The Ultimate Equipment Cleaning & Infection Control Solution.















ew Zealand's aged care sector is undergoing significant scrutiny in response to the growing needs of its aging population. By 2060, approximately 25 percent of the population will be over 65, highlighting the urgent need for a comprehensive and actionable plan to support this demographic effectively.
In light of this, Senior Analyst Rachel Mackay developed and spearheaded the Aotearoa Aged Care Action Plan. This sector-sourced and sector-endorsed initiative presents nine clear objectives with direct actions aimed at creating meaningful change for older New Zealanders and the services that support them. This plan, developed over a year in collaboration with the NZCCSS membership organisations, industry experts, and thought leaders, seeks to guide effective decision-making and policy development.
In parallel, the Health Select Committee has launched an inquiry into the aged care sector's capacity to support individuals with neurological cognitive disorders, including those with early-onset dementia. The inquiry will examine the sector's current and future ability to provide necessary services, evaluate funding models, and address the shortage of care facilities. Public submissions for this inquiry are open until August 19, 2024, and the committee encourages participation to gather a wide range of insights and experiences.
This dual activity, a strategic action plan and a detailed inquiry should go some way in addressing the pressing challenges faced by New Zealand's aged care sector. By fostering collaboration between the government, communities, and industry experts, the sector can build a robust, sustainable, and compassionate aged-care system that meets the needs of its aging population now and in the future.
Tania Walters, Publisher tania@reviewmags.com
PUBLISHER: Tania Walters
GENERAL MANAGER: Kieran Mitchell
EDITORIAL DIRECTOR: Sarah Mitchell
EDITOR-IN-CHIEF: Caitlan Mitchell
EDITORIAL ASSOCIATES: Sam Francks, Jenelle Sequeira
ADVERTISING SALES: Caroline Boe
SENIOR DESIGNER: Raymund Sarmiento
GRAPHIC DESIGNER: Raymund Santos
ISSN 2815-7478 (Print) ISSN 2815-7486 (Online)
Retail 6, Heards Bldg, 2 Ruskin St, Parnell, Auckland New Zealand P: +64 3040142 Email: edit@reviewmags.com

6 Village News
8 Malnutrition Crisis
The largest aged care nutritional study in Australian history has indicated that 40 percent of people living in residential aged care are malnourished. A further six percent are severely malnourished.
9 Registered Nurse Success
The Australian Government is pleased with the rate at which the 24/7 Registered Nurse Responsibility programme has grown since it was launched.
10 Savings in Both Time and Money HUBSCRUB is the unique and completely automated wash and UV disinfection system trusted by more hospitals and aged care facilities than any other.
12 Committee Inquiry for Better Care
Determining the future capabilities of the aged care sector has been a priority for the Health Select Committee’s inquiry.
14 Dementia Rates Skyrocket
The UK National Health Service (NHS) has released figures that show a record number of dementia diagnoses across England.






16 Driven by Passion
As the recently appointed Chief Executive of the Aged Care Association (ACA), I am both honoured and excited to step into this role.
20 Global Innovations
As the Chief Executive of Ryman Healthcare New Zealand, my mission is to help our residents live their best lives by providing exceptional care and support. We are committed to enhancing freedom, connection and wellbeing for people as they grow older.
24 New and Improved Facilities
Metlifecare and Palmerston North Māori Reserve Trust have officially opened the completion of 43 new two-bedroom independent living villas, marking a significant expansion of Metlifecare’s existing Palmerston North Village.
26 Faces of Aswathy Sreedas Since arriving in New Zealand, Aswathy Sreedas has worked her way through the aged care sector with Ryman Healthcare.
28 Meet the Chef André Kassal - Edmund Hillary Village For German-born chef André Kassal, it was the world’s finest brown trout that brought him to New Zealand’s shores.


AUSTRALIA | Sector leaders have called for all of Australia's retired population to be vaccinated against COVID-19 amid a global resurgence.
Aged Care Quality and Safety
Commissioner Janet Anderson said there is no excuse for any residential aged care service to be underprepared for COVID-19.
More than four years after COVID-19 was first detected in
Australia, every aged care provider should know what they need to do to reduce the risk of, prepare for, and minimise the impact of a COVID-19 outbreak. Providers are expected to have in place the necessary systems and processes to fulfil their obligations and safeguard residents’ health and wellbeing as far as possible.
Read more here

NEW ZEALAND | Health Minister
Dr Shane Reti officially opened Tōtara Haumaru, the country’s newest hospital facility, on Auckland’s North Shore Hospital campus. The first patients were welcomed into the 150-bed facility earlier this month which will serve the Auckland and Northland communities well into the future.
In opening the new facility, Dr Reti acknowledged the significant benefits the new building would bring to the entire region and
beyond, and the contribution it will make to planned care wait lists.
His sentiments were echoed by Brad Healey, Director of Operations at Health New Zealand’s North Shore Hospital.
“This is a fantastic facility which not only houses some of the most up-to-date clinical facilities in the country but has also been thoughtfully designed by our people to provide a welcoming environment for patients and their whānau.
Read more here

