















The Care Quality Commission (CQC) is under intense scrutiny after admitting a substantial backlog in addressing serious concerns raised about NHS providers.
The revelation came as CQC Chief Executive Sir Julian Hartley appeared before the Health and Social Care Committee to discuss findings from last year’s scathing government-commissioned review by Dr. Penny Dash.
Sir Julian Hartley and Chair Ian Dilks disclosed that the regulator is struggling

with a backlog of 5,000 unresolved notifications of concern. These include major issues flagged by providers, staff, and the public, with some cases dating back several months. The regulator processes approximately 800,000 notifications annually but has been unable to address all within the 10-day response target.
(CONTINUED ON PAGE 3...)


The latest findings from the Health and Social Care Committee paint a troubling picture of the Care Quality Commission (CQC), highlighting significant challenges that raise serious questions about its safeguarding capabilities and overall credibility.
These revelations come on the back of last year’s damning review by Dr. Penny Dash, which exposed deep-rooted failings within the regulator’s operations.
The committee’s discussions, as reported in their comments, emphasize that the CQC must urgently address the backlog of 5,000 unresolved notifications, some of which date back months.
These delays as set out by the committee pose a potential risk to safeguarding efforts, and highlighted by Labour MP Jen Craft, who expressed concern over the implications for vulnerable individuals relying on swift regulatory intervention. Compounding this issue are systemic failures in the CQC’s IT infrastructure, which have exacerbated delays and left hundreds of inspection reports trapped in limbo.
It is deeply worrying that such a critical organization appears unable to meet its own standards.
Credibility, once lost, is difficult to regain, and the CQC’s struggles undermine confidence in its ability to uphold safety and quality standards.
While reforms are underway, including changes to assessment frameworks, industry observers remain sceptical about whether these measures will be enough to resolve the root causes of inefficiency and ineffectiveness.
Against this backdrop of regulatory turbulence, it is refreshing to see innovative
Carer is published by RBC Publishing Ltd, 3 Carlton Mount, 2 Cranborne Road, Bournemouth, Dorset BH2
damage. Views expressed within this publication are not necessarily those of the publisher or the editorial team.
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden unless
solutions emerging in the wider care sector. A groundbreaking initiative by Working Chance and Care England (see page 9) aims to break down barriers by encouraging adult social care organizations to consider candidates with criminal convictions during recruitment.
This forward-thinking guidance seeks to address the high reoffending rates in the UK by creating pathways to meaningful employment for individuals with experience in the criminal justice system.
The statistics make a compelling case for such initiatives: in 2021/22, nearly 25% of adults in England and Wales reoffended within 12 months, with the rate rising to over 56% for those serving custodial sentences of less than a year.
Employment is widely recognized as a critical factor in reducing reoffending, offering individuals stability, purpose, and the opportunity to reintegrate into society.
This is not an untested concept. Our sister title, CLH NEWS, has frequently reported on the remarkable success of The Clink Charity, founded by Alberto Crisci MBE.
By providing accredited NVQ training to inmates in prison kitchens, The Clink has achieved one of the lowest reoffending rates in the UK. Fourteen years on, its results are a testament to the transformative power of employment and training opportunities for those in the criminal justice system.
We applaud Working Chance and Care England for championing this cause in the care sector. By fostering inclusivity and recognizing the potential of individuals with past convictions, the sector can tap into a valuable and often overlooked talent pool while making a tangible contribution to reducing reoffending rates.
As we navigate the challenges facing social care, from regulatory reform to workforce shortages, initiatives like these serve as a beacon of hope. At THE CARER, we are committed to spotlighting such efforts and will continue to report on developments that shape the future of care. It is our hope that both the CQC and the wider sector take bold steps toward progress, ensuring that those who rely on care services receive the quality and safeguarding they deserve.
I would also like to encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
I can always be contacted at editor@thecareruk.com


(CONTINUED FROM FRONT COVER)
SIGNIFICANT DISTRESS
A major contributing factor to the backlog is the failure of the CQC’s newly implemented IT system, which has caused significant distress among staff and hampered productivity. Approximately 500 draft inspection reports are "stuck" in the system and cannot be retrieved. Sir Julian acknowledged that IT-related issues are the primary cause of staff stress, low morale, and diminished productivity, with one-third of employees reporting physical and mental health impacts from the system’s challenges
“We currently have approximately 5,000 concerns in the backlog, which have not been addressed within the 10-day response timeframe,” Sir Julian stated. “Given we receive around 800,000 notifications annually, it is imperative to fast-track these cases, prioritizing them based on urgency.
Weekly updates are being provided to monitor progress.”
Andrew George, a Liberal Democrat member of the committee, said his “shocked” colleagues’ “jaws were on the floor when we heard this”.
FAILURES “EXTRAORDINARY”
Ian Dilks, outgoing Chair of the CQC described the IT failures as "extraordinary," citing instances where staff began work on reports only for them to become irretrievable. He noted, "No one would design a system to lose reports in the middle of processing."
“We have reports that go back for some months that are stuck in the system. People can’t get them back out” he said.
“I would love to be sitting here saying, as the outgoing chair, that this organisation is in a much better shape than everybody thought it was, and I can’t say that, for which I am personally very sorry.”
He also told the committee that he had not had regular meetings with the health and social care secretary or the relevant minister under the previous two governments, which Moran said after the meeting was “incomprehensible”.
Dilks said CQC had decided it needed to change in 2018, and had commissioned consultants two years later.
PROBLEMS “OBVIOUS”
It then decided in 2021 to carry out “a much more ambitious strategy”.
But it was not until the end of 2023, when new technology was being deployed, “that the scale of the problems really became obvious”.
He said that some of the strategic decisions were “not the right decisions”, the strategy was “too ambitious”, the technology failed to “deliver”, and CQC failed to “engage well enough” at the beginning of the process with its own staff.
Labour MP Jen Craft expressed alarm about the backlog’s potential to jeopardize safeguarding efforts, noting that some unresolved concerns date as far back as November 2023. This delay risks undermining public trust in the CQC’s ability to uphold safety and quality standards across NHS providers and care homes.
Sir Julian further admitted that some cases awaiting review date back months, with the oldest unreviewed notifications from November 2023, and the oldest without action dating as far back as August 2024. The CQC
has committed to providing the committee with a detailed update to clarify the status of these cases.
Layla Moran MP, chair of the committee, described the situation as deeply concerning. She emphasized the need for urgent improvement, stating:
“We are shocked by the extent of the backlog at the CQC. It is critical that the regulator moves swiftly to address the deficiencies highlighted in the Dash review. We will closely monitor their progress to ensure they restore credibility and fulfil their obligations to providers and the public.”
The findings of Dr. Dash’s 2023 review revealed widespread failings within the CQC. It concluded that the regulator had “lost its credibility” among the providers it oversees, undermining trust in its ability to ensure quality and safety.”
An internal review conducted by the CQC concurred with these findings, recommending a “fundamental reset” of the organization. It warned that without structural reform, the regulator would struggle to achieve its objectives.
In response to the reviews, the CQC has implemented significant changes to its assessment framework. It has revamped its scoring system, now focusing on quality statement-level scores to enable faster assessments.
The Dash Review was not the only report highlighting the CQC’s struggles. An internal review conducted by the regulator itself found that its current structure is incapable of meeting its objectives, calling for a "fundamental reset" of the organization.
In response, the CQC has implemented changes to its assessment framework, including a shift to quality statement-level scoring, to expedite evaluations. While these measures aim to improve efficiency, critics argue they fall short of addressing systemic issues.
Sir Julian also indicated that the controversial use of single-word ratings, which has drawn criticism from care providers and GPs, will remain under review. He acknowledged the need for clarity and simplicity for the public but emphasized the priority of addressing internal inefficiencies first.
Despite the CQC’s assurances of "urgent action," the regulator faces immense pressure to restore its credibility and effectiveness. With both internal and external reviews highlighting significant failings, stakeholders across the sector are calling for transparency and decisive reform.
A spokesperson for the CQC stated: “We recognize the urgency of addressing these issues and are committed to delivering more assessments at a faster pace. These changes represent just one aspect of our broader effort to reform and rebuild trust in our operations.”
The backlog raises broader concerns about the impact on safeguarding and the credibility of inspections. Care sector leaders have long stressed the importance of timely, transparent, and effective oversight, especially given the pressures faced by providers across the UK.

By Dr Jane Pritchard, Consultant Admiral Nurse at

Alzheimer’s Research UK’s analysis that dementia is now the leading cause of death in England and Wales is a stark reminder of the vital importance of the government actioning its 10-Year Health Plan, to “future-proof” NHS dementia services.
Alongside this, the UK’s population is ageing, with Centre for Ageing Better revealing that the number of people aged 65-79 is expected to increase by nearly a third in the next 40 years, while the number of people aged 80 and over is expected to more than double. Dementia is extremely common, with 1 in 11 people over the age of 65 being diagnosed with the condition in the UK, according to the NHS. It is also estimated that by 2030, the number of people living with dementia in the UK will be more than 1 million. This emphasises the need for scalable, sustainable care models.
As an Admiral Nurse (specialist dementia nurse) working for a live-in care provider, I have had the privilege of witnessing the profound positive impact care at home has on individuals living with dementia, and their families. Ensuring adequate funding for at-home care is crucial,
enabling people to remain in a familiar environment, reducing stress, confusion and anxiety.
THE ROLE OF HOME CARE IN ENHANCING WELLBEING
People living with dementia can thrive in familiar environments, and sustaining routines has been found to improve social and functional abilities, as well as offer greater comfort, which in turn reduces agitation.
It also plays a preventative role in reducing unnecessary hospital visits through people being better able to manage their health issues through continued monitoring from dedicated carers. With proper medication management administered at home, this can lower readmission rates for people living with dementia.
Home care can also foster stronger connections between family members as it allows them to stay actively involved in their loved ones’ lives. Research has shown that this can improve health and quality-oflife outcomes in dementia.
The Good Care Group’s recent study reinforces the importance of home care for fulfilling people’s desire to age in place, revealing that 41% of survey participants said their home is crucial for their mental health, with over half (58%) stating they would be ‘devastated’ if they had to leave their homes.
Alongside this, it’s imperative that early diagnosis for people living with dementia is prioritised through increased investment in local memory services.Budgets have been significantly reduced over the last ten years, as part of cuts to mental health services more widely and with COVID-19 causing increased waiting times. It’s vital that funding is utilised for memory clinics to provide support early on in someone’s dementia diagnosis.
Early diagnosis also enables individuals to make choices in their care, and to access medications, therapies and strategies that can slow down the progression of symptoms. It also enables timely access to emotional and practical support, including that provided by Dementia
UK, through its Admiral Nurses.
Managing dementia in its early stages is also integral in reducing the need for costly emergency interventions and hospitalisations.
In addition, an increased focus on early diagnosis can also promote understanding of dementia and help frame it as a medical condition that can impact people of all ages, rather than positioned as being a natural part of ageing.
Investment in dementia research is integral for the development of preventative measures which can help to reduce the onset or severity of dementia, enabling individuals to live more independently.
While the government has recently provided h funding to support research into dementia diagnosis through UK Research and Innovation, it’s also imperative it continues to invest in areas such as data collection, which can drive research into dementia care and treatment. Research into care and support, as well as cure is also important. A vital element of this will involve partnering with live-in care providers to help enhance services and keep individuals in their homes for longer.
Investing in home care alongside wider funding provision will have the effect of reducing strain on the NHS. The Good Care Group’s 2023 outcomes data shows that 87% of individuals were able to fulfil their preferences by dying at home, highlighting how home care is integral to allowing people to preserve dignity in their final days, while reducing pressure on hospitals.
Investing in dementia care is a crucial step for the government in addressing current and future healthcare challenges, ensuring equitable and compassionate care for its ageing population, and a better standard of living for all.
Residents at a dementia care home in Wellington, Somerset have been busy preparing fat-balls for the birds who visit their garden ahead of the UK’s largest annual garden-based citizen science project which is due to take place next weekend.
Manager Zillah Oakes said: “Lots of the ladies and gents who live at Camelot House and Lodge have had a life-long interest in birds and are aware of their dramatic decline over the past 50 years, so they’re very keen for us to gather and share data with the annual Great Garden Birdwatch.
“Many of them have enjoyed feeding birds in their own gardens, and there’s a lot of interest in the feathered friends who frequent the gardens at the home.
“We’ve got bird-feeders located in clear view of the lounge and we support our residents to use binoculars so they can have a good up-close look at our little visitors, which means we’re well placed to take part in the survey.

“All we have to do next weekend is just spend an hour watching and recording the birds we see in our garden and send our results to the RSPB.”
The RSPB’s Big Garden Birdwatch takes place on the last weekend of January every year and has been running since 1979, originally as a project for junior members of the charity.

Zillah Oakes said: “Apparently one in four species is now under serious threat, and this event offers us the chance to play a part in helping conservationists understand how various species are faring, which can feed into them creating action plans to help our native birds.
“It’s an activity that will make our bird-spotters feel really useful and that’s a very important part of the care we provide – everyone likes to feel needed.
“Activities like creating fat-balls to put on our feeding stations also help give our ladies and gents a feeling of usefulness, and we keep the bird tables in our gardens well stocked so there’s always some activity to watch out there, which is especially lovely at this time of year and keeps us all feeling connected to nature.” So far this year sparrows, starlings, gold finch and blackbirds have been spotted in the garden at Camelot House and Lodge, as well as robins and various species of tit.
Residents’ interest is also being kept engaged with various other bird-themed activities, including colouring activities and quizzes.
The bird-watching project is running as part of a wide and varied programme of activities designed to maintain engagement and socialising among the residents of Camelot House and Lodge.

Dementia is on track to become the third leading cause of death worldwide by 2040, according to a newly published commentary in Nature Reviews Neurology by Alzheimer’s Disease International (ADI). The report, developed in collaboration with academics from the London School of Economics, highlights the need for policymakers to treat dementia as a non-communicable disease (NCD) and integrate it into global health frameworks. Non-communicable diseases, such as cancer, cardiovascular disease, and diabetes, are defined as long-term medical conditions not spread from person to person. Despite dementia meeting these criteria, it is frequently excluded from policies addressing NCDs. This omission impacts funding, governmental responses, and public health initiatives. ADI’s commentary argues that dementia’s growing prevalence and severity demand urgent recognition and inclusion in global NCD strategies. The commentary reveals alarming statistics: dementia is projected to rank among the top 10 causes of death in 166 out of 195 countries and territories by 2040. In 121 of these, it will be among the top five causes, and in 53 countries, it will rise to the top two. Furthermore, dementia is expected to be the leading cause of death in 19 countries by 2040. When considering years of life lost (YLL)—a measure of premature mortality—it is anticipated to rank as
the fifth leading cause globally.
Paola Barbarino, CEO of ADI and a lead author of the paper, called for urgent action: “Although dementia is forecast to become the third leading cause of death by 2040, governments continue to misrepresent the condition. Unlike other NCDs such as cardiovascular disease, cancer, and diabetes, dementia does not receive adequate funding or inclusion in health policy. This is perplexing, given that the number of people living with dementia is projected to nearly triple by 2050, reaching 139 million.”

The exclusion of dementia from NCD frameworks is particularly concerning as it limits the progress needed to mitigate the growing impact of the disease. Recent international reports, such as the World Health Organization’s guide on “Strengthening NCD Integration in Humanitarian Emergencies,” have overlooked dementia, focusing predominantly on conditions associated with premature mortality (under 70 years).
Lewis Arthurton, ADI’s Head of Communications and Policy, highlighted the importance of recognising dementia as a major public health issue: “The exclusion of dementia from NCD policies represents a significant gap. Projections show it will become one of the leading causes of death globally by 2040. Policymakers must allocate appropriate resources to ensure better support for those living with dementia and their carers.”
As the world prepares for the 4th High-Level Meeting on NCDs at the United Nations General Assembly in September 2025, ADI is calling for dementia to be prioritised in these discussions. The meeting will shape the global strategy for addressing non-communicable diseases, and ADI argues that the inclusion of dementia is essential to ensure equitable access to care and resources.
The residents and staff at Elm Bank care home in Kettering were delighted in attending the local St Thomas More School for an afternoon of Archaeology and dinosaur’s.
Residents were very excited to have been invited to a wonderful afternoon at their local St Thomas More School’s archaeology afternoon that was delivered by the talented team from ‘Giant Journeys’. The residents and children immersed themselves in learning about the world of dinosaurs and thrilled to have been a part of the fantastic educational afternoon. Darren from Giant Journeys along with his team educated the children and residents about the amazing artefacts that they had with them, when everyone thought that it was all over, the hall was full of surprise as a giant dinosaur surprised all.
Resident Beryl said, “It was lovely, to see all the children all so keen to learn, I was a teacher myself and this afternoon was just perfect. The dinosaur now he was a surprise as no one was expecting to

see him.”
Marvellous Bindura, General Manager said, “It was lovely that the local school opened their doors to our residents, it means so much to the residents, it allows for the young and the old to mix and the wonderful experiences are shared. Beryl was a teacher, so this meant so much to her. I believe as do we all here at the home, it is crucial to create links with our local schools and within the community to continue for our residents to remain a part of the community.”

WE NOW SUPPLY A WIDE RANGE OF FURNITURE
RSM UK’s head of healthcare Suneel Gupta and head of NHS Clive


Funding and investment - The average deal value of private equity buyouts in the healthcare industry was £68m in 2024, over double the average of £32m in 2023, according to Pitchbook. That said, while deal values jumped from £3.5bn in 2023 to £6.8bn in 2024, the number of deals fell from 110 to 99 in the same period.
Suneel Gupta: “The healthcare industry has long been viewed as a robust option for investors, but it hasn’t been sheltered from the impact of high interest rates, rising cost of debt, and uncertainty, which have hindered investment opportunities. Investors have been more risk adverse and favoured larger established businesses with a proven track record. With immense pressure on the NHS and growing waiting lists, it is clear support from the private sector is needed to ease the
burden. As interest rates slowly come down, there’s a renewed optimism that we will see an increase in investment activity in 2025 and beyond. There will however be a greater focus on more robust due diligence, with high quality data being increasingly important during the deal process to drive value and build investor confidence. As a result, deals may also take longer to complete.”
Suneel Gupta: “A significant headwind for the healthcare sector is the increase in employers’ National Insurance contributions (NIC) from April 2025, along with a 6.7% rise in National Living Wage (NLW). Whilst welcome news for workers in the industry, many of whom are under immense pressure and facing burn out, margins will be significantly hit. Businesses across the health and care sector are often heavily dependent on staff that are paid the NLW, so the impact will be severe, and in some cases devastating, and it places further strain on squeezed margins. Businesses will need to think of creative ways to mitigate these costs, for example, the adoption of technology to create efficiencies will be a gamechanger. Healthcare leaders will also need to consider transforming their care models and redesigning jobs in order to address the skills shortage in the sector.”
Suneel Gupta: “Private hospital admissions reached 232,000 in Q2 2024, the second highest total on record*. The NHS is already collaborating with the independent sector to support with increased patient demands, which will only increase further as part of the government’s
efforts to reduce waiting lists. The private sector plays a huge role in supporting the NHS, delivering care and investing in new products and technologies. Plus, with resources in the NHS significantly constrained, harnessing the skills, innovation and capacity of the private sector will be key in easing this pressure. But investment and collaboration within the sector must be done carefully, so patient outcomes are not compromised at any stage.”
Clive Makombera: “Advanced data sharing and increased digital maturity is a crucial strand in making the NHS fit for purpose. In addition, AI has the potential to transform healthcare by optimising both administrative functions and care delivery with improved care quality, enhanced patient experience, and greater clinician satisfaction. There needs to be a shift from a reactive culture to being more proactive, and investment in technology is needed to make this happen. Tech can be hugely powerful in driving down costs while improving productivity, and diagnostic capability and quality. An example is investing in diagnostic imaging equipment to help with the early detection of illnesses which would massively reduce the pressure on the NHS, or using AI to efficiently analyse and process vast amounts of data. However, as more collaboration and data sharing takes place between the NHS and private sector, this will also mean an increase in cyber threat. It is therefore more important than ever that organisations adopt cyber security foundations early on to avoid falling victim to an attack.”
Residential and home care provider, Care South, has won a national award recognising its specialist Dementia Care Coach training scheme. The care provider, which is a registered charity, has been presented with the Hennell Award for Innovation and Excellence in Dementia Care by the Association for Dementia Studies at the University of Worcester. The award celebrates one individual or team per year which has implemented positive change for the benefit of people living with dementia. are South has Dementia Care Coaches who have completed the inhouse training programme across its care homes and care at home offices, which are based across Dorset, Devon, Somerset and West Sussex.
Simon Bird, CEO of Care South, said: “We are absolutely delighted to receive the Hennell Award for our Dementia Care Coach training programme which champions the very latest, best practice around personcentred dementia care. I’m incredibly proud to have Dementia Care Coaches working in every care home and care at home office, who support their colleagues to provide compassionate care and making a real difference in the lives of residents with dementia.”
Social Care TV continue to fly the flag for highest quality online training for Health and Social Care, after unwavering commitment to excellence within the sector for over 25 years.
Their widely-used health and social care specific courses - produced and edited in-house - are expertly designed to make learning engaging, informative and, therefore, highly effective for learners.
Accredited by CPD and endorsed by Skills for Care, training with Social Care TV is quality assured, comprehensive and relevant.
As one of the leading online training providers in the health and social care sector in the UK, they supply training for local authorities, recruitment agencies, care home groups and other health and social care organisations.
Their feature-rich Manager platform has further been enhanced this year with the introduction of several new Manager tools designed to aid with compliance, reporting and trainee management. Features now available include:
• Compliance Dashboard with Traffic Light System
• Downloadable Trainee Matrix

• Custom Bundles
• Trainee Groups
• Bulk Uploads
The scheme, led by Karen Hodges, Group Dementia Lead at Care South, sees the Dementia Care Coaches work closely with colleagues and residents to further develop the best care practices for the enhanced wellbeing of residents living with dementia. They also provide additional support to the family of residents and loved ones living with dementia.
Karen Hodges, Group Dementia Lead at Care South, said: “It is a real honour to receive this award which is testament to the hard work of our Dementia Care Coaches who support their colleagues with coaching and on-the-job guidance to ensure best practice with residents living with dementia and their loved ones. It’s inspiring to see the difference they make to the lives of our residents, enabling them to live with dignity, respect, and joy while providing invaluable support to their families.”
Nicola Hook, Activities Lead at Alexandra House care home who has trained as a Dementia Care Coach, said: “I found the Dementia Care Coach training really interesting as it has taught me that small changes can make a difference. It’s very rewarding to support my colleagues in enabling them to provide the best possible care to all residents, including those living with dementia.”

