ADDRESSING VACCINE HESITANCY

 Laura Shepherd in partnership with Southern Plains Tribal Health Board
Laura Shepherd in partnership with Southern Plains Tribal Health Board


 Laura Shepherd in partnership with Southern Plains Tribal Health Board
Laura Shepherd in partnership with Southern Plains Tribal Health Board

 1. Communication Approaches
2. Activity
3. Addressing Misinformation
4. Monitoring and evaluation
5. Closing
1. Communication Approaches
2. Activity
3. Addressing Misinformation
4. Monitoring and evaluation
5. Closing


Topic One

Effective provider communication education is central for approaches on increasing vaccination rates vaccine hesitancy. Communication parent/patient has been important vaccine decision-making and reasons why parents changed accept vaccines. Effective approaches be open, honest, and comprehensive include patient education, communicating effectively with parents, providing ways to describe scientific concepts to a nonscientific audience, and suggests answers to questions frequently asked by parents/patients.



§ It is important to consider that cognitive biases do not indicate that someone is irrational- it merely indicates that actions may not line up with thoughts and beliefs. Parents who chose not to vaccinate their children may harbor powerful cognitive biases that can lead to responses that may seem counterintuitive to what we know every patient/parent wants for themselves and their children.
§ Providers have the ability to breakdown some of these biases by going thru some of the tips presented here . Regardless of the motivation not to vaccinate, providers must present clear, consistent, and transparent information so that patients and their families can make informed decisions.

¡ Point to your own experiences and perhaps support vaccinations by discussing your own confidence with them.
¡ Gather support from the fact that most of the money made within the pharmaceutical market comes outside of vaccines (vaccines offer little profit to pharmaceutical companies).
¡ Have supporting data and studies to point to when misinformation related to such conditions comes up in vaccine conversations.
¡ While it is not expected or recommended to know every detail of a vaccines ingredients it would be helpful to know about certain concerns parents may have such as thimerosal and aluminum.
¡ As a provider, giving information on the functions of a vaccine may help encourage these people to receive a vaccine.
¡ Point out that vaccines enable us to intentionally cultivate these diseases in milder environments.
¡ Providers may want to reinforce that vaccines teach the body to fight illnesses naturally and it gives the body tools to build up its own immunity against a particular disease.
§ One size does not fit all relating to communicating with patients. Their hesitancy, life context, and values will be very different ranging from an unquestioning acceptor to an outright refuser.
§ Good communication Includes offering a discussion and identifying the barriers of patients over a certain length of time that will hopefully build trust and identify future concerns

§ Avoid the “this is what you need” discussion and focus more on the reasons for getting a vaccine.
§ Compassion and active listening are good tools providers can use when discussing vaccinations and may include listening to parents/patients' personal experiences and offering you an understanding of their hesitancy.
§ It is important to be aware of your own individual biases when it comes to vaccinations and see conversations as an opportunity to educate and build trust.
§ Being able to chart some of that information and providing literature for community members about the benefits to them (not just vaccine information) to read on their own time are important (information sharing centers on the EUAs, VIS forms, CDC parent guides to immunizations).
§ Motivational Interviewing (MI) technique is used by health care professionals to harness people’s innate drive for change
§ Discussing data in layperson terms and being able to avoid telling the person what to do and focusing on the why.
§ When parents/patients are hesitant to receive a vaccine, you may explore and use MI techniques to best determine the causes of vaccine hesitancy. It is best not to talk a patient into making a change or making them feel bad about their behavior but to respond with empathy and support.
§ Avoid the “this is what you need” discussion and focus more on the reasons for getting a vaccine .
§ Compassion and active listening are good tools providers can use when discussing vaccinations and may include listening to parents/patients' personal experiences and offering you an understanding of their hesitancy.
§ The goal of MI should include getting patients to build their intrinsic motivation to make behavioral changes
§ MI is about asking open questions, practicing reflexive listening (affirming and summarizing), dealing with denial, and asking for permission to provide information in nonrigid framework.
Topic Two

¡ Pre-bunking is often referred to as social inoculation. Just like vaccines increase people’s resistance to a particular pathogen, social inoculation does the same thing but increases people’s resilience and resistance to misinformation and to manipulation, media manipulation techniques that they may be exposed to, as they go about in their everyday lives


¡ Pre-bunking is a process of debunking misinformation before it strikes, which means that the falseness or hollowness of a concept or belief is exposed. Disinformation techniques can include actively lying, utilizing misleading tactics, or knowingly providing false interpretations of data and sources. Pre-bunking, also called inoculation, makes people resilient to misinformation, which is spread unknowingly, and disinformation, which is spread with intent to confuse.


