

















The care sector is, as we know, no stranger to challenges. From chronic underfunding and staffing shortages to rising operational costs and the ever-increasing demand for high-quality care, the industry has been navigating a perfect storm for years.
Against this backdrop, a new report titled People-Powered Care, published by Care England, in association with the Employee Ownership Association (EOA) has sparked a timely and thought-provoking discussion about whether employee ownership (EO) could be a viable solution to the sector’s ongoing crisis.
The report, which can be accessed here, highlights the potential benefits of employee ownership models in addressing some of the most pressing issues facing care providers. It also draws on successful examples of EO in other sectors, suggesting that this approach could foster greater staff engagement, improve retention, and ultimately enhance the quality of care. But is this a realistic proposition for the care sector, and could it truly help resolve the current crisis? Let’s delve deeper.
Employee ownership is not a new concept, but its application in the care sector has, from what I have seen, been limited. The model involves employees having a significant stake in the business, whether through shares, trusts, or other mechanisms.
This ownership stake is intended to align the interests of staff with those of the organisation, creating a sense of shared responsibility and accountability.
The People-Powered Care report argues that EO could address several key challenges in the care sector:
1. Staff Retention and Morale: One of the most significant issues facing care providers is high staff turnover. By giving employees a stake in the business, EO could foster a greater sense of ownership and commitment, leading to improved morale and retention rates.
2. Quality of Care: When employees feel valued and invested in the success of their organi-
sation, they are more likely to go above and beyond in their roles. This could translate into higher standards of care for residents.
3. Financial Sustainability: EO models often lead to more efficient and innovative business practices, as employees are motivated to find ways to improve performance and reduce costs. This could help care providers navigate the financial pressures they face.
The report cites examples of EO success stories in other industries, such as the John Lewis Partnership, where employee ownership has been credited with driving innovation and maintaining high levels of customer satisfaction. While the care sector is undoubtedly different, there are already some encouraging examples of EO in action. For instance, Care & Share Associates, a social enterprise operating in the care sector, has demonstrated how employee ownership can create a more engaged and motivated workforce.
However, the report has also sparked debate within the sector. Some care providers have welcomed the idea, seeing it as a way to empower staff and improve outcomes. Others, however, remain sceptical, citing the complexities of transitioning to an EO model and the potential risks involved.
So, is employee ownership a viable proposition for the care sector?
The answer, which is well above my “pay grade”, is, as with most things, not straightforward.
While EO has the potential to address some of the sector’s most pressing issues, it is not a one-size-fits-all solution.
Careful consideration would need to be given to the specific needs and circumstances of individual providers, and the transition would require significant investment and support.
That said, the People-Powered Care report has undoubtedly opened up an important conversation.
At a time when the sector is facing unprecedented challenges, it is essential that we explore all possible avenues for improvement.
Employee ownership may not be the answer for everyone, but for some providers, it could be a “game-changer.”
As the debate continues, one thing is clear: the care sector needs bold and innovative solutions. Whether EO is part of that solution remains to be seen, but it is certainly an idea worth exploring further.
What are your thoughts? Could employee ownership work in your organisation? We’d love to hear from you.
Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2 5BR.
I can always be contacted at editor@thecareruk.com

damage. Views expressed within this publication are not necessarily those of the publisher or the editorial team.
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden unless

(CONTINUED FROM FRONT COVER)
In their recent Sector Pulse Check survey in partnership with Hft, Care England, a registered charity found that 29% of providers shared that they were considering leaving the market for a third year running, noting that the most recent results show that the “the approach to health and social care is not working”.
FINANCIAL PRESSURE
Just over 90% of those surveyed cited “workforce-related costs” being the largest financial pressure, dominated by local authority fees to providers not increasing in line with National Living Wage, with other significant strains including utilities, maintenance costs and non-payment of bills by local authorities.
With increases to employer National Insurance expected to cost the sector a further £2.8 billion, the Health and Social Care think tank Nuffield Trust, warn that “swathes of the social care market” could collapse as a result.
The paper explores how providers in the Adult Care Sector looking to exit the market could help build in sustainability, a better working life and better quality of care by selling their business to their employees.
A particularly significant compounding challenge the paper reveals is the “workforce crisis in care,” characterised by high turnover and vacancy rates.
Although the sector’s turnover rate has decreased to 24.8% (from 29.1% in 2022/23), and the vacancy rate has similarly decreased to 8.6% from a historic peak of 10.6% in 2021/22, both figures remain significantly higher than other sectors.
RECRUITMENT COMPETITION
Insight shared by EOA members in this sector indicates significant competition between providers for recruitment, while the care sector as a whole struggles to compete with other low-wage sectors, such as retail, where financial reimbursement and workload are less intensive.
HIGH WORKLOAD
Care is seen as a low-wage industry, where employees typically report feeling undervalued, with limited progression and development opportunities also often cited as contributors to the workforce crisis, alongside a high workload and a lack of consistent training or standards across the sector.
The paper links these impacts to the self-compounding issue of an overall poorer quality of care and poor staff retention, resulting in a high new starter rate across the sector of 38%, making it materially difficult to establish and maintain standards within or across businesses when such a high proportion of the workforce is less experienced and close to 1 in 3 employees leave their roles each year.
Taken together, the paper says, the challenges facing the care workforce continue to threaten the overall sustainability of the sector. With the significant existing constraints on capacity, the threat of a mass exodus of providers from the market would, therefore, be disastrous for the delivery of care in the UK EO “POWERFUL MODEL”
Professor Martin Green OBE, Chief Executive of Care England, said: “In our society, adult social care is the foundation of support for millions of individuals and their families, enabling them to live with dignity, independence, and choice. Despite its critical importance, the sector faces extraordinary challenges, from financial pressures to workforce shortages.
“Employee ownership stands out as a powerful, innovative model that can transform how care is delivered, creating a system that prioritises the wellbeing of those who give and receive care.”
The EO sector has grown rapidly in recent years, with over 2,200 employee owned businesses (EOBs) in the UK by the end of 2024. This represents a fifteenfold increase since 2014 when there were only 150 EOBs; more recently the number of EOBs has more than doubled since the end of 2021 and almost quintupled since the end of 2019.
Reflecting this significant growth, evidence suggests that EO is now one of the UK’s most popular succession options, making up 12% of all private company transactions and being the preferred exit strategy of 18% of business owners.
The most common reasons for transitioning to EO include protecting the business’s independence, culture and values, and securing the long-term wellbeing of employees. Also important are the generous tax advantages offered by the EOT, including a complete Capital Gains Tax exemption for owners disposing of a majority of shares to their employees.
James de le Vingne, Chief Executive of the EOA, said: “Harnessing the evidenced power of EO to drive employee wellbeing, increase productivity and innovation, and root that in communities for the longer term is a compelling proposition for policy makers – in the care sector it could be pivotal in sustaining capacity and delivering the quality of care we all would hope for ourselves when we are at our most vulnerable.”
“While on its own it is not a silver bullet to cure the pressures the sector faces, we firmly believe it can be part of the answer and offer our full support in exploring the opportunity.”
The fast-growing sector has seen a period of learning that has developed a framework of practices that deliver Great EO, with hundreds of case studies demonstrating success.
Shaw Healthcare, which provides a range of residential and non-residential care services for both the elderly and those needing complex care such as those with dementia or additional needs, was crowned Employee Owned Business of the Year in November 2024.
Russell Brown, CEO of Shaw Healthcare, which has 3300 employees, operating 64 registered care services across 57 sites plus Facilities Management services at a further 12 sites, said:
“Employee ownership using the EOT model has been a great journey for us and our employees who now have a stake and a say. Employee ownership has helped us retain our independence and has had a huge impact on staff retention in a challenging sector.
Shaw transitioned to employee ownership in May 2020, two months into the pandemic, feeling the imperative of the move to EO was even greater given the pressures that health and social care would face. In that time, they have seen a 25% increase in turnover, supported in part by reducing costs by reducing employee turnover to below 17%, from 30%.
Russell added: “I’m very pleased that our collective hard work has meant employees have received a share of over £5.5m of profits since becoming an EOT in addition to an improved benefits package. Importantly, our employees understand it’s because of the excellent care that they’ve delivered.”


In the care industry, reputation is everything. Choosing a care facility or in-home provider is a deeply personal decision based on location, budget and individual needs.
It’s also based on trust. Families rely on providers to deliver quality care, so a strong reputation is essential.
In the UK, adult care homes are rated by official bodies like the Care Quality Commission (CQC) and by residents and their families. However, as the CQC undergoes reform, personal feedback and reviews have become critical in offering an unfiltered view of the resident experience.
Selecting a care facility or in-home provider is a deeply personal decision based on trust, location, budget, and individual needs. Families rely on providers to deliver quality care, so a strong reputation is essential.
The growing reliance on authentic reviews offers facilities an opportunity to set themselves apart and offer the insights prospective patients seek. Yet, a recent research report reveals that in-home care providers aver-
age just nine reviews annually, with the top 20% receiving fourteen reviews. This indicates a gap in review engagement that providers can turn into an opportunity.
The difference between a trusted care facility and a questionable one often comes down to how effectively a provider manages its reputation. Managing various listings and online reviews can weigh heavy on a facility with stretched resources.
ENCOURAGING
The true measure of reputation comes from the experiences shared by current and former residents and their families. Proactively soliciting feedback is powerful - 22% of the public report they leave reviews when asked. A steady flow of fresh feedback prevents outdated sentiment from impacting perception. In a market with such high demand for care home places, this could have serious consequences.
Reviews need to be managed and cultivated as part of continuous improvement within customer service, as they’re one of the primary indicators of quality.
BUILDING TRUST WITHIN THE COMMUNITY
By Chris Sparling, Senior Director,
It is important that reviews are managed transparently, so providers can build trust with their current and future patients. The same report found that top-performing care providers respond to over 80% of reviews, while the industry average lags at 68%. However, these numbers drop significantly for negative reviews, which is a missed opportunity.
Acknowledging both positive and negative feedback is crucial for building credibility. Doing this will reassure prospects that a facility is open to listening and proactively addressing concerns. Filtering reviews to exclude the negative ones presents an unrealistic image and will deter prospects evaluating whether a facility is the right one for them.
Responding to online feedback is an extension of customer service quality, and many prospective patients seek this level of engagement. By providing thoughtful and timely responses, care providers can increase customer satisfaction and strengthen their overall reputation.
Facilities that listen to residents and their families, and take proactive steps see improved satisfaction and stronger relationships with those they serve. Addressing negative reviews can even turn challenges into positive outcomes.
Industry leading providers are already leveraging technology to maximise the impact of online reviews. Many automate review responses, ensuring that every reviewer feels respected and appreciated. This approach also eases the pressure on internal resources by streamlining the feedback response process. Moreover, facilities can use data from reviews to identify strengths and weaknesses, addressing areas of concern proactively. For those with smaller budgets, data-backed insights help allocate funds effectively, so that the focus remains on what matters most to residents and families. Whether that’s staff excellence or a provider’s welcoming environment, marketers should highlight these strengths in their promotional materials, and use customer feedback as a way to validate them.
Care providers should embody their commitment to people-centred service in their online interactions, regardless of whether feedback is positive or negative. Reputation management is a crucial part of this commitment, as it ensures that patients feel valued and heard, while offering sought-after insights to those trying to make big decisions.
With the right tools and strategies in place, care providers can harness the power of online reviews to build trust, improve satisfaction, and build a lasting reputation that resonates with both current and future residents.
Residents of Simonsfield Care Home, Liverpool, part of Qualia Care, went on a whirlwind adventure to Rome, the Grand Canyon and were taken on a Kenyan Safari.
Thanks to virtual technology, these unforgettable journeys were brought to the residents without leaving the comfort of Simonsfield.
The virtual tour is an example of the wide range of activities provided by the home for its residents. Other activities include afternoon teas, exercise classes,
shopping trips and dining out at local cafes and restaurants, the fun never stops!
Residents also get to enjoy films together, dancing lessons, bingo, and visits from local primary school children for reading sessions. Simonsfield knows how to bring joy and entertainment to its residents.
Karen Evans, the home manager said: “At Simonsfield, we strive to keep our residents interested and active. The virtual reality tour was a big success as the residents enjoyed it. Their adventures provided plenty of excited conversation.”

Residents at Longview Care Home, part of the Runwood Homes Group, enjoyed a lively and engaging seated tap dancing class on 3rd February, as part of a new initiative bringing dance into care homes. The session, led by a local tap dance instructor, aimed to provide a fun and innovative way for residents to stay active while enjoying the rhythm of music.
Residents were provided with tap slippers to wear over their shoes and special gloves with clickers to enhance the experience. They followed the instructor’s lead, dancing and clapping along to the lively tunes. Family members also joined in, making the event a truly inclusive and heartwarming experience.
Resident Hazel

too.”
The event, which saw a full lounge of residents and even young carers getting involved, was a huge success. Jessica, Lifestyle Coordinator at Longview, highlighted the importance of bringing new and creative ways to incorporate exercise into residents’ daily lives. “It’s also lovely to have someone from the community involved, and we’re excited to make this a monthly class moving forward,” she said. The atmosphere was full of joy and energy, with the highlight being the instructor dancing one-on-one with each resident at the end of the session, making them feel special and celebrated.
With such an overwhelmingly positive response, Longview Care Home is excited to continue offering this unique activity, proving that age is no barrier to dance, joy, and movement.

The social care provider organisation, The Independent Care Group (ICG) has thrown its weight behind a national day of action to call on the Government to help the sector.
ICG representatives will join care providers from across the country when they converge on Westminster on 25th February.
They will be calling on the Government to review the impact the proposed increase in Employer’s National Insurance Contributions and rise in the National Living Wage will have on social care.
ICG Chair, Mike Padgham urged all providers to join the day of action, which is being organised by Providers Unite, a coalition of social care representatives.
“Enough is enough – we have to make a stand and show that the country cannot go on neglecting and ignoring social care any longer,” he said.“We have had three decades of under-finding and neglect, of broken promises and of waiting for reform that has never come.”
“And that has led us to a point where 2m people cannot get the care they need to enjoy a decent quality of life.”

“That is a betrayal of people who deserve better –of grand-parents, parents, husbands and wives, aunts, uncles and friends.”
“We have been politely asking for reform for 30 years or more and it has never come. On the 25th of February care providers have an opportunity to stand up and speak for those who don’t have a strong voice and to demand reform.”
“I urge everyone who can get down to Westminster to go and show the Government that this time social care has to change.”
The planned day of action is a demonstration of the level of concern social care providers have over the impact budget measures will have on the delivery of care. They say that without Government help, the combined impact of increases in the Employer’s National Insurance Contributions and the National Living Wage could be devastating on a sector that is already on its knees. They fear provider closures and more people going without care.
Campaigners want the Government to review the budget measures, make social care providers exempt from the rise in National Insurance or to put more funding into the sector to help them cope with rising costs.
The day of action takes place on Tuesday, 25th February. More details: www.providersunite.co.uk



By Prof. Richard Harding, Director and Anna Peeler, Postdoctoral Researcher at Cicely Saunders Institute of Palliative Care, Policy & Rehabilitation, King’s College London

With a growing and aging population, healthcare systems in the UK and around the world face significant challenges. More people than ever before are living with chronic and progressive conditions, at home and in care homes, which can greatly impact their quality of life and their ability to do the things that matter to them. As the debate to the right to assisted suicide continues in the UK, many are rightfully calling on the UK to improve access to palliative care.
Together with Dr Asmus Hammerich, Director of Noncommunicable Diseases and Mental Health at the WHO Office for the Eastern Mediterranean Region, and an international team of palliative care experts, we have published a report, ‘Palliative Care: How can we respond to ten years of limited progress’ launched at the recent World Innovation Summit for Health (WISH) – the Qatar Foundation’s global health initiative aimed at improving healthcare for the world’s most vulnerable.
In this report, we highlight how the one percent of people who die annually consume 10% of the health budget in high-income countries like the UK, often on care and procedures that do not improve or extend their lives. Moreover, millions of people around the world are experiencing preventable suffering caused by lifelimiting conditions, which will continue to increase as people live longer and chronic diseases become more prevalent. We have a solution to this global challenge, i.e. expanding access to highquality palliative care, an approach that prioritises quality of life and person- and family-centred care for people with life-limiting conditions such as cancer, heart diseases, dementia, and chronic lung disease. There is a critical need for generalist palliative care to be made available to everyone who needs it beyond specialised inpatient facilities.
A decade after the World Health Assembly introduced Resolution 67.19, aimed at making high-quality palliative care universally accessible, progress remains too slow. Only 14 per cent of palliative care needs are met around the world today, highlighting the urgent need for increased efforts to meet the rising demand for compassionate palliative and end-of-life care.
The need for palliative care is expected to increase dramatically in the coming years and could double by 2060. If this global chal-

lenge is to be tackled, care needs to be shifted from hospitals to communities, including primary care and care homes, and there must be a reframing of understanding of palliative care to include anyone with a life-limiting condition, not just people who are close to dying.
In our report, we have highlighted innovative and cost-effective models of training and care from around the world. The recommendations in this report offer a way to provide effective, costsustainable palliative care for those who need it most, and care facilities in the UK and elsewhere are advised to review the report for see how they can adapt these best practices and key learnings. For example, all general healthcare providers and social care staff should receive basic palliative care training so they have the knowledge and confidence to incorporate the principles of palliative care into their work and identify people who might need additional support from specialists. With this approach, all patients, regardless of their condition, can receive comprehensive support and person-centred care, making it accessible and equitable across the board.
Additionally, we recommend that researchers and health and social care workers use person-centred outcome measures like the Integrated Palliative Outcome Scale to screen people and understand needs and to monitor service quality over time. This measure includes questions like “What have been your main problems or concerns over the past week?” and “To what extent has pain affected you over the past week?” to monitor symptoms and other concerns and assess the impact of palliative care services. This ensures care is holistic, meaning it encompasses their physical concerns as well as their psychological, social, and spiritual concerns, and can be tailored to what matters most to the individual.
In the UK, care homes are uniquely positioned to provide highquality core palliative care services to their residents, most of whom likely have palliative care needs. As staff have constant interaction with residents and are able to build relationships over time, they are well positioned to recognise changes in symptoms and quality of life, offer support where needed, and refer to other services when necessary, such as specialist palliative care providers. Having some core palliative care training and using person-centred outcome measures to screen for needs and monitor changes over time could help identify those with needs early and intervene in time to preserve and improve quality of life for residents with life-limiting conditions.
Collaborative efforts and targeted intervention can strengthen the delivery of, and access to, palliative care as an essential, effective, cost-effective service for all who need it. The risk of maintaining the status quo and not significantly and purposively expanding access to palliative care equitably would represent a failure to respond to the enormous – and growing – level of preventable suffering over the next few decades.
Chiltern Water & Environment was established in 1991 by Robert Hunt after gaining 25 years' experience as an operational and analytical scientist in the water supply industry. The company gained engineering and further management knowledge when David Hunt joined in 2012. Since then, other water industry professionals have added to the breadth of knowledge and experience within the company.

We have always provided high-quality consultancy, testing and remedial services in a professional but personable manner. Our steady growth has reflected our clients' trust in our services. Our current clients include large housing associations, pharmaceutical companies and facilities management companies, as well as individual landlords and small businesses. We ensure all our customers receive the same level of care and attention to detail.
Duty Holders of all commercial and public building premises are legally required to assess the risk from legionella to anyone using the water systems and put in place legionella control measures if required. The HSE has produced ACoP L8 and HSG274 as guidance for Duty Holders obligations. We have clients throughout the South East, London and the Midlands, and carry out water tests nationally and internationally. We currently provide regular water sampling and testing for over 500 sites.
Tel: 01844 347678
Email: info@chilternwater.co.uk www.chilternwater.co.uk
Care England has played a central role in shaping the Care Provider Alliance’s (CPA) newly published report on the Care Quality Commission’s (CQC) Single Assessment Framework (SAF).
The report, they say, is a direct result of the efforts of members, and colleagues in the CPA, to ensure that the voices of care providers are heard, and that regulatory oversight is fair, transparent, and effective.
Professor Martin Green OBE, Chief Executive of Care England, stated: “This report would not exist without the engagement, persistence, and unity of the social care sector. While previous reports by Dr Penny Dash and Sir Mike Richards identified fundamental failings in the CQC’s approach, they did not sufficiently reflect the lived experiences of providers on the ground. That has now changed. This review is the first to truly centre provider feedback, and it stands as a powerful tool to hold the CQC to account.”
The findings lay bare the significant challenges providers have faced with the Single Assessment Framework—ranging from confusion and inconsistency to a lack of meaningful engagement with the sector. For too long, providers have felt unheard, navigating a system that is burdensome, unclear, and at times detrimental to staff morale and service improvement. Now, thanks to the collective efforts of Care England, our members, and the wider CPA, these concerns are impossible to ignore.”

