Mark C. Houston MD, MS, MSc, FAARM, ABAARM
James LaValle RPh. CCN, MT
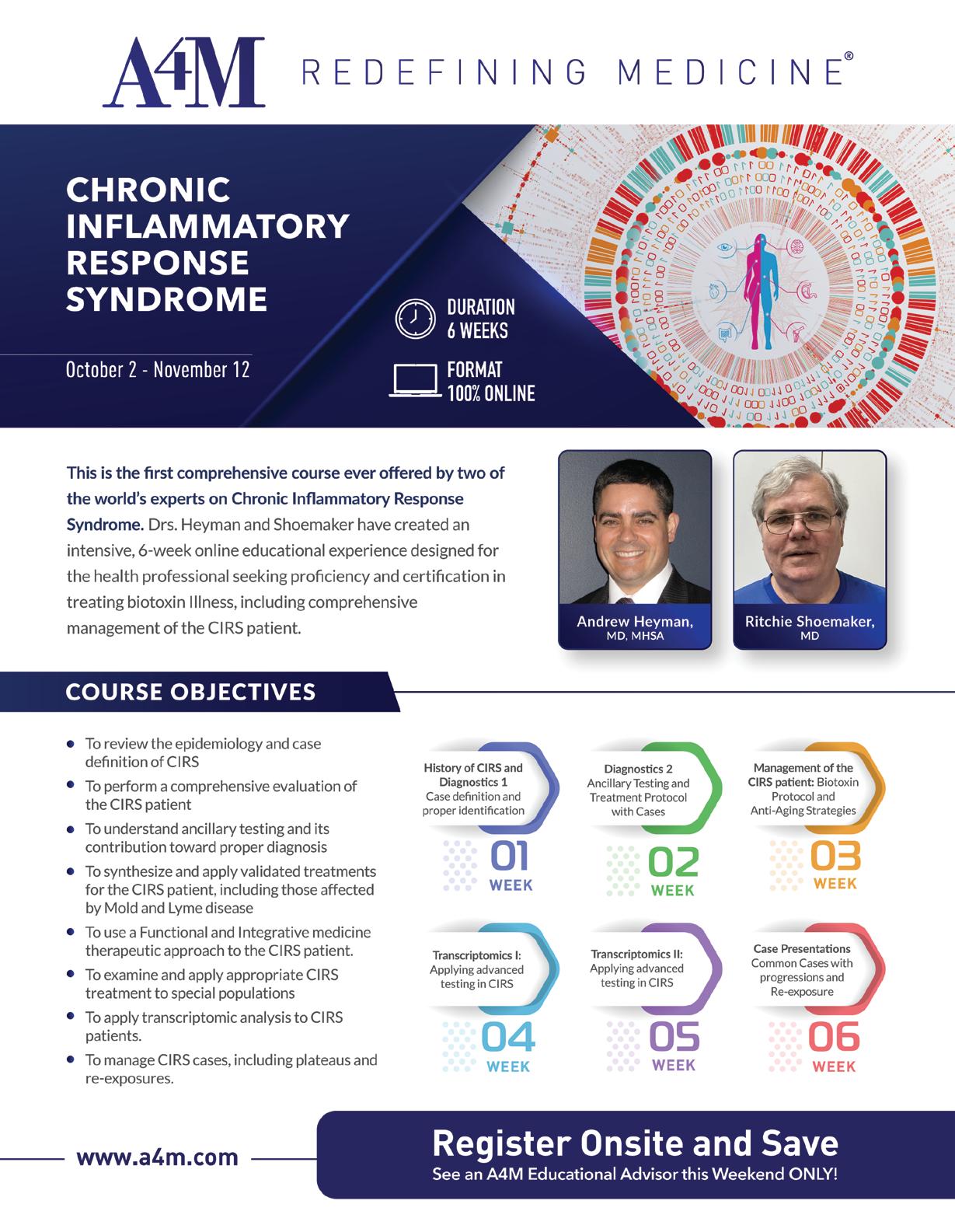
Mark Rosenberg MD, FAARM, ABAARM
Robert Goldman MD, PhD, DO, FAASP Co-Founder
Pamela W. Smith MD, MPH, MS
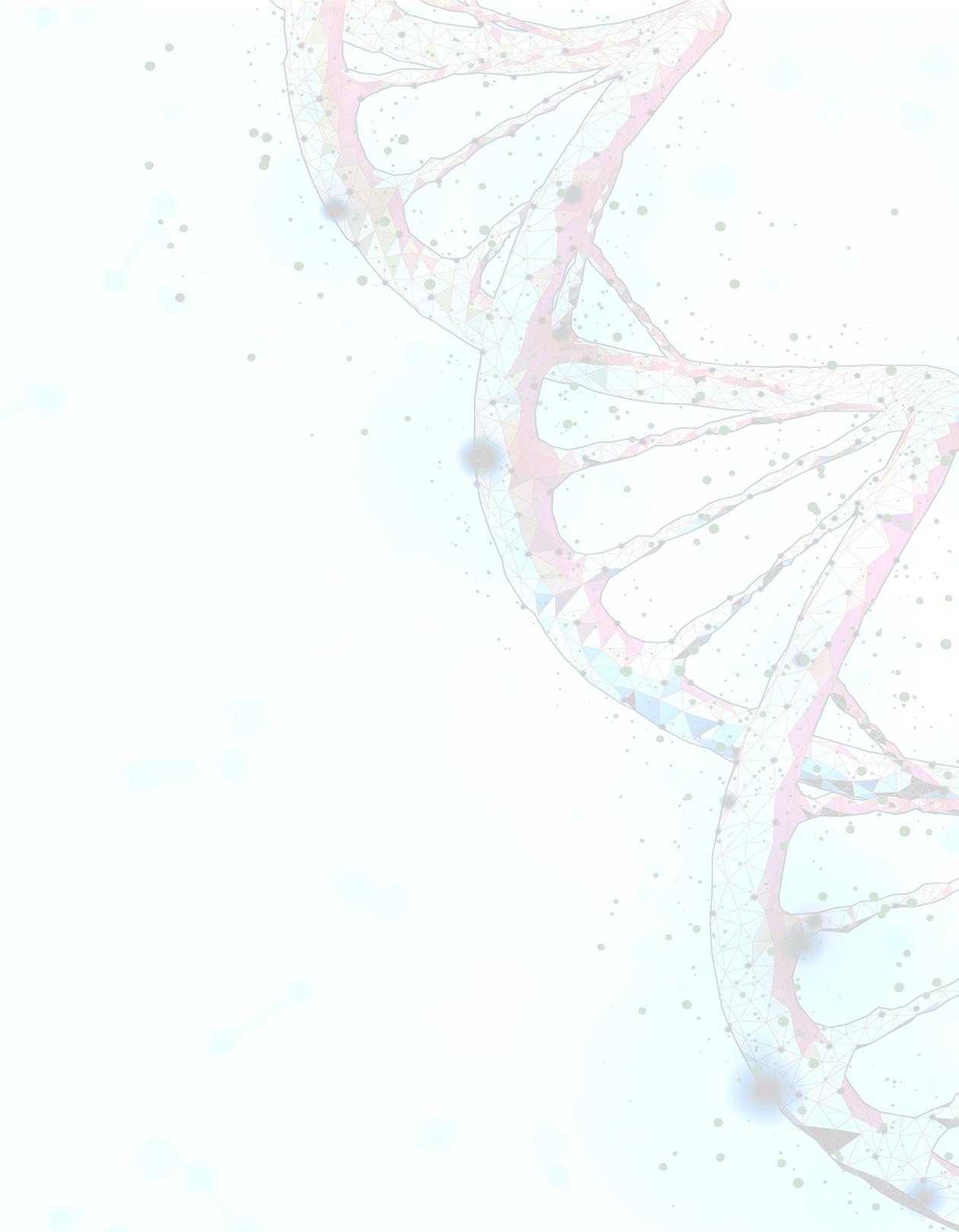
Andrew Heyman MD, MHSA, ABFM, ABIHM Director of Academic Affairs
Sahar Swidan PharmD, BCPS, ABAAHP, FAARFM Director of Professional Programming
Ronald Klatz MD, DO Co-Founder
Mark C. Houston MD, MS, MSc, FAARM, ABAARM
James LaValle RPh. CCN, MT
Mark Rosenberg MD, FAARM, ABAARM
Robert Goldman MD, PhD, DO, FAASP Co-Founder
Pamela W. Smith MD, MPH, MS
Andrew Heyman MD, MHSA, ABFM, ABIHM Director of Academic Affairs
Sahar Swidan PharmD, BCPS, ABAAHP, FAARFM Director of Professional Programming
Ronald Klatz MD, DO Co-Founder



FRIDAY |
SEPTEMBER 29TH
11:30 am - 12:30 pm
Using the DUTCH Test in Cycling Females: Fertility, Menstrual Dysfunction, and More
Presented by: Mark Newman, MS
12:00 pm - 1:00 pm
Sponsored by:
Hormone and Urinary Metabolites Assessment Profile (HuMap): A Comprehensive Overview
Presented by: Laura Neville, ND
12:00 pm - 1:00 pm
Sponsored by:
Master Personalized Anti-inflammatory Diets and Nutraceuticals Care Plans; Strategies for Implementing KBMO’s Advanced Assessments of Food Triggers and Gut Barrier Dysfunction

Presented by: Kristi Morlan-Hughes, ND, IFMCP, FMCHC
12:00 pm - 1:00 pm
Elevate Your Practice: Single Solution to Open a World of Possibility

Presented by: Jeff DeNeui, Executive Vice President
Sponsored by:
Everything you need to know about the laws, diagnosis , labs, treatments and follow up

Presented by: Andrew Jurow, MD, MS, FACOG, ABAARM
SATURDAY |
SEPTEMBER 30TH
12:00 pm - 1:00 pm
Sponsored by:
Presented by: Dan Powell
12:00 pm - 1:00 pm
Presented by: Christopher Wakely, ND
5:30 pm 6:15 pm
Sponsored by:
Sponsored by:
Presented by: Anne Marie Barrette, PhD, Arbella Sarkis, MD, William Gael, MD, John Bumb, CEO Metaverse One

