RIGHTS More protection for union delegates
page 19

Action follows Ramsay’s low offer page 20

RIGHTS More protection for union delegates
page 19

Action follows Ramsay’s low offer page 20
Aware Super is here to help NSWNMA Members get retirement ready, whether retirement is 2 or 20 years away.
Get started with My Retirement Planner™ – it’s free and available to everyone. More than just a calculator, it can help answer questions like how much super do you need for retirement? Are you on track to save this in time? And what changes could you make now to help grow your savings?
Providing a step-by-step action plan – at no extra cost.
With super advice and super returns Aware Super is super helpful.

NSW Nurses and Midwives’ Association
For all membership enquiries and assistance, including The Lamp subscriptions and change of address, contact our Sydney office.
Sydney Office
50 O’Dea Avenue, Waterloo NSW 2017 (all correspondence)
T 8595 1234 (metro) 1300 367 962 (non-metro)
F 9662 1414 E gensec@nswnma.asn.au W www.nswnma.asn.au
Hunter Office
8–14 Telford Street, Newcastle East NSW 2300
NSWNMA Communications Manager
Gia Hayne
T 02 8595 1234 (metro) T 1300 367 962 (regional)
For all editorial enquiries, letters and diary dates
T 8595 1234 E lamp@nswnma.asn.au
50 O’Dea Avenue, Waterloo NSW 2017
Produced by
Hester Communications T 0414 550 376
Press Releases
Send your press releases to: F 9662 1414 E gensec@nswnma.asn.au
Editorial Committee
Shaye Candish, NSWNMA General Secretary
Michael Whaites, NSWNMA Assistant General Secretary O’Bray Smith, NSWNMA President
Michelle Cashman, Long Jetty Continuing Care
Richard Noort, Justice Health
Liz McCall, Byron Central Hospital
Diane Lang, South East Regional Hospital, Bega Valley
Karen Hart, Wagga Wagga Base Hospital
Printed by
Printed by IVE Group Sydney
Advertising
Danielle Nicholson T 8595 2139 or 0429 269 750 F 9662 1414 E dnicholson@nswnma.asn.au
Information & Records Management Centre
To find archived articles from The Lamp, or to borrow from the NSWNMA nursing and health collection, contact: Adrian Hayward, Coordinator. T 8595 2175 E gensec@nswnma.asn.au
The Lamp ISSN: 0047-3936
General Disclaimer
The Lamp is the official magazine of the NSWNMA. Views expressed in articles are contributors’ own and not necessarily those of the NSWNMA. Statements of fact are believed to be true, but no legal responsibility is accepted for them. All material appearing in The Lamp is covered by copyright and may not be reproduced without prior written permission. The NSWNMA takes no responsibility for the advertising appearing herein and it does not necessarily endorse any products advertised.
Authorised by S. Candish, General Secretary, NSW Nurses and Midwives’ Association, 50 O’Dea Avenue Waterloo NSW 2017
Privacy Statement
The NSWNMA collects personal information from members in order to perform our role of representing their industrial and professional interests. We place great emphasis on maintaining and enhancing the privacy and security of your personal information. Personal information is protected under law and can only be released to someone else where the law requires or where you give permission. If you have concerns about your personal information, please contact the NSWNMA office. If you are still not satisfied that your privacy is being maintained, you can contact the Privacy Commission.
Subscriptions for 2024
Free to all Association members. Professional members can subscribe to the magazine at a reduced rate of $30. Individuals $84, Institutions $140, Overseas $150


Public sector nurses and midwives held more than
statewide in late July in support of our
12 PAY CAMPAIGN
Strong start to Belmont’s pay campaign Branch teamwork brings encouraging response to union pledge drive.
19
WORKPLACE RIGHTS
More protection for union delegates Union delegates have new and important rights and protections that recognise their critically important work and the tremendous barriers they can face in the workplace.
20
PRIVATE HOSPITALS
Industrial action follows Ramsay’s low offer
NSWNMA members at Ramsay Health Care have taken protected industrial action for the first time.
PRIVATISATION
22
Hawkesbury campaign rescues leave entitlements
NSWNMA members take action to defend annual leave, long service leave and sick leave, as the hospital returns to public hands.





Recruit a new member and you could win a 4-night wellness retreat at Billabong Retreat. You and a friend will stay in a Treehouse Ensuite Cabin with the following inclusions:
All meals, drinks and snacks
Daily yoga and meditation
Access to retreat program during stay
Two x spa treatments per person (per stay)
One x infrared sauna session per person.
Every member you sign up over the year gives you an entry in the draw! Award winning Billabong Retreat was founded and opened in 2010. The 26 room eco retreat is located on 12 acres of natural bushland in Maraylya, just 45 minutes from the Sydney CBD. The wellness haven delivers day retreats as well as overnight retreats that include delicious wholefoods, daily yoga, evening meditation and education workshops to empower and inspire. For more information visit billabongretreat.com.au
NOTE: Join online at www.nswnma.asn.au
If you refer a member to join online, make sure you ask them to put your name and workplace on the online application form, so you will be entered in the draw.

GENERAL SECRETARY
After the devastation of COVID-19 and the suppression of pay through a decade-long, coercive cap on wages, it is time to rebuild our public health system, starting with some respect for the workforce.
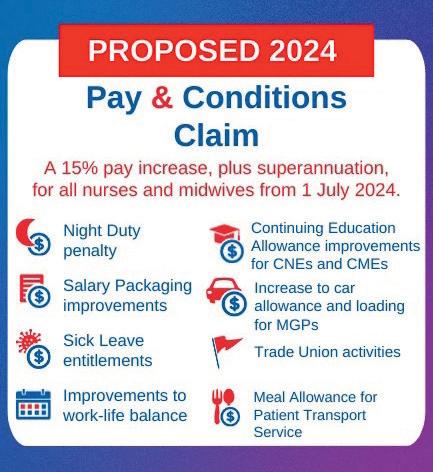
Our fight for a 15 per cent pay rise has escalated with more than 50 rallies held throughout the state in July.
Our claim is fair and justified, and essential if we are to fix the staffing crisis in the public health system and to stop nurses and midwives leaving the industry or moving interstate for better pay and conditions.
NSW public sector nurses and midwives are now the lowest paid in the country. In real terms, their wages are sitting at 2008 levels, while dealing with 2024 costs.
The NSW government must face up to, and rectify, the dysfunctional labour market that has arisen from the suppression of wages over more than a decade by the previous government through its notorious “wages cap”. It also needs to show it is serious about gender equity. While male-dominated jobs like firefighters and train drivers have seen significant pay increases, the female-dominated caring professions have fallen behind.
We are now losing many nurses across our borders, both north and south. In Queensland a new grad makes $12,000 more and is 18 per cent better off compared to a first year NSW nurse. If the state government wants to attract and retain skilled and experienced nurses and midwives, it must pay them a wage that reflects the vital work they do.
OUR CLAIM IS BASED ON SOLID EMPIRICAL
Two recent reports – one by the University of Sydney Business School and another by Deloitte Financial Advisory – validate our pay claim. The first points out that nurses and midwives’ pay is lower than in 2011 and a 15 per cent increase is justified to make up for the distortions in the nursing and midwifery labour markets caused by the State government’s wages cap between 2011 and 2023 (see p. 14).
If the state government wants to attract and retain skilled and experienced nurses and midwives, it must pay them a wage that reflects the vital work they do.
The second establishes a business case to fund a 15 per cent pay rise and the roll out of ratios statewide (see p. 16).
These improvements – ratios and better pay - will attract nurses and midwives back to NSW Health and make our hospitals competitive with other states in the job market.
These reports by respected business experts identify ways in which the government can fund these improvements. So, it cannot keep using a lack of money as a reason to refuse implementing these improvements. If they continue to say “No”, it is not because they can’t pay, it’s because they won’t pay.
We can take some inspiration from our colleagues in Victoria who have just won a 28.4 per cent pay increase over 4 years after a protracted period of industrial action – an outcome that will help retain and recruit the staff needed to rebuild their public health system.
Even though Victoria’s budget is in deficit, the government still eventually found a way to acknowledge the value of nurses and midwives.
However, it still took pressure and perseverance from ANMF Vic members.
As in all our campaigns we will need to be organised and, as always, we achieve success through the courageous actions of our members.
Branch officials, delegates and activists are the backbone of our union. Every day they unselfishly and bravely represent our members in dealings with their employer. They provide an important voice for nurses and midwives in our workplaces.
We understand this role can be very difficult. Many employers don’t want their employees to have a voice in the workplace. One study in the early 2000s found that 23 per cent of delegates experienced hostility from their employer.
As respected IR commentator David Peetz says: “This hostility can put a lot of pressure onto people who, in the end, are only volunteers”.
So, we welcome the introduction of a new framework of rights and protections into the Fair Work Act that recognises the critically important work that delegates undertake and the daunting barriers they can face in the workplace. (See more p. 19).
I hope these new rights and protections will encourage more of you to become involved in the life of our union as we seek to give nurses and midwives a greater voice and increase the power of our advocacy in the public and private health systems and aged care for our patients and residents.n
Pamper yourself this winter in the comfort of your own home! Australian owned and operated, Annabel Trends has been a leader in providing quirky gifts and funky homewares to Australians for over 50 years. Check out their range at www.annabeltrends.com
Win The Lamp has partnered with Annabel Trends to give you the chance to win the ultimate self-care bundle.






Snuggle up with the cosy, luxe heat pillow and keep your tootsie’s warm and toasty with these cute winter booties
Wind down and relax with a Linen Eye
Rest Pillow filled with flaxseed and lavender. Perfect post any long shift
Treat yourself to a spa-like escape right from the comfort of home with a selection of shower steamers that will transform your shower into a luxurious, aromatic escape
Scan to enter
Be the envy of your work besties with a matching neoprene lunch bag and double walled stainless steel drink bottle


Nurses deserve a government that cares

I’m a nursing student, due to graduate in 2024 and enter the workforce in 2025.
I wanted to be a nurse because I believed that nursing was a well-respected and secure job where I could make a difference to the lives of others. As I near the end of my degree, my eyes have been opened to the workforce that awaits me, and I’m afraid.
ENJOY 10% OFF STOREWIDE* during August and September. Simply use promo code NSWNMA10% at annabeltrends.com checkout.
apply. Competition entries from NSWNMA members only, limited to one entry per member. Competition opens 1 August 2024 and 30 September 2024. Prize drawn 1 October 2024. 10% storewide discount valid 1 August –30 September 2024.
Nurses and midwives in NSW are among the lowest paid in the country. With Sydney being the most expensive city in Australia, it is no wonder nurses and midwives are leaving an already stretched workforce, to work in states where they can afford day-to-day living. How does the NSW Government justify telling nurses and midwives they are essential and are valued in maintaining a healthy population, but then do nothing to incentivise them to stay?
I now see nurses who are overwhelmed by unsafe ratios and unsafe overtime. Experienced nurses are leaving the profession, exhausted and defeated. New graduate nurses need the support and mentorship provided by experienced nurses, to mould us into competent healthcare providers. I hate to imagine the consequences of an inexperienced workforce.
This year, I lost my mother to oesophageal cancer. I am eternally grateful for the nurses who cared for her during her final months. They drew her blood, administered her chemotherapy, traded soup recipes when my mum could no longer swallow solid food, and held her hand when she was afraid. They weren’t just healthcare providers - they were so much more.
It’s heartbreaking to think that the nurses who cared for my mum during her most vulnerable moments aren’t being cared for by our government. It is past time for the NSW Government to step up, listen to the nurses and midwives of NSW, and treat them with the same respect, compassion, and integrity that they demonstrate each and every day.
Dimity Morrison, Nursing student
If there’s something on your mind, send us a letter and have your say. You could