Through extensive engagement – including surveys, workshops, and ongoing dialogue – Care England and our CPA partners have ensured that the concerns of care providers were not just acknowledged but embedded within this review. Over 1,200 providers contributed, reinforcing the power of a united sector in driving change.
The report outlines 11 key recommendations aimed at improving the CQC’s regulatory approach and rebuilding trust with care providers.
THESE INCLUDE:
• Create a reduced set of quality statements and assess all providers on a consistent set of statements for every routine inspection.
• Create guidance for each service type at the quality statement level.
• Use the information in the Provider Information Return to plan a timeline, CQC staffing, and priorities for
assessment. Share this assessment plan, including evidence requests, with providers and give them advance notice of inspection.
• Ensure that evidence included in decision-making has been corroborated rather than taken at face value, to produce a balanced appraisal of the service and is not wholly focused on finding issues or risk.
• Re-write the reports of providers who have been assessed in the period of time between the implementation of the SAF and the stabilisation of the regulatory approach to a consistent and meaningful process.
• Develop a shared, meaningful approach to co-production with providers for use in further work to be completed during CQC’s ongoing recovery programme. Re-introduce a single point of contact/named inspector for providers Train inspectors, with the involvement of care providers, to understand and respect each type of care service and the people that they support.
Establish an independent body to mediate all complaints and challenge processes.
Ensure that all changes in regulatory approach thus far and in future are effectively communicated to all inspectors to reduce inconsistencies in implementation.
The recommendations can be read in full on the CQCs website
Care England said it will continue to push for urgent and lasting improvements to the CQC’s regulatory approach, and will continue to advocate for a system that works with providers, not against them, ensuring a fair and proportionate framework that supports quality care.
The importance of this report has been acknowledged by the CQC’s leadership, with Sir Julian Hartley, Chief Executive of CQC, recognising it as ‘instrumental in ensuring we hear the voices of a wide range of adult social care providers.’ James Bullion, Chief Inspector of Adult Social Care and Integrated Care, further emphasised that the report provides ‘a practical agenda for change‘ and will be incorporated into the CQC’s urgent improvement work.
He also acknowledged the distressing impact that past regulatory approaches have had on providers, as well as the need for significant improvements to inspection processes, technology systems, and communication with the sector.
Chacombe Park care home in Banbury was transformed into a little corner of the Caribbean to celebrate what would have been Bob Marley’s 80th birthday on 6th February.
Born in Nine Mile, Jamaica, Robert Nesta Marley, or Bob Marley as he was better known, died of a rare type of skin cancer in 1981, aged just 36. He was considered one of the pioneers of reggae and was known for his distinctive, soulful vocal and song writing style. He is hailed as a cultural icon who increased the visibility of Jamaican music worldwide, despite his relatively short career. His album Legend is the best-selling reggae album of all time. Rolling Stone ranked him 11th on its list of the


100 Greatest Artists of All Time.
General Manager, Shaju Paul, said: “Lots of our residents are big Bob Marley fans and still love his music. We’ve had a fantastic day listening to all his hits, finding out about his life and what influenced him. We watched his past performances whilst the residents indulged in a glass of Jamaican spiced rum and Ginger cake!”
John, a resident said: “I loved listening to Bob Marley growing up. Listening to all his old hits has brought back so many memories, we were all transported to the Caribbean for a slice of island life and the rum definitely added to the overall reggae vibe.”
• We specialise in the sale and purchase of quality used wheelchair
and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.



By Christopher Love, Head of Corporate Recoveries and Insolvencies at Primas Law

The care home sector in the UK is a cornerstone of support for some of the most vulnerable members of society. However, in recent years, rising costs, staffing shortages, and systemic funding issues have created the perfect storm of financial pressures, making it increasingly difficult for businesses to stay afloat.
But there is light at the end of the tunnel. With the right strategies in place to mitigate financial challenges, businesses can set themselves up to weather tougher financial periods, avoid insolvency and continue to provide a vital care service for those who need it most.
Factors contributing to insolvency risks
Rising staffing costs, particularly due to changes in National Insurance Contributions (NICs), have placed a heavy burden on budgets, with even small increases in employment expenses having a significant impact. At the same time, severe staff shortages, exacerbated by reduced EU immigration, growing competition in the labour market, and post-pandemic disillusionment, have left many care homes struggling to fill essential roles.
On an economic level, the increasing cost of funding, driven by higher interest rates, has made borrowing more expensive for businesses, limiting investment in critical infrastructure and resources. Inflation has also taken its toll, pushing up costs across the board—from energy bills to food and medical supplies—while the sector’s tight margins make it difficult to pass these increases onto consumers.
Many care homes rely on local authority funding, which frequently falls short of covering the true cost of care, creating an unsustainable financial gap. Meanwhile, shareholder expectations for dividends persist even in difficult economic conditions, further straining resources.
Ultimately, successive governments’ failure to adequately address systemic issues in social care has left the sector underfunded and ill-equipped to manage the growing demands of an ageing population.
How to manage financial pressures
While the challenges facing the care home sector are daunting, businesses can take proactive steps to mitigate financial pressures and avoid insolvency.
Maintaining robust financial oversight is crucial, with regularly updated management accounts and projections giving directors a clear view of their company’s position. This transparency allows for informed deci-
sion-making and early identification of risks. Refinancing debt can also help reduce borrowing costs and ease the burden of high-interest loans.
Staff retention is a challenge for the sector as a whole, but engaging with employees, addressing concerns, and offering training or career development opportunities can reduce turnover. It is more costly to recruit than to retain staff, so investment in wellbeing and retention helps mitigate staff shortages and expensive temporary staff.
Managing shareholder expectations is equally important, with open communication helping balance operational priorities and financial sustainability. Where feasible, care homes should review pricing structures to offset increased costs while maintaining transparency with residents and families.
Engaging with policymakers, such as local MPs, and advocating for greater government support is also crucial. Whilst it’s not an overnight fix, the care home sector needs systemic change to ensure long-term viability, and operators must be vocal about challenges to drive government action.
Steps to take when facing insolvency
When insolvency becomes a possibility, businesses must act swiftly and responsibly to protect creditors and stakeholders.
Seeking professional advice at the earliest sign of financial distress is crucial, as insolvency experts can provide tailored guidance and explore potential solutions to avoid or manage the situation effectively.
Companies should also avoid incurring new liabilities that they may struggle to meet, as this prevents further financial deterioration and demonstrates responsible leadership.
Additionally, directors have a legal obligation to prioritise creditors over shareholders in times of financial difficulty, reducing the risk of personal liability and increasing the chances of a fair resolution for all parties involved.
Practical steps to avoid insolvency
With timely action and the right support, care homes may be able to avoid insolvency altogether.
Seeking advice at an early stage is key here, as this improves the chances of achieving a better outcome for stakeholders. Proactive measures allow businesses to explore all available options and minimise the impact of financial distress.
Obtaining early professional advice can assist in avoiding action by creditors and it may be possible to obtain a moratorium to take away the pressure from immediate debt collection attempts.
Engaging with creditors with open and honest communication will also ensure a better outcome. Creditors may negotiate on payment terms or temporary relief if they’re engaged early, buying time for businesses to stabilise their finances.
The care home sector is facing unprecedented financial challenges. However, by maintaining financial visibility, engaging with key stakeholders, and seeking professional advice when necessary, businesses can improve their resilience and ensure the continued provision of vital care services. As the sector waits for meaningful government action, it is up to individual operators to weather the storm and protect the future of care.
The focus week this year, starts on Monday 17th March and runs until Sunday 23rd March. These are challenging times for health and social care BUT Nutrition and Hydration Week provides an opportunity to highlight the good work taking place through the delivery of quality food and drink for the people these services care for. This is the annual platform to share and highlight information and initiatives, through sharing initiatives and projects, it allows others to learn and develop their own tailored information, plus for those sharing it is the chance to see other projects and ideas and further enhance theirs.
The initiatives that are shared also provide a weekly focus throughout the year on the Nutrition and Hydration Week social media platforms on X and Facebook, as a Tip of the Week or during the Thirsty Thursday campaign which runs from the end of May until early July. Throughout October we share a daily tip to embed Mealtimes Matter including how to embed Protected Mealtimes.

During the week a host of activities will take place in the form of information stands; launch of new food and drink initiatives; daily themed food days; poster displays; themed
Social Care TV continue to fly the flag for highest quality online training for Health and Social Care, after unwavering commitment to excellence within the sector for over 25 years.
Their widely-used health and social care specific courses - produced and edited in-house - are expertly designed to make learning engaging, informative and, therefore, highly effective for learners.
Accredited by CPD and endorsed by Skills for Care, training with Social Care TV is quality assured, comprehensive and relevant.
As one of the leading online training providers in the health and social care sector in the UK, they supply training for local authorities, recruitment agencies, care home groups and other health and social care organisations.
Their feature-rich Manager platform has further been enhanced this year with the introduction of several new Manager tools designed to aid with compliance, reporting and trainee management. Features now available include:
• Compliance Dashboard with Traffic Light System
• Downloadable Trainee Matrix
• Custom Bundles
• Trainee Groups
• Bulk Uploads
drinks trollies; and for a lot of the week’s supporters the main event is the Global Afternoon Tea on the Wednesday 19th. The Global Afternoon Tea is an invitation for health and social care professionals around the world to join in and celebrate with that most British event an Afternoon Tea. Still looking for ideas and inspiration, then visit the websitehttps://nutritionandhydrationweek.co.uk ; and remember to follow Nutrition and Hydration on social media - X and Facebook.
The week has expanded beyond its health and social care roots and is now utilised for staff well being in a myriad of organisations who see the benefit for their staff teams in access to fluids in particular during working hours. This is particularly pertinent for those organisations who workers work shifts, or remotely with limited access to food and drink during their working hours.
Since its inception, the ‘Week’ has become the primary focus for food and drink providers in social care to highlight their practices and this year, as always, we look forward to this continuing. It is amazing the work people do to enhance the nutrition and hydration provision for those they care for.

• Bulk Enrolment Onto Custom Bundles
• Course Enrolment Notifications
• Course Reminders
SCTV regularly release new and updated high-quality courses. Previews for all courses can be viewed at: Courses - Social Care TV (www.social-care.tv/courses/course-details)
To enhance their learners' experience further they have created free, comprehensive subject-specific workbooks which were rolled out across all courses this year. This unique addition provides excellent value and a fully robust training package.
SCTV are delighted to have won several awards over the last 12 months including:
– Global
• Best Online Health and Social Care Learning Platform’
Health & Pharma Social Care Awards 2024
• ‘CPD Provider of the Year’ – The CPD Awards
• Social Care Training Provider of the Year’ - Corporate Livewire
Innovation & Excellence Awards
Gold standard customer service remains a core staple of the business, with expert support and guidance provided via telephone, email and live chat. They place great importance on the training and development of their customer services team to ensure that they continue
to provide a personal, friendly and knowledgeable service.
Their much-loved ‘Care Worker of the Month’ award recognises and rewards the selfless dedication shown by care workers across the UK and they proudly support the Care Workers Charity who aim to advance the financial, professional and mental wellbeing of social care workers.
SCTV believe that high quality training should be accessible to all and offer regular, free courses which include a digital certificate accessible via their website.
The company stands behind a clear mission and set of values which define their ethos and their dedication to both the Care Sector and those within it. These can be viewed at: Mission Statement and Core Values - Social Care TV
(www.social-care.tv/about/mission-statement-and-core-values)
Social Care TV are a responsible business, committed to ensuring that their actions have a positive impact on their employees, customers, the wider health and social care community and the environment.
Above all, SCTV consistently strive to make a meaningful contribution to the wellbeing of those being cared for.
For more information please see: Homepage - Social Care TV (www.social-care.tv) and see advert on the facing page.
More than £69 billion in funding for England’s councilshas been confirmed as the government delivers on its commitment to restore trust and stability in public services, with the final local government finance settlement for 2025 to 2026 making available up to £3.7 billion in additional funding for social care authorities.
Following the provisional Settlement in December, the final Settlement providesa 6.8% in cash terms increase in councils’ Core Spending Power compared to 2024-25. With increased demand and running costs rising, this money is a lifeline and will guarantee no council sees a decrease in their Core Spending Power.
With families across the country relying on crucial council services such as social care, the government is to provide up to £3.7 billion additional funding to social care authorities which they say will deliver this.
The settlement also includes an £880 million uplift to the Social Care Grant, compared to 2024-25.

A new £270 million Children’s Social Care Prevention Grant will support the national roll out of vital family help, keeping children safe and ensuring they get the best start in life as set out in the Plan for Change.
The £60 million has also been confirmed to fund long-term improvements to the local government sector over the next year, including empowering mayoral areas leading the devolution revolution in delivering local priorities and supporting councils’ financial reporting with a fit and legal audit system to ensure transparency.
Deputy Prime Minister, Angela Rayner said:
“Councils deliver vital services across the country – driving growth and local economies and providing a lifeline for those that need it most. “
“Through our Plan for Change we are determined to fix the foundations of local government; investing where it is needed, trusting local leaders and working together to deliver growth, better health and social care services and the affordable homes people need.”
This final Settlement marks an important step towards a government focused on efficiency, value-formoney and a community first approach. For the first time, a new £600 million Recovery Grant will help support places most in need, which maximises public spending to ensure it delivers more meaningful outcomes.
The sector is already having its say via an open consultation on how to best streamline the outdated funding model and distribute taxpayer’s money more fairly, based on an updated assessment of need, enabling every council to deliver high quality services to their communities.
As part of handing local leaders more power and control of their funding, the government will end out-
dated processes and bureaucracy of bidding for different funding pots and bring forward the first multi-year settlement in a decade in 2026-27 to provide certainty and economic security to councils setting budgets.
The provisional settlement consultation was open for 4 weeks and closed on 15 January 2024.
Cllr Barry Lewis, Finance Spokesperson for the County Councils Network, said:
“Today’s final Local Government Finance Settlement will be a disappointing one for the majority of county and unitary councils, and sets up a difficult twelve months for those authorities. With the government choosing to heavily target its £600m ‘Recovery Fund’ to local authorities covering major cities and towns at the expense of county areas, just 3% of this grant will go to County Councils Network (CCN) councils.”
“Compounding this is the increase in the National Living Wage and employers’ National Insurance, with the costs of these policies outweighing any additional funds made available in this finance settlement for county and unitary councils.”
“Consequently, more than four in five CCN members say they are in a worse position than before the Autumn Budget and this finance settlement, and one third say their service reductions next year will now be severe. Considering there is very little fat left to cut from many of these services already, a further reduction will have a material impact on our residents.”
“It is important that decisions made in the finance settlement and the manner in which they have been made does not set a precedent ahead of the upcoming fair funding review. There has been nothing published so far that backs up ministers’ decisions to target funding so specifically by exclusively using deprivation within the funding formula, so it is imperative the fair funding review is carried out transparently.
“Whilst deprivation is a reason some councils’ costs are high, it is not the sole reason. The CCN’s evidence shows that demand and market failure across adult and children’s social care and special educational needs services are the main reasons as to why councils across all four corners of the country are struggling. If the trend of this finance settlement does continue, the government will completely understate the very real financial pressures faced by councils outside of towns and cities and it will push many county and unitary councils to the brink.
“The Local Government Secretary’s written statement today also references ending the ‘two-tier’ premium paid by taxpayers in county areas, and mending this broken system. If the government is to achieve its aim of streamlining local government, reform must be at the correct scale to make a difference to public services and to generate efficiency savings. That means building on the principle of new unitary councils covering populations of 500,000 people or more.”



As financial pressures mount and regulatory demands grow, care providers face an increasingly fragile operating environment. Workforce shortages, rising costs, including changes to Employers’ National Insurance Contributions, and the everevolving compliance landscape are stretching the adult social care sector to its limits.
Against this backdrop, Care England has commissioned Cornerstone Care Solutions to produce a series of reports under the Restructuring Social Care Services initiative. This series examines the underlying causes of care home failures and presents proactive strategies to ensure long-term sustainability.
The latest report in the series, Identifying and Addressing Failing Care: A Guide for Care Home Professionals, explores how clinical and financial Key Performance Indicators (KPIs) can serve as critical early warning signs, helping providers identify emerging risks before they escalate. By closely monitoring trends such as infection rates, occupancy levels, and financial performance, care home
leaders can intervene swiftly to prevent small challenges from becoming systemic failures.
Professor Martin Green OBE, Chief Executive of Care England, commented:
“Care providers are operating under relentless financial and workforce pressures, and the margin for error is vanishingly small. Without a clear view of the warning signs, services can quickly become unsustainable, putting both residents and staff at risk. This report highlights the importance of tracking clinical and financial KPIs, not as a bureaucratic exercise, but as a crucial safeguard for quality care. The ability to spot issues early, whether it’s a rise in falls, a drop in occupancy, or creeping financial instability, can make all the difference between survival and closure. In such a challenging climate, we need to move away from reactive firefighting and towards a smarter, more strategic approach to running care services.”
This second report builds on the first in the Restructuring Social Care Services series, which examined financial viability, workforce stability, and operational efficiency. Now, the focus shifts to embedding a culture of continuous improvement through data-driven decision-making.
To explore these findings further, Care England will host a webinar on 4 March 2025, offering practical guidance on using KPIs to safeguard care homes. To register, click here
By Nicola Smyrl, partner at Taylor Walton Solicitors

The topic of adult social care has not been far from the headlines in recent months. Wes Streeting, the current Health Secretary has stated that the social care system is failing. He has highlighted that this issue is responsible for creating more pressure on the NHS. In November 2024, more than 12,400 hospital patients a day were well enough to leave but had to stay overnight, and one in three of these delays were due to lack of available social care.
The Government has therefore made quality social care a priority. In doing so, it has acknowledged that recruitment and retention of appropriate staff to provide adult social care has historically been a problem, and that this needs to be addressed if social care is to improve. In its recent fact sheet setting out further details of its plans the Government states: “The sector is characterised by weak domestic recruitment and high turnover, with growth in staff levels driven by international recruitment in recent years. Alongside other factors, evidence shows that low pay and poor terms and conditions affect domestic recruitment and retention.”
FAIR PAY AGREEMENTS
The Employment Rights Bill was published late last year, setting out details of how the Government will implement its plan to “Make Work Pay”. The Bill includes specific provisions on the adult social care sector. The Government intends to establish an Adult Social Care Negotiating Body that would be responsible for facilitating negotiations on a "Fair Pay Agreement" specifically for the adult social care sector. The intention is for the Negotiating Body to be made up of representatives from employers and trade unions, who will agree minimum standards for pay, conditions and training within the sector. Under the Bill, where ministers are in agreement with the Body’s proposals, further regulations ratifying them can be made, meaning the agreements would be binding on adult social care employers in England and would need to be reflected in workers’ contracts. The new standards would be enforceable in a similar way as current minimum wage legislation is, with such enforcement being the function of a new Fair Work Agency. Where ministers are not in agreement with the Body’s proposal, they can require the Body to reconsider matters, meaning the Government will retain significant control of how the negotiations con-
clude.
Whilst the objective of a Fair Pay Agreement is to improve terms and conditions in the sector, hopefully enabling employers to attract and retain high quality staff, many employers are concerned about how they will manage increased employment costs in practice. With local authorities responsible for picking up the costs of a significant amount of adult social care, this may limit the ability of providers to increase fees, leading to a reduction in care standards. The Government’s own impact assessment of the proposals acknowledges that many small providers may be forced out of the market altogether. Professor Martin Green OBE, Chief Executive of Care England neatly summarises this point when he says: “any increase in employment costs could significantly jeopardise the ability to provide care to those in greatest need...We must ensure that this legislation is adequately funded to protect both our workforce and the vulnerable individuals they serve.”
As well as fair pay agreements which are specific to the adult social care sector, employers in the sector will have to plan for other changes in the Employment Rights Bill applicable to all employers.
An area which is likely to have a significant impact on care providers is proposed changes to zero hours contracts, it is estimated that around a quarter of the workforce in social care is engaged on this basis.
Whilst there will be no outright ban on the use of zero hours contracts, employers will be required to make an offer of guaranteed hours to a qualifying worker at the end of every reference period, anticipated to be 12 weeks. A qualifying worker will include workers engaged on a zero hours contract and those with a low number of guaranteed hours. What amounts to “low hours” is not yet clear.
Employers will also be required to provide reasonable notice of shifts and changes to shifts. Compensation will be payable where changes are made at short notice.
It is possible that under these new rules, employers will end up with too many staff. In that case, redundancies may be needed. This will need to be carefully managed as the right to claim unfair dismissal will apply from day one.
PREPARE NOW
The changes are not expected to come into force until 2026 – businesses should start thinking about how the changes will affect their workforce and mitigating the impact. This might include assessing how the business would manage if wages for care workers increase by certain amounts, looking at potential costs saving measures and conducting an audit of the workforce to ascertain how the business may be affected by the proposed new rules on zero hours contracts and unfair dismissal.
Taking steps now to assess how the changes will impact your business will mean that you are better prepared as and when further details of the changes become available.
This winter, Recreo VR is offering care homes an exciting opportunity to enhance resident wellbeing through the power of Virtual Reality (VR). By signing up for one of our 24-month Recreo Theatres packages, you’ll receive a free VR headset and staff training.
Our platform provides person-centred, budget-friendly activities that are fun, engaging, and accessible, especially for residents who are bedbound or socially isolated. Co-created with Alzheimer’s Society and individuals with dementia, our service empowers staff to deliver personalised reminiscence and one-to-one sessions that promote memory recall and connection.
Our VR headsets have been recognised as good practice by the Care Quality
Commission (CQC), further validating their impact on care. Regular use of Recreo VR has a proven positive effect on wellbeing, with residents reporting increased activity, engagement, and social connection, often leading to a reduction in the need for PRN medication.
Whether combating loneliness, promoting relaxation, or enhancing cognitive health, VR offers a non-pharmacological solution to enrich care and elevate quality of life. Don’t miss out! Take advantage of this exclusive offer and see how VR can transform your care home experience.
For more information, visit recreovr.co.uk. Or contact us at info@recreovr.co.uk or 01482 526940.