AUSTRALIA | AI is already transforming healthcare. What do we need to watch for?
Artificial intelligence (AI) is rapidly transforming the healthcare industry, offering numerous benefits such as improved diagnostics, personalised treatments, and streamlined administrative processes. What do the public, patients, and healthcare professionals think of the use of AI in healthcare?
Analysing 105 publications spanning 2001 to 2021, Monash University explored the perspectives of the general public, patients, and healthcare professionals on the use of AI in healthcare. More specifically, it extracted information on how knowledgeable and familiar with AI they saw themselves, what they viewed as AI’s benefits, risks, and challenges, and how acceptable AI was to them. The team also examined what patients, the public and healthcare professionals thought of AI’s development, implementation, regulations, and the Human – AI relationship.
Despite widespread positive attitudes toward AI integration, stakeholders voiced concerns, including data privacy, algorithmic bias, and professional autonomy. Read more here
NEW ZEALAND | Ensuring the health system has the necessary ‘digital and physical infrastructure’ requires more than just words, according to the Digital Health Association (DHA). Adequate and ongoing funding is essential to building a robust and state-of-the art digital technology ecosystem.
Ryl Jensen, chief executive of the DHA, acknowledged that the Government Policy Statement (GPS) on Health emphasises the need for digital initiatives and solutions.
“At face value, the GPS is encouraging due to its focus on digital health,” said Jensen. Read more here


NEW ZEALAND | Experts are calling for greater support for the thousands of Kiwis aged 65+ who are most at risk of an intensely painful and debilitating disease.[1]
Shingles is a viral infection caused by the reactivation of the varicella-zoster virus, the same virus that causes chickenpox. Even those who appear healthy but are aged 50+ are at risk of developing shingles.
Almost all adults aged over 50 already have the virus that causes shingles lying dormant
in their body due to an initial chickenpox infection. Around a third of these will develop shingles in their lifetime when the virus reactivates.[2]
Shingles can also be intensely painful, and the disease is associated with a range of complications which for some people can include potentially long lasting nerve pain, vision loss, hearing loss, scarring and neurological problems and less common, cardiovascular and stroke events.
Read more here


The largest aged care nutritional study in Australian history has indicated that 40 percent of people living in residential aged care are malnourished. A further six percent are severely malnourished.

he study’s authors, from Monash and Griffith Universities, warn that insufficient processes have meant that many residents are not recognised as being malnourished and remain untreated.
It is estimated that the number of people 60 years and older will double and that those 80 years or older will triple by the year 2050.
The Australian Government has estimated the cost of the malnutrition crisis in residential aged care facilities to be approximately AUD $9 billion a year. A 2021 report by the Royal Commission into Aged Care Quality and Safety outlined that there had been a failure to meet the nutritional needs of people by operators of the residential aged care sector for whom they care.
The Commission specifically identified improving nutrition as a priority area for immediate attention.
The study spanned 10 facilities across New South Wales, South Australia and Queensland, and involved over 700 residents. The median age of residents who partook was 84, whilst 63 percent were female. According to lead author of the study, Dr Jonathan Foo, from Monash University’s Department of Physiotherapy, good nutrition plays a crucial role in healthy ageing.
“Malnutrition is associated with poorer overall health, increased hospitalisation rates, higher rates of falls and fractures, slower wound healing, higher infection risk, and accelerated mortality,” said Dr Foo.
“Despite such risks, aged care providers are not suitably resourced to perform routine screening using validated
tools, meaning many malnourished residents are likely to be undetected and therefore untreated.”
Dr Marie-Claire O’Shea from Griffith University’s School of Health Sciences and Social Work said older Australians deserve better nutritional care, and the time is now when malnutrition is a national problem.
“The rates of malnutrition can vary from home to home with some statistics reporting up to 78 per cent, however, our study, which was significant in number, reported a rate of around 40 per cent,” Dr O’Shea said.
“Early malnutrition identification is just the first step, as improvements in food quantity and food quality are also required. We are working with aged care providers and residents to enhance the dining experience, and we believe this is the key missing piece of the malnutrition puzzle.”
Australia’s aged care sector is responsible for more than 190,000 individuals, and for more than two decades, has encountered significant scrutiny in regard to its handling of the malnutrition crisis.
The study also recommended regular screening, as it has become crucial to identify those who need a full malnutrition assessment and intervention.
“Our research group is currently working on implementing automated malnutrition screening and food-first malnutrition support pathways with our forward-thinking aged care partners,” Dr Foo said.
“The sector is already overwhelmed by all the requirements of providing care to ageing Australians, we need to focus on approaches that overcome challenges rather than burdening providers.”
The Australian Government is pleased with the rate at which the 24/7 Registered Nurse Responsibility programme has grown since it was launched.