Case study of a program to increase literacy about HPV vaccination in Denmark
In response to negative media reports concerning the safety of the human papillomavirus (HPV) vaccine and a decline in the number of teenage girls getting it, Denmark's health authorities launched a media campaign to restore public confidence. Using data from surveys and focus groups with parents concerned about the HPV vaccination, health authorities found that there were a lot of things the parents didn't know about the vaccine, and they were able to design the campaign accordingly. In the year following the campaign, HPV vaccination doubled compared to the year before.





Monitoring and evaluation

¡ M&E are indispensable components of effective program implementation and management.
¡ Used to help with decision-making, assessment, and improvement of care and programs.
¡ Allows us to advocate for the unmet needs of our target populations.
¡ Successful M&E
¡ Ongoing.
¡ Follows a plan.
¡ Identifies success or missed opportunities.
¡ Allows for flexibility to readjust goals and outcomes.
¡ Provides an opportunity to educate and inform your audience.
1. Day prior to scheduled appointment:
a. look up vaccine record in chart and OSIIS.
b. Identify any late or missing vaccinations needed.
c. Add/edit appointment note as a reminder to nurse/provider to have a conversation about vaccinations.
d. Check supply and inventory to see if the needed vaccines are in stock.
2. Day of appointment:
a. Provide patient with a copy of vaccine record with highlighted missing or late vaccinations.
b. “It looks like you are needing a Tdap vaccine today, do you have a preference on what arm you want us to use today?” Try not to ask, “Do you want your Tdap vaccination today?” People rarely desire a vaccine, and if we word it in this way sometimes it helps encourage our patients to get caught up on their vaccination schedule.
c. Some patients come in sick and might not feel comfortable getting their vaccination while they are sick. If they decline, no worry! Offer to schedule a f/u nurse visit in 5-10 business days. If they schedule before they leave, they are more likely to follow through with the appointment. This helps us catch those kiddos that are occasionally in our clinic or only come for sick visits. Encourage them to schedule a well child visit once they are well. If they see a pediatrician for well child visits, please still encourage them to come back for a nurse/vaccine visit. WHY? Occasionally pediatricians’ offices out of vaccines or have a limited supply. If a child misses a dose, it impacts their entire vaccine schedule, and catch-up schedules can be confusing. ALSO! Most health departments are walk-in only for VFC vaccine. This is a barrier for parents. Some parents are not willing or do not have transportation or the resources to sit and wait. We can help fill that gap and meet the need. Encourage parents (or individuals) to schedule a nurse/vaccine visit before leaving the clinic.
d. If parents or individuals want to alter the CDC vaccine schedule, it is ultimately up to them and their medical provider. Remind parents and patients that a lot of research goes into developing a vaccine schedule. They are spaced strategically to promote the best possible immune system response and outcome.
e. If patient receives a vaccine, insert the vaccine into OSIIS (all patients). Provide patient with a copy of the UTD vaccine record, highlight dates for future immunizations, and encourage them to schedule next vaccine appointment before they leave.
3. Weekly M&E:
a. Complete vaccine count and inventory.
b. Order vaccines as needed.
4. Monthly M&E:
a. Reconcile vaccine the first week of each month.
b. Upload temp logs.
c. Run Reports
i. Number of vaccines administered/dosage report.
ii. Number of missed opportunities.
iii. Immunization rates.
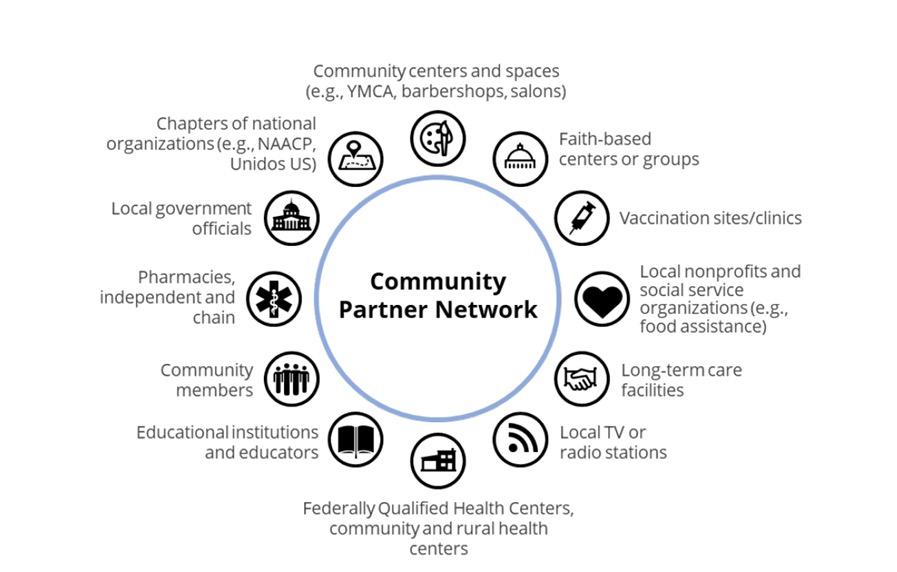
¡ Know your community and know your resources.
¡ Build relationships and partnerships.
¡ https://youtu.be/ic2ns6Th2EE
¡ COVID-19 Vaccination Message from AAIP Physicians OKC PSA – YouTube
¡ Vaccine Hesitancy - YouTube
• Do your part.
• Build authentic relationships.
• Prioritize community engagement.
• Check your own personal biases.
• Utilize trustworthy sources your patients can personally identify with.





