n this issue, we look at the challenges in care for those with dementia and also how it can impact eating habits. Almost 70,000 Kiwis are living with dementia currently, with an estimated 170,000 Kiwis likely to be living with dementia by 2050. Dysphagia, which can become a concern with older adults comes with additional challenges when the resident has dementia. It can lead to a loss of interest in food, refusal to eat, or even spitting food out. It’s not uncommon for someone with dementia to become agitated or display challenging behaviour during mealtimes, which can make the experience even more challenging. When a person isn’t eating enough, resulting weight loss and reduced muscle strength makes the resident more vulnerable to falls, infections or be slower to recover from illness. Dysphagia also increases the risk of malnutrition and dehydration and several physical factors can contribute to poor appetite. Difficulties such as problems with teeth, chewing, swallowing, or constipation can make eating uncomfortable. In the case of dysphagia,
the swallowing reflex may be weakened, leading to coughing, choking, or food becoming lodged in the throat.
Communication barriers with residents with dementia can also complicate mealtimes as they may struggle to express hunger, a dislike for a certain dish, or discomfort if the food is too hot. In such cases, they might refuse to eat or hold food in their mouth. Offering choices or using visual aids can help them better communicate their preferences.
Tiredness and difficulty concentrating may cause a person with dementia to abandon meals partway through. Supporting them to eat when most alert can make a significant difference.
Tania Walters, Publisher tania@reviewmags.com
PUBLISHER: Tania Walters
GENERAL MANAGER: Kieran Mitchell
EDITORIAL DIRECTOR: Sarah Mitchell
EDITOR-IN-CHIEF: Caitlan Mitchell
EDITORIAL ASSOCIATES: Sam Francks, Jenelle Sequeira
ADVERTISING SALES: Caroline Boe
SENIOR DESIGNER: Raymund Sarmiento
GRAPHIC DESIGNER: Raymund Santos

Bringing the Comforts of Home to Aged Care: Creating Inviting Social Spaces
Aged care facilities don’t have to compromise on the comforts of home.
Supporting the aged care sector with work-based training for 30 years Thirty years and still going strong.
Welcoming A New Voice
Michelle Palmer has taken over from John Collyns as Executive Director of the Retirement Villages Assoication.
Offering the Best Quality of Life For any retirement village, the mobility and care of residents is the top priority.

The Benefits of Daylight Magnifier Lamps for the Elderly
As we age, certain tasks that were once second nature can become more difficult.
Supporting Aging Memory
Over the course of three years, a team from Western Sydney University’s MARCS Institute for Brain, Behaviour and Development created a flexible technology solution that can support daily living activities.
Commissioner Celebrates World Alzheimer’s Month
Aged Care Commissioner Carolyn Cooper has acknowledged World Alzheimer's Month.
Stigma Impact for Dementia
New research has highlighted the toll and main impacts that families and loved ones experience.
Driving change through education: A new approach to dementia care
As we move into an era where one in four New Zealanders are expected to experience some form of cognitive decline.
Appointment at Maggie Beer Foundation
The Maggie Beer Foundation has appointed Jane Mussared as CEO.







Subhashni Sharma has been a hairdresser with Ryman Healthcare for nearly seven years.
As retirement villages have become dynamic hubs for residents, a standout addition has been the inclusion of hair salons.
Arvida's
Ryman
The controversial star rating system in the Australian aged care sector has come underfire by a raft of industry leaders.

AT RADIUS TAUPAKI
GABLES in Taupaki, creativity and sustainability go hand in hand. Located on the busy Taupaki Road, the care home’s community exchange station offers a space for residents and passersby to share, recycle and repurpose everyday items, from toys to books. What began as a simple idea, modelled after similar initiatives in the area, has evolved into a vibrant hub.
“We saw the potential in creating a space where things could be reused, not discarded,” said Laurel Winwood, manager of Radius Taupaki Gables.
“The traffic passing
AUSTRALIA | As it's population ages, the Australian aged care sector is poised for significant growth following recent momentum.
The Australian Retirement Villages and Aged Care sector collectively account for approximately 430,000 places. This was uncovered by recent data accumulated to project how and when the next generation of Australians will retire, and what challenges may be encountered over the next two decades.
Recent market insights from CBRE Group have
by means there’s always someone stopping to drop off or pick up something, keeping the station lively and fresh.”
Popular items like children’s toys and books are snapped up quickly, and the station’s constant turnover keeps people coming back for new treasures.
Residents lead the charge
The residents of Radius Taupaki Gables are deeply involved in the home’s sustainability efforts.
“Our residents are active and intrigued by what we’re doing,” said Winwood.
“During resident
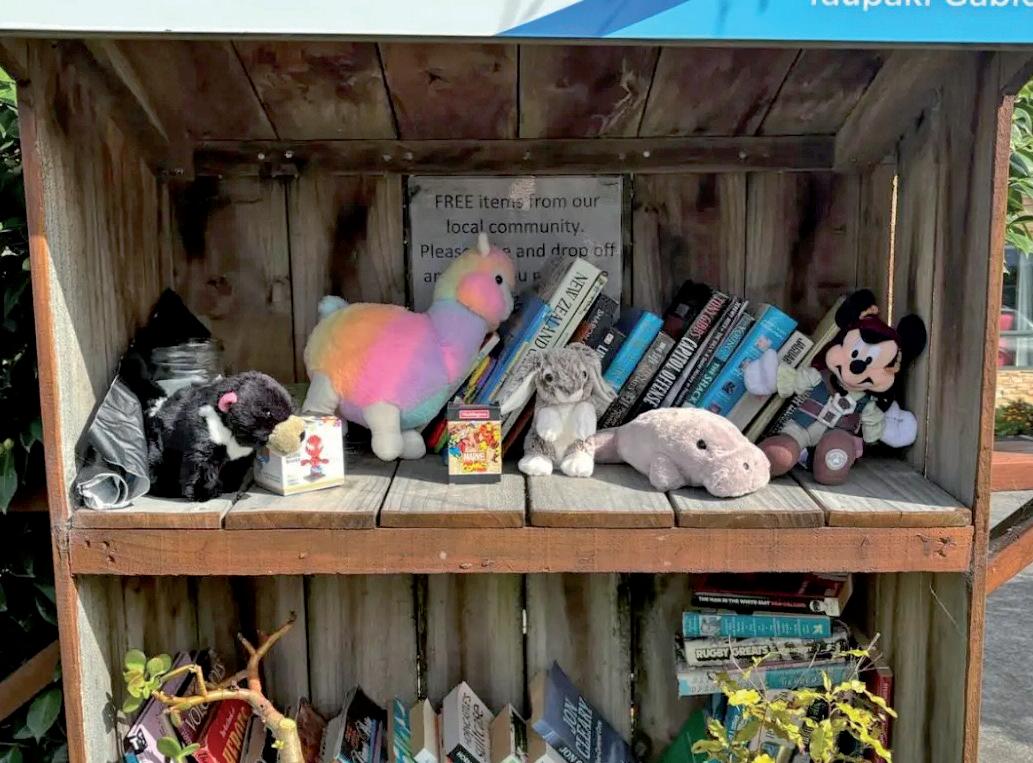
meetings, they’re full of ideas for new initiatives, and we love exploring what’s next.”
These efforts extend beyond the exchange station. Staff and residents have creatively turned old carpets into mini-golf courses, used bottle caps as bingo counters, and transformed discarded
furniture into computer desks. Raised garden beds produce silverbeet and tomatoes for the kitchen, with residents happily tending to the plants.
“We had a bumper crop of tomatoes last summer, and we’ve been enjoying silver beet more recently,” added Winwood.
Read more here

estimated that the senior housing sector is nearly four times larger than student accommodation and 10 times larger than the current build-to-rent sectors.
Although it’s population demographic has a commanding lead, the sector has lowlevels of institutional ownership and we foresee significant opportunities
for consolidation. For example, the market share for top five operators in retirement villages is ~13 percent and aged care ~17 percent.
Read more here

