prescribers will no longer need to consult the CURES database before prescribing fenfluramine
Expands the requirement for a prescriber to discuss specified information about opioids to any patient before directly dispensing or issuing the first prescription for a controlled substance containing an opioid in a single course of treatment (previous law applied only to minors) . Deletes previous exception for treatment for chronic intractable pain Retains other exceptions for prescribing to hospital, skilled nursing facility, intermediate care facility, home health agency, or hospice patients; for treatment for terminal illness or substance use disorder; for patients receiving emergency care or emergency surgery ; or in instances where in the prescriber’s professional judgment, providing the required disclosures would be detrimental to patient health or safety, or in violation of patient rights regarding confidentiality
Requires each board that licenses prescribers to develop and annually disseminate to each licensee informational and educational material regarding the “Three Day Rule,” and to post that material on their website to increase awareness of medication-assisted treatment (MAT) pathways (Rule allows prescribers not in a narcotic treatment program to prescribe up to three days’ worth of MAT for opioid use disorder .) Also requires the medical board to annually disseminate materials to acute care hospitals in the state.
HEALTH CARE COVERAGE AND MANAGED CARE
CMA Position: Support
Requires a health care service plan or health insurer offering an outpatient prescription drug benefit to provide coverage for at least one medication approved by the U.S. Food and Drug Administration in each of the following categories without prior authorization, step therapy, or utilization review: (1) medication for the reversal of opioid overdose, including a naloxone product or another opioid antagonist; (2) medication for the detoxification or maintenance treatment of a substance use disorder, including a daily oral buprenorphine product; (3) a long-acting buprenorphine product; (4) a long-acting injectable naltrexone product. A B 2
CMA Position: Support
Requires health plans and health insurers to cover the diagnosis and treatment of Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infections (PANDAS) and Pediatric Acute -onset Neuropsychiatric Syndrome (PANS), when prescribed or ordered by a treating physician and is medically necessary under current nationally recognized clinical practice guidelines, as specified Requires coverage for specified treatment, including antibiotics, medication and behavioral therapies to manage neuropsychiatric symptoms, immunomodulating medicines, plasma exchange, and intravenous immunoglobulin therapy. Prohibits plans and insurers from imposing a higher cost-sharing for PANDAS and PANS than other benefits, and from denying or delaying coverage based on previous treatment or different diagnostic names A B 2
Requires a patient who is 18 years of age or older receiving health care services where primary care services are provided, to be offered tuberculosis (TB) screening, if TB risk factors are identified and to the extent these services are covered under the patient’s health care coverage ; excludes emergency department of a general acute care hospital . Requires a health care provider to offer or refer a patient for follow-up care if a patient tests positive for TB. Provides that a health care provider shall no t be subject to disciplinary action or civil or criminal liability due to the provider’s failure to comply with these requirements. Requires Medi-Cal managed care plans to ensure access to care for latent TB infection and active TB disease, and to coordinate with local health dep artment TB control programs
A B 2 2 5 8
Prohibits health plans and health insurers from imposing cost-sharing for any items or services that are integral to the provision of preventive care services, including but not limited to cervical and colorectal cancer screenings, HIV prophylaxis (PrEP and PEP), and home test kits for sexually transmitted diseases; prohibition applies regardless of whether the integral item or service is billed separately from a preventive care item or service Prohibits health plans and health insurers from imposing cost sharing for office visits associated with a preventive care service if the primary purpose of the office visit is the delivery of the preventive care service, and the preventive service and office visit are not billed separately or tracked as separate en counters
Require health plans and health insurance polic ies issued, amended, renewed, or delivered on or after July 1, 2025, to provide coverage without cost sharing for emergency room medical care and follow up treatment following a rape or sexual assault for the first 9 months after an enrollee initiates treatment, as specified Prohibits a health plan or health insurer from requiring an enrollee or insured to file a police report, charges to be brought against an assailant, or an assailant to be convicted of rape or sexual assault, as a condition of providing co verage.
