










Welcome to Issue 45 of The Meducator! The healthcare field is rapidly evolving, with new discoveries and advancements emerging everyday. This embodies a modern-day Renaissance—an era characterized by profound shifts in social attitudes and scientific innovation. Henin Ye captures these principles in her illustration of Issue 45’s cover, inspired by Michaelangelo’s iconic Renaissance masterpiece, The Creation of Adam. Likewise, we extend a hand in joining us in exploring revolutionary connections and transformations unfolding in the medical field today, through our winter issue.
Editors Dominic Gangemi and Ria Patel begin Issue 45 by describing novel health developments worldwide, including the first FDA-approved Chikungunya vaccination in Brazil and Canada’s research on modelling pexophagy pathways to treat neurodegenerative diseases. We continue The Meducator’s collaboration with the International Women and Children’s Health Conference by featuring abstracts from Brittney Davy on Black women’s health and Deepikaa Jeevanthan on the vaginal microbiome. Through extensive literature review, Florence Deng and colleagues describe the pathophysiology and treatment landscape of Crohn’s Disease. In a Critical Review, Morgan Puusaari and colleagues describe a novel α-synuclein seed amplification assay for early detection of Parkinson’s disease.
In this issue we are excited to feature articles that explore health from a multifaceted perspective. In MeduAmplify Local, Parth Arora and colleagues characterize Hamilton’s opioid epidemic and potential response strategies. In another MeduAmplify, Aditya Misra and colleagues discuss the ‘orange jumpsuit’ stigma by exploring the health of incarcerated peoples.
We take tremendous pride in our journal’s emphasis on diversity in healthcare. In a MeduAmplify, Veronica Grignano and colleagues explore the evolution of art in medicine, highlighting the underrepresentation of marginalized bodies in anatomical illustrations. Meanwhile, artists Arim Yoo and Elaine Wang present “Echoes of Representation,” a centrefold illustration depicting how predominantly white representation in medical textbooks affects clinical practice.
We extend our heartfelt appreciation to our 95 talented staff, executive members, faculty reviewers, and the McMaster community for their invaluable partnership throughout the 45th publication cycle. Finally, we offer our sincerest appreciation to you, our reader, for your continued support of our publication. We feel privileged to have served the McMaster community. We wholeheartedly welcome Florence Deng and Anna McCracken as the Editors-in-Chief for the upcoming academic year. We believe their potential is unlimited and cannot wait to see them uphold and advance the Meducator’s legacy.

Improved cellular recycling could benefit patients with neurodegenerative conditions
CANADA | January 2024
Researchers at SickKids Hospital are discovering new ways to treat neurodegenerative conditions. Zellweger Spectrum Disorders (ZSDs) are a set of rare inherited neurodegenerative diseases characterized by dysfunctional peroxisomes: organelles commonly used in lipid metabolism. the autophagic degradation of peroxisomes, was analysed to model similar selective autophagy pathways. showed that similar ‘recycling pathways’ could not effectively break down other cellular waste.2 Their findings extended to in vivo cell models of ZSD and other neurodegenerative conditions, like Parkinson’s Disease and Huntington’s Disease.2 Hence, therapeutically enabling a cell to better recycle its own components could reduce the accumulation of damaged cellular material.2,3
North Carolina’s Duke University is now home to the first ever heart valve transplant that has grown with its neonate recipient for one year.4 Dr. Joseph Turek sought to address the issue of recurrent implant exchanges for children born with irreparable heart valve dysfunction as their heart grows with age.5 A partial heart transplant from a neonate donor provides the ideal treatment since the patient now requires fewer immunosuppressants and further surgical intervention is minimized. door to more life-saving partial heart transplants, tissue engineering of heart valves, and the potential for domino transplants where a single heart can save multiple patients.
Chikungunya vaccination could help millions in South America
BRAZIL | November 2023
Originating from Tanzania in 1953, mosquito-borne chikungunya virus—“disease that bends up the joints” in Swahili—is characterised by severe joint pain. tropical disease has spread across Africa, Asia and, notably, South America, which faces an ongoing epidemic with an estimated total of 3.7 million cases. the form of the first FDA-approved chikungunya vaccine, called Ixchiq, developed by Valneva. shown that 99% of people develop long lasting antibodies after a single shot.11 Discussion around vaccine rollout, prioritising South Americans or tourists, is ongoing.




TheFightingTemeraire, 1838 (England)
Untitled, 1999 (Uganda)

DOMINIC GANGEMI 1 & RIA PATEL 1
Bachelor of Health Sciences (Honours), Class of 2027, McMaster University & CHRISTINA TAM 3
Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
A groundbreaking study led by Genomics England has shown that whole-genome sequencing (WGS) could be the key to more precise and personalised cancer treatments.12 The Cancer Programme of the 100,000 Genomes Project, initially announced in 2012, analysed WGS data from 13,880 solid tumours across 33 types of cancers.12,13 From this data, researchers found that over 90% of tumours in the brain, and over 50% in the lungs or colon, exhibited genetic alterations that would impact patient treatment.14 Furthermore, 13% of 1,617 sequenced sarcomas expressed large structural variants.12 These discoveries help highlight precision oncology as a promising avenue for cancer treatment.

GallopingHorse, 1953 (China)
Prostaglandin degradation enzyme found to be potential therapeutic target for ischemic stroke
Researchers in China are paving the way for a new treatment for ischaemic stroke. Where standard treatments seek to catalyze plasminogen into plasmin to dissolve blood clots, this research targets an enzyme responsible for the degradation 15‐Hydroxyprostaglandin dehydrogenase (15‐PGDH) is the degrading enzyme of prostaglandin E2 (PGE2), which has been shown to be important for the control of When inhibited, new research shows the activated PGE2/EP4 axis transcriptionally upregulates vGPX4, a protein responsible for regulating cell death through ferroptosis.16,17 Therefore, inhibition of 15-PGDH alleviates ischemic stroke and, consequently, presents a promising therapeutic target for the near future.16
Novel model for rheumatic heart disease treatment
Rheumatic heart disease (RHD), a condition caused by chronic heart valve damage following rheumatic fever, is the leading cause of heart disease for youth in Uganda.20 To streamline RHD screening and recurrent antibiotic admission, the Ugandan Ministry of Health is advancing the "Accelerating Delivery of Rheumatic Heart Disease Preventive Interventions in Uganda" It offers free RHD screening in schools, health centres, and community events from nurses and clinical officers who received training from experts at the Uganda Heart Institute.21 To improve secondary treatment times, Uganda moved their existing RHD registry from a centralised location to the Uganda’s exemplary work sets effective standards for global RHD treatment and situational public health action.
