HEALTH, LIFE & HIV



Advocating for women living with HIV
This is only a brief summary of important information about BIKTARVY® and does not replace talking to your healthcare provider about your condition and your treatment.
BIKTARVY may cause serious side e ects, including:
Worsening of hepatitis B (HBV) infection. Your healthcare provider will test you for HBV. If you have both HIV-1 and HBV, your HBV may suddenly get worse if you stop taking BIKTARVY. Do not stop taking BIKTARVY without fi rst talking to your healthcare provider, as they will need to check your health regularly for several months, and may give you HBV medicine.
BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in adults and children who weigh at least 55 pounds. It can either be used in people who have never taken HIV-1 medicines before, or people who are replacing their current HIV-1 medicines and whose healthcare provider determines they meet certain requirements.
BIKTARVY does not cure HIV-1 or AIDS. HIV-1 is the virus that causes AIDS.
Do NOT take BIKTARVY if you also take a medicine that contains:
dofetilide
rifampin
any other medicines to treat HIV-1
Tell your healthcare provider if you:
Have or have had any kidney or liver problems, including hepatitis infection.
Have any other health problems.
Are pregnant or plan to become pregnant. Tell your healthcare provider if you become pregnant while taking BIKTARVY.
Are breastfeeding (nursing) or plan to breastfeed. Talk to your healthcare provider about the risks of breastfeeding during treatment with BIKTARVY. Tell your healthcare provider about all the medicines you take:
Keep a list that includes all prescription and over-thecounter medicines, antacids, laxatives, vitamins, and herbal supplements, and show it to your healthcare provider and pharmacist.
BIKTARVY and other medicines may a ect each other. Ask your healthcare provider and pharmacist about medicines that interact with BIKTARVY, and ask if it is safe to take BIKTARVY with all your other medicines.
BIKTARVY may cause serious side e ects, including:
Those in the “Most Important Information About BIKTARVY” section.
Changes in your immune system. Your immune system may get stronger and begin to fight infections that may have been hidden in your body. Tell your healthcare provider if you have any new symptoms after you start taking BIKTARVY.
Kidney problems, including kidney failure. Your healthcare provider should do blood and urine tests to check your kidneys. If you develop new or worse kidney problems, they may tell you to stop taking BIKTARVY.
Too much lactic acid in your blood (lactic acidosis), which is a serious but rare medical emergency that can lead to death. Tell your healthcare provider right away if you get these symptoms: weakness or being more tired than usual, unusual muscle pain, being short of breath or fast breathing, stomach pain with nausea and vomiting, cold or blue hands and feet, feel dizzy or lightheaded, or a fast or abnormal heartbeat.
Severe liver problems, which in rare cases can lead to death. Tell your healthcare provider right away if you get these symptoms: skin or the white part of your eyes turns yellow, dark “tea-colored” urine, light-colored stools, loss of appetite for several days or longer, nausea, or stomach-area pain.
The most common side e ects of BIKTARVY in clinical studies were diarrhea (6%), nausea (6%), and headache (5%).
These are not all the possible side e ects of BIKTARVY. Tell your healthcare provider right away if you have any new symptoms while taking BIKTARVY.
You are encouraged to report negative side e ects of prescription drugs to the FDA. Visit www.FDA.gov/medwatch or call 1-800-FDA-1088. Your healthcare provider will need to do tests to monitor your health before and during treatment with BIKTARVY.
Take BIKTARVY 1 time each day with or without food.
This is only a brief summary of important information about BIKTARVY. Talk to your healthcare provider or pharmacist to learn more.
Go to BIKTARVY.com or call 1-800-GILEAD-5.
If you need help paying for your medicine, visit BIKTARVY.com for program information.










People featured are compensated by Gilead.










*Source: IQVIA NPA Weekly, 04/19/2019 through 05/19/2023.
















“I’ve learned how to live with HIV, and my children and my family are a huge part of that.”
MARICELA SWITCHED TO BIKTARVY®
Ask your healthcare provider if BIKTARVY is right for you. For her today and her tomorrow.






BIKTARVY is a complete, 1-pill, once-a-day prescription medicine used to treat HIV-1 in certain adults. BIKTARVY does not cure HIV-1 or AIDS.






#ADVOCACY

Fighting against HIV and AIDS has always been a struggle. Much work remains to end the epidemic. POZ encourages you to get involved in advocacy. Go to poz.com/ advocacy to find the latest news and learn how you can make a difference in the fight.
D #CRIMINALIZATION

Advocates around the world are working to change laws that criminalize HIV, which harm people living with the virus. For more information and to learn how to get involved in reform efforts to make such laws reflect current science, go to poz.com/criminalization
D #UNDETECTABLE

The science is clear: People who have an undetectable viral load don’t transmit HIV sexually. In addition to keeping people healthy, effective HIV treatment also means HIV prevention. Go to poz.com/undetectable for more.
D
POZ DIGITAL

Scan the QR code (left with your smartphone camera or go to poz.com/digital to view the current and past issues online.

Valencia Landry is a Texas-based HIV advocate.


22 BE THE LIGHT Bridgette Picou, a nurse living with HIV, helps women advocate for themselves. BY ALICIA GREEN
28 SHARING KNOWLEDGE THROUGH ART A new illustrated book raises awareness about HIV. BY TIM
MURPHY
3 FROM THE EDITOR With a Little Help From My Friends
4 POZ Q&A
ACT UP veteran Keiko Lane puts her memories to paper in Blood Loss: A Love Story of AIDS, Activism, and Art
6 POZ PLANET
AIDS Quilt records get digitized • HIV clinic opens in Minneapolis • Maine insurer agrees to cover common HIV treatment • POZ Stories: Evaline Beaird • $4 million to advance viral load detection
• Everyday: milestones in the epidemic • Positive Destinations, an online travel resource • AIDS Fund Philly closes
12 VOICES
Winners of the 9th annual POZ Awards, which highlight HIV and AIDS in media and culture, are revealed, and The Well Project centers Black women living with HIV.
14 SPOTLIGHT
R.I.P. Cindy Stine and Bryan C. Jones
16 NUTRITION & FITNESS
Baked falafel • massage therapy
17 BASICS
HIV and the brain
18 CARE & TREATMENT
Breakthrough of 2024: twice-yearly PrEP • U.S. approves positive-to-positive transplants • eighth person may be cured of HIV
• IAS-USA updates HIV recommendations
20 RESEARCH NOTES
Apretude PrEP effective in real-world studies • doravirine/islatravir combo shines in late-stage study • double dolutegravir dose shrinks viral reservoir
32 HEROES
HIV advocate Valencia Landry
EDITOR-IN-CHIEF
ORIOL R. GUTIERREZ JR.
MANAGING EDITOR
JENNIFER MORTON
DEPUTY EDITOR
TRENT STRAUBE
SCIENCE EDITOR
LIZ HIGHLEYMAN
COPY CHIEF
JOE MEJÍA
EDITORIAL ASSISTANT
LAURA SCHMIDT
ART DIRECTOR
DORIOT KIM
ART PRODUCTION MANAGER
MICHAEL HALLIDAY
CONTRIBUTING WRITERS
SHAWN DECKER, OLIVIA G. FORD, ALICIA GREEN, MARK S. KING, TIM MURPHY, MATHEW RODRIGUEZ, CHARLES SANCHEZ
CONTRIBUTING ARTISTS
JOAN LOBIS BROWN, LIZ DEFRAIN, ARI MICHELSON, JONATHAN TIMMES, BILL WADMAN
FOUNDER
SEAN STRUB
LEGACY ADVISER MEGAN STRUB
ADVISORY BOARD
GUILLERMO CHACÓN, SABINA
HIRSHFIELD, PhD, KATHIE HIERS, TIM HORN, PAUL KAWATA, NAINA
KHANNA, JESSE MILAN JR., DANIEL TIETZ, MITCHELL WARREN
PRESS REQUESTS NEWS@POZ.COM
SUBSCRIPTIONS HTTP://ORDER.POZ.COM
UNITED STATES: 212-242-2163
SUBSCRIPTION@POZ.COM
FEEDBACK
EMAIL WEBSITE@POZ.COM OR EDITOR-IN-CHIEF@POZ.COM
SMART + STRONG
PRESIDENT AND COO
IAN E. ANDERSON
EDITORIAL DIRECTOR
ORIOL R. GUTIERREZ JR.
CHIEF TECHNOLOGY OFFICER
CHRISTIAN EVANS
VICE PRESIDENT, INTEGRATED SALES
DIANE ANDERSON
INTEGRATED ADVERTISING MANAGER
JONATHAN GASKELL
INTEGRATED ADVERTISING COORDINATOR
SARAH PURSELL
SALES OFFICE
212-938-2051; SALES@POZ.COM
CDM PUBLISHING, LLC
CEO
JEREMY GRAYZEL
CONTROLLER
JOEL KAPLAN


ITESTED HIV POSITIVE IN 1992. At 22 years old, I had graduated from college but still lived with my parents. As a closeted gay man, my life was suddenly even more complicated. The virus was the cherry on top of a hot mess.
All that changed in 1993 after a little help from my friends. I moved from my parents’ house in Queens, New York, to a shared apartment in the East Village. I found a sense of belonging among like-minded folks. My despair turned into hope, which wasn’t easy to achieve before effective treatment. I’m forever grateful for their support.
As unlikely as it may sound, for many of us living with HIV—me included—the virus eventually pushed us onto a better path than the one we were on. Instead of staying in the closet without a plan for my life, I found a way forward after testing HIV positive. I’d rather that the virus had never entered my life, but I’ll make that lemon into lemonade for as long as I can.
Our cover subject, Bridgette Picou, can relate. In 2012, just before her 40th birthday, she had a sore throat and got antibiotics at a local clinic, which offered her an HIV test. She got an unexpected positive result. After some time to reflect on her new reality, she decided to go to nursing school to become an HIV health care provider. Please go to page 22 to read more about her journey.
Picou’s advocacy, which purposefully spotlights women living with HIV, is a great fit for this special issue of POZ focused on women. We also highlight the efforts of Monica Johnson, Tamela King, Keiko Lane, Evaline Beaird and Valencia Landry.
Monica, a long-term survivor and the founder of the HIV community organization HEROES, based in Louisiana, and her

friend Tamela, a high school art teacher, have produced an illustrated primer on HIV. Many images were created by Tamela’s students. Go to page 28 to learn more and see the artwork.
As a teenager in Los Angeles in the late 1980s and early ’90s, Keiko was one of the youngest members of both ACT UP and Queer Nation. Now a therapist and an author, she has written a memoir of those times. Go to page 4 to read more about her experiences.
As a long-term survivor, Evaline has undergone a lot in her HIV journey. In 1992, she became pregnant, then tested positive for the virus. Married to a military serviceman, she was surprised by the diagnosis, which set off a chain reaction of challenging events. Go to page 8 to find out how she’s coping today.
Valencia knows what it’s like to be an HIV advocate in a conservative state. A native of Louisiana, she now lives in Texas. Since testing positive for the virus in 2005, she has been an outspoken member of her community, helping other people with HIV live with dignity. Go to page 32 for more about her work.
As this issue was going to press, we learned of the passing of two dedicated and respected HIV advocates: Cindy Stine and Bryan C. Jones. Go to page 14 to read remembrances of them.