The following article is not endorsed and/or supported by The American Academy of Anti-Aging Medicine.
The purposes of this publication do not imply endorsement and/or support of any author, company or theme related to this article.
Testicular cancer is the most common solid tumor among males 15 to 34 years of age, with an estimated 8,850 new cases and 410 deaths during 2017 in the United States. With e ective treatment, the overall ve-year survival rate is 97%.1 e signs and symptoms of testicular cancer include scrotal swelling, scrotal heaviness, painless, sold testicular mass, rmness of the testis, dull ache in the scrotum or abdomen, acute pain in the testis or scrotum.2 Epididymitis is an important part of the di erential diagnosis of a scrotal mass. If tenderness, swelling, or examination abnormalities persist after antibiotic treatment, further evaluation is necessary to rule out testicular cancer. 3
Risk factors for testicular cancer are numerous. 4
In patients with undescended testis (cryptorchidism), the relative risk of developing testicular cancer ranges from 2.9 to 6.3; the risk is increased in both testes, although the risk is much higher in the ipsilateral testis. 5-6 Among these patients, the risk of cancer increases when orchiopexy is delayed until after puberty or never performed compared with early orchiopexy.7-8 Even after early orchiopexy, the risk of testicular cancer remains elevated compared with the general population.9
Patients with a personal history of testicular cancer have a 12-times greater risk of developing a contralateral testicular cancer than the general population. However, the greatest risk is in the rst ve years after diagnosis, and the 15-year cumulative risk is 1.9%.10 In addition, patients with a father or brother with testicular cancer have a signi cantly great risk of developing the disease.11-13
Moreover, men with infertility have an increased risk of developing testicular cancer, with a standardized incidence ratio of 1.6 to 2.8, although the underlying mechanism is unclear.14-16 Human immunode ciency virus infection/AIDS increases the risk of seminoma, but this is negated with the antiretroviral treatment.17 Associations between testicular cancer and marijuana use, inguinal hernia, diet, maternal smoking, and body size are inconclusive. 1820 Testicular microlithiasis, and vasectomy are not risk factors for testicular cancer.21
Infections with human papillomavirus (HPV), Epstein-Barr virus (EBV), cytomegalovirus (CMV), parvovirus B-19, and human immunode ciency virus (HIV) increase the patient’s risk.22
In addition, trauma to the testicle is a risk factor.23-24 Furthermore, high maternal estrogen levels are a risk factor.25
If a solid intratesticular mass is discovered, orchiectomy is both diagnostic and therapeutic. Radical inguinal orchiectomy, including removal of the spermatic cord to the internal inguinal ring, is the primary treatment for any malignant tumor found on surgical exploration of a testicular mass. Testis-sparing surgery is generally not recommended but may be performed for a small tumor in one testis or for small bilateral tumors. Orchiectomy may be delayed if life-threatening metastases require more urgent attention.27-28 Treatment after orchiectomy is based on histology, staging, prognosis, and an individualized discussion with the patient on the bene ts and harms of treatment options.29 Adjunct therapies may include radiation and/or chemotherapy.
e high survival rate and young age of patients with testicular cancer result in long periods of survivorship with multiple sources of potential morbidity and mortality. Complications arise from both the disease process and treatment and vary according to individual course.
Secondary malignancy may be a concern in these patients. Testicular cancer survivors treated with radiotherapy or chemotherapy are at increased risk of secondary malignant neoplasms. ere is a threefold increased risk of leukemia among testicular cancer survivors treated with radiotherapy to the abdomen and pelvis. Cisplatin and etoposide therapies also increase the risk of secondary leukemia.30 Radiotherapy and chemotherapy increase the risk of solid cancers beginning ve years after treatment.31 Sites of secondary malignancy, in order of greatest to least risk, included stomach, pancreas, pleura, bladder, colon, and esophagus.32
Infertility and hypogonadism should be addressed with the patient. Cancer alone may a ect fertility. A systematic review found that up to 50% of patients with testicular cancer have semen abnormalities prior to orchiectomy.33 Orchiectomy and the e ects of chemotherapy and radiation also carry signi cant risks of future infertility. RPLND may induce retrograde ejaculation or anejaculation, although advances in surgical techniques have reduced this risk.34
Adjuvant therapy increases the short- and long-term risks of cardiovascular disease in testicular cancer survivors. A recent
population-based study of more than 15,000 testicular cancer survivors found a vefold increased risk of cardiovascular mortality within the rst year after chemotherapy compared with orchiectomy alone. is cardiovascular risk was not signi cant beyond the rst year.35 A retrospective study of testicular cancer survivors compared with age-matched control patients showed that radiotherapy or chemotherapy imposes greater than a twofold increased long-term risk (after 10 years posttreatment) for atherosclerotic disease; combined therapy increased the risk to almost vefold.36 Mediastinal irradiation, in particular, carries more risk than subphrenic irradiation.37 ere are no evidencebased recommendations for heart disease screening in testicular cancer survivors. Physicians and other health care providers should be aware of potential cardiovascular risk in cancer survivors with attention to standard risk factor screening and lifestyle interventions for primary cardiovascular disease prevention.
Anti-Aging Medicine therapies include all the conventional approaches discussed previously along with the following treatments.
If the patient smokes, work with the patient on smoking cessation therapies.
Stress from any cause is known to modulate the immune response and can partially suppress certain aspects of immune function.38 In addition, prolonged psychological stress appears to be correlated with cellular aging, inducing characteristic senescence features such as increased oxidative stress, reduced telomere length, chronic exposure to glucocorticoids, decreased thymus, changes in cell tra cking, decreased cell-mediated immune response, steroid resistance, and chronic low-grade in ammation.39-41 In fact, immunosenescence (alteration of immune function due to aging) has been widely reported in older individuals, as a result of the chronic antigen stimulation and cellular stress encountered throughout life. 42 However, other factors are also associated with the acquisition of precocious senescent features in immune cells, including tissue damage, oxidative stress, cytotoxic therapies, DNA damage, chronic in ammation, and chronic psychological stress.43 Furthermore, both biological and psychological stress experienced during cancer therapy may be responsible for stimulating molecular processes that induce premature aging and
deterioration of immune system in testicular cancer survivors, leading to an increased susceptibility to infections, cancer, and autoimmune diseases.44-45
e increasing evidence described above, that some cancer treatments may induce cellular senescence and aging of the immune system, may have implications on the development of secondary medical conditions later in life.46 Testicular cancer survivors have an increased risk to su er of late adverse events, including hypogonadism, infertility, metabolic syndromes, neurotoxicity, lower cognitive functions, reduced renal function, heart disease, and secondary cancers.47 Hypogonadism also increases the risk of developing metabolic syndrome, including cardiovascular complications and diabetes, which appears to be greater after combination therapy (chemo-radiotherapy).48-49 In addition, testicular cancer survivors struggle with high rates of anxiety and PTSD.50-52
One study hypothesized a correlation between low testosterone levels and increased secretion of pro-in ammatory cytokines in the genesis and maintenance of chronic diseases.53 Lower the in ammatory component in the body with EPA/DHA, curcumin, and low-dose naltrexone.
e results of increasing studies indicate that LDN exerts its immunoregulatory activity by binding to opioid receptors in or on immune cells and tumor cells. ese new discoveries indicate that LDN may become a promising immunomodulatory agent in the therapy for cancer and many immune-related diseases.54 It has also been reported that LDN is able to reduce tumor growth by interfering with cell signaling as well as by modifying the immune system. is data supports further the idea that LDN possesses anticancer activity, which may be improved by modifying the conventional treatment schedule.55
A recent study is the rst to investigate the e ect of testosterone substitution in testicular cancer survivors with mild Leydig cell insu ciency.56 Consider HCG or clomiphene citrate to raise testosterone levels in younger men if levels are low. Consider testosterone replacement in males that are in andropause that have a history of testicular cancer. A study revealed that all three treatments were equally e ective in restoring testosterone levels.57
Conclusion
As you have seen there are both conventional and Anti-Aging Medicine treatments that are successful for testicular cancer. Also
References
1. Baird, D., et al., “Testicular Cancer: Diagnosis and Treatment,” Amer Fam Physician 2018; 97(4):261-68.
2. Shaw, J., et al., “Diagnosis and treatment of testicular cancer,” Amer Fam Physician 2008; 77(4):470.
3. McConaghy, J., et al., “Epididymitis: an overview,” Amer Fam Physician 2016; 94(9):723–26.
4. Ibid., Shaw.
5. Lip, S., et al., “A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life,” Arch Dis Child 2013; 98(1):20–6.
6. Akre, O., et al., “Risk of contralateral testicular cancer among men with unilaterally undescended testis: a meta analysis,” Int Jour Cancer 2009; 124(3):687–89.
7. Walsh, T., et al., “Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer,” Jour Urol 2007; 178(4 pt 1):1440–46.
8. Chan, E., et al., “FRCSC for Canadian Association of Pediatric Surgeon Evidence-Based Resource. Ideal timing of orchiopexy: a systematic review,” Pediatr Surg 2014; 30(1):87–97.
9. Pettersson, A., et al., “Age at surgery for undescended testis and risk of testicular cancer,” NEJM 2007; 356(18):1835–41.
10. Fossa, S., et al., “Risk of contralateral testicular cancer,” Jour Nat; Cancer Inst 2005; 97(14):1056–66.
11. Hemminki, K., et al., “Familial risk in testicular cancer as a clue to a heritable and environmental aetiology,” Brit Jour Cancer 2004; 90(9):1765–70.
12. Del Risco Kollerud, R., et al., “Family history of cancer and risk of paediatric and young adult’s testicular cancer: A Norwegian cohort study,” Brit Jour Cancer 2019; 120(10):1007-14.
13. Hemminki, K., et al., “Familial risks in testicular cancer as aetiological clues,” Int Jour Androl 2006; 29(1):205-10.
14. Jacobsen, R., et al., “Risk of testicular cancer in men with abnormal semen characteristics: cohort study,” BMJ 2000; 321(7264):789–92.
15. Walsh, T., et al., “Increased risk of testicular germ cell cancer among infertile men,” Arch Intern Med 2009; 169(4):351–56.
16. Eisenberg, M., et al., “Increased risk of cancer in infertile men,” Jour Urol 2015; 193(5):1596–1601.
17. Goedert, J., et al., “Risk of germ cell tumors among men with HIV/acquired immunodeficiency syndrome,” Cancer Epidemiol Biomarkers Prev 2007; 16(6):1266–69.
18. Gurney, J., et al., “Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis,” BMC Cancer 2015; 15:897.
19. Manecksha, R., et al., “Epidemiology of testicular cancer,” BJU Int 2009; 104(9 part B):1329–33.
20. Lerro, C., et al., “A systematic review and meta-analysis of the relationship between body size and testicular cancer,” Brit Jour Cancer 2010; 103(9):1467–74.
21. Ibid., Hemminki.
22. Garolla, A., et al., “Role of viral infections in testicular cancer etiology: Evidence from a systematic review and meta-analysis,” Front Endocrinol (Lausanne) 2019; 10:355.
23. Coupland, C., et al., “Risk factors for testicular germ cell tumours by histological tumour type. United Kingdom Testicular Cancer Study Group,” Brit Jour Cancer 1999; 80(11):1859-63.
24. Haughey, B., et al., “The epidemiology of testicular cancer in upstate New York,” Amer Jour Epidemiol 1989; 130(1):25-36.
25. Depue, R., et al., “Estrogen exposure during gestation and risk of testicular cancer,” Jour Natl Cancer Inst 1983; 71(6):1151-55.
26. Gaddam, S., et al., Testicle Cancer, StatPearls (Internet). Nov. 7, 2021.
27. European Association of Urology. Guidelines. Testicular cancer. 2015. https:// uroweb.org/guideline/testicular-cancer. Accessed September 30, 2020.
28. American Cancer Society. Can testicular cancer be found early? http://www. cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-detection Accessed December 4, 2021.
29. Albers, P., et al., “European Association of Urology. Guidelines on testicular cancer: 2015 update,” Eur Urol 2015; 68(6):1054–68.
30. Fung, C., et al., “Long-term morbidity of testicular cancer treatment,” Urol Clin North Amer 2015; 42(3):393–408.
considering possible risk factors for other diseases that need to be mitigated as the patient ages are paramount along with therapies to improve their lifestyle.
31. Ibid., Fung.
32. Travis, L., et al., “Second cancers among 40,576 testicular cancer patients: focus on long-term survivors,” Jour Nat Cancer Inst 2005; 97(18):1354–65.
33. Djaladat, H., et al., “The association between testis cancer and semen abnormalities before orchiectomy: a systematic review,” Jour Adolesc Young Adults Oncol 2014; 3(4):153–59.
34. Ostrowski, K., et al., “Infertility with testicular cancer,” Urol Clin North Amer 2015; 42(3):409–20.
35. Fung, C., et al., “cardiovascular disease mortality after chemotherapy or surgery for testicular nonseminoma: a population-based study,” Jour Clin Oncol 2015; 33(28):3105–15.
36. Haugnes, H., et al., “Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study,” Jour Clin Oncol 2010; 28(30):4649–57.
37. van den Belt-Dusebout, A., et al., “Long-term risk of cardiovascular disease in 5-year survivors of testicular cancer,” Jour Clin Oncol 2006; 24(3):467–75.
38. Glaser, R., et al., “Stress-induced immune dysfunction: Implications for health,” Nat Rev Immunol 2005; 3:243–51.
39. Bauer, M., “Chronic stress and immunosenescence: a review,” Neuroimmunomodulation 2008; 15:241-50.
40. Reed, R., “Stress and immunological aging,” Curr Opin Behav Sci 2019; 28:38–43.
41. Epel, E., “Psychological and metabolic stress: a recipe for accelerated cellular aging?” Hormones 2009; 8(1):7–22.
42. DePadova, S., et al., “Immunosenescence in testicular cancer survivors: Potential implications of cancer therapies and psychological distress,” Front Oncol 2020; 10:564346.
43. Smith, P., Max Your Immunity. Garden City Park, NY: Square One Publishers, 2021.
44. Ibid., DePadova.
45. Bauer, M., et al., “ The role of stress factors during aging of the immune system,” Ann NY Acad Sci 2009; 1153:139–52.
46. Cupit-Link, M., et al., “Biology of premature ageing in survivors of cancer,” ESMO Open 2017; 2:e000250.
47. Lubberts, S., et al., “Early ageing after cytotoxic treatment for testicular cancer and cellular senescence: Time to act,” Crit Rev Oncol Hematol 2020; 151:102963.
48. Haugnes, H., et al., “Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study,” Jour Clin Oncol 2010; 28:4649–57.
49. La Vignera, S., et al., “Hypogonadism and sexual dysfunction in testicular tumor survivors: A systematic review,” Front Endocrinol Lausanne 2019; 10:264.
50. Smith, A., et al., “ The prevalence, severity, and correlates of psychological distress and impaired health-related quality of life following treatment for testicular cancer: a survivorship study,” Jour Cancer Surviv 2016; 10(2):223–33.
51. Kreiberg, M., et al., “Psychological stress in long-term testicular cancer survivors: a Danish nationwide cohort study,” Jour Cancer Surv 2020; 14(1):72–9.
52. Dahl, A., et al., “Aspects of posttraumatic stress disorder in long-term testicular cancer survivors: cross-sectional and longitudinal findings,” Jour Cancer Surviv 2016; 410(5):842–9.
53. Maggio, M., et al., “Correlation between testosterone and the inflammatory marker soluble interleukin-6 receptor in older men,” Jour Clin Endocrinol Metabol 2006; 91(1):345-47.
54. Li, Z., et al., “Low-dose naltrexone (LCN): A promising treatment in immunerelated diseases and cancer therapy,” Int Immunopharmacol 2018; 61: 178-84.
55. Liu, W., et al., “Naltrexone at low doses upregulates a unique gene expression not seen with normal doses: Implications for its use in cancer therapy,” Int Jour Oncol 2016; 4992):793-802.
56. Bandak, M., et al., “A randomized double-blind study of testosterone replacement therapy or placebo in testicular cancer survivors with mild Leydig cell insufficiency (Einstein-intervention),” BMC Cancer 2017; 17:461.
57. Habous, M., et al., “Clomiphene citrate and human chorionic gonadotropin are both effective in restoring testosterone in hypogonadism: a short course randomized study,” BJU Int 2018; 122(5):889-97.
Conclusion
As you have seen there are both conventional and Anti-Aging Medicine treatments that are successful for testicular cancer. Also
References
1. Baird, D., et al., “Testicular Cancer: Diagnosis and Treatment,” Amer Fam Physician 2018; 97(4):261-68.
2. Shaw, J., et al., “Diagnosis and treatment of testicular cancer,” Amer Fam Physician 2008; 77(4):470.
3. McConaghy, J., et al., “Epididymitis: an overview,” Amer Fam Physician 2016; 94(9):723–26.
4. Ibid., Shaw.
5. Lip, S., et al., “A meta-analysis of the risk of boys with isolated cryptorchidism developing testicular cancer in later life,” Arch Dis Child 2013; 98(1):20–6.
6. Akre, O., et al., “Risk of contralateral testicular cancer among men with unilaterally undescended testis: a meta analysis,” Int Jour Cancer 2009; 124(3):687–89.
7. Walsh, T., et al., “Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer,” Jour Urol 2007; 178(4 pt 1):1440–46.
8. Chan, E., et al., “FRCSC for Canadian Association of Pediatric Surgeon Evidence-Based Resource. Ideal timing of orchiopexy: a systematic review,” Pediatr Surg 2014; 30(1):87–97.
9. Pettersson, A., et al., “Age at surgery for undescended testis and risk of testicular cancer,” NEJM 2007; 356(18):1835–41.
10. Fossa, S., et al., “Risk of contralateral testicular cancer,” Jour Nat; Cancer Inst 2005; 97(14):1056–66.
11. Hemminki, K., et al., “Familial risk in testicular cancer as a clue to a heritable and environmental aetiology,” Brit Jour Cancer 2004; 90(9):1765–70.
12. Del Risco Kollerud, R., et al., “Family history of cancer and risk of paediatric and young adult’s testicular cancer: A Norwegian cohort study,” Brit Jour Cancer 2019; 120(10):1007-14.
13. Hemminki, K., et al., “Familial risks in testicular cancer as aetiological clues,” Int Jour Androl 2006; 29(1):205-10.
14. Jacobsen, R., et al., “Risk of testicular cancer in men with abnormal semen characteristics: cohort study,” BMJ 2000; 321(7264):789–92.
15. Walsh, T., et al., “Increased risk of testicular germ cell cancer among infertile men,” Arch Intern Med 2009; 169(4):351–56.
16. Eisenberg, M., et al., “Increased risk of cancer in infertile men,” Jour Urol 2015; 193(5):1596–1601.
17. Goedert, J., et al., “Risk of germ cell tumors among men with HIV/acquired immunodeficiency syndrome,” Cancer Epidemiol Biomarkers Prev 2007; 16(6):1266–69.
18. Gurney, J., et al., “Cannabis exposure and risk of testicular cancer: a systematic review and meta-analysis,” BMC Cancer 2015; 15:897.
19. Manecksha, R., et al., “Epidemiology of testicular cancer,” BJU Int 2009; 104(9 part B):1329–33.
20. Lerro, C., et al., “A systematic review and meta-analysis of the relationship between body size and testicular cancer,” Brit Jour Cancer 2010; 103(9):1467–74.
21. Ibid., Hemminki.
22. Garolla, A., et al., “Role of viral infections in testicular cancer etiology: Evidence from a systematic review and meta-analysis,” Front Endocrinol (Lausanne) 2019; 10:355.
23. Coupland, C., et al., “Risk factors for testicular germ cell tumours by histological tumour type. United Kingdom Testicular Cancer Study Group,” Brit Jour Cancer 1999; 80(11):1859-63.
24. Haughey, B., et al., “The epidemiology of testicular cancer in upstate New York,” Amer Jour Epidemiol 1989; 130(1):25-36.
25. Depue, R., et al., “Estrogen exposure during gestation and risk of testicular cancer,” Jour Natl Cancer Inst 1983; 71(6):1151-55.
26. Gaddam, S., et al., Testicle Cancer, StatPearls (Internet). Nov. 7, 2021.
27. European Association of Urology. Guidelines. Testicular cancer. 2015. https:// uroweb.org/guideline/testicular-cancer. Accessed September 30, 2020.
28. American Cancer Society. Can testicular cancer be found early? http://www. cancer.org/cancer/testicularcancer/detailedguide/testicular-cancer-detection
Accessed December 4, 2021.
29. Albers, P., et al., “European Association of Urology. Guidelines on testicular cancer: 2015 update,” Eur Urol 2015; 68(6):1054–68.
30. Fung, C., et al., “Long-term morbidity of testicular cancer treatment,” Urol Clin North Amer 2015; 42(3):393–408.
considering possible risk factors for other diseases that need to be mitigated as the patient ages are paramount along with therapies to improve their lifestyle.
31. Ibid., Fung.
32. Travis, L., et al., “Second cancers among 40,576 testicular cancer patients: focus on long-term survivors,” Jour Nat Cancer Inst 2005; 97(18):1354–65.
33. Djaladat, H., et al., “The association between testis cancer and semen abnormalities before orchiectomy: a systematic review,” Jour Adolesc Young Adults Oncol 2014; 3(4):153–59.
34. Ostrowski, K., et al., “Infertility with testicular cancer,” Urol Clin North Amer 2015; 42(3):409–20.
35. Fung, C., et al., “cardiovascular disease mortality after chemotherapy or surgery for testicular nonseminoma: a population-based study,” Jour Clin Oncol 2015; 33(28):3105–15.
36. Haugnes, H., et al., “Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study,” Jour Clin Oncol 2010; 28(30):4649–57.
37. van den Belt-Dusebout, A., et al., “Long-term risk of cardiovascular disease in 5-year survivors of testicular cancer,” Jour Clin Oncol 2006; 24(3):467–75.
38. Glaser, R., et al., “Stress-induced immune dysfunction: Implications for health,” Nat Rev Immunol 2005; 3:243–51.
39. Bauer, M., “Chronic stress and immunosenescence: a review,” Neuroimmunomodulation 2008; 15:241-50.
40. Reed, R., “Stress and immunological aging,” Curr Opin Behav Sci 2019; 28:38–43.
41. Epel, E., “Psychological and metabolic stress: a recipe for accelerated cellular aging?” Hormones 2009; 8(1):7–22.
42. DePadova, S., et al., “Immunosenescence in testicular cancer survivors: Potential implications of cancer therapies and psychological distress,” Front Oncol 2020; 10:564346.
43. Smith, P., Max Your Immunity. Garden City Park, NY: Square One Publishers, 2021.
44. Ibid., DePadova.
45. Bauer, M., et al., “ The role of stress factors during aging of the immune system,” Ann NY Acad Sci 2009; 1153:139–52.
46. Cupit-Link, M., et al., “Biology of premature ageing in survivors of cancer,” ESMO Open 2017; 2:e000250.
47. Lubberts, S., et al., “Early ageing after cytotoxic treatment for testicular cancer and cellular senescence: Time to act,” Crit Rev Oncol Hematol 2020; 151:102963.
48. Haugnes, H., et al., “Cardiovascular risk factors and morbidity in long-term survivors of testicular cancer: a 20-year follow-up study,” Jour Clin Oncol 2010; 28:4649–57.
49. La Vignera, S., et al., “Hypogonadism and sexual dysfunction in testicular tumor survivors: A systematic review,” Front Endocrinol Lausanne 2019; 10:264.
50. Smith, A., et al., “ The prevalence, severity, and correlates of psychological distress and impaired health-related quality of life following treatment for testicular cancer: a survivorship study,” Jour Cancer Surviv 2016; 10(2):223–33.
51. Kreiberg, M., et al., “Psychological stress in long-term testicular cancer survivors: a Danish nationwide cohort study,” Jour Cancer Surv 2020; 14(1):72–9.
52. Dahl, A., et al., “Aspects of posttraumatic stress disorder in long-term testicular cancer survivors: cross-sectional and longitudinal findings,” Jour Cancer Surviv 2016; 410(5):842–9.
53. Maggio, M., et al., “Correlation between testosterone and the inflammatory marker soluble interleukin-6 receptor in older men,” Jour Clin Endocrinol Metabol 2006; 91(1):345-47.
54. Li, Z., et al., “Low-dose naltrexone (LCN): A promising treatment in immunerelated diseases and cancer therapy,” Int Immunopharmacol 2018; 61: 178-84.
55. Liu, W., et al., “Naltrexone at low doses upregulates a unique gene expression not seen with normal doses: Implications for its use in cancer therapy,” Int Jour Oncol 2016; 4992):793-802.
56. Bandak, M., et al., “A randomized double-blind study of testosterone replacement therapy or placebo in testicular cancer survivors with mild Leydig cell insufficiency (Einstein-intervention),” BMC Cancer 2017; 17:461.
57. Habous, M., et al., “Clomiphene citrate and human chorionic gonadotropin are both effective in restoring testosterone in hypogonadism: a short course randomized study,” BJU Int 2018; 122(5):889-97.