A collaboration with the 2023-2024 Women’s and Children’s Health Conference at McMaster University
ARTISTS: MISHAL HOSSAIN 1 & ARIM YOO 21Bachelor of Health Sciences (Honours), Class of 2025, McMaster University
2Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
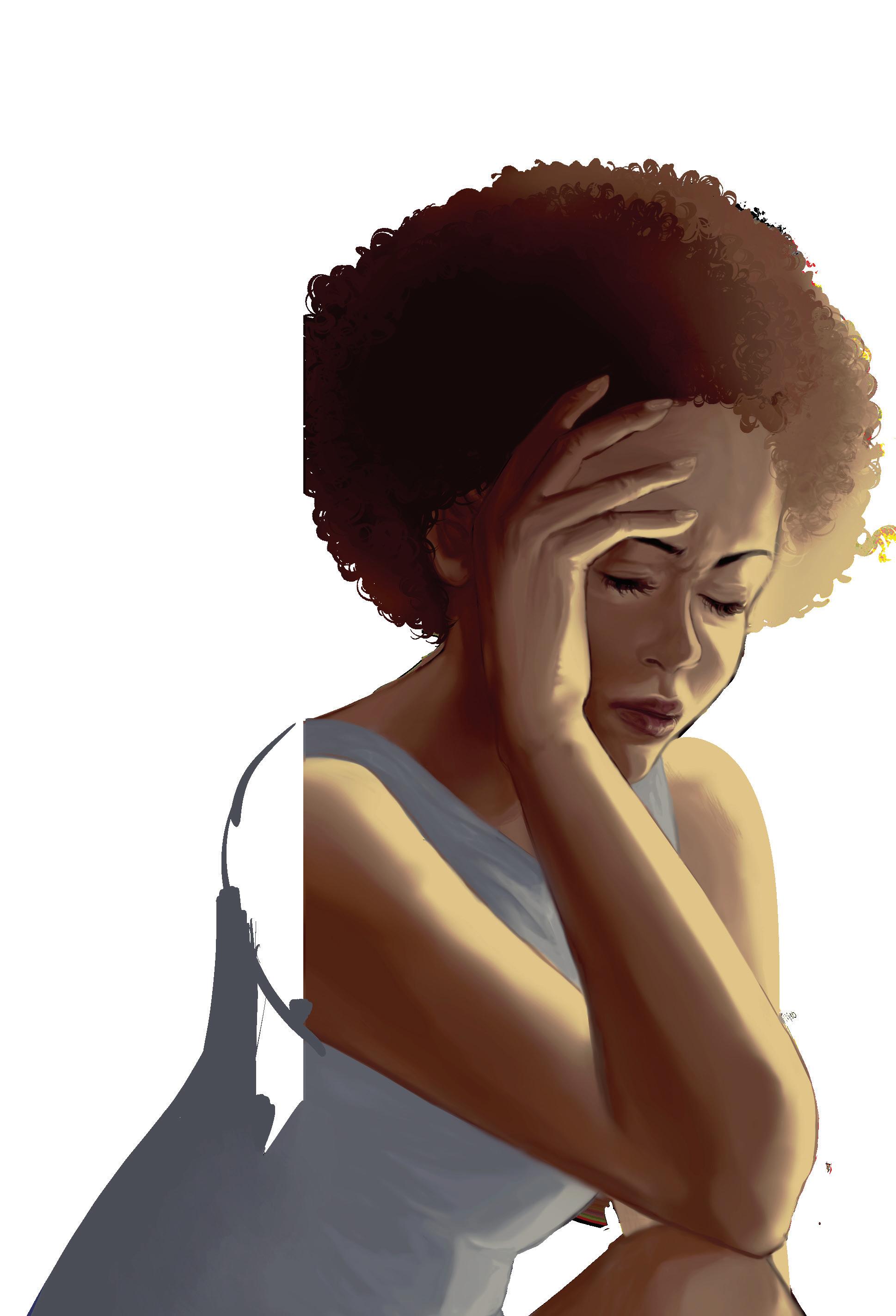
Black womens’ health matters: A literature review of the impact of racial stereotypical narratives on Black womenAUTHOR: BRITTANY DAVY (BCBA, MA ADS) 1 1Department of Health, Aging & Society, McMaster University
Black women have been disproportionately affected by negative stereotypical narratives and complex representations of their community. The “strong, Black woman” stereotype and many others which are contextually similar possess diverse meanings dependent on social context and lived experience. Studies exploring the implications of normative and stereotypical narratives of Black women on their health have revealed differences in health outcomes dependent on experiences and perception of these stereotypes.
This literature review explores a range of popular meanings attributed to similar racial stereotypes. The researcher, an Afro-Caribbean Black doctoral student in Ontario, examined published research in North America to highlight patterns in the positive and negative mental health experiences of Black women who have been exposed to common racial and gender-focused stereotypical narratives. Studies included in this review discussed the experiences of women that identify as Black members of African descendent populations including but not limited to African American and Afro-Caribbean, from various age groups as early as firstyear college students to women approaching old age (approximately 60 years old).
Researchers that have previously interviewed Black women within the North American context found that there were several theses associated with stereotypical narratives specifically applied to Black women: strong/assertive, independent, educated, hardworking/ambitious, caring, and self-confidence. Several Black women expressed their beliefs that internalizing and perpetuating strong, Black women traits has been a source of empowerment and promotes self-sufficient and resilient behaviour in this marginalized population. Comparably, these narratives can be particularly debilitating and oppressive as Black women may feel objected to altering their behaviour to fit within the boundaries ascribed by the stereotype. Other Black women have displayed symptoms commonly associated with depression, which have been correlated with their exposure to these stereotypes which have harmful effects on their physical and psychological health. Predominant stereotypes and lifestyle behaviours contribute to experiences of threatened mental health as society constantly reproduces unattainable images of an ideal.
Further investigation by the researcher is expected to reveal differentiated but interrelated results between the endorsement of Black women centered narratives and health experiences throughout the life course. This research is crucial as much of the published literature is conducted within the United States of America and the importance of the deep-rooted slavery history, culture, and covert racist treatment of Black people today may hinder the generalizability of the findings to the Canadian context. While Black women remain disadvantaged within Canada, literature regarding the impact of these stereotypical narratives on Black women within the Canadian context is underrepresented within published research.