CMA Position: Sponsor
Requires a health plan or disability insurer using artificial intelligence, algorithm, or other software tool for utilization review or management based in whole or in part on medical necessity to comply with specified standards, including requirement that an AI, algorithm, or software tool base medical necessity determinations on the enrollee’s clinical history and individualized clinical circumstances as presented by the requesting provider, and adhere to other specified criteria relating to nondiscrimination, fairness and equity, regulatory audits, oversight policies and procedures, privacy and permitted uses of patient data, period review of tool’s accuracy and reliability, patient safety, and preservation of the health care provider’s role in making health care decision s. Prohibits AI, algorithm, or other software tool from denying, delaying, or modifying health care services based in whole or in part on medical necessity; requires such adverse determinations to be made only by a licensed physician or a licensed health care professional competent to evaluate the specific clinical issues involved in the request.
HEALTH CARE FACILITIES AND FINANCING
Authorizes a Distressed Hospital Loan Program recipient, a small hospital, a rural hospital, a critical access hospital, or a health care district hospital, to seek approval from the Department of Health Care Access and Information for a delay to the Janua ry 1, 2030, compliance deadline by up to 3 years . Requires hospitals seeking a delay to submit a seismic compliance plan, and, if necessary, a Nonstructural Performance Category-5 evaluation report
CMA Position: Sponsor
Requires all general acute care hospitals with an emergency department to adopt and implement policies and procedures to facilitate the self -identification of an emergency department patient as a victim of human trafficking or domestic violence to hospital personnel Requires policies and procedures to meet certain requirements, includin g providing for patient confidentiality and facilitating a reasonably prompt, private, and voluntary interview of the patient by medical personnel, for the purpose of providing certain information to the patient relating to local services and resources for victims of human trafficking or domestic violence.
Increases the notice period required before proposed closure or elimination of the supplemental service of inpatient psychiatric unit or a perinatal unit from 90 days to 120 days Requires the health facility to provide public notice of the proposed elimination of the supplemental service of either inpatient psychiatric unit or perinatal unit , and conduct at least one noticed public hearing within 60 days of the notice of proposed elimination.
MEDI - CAL
Requires a site certifier of a primary care clinic or affiliate primary care clinic to be a clinician who oversees the provision of Family Planning, Access, Care, and Treatment (Family PACT) Program services and
authorizes certain clinic corporations to enroll multiple, but no more than 10, service addresses under one site certifier Authorizes the Department of Health Care Services to elect to not disenroll an individual or entity as a program provider following the revocation, suspension, or loss of a license, certificate, or other approval to provide health care based solely on conduct that is not deemed to be unprofessional conduct under California law. Subject to obtaining any necessary federal approvals
MEDICAL PRACTICE AND ETHICS
A B 3
Requires a health facility, clinic, physician’s office, or office of a group practice that uses generative artificial intelligence to generate written or verbal patient communications pertaining to patient clinical information to ensure that those communications include both (1) a disclaimer that indicates to the patient that a communication was generated by generative artificial intelligence and (2) clear instructions describing how a patient may contact a human health care provider. Disclosure not required for patient communications read and reviewed by a human licensed health care provider, or to communications pertaining to non-clinical or administrative matters, such as appointment scheduling, billing, or other clerical or business matters.
Prohibits a person (including an individual or entity) from furnishing information about a medical debt to a consumer credit reporting agency, and makes such medical debt void and unenforceable if a person knowingly violates this provision. Requires a contract creating medical debit entered into on or after July 1, 2025, to include these requirements Defines medical debt to mean a debt owed by a consumer to a person whose primary business is providing medical services, products, or devices (excluding cosmetic surgery); medical debt includes but is not limited to medical bills that are not past due, or that have been paid. A violation of this law by a person holding a license or permit issued by the state will be deemed a violation of the law governing that license or permit.
Prohibits a consumer credit reporting agency or an investigative consumer reporting agency from making a consumer credit report or an investigative consumer report containing information about medical debt. Prohibits a person who uses a consumer credit report in connection with a credit transaction from using medical debt listed on the report as a negative factor when making a credit decision.
Requires a hospital to maintain all records relating to money owed to the hospital by a patient or their guarantor. Any contract entered into by a hospital related to the assignment or sale of medical debt must require the assignee or buyer and any subsequ ent assignee or buyer to maintain records related to litigation for 5 years.