As a mental health nurse, I work closely with patients presenting with varying levels of mental health crises. As a mental health nurse for the entirety of my employment, I have been on the receiving end of violence, physical assaults and mistreatment. I have had patients hit, kick, punch, scratch and spit on me, whilst I’ve also been in the firing line of some absolutely abysmal verbal abuse. What has also become apparent to me is not only a surge in mental health presentations to the emergency department, but also an obvious clinical deterioration in the mental health status of those presenting.
The current surge and increase in acuity of mental health presentations is largely due to the insufficiencies of our health system, both within an inpatient and community-based setting.
Currently the services and resources along with the staff employed in them are completely at breaking point. We are burnt out, over worked, undervalued and under paid for our skill level, experience, and patience. But it keeps falling on deaf ears.
The recent increase in assaults on healthcare workers is just another symptom of a broken system that is set up on systemic bias and failure.
Teaghanne Sarina, RN
My nursing journey began as an AIN within Justice Health, where I first discovered the power of advocating for my colleagues against bullying and challenging work cultures.
Last year I completed my newgrad, and I witnessed firsthand the impact of our working conditions, from working on the floor, to the struggle our fellow nurses and midwives face on our current pay.
This experience ignited my desire to advocate for our members – it’s a commitment that remains steadfast today. Hearing the concerns of my colleagues, witnessing their challenges and empathising with the burdens imposed by our current healthcare system on their livelihoods, has deeply motivated me to advocate on their behalf.
Today, navigating through the wards and units of our expansive hospital has been both enriching and challenging. From brief, uplifting conversations about how excited or ready members are for action to difficult discussions about the essence of unionism and the power of our collective strength. It is a privilege to listen to my colleagues’ stories, frustrations and aspirations. These interactions have reinforced my resolve to unite our efforts towards common goals, whether advocating to support ongoing 12-hour shifts patterns, challenging the use of inotropes in ward settings to addressing staffing concerns impacting on patient safety.
I have had the opportunity to participate in training and to attend rallies, including one in front of the Ministry of Health. It was inspiring to witness passionate nurses and midwives united in voicing our collective struggles, and demanding our need for 15 per cent. We cannot live with 2024 rents and mortgages on our stagnating 2008 wages!
Members are now out on the floor. We began by wearing badges and sparking conversation about getting involved in our fight for better pay. Our solidarity defines us, and now more than ever, we stand prepared to champion better pay and conditions for our essential work.
Justin del Prado, RN, Westmead branch president

I want to acknowledge the amazing women in my family who have chosen to pursue a career in nursing. My mum, Janet, my sister, Lily, and myself, are all at different stages and specialties in nursing.

Our mum, Janet, is an EEN in a rural multidisciplinary hospital; she works across many specialities on any given shift.
My sister, Lily, will graduate from Armidale University later this year to begin her career as an RN.
I have spent nearly 20 years working as an RN in operating theatres in both the public and private sectors in NSW and QLD.
You might have clocked the age difference here. My mum is still working in her early 60s, I am 40 and have spent my entire career until now nursing in hospitals, and my 22-year-old sister is just stepping into her first nursing role. As the one in the middle of Mum and Lily, I can see how nursing is changing; the shift to more autonomous roles and the reliance on experienced nurses to prop up healthcare facilities, especially so in rural areas.
I am lucky to have a family who not only understands my job, but also does my job – they’re my support crew.
Shay Baynton, RN
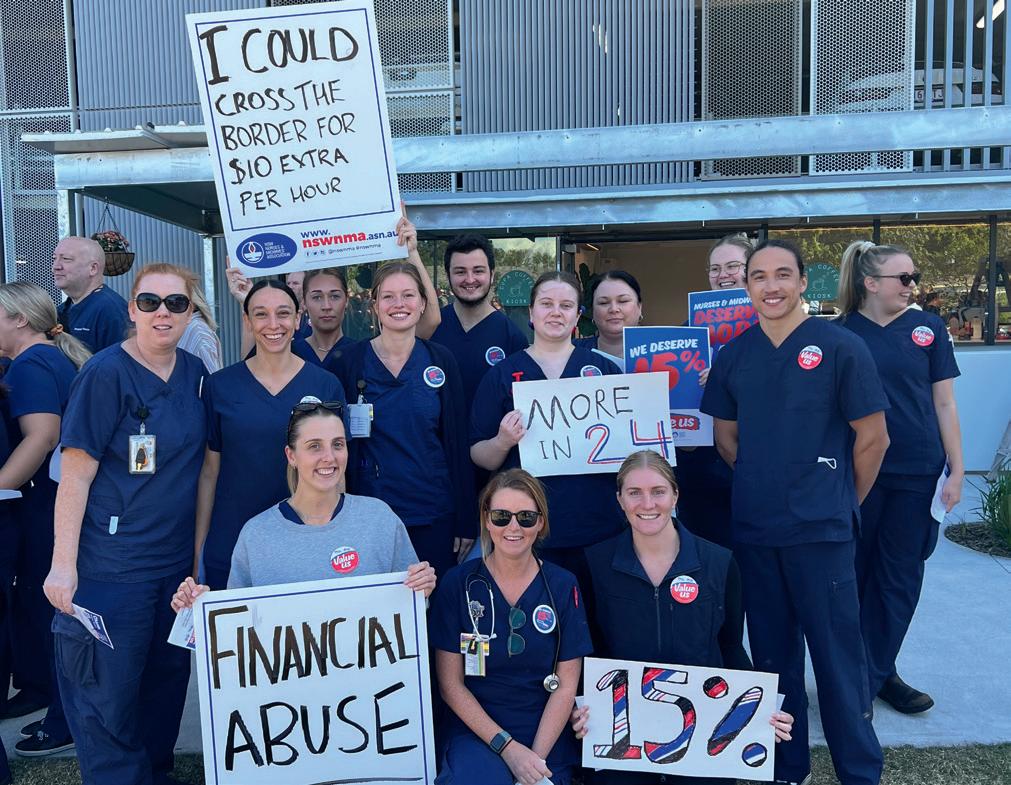
Public sector nurses and midwives held more than 50 rallies statewide in late July in support of a one-year 15 per cent pay rise to fix the staffing crisis in the public health system.

NSWNMA General Secretary Shaye Candish said the pay rise was needed to stem the flow of nurses and midwives leaving the industry or moving interstate for better pay and conditions.
“To attract and retain experienced nurses and midwives, the NSW government must pay wages that reflect their vital work, and also respect and value the state’s largest female-dominated professions,” she said.
“Nurses and midwives have been underpaid and undervalued
by successive Coalition state governments for more than a decade, and their wages are sitting at 2008 levels in real terms.
“While male-dominated jobs have seen significant pay increases, our most trusted professions are falling behind.”
REAL WAGES HAVE FALLEN BY 10.5 PER CENT
At Royal Prince Alfred Hospital, more than 200 nurses and midwives gathered in support of our pay claim on July 23.
RPA Branch President Katina Skylas said it was becoming increasingly difficult “to keep our colleagues with our current pay and working conditions the way they are”.
“Why are we here? We are here because our public health system is at breaking point.
“Every day, inflation is making it hard just to buy the groceries. Our wages have fallen by more than 10 per cent over the last four years. NSW is lagging behind.
“Our colleagues are changing careers and changing states. They are

‘ We are here because our public health system is at breaking point.’
— Katina Skylas, RPA Branch President
moving to Queensland and Victoria where their governments recognise their value. In Queensland they are getting $12,000 a year more. They are 18 per cent better off than we are here in NSW.
“We are here to let the state government and Ryan Park know that we are not happy. We demand that you value us.”
NSWNMA President O’Bray Smith said there were simply not enough nurses or midwives.
O’Bray pointed out that while maledominated jobs have seen significant pay increases, the female-dominated caring professions have fallen behind.
“A third-year nurse makes $77,000 per year. Firies earn $90,000 per year, train drivers 110,000.
“We need to get out and fight. The first step is to talk to our peers. Our wages have been suppressed since

‘Start talking to your colleagues. Wear badges. Be proud. Keep up the fight.’
— NSWNMA President O’Bray Smith
2010. We need to send a message to our local MPs that NSW is lagging behind.
“Start talking to your colleagues. Wear badges. Be proud. Keep up the fight.”
Shaye Candish says the state government could learn from the way the federal government is addressing the gender pay gap and addressing the staffing crises in aged care and childcare.
“The NSW government needs to show it’s serious about gender equity and do the same.
“The longer the government fails to act the worse it is going to get. Now is the time to intervene.
“Implementing safe staffing levels and valuing the work is what is needed to rebuild the nursing and midwifery workforces.” n
More than 20,000 nurses and midwives exhausted all their annual sick leave entitlements during the 2022/23 period
The latest turnover rate for public sector nurses was 11 per cent – almost double the six per cent in 2010
Nurses and midwives worked more than 2.8 million hours of overtime during the 2022/23 period
There are record presentations to emergency departments across the state – more than 810,000 in January-March 2024
There were more than 1.9 million agency hours over the last two financial years across NSW.
Members voice enthusiastic support for 15 per cent claim at city and regional hospitals across New South Wales.

The NSWNMA rally at Maitland Hospital in the lower Hunter region started with a march from inside the hospital, through the outpatients’ clinics and out the front gate, where staff got a warm reception from passing motorists.
It was Maitland’s biggest rally in recent memory drawing more than 80 people, said Branch President Monique Murray. Nurses from Maitland’s mental health branch and community nurses joined in along with members from Dungog and Cessnock hospitals. “We will probably call a branch meeting in a couple of weeks to have a debrief on the rally and get people’s opinions and ideas for our next action,” Monique said.
Rally speakers included newly graduated nurse Ashley Ball, mental health nurse Laurel Kibble, Branch Assistant Secretary Melissa Gole and Monique. She said the rally got widespread favourable media coverage including from ABC radio and TV, NBN News, the Newcastle Herald and Maitland Mercury.
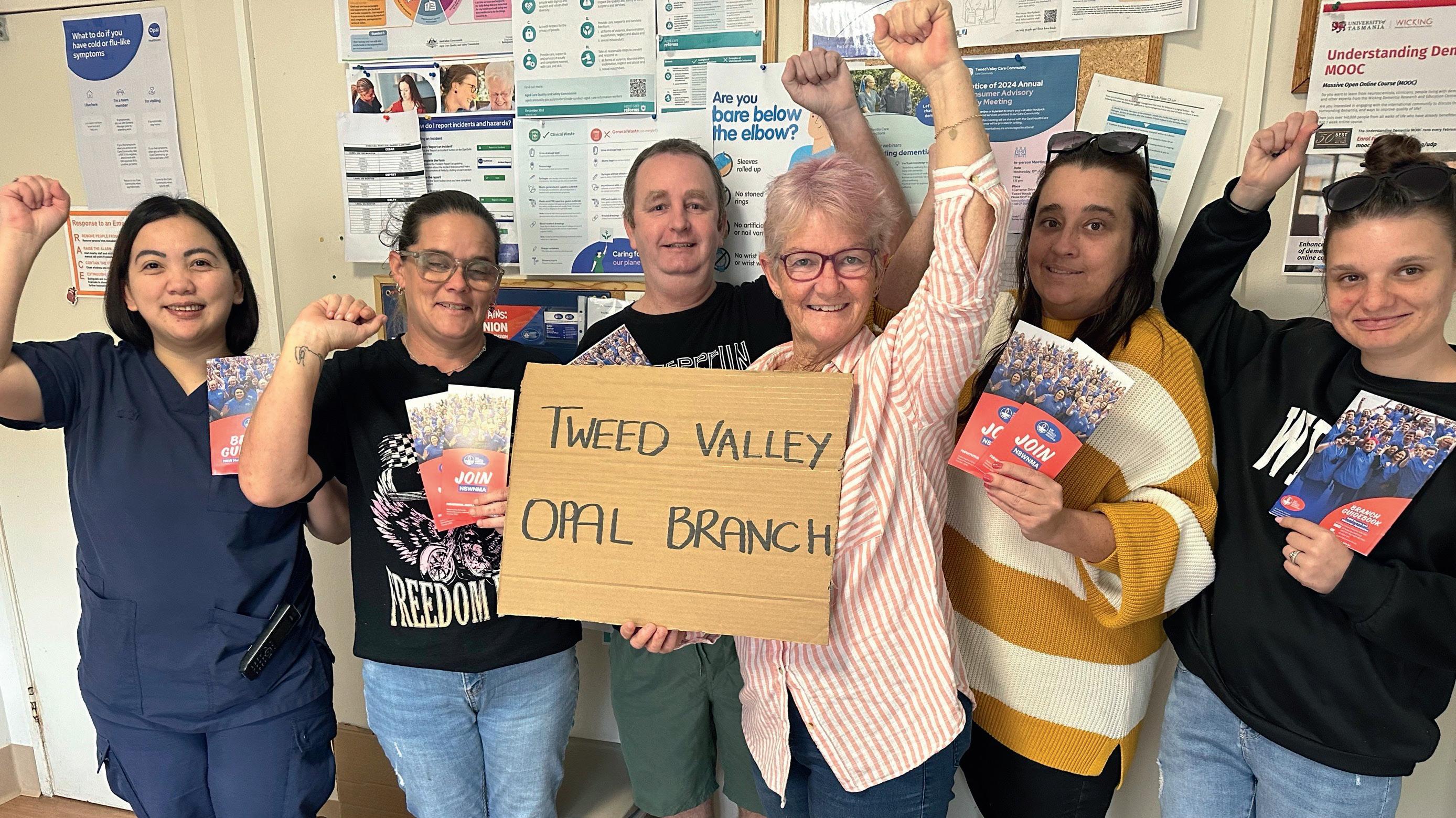
In northern NSW, about 200 nurses and midwives supported by medical and administrative staff rallied outside Tweed Valley Hospital in a powerful show of support for the NSWNMA campaign. “It was an amazing response,” said NSWNMA Branch President Kristin RyanAgnew. Members of the public also attended in response to advertising by the branch via social media, posters, stickers and badges.
Representatives from other healthcare facilities in Northern NSW LHD were also at the Tweed Valley Hospital rally. Kristin said NSWNMA branches in the LHD including Ballina, Grafton, Lismore, Murwillumbah and Tweed Valley had recently stepped up their joint work to share information, resources and support.
Rally speakers included Lismore Base Hospital Branch President Penny Anderson, NSWNMA General Secretary Shaye Candish, and Kristin.