AUTHORS: DEEPIKAA JEEVANANTHAN 1,2 , AISHA NAZLI (MSc, MPhil, PhD) 1,2 , & CHARU KAUSHIC (MSc, PhD) 1,2
1Department of Medicine, McMaster University 2McMaster Immunology Research Center, Michael G. DeGroote Center for Learning and Discovery, McMaster University
The prevalence of sexually transmitted infections (STIs) remains a major issue worldwide. The composition of the vaginal microbiome (VMB) has a crucial role in maintaining reproductive health. A eubiotic VMB is colonized by Lactobacillus crispatus and is considered protective against STIs. A dysbiotic VMB is populated by anaerobic species such as Gardnerella vaginalis, which are associated with increased susceptibility to STIs and often aggregate to form biofilms. With antibiotic resistance presenting an ever-growing concern, it is important to examine biofilm formation – one of the resistance mechanisms developed by bacteria to overcome clinical treatments. Biofilms are communities of aggregated bacterial organisms contained within a thick matrix of extracellular polymeric substance (EPS). The physical shield created by the biofilm EPS confers antibiotic resistance by protecting the bacteria and decreasing their response to antibacterial agents. The formation of bacterial biofilms by dysbiotic bacteria in the vagina can thus increase the likelihood of treatment failure and recurrence of vaginal infections. Investigating the important structural components of biofilms can help develop ways to target and disperse these communities, leaving bacteria less resilient and more susceptible to treatment. Extracellular DNA (eDNA) released by bacteria, either actively or through cell lysis, is considered to be an important component of biofilms. eDNA has been shown to be critical in bacterial attachment and aggregation of biofilms on surfaces, especially in the early states of biofilm formation. It also helps maintain the structural stability of the rigid biofilm matrix that protects the bacterial cells within. The role of eDNA in the VMB is not well-researched, but could be a target for disaggregation of biofilms. Determining the role of eDNA in biofilm formation and vaginal health can aid the development of treatments for recurring vaginal infections.
We assessed the timing of DNA release in 4 different bacterial species: dysbiotic bacteria Prevotella bivia and Gardnerella vaginalis, eubiotic bacteria L. crispatus, and an intermediate between dysbiotic and eubiotic state, Lactobacillus iners. The release of eDNA in the stationary-growth phase is indicative of bacterial lysis, while maximal eDNA release in the early exponential-growth phase is associated with active release mechanisms. We found that eDNA release in G. vaginalis only peaked in the early exponential growth phase, which represents active release, rather than bacterial lysis. In contrast, eDNA release in L. crispatus, P. bivia and L. iners peaked in the stationary phase, indicating release of eDNA after bacterial cell lysis. Currently, we are investigating the effects of eubiotic and dysbiotic bacterial eDNA on vaginal epithelial cells by assessing changes in vaginal epithelial barrier integrity, as well as immune factors induced by eDNA in vaginal cells. Preliminary findings have shown that eDNA derived from L. crispatus upregulates anti-inflammatory factors in vaginal epithelial cells, while eDNA from G. vaginalis and L. iners induces upregulation of pro-inflammatory factors. In the future, we will determine whether the eDNA of different bacterial species can modulate the inflammatory response in vaginal epithelial cells against an immune insult. This study will help to understand the role of eDNA in biofilm formation to potentially improve biofilm treatment options for women suffering from recurrent infections.
ARTISTS:
ARIM YOO 1 & ELAINE WANG 2
1Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
2Bachelor of Health Sciences (Honours), Class of 2026, McMaster University

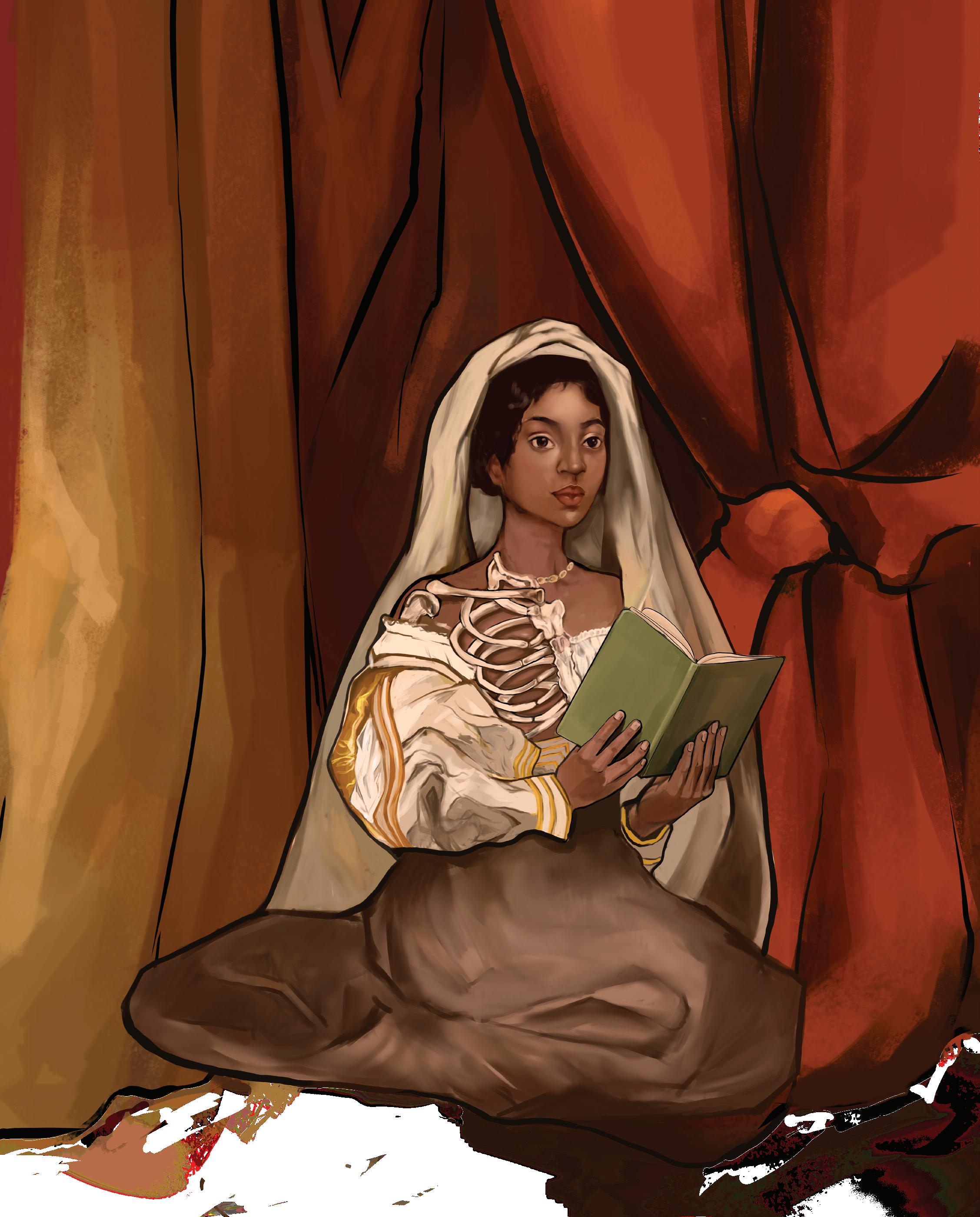
“ECHOES OF REPRESENTATION”
The representation of diverse bodies in medical illustrations has been consistently lacking throughout history. Medical textbooks, posters, and scientific models all tend to depict the white male body as the standard. In contrast, bodies of those who are Black, Indigenous, and People of Colour (BIPOC), fat, or disabled, are significantly underrepresented. In a 2021 study by Massie et al., it was found that just 18% of the medical images from the New England Journal of Medicine depicted non-white skins.1 It is necessary to improve diversity in medical illustrations in order to render medical education of both providers and patients more equitable for the underrepresented populations.