ne year on from the introduction of the 24/7 Registered Nurse Responsibility, the Albanese Government is continuing to deliver on its promise to put nurses back into residential aged care.
Aged care homes now have an registered nurse on-site and on duty 24 hours a day, on average 99 percent of the time, which has allowed greater care for older Australians and has continued the Government’s mission to restore dignity to aged care.
About 92 percent of aged care homes have reported having a registered nurse on-site 24/7, a six percent increase from 86 percent in July 2023.
The Government has also seen improvements to the care minutes being delivered in residential aged care. Federal Minister for Aged Care, Hon. Anika Wells, said when the Labor party entered government, it was determined to improve the quality of care for older Australians.
“The fact there is now a registered nurse onsite in aged care 99 percent of the time on average across Australia shows we have delivered,” said Minister Wells.
“Under the Albanese Government, older people in aged care can receive attention from an registered nurse whenever they need it.”
Older people in residential aged care now receive an additional 3.9 million minutes of direct care every single day under the Albanese Government, which has included 1.7 million additional minutes of care from registered nurses.
The sector has also delivered an average of 204.2

total care minutes, which includes 40.2 minutes from a registered nurse.
“This is what caring for our older generation looks like, and I want to thank the nurses who have worked with us to lift the standard of aged care.”
Fewer rural and remote aged care providers have sought an exemption from the 24/7 registered nurse responsibility in its second year, as they have been able to meet or surpass the minimum registered nurse coverage threshold.
This continuous improvement reflects the collective impact of aged care reforms delivered by the Government, including workforce reform, and strong support from the aged care sector, which is committed to providing the best possible care to residents.


HUBSCRUB is the unique and completely automated wash and UV disinfection system trusted by more hospitals and aged care facilities than any other.
ith more than 30 years supplying North American Hospitals and rest homes, Hubscrub has also made significant impact in New Zealand and Australian hospitals and aged care facilities. Hospitals from as diverse a mix as The Prince Albert Hospital in Sydney to Taranaki Base Hospital in New Plymouth appreciate the versatility and effectiveness of its equipment cleaning and infection control system, with demand for units in hospital settings steadily increasing over the past couple of years to now total over 20 units in actions.
Hubscrub now plays an integral role in the cleaning and safety at a dozen or so hospitals and mobility suppliers from Whangarei in the north to Dunedin Hospital in the South. Additionally Enable and Accessable NZ rely on the speed and guaranteed cleaning of Hubscrub to ensure thousands of ACC and community loan equipment are well cleaned between each customer. Cubro and Permobile all rely on Hubscrub for their rental equipment, ensuring each item is as good as new despite frequent rentals.
Following huge demand in North American aged care facilities, Hubscrub is now being made available to Retirement Villages and Aged Care homes in New Zealand.
The key features of being able to wash, sterilise and disinfect a range of medical and mobility equipment quickly and safely with the push of just one button is proving to be very popular with Retirement Village and Aged Care facility management, resulting in increased enquiries to either purchase or lease a Hubscrub.
The ability to both wash and sterilise with its unique UV system, makes the Hubscrub a natural choice in environments with limited space – and stretched personnel.
There are many benefits to using a Hubscrub but the top three comments the Hubscrub team hear are:
• The huge savings in both staff time and money.
• The quality of cleaning and decontamination.
• The ease with which it can be operated – it's quick, efficient and works at the touch of a button!