More than 100 nurses and midwives attended the NSWNMA rally at Gosford Hospital on the Central Coast. Branch President Meg Pendrick said the big turnout showed members “have had a gutful” and are ready to take action “as often as we have to to get results. We know we are worth a lot more than they are paying us.”
Meg said nurses and midwives “feel undervalued and they’ve had enough. They can’t believe this government doesn’t value us and won’t fix what they promised to fix. Health is something everyone needs, and everyone uses. Why doesn’t the government care?”


A lively rally at Port Macquarie Hospital on the Mid-North Coast saw nurses and midwives “fired up and ready for the next phase of the campaign” with widespread support for strike action, said NSWNMA Branch President Mark Brennan.
“We are eight hours from the border and haemorrhaging staff to Queensland. I work on a small ward where we recently lost two young staff members who went to Queensland for better pay and conditions,” he said.
Up to 50 staff joined the demonstration despite a medical emergency involving a shark attack victim, which prevented ED and theatre nurses from attending.
Speakers at the rally included NSWNMA Assistant General Secretary Michael Whaites and Mark.

Nurses and midwives at the Sutherland Hospital rally in Sydney’s south were urged to join an emailwriting campaign directed at their local MPs.
NSWNMA Branch Secretary Liz Turner said the branch would help people write emails using templates developed by the union. “We want to make it as easy as possible but also meaningful and original, so the politician isn’t just receiving a form letter,” Liz said.
She added, “The mood at the rally was strong; people feel they are undervalued and disrespected and that we deserve a 15 per cent pay rise this year. Community members approached me at the rally and asked if there was a ‘friends of nurses and midwives’ support group they could join. I will make enquiries because it seems like a good idea.” n
Branch teamwork brings encouraging response to union pledge drive.
The NSW Government’s refusal to give nurses and midwives a pay rise greater than 4 per cent last year sparked action by NSWNMA branch members at Belmont Hospital in Lake Macquarie.
“With COVID-19, we went through something very significant, hard and traumatic, but the low pay increase showed that our premier and treasurer still could not see our worth,” said emergency nurse Sarah Howell.
She took on the role of branch delegate and assistant secretary early this year, joining other newly elected officials such as president Danika Weller, secretary Laura Ford, and vice president Leonie Brewer.
“We were furious about the 4 per cent and we all agreed we were not going to take it lying down,” Sarah said.

“We weren’t happy, and we could see our colleagues weren’t happy. We decided to get more active and try to make a difference.”
‘We weren’t happy, and we could see our colleagues weren’t happy. We decided to get more active and try to make a difference.’
— Sarah Howell, branch delegate
After years of strict wage caps, understaffing and heavy workloads, anger over the 4 per cent increase helped drive branch membership to a record high at Belmont, which has 128 beds.
Belmont branch officials recently collected over 200 signed pledges from nurses willing to take action in support of the union’s public health sector 15 per cent pay claim.
“Between the branch officials, we were able to cover all wards, as well as the drug and alcohol centre,
which is located adjacent to the main hospital,” Sarah said.
“We have great teamwork among branch officials – we help each other out and we delegate to other people.
“We can go to them and ask if they are happy to distribute information to a particular ward. We might ask them to tell five people about an issue, and ask each of those five to tell five more people.
“We walked around the wards during our breaks and had conversations with whoever was in the tearooms. We also spoke with nurses as they changed shifts, and with people we ran into in the corridors.

