

Nourished Aging Toolkit:
Nutritional Approach to Wound Care


Message From Sysco’s Nutrition Services Team
Older adults, living within in long term care or retirement settings, can be at increased risk of experiencing skin breakdown and developing pressure ulcers. As a result, it can significantly impact an individual's overall health and quality of life.
This resource will provide education on nutritional interventions to help promote wound healing for residents within your communities. This toolkit will highlight the following:
• Importance of adequate energy and protein intake
• Increasing fluid intake to promote wound healing
• Vitamins and minerals to support wound healing
• Oral Nutritional Supplements (ONS)
Please reach out to your Sysco Account Representative for more information on Synergy Tech Suite and product listings.
Note: The information provided within this toolkit are suggestions and should be implemented in consultation with a Registered Dietitian and in accordance with your home specific policies. This toolkit is not intended to substitute clinical assessment by a healthcare professional to meet individual resident's clinical assessment needs, it is solely intended for education purposes only


Causes of Skin Breakdown
POOR NUTRITION
PRESSURE WOUNDS
HEALTH CONDITIONS
LACK OF MOBILITY
• Skin is the largest organ in our body, and it helps regulate our body temperature, excrete waste, and protect our organs1
• As we age, our skin loses elasticity and natural oils – resulting in dry and fragile skin that is at risk of breaking down1
• Skin tears and pressure wounds are common in seniors due to a combination of poor nutrition, inadequate hydration, medications, weight loss, immobility, incontinence, decreased level of consciousness, comorbidities, and poor circulation2,3


Stages of Pressure Injuries

Stage 1
• No visible breaks or tears on surface of skin4
• Reddened area4
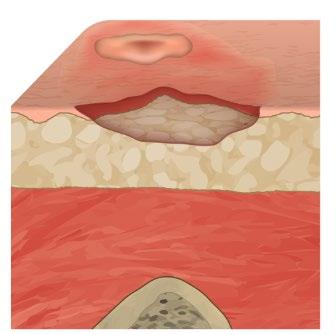
Stage 2
• Open area visible on skin4
• Tender and painful area4
• Affects deeper layers of skin4
• Appears as a blister or shallow crater4

Stage 3
• The sore continues to deteriorate and affect tissue beneath the skin4
• Fat may be visible4
• A small crater is present4
Other Categories of Pressure Wounds:
• Unstageable Pressure Injury: Stage is unclear as the base of the sore is covered by a layer of other tissue and pus4
• Deep Tissue Injury (DTI): Wound is unopened, but tissue beneath the surface is damaged4

Stage 4
• Pressure injury is deep and may damage deeper tissues, tendons, and joints4

Resident Wound Prevention Tips
Monitor for Physical Changes in your skin. As we age, our sense of touch and pressure declines. Be aware of reddened skin areas, blisters and open sores5.
Fall prevention. The risk of falling increases as we age. It can be due to aging, problems with the inner ear, medications, infections, poor blood circulation, etc5. Balance can be improved through exercise.

Eat balanced meals. It is important to eat balanced meals and stay hydrated5. Nutrient deficiencies can alter skin integrity and increase the risk of breakdown5
Take good care of your skin. As we age, our skin produces less oil and can feel dry and itchy5. Apply moisturizer regularly to keep skin moist5.
Prevent the development of pressure ulcers. Do not massage the area around the pressure wound as it can cause skin tears and break blood vessel5. Speak to a healthcare provider to get assessed for equipment that could help alleviate pressure5.
Get medical Treatment. Seek medical treatment if there is pain at the wound site, redness or swelling, foul odor, drainage from the wound, or other physical symptoms (i.e. fever, chills, etc.) 5 .
Managing Pressure Wounds
Managing pressure wounds requires an interdisciplinary approach. Nursing care and mobility are two important factors that can help promote wound healing.
Adequate nutrition is important for wound healing:
• Ensure adequate intake of calories, protein, vitamins, minerals, and fluids
• Conduct nutritional assessments using anthropometric, biochemical, clinical, dietary, and medical measures3
• Complete Nutrition Risk Screening Tool for residents who are at risk of pressure injury or malnutrition6

Adequate Calorie and Protein Intake
It is important to ensure residents are meeting their calorie and protein needs to promote wound healing.
• Calories provide energy to help promote the growth of new skin cells and remove old and damaged cells1
• Recommended energy intake for skin impairment is 30-35 kcal/kg2
• Suggestions to increase your calorie intake include grating cheese onto vegetables, using full-fat yogurt, milk, cheese, adding sliced avocado to sandwiches, adding olive oil to smoothies, pasta, or cooked vegetables7

