WE SuppoRtBREASt CANCERAWARENESS MoNth
Saluting survivors and remembering those we have lost to the disease.

WE SuppoRtBREASt CANCERAWARENESS MoNth
Saluting survivors and remembering those we have lost to the disease.
- 10 signs you may have breast cancer
- Local survivor stories
- 3 ways to help someone with breast cancer

Wednesday, October 4, 2023
NOW THROUGH OCTOBER 31ST IS GOING
FIVE STAR SUBARU
Five Star Subaru is making a $5 donation to the Breast Cancer Research Foundation, for every customer that receives service on their vehicle during the month of October. For more info regarding this foundation, visit wedosubaru.com.
The World Health Organization reports that roughly 2.3 million women were diagnosed with breast cancer in 2020. By the end of that year, there were nearly eight million women alive who had been diagnosed with the disease in the previous half decade.

A breast cancer diagnosis inevitably leads to questions about the disease. The bulk of those questions undoubtedly are asked by the millions of women who are diagnosed with breast cancer. But millions more individuals, including friends and family members of recently diagnosed women, may have their own questions. Women can discuss the specifics of their diagnosis with their physicians. In the meantime, the following are some frequently asked questions and answers that can help anyone better understand this potentially deadly disease.
Cancer is a disease marked by the abnormal growth of cells that invade healthy cells in the body. Breast cancer is a form of the disease that begins in the cells of the breast. The National Breast Cancer Foundation notes that the cancer can then invade surrounding tissues or spread to other areas of the body.
The NBCF notes that exercise strengthens the immune system and women who commit to as little as three hours of physical activity per week can begin to reduce their risk for breast cancer. However, even routine exercise does not completely eliminate a woman’s risk of developing breast cancer.
The organization Susan G. Komen®, a nonprofit source of funding for the fight against breast cancer, reports that studies have shown eating fruits and vegetables may be linked to a lower risk for breast cancer, while consuming alcohol is linked to an increased risk for the disease. In addition, the NBCF reports that a high-fat diet increases breast cancer risk because fat triggers estrogen production that can fuel tumor growth.
Do you know someone who’s been diagnosed with breast cancer? Perhaps you have another reason this cause is close to your heart. In addition to helping someone you know who has the disease, you can get involved in several other ways. Here are a few.
• Become a volunteer. Offer your unique skills and interests to a support organization. You may, for example, be able to invite or welcome participants to a fundraising event, provide administrative support or head up a conference.
The NBCF reports that women who have been using birth control pills for more than five years are at an increased risk of developing breast cancer. However, the organization notes that risk is very small because modern birth control pills contain low amounts of hormones. Can breastfeeding reduce breast cancer risk?
Breastfeeding and breast cancer are linked, though the NBCF notes that the role breastfeeding plays in lowering cancer risk depends on how long a woman breastfeeds. The World Cancer Research Fund International notes that evidence indicates that the greater number of months women continue breastfeeding, the greater the protection they have against breast cancer.
The NBCF notes that researchers have found that traumatic events and losses can alter how the immune system functions, which can provide an opportunity for cancer cells to establish themselves within a person’s body. The NBCF urges women to identify ways to keep their stress levels in check.

Breast cancer education can be a valuable asset as women seek to reduce their risk for the disease.
• Support businesses that support the cause. Make your shopping dollars count by opting for products whose profits go in part to a foundation dedicated to breast cancer research or patient support.
• Promote the cause on social media. Is there a breast cancer fundraiser or awareness event happening in your area? Spread the word on Facebook, Instagram or wherever you do your online socializing.
• Make cash donations. Various organizations collect funds for breast cancer research or to help patients and their families. To support their causes, consider making monthly financial contributions.
• Organize a fundraiser. Do you want to further support the cause? Roll up your sleeves, gather a group of motivated people and plan your own fundraising event.