ORIOL R. GUTIERREZ JR. EDITOR-IN-CHIEF editor-in-chief@poz.com Want to read more from Oriol? Follow him on X @oriolgutierrez and check out blogs.poz.com/oriol.





ACT UP veteran Keiko Lane puts her memories to paper.
KEIKO LANE, A LOS ANGELES–BASED THERAPIST AND AUTHOR, was only a high schooler when she joined ACT UP LA and Queer Nation in the late 1980s and early ’90s.
Through those AIDS and LGBTQ activist groups, she met older queer people who became her mentors, protectors and “chosen family”—among them men living with AIDS with whom she became incredibly close, only to witness their deaths in the years ahead. Lane left LA for college but has for decades carried the memories of those years of protest, performance art, parties and self-discovery.
Now, she has captured them in Blood Loss: A Love Story of AIDS, Activism, and Art (Duke University Press), a deeply poetic and moving memoir of a queer political immersion at an early age. Lane talked with POZ about her book.
You’re a longtime therapist with a strong focus on HIV and AIDS and LGBTQ issues. Did your early activism lead you to that career?
I’m sure it did. In LA, there was so much organizational overlap between Queer Nation and ACT UP, but people took different tracks—some were good at policy, or art and graphics, or community mobilization. But I was more interested in the care work [of being in those groups] and the slowness of intimacy. There was so much franticness to working on policy and a sense of urgency, but it wasn’t my comfort zone. It took me a long time to figure that out.
When did you get the idea for this memoir, and how did you go about writing it? I was always writing about it, but my first literary training was in poetry, not
prose. I tried to write this as fiction about 15 years ago, but it didn’t work for me. I had no experience as a fiction writer, and I felt like I didn’t quite know what I was doing.
And I was fictionalizing it to not have to deal with myself, but then, I also felt like I wasn’t doing justice to these incredible people whom I’d loved—and still love. To fictionalize them felt like a disservice.
But it still took me a long time to figure out how to write this as a memoir. [The performance artist] Ron Athey [a key figure in the LA scene] was giving a lecture about 10 years ago, and I was there.
As part of a slideshow, he showed one of the covers of [the zine] Infected Faggot Perspectives, which Cory [Roberts-Auli, an artist who died of AIDS in 1996] and I produced after Wayne [Karr] died in 1995. I asked Ron, “Are you writing about Cory?
Someone should.” He said, “It’s your turn—you do it.”
So when I started, I thought I was writing a long-form essay about Cory’s art practice and resisted for a year or two the idea that I was telling a bigger story that I was a significant character in. I was grappling with how to bring myself into the story and center my voice in a way that felt ethical and made it clear that I was remembering from my own subjectivity and not trying to write biographies about them.
Didyouworkfromsomesortofoutline?
I didn’t have one for a long time. I started with the questions I was obsessed with, that I couldn’t let go of—that first section about how we remember things. Then, a draft or two in, once I felt like I had the feeling of all of us, I went back and started making a political timeline—of what we were fighting policy-wise when this or that particular personal thing happened.
The years in question are the late 1980s and early ’90s.
I’d started doing coalition-building work with ACT UP. In LA in the late 1980s, if you wanted to mobilize the left fast for a demonstration, you called ACT UP, you called the Student Coalition, a young person’s activist group that initially formed around apartheid, and you called CISPES, which was the Committee in Solidarity with the People of El Salvador. I’d started going to ACT UP demonstrations in 1989 and meetings of ACT UP and Queer Nation in early 1991, when I was 16.
What was proximity to so much illness, death, grief and loss like at that age?
From the age of 12 or 13, I’d already been involved in activism—working in community with refugees and asylum seekers, at demonstrations against police brutality in LA and at demonstrations at the South African Consulate in LA against apartheid, so that was already my normal.
So when I was in ACT UP and Queer Nation, I was heartbroken and traumatized a lot, but I also couldn’t imagine walking away from the sense of com-
munity those groups gave me as a young person. And because I was one of the youngest in the group, if not the youngest, I was loved and taken care of. People were very protective of me.
How do you think the experience shaped you?
It’s both an easy and complicated answer. The easy answer is that I was absolutely traumatized—I think we all were. But there’s often a fantasy that if something has been traumatic, that if we could go back, we wouldn’t do it again. But if I had to go back, I wouldn’t walk away from it just to avoid loss.
in the room, but the People of Color Caucus was extremely loud. The people I was closest to weren’t the white people on the problematic side but rather the folks of color and the white people coming out of antiracist organizing.
Did you feel no fear about the risk of getting HIV?
The virus wasn’t as big a fear for me as the fear of losing people and hence grasping at the kind of intimacies that were available to us.
Did people in the groups ever ask you what you were doing there? Or were you ever self-conscious about being


“I was loved and taken care of.”
Youwriteinthebookaboutyourmother, who is Okinawan and was born in a U.S. internment camp for Japanese Americans during WWII. Do you think that family history shaped you in any way? I grew up knowing about that as a story in my family that was told in a pretty matter-of-fact way. Understanding the emotional toll of it was something I came to much later.
A lot of the people in your inner circle were people of color, like yourself. What percentage of ACT UP LA was people of color?
I’m not the political historian of the group, like the people working on the ACT UP LA Oral History Project. I have no idea what the percentages were like overall at different points in time.
Among my close circle of friends, family and comrades, I remember the percentage being about half or more than half. There was a lot of whiteness
HIV negative while in the company of so many people with AIDS?
I was most self-conscious when faced with the decision of leaving to go away to college. I could leave. I wouldn’t be surprised if some people had critiques or questions about me, and I would’ve understood. But also, by the time I started going to ACT UP meetings, I had a solid group of people I’d been going to Queer Nation with whom I was very close to. So that was another buffer.
Why was it important for you to tell this story?
I wanted to show how I was shaped by it and also how those of us who are left have continued to be with each other.
The question that organizes my life is “How did we end up who we are?” And when I ask that question about myself, those years are so core for me. I’ve always felt responsible for remembering because [most of them] are no longer here. ■


The archive is reunited with digitized Quilt panels.
The Library of Congress (LOC) has released an online collection of the National AIDS Memorial Quilt Records, making one of the most poignant symbols of the AIDS epidemic in the United States available to a global audience. As the largest communal art project in the world, the AIDS Memorial Quilt honors the lives of Americans who have died of AIDS since 1981, when the disease was first identified.
Released to coincide with World AIDS Day 2024 commemorations, the newly digitized collection offers a unique window into the deeply personal stories behind the 55-ton quilt and its panels. The digitized collection, totaling more than 125,000 items, includes letters, diaries, photographs and other materials documenting the lives of those represented in the Quilt.
The digitized archive is now reunited online with the communal folk art of the quilt panels. Together, these digitized collections will be a boon for researchers, families of those lost to AIDS, policymakers and more. While the Quilt itself is housed at the National AIDS Memorial in San Francisco, its voluminous records have been entrusted to the American Folklife Center at LOC since 2019.
“The digitized AIDS Memorial Quilt Records collection is a major milestone not only in our preservation efforts but also in ensuring that the stories, lives and collective memory of those lost to the AIDS epidemic remain accessible to future generations around the world,” said Librarian of Congress Carla Hayden.
The Quilt, first created by community volunteers in San Francisco in 1987, has not only been a testament to the lives lost to AIDS but also a tool for advocacy and a reminder of the impact of the epidemic on a local, national and global scale.
“The National AIDS Memorial is so appreciative of this historic partnership with the Library of Congress and the American Folklife Center for stewarding the AIDS Memorial Quilt collection forward and completing its digitization,” said John B. Cunningham, chief executive officer of the National AIDS Memorial. “Through this project, the power of the collection will now be available to all through the digital platform and can now be reunited with the Quilt panels to which they were originally connected. This collection keeps the stories of the lives cut short alive and allows society to learn from them.”
LGBTQ activist Cleve Jones created the Quilt’s first panel in honor of his friend Marvin Feldman, a 33-year-old actor who died of AIDS-related illness in 1986.
“There’s a promise in a quilt. It’s not a shroud or a tombstone,” Jones said, reflecting on the Quilt’s significance. “I don’t want to stop remembering Marvin Feldman and all the other friends of mine who have gone.”
Top left: The Quilt in Washington, DC; top right: roses laid on the Quilt; bottom: sewing machine used by volunteers to stitch Quilt panels
Similarly, Judy Soons, a mother who lost two of her six children, Sydney and Jim, to AIDS, crafted a shared panel to commemorate the closeness of her sons. Soons channeled her grief into supporting others, drawing strength from the community formed through the Quilt.
One Quilt panel honors the late Sylvester James, a gay, African-American disco star, who became a symbol of the fight for LGBTQ equality. Known for his bold and unapologetic embrace of his identity, James rose to international fame with his anthem “You Make Me Feel (Mighty Real)” serving as a soundtrack for sexual and gender liberation movements. His life and legacy continue to inspire generations, celebrating resilience, self-expression and joy in the face of adversity.
Digitization of the archive was made possible by the generous support of the Ford Foundation, which provided core funding for LOC’s “For the People: Fund for Powering Knowledge,” designed to connect Americans with important social movements and showcase how they shape the fabric of American life and government.
The AIDS Memorial Quilt Records, totaling over 200,000 items, offer an intimate look at artifacts such as photos, manuscript letters, diaries, greeting cards, notebooks, tributes, obituaries, epitaphs, pamphlets, fabric swatches and original artwork. More than half the collection has now been digitized, allowing the public to engage with and reflect on this important piece of history. —LOC.gov