Adequate or increased protein intake is important:
• Protein produces enzymes that react to form healthy layers of skin1
• Recommended protein requirement for skin impairment is 1.25-1.5 g/kg/day2
• Protein rich foods include animal protein (meat, poultry, egg, fish, seafood), milk products (milk, kefir, cheese, and yogurt), and plant protein (beans, peans lentils tofu, nuts, and seeds)8
• Suggestions to increase protein intake include cooking hot cereal in cow or soy milk, top fruit or cereal with Greek yogurt, add hard boiled eggs to salads or part of snacks, add skim milk powder to milk, or mix into mashed potatoes, soups, or puddings8
Increasing Fluid Intake
Fluid is important for maintaining skin integrity, regulating our body temperatures, and transporting materials in and out of our cells5.
Signs and symptoms of dehydration include changes in weight, poor skin turgor, low urine output, and elevated serum sodium levels6

Fluid Options:
• Gelatin desserts
• Soups
• Ice cream
• Popsicles
• Puddings
• Canned fruits
• Water, juices, beverages; fruits and vegetables provide ~95% water
• Supplements contain ~75% water6
•
• Equip
• Provide fluids between meals 9
• Offer additional fluids when taking meds or checking in with resident etc.)9
Vitamin C
• Supports collagen formation to help support wound healing5
Vitamins and Minerals
Research to support vitamin and mineral supplementation for wound healing is inconclusive.
Encourage micronutrient intake from food first wherever possible prior to using supplements6.
• Food sources: Citrus fruits and juices, tomatoes, potatoes, broccoli5
Zinc
• Supports collagen formation, protein metabolism, and immune function; promotes blood clotting5
• Food sources: Meats, liver, eggs, and seafood2
Copper
• Supports red blood cell formation and helps strengthen skin5
• Food Sources: Nuts, dried fruit, organ meats, dried beans, whole-grain cereal5


Iron
• Transports oxygen to the cells and creates energy from cells; participates in collagen formation6
• Food sources of iron that are well absorbed by the body include meats, poultry, and fish6
• Vegetables, grains, eggs, meat, and fish contain iron but is not easily absorbed by the body6
Vitamin A
• Involved in protein synthesis, collagen formation, and immune function; aids in maintenance of skin tissue6
• Additional supplementation may delay wound healing in older adults who are taking corticosteroids6
• Food Sources: Beef liver, milk, dark green and yellow vegetables (carrots, sweet potatoes, broccoli, spinach, apricots)6
Vitamin E
• Aids in fat metabolism, collagen synthesis, and cell membrane stabilization6
• Food Sources: Vegetable oils, sweet potatoes6
Supporting Intake Beyond Food
Create pleasurable dining experiences
• Encourage socialization during mealtime:
o Pair residents with close friends at their table
o Encourage team members to interact with residents during meal service
o Create a welcoming and relaxed dining environment:
o Create a calm ambience with warm lighting
o Play soft music in dining rooms or personal rooms
o Add a flare to table settings with coloured napkins and placemats and beautiful center pieces
o Reduce loud noises like dish scraping or kitchen noise
Ensure all meal components are accessible & within reach
• Assist with opening all packaging as needed including condiments, cutlery, and straws
• Assist with preparing items for consumption including
o Spreading margarine & jams on bread
o Preparing beverages like coffee and tea
o Cutting up proteins, vegetables, and bread
• Ensure cutlery, napkins, and beverages are within reach and where residents prefer




Oral Nutritional Supplements
Residents with severe wounds may have increased calorie, protein, and fluid needs of ~150%10,11. A "Food First" approach is ideal to promote wound healing, however, Oral Nutritional Supplements (ONS) may be required to augment residents’ food intake.
• The type and quantity of supplement must be individualized –staff should assess goals of care for residents who refuse nutritional support6
• Supplements can be purchased as a powder, beverage, pudding or ice creams.
• Supplements are often administered post-meal or during medication pass to ensure residents are not satiated prior to meal service
• Residents should be assessed individually to determine if the supplements are required



Oral Nutritional Supplement Selection
HIGH CALORIE LIQUID SUPPLEMENT
(1.5 or 2.0 kcal/mL)
Beneficial for residents who consume minimal fluids11
PUDDING SUPPLEMENT
Great option for residents who are on thickened fluids11
PROTEIN POWDER
Ideal for residents who require additional protein – it does not provide a significant number of calories (i.e., whey, soy, hemp, pea protein)8,11


HIGH PROTEIN SUPPLEMENT
(15 g of protein per 250 mL)
Provides a greater proportion of calories from protein11
SPECIALIZED SUPPLEMENT
Suitable for residents who have chronic conditions such as diabetes or renal disease11



https://www.osnac-fnat.com/ and Wounds Canada
https://www.woundscanada.ca/