The number of women diagnosed with breast cancer in 2020 exceeded two million. That figure, courtesy of the World Health Organization, underscores the significance of the threat posed by the disease.
Though no one is immune to breast cancer, researchers have concluded that certain groups have a higher risk of developing the disease than others. Women who recognize their personal risk for breast cancer may not be able to change certain factors that increase their chances of developing the disease. However, recognition of their personal risk could put women in position to lower that risk in other ways. According to the WHO, the following are some groups who are at elevated risk of developing breast cancer.
• Women: Johns Hopkins Medicine reports that less than 1 percent of all breast cancer cases occur in men. Though it’s still important for men to recognize they’re not immune to the disease, women must also recognize that nearly all of the more than two million annual breast cancer diagnoses across the globe are found in women.
• Women 50 and older: The Centers for Disease Control and Prevention reports that most breast cancers are found in women who are 50 years old or older. A report from the National Cancer Institute indicates that
a 30-year-old woman has a 1 in 204 chance (0.49 percent) of being diagnosed with breast cancer, while a 40-year-old has a 1 in 65 chance (1.55 percent) of being diagnosed. By the time women reach age 60, their risk is 1 in 28 (3.54 percent), while a 70-yearold has a 1 in 24 chance (4.09 percent) of being diagnosed. Though women of any age can get the disease, the risk clearly increases as women get older.
• Women who meet the criteria for being overweight or obese: The nonprofit organization Susan G. Komen®,
which helps to raise funds for the fight against breast cancer, notes that women who are overweight or obese after menopause have a 20 to 60 percent higher risk of developing breast cancer than women who are not overweight or obese. The American Cancer Society reports that having more fat tissue increases breast cancer risk because it raises estrogen levels. However, the ACS notes the link between weight and breast cancer risk is complicated, so it’s worth it for women concerned about their cancer risk to
open a dialogue with their physicians.
• Women who consume alcohol: The MD Anderson Cancer Center reports that alcohol consumption and breast cancer risk are linked. Though the precise cause of the link is unknown, one theory suggests that consuming alcohol can increase estrogen levels as well as the levels of other hormones associated with breast cancer. However, the MDACC warns that the risk is very low, particularly for women who limit their consumption to one drink or less per day. Routinely consuming more than one alcoholic drink per day is a cause for concern.
It’s vital that women recognize their risk for breast cancer. Though any woman can be diagnosed with breast cancer, certain factors, including some that can be avoided, can increase a woman’s risk for the disease.
 By Monica Calzolari Contributing Writer
By Monica Calzolari Contributing Writer
Lisa Meschutt was 52 years old when she was first diagnosed with breast cancer after a routine mammogram. There was something suspicious on her mammogram the previous year, but after further testing, she was told it was “nothing to worry about.”
In retrospect she said, “I should have been doing self-exams because by the time the tumor was found, it was the size of a golf ball.” Her oncologist recommended shrinking the tumor on her right breast with two types of chemotherapy, plus surgery and radiation.
Being a science teacher, Meschutt wanted to understand more and learned there were many different types of breast cancer. She was told she had “the most aggressive form of breast cancer called HER2 Triple Positive,” and she would need the most aggressive form of treatment.
She decided to get a second opinion from Memorial Sloan Kettering Cancer Center in New York City, which specializes in more than 400 types of cancer. The two oncologists she consulted did not agree on her treatment plan because of her family history of heart disease.
She explained, “The type of chemotherapy they recommended can damage your heart. Chemo is essentially a poison. I needed four rounds of the strongest type of chemo followed by 12 rounds of another type of chemo every week. The chemo I was given was so strong, the nurse who administered it wore what I can only describe looked like a HAZMAT suit.”
The worst part for Meschutt was not being prepared for the side effects. No two cancers are exactly alike. Her friend had the same type of breast cancer, the same doctors and treatments, but had entirely different side effects.

Meschutt shared vivid details of her battle with breast cancer with a live audience at TEDxOneonta in 2022.
Her powerful 23-minute speech is available on YouTube. She said, “If more women cancer survivors had been willing to share more of their intimate details with me, I would have gone into every decision feeling more confident and better prepared.”
As her treatment progressed, doctors recommended a mastectomy, not a lumpectomy. She said, “my surgeon did not prepare me for what it would look like or feel like…My breasts are two different shapes and two different sizes.”
Meschutt said, “If by sharing my story I can help anyone to navigate those awful waters, then it is worth it to me … because cancer is cruel.”
Meschutt, 56, has two grown sons. One son, Alex, was a military officer being trained in special forces when she was going through her cancer treatments. Her other son, Jon, was living in New York City, and came home to support her soon after she was diagnosed.
One of the things that Meschutt is proud of doing for herself was creating a “care calendar where friends could sign up to take walks with me.” Her doctor told her that exercise helps the chemotherapy work better and would also help her fight the weight gain associated with her type of cancer. She found comfort in her volunteer work with Super Heroes Humane Society.
Meschutt calls Oneonta Middle School, where she works, “my happy place.” She added, “I wanted to be around my students as much as possible. They give me energy and make me smile. I love my job.”
Breast cancer taught Meschutt not to wait to do the things she wants to do. “Attitude is everything and I believe my positivity got me through it. But I also realize now that I may never feel healthier than I do today and will
never be younger than I am today, so I’m crossing things off my bucket list while I can,” Meschutt said. Her TedxOneonta talk can be seen at https://tinyurl.com/mva5sym5.
Breast cancer taught Lisa Meschutt not to wait to do the things she wants to do, such as go on an African Safari. |Contributed
 Lisa Meschutt shared this undated photo of herself after losing her hair to breast cancer. She volunteers for Super heroes humane Society, where she adopted her dog and exercise partner. |Contributed
Lisa Meschutt shared this undated photo of herself after losing her hair to breast cancer. She volunteers for Super heroes humane Society, where she adopted her dog and exercise partner. |Contributed
“If by sharing my story I can help anyone to navigate those awful waters, then it is worth it to me … because cancer is cruel.”
Lisa Meschutt

Breast cancer is a cause for concern for millions of women. Each year about 264,000 cases of breast cancer are diagnosed in women in the United States, according to the Centers for Disease Control and Prevention. The Canadian Cancer Society indicates around 28,600 Canadian women will be diagnosed with breast cancer this year. Globally, data from the World Health Organization indicates roughly 2.3 million women were diagnosed with breast cancer in 2020.
One of the more notable symptoms of breast cancer is the presence of a lump in the breast. Though not all lumps are malignant, it’s important that women learn about breast anatomy and lumps as part of their preventive health care routines.
Mount Sinai says that breast lumps can occur at any age in both men and women. Hormonal changes can cause breast enlargement and lumps during puberty, and boys and girls may even be born with lumps from the estrogen received from their mothers.
It is important to note that the vast majority of breast lumps are benign. The National Institutes of Health says 60 to 80 percent of all breast lumps are non-cancerous. The most common causes of breast lumps are fibroadenomas and fibrocystic changes. Fibroademomas are small, smooth, moveable, painless round lumps that usually affect women who are at an age to have children, indicates


the Merck Manual. They are non-cancerous and feel rubbery.
Fibrocystic changes are painful, lumpy breasts. This benign condition does not increase a woman’s risk for breast cancer. Symptoms often are worse right before one’s menstrual period, and then improve after the period begins.