MENTAL HEALTH
CMA Position: Support
Authorizes a person’s treating physician to request a hearing for a new determination of a person’s capacity to refuse treatment with antipsychotic medication at any time in the 48 hours prior to the end of the duration of the current detention period when it reasona bly appears to the treating physician that it is necessary for the person to be detained for a subsequent detention period and their capacity has not
been restored Under exigent circumstances, requires the hearing to determine a person’s capacity to refuse treatment to be held as soon as reasonably practicable and within 24 hours.
S B 1 2 3 8 ( E g g m a n ) – H
CMA Position: Support
Expands the definition of “psychiatric health facility” for purposes of involuntary holds under the Lanterman-Petris-Short (LPS) Act to also include a facility that provides 24 -hour inpatient care for people with severe substance use disorders, or cooccurring mental health and substance use disorder ; and expands the services such a facility may provide to include substance use disorder services.
S B 1 3 2 0 ( W a h a b ) – M
CMA Position: Support
Requires a plan or insurer to establish a process to reimburse providers for mental health and substance use disorder treatment services that are integrated with primary care services , for plans issued, amended, or renewed on or after July 1, 2025.
PEER REVIEW
B 2 2 2 5 ( R
Extends the existing exemption from discovery in civil proceedings to include the proceedings and records of prehospital emergency medical care personnel committees and review committees focused on evaluating and improving care quality.
PROFESSIONAL LICENSING
Requires a healing arts board to require a licensee or registrant who electronically renews their license or registration to provide to that board the licensee’s or registrant’s individual National Provider Identifier, if they have one
CMA Position: Sponsor
Prohibits the Medical Board of California from requiring an applicant for a physician’s and surgeon’s license or a physician’s and surgeon’s postgraduate training license, or a renewing licensee, to disclose information regarding a condition or disorder that does not impair the applicant’s ability to practice medicine safely.
Updates continuing education requirements for general internists and family physicians who have a patient population of which over 25% are 65 years of age or older to include training on the special care needs of patients with dementia as part of the 20% of all mandatory continuing education hours in a course related to geriatric medicine or the care of older patients
PUBLIC HEALTH AND HEALTH EQUITY
CMA Position: Support
Beginning January 1, 2030, prohibits a person or entity from manufacturing, selling, or distributing into commerce in the State of California certain intravenous (IV) solution containers made with intentionally added DEHP; provides a 2-year extension for a person or entity who has a pending FDA approval or who lacks adequate equipment to manufacture DEHP-free IV solution container and meets other requirements, including providing prescribed notices to consumers. Beginning January 1, 2035, prohibits a person or entity from manufacturing, selling, or distributing into commerce in the State of California certain IV tubing made with intentionally added DEHP.
REIMBURSEMENT
Authorizes an emergency physician to choose to grant eligibility for a discount payment policy to patients with incomes over 400% of the federal poverty level . Clarifies that out-of-pocket costs for “high medical costs” means any expenses for medical care that are not reimbursed by insurance or a health coverage program, such as Medicare copays or Medi -Cal cost sharing. Requires a hospital’s charity care or discount payment policy to clearly state eligibility criteria based on income consistent with applica tion of the federal poverty level. Prohibits a hospital from considering a patient’s monetary assets in determining eligibility for charity care or discount payment policies, but authorizes a hospital to consider availability of a patient’s health savings account. A B 3 2 7
CMA Position: Support
Beginning January 1, 2026, requires health care service plans and health insurers, including Medi -Cal managed care plans, to reimburse complete claims within 30 calendar days or notify claimants of contested or denied claims within the same timeframe . Requires a complaint made by an enrollee about a delay or denial of a payment of a claim to be treated as a grievance , regardless of whether the enrollee uses the term “grievance.” Provides the California Department of Managed Health Care and the California Department of Insurance an exemption from the Administrative Procedure Act to issue implementing guidance and amend existing regulations for consistency
Requires a health care service plan contract or health insurance policy issued, amended, or renewed on or after July 1, 2025, to establish a process to reimburse for services provided by a community paramedicine program, a triage to alternate destination p rogram, and a mobile integrated health program
REPORTING REQUIREMENTS
CMA Position: Support
Requires the California Department of Public Health to collect voluntarily provided self-identification info about sexual orientation, gender identity, and variations in sex characteristics/intersex status (SOGISC) from
third parties, including but not limited to local health jurisdictions, on any forms or electronic data systems, unless prohibited by law; collection of this data is not required for individuals under 18 years of age. Adds an adult patient’s voluntary self-identified SOGISC and sex assigned at birth to list of data that providers, schools, and other agencies must disclose to local and state health department immunization registries; prohibits a provider from disclosing that information for a patient or client who is under 18 years of age.