Hubscrub saves hours in labour and removes the need for manual cleaning – which can be a bit of a hit and miss. Using a Hubscrub instead of manually cleaning and disinfecting assistive equipment can also save thousands of dollars a year. With the cost and scarcity of labour being an immediate issue with many facilities, the purchase or lease of a Hubscrub can make a significant contribution to village operations – and finances.
Hubscrub is the ultimate equipment cleaning and infection control solution with proven effectiveness against infectious pathogens including COVID 19, Sars, C-Diff, MRSA and CRE. Using state-of-the-art UV technology and an automated system that efficiently uses water and chemicals, Hubscrub is the only machine that washes and uses UV technology together - resulting in the most effective and efficient equipment cleaning and infection control system available.
Hubscrub efficiently cleans and decontaminates
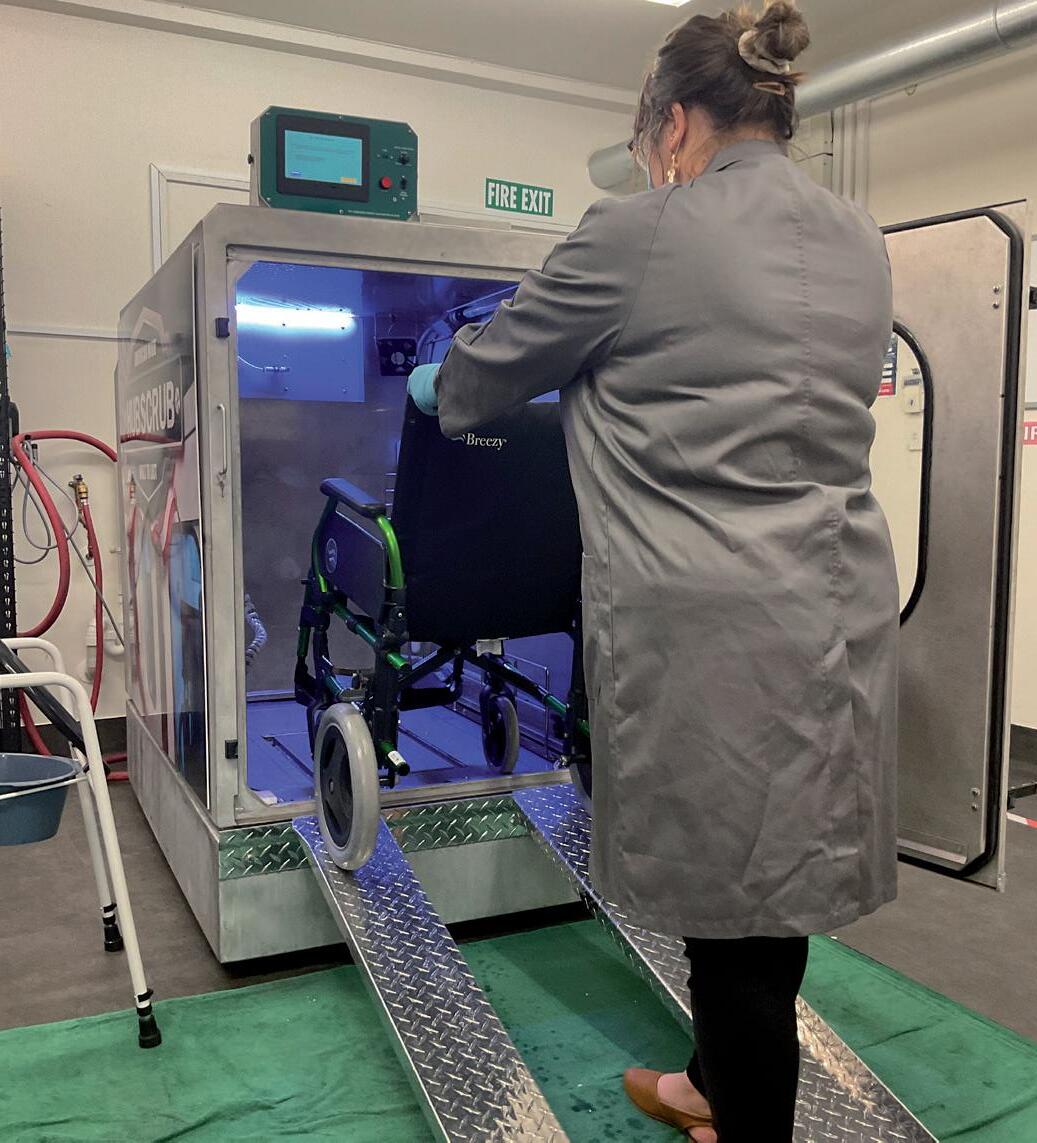
almost all mobility and medical equipment in 6 minutes at the simple push of a button. It also gives the operator a range of cleaning options – including a dry sterilisation UV only option - going far beyond any cleaning system that currently exists in the sector.
HUBSCRUB is trusted by hospitals, aged care and suppliers of assistive products. Used by retirement villages, care homes and hospitals for over 30 years, HUBSCRUB has a proud history of supplying guaranteed equipment sterilisation to hundreds of organisations in New Zealand, Australia, Canada and USA.
With Purchase and Rental options, as well as a mobile service for large one-off cleans, such as following an infection outbreak, there’s a service model to suit your organisation. And because HUBSCRUB is compact and portable, they can demonstrate at your place – all they need is access to power and water!
To find out what other aged care establishments are calling a “breakthrough in infection control”, why not have a trial?
HUBSCRUB are so confident you'll see the benefits of HUBSCRUB, they are offering a 2-hour trial absolutely FREE - at your place* They'll clean and sterilise commodes, wheelchairs, bedpans, walkers and more, totally free.
*Out of Auckland trials subject to availability of HUBSCRUB travelling unit. Offer ends 30 November, 2024, and available only to Aged Plus readers.