doi: 10.35493/medu.45.08
AUTHORS:
VERONICA GRIGNANO 1, MATTHEW OLEJARZ 2, & DEVLYN SUN 2
1Bachelor of Health Sciences (Honours), Class of 2027, McMaster University
2Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
Across human history, the intersection between the visual arts and human anatomy has revealed an unlikely partnership between scientific accuracy and creative artistry. From historical anatomical sketches to current 3D medical models, the visual representation of the human form has facilitated the advancement of modern medicine throughout the world. This relationship has changed the methods of dissemination of healthcare information, aided in the understanding of anatomy, and led to anatomical accuracy in historical works of art. However, the methods by which artistic and anatomical knowledge have been acquired throughout history were not always ethical. In fact, nonconsenting marginalized populations were often the victims of human cadaver dissections that were later adapted to visual representations. Despite this fact, anatomical illustrations in historical and contemporary scientific texts still exhibit a lack of diversity and clear biases toward a depiction of the white male archetype. An improved understanding of the complex interplay between art, anatomy, and the abuse of marginalized groups in these fields is crucial to foster inclusivity and protect the rights and autonomy of all individuals involved in anatomical art–both in the past and the future.
EARLY DEVELOPMENT OF ART IN ANATOMY: A GLOBAL PERSPECTIVE
Although the Renaissance period is often cited as the era of anatomical revolution, it is important to note that advances in art and anatomy are not limited to this era, nor Western civilization. In fact, the convergence of art and anatomy dates back to over 25,000 years ago, with evidence of anatomical artifacts, sculptures, and drawings found in caves across Western Europe, Africa, Asia and Australia.1
Ancient Egypt
Some of the earliest records that contributed to modern knowledge of human anatomy are credited to the Ancient Egyptians. While their knowledge was crude, Ancient Egyptian sculptures and drawings marked a turning point where the perception of medicine moved away from a simple practice to a highly regarded and skillful craft.1
Persia
A Persian anatomist, Mansur ibn Elyas, is credited with publishing the first illustrations of the human body in its entirety in his manuscript, Tashrih-i Badan-i Insan. The book contained six coloured figures, each detailing a different anatomical system: the skeletal system, the nervous system, the muscular system, the veins and arteries of the cardiovascular system, and the female reproductive
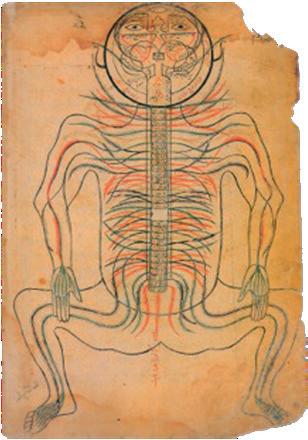

system via a pregnant woman delivering a breech baby.2 The colour illustration of the pregnant uterus is thought to be the first depiction of the gravid uterus. Each illustration was accompanied by detailed descriptions of various systems of the body, including the visual pathway and the development of the embryo.2 Despite some deficits in accuracy, the diagrams in Tashrih-i Badan-i Insan were so significant that they were still used in Persian and Arabic medical manuscripts for more than two generations after their original publication.
Ancient China
Early anatomical illustrations also developed throughout Ancient China. Artist Yan Luozi drew six human anatomical maps, titled Illustrations of Inner Body, that depicted various parts of the human body. Figure 2 displays a drawing made by Yan of the inner body as viewed from the back. This particular illustration correctly identified the existence of various internal organs, despite placing these organs in the wrong locations. Notably, Illustrations of Inner Body accurately depicted the location of the kidneys. Illustrations of Inner Body constitutes one of the earliest attempts at visualizing anatomy, ending the era of “talking without drawings” in China and permanently altering the way of communicating medical information.3

Ancient Greece and Ancient Rome
The Greeks and Romans, too, dominated much of early anatomy. Due to the strong influences of religion, the use of human cadavers was forbidden, and animal dissections became increasingly popular in advancing medical knowledge.1 During this time, theories in the field of anatomy were predominantly governed by physician Claudius Galenus, whose anatomical theories were misinformed. Anatomist Andreas Vesalius took note of these inaccuracies and challenged societal norms by incorporating the dissection of human cadavers into his understanding of anatomy, challenging centuries of medical dogma and encouraging a more empirical approach to medicine and science. These dissections and studies led to the creation of Vesalius’ work, De Humani Corporis Fabrica (Figure 3), published in 1543. His textbook contained
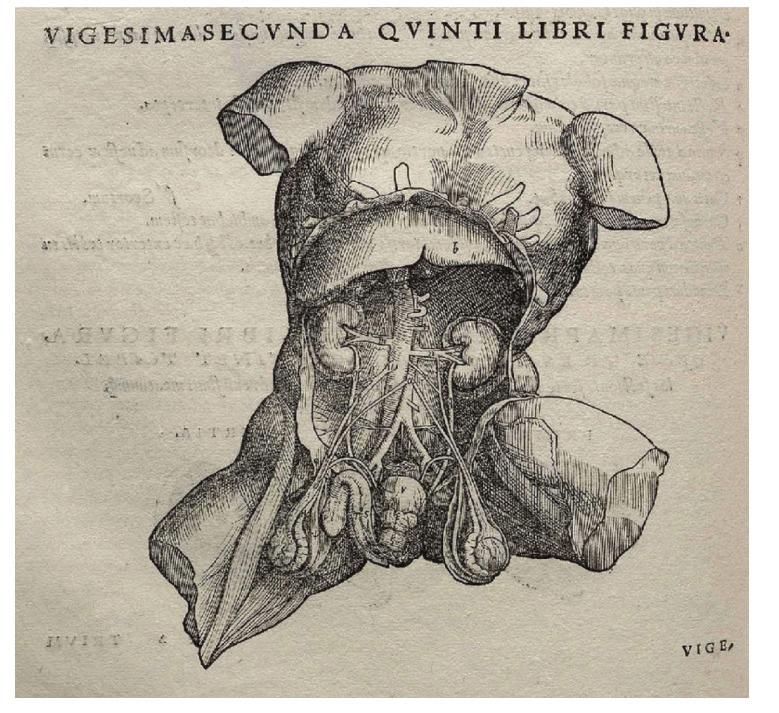
numerous detailed drawings completed by disciples of the great Italian Renaissance painter, Titian. Both a groundbreaking exploration into human anatomy and an astounding artistic work, this textbook revolutionized the understanding of anatomy with didactic text and accompanying imagery.4 The work was comprehensive, covering the full spectrum of human anatomy in unprecedented detail. This allowed for a more nuanced understanding of the human body, facilitating advancements in surgical techniques and medical treatments. The anatomical drawings in particular served as crucial pedagogical tools, aiding in the dissemination of knowledge throughout the medical and artistic communities. This was a significant advancement in medical education and meant that those who might not have direct access to human dissections could still learn about medicine. In addition, the direct observation and dissection methodologies introduced by Vesalius have persisted into modern medical education, emphasizing the importance of experiential learning.