Over the last 30 years, we have supported tens of thousands of aged care staff to achieve life changing and nationally recognised qualifications, all via our work-based learning programmes. Employers have the confidence of knowing that their staff have demonstrated the required competencies, and ultimately deliver a better standard of care to residents. For 15 reasons why you should entrust your workforce development to Careerforce, check out careerforce.org.nz/careerforce-difference careerforce.org.nz/aged-care 0800 277 486 YEARS Celebration 1994 - 2024
AUSTRALIA | The Government has announced an investment to support the aged care sector, in order to deliver a higher standard of care for Australian seniors.
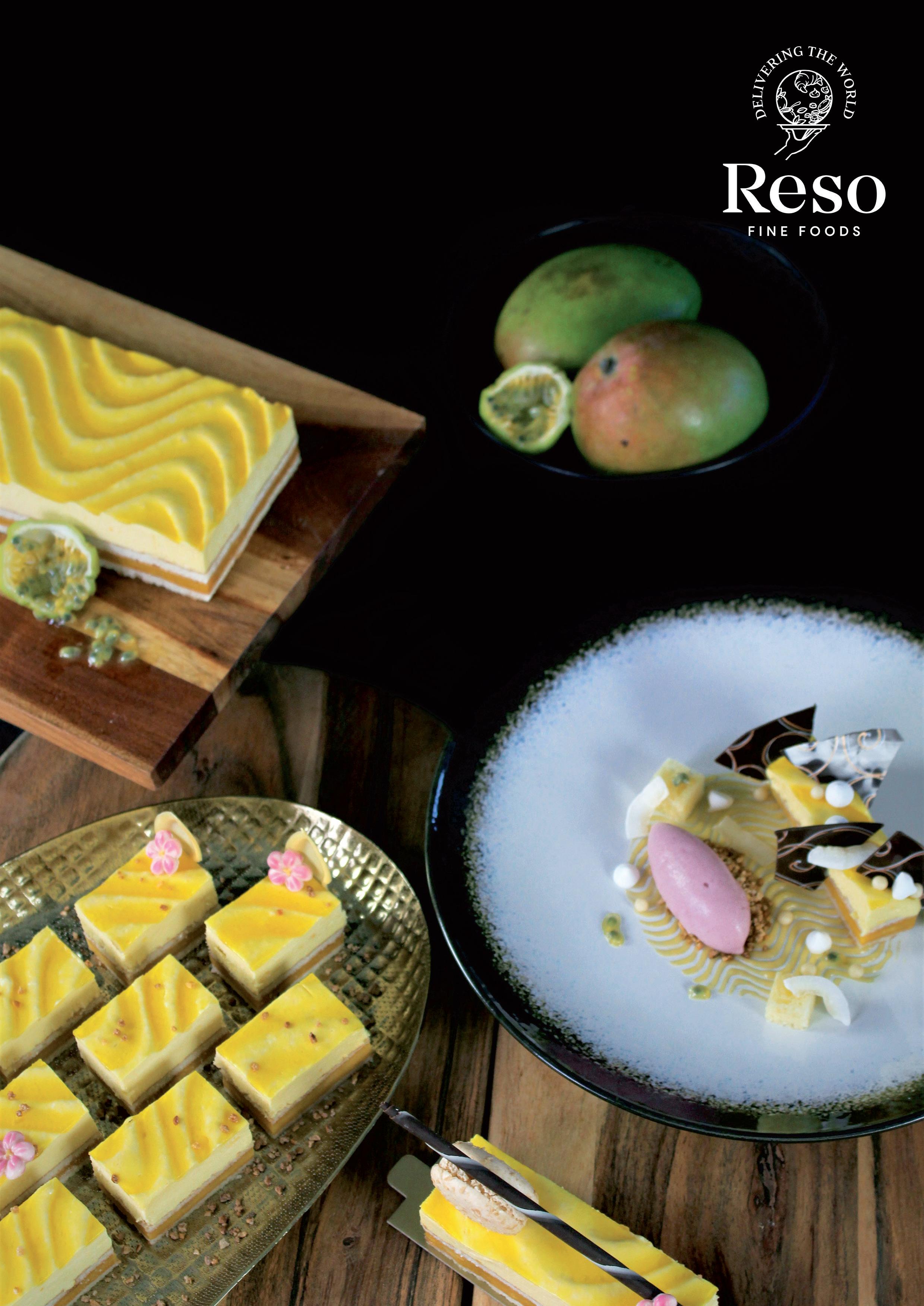
AUSTRALIA | What do mangoes, mint and papaya share in common?
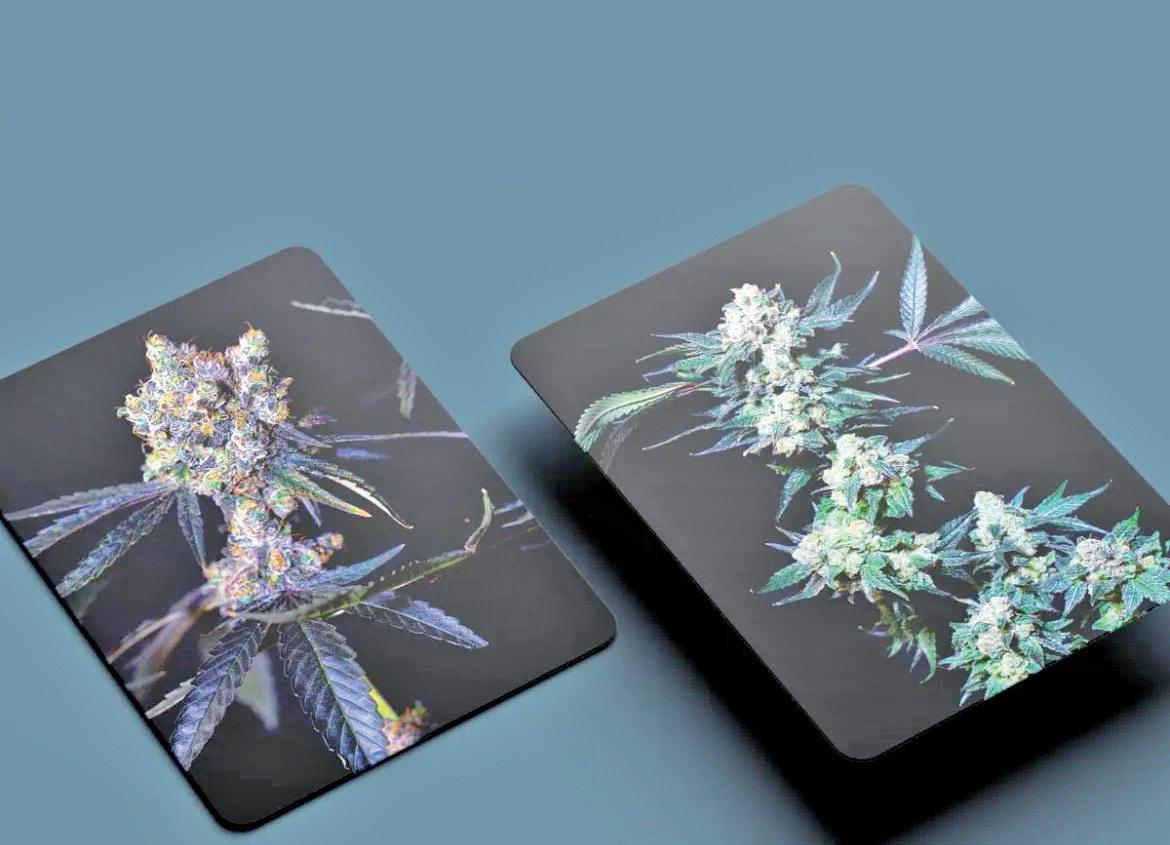
Biortica Agrimed, Australia’s largest B2B grower of medicinal cannabis continues to make new genetic varieties available to the Australian market and so to Australian patients.
Mango Mintality and Papaya Bomb are just 2 of the 49 new varieties most recently imported by Biortica from it’s wholly owned Canadian subsidiary Apollo Green, owner of one of the world’s largest libraries of medicinal cannabis genetics.
Mango Mintality is a leader from Purple City Genetics of Oakland, California, displaying vigorous growth and high flower yields.
Lime green flowers heavy with orange pistils characterise this genetic, which exhibits the scents of ripe mango together with crisp minty notes. Read more here
The Albanese Government is investing AUD $3.8 billion over four years to support the aged care sector and deliver a higher standard of care for older Australians, by funding pay rises for workers from the first of January 2025.
This AUD $3.8 billion
investment will fund the Fair Work Commission Aged Care Work Value Case Stage Three decision, which is anticipated to benefit 340,000 aged care workers in residential and home care.
This funding builds on the Government's $11.3 billion commitment in 2023, to fund the previous 15 percent award wage increase determined by the FWC and is on top of the $5.6 billion announced by the Prime Minister last week. Read more here


MULGRAVE’S NEWEST retirement living community will proudly bear the name of one of
Australia’s most respected sportsmen. Ryman Healthcare announced its ninth
Australian retirement village will be named in honour of Sir Hubert Opperman.
Affectionately known as ‘Oppy’, the legendary endurance cyclist joins Weary Dunlop, Nellie Melba, John Flynn, Charles Brownlow, Deborah Cheetham, Raelene Boyle, and Bert Newton in having a Ryman village named after him.
A multi-record breaker and Europe’s most popular sportsman of 1928, Opperman exemplified a life lived remarkably, putting Australian cycling on the map at competitions including the Tour de France, The Paris-BrestParis, and Bol D’or.
Read more here

ON THIS NATIONAL Diversional and Recreational Therapy Day, Bupa has highlighted the inspirational work and dedication of its staff. It’s National Diversional and Recreational Therapy
Day and Bupa has celebrated some of its own specialised team.
Bupa Northhaven Care Home Diversional Therapist Jayne Weir recently returned from the National Therapists
Conference in Auckland, where she won an award for her ‘Sea for All’ entry – an immersive solution for sea loving residents. Weir came up with the idea of an adaptive sea chair after listening to her
residents and, wanting to do more, she did something about it.
“It started with a conversation with a resident reminiscing about her love of the sea and how much they missed swimming. So, last summer…. we made it happen. We investigated and found that a local Surf Lifesaving Club has a specially adapted chair for the disabled. We then took a number of residents on the chair and they really enjoyed being immersed in the sea,” said Weir.
“This new outing has been incredibly popular. Many residents only want to go into the sea up to their waists but several enjoy going deeper and floating in the water. Read more here


Aged care facilities don’t have to compromise on the comforts of home. With thoughtful design and the right furniture, these spaces can feel just as welcoming and cozy as any family home. One of the key elements in achieving this is the focus on social and shared spaces where residents can connect with family and friends.