Additional factors can contribute to the formation of lumps. Breast cysts are fluid-filled sacs that likely go away on their own or may be aspirated to relieve pain. Complex cysts may need to be removed surgically. Sometimes cysts also may form in milk ducts throughout the breasts.
Lumps also may be the result of injury. Blood can collect under the skin and form a type of lump called a hematoma. Other lumps may be traced to lipomas, which is a collection of fatty tissue or breast abscesses, which typically occur if a person is breastfeeding or has recently given birth.
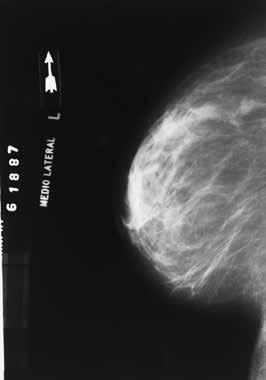
Additional causes of lumps can be discussed with a doctor. Though the majority of lumps are not a cause for concern, it is important for people to regularly feel their breasts to check for abnormalities. Doctors may recommend annual mammograms to women age 40 and older. In its earliest stages, breast cancer may produce little to no visible symptoms, but a mammogram may be able to catch something early on.

The development of breast cancer can be subtle. However, certain signs and symptoms — which may indeed be benign — should prompt you to make an appointment with your doctor immediately to be sure of where you stand. Here are 10 things to look for.
1. A painless lump in a breast
2. A change in breast size or shape


3. The appearance of dips or folds in the skin

4. Heat, redness or swelling in one breast
5. Persistent itching

6. Crusting or flaking nipple skin
7. Discharge coming from a nipple without squeezing
8. A lump in the armpit
9. An inverted, or turned-inward, nipple
10. A hardening or thickening of the breast tissue Make a habit of inspecting your breasts every month to spot any changes. Above all, remember that early diagnosis increases your chance of recovery.

A recent article in the January/ February 2023 edition of CA: A Cancer Journal for Clinicians noted that roughly 3.8 million cancer deaths have been averted since 1991. That figure represents a 33 percent overall reduction in the cancer death rate over the last three-plus decades. A host of variables have combined to make that reduction possible, and advancements in cancer treatment are one such component. Despite improvements in cancer survival rates, the disease remains a formidable foe. Women know that all too well, as various forms of the disease, including breast cancer, continue to affect millions of women each year. The World Cancer Research Fund International reports that breast cancer was the most common cancer in the world in 2020, accounting for 12.5 percent of all new cases diagnosed in that year. When diagnosed with breast cancer, women will soon begin treatment, and the following are some of the options doctors may consider as they devise treatment plans.
• Chemotherapy: The aim of chemotherapy is to destroy cancer cells or slow their growth. The National Breast Cancer Foundation® notes that chemotherapy employs
a combination of drugs, which are usually administered orally or intravenously. Chemotherapy is a systemic therapy, which means the drugs will travel in the bloodstream throughout the entire body. That’s likely why, according to the organization Cancer Research UK, nearly everyone who receives chemotherapy experiences some level of fatigue.
• Radiation: The NBCF notes that radiation therapy utilizes high-energy rays to kill cancer cells. Radiation therapy affects only those parts of the body that are treated with radiation, so it might not lead to the same level of fatigue as chemotherapy. However, cancer care teams often utilize both radiation and chemotherapy to treat cancer. When treating breast cancer, radiation therapy is often utilized to destroy any remaining mutated cells in the breast or armpit area after surgery.
• Hormone therapy: The American Cancer Society notes that some types of breast cancer are affected by hormones. In such cases, the receptors on breast cancer cells attach to hormones like estrogen and progesterone, which enables them to grow. Hormone therapy prevents such attachments. The ACS
indicates that hormone therapy is often utilized after surgery to help reduce the risk of recurrence. Unlike chemotherapy and radiation therapy, which are generally administered over a relatively short period of time, hormone therapy is usually taken in pill form for five years.
When discussing a course of treatment with breast cancer patients, doctors may also recommend newer treatments like targeted therapies.
The length of time a women will receive treatment for breast cancer will ultimately depend on a host of variables unique to each individual. According to the nonprofit organization Living Beyond Breast Cancer, an individual diagnosed with early-stage breast cancer can be in active treatment for about one year. The administration of medicine, the performance or surgery and ongoing therapies are all considered part of active treatment. The Mayo Clinic reports that chemotherapy, a treatment option that utilizes various drugs to destroy cancer cells or slow their growth, can last between three to six months for patients diagnosed with early-stage breast cancer. Treatment with chemotherapy can extend beyond six months for individuals with advanced stage breast cancer. Hormonal therapy also can extend the time breast cancer patients are in treatment, as the American Cancer Society reports that this option typically requires patients to take a pill for five years. However, hormonal therapy can extend past five years in certain instances.
The NBCF notes that these treatments, which utilize drugs designed to block the growth of breast cancer cells in specific ways, are often administered in combination with chemotherapy.
Doctors utilize various treatments to help breast cancer patients overcome their disease. Women are urged to ask as many questions as possible as they discuss treatment options with their cancer care teams.

Individuals can experience a whirlwind of emotion upon being diagnosed with cancer. No one ever expects to receive such a diagnosis, so the moment a physician delivers such news can be emotional and compromise a person’s ability to focus. Once those emotions settle down and individuals resolve to overcome the disease, they typically have a lot of questions.
One of the questions doctors will attempt to answer is which subtype of cancer a person has. For example, when doctors initially deliver a breast cancer diagnosis, they may explain that further testing will be necessary to determine precisely which type of breast cancer an individual has. Identifying the subtype of breast cancer helps doctors choose the most effective course of treatment, but it’s understandable if patients and their families become confused during the process. The following rundown can help breast cancer patients understand this crucial next step after diagnosis.
The American Cancer Society notes that breast cancer type is determined by the specific cells in the breast that become cancer. The Mayo Clinic reports that a medical team will use a tissue sam-