As medical advancements were made, anatomical knowledge permeated artistic communities across the globe. Modern analyses of historical artworks have concluded that ancient artists actually possessed a firm grasp on human anatomy—a fact that is frequently overlooked due to the separation of these fields. The Fasting Buddha sculpture is one such example. Carved by Ancient Indian sculptors of the Gandhara region in the 2nd or 3rd century AD, the statue depicts the fasting, emaciated Buddha seated in a meditative pose (Figure 4).5 The statue was carved with generally correct muscle, neck, bone, and joint anatomy, demonstrating the expansive knowledge that the ancient artists possessed regarding the approximate shape, size, and position of various musculoskeletal features.5 In addition, the sculpture exhibits an understanding of the physiological changes that occur during starvation, evident by the Buddha’s skinny appearance.5 Certain errors were noted, including an extra number of ribs and a segmented sternum.5 However, this statue still demonstrates the undeniable connection between art and medicine—a connection marked by a shared pursuit of understanding the intricacies of the human form. This connection can also be considered symbiotic in nature; anatomists benefit from artistic visual depictions, and artists infuse scientific accuracy into their work based on anatomical knowledge. marked by a shared pursuit of understanding the intricacies of the human form. A symbiotic relationship of sorts; anatomists benefit from artistic visual depictions and artists infuse scientific accuracy into their work based on anatomical knowledge.
Renowned figures such as Leonardo da Vinci and Michelangelo also epitomize this unique relationship between science and art. Da Vinci’s detailed anatomical sketches, like the famed Vitruvian Man, reflect an astute understanding of anatomy that transcends artistic boundaries.6 Similarly, Michelangelo’s meticulous dissections, notably of human cadavers, informed his masterpieces like the Statue of David.7
The visual language developed in eras past became a crucial tool for conveying complex anatomical concepts and dismantling anatomical misconceptions, laying the foundations of art in medical anatomy into the 19th and 20th centuries. By the early 19th century, the use of human cadavers became commonplace.8 In fact, demand for human bodies grew so high that professors and surgeons in England turned to an unethical and nonconsensual practice. Anatomists often acquired cadavers from ‘body snatchers’, who illicitly removed corpses from burial sites.9 As the study of medical science and practice grew, anatomists began to favour direct engagement with human cadavers, and wax models of the Renaissance and Enlightenment were quickly disparaged.10

TThe uptick in the use of cadavers led anatomist Wilhelm Braune to adopt a new technique in anatomical study.11 In 1870, Braune received a cadaver of a young woman who had committed suicide during the last month of her pregnancy. Braune froze the body before slicing it into sections and traced the outlines of the tissues and cavities, creating a drawing that would be reproduced, debated, and replicated in several publications.12 Braune’s frozen sections simplified the three-dimensional intricacies of the human body onto a precise and detailed two-dimensional surface. Proponents of this practice hailed these frozen sections as revolutionary for understanding the body’s spatial relationships, but those traditionally opposed to artistic aid in anatomy argued that direct engagement with bodies through dissection was the only reliable way to acquire anatomical knowledge.12 Nonetheless, frozen sectioning spread across Europe and North America, marking a reconvergence of art and anatomy.13 Little information is available on the pregnant woman that Braune dissected, including her race, income, and the circumstances of her death. It is likely that she did not provide consent for her body to be used in such a manner. The authors wanted to highlight the inherent trauma ingrained into this practice and emphasize that despite the medical advancements made from this act, the immorality and breach of autonomy should not be overlooked.
The use of art in medical anatomy continued through the next century. Published books of anatomical illustrations became richer in detail and more vivid in color, revealing intricate details of skin, muscle, tendons, nerves, and bone. However, as seen above, the routes to this enhanced artistic production were often unethical. At the University of Vienna, Eduard Pernkopf received enhanced artistic production were often unethical. At the University of Vienna, Eduard Pernkopf received the bodies of executed prisoners for dissection, including political dissidents and members of historically marginalized populations. Using such unethically obtained information, Pernkopf published the Atlas of Topographical and Applied Human Anatomy. His atlas features over 800 illustrations, which despite having roots in violence and trauma, is still used today.14 It is essential to
Figure 3: An anatomical sketch by Andreas Vesalius from the De Humani Corporis Fabrica.1recognize that the continued influence of works like Pernkopf’s atlas, partnered with the lack of transparency regarding the dark history of the information featured in this work, underscores the lengthy road toward reconciliation that still remains in this field.
The discussion of art in anatomy is inextricably tied to a discussion of ethics, with considerations oscillating between the pursuit of medical advancement and the preservation of human sanctity and autonomy. Much of our past and present understanding of anatomy is tied to unethical dissections and graphic distributions of unconsenting people. From ancient Greece to the 20th century, vivisections were conducted on prisoners under the rationale of utilitarianism, which stripped individuals of their rights and autonomy and led to societal criticism and scrutiny. Grave robbing and burking for the purpose of dissection particularly plagued communities of low socioeconomic status, further demonstrating the horrific ethical transgressions in anatomical practice.15 In 1942, Germany passed legislation that denied families of executed Poles and Jews the right to claim the bodies.16 Countless more examples across history demonstrate a complete lack of regard for the respect of human life, particularly for historically marginalized populations. These tragedies should serve as a reminder that the advancement of anatomical understanding cannot justify the disregard of moral values. Ethical considerations must be paramount in all scientific and artistic endeavours.