“We asked people to consider taking on whatever action they felt comfortable doing.
“The big majority indicated they were up for taking action, from wearing a badge to going on strike.
“If you walk into our car park on any given day, you will see NSWNMA bumper stickers everywhere.”
Sarah said 42 members attended a recent monthly branch meeting in person, while many others joined online.
“It was an awesome turnout both in person and online. The result was 99 per cent of members voting for action, which shows there is a lot of fight and passion around the issue.
“A lot of members pointed to the recent pay rise (28.4 per cent over four years) won by nurses and midwives in Victoria.
“They fought and won and set a precedent for us in NSW. We feel it’s our turn now; if they can get a decent increase, so can we.”
“WE WANT MORE IN ’24”
The branch meeting decided to support the wearing of union scrub shirts and badges every day until the pay dispute is won.
“We will have another branch discussion very soon about our next
‘We asked people to take on whatever action they felt comfortable doing.’
steps. We might ramp it up with kerbside rallies or join in an action across the LHD, like we did two years ago at Civic Park in Newcastle,” Sarah said.
The Belmont branch joined other branches in the Hunter New England LHD to kick off the public phase of the pay campaign.
This took the form of a lively protest at the second women’s State of Origin game played at Newcastle’s McDonald Jones Stadium.
“We advertised the event on our branch Facebook page and put up posters in the tea rooms, and we met at the park across the road from the stadium before the game,” Sarah said.
“As the crowd walked through the gates, we were on the side chanting, “We want more in 2024”, “Pay us fair” and “Stand up fight back”.
“It was torrential rain so we all wore blue union ponchos with the NSWNMA emblem. We had blue wigs and feather boas and lots of blue glitter.”
Belmont nurses carried placards with “Try” on one side and “Try Harder Treasurer” on the other – combining support for the NSW Sky Blues with a message for the state treasurer, Daniel Mookhey.
Sarah said the Belmont branch is welcoming a number of new nurses, including newly graduated nurses who recently joined the hospital.
“We will make them aware of what the branch can do for them – for example, advising them of benefits they are entitled to under the Award.
“Our experience as branch officials has given us the confidence and strength to support our nurses and midwives on a range of issues.” n
University report says a 15 per cent pay increase is justified to make up for lost spending power and current inflation.
Real wages of NSW nurses and midwives have fallen by more than 10 per cent since 2020, said a report from the University of Sydney’s Business School.
It said real wages are now lower than before 2011, when a state Liberal government imposed a 2.5 per cent wages cap for public sector workers.
The term “real wages” means wages adjusted for inflation, to take into account movements in the prices of goods and services.
The report was prepared for the NSWNMA by Professor John Buchanan, Dr Troy Henderson, and Associate Professor Jo-An Occhipinti.
It said NSW nurses and midwives now “earn less than just about all other professions and many nonprofessional occupations, such as real estate agents (by up to $75,000 per annum), finance brokers (by over $100,000 per annum) and many sales representatives (by $10,000 to $20,000 per annum)”.
“Compared to a range of professionals (i.e., occupations requiring a degree to practice) nurses and midwives are among the lowest paid at all ages. The issue is stark among nurses aged over 40,” the report stated.
“Among NSW public sector workers, entry level nurses and midwives are paid less than teachers, police and firefighters (often by margins of 10 to 20 per cent).
It is time to escape the curse of NSW Treasury’s wage cap and begin the move to wage levels that are compatible with a sustainable nursing and midwifery labour market.’
“Given recent wage agreements this situation is set to worsen, especially in comparison with paramedics.”
The report pointed out that NSW nurses and midwives are paid less than many other states and territories.
NSW
At entry level, NSW pays the second lowest rates in the country.
Entry level nurses and midwives in Queensland earn a base rate of $82,753 – 18 per cent more than the $70,050 paid in NSW.
“At the top of the incremental structure, NSW is in the middle of the pack,” the report said.
Top-level RNs and midwives in Queensland earn $106,144 – 8 per cent more than the $98,315 paid in NSW.
The report said that in real terms, the relative pay of NSW nurses and midwives is further behind all other higher paying states and territories, where the cost of living is also “significantly cheaper”.
Current base pay rates for RN at entry level and highest automatic increment, by jurisdiction, as at April 2024
Source: Escaping NSW Treasury’s Curse – NSW Nurses and Midwives’ Pay, 1999–2024 and beyond, Buchanan et al., University of Sydney Business School, 17 May 2024.
‘ Compared to a range of professionals, nurses and midwives are among the lowest paid at all ages. The issue is stark among nurses aged over 40.’
The report described the 2.5 per cent wages cap (introduced by the previous Liberal government) as “the direct cause of wage stagnation and rising cost of living pressures for the State’s essential services workforce”.
“Between 2011 and 2023, NSW nurses and midwives’ pay was deliberately suppressed. During that time, no consideration was given to the deepening problems afflicting the profession.”
The wages cap “entrenched uncompetitive wage rates that now result in growing losses of skilled workers – including nurses and midwives – to other states and territories”.
It said, “Given all the above, it is unsurprising that the nursing and midwifery labour market in NSW is under severe stress.
“This is evident in high levels of unfilled vacancies and registered nurses not working in the profession. The labour market is talking – it is time to listen and act.”
After the state Labor government abolished the wages cap in 2023, nurses and midwives received a 4 per cent pay increase, which the report described as “modest”.
“It is now time to devise and implement a sustainable wages policy,” the report said.
It warned that any claim for a wage increase “necessary to put the health system on a more sustainable basis will be met by the usual mantra: ‘nice idea, but we just can’t afford it.’
“This tired narrative should be called out for what it is: the foundations of inefficient wages levels currently contributing to a dysfunctional labour market, marred by high turnover, chronic excess demand, and many registered nurses and midwives not practising in the profession.” n
The report from the University of Sydney’s Business School said a pay increase of 15.2 per cent for NSW nurses and midwives in 2024–2025 “can be justified”.
“This number represents 4.2 per cent to take account of anticipated inflation and average movements in productivity.
“The remaining 11 per cent would restore real purchasing power and ensure NSW nurses and midwives begin to share more fairly in the cumulative national productivity improvements of recent decades.
“This claim may seem large in terms of the recent history of wage movements – but that is the point,” said the report.
“It is the wage movements of recent times that have been the problem (as witnessed by a dysfunctional nursing labour market).
“It is time to escape the curse of NSW Treasury’s wage cap and begin the move to wage levels that are compatible with a sustainable nursing and midwifery labour market.” n
The University of Sydney Business School report said the Australian economy has had the capacity to provide “serious real wage increases”, but these have not occurred.
To the question “Where has the money gone?” it answered – to higher company profits.
“The wages share of GDP (gross domestic product) is now at its lowest level in 50 years: down from a high of over 60 per cent in the 1970s, to just on 50 per cent today.
“On the other hand, the proportion accruing to corporations has risen from 20 per cent of GDP fifty years ago, to 30 per cent today.
“Unless wages settings change significantly, this situation will at best remain stagnant, and at worst these factor shares of national income will become more unbalanced in favour of corporate profits.”n
Proportion of GDP going to employees and corporations 1960-2022
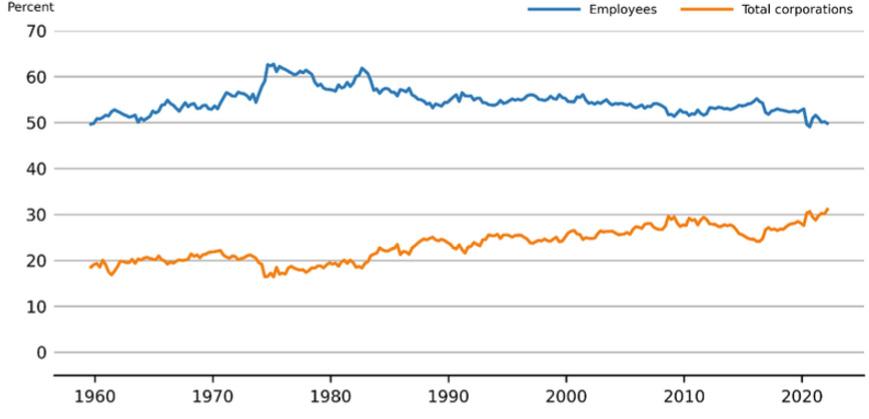
Source: Escaping NSW Treasury’s Curse – NSW Nurses and Midwives’ Pay, 1999–2024 and beyond
The NSWNMA asked Deloitte Financial Advisory to calculate and compare the costs and financial rewards of a 15 per cent wage increase and rolling out agreed staffing ratios.
The Association has handed the NSW Government a business case for a 15 per cent wage increase for nurses and midwives and safer hospital staffing.
Our proposal to the NSW Treasury department shows the government where it can find the money to pay for these and other improvements.
The improvements will attract more nurses and midwives back to NSW Health and make NSW public hospitals competitive with other states in the job market, the proposal said.
Costings for the business case –including revenue opportunities, cost savings and benefits – were calculated by Deloitte Financial Advisory for the NSWNMA.
The business case put forward three major initiatives:
1. Finish implementing ratios across agreed clinical areas – to cost about $204.4 million.
2. Pay a 15 per cent wage increase – to cost about $863 million.
3. Make assistant in nursing (AIN) positions supernumerary – to cost about $130 million.
The state government can fund the three initiatives by accessing “system-wide funding opportunities” identified in the business case.
They include “technical efficiency” measures, which aim to secure additional funding from the Commonwealth without increasing patient activity.
NSW public hospitals have left billions of dollars of Commonwealth funding on the table by not undertaking these technical efficiency measures, the business case argued.
It said the state’s “cumulative forgone Commonwealth funding contribution” amounted to about $3.28 billion between FY19 and FY23.
The report also proposed “allocative efficiency” measures that involve reallocating patients to more appropriate parts of the healthcare system.
The business case calculated the economic value of finishing the rollout of ratios in agreed areas, a 15 per cent pay rise and making AINs supernumerary.
Benefits include:
• avoided cost of staff turnover
• improved Commonwealth revenue due to reduced hospital-acquired complications
• increased spending in the economy
• reduced cost of overtime and agency fees
• enhanced patient outcomes.
A reduction in the nursing and midwifery staff turnover by 3 per cent could result in an avoided cost of $86 million.
A one-third reduction in hospitalacquired admissions could result in improved Commonwealth revenue of $30.3 million.
A 15 per cent wage increase could lead to an economic benefit of $539.2 million through increased spending in the economy.
By recruiting additional nurses and midwives to finish the rollout of safe staffing levels, and by converting AIN positions to supernumerary, the state could save $54 million in overtime and agency fees, and reap an economic benefit of $129.8 million through new job creation.
NSWNMA General Secretary Shaye Candish said the significant funding opportunities and cost savings identified in the report were compelling and further strengthened the feasibility of the Union’s 2024 pay and conditions claim.
“This report demonstrates how the NSW Treasurer can afford both higher wages and more nursing and midwifery positions, by removing systemic inefficiencies in the healthcare system,” Shaye said.
“We can see more than $3 billion in untapped Commonwealth funds from the past five years because patient data is not being captured correctly.
“Our proposal shows that by improving NSW Health’s current patient reporting and accurately processing each treatment, access to Commonwealth funding, and the subsequent cap, will increase substantially.
“We know patients are getting sicker and presenting to NSW public hospitals acutely unwell and in need of care, but the data being captured by NSW Health is not reflecting the treatment that is provided, resulting in available Commonwealth funding not being claimed.” n
NSWNMA business case for 15% pay rise and better staffing
Additional
Additional Commonwealth revenue from Additional Efficiencies $277.5m
Cost savings RAC optimisation $233.4m
Cost savings sub-acute optimisation $142.8m
Proposed cost of initiatives
Completion of safe staffing levels ($204.4m)
Increased wages for nurses and midwives ($862.8m) Conversion of AiN positions to super numerary ($129.6m)
Revenue opportunities, cost savings and benefits
Cost savings achieved by reducing the nursing turnover by 3%
Increased Commonwealth revenue due to a reduction of HACs by one-third $30.3m
Reduced cost of overtime and agency costs $54.0m
Increased spending in the economy as a result of the 15% wage growth
Increased spedning in the economy as a result of recruiting additional nurses and midwives to complete the implementation of safe staffing levels and converting AiN positions to supernumerary
The NSWNMA business case pointed out there is a shortage of nurses and midwives willing to work under existing conditions, resulting in understaffing and piling pressure on the existing workforce.
“This, in turn, increases their workload and stress levels, leading to significant burnout,” it said.
“NSW public hospitals find it challenging to compete with healthcare systems in other states, which offer better salaries, working conditions (ratios) and benefits packages.
“As a result, NSW Health appears to be falling behind as an employer of choice. This is leading to LHDs struggling to both recruit and retain nursing and midwifery roles.”
The proposal said NSW has consistently had the highest proportion of non-practising RNs and midwives, who are choosing not to participate in and/or are not being used by NSW Health.
It calculates that by making working conditions and pay more attractive, NSW could bring an estimated 617 experienced nurses and midwives back into the healthcare system. This would reduce its proportion of non-practising nurses and midwives to align with the Queensland/Victoria average.
It said NSW nurses and midwives’ wages have declined in real terms.
A first-year nurse/midwife in 2023 was $2,825 worse off than they were in 2012, when salaries are adjusted for inflation.
$539.2m
$129.8m
Total $170.3m $669.0m
“The stagnated wage growth is a direct result of the previous state government-imposed annual cap on wage growth for public sector workers.
“The new Industrial Relations Act removes any such cap; however, given the current cost of living and previous stagnation, significant improvements will be needed to achieve a competitive workforce,” the proposal said. n
The NSWNMA has set up an online area where you can find updates on the campaign, things you can do and resources to download as we push for a 15 per cent pay rise in our public health campaign. Escaping NSW Treasury’s Curse
campaign. Rapid Business Case supporting submission for the NSWNMA 2024 Award Claim
A report by Deloitte Financial Advisory that outlines the system-wide opportunity for NSW to capture untapped Commonwealth funding and evaluates revenue opportunity, cost savings an
read the latest updates on



Union delegates have new and important rights and protections that recognise their critically important work and the tremendous barriers they can face in the workplace.
The union movement has won important new rights and protections for delegates, which have been incorporated into the Fair Work Act and became operative from 1 July.
All new enterprise agreements must include the new provisions.
The ACTU described the new rights and protections as “a significant achievement”.
A workplace delegate now has a clear right to represent the industrial interests of members (or persons eligible to be members).
“Industrial interests” are what members band together to fight for at work. These include lobbying a government for more funding for a delegate’s sector, signing up members to the union, or organising protected action.

In their role, under the new laws, union delegates are entitled to:
• reasonable communication
• reasonable access to the workplace and workplace facilities, and
• reasonable access to paid time during normal working hours to attend related training.
‘The new rights) will have positive effects over the long run, on pay and conditions, union membership, workplace cooperation, grievance resolution and productivity.’
— David Peetz
Workplace delegates also have important new protections.
An employer of a workplace delegate must not:
• unreasonably fail or refuse to deal with the workplace delegate, or
• knowingly or recklessly make a false or misleading representation to the workplace delegate, or
• unreasonably hinder, obstruct or prevent the exercise of the rights of the workplace delegate.
To be able to exercise these rights, a delegate needs to give their employer written notice of their appointment or election.
An employer must provide a workplace delegate with up to five days of paid training in their first year, and then one day of training annually in subsequent years.
Respected industrial relations expert David Peetz says the new rights and protections “will increase the voice of employees in the workplace”.
“(They) will have positive effects over the long run, on pay and conditions, union membership, workplace cooperation, grievance resolution and productivity,” he wrote in the online journal Pearls and Irritations
“OECD research shows that consultation with employee representatives is crucial for ameliorating the impact of new technology, particularly artificial intelligence, including on safety.
“The OECD found that direct voice between workers and managers was associated with a higher quality work environment.” n
NSWNMA members at Ramsay Health Care have taken industrial action for the first time.
NSWNMA members at Ramsay Health Care launched industrial action for a pay increase and safer staffing in July.
Members at the company’s NSW facilities voted strongly in favour of action in a secret ballot conducted by an independent agency.
They voted between 86 per cent YES and 96 per cent YES to each of 10 specific forms of action.
These ranged from wearing union badges and campaign clothing, to work stoppages of up to four hours. The company and the NSWNMA Ramsay bargaining committee have held 11 negotiation sessions for a new enterprise agreement since April 2023.
Despite these talks, Ramsay was only offering an 11 per cent pay increase over three years when this edition of The Lamp went to print.
This was the company’s second offer, following its original proposal of 9 per cent over three years. The last Ramsay pay increase was 1.5 per cent in July 2022.
Deanna Hayes, NSWNMA branch secretary and delegate at St George Private Hospital, is a member of the bargaining committee, which includes 10 member-representatives from Ramsay hospitals across NSW.

‘Ramsay is a very profitable business and continues to build new hospitals and buy others.’
— Shaye Candish, NSWNMA general secretary
“We will start with low-level action, such as wearing campaign badges, distributing flyers to patients and visitors, taking our message to the media, and posting information on our social media accounts,”
Deanna said.
“We will escalate action potentially to a stopwork meeting if Ramsay doesn’t come up with something better.
“We are frustrated we have to resort to industrial action to be heard.
Ramsay is not listening to us, despite telling them all the reasons why their offer is insufficient.
“We are doing increasing hours of overtime and regularly miss out on lunch breaks, as a result of staffing shortages. We worry we can’t provide the care our patients deserve under these conditions.
“We feel extremely undervalued and underpaid. Ramsay needs to pay us what we’re worth, or risk losing more staff.”
Deanna said she had seen some nurses quit in the last 12 months and take jobs in the public sector or at other private hospitals.