reating a homely atmosphere in aged care facilities involves thoughtful design choices that prioritise comfort, warmth and connection. This includes the use of warm colors, soft furnishings, and ample natural light to create an inviting environment. Comfortable seating areas, designed for both social interaction and private reflection, can significantly enhance the residents’ experience.
Social spaces are particularly important in aged care facilities. Findings from ‘The Social Report 2016’ show that 10% of New Zealanders aged 65-74, and 13% of those aged over 75 feel lonely all, most, or some of

the time. Investing in the social spaces that serve as the heart of the community, where residents can gather with family members, host visitors, and engage in group activities, builds connection equity. Thoughtful design of these spaces can foster a sense of connection and belonging. For example, incorporating flexible seating arrangements allows for both large family gatherings and more intimate conversations. These spaces should be as much a source of joy and connection for the residents as they are an exciting place for grandchildren to visit for catch ups.
The integration of nature into the design also plays a crucial role. Access to outdoor
Continued on page 20.
Continued from page 19.
spaces, such as gardens and courtyards, provides residents with the opportunity to enjoy fresh air and natural surroundings. These areas can be designed to be easily accessible and safe for residents with varying levels of mobility. Indoor plants and natural materials can also be used to bring a touch of nature indoors, promoting a sense of calm and well-being.
The layout and functionality of the space are critical. Open floor plans that allow for easy navigation, along with strategically placed handrails and non-slip flooring, can help prevent accidents and promote independence. Furniture arrangements can be used to demarcate different zones throughout the open plan, such as areas for socialising, dining, and quiet relaxation. Thoughtful design can also facilitate social interaction among residents, which is important for their mental and emotional health, and building on connection equity.
Aged care facilities can create environments that not only meet the physical needs of their residents but also enhance their overall quality of life by focusing on comfort, social spaces, and personalization. These design principles can help transform aged care facilities into welcoming and supportive homes for their residents.
If you’re looking for more options to bring life and a sense of home into your aged care facilities, talk to Harrows today - beautiful tailored furniture for social interaction.
0800 142 233 sales@harrows.co.nz https://harrows.co.nz/spaces/wellness-care/



Thirty years and still going strong
areerforce has been developing work-based training programmes for the health and wellbeing sector for over thirty years. It offers a range of Health and Wellbeing programmes, leading to NZQA recognised qualifications from Level 2 certificates through to Level 5 diplomas.
In September 2024 Careerforce celebrates its 30th anniversary. First established as Community Support Services ITO (CSSITO) in 1994, the trading name changed to Careerforce in 2006. Industry Training Organisation (ITO) consolidation between 2011 and 2016, included mergers with Social Services ITO (SSITO), Building Service Contractors ITO (BSCITO) and Health Ed Trust (HET).
From humble beginnings with just 9 staff in 1994, the organisation has grown to one with over 170 staff supporting over 2000 employers nationally and over 15,000 learners annually. Though trading names and structures have
changed across the 30 years, the one constant has been Careerforce’s focus on workplacebased learning for the health and wellbeing sectors.
According to Rod Bentham, Careerforce Executive Director, “Across our 30 years, we have supported tens of thousands of learners into life changing careers, and this is something that we are immensely proud of. These learners support many of New Zealand’s most vulnerable people, and we can feel confident that we have helped to improve the quality of care and support of these people, through qualifications that our sectors and employers have helped shape across the 30 years”.
Careerforce programmes for the aged care sector
Careerforce programmes cover entry level through to leadership level ranging

Continued from page 13.
from Level 2 Certificates, through to Level 4 Apprenticeships and the Diploma in Leadership and Management, as well as specialist programmes such as the Dementia Care Limited Credit Programme.
As Careerforce programmes are all fully workplace based, employers can have the confidence of knowing that their staff have demonstrated the required practical and theory competencies to the required standard, in an actual workplace setting. Careerforce also recognises that not all learners are the same and has been evolving its learning supports across the past 30 years to recognise these learning differences and improve learner outcomes.
Here are some learner stories that Careerforce has celebrated over recent years.
Ruth Snowden is a proud wahine enriching lives
Thanks to her employer, Oceania Healthcare and Careerforce, Ruth Snowden was very proud to successfully complete her Apprenticeship in Diversional Therapy.
“This has been a big accomplishment for me. I feel very proud that I’ve done it, and
very thankful,” says the Auckland based diversional therapist. Ruth has a natural ability to connect with the elderly, lift their spirits and enrich their lives.
Careerforce Apprenticeship Advisor, Shane Bennet says “It was an absolute pleasure working with this awesomely gifted wahine toa. Ruth has an infectious passion for her residents and supporting her to transfer that dedication into her apprenticeship assignments was a genuine pleasure.”
Support worker Joanna Hood finds that dyslexia is no barrier to success
Joanna Hood is overcoming the challenges of dyslexia to succeed as a diversional therapist at Alzheimers Manawatu. The apprentice helps to run day centre programmes for people affected by dementia across the region and she is bringing joy to people’s lives.
Joanna lives with Irlen Syndrome, a particular type of dyslexia, where the brain is unable to properly process visual information, because of sensitivity to certain wavelengths of light. She quit school early after being told by some of her teachers that she was dumb and would never get anywhere. Her dyslexia was not picked up until much later.
Careerforce Literacy and Numeracy Advisor Cushla Wilson was able to provide
one-on-one support and is helping Joanna to navigate Careerforce’s learning and assessment platform, and work with various tools that can successfully support her apprenticeship training.
Deaf learner Santana Ngawharau has overcome challenges to pursue her goals
Whangārei caregiver, Santana Ngawharau carries out housekeeping and laundry duties at Metlifecare’s Whangārei Park Retirement Village. Being profoundly deaf, Santana’s first language is New Zealand Sign Language (NZSL). She communicates using a combination of lip reading and NZSL.
With her own determination and support from her employer, Santana has completed her New Zealand Certificate in Cleaning (Level 2) with Careerforce and has now enrolled in the Certificate in Cleaning (Level 3) Contagion and Specialised Infection Control programme, also with Careerforce.
Former sports reporter Frank Malley finds his calling
Frank Malley discovered his true passion, supporting elders in a role he was born to do. While Covid ended his career as a sports reporter, a role he held for over 17 years, he is now finding fulfilment working in the rewarding care and support sector.
This has been a big accomplishment for me. I feel very proud that I’ve done it, and very thankful.
A few challenges resulting from the pandemic led Frank to pursue a role at Switzer, a rest home, hospital and secure dementia unit in Kaitaia, and in 2023 started a full-time role as a diversional therapy assistant.
Frank has now qualified in his new chosen career, having completed his Apprenticeship in Diversional Therapy with support from his employer and Careerforce.
Nika Harley is breaking the stigma around aged care work
Central Hawke’s Bay diversional therapist
Nika Harley has ‘found her place’ in aged residential care and wants other young people to consider the career path too.
The youngster from Takapau is an Activities Assistant at Waipukurau’s Woburn Rest Home. It’s a role she never even knew existed.
“I absolutely love this job, it allows me to do everything I enjoy, every day,” says Nika.
Nika’s life is enriched working with those who’ve lived theirs to the full. She has successfully completed her Diversional Therapy Apprenticeship which will enable her to advance her career in the health and wellbeing sector.
To read more about Careerforce learners, visit careerforce.org.nz/news.

Michelle Palmer has taken over from John Collyns as Executive Director of the Retirement Villages Assoication, a role he held for over 17 years.

MICHELLE PALMER Executive Director, RVA
lthough Michelle Palmer became executive director of the Retirement Villages Association (RVA) in August, her interest in the aged care sector dates back 20 years to when her late mother moved into a village.
“I am passionate about retirement villages because I saw the difference it made for her,” said Palmer.
“It was quite an old school village, and if it had the facilities that villages have now, I think she would have made the move earlier – especially a bowling green – but the quality of life and security that she enjoyed there was amazing.”
Palmer has come to the role with a background of senior leadership roles in the public and private sector, including city councils, the Ministry of Health, Director of Partnerships at the Department of Conservation, chief executive of Marlborough Winegrowers Association/Wine Marlborough Ltd and executive director of
Natural Products New Zealand.
“My career has been varied but the common thread has been people, leadership and strategic thinking, being creative and thinking about that value we add as a team and an organisation,” she said.
“I have a deep understanding of how membership organisations work and the people that we serve. For the RVA that is twofold, we’re serving both the operators and managers of villages, and the people who live in the villages.”
Palmer has an understanding of the political world, as her central government experience has given her the knowledge of how the machinery of government truly works.
Her immediate focus is to continue to build on the work achieved by Collyns and the RVA team along with updating processes and continuing with our programme of supporting and upskilling members.
“The review of the Retirement Villages Act is very significant for the sector. We are waiting to hear what comes out from the Ministry of Housing and Urban Development and the Minister on that, which should be very soon, and that will be a priority.”
While the RVA has been supportive of change, its biggest concern is if mandatory buybacks of licences to occupy were imposed.
“We certainly don’t disagree with operators sharing in the pain of a lengthy settlement, regardless of whether it is the operator’s fault or more likely subdued market conditions,” said Palmer.
“But the time that an existing retirement unit is refurbished, put on the market and then sold is just the start of the journey. That new purchaser most usually has to place their house on the market, make a sale and then get settlement before they can move to their village.”
She added that money previously paid by the original purchaser will have repaid the bank, or been reinvested in the village, and there was no pot of money available as some people suggest.
“So the only way that a mandatory period could work would be for villages to hold large lines of credit with the cost that would bring. At the very least it would quickly make smaller regional and charitable villages insolvent and disappear
and increase costs for all parties.
Palmer said the RVA believed a more sensible and fairer way was to have interest applied to the repayment sum after a defined period. This will ensure operators are fully incentivised, as in addition to the interest, they will not be receiving village tariffs or any deferred management fees. But at least they will be able to carry on and ensure the other residents in the village are not disadvantaged.
In terms of challenges, she saw misinformation being spread about retirement villages as an important issue to address.
“We continue to provide a voice of reason and let people know the sector is consistently looking at how we can improve our practices and the experience for residents. This is a sector that has undertaken huge transformation as it has grown and reflected and it will continue to do so. We are very keen to get on with making further changes,” said Palmer.
“Other challenges are rising costs, particularly the costs of construction materials and maintenance, and also the ability to recruit and retain good staff. Those things are a challenge for all sectors and we are not immune to them.”
The ability of retirement villages to rise to a challenge was very clear during the pandemic. Palmer said that villages had to become closed communities and thought they did a remarkable job in managing that and supporting residents. They have recovered very well from the impacts of the pandemic. There is now a huge demand from seniors, with 130 people a week moving into villages around the country.
“We organise regional forums where we encourage operators and managers to get together and connect around best practice, and to share ideas and carry those back to their villages and ultimately continue to provide a better and better experience for residents,” added Palmer.
“I’m looking forward to getting out around the country to meet operators, managers and residents. I’m on a very rapid learning journey and a personal priority is to soak up as much information as possible. I’m tapping into the wisdom and knowledge of people around me who have been in the sector for a long time.”
For any retirement village, the mobility and care of residents is the top priority.