Determining the future capabilities of the aged care sector has been a priority for the Health Select Committee’s inquiry.
he inquiry has been called for because of critical concerns of the support for neurological disorders such as dementia.
The inquiry has also fulfilled a Coalition Agreement between National and New Zealand First to undertake a select committee inquiry into aged care provision to include supporting people with early onset conditions and what asset thresholds are appropriate.
Committee chair, Tauranga MP Sam Uffindell, said the inquiry’s concerns were based on ensuring appropriate asset thresholds for sustainable services.
As New Zealand’s population has aged, life expectancy has also increased. The Committee will look into a range of issues related to the aged care sector and what the best outcome

will be for those in need of specialist care. The inquiry will also investigate the sector’s ability to provide care and services to the current and expected number of seniors who are and will suffer from early-onset conditions.
Uffindell said that the inquiry will look at whether the funding model has been updated to reflect the current best provision for these conditions.
“New Zealand’s population is aging, and life expectancy is climbing. It’s the right call for our committee to look into a range of issues related to the aged care sector,” said Uffindell.
The Ministry of Health has begun the second phase of the Aged Care Funding and Service Model Review, which has aimed to improve service sustainability and ensure equitable access and outcomes. Uffindell added that the Select Committee inquiry will have a focus on the early onset provision and could provide valuable insights to support a funding change.
Committee member, NZ First MP Jenny Marcroft, said the committee owed it to seniors to explore a range of issues around aged care and how the Ministry of Health can best support New Zealanders as they age.
Marcroft said there was challenges in the current aged care provision for those with early onset dementia, and that an increasing number who are under the age of 65 also require support. She added that dementia can impact couples who would normally
live together but must be separated due to individual care needs, which required the Government’s attention.
“We are pleased to see progress on this commitment from the National – NZ First Coalition Agreement,” said Marcroft.
The Committee will also examine multiple matters that relate to appropriate services for people with neurological and cognitive disorders across the care continuum, including from home and community care to residential care, to palliative care. The funding model, amount of funding available, including best practice and international examples of funding models will also be examined.
The committee will also explore the current resources available, the health system’s ability to provide appropriate care, and what support enables “aging in place,” including for priority populations.
“The most recent census data shows the population continues to age. It is important that our committee does the work to investigate a range of issues related to the aged care sector, particularly for those with neurological cognitive disorders,” said Uffindell.
“I look forward to working with the public alongside my colleagues on the Health Select Committee collaboratively throughout the inquiry so we can get the best outcomes for our seniors.”

The UK National Health Service (NHS) has released figures that show a record number of dementia diagnoses across England.
he latest data showed that an astonishing 487,432 people in England had a diagnosis in June. Although dementia diagnosis rates have been at the highest point since the start of the Covid-19 pandemic at 65 percent, the NHS is still confident it will meet its goal of diagnosing 66.7 percent of the total number of people that could live with a form of the disease without being aware.
NHS staff across the UK have proactively assessed care home residents to support the identification of people who may have dementia in order to boost numbers further

for patients and their families.
England has one of the highest dementia diagnosis rates in the world, with highincome countries typically in the range of 20 to 50 percent.
A timely diagnosis of dementia has become a vital concern for officials, so more people can get the support and care they need to live with the illness.
England’s top dementia doctor, Dr Jeremy Isaacs, has praised the hard work of staff in their efforts to boost diagnosis but acknowledged there is still more to do. Dr Isaacs, who is the national clinical director for dementia in the NHS, said that getting a diagnosis of dementia was the first step in supporting people, as there is a wide range of NHS services able to help.
The NHS has encouraged people to come forward and get checked if they have any common early signs or symptoms of dementia.
“NHS staff have worked hard to recover services with the number of people with a diagnosis rising significantly over the last year, and now at a record level, but there is more work to be done,” said Dr Isaacs.
“Thousands more individuals are being diagnosed each month and more medication reviews are being done within 12 months.
Dr Isaacs said that common early symptoms of dementia include forgetting
Thousands more individuals are being diagnosed each month and more medication reviews are being done within 12 months.
bits of information, saying the same thing repeatedly, struggling to follow a conversation or find the right word and being confused about time and place. Usually, these problems will be more obvious to the person’s family and friends than to the individual themselves.
The latest figures show that 86,434 people diagnosed with dementia had their medication reviewed in the preceding 12 months. In contrast, the figure for June 2023 was 77,112.
In 2022, the NHS England announced 14 new pilot schemes in which specialist nurses and other healthcare professionals proactively assess care home residents for dementia.