• Bulk Enrolment Onto Custom Bundles
• Course Enrolment Notifications
• Course Reminders
SCTV regularly release new and updated high-quality courses. Previews for all courses can be viewed at: Courses - Social Care TV (www.social-care.tv/courses/course-details)
To enhance their learners' experience further they have created free, comprehensive subject-specific workbooks which were rolled out across all courses this year. This unique addition provides excellent value and a fully robust training package.
SCTV are delighted to have won several awards over the last 12 months including:
• Best Online Health and Social Care Learning Platform’
– Global Health & Pharma Social Care Awards 2024
• ‘CPD Provider of the Year’ – The CPD Awards
• Social Care Training Provider of the Year’ - Corporate Livewire Innovation & Excellence Awards
Gold standard customer service remains a core staple of the business, with expert support and guidance provided via telephone, email and live chat. They place great importance on the training and development of their customer services team to ensure that they continue
to provide a personal, friendly and knowledgeable service.
Their much-loved ‘Care Worker of the Month’ award recognises and rewards the selfless dedication shown by care workers across the UK and they proudly support the Care Workers Charity who aim to advance the financial, professional and mental wellbeing of social care workers.
SCTV believe that high quality training should be accessible to all and offer regular, free courses which include a digital certificate accessible via their website.
The company stands behind a clear mission and set of values which define their ethos and their dedication to both the Care Sector and those within it. These can be viewed at: Mission Statement and Core Values - Social Care TV
(www.social-care.tv/about/mission-statement-and-core-values)
Social Care TV are a responsible business, committed to ensuring that their actions have a positive impact on their employees, customers, the wider health and social care community and the environment.
Above all, SCTV consistently strive to make a meaningful contribution to the wellbeing of those being cared for.
For more information please see: Homepage - Social Care TV (www.social-care.tv) and see advert on the facing page.
Care England challenges recent assertions that a lack of capacity in social care is driving NHS delays, citing data from the Capacity Tracker that highlights significant available care home beds across the country.
The “corridor care crisis”, has been reportedly caused by difficulties finding care homes or community care packages for elderly and vulnerable individuals, exacerbating delays in emergency departments and overcrowding.
However, data from the Capacity Tracker reveals that care home occupancy for older persons nationally remains stable at around 85%, with over 43,000 beds currently available for admission.
Professor Martin Green OBE, Chief Executive of Care England, said: “This is not a capacity issue; it’s a planning, funding, and coordination issue. Care homes across England have been reporting admittable vacancies, yet the system is unable to utilise this capacity effectively. We warned the Department of Health and Social Care (DHSC) about the risks of inadequate winter planning before. These warnings were ignored, leaving hospitals struggling to manage the entirely predictable pressures of winter.”

The failure of health and social care commissioners to engage and work with the sector has been compounded by insufficient funding from the Government. For example, the Improved Better Care Fund (iBCF) has remained at £2.14 billion since 2022-23, despite rising inflation and increased costs – eroding the of purchasing power of local authorities who are now unable to meet the critical objectives of the iBCF policy framework, including:
• Supporting timely hospital discharges.
• Providing the right care in the right setting to promote independence.
Professor Green added: “The absence of real-term funding growth in the iBCF has forced local authorities and providers into untenable decisions, reducing service availability when it is needed most. However, this is just one example of how the Government has introduced unfunded policies that undermine the sector. They must urgently address their entire approach to funding the sector to prevent further strain.”
Winter Pressures Are Not ‘Business as Usual’
Care England has voiced serious concerns over the lack of proactive winter planning, warning that the absence of such measures downplays the urgency of the situation and risks exacerbating pressures on the sector.
“The absence of winter planning signals a ‘business as usual’ approach, which is both dismissive and dangerous,” Professor Green continued. “It fails to recognise the cascading effects of delayed planning, chronic underfunding, and systemic inefficiencies that leave the NHS struggling to cope.”
IN RESPONSE TO THIS ESCALATING AND UNNECESSARY CRISIS, CARE ENGLAND IS CALLING ON THE GOVERNMENT TO:
• Develop a recurring national winter strategy for social care to prevent repeated failures and guarantee consistent readiness across the health and social care ecosystem during peak demand periods.
• Commit to adequate and sustainable social care funding, by increasing the iBCF in line with inflation to address immediate financial pressures, and establish a long-term, sustainable funding settlement for adult social care.
“Social care is the backbone of the NHS, and its underfunding is crippling the entire system. Without swift and decisive action, the consequences for individuals, who deserve the right care, will be severe,” Professor Green concluded.
Blakelands Lodge care home recently had the pleasure of hosting the High Sheriff of Bedfordshire, Bav Shah, for a memorable visit.
During his time at the home, High Sheriff Shah spent several hours getting to know the residents and staff, engaging in heartfelt conversations, and learning more about the daily activities and initiatives at the home.
One resident was recognised for her long and dedicated service with the NHS, and the High Sheriff expressed his appreciation for her contributions to healthcare. He also promised to return for another visit in the near future, much to the delight of everyone at Blakelands Lodge.
High Sheriff Shah commented: “I was delighted to be invited to

Blakelands Lodge Care Home to meet the residents and have some wonderful conversations. It was great to see the range of activities that Blakelands offers to keep the residents engaged.
“We also had a chance to discuss what can be done to collaborate with the local community, and I look forward to working together in the future.”
James Eeles-Feeney, Home Manager, said: “It was wonderful of the High Sheriff to take the time to visit us and meet some of our incredible residents and staff. The residents really enjoyed meeting him, and it was a talking point for many days afterwards.”

By Henny Braund, Chief Executive of Anthony Nolan (www.anthonynolan.org),

One in two of us will develop a form of cancer during our lifetimes. And we will all be affected by cancer in some way – be it caring for a loved one, receiving treatment ourselves or losing someone we love. Despite many incredible advances in cancer treatment and care, the UK falls behind comparable countries when it comes to cancer outcomes.
Across the health and care sector, it is recognised that hearing the patient voice and acting on their valuable insight is vital. This is what led the Specialist Cancer Charities Group (SCCG) to embark on research to hear from cancer patients. We asked Thinks Insight & Strategy to facilitate a citizens’ jury of cancer patients to suggest where the new government should focus its efforts to improve cancer care, within the context of today’s tight fiscal environment. Importantly, we not only wanted to learn which areas cancer patients would prioritise for improvement, we also wanted to test how a citizens’ jury approach could work in this context.
CREATING THE JURY
The jury consisted of 17 adults who had received treatment for cancer from the NHS in the past five years. This group had experience across various cancer types and represented a mix of ethnic backgrounds and socioeconomic grades. It also included interviews with three children and young people and their families.
Fieldwork included one-to-one interviews with each juror to understand their individual experiences. This was followed by four online workshops where jurors heard expert testimony from ‘witnesses’ on different aspects of the healthcare system. Four areas of policy were explored in detail: two were chosen by the SCCG, and the other two were chosen by jurors. This allowed jurors to shape the discussion and ensure conversations included the issues that mattered most to them.
At the end of the month of testimony, jurors deliberated to come to a consensus on priorities for the government, and made recommendations for what improvement in this area could look like in practice.
THE JURORS’ PRIORITIES FOR CHANGE
Improving diagnosis was a top issue for all jurors. The group spoke about long waiting times, poor emotional support and inadequate information about their diagnosis. They also emphasised how improving diagnosis is vital to improving cancer care overall, because patients being diagnosed late or in urgent and emergency settings leads to more intensive treatment and lower survival rates.
Jurors also highlighted that care is not equivalent across the four nations of the UK, with individuals from Scotland and Northern Ireland feeling aspects of their care were worse. Multiple jurors from minority ethnic backgrounds described difficulties in accessing good quality care. For example, jurors from minority ethnic backgrounds were more likely to say that they had struggled to get a diagnosis due to their symptoms being repeatedly ignored by GPs. However, it was hard for jurors to personally acknowledge that they might have experienced inequalities, and none of these jurors explicitly related the problems in their cancer care to health inequalities.
Also important was mental health. Many jurors experienced mental health challenges, citing worries about the future, changes to their relationships and financial concerns. Negative and unempathetic interactions with healthcare professionals were also reported to have had an impact on emotional wellbeing.
A template for patient-led policy making
At the start of the process, we found jurors had an individual mindset – focusing on their own experiences and what could have made these better. However, over the course of the process their perspectives evolved. Hearing the experiences of other patients and information from expert presenters and having time for structured and in-depth discussion enabled jurors to adopt a ‘citizen mindset’ and consider system changes beyond their personal experiences.
Furthermore, jurors’ perceptions of the current state of cancer care did not always align with the data provided by experts and stories in the media, underlining the importance of speaking directly with patients on the elements of their care that matter most to them.
Finally, many jurors commented on the way the process left them feeling empowered as a patient and able to make a meaningful difference to others like them. Ultimately, those with lived experience are experts on cancer care, and deserve to have their voices heard in shaping those policies that directly impact them.
We found the citizens’ jury to be an effective method for meaningful patient involvement and turning their insights into actionable recommendations for change. As well as calling for urgent action to address the recommendations, we are urging the citizens’ jury model to be adopted more widely to ensure patients’ voices are heard front and centre in policy making.
It's encouraging to see public deliberation being adopted in projects such as the 10-Year Health Plan consultation, which represents a huge opportunity for the government to embed patient voice in their future healthcare policy making. But the government shouldn’t stop there. This report shows how adopting a citizens’ jury approach could help enable more considered public engagement and ensure the health service is shaped to meet the diverse needs and unique challenges of all those who need it.
The full report, including all the jurors' recommendations and our advice for delivering a citizens’ jury, can be accessed here:
www.anthonynolan.org/what-we-do/influencing-change/being-a-voice-patients/sccg-citizens-jury
With expert guidance from Barchester’s Hospitality Development and Standards Manager, Mervyn Knights, 38 talented chefs – the Class of 2024 – have just completed a year’s training and graduated from the Barchester Chef Academy.
The Academy is the brainchild of Knights, who joined Barchester 22 years ago as a Kitchen Assistant and worked his way up through the ranks to head chef and then to his current position as part of the team overseeing hospitality training across the whole of Barchester.
Along with the rest of the hospitality team, it is Mervyn’s job to ensure that the food being produced in all of Barchester’s 264 care homes and private hospitals for residents and patients meets Barchester’s very high standards in terms of quality, taste, nutrition and presentation, and that dishes are being prepared to the exact requirements of our individual residents.

The Barchester Chef Academy helps chefs to both hone their skills and learn new ones, covering many different modules including cooking for residents living with dementia, budgeting, balancing flavours, minimising wastage, presentation skills and so much more. The 38 chefs who completed this year’s course were full of praise for all they had learned; the chance to perfect new techniques and recipes, share hints
and tips, to network and make new contacts and to expand their skill set. Back in their divisions, these chefs will help to train the hospitality teams in their sister homes.
Speaking about the Academy’s success, Mervyn Knights commented: “I am absolutely delighted at how well the Academy has been received by everyone who attended the course, it has been such a positive experience for all involved.
We are already planning and recruiting the Academy’s new Class of 2025 who I know will go on to achieve great things, just as our 2024 chefs have.”
Dr Pete Calveley, CEO of Barchester Healthcare, added: “The Chef Academy is a wonderful initiative which is going from strength to strength each year under Mervyn’s excellent leadership.
I have the pleasure of sampling some of the fantastic dishes produced by our talented chefs each year and I am always impressed by the high standard of cooking and by how beautifully everything is presented.
I am incredibly proud of all of the chefs that took part in the Academy in 2024, I know they produce wonderful food for our residents and patients, cooked to their individual preferences, every single day.”
HC-One’s Larchwood Care Home, in Braintree, Essex, has been hosting weekly Songs & Smiles sessions to tackle social isolation through human connection.
Larchwood, a residential dementia care home, have held weekly Songs & Smiles sessions every Tuesday morning with The Together Project and a fully trained professional group leader, who has run the sessions since November 5, 2024. As well as reducing loneliness for parents, guardians and older people, the Songs & Smiles sessions incorporate a growing body of research around child development. Bringing together singing, movement, social interaction and other stimuli, the programme is designed to develop rhythm and coordination, build confidence and stimulate the senses in a way that promotes healthy development for both babies and care home residents.
Both the residents and the little visitors experience a 45-minute singalong session using different instruments, toys, coloured scarves and a bubble machine. At the end of the session, Larchwood residents have time to chat with parents,

guardians, and toddlers, as well as enjoy cuddles with the little ones. Each session provides music, fun and friendship for Larchwood residents. The residents have been able to strike a bond with little visitors and their parents and guardians, especially the youngest baby 'Martha' who was only eight-weeks-old when she attended the first session.
Donna Owen, HC-One’s Larchwood Care Home Manager, commented:
“Songs & Smiles has been a huge success. The residents have benefitted so much from the interactions with the children. All the residents living with dementia had a great sense of comfort and joy from these sessions.”
Suzy Dodge, HC-One’s Larchwood Care Home Wellbeing Co-ordinator, said:
"Holding the Songs & Smiles sessions is always a heart-warming experience. It's incredible to see how the music can bring so much laughter and togetherness, which has sparked memories and created connections."
In a groundbreaking publication, Working Chance and Care England have launched new guidance to encourage and support adult social care organisations in considering candidates with criminal convictions during recruitment. This pioneering effort aims to dismantle barriers and highlight the significant benefits of employing individuals with experience in the criminal justice system.
The joint publication provides practical advice on how hiring individuals with convictions can address staff shortages and foster a more inclusive and diverse workforce. By prioritising a candidate’s skills and experience over past mistakes, employers can tap into a pool of talented, dedicated individuals eager to make a positive impact in their communities.
Natasha Finlayson OBE, Chief Executive of Working Chance, said: “People with convictions are often overlooked when employers think about attracting talent or enhancing their organisation’s diversity. Hiring people with convictions has many benefits for employers and communities, so there’s much to be gained by changing recruiting practices for

the better. I hope you’ll come away inspired to open up more opportunities in your organisations to people who need someone to believe in them.”
Professor Martin Green OBE, Chief Executive of Care England, said: “Opening our doors to people who have moved beyond a past criminal conviction can make good sense for our organisations and the people we exist to serve. This guidance provides an important first step in understanding the benefits and offers practical, actionable steps to make inclusive hiring a reality.”
The guidance comes at a critical time for the adult social care sector, which is facing difficulties in finding the right staff for the right roles. The 2024 HfT and Care England Sector Pulse Check report outlines recruitment and retention of domestic workers, pay, and high attrition as key challenges facing social care. By joining forces, Working Chance and Care England hope to change the narrative around hiring individuals with convictions and demonstrate the significant benefits of a more inclusive approach to recruitment.
For more details and to download the full guidance, please visit https://tinyurl.com/yu3pax9f
Resident, Greta Lumbers, at Hilton Park Care Home in Bottisham had always wanted to experience a High Tea Afternoon at The Carriages of Cambridge so staff at the home made her wish a reality proving the old adage, it’s never too late. Despite only living at Hilton Park since December, Greta is already beloved by staff and residents alike.. Staff at the home were delighted to be a part of making Greta’s dream come true, as they knew how much it meant to her, and they all wanted to be there to see the smile on Greta’s face when she returned back to Hilton Park.
Staff found out about Greta’s dream soon after she arrived at Hilton Park and, ever since then, they have been dedicated to helping her achieve it. Greta was also accompanied by friend and fellow resident, Pat James, along with staff mem-
bers Jenny Szabo and Lily Ashley, who were there to witness this momentous occasion.
In response to this wonderful surprise, Greta, said: “I was on the verge of tears. It is such an amazing feeling to know that such a loving group of people care so much about me that they helped me to live out a dream – and I didn’t even ask.”
Geanina Tinca, General Manager at the home, said: “We believe that every moment is worth cherishing. We want everyone we care for to know how important they are to us here at Hilton Park. It is testament to the hard work and dedication of the team here in making our residents’ dreams come true. It was wonderful to see how happy Greta was – and the staff loved being a part of this as well.”


By Sam Pawson, Partner and Head of Employment Law at Yorkshire law firm Chadwick Lawrence

In October 2024, the government unveiled the ‘biggest reforms to employment support for a generation’. This landmark legislation proposes to deliver on the Labour Party’s promise to improve employment conditions, as outlined in their ‘Make Work Pay’ manifesto.
For those working in the care sector, the Employment Rights Bill brings potential opportunities, as well as potential challenges. It aims to addresses long-standing issues in the care sector by creating a new Adult Social Care Negotiating Body and introducing broader changes to working conditions. Here's everything you need to know.
Unveiled on 10 October 2024, the proposed Bill contains several reforms aimed at creating fairer and more secure workplaces. These include:
• Unfair Dismissal – removing the requirement for an Employee to have 2 years of service to gain protection from Unfair Dismissal
Flexible Working – strengthening the right to request flexible working by preventing employers from refusing a flexible working request, except where there is a specific statutory reason ‘Fire and Rehire’ - restricting employers’ ability to ‘fire and rehire’ workers by limiting their rights to dismiss an employee for refusing to agree to changes to their employment contract.
• Zero-Hour Contracts – introducing a right to request guaranteed hours to reflect the hours worked over a reference period.
For the care sector, one of the most significant proposals is the establishment of an Adult Social Care Negotiating Body.
This new body is designed to bring together representatives from across the industry to address critical issues, including staff pay, funding and working conditions. The Negotiating Body will be regulated by The Secretary of State, with decisions implemented through secondary legislation, aiming to create a more structured and equitable system for addressing workforce concerns.
As well as creating the Adult Social Care Negotiating Body, the Bill proposes to introduce new protections for workers on zero-hour contracts. These cover reasonable notice for shifts, payment for cancelled shifts and the right to request regular hours based on actual work patterns. Further, lower-paid workers stand to benefit from the removal of the earnings limit for Statutory Sick Pay, as well as immediate eligibility for SSP from the first day of sickness.
These proposed changes come amidst immense pressures on the care sector. In recent years, the demands of an ageing population, coupled with staff shortages and high turnover have placed many care providers under pressure. It is hoped that these reforms could lead to better wages and terms, helping to attract and retain workers to support the sector.
Whilst the proposed Bill potentially offers a boost for workers, it could raise financial and operational challenges for care providers.
A concern for many in the industry is funding. Homecare Association’s CEO Jane Townson said in her statement that whilst the Association fully supports the measures to ‘enhance workers’ rights and improve job security’, by their calculations, there would be a shortfall in funding to fund the measures. By their calculations, the change to day-one SSP rights could add 10p per hour to the cost of delivering homecare for providers. Whilst this may seem insignificant, for providers operating on already tight margins, there is a concern that this increase could push these providers into financial difficulty.
Similarly, the care sector’s reliance on flexible staffing means that the proposed reforms to zero-hour contracts could present operational difficulties. The Bill proposes to end ‘exploitative’ zero-hour contracts. Whilst this does not ban the use of zero-hour contracts in their entirety, it does propose that workers will have the right to reasonable notice, to payment for cancelled shifts, and to request regular hours based on the hours that they have actually worked over a set period. This has been proposed to provide more security to those employed on zero-hour contracts. However, some providers have expressed concern about how they will manage these changes and maintain flexibility in a sector with unpredictable demand.
With 21% of all adult social care positions being filled by workers on zero-hour contracts, representing 29% of care worker posts and 43% of home care worker posts, the impact could be considerable.
The majority of changes are unlikely to take effect until Autumn 2026. This should allow providers adequate time to prepare.
As a first step, providers should begin by evaluating the financial impact of the SSP changes and should budget for potential wage increases. Given the National Minimum Wage increases due in April of this year, budgeting for wage increases would be advisable regardless of the Bill’s content. However, considered financial and workforce planning will now be even more crucial.
Providers should also assess their workforce model by assessing their organisation’s reliance on zerohour contracts and exploring ways to adapt to new requirements. They should also prepare for the changes to flexible working policy by reviewing their Handbooks, policies and processes.
The Employment Rights Bill could present a significant step towards improving conditions for workers, particularly in the care sector. The introduction of the Adult Social Care Negotiating Body and other reforms do have potential to improve the industry by addressing staffing challenges and enhancing job security.
However, these proposed changes could come with significant financial and operational challenges. Without adequate funding, these reforms could put a strain on providers and risk unintended consequences for care quality. In light of this, providers should use the time between now and the Bill’s implementation to prepare for these changes.
HC-One Scotland’s Redmill Care Home in East Whitburn, West Lothian, was visited on Friday 17th January by MSP for Linlithgow & Cabinet Secretary for Transport, Fiona Hyslop.
Residents and colleagues of the HC-One Scotland owned care home enjoyed meeting MSP Fiona Hyslop and chatting to her about what life is like at Redmill Care Home – which is an integral part of the local East Whitburn community.
MSP Fiona Hyslop enjoyed learning about how Redmill involves the local community in activities with residents and how the variety of activities cater to

all resident’s needs.
MSP Fiona Hyslop enjoyed a tour round the 68 bedded nursing and nursing dementia care home, including the hair salon, café, lounge, sensory garden, and ensuite bedrooms.
Joanne Cunningham, Home Manager at HC-One Scotland’s Redmill Care Home, commented: “We were delighted to welcome MSP Fiona Hyslop to our home. Everyone had a great time, chatting and discussing key issues they care about and what actions can be taken to overcome them.”
Henbrook House, a luxury care home in St Neots, recently arranged an inspirational visit to the Fitzwilliam Museum in Cambridge for resident and accomplished artist Reg. The trip, coordinated by Henbrook’s dedicated events team, was designed to help Reg develop his lifelong passion for art which began when he started sketching as a child.
During retirement Reg has loved throwing himself into his painting and drawing. Unfortunately, in recent years he has struggled to keep up his craft due to ill health. With Henbrook’s support, including tailored physical therapy sessions every week with PT Lisa to rebuild his grip strength, Reg has managed to once again pick up his paintbrush!
To celebrate his progress and provide further inspiration, Henbrook’s Life Enhancement and Wellbeing Coordinator Stephen Orwin and Events Manager Brian Moore organised the visit. The Fitzwilliam Museum houses a world-class collection of over half a million masterpieces and historical artefacts. On his return, Reg said “It was a great day, I thoroughly enjoyed it.”
Catherine Frost, General Manager of Henbrook House, reflects on the visit:

“It was so great to see Reg enjoy his trip to the museum and to have such a spring in his step when he got back! On his return, Reg was keen to show us a couple of pictures that he had painted, which were truly amazing and worthy of being in a gallery themselves! Helping residents rediscover their passions is one of
the best things about working in care; and we can’t wait to continue this work in 2025!”
The Fitzwilliam visit not only reinvigorated Reg’s passion for painting, but also created a kind of mini-Renaissance at Henbrook! By popular demand, the home now offers regular classes in watercolour painting, rock art, cupcake decorating, and other arts and crafts activities.
Studies show this kind of ‘art therapy’ can boost mental well-being and selfesteem amongst older people in care settings by giving them a regular outlet for creative expression. In care homes it has also been found to improve psychological functioning, cognition, social relationships amongst residents; particularly when enjoyed as part of a group.
The team hopes to lead the charge on the integration of art therapy in care homes; which involves close collaboration between art therapists, care staff, and residents. Commenting on the project, Lifestyle and Wellbeing Enrichment Coordinator Stephen Orwin said:
“At Henbrook, we believe it’s never too late to start a new project and build a new skill. Happily, our arts and crafts sessions have been a big hit with residents, who really value the experience of creating things with their own two hands. These are the kind of fun, rewarding activities that stimulate the mind and give a real sense of purpose”.

Care England has raised serious concerns over the Home Office’s proposed fee increase for Certificates of Sponsorship (CoS), warning it will exacerbate the intense financial pressures already crippling the sector.
The proposal would more than double the CoS fee, from £239 to £525 per individual, imposing an additional £286 cost per international recruit. This equates to an estimated £10.3 million sectorwide cost for care providers already grappling with severe workforce shortages, escalating operational expenses, and funding deficits compounded by the Employer National Insurance Contribution increases announced in the 2024 Autumn Budget. This comes on top of the government retaining severe restrictions introduced in the April 2024 immigration changes, including the ban on dependents for overseas social care workers, which caused a drop from 105,000 international recruits in 2023/24 to 18,000 in the first half of 2024 according to Skills for Care. Despite policy decisions seemingly designed to make international recruitment as unappealing as possible, providers are left with no viable alternative in the absence of a comprehensive workforce strategy to support the domestic care workforce.
Care England has long emphasised the vital role international recruitment plays in addressing workforce shortages within the care sector. The Sector Pulse Check 2024 Report, recently pub-
lished in collaboration with Hft, highlights the deepening crisis: 40% of providers have been forced to rely more heavily on agency workers to cover staffing gaps. These figures highlight the indispensable need for international recruitment to address persistent, long-term vacancies. Introducing these policies directly undermines what the sector desperately needs at its most vulnerable moment, piling further financial strain on providers when demand for care services is surging and the system is already stretched to breaking point.
Professor Martin Green OBE, Chief Executive of Care England, stated: “These proposed fee increases represent yet another blow to social care providers, compounding what is already a devastating situation for the sector. The 2025/26 financial year is set to be the hardest yet, with providers facing an attack on all fronts. The Autumn Budget dealt an incredibly harsh blow, leaving many providers scrambling to plan how they will survive the coming year.
This latest announcement only exacerbates the crisis.
International recruitment has been a lifeline for the sector, proving to be the saving grace as providers endure an unprecedented domestic workforce crisis with no meaningful government support to address it. Targeting international recruitment with these fee increases is an attack at the very heart of the sector’s ability to function. Care providers are already fighting to sustain services, and these additional costs will push many to breaking point. The Government must reconsider its position immediately. Without urgent action, this relentless financial strain will jeopardise care delivery for the millions of people who depend on it. The time for meaningful workforce reform and investment is long overdue.”
Care England calls on the Government to urgently reconsider the proposed fee increases for CoS and to develop a comprehensive workforce strategy that supports both domestic and international recruitment, ensuring the long-term sustainability of the adult social care sector.













The latest UK Care Homes Trading Performance Review 2024 shows occupancy levels rising to 88.3%, a positive sign of market recovery. However, while this progress is encouraging, it reveals significant untapped potential in how care homes attract and convert prospective residents.
Presenting care homes effectively is not just about showcasing services—it's about creating emotional connection and trust. Families are making difficult decisions in emotionally charged situations, which requires a sophisticated approach to relationshipbuilding and conversion. Care homes are offering something no one truly wants to need, making the challenge even greater.
To truly drive sustainable occupancy growth, care homes must focus on transforming the customer journey—from raising awareness to handling enquiries and guiding families through to admissions. Many providers are still missing key opportunities. Too often, care homes fall short in delivering the basics well, leading to lost enquiries and missed revenue potential.
CRITICAL AREAS NEEDING IMPROVEMENT INCLUDE:
• Generating Quality Leads: It's essential to attract the right audience from the outset through targeted campaigns, high-value content, and strategic outreach across multiple channels, including community outreach, digital marketing, partnerships, referral networks, local events, print ads, and door drops.
Empathetic First Contact: Enquiries must be handled with care, expertise, and emotional sensitivity, recognising the difficult decisions families face.
Personalised Tours: Showrounds should go beyond listing services, highlighting quality of life benefits such as personalised care plans, engaging activities, and the warmth of community life.

By Ali Powell, CEO and Founder at Commercial
Clear Value Communication: Families need transparent, outcome-driven explanations of the value of care— focusing on dignity, well-being, and peace of mind, not just amenities.
Consistent Post-Visit Engagement: Many care homes neglect follow-up strategies after visits, losing potential residents who may need further reassurance or time to decide.
TRACKING THE RIGHT METRICS:
To ensure the customer journey is effective, care homes should track key performance metrics, including:
Monthly Lead Generation: Number of leads that meet predefined criteria indicating genuine interest or fit.
• Monthly Visits: The number of on-site or virtual tours conducted within the month.
Monthly Admissions: The total number of new residents admitted each month.
Lead Source Performance: Breakdown of leads by marketing channel (e.g., online ads, social media, referrals, events) to identify the most effective sources.
Average Admission Cycle Length: The average time from initial lead generation to a confirmed admission.
• Monthly Marketing Spend: Total amount spent on marketing each month.
Website Traffic: Total visitors to the website and engagement rates for the month.
• Social Media: Total followers and engagement on platforms like Facebook, LinkedIn, and Instagram.
THE OPPORTUNITY:
Investing in marketing and relationship-building efforts is not a luxury—it's essential. The cost per acquisition is often minimal compared to the hundreds of thousands in lifetime revenue generated from new residents. By focusing on consistency and excellence throughout the entire customer journey, care homes can significantly impact both occupancy rates and short- and long-term growth. The data is clear: doing the fundamentals well is not just good practice—it’s essential for both immediate results and lasting success. It’s time for care homes to move beyond filling rooms and start focusing on creating an inspiring customer journey that builds confidence, trust, and emotional connection with families.
If you need an expert in this area, contact Ali at Commercial Acceleration—specialists in strategy and implementation for transformational and turnaround results. ali@comaccel.co.uk | comaccel.co.uk
Residents at Hampton Grove in Peterborough celebrated
International Flower Day which took place on January 19th.
International Flower Day promotes the psychological boost that flowers can give to people. From growing and nurturing plants and flowers, to gifting flowers to show love and appreciation, and sometimes just the simple act of admiring their beauty – flowers have the power to make someone’s day.
Residents took part in flower-based activities throughout the day including flower arranging reminiscing about their gardens/flowers in the home’s garden, a flower quiz and even
making their very own keyring and coaters out of moulds, which everyone really enjoyed. Their collective knowledge about flowers gained from years of gardening experience was very impressive.
Ewa Drzewicka, General Manager at Hampton Grove said: “Our garden is a much loved space, residents really enjoy looking after the plants and flowers and watching them grow and change through the seasons. We don’t have many flowers at the moment so our residents very much enjoying the arranging of flowers and decorating keyring and coasters”



Taylor & Taylor, a group of family-owned residential care homes approached food procurement experts, allmanhall to achieve scalable cost savings and efficiencies to support their growth plans. They needed to ensure no detrimental impact to the excellent quality of their food offering and their residents’ dining pleasure.
Their desire was to achieve a 5% food cost saving and to ensure ongoing effective management of catering budgets and invoicing. Operationally, access to reports and insights were key, as was ease of ordering and management of stock and deliveries.
allmanhall undertook a like-for-like benchmark and identified achievable food cost savings of 11.4% - more than double the initial objective!
allmanhall delivered tech demos of the catering control platform for Taylor and Taylor, ensuring it met their needs and provided training for the team. As well as providing useful operational functionality like stock taking and standing orders, the catering control platform proposed would also give access to management reports and facilitate central billing and conversion of all supplier invoices in to 1 per month. Samples and on-site supplier meetings were also arranged on behalf of the homes, to confirm that the quality was to the required standard.
allmanhall have also supported Taylor and Taylor with the launch of a community engagement event for one of their newest homes.
A few months into the contract, the actual results were found to be an 18% food cost saving! You can watch this short video on You Tube to find out more…
“From day 1, the care and attention provided by allmanhall has been exceptional. The team truly listen to us, to what our challenges are and are always willing to help in any way they can. Their approach is thorough and responsive, meaning we feel fully supported. Everyone we’ve met from allmanhall has been hands-on, down to earth, genuine and considerate.
I’ve been impressed by the savings we’ve already seen, the flexibility regarding suppliers and by the excellent quality. The consolidation of invoices into 1 per month is a huge win.
We have relationships and contact with people across the allmanhall team – all there to help and to advise or resolve depending on what we need. With challenges around labour shortages and food inflation, this is hugely valued. It frees up the team and gives us peace of mind.
I would wholeheartedly recommend allmanhall’s services to others in the care sector and I look forward to continuing to grow our offering and provide outstanding food for our residents, with allmanhall as our trusted partners.”
– Chris Rees, Group Executive Chef
allmanhall is an owner-managed, award-winning and trusted food procurement partner for care organisations across the UK. We help clients with a range of needs, including cost savings, administrative efficiencies, supplier management, dietetics and nutrition support, and sustainability goals. Get in touch to find out more:
Email: hello@allmanhall.co.uk
Telephone: 01225 745520
Website: allmanhall.co.uk
LinkedIn: @allmanhall


Under-25s (Generation Z) have much to offer the world of care, especially as it progresses. In a constantly adapting industry, young people are key to helping care companies grow with the times, especially surrounding technology.
However, young people make up only 11% of care workers. Why is this? What is keeping Gen-Z from joining and staying in the world of care?
With the average care worker aged 45 and over a quarter of the workforce potentially choosing retirement in the next 10 years, there aren’t enough young workers to pick up the many mantles left behind. With social care already having the highest number of vacancies in the UK, care providers cannot afford for this number to grow and for their workforces to decrease.
Supporting service users is no 9-5 or Monday to Friday job. This alone can be off-putting to the under-25s, who may juggle education and prioritise a larger social life.
This is what Gen-Z values. They have entered the career world understanding the importance of mental health and their worth in the workplace - and they are often viewed negatively for this. But they couldn’t be more correct.
Just as care services get a bad rep for offering a poor work-life balance, Gen-Z gets a bad rep for prioritising a healthy one. You can see the dilemma. So, how can this be fixed?
Irregular, unsociable hours, poor workload management, and low resources can easily lead to poor staff retention. From the most recent

findings in 2021-2022, care saw a high turnover rate of 53% for those under 20 years old while care workers over 60 had a rate of 24%.
It’s common for shift-based workers to feel they have very little control over their working lives, leading them to accommodate the shifts they have no say over. Especially due to last-minute scheduling and changes, many shift workers often must change or completely scrap personal plans - or wait until after shifts are allocated - resulting in lives only revolving around work.
As much as someone can be a work-first individual, removing time
By Becky Mundie, RotaCloud (www.rotacloud.com)
for personal and social lives - and simply downtime - can be damaging in the long run, causing stress and mental health issues. Factor in graveyard shifts or being on-call, and the feeling is greatly exacerbated.
Is there any wonder, when combining this with the high workload and responsibility that comes with care, that the under-25s - the generation valuing mental health - make up so few care workers?
There are simple ways to remedy this, however.
Simply offering flexibility, allowing staff to have a say in the days and hours they work, and offering the ability to oversee shifts further in advance, can make all the difference.
Implementing digital automation allows staff to feel more in control of their work and lives. This alone can greatly improve employee experience.
Surprisingly, employee experience can go hand-in-hand with updated technology - and what goes hand-in-hand with technology? The generation that has grown up with it.
Not only does digital automation benefit your service users, employees, and overall business growth, but it will also make your workplace more attractive to the new generation - who, once joining, can make adopting these new technologies and processes all the smoother. Under-25s are the future, as well as new technologies. It’s time to start investing in both.
Athena Care Homes are pleased to introduce Andreea Militaru as the new manager at Langdon House care home in Cambridge.
With big plans for the year ahead, she’s focused on getting to know everyone and creating a vibrant, supportive environment for residents and here team alike. Andreea brings a wealth of experience and a passion for care to her new role. Originally from Romania, she began her nursing journey there before moving to the UK in 2014 to explore new opportunities.
Starting as a carer, Andreea quickly progressed to nursing and has since dedicated her career to the care home sector. Her roles as a unit manager and deputy manager have given her invaluable insight into the needs of our residents, their families, and our care teams.
What draws Andreea to working in a care home is the unique opportunity to form meaningful connections. "In a care home, you build a bond with the resi-
dents and their families," she said. "You’re part of their journey, which is something you don’t often get in a hospital setting."
Andreea’s decision to join Langdon House was inspired by the warm, familyoriented values of Athena Care Homes. Since arriving, she’s enjoyed a fantastic welcome from the team and is excited to work together to make great strides in 2025. "It’s all about teamwork," she explains. "A strong team is the key to success."
Living on the Suffolk-Cambridgeshire border, Andreea has always wanted to work in Cambridge, a city she loves. Now, as part of the Langdon House family, she’s eager to bring fresh ideas and energy to the role. Outside of work, Andreea has two children who keep her busy but when she does take a moment to unwind, you’ll likely find her with a good crime thriller in hand.


A White Paper commissioned by Care England has suggested that an innovative mattress-turning system has the potential to prevent pressure ulcers occurring for people in adult social care, while improving their comfort and promoting healing – all while delivering significant cost and resource savings to care providers and the NHS.
The paper, called Preventing Pressure Ulcers: The Role of Automatic Lateral Turning Systems for Innovative Approaches to Pressure Ulcer Prevention in Care Homes examines and summarises a 12-week trial of the Levabo Turn All automatic lateral turning system (ALTS), developed in partnership with Algeos Ltd (UK).
The White Paper says that pressure ulcers are one of the most painful and preventable conditions faced by some of the most vulnerable individuals in adult social care.
Care England, the voice of care, is a registered charity, is the leading representative body for small, medium and large providers in England.
The report stated pressure ulcers affect 700,000 people a year in the UK at a cost to the NHS of £1.4 to £2.1 billion a year.
It added that “the realities of staff shortages, increasing demand, and the need for manual repositioning often place an undue burden on both caregivers and residents,” so residents did not always receive the attention they needed to ease the pain caused by their ulcers.
Furthermore, Professor Martin Green OBE, Chief Executive of Care England, said “technological solutions like this would not only ease the workload of the caregiver, but it would also offer a more dignified care solution to the individual as well as an improved quality of life”.
The trial took place in three care homes in the UK and involved 24 residents across 12 weeks, addressing manual repositioning for pressure ulcer prevention using the Levabo Turn All solution which is an automatic tilting system (ALTS) that helps prevent and treat pressure ulcers by positioning a person in a 30-degree side position alternating between the right and left side. The system can be used in any healthcare bed with a removable mattress, where it is placed under the mattress.
The trial focused on residents with dementia with multiple and complex comorbidities, and those receiving palliative end-of-life care who are particularly vulnerable to pressure ulcers due to immobility and frailty.
The primary aims were to assess the effectiveness of the system in reducing pressure ulcer incidence, its impact on caregiver workload, resident comfort, and overall cost-effectiveness.
During the trial, the system was successful for residents with both dementia or dementia with challenging behaviours; existing pressure ulcers/vulnerable at-risk skin; limited or no mobility; pressure ulcer prevention and treatment; end of life/palliative care; critical illness and spinal/neurological conditions.
Key findings from the trial included that using ALTS in a care setting has several key benefits, particularly for residents at risk of developing pressure ulcers and those in end-of-life palliative care.
The system was effective in preventing and managing pressure ulcers by automatically repositioning residents, thus reducing prolonged pressure on vulnerable areas, significantly lowering the risk of further breakdown of skin without unnecessarily disrupting residents, leading to improved sleep and quality of care by automating the manual task of turning residents which can be every 4 to 6 hours, day and night requiring two caregivers’ time and effort to reposition. The system freed up caregivers’ time to focus on other critical tasks and areas of care – often up to two hours a day per person.
The White Paper also found that use of the system delivered cost savings in preventing the occurrence of pressure ulcers and the need to treat them.
In addition, residents using ALTS generally showed fewer signs of discomfort or agitation during repositioning, an important factor for those with dementia. The report stated for residents in palliative care, ALTS provided a gentler, less invasive approach to repositioning, supporting their comfort and dignity during end-of-life care.
One of the homes taking part in the trial, the Taylor and Taylor group, said that each caregiver would save two hours a day through not having to manually turn an individual during a 24-hour period. Given 11 people needing this facility, that would save 22 hours a week which in monetary terms based on an average salary, equates to circa £1,600 a week and roughly the same cost of one system itself.
Professor Green said: “The trials have shown that a system of this type can in many cases provide big benefits in pain reduction and healing for the individual, while easing the burden of care to the caregiver and doing so at a net saving of cost to the care provider or allowing them time to support other aspects of their care plan”.
“The trial has shown that once again, technology can work hand-inhand with excellent care provision to offer dignity, pain reduction, and enhanced healing to those most in need of it.”
Beth Mercer, Commercial Manager at Algeos Ltd (UK) said: “The trials have shown exactly what we hoped – that the Levabo Turn All system not only makes life more bearable and dignified for the individual by reducing their risk of pressure damage, pain and discomfort; it eases the workload and burden of repositioning to staff, freeing up time to focus on other aspects of care, and demonstrated time, cost savings, and efficiencies thus providing benefits to caregiver and care receiver alike.”