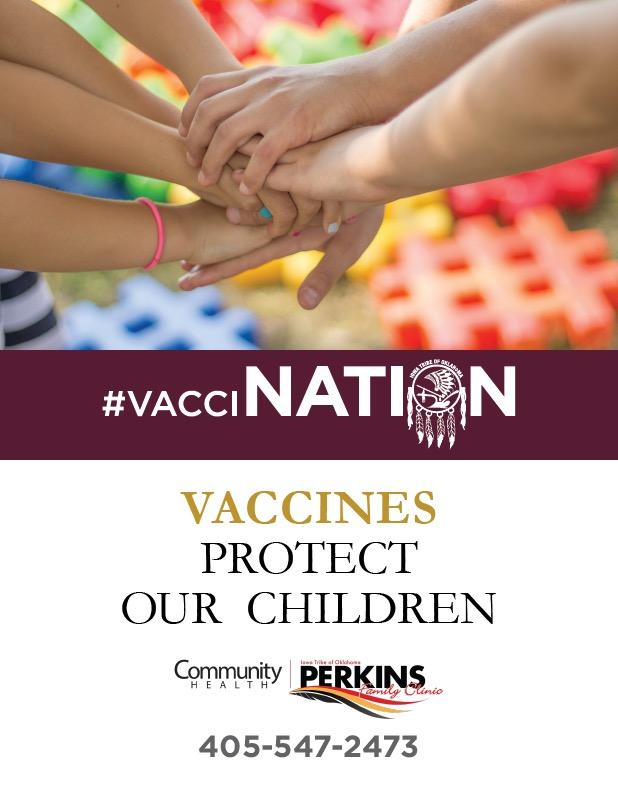
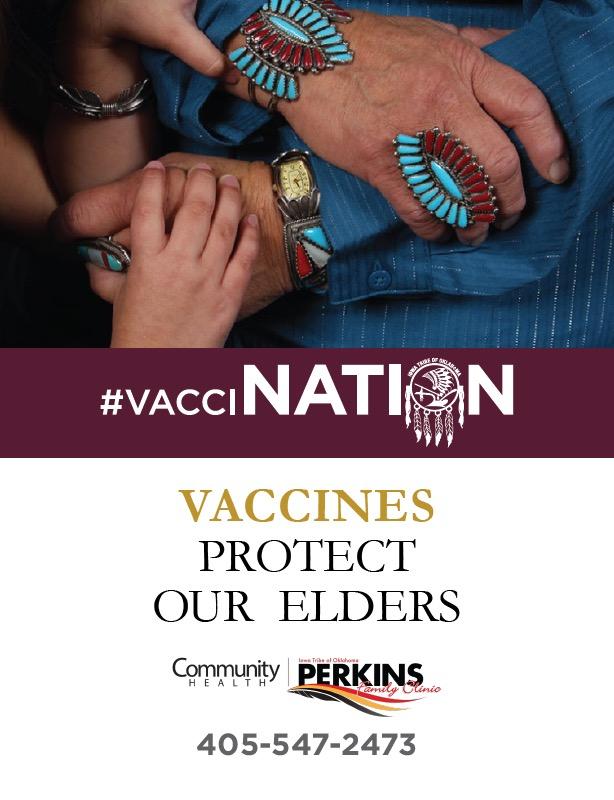
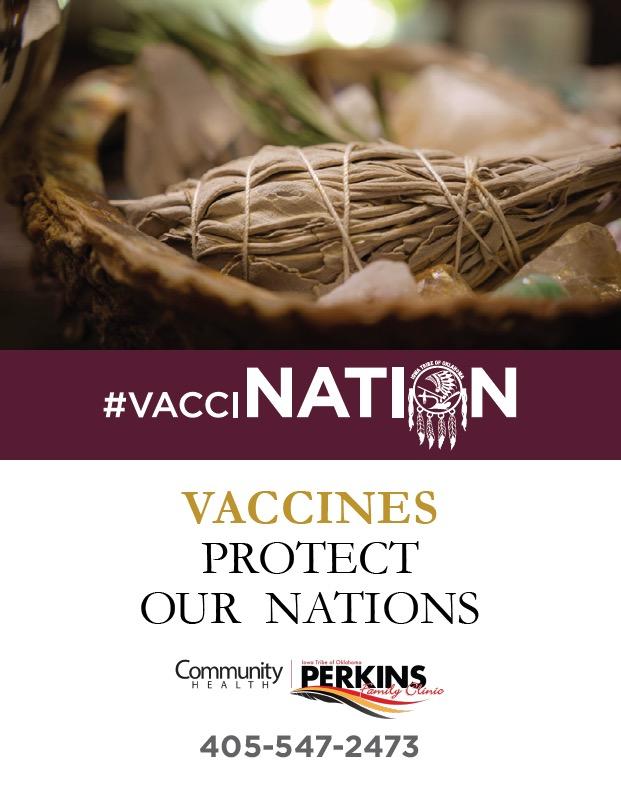
As a provider, you understand the importance of effective patient communication. Today we will discuss several strategies to address the issue of vaccine hesitancy within our tribal communities. Empowering our patients with knowledge will help them make informed decisions.


Thank you for attending! Together, we are making a difference.
Key topics include:
Approaches to Communication
Pre-bunking: Proactive Approach to Debunking Myths
Monitoring and Evaluation
Scan to follow along.
 A presentation by Laura Shepherd, in partnership with Southern Plains Tribal Health Board
A presentation by Laura Shepherd, in partnership with Southern Plains Tribal Health Board
• Importance of Patient Communication

• Addressing Bias in Vaccine Conversations
• Common Barriers to Effective Communication
• Vaccine Education Strategies
• Addressing Misinformation
PRE-BUNKING: PROACTIVE APPROACH TO DEBUNKING MYTHS:
• Vaccine Literacy and Misinformation
• Evaluating Preliminary Studies
• Utilizing Personal Stories
• Staying Updated with Scientific News
APPROACHES TO COMMUNICATION: MONITORING AND EVALUATION:
• Addressing Vaccine Hesitancy Levels
• Tracking Communication Strategies
• Measuring Effectiveness of Intervention