CMA Position: Support
Requires employees and contractors to annually sign the confidentiality agreements prior to accessing confidential HIV-related public health records agreement and repeal s the annual review of the agreement. Expands and simplifies authority of the State Department of Public Health to disclose personally identifiable information in HIV-related public health records with federal agencies and collaborating researchers when necessary for specified purposes, including to coordinate, link, or reengage care; removes requirement for written authorization from the subject or their guardian if disclosure meets specified necessity criteria
REPRODUCTIVE ISSUES
Requires the maternal mental health program to consist of at least one maternal mental health screening during pregnancy, at least one additional screening during the first 6 weeks of the postpartum period, and additional postpartum screenings, if determin ed medically necessary and clinically appropriate in the judgment of the treating provider .
CMA Position: Support
Enhances penalties for crimes related to the harassment or intimidation of reproductive health care patients, providers, or assistants by making the following violations punishable as either misdemeanors or felonies: doxing a reproductive health care services patient, provider, assistant, or other individuals residing at the same home address, if bodily injury occurs; impeding access to reproductive health services facilities through use of force, threat of force, or physician obstruction or otherwise violating the California Freedom of Access to Clinic and Church Entrances Act; or committing a hate crime involving force or threats of force
CMA Position: Support
Requires a contract between a health care service plan or health insurer and a health care provider issued, amended, or renewed on or after January 1, 2025, to authorize a provider to separately bill for devices, implants, and professional services, associated with immediate postpartum contraception if the birth takes place in a general acute care hospital or licensed birth center Prohibits a provider contract from considering those devices, implants, or services to be part of a payment for a general obstetric procedure. A
Requires implicit bias programs to include recognition of intersecting identities and the potential associated biases, and extends implicit bias training requirements for health care providers involved in perinatal care to include all providers who are regularly assigned to provide perinatal care , as well as to all persons who are regularly assigned to positions where they interact with perinatal patients
Requires providers subject to this requirement to comp lete initial basic training on implicit bias based on the revised components by June 1, 2025, (or within 6 months of the start date for new hires ). Requires facilities, by February 1 of each year starting in 2026, to provide proof of compliance and report certain data to the Attorney General regarding compliance rates for all providers who are subject to the training requirement
WORKFORCE AND OFFICE SAFETY ISSUES
CMA Position: Sponsor
Enhances criminal penalties for an assault or battery committed against a physician, nurse, or other health care worker of a hospital engaged in providing services within the emergency department , making such crimes punishable by imprisonment in a county jail not exceeding one year, by a fine not exceeding $2,000, or by both that fine and imprisonment . Authorizes a health facility that maintains and operates an emergency department to post a notice in the emergency department stating that an assault or battery against staff is a crime, and may result in a criminal conviction
Requires the Division of Occupational Safety and Health, before December 1, 2027, to submit a draft rulemaking proposal to revise specified regulations on first aid materials and emergency medical services to require first aid materials in a workplace to i nclude naloxone hydrochloride or another opioid antagonist approved by the United States Food and Drug Administration to reverse opioid overdose and instructions for using the opioid antagonist . Requires the division’s regulations to provide guidance to employers on proper storage. Also requires the Occupational Safety and Health Standards Board to consider adopting revised standards relating to the above by December 1, 2028. Expressly reiterates existing law protecting from civil liability an individual who administers naloxone hydrochloride or another FDA-approved opioid antagonist in a suspected opioid overdose emergency
SB 909 (Umberg) – Steven M. Thompson Physician Corps Loan Repayment Program
CMA Position: Support
Eliminates the $105,000 maximum limit for loan repayments per eligible licensed physician Adds psychiatry to the list of primary specialty areas Decreases service obligation in a medically underserved area from 3 years to 2 years. Authorizes the Department of Health Care Access and Information to create additional positions, not using funds from the Medically Underserved Account for Physicians, for specialties outside of the primary specialties and that are not subject to 20% limit of available position s
For more information on these and other new health care laws, visit cmadocs.org/newlaws 2025.