Specialist business property adviser, Christie & Co, has today launched its Business Outlook 2025 report which reflects on the themes, activity and challenges of 2024 and forecasts what 2025 might bring across the sectors in which Christie & Co operates, including in the care sector.
Christie & Co labels 2024 as a year of growth in the UK care market, with the majority of operators having reported improved occupancy levels, a reduction in agency usage, and a return in buyer confidence which resulted in an increase in transactional activity across the market.
‘Small/medium-sized groups’ (groups of 3 to 19 care homes) were the most active buyer group in 2024 thanks largely to the return of occupancy, this is a notable shift from the most active in 2023 which was first-time buyers and independent purchasers. However, deal times continued to be delayed as issues with the Care Quality Commission (CQC) persisted.
Christie & Co also notes a reduction in the number of closed, vacant care homes in 2024 – this asset class made up 12 per cent of the company’s healthcare sales in 2024 compared with 16 per cent in 2023. This is largely due to a material reduction in closed care home instructions and is not a reflection in declining investor appetite for re-purposing this stock.
There was a clear reemergence of real estate investment activity following a relatively benign market environment in 2023 whereby investors adjusted to a range of factors including higher interest rates, inflationary pressures, and an upward movement in government gilts. Christie & Co witnessed yields stabilise in 2024, with market activity seeing a notable pick up.
The land and development market faced stronger headwinds due to construction cost inflation, ongoing challenges in the planning system, and the availability of debt. However, the need for future-proof care beds remains undiminished and the underlying ESG credentials, together with future bed demand, remain compelling for investors.
Christie & Co expects the combination of improved operational trading performance and stabilisation of construction costs, to provide increasing confidence to return to the development markets, resulting in an uptick in demand for consented sites and transactional activity forecast for 2025. A greater number of developments are coming forward in untapped regions including the southwest of England, Wales and London and it is expected that this will continue into 2025.
PRICE MOVEMENT
Christie & Co notes that higher interest rates hampered new deal activity early in 2024 and the calling of a general election created uncertainty in the market. This led to buyer hesitancy and a decline in the number of care homes coming to the market. Positively, activity levels increased in Q3 following a reduction in interest rates and the general election result. The impact of the changes in employer National Insurance contributions (NICs) in the Autumn Budget is yet to be fully understood but the momentum of the transactional market was undiminished in Q4. Given the wider turbulence, underlying demand from investors remained strong with good prices achieved. Christie & Co’s price index reflects this with a 1 per cent overall increase.
MARKET SENTIMENT
As part of its annual sentiment survey, the company surveyed care providers across the country to gather their views on the year ahead. When asked about their sentiment in 2025, 31 per cent said they feel positive, while the majority (39 per cent) said they feel negative about the year ahead. When asked about their sale and acquisition plans, 59 per cent stated that they are looking to buy and/or sell this year.
MARKET PREDICTIONS
In the care market in 2025, Christie & Co expects: Increased activity with interest rates easing
• Increased deals funded by REITS
• Continued first-time buyer activity
• Margins squeezed on those dependent on local authority fees
• ESG credentials will become increasingly important for both owners and funders
Existing operators will continue to expand with a preference for businesses with upside
• Concern around staffing cost increases versus local authority fees
• Healthcare will continue to be a key target sector for investors
Richard Lunn, Managing Director – Care at Christie & Co, comments, “2024 was another challenging year and the care sector which, like many, employs a significant workforce is notably impacted by the increase in employers’ National Insurance contributions with little certainty that local authority fee increases will be sufficient to cover the differential. However, strong operators are alive to all the challenges, and we are sure that appetite for the whole spectrum of care busi-

nesses will continue and, therefore, 2025 will see an increase in activity from a range of buyers and REITS.”
Jordan Rundle, Director & Head of Healthcare Development & Investment, comments, “Following a prolonged period of headwinds in the land and development market, momentum is building in the new build sector and this has been largely driven by stabilisation of costs and improved underlying trade performance in the private pay arena. As confidence returns, we are already seeing a noticeable uptick in demand from operators for good quality consented care home sites and anticipate greater land deal volumes over the next 12 months.”
To read the full business outlook report, visit: https://www.christie.com/news-resources/business-outlook2025/care/uk

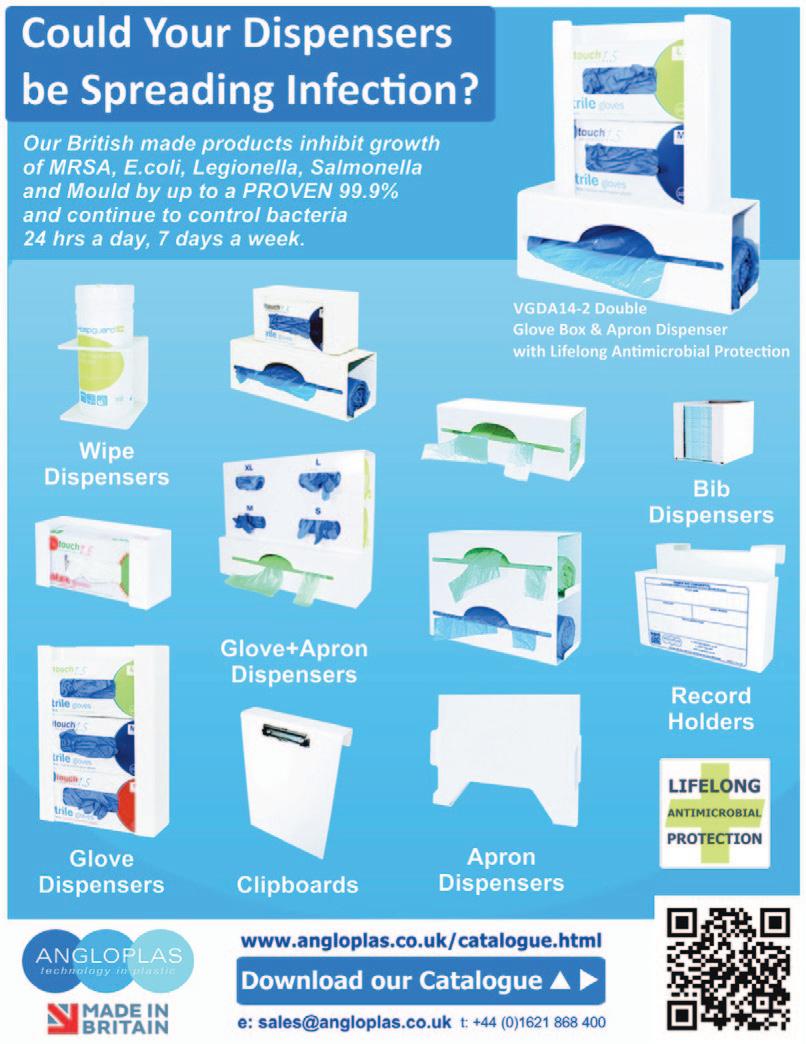
Throughout the year, Elmfield Care, residential care home providers, undertake many fundraising and charity activities within their care homes to give back to the local community.
Across their three care homes, Elmfield have raised a total of £2,348.23 for various charities, with details below of some of the fundraising work that has been happening at their care homes.
NODENS MANOR – LYDNEY

Through recent charity work and fundraising events at Nodens Manor care home in Lydney, £1,089.69 has been raised for Great Oaks Hospice, a local charity in the Forest of Dean.
Bartosz Turewicz, General Manager at Nodens Manor raised an incredible £700 by facing his fears and doing a Skydive, jumping from an altitude of 15,000ft.
The care home also organised a summer party raffle, with staff bringing in home-made craft items including crystal resin decorations by Sara Uzzell, Care Assistant, handmade pottery ornaments by Charlotte Scarrow, Front of House and polymer clay earrings by Lenka Stastna, Care Assistant. The Summer party raffle raised a total of £389.69 for Great Oaks Hospice.
Nodens Manor’s charitable efforts don’t stop there, as they recently welcomed New Start Cat Rescue in for a volunteer visit with two kittens and a cat they had rescued, with further visits scheduled, allowing the residents to play and bond with the cats. The care home will be supporting the charity with cat food donations.
Donations are also being collected for ‘The Forest Foodbank’, with the care home hoping to top last year’s donation of 24.9 kg, to help those in need over the winter months and Christmas period.
OLD SARUM MANOR – SALISBURY

Fundraising activity at Old
raised £412.50 so far for The Care
to advance the financial, professional and mental
care workers.
This money was raised at the care home’s Country and Western themed summer party, which featured a tombola, raffles, arts and crafts made by the residents on sale, a cake sale and plenty of party games!
Old Sarum Manor will be continuing to fundraise for The Care Workers Charity this month, with an event planned for the care home staff to wear orange to work. As orange is the colour of The Care Workers Charity, this will help to encourage donations to the charity, alongside the added benefit of brightening up the resident's day.
FLOWERS MANOR – CHIPPENHAM
Across the last 12 months, Flowers Manor care home in Chippenham has raised £846.04 for Dementia UK, their chosen charity for the year. Dementia is a growing cause for concern in the UK so the money raised
will go towards vital research and supporting those in need.

The money has been raised by hosting raffles with prizes ranging from Easter hampers to beauty sets to delicious shortbread biscuits. The home also hosted afternoon teas for not only the residents but extended the invite to their friends and families. This helped to engage the wider community in the fundraising efforts.
Flowers Manor residents have been involved in selecting their next charity of the year, Bath Cats and Dogs Home, and they will be fundraising from now until September 2025 for the charity.
The charity is close to the resident’s hearts, and they take in cats and dogs from the public RSPCA inspectors, police and dog wardens. They also reunite animals with their owners and manage the adoption of rescue pets.
Raising money isn’t the only positive outcome of such activity, as Emily Luckhurst, Lifestyle Manager at Old Sarum Manor, shares the additional benefits of care homes running fundraising activities, “Having fundraising events in the care homes give the residents and staff a welcome break from everyday routines and can bring emotions such as joy and excitement by having something to look forward to and plan for.
“They also help to get the residents actively involved and bring with it increased engagement and confidence. Whether they are baking a cake for a bake sale or manning a raffle stall, the importance placed on their role and greatly impacts their experience at the care home.”

A Rugeley home has had two residents celebrating their 100th birthdays in the month of January.
Two residents at MHA Briar Hill House Joan Hollins and Viney Jordan celebrated their 100th birthdays with parties arranged by the home.
Viney worked as an tax officer for inland revenue and in her younger days lived in her grandparents pub, the Jolly Collier, in Brownhills.
Joans party included her four grandchildren, 10 great grandchildren, eight great great grandchildren and one great great great grandchild.
Both residents also receive a telegram from King Charles.
MHA Briar Hill House provides residential and nursing care for 36 residents.
Nina Varndell, activity coordinator said: “Both residents had a great time celebrating their birthdays.
“It felt very special having two residents turning 100 in the same month.
“Viney told us she always worked hard, kept herself fit and ate healthy food, something which she thinks may have contributed to her living a long life.
“Joan really enjoyed having her family members around her and it was amazing to see five generations of her family under one roof.
“Both parties went really well, everyone enjoyed themselves and we were all very happy for Joan and Viney.”

HC-One’s Daneside Mews Care Home, in Northwich, Cheshire, has been celebrating all things cheese to mark National Cheese Lovers Day on Monday, January 20, 2025.
Cheese Lovers Day is an annual event which celebrates the art of cheesemaking, and the different types of textures, rich flavours and types of cheeses that enhance culinary experiences.
Residents at Daneside Mews Care Home have enjoyed celebrating the special day by hosting a cheese and wine night. Residents enjoyed the cheese and wine night alongside their family and friends.
Residents enjoyed expanding their taste buds to explore the vast diverse range of cheeses on offer, including sampling new and exotic varieties to revisiting their
beloved classic favourite cheeses. Residents indulged in their favourite dairy delights, including tangy blue cheese, creamy Brie cheese, sharp cheddar cheese, Cranberry, Apricot and much more.
The selection of cheeses was accompanied by a choice of wines, including red and white. Residents enjoyed taking part in a singalong and were soon tapping along and up on their feet dancing to their favourite tunes.
Kali Whitbread, Home Manager at HC-One’s Daneside Mews Care Home, stated: “All of our residents and their family and friends enjoyed our cheese and wine night. It was so lovely to see the residents socialising and having a great laugh together.”

Last week was the busiest yet for the NHS this winter, amid sky-high virus rates which have left hospitals ‘jampacked’ with patients.
New data from NHS England shows that more hospital beds were occupied last week (w/e 12 Jan) than at any point so far this winter (97,636), with 96% of adult general and acute hospital beds occupied.
In the same week, almost 1 in 7 occupied hospital beds (13,585) were taken up by patients who were fit to be discharged.
Flu cases in hospital are down from their peak, but England’s leading emergency doctor has warned today that hospitals are ‘not out of the woods yet’, with flu rates still 3.5 times higher than last year – 4,929 patients were in hospital with flu on average each day last week.
As winter viruses and cold weather continue to create enormous pressure on front line services – leading many hospitals to declare critical incidents – there were also 1,112 patients in hospital with Covid on average every day last week.

There were also 650 norovirus patients, up 4% on the previous week and up 44% on last year, as well as almost double the number of children in hospital with RSV compared with the same week last year (52 vs 27).
Amid the high levels of demand, the NHS has opened 1,000 more beds compared to same week last year (103,847 vs 102,784 last year), and despite the huge pressure, time lost to ambulance handovers was down almost 40% on the week before (29,956 vs 49,002).
Ahead of winter, the NHS put in place measures to manage extra demand including upgraded 24 hour coordination centres, support for frequent users of A&E services, strengthening same day emergency care and providing more care in the community.
NHS teams have also delivered a total of 29 million flu, Covid and RSV vaccines since the autumn cam-
paign kicked off, and while the national vaccination booking system has now closed, those eligible can still get protected by visiting a COVID-19 walk-in vaccination site or finding a pharmacy offering the flu vaccine.
Professor Julian Redhead, NHS National Clinical Director for Urgent and Emergency Care said:
“While it is encouraging news that flu cases are no longer increasing, hospitals are not out of the woods yet.”
“Staff are working incredibly hard in sometimes challenging surroundings, but winter viruses are much higher than usual for this time of year, and this coupled with the cold snap and problems discharging patients means hospitals are jampacked with patients – even as more beds have been opened to manage increased demand.”
“With pressures on hospitals still formidable, it’s vital people continue to use NHS services in the normal way – using 111 and 111 online if you need advice and support for health conditions, and only using 999 or attend A&E in life-threatening emergencies.”
Health and Social Care Secretary, Wes Streeting said:
“Despite NHS staff doing their level best, the experiences of patients this winter are unacceptable. Annual winter pressures, which will always exist, should not automatically lead to an annual winter crisis.”
“We have ended the strikes, so for the first winter in 3 years staff are on the front line not the picket line, and introduced protected more patients with flu vaccinations than last year, but there is much more to do.”
“It will take time to turn the health service around so patients receive the standards of care they deserve, but it can be done. Through our Plan for Change this government is making the investment and fundamental reform needed to make sure the NHS can be there for us when we need it, once again.”
This winter, Recreo VR is offering care homes an exciting opportunity to enhance resident wellbeing through the power of Virtual Reality (VR). By signing up for one of our 24-month Recreo Theatres packages, you’ll receive a free VR headset and staff training.
Our platform provides person-centred, budget-friendly activities that are fun, engaging, and accessible, especially for residents who are bedbound or socially isolated. Co-created with Alzheimer’s Society and individuals with dementia, our service empowers staff to deliver personalised reminiscence and one-to-one sessions that promote memory recall and connection.
Our VR headsets have been recognised as good practice by the Care Quality
Commission (CQC), further validating their impact on care. Regular use of Recreo VR has a proven positive effect on wellbeing, with residents reporting increased activity, engagement, and social connection, often leading to a reduction in the need for PRN medication.
Whether combating loneliness, promoting relaxation, or enhancing cognitive health, VR offers a non-pharmacological solution to enrich care and elevate quality of life. Don’t miss out! Take advantage of this exclusive offer and see how VR can transform your care home experience.
For more information, visit recreovr.co.uk. Or contact us at info@recreovr.co.uk or 01482 526940.


Digital Care Hub has launched a new support programme for adult social care providers with up to 50 staff in the North West, West Midlands and South West.
Funded through the Department of Science, Innovation and Technology’s Cyber Local programme, this new service will help providers to strengthen their ability to manage cyber security incidents. It includes in-person workshops, cyber vulnerability assessments, and webinars based on typical cyber incidents.
Cyber Resilient Care is being delivered by four of our local support organisations in partnership with our national team and police-led Cyber Resilience Centres. The workshops and assessments are available to ten care providers in each of the three regions and will prioritise CQC-registered services and day care. The webinars are open to all small providers.
Speaking about the launch, Daniel O’Shaughnessy, Head of Programme Delivery at Digital Care Hub, said:
“Digital Care Hub is delighted to offer this really practical support to small care providers. We know they often struggle to have specialist knowledge and skills in place to manage security incidents. Our Cyber Resilient Care programme will build their skills and confidence in an accessible, practical way based around typical cyber security scenarios that are most likely to affect small providers.
“This new programme builds on our existing work: it will be delivered by four of the trade associations that currently support our Better Security, Better Care programme. But we are also bringing in additional technical assistance from local police-led Cyber Resilience Centres, as well as adapting existing exercises and resources from the National Cyber Security Centre. So providers can be reassured that the support they receive is delivered by cyber and social care experts. It’s a great combination.”
The project is being run between January and March 2025. The following local support organisations are inviting small adult social care
providers in their regions to take part:
Partners in Care Dorset and the Registered Care Providers Association, Somerset: for care providers across the South West. West Midlands Care Association: for care providers across the West Midlands.
Liverpool Social Care Partnership: for care providers across the North West.
If a care provider meets the eligibility criteria and have not been invited to take part by mid-January, they may wish to contact the support organisations.
Details available at www.digitalcarehub.co.uk/CyberResilientCare
Phoebe Layfield received the most nominations throughout the year
A 24-year-old care assistant at a Burnley home has been recognised for her tremendous work ethic and attitude and has been awarded the home’s employee of the year.
Phoebe Layfield started working at MHA Heather Grange in May 2023 after finding out about the home from her sister who worked there.
Phoebe started her journey of working in social care three years ago but says the love for her job and the work she does grew when she joined MHA Heather Grange.
The employee of the year award is given to someone who is recognised by staff, residents, family and friends as someone who goes above and beyond in their role.
Phoebe received the most nominations throughout the year for her caring nature and the kindness shown to those she cares for and works with.
The home offers residential and dementia care for 70 residents
Speaking after winning the award she said: “I was aware of the employee of the


month awards, but the one for the year was a total surprise.
“It feels really nice to be recognised and I feel extremely proud.
“I really enjoy working in care, my role includes supporting residents in everyday needs, including general care and mobility.
“The residents and staff at MHA Heather Grange are great, they are easy to work with and we all get along really well.
“The home’s atmosphere is what makes it a great place to work.
“I am so glad I decided to join just over a year ago and I am very happy with where I am.
“Working in social care you do need to have certain attributes like being compassionate and caring.
“For me, I want to make a career in care, progress forward and hopefully become a nurse.”


• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.



Pauline Quirke has been diagnosed with dementia and will be stepping away from acting, her husband has confirmed.
The 65-year-old actress, best known for playing Sharon Theodopolopodous in the hit comedy sitcom Birds of a Feather, was diagnosed with the condition in 2021.
In a statement released yesterday (Tuesday) Steve Sheen, who has been married to Pauline since 1996, said it was “with a heavy heart” that she was stepping back from her professional and commercial duties because of her diagnosis.
Steve added: “We are deeply grateful for the support of her peers, the public and the dedicated staff and Principals at PQA [Pauline Quirke Academy of Performing Arts].
“We kindly request privacy and understanding for Pauline and our family during this difficult period. Pauline just wants to spend time with her family, children and grandchildren.”
Pauline and Steve have pledged future support to Alzheimer’s Research UK and will be working alongside the charity to drive funds for research and awareness of dementia.

Steve said: “We are very proud of what our family friend Scott Mitchell is doing with Alzheimer’s Research UK in his late wife Dame Barbara Windsor’s name. So, when we feel able, we will also align ourselves with the charity.”
Pauline remains one of the most recognisable stars of British comedy, with Birds of a Feather attracting nearly 20 million viewers at its height. The show premiered on the BBC from 1989 until 1998 before being
resurrected by ITV in 2014 where it continued for another six years.
With a career spanning over 50 years, Pauline has starred in more than 60 TV and film productions, including a BAFTA-nominated performance in The Sculptress. She has also had roles in Broadchurch, Carrie’s War, North and South, Casualty, Cold Blood, My Family and Emmerdale.
Pauline was awarded an MBE in the late Queen’s final Birthday Honours, in recognition of her work with young people, contributions to entertainment and dedication to charitable causes.
If nothing changes, one in two people will be directly affected by dementia – either by developing the condition themselves, caring for someone with it, or both. Alzheimer’s Research UK is striving for a cure for dementia by revolutionising the way the condition is treated, diagnosed and prevented.
Hilary Evans-Newton, Chief Executive of Alzheimer’s Research UK, said: “We are saddened to hear of Pauline’s diagnosis and send our best wishes to her, Steve and the wider family. The family should be praised for making the brave decision to make her diagnosis public, which will not only provide more freedom for them, but also raise such vital awareness of the condition.
“We’re so grateful that Pauline and Steve have pledged to support our work when the time is right. We look forward to working with them to raise further awareness of dementia and funds for research.”