Currently, it is widely accepted that prisoners have full rights over their bodies, and after death, their rights are then passed on to their next of kin. Furthermore, body donor programs are now the most common way of receiving cadavers, with a significant emphasis on respect, controlled graphic distribution, and informed consent. Activism and other progressive movements have also considerably reshaped the educational landscape, promoting awareness for inclusivity and equity.17 A prominent manifestation of these movements is the decolonization of education, which aims to address and rectify the historical biases and injustices found within anatomical curricula. This effort involves recognition of the injustices committed against minorities for scientific advancement and an overall reflection of how these events have shaped knowledge dissemination and the perpetuation of unjust social structures. More emphasis has been placed on diversifying anatomical information and moving away from the colonialist view of anatomy.18 In addition, the model of the white male is often presented as the universal standard of the human form, which is an untrue and incorrect perspective. This misrepresentation has led to an underrepresentation of certain bodies in anatomy, both in terms of cadavers used and educational imagery such as textbook diagrams and physical models.18 The omission of diverse bodies in education perpetuates biases and discrimination within the healthcare system, and educational and medical professionals must work to undo these unjust representations.
With the increasing emphasis on ethics in anatomy, modern educational systems have experimented with the visual mediums used during education. Interestingly, the visual medium used in a course has been proven to impact the engagement of students with the material presented. In a 2020 study conducted at The University of Thessaly, researchers found that the use of painted models in anatomy lectures improved interest
and understanding in undergraduate students as opposed to classical images. Further, many students hoped that this would become a permanent hallmark of the curriculum.19 These applications extend beyond undergraduate education. Medical students at Yale University are already required to participate in a program which involves learning through museum observations. The philosophy behind this method rests on visual literacy—the idea that meaning can be derived from the visual cues of an object. The program encourages students to first understand and see structures before applying their knowledge to a clinical setting. Following exposure to a piece, students are asked to observe and inventory the artistic details. They are then asked to analyze and derive meaning from their observations, prompting them to draw conclusions about the piece. According to the program director, this method of study allows the students to emulate the act of observing signs and symptoms, and providing an analytical diagnosis to a patient. A randomized controlled study was conducted to test the effectiveness of this intervention, and found that with this program, students identified visual cues required for a diagnosis with greater accuracy.20 Applications of art in medical education have found their way into residency programs as well. A systematic review conducted in 2022 showcased various art-based humanities approaches to teaching surgical residents, as well as the effects on their performance. The review concluded that anatomical drawing and modeling was found to enhance surgical learning. One example involved trainees creating three-dimensional models out of PlayDoh based on two-dimensional images, enhancing their ability to better conceptualize the three-dimensional conformation of various structures. An additional observation derived from this review indicates that art training helped enhance drawing and communication of their operations. This was exemplified in one study which found that with an increased focus of drawing, sculpting, and casting in classroom education, residents were better able to grasp the technical aspects of operations. Finally, drawing was actually found to be a particularly useful evaluation tool. Whether artistic competence was evaluated through sculpting exercises, the ability to draw accurate surgical markings, or the drawing of a therapeutic operative procedure, the ability to perform well in these tasks was associated with improved performance in the associated procedure.21
From historical compositions to educational methods, the art of anatomy has become a hallmark of human history within the last few centuries. The intersection of art and anatomy over the centuries has brought about significant ethical concerns. However, the evolution of ethical approaches to artistic anatomical practices reflects moral progress within society and a newfound responsibility to uphold the respect for and autonomy of every individual in pursuit of scientific knowledge. Nonetheless, art will continue to shape our perception of the human form and its complexities for generations to come.
THIS ARTICLE WAS ANONYMOUSLY REVIEWED BY AN ASSISTANT PROFESSOR OF PATHOLOGY & MOLECULAR MEDICINE AT MCMASTER UNIVERSITY.
doi: 10.35493/medu.45.12
AUTHORS:
PARTH ARORA 1, ADITYA MISRA 1, & ALINA PACE 2
1Honours Integrated Science (Biology Concentration), Class of 2026, McMaster University
2Bachelor of Arts & Science (Honours), Class of 2025, McMaster University
ARTIST:
HAMNA MALIK 3
3Bachelor of Engineering and Biomedical Engineering, Class of 2025, McMaster University
For the past two decades, Hamilton, Ontario—like many Canadian cities—has faced an escalating opioid crisis. In 2021, there were 162 opioid overdoses that resulted in death, 43% higher than the provincial average.1 In 2023, the Hamilton City Council declared opioid-related deaths an official emergency.2
The complex nature of opioid use disorder (OUD) in Hamilton necessitates a thorough investigation into its origins and a critical analysis of the current stratgies available to address this ongoing public health concern. Opioid addiction functions as both a clinical and social phenomenon, requiring contextualization

of the opioid epidemic within the history of Hamilton. Against this backdrop, the clinical aspects of opioid use are multifaceted. Hamilton emergency responders face the challenge of rising rates of opioid-related overdoses, 911 calls, and managing opioid dependence in conjunction with other comorbidities. As a result, a comprehensive understanding of the clinical condition is vital for effective implementation of prevention, intervention, and treatment strategies. This article will explore the specific patterns of opioid use in Hamilton, at-risk populations, and health outcomes.
To respond to the epidemic, the municipal government and local nonprofits have designed a variety of interventions. Analysing these response strategies implemented in Hamilton has revealed their response strategies implemented in Hamilton has revealed their effectiveness on a local scale and areas for improvement. Whether through harm reduction initiatives, drug-replacement therapies, or community-based interventions, it is critical that policies are tailored to the unique needs of Hamilton’s population. There are funding gaps that create barriers for users to receive treatment, and exacerbate challenges created by recent increases in polysubstance use, specifically when preventing overdoses.
By elucidating the specific challenges faced by the community, this
article aims to contribute to the ongoing dialogue surrounding the opioid epidemic, providing a foundation for targeted interventions to address this pressing public health crisis in Hamilton.
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, OUD is a clinically diagnosed condition involving a harmful pattern of opioid use leading to significant impairment or distress.3 OUDs are categorised as mild, moderate, or severe based on criteria such as tolerance, withdrawal symptoms, and impact on daily life. The repercussions of OUD on an individual’s health are two-fold, are two-fold, affecting both mental and physical well-being. Individuals with OUD often struggle with mental health disorders, such as depression and anxiety, and face physical health challenges, including respiratory problems and a higher susceptibility to infectious diseases.4,5 These complexities underline the critical need for holistic treatment strategies that concurrently address the physical and psychological facets of OUD.6 The broader term ‘opioid addiction’ is often defined as a chronic and compulsive disorder that involves the uncontrollable use of opioids despite harmful consequences. Understanding OUD and differentiating it from the more stigmatised and historically used term ‘opioid addiction’ is crucial for encouraging open dialogue and promoting effective treatment.1 Stigma, in the context of OUD, often stems from misconceptions about the disorder, which can lead to discrimination and social exclusion.1 However, the term ‘addiction’ has evolved to bear social stigma and thus, replacing it with OUD supports the notion that this condition is a health issue rather than a personal shortcoming.