1. Salvador L, Singaravelu G, Harley CB, Flom P, Suram A, Raffaele JM. A Natural Product Telomerase Activator Lengthens Telomeres in Humans: A Randomized, Double Blind, and Placebo Controlled Study. Rejuvenation Research. December 2016. 16(5).
2. Fernandez ML, Thomas MS, Lemos BS, DiMarco DM, Missimer A, Melough M, Chun OK, Murillo AG, Alyousef HM, Medina-Vera I. TA-65, A Telomerase Activator improves Cardiovascular Markers in Patients with Metabolic Syndrome. Current Pharmaceutical Design. 2018;24,1-7.
3. Singaravelu G, Harley CB, Raffaele JM, Sudhakaran P, Suram A. Double-Blind, Placebo-Controlled, Randomized Clinical Trial Demonstrates Telomerase Activator TA-65 Decreases Immunosenescent CD8+CD28-T Cells in Humans. OBM Geriatrics. 2021 vol. 5, issue 2.
4. Bawamia B, Spray L, Wangsaputra VK, Bennaceur K, Vahabi S, Stellos K, Kharatikoopaei E, Ogundimu E, Gale CP, Keavney B, Maier R, Hancock H, Richardson G, Austin D, Spyridopoulos I. Activation of telomerase by TA-65 enhances immunity and reduces inflammation post myocardial infarction. Geroscience. 2023 Apr 22:1–17.