‘Ramsay needs to pay us what we’re worth, or risk losing more staff.’
— Deanna Hayes, NSWNMA branch secretary
Ramsay is one of the world’s biggest private healthcare companies, with 31 hospitals and clinics in NSW alone. It declared a net profit of $298.1 million for the year to June 2023.
While Ramsay operates in Europe, the UK and until recently, Asia, its Australian hospitals remain its most profitable business.
Ramsay sold its Asia division in December and is reported to be considering selling some or all of its biggest offshore investment, French hospitals group Ramsay Santé.
The Australian Financial Review (AFR) said Ramsay Santé has only ever made one-third to one-half of the profit the company makes from its 72 facilities in Australia.
The AFR said Ramsay might use the proceeds from the sale of overseas assets “to make its Australian business bigger, expanding while smaller and poorly capitalised hospital groups are struggling.”n
“They were fed up with Ramsay pay and conditions and how long the enterprise bargaining was taking,” said Deana.
The vote in favour of industrial action followed a powerful “No” vote in a ballot on Ramsay’s proposed enterprise agreement in May.
Eighty-two per cent of nurses and midwives participated in that ballot, with more than 3500 of them (81 per cent) rejecting Ramsay’s offer.
The NSWNMA is seeking an 18 per cent increase over three years and improvements to conditions, including increases to paid parental and personal leave entitlements, and protection of existing conditions.
NSWNMA General Secretary Shaye Candish said it was disappointing Ramsay hadn’t come to the table with a pay and conditions offer that recognised and valued their employees.
“Ramsay is a very profitable business and continues to build new hospitals and buy others,” Shaye said.
RAMSAY CAN AFFORD IT
“We know they can afford to pay our hardworking nurses and midwives what they’re worth.
“This is the first time our members are taking protected industrial action against Ramsay in NSW.
“This decision is not being taken lightly, but Ramsay has repeatedly refused to come to the table with an offer that reflects the incredible work of nurses and midwives.”
Shaye said Ramsay’s most recent offer of 11 per cent over three years was well below inflation and did not address cost-of-living pressures.
“Under Ramsay’s latest offer, its nurses and midwives in NSW would be paid up to 14 per cent less than their Queensland counterparts.
“Ramsay staff fear they will be paid less than NSW public sector colleagues when their deal is struck.
“Ramsay also refuses to consider staffing ratios, to ensure safe patient care and safe workplaces for nurses and midwives.
“As part of our claim, we want to see shift-by-shift nurse/midwife-topatient ratios introduced in all wards and units in Ramsay hospitals,” said Shaye.
“Our members are struggling to keep up with workloads due to staffing shortages. It is not safe for staff or patients, and we urge Ramsay to commit to implementing staffing reforms across its NSW sites.”
Shaye added the company was seeking to cut conditions such as eligibility for the higher on-call allowance, no in-charge patient-load hospitals, and weekend penalty rates for casual employees. n



NSWNMA members take action to defend annual leave, long service leave and sick leave, as the hospital returns to public hands.

Apublic rally and petition campaign by NSWNMA members has helped to protect leave entitlements for more than 700 staff at Hawkesbury Hospital.
Their entitlements to long service leave, annual leave and accrued sick leave were under threat of being paid out as a result of the hospital’s transfer back into public hands.
On 1 July, the operation and management of Hawkesbury District Health Service was transferred from St John of God Health Care to Nepean Blue Mountains Local Health District, under the new name of Hawkesbury District Hospital.
St John of God Health Care had operated the 131-bed facility for the previous eight years, providing
public patient services under a public–private partnership (PPP) with the LHD.
An announcement on the St John of God website said, “Operating a single public–private partnership hospital in New South Wales creates a range of operational and financial challenges.”
Before St John of God Health Care took control in 2015, the hospital was operated as a PPP by Catholic Healthcare, which took it over from the state government in 1996.
In March, staff learned their leave was intended to be paid out, due to the transfer of business between the public and private sectors.
As NSW Parliamentary Secretary for Health Dr Michael Holland put it in a letter to state MP Robyn Preston, as
‘We’ve now been assured that all our sick leave will be transferred, and our current salary packaging arrangements will continue for another two years.’
— Ben Wright, NSWNMA branch secretary, Hawkesbury DHS
quoted in The Hawkesbury Post: “The Australian Government legislation (Fair Work Act 2009) prevents staff from being able to be transferred directly to the district. This means that once a staff member’s employment at St John of God ends, the Act prescribes obligations on the employer to pay annual and long service leave entitlements.”
Following protest action by nurses and midwives, and negotiations between the NSWNMA and the NSW Government, agreement was reached to give all staff the option to transfer their accrued annual and long service leave entitlements to their new employer – NSW Health –or have them paid out.
NSWNMA General Secretary Shaye Candish thanked the NSW Government and St John of God Health Care for working collaboratively with the union to achieve a positive outcome for staff.
“This has been an incredibly
stressful and anxious time for our members, so this decision means a lot to them and their families,” she said.
NSWNMA branch secretary at Hawkesbury DHS Ben Wright said staff had faced “a forced leave payout, a loss of accrued sick leave entitlements and a drop in takehome pay due to changes in salary packaging arrangements”.
Ben said getting entitlements paid out in a lump sum would have affected government support payments such as family tax benefits, paid parental leave and childcare rebates, and would have pushed some people into higher tax brackets.
He added: “We’ve now been assured that all our sick leave will be transferred, our current salary packaging arrangements will continue for another two years, and members will have the choice to transfer their long service and annual leave entitlements.”
ONLINE PETITION SIGNED BY 2500 Nurses and midwives organised an online petition that quickly attracted more than 2500 signatures.
They rallied outside the hospital at Windsor in northwest Sydney in their own time, calling for a transition that did not disadvantage staff.
The rally attracted more than 100 hospital employees and community members, including state MP Robyn Preston.
NSWNMA delegate for Hawkesbury DHS branch Ann Jackson said federal MP Susan Templeman was unable to attend but sent a letter of support, with an undertaking to lobby for


‘The level of public support really demonstrated what a fantastic community we have in the Hawkesbury.’
— Ann Jackson, NSWNMA delegate, Hawkesbury DHS branch
changes to unfair provisions of the law affecting employee transfer.
Ann, who has worked at the hospital for almost 30 years, described the outcome as a win and a big relief for staff.
“People now have a choice: they can transfer their leave entitlements or have them paid out. If they choose a payout, they will have the option to take leave without pay later on,” she said.
Ann said the leave arrangements originally announced would have hurt the longestserving and most loyal staff.
“Some people had thousands of dollars’ worth of leave, but it wasn’t just about the money – it was also about the time. Many people have not been able to take their leave because of the COVID pandemic.
“It’s not unheard of for some people to have 400 hours of leave and 12 months long service leave if you’ve been there for 30-odd years.”
Ann said gaining community support was a big factor in the win.
“People came up to us asking what they could do to help, and we pointed them to the petition.
“The level of public support really demonstrated what a fantastic community we have in the Hawkesbury.
“We are very appreciative of the NSWNMA, NSW Health and St John of God Health Care for working together to resolve this for us.”
Ann said there was still some confusion about the tax implications of the transfer of employment.
“A small minority of staff may face negative tax implications due to factors outside the control of NSW Health and St John of God.
“Some people could find themselves in a higher tax bracket as a result of Tax Office requirements. The federal government needs to look at this so it doesn’t happen to other nurses in the future.”
Ann said Hawkesbury Hospital, originally built as a convict barracks in 1820, held a special place in the hearts of the community. It was converted into a hospital for convict gangs, became a hospital for the poor and later opened as a state hospital.
St John of God said it would keep its two other NSW hospitals at Richmond and Burwood. They are private mental health facilities. n

Our members in aged care have achieved memorable victories in recent years as their campaign for a better resourced sector bore fruit, with significant increases in federal government funding.
The challenge going forward for the sector is to ensure these extra resources are deployed as they were intended: to improve care and to solve the endemic issue of workforce shortages and poor working conditions for aged care staff.
The COVID-19 pandemic starkly exposed the dire state of the sector and the poor track record of aged care providers in ensuring taxpayers’ money was efficiently allocated to improved care.
Making employers accountable is the next step in our campaign to improve the lives of Australia’s elderly in aged care, and bargaining campaigns are a vehicle to advance our goals.
Historically, aged care has been a difficult area to get results, but with an increased union presence in workplaces, good branch organisation and the increased funding, we can achieve our goals.
Building the capacity to win will be helped by new federal laws that give improved rights and protections to union delegates (see pp 19).
Branch Beat looks at how our members at Opal are organising to improve the lives of their residents.
Using one-on-one conversations, Zoom meetings, and local WhatsApp and other social media groups, Opal members are now organising and ramping up the pressure on Opal to come back to the table with an offer that recognises Opal staff’s hard work.
For the first time, NSWNMA members at 47 Opal HealthCare aged care facilities voted down a new agreement after management offered a paltry pay increase, no improvements in sick leave and no improvements in staffing.
The No vote came after Opal ignored a petition from 1700 staff calling on the company to meet with union representatives to discuss a better offer.
Marta Frasca, who has worked as an AIN at a residential care centre on the NSW Central Coast for 23 years, said staff are close to breaking point.
“There has always been an issue with a shortage of staff, but in the last few years it has become more prominent,” she said.
Staff workloads have increased at her facility, as more residents now have higher care needs.
“We have more demented and sicker residents, and they can be violent and suffer from mental illness, which makes it more difficult. At the same time, staff levels haven’t gone up.”
Marta is one of a growing group of member leaders at Opal who are driving an organising effort that has seen membership growth by a third at Opal sites this year and the formation of new Opal branches.
“Staff are stressed out, we are unhappy, and we are anxious that we can’t give proper care to each of the residents,” said Marta.
Marta, who has been a member of our union for around 20 years, said she talks “all the time to staff about their problems”, in the staffroom, as well as on WhatsApp and Messenger groups, to reach people who work late shifts.
Staff are also organising around care minutes with many Opal facilities reporting direct care minutes below the mandated requirement.

‘Staff are stressed out and anxious that we can’t give proper care to each of the residents.’
— Marta Frasca, AIN
COVID HAS CHANGED THE GAME
Inadequate sick leave is another big issue for staff. Although the Aged Care sector is prone to sickness and infections, employees are only entitled to the legal minimum of 10 days sick leave by their employer.
“Here, infection controls such as masks and PPE ended about three months ago. Soon after we had an outbreak of influenza, and then COVID came back again,” said Marta, who has just been off work herself after contracting COVID.
Staff who contract COVID when the residents have COVID can be paid for “disaster leave”.
But Marta said because she was diagnosed with COVID just before the resident got it, she had to use sick leave.
Judy Woodward, an EN at an Opal site in the Tweed Valley, agrees with Marta that staffing levels are the number one issue for members. And it is an issue that is motivating Opal workers to join the union.
Like Marta, Judy also noted the way COVID has changed the game when it comes to sick leave, with NSW staff only entitled to 10 days a year.
“If we get COVID, whether it’s from the facility or from just carrying on our everyday lives, we then have to be out of the facility for seven days. So, if you’ve had a couple of lockdowns at work in the past 12 months, and
if you consider that we have to take seven days each time, then we’re out of pocket,” said Judy.
“Victoria Opal gives staff 16 days leave, whereas we get 10. We’re just trying to get a fair deal.”
Along with other union members at her facility, Judy has recently helped form a new union branch, one of more than a dozen new branches to form at NSW Opal sites this year.
“We are more than a number in their facility,” Marta said. “We are people working hard to care for residents and to make the company money.” n