hanges that can occur with aging can lead to problems with mobility, be it unsteadiness whilst walking, falling, or difficulty when standing up.
Muscle weakness, neurological difficulties, joint problems and various diseases are common conditions that can limit mobility. Even mild issues can have a serious impact.
For residents with dementia or Alzheimer’srelated conditions, their mobility can suffer vast setbacks. Having residents stay active throughout the day can help to limit any risks for pressure ulcers and other future complications.
Modifications around dementia or Alzheimer’s residents’ living areas will also improve their mobility. This could be simple adjustments such as handrailings and secured rugs, to ensuring that sufficient lighting is available to reduce hazards.
The Department of Health in Victoria, Australia, supported the argument that mobility and self-care support independence, as well as social connectedness, security, activity and dignity.
In a statement, the Department said that during a hospital stay, a person-centred partnership with seniors was necessary in order to ensure that mobility and self-care are maintained or improved. It also stated that awareness of how mobility restrictions and using gait aids can have a significant impact
on a person’s ability to access their living area and neighbourhood was important. This can result in difficulty maintaining and initiating social connections within their community.
Care for residents with mobility challenges is just as crucial to their safety. Whilst it is a given that retirement villages have sufficient wheelchair access, minimal stairs and handrailing for convenience, offering the best quality of care will put families at ease, knowing their loved ones have been taken care of.
For residents unable to or difficult for staff to move, investing in state-of-the-art hoists will be of great benefit to villages, especially in order to offer the best quality of life and care for residents.
Hoists also allow residents to keep their dignity, especially when the more personal elements of care are concerned. Allowing residents to be transported with as little discomfort as possible will increase options for more dignified personal care. An example of this is how hoists allow residents to access the bathroom instead of being required to wear pads. Better management through the use of hoists will allow residents to maintain their personal privacy and dignity.
Mobility and care equipment within retirement villages are ever-changing. Villages must remain focused on improving the quality of life for residents while ensuring their safety, health, and dignity are all intact


Mobility scooters, walkers and wheelchairs are essential for residents who are unable to walk long distances unassisted. Although useful, there is an element of risk that facility operators should be mindful of in order to uphold the safety of their residents.
However, mobility scooters do not offer the same protection physically as cars do, which has underlined the need for safety precautions.
Allowing residents to familiarise themselves with their mobility scooter will allow them to understand the features and safety guidelines, as well as trust within the scooter. To enable this, allow residents to practise operating their scooters in a safe and controlled environment before they set forth into the public arena.
Encourage residents to be visible when operating mobility scooters, such as the use of proper lighting, reflectors, a flag or a horn. Using mobility scooters in low-light conditions can be a safety hazard, and can often require operators to be vigilant at all times.
any aged care residents operate mobility scooters as a way of connecting with family and friends outside their village, or by simply visiting local neighbourhoods and shopping centres. It helps them to connect and socialise, which also limits the risk of loneliness. As more residents opt for mobility scooter usage, village management should be mindful of the risks associated with mobility scooters when not operated correctly.
Mobility scooters have become an instant tool for residents, and no diving license or warrant of fitness is required to operate them.
Encourage residents to be mindful of pedestrians and drive socially. Allowing pedestrians space on the footpath when manoeuvring and maintaining a safe speed and distance are important to both the welfare of residents and to pedestrians.
Regular maintenance on mobility scooters will ensure the best possible journey for residents. This includes making sure tyres are inflated properly, breaks are checked, and all mechanical components are in a suitable working condition.
Mobility scooters allow residents to have their own independence and can benefit their social interactions as well. Reminding residents on a regular basis to ensure their mobility scooters are in sufficient condition will limit any unfortunate incidents and encourage them to practise safe and social driving whilst out and about.



As we age, certain tasks that were once second nature can become more difficult. Reading the small print on medicine labels, doing hobbies like knitting or crossword puzzles, or simply enjoying a good book can strain the eyes.
ne simple yet highly effective tool for alleviating this is the daylight magnifier lamp, which combines magnification and optimal lighting to improve visibility for older adults.
One of the primary benefits of a daylight magnifier lamp is the enhanced vision it provides. The built-in magnifying lens makes small text or intricate details more visible, reducing the strain on aging eyes. For seniors who struggle with presbyopia, macular degeneration, or cataracts, this can be life-changing. Whether it’s reading a book, working on a crossword puzzle, or even seeing the fine details of a photograph, a magnifying lamp provides the clarity needed without causing additional strain.
Unlike regular lamps, daylight magnifiers are designed to simulate natural sunlight, providing a clear, bright light that is easier on the eyes. This type of lighting is especially helpful for seniors, as it reduces glare and shadows, both of which can contribute


to eye strain. The bright yet diffused light enhances contrast, making it easier to differentiate colors and see fine details. Improved lighting can also reduce the risk of falls, as brighter environments help seniors see obstacles more clearly.
For many elderly individuals, the ability to read independently or pursue hobbies without assistance is essential to maintaining their quality of life. Daylight magnifier lamps empower seniors to remain independent. Whether it’s enjoying a favorite book or engaging in a hobby, these lamps enable them to see clearly without needing constant support from others.
Prolonged activities like reading or crafting can lead to eye fatigue, especially for the elderly, who are already at risk for eye-related issues. The combination of magnification and natural light minimizes the need for squinting and focusing hard on
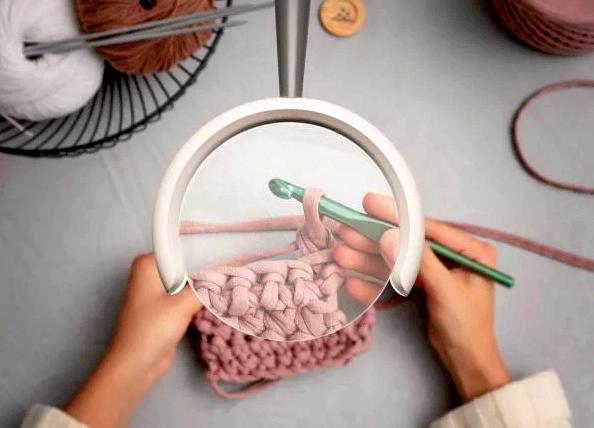

small details, making these activities more enjoyable and less tiring.
In conclusion, daylight magnifier lamps offer a practical solution to many agerelated vision issues. By improving lighting and visibility, they help seniors maintain their independence and continue enjoying activities that bring them joy. It’s a small investment that can make a significant difference in their everyday lives.