In Hamilton, managing OUD presents challenges unique to the city. Hamilton is grappling with the need to balance evolving national and provincial chronic pain opioid prescribing guidelines with the increasing demand for chronic pain treatment and surging overdose deaths. Hamilton’s approach to OUD management needs to contend with the intertwined issues of homelessness, mental health, and substance abuse, highlighting the necessity for a comprehensive approach to controlling OUD.
Within the past five years, Hamilton has seen a large increase in opioid-related incidents and deaths. In 2023, Hamilton Paramedic Services responded to 964 incidents related to suspected opioid overdoses, compared to 814 incidents in 2022, representing a 16% increase in a single year. number of opioid-related deaths has also been increasing annually from 52 confirmed deaths in 2016 to 106 in 2023. In January 2024 alone, there have been 36 incidents of suspected opioid overdoses in the city of Hamilton.
The impacts of the opioid epidemic in Hamilton are profound. Geographically, the opioid crisis is widespread across Hamilton, with overdoses reported in every ward. However, areas with higher rates of unemployment and lower median home values have higher rates of opioid prescriptions, opioid-related hospital visits, and opioid overdose deaths.
The public health impacts are equally important to consider as the socioeconomic impacts. The rise in opioid use has led
to an increase in emergency room visits, neonatal abstinence syndrome, and OUD treatment admissions.13 Demographically, more than 65% of opioid deaths in Hamilton are among men aged 25 to 65.11 Older adults also present a significant concern, with approximately 15% of Hamilton citizens over the age of 50 being exposed to opioids.14 Overall, the opioid crisis has strained public health services, with Hamilton Paramedic Services and local hospitals responding to an increasing number of opioid-related incidents.10
The types of opioids used clinically in Hamilton are diverse. Codeine and tramadol are often the first-line opioids for mild to moderate chronic non-cancer-related pain.15 If these prove ineffective, stronger opioids like oxycodone, hydromorphone, and morphine are prescribed. For the treatment of OUD, methadone or buprenorphine-naloxone are commonly used.16
The opioid crisis in Hamilton has also led to a rise in the number of children and young adults exposed to opioids. The City of Hamilton found that childhood risk markers predicting opioid use include male sex, tobacco use, depression, conduct disorder, cannabis use, having peers exhibiting social deviance, and elevated systemic inflammation. These factors contribute to the risk through a mix of social, psychological, and biological vulnerabilities, such as societal norms, dependence pathways in the brain, mental health issues, impulsivity, peer influence, familial instability, and potential links between inflammation and dependence vulnerability.17

In June of 2023, the city’s Public Health Board implemented the Hamilton Drug Plan, an 18-month action plan focused on reducing opioid harm and deaths and increasing access The specific initiatives included scaling up supervised consumption sites, developing safer-use policies, increasing availability of drugchecking services, and expanding support for families and youth prevention programs. This comprehensive plan reflects a commitment to both immediate and sustainable long-term solutions, emphasising collaboration, evidence-informed recommendations, and the inclusion of individuals with lived experience in the decision-making process.7
However, gaps exist in Hamilton’s approach. The city’s strategy was put on pause during the pandemic to focus on COVID19-related relief, leading to an increase in deaths linked to This suggests a need for a more resilient strategy that can adapt to external shocks like a pandemic. Additionally, most drug-related deaths in Hamilton occur in private residences, indicating a need for more community-based
interventions.7 Private residences may lack immediate access to emergency services and overdose prevention tools like naloxone.19 Community-based interventions could include educational outreach programs, increased resources, direct in-home support, as well as training for family and friends on how to respond to overdoses, which could be crucial in preventing fatalities.7
Comparatively, the opioid crisis is also a global issue, with different regions executing a variety of strategies which Hamilton can also implement. For instance, in the United States, strategies primarily involve targeted naloxone distribution and medication-assisted treatment.6 In Europe, regulatory restrictions, drug policy measures, and large-scale implementation of opioid dependence treatments have been used.18
Moving forward, the City of Hamilton could adopt strategies proven successful in other countries. For instance, the U.S. emphasises specialised care, acknowledging different stages of OUD that specific citizens are facing, and promoting collaboration among community entities.6 Europe’s approach of better accessibility and full reimbursement of OUD treatments could also be beneficial to reduce the financial burden of treatment and incentivize more citizens to seek help.18 By incorporating elements from both the American and European strategies, Hamilton can develop a more robust response to the opioid crisis that addresses various aspects of prevention, treatment, and recovery support.
In addition to the challenges mentioned, the rising use of other drugs along with opioids has created new issues. A 2023 report by Public Health Ontario notes that “opioids and stimulants in combination with each other made up the highest proportion of toxicity deaths during the COVID-19 pandemic (43.1%).”20 They also reported that deaths in Ontario where the primary cause was alcohol, stimulants, or benzodiazepine use, over 80% also involved opioids. In many of these cases, people may be unaware that their drug supply is impure and could contain additional opioids or stimulants in their drug supply. Since polysubstance use is associated with higher fatality rates, this further suggests that Hamilton needs better substance management programs for all substances. Addressing polysubstance use may help reduce the number of deaths due to opioid-related and overall overdoses.
Opioid-related morbidity and mortality data has been collected in Ontario since 2004, and the City of Hamilton’s opioid-related death rate has been consistently higher than the provincial average.10 To respond to the recent surge in opioidrelated deaths, the City has implemented various communitybased initiatives through the Hamilton Drug Plan, which will tackle the emergency based on a comprehensive, evidencebased approach. The recent shift in the substance abuse landscape towards polysubstance abuse is poised to become a problem if the city does not address these concerns. Although there are still gaps in the City’s response, only time will tell the effectiveness of ongoing initiatives. Nevertheless, the pressing need to reshape the narrative of stigma associated with opioid addiction and OUD still remains. It will take the collective efforts of the community, healthcare workers, and policymakers for a sustained response to the opioid emergency in Hamilton to be effective and successful in preventing deaths.