I have been sent a jury summons that states I must attend court and may be selected for a trial that could take up to six months. I want to do my civic duty, but are nurses exempt from jury duty?
No. Nurses can apply for an exemption if they wish too, but nurses are not excluded from jury duty.
Schedule 1 of the Jury Act 1977 (NSW) lists those who are excluded. Lawyers, people employed by a court, police officers, those with some criminal history and bankrupts are an example of those who are excluded. Nurses, however, are not listed in this schedule.
Schedule 2 lists those who have a right to request an exemption, and this list includes nurses. Please note the legislation clearly states it is the choice of those listed in this schedule whether they want to seek an exemption, and their employer can’t influence these decisions. There are penalties for employers who seek to interfere.
If you’d like to discuss this further, please get in contact with the Association and ask to speak with an information officer.
Requesting Continuing Education Allowance
Does the NSW Health Continuing Education Allowance (PD2018_008) policy directive state that employees alone are responsible for requesting the CEA?
No. Management also has some responsibility to ensure employees are aware of their CEA entitlements.
Management is responsible for correctly applying the CEA provisions set down in the Award and Policy Directive. It should monitor its processes for considering CEA applications by nurses and midwives, to
When it comes to your rights and entitlements at work, NSWNMA General Secretary Shaye Candish has the answers.
ensure they are efficient and effective, and it is they that are responsible for the timely and accurate assessment of CEA applications and of their calculation and payment.
Management is also responsible for promptly notifying employees as to the status of their application and must ensure employees’ CEA records are accurate and complete.
If a public health entity does not notify an employee they are entitled to the CEA when they commence a new role, nor monitor this issue in the subsequent time or years that follow – it may constitute an “exceptional circumstance” for backpay purposes of the CEA.
What are some suggestions on how a workplace rep can assist a member who is undergoing a performance improvement plan to prepare for a meeting where this plan is discussed?
Some suggestions include:
• explore ideas by asking open questions
• emphasise common ground
• state what is non-negotiable (those things the member must do to fulfil the employment contract) and ensure the member understands these are requirements of them as an employee
• keep the discussion on track
• focus on positive possibilities
• offer assistance where appropriate, such as further training, mentoring, flexible work applications and/ or redefining roles and expectations
• reiterate with the member their responsibility to complete the plan
• advise the member of any timeframes for reviewing the Performance Improvement Plan
• advise the member of what support is available.
and laundry allowances
In the public health system, when are shoe and laundry allowances payable?
If an employee is required to wear an NSW Health-issued uniform and shoes, then both the uniform and shoe allowance should be paid, unless they are supplied.
If an employee is not required to wear a uniform but is engaged in direct clinical care, then laundry allowance only is generally paid.
If an employee is not required to wear a uniform and is not engaged in direct clinical care, then neither uniform nor laundry allowance should be paid.
This is a general guide only and there may be exceptions or variations to the above. For example, no allowance is payable when an employee is on unpaid leave. See clause 23 of the Public Health System Nurses & Midwives’ (State) Award 2023 for further information.
Bonus paid parental leave
I am employed with NSW Health. My partner is employed in the private sector and has access to 10 weeks of employer paid parental leave. Am I still eligible to access the two weeks bonus paid parental leave, even though my partner also has access to employer paid parental leave?
Yes. As outlined in section 5.1.2 of the Leave Matters for the NSW Health Service Policy Directive, you are still entitled to access the two weeks bonus paid parental leave. However, unlike employees who may be a single parent or whose partner does not have access to employer paid parental leave, both you and your partner must have exhausted your paid parental leave entitlements prior to accessing the two weeks bonus paid parental leave.
Voting for industrial action
I work at a private hospital, and we are currently bargaining for a new enterprise agreement. We’ve recently been asked to vote in a ‘protected action ballot’. What does that mean?
Under the Fair Work Act 2009 (Cth), workers are allowed to take action in support of their bargaining claims (higher wages, better conditions, staff ratios etc.) only during a bargaining period and where the Fair Work Commission has given an order.
The ballot shows the Fair Work Commission there is majority support to consider taking industrial action. If you have any questions about industrial action, please contact your bargaining team or the Association office.
Rostering and multiple 12hour shifts
I work in a rural Multi Purpose Service (MPS) and have
recently been put on 12-hour shifts for five days in a row. I’m exhausted but I don’t know if this roster is wrong.
This roster is in breach of the Public Health System Nurses and Midwives’ (State) Award and presents a serious health and safety risk for both nurses and their patients.
In specific wards, units or services where an agreement has been reached between management and the nurses or midwives working in that area, with the assistance of NSWNMA, 12-hour shift rosters are in place.
An alternative shift pattern must be made available if you elect not to work 12-hour shifts, as 12-hour shift rosters are voluntary.
Clause 5(v)(f) of the award provides that you cannot be required to work more than three consecutive shifts in a 12-hour shift system, or more than four consecutive shifts once per 6-week cycle, when you have requested.
There is also an overriding principle that rosters must be safe. If you are experiencing hours like this, please ask your manager to rectify the roster immediately. If you’re unable to resolve the matter, please contact NSWNMA for assistance.


“Nurses and midwives are the canary in the coal mine”
with QNMU Secretary Sarah Beaman
Go online to register for these education sessions and our free range of live webinars. Use the dropdown search fields to search by topic (Professional Courses, WHS Courses and Webinars), suburb or month
Further topics and sessions are under development for 2024 and will be published as they are confirmed.
Waterloo
Law, Ethics and Professional Standards in nursing and midwifery
Thursday 26 September and Thursday 21 November, 9am-4pm, 6 CPD Hours
Members $95/non-members $190
Blacktown
Aged Care Seminar
Friday 20 September, 9am-4pm, 6 CPD Hours
Members $60/non-members $120
Broken Hill
Nursing & Midwifery Seminar
Rescheduled, date TBC, 9am-4pm, 6 CPD Hrs
Members $75/non-members $150
Coffs Harbour
Medications: How we do it better Thursday 28 November, 9am-4pm, 6 CPD Hours
Members $95/non-members $190
Gymea
Wound Care: Understanding Wound Care Products
Wednesday 20 November, 9am-4pm, 6 CPD Hours
Members $95/non-members $190

Clinical Communication and Documentation
Wednesday 18 September, 9am-4pm, 6 CPD Hours
Members $95/non-members $190
Port Macquarie
The Deteriorating Patient
Tuesday 10 September, 9am-4pm, CPD Hours
Members $95/non-members $190
Understanding Your Annual CPD Obligations
Wednesday 11 September, 9am-1pm, 3.5 CPD Hours
Members $50/non-members $100
Shellharbour
Effective and Timely
Management of the Deteriorating Older Person
Thursday 17 October, 9am-3pm, 5 CPD Hours
Members $95/non-members $190
Wagga Wagga
The Deteriorating Patient Thu 7 Nov, 9am-4pm, 6 CPD Hrs
Members $95/non-members $190
Understanding Your Annual CPD Obligations
Fri 8 Nov, 9am-1pm, 3.5 CPD Hrs
Members $50/non-members $100
As health professionals we need to ensure people in our care who are having difficulty can be appropriately managed and cared for.
This workshop will cover key elements of deterioration such as: When to worry; A-G Assessment; Urinary system changes; Neurological changes; Respiratory system changes; Circulatory system changes; and Communication for detecting and maintaining patient safety.
Join us for this interactive workshop where you’ll learn the ins and outs of your annual CPD obligations.
You will learn: How develop your learning plan each year; How you identify your learning needs and objectives; How to record your CPD activities; An understanding of reflective practice; What to do if you get audited.

Friday 20 September, 9am-4pm
Club Blacktown
40 Second Avenue, Blacktown NSW 2145
Hear from a range of speakers, network with colleagues and share experiences across the aged care sector.
For RNs, ENs and AINs in residential, community and hospital aged care settings, across private and public sectors, or anyone with an interest in the aged care sector in NSW.
PROGRAM:
• Keeping on the weight – Preventing weight loss in older people and enhancing quality of life
• Engaging older people in service delivery and navigating complaints
• Sexuality and Ageing with Dementia
Lunch and refreshments are provided and there will be time throughout the day to network with colleagues. REGISTER NOW


• Why Work Health and Safety Laws Work for Members: Four fundamentals on what WHS laws mean for members Program subject to change
Cost: Members $60 / Non-members $120
Thursday 17 October, 9am-3pm
The Shellharbour Club
Cnr Wattle and Shellharbour Roads, Shellharbour NSW 2529
Older people with multiple co-morbidities are at greater risk of rapid deterioration resulting in ‘unexpected death’. The Serious Incident Management Scheme (SIRS) has identified ‘Neglect’ and ‘Unexpected death’ as reportable incidents to the Commission. This places us and our organisation at risk, but mostly highlights the importance of early detection and response to a deteriorating older person.
This workshop is targeted to Nurses and and Managers in Residential Aged Care and Community Care.

Cost: Members $95 / Non-members $190 REGISTER NOW 5 CPD
Do I have professional obligations to escalate concerns about workloads and staffing levels or skill mix?
As nurses and midwives, we must comply with the Nursing and Midwifery Board of Australia’s (NMBA’s) professional standards, which outline the practice and behaviour expected of nurses and midwives. The NMBA professional practice frameworks include the codes of conduct, standards for practice, the decision-making framework, and the codes of ethics.
Professional and safe practice is at the heart of our professional obligations. We all have a professional obligation to evaluate our practice environment and to take appropriate action to address the factors that compromise care.
Codes and standards require that nurses and midwives take action if they believe staffing levels and/or skill mix is inadequate for them to be able to provide safe and professional care. This obligation to act applies to all nurses and midwives. It includes those working in a direct or non-clinical relationship with patients or clients, working in management, administration, education, research, advisory, regulatory, policy development roles, or other roles that impact on safe, effective delivery of services.
The Association’s professional team answer your questions about professional issues, your rights and responsibilities.
Could I “lose my registration” for participating in certain types of industrial action?
The NMBA or a tribunal may suspend a nurse or midwife as a form of immediate action in the public interest, if it believes the nurse or midwife presents a serious and immediate risk to public and that a suspension is the proportionate way to address that risk until the matter has been resolved.
It is very unlikely that participating in industrial action that is focused on improving patient safety would be viewed as a serious and immediate risk to public.
I feel that the industrial action may impact essential care –what is your advice about the ethics of this?
We know that for some time, far too many nurses and midwives in NSW have been enduring workloads that make it impossible for them to provide care that is person-centred and evidence-based. There are simply not enough staff to attend to every patient relying on us.
The overarching principle of industrial action is to draw attention to the campaign and to highlight how valuable nurses and midwives are to the NSW health system. One form of industrial action is work bans. These are typically specific to the work environment and are typically not related to direct patient care. Examples of work bans might include not touching linen bags, or not cleaning beds. When undertaking these bans, the message members are trying to send is ‘Given the unsafe staffing levels, we are focusing on nursing and midwifery care and prioritising more urgent clinical issues.’
We understand that making the decision to be active in an industrial campaign is easy for some and not so easy for others. The question for all members is whether it is more ethical to allow the status quo, or to act to change the status quo. If we choose to act, we should always do so in a way that ensures life-preserving care is maintained.


The NSWNMA is committed to protecting the interests of nurses and midwives by purchasing a range of insurances to cover members.
Journey Accident Insurance
provides cover for members who are injured as a result of an accident while travelling between their home and their regular place of employment.
Professional Indemnity Insurance*
provides legal representation and protection for members when required.
Make sure your membership remains financial at all times in order to access the insurance and other benefits provided by the NSWNMA.


Roz Norman was an outstanding activist, branch official and Councillor of the NSWNMA and ANMF. In honour of her outstanding contributions, the Roz Norman Scholarship was created to further humanitarian, social or community causes. The scholarship covers fees for an approved course promoting activism and the development of campaigning skills or public advocacy, including ongoing financial support for reasonable costs associated with campaigning for a period of one year, up to a maximum of $5,000.
NSWNMA Branch Officials or highly active members who can demonstrate leadership qualities are encouraged to apply. Successful recipients are required to report back to Committee of Delegates (COD) at the end of the scholarship period.

Did you know, if you’re going on parental leave, paid or unpaid, we’ll waive your Association fees until you return to work? You’ll still be entitled to access advice and receive The Lamp. Contact the Association and let us know when you plan to take parental leave so we can set up your waiver. Call 1300 367 962 or email gensec@nswnma.asn.au www.nswnma.asn.au
COVID exposed the risks. Now the International Labour Organization (ILO) is responding with the world’s first international convention on biological hazards.
The NSWNMA argued at the ILO’s conference in June that the COVID pandemic demonstrated that workers need the highest level of protection in the face of an unknown hazard.
The Association’s workplace health and safety expert, Veronica Black, attended the conference as a member of the Standard-Setting Committee on Biological Hazards.
“We’ve seen with COVID that where there isn’t any scientific evidence yet for new and emerging diseases, the highest level of protection must be afforded to people exposed to those hazards until we’ve learnt more about the nature of transmission,” says Veronica.
“When COVID emerged, we realised that many measures you would expect to be in place in the health system to protect workers were either inadequate or did not exist.
‘When COVID emerged, we realised that many measures you would expect to be in place in the health system to protect workers were either inadequate or did not exist.’
“In Australia, our WHS legislation is very broad. It requires employers to ensure that workers are safe at work. However, there is nothing in the existing WHS legal frameworks specific to biological hazards or that sets out the responsibilities of employers and governments to ensure that workers are safe.”

Without clearly codified rights and responsibilities at the outbreak of COVID, the NSWNMA had to work hard to lobby the government and large employers. The Association fought for improvements in PPE supplies, the first FIT testing for nurses, and for income support for workers. We also supported local workplace representatives to raise issues and concerns with management.
“An international convention would form the foundation for law and practice on managing biological hazards in workplaces for countries around the world,” said Veronica.
“Any country that ratifies such a convention will have to introduce strict measures to protect workers in events such as future pandemics and other biological hazards at work.”
The ILO tripartite standing-setting committee includes workers, employers and government
representatives, and Veronica is pleased to report several wins for workers in the committee’s final document. These include a broad definition of what constitutes a biological hazard, a right to be consulted and the right to refuse work, and a definition of health that includes mental health and wellbeing.
“An important lesson of COVIDbefore vaccines were developed and when people were dying around the world, and when our members had to go to work without necessary PPE - is that we need a broad understanding of biological hazards to include both people’s physical and mental wellbeing,” said Veronica.
The committee will conclude developing the convention document at the next ILO conference in June 2025. A two-thirds majority of delegates is needed to approve the document. The next steps will be for countries to ratify and implement the new convention. n
Have you recently moved house? changed jobs or classification? updated your email?