The following article is not endorsed and/or supported by The American Academy of Anti-Aging Medicine.
The purposes of this publication do not imply endorsement and/or support of any author, company or theme related to this article.
Introduction
e importance of the hypothalamic-pituitary-adrenal axis (HPA) in mediating the stress response and maintaining physiologic homeostasis has long been described. It is well established that chronic stress propagates a systemic cascade of dysfunctional metabolic events initially intended to be adaptive. Dysfunction of the HPA axis appears to be a major initiating and contributing factor to this process, ultimately giving rise to disruption of the normal diurnal cortisol release pattern.
Maladaptive cortisol release patterns can be characterized as hypercortisol, which is an overly exaggerated response to stress, or hypocortisol, which is an underproduction of cortisol under stressful circumstances. While the latter has been often characterized as ‘Adrenal Fatigue,’ this notion does not fully appreciate the complex, multi-step process that results in low cortisol states, or the body of literature that characterizes hypocortisolism as an adaptive response to stress.
is paper reviews the components of the stress response, mechanisms of alterations in cortisol production, and common botanical therapies utilized in mitigating the stress response and protecting the health of the individual.
Physiologic stress is a “state of disharmony or threatened homeostasis” that occurs in the central nervous system (CNS) and surrounding tissues and organs.1 It triggers an intricate series of metabolic responses collectively called the “adaptive stress response” that is intrinsically designed to help the body reestablish equilibrium to counteract a perceived extrinsic or intrinsic “stressor.”1-4
Lifestyle behaviors along with stress duration, intensity, and frequency can add to dysregulation of the stress system and result in a myriad of health problems and ultimately, disease, thus a ecting an individual’s ongoing resiliency or “successful adaption to change.”1-6 e brain’s ability, in particular, to resist the e ects of a stressor plays a central role in determining the integrity of the stress response itself, and whether it remains intact or develops abnormal patterns of reaction over time.1,2,5
e ability to achieve stability through change or “Allostasis” within the stress response is reliant upon a system of healthy interactions across the neuroendocrine, cellular, and molecular components of the stress system, including the hypothalamic-
pituitary-adrenal (HPA) axis and the autonomic nervous system (ANS), central nervous system (CNS) and periphery, in addition to the cardiopulmonary, endocrine, immune and gastrointestinal tract.1-4 When these systems remain resilient and produce a positively coordinated reaction to stress, resiliency and metabolic reserve is maintained and the health of the individual protected.
Allostatic Load: Overwhelming the Stress Response
Chronic activation of the stress system contributes to the “Allostatic load” as coined by McEwen and Stellar, which re ects the total strain on the stress response.1 Contributors to allostatic load include major life events, trauma, abuse, work, home, community, as well as day-to-day lifestyle behaviors including su cient rest, diet, nutrition, exercise, toxins, and substance abuse.1-8
If allostatic load overwhelms the body’s ability to compensate, thus degrading allostasis, a number of emotional and physiological manifestations can arise including: 1-9
Mood Depression, Anxiety and Sleep Disorders; Altered perception, behavior and social interactions
Cognition
Endocrine
Memory loss, word finding difficulties, decreased executive function
Obesity, Insulin resistance, Diabetes, decreased leptin, increased grehlin,
Cardiovascular
Abnormal heart rate, hypertension, hyperlipidemia, elevated fibrinogen, myocardial infarction, stroke
Immune
Poor immune defense, Increased pro-inflammatory cytokines, cancers, auto-immune diseases, Atopic illnesses
Neurologic
Headaches, decreased heart rate variability (HRV), increased SNS activity (12hour urinary norepinephrine and epinephrine)
Reproductive Infertility, hormone imbalances
Gastrointestinal
GERD, peptic ulcers, Irritable Bowel Syndrome, Ulcerative Colitis
Skin Rashes, hives, atopic dermatitis
McEwen categorizes these into primary, secondary and tertiary markers of allostatic load. Primary mediators that have a direct response from stress and predictive validity in the context of longitudinal behavioral assessments include cortisol, adrenaline, sympathetic and parasympathetic activity, proand anti-in ammatory cytokines, metabolic hormones and neurotransmitters and neuromodulators.10
Secondary markers are indirect measures of immune system e cacy and a result of the aggregate impact of primary mediators including WHR, BP, cholesterol/HDL ratio, HDL cholesterol, glycosylated hemoglobin, in ammatory markers mentioned above (IL-6, C-reactive protein, and brinogen), and telomere length and telomerase activity.1-10
Individuals who experience early life adversity are likely to experience higher levels of oxidative and in ammatory stress (primary mediators) resulting in telomere shortening (secondary outcome) or obesity (secondary outcome), and are at increased risk for depression, diabetes, CVD or substance abuse.1-10
Tertiary mediators or outcomes such as CVD, decreased physical activity, severe cognitive decline, Alzheimer’s disease, vascular dementia, or cancer are the diseases or disorders that result from the extreme values of secondary outcomes due to increased allostatic load.10
e stress response begins in the paraventricular nucleus (PVN) of the hypothalamus, the anterior lobe of the pituitary gland, and the adrenal gland, otherwise known as the hypothalamic-pituitaryadrenal (HPA) axis.1-9 Neurons in the medial parvocelluar subdivision of the PVN synthesize and secrete corticotropinreleasing factor (CRF), the principle regulator of the HPA axis and automonic nervous system (learning, memory, feeding, reproduction), and vasopressin (AVP).9
In response to stress, CRF is released and binds to the CRF type 1 receptor (CRFR1) on pituitary corticotropes which activate the cyclic adenosine monophosphate (cAMP) pathway and release of adrenocoriticotrophic hormone (ACTH) into systemic circulation.1,3,4,9 Circulating ACTH binds to the melanocortin type 2 receptors (MC2-R) in the adreno-cortical zona fasciculata, causing steroidogenesis and glucocorticoid, mineralocorticoid (MR), and androgenic steroid synthesis and secretion.1,3,4,9
Stress-receptive neurons in the brain stem,relay sensory information
from cranial nerves to the PVN that excite large areas of thoracic and abdominal viscera.9 Projections from the prefrontal cortex and amygdala limbic structures regulate the behavioral responses to stress by releasing catecholamines.9 e anterior cingulate and prelimbic cortex increase ACTH and glucocorticoid responses to stress.1,2,9
Medial (MeA) nuclei of the amygdala are activated following exposure to “emotional” stressors while central (CeA) nuclei are activated by “physiological” stressors and regulate the HPA axis through intermediary brain stem neurons.1,9,10 e amygdala is a target for circulating glucocorticoids and the CeA and MeA express both GR and mineralocorticoid receptors (MR). In contrast to the e ects on hippocampal and cortical neurons, glucocorticoids increase expression of CRF in the CeA and potentiate autonomic responses to chronic stress.1-10
Activation of brain stem noradrenergic neurons and sympathetic and renomedullary circuits further contribute to the body’s response to stressful stimuli including emotion, vigilance, memory, and resiliency.1,3,9,10 Stressful stimuli alter neuronal electrophysiological activity and induce release of norepinephrine, ACTH release, anxiogenic-like activity, and immune suppresion.1-10
e extra-CNS metabolic response to acute stress includes rapid and strong elevation of plasma concentrations of glucose, insulin, glycerol, and ketone bodies, stimulation of adipose tissue lipase by circulating catecholamines, activation of the autonomic nervous system via glucagon secretion, and decrease in triacylglycerol levels.1,4,9
Several neuropeptide systems in the brain are substantially a ected by stress including norepinephrine, epinephrine, serotonin, dopamine, glutamate, taurine, GABA, glycine, phenylethylamine (PEA),and histamine.1-10 Ongoing disruption of neurotransmission can potentially lead to neuropsychiatric symptom manifestation and acceleration of neurotransmitter depletion, with the mesoprefrontal pathway being particularly at-risk, thus impacting reward-mediating neurotransmitters possibly leading to addictive behaviors.1,9,10
Activation of cerebral cholinergic transmission impacts arousal, motivation, and cognition.1,4,9,10Extracellular levels of glutamate, the major excitatory amino acid transmitter, increases in numerous regions of the brain, while changes in GABA receptor properties can also impact the stress response.4,9,10
However, several aspects of GABA-ergic neurotransmission may be obscured by endogenous steroid hormone derivatives whose synthesis is increased following stress.4,9,10 ese compounds in uence several aspects of the behavioral and neuroendocrine response to stress.9-10 Alterations in the endogenous opioid neurotransmission are implicated in stress-related endocrine and autonomic responses.9,10
Stress can induce changes in CRH and AVP expression in the PVN, and increased concentrations of ACTH in the systemic circulation, result in desensitization of pituitary CRH receptors and blunted ACTH release.1-10 is dissociation between CRH hyperactivity and refractory corticotrophin responsiveness is a pathognomonic feature of stress-associated neuroendocrine dysregulation.10
Beyond this, stress drastically a ects growth hormone secretion, thyroid axis function, and reproductive function via decreased gonadotropin levels, suppressed gonadal steroids, increased circulating prolactin, disruption of the ovarian cycle, and decreased libido.1-10
While elevated cortisol patterns are well recognized and understood, the process through which hypocortisolism evolves remains ill de ned. Although reduced availability of cortisol may be due to primary dysfunction of the adrenal glands, controversially labeled as “adrenal fatigue”, reductions in biosynthesis of hormones at di erent levels of the HPA axis likely play a greater role.
Since integrity of HPA axis function and predictable patterns of diurnal cortisol release are essential for maintaining homeostasis during periods of chronic stress, much of the available research on hypocortisolism and stress induced disease has focused on disturbances in these latter mechanisms.
Hellhammer and Wade postulated a developmental model whereby hypocortisolism may develop via hypoactivity of the HPA axis after prolonged periods of chronic stress. After an initial period of HPA axis hyperactivity and hypercortisolism, hypocortisolism may ultimately develop as a type of maladaptive “over compensation” of the self preservation mechanisms designed to protect metabolic machinery, and particular the brain, from the deleterious e ects of persistent cortisol elevation.112
An increase in hypothalamic release of CRF with subsequent adaptive down-regulation of CRF receptors at the level of the pituitary gland has also been proposed. Although this has been demonstrated
in animal studies, replication of such a process in human subjects has been di cult but may be indirectly implied. Yehuda et al. and others have postulated that an increase in the sensitivity of the HPA axis to hypercortisolism induces negative feedback control on further release of stimulating hormones thereby causing hypocortisolism.213
McEwen identi es a central mechanism for low cortisol states via alterations in the CA1 and CA3 regions of the hippocampus. Known as the ‘Neurodegenerative Model of Hypocortisolism,’ in which the hippocampus plays a central role in the regulating the entirety of the stress response. While a primary purpose of this critical brain structure is to consolidate memories, and assign importance to those memories, it also maintains the highest concentration of cortisol receptors in the brain.314
e hippocampus is therefore exquisitely vulnerable to high stress states, with cortisol potentially playing a catabolic or damaging role that can lead to alterations in both function and structure of this brain center. It should be noted that the hippocampus serves a regulatory role to the HPA axis, and once injured, can lead to low cortisol states. e neuroin ammation and neurodegeneration associated with the damaging e ects of cortisol in the brain argues for therapeutic strategies that limit injury of cortisol to key brain areas, reduce in ammation and induce neurogenesis.
Intrinsic dysfunction of the adrenal gland has also been proposed as well, but overall limited data exists in comparison to other mechanisms that lead to hypocortisolism. Heim and colleagues have reviewed studies on the e ects of chronic stress on the adrenal glands and have concluded, “ ere is a considerable body of evidence of reduced adrenal gland activity and reactivity in human subjects living under conditions of chronic stress.”415
Scott and colleagues found patients with CFS and abnormal endocrine parameters to have a signi cant reduction in adrenal gland volume compared to control subjects.516 Another study by Cleare et al. found CFS patients to have impaired adrenal cortical function as evidenced by not only decreased basal cortisol levels but also blunted cortisol responses to stimulation testing.617
Regardless of the underlying process, some believe the maladaptive physiological changes induced by hypocortisolism may actually be protective to ensure survival. As postulated by Fries et al, “Hypocortisolism is a protective response dampening chronic HPA axis activity and thereby reducing the damaging e ects of the glucocorticoid response to daily hassles at the expense of symptoms such as high stress sensitivity, pain, and fatigue”.18
In further support of this theory, Fries and colleagues have observed comparable groups of pregnant women and found those with lower morning cortisol levels had higher daily stress compared to their counterparts experiencing normal or low daily stress loads. e authors speculate that the hypocortisolism may be a counterregulatory protective mechanism designed to protect placental CRF from maternal cortisol.718
Raison and Miller suggest that hypocortisolism enhanced stimulation of the immune system may be protective as well. In individuals su ering from recurrent or ongoing infectious assaults, reduced glucocorticoid signaling impairs the normally adaptive inhibitory mechanisms thereby promoting the body’s ability to mount adequate retaliatory defenses. Other authors have coined the term “sickness response” to describe the anorexia, fatigue, anhedonia, hyperesthesia, and concentration di culties often accompanying the body’s response to infection via elevated immune activity.819
In his 1988 paper, Hart wrote that the sickness response results from the body’s adaptive attempts to ration and prioritize its defenses to better eliminate the pathogen.920 Many symptoms of the sickness response mimic those of stress related bodily disorders, and an association between hypocortisolism induced FMS and the sickness response has been observed. e notion that hypocortisolism is actually protective is intriguing.
Hypocortisolism, has been linked to bromyalgia (FMS), posttraumatic stress disorder (PTSD), irritable bowel syndrome (IBS), low back pain (LBP), burn-out, atypical depression, chronic pelvic pain (CPP), chronic fatigue syndrome (CFS), insomnia, and degenerative neurological diseases.2-7 Damaging e ects on the immune system occur due to increased levels of pro-in ammatory cytokines and natural killer cells (NK) and T-lymphocytes which lower resistance to in ammatory and infectious disease.1-7
Breast cancer patients demonstrate signi cant post-treatment exhaustion and have been shown to have signi cantly altered HPA axis activity in combination with elevated IL-6 levels, attened cortisol curves, increased mortality, and metastases. Furthermore, the more attened the cortisol curve the worse the prognosis and the earlier the mortality.
Additional studies have found elevations in interleukin-1 , natural killer cells, antinuclear autoantibodies, thyroid antibodies, and prostaglandins in patients with PTSD, in patients with intrusive traumatic memories, in sexually abused girls, and in patients with CFS, FMS, and chronic pelvic pain respectively.
e hypocortisol state also permissively allows an increase in sympathetic nervous system and catecholamine activity since normal cortisol-mediated suppression is lacking. Increased levels of catecholamines have been observed in patients with both PTSD and FMS.
Furthermore, exaggerations in sympathetic tone, in conjunction with underlying hypocortisolism, further fuels the production of pro-in ammatory cytokines. Associations between insulin resistance, obesity, diabetes, osteoporosis, mood disorders, and chronic pain have been described in patients with elevated levels of cytokines, particularly interleukin-6.
Alterations in rhythmicity of cortisol release have been associated with various negative outcomes, including tumor growth, early mortality in cancer, obesity and disrupted glucose metabolism. Increased coronary artery calci cation and metabolic syndrome have also been linked to circadian abnormalities in cortisol, particularly attened cortisol curves.
Emerging metabolic measures of stress or “biomarkers” assist in evaluating the complex multi-system brain-body biological interactions that occur and predict the risk of disease and response to proposed interventions that can impact mental and thereby physical wellness for a lifetime.10