The Aliveness Project, an HIV community center in Minneapolis, opened its first Thrive clinic in the city, which supports Minnesotans living with and at risk for HIV. In the near future, the clinic will also include a pharmacy.
For nearly 40 years, the Aliveness Project has provided free HIV services to thousands of Minnesotans. Both the Aliveness Project and the Thrive clinic are located near Nicollet Avenue and 38th Street.
While the Aliveness Project offered people links to HIV resources, the new Thrive clinic provides free HIV support services on site, including HIV testing, counseling and prescriptions for pre-exposure prophylaxis (PrEP), medications used by HIV-negative people to reduce their risk of contracting HIV. Currently, PrEP is available as daily tablets and a long-acting injectable given every two months.
“There are a lot of primary [care] providers who, for whatever reason, are uncomfortable prescribing PrEP, which doesn’t make any sense to me. It’s no different than giving somebody a vaccine,” Thrive clinical services director Matthew Hoppe told the Minnesota Daily. “We eliminate as many barriers as we can. We try to make it as easy as possible and as low cost as can be.”
Hoppe said he is the highest-prescribing injectable PrEP provider in the state. What’s more, the clinic already sees between seven to 15 clients a day, whether for various forms of PrEP, mental health issues or other reasons.
Almost 10,000 people in Minnesota are living with HIV; an additional 1,100 people are unaware of their HIV-positive status, according to the Minnesota Department of Health. In 2023, 324 Minnesotans were diagnosed with HIV, up about 24% from 2022.
What’s more, Minnesota is currently experiencing HIV outbreaks in several areas of the state. State officials encourage health care providers to offer HIV testing to those who are at risk. —Laura Schmidt
The Maine health plan responded to a discrimination complaint.
Harvard Pilgrim Health Care’s health insurance plans in Maine reversed course and will now cover Biktarvy along with four other HIV medications. The change came about after health advocates led by the HIV+Hepatitis Policy Institute filed a discrimination complaint with the Maine Bureau of Insurance, which investigated the matter.
HIV+Hep filed similar complaints against Harvard Pilgrim plans in Rhode Island and New Hampshire. The advocacy group notes that Rhode Island health insurance officials had rejected the advocates’ discrimination claim against Harvard Pilgrim.
Biktarvy (bictegravir/tenofovir alafenamide/emtricitabine) is the most commonly prescribed HIV therapy today; indeed, about half of people on HIV treatment take this combo pill, according to HIV+Hep. The once-daily single-tablet regimen, manufactured by Gilead Sciences, was approved by the Food and Drug Administration in 2018.
National HIV treatment guidelines list four recommended regimens for initial therapy and alternatives for specific situations. It is standard practice for health insurance plans to cover these treatments; failure to do so is considered discriminatory.
Harvard Pilgrim Health Care (also known as Point32 Health) in Maine will now cover those regimens. Harvard Pilgrim is one of two options for people who are enrolled in the Maine AIDS Drug Assistance Program.
“While this action is certainly welcome, the fact remains that Harvard Pilgrim removed lifesaving HIV drugs from its coverage formulary, disrupted the treatment of people living with HIV and violated the nondiscrimination protections [of the Affordable Care Act (ACA), or Obamacare],” said Carl Schmid, executive director of HIV+Hep. “This demonstrates the need for greater oversight of the health insurance industry and enforcement of the safeguards in place to protect patients against the abuse of insurers.”
The Maine Bureau of Insurance noted that as a result of its investigation, all health insurance plans available on CoverMe.gov (the website for Maine’s health insurance marketplace) will cover Biktarvy on their 2025 formulary plans. —Trent Straube

Long-term survivor Evaline Beaird learned she was HIV positive during a pregnancy.
I tested positive in April 1992. I probably acquired it in 1991 because when my husband returned from the Gulf War, I was sick with flu-like symptoms for two weeks. I had a fever of 104°F, a red rash on my face, body aches, chills, loss of appetite and was vomiting.
My husband went to school in Fort Gordon, Georgia, to change his military occupation specialty. I stayed in Columbus, Georgia, working in the accounting department at Aflac and attending Columbus State University at night to finish my bachelor’s degree in criminal justice.
I had been off birth control pills for about 10 months before deciding it was time to start up again. I scheduled an appointment to go to a nearby military clinic. After the exam, the doctor came back in and told me I was pregnant. She referred me to the Martin Army Community Hospital.
I left confused, as I was not expecting this news. We were not trying to get pregnant. I scheduled an appointment at the hospital.
On the day of my appointment, they drew several tubes of blood and asked if I would like to have an HIV test. I said, “Fine.” Because I was married, I wasn’t worried about the results. I left and went to work and forgot about the blood test. About three or four weeks later while getting ready for work, I received a phone call from a medical case manager who requested I come in as soon as possible and said she could not discuss the matter over the phone. I told her I was on my way to work and very busy and could not come in. She said, “Mrs. Beaird, I have to inform you that if you don’t come in I will send the MP [military police] escort to
come pick you up.”
I started laughing. I thought my boss or friends were playing a cruel joke on me. I told the lady I would have to call her back. I called my boss to see if she was in on the joke and told her what the lady had said. She said, “That sounds serious—you should go.”
I went to the office, which was located at Fort Benning. When I arrived, I checked in at the front desk and sat for a few minutes before a lady came and escorted me back to her office. She asked me to verify my name and other information. Then she looked at me and said my blood had tested positive. I said it had to be a mistake. She said she thought so too and asked me to come in to give another blood sample to retest. It would take about a week or so to get the results. I was sure there had been a mix-up in the lab.
About a week later, she contacted me and asked me to come in. When I arrived, I was taken back to her office. After verifying my personal info, she said the new blood sample tested positive too. I gave another blood sample, and she said she would hand-deliver it to the lab herself to make sure it did not get mixed up with any other blood samples.
I waited to get the results. She called and requested I come back into the office. The results were also positive. I gave another sample, and after the third test, she said “Mrs. Beaird, we have to believe your test results are truly positive. We have to follow protocol and contact your husband’s commander and make him aware of what is happening and get the soldier tested.” She told me she was sure his test would be positive and asked if I would be OK. I forgot all about being pregnant at this point.
I don’t remember even telling my husband about the pregnancy. I didn’t know what or how to feel. I had to deal with an HIV diagnosis and the pregnancy news.
Evaline Beaird
I went back to work. I wanted to share the news with my supervisor, but the case manager had cautioned me not to tell anyone at work. I was afraid they would fire me so fast I wouldn’t see it coming. I lied to my supervisor and told her they had to give me a test to determine if something was wrong with my baby.
My husband tested positive. He had orders to be deployed overseas to Germany, but after the positive HIV test, the orders were canceled, and he was deployed stateside to Fort Carson, Colorado. I ended up quitting my job and moving to Colorado and found an apartment the first week there.
After living in Colorado, my husband, son and I relocated to Tennessee. We had another son. He lived for only a few months. We were told he was HIV negative but found out later he was HIV positive. He was born June 18, 1996, and died of RSV and other complications on January 19, 1997. My husband died of non-Hodgkin lymphoma on Father’s Day in 1999.
Today, I am living and thriving in Tennessee. I have a son who is in his 30s. I am a member of the Nashville Regional HIV Planning Council, and I work parttime at Nashville CARES as a HealthyU peer associate. I had to learn to advocate for myself through attending workshops, conferences, support groups and working at nonprofit agencies. I am sharing my story to help break down the shame, silence and stigma surrounding the virus.

What three adjectives best describeyou?
Resourceful, organized, creative.
What are your greatest achievements?
Graduating from college and raising an African-American son without a mate.
Do you have any regrets? I regret not doing HIV advocacy sooner. I regret not being a better money manager as a teenager and in my 20s.
What keeps you up at night?
Fear about the future of this world; not having enough money to live my best life.
If you couldchange one thing about living with HIV, what would it be?
The criminalization of it.
What is the best advice youeverreceived?
Live your life. People are going to talk about you regardless.
What person in the HIV communitydoyou mostadmire?
Sheryl Lee Ralph.
What drives you to do what you do?
Getting rid of the internal stigma that I allowed to be deposited into my psyche.
Read other POZ Stories or share your own at poz.com/stories.
Three companies receive more than $4 million in funds.
The National Institutes of Health (NIH) has awarded more than $4 million in funds and support services to three diagnostic technology developers as part of the Rapid Acceleration of Diagnostics (RADx) Tech’s Advanced Platforms for HIV Viral Load Monitoring program.
Launched in 2024 by the National Institute of Biomedical Imaging and Bioengineering (NIBIB), in collaboration with the NIH Office of AIDS Research and the National Institute of Allergy and Infectious Diseases, the program is aimed at advancing HIV viral load detection technologies for use at the point of care.
The awardees are Cepheid in Sunnyvale, California; Baebies, Inc., in Durham, North Carolina; and Prompt Diagnostics in Baltimore.
NIHsupported research has shown

that when the virus is undetectable in the bloodstream of people living with HIV who are on effective treatment, sexual transmission does not occur—a concept known as Undetectable Equals Untransmittable (U=U). U=U is a game changer because it enables people with HIV and their partners to be in a relationship without fear of transmitting HIV.
HIV is still in the body when viral load is suppressed, even when it is undetectable. Under some circumstances, HIV viral load may increase to detectable levels, leading to the potential for viral transmission and disease progression.
“For those with HIV, easy access to viral load monitoring empowers them to protect their health and helps
prevent viral transmission,” said Bruce J. Tromberg, PhD, NIBIB director and leader of the RADx Tech program. “NIH support is aimed at making rapid progress in pointofcare HIV viral load detection technologies so that this information is readily available on demand for all who want it.”
The awards mark the advancement of these projects to receive individual contracts and begin milestonedriven activities during 2025. Each technology will be honed under the guidance of a national network of expert technical, clinical, commercialization and regulatory advisers assembled by the RADx Tech program. —NIH.gov
poz.com/aidsiseveryday
NATIONALWOMEN AND GIRLS HIV/AIDS AWARENESSDAY

19 10





LARRYKRAMER’s essay “1,112 and Counting” on the emerging AIDS epidemic runs on the front page of the New York Native. “If this article doesn’t rouse you to anger, fury, rage and action,” he wrote, “gay men may have no future on this Earth.” (1983)


MY BROTHER’S KEEPER, a movie about identical twin brothers (played by John Lithgow) who sue an insurance company to pay for a lifesaving bone marrow transplant for one of the brothers, who is living with HIV, premieres on CBS. (1995)
14 20

Larry Kramer
The Centers for Disease Control and Prevention launches “TAKECHARGE. TAKETHETEST,” an HIV awareness campaign reminding Black women that they have power to protect themselves against HIV. (2012)

21
NATIONALNATIVE HIV/AIDS AWARENESS DAY
Actor DACKRAMBO, known for roles on Dallas and Another World, dies of AIDSrelated complications at age 52. He was one of the first actors in Hollywood to publicly acknowledge he was living with HIV. After he was diagnosed, he retired from acting and spent the rest of his life raising awareness about AIDS. (1994)



The Global Database on HIV-Specific Travel and Residence Restrictions, an online resource that helps people with HIV plan their travel or relocation with reliable, up-to-date information on regulations that impact them, will now be known as Positive Destinations (PositiveDestinations.info). The combination relaunch/rebranding comes courtesy of the HIV Justice Network (HJN), according to a news release.