Email: office@terrys.co.nz www.terryapparel.co.nz/collections/daylightmagnifiers-lamps/products/daylights-omega-5magnifier
Over the course of three years, a team from Western Sydney University’s MARCS Institute for Brain, Behaviour and Development created a flexible technology solution that can support daily living activities and meaningful technology for those living with dementia.

emoryAId can be delivered flexibly across familiar and existing hardware options already in the home, such as large-screen devices like televisions, tablets, telephone handset attachments, and a small wearable device that can pair with the system to provide alerts.
Professor Celia Harris, project lead, said the modular concept allowed people to select the hardware options that were most suitable for their circumstances and to use what they already have to enable people living with dementia to interact with the technology in ways that they prefer and find most useful.
“This idea came from a lot of background research and talking to people about what they wanted from technology. We knew that it had to be user-friendly, as well as custom-
made for older people,” said Professor Harris. MemoryAId has been designed to require minimal initiation or management once in use and can adapt to the individual needs of dementia patients as individual cases progress.
Throughout development, Professor Harris said consultation with people living with dementia, as well as carers and families, had revealed the value of being able to precisely tailor prompts for the individual needs of the user, highlighting that good technological solutions need to adjust prompts for changes in cognition, including fluctuating ‘good days’ and ‘bad days’, and for changes in support needs over time.
Adjustments to the nature of prompts and activities offered could be made over time to accommodate changes in preferences and

abilities. The concept involved a ‘humanin-the-loop’ approach to smart technology, to make it as tailored, modifiable, and userfriendly as possible.
Research partner Dr Simon Parker, Head of Major Projects at Deakin University’s Applied Artificial Intelligence Institute, said the MemoryAId innovation aims to have transformative impact for people living with dementia by actively enabling and supporting living at home independently for longer.
“Our research to understand the most pressing needs for people with dementia living at home yielded three domains where people wanted support - completing activities of daily living, engaging in meaningful activities, and maintaining social relationships. Our vision for MemoryAId
This idea came from a lot of background research and talking to people about what they wanted from technology. We knew that it had to be userfriendly, as well as custommade for older people.

is that it will be a flexible and customisable platform for meeting all these needs and can support any kind of activity that is valued by a particular individual,” he said.
Professor Harris added that the MemoryAId was a tool for independent use, and that every room in aged care environments could have one. She said it also encouraged social communication, as it would be less hassle for seniors to use.
“We have had a lot of enquiries of people asking where they can buy one, and part of it’s appeal is that it is not a medical device, it’s similar to an iPad. In doesn’t require doctor approval, and could be available to everyone.”
The ‘MemoryAid’ project team was supported by partners at Deakin University’s Applied Artificial Intelligence Institute.
Aged Care Commi-ssioner Carolyn Cooper has acknowledged World Alzheimer's Month as a time for the inclusion of different cultures and languages.

orld Alzheimer’s Month is an international campaign to raise awareness and challenge stigmas about Alzheimer’s and dementia according to the Aged Care Commissioner.
Each year Alzheimer’s and dementia associations, along with those involved in the treatment, care and support of people living with dementia, unite to advocate for action on prevention, diagnosis and treatment for people living with dementia mate wareware.
Around 70,000 people have been diagnosed with dementia in New Zealand, and this is expected to triple by 2050. Dementia has remained underdiagnosed so this is an underestimate of the actual number.
This year’s global theme is ‘Attitudes to Dementia’, which centres on understanding and addressing the current perceptions
towards dementia mate wareware.
A key misconception is that dementia mate wareware is a normal part of ageing and that nothing can be done to prevent it. Evidence suggests that 40 percent of dementia could be delayed by preventative actions like treating hearing loss, improving nutrition, and regular exercise.
One of the recommendations in Aged Care Commissioner Carolyn Cooper’s report, Amplifying the Voices of Older People Across Aotearoa New Zealand, is to support the preventative public health actions outlined in the Dementia Action Plan.
This has included addressing loneliness by investing in community-driven social connection programmes for older people and their families. An increase in the hearing aid subsidy would also provide more affordable access to hearing support to influence another modifiable risk.

Promoting positive attitudes has meant supporting people living with dementia to maintain their dignity, independence and quality of life. Using positive language when speaking about dementia has the power to help build dementia-friendly communities. Words and phrases that treat people living with dementia with dignity and respect can help people feel valued and change how society views and treats them.
“A simple way to change our language, is to avoid labelling people. For example, a person may be living with dementia mate wareware, but they are not a ‘sufferer’. A person may also be experiencing changes in their behaviour, but this is not ‘challenging behaviour’,” said Cooper.
“Behaviours are the things we all do to meet a need, for example, eating when we are hungry. These basic needs do not change for people living with dementia mate wareware, but the behaviour used
A simple way to change our language, is to avoid labelling people. For example, a person may be living with dementia mate wareware, but they are not a ‘sufferer’. A person may also be experiencing changes in their behaviour, but this is not ‘challenging behaviour.
to express a need may change as people’s cognitive abilities decline. It’s important to move beyond labelling behaviours and focus on understanding what the individual is expressing and coming up with solutions to meet their needs.”
Cooper said that is was essential to recognise that the language around dementia is not always appropriate for different cultures and languages. Public health actions for dementia must promote cultural safety and person-centred approaches.
“To build a dementia-friendly society we can all help promote positive attitudes towards dementia. I encourage everyone to reflect on their understanding of dementia mate wareware and normalise conversations around it in their own communities.”

New research has highlighted the toll and main impacts that families and loved of a dementia diagnosis.
oneliness and isolation are some of the major impacts a dementia diagnosis can have on families around the world, new research into the stigma of dementia has shown.
Alzheimer’s Disease International (ADI) has released the World Alzheimer Report 2024 to mark World Alzheimers Month this September. The report has explored the findings of an international survey on global attitudes to dementia –building on the original report from 2019.
The report has highlighted how the impact of stigma has worsened. It shows 30 percent of people with dementia actively avoid social situations and almost 50 percent of care partners stop accepting invitations from friends and family.
Stigma is the attitudes and beliefs people
hold around dementia, while the resulting discrimination can be seen in how people are treated and whether the system supports them.
Sisa Talataina – who is a member of the Alzheimers NZ Lived Experience Advisory Group – is one of the more than 530 Kiwis who responded to the survey.
Her family has been supporting her father, Poa, on his dementia journey since his diagnosis around 2016. She said there is still a lack of knowledge and education within the Pacific community about what dementia is, other than what they have heard, may know or have seen from other family members going through this.
“They say ua fa’aletonu le mafaufau – that there is something wrong with that person’s head or thought process,” said Talatina.
She said she had also heard someone else

say he was going cuckoo, which was very upsetting.
“There’s a real lack of knowledge about dementia in the Pacific community and a lot of misunderstanding and stigma associated with it.”
Alzheimers NZ chief executive, Catherine Hall, said stigma and discrimination can make a dementia journey that much harder by reducing the opportunities available to people at what is already a difficult time in their lives.
“The discrimination is systemic too – what other health condition would struggle to get policy attention and financial support if it was to forecast a 240 per cent increase in numbers?,” said Hall.
“In our case, we’ve already got a Dementia Mate Wareware Action Plan which outlines how we can combat the issue – but we need
The discrimination is systemic too –what other health condition would struggle to get policy attention and financial support if it was to forecast a 240 per cent increase in numbers?
Government to fully fund and implement the Plan.
Hall said that in the meantime, everyone can all do their bit to help create a more inclusive and accepting New Zealand.
“Some of the things we can do is have a conversation about dementia, learn more and back our call for the Plan.”
Talataina said increased education, such as resources in various Pacific languages to enhance and increase dementia awareness, can help break down some of the stigma associated with dementia.
As we move into an era where one in four New Zealanders are expected to experience some form of cognitive decline, the importance of education around dementia cannot be overstated.


TRACY MARTIN Chief Executive Aged Care Association
ementia affects not only those living with it but also their whanau, friends, and the dedicated staff who care for them. As the Chief Executive of the Aged Care Association, I believe it is essential that we deepen our understanding of this illness, both within our workforce and among the broader community, so we can provide the highest level of care and support to those affected. Dementia is a complex and often misunderstood condition, and for many families, it brings with it a sense of guilt, helplessness, and frustration – frustration that can manifest as misguided anger towards care facilities. I hear from families regularly about the emotional turmoil they face when placing a loved one in care. They question whether they’ve done the right thing, whether they

should have tried harder to manage at home, or whether the care facility will be able to provide the compassionate, individualised care their loved one deserves.
This guilt, while understandable, can be minimised with better education and awareness across the entire country. The more we can elevate understanding about dementia - its progression, its inevitable impact, and the role that expert care can play - the more we can ease the burden on whanau.
In New Zealand, 89 percent of care facility residents experience some form of cognitive decline. While this statistic may sound alarming, what’s important to note is that the majority of these residents are managed well within standard care facilities, without the need for secure units. This challenges the
outdated belief that all those with dementia are destined to be placed in locked-down, segregated environments.
What does this mean for the future of dementia care? It means we need to rethink our approach. Secure units certainly have a place for those residents with the most acute needs, but they are not the future for everyone living with dementia. Many people with cognitive decline can be better supported in a more integrated, holistic environment, where their care is individualised to their unique needs.
Our vision at the Aged Care Association is to elevate the training and resources available to our workforce, empowering them to manage the complexities of dementia with confidence. Education helps us ensure that our carers not only understand the clinical aspects of dementia but also how to interact with empathy, patience, and understanding. Dementia education needs to go beyond the physical tasks of care; it should encompass communication skills, emotional intelligence, and the ability to engage with residents in a way that honours their individuality and past experiences.
As alluded to earlier, it is vital we bring whanau into the fold of dementia education. Whanau need to be supported with accurate information about what dementia is, how it progresses, and how they can continue to be involved in their loved one’s life while navigating the emotional challenges it brings. It is equally important for whanau to understand the model of care at the facility their loved ones are in, as care models can vary between providers. This understanding helps align expectations, ensuring whanau feel confident in the care being provided, fostering smoother communication, and ultimately creating a partnership between whanau and care staff built on trust, communication, and shared understanding.
Our goal is not just to care for those with dementia but to transform the way we approach dementia care across New Zealand. By investing in education for whanau, the workforce, and the wider community, we can reinforce that those among us with cognitive decline are still “us” - part of our community, regardless of where their “home” inside community is.
The Maggie Beer Foundation has appointed Jane Mussared as CEO, to scale the Foundation and achieve its mission to raise the bar and change the food and dining experience in the aged care sector.