One of the key features of the HPA axis is its circadian rhythm that results in a predictable diurnal cortisol secretion pattern, whereby cortisol levels are naturally highest just before awakening, and decline over the course of the day.2
e preferred method for measuring the stress response is a singleday, four-point cortisol test, with the most important measurements being the rst morning cortisol or cortisol awakening response (CAR) measured 30-40 minutes after awakening, and last sample prior to bedtime.2
Clinicians may ask patients to refrain from exercise on day of testing to avoid mis-diagnosis of hypercortisolism or diurnal dysrhythmia.2 CAR is used signi cantly more than the overall diurnal salivary cortisol to de ne stress-induced HPA axis abnormality as a mini “stress test”as it is in uenced by overall HPA reactivity and a person’s anticipation of stress.2 A blunted cortisol response upon wakening is a sign of burnout or chronic fatigue, while higher CAR is can be indicative of depression.2 Testing should be done on a “normal” day of anticipated stress, but if an abnormal stressor is encountered, they
can rinse out the collection tubes and repeat the test on a “normal” day.2
Additionally, common abnormal diurnal patterns include persistently elevated cortisol throughout the day, ‘hypercortisolism,’ and conversely abnormally low cortisol, or ‘hypocortisolism.’ Each has been associated with a variety of symptomatic and clinical states, but hypocortisolism is thought to represent a more ‘injured’ stress response and higher risk for morbidity and mortality overall, likely due to releasing of the immune response yielding higher baseline levels of in ammation.
‘Adaptogens’ are a diverse group of herbs that restore overall balance and functioning of the body as a whole through
Astragaluls (Astragalus membranaceus)
Ashwagandha (Indian ginseng, Poison gooseberry, Winter cherry)
Bacopa (Bacopa
stimulating, relaxing, helping to improve focus or immune function, or normalizing unbalanced physiological processes. ey have been shown to clinically reduce self-reported stress, improve mood and energy, and strengthen the immune system.
ey are often particularly helpful in stress-related conditions due to their shielding e ects on the brain, immune and cardiopulmonary systems. Some, such as ginseng, ashwagandha, and rhodiola, are speci cally neuroprotective by blunting the impact of cortisol within the CNS by reducing neuroin ammation and even encouraging repair..
Cordyceps (Cordyceps sinensis)
Enhances mental and physical performance, learning ability, stress, fatigue, resistance to cancer and diabetes, immune function, chemoprotective, increase oxygen to tissues
Strengthen immunity to colds and infections, improve physical and athletic ability, increase vitality, male fertility and libido, regulate blood sugar, antioxidant, antibiotic, anti-in ammatory, rejuvenating, astringent, anti-anxiety, anti-tumor, diuretic, insomnia, reduce cholesterol, arthritis, tuberculosis, asthma, leukoderma, bronchitis, backache, bromyalgia,menstrual problems, hiccups, chronic liver disease, balances cortisol, supports HPA axis, boosts thyroid hormones
Cognitive function, concentration, fatigue, antioxidant, anxiety, epilepsy
Strongest anti-cancer mushroom with an epochal e ect in breast, liver, uterine and gastric cancer, hypertension, diabetes, tuberculosis (TB) of the bones, strengthen immune system, antiin ammatory, anti-ulcer, anti-tumor, DNA Repair, anti-mutagenic
Immunosuppresive, anti-aging, antioxidant, decreases proin ammatory monoamine oxidase and lipid peroxidation activity, liver and lung protection (increase oxygenation), asthma, bronchitis, chemoprotective, anti-cancer, chronic renal failure, atherosclerosis, antiarrhythmic e ects
Invigorate qi (chi or energy) or endurance, strengthen immune system, memory, chemoprotective, DNA repair, antiin ammatory, normalize body function, particularly kidney, spleen and heart meridians, radiological protection, anticholesterolemic, anti-oxidant, angina, headache, insomnia, poor appetite, stress, fatigue, HPA-axis dysfunction
250-500mg, 3-4 times daily of a standardized extract (at least 0.4% 4’-hydroxy-3’methoxyiso avone 7-sug.); 3 weeks on, 2 weeks o cycle
400-900 mg daily of a standardized extract (at least 2.5% withanolides); 3 weeks on, 2 weeks o cycle
50-100g, 1-4 times a day of a standardized extract (20% bacosides A&B)
1050mg, 2-3 times per day of a standardized extract (0.14% adenosine and 5% mannitol)
Glycyrrhiza Glabra (Licorice)
Adrenal stress, expectorant, phytoestrogen e ects, food sweetener, reduces cholesterol manufacturing, antiviral
250-500mg, 3 times daily standardized to contain 20% glycyrrhizinic acid or 15-30 drops of liquid extract, 3 times daily in juice or beverage
Holy basil (Tulsi, Ocimum tenui orum or Ocimum sanctum)
Enhance body’s natural response to physical and emotional stress, reduce bloating and gas, antioxidant, support healthy adrenal function, cortisol release and immunity, radiation protection, lipid balance, blood sugar regulation, anti-in ammatory (COX-2 inhibitor), cancer prevention, slow age-related memory impairment, lower cholesterol
400-800mg daily of a standardized extract (1.0 - 2.5% ursolic acid; supercritical extracts 7-11% eugenol & 4% caryophyllene; hydroethanolic extracts 0.7-4.0% triterpenoic acids, ursolic and oleanolic acids; steam distilled extracts 40% eugenol & 15% caryophyllene
L-theanine
Mastic (Pistacia lentiscus)
Mucuna pruriens (Cowhage, Velvet bean)
Muira puama (Ptychopetalum olacoides)
Panax ginseng
Phenyl-GABA
Found in green tea, induces relaxation through increased dopamine and serotonin, and improves sleep quality
Adrenal stress, expectorant, food sweetener, H.pylori infections, oral health/cancer, phytoestrogen e ects,
Lower stress as a source of L-DOPA the precursor for dopamine, neuroprotective, Parkinson’s disease, antioxidant, blood sugar, weight loss, metabolic syndrome, male infertility
Neuroprotective, stress, libido, depression, mood
Mood, cognition, immunity, antifatigue, protection against mental, physical and environmental stress
Phosphatidylserine (PS) Decrease symptoms of mild depression in mood disorders
Relora Plus
Rosa Majalis
Reishi or Lingzhi (Ganoderma lucidum)
Proprietary blend of plant extracts from Magnolia o cianalis, Phellodendron amurense, and B-vitamins that normalizes cortisol levels, stress-related eating, decreases weight gain, and anxiety
Anti-cancer, anti-oxidant, source for Vitamins A,C,E
Adaptogen (mental, physical performance, learning, decrease stress and fatigue), blood pressure stabilizer, antioxidant, analgesic, kidney and nerve tonic, strengthen immune system, anti-in ammatory, anti-viral, anti-tumor, anti-parisitic, liver protectant, blood glucose regulation, chemoprotective
Rhaponticum Strength or endurance or reduce fatigue, impotence or aphrodisiac
100 mg-200mg, 1-3 times daily
Oleoresin: 500mg, 2-4 times daily
100-200 mg of a standardized extract (20-95% L-Dopa) once daily in the morning, 30 minutes before breakfast
500mg up to 3 times daily
200mg BID
250mg, 3 times daily
150-300mg, 3-4 times daily of standardized extract (4% triterpenes and 10% polysaccharides (β-1, 3-glucans))
Valerian (Valeriana
Adaptogen, strength or endurance, reduce fatigue, mental and physical performance, decrease recovery time, antioxidant, learning, adrenal stress, depression, improve immunity, sleep patterns, mood stability, and motivation, resistance to cancer, type 2 diabetes, cardio-protective
Antioxidant, infection-resistant, increase skin health, liver protectant, stress/fatigue, enhance mental and physical performance, learning, adaptogen, improve resistance to cancer and diabetes, improve immune function, chemoprotective
Enhances mental and physical performance, increases learning ability, and decreases stress and fatigue, may improve resistance to cancer and diabetes, immune function, antiviral, chemoprotective
150-300mg, 1-3 times daily, standardized (3-5% rosavins and less than 1% salidrosides)
100-200mg, twice daily with food standardized (9% schisandrans), taken 3 weeks on, 2 weeks o
100-400mg 3 times daily of a standardized extract
Stress and cortisol balance, energy/fatigue, weight loss, erectile dysfunction, testosterone balance, infertility, athletic performance, antioxidant, anti-in ammatory
200-400mg daily of a standardized water extract of the root (50:1 to 200:1 water extraction; 200:1 standardized to 1% eurycomanone, 22% protein, 30% polysaccharides, 35% glycosaponins; LJ100 = 100:1 water extraction; contains 40% glycosaponins and 22% eurypeptides)
Insomnia, anxiety, sedation, stress/sleep disorders
Nervines are a class of botanicals that reduce sympathetic overdrive, anxiety, and irritability by sedating the autonomic nervous system
200-500mg of standardized extract (0.4-1% valerenic acids), or 30-60 drops of liquid extract (1:4 w/v) in water 1-2 hours before bedtime or as needed
and inducing a sense of calm or relaxation. ey can be used during the day to blunt a hyperaroused state, or in the evening for sleep induction.
Antidepressant, anxiolytic, nervous system tonic & trophorestorative, nutritional, hypolipidemic (as food), cardiotonic, demulcent, emollient, vulnerary, antispasmodic
Infusion: 1 heaped Tbsp (approx. 3 g) to 1 cup Water; steep until at room temperature. Drink throughout the day. Tincture: (1:5, 25%), 1-5 ml TID.
Bath: Add 1 heaping cup to bath water, enjoy!
Bacopa monniera (Brahmi)
Cognition & memory enhancer, nerve and brain tonic, mild anti-convulsant, antioxidant, antiin ammatory, cardiotonic, vasocontrictor, bitter, emetic, laxative & diuretic (leaf), aphrodisiac
Powdered herb: 5-10g, QD. Extract: 300mg, QD.
Capsule: 3000mg BID.
Skin rub: skin mixed with oil applied prn. Tincture: (1:2, 25%), 5-13ml QD
Verbena o cinalis (Blue vervain)
Leaf: Diuretic, demulcent, emollient, refrigerant, adrenal restorative, galactagogue, expectorant. Oil: in ammatory modulating, anti-atheroslcerotic, anti-platelet, hypolipidemic, atopic dermatitis, dysmenorrhea, PMS, cyclic mastalgia, hypertension and diabetic neuropathy.
Strengthens nervous system, function, memory, relaxant, detoxifer, diuretic, topical antibiotic, peripheral vasodilator, anti-rheumatic, vulnerary, venotonic, keratolytic, anti-mycobacerial, bitter, digestive, antiin ammatory, laxative, dermatological builder, connective tissue builder, cellulite, cirrhosis of the liver, keloids and hypertrophic scars, leprosy, scleroderma, varicose veins and venous insu ciency, and wound repair.
2 tsp dried herb/cup; 1 cup BID. Tincture: (1:5, 60%), 1-10 ml BID. Juice pulp from fresh leaves, 10 ml BID. Seed oil: 500 mg capsule: 1-4 capsules daily.
Tincture: (1:2, 45%), 3-6ml QD. Dried leaves: 0.6g TID. Infusion: 1 tbsp/cup, infuse 10 min, TID. Poultice. Extract: standardized to contain asiaticoside (40%), 60-120mg QD.
Infusion: 2-4 g / cup QD to TID
Tincture (1:5, 40%), 1-4 ml TID
Anti-depressant, anti-in ammatory, antimicrobial, astringent, nervine tonic, topical wound healing (burns)
Standardized extract: 500 to 1000 mg divided daily of extract standardized to 0.3% hypericin for mildmoderate depression.
Vinca major/minor (Periwinkle)
Nervines Tonics
Digestive tonic that increases intestinal motility, parasympathomimetic, anti-spasmodic, mild analgesic, nervous system tonic, hepatic stimulant, depression, melancholy
Astringent, cerebral circulatory stimulant, cytotoxic (anti-cancer), diabetes, glaucoma, stroke, brain trauma, poor memory, disordered thinking
Infusion: 1 tsp/cup water, 1 cup QD – TID (fresh 3x dried). Tincture: (1:5, 25%), 2-5 ml TID. Fluid extract: (1:1, 25%), 1-3 ml TID.
Tincture: (1:5, 60%), 1-5 ml TID. 100 ml weekly max.
Lavendula o . (Lavender)
Carminative, nervous system relaxant, sedative, antispasmodic, anti-depressant, anti-septic, aromatic, uterine stimulant, emmenagogue, diuretic, hypotensive, anti-rheumatic
Tincture: (1:2, 60%), 2-5ml QD. Dried owers: 1-2g, TID. Capsules: 500mg, BID. Infusion: 1 tsp/cup, infuse 15 min, TID. Essential oil: 1-4ggt inhalations, chest rub, massage oil, pillow, douche. Bath: 100g infused and strained, added to bath.
Scutellaria laterifolia (Skullcap)
Sedative, hypnotic, diuretic, analgesic, topical antibacterial, astringent, antispasmodic, premature ejaculation, restlessness, nervous tension, headache, indigestion, restless leg syndrome, anxiety, phytoestrogen (PMS or menopause-related hormonal imbalances)
Nervous system tonic and relaxant, carminative, sedative, diaphoretic, antidepressant, anti-viral, antimicrobial, hyperthyroidism choleretic, antispasmodic, anti-histamine, mild analgesic, cardiotonic, hepatic, gout, herpes, rheumatism, neuralgias
100 mg 2 times a day of standardized product (5.2% bitter acids & 4% avonoids)
Capsules: 2-4 g QD. Infusion: 2 tsp/ cup, BID. Tincture: (1:2, 45%), 3-6 ml TID (maximum of 100 ml per week). Topically: poultice, compress, Herpelieve: apply 2 – 4 times daily.
Nervous system sedative, antispasmodic, analgesic, anti-in ammatory, antiseptic, carminative, antimicrobial, anti-allergic, anti-uler, wound healing, neuralgia, rheumatic and muscular pains
Infusion: 1-2 tsp/cup water; steep 3-5 min. covered; 1 cup TID. Tincture (1:5, 45%), 1-4 ml TID; max. weely dose 100 ml. Baths, Steams, Enemas. Note: Matricaria is best dosed on the low end of its dosage range over a long period of time.
Sedative, mild diuretic, carminative, aromatic, skeletal muscle relaxant, astringent, alterative, circulatory tonic
Sedative, nervous system relaxant, antispasmodic, anticonvulsant, hypotensive
Infusion: 1 tsp/cup TID. Tincture: (1:5, 45%), 2-6ml TID. Dried herb: 2-4g, TID. Poultice, mouth wash/gargle.
Powdered herb: 1-2 g QD. Infusion: 1 tbsp/cup, TID. Tincture: (1:2, 45%), 2-4 ml TID (weekly max. = 100 ml).
Passi ora incarnata (Passion ower)
Antispasmodic, sedative, hypnotic, vasodilator, cardiotonic, analgesic, anxiolytic, relaxant, diuretic, anti-depressant, insomnia
Anxiolytic, hypotensive, sedative, diaphoretic, antispasmodic, diuretic, emollient, immunomodulator, anti-in ammatory, expectorant, anti-coagulant, mild astringent, peripheral vasodilator
Nervous system relaxant, sedative, analgesic, hypnotic, narcotic, antispasmodic, whooping cough, rheumatism, aphrodisiac
Anxiety: 100-250mg, 2 times daily standardized (3.5-4% isovitexin); Insomnia/sedation: 200-500mg at bedtime standardized ((3.5-4% isovitexin)
Infusion: 1tsp/cup, 3-5 times QD. Tincture: (1:5, 40%), 3-5ml TID. Dried owers: 2-4g, TID.
Dried leaves: 0.5-3g TID. Infusion: 1 tsp/cup, infuse 15 min, TID. Tincture: (1:1, 25%), 0.5-3ml TID.
Sedative, nervous system, anticonvulsant, local anesthetic, analgesic, anti-fungal, anti-spasmodic, stimulant, anti-depressant, muscle relaxant, euphoric, anti-in ammatory, diaphroretic, carminative, diuretic, interstitial cystitis, restless leg syndrome, anxiety, cognition
100-300mg, 1-3 times daily (for no more than 3 months) standardized to contain 30-70% kavalactones
1. McEwen, B.S. (2006). Protective and damaging effects of stress mediators: a central role of the brain. Dialogues in Clinical Neuroscience 8(4), pp. 367-381.
2. Guilliams T. The Role of Chronic Stress and the HPA Axis in Chronic Disease Management. 2015. Point Institute.
3. Tsigos C, Kyrou I, Kassi E, et al. Stress, Endocrine Physiology and Pathophysiology. Updated 2016 Mar 10. In: De Groot LJ, Chrousos, Dungan K, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK278995/?report=reader.
4. Schneiderman N, Ironson G, Siegel S. Stress and Health: Psychological, Behavioral, and Biological Determinants. Annu Rev Clin Psychol. 2005;1: 607–628. doi:10.1146/ annurev.clinpsy.1.102803.144141
5. Guilliams and Edwards (2010). Chronic Stress and the HPA Axis: Clinical Assessment and Therapeutic Considerations. Point Institute.
6. Fries, E. et al. A new view on hypocortisolism. Psychoneuroendocrinology. 2005;30(10), pp. 1010-1016.
7. Sterling, P. (2012). Allostasis: A model of predictive regulation. Psychology & Behavior 106 (1), pp. 5-15.
8. Edwards L, Heyman A, Swidan S, Hypocortisolism: An Evidence-based Review. Integrative Medicine. Sep-Oct 2011;10 (4): 26-33.
9. Smith S, Vale W. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues in Clinical Neuroscience. 2006; 8 (4): 383-395.
10. McEwen BS, Gray JD, Nasca C. Recognizing resilience: Learning from the effects of stress on the brain. Neurobiology of Stress. 2015;1:1-11. doi:10.1016/j. ynstr.2014.09.001.
11. Heyman A, Edwards l, Lavalle J, Swidan S. Cardiometabolic disease in men: an integrative approach to managing hormonal risk factors. JMH. March 2010; 7(1): 92-101.
12. Fries E, Hesse J, Hellhammer J, Hellhammer DH. “A new view on hypocortisolism”. Psychoneuroendocrinology. 2005; 10:1010-6.
13. Yehuda R. “Sensitization of the hypothalamic-pituitary-adrenal axis in posttraumatic stress disorder.” Ann NY Acad Sci. 1997; 821: 57-75.
14. McEwen BS. “Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators”. Euro J Pharmacol. 2008; 583:174-185.
15. Heim C, Ehlert U, Hanker JP, Hellhammer DH. “Abuse –related posttraumatic stress disorder and alterations of the hypothalamic-pituitary-adrenal axis in women with chronic pelvic pain”. Psychosom Med. 1998; 60:309-318.
16. Scott LV, Teh J, Reznek R, Martin A, et al. “Small adrenal glands in chronic fatigue syndrome: a preliminary computer tomography study”. Psychoneuroendocrinology. 1999; 24:759-768.
17. Cleare AJ, Miell J, Heap E, Sookdeo S, et al. “Hypothalamic-pituitary-adrenal axis dysfunction in chronic fatigue syndrome, and the effects of low-dose hydrocortisone therapy”. J Clin Endocrinol Metab. 2001; 86(8):3545-3554.
18. Fries E, Hesse J, Hellhammer J, Hellhammer DH. “A new view on hypocortisolism”. Psychoneuroendocrinology. 2005; 10:1010-6.
19. Raison CL, Miller AH. “When not enough is too much: The role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders”. Am J Psychiatry. 2003; 160(9):1554-1565.
20. Hart BL. “Biological basis of the behavior of sick animals”. Neurosci Behavior Rev. 1988; 60:309-18.