The care sector is no stranger to challenges. With an aging population, increasing demand for services, and financial pressures, care providers are constantly battling to stay ahead. Add to this the need for positive public perception in a media environment often fixated on crises, and it’s clear that strong communication isn’t just a nice-tohave—it’s essential. That’s where DAPS Agency Ltd comes in, a specialist communications agency helping care organizations navigate these turbulent waters and emerge stronger.
UNDERSTANDING THE CARE SECTOR’S UNIQUE CHALLENGES
DAPS Agency is no ordinary PR outfit. Founded by seasoned communications professionals Anneli Lort and Firgas Esack, the agency has carved out a niche for itself by understanding the unique hurdles faced by care providers, from technology innovators to care home operators.
“The care sector is about more than delivering services; it’s about creating meaningful experiences for residents, building trust with families, and supporting staff,” says Anneli Lort, co-founder of DAPS. “But these stories often get buried under the day-to-day pressures providers face.”
One of the biggest hurdles for care organizations, whether they’re home groups or care technology suppliers, is visibility. With so many competing voices in the sector, standing out is no easy feat. Providers need to balance the operational challenges of driving occupancy and adapting to new technologies while maintaining strong relationships with stakeholders. According to Firgas Esack, this is where targeted and tailored communications can make all the difference.
“Visibility is critical,” Esack explains. “We help care providers showcase their unique strengths, whether it’s innovative resident care programs or cutting-edge technology that’s changing how the sector operates. Our aim is to make sure their voices are heard where it matters most.”
PUTTING CARE PROVIDERS IN THE SPOTLIGHT
DAPS excels at elevating their clients’ profiles by crafting narratives that resonate. Whether it’s securing positive press coverage or positioning an organization as a thought leader through white papers and industry commentary, the agency’s strategies are rooted in authenticity.
“Care home groups face enormous pressures to attract and retain residents while maintaining financial sustainability,” says Esack. “We’ve worked with clients to highlight innovative approaches they’ve taken to deliver high-quality care on a budget, securing media coverage that positions them as forward-thinking leaders.”
The team’s expertise isn’t limited to traditional care providers. In an industry increasingly driven by technology, DAPS has also helped care tech companies gain recognition for their solutions. From illustrating how a software tool is transforming care home operations to showcasing new assistive technologies that improve residents’ quality of life, DAPS knows how to translate technical innovation into stories that matter. TACKLING THE TOUGHEST ISSUES
The care sector is not without its share of crises—media scrutiny, financial difficulties, and regulatory challenges can arise at any moment. This is where DAPS’ experience in crisis communications comes into play. Having run global press offices and handled high-stakes issues for clients, the agency offers a steady hand when it’s needed most.
“When a crisis hits, it’s easy to feel overwhelmed,” says Lort. “Our role is to step in, take control, and guide our clients through the storm while safeguarding their reputation.”
Their work doesn’t just stop at damage control. Proactive thought leadership—opinion pieces, keynote speeches, and lobbying efforts—ensures that their clients are shaping the narrative, rather than simply reacting to it. By working closely with stakeholders, DAPS ensures that their clients’ voices are heard at both local and national levels.
What sets DAPS apart is its unashamedly remote working model. Lort and Esack believe this approach allows them to deliver exceptional results without the traditional overheads of a bricks-and-mortar agency.
“Every penny our clients spend goes toward achieving results,” says Lort. “And because our team is made up of senior professionals, clients know they’re always working with experts who understand the complexities of their sector.”
This lean, results-driven ethos has helped DAPS build a reputation as a trusted partner for care organizations of all sizes. Whether working with a large care home group or a niche technology provider, the agency’s approach is the same: tailored, proactive, and relentlessly focused on outcomes.
One of the most rewarding aspects of DAPS’ work is celebrating the positive stories that come out of the care sector. In an industry that’s often under scrutiny, shining a light on success stories is vital.
“Whether it’s a care home running an innovative intergenerational program or a technology provider making a measurable difference in residents’ lives, we make sure these stories get the attention they deserve,” says Esack. “We want to celebrate the people and innovations driving the sector forward.”
This focus on positivity isn’t just good PR; it’s also good for morale. Recognizing and sharing achievements boosts confidence within organizations and strengthens their reputation with external stakeholders.
As the care sector continues to evolve, the need for strategic, impactful communications will only grow. For care providers looking to amplify their voice, tackle challenges head-on, and secure their place as leaders in the sector, DAPS Agency offers the expertise and passion to make it happen.
“We’re here to tell the stories that matter,” says Lort. “The care sector does incredible work, often under tough circumstances, and it’s our job to make sure that work is seen, understood, and celebrated.”
In a sector where the stakes couldn’t be higher, DAPS is proving that the right communications partner can be transformative. Whether navigating a crisis, celebrating a success, or shaping the future of care, this dynamic agency is helping its clients rise to the occasion.
To book a free, no-obligation one hour consultation with DAPS to discuss your communications challenges and needs, go to daps.life/DAPS60 www.dapsagency.com
York now has a nursing home with specialist 24/7 care for people with complex dementia for the first time, following the opening of Wellen Court, Schoen Clinic York.
The home is based on Haxby Road and employs around 50 staff including dementia carers and specialists, chefs and catering staff, nurses, health care professionals and occupational therapists.
Adam Bloor, Clinical Director, said: “We would like Wellen Court to be a hub of the community supporting residents with complex dementia and their families and carers.
We want our service users to be as independent as possible with the flexibility to have support if they should need it.
Our service users are at the heart of everything we do.” Wellen Court supports those with complex dementia and its associated behaviours.
As well as privately funded patients, it welcomes local authority

The pobroll® is the invention of Pat O’Brien, a physiotherapist, Moving and Handling trainer, and Conflict Management tutor with over two decades of experience in care homes and nursing homes
Care home managers often face challenges in delivering intimate care while balancing efficiency and managing costs, particularly when these essential tasks provoke behaviours that can be challenging to safely manage. Traditional methods—especially for bed-bound residents—often lead to lengthy processes and frequent linen changes, driving up costs and consuming valuable staff time. The pobroll® provides a transformative solution that supports dignified care, achieves significant cost savings, and reduces the need for additional staffing.
The pobroll® is an innovative bed-bathing wrap specifically designed to enhance comfort and dignity during personal washing for individuals who require in-bed care. Centred on the resident’s experience, it minimizes distress by providing sensory comfort. Crafted with two layers of high-quality cotton-terry toweling and a waterproof layer in between, it delivers a soothing, calming experience while keeping the bed completely dry. Sized for a standard single bed, the pobroll®’s dual-layer design offers warmth and a sense of security and privacy, allowing residents to maintain comfort and dignity during bed-based bathing routines.
BOOSTING COST SAVINGS AND OPERATIONAL EFFICIENCY

The pobroll®'s waterproof design enables caregivers to provide a complete wet wash without the risk of soaking the bed, minimising the need for frequent linen changes. This leads to fewer laundry loads, reducing labour and utility costs, as well as wear on linens. By reducing logistical tasks, caregivers have more time to focus on direct resident care, enhancing productivity overall. Additionally, reduced reliance on disposable wipes results in further cost savings and supports environmentally sustainable practices. With its durable, reusable design, the pobroll® maintains hygiene standards and allows for extended use across multiple residents. As care homes face increased pressure to adopt sustainable practices, the
referrals to ensure its specialist care services are accessible to everyone.
The environment is designed to be dementia-friendly, including low window sills and wide-opening doors. The smallest of details have been considered, even down to dementia-friendly crockery and cutlery sourced from specialist suppliers.
According to Alzheimer’s UK, 982,000 people are estimated to be living with dementia in the UK. By 2040, this figure is expected to rise to 1.4 million.
Adam added: “Our service to our residents is based around what they enjoy doing. There are no set visitor times, encouraging family and friends to come and spend as much time with their loved ones as they wish including children and pets, and they can do so in the privacy of one of our multi-purpose rooms if that suits best.”
pobroll® provides an effective solution that supports both economic and environmental goals.
Managing resident agitation—particularly for those with dementia—often requires specialised training in restraint techniques. The pobroll® significantly reduces the need for physical intervention by providing a warm, secure covering that alleviates resident distress. This gentle approach minimizes aggressive or defensive reactions, reducing the number of staff needed for these interactions. As a result, facilities can potentially lower staffing levels without compromising care quality, yielding substantial cost savings. Additionally, reduced dependence on physical intervention decreases training costs associated with restraint techniques. By simplifying the process of intimate care, the pobroll® reduces the need for specialised training, making onboarding smoother and lowering turnover-related training expenses.
The pobroll® supports compliance with restraint reduction guidelines, helping facilities minimise documentation burdens and regulatory liabilities linked to physical interventions. This non-invasive solution improves safety for both residents and caregivers, fostering a culture of dignity and respect that boosts satisfaction among residents and their families.
CONCLUSION: A VALUABLE ASSET FOR QUALITY CARE AND COST MANAGEMENT
For care homes, the pobroll® represents a strategic investment, offering measurable savings by reducing reliance on disposable products, lowering laundry and training costs, and enabling efficient staffing. Most importantly, it prioritises resident dignity and comfort, setting a high standard for compassionate, personcentred care. For facilities seeking to enhance financial performance and care quality, the pobroll® is an invaluable addition to their resources.
Fof further information, see the advert on the facing page.

With costs set to rise by up to 54% from April 2025 – and of up to 70% by 2028 – Care England is drawing on the successes of its historic energy tender and launching a National Water Tender to cut water costs so providers can stay afloat.
Professor Martin Green OBE, Chief Executive of Care England, said: “These relentless cost increases are placing unbearable strain on care providers. They’re already battling rising National Insurance costs, soaring energy bills, and wider cost-of-living pressures. Now, with water bills set to skyrocket, the financial viability of many care services is at further risk. This isn’t just about business expenses; it’s about ensuring that care providers can continue delivering the high-quality support that vulnerable people rely on every day.”
Care England is determined to turn the tide. Following the success of its Energy Tender – which
has saved millions of pounds for care providers – the National Water Tender will harness collective purchasing power to again negotiate better deals and protect providers from excessive price hikes.
Professor Martin Green OBE continued: “Our Energy Tender has been a gamechanger, proving that when care providers come together, they can secure better deals. Now, we’re applying the same approach to water to combat excessive increases about to his the sector. Keeping costs manageable is crucial for care providers to remain sustainable and continue supporting those who rely on them. Many are already stretched to their limits, and without action, rising costs will mean that many may not be able to continue operating. We are committed to standing with them, securing fairer deals and ensuring they have the resources to keep delivering high-quality care.”
While the Care England National Water Tender will provide much-needed relief, it is only part of the solution. We are calling on the government to recognise the urgent need for financial support and meaningful intervention to stabilise the sector. Without action, these escalating costs will push many care providers to the brink, threatening the future of social care in England.
For more information on the National Water Tender and how to get involved, visit: Care England National Water Tender.

Whatever the reasons for funding reform intransigence, it has now brought the sector to a tipping point.
By Simon Spiller, a former care home owner and social care commentator.

Social care operators are angry that latest Government review into social care in England is to take three years to report when the sector's crisis is coming to a head after three decades of chronic underfunding of state-funded care for the disabled and elderly. They can’t comprehend why the critical care needs of those they care for are being pushed into the long grass, once again. Yet, this decision is entirely in keeping with a pattern of past Government antipathy towards social care and it seems Labour isn’t concerned about potentially making matters worse.
The decision by the Chancellor to impose Employers National Insurance on social care providers, while exempting NHS employers, feels like the final straw for many social care operators struggling to make ends meet. Surveys by various sector representative bodies suggest between 20 and 30% of care operators will be handing back their local authority contracts, or shut up shop entirely. This is particularly the case for Home Care providers, who operate on much tighter margins than care homes.
This new financial pressure has caused some of the 17,000 social care providers in England to take unprecedented steps, including clubbing together in order to put pressure on the Government. One such initiative is #ProvidersUnite, which is organising a march on Westminster, petitions, potential legal cases and other actions to try and force the Government to U-turn and exempt social care employers from the ENI increase and move much faster than the Casey review to implement funding reform. But the Government is so far immune to this pressure and appears unlikely to deviate from their plans. Like successive Governments, Labour is ambivalent to the social care crisis. Those being hit hardest, according to Age UK, are the millions of people in England unable to get Government funded care. This includes 2.6 million people over 50 on care waiting lists and 5 million unpaid family members caring for loved ones without sufficient professional support - often having to sacrifice work to do so. Funding tradeoffs are always required when Government purse strings have to be pulled tight, but why is social care never on the list of priorities?
Three explanations for this long term Government intransigence come to mind. The first, arguing that Governments haven’t understood the extent of the funding crisis, just doesn’t hold water. There have been 25 social care commissions and reviews over the last three decades. All concluded that social care is significantly underfunded. The Government’s own policy documents describe the extent of the problem and Wes Streeting, Health and Social Care Secretary, has made it very clear he believes the social care system as currently in a pressing crisis.
The second rationale that the system is “just too hard and expensive to fix” has often been touted by Governments as the reason they need to conduct a review, or Commission. The announcement of these reviews then becomes an action that politicians point at as their plausible reason for why nothing is being done immediately. In the recent past, these announcements feel like a hollow explanation when the figures needed to ensure that publicly funded social care provision delivers good quality care are not exorbitant. The 2003 Dilnot Commission Report was an exception. It did have expensive recommendations because the focus was on protecting the financial resources of the middle classes with a cap on care costs if individuals didn’t qualify for Local Authority funding. But that wasn’t a funding solution for the publicly funded care sector.
The Government’s Health and Social Care Select Committee has quantified the amount of additional funds needed by the sector to meet the current and future care needs of the elderly and disabled. When it was led by Jeremy Hunt MP the amount sat at £7 Billion per annum. The Health Foundation's latest assessment of the sector estimates underfunding at circa £8 Billion per annum. This represents a drop in the
ocean compared to the regular funding boosts actually received by the NHS each year, the latest being £25 Billion.
We can all speculate on the legitimacy of these two reasons. But, ultimately, this ongoing intransigence comes down to a lack of political will to fix the system. MPs will often say they receive more complaints about pot holes than social care shortcomings. Maybe if the disabled and vulnerable had more representation to MPs by their families, carers and social care providers, the Government would start to pay attention. But that hasn’t yet happened. Social care in England is a market of over 17,000 employers, dominated by independent SMEs, and at least 30 representative bodies - whose role it is to advocate for the needs of providers and those they care for. Regrettably, this highly fragmented representation has enabled Governments to side step the need for better funding in the sector - unlike the case with pay demands of train drivers, junior doctors and nurses, all represented by Unions.
Cynics will say the lack of political will can be attributed to an underlying ageism, pervasive across society and mirrored in our political classes. This may well be the case. Others say that because most publicly funded social care is delivered through Local Authorities, therefore Central Government has an arms length relationship with the sector and doesn’t really feel the pain associated with funding inaction. Why act when you can blame Local Government for the problems? Or perhaps Governments are gun shy over the issue after past efforts to transform funding have been pilloried by political opponents and the media, like Theresa May’s "Dementia Tax."
More recently, with the arrival of a Labour Government, there's speculation within the social care sector that the Government has a deliberate desire to let the care system fail in order to ease implementation of a publicly provided “National Care Service” that doesn’t line the pockets of private providers. Over 85% of social care provision in England currently comes from private, for profit, providers. Most charity and Local Authority care homes and home care services buckled a long time ago - under the pressure of under funding. There’s also speculation that Labour wants social care to be provided by a smaller number of larger providers. In which case, some degree of short term sector failure is necessary to help force the desired consolidation of providers.
Whether deliberate, inadvertent or somewhere in between, the reasons for funding reform intransigence by successive Governments have now brought the sector to a tipping point. With 30% annual care staff turnover and skilled immigration no longer filling those gaps, the sector’s ability to bounce back once Baroness Casey eventually delivers a report will be compromised - there simply won’t be enough staff. It’s almost impossible to attract staff into the sector and the Government's intended “Fair pay deal for care workers” will be too little too late. Parallels with the construction industry are worth noting. Government targets to build half a million homes each year are expected to be held back by a lack of skills in the sector - there simply aren’t enough bricklayers and carpenters to build the houses. By the time any Government has decided to finally address their social care funding shortfalls - it's unlikely there will be sufficient carers to deliver the required care support for an ageing population.
Finding people with a genuine aptitude for care is never easy, and training them to deliver high quality care, whether in people’s homes or care homes, will take years. In the interim, more family members will be taken out of the workforce to care for their loved ones. Recent headlines about the plight of “sandwich carers”, those in their 30s and 40s looking after children and parents, will become more prevalent. While the economy will suffer as a result of labour shortages.
Much with the housing crisis, those with wealth will never suffer. Indeed, the minority segment of social care operators supporting people with resources to pay for their own care is growing, with profit margins increasing. Retired politicians fall into this category. Their generous pensions will pay for their care for as long as they need it. It’s the majority of the rest of the population who will need to rely completely, or partially, on the state to fund their care, and who will be left to rely on their families, or linger in hospitals when they are medically fit to leave.
Irrespective of the reasons for neglecting the sector, if campaigners, advocates and voters are unable to convince the Government to prioritise immediate funding increases for the social care sector, the prognosis for our vulnerable, their families as well as the implications for the economy are not good.
The Cleaning Show 2025 will return from 18-20 March at ExCeL, London, with industry leaders set to tackle the cleaning and hygiene industry’s biggest challenges in this year’s Conference programme. The 2025 theatre will see expert speakers from across the sector sharing insights on pressing topics from sustainability, education and workforce development to technological advancements and future preparedness.
SUSTAINABILITY: DRIVING CHANGE FOR A GREENER FUTURE
Sustainability remains a top priority for businesses, consumers and regulators alike. The Cleaning Show 2025 will dedicate several sessions to exploring innovative solutions and practices to help the sector reduce its environmental footprint. Attendees will gain valuable insights into the practical steps required for compliance and the long-term benefits of adopting sustainable practices.
Education and development: building the workforce of tomorrow

Recruitment, education and training remain pivotal for the growth and resilience of the cleaning and hygiene industry. This year’s programme will address the challenges of attracting and retaining talent and the importance of upskilling to meet future demands.
Delia Cannings, Chair of the British Cleaning Council (BCC), will open the show and announce the launch of a new website called the UK Cleaning Career Development Zone, a significant new initiative which will bring training and career development information from across the cleaning and hygiene industry sector together into one easily-accessible place, for the first time.
The rise of artificial intelligence (AI) and technology presents transformative opportunities for the cleaning sector. Attendees will discover how these advancements can enhance productivity, efficiency and innovation in the sessions “AI in the Cleaning Sector – Change is a Fact… But How Do We Embrace It?” and “The Evolution of Cleaning in FM”.
As the world continues to navigate the aftermath of COVID-19, the conference will also examine how the cleaning industry can be ready for future challenges. In “Preparing for the Next Pandemic – Lessons Learned”, industry leaders including Neil Nixon, Conference Director of The Cleaning Show and Duncan Holdsworth, Head of Technical at GV Health, will reflect on the successes and shortcomings of the industry’s pandemic response and identify steps to improve resilience and readiness for potential future crises.
Paul Sweeney, Event Director of The Cleaning Show, said: "We’re proud to welcome the industry’s leading voices to the conference stage at The Cleaning Show this March. From tackling recruitment challenges and embracing sustainability, to keeping up with technological advancements, it’s vital for businesses to learn from experts and apply these insights to their operations. This year’s Conference will deliver practical strategies to address the key trends and opportunities shaping the sector, and we’re excited to showcase the latest innovations driving the future of the cleaning and hygiene industry."
For further information, please see the advert on page 11 or visit www.cleaningshow.co.uk/london


The latest UK Care Homes Trading Performance Review 2024 shows occupancy levels rising to 88.3%, a positive sign of market recovery. However, while this progress is encouraging, it reveals significant untapped potential in how care homes attract and convert prospective residents.
Presenting care homes effectively is not just about showcasing services—it's about creating emotional connection and trust. Families are making difficult decisions in emotionally charged situations, which requires a sophisticated approach to relationshipbuilding and conversion. Care homes are offering something no one truly wants to need, making the challenge even greater.
To truly drive sustainable occupancy growth, care homes must focus on transforming the customer journey—from raising awareness to handling enquiries and guiding families through to admissions. Many providers are still missing key opportunities. Too often, care homes fall short in delivering the basics well, leading to lost enquiries and missed revenue potential.
CRITICAL AREAS NEEDING IMPROVEMENT INCLUDE:
Generating Quality Leads: It's essential to attract the right audience from the outset through targeted campaigns, high-value content, and strategic outreach across multiple channels, including community outreach, digital marketing, partnerships, referral networks, local events, print ads, and door drops.
• Empathetic First Contact: Enquiries must be handled with care, expertise, and emotional sensitivity, recognising the difficult decisions families face.
Personalised Tours: Showrounds should go beyond listing services, highlighting quality of life benefits such as personalised care plans, engaging activities, and the warmth of community life.
By Ali Powell, CEO and Founder at
Clear Value Communication: Families need transparent, outcome-driven explanations of the value of care— focusing on dignity, well-being, and peace of mind, not just amenities.
• Consistent Post-Visit Engagement: Many care homes neglect follow-up strategies after visits, losing potential residents who may need further reassurance or time to decide.
TRACKING THE RIGHT METRICS:
To ensure the customer journey is effective, care homes should track key performance metrics, including: Monthly Lead Generation: Number of leads that meet predefined criteria indicating genuine interest or fit.
Monthly Visits: The number of on-site or virtual tours conducted within the month.
• Monthly Admissions: The total number of new residents admitted each month.
Lead Source Performance: Breakdown of leads by marketing channel (e.g., online ads, social media, referrals, events) to identify the most effective sources.
Average Admission Cycle Length: The average time from initial lead generation to a confirmed admission.
Monthly Marketing Spend: Total amount spent on marketing each month.
Website Traffic: Total visitors to the website and engagement rates for the month.
Social Media: Total followers and engagement on platforms like Facebook, LinkedIn, and Instagram.
THE OPPORTUNITY:
Investing in marketing and relationship-building efforts is not a luxury—it's essential. The cost per acquisition is often minimal compared to the hundreds of thousands in lifetime revenue generated from new residents. By focusing on consistency and excellence throughout the entire customer journey, care homes can significantly impact both occupancy rates and short- and long-term growth. The data is clear: doing the fundamentals well is not just good practice—it’s essential for both immediate results and lasting success. It’s time for care homes to move beyond filling rooms and start focusing on creating an inspiring customer journey that builds confidence, trust, and emotional connection with families.
If you need an expert in this area, contact Ali at Commercial Acceleration—specialists in strategy and implementation for transformational and turnaround results.
ali@comaccel.co.uk | comaccel.co.uk