Update your details using our online portal during 1 April 2024 - 30 March 2025 and you will automatically be entered in the draw to win.
We are giving away two gift card bundles, each prize valued at $350.
Winner may choose one gift card valued at $350 or a selection* of gift cards to the value of $350.




1 Scan or go to nswnma.info/mc
2 Update your details
3 Go into the draw to WIN one of two gift card bundles
* Up to a maximum of three different gift cards, to the total value of $350 per prize. **Winner must be a financial member of the NSWNMA. The Association will contact winners, ascertaining preferred gift cards. Gift cards are subject to availability and supplier t&c’s apply.
Keeping your membership details up to date is very important. If you’re a dualqualified nurse/midwife, you can now update your role at nswnma.info/mc
Several measures came into play on 1 July that will alleviate the cost-of-living crisis for Australian working families.
A rise in the minimum wage, tax cuts, the energy relief rebate, an increase in employer super contributions and an increase in paid parental leave will significantly boost take-home pay and improve workers’ personal finances, says the ACTU.
These initiatives from the Federal Government came into play on 1 July.
The 3.75 per cent rise in minimum wages started from the first full pay period after 1 July.
‘Finally, working people will be getting ahead again.’
ACTU Secretary Sally McManus
The government’s cost-of-living tax cuts also started from this date, providing every Australian taxpayer with a tax cut. A person on average annual earnings of $72,753 got a $1,498 annual tax cut, or an extra $28 in their weekly take-home pay packet.
The Federal Government’s $300 energy relief rebate also started to flow to households in four $75 quarterly credits.
Employer super contributions increased from 11 per cent to 11.5 per cent, under superannuation guarantee increases that unions have long campaigned for.
The Super Members Council found that the superannuation guarantee increase would deliver a 30-year-old a projected $17,570 more at retirement.
Paid parental leave also increased to 22 weeks, up from 20 weeks, from 1 July.
“July is a great month for working people after years of being hit with cost-of-living pressures made worse by big business price gouging. Finally, working people will be getting ahead again,” said ACTU Secretary Sally McManus.


After more than 50 days of protected industrial action, Victorian nurses and midwives won a pay deal that will help retain and recruit the staff needed to rebuild the public health system.
The ANMF (Victoria Branch) initially rejected a government offer of 12.5 per cent, but nurses and midwives voted to accept a revised offer that will see them get a 28.4 per cent increase by November 2027 in all classifications.
There will be two pay rises per year:
• In 2024 increases will total 5 per cent
• In 2025 increases will total 4.22 per cent
• In 2026 increases will total 4.09 per cent
• In 2027 increases will total 12.72 per cent.
A graduate nurse/midwife earning a current weekly base rate of $1298.60, will earn $1667.60 by November 2027. A Grade 2 Year 7 will rise from $1762.70 to $2263.40.
There were also a number of improved conditions, including:
• improved night-shift penalties for permanent nurses and midwives
• improved on-call and recall allowances
• a 92 per cent increase to the qualifications allowance by the end of the four-year agreement
• a right-to-disconnect clause.
NSWNMA General Secretary Shaye Candish congratulated our Victoria colleagues on a significant achievement.
“Even though Victoria’s budget is in the red, the government has still found a way to acknowledge the value of nurses and midwives,” she said.
‘Even though Victoria’s budget is in the red, the government has still found a way to acknowledge the value of nurses and midwives.’
Shaye Candish, NSWNMA General Secretary
The NSW Select Committee on Birth Trauma has released a report that includes 43 recommendations to overhaul maternity care in the state.
The recommendations focus on investing and expanding midwifery-led continuity-of-care models and addressing staffing shortages through improvements to pay and conditions for midwives.
The inquiry received a record 4000 submissions and held six hearings across the state.
NSWNMA Assistant General Secretary Michael Whaites said the inquiry had shone a light on areas of midwifery and maternity services that have been ignored for too long.
“We hope this is the start of positive change that will benefit women on their maternity journey, and ensure this incredibly rewarding profession has the structures, resources and support systems to deliver safe, woman-centred care.
“We are pleased to see the inquiry supports our view of addressing midwife shortages with competitive pay and working conditions, and a staffing model with the appropriate skill-mix.
“It’s encouraging to see the committee recognises the impact of birth trauma on midwives too, by recommending debriefing and psychological support for maternity clinicians following their exposure to a traumatic birth.
“We know birth trauma rates can, and must, be reduced, and we’ll continue to advocate for universal access to midwifery-led continuity of care.”
A survey of 8000 mothers by the University of Western Sydney found one in three experienced birth trauma in Australia.

‘We hope this is the start of positive change that will benefit women on their maternity journey.’
— NSWNMA Assistant General Secretary Michael Whaites
Clinical epidemiologists, using baseline data from previous conflicts, calculate that the death toll in Gaza will be drastically higher than the currently known figures.
Over the last nine months the Israeli army has killed about 38,000 people in Gaza, according to Gaza’s health ministry. These numbers have been acknowledged by the United Nations, the World Health Organization and even the Israeli intelligence services.
About another 10,000 are believed to be dead underneath the rubble that have not been counted among the fatalities.
But war doesn’t just kill people through direct violence. Epidemiologists have also begun to count the fatalities that come from the spread of disease caused by malnutrition, lack of unsanitary conditions and the collapse of healthcare systems.
Three prominent epidemiologists, in a letter to the Lancet, point out that in recent conflicts “such indirect deaths range from three to 15 times the number of direct deaths.
They wrote: “Applying a conservative estimate of four indirect deaths per one direct death to the 37,396 deaths reported, it is not implausible to estimate that up to 186,000 or even more deaths could be attributable to the current conflict in Gaza. Using the 2022 Gaza Strip population estimate of 2,375, 259, this would translate to 7.9 per cent of the total population of the Gaza Strip.”
‘In recent conflicts indirect deaths range from three to 15 times the number of direct deaths.’

The Fijian health system and workforce were devastated by COVID-19, but the fierce determination of nurses and midwives could lead to its renaissance.
COVID-19 smashed the Fijian health care system. In 2021, 26 per cent of Fijian nurses quit their jobs. The situation worsened in the following two years. Nurses and midwives were demoralised and exhausted as their colleagues left in droves.
But there has been a revival. Spearheaded by the Fiji Nursing Association (FNA), who have won stunning pay increases, this should attract nurses back to the healthcare system.
During their pay campaign the FNA mobilised nurses, which led to a 70 per cent vote of the total workforce in favour of industrial action.
The campaign led to a stunning outcome, with differing classifications receiving 16.67 per cent, 28.21 per cent, 33.3 per cent and 41.3 per cent pay increases for nurses.
The General Secretary of the FNA, Filomena Talawadua, attributed the win to “patience, dialogue, and providing evidence on the ground”.
Fijian nurses still face many challenges. The nation is composed of many small, remote islands, and is highly impacted by global warming. Nurses are on the frontline of the increasingly deadly cyclones that impact their communities’ health.
The pandemic was also used to push through controversial privatisations (supported by the Australian Government’s aid program), which undermined the workforce and the public health system.
‘The pay win was built on ‘patience, dialogue, and providing evidence on the ground.’
— General Secretary of the FNA, Filomena Talawadua
One in four Australian employees – 2.6 million workers –will benefit from this year’s minimum wage increase. The increase will raise the minimum weekly wage to $915.90 (up from $882.80). Hourly wages will increase to $24.10 (from $23.23), the Fair Work Commission said.
While jobs in the Retail, Accommodation and Food sectors fell in the year to December, jobs in the Healthcare sector rose 9.2 per cent and hours worked jumped by the same amount.
The ACTU said it was disappointed the commission did not act immediately to provide interim pay rises to workers in key feminised work, but it did welcome the commission’s acknowledgement that workers in feminised industries and occupations have been undervalued.
ACTU Secretary Sally McManus said the pay rise was a win for workers, their families, and the broader Australian economy.
“We welcome the commission again rejecting the employer groups’ argument that modest real wage rises would somehow be unaffordable or would fuel inflation.
“In the last couple of years, workers on minimum and award wages saw historic pay rises, while inflation dropped from 7.8 per cent to now 3.6 per cent. Australians are smart enough to see through the employer groups’ spin, especially when corporate profits have grown nearly three times faster than wages since the pandemic,” she said.
‘We welcome the commission again rejecting the employer groups’ argument that modest real wage rises would somehow be unaffordable or would fuel inflation.’ ACTU Secretary Sally McManus
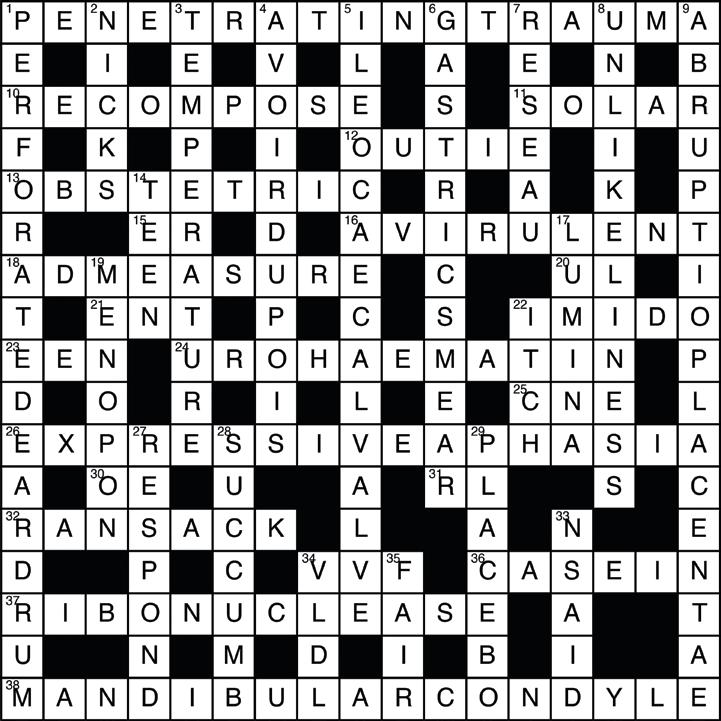
A landmark resolution passed at the World Health Assembly in Geneva emphasises the importance of viewing health spending as a long-term investment rather than a short-term cost.

At the assembly, the Chair of the World Health Organization Council on the Economics of Health for All, Prof. Mariana Mazzucato, highlighted the need for collaboration between ministers of health, industry, and finance in designing economies that prioritise the wellbeing of their citizens.
She said this is of particular importance as austerity has returned to many countries and threatens health budgets, while the demands continue to rise (for example, through increased risks of pandemics due to climate change).
Investments in health are, in fact, long-term drivers of growth, Prof. Mazzucato said.
Attacks on healthcare facilities surged by 25 per cent last year, while fatal attacks on healthcare workers doubled. Attacks on health workers and facilities in conflict zones jumped in 2023 to the highest level since records began 11 years ago, with nearly half attributed to state forces, according to a new report.
The Safeguarding Health in Conflict Coalition reported 2562 incidents of violence or obstructions including arrests, killings and kidnappings of healthcare workers and strikes across hospitals in 30 conflicts.
That is up by about a quarter compared with 2022.
More than 480 health workers were killed, almost double the number reported the previous year.
The toll included doctors, nurses, ambulance drivers, pharmacists, lab technicians, paramedics, and psychologists. The total is likely an undercount, as data collection on violence is impeded by insecurity, communication blockages, and the reluctance of parties to share data on violence.
“A modern industrial strategy should focus on bold social and environmental missions, which will then catalyse investment, innovation, and growth across relevant segments of the economy,” she said.
But she warned that unless innovation is governed for the common good, the benefits may not be widely shared.
“Governments should set stronger conditions for those seeking public support for health innovation, not least by requiring that the resulting health products and services be made widely available and affordable,” she said.
“Rather than pursuing economic growth regardless of the consequences, we should orient economic activity towards the goals of human health and wellbeing, and towards ensuring a healthy and sustainable environment.”
‘We should orient economic activity towards the goals of human health and wellbeing, and towards ensuring a healthy and sustainable environment.’
Prof. Mariana Mazzucato, Chair, WHO Council on the Economics of Health for All
The report details that both government forces and non-state armed groups bombed, occupied, raided and vandalised health facilities throughout the year.
Health facilities were increasingly occupied or repurposed for military use, in violation of humanitarian law.
The most severe impacts of these attacks involved the virtual collapse of health systems, as in Gaza, where most hospitals have been destroyed and closed, access to essential supplies is blocked, and infrastructure damaged. This was also true in Sudan, Burkina Faso, Central African Republic, and Tigray in Ethiopia.
‘Government forces and non-state armed groups bombed, occupied, raided, and vandalised health facilities throughout the year. ’
Safeguarding Health in Conflict Coalition
More Offers + Bigger Discounts =
As a NSWNMA member, you have access to:
An expanded range of discounts on eGift cards at over 100 retailers including groceries and fuel
Great discounts on travel including hire cars and hotels at international destinations
Discounts on tax preparation and financial planning
Savings on tech, electronics, whitegoods and more!