For decades we have been told our medical system is broken. We might have known this long before the COVID-19 pandemic started, but unfortunately, now we see its gaping holes so much more clearly.
COVID deaths were sadly multiplied by the inept medical care provided to too many hospitalized patients. For example, it took one year to realize that placing patients on their bellies saved lives by allowing more oxygen to move into their lungs. What kind of craziness is this? Has common sense been eradicated from medical education and the practice of medicine? Didn’t we all know lungs expand better if you’re on your belly? And what about blowing people’s lungs out with respirators that didn’t help?
I’ve listened to horror story after story from my patients and peers about the fearmongering that rules the healthcare system and about how many unnecessary tests and procedures we are subjected to on an ongoing basis. Recently, I heard a commercial on the radio from a cancer center telling listeners in no uncertain terms that “cancer rates have gone up”since the beginning of COVID because patients no longer show up for routine screenings like they did before.
Where is the data to back up that statement? Why is this ad even allowed to be broadcast? Is it because freedom of speech now means freedom to bully and scare the living daylights out of patients and open the door for the healthcare system to make up for all the money it lost during the pandemic? How horri c is this?
We spend money like water and never get to the root cause of the problems we are so glibly treating with drugs and procedures and testing. We don’t really help patients; we only make more money for the broken system.
e fact that we have the most expensive healthcare globally, but our outcomes are not so great makes one wonder where we have gone wrong? e US spends at least 18% of its GDP ($3.35 trillion) on health expenditures. If costs continue to rise, by 2050, Medicare and Medicaid alone will account for 20% of the GDP. And still all projections point to continued rises in chronic disease.
Every patient I speak to tells me how afraid they are to go to the hospital. ere is no such thing as physical examinations or history-taking anymore. Decades have proven these diagnostic tools to work, yet now we have replaced them with an obligatory CT scan and 20 test tubes of blood. Why wouldn’t people be afraid to go to hospitals?
ese tests, medications, and even surgeries are the last things you need unless you get run over by a bus, have an internal catastrophe, or are in some kind of other accident. We don’t talk about the root cause of our health problems because we will eliminate trillions of dollars overnight from healthcare expenditures if we start there. We say we talk about prevention, but we don’t. Many doctors advertise that they specialize in prevention, yet it’s often lip service. ere is no training in medical school on lifestyle and prevention. It’s only still considered voodoo by conventional medical training. Most medical students and physicians do not receive adequate training in even the basics of lifestyle medicine, such as nutrition, sleep, stress management and physical activity.
But the truth is simple. We can easily help make our patients’ lives better. Here’s how our patients are doing damage to their health:
• Patients frequently drink alcohol.
• Patients don’t hydrate with water and wait until dehydration sends them to the emergency room.
• Patients eat junk food and don’t realize that’s why they are full of in ammation and become chronically ill.
• Patients are often sedentary and spend a great deal of time watching the small, medium, and large blue screens that destroy their vision and cognitive functions with impunity.
• Patients don’t sleep even though we all know the importance of sleep in rejuvenation and healing.
• Patients don’t understand the importance of meditating or breathing or just managing their stress, even though we know the less they react to stress, the less they will get sick and the better their immune system will work.
• Our patients don’t ever stop. ey just keep running themselves into the ground. And having more tests and procedures and taking more medication is only another way to destroy their lives and avoid preventing disease.
Preventative and lifestyle care is healthcare that prevents disease, injury, or illness, rather than treating a condition that has already become catastrophic or chronic. e goal of preventative care is to help people stay healthy, to improve their healthspan. Often, evidence-based lifestyle therapeutic interventions, including a whole-food plant-dominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection, are primary modalities
delivered by clinicians trained and certi ed.
Preventive care helps lower healthcare costs in America by preventing or treating diseases before they require medical care.
Lifestyle medicine intervention could help reverse chronic disease, leading to signi cant health care cost savings, according to a study conducted by the American College of Lifestyle Medicine published on 10/29/21 in the International Journal of Environmental Research and Public Health.
As the established global leader for continuing medical education, the American Academy of Anti-Aging Medicine (A4M) is rooted in a forward-focused mission to rede ne modern medicine through prevention, lifestyle, and whole-person care. Founded in 1992, the