Karuna Manor Care Home recently celebrated International LEGO Day by hosting a special event with children from Ghanshyam Nursery, bringing generations together through the joy of creativity, play, and social interaction.
The event highlighted the importance of intergenerational bonding and showcase how activities like LEGO building can foster meaningful relationships and mental stimulation for all participants.
The event featured engaging LEGO-building activities where residents and children collaborated on imaginative projects, fostering creativity and shared experiences. Through hands-on play, participants engaged in teamwork and storytelling, creating cherished memories in a warm and inclusive environment.
The activities planned included a collaborative LEGO city-building challenge, themed storytelling sessions, and free-building time where children and residents worked together to construct unique designs.
“At Karuna Manor, we believe in the power of community and the importance of meaningful interactions between generations,” said Ruth Kigaa, Home Manager at Karuna Manor Care Home. “LEGO is a fantastic way to encourage creativity and

connection, and we are thrilled to share this special occasion with the children from Ghanshyam Nursery. Seeing the joy that these interactions bring to our residents is truly heartwarming.”
Teachers from Ghanshyam Nursery also expressed their enthusiasm for the event. “Bringing our children to interact with the residents of Karuna Manor is a truly heartwarming experience. It teaches them empathy, patience, and the joy of shared creativity. LEGO provides the perfect medium for them to engage with the elderly, allowing both generations to learn and grow together,” said Mrs.Patel, a teacher at Ghanshyam Nursery.
Studies have shown that intergenerational activities like these can have profound benefits for both seniors and young children. Older adults experience improved mental health, reduced feelings of loneliness, and a greater sense of purpose when engaging with younger generations. Meanwhile, children develop social skills, empathy, and an appreciation for the wisdom and experiences of their elders. The International LEGO Day celebration at Karuna Manor Care Home is a perfect example of how simple activities can create powerful connections.
A leading care management software provider has launched ‘Customer Checklists,’ a new feature that helps make care processes simpler, more consistent and easier to follow.
The latest feature from PASS by everyLIFE helps care managers stay on top of important tasks, such as compliance checks, onboarding new clients and health monitoring – all in one place.
The checklist ensures that nothing is missed – if a task isn’t completed, carers get an automatic reminder so they can follow up. This helps keep care on track, reduces mistakes and gives carers more time to focus on the people they support instead of paperwork. Key benefits of the Customer Checklists tool, include: Easier onboarding – Helps new customers settle in smoothly by guiding care teams through every step, from first assessment to first visit. Better compliance – Makes sure important care plan reviews and tasks are completed on time, reducing the chance of anything being missed.
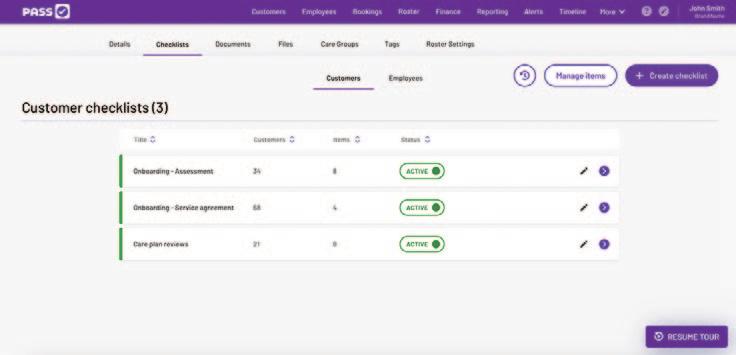
thing on track.
Duncan Campbell, Director of everyLIFE Technologies, said: "We’ve always been committed to putting people first in care. Customer Checklists is another way we’re helping care professionals with the tools they need to provide great, person-centred care. We believe this feature will make a real difference to the people they support.”
Founded in 2014, PASS by everyLIFE is a digital platform designed to make managing home care easier. PASS includes tools for care planning, tracking progress, mobile access and real-time communication, helping teams stay connected and organised. PASS is used by over 84,000 care professionals every day to help plan, manage and deliver care. Services using PASS are 37% more likely to receive an ‘Outstanding’ rating from the CQC compared to the national average,
Personalised care – Checklists can be customised for each person, ensuring their care meets their specific needs.
Clear team roles – Tasks can be assigned to the right

A team at University College London (UCL) has found a link between regular physical activity throughout life and changes in the brain which could help protect people from developing dementia. Understanding more about how exercise physically changes the brain could lead to new interventions that could stop it from happening in the first place.
The results are from Insight46, a study funded by Alzheimer’s Research UK and the Medical Research Council (MRC) which analyses health data collected from a unique group of volunteers from England, Scotland and Wales, born in the same week of 1946. Researchers have monitored the participants’ health throughout their lives as part of a larger, ongoing health study. Insight46 wants to see how the participants’ health across their lifetime is linked to their memory, thinking and physical brain changes in later life. The study, which began in 2015, has helped shape our understanding of how factors like heart health, education and head injury can affect the brain in old age.
Dr Sarah-Naomi James, based at the UCL Dementia Research Centre and MRC Unit for Lifelong Health and Ageing at UCL, leads on one arm of Insight46. Her team are exploring how being active could help a person become more ‘cognitively resilient’, or less likely to develop dementia. Previous studies have linked low physical activity to a higher dementia risk, but Dr James’ research begins to shed light on why this is the case.
Dr James’ team collected information on how active people were in their leisure time across 30 years, spanning before and after they turned 50. They were interested in whether people said they did activities
like sports, walking, or any other physical exercise for leisure, once a month or more.
The team then analysed brain scans taken when the participants were 70 years old, to see how physical changes in the brain were linked to their exercise habits throughout life.
Insight46 participants who reported regular exercise during leisure time before they were 50 years old tended to have a larger hippocampus, the part of the brain mainly responsible for memory. This area is often the first brain region affected in Alzheimer’s disease. Dr James’ team think that this could protect against memory loss, a symptom of dementia.
People who exercised throughout life were also less likely to experience cognitive decline, even if they had markers often seen in Alzheimer’s, such as build-up of the protein amyloid in the brain or brain shrinkage. Being active also appeared to help those with early Alzheimer’s disease markers to maintain and buffer their cognitive function, and this was particularly the case for women.
Dr James says: “Exercise is essential for keeping our brains healthy. But we are still building a picture around what physical changes happen in the brain to protect it against dementia.
“Insight46 has given us valuable clues to what changes are happening in the brain, opening new exciting research avenues.
“More work will be crucial to fully understand how exercise, and taking part in leisure activities throughout our lives, could be a powerful tool to protect people against dementia for as long as possible.”
Turning 100 is a remarkable milestone, and for Doris, it became even more special thanks to an outpouring of love from her community.
Doris’ 100th was a milestone celebration the team at Sweyne Court Care Home wanted to make special, so ahead of her big day, they shared an appeal on their Facebook page to get Doris 100 birthday cards!
The post immediately struck a chord with their Facebook followers, and their online community rallied to support them in their mission to get Doris a card for every year of her life. In total, the post was shared 69 times, reached over 14,000 people and found its way into the local paper, further supporting their ambitions.
With this kind of visibility in the community, birthday cards for Doris began to arrive in their numbers! It was exciting to see how many people took action to make Doris’ 100th, extra special!
On the day of her birthday, Doris couldn’t believe how many birthday cards were waiting for her. She questioned, “Are these all for me?”

Doris was in disbelief, but after learning about the popularity of the post the team shared online, she was excited to look through all of the cards and see who they were from. This included close family members, friends and team members at the home, but also people in the community with no connection to Doris; just a shared desire to wish her a very happy 100th birthday.
After counting all of the cards, the team revealed Doris had received a total of 200 birthday cards! She was overwhelmed with the support she had received and overcome with emotion seeing all of her cards lined up on a large table in the lounge.
Doris said, “I would like to thank everyone who sent me a birthday card, I was in shock and couldn’t believe how many kind people took the time to write me a card. It’s something I will never forget!”
This wonderful act of kindness made Doris’ 100th birthday an occasion to remember and showcased the power of community spirit!
The foundation of exceptional care home service lies in collaboration, efficiency, and reliability. For over a decade, Care Quality Pharmacy (CQP) has stood as a trusted partner for care homes across England, Scotland, and Wales. With a specialised approach to care home pharmacy services, CQP ensures residents receive timely and accurate medication, allowing carers to focus on what truly matters: quality time with their residents.
One of the most significant challenges for care homes is navigating missing or out-of-stock medications. CQP’s proactive system addresses this with precision. Their team checks prescriptions, liaises with GP services on behalf of the care home, and resolves discrepancies swiftly. Additionally, CQP’s access to national wholesale suppliers and long-standing relationships ensures a robust strategy for managing short supply issues, keeping residents’ needs a top priority.
Medication errors, often a stress point for staff, are almost eliminated thanks to CQP’s cutting-edge systems. Medications are picked using robotic technology, followed by a meticulous two-stage accuracy check by a pharmacist. This stringent robotic process has achieved an impressive error rate of less than two parts per million. Furthermore, integrations with market leading eMAR providers and coloured paper MAR entries are handled by CQP, reducing the administrative burden for care home teams. Timely delivery is another hallmark of CQP’s service. Monthly deliveries are scheduled up to six days in advance, and their teams ensure precision and dependability making the booking-in process hassle free. For urgent needs, a 4pm interim cut-off guarantees next-day delivery, including Saturdays. CQP’s commitment to care extends beyond medication. Their open communication lines, available seven

days a week, foster seamless interactions. Moreover, their Quality Assurance Team conducts annual face-to-face compliance audits, enhancing regulatory compliance and resident satisfaction. Added services, such as guidance on covert medicine administration and homely remedies advice, showcase their dedication to meeting every need.
Leading national care home partners trust CQP completely to manage pharmacy services across their entire estates. This unwavering confidence is a testament to the expertise, efficiency, and reliability that CQP brings to the table. Care homes also benefit from no-cost residential returns collection and free online medication training sessions. CQP supports staff development, ensuring a high standard of care using the CQP systems and processes.
By embracing the ethos of collaborative working, Care Quality Pharmacy sets the benchmark for care home pharmacy services. Their efficiency, responsiveness, and focus on compliance empower care homes to achieve the best outcomes for their residents. In an ever-demanding sector, CQP remains a steadfast partner, proving that the right support makes all the difference.
NHS prescription item dispensing data from October 2024 shows CQP to be the 6th largest distance selling pharmacy in England and therefore possibly making it the largest independent specialist care home pharmacy in the country.
Care Quality Pharmacy can be contacted by telephone on 0800 970 8844, online at cqpharmacy.co.uk/care or by contacting the National Partnerships Director, Patrick Bell directly at patrick@cqpharmacy.co.uk
National care home only pharmacy operating since 2011, based in the Midlands – serving England, Scotland and Wales.
Missing medication? Our team checks all your prescriptions for you and informs you of missing medication - huge time and cost saving to the home, freeing up your quality time with your residents.
Out of stock medication? We manage the entire short supply and out-of-stock medication process. Medication errors? Our resident order is picked by robots, then a 2 – stage independent accuracy check by pharmacists ensures you have the right medicine, on time, every time.
eMAR Integrations - Our systems work alongside all major eMAR providers
Are your deliveries on time? Our monthly deliveries are up to 6 days in advance, giving you plenty of time to book in medication. Saturday deliveries included.
Open Communication - One direct communications team, answering calls & responding to emails giving you one SLA for all of your homes.
Compliance - Quality Assurance Team – guaranteed face-to-face annual compliance audits. Consistency of service and delivery with audit trail.
We are Specialists in care home only dispensingDouble labels, Covert administration and Homely remedies advice.
Free Residential Returns Residential home’s returns are collected – no cost implications to you.
Free Medication Training – Both online and face-toface options available.
Become part of the care home pharmacy delivering excellence in medication management across the country.
References available on request.
To organise an introductory meeting please contact National Partnerships Director, Patrick Bell: Email: patrick@cqpharmacy.co.uk
As 2025 gets into full swing, the social care sector finds itself grappling with the lingering challenges of a difficult 2024. In response, Log my Care, the intuitive care management platform, has launched Shaping Social Care 2025, a new e-book full of expert perspectives and strategies to support the sector. This article by Mark Topps is an extract from the report, which features six additional chapters of predictions and advice from leading experts covering topics across legal, CQC, HR, complex care, and technology. When discussing efficiency, we often focus on time savings, which shifts our attention from evaluating existing processes. Additionally, we must consider our teams and those we support, balancing efficiency with quality. Here are practical strategies to achieve both.
A large part of social care involves administration, making it an ideal area for streamlining. However, social care often lags in adopting digital tools and AI. While technology isn’t a cure-all, it’s an accessible way to improve workflows without hefty costs.
Many providers already use Digital Care Planning systems, but are these systems being fully utilised? Often, key features are disabled during setup, integrations face challenges, and tools go unused due to limited training. Revisiting these systems and addressing gaps can unlock untapped efficiencies. Proper training can save time, reduce manual work, and allow teams to focus on high-quality care. Here are some strategies and tools to enhance efficiency:
● Digital Care Planning and EHR Integration: Integrating Digital Care Planning systems with electronic health records (EHRs) ensures quick access to essential information, improves accuracy, and reduces time spent on communication with healthcare professionals.
● Digital Rostering: Tools like Log my Care’s Rostering add-on simplify rota creation, optimise staff deployment, and align carers with service users’ needs, improving both efficiency and care quality.
● Process Mapping: Visualise workflows to identify inefficiencies and bot-
tlenecks. Regular updates ensure relevance and provide clarity for teams.
● Simplify Workflows: Eliminate redundant tasks and combine actions where possible. Streamlined workflows save time and reduce errors. These strategies help create efficient systems, allowing more focus on delivering quality care.
Time management is crucial for productivity and quality care. Investing in training and development can significantly enhance efficiency. Consider the following:
● Time Management Training: Tools like the Eisenhower Matrix help staff prioritise tasks based on urgency and importance, ensuring critical items are addressed promptly.
● Goal-Setting and Task Management: Training staff to set realistic goals, break projects into manageable steps, and establish achievable deadlines fosters accomplishment and reduces burnout.
● Continuous Learning: Encourage staff to stay updated on best practices and emerging technologies. This keeps teams engaged, skilled, and ready for challenges.
● System Reviews and Innovations: Regularly evaluate current systems and explore new technologies to identify tools that enhance both efficiency and care quality.
Investing in these areas builds a proactive, capable team ready to meet the demands of modern social care.
While most claim to deliver person-centred care, it’s worth reflecting on whether unique needs are genuinely met. Consider the following:
● Reflect on Care Delivery: Imagine care without constraints like cost or staffing—what would you change? Use these insights to identify actionable steps, such as adopting new technology, reviewing care plans more frequently, or increasing staffing levels.
● Feedback Utilisation: Evaluate how feedback is gathered, analysed,
and acted upon. Effective systems not only highlight improvements but also show service users and staff their input is valued.
● Rethink Staffing Ratios and Rostering: Analyse staffing data to identify needs and explore different shift patterns or task-sharing opportunities. Involving staff in this process can lead to innovative solutions that enhance care and efficiency.
By reflecting, gathering feedback, and actively involving your team, you build a foundation for continuous improvement.
TEAM COLLABORATION AND COMMUNICATION
Streamlining communication is critical for operational efficiency:
● Consolidate Communication Tools: Using multiple systems can cause confusion and duplication. Centralising tools enhances coordination and reduces administrative burdens.
● Optimise Meetings: Regular, focused meetings with clear objectives are more effective than broad, infrequent gatherings. Purpose-specific meetings foster engagement and clarity.
● Collaborative Culture: Streamlined communication and purposeful meetings build trust and morale, empowering teams to work together effectively. This enhances processes and ensures exceptional personcentred care.
Efficiency in social care goes beyond saving time—it’s about maximising resources, eliminating unnecessary tasks, and streamlining processes.
The ultimate goal is improving outcomes for the people we support. By fostering collaboration, leveraging technology, and focusing on quality, we can create a system that balances efficiency and care excellence.
Scan the QR code to read the full ebook for free

Dave and Sue Jones, who are residents of Nayland House care home in Colchester, are celebrating an incredible 65 years together this Valentine’s Day.
They met in Brightlingsea on the Essex coast while in their early twenties and started dating, enjoying evenings at the cinema, dances at the village hall and visits to the local pub.
The couple married on 3rd September 1960 and honeymooned in Knaresborough, Yorkshire, where they returned year after year for holidays –subsequently with their three sons. As the boys grew older, Dave and Sue explored locations they had once only dreamed of, travelling the world together.
When the time came to think of downsizing and planning for their retire-
ment years, Dave and Sue knew they could never bear to be parted, so they decided to move into a care home together, becoming residents of Nayland House in September 2024.
“These days we find joy in the little things,” said Dave. “Joining in with activities, sharing stories with our fellow residents and cherishing each other’s company as we always have.”
This Valentine’s Day, after 65 happy years together, Dave and Sue, together with staff and residents at Nayland House, as well as friends and family, are celebrating their life of devotion and love together.
“The world may have changed around us,” said Sue, “but our love remains as steady and true as ever.”


Residents at Silvanna Court Care Home, part of the Runwood Homes Group, have proven that nothing is impossible, as they took part in a series of exciting and ambitious activities throughout January. The 'Join in January' initiative aimed to encourage residents to stay active and push their boundaries, showing that age and mobility are no barriers to adventure. From wheelchair ice skating at Chelmsford Ice Rink to swimming and gym sessions in Wickford, rock climbing at The Rock Hub in Basildon, and even a cycling challenge covering the 930 miles from Land’s End to John O’Groats, the residents of Silvanna Court took on challenges many never thought possible.
Louise, Deputy Manager of Silvanna Court, praised the residents for their enthusiasm. "We want our residents to live fulfilled and contented lives, participating in activities that enhance both their physical and emotional well-being. Our team worked tirelessly to find accessible and inclusive opportunities for everyone."
The initiative received overwhelming support from residents and their families. Valarie, a resident who participated in wheelchair ice skating, described the experience as "magical," saying, "I felt like I was flying." Andy, another resident who took part in the swimming sessions, shared, "I never thought I would be able to do this again." Sheila, who bravely attempted rock climbing, expressed disbelief at her achievement: "I can't
believe I actually did it. I managed to get so high!"
Families of the residents were equally amazed. One relative, Lynne, remarked, "What other care home does this?" while another, Jan, added, "We can't imagine any other care home doing this with their residents. It's incredible!"
The atmosphere throughout the month was one of excitement and positivity, with both residents and staff eager to complete their challenges. "The staff are as mad as a box of frogs, but that’s what gives Silvanna Court its character, we love it," joked family member Trudy, reflecting the fun and engaging environment fostered at Silvanna Court.

This initiative was the result of collaborative effort between residents and staff, who held meetings to brainstorm activities. The home’s wellbeing team went above and beyond to make these activities possible, dedicating personal time to arranging and coordinating each event.
The success of 'Join in January' highlights the innovative approach Silvanna Court takes in creating meaningful experiences for its residents. With the overwhelming positive response, the care home is now looking forward to planning even more adventurous activities in the future.
The message from Silvanna Court is clear: age is just a number, and anything is possible with the right support and determination.
Wandsworth Common Care Home hosted the National Executive Meeting of the National Association of Care Catering (NACC) on 5th and 6th February 2025.
This prestigious event brought together key industry leaders, experts, and practitioners to discuss ways to raise standards in care catering and enhance its profile across the sector.
Over the two days, attendees engaged in discussions, workshops, and presentations at the Avery Healthcare-owned care home, focused on shaping the future of care catering in the UK.
The event encouraged collaboration and innovation, offering delegates a chance to share insights on care improvements and network while enjoying Wandsworth Common Care Home’s high hospitality standards.
The new Head Chef Tom Nurse, and Sous Chef Krunoslav Konc, working with Hospitality Manager Desire Jackson, prepared creative and nutritious meals that were a highlight of the event.

Thomas Holden, General Manager of Wandsworth Common Care Home, reflected on the significance of the meeting, stating,
“It was a privilege to welcome industry leaders to our home. We, like the NACC, are committed to improving care every day, and for me, that starts with staff well-being and development.”
He continued, “Our Head Chef will be among the first applicants for the Care Chef of the Year Awards,
showcasing his skills and passion for care catering.”
The meeting culminated in the official launch of the 25th Annual Care Chef of the Year Awards at the House of Lords.
This landmark event celebrated the achievements of care chefs across the UK and set the stage for a new chapter in the competition’s history.
The prestigious launch ceremony was attended by prominent figures, including Baroness Barker and Vic Raynor OBE, alongside representatives from major care providers and industry bodies.
Allan Brazier, NACC Treasurer and Avery Healthcare’s Director of Resident Experience, highlighted the competition’s ongoing importance, stating, “The NACC Care Chef Competition is the longest-standing event of its kind. This competition continues to set the benchmark for excellence in care catering.”
Avery Healthcare is proud to have had two past winners, Martin McKee in 2019 and Simon Lawrence in 2013.
Neel Radia, National Chair of the NACC, also expressed his appreciation for Avery Healthcare’s hospitality by adding, “Wandsworth Common Care Home’s hospitality was incredible, and the effort made to cater for all dietary needs was greatly appreciated. The passion for care and quality was truly inspiring.”
The Care Chef of the Year 2025 competition will focus on sustainability, creativity, and reducing food waste, with a £1,000 prize for the winner.
With the staff recruitment drive for Holsworthy’s Deer Park Nursing Home now in full swing ahead of the home’s opening later this year, operators Camelot Care have confirmed its management team is now complete with the appointment of both manager and deputy.
Amanda Williams has been selected as the home’s new deputy manager, joining manager Suzanne Evans whose appointment was announced last year.
Amanda has already clocked up 27 years in the care sector.
She said: “I knew from a very young age I wanted to be a nurse so I started working as a Health Care Assistant in the NHS.
“I have worked as a home manager in the private sector as well as with the NHS and am excited to start working for Camelot Care: I was attracted by their reputation, their specialism in dementia care and the fact that the organisation is family run.