TRACY MARTIN Chief Executive
Aged Care Association
As the recently appointed Chief Executive of the Aged Care Association (ACA), I am both honoured and excited to step into this role. My decision to apply for this role was driven by my passion and unwavering commitment to ensure that all of our seniors receive the care they need when and where they need it.

s the Minister for Seniors from 2017 to 2020 I witnessed firsthand the dedication and resilience of those working within the aged care sector - a sector that has for too long has been under-resourced and underappreciated by those with little knowledge of the diverse needs that provide for.
My time as Minister deepened my understanding of the complexities involved in caring for our older New Zealanders, and I am eager to use this experience to support the aged care sector in the ongoing fight to provide excellent care, dedicated support and appropriate resourcing for the growing number of elder New Zealanders.
It is crucial that every government, whatever the political landscape, recognises


that our seniors are not just numbers or statistics, they are their people. They are fellow New Zealanders who are entitled to quality care, regardless of their age.
In the coming months, I will be focusing on a few key areas:
Working to raise the profile of the coming wave of older New Zealanders and the vital part our sector does and will play in the provision of their health and wellbeing; Engaging directly with politicians, media and stakeholders across New Zealand to spread the understanding of our sectors reality: that on average, entry into residential care is happening at a more advanced age, with greater co-morbidities and for shorter periods of time;
Continued on page 14.

Continued from page 15.
Improving the provision of dementia and psychogeriatric care, enabled through either a more realistic day rate and/or access to capital for new builds.
Through the New Zealand First – National coalition agreement we have been presented with a timely opportunity to highlight this last point.The Health Select Committee has officially opened public submissions for the Inquiry into the aged care sector’s current and future capacity to provide support services for people experiencing neurological cognitive disorders.
We encourage all those involved in providing care for residents with neurological cognitive disorders - whether you are a care provider, supplier, or support service - to submit, both in writing and orally, to the committee so that we do not miss this chance to give the Select
Committee members an “in colour” picture of the reality of this work and its challenges. We firmly believe that there must be multiple styles of provision for aged care and view the Inquiry as an opportunity to make this clear to Government and decision-makers. We are advocating for a future that offers a variety of care options to cater to the increasingly diverse needs of our elderly population. Residential care facilities, while an excellent solution for some, cannot accommodate all individuals, especially those with more complex needs such as violent behaviours. Similarly, staying at home is a wonderful option for many, but it is not feasible for every individual or their whanau. The ability to age at home or in the community can be constrained by the cost, time commitments, and availability of appropriate support – be it support from

family, friends, or professional in-home healthcare.
Our vision for the future of aged care emphasises the importance of co-design, ensuring that those who are directly involved in delivering services have a significant role in shaping the delivery models developed by Te Whatu Ora.
The voices of those on the front lines of aged care delivery are critical in this endeavour. By participating in the public submission process and sharing your experiences and insights, you can help ensure that the Select Committee appreciates the full scope of the challenges the sector faces. If you need help navigating the submission process or have questions, please reach out.

Our vision for the future of aged care emphasises the importance of co-design, ensuring that those who are directly involved in delivering services have a significant role in shaping the delivery models developed by Te Whatu Ora.

As the Chief Executive of Ryman Healthcare New Zealand, my mission is to help our residents live their best lives by providing exceptional care and support. We are committed to enhancing freedom, connection and wellbeing for people as they grow older.

CHEYNE CHALMERS Chief Executive Ryman Healthcare New Zealand

o achieve this, we stay up to date with global advancements in aged care and retirement living, and continuously explore new innovations to ensure we are always pursuing the best ways to support our ageing population here in New Zealand.
Here are some of the innovations from around the world that are shaping the future of aged care and retirement living.
Ageing in place means that as we grow older, we have the flexibility to remain in our homes. In a retirement village setting, this means supporting residents so they can continue living independently while receiving care rather than moving to a care centre. Digital innovation plays a huge role in this.
In the UK there over 10,000 NHS virtual wards (also known as hospital at home) available across England and at least a further 15,000 are planned. Virtual wards provide hospital-level care at home (or in care homes) using technology such as apps, wearables, and daily virtual check-ins by medical staff, aiming to monitor

and manage patients remotely, freeing up hospital and aged care beds for others.
Evidence shows virtual wards work well for seniors who are at the highest risk of hospital admission, as well as those eligible for discharge to continue treatment at home. They reduce the risk of hospital complications and deconditioning.
Alongside this, virtual assistants and chatbots support health professionals with treatment advice and patients with care information, connecting them to electronic health records, scheduling appointments, and medication reminders.
As we grapple with the challenges of an ageing population in New Zealand including the increasing shortage of care beds, we anticipate that technology will play an increased role in helping our seniors to live independently for longer.
We know that isolation and loneliness can have a serious impact on older people’s longevity, physical and mental health, and we are now seeing innovative ways to combat this with the latest tech.
Virtual reality is emerging as a powerful wellbeing tool among seniors through immersive digital therapies. Eidsvold Hospital in Queensland has adopted this by offering virtual travel, social interactions, and therapeutic activities, with aged care patients reporting immediate health benefits and a sense of freedom and connection.
Also in Australia, a care home in Sydney uses an AI-powered robot, ‘Viv’, to support dementia patients by providing companionship and engaging them in conversations. Developed with input from people
Continued on page 18.