Academy o ers graduate level education designed to produce the “complete practitioner” in all aspects of whole-person care. A4M has spent three decades equipping thousands of clinicians from across the globe with multifunctional tools to combat the growing burden of chronic disease and improve the human health span.
Use the COVID crisis to stop and look at your patient care. Don’t think you know enough and do seek additional education and training in the areas that will help your patient prevent disease, change lifestyle habits, and reach healthy longevity and lead productive lives.
Ericka Schwartz, MD is a leading expert in prevention, bioidentical hormone therapy, peptides and longevity medicine. Founder and CEO of Evolved Science and the Better Health Initiative, a 501c3 foundation committed to education in prevention and the optimization of the Doctor Patient relationship. Dr. Erika is the author of 8 bestselling books, TEDx speaker and sees patients in NYC from all around the globe.

Recent research has uncovered the decisive role of the endothelial glycocalyx, which both protects and regulates the entire vascular system. Arterosil HP plays a foundational role in overall health.*
Arterosil HP contributes to healthy vascular function in multiple ways:*
• Supports normal circulation*
• Helps support normal artery function*
• Helps maintain a healthy artery wall*
• Supports a healthy heart*
• Arterosil HP supports a strong and vital glycocalyx— the micro-thin gel lining in your veins and arteries.*


The physiological importance of nitric oxide was established in the 1990s and has since been confirmed by scientific studies and clinical experience. In an IRB-approved study, a single dose of Vascanox HP increased salivary nitric oxide levels for up to 24 hours.*††
Optimal nitric oxide levels have been shown to:
• Support a healthy cardiovascular system*
• Support and maintain blood pressure in the normal range*
• Support healthy circulation*

Learn more about these two vascular health products at Calroy.com
† As demonstrated in an independent third-party laboratory in vitro study
††As measured by saliva NO test strips in an open label IRB-approved study. To learn more please visit Calroy.com
*These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent any disease.
Total Gut Restoration is a comprehensive 3-month program designed to support restored gut health. Protocols that address only one aspect of gut health are often ineffective. Combined support from three unique supplements in Total Gut Restoration promotes a healthy gut, including maintaining a healthy microbial ecosystem and a protective gut barrier. The Total Gut Restoration program is supported by research, proven by practice, and approved by clients.**
The Total Gut Restoration program employs this triple-action approach**
MegaSporeBiotic™ is the trendsetting 100% spore-based probiotic shown to RECONDITION the gut by promoting greater microbial diversity and encouraging health-supportive gut bacteria growth.**
MegaPre™ Precision Prebiotic™ REINFORCES the health-supportive microbial changes created by MegaSporeBiotic™.**
MegaMucosa™ is innovative mucosal support formulated to REBUILD a healthy mucosal barrier and promote optimal immune function in the gastrointestinal mucosa.**
Visit us at microbiomelabs.com to order your Total Gut Restoration kit today!
**These
From sports medicine to novel treatments for Metabolic Syndrome and all its co-morbid conditions, the use of bioactive peptides in medicine is a subject to which clinicians and their patients, should be exposed. Sleep and cognitive problems, improved performance and recovery, tendon and ligament repair, sexual dysfunction and weight issues are just some of the applications for patients seeking healing and rejuvenation.
The BIOPEP (bioactive peptide) database currently stores about 4000 bioactive peptides, encompassing approximately 992 Angiotensin-I-Converting Enzyme (ACE) inhibitory peptides, 652 antioxidant peptides, 500 antibacterial peptides, 488 dipeptidyl peptidase (DPP) inhibitory peptides, 113 neuropeptides, 20 antiviral peptides, 47 calmodulin-dependent protein kinase II (CaMKII), and many other functional peptides.
Sales of novel peptides globally have grown from US $14.1 billion in 2011 to almost US $28.5 billion in 2020. Currently, the United States market is 40% of global peptide sales. Although mass-produced in China also, peptides manufactured by compounding pharmacies in the United States with a 99% or greater purity are recommended.