The North Devon community gathered at Kenwith Castle care home for the annual Candles on the Lake event. Kenwith Castle, which is operated by not-for-profit charity, Care South, hosted the commemorative event for members of the public and local carers who work in and around Bideford, as well as residents and their families to congregate in memory of their loved ones. It was also attended by residents of the Kenwith Castle Gardens and Kenwith Meadows assisted living bungalows, which are based overlooking the lake and grounds in the wider care village in the expansive Devon countryside.
The event’s attendees were invited to sponsor a candle and write a message to their loved one on a heart before it was placed with the candle onto the lake. All donations from the event went to North Devon Hospice, which provides specialist care support to people with life-limiting conditions. Residents from Fremington Manor care home, a neighbouring care home also run by Care South, had a
specially dedicated float at the event filled with candles in memory of the residents’ relatives and friends. The float served as a poignant tribute, allowing residents to honour and reflect on those they have lost in a heartfelt and meaningful way.
Jo Passmore, Home Manager at Kenwith Castle care home, said: “It was incredibly moving to see the residents joined by so many members of the local community for a moment of reflection, as well as residents from the wider care village. We are so lucky to have such a beautiful lake within the grounds of the care village and it was the perfect setting to host our annual Candles on the Lake event in partnership with North Devon Hospice, which supports people in the local community.”

Eileen, who lives at Kenwith Castle care home, said: “I dedicated a candle to my husband. I miss him deeply but the event was a lovely way to remember him.”
Mary, who also lives at the care home, said: “I wrote on two hearts for my husband and my son. It was a very well organised event and a lovely way to remember our loved ones.”
On 7th November, whilst the tectonic political plates were shifting, here and in the USA, another event of national significance was happening – launch of the UK’s first national urgent acute medical service, by pioneering digital health company Virtue. We’re pleased to provide a sneak preview of their launch, which will be covered by national press in January, explaining what this means for your patients, together with your businesses, both of which stand to benefit by this transformational service that brings together acute and social care in a novel way.
For the first time in the history, the people of Great Britain can access urgent acute medical treatment, nationally, by an organisation other than the NHS. Not only this, but care can be received instantly, in the comfort and convenience of home, simply by calling Virtue. This offers patients an alternative to attending NHS A&E or suffering the impact of a hospital admission.

This appears a momentous step change in the evolution of our national healthcare infrastructure, which could be a vital component in ensuring members of the public, can access acute care quickly, in spite of the rising pressures on the NHS system.
For just £14.99 per month, anyone over the age of 18 can become a Virtue Member. Virtue Members receive a Welcome Pack which includes a range of smart medical devices that enable Virtue’s remote team of nurses and consultant specialists, to respond to an urgent medical need immediately. Their clinical team then monitor the patient, prescribe medication and even provide online physiotherapy to support holistic and faster recovery. Where needed, Virtue also provide IV antibiotics in the home. Virtue call it ‘Acute Hospital-at-Home’, also coined ‘virtual ward’.
Before you think it’s too good to be true, Virtue do also charge a fee of £125 per night for treatment, which given the average ‘length of stay’ of 7 nights, can add up to £875. So overall, it’s not cheap. So, is it worth it?
We asked Dr Andrew Barlow, Chief Medical Officer of Virtue, his view and justification for the cost. Dr Barlow, who is recognised by NHS England as founder of the first NHS Covid virtual ward explains, “a hospital admission is a catastrophic life event, especially for someone over the age of 70. Patients are suffering from a serious, often life-threatening medical situation, which is made more traumatic by separation from their family, familiar environment and care team. Patients are at risk of acquiring infections, which during the pandemic caused one third of covid cases. Perhaps worse of all, is the ‘hospital-acquired degeneration’, which research shows to leave patients with an average 50% loss of functional ability. Patients leave hospital a shadow of their former self, and at that age, they just don’t recover. This often means patients are discharged into a care home, meaning they leave their domiciliary care provider and are forced to sell their family home”.
So is it worth it? We think so. In fact, we think this is revolutionary.
Not only is this a game changer for the patient, but Virtue CEO and Founder Robert Orford believes it will play a key role in fixing the fundamental historic divide between the acute and social care sectors. Robert explains, “we offer a partnership programme to domiciliary care and nursing homes providers, meaning they benefit financially from the delivery of our treatment, at a rate of £40 per hour. This enables our partners to pay their staff more, recruit and retain talent and fundamentally change the profitability of their business”. Interested

Patients dying in corridors, lack of equipment and unsafe practices are the findings of a new RCN report documenting the experiences of more than 5,000 NHS nursing staff.
Almost 7 in 10 (66.8%) respondents to an RCN survey said they’re delivering care in over-crowded or unsuitable places – such as corridors, converted cupboards and even car parks – on a daily basis.
Demoralised nursing staff report caring for as many as 40 patients in a single corridor, unable to access oxygen, cardiac monitors, suction and other lifesaving equipment. They report female patients miscarrying in corridors, while others said they cannot provide adequate or timely CPR to patients having heart attacks.
More than 9 in 10 (90.8%) of those surveyed said patient safety is being compromised.
RCN General Secretary and Chief Executive Professor Nicola Ranger said: “This devastating testimony from frontline nursing staff shows patients are coming to harm every day, forced to endure unsafe treatment in corridors, toilets and even rooms usually reserved for families to visit deceased relatives. Vulnerable people are being stripped of their dignity and nursing staff are being denied access to vital lifesaving equipment. We can now categorically say patients are dying in this situation.”

More than a quarter of nursing staff surveyed said they weren’t told the corridor they were providing care in was classed as a “temporary escalation space”, as described by the NHS in England.
This means risk protocols and additional measures may not be in place to ease pressures and protect patients.
The report follows a letter sent to the Westminster government and NHS England from an RCN-led coalition, calling on officials to publish how many patients are being cared for in corridors and other inappropriate places.
Nicola added: “The revelations from our wards must now become a moment in time. A moment for bold government action on an NHS which has been neglected for so long. Ministers cannot shirk responsibility and need to recognise that recovering patient care will take new investment, including building a strong nursing workforce.”
Assistant Director of Policy, Tim Gardner, said: ‘Today’s report from the Royal College of Nursing brings into sharp focus the harrowing experiences facing some patients and staff in NHS hospitals this winter.
‘Delays in A&E and resorting to corridor care is not a safe way to run a health service, putting patients at risk of avoidable harm and, as these testimonies highlight, taking a major toll on NHS staff.
‘Trolley waits in A&E – one measure of the problems in emergency care – hit record levels in 2024, with over half a million patients waiting over 12 hours for admission to a hospital bed. Such delays were a rarity before the pandemic but are now the worst we have seen since records began in 2011. This is a symptom of an NHS worn down by the pandemic and the decade of underinvestment that preceded it.
‘This report illustrates the scale of the challenge faced by the new government, just in getting the NHS back on its feet and delivering the standards of care people expect, let alone the complexities of longer-term reform. Unfortunately, there are no quick fixes and action is needed right across the health system, including investment in additional capacity in both primary and acute care, new technology and skills to streamline services and boost productivity, as well as long overdue reform and investment in social care.’
Tim Baverstock, Head of Local Systems Influencing, Alzheimer’s Society said; “It has been very difficult to read the harrowing accounts of nurses working on the increasingly demanding front line of NHS ‘corridor care’ reported by the Royal College of Nursing, particularly when patients with dementia have been distressed or unable to receive appropriate care. We hear many similar traumatic stories from family members who contact the Alzheimer’s Society support line.”
“It is vital that we prioritise interventions like early diagnosis and effective treatment, alongside adequate dementia training for the social care workforce, to reduce unnecessary hospital admissions for people living with dementia and relieve the pressure on overcrowded hospitals while protecting patient safety and dignity. These interventions must be considered as key elements of the government’s 10-year Health Plan consultation process. Dementia, and the impact on the NHS workforce, is a whole-system challenge and must be prioritised with the utmost haste.”
Caroline Abrahams, Charity Director at Age UK said: “Nye Bevan must be turning in his grave: the apparent normalisation of ‘corridor care’ is an affront in a civilised society and for the sake of the public and staff alike must cease. We know that older people are especially likely to be on trollies for long periods and this is no place for them to spend what for some will be their last hours and minutes. We urgently need to see a plan from the Government & the NHS to phase out this shameful practice as swiftly as possible, and if the Treasury needs to come up with some extra funding to enable this to happen it should.
“It’s hard to think of a more certain way of both undermining public trust in the NHS and the retention of skilled nurses than tolerating very sick older people being ‘stacked up’ in passages, as if they were lorries on a motorway.”

Care provider Hartford Care has invested £4 million across its care and nursing homes on the Isle of Wight: Highfield Nursing Home in Ryde, Springfield Nursing Home in Shanklin and Inver House and The Elms in Bembridge.
Work has recently commenced on an £850,000 improvement project at Inver House on Foreland Road, Bembridge, which will involve the refurbishment of the communal areas and new carpets, furniture and fittings throughout, along with external redecoration and improvements to the approach to Inver House and the car park.
In October last year, Springfield Nursing home on Arthurs Hill, Shankin, unveiled a newly-built extension with 16 en suite bedrooms, alongside a new lounge, dining area and hair salon. The £2.5 million project also included the redecoration of the existing communal areas with new furniture, to take the home up to 58 bedrooms.
Highfield Nursing Home on Queen’s Road, Ryde, also benefitted from a £500,000 investment, with solar panels to aid the homes energy efficiency and the refurbishment of communal areas, corridors and bedrooms, including the addition of five en suite wet rooms to existing bedrooms.
Finally, The Elms on Swains Road, Bembridge, completed a £150,000 project to improve its parking facilities, including resurfacing.

Kevin Shaw, Chief Executive of Hartford Care, comments: “Future-proofing our homes is a top priority in the company’s sustainability journey. We are continually investing in our homes and exploring new ideas in energy saving technology to put us at the forefront of the industry. Improving our energy efficiency across the board and saving costs with these initiatives will not only protect our planet, but will ultimately mean that we’re able to plough these savings back into our homes to enhance our offering and reinforce the high quality of care we already offer our residents.”
Residents at The Cedars Care Home - Barchester Healthcare were thrilled to see the beautiful birds both in the Garden Lounge and in individual bedrooms. Every resident was given the opportunity hold one of these beautiful and majestic birds; as well as being treated to a display of flight that wowed them all.
Five owls- including a Tawney owl, two barn owls and a long-eared owl visited us with Falconer Ryan, along with a falcon called Maverick. Residents were interested to learn about the birds- did you know that the reason owls stand out from other birds is that they are the only bird with eyes on the front of their heads, and that an owl (if he could read) could read a newspaper headline from up to one mile away?
Tony had been looking forward to the event all week, and he wasn’t dis-
appointed. He said ‘I thought it was brilliant. I’ve never been that close to a barn owl before- it was amazing to see. I have seen the fly past before but they look so much smaller in the air!’ and; and Lydia commented that the animal week at the Cedars has ‘got better and better’- starting with a visit from Darwin the therapy Horse, meeting Alpacas via our virtual event team and ending on a crescendo with the Owl Adventures.
Senior General Manager Rebecca Aldred said: “Our residents have really enjoyed their unusual visitors today. We knew that having the owls here would be a bit of fun for all our residents, especially as some find it difficult to go on many outings in our minibus. We are always looking for new activities for the residents and today we have seen the seen the enjoyment and the therapeutic influence animals can have on people.”


Lighting plays a vital role in every aspect of our daily lives. As nursing and care homes continue to navigate rising energy costs, lighting has emerged as a critical area for improving energy efficiency with the potential to reduce lighting costs by as much as 85 to 90%1 by using efficient solutions. The type of light bulb used can impact the time and cost spent on maintenance which is particularly important in care settings where costs saving measures are prevalent2
By adopting smarter lighting solutions, nursing and care homes can reduce energy consumption while enhancing the overall environment for occupants. In this article, Dyson shares how the sector can adopt smarter lighting solutions that not only help to cut costs but also support inhabitants’ wellbeing.
Many nursing and care homes across the country are now equipped with motion activated lighting, reducing costs, improving energy efficiency and avoiding unnecessary usage. By investing in lighting that is also controllable by an app, care managers have the flexibility to turn off lights remotely at the touch of a button adding an additional level of peace of mind.

Changing light bulbs regularly takes time, investment and organisation. Fluorescent lighting can be inefficient, waste light and use costly-to-replace bulbs. Without proper cooling, LED bulbs can quickly overheat, causing fading, discolouring and them to work efficiently. Lights such as the Dyson Solarcycle task light that use Heat Pipe technology can effectively cool the LED and protect the light quality for 60 years3. In turn, this allows the user to reliably adjust its colour and brightness without flickering bulbs and outages.
Recognising the importance of fostering a happy, healthy, and supportive care environment, care home settings are placing increased emphasis on these aspects. While lighting may seem inconspicuous, it profoundly impacts the wellness of residents and caregivers alike.
In many nursing and care homes, lighting can feel clinical with a ‘one size fits all’ approach to lighting which creates strain on the eyes. Acknowledging that individuals have diverse needs and perceptions regarding wellness and mental health, these spaces must remain adaptable to meet these varied requirements effectively. By creating bespoke lighting options in individual rooms, a user can adjust the lighting to suit their specific needs.
Low quality light can cause negative side effects such as migraines, headaches and eyestrain. By giving occupants the option to adapt something as simple as lighting to suit their needs will have positive effects on their wellbeing and comfort.
In addition, we spend about 90% of our time indoors4, exposing ourselves to artificial lighting more often than not, with many neglecting to think about how this can affect their sleep cycle. Light is a primary external factor influencing sleep patterns. While the notion that darkness aids sleep is commonly understood, the relationship between light and sleep is far more intricate.
Light plays a pivotal role in regulating the body's circadian rhythm, the internal clock dictating periods of wakefulness and rest. Moreover, it impacts the production of melatonin, a hormone crucial for promoting sleep. The daily exposure to light, including its quality, timing, and duration, significantly impacts sleep quality. Understanding the intricate connections between light and sleep empowers individuals to optimise their residing environment for consistent and restorative sleep.
In conclusion, strategic lighting design and innovation go beyond energy savings. By adopting human-centric lighting solutions, nursing and care homes can create environments that not only enhance their residents’ wellbeing and prioritise their health but also support the productivity and comfort of their caregivers. Lighting, when done right, can be a powerful tool in fostering a happier, and healthier nursing and care home.


1 https://www.lbhf.gov.uk/business/business-connects/support-and-advice-businesses/costdoing-business/guide-energy-efficiency-and-cost-savings-your-workplace
2 https://www.gov.uk/government/news/more-funding-to-schools-hospitals-and-publicbuildings-to-lower-energy-use-and-save-on-bills-and-cut-carbon-emissions
3 LED-life
4 https://ec.europa.eu/commission/presscorner/detail/en/IP_03_1278
To learn more on how to create a nursing and care home that enhances residents’ and workers’ well-being with bespoke lighting solutions, visit Dyson technology’s business hub and book a call:
This month Age Cymru is launching Supporting the wellbeing of older care home residents – A toolkit to bring together helpful resources to enable care homes, families, friends and residents to create the ideal environment for supporting resident wellbeing.
This toolkit, funded by the Welsh Government, has been informed by conversations with residents and professionals across care homes in Wales, as well as local authorities and health boards, drawing on a huge wealth of knowledge and experience.
The toolkit is designed to focus on the four main stages of life in a care home experienced by residents: moving successfully into a home; taking part in meaningful activities; finding a sense of purpose; and having a dignified end of life.
Mirroring the principles underpinning the Welsh Government’s Social Services and Well-being (Wales) Act 2014, the toolkit strives for residents to feel safe and protected, able to learn new things, and have personal dignity throughout their time at the home.
The research found that many care homes are already deploying a wide range of innovative activities. One care home regularly hosts silent discos where the residents get to choose the music they want to hear. Other homes were offering pet therapy or using special celebrations to serve up new foods and provide experiences of different cultures.
The toolkit says providing a good ending for a resident can have a positive impact on the wellbeing of the resident’s friends and family, as well as the care


home staff. It suggests relaxing visiting hours to allow family members to be there when they wish, offering to clear a resident’s room if it is distressing for the family to do so, and honouring the resident by placing their photograph in a prominent place and lighting a candle during their funeral.
Age Cymru’s Kelly Barr, who co-ordinated the toolkit, says: “Care homes have faced unimaginable pressures and challenges over the last few years, and despite this, we have heard incredible examples of how care homes continue to put residents at the centre of their care.
“Staff are recognising the impact that person-centred care can have on the wellbeing of their residents. They also want to integrate residents’ families and carers into their lives as well as those active in the local communities. Older residents should be able to take part in activities that matter to them, feel useful, learn new skills, and stay connected to people that matter to them.
“This toolkit brings together a wealth of resources as well as examples from care homes themselves to help equip staff, residents, and communities with the means to provide the best possible experiences for older care home residents.”
Minister for Children and Social Care, Dawn Bowden said “Care homes play an invaluable role in our communities, and I am pleased that we are supporting them in enhancing the care they provide.
“We know that person centred care can boost the wellbeing of older people, and this Toolkit will contribute towards a positive experience for residents and their families across Wales, throughout their time living in a care home.”
HC-One’s Broadoak Manor Care Home, in St Helens, Merseyside, has been marking the Big Garden Birdwatch taking place from January 24 to 26, 2025. The Big Garden Birdwatch encourages nature lovers to help build a picture of how garden birds are faring by spending an hour or more watching birds in their nearby area and recording the birds that land and submitting their findings to the RSPB.
There are a number of therapeutic and wellbeing benefits for both residents’ minds and bodies, who take part in bird watching activities. This is a fantastic way to engage with nature, keeps the mind stimulated and expands knowledge, encourages residents to be active, and have some fun.
Resident Trevor Howard who has an interest in bird watching researched what birds to look out for in the home’s local area. Trevor, aged 74, went to the local park, Nanny Goat Park in Parr, St Helens, with some bird feed, accompa-
nied by David Baines, Wellbeing Lead, to enjoy a spot of bird watching. Trevor enjoyed the fresh air and observing the feathered visitors on the ground including Robins, Blue Tits, sparrows and the majestic Great Tit. David Baines, Wellbeing Lead at Broadoak Manor Care Home, commented:
“Trevor enjoyed his trip to the local park to bird watch and enjoyed observing their behaviour and seeing all of the unusual birds. Bird watching is a great activity to encourage residents to get involved with as it’s a fantastic individual or group activity to participate in and can be a very thought-provoking activity.
“Residents enjoy bird watching in a tranquil and calming place without any distractions around them to be able to immerse in the full experience. Bird watching also has a number of wellbeing benefits for our residents including reducing stress, anxiety and depression.”
Millcroft care home in Redditch recently hosted a ‘Kindness to Carers’ tea party in its in-house café, bringing together families, local community members, and residents for a special afternoon of gratitude and celebration.
The event was designed to express appreciation for the unwavering dedication and support of carers, both professional and familial, who help loved ones in their care journey.
“Our residents were delighted to be part of the celebrations, and it was heartening to see the café so full of laughter and good conversation," said Lyndsay Sard, Home Manager at Millcroft.
"It’s important to take the time to thank those who play such an integral role in the lives of our residents, and we’re grateful for the opportunity to
show our appreciation."
In addition to the tea party festivities, financial advisor Simon Adkins from Lifestyle Future Ltd was on hand to offer valuable advice to families regarding later-life finances.
Simon, who will be visiting Millcroft every five weeks, provided expert guidance to help families plan for the future and navigate financial decisions related to elderly care.
“We are excited to offer this continued support to families and the wider community,” said Simon Adkins. “I look forward to helping more people with the financial aspects of care, ensuring peace of mind for families during what can be a challenging time."

Not-for-profit care group Greensleeves Care has announced that Chris Doherty, currently Chief Financial Officer, will step into the role of Acting Chief Executive in February 2025.
This follows the recently announced departure of Paul Newman, who is leaving the organisation after over a decade to take up a new role as Group Chief Executive of the Summit and We Care groups.
Chris Doherty has been an integral part of Greensleeves Care’s leadership team for more than ten years. As CFO, he has overseen the organisation’s financial growth and stability, and his experience and knowledge of the charity’s operations will ensure a smooth transition.
Speaking about his appointment, Chris said: “I am privileged to have the opportunity to lead Greensleeves Care during this transitional period. I look forward to working closely with our team to maintain our focus on delivering high-quality care and sup-
porting our residents and colleagues.”
The recruitment process for a permanent Chief Executive is underway and is being led by Green Park Executive Search. Greensleeves Care is committed to appointing a leader who will build on its strong foundation and drive its mission of delivering exceptional care for older people.
Dallas Pounds, Chair of the Board of Trustees, said: “Chris has been part of Greensleeves Care’s success for over ten years and is well-placed to lead the charity as Acting CEO.
We are also looking forward to welcoming a permanent Chief Executive to steer us into the future and remain incredibly grateful to Paul for his transformative leadership over the past decade, during which Greensleeves Care has grown into one of the sector’s leading organisations.”