While HIVtravel.org served as the world’s most trusted resource for more than 20 years, HJN leaders believe the name Positive Destinations better represents its mission.
Formerly found at HIVTravel.org, the database includes guidance, news, stories about traveling with HIV, a searchable country directory and much more. You can watch a video about Positive Destinations at the HIV Justice’s YouTube channel.
Although the number of countries with HIV travel restrictions has declined in recent years, 56 countries still have some entry regulations for people living with HIV, and seven don’t allow entry at all, including Brunei, Jordan and United Arab Emirates, according to Positive Destinations.
The ability to travel, migrate or relocate safely ought to be available to everyone. For people living with HIV, short- or long-term travel sometimes involves answering questions about their HIV status on visa forms, navigating mandatory health screenings, enduring border officials with limited knowledge of laws and considering access to their HIV treatment while abroad.
Positive Destinations regularly updates its website on regulations that restrict entry, stay and residency based on HIV-positive status as well as access to HIV treatment for nonnationals, according to the website.
“This rebrand to Positive Destinations reflects our commitment to a world where people living with HIV, in all our diversities, can enjoy our human rights and live in dignity, without fear of unjust criminalization, regulation or control,” said HJN executive director Edwin J. Bernard in the release.
With this rebranding, Positive Destinations goes beyond providing information on global travel restrictions. The platform now offers additional tools to help users advocate for themselves, including regularly updated news and resources to challenge unjust restrictions.
The new website features a completely redesigned interface optimized for mobile phones, making it easier to access information on travel and treatment on the go. What’s more, it links users to local organizations in various countries that can help migrants with access to HIV services. The platform also highlights stories of successful advocacy to foster understanding and solidarity.
“With this platform, we aim to amplify the voices of those most affected and build a movement that challenges and changes unjust, unscientific policies,” Bernard said. “Travel or relocation for love, work, family or pleasure should be available to everyone, regardless of HIV status, and we are dedicated to ensuring that every destination is a truly positive destination for all.” —Laura Schmidt
AIDS Fund, an HIV nonprofit that served greater Philadelphia since 1989, shuttered at the end of 2024, according to an announcement posted on Facebook by the AIDS Fund Philly staff and board, who wrote, “With the HIV crisis greatly reduced, AIDS Fund makes bittersweet decision to say ‘Farewell.’”
For many years, AIDS Fund Philly organized the monthly GayBINGO and the annual AIDS Walk—two popular fundraisers.
Beginning in January, the local nonprofit Action Wellness took over production of GayBINGO; the future of the AIDS Walk is to be determined.
AIDS Fund provided emergency financial assistance to people living with HIV disease in the Greater Philadelphia region while providing education and increasing public awareness of HIV/AIDS issues, according to its website.
According to 2022 data, 18,226 people were living with HIV in Philadelphia, which has a total population of about 1.6 million.
AIDSVu.org, which visualizes HIV data, notes that 63% of the city’s HIV population is Black, 17% is Latino and 16% is white. New diagnoses dropped from 445 in 2018 to 381 in 2022.
—Trent Straube

IAS 2025, the 13th IAS Conference on HIV Science, will take place in Kigali, Rwanda, from 13 to 17 July 2025, with pre-conferences on 13 July.




The IAS Conference on HIV Science is the world’s most influential meeting on HIV research and its applications. This biennial conference presents the critical advances in basic, clinical and operational HIV research that move science into policy and practice. Through its open and inclusive programme, the meeting sets the gold standard of HIV science, featuring highly diverse and cutting-edge research.

Z AWARDS 2024
BEST CELEBRITY ADVOCATE
Madonna
In the fifth decade of her career, Madonna hasn’t let up on her HIV advocacy. At each of the stops on her 2024 victory lap of a concert tour, titled Celebration, the pop icon created a living musical memorial to the people she’d known who died of AIDS-related illness as well as many whom she had never met. The singer mined the Instagram account @theAIDSMemorial to gather photos of many people lost to the virus. At several shows, she spoke about how deeply personal the loss was to her.
BEST IN FILM OR TELEVISION
Fellow Travelers
Based on the 2007 novel of the same name, this eight-part miniseries tells the love story between two political staffers, Hawkins “Hawk” Fuller and Tim Laughlin, during and beyond the 1950s Lavender Scare. While the show begins with one moral panic, it spans decades, eventually showing the relationship between the two characters in the 1980s, when Tim is diagnosed with HIV while living in San Francisco. The series gives us American history through a queer lens and packs an emotional punch. The finale includes real panels from the AIDS Memorial Quilt. Travelers went on to receive much critical acclaim, winning a
Peabody Award and earning three Primetime Emmy nominations.
BEST IN LITERATURE
Criminalized Lives: HIV and Legal Violence by Alexander McClelland Despite the many advances made in HIV treatment and prevention since the beginning of the AIDS crisis, the legal framework regarding people with HIV lags woefully behind in many cases. With Criminalized Lives, Carleton University professor Alexander McClelland, a member of the Canadian Coalition to Reform HIV Criminalization, aims to lay out this harmful legal framework. Not only does McClelland dive deep into the ways that Canada’s laws harm people with HIV, but he also emphasizes their disproportionate impact on marginalized people, including people of color, Indigenous people, LGBTQ people and people living in poverty. In addition to McClelland’s own views, the book includes personal stories from people who faced HIV criminalization firsthand.
BEST IN VISUAL ARTS
The Body, The Host: HIV/AIDS and Christianity
Allen Memorial Art Museum, Oberlin, Ohio
There’s no doubt that the relationship between the HIV community and religion
is fraught. While some nuns responded to the early crisis by caring for the sick, some preachers spouted openly serophobic sermons. Regardless of your own take on the relationship between AIDS and religion, Christian iconography is deeply embedded in our collective subconscious, and artists creating works about AIDS often incorporate these images in their pieces. This show explores artists who used Christian motifs to respond to the AIDS crisis as well as concerns regarding “judgment, shame, guilt, suffering, martyrdom, plague, death, redemption, resurrection, salvation through blood and the sacredness of wounded bodies.”
BEST REASON TO KEEP ACTING UP
Project 2025
Project 2025—an overarching conservative vision to reimagine and dismantle the federal government—was launched before the reelection of Donald Trump to the presidency. There is almost no marginalized group of people that won’t be negatively affected by Project 2025, which would endanger the health of all people, workers’ rights, reproductive freedom, LGBTQ rights and more. Some lowlights include consolidating presidential power, reducing spending on fighting poverty and eliminating the Department of Education. ■

“Black Women, Racism and HIV in the U.S.” is a POZ.com blog post by The Well Project, which was a cross-post of a fact sheet from TheWellProject.org. Below is an edited excerpt.
IN THE UNITED STATES AND around the world, Black women living with HIV have been innovators and change-makers in the HIV community and intersecting movements since the earliest days of the pandemic.
Yet Black women’s contributions are regularly ignored or made invisible in the HIV field and in U.S. society in general, where leadership roles have historically been held by white men. This disregard is a symptom of the same cause driving HIV among Black women.
According to the Centers for Disease Control and Prevention, U.S. Black women are 10 times more likely to be diagnosed with HIV than their white counterparts, and between 44% and 62% of Black women of transgender experience (trans women) are estimated to be living with HIV.
Most health experts report that this health disparity is caused by structural determinants of health, including poverty, racism, gender inequality and ableism, caused by generations of white supremacist ideology among individuals and throughout society. Due to these complex, intersecting biases, Black women living with HIV experience stigma in profound and multifaceted ways. Some may face exclusion from support networks and communities or experience layers of
rejection, abandonment and neglect.
For many Black women living with HIV, these struggles may lead to internalized stigma, isolation or shame. Some may withdraw from social interactions. These combined effects often increase stress, anxiety and depression, affecting access to care, mental health and overall well-being. Stigmas, biases and stereotypes may ripple into every facet of their lives, following them into the health care, educational, justice, economic and political systems.
To be Black, a woman and living with HIV in a society that has historically hailed whiteness, maleness and wellness as the pinnacle of humanity is to be in a consistent quest to maintain personal power. Personal power involves having autonomy, confidence and the capacity to make decisions that shape one’s destiny.
Possessing personal power as a Black woman living with HIV means acting with purpose and direction despite the opposition. Miraculously, many Black women living with HIV continue to overcome generations of oppression while working to end HIV-related stigma, decrease HIV transmissions and bring awareness to vulnerable communities.
The redistribution of power necessary to improve the overall well-being
of Black women living with and impacted by HIV will require the strategic, consistent and long-term effort of people from all walks of life. Like most struggles for power, those deemed as oppressed who are on the front lines take the charge to improve their own condition. HIV is no different.
Ultimately, to be successful, Black women living with and impacted by HIV must be at the forefront of efforts to end the HIV epidemic. Their lived experiences hold the wisdom necessary to confront the plethora of issues faced by millions in the United States.
This is what it means to center Black women living with HIV: to put people most likely to be pushed to society’s margins at the center of our work; to approach each endeavor from the perspective of the changes that need to be made, or barriers removed, for Black women living with HIV to thrive; and to listen to and follow the leadership of Black women living with HIV.
As the HIV community moves forward to end this epidemic, we must be cognizant of the work being done by the people and for the people and support these efforts. When Black women living with HIV are at the center of coalitionbuilding and policy change efforts, the needle will move exponentially toward justice. ■
The HIV community lost two fierce warriors last December. Cindy Stine and Bryan C.
Jones committed much of their lives to fighting the stigma linked to the virus, particularly regarding laws that criminalize people living with HIV.
An HIV advocate since the ’90s, in 2012, New Jersey native Stine volunteered to coordinate the Sero Project’s outreach program to incarcerated people living with
HIV. A network of people living with HIV and their allies, the Sero Project fights for freedom from HIV stigma and injustice. The HIV-negative ally ultimately became one of Sero’s first full-time staffers and helped launch the biennial HIV Is Not a Crime National Training Academy.
Cleveland-based Jones became an HIV advocate following his own diagnosis with the virus in 1984. He was a founding member of the Ohio Health Modernization Movement, which aims to update HIV nondisclosure laws, and a national founding member of the Undetectable Equals Untransmittable (U=U) campaign. He also developed the
DIRT (Direct, Inspiring, Reachable, Teachable) model of advocacy as a way to discuss HIV with Black people outside of classrooms and conferences.
The impact of their deaths was immediately palpable on social media, where many folks shared heartfelt tributes.