ple from a patient’s breast biopsy or, for patients who have already undergone surgery, the tumor to identify the cancer type.
There are many types of breast cancer, but some are more common than others. Invasive and non-invasive (also referred to as “carcinoma in situ”) are the two main subtypes of breast cancer. According to the University of Pittsburgh Medical Center, the most common types of invasive breast cancer are invasive ductal carcinoma, which affects the inner lining of the milk ducts, and invasive lobular carcinoma, which originates from the glands that produce milk.
The UPMC reports that the most common in situ types are ductal carcinoma in situ, which is cancer that remains within the milk ducts, and lobular carcinoma in situ, which does not often develop into breast cancer though it is considered a risk factor for an invasive form of the disease.
The ACS notes that triple-negative breast cancer is an aggressive form of breast cancer that accounts for roughly 15 percent of all breast cancers.
Triple-negative breast cancer can be difficult to treat.
Less common types of breast cancer, each of which account for between 1 and 3 percent of diagnoses in a given year, include Paget disease of the breast, angiosarcoma and phyllodes tumor.
A breast cancer diagnosis marks the beginning of a sometimes lengthy but often successful journey that has ended in full recovery for millions of women across the globe. More information about the various types of breast cancer can be found at cancer.org.





Millions of women across the globe are survivors of breast cancer. Those women serve as inspiration to millions more individuals, even as they bravely live with the threat of recurrence.
The Cleveland Clinic notes that most local recurrences of breast cancer occur within five years of a lumpectomy, which is a common breast cancer treatment during which cancer cells and a small margin of healthy breast tissue are removed. Even if recurrence is unlikely and/or beyond a woman’s control, the lingering notion that breast cancer return at any moment can be difficult to confront. Learning about recurrence could calm the nerves of breast cancer survivors and their families.
A second diagnosis of breast cancer does not necessarily mean women are experiencing a recurrence. The Cleveland Clinic notes that breast cancer that develops in the opposite breast that was not treated and does not appear anywhere else in the body is not the same thing as recurrence. Recurrence occurs when the cancer is detected in the same breast in which the disease was initially detected. Breastcancer.org notes that cancer found in the opposite breast is likely not a recurrence.

Treatment for breast cancer is often very successful, particularly in patients whose cancer was discovered early. Recurrence can happen when single cancer cells or groups of cancer cells are left behind
after surgery. Breastcancer.org notes that tests for cancer cannot detect if single cancer cells or small groups of cells are still present after surgery, and a single cell that survives post-surgery rounds of radiation therapy and chemotherapy can multiply and ultimately become a tumor.

There are different types of breast cancer recurrence, including:
• Local recurrence: The Cleveland Clinic notes that a local recurrence diagnosis indicates the cancer has returned to the same breast or chest area as the original tumor.


• Regional recurrence: A regional recurrence means the cancer has come back near the original tumor, in lymph nodes in the armpit or collarbone area.
• Distant recurrence: A distant recurrence indicates the breast cancer has spread away from the original tumor. The Cleveland Clinic notes this is often referred to as stage 4 breast cancer. This diagnosis indicates the tumor has spread to the lungs, bones, brain, or other parts of the body.
The risk of recurrence

Johns Hopkins Medicine notes that certain variables unique to each individual affect the risk of breast cancer recurrence. This is an important distinction, as women who have survived breast cancer but are concerned about recurrence should know that they will not necessarily experience one, even if a first-degree relative or friend did. The type
of cancer and its stage at diagnosis can elevate risk, which also is highest during the first few years after treatment.
The Cleveland Clinic notes that women who develop breast cancer before age 35, which is uncommon, are more likely to experience a recurrence. In addition, women diagnosed with later stage breast cancers or rare forms of the disease, including inflammatory breast cancer, are more likely, though not guaranteed, to experience a recurrence.
The fear of breast cancer recurrence can be tough for survivors of the disease to confront. Sharing concerns with family members and a cancer care team could help survivors overcome their fears.

“Iam planning to be around another 30 years,” said Lynne Bolstad, 67, who is currently in treatment for breast cancer. “My mother had five types of cancer and she lived to be 87.”
Bolstad encountered hundreds of patients with cancer, including breast cancer, when she worked as a physician assistant at the Cancer Center at FoxCare with her medical oncologist husband, Dr. Yoshiro Matsuo, now retired.
Educating patients about their disease and their treatment plans, including chemotherapy and radiation therapy and their side effects, was a big part of her career in oncology, she said. She continued to focus on patient education in addition to diagnosis and treatment in her last 10 years working as a PA and hospitalist.
“One in eight women get breast cancer,” said Bolstad. “It’s frightening. It’s confusing. It is very overwhelming. I am lucky that I can navigate my way through it.”
She explained, “Premenopausal tumors tend to be more aggressive. Postmenopausal tumors tend to be less aggressive. I have one of the most common types of breast cancer: hormone receptor positive, HER2 negative. It is one of the most favorable combinations. Based on this and other analysis of my tumor, chemo was not recommended for me.”
Twenty years ago, Bolstad had an abnormal mammogram, so she had a lumpectomy, she said.
No cancer was found. Twenty years later at the site of her scar on her right breast, she felt something suspicious and requested a mammogram several months before she was scheduled to receive her routine screening.
This time, Bolstad tested positive for cancer. “I had a lumpectomy and sentinel node biopsy. My tumor was 2.5 centimeters and two out of five of my lymph nodes which were removed were cancerous. If you have a lumpectomy, radiation is advised to kill any remaining cancer cells.”
Bolstad is receiving 30 radiation treatments at FoxCare Cancer Center, Monday through Friday. She said, “Radiation itself is painless. Over the next few weeks, I will have some damage to my skin, like a bad sunburn, and some progressive fatigue. Over time, these will improve. There are other possible, less common side effects, and there will probably be some long-term skin and tissue texture changes. Radiation damages healthy cells, but it is a lot more toxic to cancerous cells.”
After her radiation therapy is done, Bolstad said, will take medication to minimize estrogen activity in her body. She stressed how much medicine has advanced in the past 20 to 30 years and that is one of the reasons the long-term survival rate from breast cancer has increased.