NHS staff have ramped up the flu vaccination campaign by jabbing almost a quarter of a million more people this winter compared to last winter.
Services across the country have faced extreme pressures from one of the worst winters on record with 5,408 patients a day in hospital with flu in the first week of January.
NHS staff delivered 239, 679 more vaccinations so far this winter compared to the same period last year. This is despite starting the full programme rollout in October, a month later than last year, to offer people the best chance of protection based on advice from the Joint Committee on Vaccination and Immunisation.
The latest figures show a total of 17,996,305 flu vaccinations were delivered by NHS staff between 1 September 2024 and 5 January 2025, compared to 17,756,626 between 1 August 2023 and 7 January 2024.

In recent weeks, flu vaccinations are up more than a quarter (27%) compared to last year with an extra 85,000 jabs delivered in the last 3 weeks. [figures up to 5 January 2025].
Covid, RSV and norovirus cases also remain high with more than 1,100 patients in hospital with Covid in the first week of January, as well as 626 patients with norovirus – up almost 50% on the same week last year (424). There was also an average of 72 children in hospital with RSV every day, up 47% from last year (49).
While the national vaccination booking system has now closed, those eligible can still get protected from flu, Covid-19 or RSV by visiting a COVID-19 walk-in vaccination site, or finding a pharmacy offering the flu vaccine.
England’s top doctor warned that with a deluge of flu cases, the public can play their part by getting vaccinated and continuing to use services as they usually would.
Ahead of winter, the NHS put in place measures to manage extra demand including upgraded 24 hour coordination centres, support for frequent users of A&E services, strengthening same day emergency care and providing more care in the community.
Professor Sir Stephen Powis, NHS National Medical Director, said: “As hospitals face a deluge of flu cases, NHS staff have once again stepped up the vaccination programme this year, protecting almost 18 million people against flu this season – 239,000 more people than last winter.”
“The NHS is experiencing one of the busiest ever starts to the year, with hospitals full to the rafters with flu cases as well as dealing with the recent cold snap.
“The best way to fight the flu is to get vaccinated, and so I would urge those eligible to contact their GP or local pharmacy to get a flu jab as soon as possible.”
“People should continue to only use 999 and A&E in life-threatening emergencies and use NHS 111 and 111 online for other conditions, as well as using your GP and pharmacy in the usual way.”
Minister for Public Health and Prevention Andrew Gwynne said: “Flu is a serious illness which has put significant pressure on the NHS this winter.
“Hospitals remain incredibly busy and the best way to protect yourself is by getting vaccinated, which also helps to ease pressure on the NHS.
“Thanks to all the incredible healthcare staff who have gone above and beyond to vaccinate 18 million people against flu.”
IN LINE WITH ADVICE FROM THE JOINT COMMITTEE ON VACCINATION AND IMMUNISATION,
THOSE CURRENTLY ELIGIBLE FOR A FLU VACCINE THIS YEAR INCLUDE:
• pregnant women all children aged 2 or 3 years on 31 August 2024
• primary school aged children (from reception to year 6)
• secondary school aged children (from year 7 to year 11)
• all children in clinical risk groups aged from 6 months to less than 18 years
• those aged 65 years and over
• those aged 18 years to under 65 years in clinical risk groups (as defined by the Green Book) those in long-stay residential care homes
• carers in receipt of carer’s allowance, or those who are the main carer of an elderly or disabled person
• close contacts of immunocompromised individuals.
• frontline workers in a social care setting without an employer led occupational health scheme including those working for a registered residential care or nursing home, registered domiciliary care providers, voluntary managed hospice providers and those who receive direct payments (personal budgets) or personal health budgets, such as personal assistants
On 15th January, residents and staff at Heron Court Care Home, part of the Runwood Homes Group, have spent the past three months transforming an unused greenhouse into a thriving space for gardening activities. The project, spearheaded by Lifestyle Coordinator Ariel Da Costa, involved cleaning, repairing, and organising the greenhouse, turning it from an overlooked structure into a vibrant hub for horticulture.
The initiative brought together residents Miriam, Joe, and Barbara, as well as carer Ganesh and Ariel, who worked tirelessly to achieve their goal. What started as an ambitious project became a testament to teamwork and determination. Joe, a resident at Heron Court and avid gardener, reflected on the accomplishment: "This greenhouse still needs some improvement, but I think we did a great job, and now it's time to enjoy it."
The idea for the project arose when staff and residents noticed the greenhouse taking up space in the backyard without serving any purpose. Determined to make
it useful again, they embarked on the challenging task of rehabilitating it. Initially, some were sceptical of the effort required, but the atmosphere shifted as progress became visible. Ariel Da Costa noted: "At first, it wasn’t difficult to find people who laughed at us because there was a lot of work ahead. But as we cleaned and tidied up, the greenhouse transformed into what it once was—a place to care for plants."
The residents and staff found immense pride in the completion of their work, especially during two standout moments: the daunting realisation of the challenge they had taken on and the joy of seeing it through to the end.
With the greenhouse now ready for use, Heron Court residents look forward to gardening activities that will foster creativity, relaxation, and community bonding. Ariel emphasised the significance of the project: "This was more than just cleaning and organising; it was about setting a medium-term goal and achieving it together. Now, we have a beautiful space to enjoy and be proud of."

Challenge Works, a global leader in the design and delivery of challenge prizes, has joined forces with expert researchers from the London School of Economics (LSE) to help evaluate the five finalist technologies in the Longitude Prize on Dementia that could revolutionise life for people living with dementia.
The Longitude Prize on Dementia is a £4.4 million prize funded by Alzheimer’s Society and Innovate UK and delivered by Challenge Works.
The prize announced 24 semi-finalists in June 2023, each receiving £80,000 and a package of expert support. Five finalists were selected in October 2024, ranging from high-tech specs to help people recognise objects to football pitch sensor technology applied to predict and prevent falls.
The finalists have each received a further £300k and a package of expert support. They will have until November 2025 to develop their products, before a winner is announced in early 2026 and awarded the £1 million grand prize.
The research, which has been funded by the National Institute for Health and Care Research, will see academics from CPEC, LSE working alongside Challenge Works to evaluate the products. The specialists in health and social care will assess the success of the technologies and provide independent expert analysis to inform the discussions and decisions of the Lived-Experience Advisory Panel – a group of people who have lived experience of dementia including people living with dementia, carers and former carers – and the Judging Panel when selecting the £1 million prize winner.
The LSE team will produce a series of reports detailing each of the five finalists’ products, including the
development process and use of co-design. It will include examination of the effects of the finalist technologies on the quality of life for people living with dementia and determine which, if any, additional resources are needed to improve the products. The report will be published in late 2025.
Martin Knapp, Professor of Health and Social Care Policy at LSE, will oversee the evaluation and will be supported by colleagues including Juliette Malley, Associate Professorial Research Fellow at CPEC, Chiara De Poli, and Valentina Zigante, both research officers at CPEC.
Caroline Purslow, Head of Global Health, Challenge Works said: “These five groundbreaking technologies have been designed to help people living with dementia maintain independence in their home and continue their day-to-day activities. The researchers supporting the prize have significant experience in advanced, evidence-based methods for measuring the impact of health and social care-focused technologies. Their input to the prize and assessment of the solutions will be crucial.”
Martin Knapp, Professor of Health and Social Care Policy, LSE said: “Advanced assistive technology holds immense potential in revolutionising the lives of people with dementia. Using the best possible evaluation process for this prize, in collaboration with colleagues at Challenge Works and the finalists themselves, we can help ensure these products can make a real difference.”
To find out more about the Longitude Prize on Dementia and the five finalists in the running for the prize, visit www.dementia.longitudeprize.org
Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being.
We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or Live Chat on our website, our team is always ready to offer advice and help you find just the right products to bring your ideas to life.
While we embrace the convenience of technology to expand our resources and share knowledge, we remain firm believers in the irreplaceable power of sensory


MOWOOT II – proven solution to chronic constipation without medication
Developed by a team of doctors and other healthcare professionals, MOWOOT II performs gentle abdominal massage to speed up intestinal passage in people experiencing chronic constipation.
Clinically proven, safe and effective, relaxing and sideeffects free, MOWOOT II

Abdominal Massage Therapy System combats constipation and provides soothing relief to affected people.
Easy to use and comfortable, the MOWOOT II treats and manages constipation in people with spinal cord injuries, multiple sclerosis sufferers, Parkinson’s Disease patients and people with constipation related to prescription medication. MOWOOT II also helps to relieve idiopathic constipation experienced by menopausal and post-menopausal women
and older and elderly people.
In clinical studies
MOWOOT II increased evacuation frequency, softened stools, improved regularity, reduced gasses, relieved bloating and eased off abdominal discomfort.
10 to 20 minutes daily of relaxing abdominal massage with MOWOOT II rapidly reduces symptoms of constipation. Evident results are experienced only a few days after the first treatment. Regular abdominal massage with MOOWOOT II ensures lasting health benefits and better quality of life.
MOWOOT II – effective solution to chronic constipation for better quality of life!
Supplied by Win Health Medical Ltd - 01835 864866 - www.win-health.com
See page 3 of this issue for other Win Health products.
Consort Claudgen’s innovation in the electric heating industry takes another leap forward by introducing Wi-Fi-enabled heaters to their low surface temperature (LST) range. These cutting-edge heaters offer unparalleled convenience and efficiency. The heaters connect directly to Wi-Fi, enabling users to control heating through the digital control panel on the heater or via the Consort Connect app. With a comprehensive 7-day timer, which allows 24 individual heating periods per day, and features such as a lock function, open window detection, and custom automation, users can tailor their heating needs to their preferences. Adding to the ease of use, users can view the

energy consumption statistics of all connected heaters, providing insights into usage patterns and potential savings. The LST heaters with Wi-Fi and occupancy sensors have a self-learning control ability. They utilise inbuilt occupancy sensors to detect and learn a user’s weekly presence in a room, creating an intuitive heating schedule. When the space is unoccupied, the heater conserves energy by switching to a setback temperature or frost protection mode.
BIM (Building Information Modelling) objects for the heaters are available for download from Consort’s website. 01646 692172 | sales@consortepl.com | www.consortepl.com
See the advert on page 9.
engagement. That’s why we continue to make our Reminiscence Kits and Sensory Bags with real, tactile items that stimulate the senses. Some experiences—like popping bubbles for the splash, breathing in a familiar scent, or piecing together a puzzle with others—simply can’t be replicated on a screen. These sensory moments are invaluable in encouraging storytelling, sparking memories, and fostering conversation.
Our values remain rooted in this commitment to meaningful connection. We’re here to partner with you—the professionals on the front lines of care—to create a sense of structure, well-being, and fun for those who need it most.
Are you longing for your activity diary to be full? Look no further www.activitiestoshare.co.uk are here for you! See the advert on page 5 or:
customers@activitiestoshare.co.uk
0117 966 6761
07900 6751 50
C&S Seating Ltd have provided postural control equipment to residential homes, hospices, medical equipment services and NHS trust hospitals nationwide since 1991. With 9 different sizes of TRolls and Log Rolls, in a removable and machine washable Waterproof Titex or Soft Knit material. These rolls are used to control posture and position of the body in either supine or side lying. Our Knee & Leg support wedges are available in 2 sizes.
abducted lower limb is required.
Our popular and vibrant range of Soft Knit covers in a choice of 5 colours, provide a softer alternative, ideal for the colder seasons and are designed to fit snug over our waterproof rolls for maximum protection and comfort.

C&S Seating Ltd is the sole manufacturer of the Alternative Positioning Support – also available in two sizes, which has removable side cushions and middle pommel for when more control of the
Contact us on 01424 853331 or visit www.cands-seating.co.uk
Since our incorporation in 1997, Alpha Furniture have always striven to provide the best levels of customer service. At the heart of what we do is listening to our clients’ requirements, and helping to propose the best furniture providing practicality and durability for their unique situation.
• Our chairs aren’t just your typical “care” chairs. Working with multiple manufacturers and designers, we have collated a varied range of styles that move away from the archetypal hospital chair while still maintaining the benefits and practicality of high backs, wings, and easy-clean upholstery.
• Everything we sell comes to you from UK manufacturers, supporting the economy and jobs.
• All of our products come with a minimum 5 year guarantee, so you can have the peace of mind knowing your furniture is built to last.
• Our storage furniture in particular, for bedrooms, lounges and dining rooms, is all delivered fully assembled, and finished with solid backs and drawer bases to prevent bowing or leaning, and so much better suited to a healthcare environment than many high street equivalents.
• We have options for all budgets, with a wide variety of care home suited vinyls and waterproof fabrics across numerous fabric bands.
• We have options for all timescales, with dining sets, lounge chairs and bedroom furniture sets available within 10 working days.
• Our vast range isn’t the end of what we’re able to offer, so if you are looking for something specific

our helpful sales team will help to track down the perfect product.
• Our friendly after-sales team will keep you updated with your delivery, and always look to deliver as soon as possible, often able to bring delivery forward even for made-to-order items.
• Full furniture installation and removal of packaging is an available service* allowing you to concentrate on the busy day-to-day of running a home on the day of delivery.
• As the majority of our furniture is made to order in the UK, almost everything can be adapted, whether you require a wider chair, a narrower dressing table, or simply combining materials on a chair to enhance the design – all for very little additional cost if at all.
For further information, see the advert on page 13 or visit www.carehomefurnituredirect.co.uk
*Additional charges may apply.
Planning and preparation by catering teams in the build-up to Christmas are crucial to ensure smooth operations and a successful festive period. Tess Warnes, Dietician at independent food procurement specialist allmanhall (allmanhall.co.uk), offers her tips on preparing for one of the busiest times of the year.
START EARLY: ORDERS AND DELIVERIES
From the start of November, the demand for festive products surges, leading to limited stock availability across the market. It is important to forecast and place orders as early as possible, enabling suppliers to allocate stock more effectively, thereby reducing the risk of short deliveries and out of stocks.
By placing orders early, catering teams can also take advantage of supplier promotions and manage budgets more efficiently, but still allow for small adjustments closer to the delivery date when more exact operational requirements are known.
While placing forward orders helps suppliers allocate products, it does not guarantee stock. The closer the delivery is to Christmas, the higher the likelihood of shortages. Where there is feasible storage, place orders for non-perishable and long-shelf-life items several months in advance to secure the stock. This also allows more time for contingency plans should there be any stock issues on any products. For fresh produce, work with suppliers or through your procurement partner to schedule advance orders with delivery dates.
Double-check order details, quantities, and delivery dates to avoid
last-minute surprises.
SUPPLIER ENGAGEMENT AND COMMUNICATION
During the busy festive season, maintaining communication within the supply chain is crucial. Regularly engage with suppliers to stay informed about market conditions, commodity challenges, and product availability.
Shortages can arise from limited availability further down the supply chain, such as failed deliveries. Suppliers will attempt to recover stock and, where feasible, source alternative supply chain routes, but it's essential to understand these challenges early so contingency plans can be made.
Currently there are challenges within the potato and cocoa markets, impacting products which are normally high on the requirements for festive menus, so securing stock as early as possible is vital. Once the availability of these products becomes limited, finding any routes to market will be challenging, with associated cost implications.
With surges in demand and limited supply, prices can be volatile during the festive period. Without any prior negotiation or supplier management, costs for products can quickly escalate often resulting in a budgetary overspend and overuse of resources reviewing the market for the most cost-effective options.
By regularly conducting market analysis and monitoring key commodities, catering teams can identify trends and anticipate challenges.
This enables early negotiation with suppliers, ensuring fixed, favourable pricing for the festive period.
The effective use of technology significantly enhances efficiency and accuracy. While these benefits are evident year-round, they become even more crucial during the busy festive period, further aiding operations.
Implementing a catering controls platform can be particularly beneficial, aiding in budget management through recipe building, costings, invoice management, and stock reporting.
Inventory management can be particularly challenging during the festive season, but by using a catering controls platform, catering teams can significantly simplify stock management and have more accurate reports, optimising stock levels.
Catering control platforms provide a comprehensive audit trail from orders to invoices, ensuring complete accuracy in ordering processes. This feature allows catering leads to verify all placed orders, minimising errors and ensuring smooth operations during the frenetic festive season.
“Proper planning and preparation from a procurement perspective are essential for catering establishments to navigate the season successfully”, comments Warnes. “ By starting early, managing supplier relationships, monitoring market conditions, managing inventory, and incorporating technology, catering teams can ensure a smooth, costeffective, and successful festive period.”
Albany Products are working closely with Flavour Creations to bring their market leading and award-winning dysphagia products to the UK market.
This has started with Screamies no-melt Ice-Scream, Shape It food moulds and Powder and initial trials of their extensive pre-thickened drinks range that are available in their award-winning dysphagia cup.
Screamies won the best texture modified food award at IDDSI in 2023. They are supplied ambient and can be frozen prior to eating. Screamies have a specialised no-melt formula, resulting in shelf-stable ice-cream products that never get softer than IDDSI Level 4, making it the perfect treat for those with dysphagia.
Screamies are available in Chocolate, Strawberry and Vanilla flavours along with two added Protein variants, Chocolate and Salted Caramel. Take up in the care sector is already pleasing and products are already available through Birchall’s Food Service.

Feedback through Exemplar and other care homes is that patients love them. It has been possible for Ice-Cream Fridays to include all patients for the first time. Even staff can’t resist.
Shape It moulds offer more units per mould than others and their quality and durability is also exceptional. The Shape It moulding powder is Agar Agar based and works at all IDDSI levels, making a differ-
ence to food presentation at level 5-6 particularly.
Care homes and NHS hospitals have already started using the Shape It range. Flavour Creations pre-thickened ready to drink products are making a real difference in trials within care homes and the NHS. With hand thickening resulting in inconsistency and risk to patients, along with being time consuming and training intensive FC’s RTD products offer a solution.
The drinks have assisted in the comprehensive evaluation of patients’ needs, with more patients being provided with thickened drinks at the correct level and improved hydration. The ranges offered include nutritionally complete variants, fruit juice, cordials, dairy options with a Lactose Free dairy the latest range addition. The award-winning cup that is used for all RTD’s makes it easy for patients to use independently.
Additional fortified snacking lines are also available and can make a real difference to patients where BMI is an issue.
To find out more simply contact Albany Products at enquiries@albanyproducts.co.uk or call on 01706
632233


It’s time for an upgrade! At Diversey Washcraft, we know how frustrating it is when laundry equipment fails, especially when you’re in the middle of a busy season. Is your dryer breaking down, costing too much to run, or leaving you with laundry backlogs? Don’t let that happen this winter! Upgrade now to our cutting-edge energy-efficient Danube & LG dryers and get your laundry operations back on track. Why Choose Diversey Washcraft?
3 Save on Energy Costs: Our dryers are designed with energy-efficient technology to help your business save money while maintaining top performance. Imagine reducing your utility bills while processing more laundry - it’s a win-win!

3 No More Breakdown Worries: Say goodbye to constant repairs! With our reliable equipment, you’ll experience fewer breakdowns and disruptions. This means more uptime, fewer headaches, and smoother daily operations for your team.
3 Maximize Space: Our stackable LG 10KG and 15KG dryers allow you to fit more drying capacity in a smaller space. Perfect for businesses with limited room but high demands, you can double your drying capacity without
needing extra square footage.
3 Perfect Fit for Care & Hospitality: We understand that laundry needs in the care and hospitality sectors are high-volume and constant.
That’s why our solutions are tailored to handle even the heaviest loads, ensuring your linen, towels, and uniforms are always fresh and ready, no matter the season. The Best in Commercial Laundry Solutions At Diversey Washcraft, we’re not just about selling machines; we’re about delivering solutions that truly make a difference in your business. Our range of highperformance commercial laundry equipment is trusted by care homes, hotels, and businesses across the UK.
We pride ourselves on offering the best products backed by exceptional customer service. When you choose Diversey Washcraft, you’re not just getting top-tier laundry machines - you’re getting the support of a knowledgeable, friendly team that’s dedicated to helping you find the right solutions for your needs. We’re with you every step of the way, from consultation to installation and beyond!
For further details contact Francis Ayscough on 07714 391900 or Faye Marland at fmarland@solenis.com.'
As the economic crisis continues across the UK, care homes can find themselves facing acute pressures. The unprecedented rises in energy costs will now combine with the increase in National Insurance contributions and a higher minimum wage. This will impact staffing budgets and leave many care providers grappling with how to balance rising operational costs whilst maintaining the quality of care that their residents deserve. In this challenging financial climate, efficient budgeting and resource management have never been more critical for the sector.
Forbes Professional understands the pressures facing care homes today. Providing laundry and ware-washing appliances to care homes across the UK, we strive to be a trusted partner in helping care homes to navigate the challenges of delivering essential services. Our flexible, all-inclusive contracts enable clients to access highly energy and water efficient equipment without the burden of costly upfront payments. Our simple monthly payment structure makes it easier to budget and forecast long-term, offering peace of mind in an era of rising unpredictability.