The trustees of the Lions Nurses’ Scholarship Foundation invite applications for scholarships. Nurses eligible for these scholarships must be resident and employed within the State of NSW or ACT.
You must currently be registered with the Nursing and Midwifery Board of Australia and working within the nursing profession in NSW or the ACT, and must have a minimum of three years’ experience in the nursing profession –the last 12 months of which must have been spent in NSW or the ACT.
Details of eligibility and the scholarships available (which include study projects either within Australia or overseas), and application forms are available from: www.nswnma.asn.au/education
Administration Liaison, Lions Nurses’
Foundation 50 O’Dea Avenue Waterloo NSW 2017 or contact Matt West on 1300 367 962 or education@nswnma.asn.au








Peer-led support and counselling
For nurses, midwives and our students
Safe, confidential, free service




Good mental health involves managing your thoughts, feelings and behaviours.
Incorporating self-care strategies into your everyday life can benefit all aspects of your health.
Self-care strategies:
• get enough sleep
• make sure you have regular physical activity and exercise
• maintain a well-balanced diet
• keep stress levels at a functional level
• practice mindfulness
• ensure you have some ‘down time’ and relaxation, and
• keep socially connected with your community, colleagues and friends.
It can also be helpful to be mindful of your negative coping strategies. These could include turning to addictive behaviours like increasing alcohol or drug use, gambling or overeating — behaviours that can vary from person to person.
Here is a breathing relaxation exercise you can try:
• sit (or lie) down and close your eyes, or let your eyes rest on an object in the room
• inhale deeply and slowly, while counting to four
• exhale slowly, counting to four
• inhale deeply and slowly again as you count to four, then hold your breath for two seconds
• exhale slowly, counting to four
• repeat inhale and exhale cycle for several minutes, and relax consciously
• as you inhale, imagine yourself in a safe, comfortable, beautiful place, continue to breathe as you
hold the image in your mind, feel how relaxed you are, and
• when you are ready, become aware of yourself in the room once again, wriggle your fingers and toes, and slowly open your eyes.
When you feel stressed, your muscles might feel tense making it hard to relax. Try this progressive muscle relaxation technique to get your body to relax:
• rest your arms by your side, and close your eyes
• inhale as you count to four, and exhale as you count to four, until your mind is quiet, and you feel calm
• as you continue to breathe slowly, tense each muscle group for ten seconds (don't tense so much that you feel cramp or pain), then relax for ten seconds, starting with your:
» feet: curl your toes, then relax
» calves: tighten your calf muscles, then relax
» thighs: tighten your thigh muscles, then relax
» buttocks: tighten your buttocks, then relax
» stomach: pull your tummy in, then relax
» chest: breathe in deeply, then breathe out and relax
» hands: clench your hands into fists, then relax
» lower arms: bend your hands up at the wrists, then relax
» upper arms: bend your arms up at the elbow, then relax
» shoulders: lift your shoulders up, then relax
» neck: roll your neck gently to the left, then the right, then forward, and relax
» jaw: clench your teeth, then relax
» forehead and scalp: close your eyes tightly, then relax, and
» eyes: raise your eyebrows, then relax
• continue slow, controlled breathing for five more minutes, and enjoy the feeling of relaxation, and
• when you're ready, have a good stretch and bring your awareness back into the room.

Nominations for the 2025 HESTA Australian Nursing & Midwifery Awards open on 24 August, with total prize money of $30,000.
As the first nurse practitioner to specialise in gynaecology in Australia, Shannon Philp has pioneered programs that help women with gynaecological cancers recover quickly after surgery. Her work at Sydney’s Chris O’Brien Lifehouse was recognised in 2021 when she was awarded Nurse of the Year at the HESTA Australian Nursing & Midwifery Awards.
Nurse and Midwife Support provides free and confidential support 24/7, to nurses, midwives and students
Australia wide. If you would like to speak to someone, call 1800 667 877, or you can request support via email.
“The award really motivated me to do more and think of new ways to make a difference for my patients,” Shannon said. “I would definitely encourage people to nominate someone who they think is doing a great job and is the leading the way in their area or speciality,” she said. Judges declared Shannon the Nurse of the Year for the programs she has developed that improve post-surgery recovery
for women and provide support on the physical, psychological, emotional and social impacts of gynaecological cancers, including through sexual intimacy counselling.
The prize money she received allowed her to attend conferences and develop her research networks.
“I am now involved in important projects and research,” said Shannon.
The HESTA Australian Nursing & Midwifery Awards cover several categories:
• Nurse of the Year, and Midwife of the Year (two award categories)
• Outstanding Organisation Employers, patients, colleagues, nurses and midwives can nominate themselves or a special individual or team, who has made a real difference to the lives of patients or to the quality of a service.
More information: www.hesta.com.au/awards/ nursing-midwifery-awards

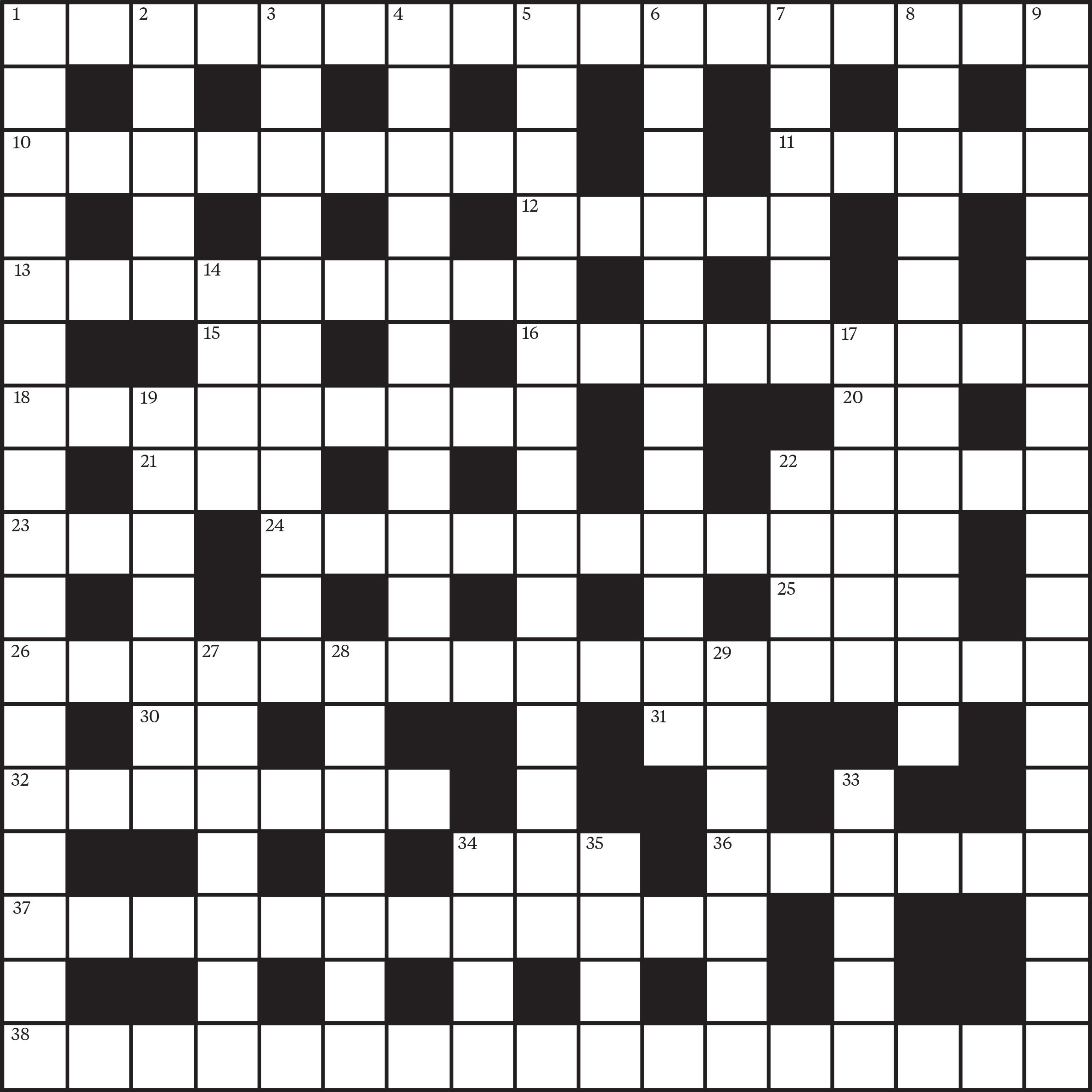
ACROSS
1. Injury caused by an object entering the body (11.6)
10. Create anew, rearrange (9)
11. Relating to the sun (5)
12. A protruding navel (5)
13. Related to childbirth and pregnancy (9)
15. Symbol for erbium (2)
16. Not causing disease (9)
18. Apportion (9)
20. Upper Limb (1.1)
21. Otorhinolaryngology (1.1.1)
22. Chemical group containing nitrogen (5)
23. Exclusion enteral nutrition (1.1.1)
24. Urine pigment compound (11)
25. Nurse trainer in a medical setting (1.1.1)
26. Difficulty in expressing thoughts through speech or writing (10.7)
30. Symbol for oersted (2)
31. Reinforcement Learning (1.1)
32. Search thoroughly and messily (7)
34. Vesicovaginal Fistula (1.1.1)
36. A milk protein (6)
37. Enzyme that breaks down RNA (12)
38. Part of the jaw joint (10.7)
DOWN
1. Condition involving a hole in the tympanic membrane (10.7)
2. Small cuts (5)
3. Measure of heat or cold (11)
4. A system of weights (11)
5. Digestive passage regulator (15)
6. Medical test involving stomach cell examination(12)
7. Network of lines (6)
8. State of being improbable (12)
9. Premature separation of the placenta from the uterine wall (8.9)
14. Adolescent (4)
17. Spaces within an arteries, veins, intestines, or tubes (6)
19. Parasitic louse found on birds (7)
22. An irritating skin sensation (4)
27. To react to a stimulus or to a treatment (7)
28. Yield, give in (7)
29. Inert substance given as a medicine for its suggestive effect (7)
33. Aspirin and ibuprofen (1.1.1.1.1)
34. Type of lipoprotein involved in transporting triglycerides (1.1.1.1)
35. Just (4)
Access to online CPD
FREE for NSWNMA members and student members
Hundreds of hours of FREE CPD online
Meeting your Continuing Professional Development (CPD) obligations is now even easier with this great benefit for NSWNMA members. As a financial member you have access to over 200 CPD modules – all part of your Association membership.
FREE access to over 200 CPD modules online
Highly visual and interactive modules you can do at your own pace
New modules added regularly
Your own personalised ePortfolio and CPD tracker so you can provide evidence to the Nursing and Midwifery Board of Australia (NMBA) of participation in CPD annually.