“Because we can analyze tumors, we can look at the characteristics of your tumor and target our therapies to
treat your tumor,” she said. “If your grandmother or mother had breast cancer many years ago and had a radical mastectomy, your treatment options will be very different today compared to then.”
Bolstad described herself as “painfully shy in high school and college.” A summer job working in a hospital laboratory in Hudson changed her career trajectory. She found she was bored with lab work. When she was taught how to do EKGs and draw blood, she discovered that she liked working with patients and answering their questions, she said.
After completing a bachelor’s degree in biology and engineering at Union College, Bolstad entered the seventh class of the Physician Associate Program at Yale University, graduated as a PA in 1979, and came to work in Oneonta.
Bolstad encourages patients to “always ask questions and be proactive in screening and any treatment programs being planned” saying, “You are the boss.” Also, “Attitude is important. Be positive, let friends and family support you, and keep moving forward.”
“You are the boss.”
“One in eight women get breast cancer. It’s frightening. It’s confusing. It is very overwhelming. I am lucky that I can navigate my way through it.”
Lynne BolstadLynne Bolstad, a retired physician assistant, is shown in September 2023 on her back porch in Davenport. |MoniCA CALZoLAri
A breast cancer diagnosis affects every facet of a woman’s life. While women and their families must prioritize treatment, a host of additional variables, including work, also merit consideration after a breast cancer diagnosis.
Work is an important part of life, so it’s understandable if women are concerned about how a breast cancer diagnosis will affect their careers. With that in mind, women can consider these tips as they share news of their diagnosis with their employers.
• Prioritize your own comfort when speaking to an employer about your diagnosis. Breastcancer.org notes that a woman’s comfort level is the most important factor when sharing news of a breast cancer diagnosis with an employer. Some women may want to inform only a few coworkers they’re close with, while others may find it easier to let everyone know. There’s no wrong or right way to share a diagnosis, so women should prioritize their own comfort when choosing which way
to go. To ensure things go smoothly and your wishes are honored, consider first breaking the news to a supervisor in a private face-to-face meeting or Zoom call.

• Decide what you want to share. The Australia-based Cancer Council notes that individuals must decide what they want to share regarding their diagnosis. Women can speak to their physicians to determine how long they will continue working, if their ability to work full-time will be affected by treatment and the projected length of treatment. Answers to the these questions can help women decide how much to share with their employers. If treatment will be lengthy and require time off to recover, then sharing such information can help employers arrange to cover your responsibilities.
• Take additional measures to overcome side effects of treatment. Breastcancer.org notes that treatment can produce cognitive side effects such as memory loss or difficulty concentrating. Success-


ful professionals will undoubtedly want to maintain the standard they have established for themselves, and that can be done by taking a few simple steps to overcome any cognitive issues that may arise during treatment. Record Zoom calls so you can go back and view them, if necessary. Take copious notes during strategizing sessions. Begin using a planner so you can stay on top of deadlines. These simple measures are easy to employ and can ensure women don’t miss a beat during treatment.
• Take time off, if necessary. Time off should always be a consideration during cancer treatment. Breastcancer.org notes that various programs can help women meet their financial obligations if they’re no longer earning income. Some employers may pay full salaries during treatment and not count time off as vacation or personal time, while others may grant short-term disability benefits that can provide some income during extended time off. Explore all of your options with
A breast cancer diagnosis may require women to alter their work habits and schedules. Even the simplest tweaks can have a profound impact and allow women to direct much of their energy and focus on their treatment.

Cancer is a formidable disease that the World Health Organization reports is the leading cause of death worldwide. Figures vary, but organizations such as the WHO and the American Cancer Society estimate that around 9.5 million people die from cancer every year.
No type of cancer causes more deaths in women across the globe than breast cancer. Though the fiveyear survival rate for breast cancer patients has increased by a significant margin in recent decades, a 2019 study published in The Asian Pacific Journal of Cancer Prevention reported a significant increase in breast cancer mortality rate in the 25-year period preceding the study. The researchers behind the study theorized that the spike in mortality rate could be due to an increase in incidence and prevalence of breast cancer.
Like all cancers, breast cancer cannot be prevented. However, various healthy habits could help women reduce their risk for the disease.

• Avoid alcohol. The ACS reports that alcohol consumption is a clear risk factor for breast cancer. Risk increases with the amount of alcohol a woman consumes. For example, a woman who consumes one alcoholic drink per day has a 7 to 10 percent higher risk of getting breast cancer than a woman who abstains from alcohol. Drinking two to three drinks per day could increase risk by around 20 percent.
• Establish and maintain a healthy weight. Being overweight or obese increases breast cancer risk, particularly among postmenopausal women. According to the ACS, after menopause women get most of