In Memoriam
In Memoriam
ANGE MOUTAPPA, MD
1942- 2025
Dr. Ange Mouttapa, beloved pediatrician in Stockton, California, passed away peacefully at Hospice of San Joaquin on January 25, 2025, at the age of 82. He was born on November 23, 1942, in Hanoi, Vietnam. He dedicated his life to the care and well-being of children, leaving a lasting impact on countless families throughout his career.
Dr. Mouttapa earned his medical degree from the Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER) in Pondicherry, India, in 1967. Shortly after completing medical school, he married his devoted wife, Rosemary, and together they embarked on a new journey to the United States, becoming the first in both of their families to settle there.
Dr. Mouttapa completed his internship at Rutgers Health in Newark, New Jersey, in 1968, followed by a residency at Montefiore Medical Center, Bronx, New York, in 1970, and a second residency at Harlem Hospital Center in Manhattan in 1972. He began practicing Pediatrics in Little Falls, New York, before relocating to and practicing in Tracy, California, in 1973. In 1977, he moved his young family to Stockton, California, where he eventually partnered with Dr. Rene Marasigan and later with Dr. Danilo Yumul. Dr. Mouttapa provided compassionate and selfless care to his community until his retirement in 2015. Having lived in Stockton for nearly 48 years, he developed a deep affection and sense of responsibility for his community, which he considered home. He was a member of the San Joaquin Medical Society for 51 years.

Outside of work, Dr. Mouttapa was dedicated to his physical fitness. He could often be seen jogging near Delta College or working out at the gym, embodying the same discipline and perseverance that he brought to his medical practice. He traveled with Rosemary to many countries and US destinations. In retirement, he found joy in visiting his grandchildren in Orange County and San Jose, California.
Dr. Mouttapa is survived by his loving wife, Rosemary of 57 years; his son, Peter Mouttapa (Navajothi); his daughter, Michele (Brian) Matek and his cherished grandchildren, Antonio Mouttapa, Hayden and Theodore (Teddy) Matek. His warmth, generosity, sense of humor, acceptance of everyone, and unwavering commitment to both his family and his community will be deeply missed by all who had the privilege of knowing him.
RESID ENTS' REPORT

A PLACE FOR ALL NEWS HIGHLIGHTING RESIDENTS AND GRADUATE MEDICAL EDUCATION
The Resident’s Report is dedicated to all the good news related to our hard-working residents training at San Joaquin General Hospital and St. Joseph’s Medical Center. Please email your submissions, written in third person with accompanying photo to Lisa@sjcms.org.
SJMC Internal Medicine
Residents Start 4th Grade Medicine
Project At McKinley Elementary School
Dignity Health Saint Joseph’s Medical Center Internal Medicine residents kicked off this school year’s 4th Grade Medicine Project in December 2024. Eager, keen and inquisitive McKinley elementary school students each received their own stethoscopes, addressed one another as “doctor”, learned how to check their own pulses, and pondered “what a doctor looks like.” Arthur, one of the classroom educators, observed how nearly all the resident-physicians volunteering at the event looked like his neighbors with which he grew up. Vish Tuchscherer, one of the resident-physicians who helped establish this project last May, expressed how these outreach sessions with curious students remind him of why he became a doctor in the first place.
ABIM Grant resident-physician coordinators
Clarissa Chan, Breeana Hernandez, and Rene Rodriguez under the guidance of Dr. Kwabena Adubofour, continue to coordinate these biweekly Friday sessions to teach, mentor, and encourage kids in the south side of Stockton to become future physicians and to come back to serve their community.




Practice News and Resources
Free to SJMS/CMA Members!

The Office Managers Forum empowers physicians and their practice manager staff with valuable tools via expert led education sessions from industry professionals who are committed to delivering quality healthcare. This quarterly forum is normally held on the second Wednesday of March, June, September and December at Papapavlo's in Stockton.
Registration is required!
If you don’t receive an invitation via E-Mail, please email Jessica@sjcms.org
March 12th, 2025: 11:00AM to 1:00PM
2025 Employment Law Updates

Discover how to navigate complex employment law changes and stay on track for a successful year. This will help businesses navigate California’s challenging employment and labor laws.