In addition to our competitive pricing model, our award-winning service support is included at no extra cost for the life of the contract. This means no unexpected repair bills or downtime, ensuring that laundry operations run smoothly so that care operators can focus on delivering the best care to residents. With installations included as part of our service, we provide a comprehensive, hassle-free solution that saves both time and money.
As care homes plan for the future, it is essential to scrutinise contracts and operational costs, especially for high-use areas such as laundry facilities. If your current laundry contract is due to end in 2025, now is the time to consider how Forbes can help you reduce costs whilst maximising efficiency. We offer complimentary site surveys to identify your unique needs and discuss tailored solutions that support your financial and operational goals.
By aligning with reliable service partners, care homes can also take a proactive step towards managing budgets and ensuring the seamless operation of an essential service.
forbespro.co.uk | info@forbes-professional.co.uk | 0345 070 2335

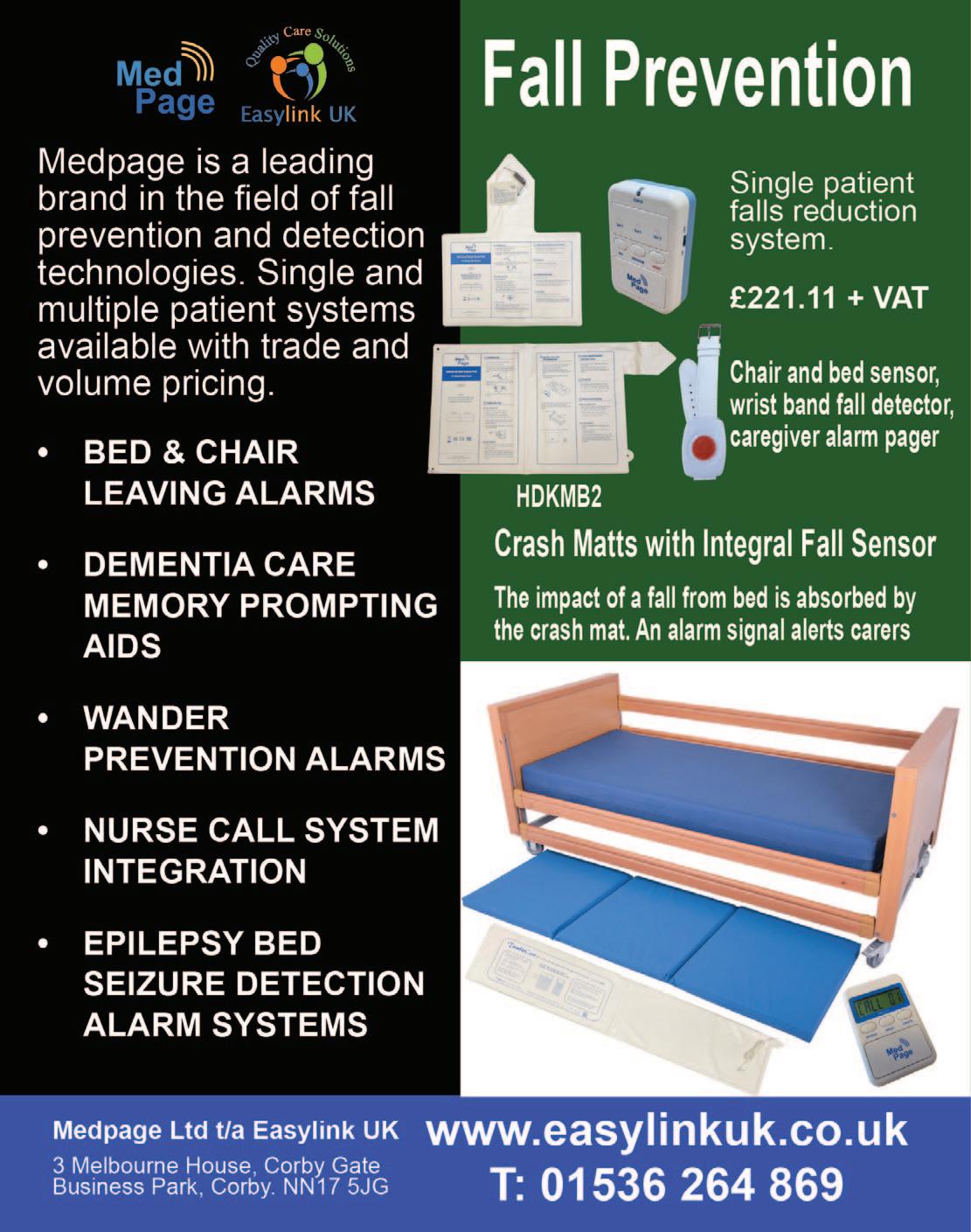
Fall Savers®, are an experienced market leading healthcare provider of resident safety solutions for over 15 years.
FALL SAVERS ® WIRELESS MONITOR

Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The NEW Fall Savers® Wireless eliminates the cord between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff Bed and chair pads available One monitor works with two sensor pads Integrates with most nurse call systems A variety of options, including: Call button Pager

FEATURES INCLUDE:

In the post pandemic world, we have all seen the effects of supply chain problems with the invasion of Ukraine and other alarming global factors, ever increasing costs of living and other more local issues which have driven up the rate of inflation over the last few years. The impact of this meant that most manufacturers of electronic products had to increase their prices as costs spiralled. This, of course, has impacted the end user. The most dramatic impact has been on the Care Industry. An industry that has lacked the support it desperately needs in these trying times.
Courtney Thorne, at the same time, took a strategic decision to take a close look at our core products, right down to component level, the objective being to make us less vulnerable to future global supply chain issues, and to reduce the cost of each product with the amin of ensuring that we deliver the same high quality product at a cost protected price. We had to ensure that this would happen without jeopardising the superb lev-

els of support we provide to our valued customer base.
This ground up review involved all departments from Research and Development right through to the Field Service team (and everything in-between). This in-depth collaboration took time as we had to ensure that each and every element was refined, perfected and tested to our (and our customers) rigorous requirements.
Whilst many organisations have limited-time or end of product line offers, we are very pleased to announce a price reduction on our core Connect and Connect Health Nurse Call system ranges. With flexible terms, full integration with Care Apps, celebrated service delivery and the most reliable and robust solution now at a new lower price, there has never been a better time to talk to us about a new nurse call system.
For more information email us at: info@c-t.co.uk or see the advert on this page.
Blaucomm’s Nurse Call Messaging Service (NMS) is the market leading solution to remove the dependency on noisy nurse call panels and pagers, through its intelligent software, which delivers the alerts straight to the care staff who need them.
Care homes are rapidly introducing smartphones for digital care planning and eMarnow, the same devices can be used to receive the nurse call alerts they need for the residents under their care.
Furthermore, Blaucomm NMS is deeply linked into Person Centred Software MCM, so call bell data is linked straight to care plans. This unlocks a huge benefit to care homes to enhance the staff performance with how they accept and respond to residents, which ultimately promotes better response times and visibility for management to audit their performance.

The best part is that Blaucomm NMS links into your existing nurse call system - we work with all major
brands such as Aidcall, ARM, Courtney Thorne, C-TEC, ENS, Intercall, Medicare, SAS and TeleAlarm.
Care operators are constantly recognising Blaucomm NMS for its reliability and dependability to their care operations, which is why we’ve been chosen time and time again over other solutions.
Head of IT Trudi Harrow at WCS Care had this to say about Blaucomm NMS:
“We find Blaucomm is a genuinely fantastic company with a reliable product.
"We would highly recommend this to anybody who wants to replace expensive pagers and silence those annoyingly loud nurse call screens!”
To find out more about Blaucomm NMS, visit
www.blaucomm.co.uk/healthcare
See the advert page 5 for more details.
Medpage Limited has collaborated with a leading UK manufacturer of crash mats to deliver a cost-effective tool for falls management strategies. The inclusion of the new TumbleCare full-length pressure mat sensor ensures that should a patient tumble out of bed, an alarm signal is generated to alert care staff to the incident, resulting in a recordable improvement to patient safety and service.
Crash mats act as a protective barrier, absorbing the impact of a fall and reducing the risk of serious injuries when a person tumbles out of bed. Beneficial for individuals who are at high risk of falling, such as older adults, patients recovering from surgery, or those with neurological conditions such as epilepsy.

Falls can pose significant risks, especially in healthcare settings and senior care facilities. Every year, thousands of people suffer injuries due to falls from beds and other furniture. To prevent these accidents and ensure the safety of patients and residents, it is essential to implement effective falls and safety management strategies.
Further details can be obtained by telephoning 01536 264 869 or emailing sales@easylinkuk.co.uk
See the advert on the facing page for details.


At Windlesham Manor, we’ve had the privilege of being the first care home in the UK to pilot Loopeli, an easy-to-use video call system designed to enhance communication for residents, families, and staff. Since introducing it, we’ve seen some unexpected changes, and I would like to share what we have learned so far.
MAKING LIFE EASIER FOR RESIDENTS AND STAFF
Loopeli is so simple to use that many of our residents can make video calls on their own, which has been a huge boost to their independence. For our care staff, this has freed up precious time on other tasks, which has been a real help.
BRINGING FAMILIES CLOSER
Families who use Loopeli have told us they appreciate it. Many feel more connected than ever, with some saying they have started to recog-
nise the person they used to know before they entered the world of care through the video calls. For residents, it has been heartwarming to see their loved ones more often—even those living abroad. Watching a resident light up while chatting with a grandchild across the world is truly priceless.
A GAME-CHANGER FOR DOCTORS’ VISITS
One of the most useful aspects of Loopeli has been during doctors’ visits and meetings with clinical professionals. Families can join via video call in real time, staying informed and involved without staff having to relay information afterward. This not only prevents misunderstandings but also helps families feel like they’re part of the process of ensuring their loved ones receives the best possible care.
INSTANT HELP FOR BEST INTEREST MEETINGS
We have also used Loopeli during best interest meetings and care discussions. When decisions need to be made, it’s easy to bring a family member into the conversation straight away. This has saved time and made these discussions more collaborative.
BREAKING DOWN LANGUAGE BARRIERS
Loopeli has helped with translation needs. If there is ever a language barrier, family members can join the call and assist, making communication smoother for everyone.
BOOSTING WELL-BEING AND REDUCING MEDICATION
One of the most surprising benefits has been how Loopeli has improved emotional well-being. For some residents, being able to connect with their family more often has reduced the need for calming PRN medication, especially during the late afternoons when anxiety levels tend to be higher.
FROM APPREHENSION TO
After over 30 years, care charity Imagine, Act and Succeed finally swapped their paper rotas and timesheets for a digitised system to help manage their 85 locations and 460+ staff.
Emma Hobbs, Payroll Officer at the charity, grew frustrated over the inaccuracies and errors of this cumbersome process – especially when it led to wages. The system was often outdated and staff frequently missed shift changes. This led to lost time, money, and patience for both managers and employees. So, how can turning to digital systems like RotaCloud improve this?
“The information is accessible to us in payroll straight away, which is an absolute godsend. Being able to see instantly where someone is working, what shift they’ve actually done, the clock-in and clock-out records are just – it’s made our payroll side so much more streamlined to what it was beforehand.”

When we first introduced Loopeli, a few staff were hesitant, thinking it might just be another tech gimmick. But it didn’t take long for them to see how much easier it made their day-to-day work. They now see it as a tool, and we have since purchased extra tablets so more residents can benefit.
SUPPORTING OUR CQC REPORTING
Loopeli has also given me confidence as a manager when completing CQC’s annual provider information return (PIR) especially question 2.7, 2.7a and 2.13 in the PIR, which involves Communication preferences and Access to Information Standard (AIS)
THE BIGGER PICTURE
At the heart of it all, Loopeli has opened new ways for our residents to stay connected to the people they love. Whether it is helping with doctor’s visits, supporting important care decisions, or simply letting a resident see their grandchild on the other side of the world, it’s a service that has made a big difference in our residents’ lives.
We’re proud to have been the first to try Loopeli, and we can confidently say it’s been a success. I would encourage any care home to consider it—it’s simple, effective, and makes a positive impact. I see many other ways Loopeli can help meet the growing demand for care, especially in home care services.
Peter Granstrom RGM Windlesham Manor.
Accuracy is the biggest benefit for Emma and her team. There’s no more chasing people for paperwork or last-minute runs for payroll. Managers can instantly access live reports, from labour costs to attendance, with clocking-in data automatically feeding to timesheets. When clocking in and out is as simple as a click or tap via mobile, web, or a terminal, employees (and Emma) can trust that all wages are correct.


Communication has also improved. By having everything at their fingertips, from shifts to requests, everyone works from the same page. It has made staff’s lives much easier and saved managers time. Enabling notifications also means any updates to the rota, annual leave requests, or available shifts are immediately sent to the appropriate staff. No more sending out WhatsApp updates, missed messages, or stress trying to find cover.
Before RotaCloud, Imagine, Act and Succeed managers sat down for two days to create rotas – before any changes were made! It now takes less than two hours to complete, and any changes are as simple as a dragand-drop on the rota, which instantly notifies staff.
They have saved time and costs this way and can even track labour costs while scheduling shifts. This saved time and money can now be better spent on service users and staff training!
All of this contributes to improving the work-life balance of all staff. Simply offering staff the ability to view rotas far in advance allows them to plan their lives accordingly. They can even input their availability into the app, from specific hours to days, meaning they feel in control of what they work and when. With the option to pick up additional shifts, too, employees have that flexibility to plan work around their lives – not the other way around.
Staff are happier when they feel in control, whether it’s transparency or trusting their wages will be correct. Managers are happier when they have more time and money to spend on more important tasks. Happy staff, happy service users.
When one digital system creates all of this… Well, you understand why so many care services are reaching for the recycling bins.
See the advert on the front cover for details or visit www.rotacloud.com/care-homes
Providing exceptional care isn't just about meeting today’s needs; it’s about offering peace of mind to


PASS supports over 1,000 care providers every day, giving them access to market leading care management tools hand in hand with unlimited 24/7/365 support from our dedicated and friendly PASS team.

Assured by NHS Transformation Directorate, PASS provides a secure platform that allows you to plan, record and evidence the care you deliver. The only assured solution built specifically for the home care sector, it provides comprehensive real-time functionality and allows you to share progress against outcomes with customisable, exportable reports.
CARE PLANNING AND ROSTERING FROM A SINGLE PLATFORM
To meet the wider needs of the PASS community All-in-one PASS
has recently been launched , bringing advanced rostering functionality to our established digital care planning platform. As a result advanced staff scheduling, payroll and invoicing functionality is now seamlessly linked with care planning and reporting, reducing the technical complexity, risk and overhead associated with integrating two separate systems.
As a result, PASS now provides an all-in-one suite of digital care management tools, available from a single platform, designed to:
Save you time
• Increase the efficiency of your teams
Improve the quality of care
• Deliver better outcomes

Our commitment to the continual evolution of PASS is further illustrated by the addition of GP Connect. The first product of its type to offer this feature, PASS is still one of only a handful of digital care management solutions to have completed this NHS Digital integration, and
is the only one offering it to the home care market.
PASS GP Connect provides authorised social care staff with realtime access to their client’s GP records. It makes medical information available when and where it is needed, leading to improvements in both care safety and outcomes:
• Visibility of allergies, vaccinations and medications, especially useful for clients unable to reliably share their personal information
Using medical information to inform care planning
Ensuring that the right medication is delivered to the right person in the timeliest manner. In one case, this allowed the administration of antibiotics on a Friday evening, aiding the service user’s swift recovery from infection
Available to all PASS users at no additional cost, PASS GP Connect is significantly more efficient than waiting for a GP response. It’s also a positive step forward on the path to the DHSC’s goal for widespread digitally enabled care and is in full alignment with their ambition for joined up care for everyone.
Get in touch: www.everylifetechnologies.com
hello@everylifetechnologies.com
Our domiciliary care sector is facing serious challenges with workforce shortages, rising costs, and an ever increasing demand for home-based care. Technology must be part of the answer, however the low adoption of smartphones and tablets by older adults has only highlighted the need for a different approach.
We believe the solution lies in the most common, and most familiar technology: the TV.
SIMPLIFYING COMMUNICATION
Many elderly individuals find smart-screen gadgets intimidating, but TVs are familiar. By delivering video calls through the TV, care providers can offer simple, accessible communication. Routine check-ins can be conducted virtually, reducing the need for some physical visits while maintaining personal connection. Family members can be more involved, offering reassurance and better support.
PROACTIVE MONITORING WITH SENSORS AND CONNECTED DEVICES
Internet of Things (IoT) devices, such as motion sensors, health monitors, and smart medication dispensers, provide real-time data on an individual’s health and environment. For instance, sensors can monitor wellbeing (e.g. sleeping patterns), or poorly regulated heating in the home. These insights allow carers to respond proactively.
BOOSTING EFFICIENCY AND PROMOTING INDEPENDENCE
Video calling reduces the need for unnecessary travel, enabling carers to focus on urgent or high-priority cases. IoT alerts further optimise resource allocation, helping providers manage workloads effectively. At the same time, this technology empowers clients to live safely and independently at home, aligning with the UK’s focus on “aging in place” and person-centred care.
HOMESIGHT IS THE WAY FORWARD
Our HomeSight system is the first to use the TV for health and wellbeing support . It’s an incredibly simple system, easily connecting to any TV with an HDMI port (which almost all TVs have), blending
seamlessly into the home. With an ergonomically designed remote control and a user-friendly TV interface, it’s intuitive enough to require almost no training. With two presses clients can connect with carers or family members effortlessly.
It ensures accessibility for all ages and technical abilities while maintaining the familiarity of using a TV.

Beyond video calls, the system keeps everyone in the loop. Family members can use dedicated phone apps to stay connected, while carers access a secure web portal for real-time updates and communication. This integration ensures that clients receive the care and connection they need without disruption to their daily routines. It’s a practical, stress-free way to enhance support and communication in domiciliary care.
For further information, see the advert on the facing page or visit www.atsolutions.uk



At AFG, our aim is simple – to help those we support live more independent lives. Technology is becoming more integral to helping people with a learning disability or with autism to be more independent. But while the technology exists today, the challenge for tomorrow is scaling its adoption across health and social care.
THE STATE OF THE MARKET: TECHNOLOGY IN SOCIAL CARE
The potential for technology to enhance lives in the care sector is evident. But many people who could benefit lack access to the tools that would make a difference to them.
According to a report by Ofcom, people with learning disabilities are less likely to own computers and smartphones or use of the internet than non-disabled people[1].
At AFG we established our Technology Lending Library two years ago. This simple idea has had a positive impact on many of the people we support. For example, borrowing a tablet device enables someone who is non-verbal to communicate with their family and friends. Another person was supported to watch videos that gave them the confidence to attend the dentist for the first time in years.
SCALING UP: MOVING BEYOND
All this is worthwhile. But for real change in social care to happen, we need to be able to scale up technology within our sector and integrate it into the way we live, work and play.
At AFG, we have partnered with assisted living technology experts, My Ecosystem to take a holistic approach that combines health, care and housing.
Led and funded by Lancashire County Council, several bungalows at our 24-hour supported living housing in Parklands Court in Lancashire have been retrofitted with bespoke, industry-first technologies, including sensors, communication devices and health monitoring tools. This set up not only supports residents, but also aids those supporting them too in delivering the right care, at the right time through real-time monitoring and adjustments.
By Andrew Kendall, Chief Commercial Officer at Alternative Futures Group
However, this is one of few examples of such integration. To make this approach accessible on a broader scale, we need to develop the right model so that the right assistive technology becomes a natural part of someone’s support.
The impact of personalised, integrated technology on both the individuals and the wider health and social care sectors can be transformative. By reducing pressure on the NHS and local authorities, this approach brings real value to users while creating efficiencies and cost savings across the sector.
So, what needs to happen to make this model work on a national level? What do we need to do as a sector to understand how we do this and how it gets funded and paid for?
Firstly, we need clear evidence of what works in what situation (depending on the person, their home and the community) and what doesn’t. What are the costs and the benefits (financial and non-financial)?
Secondly, there needs to be more education and knowledge sharing of the wide range of assistive technologies that are available for people with a learning disability and autism – this covers consumer technology, specialist standalone technology, telecare approaches and connected ecosystems. And what skills do we need to assess needs and ‘prescribe’ the right technology?
Thirdly, we need to be working together across systems and organisational boundaries to make the best use of technology. Social care, health and housing need to work around the shared goal of achieving better outcomes for people and helping them be more independent.
Fourthly, we need to build assistive technology into how support is commissioned and provided. New homes should come with a base ecosystem in place that can be added to according to the specific needs of the individual living there.
There is no doubt that technology is going to change all our lives in the future. However, as health and social care professionals we have a responsibility to those we support – in our case those with learning disabilities and mental health conditions – to ensure that they are prioritised rather than left behind in this technological evolution. By taking a thoughtful, systematic approach to technology in health and social care, we can empower those we support to live more independent, fulfilling lives.
Residents can continue to have traditional big button telephones in their rooms but with shorter contracts, free calls and no cabling.
GHM Care has launched a new resident telephone service that not only future proofs residents for the Analogue Switch Off but uses the latest in digital technology to avoid cabling and unpopular long-term contracts.
The new IP telephones from GHM Care bypass the need for a physical telephone line and instead use the internet to make and receive calls.
Residents can access rolling 30-day contracts for the first time ever, get free calls and the big button phones arrive fully configured by GHM Care.
Care homes don’t pay anything for the service and can offer the new service to residents without worrying about cabling or structural work. Homes just need to provide a power supply and WiFi connection for the phones to work.