ane Mussared joins the Maggie Beer Foundation from an advisory role to Federal Health and Aged Care Minister, Mark Butler. She has spent the last three decades as a non-Executive Board Director (including previously on the Maggie Beer Foundation Board), Chief Executive, policy and political lead and senior executive and has garnered a wealth of knowledge, networks and skills in public and for purpose policy analysis and advocacy, leadership, strategy, communication and governance.
Mussared will spearhead the Foundation’s alliance of chefs, cooks, scientists, dietitians, philanthropists, corporations and organisations who have the ability and empathy to improve the quality of life of older Australians through tasty and nutritious food.
The Maggie Beer Foundation was established ten years ago and its ambition remains true; focused on addressing the quality of food and the dining experience for all older Australians via education and training of the cooks and chefs at the coalface of the industry. Philanthropic collaborative partnerships and fundraising will continue to be integral to the future growth of the organisation.
With Mussared at the helm, the Foundation can continue to evolve and scale its aged care chef and cook training programmes including
its online education modules, professional hands-on Trainer Mentor Chef Programmes, and involvement in research and policy development. Jane will also lead the Foundation’s involvement in the development of new training, careers and qualifications for the cooks and chefs in partnership with the aged care and vocational education sectors.
“From the recent TV series showcasing the crucial need for and role of the Foundation, and in celebrating its tenth year this year, the time is right to engage someone with Jane’s expertise who can scale the Maggie Beer Foundation to affect greater change in the food and dining experience within aged care,” said Maggie Beer Foundation Chair, Jon Clarke.
“We’re thrilled to have someone of Jane’s calibre who has such a deep passion and understanding of advocacy and the aged care sector, lead us into the future.”
Maggie Beer will continue an active role within the Foundation, focusing on where her passion lies - educating and mentoring chefs and cooks in the kitchen.
Jane Mussared is thrilled to be working with Maggie.
“For 10 years, Maggie Beer has been at the forefront of the Foundation and instrumental in every facet of the business. Maggie’s knowledge, expertise and passion will continue to lead, educate and inspire in a way only Maggie can, but I look forward to working with her as we grow the Foundation’s reach, influence and footprint,” said Mussared.
“There is much work to be done but the journey is so exciting,” said Beer.
“Food is nutrition not just for the body, but also for the soul. It’s what fires our appetite for life, no matter what age. Every mouthful counts as we age, and I’m delighted to have Jane at the helm, to help achieve our goal of making good food and good eating the reality for each and every older Australian.”





Entrepreneurs Sam Bridgewater and Maia Royal, the founders of The Pure Food Co, have won the EY Entrepreneur of the Year – Services category in New Zealand. The award-winning entrepreneurs are changing the way food is approached in the aged care sector to help solve one of society’s major problems: safe nutrition for the elderly.
e’re using food science and innovation to make nutrition commercially accessible to every resident in an aged care facility,” said Bridgewater.
“This is not just a healthcare issue but a social responsibility we can no longer afford to overlook.”
Bridgewater said that the risks of malnutrition, weight loss, and eating
challenges are reduced when aged care residents receive proper nourishment despite complex dietary needs.
“Older people require almost twice as much protein as elite athletes, yet most get as little as 60 percent of what they need,” he said.
“Meal times are among the most anticipated moments in a resident’s day, so we must get the food right.”
Jason Macgregor, director of EY Entrepreneur Of The Year, New Zealand, said he noticed an increased awareness of
social issues among the finalists.
“These phenomenal entrepreneurs have shown how they addressed a problem in society, found their niche, tackled hardship, and ultimately combined passion, purpose and profitability in their path to success.”
Bridgewater and Royal are using their pioneering work in the textured modified food space to solve critical issues related to elderly nutrition and have set new benchmarks for quality care.
The business the entrepreneurs started 11 years ago is now the largest supplier of textured-modified foods to age care facilities in Australia, New Zealand and France.
It's a solution to a growing issue in aged care that has been recognised, with the entrepreneurs winning the EY Entrepreneur of the Year - Services category.
According to Bridgewater, innovation in aged care isn’t just about developing new foods or menus; it’s about tailoring these innovations to help solve the real-world challenges that facilities, staff, and residents face.
“We’ve seen positive impacts on the mandatory aged care quality indicators such as improvements in unplanned weight loss, reduced falls and a reduction in pressure injuries through the increase in protein intake, which has led to a drop in supplement costs and work care complaints.”
The entrepreneur’s mission to nourish the world's seniors began after Bridgewater witnessed his step-dad’s battle with cancer, where he struggled to access the food he wanted and the nutrition he needed. The experience highlighted a critical gap in healthcare, inspiring him to explore how proper nutrition could improve health outcomes for seniors.
“It’s about changing the way aged care facilities approach food and nutrition, making it a key factor in improving long-term health outcomes, particularly for residents with dysphagia and other swallowing issues.”
“By reshaping pureed and textured modified fortified foods to look like regular meals, Bridgewater says they've overcome one of the key barriers in aged care nutrition, the reluctance of residents to eat when the meal looks unappetising or unrecognisable.
“We know that preparing flavoursome and aesthetically appealing and nutritionally fortified foods that comply with IDDSI textures is a challenge that's moved to a medical space.”
Bridgewater and Royal have successfully built partnerships with aged care networks and hospitals, offering training, implementation, and menu development support. This has been key to facilities meeting aged care guidelines, reducing costs, and easing the burden on their kitchen staff.
This is not just a healthcare issue but a social responsibility we can no longer afford to overlook.
“When we work with facilities, we see satisfaction outcomes go up, and plate waste goes down.”
Bridgewater said that by outsourcing one of the most complex and time-consuming aspects of food preparation, facilities meet IDDSI standards, reduce compliance risks and free up chefs and kitchen staff to focus on more personal aspects of the dining experience.
It’s a mission shared by Janet Anderson, Commissioner of the Aged Care Quality and Safety Commission, who echoed this sentiment in her most recent quarterly report, stating, “When you get the food right, many clinical risks are reduced, and a person’s quality of life is improved.”

The Australian Government and the Aged Care Quality and Safety Commission are continuing their mission to ensure that all older Australians in aged care receive nutritious, safe, and appetising food.

he commission's dedicated Food, Nutrition and Dining Unit Hotline gives older people, their families and carers, and aged care workers and providers an easy way to raise concerns, get advice or make a complaint about the food, nutrition and dining in aged care.
Established by the Australian Government, the unit has expert dietitians and speech pathologists to provide advice, education and resources.
The unit has undertaken 720 targeted assessments with residential services to ensure they provide residents with tasty, nutritious meals and an enjoyable dining experience.
Older people accessing aged care, their families, carers, providers, and workers can call the Food, Nutrition, and Dining Hotline. The hotline's work is just one way to reform aged
care and create a high-quality and accountable system that puts older people at the centre.
The Australian Government's $5 million investment in the Maggie Beer Foundation is improving workforce capability. Opportunities to participate are available for all cooks and chefs working in aged care homes.
These strengthened quality standards will include a dedicated food and nutrition standard to ensure aged care residents receive food and drinks that are appetising, safe, and meet their needs and preferences.
"We saw what a difference an improved food and dining experience can make in Maggie Beer's Big Mission," said Minister for Aged Care Anika Wells.
"Maggie Beer is an incredible advocate, and I am grateful for her passion and expertise in helping us deliver the dining experience older people in aged care need and deserve.
"But you don't need to be a celebrity chef to improve food and nutrition in aged care – we have the tools you need to continue our big mission," explained Minister Wells.
"Australians were shocked when the Royal Commission into Aged Care Quality and Safety found that 68 percent of aged care residents were malnourished or at risk of malnourishment.
"The Food, Nutrition and Dining Unit Hotline's work is another important tool in our mission to ensure older people have delicious and nourishing food that supports a high quality of life," she concluded.
"The Food, Nutrition and Dining Unit and Hotline can help if you have questions about the food, nutrition or dining experience that you or someone you know is receiving from an aged care provider," said Aged Care Quality and Safety Commissioner Janet Anderson, PSM.
"Aged care workers and providers can get advice and support from the Food, Nutrition and Dining Unit and Hotline to help them meet the needs and preferences of the people in their care."
"It is everyone's right to choose the foods and drinks they consume. In one example, staff at a service were supported by our Food Nutrition and Dining Unit and Hotline to help residents make informed choices about eating 'normal' food after they had been prescribed a soft food diet.
"With our help, the consumer was able to exercise their right to choose to eat and drink what they wanted, and the provider supported their choice while still providing quality, safe care," said Anderson.