Jamie Bossuat, a shareholder and employment lawyer at Kroloff will present an update on the most pressing issues in employment law and will offer practical suggestions for reducing liability. Issues will include recent changes in wage and hour requirements, updates to leave of absence laws, and current litigation trends.
June 11th, 2025: 11:00AM to 1:00PM
Know Your Rights: How to Identify and Stop Unfair Payment Practices
• Claim submission deadlines
• How much time does a payor have to pay my claim?
• What are the interest and penalty requirements for late payment?
• What are my appeal rights and how much time do I have to appeal?
• How do I get my contracted fee schedule?
• What are my rights regarding notices of overpayment?!

Mark Lane, Associate Director in the CMA’s Center for Economic Services, began his career as a claims processor for plans such as Blue Shield and Health Net. Over the next 18 years, his experiences in claim operations, customer service, provider relations and contracting have allowed him to get a unique vantage point on the relationship between physicians and payors. Having experienced the physician-payor relationship from both ends, Mark is able to understand the needs and positions of the respective sides, making him an ideal candidate to educate providers on overcoming the ever-changing challenges of the healthcare landscape.
CMA PRACTICE RESOURCES
DWC updates workers’ compensation physician fee schedule
UHC delays Designated Diagnostic Provider program in CA until Jan. 1, 2022
The California Division of Workers’ Compensation (DWC) recently updated its Official Medical Fee Schedule for Physician Services/Non-Physician Practitioner Services to conform to relevant 2025 changes in the Medicare payment system. The update is effective for dates of service on or after February 1, 2025.
The new fee schedule includes the following adjustments:
• Updated relative value units
• Updated CPT coding
• Updated conversion factors
• Updated National Correct Coding Initiative Edits
• Updated Table A – anesthesia conversion factors adjusted for Geographic Practice Cost Index localities
• Updated telehealth list
Questions can be directed to DWC at DWCFeeSchedule@ dir.ca.gov. The order and related documents can be found on the DWC OMFS physician fee schedule webpage.
Medi-Cal phasing out transaction services, providers must use Provider Portal
Effective January 20, 2025, all Medi-Cal providers must be registered for the Medi-Cal Provider Portal in order to perform electronic transactions with Medi-Cal. After that date, providers will no longer be able to login using an NPI through Transaction Services and will be required to log in through the Provider Portal.
This is part of a series of changes being implemented by the California Department of Health Care Services (DHCS) to enhance electronic tools and services for Medi-Cal providers and submitters. According to DHCS, these changes are geared toward improving the user experience, promoting user self-service and enhancing security.
Providers are encouraged to register as soon as possible to prevent interruptions in day-to-day electronic transactions with Medi-Cal. To register, an authorized representative of the organization should call the Medi-Cal Telephone Service Center at (800) 541-5555 to be issued an electronic registration token.
The following information will be required:
• Provider Employer Identification Number/Social Security Number
• Unique email address
• Valid phone number
Public Health Update

Refresh San Joaquin: Reimagining Retail for Better Health
BY ANKEETA SASEETHARRAN, MPH AND ROSAELENA MENENDEZ, MPH
A healthy diet is linked to a lower risk of obesity, heart disease, type 2 diabetes, and certain cancers, which is why it is a key factor in chronic disease prevention. Marketing and accessible placement of fruits and vegetables can encourage purchases of healthy foods and beverages. Unfortunately, many neighborhoods in San Joaquin County experience inadequate access to these healthy products, and the advertising of unhealthy foods and beverages further reinforces unhealthy eating patterns among individuals.1
HISTORY AND GOALS OF REFRESH SAN JOAQUIN
To address the problem of inadequate access on an environmental level, San Joaquin County Public Health Services (PHS) programs, including CalFresh Healthy Living (CFHL), Smoking & Tobacco Outreach/ Prevention (STOPP), and Lifetime of Wellness, came together to create the Refresh San Joaquin program in 2016. The goal was to improve the health of residents by increasing the availability of healthy foods, fresh produce, and low or no-sugar beverages, while decreasing the harmful effects of unhealthy products and advertising in the community.