1. Maria Mejia of The Well Project and LatinX+ (seated, third from right) shared an image of the folks behind LatinX+ in a tribute to Stine (back row, fourth from left), a key adviser to the Latino HIV group whom Mejia called a “guardian angel.” 2. The Sero Project’s co–executive director Kamaria Laffery (foreground, second from right) noted the massive imprint Stine left on so many lives Laffrey’s post referenced Turn It Up!, a magazine promoting health among incarcerated people that Stine helped launch.
3. Sero Project’s Robert Suttle called Stine “a pillar of support,” sharing, “Her impact on my life and advocacy is immeasurable.”
4. Bruce Richman, of the Prevention Access Campaign, which spearheaded U=U, worked often with Jones, an inaugural ambassador of the U=U message. He shared, “I’ve lost a rare true friend and one of the most brilliant, innovative, resilient and kind humans I’ve ever had the privilege to know.” 5. In a tribute, AIDS United quoted its vice president for public Affairs, Carl Baloney Jr.: “It was impossible not to recognize and acknowledge Bryan’s presence especially in spaces like AIDSWatch, where change was always on the agenda.” 6. Olga Irwin, of Positive Women’s Network–USA (seated, front), a fellow Ohio resident, advocated side by side with Jones for 20 years 7. PrEP educator Damon Jacobs recalled how Jones, also known for his sense of humor, cracked him up at the International AIDS Society conference in Montreal in 2022.




your event photos to POZ



Try a healthier baked—not
deep-fried—version.
THESE HERBY CHICKPEA BALLS ARE PACKED WITH PROTEIN plus fresh garlic and onion
to support the immune system Many chefs deep-fry them, but baking them results in crisp, flavorful falafels without the extra oil or mess from deep frying.
Tzatziki is a classic, easy-to-make and cooling Greek yogurt sauce that also packs a protein punch. The added mint is not only refreshing but also aids in digestion.
Falafel: SERVINGS: 4 / INGREDIENTS: 8 Tzatziki: SERVINGS: 6 / INGREDIENTS: 7
INGREDIENTS:
Falafel
2 tablespoons olive oil (for the baking sheet)
1 (15.5-ounce) can of chickpeas
Tzatziki sauce
16 ounces whole-milk plain Greek yogurt
DIRECTIONS
Falafel
1 red onion, cut into chunks
2 garlic cloves, peeled
1 cup fresh cilantro, roughly chopped
1 cup fresh parsley, roughly chopped
½ large English cucumber, peeled, seeded and diced ½ cup mint leaves, chopped
½ cup chickpea flour, almond flour, whole-wheat flour or all-purpose flour
Salt and pepper, to taste
½ small garlic clove
Juice from half a lemon Salt and pepper, to taste
1. Preheat the oven to 350°F Line a baking sheet with parchment paper and coat it with olive oil. Set aside.
2. Add the remaining ingredients to a blender or food processor and blend until the mixture is the consistency of moist cookie dough Let the mixture sit for 15 minutes.
3. Make 1-inch-sized balls from the mix and place on the oiled baking sheet, leaving space in between the balls (should yield approximately 8 balls). Bake for 15 minutes, flipping about halfway through the cooking time. Remove the pan from the oven. Serve immediately with the tzatziki.
Tzatziki
1. Set a colander over a bowl and salt the cucumber. Let drain for 20 minutes. Pat dry.
2. Chop the garlic into very small pieces and add a generous pinch of salt.
3. In a medium bowl, mix the garlic paste with yogurt, lemon juice, mint leaves and pepper to taste Stir in the cucumber Taste for seasoning Keep in the refrigerator until ready to eat.
NUTRITION FACTS (per serving)
Falafel
Calories: 278; fat: 11 g; saturated fat: 1 g; polyunsaturated fat: 2 g; monounsaturated fat: 6 g; carbohydrates: 37 g; sugar: 7 g; fiber: 10 g; protein: 11 g; sodium: 419 mg
Tzatziki
Calories: 75; fat: 4 g; saturated fat: 3 g; carbohydrates: 5 g; sugar: 3 g; fiber: 1 g; protein: 6 g; sodium: 264 mg

©2025 Fred Hutchinson Cancer Research Center, a 501(c)(3) nonprofit organization. Used with permission.
By Craig Ramsay
The potential benefits of a back rub include:
1. Boosting immunity by increasing white blood cells;
2. Reducing bloating and mood swings;
3. Raising alertness and improving circulation and energy;
4. Curbing headaches and reducing migraines;
5. Increasing blood flow to encourage lymphatic drainage, which adds vitality to a dull complexion and lackluster hair;
6. Easing side effects of cancer treatment, such as fatigue, pain, anxiety, depression and nausea;
7. Reducing anxiety and depression by lowering levels of the stress hormone cortisol;
8. Relieving pain and decreasing stiffness;
9. Improving sleep and alleviating stress.
Craig Ramsay is a fitness expert, an author and a winner of season 8 of The Amazing Race Canada. Follow him on Instagram at @craigramsayfit.








Starting antiretroviral treatment and staying mentally active can improve your neurological health.
manifestations of HIV are less common today thanks to effective antiretroviral treatment, but many people living with the virus still have mild or moderate neurological and cognitive problems, collectively known as HIV-related neurocognitive disorder (HAND). What’s more, the aging HIV population is prone to age-related cognitive decline.
In the early years of the epidemic, HIV-related neurological problems— including AIDS dementia—were a major concern. HIV can enter the brain, and studies have shown that this may happen within days after initial infection. The virus can damage the brain directly, and opportunistic infections can cause serious neurological disease.
Yet even when viral load is undetectable, HIV can cause chronic immune activation and inflammation that take a toll on the brain. In the era of effective treatment, HIV-positive people may experience problems with thinking, concentration, memory, learning, verbal
fluency, mood, sleep and, in some cases, physical coordination and mobility. Often, these deficits are subtle enough that they do not affect daily life and can only be detected with special tests.
More than half of people living with HIV are age 50 or older, meaning agerelated neurocognitive problems—from increased forgetfulness to Alzheimer’s disease and other forms of dementia— are a growing concern. Some evidence indicates that HIV-positive people may experience age-related cognitive decline earlier than their HIV-negative peers. But age-related changes in cognition and memory are normal, and it can be hard to tease out the specific effects of HIV. It is not yet known whether people with mild cognitive symptoms are at greater risk for developing dementia.
Many factors can contribute to neurological and cognitive problems among people living with HIV, including a high viral load, a low CD4 count, AIDS-related illnesses, non-AIDS comorbidities and depression or other mental health issues. Alcohol and drug
use can also play a role. Some antiretrovirals—especially efavirenz (Sustiva)— and medications for other conditions can cause neuropsychiatric side effects, such as brain fog (slowed thinking and poor concentration), mood changes and sleep problems.
While it may not be possible to prevent HAND entirely, you can take steps to improve your neurological health. The first is starting and staying on antiretroviral treatment to keep your viral load undetectable. Although it was once considered important to select medications that cross the blood-brain barrier, modern antiretrovirals can control HIV throughout the body.
Managing other conditions that can contribute to worsening brain function is also key. This includes treating coexisting diseases, such as hepatitis C, and controlling high blood pressure and elevated blood sugar and lipid levels. If you smoke, try to quit, and limit use of alcohol and drugs. Exercising, eating a balanced diet and getting enough sleep are all important for overall health, including the health of your brain.
Research shows that staying mentally active throughout life can help stave off cognitive decline. This includes doing puzzles, playing memory games, reading or learning a new language—anything that keeps your brain sharp. Social engagement is also important.
Let your health care provider know if you experience changes in thinking, concentration, memory, mood or other neurocognitive symptoms, especially if they are getting worse over time. It may be helpful to document such symptoms in a diary. Your doctor will try to rule out other causes before settling on a diagnosis of HAND.
There are many tips for coping with poor concentration and memory. These include writing reminder notes or recording memos on your phone, keeping weekly and monthly checklists to help you remember important errands and bills you need to pay, and using a pill organizer to sort your medications. Don’t hesitate to ask friends or family members for support and assistance.
Despite decades of research, much remains to be learned about neurological and cognitive problems among people living with HIV. The picture will likely become clearer with more research as the HIV population ages. Ask your provider or visit ClinicalTrials.gov t fi nd studies that aim to learn more about HIV-related neurocognitive problems and develop new treatments. ■
Twice-yearly lenacapavir pre-exposure prophylaxis (PrEP) is the 2024 breakthrough of the year, according to Science magazine. Lenacapavir for PrEP isn’t approved yet, but studies showed that the HIV capsid inhibitor dramatically reduces the risk of acquiring the virus. Lenacapavir is an antiretroviral drug— not a vaccine that trains the immune system to fight HIV—but vaccine candidates have repeatedly failed, so long-acting PrEP is the next best thing.
“Science acknowledges the next, but by no means final, step in the drive to fight AIDS, where the rigors of the laboratory and the needs of humanity are inseparable,” wrote Holden Thorp, PhD, the journal’s editor-in-chief.
The PURPOSE 1 trial showed that twice-yearly lenacapavir PrEP was 100% effective for young cisgender women in Africa. None of the women who received the injections every six months acquired HIV. Similarly, PURPOSE 2 showed that twice-yearly lenacapavir reduced HIV risk by 96% compared with background incidence for gay and bisexual men and gender-diverse people in the United States and six other countries.
Oral PrEP was first approved in 2012, but it has still not reached its full potential. Some people have trouble remembering to take a pill every day, while others may feel stigma around using antiretrovirals or are hesitant to have pill bottles that could be lost or stolen. While a twice-yearly prevention shot would be a game changer, Gilead Sciences recently revealed that it is working on new lenacapavir formulations that could potentially be administered just once a year. However, researchers, advocates and global health officials stress that the promise of long-acting PrEP can be realized only if it is accessible to everyone who needs it worldwide.