their estrogen from fat tissue. Fat tissue increases estrogen levels in the body, which in turn increases a woman’s risk for breast cancer. Elevated levels of insulin in the body, which is common among individuals who are overweight, also has been linked to higher breast cancer risk. Establishing and maintaining a healthy weight cannot prevent breast cancer, but it can help women reduce their risk for the disease.
• Maintain a physically active lifestyle. A sedentary lifestyle increases a person’s risk for various conditions and diseases. Women who live such a lifestyle are at elevated risk for breast cancer. The ACS notes that sedentary behavior such as sitting, lying down, watching television, or engaging with screen-based forms of entertainment that do not require physical activity can increase breast cancer risk, especially for women who spend most of their work day sitting down. A more physically active lifestyle that includes routine exercise can help women reduce their breast cancer risk.
• Adopt a nutritious diet. Eating right is another way for women to reduce their breast cancer risk. Vegetables, fiber-rich legumes such as beans and peas, fruits across the color spectrum, and whole grains are some components of a healthy, nutrient-rich diet that can help lower breast cancer risk. Women also can avoid certain foods, such as red and processed meats and refined grains, to lower their breast cancer risk.
Though there’s no guaranteed way to prevent breast cancer, women can embrace various healthy habits to lower their risk for the disease.
Family history is considered a risk factor for various diseases, and breast cancer is no exception. According to Cancer Research UK, having a first degree relative, which includes a mother, sister or daughter, diagnosed with breast cancer approximately doubles a woman’s risk for breast cancer. However, the American Cancer Society notes that only about 5 to 10 percent of breast cancer cases are thought to be hereditary. Hereditary cases of breast cancer are those that result directly from gene mutations passed on from a parent. The relatively small percentage of hereditary cases is important to note, as it means that the vast majority of women who are diagnosed with the disease have no family history of breast cancer.


A host of variables affect a woman’s risk for breast cancer. Some variables are related to a woman’s lifestyle. For example, the American Cancer Society reports that a sedentary lifestyle can increase breast cancer risk. In addition, the ACS notes that women who consume unhealthy diets are at greater risk of becoming overweight or obese, which also increases breast cancer risk.
A woman’s lifestyle is largely up to her, which means women can exert a measure of control over their risk for a disease that the World Cancer Research Fund International reports was the world’s most commonly diagnosed cancer in 2020. However, additional variables beyond a woman’s control, including breast density, can increase risk for breast cancer.

The Centers for Disease Control and Prevention notes that breast density reflects the amount of fibrous and glandular tissue in a woman’s breasts compared to the amount of fatty tissue in the breasts.
How do I know if I have dense breasts?
Women cannot self-diagnose dense breasts. The National Cancer Institute notes that only a radiologist can determine if a woman has dense breasts, and that’s only possible after a mammogram.
Breast density and breast cancer are linked, which underscores how important it can be for women to discuss breast density with their physicians. The National Cancer

Institute notes that dense breasts are not considered an abnormal breast condition or a disease, though they are a risk factor for breast cancer. Women determined to have dense breasts have a higher risk of breast cancer than women with fatty breasts.
The CDC notes that dense tissue can hide cancers, as the fibrous and glandular tissue in breasts, which is more abundant in dense breasts than fatty breasts, looks white on a mammogram. That’s significant, as tumors also look white on mammograms, which means it’s easy to mistake a small tumor for fibrous and glandular tissue.
What can I do if I have dense breasts?


It’s important that women with dense breasts open a dialogue with their physicians. This is especially important when switching physicians, as a new doctor can consider this when treating a patient for the first time. Doctors may recommend certain tests to women with dense breasts, particularly after considering a woman’s age and family history of breast cancer. The CDC notes that additional testing can produce a false positive result, so women can discuss that likelihood as well. But in some cases, a breast ultrasound or a breast MRI may detect a tumor that a mammogram did not find, so additional testing should not be written off.
Breast density and breast cancer are linked, but the NCI notes that research has indicated that women with dense breasts are no more likely to die from breast cancer than women with fatty breasts. More information about breast density can be found at cancer.gov.





Has a friend or family member of yours been diagnosed with breast cancer? As a loved one, you can support their physical and psychological well-being in several ways. Here are three tips.

If you don’t live with the person, ask questions to get ideas for how you can help. They may like company for a chemotherapy appointment, or you may be able to do a grocery run, provide childcare or clean a bathroom. There are so many ways to make their daily life a little easier. That said, if your loved one prefers to handle things alone, respect their decision and resist the urge to insist on helping.
It’s quite often enough just to be present for your loved one. Remind them that you’re available to help or simply spend time together, reading a book or listening to music. If you feel unsure how to react or worry your actions will be awkward, say so. Your honesty is the key to a trusting relationship.
1 2 3
Breast cancer is a tough ordeal. When you’re with your loved one, it’s a healthy practice to talk about subjects that have nothing to do with their illness. For example, if they feel up to it, you could invite them to do something special like go to the movies. Don’t be afraid to share the latest gossip from your friend group or ask for their famous spaghetti sauce recipe.
Ultimately, the most important way to help your loved one through their breast cancer journey is to make them feel your love. A listening ear, a word of encouragement, a smile and a hug are all free, and they can do a world of good.

Breast cancer affects millions of women each year, but breast cancer also can be diagnosed in men. Each year in the United States, about 2,400 cases of breast cancer are diagnosed in men, according to the Centers for Disease Control and Prevention. Roughly 270 men will be diagnosed with breast cancer this year in Canada, according to the Canadian Cancer Society. Macmillan Cancer Support says men have a small amount of breast tissue behind their nipples, where breast cancer potentially can develop. Breast tissue in boys and girls is the same until puberty, when girls start to develop more. Signs of male breast cancer include a lump or swelling in the breast, redness or flaky skin in the breast, irritation or dimpling of the skin around the nipple, nipple discharge, or pulling in or pain of the nipple, states the CDC.