REFRESH SAN JOAQUIN NOW


The program has targeted smaller retail stores in low-income areas of the County that do not have full-service grocery stores nearby. Retailers participating in the Refresh San Joaquin receive support from PHS to help promote customer demand for fresh, healthy foods, and decrease access to alcohol and tobacco. This includes healthy product marketing materials, store layout improvement assistance, information on store improvement grants, training on how to market healthy food, food demonstrations, and CalFresh EBT application assistance.
Stores participating in the program receive Bronze, Silver, or Gold awards based on the improvements they make to promote healthy products and decrease the presence and marketing of unhealthy products in the store. There are currently six participating stores: Acambaro Meat Market, Arteaga’s Food Center, Discount Liquor Store and Mini Mart, El Molcajete East Side Market, La Raza Market & Produce, La Perla de Guadalajara, and Los Hermanos Meat Market. Mi Ranchito Market & Carniceria was a past participant in the program.
STORE IMPROVEMENTS
Refresh San Joaquin has provided stores with decals and posters to encourage healthy food choices. The program has also placed “shelf-talkers” in English and Spanish on store shelves to draw attention to healthy foods and beverages. These “shelf-talkers”
are point of decision signs that provide information on how to incorporate a particular healthy product into a meal (e.g., one sign recommends shoppers to add vegetables to a tuna sandwich).
THE NEED FOR NUTRITION EDUCATION
Food environment is one key part of the picture. Shoppers’ choices are another. As recommended, participating stores have attempted to offer healthier milk (i.e. low-fat milk) and bread (i.e. whole wheat bread), for example, but they did not sell as well and spoiled on the shelves. This often results in stores reverting back to stocking more of what sells, which are usually the less healthy alternatives.
Facilitating nutrition classes for adults who visit these stores would be beneficial to educate them on the importance of making healthy food choices. Nutrition education needs to be culturally appropriate, sensitive to ethnic customs and literacy levels, and offered in languages other than English. Most patrons of participating stores are Spanish speakers, so this is a key language for education. The CFHL team has hosted in-store
food demonstrations in the past and found that providing healthy recipes similar to those found in ethnic cuisines, such as ceviche, fare better with customers than non-ethnic recipes.
A ROLE FOR HEALTH CARE PROVIDERS
Since there is a lack of third places to host these classes in the neighborhoods where participating stores are located, health care clinics are a great venue to provide nutrition education to adults who do not regularly visit community centers or utilize other community resources.
Health care providers already have good rapport and trust with their patients, and are in a key position to provide education on the importance of diet to one’s health to each of their patients. Some tips to consider when discussing nutrition with patients include:
1. Personalize nutrition tips to the patient’s health status, lifestyle, and cultural preferences.
2. Collaborate with registered dietitians, nutritionists, or community health workers to improve the reach of nutrition education.
3. Provide patients with resources, such as healthy recipes, easy-to-understand handouts, and digital tools (e.g. apps) to reinforce the advice given during visits
LOOKING AHEAD
Refresh San Joaquin is working to partner with more small retailers across the county to increase education and access to healthy foods in more neighborhoods. The team is exploring ways to provide nutrition education to store patrons to support the changes made in their stores. PHS remains committed to finding more ways to provide accessible and comprehensive educational resources.
References
https://healthmed.org/how-does-advertisinginfluence-healthy-food-choices/



San Joaquin Medical Society
3031 W. March Lane, Suite 222W
Stockton, California 95219-6568
RETURN SERVICE REQUESTED
Our Efforts in Motion
HIE Grant Funding Underway
Health Plan of San Joaquin/Mountain Valley Health Plan (“Health Plan”) is continuing to strengthen connections between healthcare providers and the Health Plan-supported Health Information Exchange (HIE). To bolster data sharing initiatives, Health Plan committed $8.775 million in community investment funds for an HIE grant program.
To date, we have approved over $3M in grants for Basic HIE, Admission, Discharge, and Transfer (ADT) Data, Healthcare Effectiveness Data and Information Set (HEDIS) Data Aggregator Validation (DAV) Certification and more!



Benefits of Connecting to an HIE
Access patient data created outside of your office/facility
Close gaps in care to improve quality measures
Share information between healthcare providers
Avoid duplicating services
Health Plan is committed to supporting traditional and non-traditional providers through our HIE grant program. We have awarded funding to 14 providers and HIE grant applications are still being accepted!
Share the information with someone in your network!

www.hpsj.com/ community-reinvestment