People living with HIV can now receive liver and kidney transplants from donors who are also HIV positive outside of a research setting, according to a federal rule announced in November.
Kidney and liver transplants can be lifesaving, but a shortage of available organs limits access. The HIV Organ Policy Equity (HOPE) Act of 2013 legalized transplants between HIV-positive donors and recipients, but they were allowed only in clinical studies.
Positive-to-positive kidney transplants are safe and effective, according to a recent report in The New England Journal of Medicine. In a multicenter observational study of 198 HIV-positive adults with end-stage kidney disease, those who received a kidney from an HIV-positive deceased donor had similar rates of overall survival, graft (organ) survival and rejection events as those who received kidneys from HIV-negative donors. One person appears to have acquired a second genetically distinct strain of HIV from the donor, but there were no notable clinical consequences.
The new rule should expand access to transplants for people living with HIV, since organs from HIV-positive donors cannot be given to HIV-negative individuals. This also means people with HIV can donate their organs for others in the HIV community.
“Expansion of HIV-to-HIV kidney transplantation outside of research would be a win-win situation,” says study coauthor Christine Durand, MD, of Johns Hopkins University School of Medicine, which performed the first deceased donor kidney and liver transplants under the HOPE Act as well as the first living donor positive-to-positive kidney transplant.
An eighth person—and second woman—appears to be cured of HIV after a stem cell transplant for cancer treatment, according to a poster presented at the 2024 HIV Drug Therapy conference in Glasgow. The woman, who was treated for leukemia in France, received stem cells in July 2020 from a donor with a rare mutation that prevents the virus from entering cells. Although she stopped antiretroviral treatment in October 2023, she has not experienced viral rebound. Researchers have found no HIV RNA or DNA in her circulating CD4 cells or blood plasma, and her HIV antibody levels have declined.
Only a small number of people have been cured after donor stem cell transplants, and scientists are still trying to figure out why. Five people—including the latest patient—received stem cells from donors with two copies of the CCR5-delta32 mutation. One received cells with a single copy, one received a mix of cells with and without the mutation, and one person’s donor had “wild-type” stem cells with no copies. Some underwent intensive pretransplant conditioning chemotherapy and radiation, while others received gentler regimens. Some experienced severe graft-versus-host disease, which occurs when donor immune cells attack the recipient’s body, but others did not. The size of the preexisting viral reservoir and individual immune response may also play a role.

The risky and expensive transplant procedure is appropriate only for HIV-positive people with advanced cancer, but each new case offers clues that could help scientists develop a more widely applicable functional cure. “We need to give people hope but make it realistic,” says HIV cure expert Sharon Lewin, MD, PhD, of the Peter Doherty Institute at the University of Melbourne.
On December 1, the International Antiviral SocietyUSA (IAS-USA) updated its recommendations for the prevention and treatment of HIV and the management of overall health for people living with the virus. The guidelines are based on a review of relevant studies since the last update in 2022. The adoption of long-acting antiretrovirals was a key theme during this period.
The IAS-USA recommendations are comparable to those from the Department of Health and Human Services, which were updated in October. Both recommend that all people diagnosed with HIV should begin antiretroviral therapy as soon as possible. For most people, recommended initial regimens include an oral integrase inhibitor, specifically bictegravir (in the Biktarvy combination pill) or dolutegravir (Tivicay). Long-acting injectable Cabenuva (cabotegravir and rilpivirine) is also an option for those who prefer not to take or struggle with adherence to daily pills.
Beyond antiretroviral treatment, the revision includes recommendations on HIV pre-exposure prophylaxis (PrEP) and doxycycline post-exposure prophylaxis (doxyPEP) for the prevention of sexually transmitted infections. It also includes advice on managing cardiovascular risk, weight changes and substance use disorders among people living with HIV and a new section on cancer, which contributes to 20% to 30% of all HIV-related deaths.

Throughout the recommendations, the authors discuss barriers that impede access to HIV prevention, treatment and care. “Although the tools are available, efforts must be redoubled to reduce disparities and address inequities to realize the promise of ending the HIV epidemic,” they wrote.

Apretude (injectable cabotegravir), the longest-acting approved pre-exposure prophylaxis (PrEP) method, is highly effective in real-world use. Two studies of nearly 1,300 people in the Trio Health and OPERA cohorts found that the injections administered every other month were at least 99% effective for preventing HIV. Most people stayed on Apretude, and a majority received their shots on time. A study of 111 people who started injectable PrEP at safety net clinics in San Francisco—a population with high rates of mental health problems, substance use and unstable housing—saw no new seroconversions.
The PILLAR study looked at more than 200 cisgender and transgender men who started Apretude after using daily PrEP pills. They found Apretude to be acceptable and convenient. Recalling barriers to oral PrEP use, about a quarter worried about privacy, stigma or the need to hide their PrEP use. Six months after starting Apretude, only 1% still had such concerns. What’s more, they reported reduced stress about missing doses and increased confidence about protection against HIV.

A once-daily combination pill containing doravirine and islatravir maintained viral suppression for a year in a pair of late-stage trials. Doravirine (sold alone as Pifeltro) is Merck’s nextgeneration non-nucleoside reverse transcriptase inhibitor, while islatravir is an experimental nucleoside reverse transcriptase translocation inhibitor. Islatravir previously hit a snag when participants in early trials experienced declines in CD4 and total lymphocyte counts, but scientists determined that the doses used were too high. Two subsequent Phase III trials tested a single-tablet regimen containing doravirine plus a lower dose of islatravir. Together, they enrolled more than 1,000 adults with an undetectable viral load on Biktarvy (bictegravir/tenofovir alafenamide/ emtricitabine) or other baseline antiretroviral regimens. The doravirine/islatravir combo maintained viral suppression at 48 weeks, and researchers did not see the blood cell declines that doomed the higher islatravir dose. Merck plans to submit the data to the Food and Drug Administration for approval.

Intensifying antiretroviral treatment by doubling the dose of dolutegravir may shrink the viral reservoir. Antiretrovirals can keep HIV suppressed, but the virus inserts its genetic blueprints into human cells and establishes a long-lasting viral reservoir that the drugs can’t reach. People with HIV are at higher risk for comorbidities despite treatment, suggesting that residual viral replication may lead to chronic inflammation. In a Phase II trial, 20 HIV-positive adults with viral suppression on a standard regimen of 50 milligrams of dolutegravir plus abacavir and lamivudine either stayed on the same combo or added an extra 50 mg dolutegravir for 84 days. The intensification group saw declines in total and intact HIV DNA and unspliced HIV RNA in peripheral blood cells. Double dolutegravir was associated with some changes in biomarkers of immune activation and exhaustion, but most were not statistically significant, and intensification had no notable effect on inflammation. These results suggest that the standard regimen prior to intensification may not have completely suppressed the virus.

Nearly 846 million people ages 15 to 49—or around one in five adults in this age group worldwide—are living with genital herpes, according to the World Health Organization. The new analysis also estimates that some 42 million people acquired genital herpes in 2020. While herpes simplex virus (HSV) infection often has no symptoms, it can cause recurring painful ulcers. HSV-1 usually spreads via saliva and causes sores on the mouth, while HSV-2 is typically sexually transmitted and causes genital or anal lesions; however, both types can cause genital herpes. Herpes sores usually heal within a couple of weeks, but HSV lies dormant in nerve cells and can reactivate. People living with HIV are more likely to carry HSV-2 and are prone to more frequent and severe outbreaks. What’s more, having genital herpes facilitates both HIV acquisition and transmission. Antiviral medications can reduce the severity of herpes outbreaks, but they don’t eliminate the virus. The study authors urge more investment to develop herpes vaccines and better therapies.










advocate for oneself in medical spaces. Diagnosed with HIV in 2012, the 52-year-old vocational nurse from Inglewood, California, uses her unique perspective to help bridge the communication gap between women living with HIV and clinicians.
“I didn’t go to nursing school until I turned 40,” Picou says. “It was in part because of being diagnosed with HIV.”
About a month before her 40th birthday, Picou developed a sore throat and got antibiotics at a local clinic, which had just opened a women’s clinic. As a result, when a provider asked whether she’d be willing to get a routine Pap smear the following day, she consented.
What came next was an unexpected HIV diagnosis and a new reality for Picou.
“It’s definitely been a growing and learning process,” Picou says. “Who you think you are often changes when you come up against something like that. I had to come to terms with who I thought I was and who I was going to be moving forward.”
Picou decided to educate herself. She attended nursing school and got her license. Then she became an HIV nurse. It’s been her job ever since.
“I got my certification in AIDS care…as part of my commitment to being able to take care of folks living with HIV,” she says.
PICOU’S PERSONAL JOURNEY WITH HIV HAS informed how she navigates her job as a nurse. She remembers feeling like just another number the first time she sought care after her diagnosis.
“Everybody was being very careful to tell me that I wasn’t going to die, but nobody was telling me how I was supposed to live and what I’m supposed to do, other than take a pill,” she recalls.
As soon as she was diagnosed with HIV, Picou disclosed her status to a close female cousin because she knew she’d get the support she needed woman-to-woman. But it took her about a year or more to share with the rest of her family that she had HIV.
“I have a 33-year-old son,” she says. “It was even longer before I told him. I didn’t want people worrying about me or my family feeling they had to defend me against other people’s opinions and stigma.”
Picou was never angry or in denial about her diagnosis. Rather, she accepted it and chose to make it what she wanted it to be.
“For me, it was about learning everything I could about the virus,” she says. “That was important to me. That’s my coping skill. The more I know, the better equipped I feel to deal with it.”
Picou put her new knowledge to work as a nurse at a local HIV clinic. “It evolved into me working there almost eight years and advocating for my patients for their medication or
for a service that they needed,” she says. “Listening to their stories and how they were navigating life was teaching me how to advocate for myself. That grew into feeling like I could be doing more for other women.”
DIDN’T start treatment until six months after her diagnosis due to insurance issues.
She wasn’t aware at the time about the Ryan White HIV/ AIDS Program or the AIDS Drug Assistance Program (ADAP), which help people living with HIV obtain health insurance and the treatment they need.
“Nobody thought to tell me about that,” Picou says. “It was like, ‘Have you thought about how you’re going to get medication?’ Oh sure, let me just reach into my pocket and pull out $3,000.”
Sometimes, she’d go to pick up her meds and only two would be available.
“If I didn’t know better and hadn’t educated myself, I might be taking those two pills not knowing that without the third component, I’m increasing the potential for the virus to break through and for me to have resistance,” Picou says.
Although such incidents frustrated her, they helped make her the nurse and advocate for people living with HIV that she is today.
Today, Picou has an undetectable viral load, and as long as she maintains viral suppression, she cannot pass on the virus via sex, a fact known as Undetectable Equals Untransmittable, or U=U.
“I want to date and have a healthy sex life,” she says. “I want to be able to be in a relationship. Being undetectable is empowering because I don’t have to worry about transmitting the virus to someone.”
Picou thinks there should be more dialogue about U=U. “U=U is more than just being undetectable for sex,” she explains. “There’s a broad range of things that it covers as far as general health and mental well-being.”
PICOU ALSO KNOWS THAT ADVOCATING FOR oneself is a journey and a challenge. But it’s one of the most important things a woman can do. Picou has had
eight HIV clinicians in 12 years, which is too many, she says.
“Only two of them have ever asked me without prompting if I want or need tests for STIs [sexually transmitted infections],” she says.
“I have gone into other spaces and had an obstetrician hurt me with his stigma and bias. One of the struggles with HIV as a Black woman is finding good, quality care.”
That’s why as a nurse she helps patients living with HIV find their voice.
“It’s OK to speak up about your concerns,” Picou says. “It’s OK to fire somebody who’s not listening and find someone who will. It’s your health.”
Picou believes health care providers have a responsibility to teach people, but patients must do their part too. “There’s also a responsibility to yourself to find out information and stand up for yourself when you’re not getting that information,” she says.
Although Picou’s current doctor is a man, her experience as both a nurse and as someone who has worked in an HIV clinic has given her the ability to comfortably share her concerns with him.