Recent research conducted by JLL into the state of New Zealand’s aged care market has found that it is still dominated by the “Big Six” operators.
hile Bupa, Ryman, Arvida, Oceania, Metlifecare and Summerset collectively account for 46.7 percent of the market share, other operators collectively make up the remaining 54.3 percent. Despite a smaller number of villages, the Big Six are larger on average with 67 percent of the total aged care units across the country. Big Six village sizes average at 127 units, which is far bigger than the average of 54 units in non-Big Six villages.
Of the Big Six providers, there has been significant investment over the past year, including major investments in construction, innovation, development and staff.
Metlifecare has expanded its footprint, with recent opening such as The Anchorage at Pōhutukawa Landing in Auckland, with similar pipeline plans in place for other villages. The company has aimed for aged care units to be 20 percent of its portfolio by the end of the year, as currently, 25 out of its 36 villages offer care homes, with five more in the planning stages.
In 2023, Metlifecare provisioned 128 care suites across 11 of its villages, with additional plans to add 125 more units in the coming year. The company also received National Dementia Friendly accreditation in 2023.
Summerset acquired two new South Island land sites in Mosgiel and Rolleston for future developments. The company also trialled new technology platform, Lumin Technology, which will be expanded to more villages throughout the rest of 2024. In line with its strategic plans, Summerset has begun divesting its Parnell site, to rebalance its portfolio between metro and regional developments.
For Oceania, its reshaped portfolio saw the sale of two Auckland assets, and exiting four other sites. Although two of its rest homes were closed in Nelson, a new Northland site was purchased for future development. It’s latest flagship development, The Helier in Auckland, has introduced a new standard for luxury retirement villages upon its opening. The NZD $150 million project was targeted to high-end residential occupants, with more

developments planned for the site.
Ryman’s portfolio saw further growth for the company, despite putting certain developments on hold. These included in Ringwood East and Takapuna, with other sites listed for sale. However, the company has redirected its focus towards a new premium care suite project, expected to debut in Northwood by 2025.
Arvida has had a momentous year with various projects underway, including the construction of a resident clubhouse at Te Puna Waiora and reconfiguring apartments to meet demand sufficiently. Three of its villages were sold to New Aged Care, and land was acquired in Whitby for future retirement developments. Arvida’s next projects will aim to capitalise on the increasing demand from the Wellington and Manawatu-Whanganui regions.
Bupa has also sold off three of its villages to New Aged Care, but has expanded into new regions. The company acquired land in Porirua for a future facility, and has contributed largely to the growth of the Kapiti Coast and Wellington area, where there has been significant activity.
The report also indicated that non-Big Six developments, such as Generus Living Group and Winton Land, have also made significant strides throughout the luxury retirement sector. Generus’ The Foundation in Auckland and Holly Lea in Christchurch have been developed with high-end amenities. Winton’s Northbrook Wynyard Quarter will be Auckland’s first vertical retirement village, part of a NZD $750 million waterfront redevelopment project. These developments have also focused on premium living and catering to an affluent demographic.
Despite significant growth from aged care providers, there have been concerns about the rate of residents entering aged care. New Zealand’s elderly population, particularly those over 75, has continued to grow, albeit slower. Between 2018 and 2023, the population of this age group increased by 73,350, with projections it will grow by 68,910 between 2043 and 2048. This demographic shift has underscored the demand for more retirement and aged care units throughout the country.
JLL found that the development pipeline has reflected this growing need, with 10,174 units currently under construction out of 22,281 units in the planning stage. However, a shortage is expected in the long term, as projections have indicated that an additional 932 units will need to be built each year until 2048 to meet the anticipated demand.
By 2048, the industry would need more than 27,000 additional units to accommodate 112,624 people. Despite the Big Six leading in new development, its collective capacity may fall short unless the industry accelerates its growth.
The JLL report added that the Big Six continue to dominate New Zealand’s aged care market, with larger villages and increasing development plans. Still, the industry has challenges to meet the long-term demand for retirement and aged care facilities. Smaller operators and non-Big Six players have also contributed to this growth, particularly withiin the luxury retirement segment. With demand expected to rise, especially for care facilities, there is now a strategic opportunity for operators to scale up their offerings and address potential shortfalls in the market.

Arvida's Development team is making strides with the Bethlehem Shores Care Centre and Apartment project, aiming to secure two significant New Zealand building ratings. This ambitious development, overlooking Tauranga's inner harbour, will distinguish itself through design and sustainability.

urrently under construction, the new 14,000m² facility will include 53 independent living apartments and 55 care suites organised into six households.
The project complements the existing 273 architecturally designed villas at Bethlehem Shores. It will offer a range of amenities, including a café, lounge bar, whānau rooms, hair salon, flexi/craft room, kitchen and dining areas, and three landscaped courtyards.
The building's layout consists of five distinct wings, separated by wide, landscaped courtyards, providing privacy and ample natural light. The positioning maximises views to the north and east, overlooking the harbour and Mount Maunganui while offering vistas westward towards the river and
This state-ofthe-art care centre will offer a household model of care, providing rest home, hospital, and dementia care.
the Kaimai-Mamaku Forest Ranges.
Sustainability and durability are at the core of the design. The primary structure is made using Cross Laminated Timber (CLT), a lightweight yet strong material created by layering timber in alternating directions. This method speeds up construction and enhances the building's environmental credentials.
The project is on track to achieve Homestar Level 7 certification, ensuring a warm, dry, and healthy living environment, while also meeting Lifemark standards for adaptability, safety, and usability.
Once completed, Arvida will be one of New Zealand's first retirement village operators to secure both Homestar and Lifemark ratings for a single project. Justin Marshall, Arvida's Development Manager, noted the benefits of CLT in managing construction within an established community.
"Working on our largest single-stage project within a completed community is challenging, but CLT has enabled us to accelerate construction while reducing noise and disruption," he said.
"This state-of-the-art care centre will offer a household model of care, providing rest home, hospital, and dementia care."
The project is expected to be completed by the end of 2025.

Ryman Healthcare marked a major milestone this week, celebrating its 40th birthday with a series of events held across its villages in Australia and New Zealand. Residents, team members, and guests came together for a variety of activities, including an ‘80s-themed Happy Hour held at each village on 19 September, to honour four decades of kindness, care and community.
elebrating occasions such as this highlights Ryman's commitment to creating vibrant communities that enrich the lives of residents. In 1984, co-founders Kevin Hickman and John Ryder set out with a vision to transform retirement living. Inspired by the poor conditions he witnessed at a fire-damaged rest home, Kevin was motivated to enhance the
quality of life for older New Zealanders. This led them to convert a block of flats in Christchurch into their first rest home and name the company 'Ryman,' a blend of Ryder and Hickman.
Today, with 49 villages and over 14,000 residents across Australia and New Zealand, this vision continues to guide Ryman Healthcare. As the organisation has grown to become a major NZX-listed company, it
has remained true to its founding principle of ensuring that everything we do is 'good enough for Mum and Dad.'
As a pioneer in the retirement village industry, innovation has played a key role in Ryman’s evolution, leading to ongoing improvements in care, facilities, and resident experience. Our continuum of care model, which integrates retirement living and aged care into one community, has set a new industry standard. Meanwhile, the awardwinning myRyman app enhances residents' lives by providing easy access to village news, events, and personal scheduling, all tailored to be user-friendly for older adults.
Alongside building vibrant communities within its villages, Ryman partners with organisations that share its pioneering values and contribute to the wider community. It supports an annual charity partner, with past partners including the Fred Hollows Foundation and the Stroke Foundation, and offers scholarships to develop its people and support community initiatives. Additionally, the Ryman Prize, presented eight times by New Zealand prime ministers, was most recently awarded to renowned clinical neuroscientist Professor Vladimir Hachinski for his globally significant contributions to dementia prevention.
Ryman has been recognised many times for its commitment to quality and excellence. In 2024, it was voted New Zealand’s Most Trusted Brand in the aged care and retirement industry for the tenth time, and also won Canstar Blue’s award for Most Satisfied Customers in Retirement Villages in New Zealand. At the Asia Pacific Eldercare Innovation Awards, Ryman was named ‘Operator of the Year 2024 - Ageing in Place’ for the second consecutive year, and the myRyman resident app won the ‘Innovation of the Year 2024 - Technology Social Engagement’ award.
Dean Hamilton, Ryman Healthcare Executive Chair, said: “We are deeply grateful to our residents, team members, and the wider community for their support and dedication over the years. As we celebrate 40 years of success, our focus is firmly on the future. We are committed to meeting the evolving needs of the sector, including the growing ageing population, changing consumer expectations, and shifting market conditions. By continuing to innovate and adapt, we will ensure that Ryman remains at the forefront of retirement living, delivering exceptional experiences and care for our residents for years to come.”


Ron and Hilda Ball took a leap of faith with then smaller operator Ryman Healthcare, when they moved more than quarter of a century ago into Beckenham Courts Retirement Village.
renamed Essie Summers, after the renowned Christchurch-based romance writer. This was in line with a new tradition Ryman was establishing of naming its villages after great New Zealanders.
Ron and Hilda are now some of Ryman’s longest-residing residents in a single village, and have plenty of stories to share from their 27 years at Essie Summers. They still fondly recall moving into townhouse in 1997.
he change up – into village life – has certainly worked out for the very best, and the couple has enjoyed decades of kindness and care.
This month, Ryman celebrated its 40th birthday and Ron and Hilda remain two of the longest-residing residents in Ryman’s network of 48 villages across New Zealand and Australia.
The decision to move into the Beckenham Courts complex, now known as Essie Summers Village, came partly because Hilda faced significant health problems and it suited Ron who had just entered his retirement.
The pair thrived in the new setting, and their move in 1997 was more than a decade before the disruptive and damaging Canterbury earthquakes of 2010 and 2011, which resulted in a major rebuild of the village centre.
After the earthquakes, the village underwent a complete transformation and was
It was in that very townhouse that the February 22, 2011 earthquake shook things up. Widespread damage occurred throughout Christchurch, with brick garden walls collapsing and cracks appearing in the village walls and window frames.
Village Manager Rosemary Deane said she started in her role in November 2006 and the quake sequence that started four years later was a defining moment for her.
She was at the top of the South Island on holiday with family at the Totaranui Beach campground on February 22 when the quake struck.
“It was just by pure coincidence and serendipity really that our plumber was also at the grounds, so we jumped in his van and drove back the next morning,” she remembers.
For the next couple of years, the residents watched on as a village centre was reconstructed. Trucks and workers were constantly on the move, busy with a rebuild that included driving deep support piles into the ground to ensure the village would be stronger than ever.