“It will also be lovely to be working alongside James Marchant, Camelot Care’s operations manager again: we’ve worked together before and he’s a great person to have on your team.
“I was originally attracted to dementia care because I’ve had personal experience of caring for family members living with dementia and I am very passionate about this area of nursing.
“I particularly enjoy building a rapport with the residents and their family members, creating a trusting relationship in order to enhance the lives of the people we care for.”
Outside work mum-of-two Amanda, who lives in Barnstaple with her partner Caroline, loves the great outdoors, especially walking their three dogs in the woods and on the beach, as well as hiking – they climbed Snowdon in May 2023 – and camping in the camper van the pair converted together.
New survey insights reveal the far-reaching impact caregiving can have on physical and mental well-being, with over half (54%) of caregivers reporting weekly back, joint or muscle pain, and 1 in 5 (19%) experiencing daily stress or anxiety.[i] Dr Dawn Harper shares her tips to help cope.
There are approximately 4.7 million unpaid carers in the UK,[ii] defined as those who provide unpaid care for someone who is ill, disabled, older, has mental health issues or struggles with addiction. However, this figure excludes the many who regularly care for children, neighbours or friends and family needing support beyond the traditional definitions. Carers UK estimates that the number of unpaid carers could be as high as 10.6 million, highlighting a significant lack of personal and societal recognition of what it truly means to provide care.[iii]
A new survey, commissioned by GOPO® Joint Health – a leading supplement proven to reduce pain and stiffness and improve mobility – polled 1,001 self-defined caregivers. The findings reveal the true impact of caregiving on mental, emotional and physical health. Over one-third (37%) have experienced significant strain, discomfort or injury to their joints as a result of assisting or lifting the person they care for, and almost half (47%) frequently endure persistent aches, stiffness or pain that lingers long after caregiving tasks.i As a result, one-third (32%) rely heavily on pain medication, putting their own long-term health at risk.
The mental toll of caregiving is profound, with almost half (46%) of caregivers feeling emotionally drained by the relentless stress it brings. One in seven (13%) rely on support services for their well-being, while nearly half (44%) experience loneliness or isolation at least once a week, often facing the demands of caregiving alone.
Despite these challenges, almost half (49%) of respondents cannot remember the last time they practiced self-care, admitting that their own needs always come last.i While caregivers devote themselves to others, acknowledging the importance of self-care, and setting aside time for their own well-being is vital.
Dr Dawn Harper, formerly a caregiver to her mother, NHS doctor for over 30 years and author of ‘Live Well to 101’, comments: “Caregiving is a labour of love, but the selfless nature of the role puts many caregivers at serious risk of poor health. As a GP I see first-hand the impact that caring can have on both physical and mental ill health. To continue supporting others, it’s vital to care for yourself first. Just like the safety advice on an aeroplane – put on your own oxygen mask before helping others. Prioritising your own wellbeing ensures you have the strength, resilience and capacity to provide the care your loved ones need in the long-term.”
Dr Dawn Harper provides her top tips to support caregivers’ health and well-being: Seek support from peers: “It can be easy to lose your identity when providing care, so it’s important to connect with peers who are in a similar situation. If you are unable to leave the house often, online forums or virtual coffee sessions can provide an outlet to enable you to open up to someone who understands exactly what you’re going through. Their acceptance and understanding can be a great way to support your emotional health and leave you feeling less alone.”
Schedule self-care: “Caregiving often leaves little time for personal well-being, but self-care isn’t a luxury, it’s a necessity. Schedule self-care just like any essential appointment and if you’re struggling to find the time, start with small manageable breaks of just 5-10 minutes and commit to doing one thing that makes you feel recharged. This could be as simple as having a cup of tea in silence or reading a few chapters of your favourite book.”
Build your mental resilience: “Mental resilience helps caregivers manage stress, maintain emotional balance and continue providing care without burning out. Incorporate techniques such as mindfulness, deep breathing, yoga or meditation, all of which can be practiced in as little as 15 minutes. If you are struggling with your mental health, make sure to reach out to mental health helplines or listening services, or discuss your feelings with your GP or pharmacist.”
Prioritise your physical health: “Caregiving is a physically demanding role, and these survey findings reveal the true toll caregiving can take on your physical health. Protect your joints and posture by using proper lifting techniques when assisting with mobility, and address any aches and pains early to help prevent chronic conditions from appearing later down the line. A joint health supplement such as the galactolipid, GOPO, a compound derived from rose-hip, may be of great benefit, with research indicating that it can effectively relieve joint pain.[iv] The natural anti-inflammatory properties of GOPO make it a viable replacement to pain killers,iv without the risk of harmful side effects, and a sustainable way to manage pain long-term.”
Extensive studies involving over 400 patients with chronic pain conditions, such as osteoarthritis, have shown that GOPO® produces significant and consistent pain relief and improved joint function. In one study, 8 out of 10 patients reported a significant reduction in pain after just 3 weeks of GOPO®.[v]
GOPO® Joint Health is available from Boots, Amazon, and independent chemists and retailers nationwide. Visit www.gopo.co.uk for further information.
[i] GOPO® Joint Health survey on 1,001 caregivers in the UK. January 2025.
[ii] The Kings Fund. 2024. What are unpaid carers, who are they and how often do they provide care? Available at: https://www.kingsfund.org.uk/insight-and-analysis/data-and-charts/unpaid-carersnutshell#:~:text=According%20to%20the%202021%20Census,females%20from%20the%202011%20Census. (Accessed: January 2024). [iii] Carers UK. 2023. Annual Report 2022-2023. Available at: https://www.carersuk.org/media/ynfpnjwk/carers-uk-annual-report-22_23 (Accessed: January 2025).
[iv] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[v] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[vi] Rein
The UK Government has confirmed that local authorities across England will receive a total public health grant of £3.66 billion for the financial year 2024-2025, providing much-needed resources to support health and wellbeing initiatives.
This funding includes an uplift to cover the in-year cost impact of NHS pay awards for health services commissioned by local authorities, ensuring that frontline care and public health services remain sustainable.
The grant remains ring-fenced for public health purposes, meaning that councils must use the funds to improve health outcomes and reduce inequalities in their communities. This is particularly significant for residential and nursing homes, where local public health initiatives play a crucial role in infection control, vaccinations, mental health support, and staff training.
Local authorities will receive the grant in four quarterly instalments:
• Quarter 1: 5 April 2024
• Quarter 2: 5 July 2024
• Quarter 3: 4 October 2024
• Quarter 4: 3 January 2025
The structured payment schedule aims to provide financial stability, allowing councils to plan and implement health programmes effectively.
Local authorities will be required to report their spending through Revenue Account (RA) and Revenue Outturn (RO) returns, ensuring transparency in how funds are allocated. Any underspend may be carried forward as part of a public health reserve, though the Department of Health and Social Care (DHSC) has indicated that repeated significant underspends could lead to reductions in future grant allocations.
David Buck, Senior Fellow at The King’s Fund, said: ‘The £3.9 billion public health grant for 2025/26 represents a welcome, real terms increase on the previous year. We are yet to see government announce the separate budgets for council drug and alcohol services, so it is hard to say if there will be an overall increase in council public health budgets, but today’s announcement is a positive sign.
‘The public health grant is the bread and butter for local authorities implementing services to improve people’s health. A particularly important task at a time when Britons are spending more years of their life in poor health, and millions are out of work due to long term illness.
‘The government has stated its welcome ambition to shift from treatment to prevention, but there is a long way to go. This country plans to spend over £3000 per person on the NHS next year, compared to less than £70 per person for local authorities to prevent people from getting ill in the first place. The contrast is stark.
‘The allocation of this grant comes against a tight financial backdrop across all government departments. But the rising burden of disease across the country is itself hampering economic growth. Without further ramping up investment and resources in preventive services, it will be hard to realise one of the government’s essential goals – shifting from treatment to prevention.’
Nuffield Trust Chief Executive Thea Stein said: “After years of arbitrary and irrational cuts, today’s announcement of a 5.4% uplift to the Public Health Grant is a welcome move by government, backing up its promise to shift health care more into the community and focus on prevention.”
“Public health support – from health visitors to sexual health and drug and alcohol services – can make a real difference to people’s lives. But it has long been the poor relation to the NHS, suffering the largest fall in funding compared to other NHS services according to recent analysis.”
“Ultimately, how far today’s boost will really go depends on what happens to staff wages, which can quickly eat up funding in these services, and whether traditionally separate funding for drug and alcohol services sits within this extra money.”
Resident, Maureen at Upton Bay care home in Hamworthy had always wanted to resurrect her passion for winter sports especially ice skating, so staff at the home made her wish a reality proving the old adage, it’s never too late. Maureen has lived at Upton for over a year and is beloved by staff and residents alike. Staff at the home were delighted to be a part of making her dream come true, as they knew how much it meant to her, and they all wanted to be there to see the smile on Maureen’s face when her dream was realised.
Activities’ staff member Chloe researched and discovered that the Cool Coast ice rink at the BIC in Bournemouth allow wheelchairs on ice. As Maureen’s mobility is very poor this was ideal and she would be accompanied by her carer Lizzy and Chloe so they could make sure she had fun but felt safe
and secure.
In response to this wonderful surprise, Maureen, said: “I was on the verge of tears. It is such an amazing feeling to know that such a loving group of people care so much about me that they helped me to live out a dream –and I didn’t even ask.”
Mevin Sohorye, General Manager at the home, said: “We believe that every moment is worth cherishing. We want everyone we care for to know how important they are to us here at Upton Bay. It is testament to the hard work and dedication of the team here in making our residents’ dreams come true. It was wonderful to see how happy Maureen was – and the staff loved being a part of this as well.”













For most, skiing down the breathtaking slopes of the French Alps is a thrilling adventure. For Jac - born with cerebral palsy - it was the realisation of a dream thought impossible. With an unbreakable spirit, Jac embarked on the journey of a lifetime, proving that no challenge is too great when care and opportunity come together.
Thanks to Ski4All Wales and the expert care of Newcross Healthcare, Jac’s adventure to the Alps has become a powerful reminder that with the right people by your side, anything is possible.
DEFYING LIMITS, EMBRACING ADVENTURE
Thanks to the personalised care team from Newcross Healthcare, Jac was able to focus on the thrill of the experience, rather than the logistics and challenges of his care. From mobility assistance to medication management, the team’s care allowed Jac to embrace the adventure to the fullest.
Jac’s mother, Beth, expressed how crucial the right support was in making this experience possible.

“We've got to put Jac’s safety first and Newcross came in and really supported us. We worked with Newcross quite closely to get the right care staff in so that they met Jac’s needs and that I could have peace of mind with them”. Beth, Jac's mum CARE THAT EMPOWERS, NOT LIMITS
At Newcross Healthcare, whether skiing in the Alps or gaining independence in everyday life, we believe
care should unlock possibilities and life experiences, not place restrictions. “We've gone from everyday being at home with Jac, to out here in the French Alps just accomplishing things we never thought we'd see him do. It's been a privilege to be able to help him do this.” Carolyn, Newcross Healthcare Carer BEYOND THE SLOPES: A COMMITMENT TO LIFE-CHANGING CARE
At Newcross Healthcare, we believe every individual deserves the chance to live life to the fullest, no matter their health challenges. Our carers don’t just provide support; they open doors to unforgettable experiences, independence, and joy.
Claire Reader, Vice President of Community Care at Newcross Healthcare, shared her pride in the team’s dedication and the outcomes for Jac:
"I feel truly thrilled and privileged to work with such incredible teams who continually go above and beyond for the people we support. Enabling our care team colleagues to make a ski trip possible for two of our complex care young gentlemen is a testament to their dedication and compassion. Together, we are not just providing care but making dreams a reality and that’s something truly special." Claire Reader, Vice President, Community Care, Newcross Healthcare.
Get a glimpse of Jac’s incredible journey as he conquers the slopes of the French Alps – watch the full video of this unforgettable adventure here.
This week, residents at Portsdown View in Bedhampton took part in an exciting game of Walking Netball; a sport specially adapted for older adults. Residents played in teams of seven and competed against each other in games lasting 8-12 minutes each. The sport was a big hit, and every game was full of teamwork, gentle exercise, and plenty of laughter!
Walking Netball was developed by England Netball and Age UK as a more inclusive and accessible version of the game for people with mobility challenges. No running and jumping is allowed, and players are allowed to take an extra step with the ball. They can also hold onto the call for longer to allow more time for decision making, and the game is designed to be non-contact to reduce the risk of injury.
The game at Portsdown was a success, with residents showing off their coordination and competitive spirit whilst also practising working together as part of a team. Pippa Mafunga, General Manager at Portsdown View, offers her thoughts:

“It was so great to see the residents enjoy a day of physical activity and team-building. Before they tried Walking Netball, many of our residents thought their sporting days were over. Happily, they were more than up to the physical challenge and surprised even themselves. Indeed, one resident enjoyed it so much they even requested a rematch later the same day!”
Since its launch, Walking Netball has grown in popularity across the UK, Australia, and New Zealand, and has been particularly valuable in adult care settings. Research shows it can improve fitness, mental
well-being, and social connectivity amongst players, and provides cognitive stimulation by forcing players to strategize as part of a team.
One review of a nationwide Walking Netball program across England found it led to significant improvements in physical wellbeing and overall quality of life amongst middle-aged and older-aged women.
Another study on the mindset of the players found that many people value the sense of belonging they got from the game. This feeling of social cooperation and collaborative teamwork is crucial to the game’s success; and is also the major reason many players feel the urge to keep coming back for more.
Pippa Mafunga again: “The benefits were not just physical. The games really helped some of our residents come out of their shell and enjoy interacting as part of a team. It goes to show that however old you are, there is always something you can do to get the blood pumping and endorphins flowing. And, if you can do that whilst spending quality time with your friends, then all the better!”
After the match, the residents gathered at Portsdown’s bistro café to enjoy some well-earned hot chocolate and cake.
Portsdown View is part of the Connaught Care Collection; a new luxury care provider which has six operational homes across the country. The Walking Netball session is just one of many activities the home has planned to enhance residents’ quality of life through movement, social engagement, and a strong sense of community. Watch this space.
UK Care Week is an event exclusively for care professionals, designed to empower and equip you with the skills to enhance the lives of those in care. This event provides a vital platform to explore industry-leading content, innovative solutions, and hands-on product demonstrations.
With 100+ CPD-accredited sessions, innovative products from 150+ top suppliers, and tailored guidance at the CQC Inspector Hub, you’ll find resources to meet the highest standards. Dive into interactive features like the Virtual Dementia Tour and expert-led training to elevate care.
WHAT’S ON THE AGENDA?
The event features an impressive lineup of sessions, workshops, and opportunities to engage with the latest developments in the care sector. Key highlights include:
THE CARING VIEW THEATRE

Hosted by the passionate team behind the Caring View Podcast, this theatre promises engaging discussions and insights into the latest care practices and strategies. Meet over 150 exhibitors showcasing solutions designed to stimulate business growth and help implement sustainable care models. Discover cutting-edge technologies and practical tools to elevate your care services.
Attend interactive seminars hosted by industry experts. These sessions tackle real-world challenges in care settings and offer actionable solutions to overcome them. Gain up to 12 CPD points across 2 days. CQC INSPECTOR HUB Book
able to answer any queries, as well as dealing with registration advice.
CO-LOCATED
Gain access to additional CPD sessions and resources through co-located events, including The Alzheimer’s & Dementia Show, Neuro Convention, and Naidex. These events create a collaborative environment that unites aspects of health, social care, rehabilitation, inclusion, and diversity.
EXCLUSIVE TRAINING OPPORTUNITIES
In partnership with Training2Care, co-located event The Alzheimer’s & Dementia Show offers unique experiential training sessions tailored to dementia care:
• Virtual Dementia Tour: £60 + VAT per session
• Dementia Interpreters Workshop: £45 + VAT per session
• DIET, Dining Immersive Experiential Training: £60 + VAT per session
• Autism Reality Experience: £60 + VAT per session
Spaces for these sessions are limited, so early booking is highly recommended. Uk Care Week visitors can book onto these sessions via the Alzheimer’s & Dementia Show website - www.alzheimersshow.co.uk/train-

Parliament’s Health and Social Care Select Committee has conducted a visit to the Isle of Wight, to explore the provision of health and social care on the island, as part of its Adult Social Care Reform: The Cost of Inaction inquiry.
The Committee chose to visit the Isle of Wight to inform its inquiry, as the island’s demography is characterised by a higher proportion of residents aged 65 and above compared to the national average.
Members of the Committee visited St Mary’s Hospital, part of the Isle of Wight NHS Trust, the only NHS organisation in the country that provides Acute (hospital based) services and ambulance services.
During their visit MPs were able to see first-hand the delivery of health care services, touring the hospital’s Urgent and Emergency Care Floor and its unplanned care ward and frailty provision.

MPs met with the Trust’s CEO, Penny Emerit, and its Chief Officer, Joe Smyth, to understand the local context in which care is being delivered, and also met with the hospital’s Consultant Practitioner in Acute Frailty and Emergency Medicine Consultant amongst others.
After touring the hospital, the Committee met with Directors from the Isle of Wight Council, including its Strategic Director for Adult Social Care and Housing, and heard about the challenges they face meeting the needs of the island’s population, including working age adults.
In its meetings with employees at the hospital and the Council, the Committee explored the extent to which challenges in social care provision locally impact on the hospital’s ability to move more care into the community and its ability to focus on prevention.
At the hospital, the Committee had the opportunity to meet with representatives from community groups including Healthwatch, Age UK and Carers Isle of Wight. They heard about the changing nature of the work these groups are doing and the challenges they face around funding and providing services.
During their time on the Isle of Wight, MPs also visited Care in the Garden, a not-for-profit organisation set up to create work opportunities for adults with additional needs, and Hazel Lodge care home, where they met with both employees and residents.
The Chair of the Committee, Layla Moran MP, said: “The Committee is grateful to the Isle of Wight’s St Mary’s Hospital, Care in the Garden and Hazel Lodge for welcoming us this week and for giving up their time to ensure a constructive day for us.
“We found it very valuable to be able to see first-hand the delivery of health care services and to learn about how the NHS Trust, the Council and the voluntary sector work to provide health and social care services for a population significantly older than the national average.
“Our visit has given us much food for thought and helpful insights, which will inform our future work in our inquiry into adult social care.
“We were pleased that our visit to the island also afforded us an opportunity to visit a not-for-profit organisation supporting work opportunities for adults with additional needs and we enjoyed chatting to employees about the value of the support provided by Care in the Garden.
“A major part of adult social care is of course care provided in residential care homes, and so we are grateful to Hazel Lodge Care home for facilitating our visit to them during which we were glad to be able to speak to care workers and residents.”
Penny Emerit, Chief Executive, Isle of Wight NHS Trust and Portsmouth Hospitals University NHS Trust, said: “We were delighted to welcome the Health and Social Care Select Committee to the Island. As an Island community we face additional challenges to ensure we provide high quality care and it was great to have this recognised. We were able to showcase some of the fantastic innovations we already have in place across our integrated acute and ambulance trust and also discuss what changes would help to further progress this and our partnership working.”
Joe Smyth, Chief Officer, Isle of Wight NHS Trust, said: “The island is a great place to test innovative work, due to our unique position of having integrated acute and ambulance services. It was a real opportunity for our staff to share how we are already transforming our services. We are also keen to do more to support the development of new models of care and welcome the opportunity to work together on trialling and implementing the needs of an increasingly frail community.”
Oake Meadows care home in Taunton, Somerset, has achieved a certificate of compliance from the only Accredited and Registered Care Home Inspection Body in the UK.
The certificate of compliance was awarded following an independent inspection by Care Inspections UK (CiUK), an accredited inspection body responsible for assessing compliance with regulations for care homes across the country.
Oake Meadows is the first care home in Somerset to achieve this certification, highlighting its leadership in maintaining the highest standards of care, safety, and employment practices. This recognition is a significant endorsement of Oake Meadows’ dedication to ensuring the wellbeing and safety of its residents.

Oake Meadows is registered to provide accommodation and personal care for up to 105 residents. The recent inspection, conducted over two days, commended the home’s commitment to continuous improvement, its strong person-centred approach, and its high standards of care. Inspectors noted that the management team and staff were highly receptive to feedback and proactive in addressing any areas of concern.
Katrina Ball, manager of Oake Meadows said: “We are absolutely thrilled to receive this certificate of
compliance from CiUK. It’s a fantastic recognition of the dedication and passion our team brings every day to ensure the very best care for our residents. At Oake Meadows, we are committed to creating a safe, supportive, and dignified environment, and this certification is a reflection of that unwavering commitment.
“While this is a wonderful achievement, it’s not the finish line. We are always striving to enhance the quality of life for those in our care, finding new ways to improve and grow. I couldn’t be prouder of our incredible team, and I’m excited for what lies ahead for Oake Meadows.”
Tony Stein, chief executive of HCMS, which manages Oake Meadows, added: “This certificate is a fantastic endorsement of the team’s dedication and hard work at Oake Meadows. Providing exceptional care is at the heart of everything we do at HCMS, and it’s wonderful to see the team’s efforts recognised in this way. Quality care is not just about meeting standards; it’s about exceeding expectations and continuously striving to enhance the lives of our residents.
“I have no doubt that the team at Oake Meadows will continue to build on this success, always looking for ways to improve and innovate. Their passion and commitment are what make Oake Meadows such a special place, and I look forward to seeing them go from strength to strength.”
Taylor & Taylor, a group of family-owned residential care homes approached food procurement experts, allmanhall to achieve scalable cost savings and efficiencies to support their growth plans. They needed to ensure no detrimental impact to the excellent quality of their food offering and their residents’ dining pleasure.
Their desire was to achieve a 5% food cost saving and to ensure ongoing effective management of catering budgets and invoicing. Operationally, access to reports and insights were key, as was ease of ordering and management of stock and deliveries.
allmanhall undertook a like-for-like benchmark and identified achievable food cost savings of 11.4% - more than double the initial objective!
allmanhall delivered tech demos of the catering control platform for Taylor and Taylor, ensuring it met their needs and provided training for the team. As well as providing useful operational functionality like stock taking and standing orders, the catering control platform proposed would also give access to management reports and facilitate central billing and conversion of all supplier invoices in to 1 per month. Samples and on-site supplier meetings were also arranged on behalf of the homes, to confirm that the quality was to the required standard.
allmanhall have also supported Taylor and Taylor with the launch of a community engagement event for one of their newest homes.
A few months into the contract, the actual results were found to be an 18% food cost saving! You can watch this short video on You Tube to find out more…
“From day 1, the care and attention provided by allmanhall has been exceptional. The team truly listen to us, to what our challenges are and are always willing to help in any way they can. Their approach is thorough and responsive, meaning we feel fully supported. Everyone we’ve met from allmanhall has been hands-on, down to earth, genuine and considerate.
I’ve been impressed by the savings we’ve already seen, the flexibility regarding suppliers and by the excellent quality. The consolidation of invoices into 1 per month is a huge win.
We have relationships and contact with people across the allmanhall team – all there to help and to advise or resolve depending on what we need. With challenges around labour shortages and food inflation, this is hugely valued. It frees up the team and gives us peace of mind.
I would wholeheartedly recommend allmanhall’s services to others in the care sector and I look forward to continuing to grow our offering and provide outstanding food for our residents, with allmanhall as our trusted partners.”
– Chris Rees, Group Executive Chef
allmanhall is an owner-managed, award-winning and trusted food procurement partner for care organisations across the UK. We help clients with a range of needs, including cost savings, administrative efficiencies, supplier management, dietetics and nutrition support, and sustainability goals. Get in touch to find out more:
Email: hello@allmanhall.co.uk
Telephone: 01225 745520
Website: allmanhall.co.uk
LinkedIn: @allmanhall


The Scottish Medicines Consortium (SMC) has rejected a new Alzheimer’s drug, lecanemab (sold under the brand name Leqembi), for use on the NHS in Scotland.
The SMC said there were uncertainties about the health benefits of lecanemab set against its costs, including monthly infusions and regular monitoring for side effects.
This comes six months after the drug wasalso rejected by the National Institute for Health and Care Excellence (NICE)for use on the NHS in England and Wales.As a result, anyone eligible for lecanemab and wishing to receive it will need to pay for it privately.
After announcing its decision, the SMC said it would “welcome a resubmission from the company with changes to address the uncertainties”.