Picou became a nurse after testing HIV positive.
“YOU ARE FLAWED AND WORTHY, JUST LIKE EVERY OTHER WOMAN ON THE PLANET.”
“Not everybody has that benefit, which is why it’s so important for women to have a woman clinician,” she says. “There are things that we just know to ask from being a woman.”
on women living with HIV. She is the stakeholder liaison for the women-led nonprofit The Well Project, which helps women and girls across the gender spectrum living with or affected by HIV.
“When I came across The Well Project, that further fueled my need to be able to speak for women who feel like they can’t speak up for themselves,” she says. “Because maybe
they’re hiding their status or not ready to share it, or they don’t understand enough to be able to put it into words.”
Picou started blogging for The Well Project in 2019 after learning about the organization in a Facebook group. She was happy to find a resource with fact sheets and other information about women with HIV. But most important, she was grateful to have found so many other women like her.
Over time, she joined the community advisory board. Then, executive director Krista Martel offered her the stakeholder liaison position, a role created specifically for her.
Picou’s dual perspective as a nurse and woman living with HIV allows her to advocate for women in clinical settings and oversee partnerships.
“We’re small, but we’re a mighty team,” Picou says of The Well Project. “We’re all intimately involved in our programming and what gets on the website. It’s such an important space for women to come into and find themselves.”
Picou wants women to know about The Well Project’s new video series for women living with HIV. Titled WATCH! 2.0, it covers everything from the basics of HIV for sexual health and wellness, birthing and more.
“I plan on continuing to try to grow our partnerships because that’s going to be more important than ever with this new [presidential] administration.”
CALIfornia, where the large HIV community is predominantly male, Picou considers visibility a major challenge for women with HIV—specifically, she says, “visibility in not seeing themselves as vulnerable to acquiring HIV, visibility when it comes to feeling seen and heard and having our needs and issues addressed, visibility in spaces like research.”
With that in mind, last June in Palm Springs, Picou held the first “SHE is” Women’s Conference, a collaboration between The Well Project and the HIV + Aging Research Project, where she is board secretary.
Picou is an advocate for U=U.
The event brought women together to bond and share their experiences during a jewelry-making workshop, for example, and while attending a panel of women with varying years of survival with the virus under their belt.
“We had a really robust conversation about what that looks like and if a cure happened, would they take it?” Picou says.
Picou is proud of the acronym too. SHE stands for “shifting the narrative, healing our spirit and embracing the future.”
“There’s a song by Alice Smith called ‘She,’ which kind of gave me the idea,” she says. “It’s one of my favorite songs.”
time for women across the United States. She encourages women living with HIV to first get right mentally. That starts with practicing mental self-care.
“The biggest thing women can do is mind your mental,” she says. “I highly recommend getting sunlight in the form of a walk a couple times a week. If physical things like going to the gym or working out are not your thing, find what is.”
Picou suggests finding a creative outlet too, specifically one unrelated to HIV. She makes jewelry and paints. Sometimes, she roller skates.
“Find something for your mental health that is teaching you and separating you from the anxiety of HIV and of the political climate,” she says.
Picou also likes to write. She recently completed a 10-week playwriting course for people with HIV. Her 10-minute play Not to Be an Alarmist, but... was performed in New York City in December. She dreams of one day writing a book.
“Everything else I do as an advocate is for the greater community,” she says. “But this playwriting was just about me and for me.”
Picou also wants women living with HIV not to back down during this time. Now is the time to get involved and stay involved, she says.
“Being involved in advocacy is not just having your face on a poster or getting up on a microphone,” she says. “It’s not just being on a webinar. There are other things you should be doing.”
That could mean writing letters to lawmakers or getting involved with local government. The sad truth, Picou adds, is that no one is coming to save women. It’s up to women to fight for themselves.
is simple: Learn who you are and stand in who you are. It’ll serve you well.
“How you feel about yourself, the way that you talk to yourself and the way that you see yourself is going to reflect on how other people feel about you,” she says. “You

“THE
happen to have a virus. You are flawed and worthy, just like every other woman walking the planet.”
Picou hopes to continue showing women how to overcome stigma by living authentically. She’ll keep representing women with HIV in clinical settings and provide them with the information they need to lead healthy lives.
She also plans to host the “SHE is” conference again this year to help build community among women with HIV.
“The big picture is making sure that women living with HIV have the tools they need to be able to thrive,” she says. “I just want to be a resource. My favorite affirmation of all time is ‘When you can’t find the light, be the light.’ I want to be a little light.” ■
• A daily resource for people living with and affected by HIV and AIDS
• Clear, comprehensive prevention and treatment information
• News, personal stories, blogs, HIV-specific resources and more
• Sign up for free email newsletters




















BY TIM MURPHY
IN RECENT YEARS, MONICA JOHNSON, THE FOUNDER OF THE HIV community organization HEROES (Helping Everyone Receive Ongoing Effective Support), which is based in Columbia, Louisiana, and marks its 30th anniversary this year, was often surprised to learn that among people she met, only a few had basic, up-to-date information about HIV. Diagnosed with HIV in 1985, Johnson found that many folks didn’t know that HIV can now be managed with medication and that with effective treatment, people with HIV cannot transmit the virus sexually to others. Many people also didn’t know that you cannot get HIV from casual contact, like hugging and kissing.
Down South by Dyan King
When Johnson discussed the issue with her friend Tamela King, an art teacher at a local public high school, King said her kids didn’t know basic facts such as that HIV and AIDS are not the same thing. She said, “They’d ask me, ‘How do you get it? What can I do not to get it?’” King told Johnson her students “thought the HIV epidemic was over, basically, because nobody talks about it.”

But the epidemic is far from over, especially in the Deep South, where the rates of new HIV diagnoses are generally the highest in the country and care and services are often sparse, especially in rural areas.
In 2024, King received a grant from Wake Forest University to combat HIV stigma in the church through art. Working with Johnson, she put out a call for submissions of artwork relating to HIV and held workshops with her students to educate them about the virus. Johnson and King were so impressed with the art that was created that they decided to produce a short book explaining HIV using minimal text and featuring an abundance of colorful, folksy artwork by King and her students as well as statements by the featured artists.
The result is For Lack of Knowledge: An Artistic Experience to End the HIV/AIDS Epidemic, which was published last August. All proceeds help fund the construction of a comprehensive education center that HEROES hopes to build on five acres of land it acquired in the area.
The book’s cover features a painting by King of a church, and each page of the book opens with a line of Scripture. “Our target audience for the book was church leaders and churchgoers,” says Johnson, “because that’s where a lot of HIV stigma still is, and in the South, the church is the gatekeeper for the community.” King echoes that sentiment, noting that the image of the church is powerful, as it is a subtle call to the faith community to help disseminate accurate information about HIV and AIDS.
The book covers many topics, including the difference between HIV and AIDS, antiretroviral therapy, how to have open conversations about HIV, how folks with HIV can combat internalized stigma, how couples can get tested for HIV together, the importanceofusingnon-stigmatizinglanguagewhendiscussing HIV, an explanation of both pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) to prevent HIV, HIV among women and children and much more.
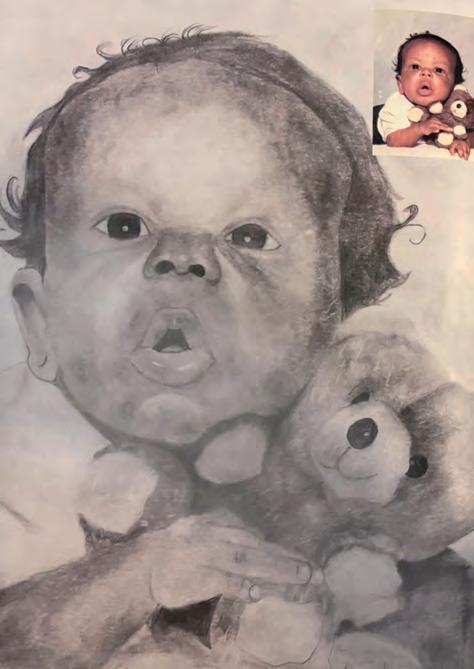
KING’S STUDENTS
“THOUGHT THE HIV EPIDEMIC WAS OVER BECAUSE NOBODY TALKS ABOUT IT.”
One of Johnson’s favorite artworks appears on the pages with information regarding HIV among young people. Titled The Struggle is Real, the painting, by Alex Rider, depicts a young Black girl carrying several heavy buckets hanging from a tree branch that weighs down her neck. Rider’s artist statement explains: “The little Black girl symbolizes the unique struggle of being Black and female while trying to navigate a world... that gives you inadequate tools...to manage real-life issues.”
Balancing Act, by My Sherie Johnson, included in the section “HIV Does Not Define a Person,” illustrates the fact that people with HIV have a lot on their plate and everything they do