Breast cancer treatments are highly effective, which is one reason why the National Cancer Institute can report that the five-year survival rate for non-metastatic breast cancer is 90 percent. However, in certain situations, doctors may feel that the existing standard for breast cancer treatment may not be enough to help women overcome their disease. In such instances, doctors may discuss clinical trials with women battling breast cancer. The American Cancer Society defines clinical trials as research studies in which people volunteer to help doctors find ways to prevent or treat disease. The National Breast Cancer Foundation, Inc.® points out that all current standards of treatment began as clinical trials. However, that does not mean women diagnosed with breast cancer should automatically sign up to participate in clinical trials. There are pros and cons to participating in clinical trials, and breast cancer patients can speak with their medical teams about the advantages and disadvantages of each trial they’re considering. One myth worth dispelling is that clinical trials are only an option for people who have been diagnosed with advanced stage cancer. In fact, the NCI notes that clinical trials are available for all stages of cancer. A database of NCI-supported clinical trials can be found at https://www.cancer.gov/about-cancer/ treatment/clinical-trials/search.



No woman wants to be diagnosed with breast cancer. A potentially fatal disease, breast cancer affects millions of women across the globe each year. Thankfully, survival rates for the disease have improved considerably in recent decades, and women now have a much greater chance of living for many years after successful treatment.
A 2017 study from the American Cancer Society found that the number of women who died from breast cancer dropped by about 40 percent in the quarter century preceding the study. A host of variables, including advancements in detecting and treating the disease and a heightened awareness of the need for screening, have contributed to that positive turn.


Though breast cancer treatment is highly effective, particularly when the disease is in its early stages at the time of an initial diagnosis, women may still experience some side effects of both the disease and the treatment their cancer care teams design. The following are some ways that breast cancer and treatment can affect a woman’s body in both the short- and longterm.
• Joint and muscle pain: According to Susan G. Komen®, a nonprofit organization that helps to fund breast cancer research, aromatase inhibitors are hormone therapy drugs used to treat hormone receptor-positive breast cancer. Researchers have found that joint pain and muscle pain are common side effects of aromatase inhibitors. This pain might be most noticeable after sleeping or a period of inactivity. Fortunately, the damage to joints and muscles is not permanent.
• Fatigue: Breastcancer.org reports that breast cancer causes changes in the body that can







lead to fatigue. That fatigue could be linked to cytokines, which are proteins released by certain breast cancers that researchers suspect cause fatigue. Breast cancer also can alter hormone levels in the body and cause inflammation, and each of those effects can contribute to fatigue.


• Skin changes: The MD AndersonCancer Center reports that certain changes to the skin are hallmarks of inflammatory breast cancer, a relatively rare yet aggressive form of the disease. Redness or another change in the skin color of the breast, swelling on one side and/or a rash that appears suddenly are changes in the skin that can appear due to breast cancer. Dimpling of the skin over the breast is another change in the skin that can result from breast cancer.
• Libido and fertility: Breastcancer.org reports that some breast cancer treatments can lower a woman’s libido, which is her desire for sex and intimacy. This side effect is possibly a byproduct of other effects of treatment that can affect a woman’s mental state, including anxiety, depression, weight changes, fatigue, and difficulty sleeping. In
addition, the National Cancer Institute notes that certain types of chemotherapy can cause infertility. Though the Centers for Disease Control and Prevention reports that most cases of breast cancer are diagnosed in women over 50, women can still get the disease at any age. Women who hope to have children after a breast cancer diagnosis are urged to discuss that goal with their cancer care teams so their course of treatment does not adversely affect their ability to give birth.
Breast cancer affects a woman’s body in various ways. Though many effects are temporary, women can still discuss strategies to overcome them as they navigate their way through treatment.
There’s never a good time to receive a breast cancer diagnosis. Such news often changes the lives of patients and their families. Though survival rates for breast cancer have improved dramatically in recent years, a diagnosis is still cause for concern. And that concern only grows when the woman who is diagnosed also happens to be pregnant.
The National Cancer Institute notes that breast cancer during pregnancy is rare. NCI data indicates breast cancer occurs in about one in every 3,000 pregnancies. However, the rarity of such diagnoses does not make them any easier to confront. Knowledge can be vital as women and their families navigate a breast cancer diagnosis during pregnancy.
The American Cancer Society reports that women can safely be treated for breast cancer during pregnancy.
However, treatment for pregnant women will likely differ from treatment for women who are not expecting. The ACS notes that the types of treatment available to pregnant women and the timing of the treatment might be affected by the pregnancy. Various factors will affect which course of treatment doctors decide to pursue when a patient is pregnant. The National Breast Cancer Foundation indicates such factors include:
• Tumor size

• Tumor location
• Which term of the pregnancy a woman is in

The ACS adds that whether or not the tumor has spread, and how far it has spread, are additional factors doctors will consider when determining a course treatment for pregnant women diagnosed with breast cancer. A woman’s overall health and personal preferences also will be con-


sidered prior to beginning treatment.
The NBCF reports that doctors will consider popular treatments like chemotherapy, radiation and hormone therapy when treating breast cancer patients who are pregnant. However, the decision to administer such treatments to pregnant women is not as straightforward as it might be when planning a course of treatment for women who are not expecting. For example, though chemotherapy can be safely administered to pregnant women, there are specific windows of time to deliver chemotherapy without harming the baby.
Radiation is considered unsafe for an unborn child, so while it’s something doctors will consider or even recommend when designing a treatment plan for pregnant women, the NBCF notes it is always administered after the child is born. The same typi-





cally goes for hormone therapy, as the NBCF reports that the effects of hormone therapy on unborn children are still not entirely understood.
Many new mothers aspire to breastfeed their newborns, but the ACS reports that doctors recommend women who are about to receive breast cancer treatment cease or not start breastfeeding. Drugs used during chemotherapy, hormone therapy and target-
ed therapy can enter breast milk and be passed on to the baby.
A breast cancer diagnosis during pregnancy is rare, but the ACS reports that most studies have found that outcomes among pregnant and non-pregnant women with breast cancer are roughly the same for cancers found at the same stage. Such studies can provide hope to women and their families as they embark on their treatment journeys.
 By Monica Calzolari Contributing Writer
By Monica Calzolari Contributing Writer
the hardest part about having breast cancer was not knowing (the outcome),” said Malissa Kano-White of Oneonta. “My daughter was only nine years old at the time. The physical part wasn’t hard. The emotional part of maybe not seeing her grow up was the hardest.”