Continued from page 17.
living with dementia, Viv assists care staff, offering a consistent and reassuring presence when they are not available.
One example of leading global dementia care involves whole villages that are cleverly designed to combine an outdoor environment and a sense of freedom with security to protect resident wellbeing. The Hogeweyk model in the Netherlands replicates a village feel within a secure complex, including hairdressers, restaurants, and local supermarkets giving residents a sense of community and autonomy. Technology supports the sense of freedom in the Hogeweyk model through innovative alert systems and clever lighting design. To minimise the risk of residents falling, infrared beams detect if a resident is leaving their bed in the night, alerting staff who can

quickly assist. Additionally, circadian lighting mimics natural light phases to help regulate sleep cycles for people living with dementia who have lost their natural wake and sleep cycles.
Lifelong learning and digital education
Picking up a new skill or pursuing a new subject matter can slow cognitive decline and the benefits of continuing education are emotional as well as cerebral. This is why we offer residents a wide range of activities aimed at stimulating their minds and bodies, such as art lessons, learning a language, and exercise classes.
In the US, University Based Retirement
Communities combine residential senior care with learning opportunities from local colleges and state universities. These facilities are like traditional campus housing but are specifically designed for seniors 55 and older. In more traditional retirement villages, operators are regularly bringing in guest lecturers and designing on-site education plans to support residents to continue to learn as they age.
As well as adopting technology to support our aged care and retirement facilities, our sector must find ways to enhance the digital skills of older citizens so that as we see more innovations come to market, they are confident in using them. The technology emerging to support all areas of ageing is exciting and can help assist our carers, our residents, and their families.
Metlifecare and Palmerston North Māori Reserve Trust have officially opened the completion of 43 new two-bedroom independent living villas, marking a significant expansion of Metlifecare’s existing Palmerston North Village.

he two parties celebrated the official opening of the new villas, with a special kōwhai planting and plaque unveiling ceremony.
The celebration was attended by leaders and team members from the co-owners, village residents and staff, local building contractors Humphries Construction, and Palmerston North Mayor Grant Smith.
Earl Gasparich, CEO of Metlifecare, said there was a strong connection between Metlifecare and the Palmerston North Māori Reserve Trust.
“The successful completion of this development is testament to the highly constructive partnership we have with the Palmerston North Māori Reserve Trust,” said Gasparich.
“With the village expansion now complete, Metlifecare can offer even more premium retirement living accommodation options to the people of Palmerston North and the wider Manawatū region. Once fully occupied, this expansion will effectively double the size of the village community.”
Gasparich said that given the village’s convenient location between Ngata and Carroll Streets, which is close to the central city, it has proven to be a popular choice over many years for local retirees.
“The new villas seamlessly connect to the existing village through landscaped walkways and a dedicated road crossing, so residents can enjoy all the facilities this friendly, and wellestablished village has to offer.”
Liz Mellish, Chair of the Palmerston North

Māori Reserve Trust, said the expansion was a result of its partnership with Metlifecare.
“Our two parties have been in a successful partnership for almost 30 years now. This latest development is a great example of bringing together the expertise and knowledge from both partners in pursuit of a beneficial outcome, not only for both parties, but importantly, for the people of Manawatū,” said Mellish.
“The Trust has provided local knowledge of the market and introduced the land opportunity to expand living options in what is a popular destination for local retirees.”
Mellish added that Metlifecare’s insight was key to the success of the expansion.
“Metlifecare provided in-house expertise to design and manage the development through


The successful completion of this development is testament to the highly constructive partnership we have with the Palmerston North Māori Reserve Trust.
Earl Gasparich CEO Metlifecare
to completion. We’re very proud of the result, which has maximised the potential of this once-vacant site.”
The village expansion project commenced in September 2021. Stage one of the project, consisting of 23 villas, was completed in July last year, and this final stage (Stage two) signals the completion of the remaining 20 villas.
The Palmerston North Village is owned and operated under a joint venture partnership between Metlifecare and Palmerston North Māori Reserve Trust.