Advances in peptide therapies for “off-label” uses offer additional therapeutic options for a plethora of health conditions, including:
Peptides are short chains of 2 to 40-50 amino acids that are linked by peptide (amide) bonds. More than 7,000 naturally occurring peptides that have crucial roles in human physiology and performance have been identified. They function as hormones, neurotransmitters, growth factors, ion channel ligands or anti-infectives. In the body, peptides cause a cell-signaling response that can have regulatory and rejuvenative actions on neuro-endocrine-immune function. Peptides can help the body recover from injury or illness faster, lose weight more efficiently, decrease inflammation and pain and improve results in the gym.
As a clinical tool, peptides can be specific and efficacious, while for the most part also being relatively safe and well tolerated. The history of peptides in clinical therapeutics began with insulin in the 1920s. There are approximately 60 US FDA approved peptide medications on the market, with continued increased interest by pharmaceutical company research and development, which by 2014 had led to approximately 140 peptide therapeutics being evaluated in clinical trials in the US and 500-600 in pre-clinical trials. Examples of approved pharmaceutical peptides include Lantus insulin, Lupron (prostate cancer treatment), and Byetta or Victoza (GLP-1, glucagon-like peptides for type 2 diabetes). New FDA approved products on the horizon include a melanocortin 4 receptor (MC4R) agonist for metabolic syndrome and weight loss and intranasal PT-141 (bremelanotide) for Female Sexual Dysfunction (and to support men’s sexual health).
· Anti-aging
· Epigenetic modulation
· Stem cell proliferation
· Blood glucose and insulin regulation
· Weight management/ appetite control
· Cardiovascular support – lipids, blood pressure, vascular function
· Metaflammation
· Improved lean muscular growth
· Increased hGH (human growth hormone) levels
· Reduced body fat –increased lipolysis
· Improved energy, stamina and decreased fatigue
· Improved immune responses
· Improved inflammatory responses

· Improve injury recovery
· Improved sleep patterns
· Improved memory and concentration
· Regulation of other hormones, i.e sex, thyroid, blood sugar, stress
· Improved sexual desire (libido)
· Improved bone mineralization and density
· Improved workouts, recovery
· Pain control
· GI support
In the U.S. market, unless specified as a drug, peptides are most manufactured in compounding pharmacies with a 503B designation. This is critical for product quality, as some peptides are commonly available on the internet and sold as “research only“ use. Most were made in China, which unfortunately cannot always be relied on for adequate product quality control and in some cases even are adulterated. A 503 B compounding pharmacy must submit products they manufacture for lab analysis to prove content and stability of the product. Many problems have been reported from the use of internet peptides sales, including local reactions and even more severe reactions leading to hospitalization. This is why peptides should be purchased from a qualified pharmacy that follows FDA approved GMPs in their manufacturing facilities.
There have been continued innovative technological advances in peptide manufacturing and drug delivery with the fields of

more plant peptides to market have been cost of production and modification of structures to increase their bioavailability and assure their absorption. Some of the plant peptides uses include:
· Antiaging, antioxidant
· Antimicrobial
· Antidiabetic – IR and MetS (hypertension, hypercholesterolemia, obesity/overweight, blood glucose regulation issues)
· Other cardiovascular issues
· Anticancer
· Pain issues
From peptides as antimicrobial agents to use for cognitive and neurological support to plant peptides for metabolic syndrome, peptides in different delivery forms certainly hold great promise for practitioners. Peptide therapies of different types are an area with a tremendous number of resources being devoted to continued research and development, and with genomics the potential combination of different sequencing for peptides is endless. We certainly can expect the number of peptides, from both animal and plant sources, available as therapeutic agents to increase dramatically over the next few decades.
genomics, metabolomics and proteomics all contributing to this innovation. Recombinant technology and genetic engineering have allowed researchers to tweak formulas ever so slightly, improving bioavailability (including CNS availability), efficacy and safety. Progressive compounding pharmacies and labs that have gene sequencing lab equipment and FDA approved Q/A testing (HPLC, mass spectrophotometry, etc.) can tailor-make therapies at a practitioner’s request. Nanotization for improved bioavailability is also an option now. Oral and intranasal peptide formulations are also becoming a reality, with improvements in GI permeability a focus of much research. Peptides are relatively unstable making manufacturing a challenge and delivery is most commonly via injection. Since injections are somewhat objectionable to consumers, oral delivery of peptides is a major area of research and development as well due to the easier delivery method of oral administration.
On the horizon also is the use of plant peptides to produce effective human peptide therapies. Some barriers of getting
There are several compounding pharmacies in the U.S. offering safe, Q/A verified, pharmacist-synthesized, and/or compounded peptides made for various delivery methods, and as long as FDA regulations continue to allow for them, the environment is unfolding for peptides to be a mainstay therapeutic option for many chronic conditions, acute illnesses or injuries, as well as antiaging and health optimization uses.
In summary, keep in mind that improved nutrition, management of hormone relationships, exercise and many other factors all plays a role in creating “whole person” health, which is the emerging term at NIH. Peptides are another tool in the kit that you can explore to revitalize and extend the health span of your patients.
PharManufacturing: Int Peptide Rev 2013:10–5.
4. Kingsberg SA, Cayton AH, Pfaus JG. The Female Sexual Response: Current Models, Neurobiological Underpinnings and Agents Currently Approved or Under Investigation for the Treatment of Hypoactive Sexual Desire Disorder. CNS Drugs. 2015;29(11):915–33.
5. Minkiewicz, Pet al. BIOPEP-UWM database of bioactive peptides: Current opportunities. Int. J Mol Sci. 2019;20(23):5978.
6. Fosgerau K, Hoffman T. Peptide therapeutics: current status and future directions. Drug Discov Today. 2015;20(1):122-8.
7. Kaspar AA, et al. Future directions for peptide therapeutics. Drug Discov Today 2013;18(17/18):807–17.
8. Lalatsa A, Schatzlein AG, Uchegbu IF. Strategies to deliver peptide drugs to the brain. Mol Pharm. 2014;11:1081–1093.
9. Brayden DJ, Alonso MJ. Oral delivery of peptides: opportunities and issues for translation. Adv Drug Deliv Rev. 2016;106:193–195.
10. Bruno BJ, Miller GD, Lim CS. Basics and recent advances in peptide and protein drug delivery. Ther Deliv. 2013;4(!1):1443-1467.
11. Lico C, et al. The use of plants for the production of therapeutic human peptides. Plant Cell Reports. 2012;31:439-51.
12. Chai TT, et al. Plant bioactive peptides: current status and prospects towards use in human health. Protein Peptide Lett. 2021;28:623-42.




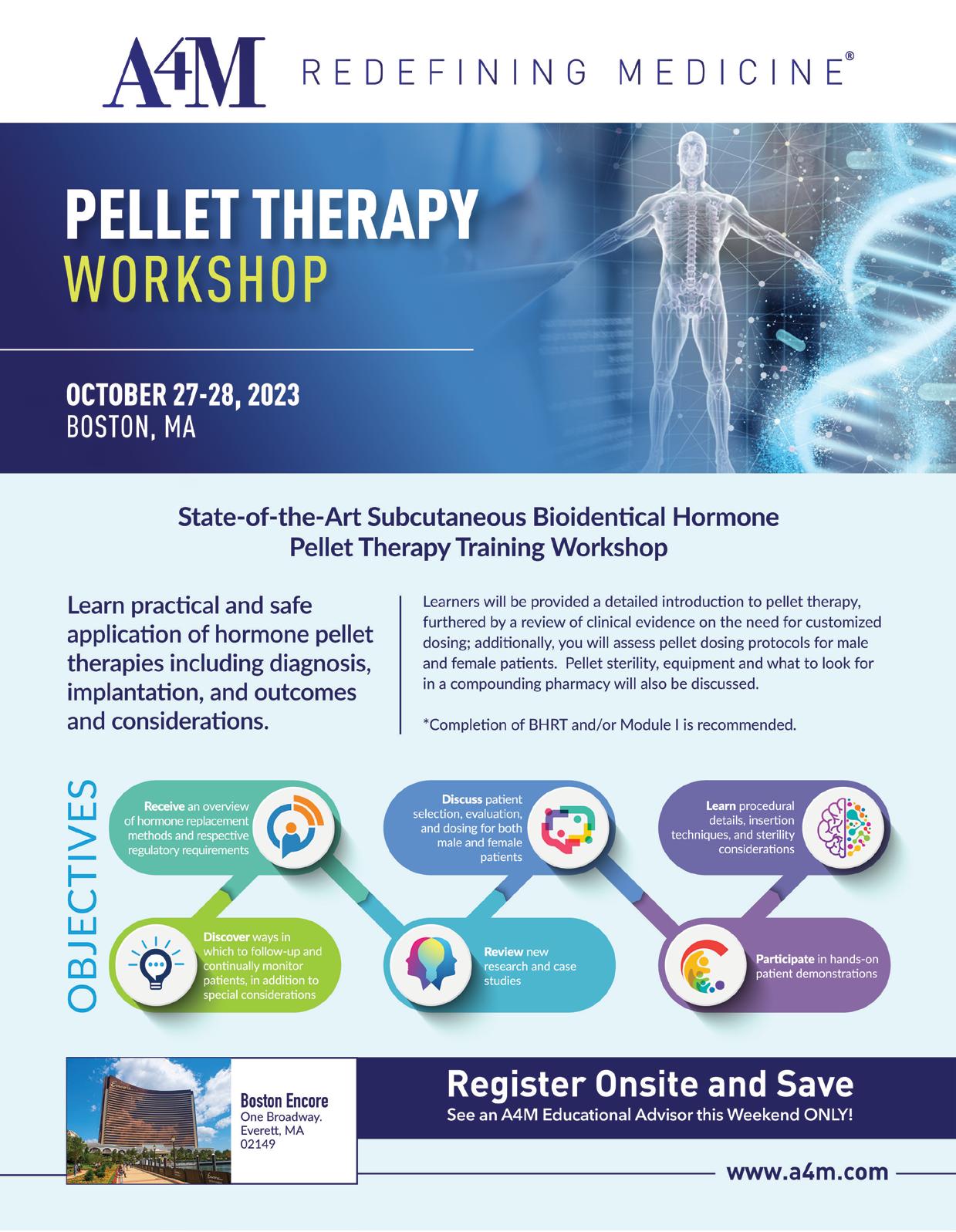
EXCLUSIVE HEALTH PRACTITIONER BRAND


PRIVATE LABEL DEVELOPMENT

PRIVATE LABEL INTEGRATION


PRIVATE LABEL FULFILLMENT

ACCESS OUR INVENTORY OF OVER 1000 BRANDS OF MORE THAN 10K PRODUCTS
CUSTOM PRODUCT DEVELOPMENT
CUSTOM PROTOCOL CREATION
NO CHARGE FOR DROP SHIPPING
NEW YORK BASED
SAME DAY SHIPPING
LIVE EXPERIENCED CUSTOMER
SERVICE REPRESENTATIVES

CUSTOM PRESCRIBER PORTAL