Charities described the decision as a heartbreaking setback. The drug’s steep price tag puts it out of reach for many families already bearing the financial and emotional burden of care, with some even giving up their careers to support loved ones.
A handful of private clinics in England are now administering lecanemab, priced at £60,000 per year. It’s estimated that just 18% of people caring for someone with dementia are in paid work.
Hilary Evans-Newton, Chief Executive of Alzheimer’s Research UK, called on the government to use this
decision as a wake-up call, stressing that the upcoming 10-Year Plan for Health must consider people affected by dementia, and help shape a future where it no longer devastates lives and the NHS.
“Without action, the NHS risks progressively falling further behind Europe, America and Asia when it comes to access to new, innovative dementia treatments – many more of which are on the horizon,” she said.
There are currently over 160 trials worldwide testing more than 125 experimental Alzheimer’s treatments. Of these, 30 are in late-stage trials that NHS England has identified as potential treatments available by 2030.
Like similar decisions in England and Wales, today’s outcome is largely driven by the costs of expanding diagnostic infrastructure, such as brain scans, and administering infusions. Evans-Newton highlighted potential solutions to address these challenges.
“One promising option would be moving from hospital infusions to injections at home — something already being explored in clinical trials and under review by the FDA in the US. But this won’t happen quickly, so it’s vital for the UK government, NHS leaders, and industry to come together and find innovative approaches to ensure people can benefit from new Alzheimer’s treatments now.”

TWO Huddersfield care homes have been declared “Veteran Friendly” after receiving accreditation by an armed forces charity backed scheme.
Aden Mount Care Home and Aden View Care Home, both on Perseverance Street, Primrose Hill, have now received Veteran Friendly Framework (VFF) status – certifying the enhanced care and support for veterans living at the homes.
The VFF initiative was launched in 2023 with the aim of tackling loneliness and isolation and delivering improved health and wellbeing outcomes for over 25,000 veterans living in care homes across England.
It is a collaboration between Armed Forces charities Royal Star & Garter and Royal British Legion, and NHS Veterans’ Covenant Healthcare Alliance (VCHA), with funding support from the Armed Forces Covenant Fund Trust.
Staff, residents and veterans at the Hill Care Group operated care homes have been celebrating their VFF status with friends and family members since receiving their certificates.
Among the veterans living at Aden View Care Home is 88-year-old John Rogers, who served as a Gunner in the Royal Artillery Regiment of The British Army from 1958-60 as part of his national service. He then spent three years in the Army Emergency Reserve, stationed at Barford Camp, at Barnard Castle in County Durham, where he developed training schemes for the officers.
At Aden Mount Care Home, resident Rodney Coates, 78, is among the veterans, having joined the 1st
Michelle
“We are so proud to become part of the VFF. Working through the program has given us a much greater understanding of the person centred care that people who have served require and thereby make such a difference for our current and future residents.
“It has been a privilege getting find out more about our residents’ war time experiences, such as Rodney’s long career in the Army. They deserve so much respect for what they did for us.”
Michaela Elwell, activities coordinator at Aden Mount Care Home, said: “Talking with Rodney is so heart-warming. He is an amazing gentleman who I feel brings light and laughter everywhere he goes and we at Aden Mount are very lucky to have him.”
Kimberley McKay, home manager at Aden View Care Home, said: “I feel honoured to help introduce the Veteran Friendly Framework to our home. We already celebrate the veterans in our care at Aden View but the VFF programme gives us even more opportunities to ensure that their status is shared with our partners and they receive as much support as possible.

“We believe in sharing peoples’ stories and experiences, so we have recently dedicated a special area in the care home to promote veterans. Since creating this space, we’ve had our residents, families and friends share many more stories with us.”
If you’re involved in caring for others – whether you’re a care provider, a health and social care professional seeking the latest products and services, a family carer in need of support, or simply someone passionate about care – the Alzheimer’s & Dementia Show is the event for you.
As the UK’s leading dementia event, it offers a unique opportunity to explore a wide range of care exhibitors, hear from expert speakers, and experience innovative training sessions. This event is more than just an exhibition; it’s a platform for learning, discovering solutions, and connecting with people who share a commitment to improving dementia care.
Taking place at the NEC in Birmingham on 19-20 March 2025, the Alzheimer’s and Dementia Show provides a vital space for families, carers and healthcare professionals to access resources and knowledge that can transform the lives of those affected by dementia.
WHAT’S ON THE AGENDA?

The show is packed with insightful sessions designed to address key aspects of dementia care. Discover the latest diagnostic tools and treatment options that are revolutionising early intervention and improving patient outcomes!
CAREGIVER SUPPORT AND EDUCATION
Access practical strategies and resources that empower caregivers to provide compassionate and effective care, ensuring the well-being of those they look after.
DEMENTIA-FRIENDLY ENVIRONMENTS
Learn about innovative designs and technologies that create safer, more comfortable living spaces for individuals living with dementia.
WHY ATTEND?
For those seeking specialised training, the show offers sessions delivered by Training2Care. These experiential programs provide actionable insights tailored to dementia care. Sessions include:
Virtual Dementia Tour: £60 + VAT per session
Dementia Interpreters Workshop: £45 + VAT per session
Dining Immersive Experiential Training (DIET): £60 + VAT per session
• Autism Reality Experience: £60 + VAT per session
Spaces are limited, so early booking is highly recommended. Book your space here - www.alzheimersshow.co.uk/training.
EXPERT-LED SESSIONS
Gain insights from top researchers, clinicians, and advocates. Key speakers include:
• Prof Fiona Ducotterd "Putting tools in the toolbox to treat dementia." Chief Scientific Officer, Alzheimer’s Research UK, UCL Drug Discovery Institute
• Hannah Gardner "Supporting children and young people living within families affected by dementia." Consultant Admiral Nurse for Children and Young People, Dementia UK
• Prof Nathan Davies "Supporting people living with dementia through to end of life" Professor of Ageing, Applied Health and Care Research, Co-lead Centre for Psychiatry and Mental Health, Queen Mary University of London
DEMENTIA CLINICS WITH ADMIRAL NURSES
1-TO-1
For personalized advice and support, visit Dementia UK’s Admiral Nurses. These 1-to-1 clinics provide tailored guidance to address your specific questions and concerns.
NETWORKING OPPORTUNITIES
Connect with a diverse community of caregivers, healthcare professionals, and innovators. Share experiences, exchange ideas, and build valuable relationships within the dementia care sector.
EXHIBITOR HIGHLIGHTS
Explore an extensive range of exhibitors showcasing products and services designed to enhance the quality of life for individuals living with dementia. From cutting-edge technologies to practical caregiving tools, find innovative solutions to meet your needs.
DON’T MISS OUT!
Running alongside UK Care Week, Naidex, and the Neuro Convention, the Alzheimer’s and Dementia Show unites interconnected aspects of health, social care, rehabilitation, inclusion, and diversity. This collaborative environment provides a comprehensive look at the broader care community. Find out more - www.alzheimersshow.co.uk






Kara Healthcare has taken a major leap forward in its growth journey with the simultaneous acquisition of seven care homes – further strengthening its commitment to exceptional elderly care.
The deal, facilitated with support from full-service law firm Shakespeare Martineau, marks a significant milestone in the company’s ambitious expansion strategy.
Founded in 2013, Kara Healthcare has built a strong reputation for providing outstanding care across its three purpose-built homes in Leicestershire, Northamptonshire and Peterborough.
Now, with the addition of six state-of-the-art properties in the North East –acquired from administrators and lender ThinCats – alongside the purchase of Olive Row Care Home from the family-run operator Peterborough Care, the organisation is poised to set new benchmarks in the sector.
In line with Kara Healthcare’s ethos of stability and excellence, all existing staff will be retained, ensuring seamless continuity of care for residents. The company remains dedicated to elevating care standards and fostering a nurturing environment where both residents and staff thrive.

Nick Somani, CEO of Kara Healthcare, expressed his enthusiasm for the expansion. He said: “This is an incredibly exciting time for Kara Healthcare. These acquisitions are not just about growth – they represent our unwavering commitment to redefining care excellence.
“At Kara, we don’t just offer care; we create meaningful experiences, spark joy and cultivate a true sense of purpose for every resident. By bringing these fantastic homes into our portfolio, we’re expanding our
reach, enriching lives and setting a new gold standard in care provision.
“And we’re not stopping here. With more acquisitions on the horizon, we are actively seeking new opportunities to further strengthen our group, ensuring more communities across the UK benefit from the exceptional care we deliver.”
With an eye firmly on the future, Kara Healthcare continues to pursue its vision of delivering high-quality, resident-centred care while expanding its presence across the country. As the company looks ahead to new opportunities, its commitment to innovation, excellence and compassionate care remains at the heart of its mission.
Shakespeare Martineau provided comprehensive support across corporate, property, insolvency and banking services.
Roger Harcourt, corporate partner at Shakespeare Martineau who led the deal, said: “We are delighted to have been involved in these acquisitions, which take Kara Healthcare’s portfolio to 10 sites across the UK, and demonstrates the group’s commitment to providing excellent care nationally.
“The deals highlight the resilience and potential within the healthcare sector. While the market remains active, there are signs of distress among some operators. However, Kara Healthcare is dedicated to addressing these challenges head-on, with plans for further expansion in the coming years. We look forward to continuing to work with and support Kara Healthcare with its ongoing growth strategy.”
The Shakespeare Martineau team also included partners Chris Gayle (banking) and Sean Moran (restructuring and insolvency), and associate Emma Ali (commercial property and development).
Old Norse Lodge Care Home in Grimsby, part of Danforth Care Homes, was transformed into a bustling Viking village on Saturday, 25th January, as residents, team members, and the local community came together for a memorable Viking Experience Day. Hosted in partnership with Havelok’s Village, the free event welcomed visitors of all ages to step back in time and immerse themselves in the fascinating world of the Vikings.
The day saw staff and residents exploring an authentic Viking encampment and engaging in traditional arts and crafts, marvelling at weapon displays and watching Grim and Havelok come to life on screen.
The highlight for many, however, was meeting the Vikings themselves, who shared their stories and brought history vividly to life.
Residents and Team Reflect on a Day to Remember
The event was met with glowing feedback from both residents and team members. Shirley G, a resident at Old Norse Lodge, shared:
“I enjoyed it, I think everyone did. It was stimulating – us elderly need stimulating, and it was good to go back in time. I took part in arts and crafts, and it was nice.”

Another resident, Wendy A, reminisced about her school days: “I really enjoyed it. The men were very informative, and they knew their stuff. They reminded me of things I had forgotten – I remember making a Viking boat at school and coming last! I very much enjoyed the battles; it was a really good day.”
The team at Old Norse Lodge embraced the day with enthusiasm, adding their own unique touches to
the event. Charlene, a team member, donned full Viking attire, immersing herself in the experience: “I dressed up for the event and my costume was very hot! Havelok told me I had to keep it on all day to see how they felt, and wow – it was warm. I couldn’t hold the shields for long; they were so heavy! They said I fitted in; I just needed to practise my battle face. It was really nice to see everyone’s smiles. The Viking children even made me a bracelet and gave me a full rundown of how they made it and what it was made from.”
Fellow team member Kea added: “I was working the Viking Day – it was a wonderful day with loads of activities. The residents especially liked the Viking children; they said it added an extra special touch.” Corrine, another team member, summed up the atmosphere perfectly: “Everyone enjoyed it – all the kids that came loved it. It was a good day.”
Rachael Smith, Manager at Old Norse Lodge, expressed her delight at the event’s success: “Seeing our residents and the local community come together to celebrate Grimsby’s rich Viking heritage was truly heartwarming. Events like this are so important, not just for the fun and excitement they bring, but for the memories they create. At Old Norse Lodge, we’re dedicated to providing engaging, meaningful experiences that enrich the lives of our residents.”
The event also served as a nod to Grimsby’s Viking roots. Over 1,000 years ago, Grimsby was the gateway between the Viking Kingdom of Jorvik and the wider Viking world. The town’s name derives from the legendary Viking Grim, who rescued the Danish prince Havelok and raised him in exile.
Care tech leader Sensio are proud to announce a strategic long-term partnership agreement with Lovett Care for their sensor technology RoomMate and digital Nurse Call system to be rolled out across their estate.
Sensio is a leading provider of care technology through pioneering software and products, solving today's and tomorrow's care challenges for the benefit of residents, relatives, care teams and society.
The long-term partnership agreement encompasses a roll out of Sensio’s digital Nurse Call system and the multi-sensor RoomMate and digital supervision to Lovett Care’s portfolio of care homes in 2025. Since Lovett Care acquired New Care in October 2024, the technology will also feature in all New Care facilities too.
RoomMate is a privacy first multi-sensor that alerts care teams when a resident is at risk of a fall and helps ensure staff are available to prevent a fall before it happens. RoomMate also captures valuable activity datat that is fed directly through to care planning software to enrich care plans and drive better quality evidencebased decision making.

The digital Nurse Call system is a wireless, silent nurse call system that transforms care home environments by removing noisy call bells. Sensio Nurse Call sends alerts directly through to care teams handheld devices, enabling teams to triage support to those most in need. Both of these solutions are designed
specifically for those living with dementia where traditional forms of alerting are not always appropriate or workable.
Lisa Delaney, Country Manager Sensio UK, says: “We are very excited to be partnering with Lovett Care and this is an important step for Sensio in the UK. We have really enjoyed working with the team so far and have been impressed by their eagerness to embrace new technology. I look forward to growing our partnership further over the next few months and help Lovett Care to deliver the best care possible for their residents.”
Following a successful pilot which demonstrated a significant reduction in falls, highlighted positive outcomes for residents, and fostered a better working environment for care teams, Lovett Care has made the decision to roll out the technology across its homes.
Keith Crockett, CEO of Lovett Care, commented: “Both Lovett Care and New Care are already leading care home operators in technology advancements, so adopting Sensio’s RoomMate and digital Nurse Call system will further enhance and improve our residents’ experiences. The trial was a success, and RoomMate proved to be highly effective in reducing falls. We’re excited to partner with Sensio to integrate this technology into our homes, further enhancing the safety and support we provide to our residents.”
For further information on Sensio please visit www.sensio.io
To find out more about Lovett Care please visit www.lovettcare.co.uk
Commercial Kitchen and Laundry Solutions (CKLS) are one of the UK's leading suppliers of commercial kitchen and laundry equipment.

Whether you are a small sized residential home or large scale nursing home group, CKLS has the expertise and equipment you need to keep your operations running smoothly.
At CKLS, we understand that the success of your business depends on the quality of the equipment you use. That's why we've made it our mission to provide businesses across the UK with the highest quality commercial laundry and kitchen equipment available. We work with only the best manufacturers in the industry to ensure that our customers get the most reliable and efficient equipment possible.
Our commitment to our customers doesn't end with the sale of our equipment. At CKLS, we know that maintenance and repairs are crucial to keeping your equipment functioning at its best. That's why we offer
a full range of maintenance and repair services to our customers, including emergency repair services available 24 hours a day, 7 days a week.
We believe that our success as a company is measured by the success of our customers. That's why we're constantly striving to provide better products and services to help our customers achieve their goals. We're proud to say that our commitment to excellence has earned us a reputation as the go-to provider of commercial laundry and kitchen equipment in the UK.
So, if you're looking for reliable, high-quality commercial laundry and kitchen equipment, look no further than CKLS. With our extensive range of products and services, we're confident that we can help you find the right equipment to meet your needs and keep your business running smoothly for years to come.
Visit our website www.ckls.co.uk contact by phone on 01200 411914 or email at sales@ckls.co.uk.
Mobile Kitchens Ltd specialises in the hire or sale of temporary catering facilities and foodservice equipment.
Ideal for events or to provide temporary catering facilities during your kitchen refurbishment, our versatile units and equipment offer an efficient and economic solution to the caterers’ needs.
Production Kitchens, Preparation Kitchens, Warewashing Units, Dry Store Units, Cold Rooms and Restaurant Units are available as individual units in their own right or they can be linked together on site to form a complete complex.

Alternatively, we can offer modular, open-plan facilities, usually for larger, longer-term hires.
We offer a free design service, and project management from concept through to delivery and installation on site, plus full technical support throughout the hire period.
The standard specification of our smallest Production Kitchen unit includes a six burner oven range, salamander grill, twin basket fryer, upright fridge, hot cupboard, single bowl sink unit with integral hand wash basin, plus ample power points to plug in Microwaves, Food Processors, Toasters etc. Internal equipment can be interchanged and clients can effectively specify their preferred layout.
We have many tried and tested design layouts and would be pleased to put forward our recommendations for your project. So if you’re planning a refurbishment or need to cater for an event then why not give us a call and we’ll be happy to provide advice and put forward a competitive proposal. For further information or to arrange a site visit, email: sales@mk-hire.co.uk or call us on 0345 812 0800, or visit our website: www.mk-hire.co.uk


Infection control is critical in care homes, where laundry processes play a vital role in hygiene management. Care homes face increased pressure and scrutiny with changes to the Care Quality Commission inspection framework, and it is absolutely fundamental that care homes know how to safely ensure efficient infection control across all areas. CQC inspections place heavy emphasis on evidence-based infection control practices, including rigorous checks on laundry processes. Compliance with these standards is essential to safeguard residents, maintain trust, and achieve strong CQC ratings.
There are various way to ensure the right levels of hygiene control; you should employ thermal and/ or chemical disinfection. Ozone is one of the disinfection options that can be successful, but it is essential to adhere to HSE recommendations, take appropriate safety precautions, and use control measures as outlined by COSHH as use of this powerful oxidant does carry potential health risks. Forbes Professional offers care homes alternatives to Ozone systems, that still meet the most exacting hygiene requirements. Their

Miele commercial laundry machines enable sluice, thermal and chemical disinfection, to meet all the industry requirements of WRAS and CQC. When paired with Forbes’ advanced chemical detergents, which kill pathogens even at low temperatures, these commercial machines deliver a complete laundry solution for optimal infection control.
Forbes understands that care homes require tailored solutions. Their industry specialists work closely with operators to recommend the right commercial machines to meet their specific needs. Beyond installation, they offer award-winning service support to ensure ongoing compliance and operational efficiency.
For any care home, laundry is a key part of infection control. It is imperative that appropriate commercial laundry equipment is used within a care setting, and that there is a reliable partnership in place for service and maintenance. By choosing Miele’s technology and Forbes Professional’s expert support, care homes can safely and effectively meet stringent hygiene standards.
See the advert on the facing page for further information on Forbes.
MAG Laundry Equipment is a multi-award-winning supplier of commercial washing machines & tumble dryers that supports over 10,000 care homes across the UK. Clean laundry and bedding is critical for care homes, hospices, nursing homes, hospitals and other healthcare organisations. With a nationwide fleet of accredited engineers MAG Laundry Equipment has successfully assisted over ten thousand care homes with their products, services, information and support.
MAG’s product range includes commercial washing machines, tumble dryers, ironers, presses and detergents. For 100 years, since 1922, MAG’s products have been developed and improved to become some of the most reliable, energy-efficient and

the machines, and giving them a check-over, to see which parts, if any, can be carried over the refurbishment. Lavamac will only carry over the highest-quality parts from the machine from pre to post refurbishment. The machine then undergoes an extensive refurbishment, with almost all the parts being replaced, with the refurbished machines being given specialist parts based on the model type.
not only contributing to a greener way of
but also saving our customers money!
We have recently set up a specialist facility in St. Neots, near Cambridge, in which we are going ahead with this specialist refurbishment programme. This programme involves purchasing existing machines, and replacing the parts on them, so that they are as good as new, whilst retaining the look and feel that existed before, but with a massively increased lifespan, and a warranty on the machines that’s as good as a warranty on a new machine to go with the refurbishment too. Our refurbishment programme in our specialist facility includes stripping down

We recently have been awarded a bronze award in sustainability by the groundworks trust, affirming our commitment to the sustainability industry – however, as much of a compliment as it is, it does not mean that the hard work stops there! The next step on our journey is to hopefully be awarded the prestigious silver sustainability award! For this, we need to ensure that our carbon emissions are being cut down from our vans, continue our sustainability and refurbishment programme and to keep making green decisions within the company! 0151 317 3127 info@laundrytec.com www.lavamac.eu