Since arriving in New Zealand, Aswathy Sreedas has worked her way through the aged care sector with Ryman Healthcare.
“I find working in aged care is a job that is very rewarding and meaningful. We get a lot of opportunities to make positive changes in others’ lives. That gives me job satisfaction,” said Sreedas.
She added that her role has a good worklife balance, which has been important to her.
Kiri Te Kanawa Clinical Manager, Sunny Sandeep described Sreedas as someone who always goes above and beyond, who has great leadership skills, has built a wonderful hospital team, and who is always approachable and accountable. Sreedas added that she wouldn’t have been able to succeed without the support of her managers.
“I have a great bunch of staff who always listen and follow as we guide. Altogether, we have a great team here.”
reedas completed her nursing qualifications in 2011 in India, and after three years, she came with her family to complete her postgraduate diploma in health management in New Zealand.
In 2015, Sreedas began working as a senior caregiver at Ryman’s Hilda Ross Retirement Village in Hamilton, whilst waiting to do her CAP course from the Waiariki Institute of Technology. After that, she began working as a registered nurse at the Kiri Te Kanawa Retirement Village in Gisborne in 2016, and was promoted to unit co-ordinator in 2019, and has been the hospital unit coordinator since 2020.
Sreedas chose the medical profession as she had always maintained a curious interest with how doctors and nurses could cure illnesses, and wanted to know more. At the same time, Sreedas wanted to help people and build relationships too.
Sreedas believed a good leader should be aware of what is goin on around them, should be empathetic and a good listener.
“We need to be spontaneous and have good communication and decision-making skills. It has to be the right staff in the right place, and they need to have a good skill mix, kindness and who work well in a team.”
In order to remain approachable with her team, Sreedas introduced weekly huddles with all her teams. Most team members will raise their concerns in the meetings, whilst some come to her privately to discuss matters. Sreedas said that she will always find the time to listen to their concerns and will give them feedback on what she has done about it.
Outside of work, Sreedas enjoys relaxing with her husband and three children. In the future, she has plans to complete her postgraduate diploma and masters degree in nursing in the coming years.

I find working in aged care is a job that is very rewarding and meaningful. We get a lot of opportunities to make positive changes in others’ lives. That gives me job satisfaction.


Meet the Chef
André Kassal EDMUND HILLARY VILLAGE
For German-born chef André Kassal, it was the world’s finest brown trout that brought him to New Zealand’s shores.

fter following his passion and working on a cruise ship, the self-confessed fishing addict worked in the Franz Josef region. He soon swapped the snow-capped mountains for the sails of Auckland’s harbour, working at popular Ponsonby eateries such as Sidart and large catering companies.
Whilst fishing remained his passion, his busy 70 to 80-hour week schedule left Kassal no spare time. His introduction to the aged care sector coincided with his desire for change. His wife, a registered nurse at Ryman’s Grace Joel Village, encouraged him to apply for a chef vacancy at the Edmund Hillary Village, where he has been ever since.



It wasn’t long before Kassal was appointed Senior Lead Chef, and he hasn’t looked back. Kassal said that the role has provided a better work-life balance, and the hours are not as ridiculous as before. He added that a highlight of the role has been the ability to interact with the residents.
Another highlight for Kassal was the launch of the new Chefs Table initiative. This is where a select number of residents are invited to have lunch with the Chef and see how the kitchen operates behind the scenes. He said residents are often surprised at what the team can do.
The kitchen team at Edmund Hillary Village prepares more than 400 meals daily for residents and at least 300 morning and Continued on page 28.


Continued from page 27.
afternoon teas as well. This can be a difficult task, as there are requirements for a balanced diet that caters to a range of needs but with plenty of variety. Kassal said this posed a challenge he was willing to face.
“The whole system is quite impressive; providing variety throughout the four-week cycle involves a lot of planning,” he said.
As Kassal’s previous experience has included working in five-star hotels and fine-dining restaurants in Europe, he has been able to showcase some of his impressive culinary skills at special occasions within the village, such as the fortnightly fine-dining nights.
Some of his courses have included a

vegetarian entree of roasted cauliflower puree topped with goat’s cheese, brown butter, watercress, and toasted almonds. For the main course, Kassal presented beef cheeks and braised carrots on ageing wholegrain mustard mash, followed by creme brulee and berries for dessert.
While fishing is his passion, he enjoys braising meat in the kitchen the most.
“Cooking a steak, beef cheek or lamb shank. I like it to be tender but not falling apart. I really enjoy this type of cooking,” Kassal said.
“European dishes are really where my strength lies. I know them inside out, and I can do them with confidence.”




European dishes are really where my strength lies. I know them inside out, and I can do them with confidence.

“I’ve swapped brie and other soft cheeses for hard varieties like cheddar, parmesan, emmental and pecorino. And if I can’t do without my brie, I always have it baked or on a pizza.”
As you age, foods you safely ate in the past may no longer be safe to eat.