Aileen Kars, New Zealand’s oldest person, recently celebrated her 111th birthday surrounded by family and friends.
he has been a resident of Arvida Olive Tree community in Highbury, Palmerston North, for 31 years. Robyn Ballard, the Village Manager, describes Aileen as a beloved figure within the community, both among residents and staff.
“Aileen has been with us since 1993. Over the years, she’s lived in a villa, an apartment, and now resides in the care centre. She has a wonderful, warm nature, and everyone loves visiting her,” said Robyn.
Aileen’s life has been one of hard work, joy, and resilience. Raised on a farm, she spent her younger years milking cows and shearing sheep. An accomplished ballroom dancer, Aileen balanced her passion for dance with the responsibilities of farm life alongside her late husband. Together, they raised their children in the Manawatu region, where family was always at the heart of their lives.
Aileen and her husband shared a marriage lasting 54 years. She is now the proud matriarch of a large family, including two children, three grandchildren, 12 greatgrandchildren, and seven great-greatgrandchildren.
Her family attributes Aileen’s remarkable longevity to her strong faith. When reflecting on her life in 2021, Aileen shared her simple but meaningful philosophy: “I’ve had a good life ... you need to have a good nature to live this long. I always got along well with others. My mother always said, ‘do unto others as you would have them do unto you.’ You get out what you put in.”

Subhashni Sharma has been a hairdresser with Ryman Healthcare for nearly seven years. Based in the Waikato region, she has worked at the group’s Hilda Ross village in Hamilton East and Linda Jones Village in Flagstaff.

harma believed that having a salon in any retirement village was very important, as it has been a place for residents to come, relax, and have a conversation as hairdressers and residents see each other on a regular basis. Residents enjoyed being able to beautify and pamper themselves.
In order to cater to the needs of residents, Sharma offers a range of services expected of a salon, including shampoo and roller sets or blowwaves, haircuts on a regular basis, and perms every three to four months.
Her salon has become more than just a place for hair care. It’s a hub of community action, where residents come together, share stories,



and form bonds. This sense of community is an integral part of the salon’s identity.
“I listen to the residents who tell me what their needs are so I can provide the services they require. Changing hairdressers can always be a challenge in the beginning,” said Sharma.
Sharma mainly uses moisture-based products, as, generally with age and medication, skin and hair can get dry and brittle. Generally for clients living with dementia, or who have major health issues, Sharma has assistance from staff, and provides services in their rooms. She said this was essential in order to include all residents.
“It’s very important to have a strong
relationship as well as patience , especially for residents living with dementia.”
To make the experience memorable, Sharma will often go out of her way to buy residents things that they might like to see or talk about.
“I also listen to their stories. Seeing them with that smile makes me a million times happier.”
For Kaylee Yaung, being a retirement village hairdresser has offered her the work-life balance that she desired.
Offering a wide range of services to seniors, from early glamour-era perms to modern hair trends, Yaung said every resident has their own individual style. Having a space that is
Continued on page 46.

easy for wheelchair access was an important requirement according to Yaung, as were windows that can open whilst doing chemical work such as perms.
Yaung’s salon is based at Ryman’s Murray Halberg Village in Auckland, a space she said was a relaxed, happy place.
“You’ve got to have kindness, patience, empathy and a caring nature to work with clients who have special needs. They should maintain good communication with their caregivers, families, and friends to arrange their appointments on their behalf since most are unable to do so themselves,” she said.
Yaung added that for many residents, visiting the hair salon has been a part of their routine for decades.
“It’s very important to build trust, and keeping consistency is key to maintaining the relationship, and keeping their confidence in you while they are in your chairs.”
Ciara Saleh of Ryman’s Miriam Corban
Village said it’s crucial that the salon is easy to access for individuals with mobility issues, and staff should be trained to handle agerelated concerns sensitively. A welcoming atmosphere and personalised service were also important for Saleh.
At her salon, Saleh has a variety of services, ranging from gentle haircuts, hair colourings
with less-harsh products, scalp massages, and styling that is easy to maintain. Additionally, Saleh’s services focus on hair health, such as treatments for thinning hair or scalp conditions.
To accommodate residents with mobility issues, the Miriam Corban hairdressing team ensure that the salon is wheelchair accessible and offer services directly in residents’ apartments if needed.
“Our staff are trained to provide patient, gentle care, especially for clients living with dementia or cognitive impairments, taking the time to explain what we are doing and reassuring them throughout the process,” said Saleh.
She said that trust and familiarity can make a big difference in the comfort level of residents, as it will allow them to feel relaxed during their visits.
“These bonds help us understand their individual preferences and needs better.”
Saleh also believed that celebrating special occasions like birthdays or anniversaries, offering complimentary refreshments, and creating a warm, friendly environment all contribute to making the experience memorable.
We focus on providing a personalised experience, remembering the little details about each client and their preferences.

As retirement villages have become dynamic hubs for residents, a standout addition has been the inclusion of hair salons.
alons can enhance the day-to-day life of residents, contribute their overall wellbeings and provide an essential service that all residents will require.
Hair salons can help with promoting self esteem and confidence within residents. A visit to the salon can be crucial in retirement villages, especially for residents that may struggle with changes in appearance and physical ability.
Salons, being conveniently located within the village, provide easy access to personal care, especially for residents with mobility or transportation issues. The stress of venturing outside the village is eliminated, ensuring that all residents have easy and convenient access to all hair care services.
Salons are not just about hair care, they are about fostering social interactions and combating feelings of loneliness and isolation. They provide a space for residents to relax, converse, and build a sense of community within the village.
A regular trip to the hair salon has become a way to informally check in on the wellbeing of residents. Creating a safe space for salon staff to report any concerns
over changes in resident behaviours or other health issues like skin conditions or scalp health can have a greater benefit on the health of residents.
Hair salons also encourage independence among residents, as they have to make decisions regarding their appearance, time, and regular self-upkeeping.
Integrating a hair salon into retirement homes is an integral way to assist residents with staying healthy, whilst offering them the best quality of service.

The controversial star rating system in the Australian aged care sector has come underfire by a raft of industry leaders.

r Rodney Jilek, Managing Director at Community Home Australia, has been vocal in his opposition to the star-rating system.
With over 30 years of experience and expertise in the sector,
Dr Jilek’s view of the so-called “once in a lifetime” reforms has been disappointing, and instead has delivered a system of smoke and mirrors that has failed to address the ongoing concerns highlighted by the Royal Commission, which has driven the aged care sector backwards.
The current institutionalisation of older Australians driven by public policy is in need of an urgent review in Jilek’s opinion, and should be inline with international best practices.
He said the largest problem was that the system failed to deliver what it promised, and
the data that informed the majority of the ratings has been provided by the operator and has lacked independent scrutiny.
According to Jilek, the current star rating system has merely reflected the lack of action by the regulator and was not directly impacted by services failing the minimum basic requirements of accreditation.
There has been a three month lag in data impacting the ratings, which meant no guarantee that the rating at a particular point in time will accurately reflect the performance of the sector.
Jilek said the system was touted by the Minister as a one-stop-shop to improve transparency and allow the general public to make an ‘apples-to-apples’ direct comparison between services.
“It was supposed to be a response to the findings of the Aged Care Royal Commission

that found that the current aged care system neglected older Australians and lacked transparency,” said Jilek.
He added that it was the perfect opportunity to drive improvement through objective review, but instead, it had become a process to manipulate public perception.
The reforms introduced by the Labor Government have largely muddied the waters according to Jilek. They have also obscured the true level of noncompliance by overinflating the perception of quality. The lack of regulatory action has allowed noncompliance to fester while simultaneously tricking the general public into thinking things had gotten better.
Jilek said the biggest threat of noncompliance to the industry was its level of standards.
“The aged care accreditation standards

DR RODNEY JILEK
Managing Director, Community Home Australia

represent the minimum acceptable standard of care and services.”
He added that practices that fail to meet the standards result in poor outcomes for residents and contribute to neglect, abuse, injury, illness and death.
In order to combat these threats, the sector will need to re-embrace a culture of innovation and best practice and move beyond a minimum standard for a better mentality. Excellence is something the current regulatory system does not encourage, and has driven mediocrity within the sector.
The Aged Care Commission recently clarified that star ratings would only come into effect if facilities had regulatory action taken against them. Former compliance staff said that this loophole has been used to alter the statistics.






Replaces a table’s existing screw-in feet
Stabilises tables with a press of the table top
Internal locks provide unrivalled stability
Enables the alignment of table tops
Independently tested by FIRA
Exceeds - international standards for Stability, Strength, Durability & Safety (BS EN 581-1:2006 & BS EN 581-3:2017)
Install in seconds. No tools required

Saves you time, money and frustration while improving your customers’ experience What makes a 5-star experience? It’s all the little things. From the moment your guest sets foot on the property, he or she begins evaluating every little detail.
Ph: 09 444 9078 I Email: sales@cooktech.co.nz Web: www.cooktech.co.nz
NO. 1 PPE STATIONS now locally available from our NZ Warehouse

Sterri-Matt® PPE Stations & Dispensers are the ultimate IPC solution with over a 100 versatile combinations to enhance your infection control programs

we also offer a wide range of Quad Glove Dispensers for added convenience & accessibility are also now available!