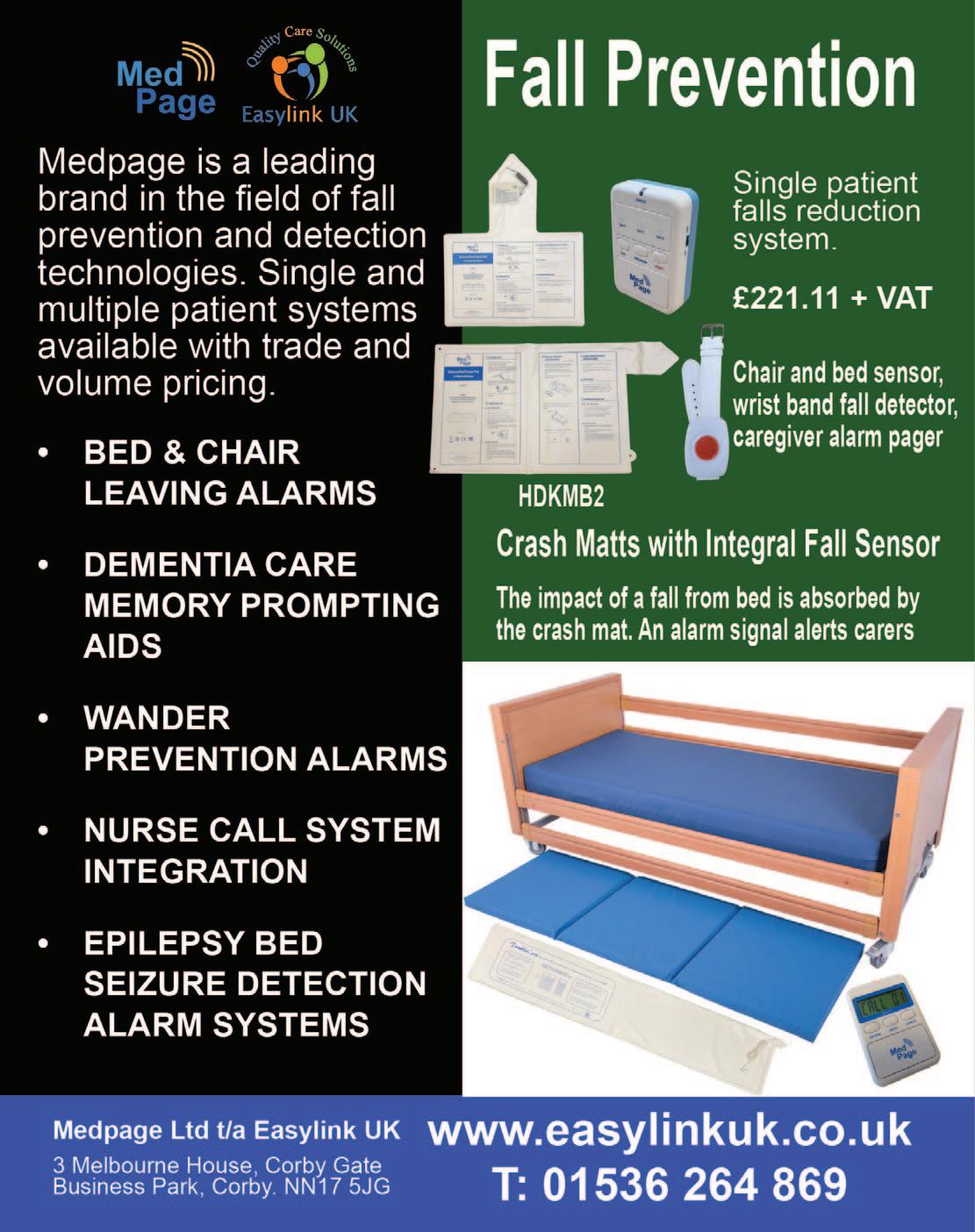
FALL SAVERS ® WIRELESS MONITOR
Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The
Fall Savers®
eliminates the
between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff Bed and chair pads available One monitor works with two sensor pads Integrates with most nurse call systems A variety of options, including: Call button Pager


In the post pandemic world, we have all seen the effects of supply chain problems with the invasion of Ukraine and other alarming global factors, ever increasing costs of living and other more local issues which have driven up the rate of inflation over the last few years. The impact of this meant that most manufacturers of electronic products had to increase their prices as costs spiralled. This, of course, has impacted the end user. The most dramatic impact has been on the Care Industry. An industry that has lacked the support it desperately needs in these trying times.
Courtney Thorne, at the same time, took a strategic decision to take a close look at our core products, right down to component level, the objective being to make us less vulnerable to future global supply chain issues, and to reduce the cost of each product with the amin of ensuring that we deliver the same high quality product at a cost protected price. We had to ensure that this would happen without jeopardising the superb lev-

els of support we provide to our valued customer base.
This ground up review involved all departments from Research and Development right through to the Field Service team (and everything in-between). This in-depth collaboration took time as we had to ensure that each and every element was refined, perfected and tested to our (and our customers) rigorous requirements.
Whilst many organisations have limited-time or end of product line offers, we are very pleased to announce a price reduction on our core Connect and Connect Health Nurse Call system ranges. With flexible terms, full integration with Care Apps, celebrated service delivery and the most reliable and robust solution now at a new lower price, there has never been a better time to talk to us about a new nurse call system.
For more information email us at: info@c-t.co.uk or see the advert on this page.
Blaucomm’s Nurse Call Messaging Service (NMS) is the market leading solution to remove the dependency on noisy nurse call panels and pagers, through its intelligent software, which delivers the alerts straight to the care staff who need them. Care homes are rapidly introducing smartphones for digital care planning and eMarnow, the same devices can be used to receive the nurse call alerts they need for the residents under their care.
Furthermore, Blaucomm NMS is deeply linked into Person Centred Software MCM, so call bell data is linked straight to care plans. This unlocks a huge benefit to care homes to enhance the staff performance with how they accept and respond to residents, which ultimately promotes better response times and visibility for management to audit their performance.

The best part is that Blaucomm NMS links into your existing nurse call system - we work with all major
brands such as Aidcall, ARM, Courtney Thorne, C-TEC, ENS, Intercall, Medicare, SAS and TeleAlarm.
Care operators are constantly recognising Blaucomm NMS for its reliability and dependability to their care operations, which is why we’ve been chosen time and time again over other solutions.
Head of IT Trudi Harrow at WCS Care had this to say about Blaucomm NMS:
“We find Blaucomm is a genuinely fantastic company with a reliable product.
"We would highly recommend this to anybody who wants to replace expensive pagers and silence those annoyingly loud nurse call screens!”
To find out more about Blaucomm NMS, visit
www.blaucomm.co.uk/healthcare
See the advert page 5 for more details.
Medpage Limited has collaborated with a leading UK manufacturer of crash mats to deliver a cost-effective tool for falls management strategies. The inclusion of the new TumbleCare full-length pressure mat sensor ensures that should a patient tumble out of bed, an alarm signal is generated to alert care staff to the incident, resulting in a recordable improvement to patient safety and service.
Crash mats act as a protective barrier, absorbing the impact of a fall and reducing the risk of serious injuries when a person tumbles out of bed. Beneficial for individuals who are at high risk of falling, such as older adults, patients recovering from surgery, or those with neurological conditions such as epilepsy.

Falls can pose significant risks, especially in healthcare settings and senior care facilities. Every year, thousands of people suffer injuries due to falls from beds and other furniture. To prevent these accidents and ensure the safety of patients and residents, it is essential to implement effective falls and safety management strategies.
Further details can be obtained by telephoning 01536 264 869 or emailing sales@easylinkuk.co.uk
See the advert on page 2 for details.

The care sector faces unprecedented challenges. A growing elderly population with increasingly complex needs, coupled with a shortage of qualified staff, puts immense pressure on care homes. But amidst these difficulties, technology offers a beacon of hope. We at 9Solutions, want to be at the forefront of tackling these issues, providing innovative solutions designed to empower caregivers and enhance the quality of life for residents.
Our location-based solution, with customizable safety zones and realtime alerts, allows for proactive intervention, ensuring resident safety while preserving their independence. Picture a fall occurring in a quiet corner. Instant notifications, pinpointing the exact location, enable staff to respond swiftly, minimizing potential harm.
Efficiency is key in today's demanding care environment. Care home staff are bombarded with alarms, leading to "alarm fatigue" and delayed responses. Our system personalizes alerts, directing them to the right caregiver, reducing workload and improving efficiency. One app manages calls, tracking, and tasks, allowing staff to focus on providing care.

Remote communication tools allow staff to check on residents virtually, reducing unnecessary physical rounds and minimizing disruptions. This frees up valuable time for personalized care and meaningful interactions – the heart of quality caregiving.
We understand that technology should be a support, not a burden. That's why our user-friendly system, developed with care professionals, combines diverse functionalities into a single intuitive platform. This min-
imizes the learning curve, allowing staff to focus on providing exceptional care. Crucially, it also integrates with Care Management softwares, ensuring smooth workflows and easy adoption.
BENEFITS OF 9SOLUTIONS TECHNOLOGY
Reduced workload: Automation and intelligent systems streamline tasks, easing the physical and emotional burden on caregivers.
Enhanced safety: Proactive alerts and location tracking ensure resident wellbeing and peace of mind for families.
Improved efficiency: Optimized workflows and personalized task management empower staff to deliver timely and effective care.
Increased resident satisfaction: Technology fosters independence while ensuring prompt assistance when needed.
The future of care is not about replacing human touch with technology, but about using technology to create space for more of it. It's about empowering caregivers, promoting resident well-being, and reimagining care in a way that prioritizes human connection.
Read more or contact us at www.9solutions.com or sales@9solutions.com

Technology has made people more connected with the world around them and the revolution in assistive care devices has made it possible for the elderly to spend their last years in a comfortable and familiar environment. These devices have also made it easier for home carers to provide quality care for their loved ones while managing their own lives. They allow you to care for your elderly whether they are travelling in the city for errands, staying alone at home, or staying in the same home as you. They are also helping nursing homes provide better care for them with discrete monitoring and quick responses to emergencies.

If you’re looking for these kinds of assistive care devices for your loved ones or nursing home, Frequency Precision produce some of the best systems available to help you with elderly care and mobility monitoring, ranging from bed, chair and floor sensor mats through fall monitoring and GPS tracking to fully integrated nurse call plug or wireless systems.
Phone: 01837 810590
Email: contact@frequencyprecision.com
Website: www.frequencyprecision.com


Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being.
We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or Live Chat on our website, our team is always ready to offer advice and help you find just the right products to bring your ideas to life.
While we embrace the convenience of technology to expand our resources and share knowledge, we remain firm believers in the irreplaceable power of sensory

Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem. As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven Antimicrobial PVC with silver

ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk See page 6 for details.
MOWOOT II – proven solution to chronic constipation without medication
Developed by a team of doctors and other healthcare professionals, MOWOOT II performs gentle abdominal massage to speed up intestinal passage in people experiencing chronic constipation.
Clinically proven, safe and effective, relaxing and sideeffects free, MOWOOT II Abdominal Massage Therapy System combats constipation and provides soothing relief to affected people.

Easy to use and comfortable, the MOWOOT II treats and manages constipation in people with spinal cord injuries, multiple sclerosis sufferers, Parkinson’s Disease patients and people with constipation related to prescription medication. MOWOOT II also helps to relieve idiopathic constipation experienced by menopausal and post-menopausal women
Consort Claudgen’s innovation in the electric heating industry takes another leap forward by introducing Wi-Fi-enabled heaters to their low surface temperature (LST) range. These cutting-edge heaters offer unparalleled convenience and efficiency. The heaters connect directly to Wi-Fi, enabling users to control heating through the digital control panel on the heater or via the Consort Connect app. With a comprehensive 7-day timer, which allows 24 individual heating periods per day, and features such as a lock function, open window detection, and custom automation, users can tailor their heating needs to their preferences. Adding to the ease of use, users can view the
and older and elderly people.
In clinical studies
MOWOOT II increased evacuation frequency, softened stools, improved regularity, reduced gasses, relieved bloating and eased off abdominal discomfort.
10 to 20 minutes daily of relaxing abdominal massage with MOWOOT II rapidly reduces symptoms of constipation. Evident results are experienced only a few days after the first treatment. Regular abdominal massage with MOOWOOT II ensures lasting health benefits and better quality of life.
MOWOOT II – effective solution to chronic constipation for better quality of life!
Supplied by Win Health Medical Ltd - 01835 864866 - www.win-health.com
See page 3 of this issue for other Win Health products.

energy consumption statistics of all connected heaters, providing insights into usage patterns and potential savings. The LST heaters with Wi-Fi and occupancy sensors have a self-learning control ability. They utilise inbuilt occupancy sensors to detect and learn a user’s weekly presence in a room, creating an intuitive heating schedule. When the space is unoccupied, the heater conserves energy by switching to a setback temperature or frost protection mode.
BIM (Building Information Modelling) objects for the heaters are available for download from Consort’s website. 01646 692172 | sales@consortepl.com | www.consortepl.com See the advert on page 6.
engagement. That’s why we continue to make our Reminiscence Kits and Sensory Bags with real, tactile items that stimulate the senses. Some experiences—like popping bubbles for the splash, breathing in a familiar scent, or piecing together a puzzle with others—simply can’t be replicated on a screen. These sensory moments are invaluable in encouraging storytelling, sparking memories, and fostering conversation.
Our values remain rooted in this commitment to meaningful connection. We’re here to partner with you—the professionals on the front lines of care—to create a sense of structure, well-being, and fun for those who need it most.
Are you longing for your activity diary to be full? Look no further www.activitiestoshare.co.uk are here for you! See the advert on page 7 or: customers@activitiestoshare.co.uk
0117 966 6761
07900 6751 50
C&S Seating Ltd have provided postural control equipment to residential homes, hospices, medical equipment services and NHS trust hospitals nationwide since 1991.
With 9 different sizes of TRolls and Log Rolls, in a removable and machine washable Waterproof Titex or Soft Knit material. These rolls are used to control posture and position of the body in either supine or side lying. Our Knee & Leg support wedges are

“Jolly
The new “Jolly Journey” from Little Islands is designed to simulate an old-fashioned travel carriage, featuring real wood panelled wall, brass luggage racks, ornate wall lights and table lamp, opposite-facing seating for four, including cushions, ‘First Class’ antimacassars and period memorabilia.
The Jolly Journey creates a familiar and stimulating environment for ‘passengers’ to return to their fondest memories, sparking conversations of time gone by. Reminisce about travel and holidays with loved ones

and furnish your opulent ‘First Class Carriage pod’ with all accessories and footage. All we require is 2.5M of clear wall space, a power socket and good access, to create your very own Jolly Journey. For more information please contact Little Islands: 01828 869802 or see the advert on page 5.


PASS supports over 1,000 care providers every day, giving them access to market leading care management tools hand in hand with unlimited 24/7/365 support from our dedicated and friendly PASS team.
Assured by NHS Transformation Directorate, PASS provides a secure platform that allows you to plan, record and evidence the care you deliver. The only assured solution built specifically for the home care sector, it provides comprehensive real-time functionality and allows you to share progress against outcomes with customisable, exportable reports.
CARE PLANNING AND ROSTERING FROM A SINGLE PLATFORM
To meet the wider needs of the PASS community All-in-one PASS has recently been launched , bringing advanced rostering functionality to our established digital care planning platform. As a result advanced staff scheduling, payroll and invoicing functionality is now seamlessly linked with care planning and reporting, reducing the technical complexity, risk and overhead associated with integrating two separate systems.
As a result, PASS now provides an all-in-one suite of digital care management tools, available from a single platform, designed to:
Save you time
Increase the efficiency of your teams
Improve the quality of care
Deliver better outcomes
INTEGRATED HEALTH AND SOCIAL CARE
Our commitment to the continual evolution of PASS is further illustrated by the addition of GP Connect. The first product of its type to offer this feature, PASS is still one of only a handful of digital care management solutions to have completed this NHS Digital integration, and is the only one offering it to the home care market. PASS GP Connect provides authorised social care staff with realtime access to their client’s GP records. It makes medical information available when and where it is needed, leading to improvements in both care safety and outcomes:
Visibility of allergies, vaccinations and medications, especially useful for clients unable to reliably share their personal information
Using medical information to inform care planning
Ensuring that the right medication is delivered to the right person in the timeliest manner. In one case, this allowed the administration of antibiotics on a Friday evening, aiding the service user’s swift recovery from infection
Available to all PASS users at no additional cost, PASS GP Connect is significantly more efficient than waiting for a GP response. It’s also a positive step forward on the path to the DHSC’s goal for widespread digitally enabled care and is in full alignment with their ambition for joined up care for everyone.
Get in touch: www.everylifetechnologies.com hello@everylifetechnologies.com
Envivo Group is at the forefront of care and support sector, driving innovation that enables people to live lives full of choices and opportunities. They have 202 locations that are now using Mainteno Facilities Management software.
“Our experience with Mainteno at TLC/Envivo Group has been really positive already. Since its rollout it has shown real and measurable benefits and has had a marked impact on the workload and assurance of our operations team.
"We can now raise issues whether large or minor, almost the instant they are spotted. We can denote the priority with which they need to be tackled and track the progress of works to rectify them. It has reduced almost completely the need to be directly contacting people to resolve issues. It has been obvious that the streamlined approach that it provides helps in prioritising works for maintenance teams and contractors, gives them plenty of detailed information
as to the exact issue and has given us an evidence base to show that issues are resolved in a consistent and effective timeframe.
"The details that are available once a job is logged are invaluable. We can evidence to regulators etc that there are plans to rectify any outstanding works that they may pick up. I've been very impressed with the details that are passed back to me through the platform as works are ongoing and also when they are completed. It's proved to be a valuable reference to ensure that we are not doubling up requests, working through tasks in a logical way and also to confirm the completion of works remotely.
"For a site of our size and complexity especially, a toolkit with this level of effectivity and scope has been an incredible help.”
Group Facilities Manager sales@redro.uk www.mainteno.com



The social care sector is evolving at an unprecedented pace, driven by increasing demand, tightened budgets, and the need to deliver exceptional care outcomes. At the heart of this shift lies digital transformation—a holistic approach to overhauling care operations, processes, and culture through the integration of modern technologies.
Far from simply replacing manual tasks, digital transformation reimagines how organisations operate. Tools like Digital Social Care Records (DSCRs) represent just the beginning. By adopting interoperable systems and cloud-based solutions, care providers can achieve seamless coordination across departments, optimise resource allocation, and ensure high-quality care. Processes such as care planning, rostering, compliance reporting, and data management become more efficient, freeing up teams to focus on providing person-centred care.
Digital solutions also offer significant benefits. Faster service delivery reduced administrative burdens, and more informed decision-making results in better care experiences for service users and care providers alike. For instance, interoperability enables real-time data sharing across platforms, reducing errors while providing a unified view of the organisation’s operations. This empowers leadership to make critical decisions backed by accurate, holistic insights. Additionally, tools like single sign-on (SSO) and multi-factor authentication bolster security, ensuring confidential data remains protected while reducing day-to-day inefficiencies for users.