Residents and their families are able to order handsets directly, removing any admin or maintenance for the care home.
Neil McManus, Managing Director of GHM Care says: “Traditional landlines for residents are often expensive with minimum contract lengths of twelve months. This has long been an issue for residents and their families.So, we’ve developed a solution that capitalises on the latest digital technologies to deliver a better solution for both residents and care homes.
“Residents and their families are really appreciating how easy the handsets are to set up and use, as well as the freedom of short-term contracts.
“Care homes are delighted to finally have a solution where the day-to-day handling and installation doesn’t impact their buildings or resources, and they’re able to offer an even better service to residents.”
Care homes can find out more at ghmcare.co.uk/Services/resident-telephones.
Training care home staff is vital for delivering high-quality care, especially when managing complex resident needs such as dementia, frailty, and mental health challenges. However, traditional methods often fall short in engaging staff, leaving critical gaps in understanding and preparedness. Innovative approaches, such as game-based learning and peer-to-peer collaboration, are revolutionising training, particularly in addressing the ethical and legal challenges of restrictive practices.
Restrictive practices—measures that limit an individual’s freedom—are sometimes necessary to ensure safety. However, they must be applied with great care, adhering to legal frameworks and ethical guidelines to protect residents’ dignity. A groundbreaking digital training resource, co-designed by Queen’s University Belfast and Focus Games, exemplifies this innovation. The resource uses interactive, expert-driven content to help staff navigate restrictive practices responsibly and effectively.

Game-based learning plays a central role, transforming topics like restrictive practices into engaging, real-world scenarios. Simulations allow staff to explore ethical dilemmas, practice
The delivery of safe care is the paramount responsibility of social care providers. Central to achieving this is the governance framework adopted by service providers. And at the core of this framework are policies and procedures. These enable the provider to comply – and evidence compliance – with relevant legislation and regulations, as well as facilitating best practices, supporting business needs, and assisting in recognising and managing risks.
Providers have a legal duty of care to the people they employ. Policies and procedures should provide clear guidelines to staff on how the organisation operates, as well as informing them of best practices and processes to be followed.
Policies should be reviewed annually as a minimum to ensure they are still fit for purpose and align with legal and regulatory requirements. They should be reviewed not only by employees of the business, but also by experts in various subject matters (e.g., infection control or medicines management).
For many small- to medium-sized providers, there may not be the in-house skills, knowledge, and experi-
decision-making, and test alternative solutions in a safe, low-pressure environment. This approach enhances critical thinking, teamwork, and retention of essential knowledge.
Peer-to-peer learning further strengthens the training by encouraging staff to share experiences and insights, fostering collaboration and practical problem-solving. This creates a dynamic learning environment where staff feel supported and empowered to deliver compassionate care.
By integrating these modern approaches, care homes can elevate training into a meaningful experience, equipping staff to balance safety with residents’ autonomy and dignity. At Focus Games, we are proud to offer tools designed to empower care home teams through innovative training. Visit www.FocusGames.com or email info@focusgames.com to learn more about our Restrictive Practice resource and how it can enhance care home outcomes for residents and staff alike.
For further information see the advert on the front of this issue or visit www.focusgames.com
ence to complete such a robust annual review. Many choose instead to purchase their policies and procedures from a reputable provider like W&P Compliance & Training, who will also complete reviews and ensure their policies and procedures remain up to date. This way a provider not only ensures they remain compliant; they also benefit from best practice policies and procedures that provide a solid foundation for safe working practices and – ultimately – protect and support service users and staff.

Diplomas have the potential to empower individuals and are the best route for most health and social care professionals to progress, according to an expert at leading training provider Realise.
Lesley O’Connor, Head of Health and Social Care at Realise, said diplomas are a strong option as they are flexible, can usually be fully funded and can be tailored to the particular needs of the employer and the learner.
Diplomas are also attractive to employers as they require little administration.
Lesley said: “I think there is still a lack of awareness and some misconceptions around diplomas. Sometimes people believe apprenticeships are their only option and they don’t realise diplomas are available under funded provision for those who are eligible.
“Some employers also mistakenly believe that diplomas are completed entirely online but, in fact, they are very hands-on and practical. This approach helps learners apply theoretical knowledge directly to real-world scenarios, which is a major advantage.
“Our diplomas are recognised and trusted by employers in the health and social care sector. They meet national standards, which means learners hold a qualification that is valued and trusted.
“If a candidate does not meet the eligibility criteria for a diploma, then alternative routes will need to be explored. Otherwise, I would nearly always recommend a diploma as a fantastic way to expand knowledge and skills.”
Under the Adult Skills Fund, diplomas are usually fully funded for anyone aged 19 and over, as long as they have lived in the UK for three years. There are some other eligibility requirements in devolved areas – and in some areas, workers from overseas can start a diploma as soon as they arrive in the country under a Health and Care Worker visa.
Learners can also qualify for funded diplomas if they earn below the low wage thresh-

old, which varies from area to area. The thresholds have recently been raised in various authorities, to £35,000 a year in Liverpool, for example, and £27,500 a year in West Yorkshire.
Realise offers Level 2 diplomas in all non-devolved regions for England and Liverpool City Region.
The provider also offers Level 3 diplomas in West Yorkshire, Liverpool City Region and West Midlands.
A Level 2 or 3 diploma is equivalent to achieving GCSE grades 9, 8, 7, 6, 5, or 4 previously graded A*, A, B, or C.
There are no formal maths or English tests at the end of the diploma, though development is encouraged throughout the programme.
Realise works with employers to develop diplomas that are bespoke and built around the six specialisms: Elderly Residential Care Services, Dementia Care Services, Learning Disability Care Services, Treatment and Recovery Care Services, Mental Health Care Services and Community Care Services.
Lesley said: “Tailoring our programmes is extremely valuable as it ensures the skills being developed are relevant to the role the learner holds. It helps them to develop in the areas they are most interested in which, in turn, leads to an enjoyable learning experience.
“Helping learners find the right programme for them is central to the Realise ethos. Some learners will be able to enter at Level 3 if they’re in the right job role, even if they don’t have another diploma.
“Anyone who is interested can talk to us and we will advise on the most appropriate programme.”
To find out more, visit www.realisetraining.com

Apprenticeships in the adult care sector provide a vital opportunity for professionals to advance their careers, develop leadership skills, and contribute to improving care standards. These programs, including Level 4 Lead Practitioner and Level 5 Leader in Adult Care, offer a structured pathway for care workers to step into higher-responsibility roles. By equipping individuals with the knowledge, confidence, and expertise needed to take on leadership positions, apprenticeships play a critical role in fostering both professional growth and better outcomes for service users.
These advanced apprenticeships go beyond acquiring qualifications. They enable care professionals at foundational levels to build essential skills such as critical thinking, problem-solving, and effective communication, preparing them for senior roles in the sector. This emphasis on personal and professional development
not only helps individuals achieve their career aspirations but also strengthens the workforce as a whole. The benefits extend to employers, who gain skilled and motivated teams by supporting staff through these programs. Investing in leadership development helps organisations improve retention rates and build a robust pipeline of future leaders, contributing to stability and high performance within care settings. Apprenticeships also provide clear guidance for newcomers to the sector, offering resources to help them understand career pathways and qualification requirements. This makes apprenticeships an excellent starting point for those beginning their journey in adult care, as well as a powerful tool for existing professionals seeking to advance.
By focusing on continuous learning and leadership development, apprenticeships in adult care empower individuals to unlock their potential while ensuring high standards of care across the sector. For employers and care professionals alike, these programs are a cornerstone of growth, innovation, and excellence in the industry. Find out more about our apprenticeships on www.paragonskills.co.uk

By Daniel O’Shaughnessy, Head of Programme Delivery, Digital Care Hub

You wouldn’t run a care home without a health and safety lead, and the same should apply to data security and protection leads. Losing access to critical data, even briefly, can be devastating for residents’ welfare and your business’s viability. If care plans and medication records are unavailable due to a cyber incident or software issue, residents’ wellbeing is at risk. Finance system failures can disrupt payroll, invoicing, and payments.
While data protection is everyone’s responsibility, having a named individual to lead on data security and protection is essential. This role provides senior leadership and ensures good practices are followed across the organisation. At Digital Care Hub, we use the term data security and protection lead to describe this role.
The lead should champion data security policies and set an example. While daily tasks can be delegated, the lead ensures standards are met. This role doesn’t have to fall to the Registered Manager but should be assigned to someone senior enough to oversee responsibilities effectively. In larger organisations, aspects of the role can be shared – for instance, one person might manage risks while another handles information governance.
It’s vital that leads have the right knowledge and skills. To address training gaps, Digital Care Hub’s Better Security, Better Care programme has launched a free, open-access elearning course tailored for data security and protection leads. This complements an existing course for all staff, which we recommend completing first.
The course, launched in January 2025, supports continuing professional development (CPD) and meets the training requirements of the Data Security and Protection Toolkit (DSPT). It is the only free resource designed specifically for this role in adult social care.
The training reflects real-world scenarios across care homes, supported living, home care, and community services, covering all client groups. The course includes four modules:
1. Data protection rights and responsibilities
Covers the lead’s responsibilities, other specialist roles, and key skills and
Plan out your approach. Don’t try to work things out on the day…take a look at the other article in this feature for more details.
PRIORITISE SOFTWARE UPDATES
you need to consider to protect your business.
BACK UP YOUR DATA
Backup your data, and importantly keep the backups physically away from the computer on a separate (but secure) media such as a USB key. See below about encrypting.
PASSWORDS
Set your systems to disallow weak passwords, and mandate regular changes.
Multi-factor authentication
This will secure access to your systems using your personal mobile phone or a security device. It stops attackers who have hacked any password.
CYBER SECURITY AND INCIDENT PLANS


Providers of commercial software will generally supply updates and fixes that are designed to fix security holes so they cannot be exploited. It’s vital to install these as soon as you get them.
ACCESS CONTROLS
Setting up your IT to secure access to both the systems and the data by separating who has access to what. Your IT supplier can do this if you aren’t sure.
EMPLOYEE TRAINING/PROCEDURES
Many attackers will use trickery (Phishing) to manipulate people into making mistakes and opening your systems. There are countless ways of doing this; don’t rely on your staff always recognising an attack. Strict procedures and training combat this. Look at how your finance staff do business and use fixed, written procedures to ensure they don’t fall for anyone or thing.
support needed for the role.
2. Keeping data secure
Explores managing data, understanding personal data rights, access to data, Information Asset Registers, and Data Protection Impact Assessments.
3. Threats to data security
Focuses on recognising, preparing for, and recovering from cyber incidents; reducing threats to digital systems, devices, and supply chains.
4. Data breaches
Explains how to differentiate between breaches, incidents, or near misses; record and learn from incidents; and respond to and report breaches appropriately.
By completing this course, data security and protection leads will enhance their knowledge of data protection and cyber security, ensuring they can safeguard their organisations, staff, and the people they support. For more information about the course and other resources, visit www.digitalcarehub.co.uk/elearning.
INSTALL SECURITY SOFTWARE
Having suitable security software installed is vital. By this, we mean anti-viral software and system tools to keep your systems clear. You should have:
• Email Security & Threat Protection
• Cyber Fraud and Phishing Defence
• Content Filtering DATA ENCRYPTION
Always ensure that any data stored in your IT systems is encrypted both at source and in transit. Don’t forget your backups!
SECURE YOUR MOBILE DEVICE
If you keep company data on it, using MDM software is a great plan. You can set rules and administer each device to be sure that they are compliant with security protocols. www.sescomputers.com sales@sescomputers.com +44 1305 820300



Background checks are vital to the healthcare industry, ensuring that only qualified, trustworthy, and compliant individuals are hired, directly influencing both patient safety, outcomes and the organisation’s credibility. It's important to emphasise that these requirements apply to all staff in health and social care services, including volunteers, and agency workers.
However, new statistics have revealed that 20% of healthcare candidates in the UK fail a background check, highlighting that the industry at times struggles to find candidates that are a perfect fit.
With the stakes so high, ensuring that healthcare professionals meet the highest standards of integrity and competency is more important than ever. But how can employers take proactive steps to protect vulnerable individuals from harm or exploitation, ensuring they hire only candidates with the necessary qualifications and experience?
The first step employers can take is conducting comprehensive background screenings, following regulations set by the Care Quality Commission (CQC). The way employers can ensure best practices include establishing clear vetting policies, training staff on these protocols, and regularly updating screening processes to maintain compliance. These
checks typically encompass criminal record reviews, identity verification, proof of qualifications, UK right-to-work assessments, and enhanced Disclosure and Barring Service (DBS) checks.
However, our statistics show less than one-in-ten healthcare businesses check whether a candidate is on a sanctions watchlist or identified in adverse media checks, and no organisations are running social media background checks. While CQC regulations ensure that candidates have the right skills, these additional checks are crucial preventative measures that help ensure the staff being hired are not only qualified but also the right kind of people for the role, safeguarding both patients and the safety and happiness of existing staff.
By following the strict guidelines laid out by CQC, healthcare organisations can protect their staff members and those receiving care from potential harm or exploitation. While also ensuring their brand doesn’t face any reputational risk.
In the UK, healthcare organisations most frequently verify a candidate’s criminal history (66%), references (60%), address (59%), and right to work certification (56%). These checks are essential for ensuring compliance with regulatory requirements, helping protect organisations from potential fines or legal action due to non-compliance. More importantly, maintaining high standards of care and safeguarding patient safety not only helps meet these regulatory requirements but also boosts the organisation’s credibility, fostering trust among patients, families, and the public.
Failure to comply with these guidelines can lead to reputational damage, eroding trust in the provider’s ability to deliver safe and effective care. Additionally, non-compliance with CQC requirements can result in severe
By Luke Shipley, CEO and co-founder at Zinc (www.zincwork.com)
penalties, including fines, legal action, and even the revocation of a healthcare service’s licence. This only highlights the importance of verifying candidates thoroughly – ensuring that these checks are done to the highest standard, and conducting regular rechecks on existing staff to ensure the safety, trust, and integrity of the healthcare institution is maintained.
LEVERAGING TECHNOLOGY FOR EFFECTIVE SCREENING Technology, specifically automation, plays a critical role in enhancing the speed, accuracy, and compliance of background checks, enabling healthcare providers to safeguard patient welfare more effectively. By automating and streamlining the background verification process, technology can provide a helping hand to organisations to meet the CQC standards efficiently, even in a fast-paced and evolving healthcare environment.
Automation of background checks can provide real-time data access from one unified dashboard, using this, healthcare providers can quickly identify red flags and assess candidates more accurately. Automation tools can also provide candidates with real-time updates on the status of background checks so they have visibility and aren’t left in the lurch wondering where things are at.
By utilising screening technology, businesses can offer a screening process that is efficient and easy to use for both candidates and their hiring teams. Moving at pace means businesses can reduce the wait time from offer to start date, ensuring they don’t lose candidates to competitors throughout the process and bringing forward start dates where possible. Ultimately, leveraging technology not only improves operational efficiency but also ensures that providers maintain high standards of care, protecting both patients and the organisation’s reputation for years to come.


The care sector in the UK is facing an unprecedented crisis, with an 82% drop in visa applications for health and social care roles since July 2023 according to the latest figures from the Home Office. This sharp decline is a direct result of the government’s recent policy changes, notably the ban on overseas care workers bringing family dependents. For many potential applicants, this restriction makes the UK a less attractive destination, especially for those unwilling to face prolonged separation from their families.
However, the decline in overseas care workers is not solely due to this policy. The cost-of-living crisis in the UK has further compounded the problem. Many care workers, who are often paid at the lower end of the salary scale, struggle to make ends meet on a single income. The inability to bring a second household income from a spouse or partner makes the financial realities of living in the UK even more daunting, discouraging many from applying. This situation is exacerbated by rising costs for essentials such as housing, utilities, and food, which significantly erode the disposable income of lower-wage workers.
Also contributing to the reduction in visa applications is the increased scrutiny and compliance demands placed on employers by government. Since late 2023, the Home Office has intensified its oversight of sponsorships in the care sector, resulting in lengthy processing delays and burdensome evidentiary requirements. Employers are now required to submit extensive documentation, including rotas, contracts, and staff details, often with very little notice. These demands have overwhelmed many care providers, leading to delays in hiring and, in some cases, the suspension or revocation of sponsor licences. The increased frequency of compliance visits has further strained employers, who are already struggling to maintain adequate staffing levels. Home Office visits can lead to significant disruptions in business operations, especially if they result in the suspension of a licence, which halts all further sponsorship and delays pending visa applications.
The impact of these issues on the care sector is profound. With a large number of vacancies remain-
ing unfilled, the sector is struggling to provide essential services to vulnerable people. Despite some arguments that the drop in visa applications could reflect a “natural correction” following the initial surge in demand when the sponsorship system first opened to care workers, the persistent high vacancy rates suggest that the need for overseas workers remains critical. The combination of restrictive immigration policies, economic challenges, and increased regulatory burdens has created a perfect storm, which threatens the ability of care providers to meet the growing demand for services.
To navigate these challenges, care providers must take proactive steps. Employers need to ensure they have adequate resources to manage their sponsorship and Home Office interactions and it is crucial they remain vigilant of any abuse or mismanagement of the system and workers. Engaging legal representatives to assist with visa applications, compliance visits, and licence management can help mitigate risks and ensure businesses remain in good standing with the Home Office.
Additionally, adopting robust recruitment practices and providing comprehensive support to overseas workers—such as assistance with accommodation, training, and relocation expenses—can help enhance retention and attract talent. Despite the recent increase in visa salary thresholds, care workers still benefit from discounted rates under the Immigration Salary List.
Looking to the future, while the government is planning to build a domestic workforce, such as through Labour’s Fair Pay Agreement and the launch of Skills England, these initiatives are unlikely to have immediate results. It could take years to train and recruit enough domestic workers to fill the current gaps in the care sector, so the reliance on foreign workers will likely continue. To ensure that care providers can maintain services during this transitional period, it is crucial that the visa system is adapted to better support the sector’s needs.
It is clear that the care sector in the UK is at a critical juncture. The combined pressures of restrictive immigration policies, economic challenges and regulatory burdens have led to a significant reduction in the number of overseas care workers, jeopardising the sector’s ability to meet demand. By taking proactive measures and advocating for supportive policy changes, care providers can navigate these challenges and continue to provide essential services to those in need.

bers and care home staff cannot fulfil this role. We eliminate this obstacle, providing a seamless and stress-free solution.
Our friendly and knowledgeable team guides both donors and attorneys through the entire process of applying for and registering an LPA, making it straightforward and accessible. With affordable and transparent pricing, we ensure this vital service is within reach for everyone.
We are eager to collaborate with care providers and build lasting partnerships. Our referral package is designed to add value to the care experience while supporting your residents effectively.
residents is securing a Certificate Provider, as family mem-
To learn more about how we can work together, please contact Malcolm Roberts on 01228 307360 or email malcolm.roberts@lpanow.com
Swift Management Services Limited provide expert support through a network of highly experienced healthcare professionals who have many years of working within the health and social care sector. These include nurses, care managers, Registered Managers, Operating Theatre staff, & ITU staff.
The team is able to provide holistic support packages ranging from a short term improvement project to substantial change management programmes including interim staff where required. Our innovative action plans which are tailored to your specific service requirements are interactive and are held on our secure server for ease of access. These have proven especially popular with CQC as it is easy to evidence progress and improvements through our ‘You said- we Did’ information programme.

We can deliver training sessions in person or remotely using a variety of platforms that are designed for your service.
We can support your service through a crisis or on an ongoing basis with our retained consultancy service package, providing regular one to one coaching and development, quality monitoring reviews, mock KLOE inspections, unlimited telephone and email support tailored service improvement plans and access to a dedicated care consultant to work in partnership with you to drive sustainable improvements. Swift Management Services Limited can create staff friendly bespoke policies and procedures for you as required to help you achieve compliance.
Tel: 020 8087 2072
Email: info@swiftmanagement.org.uk
Website: www.swiftmanagement.org.uk
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further. From helping clients make their first purchase through to allowing groups to grow significantly in size we

assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements. Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net