Kano-White was 49 when she felt a lump in her breast in December 2008. She admits, “I was a little cavalier about it because I had a lump in my other breast some years earlier, had a biopsy and it was benign. Plus, we just moved here and my dad was dying.”
Kano-White and her family moved to Oneonta from Kentucky in 2008. She accepted a job teaching theatre arts and directing the theatre at Hartwick College. Her last mammogram that same year gave no indication of a problem. Breast cancer does not run in her family.
She finally went to see her primary care physician in May and had further testing. She was back in Kentucky for the summer when she received the call that she had breast cancer.
She remembers, “It was so scary to get that call from my doctor.”
“My daughter was only nine years old at the time. The physical part wasn’t
More tests revealed that Kano-White had Triple-Negative Breast Cancer (TNBC). Her doctor told her this type of breast cancer is “very aggressive.” Only about 15% of breast cancers are of the TNBC type, which occur more frequently in younger and premenopausal women, according to Reimagining Women’s Cancers by Dr. Michele Berman, Dr. Mark Boguski and David Tabatsky.
Kano-White had surgery, followed by chemotherapy and radiation. She elected to have a mastectomy in August 2009. Because she had put off treatment for eight months, Kano-White said, “I just wanted it out.”
A patient’s reaction to cancer treatment is unpredictable. Kano-White said, “I heard that the first round of chemotherapy is supposed to knock you out. I was tired, but I was fine. I had an allergic reaction to the next round of chemotherapy. My fingers swelled up and were the size of sausages.”
Malissa Kano-WhiteHealth insurance rules made it difficult for her to switch medications. Kano-White said, “I will be eternally grateful to Lynne Bolstad at FoxCare Cancer Center. She was amazing. She stood up for me and advocated for me when I was at my most vulnerable.” That allowed her to switch to another chemotherapy drug and get past insurance company roadblocks.
Kano-White said, “I was really lucky” – referring to having good health insurance and a low deductible. She was surprised that “radiation is considered an office visit and I had to pay a $50 co-pay each time I had radiation.” It is not uncommon for breast cancer patients to receive 30 rounds of radiation.
“I often think what a horrible position some patients are in who have high deductibles and poor coverage,” she said.
Kano-White has advice for readers. She said, “If you are at risk, if cancer runs in your family, do not delay seeking treatment. I feel like I dodged a bullet. Now I say to my daughter ‘I love you’ every day.”
Kano-White has been cancer-free for 14 years. She gets regular check-ups. She said, “I could not have done it without the support of a group of women in my neighborhood. They scooped up my nine-year- old daughter and welcomed her into their world, nurtured her and even took her trick or treating.”
Malissa Kano-White, a breast cancer survivor, is a professor of theatre arts and director of theatre at hartwick College. |MoniCA CALZoLAri“I feel like I dodged a bullet .”
hard. The emotional part of maybe not seeing her grow up was the hardest.”
Many side effects of breast cancer treatment, such as fatigue, go away shortly after treatment ends. However, the organization Susan G. Komen® notes that some women experience late effects of cancer treatment, which are new side effects that present months or even years after treatment for breast cancer has ended. Late effects vary, and many breast cancer survivors experience no such symptoms. But according to Macmillan Cancer Support, a United Kingdom-based organization devoted to supporting individuals living with cancer, some late effects may be permanent.
There’s no way of knowing who will experience late effects of breast cancer treatment. However, a 2019 study published in the Journal of Midwifery & Women’s Health indicated that as much as 90 percent of breast cancer survivors experience long-term consequences as a result of treatment. Susan G. Komen notes that some of the more common late effects of breast cancer treatment include:
• Bone health problems
• Changes in the look and feel of the




breast, including after lumpectomy, radiation therapy and/or reconstruction
• Early menopause or menopausal symptoms, such as hot flashes
• Emotional distress and depression
• Fatigue or insomnia
• Fear of recurrence
• Infertility
• Joint and muscle pain

• Sexuality and intimacy issues

• Weight gain
Susan G. Komen notes that research into breast cancer care, including how to improve life for survivors, is ongoing. In the meantime, women undergoing treatment, those who have recently completed treatment or even patients who have not received treatment in years but are experiencing the aforementioned side effects are urged to speak with their physicians about the various ways to improve quality of life should any of these symptoms appear or continue to present. More information about late effects of breast cancer treatment is available at komen.org.
Breast cancer treatment can include tumor removal through lumpectomy or removal of affected breast tissue through mastectomy. The loss of one or both breasts, whether whole or in part, can be difficult for many women to accept.
Some women choose to live with a flat or asymmetrical chest, with the option of wearing external breast prostheses. Others opt for breast reconstruction. The choice is personal and unique to every patient. Here’s an overview of what breast reconstruction entails.
There are three main types of breast reconstruction:
1. Breast implants. The implant procedure involves inserting a silicone bag containing a sterile saline solution or silicone gel under the chest muscles.
2. Autologous breast reconstruction. Sometimes called “flap” reconstruction, this procedure involves grafting muscle and fat tissue from other parts of the body onto the breast. This approach provides a more natural result.
3. Nipple and areola reconstruction. This surgery is considered the finishing touch of breast reconstruction. It’s typically done three to six months after the initial operation.
The techniques differ according to the patient’s unique needs and physical characteristics. The breast reconstruction process may require multiple surgeries to complete. To learn more, visit cancer.org.