impacts their health and well-being. One section in the book, which explains how longstanding poverty and health disparities drive higher HIV rates in the Southern states, is illustrated by a painting of a pelican— the state bird of Louisiana. Of the painting (see page 28), titled Down South, artist Dyan King says: “The pelican is a symbol of Christ sacrificing himself for humanity. In nature, pelicans value community and teamwork.... I believe that if we followthepelicanandChrist,therearebrighterdaysahead.”
But Johnson says the image that most moved her, titled Da Boy, took her by surprise: a pencil drawing by Riley Volentine of Johnson’s beloved son, Vaurice, who was born with HIV and died of AIDS-related causes in 1993. “I was tearful when I saw it,” says Johnson.
King says that including the image of Vaurice was her way of honoring Johnson, her friend of about 25 years, for becoming an AIDS advocate and living openly with HIV in a small town that could often be gossipy. “Monica took the very private pain of having to bury a child and shared it with the world” in order to educate people, she says.
According to Johnson, construction of the new HEROES center is budgeted at $6 million. The facility will include offices, a farmer’s market, a gym, classrooms and walking trails. “It’s my field of dreams,” Johnson says. She admits there’s much more fundraising to do. According to King, the duo plans to visit several churches this year to promote the book and spur more sales. “Promoting a book is hard work!” she says.
The book is available on the HEROES website. People who buy it can provide feedback using a QR code. “It’s full of basic info that everyone needs to know,” says Johnson. “That’s why it’s a very important project for us.”
King says the book is more vital than ever given that HIV is not discussed as widely as it was at the height of the epidemic in the 1980s and 1990s, even though too many people are still being diagnosed with the virus, especially in communities of color in the Deep South.
“Several members of my church bought it,” she says. “One lady came up to me last Sunday and said, ‘I did not know any of the info that was in that book, but now I plan to keep it on my coffee table so everyone can see it.’” ■
Visit heroesla.us/products/for-lack-of-knowledge to purchase the book and support the work of HEROES.


Valencia Landry knows firsthand what it’s like to be an HIV advocate in a conservative state. A native of Louisiana, where she was first diagnosed with HIV in 2005, Landry now resides in Fort Worth, Texas, a state governed by conservative Republicans whose views of sex and injection drug use inform policies that create barriers to HIV prevention and treatment.
“The hardest part of preaching prevention and PrEP [pre-exposure prophylaxis] in the state of Texas is that HIV prevention policy is often abstinence-based,” Landry says. “And in Texas, you can’t go to the schools and talk about sex education. You can’t give out condoms because everything is abstinence, and that’s not helpful because people are having sex.”
People are also injecting drugs, which is especially risky in Texas because it opposes needle exchange efforts to curb HIV transmissions. Only Bexar County, home to San Antonio, over 250 miles from Fort Worth, permits needle exchange.
But instead of ditching Fort Worth for friendlier climes, Landry has dug in for battle in the Lone Star State, where she finds purpose and meaning in her HIV advocacy. With scant few legislative allies, Landry organizes locally, often filling the gaps created by state policymaking.
“I’m a part of the Tarrant County Community Advisory Board,” she says. “We drafted a step-bystep guide—from being newly diagnosed to getting the resources that you need to getting to doctors’ appointments and things like that. And they have different social services and support agencies listed in the county that can help you along the way as well.”
Landry also works with the Dallas-based Grace Project, which hosts the nation’s largest annual conference for women living with HIV and AIDS. At the most recent gathering, Landry led a breakout session about financial literacy for individuals of all ages, including older long-term HIV survivors.
Landry notes that long-term financial planning— including retirement—for people with HIV is a far cry from the early days of the epidemic, when most people with the virus couldn’t imagine growing old.
“People were getting diagnosed, and not much later they were passing away,” she says. “But now it’s just like, How can I help others with HIV live a longer life? How can I help them live life with dignity or even just dying with dignity later on?”
For Landry, living with dignity includes establishing and maintaining financial security.
When asked about the persistent stigma around HIV, Landry suggests that the battle against it often begins in the mirror.
“Sometimes we’re in our own head, and we stigmatize ourselves, and I hope that people stop doing that and live their lives,” Landry says. “Because life doesn’t stop with a diagnosis. You have to keep pushing. Every morning that we open our eyes, we have to keep going.” ■
Valencia Landry finds purpose and meaning in her HIV advocacy.
Today, it’s recommended that people living with HIV start treatment as soon as possible. Starting and staying on today’s treatment can help you get to and stay at an undetectable status and prevent transmission of HIV to others through sex. Here are some steps you can take for yourself and your sexual partner(s):
1 3 2
Ask what your test results mean for you and find out about HIV treatments that could best fit your personal routine.
The more you know about HIV, the better. You can discover resources by scanning the QR codes, or even find helpful information on your own.
Use condoms, practice safer sex, and start and stay on the treatment discussed with your healthcare provider.
If you’re living with HIV, current research shows that taking HIV treatment as prescribed and getting to and staying undetectable prevents transmitting HIV to others through sex. This is also known as U=U (undetectable=untransmittable).
A major goal of HIV treatment is getting your viral load to undetectable. Undetectable means that there is so little virus in the blood that a lab test can’t measure it. If you have questions about your lab results and what it means to be undetectable, talk with your healthcare provider.
PrEP (pre-exposure prophylaxis) means routinely taking prescription medicine before you’re exposed to HIV to help reduce your chances of getting it. There are di erent PrEP options available, some of which are 99% e ective. Just remember, PrEP doesn’t protect against other STIs, so be sure to use condoms and other healthy sex practices.
HIV advocacy can be hard work. It often involves confronting difficult and emotionally charged issues—such as stigma, discrimination and loss— which can lead to exhaustion or burnout. The practice of self-care can help HIV advocates maintain emotional resilience and be more effective in their efforts to bring about positive change in the HIV community. Check out these self-care tips:
Nourish your body.
Exercise regularly, eat well-balanced meals, stay hydrated and get enough rest. Taking care of your body will increase your energy, improve your mood and boost your immune function.
Practice relaxation. Try mindfulness meditation, deepbreathing exercises or yoga to reduce stress and calm the mind, which will help center you amid challenging work.
Set boundaries.
You can’t be an effective advocate if you’re burned out. Know your limits and establish clear boundaries to ensure you have time for yourself.
Celebrate your progress.
Advocacy can be an uphill battle, but it’s important to acknowledge the small victories along the way toward achieving your goals. Celebrating even minor successes can provide motivation and a sense of purpose.
and establish clear boundaries to ensure you have time for yourself.
You can’t be an effective advocate if you’re burned out. Know your limits and establish clear boundaries to ensure you have time for yourself.
Unplug when needed.
Unplug when needed.
Take a break from the news, social media or other sources of information if they are angering or frustrating you. Be mindful of how much time you spend online and the type of content you’re consuming.
Take a break from the news, social media or other sources of information if they are angering or frustrating you. Be mindful of how much time you spend online and the type of content you’re consuming.
Pursue your passions.
Pursue your passions.
Engage in activities or hobbies that bring you joy and help you unwind, such as painting, gardening, reading or cooking.
Engage in activities or hobbies that bring you joy and help you unwind, such as painting, gardening, reading or cooking.
small victories along the way toward achieving your goals. Celebrating even minor successes can provide motivation and a sense of purpose.
Celebrate your progress. Advocacy can be an uphill battle, but it’s important to acknowledge the small victories along the way toward achieving your goals. Celebrating even minor successes can provide motivation and a sense of purpose.
Acknowledge your emotions. It’s OK to express your emotions, including sadness, frustration or grief. Ignoring your feelings can negatively affect your mental and physical health.
Acknowledge your emotions. It’s OK to express your emotions, including sadness, frustration or grief. Ignoring your feelings can negatively affect your mental and physical health.
Find support.
Find support.
Seek supportive friends, colleagues or a mentor. Talking to others who understand the emotional challenges of HIV advocacy can provide solace.
Seek supportive friends, colleagues or a mentor. Talking to others who understand the emotional challenges of HIV advocacy can provide solace. Visit
When it comes to HIV prevention, the Centers for Disease Control and Prevention (CDC) recommends that ALL sexually active adults and adolescents be informed about PrEP (pre-exposure prophylaxis). PrEP means routinely taking prescription medicine before you’re exposed to HIV to help reduce your chances of getting it. Here are some steps you can take for yourself and your sexual partner(s):
Have a conversation with your healthcare provider about all of your HIV prevention options, including PrEP.
Regularly test for HIV and other sexually transmitted infections (STIs), use condoms, and communicate honestly with your partner(s). If you have been prescribed PrEP, continue to take it exactly as prescribed. 1 3 2
Scan the QR codes and explore resources on your own to get tips on how to be proactive about protecting your sexual health, including understanding your HIV prevention options, like PrEP medications.
Speak with a healthcare provider:
1.How can I help protect myself and others?
2.How often should I get tested and retested?
3.How can I talk to my partner(s) about my status and theirs?
It may not be easy, but having a conversation with your partner(s) about your HIV status can help:
•Normalize the conversation around status, sexual health, and testing
•Empower others to make informed decisions about their sexual health
• Encourage all people to have conversations and stay engaged with their healthcare providers
Today, it’s recommended that people living with HIV Starting and staying on today’s treatment can help status and prevent transmission of HIV to others through take for yourself and your sexual partner(s):
Ask what your test results mean for you and find out about HIV treatments that could best fit your personal routine.
Find out everything you can
The more you know HIV, the better. discover resources scanning the QR even find helpful on your own.
If you’re living with HIV, current research shows that taking HIV treatment as prescribed and getting to and staying undetectable prevents transmitting HIV to others through sex. This is also known as U=U (undetectable=untransmittable).
PrEP (pre-exposure prophylaxis) means routinely taking medicine before you’re exposed to HIV to help reduce of getting it. There are different PrEP options available, are 99% effective. Just remember, PrEP doesn’t protect STIs, so be sure to use condoms and other healthy sex
A major goal of HIV treatment is getting your viral load to undetectable. Undetectable means that there is so little virus in the blood that a lab test can’t measure it. If you have questions about your lab results and what it means to be undetectable, talk with your healthcare provider. everything can know about You can resources by codes, or information own.
Use condoms, practice safer sex, and start and stay on the treatment discussed with your healthcare provider.
HIV start treatment as soon as possible. help you get to and stay at an undetectable through sex. Here are some steps you can taking prescription reduce your chances available, some of which protect against other sex practices.