For social care providers, the move toward digitalisation represents an investment in long-term sustainability. Enhanced efficiency helps reduce operational costs, allowing resources to be reinvested in vital areas such as workforce development or service user engagement. Standardised digital frameworks also simplify the complexities of acquiring new services or locations, ensuring continuity of care during periods of growth. Choosing a digital partner who understands the complexities of care is essential to navigating this transformation successfully and tailoring solutions to the unique needs of the sector.
However, the path to digital transformation requires a clear roadmap. Providers must assess their needs, define a vision, and secure stakeholder buy-in. Selecting the right software and delivering effective training is equally critical to ensuring a smooth transition. Continuous monitoring and adjustment allow providers to refine their approach, fostering a culture of improvement and resilience.
By adopting integrated intuitive software solutions, social care providers can not only stay ahead of industry challenges but also lead the way in delivering exceptional, sustainable services. Digital transformation may not solve every challenge, but its potential to enhance care quality, operational efficiency, and financial health is undeniable.
Visit OneAdvanced at stand H24 at UK Care Week to learn how we can support your journey or download our guide to digital transformation with the QR code.
SFIncS r/3 - A Fee Income System especially for Residential and Nursing Care Homes
Designed to deliver simplicity and ease of use coupled with speed, flexibility and accuracy, SFIncS r/3 (Simple Fee Income System release 3) has a proven track record of over 12 years in use.
Originally developed and prototyped as an MS Access database, since 2017 SFIncS r/3 has lived entirely on the cloud, so is available 24/7 from anywhere in the world.
As a completely bespoke package, born of necessity and collaboration between seasoned software consultants with ties to the care industry, SFIncS r/3 offers innovations and capabilities not found in any other system.
Separation of sponsor and service user responsibilities permits unlimited sponsor/service user relationships, and as any number of charge codes may be defined, this allows complete flexibility of service user/sponsor /charge code definition.
Its unique continuous billing function is the most efficient means possible of defining recurring charges (an entry is only required when a change occurs) and both an ad hoc charge function and a
cashbox module are available for incidental expenses (either or both can be used).
Use of the balance forward accounting principle (which makes unnecessary invoice matching a thing of the past - though invoicing is included) plus super quick receipts entry using just ‘six clicks’ makes SFIncS r/3 almost effortless to use.
Paula, who owns and operates Monkstone House Residential Home in Porthcawl testifies to it’s incredible prowess: “With 41 partly private and partly sponsored service users, some of whom are multiply funded, it takes me only 30 to 40 minutes per week to keep both my accounts and fee income up to date! More importantly, I never need to worry about underpaid or overpaid fees - everything is always spot on. And the invoices and statements produced let me present the polished and professional image I need.”
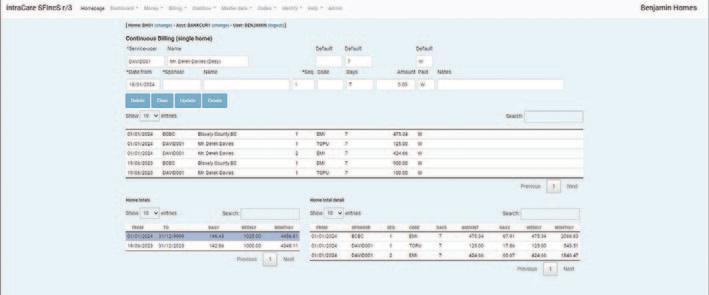
SFIncS r/3 integrates easily with any accounting package, can be used by any type of care home and by single or multiple home operators alike.
For more information email benjones@intracare.co
Better by Design: A Fee Income System especially for Residential and Nursing Care Homes
We've analysed every aspect of fee income processing to the nth degree and developed a bespoke solution that delivers simplicity and ease of use coupled with speed, flexibility and accuracy – all in one outstanding application package.
SFIncS r/3 is the ultimate fee income management and control system.
• Unlimited sponsor and charge code assignments allow complete flexibility of service user billing profiles.
• Perfect for all types of care homes - Nursing, Residential, Mixed, Specialist.
• Unique continuous billing functionality provides the most efficient charge definition possible. Only charge start points need to be maintained and all sponsor charges for each service user (including historic) are shown on just one screen.
• Completely flexible invoicing. Invoice any sponsor at any time for any charges for any service user for any period of time.
• Super fast receipt entry including ‘Six clicks’ copy functionality.
• Balance forward accounting means you can forget laborious invoice matching.
• Ad hoc charges functionality.
• Cashbox module included.
• Works for multiple or single home operators.
• Integrates with any accounting system.
• Plus all the reports, views and graphs you’ll ever need.
• In use for over 12 years.
• Free training and help with system set up.
• Historic data loading option available (charges may apply).
• 30 day free trial.
For a demo, free trial or for further information please email benjones@intracare.co or visit https://intracare.co/
By Dr Angela Brown, Founder and Chief Executive Officer of Training

several quick and easy changes which the government
could swiftly implement to significantly improve the sector in the shortterm.
A start would be to focus recruitment on the individual progression plan of the care worker. Afterall, surely a sector which traditionally has poor pay and responds to ever changing societal needs, deserves some control over what are perceived are important skills.
The sector still relies on recruitment via word of mouth and offers low pay and low recognition of the skills required in adult care as an incentive. While the workforce needs to respond to the needs of employers, we have a duty to understand the needs of the carer by providing progression of their own career pathway.
The early years sector faced a similar challenge with public perception. Since no one needs a qualification to have a child, it was perceived by many – and even some in government – that the skills required to work in the sector simply came natural.
Although the early years sector has not yet chased all of its demons, public perception of the skills required undertook a change andlargely helped by the excellent Sure Start system - parents began to understand the value of having a skilled workforce to look after our children. It seems an alien concept to us now, but it is very much where we’re at with care, and it doesn’t need to be that way.
In care today, we’re constantly seeing headlines of endemic staff shortages and staff burnout, but this could be significantly improved if the expectations of the sector are proactive rather than responsive.
This is what the Commission may conclude, but in the short-term, we need to invest in the current army of the workforce whose goodwill and compassion is relied upon to respond out of decency rather than an identified societal need.
Demands on the NHS can also only be supported by an adult care sector which is respected for the skills they possess.
For 2025 to herald in some immediate change, let’s utilise Government skills funding and Department of Social Care workforce development programmes to really drive the sector forward.
Let’s find out what the people receiving care really want from their care plan and let them have a say in what the devolved authorities are spending on.
Let’s be ambitious and listen to the sector, use its expertise and plan for a service which not only works well in conjunction with the NHS, but one which is respected and rewarded.
Let’s make 2025 the year we start seeing real change in the care sector.

In the ever-evolving landscape of adult social care, it is essential to ensure that training initiatives not only equip care professionals with the necessary knowledge and skills but also nurture an environment where they feel confident and supported to deliver their best.
As a Registered General Nurse with over two decades of experience in the care industry, I have seen first-hand how thoughtfully designed training programmes can bring about meaningful changes that resonate with both staff and residents. These programmes, when aligned with the real-world needs of care professionals, have the power to transform not only the quality of care but also the overall morale and satisfaction within the care setting.
One of the key features of impactful training is its accessibility, relevance, and applicability to the challenges faced by care staff on a daily basis. From comprehensive first aid instruction to specialised courses on dementia care, well-designed training modules can provide care professionals with the tools and techniques required to respond effectively to a variety of situations. By prioritising the development of our staff's clinical proficiency, we enable them to deliver high-quality, person-centred care that focuses on the well-being and dignity of residents.
However, building confidence and capability goes beyond technical skills alone. It is equally vital to focus on the interpersonal skills that underpin meaningful relationships with residents and contribute to their overall happiness and fulfilment. Training programmes that emphasise relational care, for instance, can help care staff appreciate the importance of creating an atmosphere of trust and understanding. By
encouraging staff to focus on these human aspects of care, we cultivate a setting that radiates warmth and kindness, ensuring that residents feel valued and respected.
Moreover, to ensure that staff can consistently provide the best possible care, our training must remain adaptable and responsive to emerging trends and best practices in the sector. By implementing regular refresher courses, we reinforce foundational knowledge, address any skill gaps, and ensure that care professionals are up to date with the latest advancements. Similarly, ongoing supervision and performance evaluations play a vital role in identifying opportunities for professional growth, creating a framework of accountability and continuous development. This commitment to lifelong learning not only enhances the quality of care but also reinforces a sense of purpose and pride among staff.
The ripple effect of robust training programmes extends far beyond individual care professionals. When staff feel confident, valued, and well-equipped, they are better positioned to deliver exceptional care that is tailored to the unique needs and preferences of each resident. This, in turn, results in improved well-being for residents, greater peace of mind for their families, and stronger outcomes for the care community as a whole.
At the core of our training philosophy lies the understanding that empowered staff lead to empowered residents. When care professionals are equipped with the knowledge, skills, and assurance to excel in their roles, they are better able to encourage residents to maintain their independence, involve them in decision-making, and take the time to truly listen to their stories and concerns.
In conclusion, aligning training with the practical needs of both staff and residents goes far beyond fulfilling regulatory requirements—it is the foundation for fostering confidence, compassion, and excellence in adult social care. As we look ahead to the challenges and opportunities of the future, let us remain steadfast in our commitment to investing in our staff, enabling them to make a lasting difference in the lives of those they care for.
By Elena Martin, Director
of
Operations
and Commissioning, Langdale Care Homes Group (www.langdalecarehomes.co.uk)
By Daniel O’Shaughnessy,

You wouldn’t run a care home without a health and safety lead, and the same should apply to data security and protection leads. Losing access to critical data, even briefly, can be devastating for residents’ welfare and your business’s viability. If care plans and medication records are unavailable due to a cyber incident or software issue, residents’ wellbeing is at risk.
Finance system failures can disrupt payroll, invoicing, and payments.
While data protection is everyone’s responsibility, having a named individual to lead on data security and protection is essential. This role provides senior leadership and ensures good practices are followed across the organisation. At Digital Care Hub, we use the term data security and protection lead to describe this role.
The lead should champion data security policies and set an example. While daily tasks can be delegated, the lead ensures standards are met. This role doesn’t have to fall to the Registered Manager but should be assigned to someone senior enough to oversee responsibilities effectively. In larger organisations, aspects of the role can be shared – for instance, one person might manage risks while another handles information governance.
It’s vital that leads have the right knowledge and skills. To address training gaps, Digital Care Hub’s Better Security, Better Care programme has launched a free, open-access elearning course tailored for data security and protection leads. This complements an existing course for all staff, which we recommend completing first.
The course, launched in January 2025, supports continuing professional development (CPD) and meets the training requirements of the Data Security and Protection Toolkit (DSPT). It is the only free resource designed specifically for this role in adult social care.
The training reflects real-world scenarios across care homes, supported living, home care, and community services, covering all client groups. The course includes four modules:
1. Data protection rights and responsibilities
Covers the lead’s responsibilities, other specialist roles, and key skills and
support needed for the role.
2. Keeping data secure
Explores managing data, understanding personal data rights, access to data, Information Asset Registers, and Data Protection Impact Assessments.
3. Threats to data security
Focuses on recognising, preparing for, and recovering from cyber incidents; reducing threats to digital systems, devices, and supply chains.
4. Data breaches
Explains how to differentiate between breaches, incidents, or near misses; record and learn from incidents; and respond to and report breaches appropriately.
By completing this course, data security and protection leads will enhance their knowledge of data protection and cyber security, ensuring they can safeguard their organisations, staff, and the people they support.
For more information about the course and other resources, visit www.digitalcarehub.co.uk/elearning.
Leanne Silverwood is the Founder and Managing Director of Local
Care Force

As Local Care Force celebrates 20 years of business, we look back on two decades of momentous changes in the health and social care sector. From technological advances to ongoing recruitment and retention issues, supply chain management companies driving down prices and quality, and changes to the agency landscape, the health, and social care sector, post-pandemic, has not only had to adapt but has also needed to rise to meet these challenges.
In 2020 the health & social care sector faced a devastating crisis in Covid19.
Care home staff were under unimaginable pressure, working long hours, managing PPE shortages, and the emotional toll of caring for residents who were isolated from their families. We had to adapt quickly, deploying staff where they were most needed, while maintaining their safety, and that of the residents they cared for. It demonstrated the resilience and dedication of our workforce - and we are so incredibly proud of the commitment they showed throughout this difficult time.
Post pandemic the issue of recruitment worsened. In 2023 the health & social care vacancy rates stood at 152,000 roles (9.9%) substantially higher than the overall UK rate of 3.4%. It was a challenging time, to say the least. Alongside issues around recruitment, were problems with retention which significantly impacted the health and social care landscape, with 390,000 (28.3%) leaving the sector in 2022/23. (The Kings Fund 2024).
As a health & social care agency, Local Care Force has been at the forefront of this ongoing crisis. The ever-growing demand for qualified healthcare professionals has proven to be a difficult obstacle to over-
come. Our role in providing experienced, skilled, and compassionate staff has never been more critical, or difficult, and it is the reason we offer specialist in-house training led by our clinical lead nurse, who also acts as a mentor to our team.
The agency sector has not been immune to challenges post-pandemic. In the past, agencies were regulated by the CQC, but for several years now, they have been unregulated. This lack of oversight has led to a surge in "back bedroom" agencies, which supply staff without conducting the necessary checks to ensure resident safety. Additionally, these agencies often disregard tax regulations when paying staff, leaving care homes liable for tax shortfalls. Consequently, we advise all clients to question any £14 hourly carer charges, as it has become easier for anyone to recruit and place nurses in care homes. This trend is particularly concerning, as we pride ourselves on our robust recruitment and safeguarding processes to ensure the wellbeing of the residents our staff support.
The Work Rights Centre report has highlighted another troubling issue within the industry: the flawed sponsorship visa system and the exploitation of foreign workers in the health and social care sector.
Migrants constitute 32% of care worker roles in England, many of whom face excessive hours or underemployment, struggling to change visa sponsorship, and fearing reprisals if they voice their concerns. As an agency, we cannot recruit staff requiring visas. However, we are disheartened to see hundreds of people on sponsorship visas applying for work with us due to unscrupulous agencies exploiting legal loopholes. We frequently hear from individuals who aren't receiving enough work from their sponsors to sustain themselves, yet they cannot legally work elsewhere without invalidating their visas. The well-being of our workforce has always been paramount at Local Care Force. We firmly believe that protecting our staff, which in turn, protects the residents they support, a principle on which Local Care Force prides itself.
As we reflect on our two-decade journey, acknowledging the significant challenges we have faced, it's equally important to celebrate the positive advances we have made during this time.
We know that with dedication, collaboration, and a focus on innovation, we can continue to weather the storm. As we celebrate this milestone, we are committed to providing the highest standard of care and supporting the health & social care sector in whatever challenges the next 20 years may bring.
The delivery of safe care is the paramount responsibility of social care providers. Central to achieving this is the governance framework adopted by service providers. And at the core of this framework are policies and procedures. These enable the provider to comply – and evidence compliance – with relevant legislation and regulations, as well as facilitating best practices, supporting business needs, and assisting in recognising and managing risks.
Providers have a legal duty of care to the people they employ. Policies and procedures should provide clear guidelines to staff on how the organisation operates, as well as informing them of best practices and processes to be followed.
Policies should be reviewed annually as a minimum to ensure they are still fit for purpose and align with legal and regulatory requirements. They should be reviewed not only by employees of the business, but also by experts in various subject matters (e.g.,

infection control or medicines management).
For many small- to medium-sized providers, there may not be the in-house skills, knowledge, and experience to complete such a robust annual review. Many choose instead to purchase their policies and procedures from a reputable provider like W&P Compliance & Training, who will also complete reviews and ensure their policies and procedures remain up to date. This way a provider not only ensures they remain compliant; they also benefit from best practice policies and procedures that provide a solid foundation for safe working practices and – ultimately – protect and support service users and staff.
Ben Erskine – Director at W&P Compliance & Training www.wandptraining.co.uk | Tel: 01305 767104 See the advert on page 2 for further information.
Training care home staff is vital for delivering high-quality care, especially when managing complex resident needs such as dementia, frailty, and mental health challenges. However, traditional methods often fall short in engaging staff, leaving critical gaps in understanding and preparedness. Innovative approaches, such as game-based learning and peer-to-peer collaboration, are revolutionising training, particularly in addressing the ethical and legal challenges of restrictive practices.
Restrictive practices—measures that limit an individual’s freedom—are sometimes necessary to ensure safety. However, they must be applied with great care, adhering to legal frameworks and ethical guidelines to protect residents’ dignity. A groundbreaking digital training resource, codesigned by Queen’s University Belfast and Focus Games, exemplifies this innovation. The resource uses interactive, expert-driven content to help staff navigate restrictive practices responsibly and effectively.

Game-based learning plays a central role, transforming topics like restrictive practices into engaging,
real-world scenarios. Simulations allow staff to explore ethical dilemmas, practice decision-making, and test alternative solutions in a safe, low-pressure environment. This approach enhances critical thinking, teamwork, and retention of essential knowledge.
Peer-to-peer learning further strengthens the training by encouraging staff to share experiences and insights, fostering collaboration and practical problem-solving. This creates a dynamic learning environment where staff feel supported and empowered to deliver compassionate care. By integrating these modern approaches, care homes can elevate training into a meaningful experience, equipping staff to balance safety with residents’ autonomy and dignity. At Focus Games, we are proud to offer tools designed to empower care home teams through innovative training. Visit www.FocusGames.com or email info@focusgames.com to learn more about our Restrictive Practice resource and how it can enhance care home outcomes for
At Meaningful Care Matters, we have the privilege of working with health and care teams across the UK, Ireland, Canada, Australia and more recently Singapore.
It is no surprise that those who can embrace the culture change of our ‘Butterfly’ and ‘Dragonfly’ Approaches - in terms of reducing the institutional and task-focused aspects of care in favour of creating a sense of fun, friendship and true belonging - have leaders who are very self-aware and emotionally intelligent. What does that look like in practice? It involves being genuine as a person, being able to acknowledge mistakes, and taking time to really get to know your team members as individuals and what makes them tick. Our team are Authorised Partners in delivering the methodology of the DiSC personality profiling assessments and the Five Behaviours of a Cohesive Team™ programme (Lencioni, P) to help support teams to work together more positively and ultimately productively. Having been through the process myself, it was striking how accurate the analysis was of what motivates and what stresses me. It also helped me to know those stressors and motivators for my peers and how to adapt my approach to better look out for each other.

our own relationship with trust, based on experiences in our lives? Do we find it easy, or does it take us time? Being in touch with your own vulnerability is not about spilling out all your deepest, darkest secrets to the people you support! But it is about being able to reflect on times in your life when you have felt lonely, scared or lost, and for these reflections to enhance our empathy for those who are struggling. Once we have established trust and a sense of belonging in our teams, we can more easily be open about the things we disagree about, and for those differences or conflicts to be regarded as healthy rather than threatening to the stability of a team - provided they are talked about openly and kindly. Many teams flounder because there is an artificial harmony i.e. conflicts are under the surface and gossip and cliques can create an unsafe and unhappy work culture.
A recent social media post caught my eye which said “Your company culture is not words on your website or posters on the wall. It’s how your people feel on a Sunday night.”
What is your response to that question, and do you think you and your team might need some time and attention in 2025 to get back on track and unlock your full potential?
People working in care homes often experience the deaths of residents but this doesn’t mean each death is easier to cope with.
Hospice UK’s Compassionate Employers Programme deliver workshops to help care professionals manage recurring and often overlooked experiences of grief through their work.

Our next virtual session will be on: Wednesday 5 March 2025, 10.00 - 12.30
The cost is just £120 +VAT per person.
At the foundation of a good team is what Patick Lencioni describes as vulnerability-based trust, and this is something we talk about a lot in training for leaders and their teams. People who we care for, and their families put a lot of trust in us. So, what is
Sally Knocker is a Consultant Trainer with Meaningful Care Matters www.meaningfulcarematters.com

Book your space or find out more at: www.hospiceuk.org/coping-professionalgrief-workshop-march

In a landmark ruling, the High Court delivered a significant judgment on 14 January 2025, in favour of Hartford Care Group Limited (HCG), challenging the Secretary of State for the Home Department's (SSHD) decision to reject HCG's application for 70 Defined Certificates of Sponsorship (DCoS). This case, The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department, sets a crucial precedent for how the Home Office assesses applications for Defined Certificate of Sponsorship (DCoS), particularly in the care sector.
THE CASE BACKGROUND
HCG, a prominent provider of care services in the UK, has held a sponsor license since April 2019. On 8 January 2024, Aston Brooke Solicitors applied for 70 DCoS on behalf of HCG. These certificates are vital for nonUK workers to obtain a visa to work in the UK. However, on 29 January 2024, the SSHD rejected HCG's application, citing insufficient evidence to demonstrate a genuine need for additional staff.
Aston Brooke Solicitors swiftly initiated a Judicial Review, challenging the legality of the decision, which could have significant consequences for the care sector, heavily reliant on overseas workers to meet staffing demands and stating HCG contracts with their service users and the Local Authority did not state the number of hours.
THE LEGAL CHALLENGE
Aston Brooke Solicitors argued that the SSHD’s decision was unlawful, irrational, and inconsistent with the Immigration Rules. Aston Brooke Solicitors contended that the Home Office had imposed requirements not set out in the rules, relied on unpublished policies, and failed to assess the evidence properly. In particular, the SSHD insisted on receiving contracts that guaranteed specific hours of work, which Aston Brooke Solicitors argued were not standard in the care sector.
The SSHD defended its position by stating that additional information could be requested to validate the applications THE ADMINISTRATIVE COURT'S RULING
"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-forprofit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So,
On 14 January 2025, the High Court ruled in favour of HCG, stating that it was irrational for the SSHD to require contracts with guaranteed hours to prove the genuineness of care worker vacancies. The Judge highlighted that flexible contracts are standard in the care sector, where the demand for staff can vary depending on factors such as local authority funding and service user needs.
The Judge also criticised the SSHD’s assumption that local authorities impose staffing quotas, pointing out that care providers have discretion over how many workers they need to meet demand. Furthermore, the Judge found that HCG’s evidence adequately demonstrated the genuine need for additional staff, rendering the SSHD’s rejection of the application irrational.
The Judicial Review application was supported by Care England and Professor Martin Green OBE chief executive of Care England stated after the verdict was delivered: “In winning the Judicial Review, Aston Brooke Solicitors has done a great service to the care sector because this victory will cause The Secretary of State for the Home Department to rethink how they behave towards the independent care providers. No one should be in any doubt that when we see unacceptable behaviour, we will be prepared to challenge it and use the law to enforce our rights.”
Gemma Melhuish, People and Culture Director at HCG said: “We are thrilled the court ruled in our favour and agreed their decision was unlawful as it is important for other Care Providers to challenge decisions that are morally not correct. We are now looking forward to welcoming new starters to our Homes from our overseas recruitment campaign undertaken last year and continuing to provide high-quality care to our residents. “
THE OUTCOME AND ITS SIGNIFICANCE
The High Court granted a quashing order of the SSHD’s decision, declaring it unlawful. Aston Brooke Solicitors will now reapply for the DCoS for HCG without the commercial risks associated with the initial rejection.
being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.
Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.

Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox Southernhealthcare.co.uk eden-alternative.co.uk"

Kashif Majeed, Head of Corporate Immigration at Aston Brooke Solicitors said, “For the care sector, the decision has significant implications. It emphasises that the Home Office must assess applications based on realistic criteria that reflect the sector's operational practices. While the SSHD can request additional information to verify the authenticity of job vacancies, it cannot impose unreasonable or unattainable requirements, particularly when those conditions do not align with the realities of the care sector.”
THE BIGGER PICTURE: IMPLICATIONS FOR THE CARE SECTOR
This case highlights the essential role that international workers play in the UK’s care sector, especially in light of the growing demand for care services due to an aging population. The judgment provides clarity for care providers seeking to hire overseas workers, reassuring them that their flexibility in staffing and contractual arrangements will be recognized.
The ruling also sets a precedent for future DCoS applications, ensuring that care providers are not burdened with unrealistic requirements. This decision affirms that decisions made by the SSHD must be grounded in the reality of the care industry, where staffing needs are often dynamic and flexible.
The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department is a major victory for the care sector, ensuring that the Home Office’s decision-making process is fair and aligned with the sector’s operational realities. The case reinforces the importance of reasonable and consistent policies in assessing DCoS applications and provides a vital precedent for care providers looking to hire international workers to meet the UK's growing care needs.
For further information on Ashton Brooke see the advert on the facing page.
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.
From helping clients make their first purchase through to allowing groups to
grow significantly in size we assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.
Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net


• Sponsor Licenses
• Skilled worker Visas ( Carers, Senior Carers, Nurses)
• Commercial Property, Leases, Developments, Sales & Acquisitions
• Commercial contracting & negotiating with Local Authorities regarding fees
• Refinancing
• Partnership agreements
• Dispute Resolution & Litigation
• Advice on Care Quality Commission (CQC) processes
• Assisting Care Providers to make License Applications, Registrations and Representation with CQC
• Wills, Probate & LPAs