REVIEWED BY: DR. DOROTHY BAKKER (MD, MA, CCFP, FCFP)
Dr. Bakker graduated from McMaster University Michael G. DeGroote School of Medicine and completed her family medicine residency at the North Hamilton Community Health Centre. She has practised as a rural family physician in Port Elgin, a student health physician at the University of Guelph, and an immigration panel physician. She completed a Master of Arts in leadership studies at the University of Guelph, and received a Certificate in Travel Health from the International Society of Travel Medicine.
EDITED BY: DOMINIC GANGEMI & RIA PATEL
1. Cheetham A, Picco L, Barnett A, Lubman DI, Nielsen S. The impact of stigma on people with opioid use disorder, opioid treatment, and policy. Subst Abuse Rehabil . 2022;13:1–12. Available from: doi:10.2147?SAR.S304566.
2. van den Brink W, Pierce M, van Amsterdam J. What lessons from Europe’s experience could be applied in the United States in response to the opioid addiction and overdose crisis? Addict Abingdon Engl . 2022;117(5):1197–8. Available from: doi:10.1111/add.15839.
3. Diagnostic and Statistical Manual of Mental Disorders [Internet]. DSM Library. [cited 2024 Jan 31]. Available from: https://dsm.psychiatryonline.org/doi/book/10.1176/appi. books.9780890425596.
4. Santo T, Campbell G, Gisev N, Martino-Burke D, Wilson J, Colledge-Frisby S, et al. Prevalence of mental disorders among people with opioid use disorder: A systematic review and metaanalysis. Drug Alcohol Depend . 2022;238:109551.
5. Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Jan 31]. Available from: http://www.ncbi. nlm.nih.gov/books/NBK553166/.
7. News · CN· C. Hamilton public health board moves forward with new opioid action plan | CBC News [Internet]. CBC. 2023. Available from: https://www.cbc.ca/news/canada/hamilton/ opioid-crisis-action-plan-1.6873396.
8. News · SB· C. Hamilton set to declare state of emergency for homelessness, mental health and opioid addiction | CBC News [Internet]. CBC. 2023. Available from:https://www.cbc. ca/news/canada/hamilton/hamilton-state-of-emergency-homelessness-1.6804478.
9. Klimas J, Hamilton MA, Carney G, Cooper IR, Croteau NS, Dong H, et al. Characteristics and incidence of opioid analgesic initiations to opioid naïve patients in a Canadian primary care setting. Can J Addict . 2022 Mar;13(1):43. Available from: doi: 10.14288/1.0407128.
10. Hamilton Opioid Information System | City of Hamilton [Internet]. [cited 2024 Jan 30]. Available from: https://www.hamilton.ca/people-programs/public-health/alcohol-drugsgambling/hamilton-opioid-information-system.
11. Hamilton has seen an “exponential rise” in opioid deaths. Is it a “state of emergency”? [Internet]. CBC. 2023. Available from: https://www.cbc.ca/news/canada/hamilton/opioidemergency-1.6713522.
12. Seltzer N. The economic underpinnings of the drug epidemic. Popul Health. 2020;12:100679. Available from: doi:10.1016/j.ssmph.2020.100679.
13. National Academies of Sciences E, Division H and M, Policy B on HS, Abuse C on PM and RS to APO, Phillips JK, Ford MA, et al. Trends tin Opioid Use, Harms, and Treatment. In: Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use [Internet]. National Academies Press (US); 2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK458661/.
14. Buckley N. The prescription opioid epidemic: a call to action for our profession. Can J Anesth. 2016;63(1):8–11.
15. Kahan M, Mailis-Gagnon A, Wilson L, Srivastava A. Canadian guideline for safe and effective use of opioids for chronic noncancer pain. Can Fam Physician . 2011;57(11):1257–66.
16. Srivastava A, Kahan M, Nader M. Primary care management of opioid use disorders: Abstinence, methadone, or buprenorphine-naloxone? Can Fam Physician . 2017;63(3):200–
5. Available from: doi:
17. Shanahan L, Hill SN, Bechtiger L, Steinhoff A, Godwin J, Gaydosh LM, et al. Prevalence and childhood precursors of opioid use in the early decades of life. JAMA Pediatr 2021;175(3):276–85. Available from:10.1001/jamapediatrics.2020.5205.
18. News · BH· C. Hamilton’s opioid deaths during pandemic among worst in Ontario, report says | CBC News [Internet]. CBC. 2021 [cited 2024 Jan 30]. Available from: https://www.cbc. ca/news/canada/hamilton/hamilton-opioids-covid-19-1.5918251
19. Partnerships Between Public Health and Public Safety | Drug Overdose | CDC Injury Center [Internet]. 2023 [cited 2024 Jan 30]. Available from: https://www.cdc.gov/drugoverdose/ strategies/public-safety.html.
20. Gomes T, Leece P, Iacono A, Yang J, Kolla G, Cheng C, Ledlie S, Bouck Z, Boyd R, Bozinoff N, Campbell, T, Doucette T, Franklyn M, Newcombe P, Pinkerton S, Schneider E, Shearer D, Singh S, Smoke A, Wu F. Characteristics of Substance-Related Toxicity Deaths in Ontario Stimulant, Opioid, Benzodiazepine, and Alcohol-Related Deaths. 2023; Available from: https://odprn.ca/wp-content/uploads/2023/09/Substance-Toxicity-Report-Final.pdf
6. Evidence-Based Strategies for Preventing Opioid Overdose: What’s Working in the United States | Drug Overdose | CDC Injury Center [Internet]. 2022 [cited 2024 Jan 30]. Available from: https://www.cdc.gov/drugoverdose/featured-topics/evidence-based-strategies.html.
doi: 10.35493/medu.45.16
AUTHORS:
FLORENCE DENG 1 & RUHANI KHATTRA 1
ARTIST:
KATIE LIN 1
1Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
Crohn’s disease (CD) is a chronic inflammatory disease of the gastrointestinal (GI) tract that falls under the umbrella of inflammatory bowel disease (IBD).1 A 2023 impact report estimated that approximately 4.1 in 1000 Canadians live with CD.2 CD is characterized by discontinuous and patchy ‘skip lesions’ and transmural inflammation. The former may impact any part of the GI tract from the mouth to the anus, while the latter extends across the entire thickness of the bowel wall.3 Symptoms are variable and may include diarrhea, abdominal pain, and weight loss, among other potential complications.3 Patients with CD experience a poorer quality of life due to unpredictable bouts of remission, relapse, and no known cure.1
Although the exact pathogenesis of CD is unknown, studies have shown that dysregulated immune responses, genetic factors, gut microbiota, and other environmental factors can modulate disease risk.3 Currently, there is ample evidence to postulate a link between the gut microbiome and IBD. Clinical and animal trials have suggested that gut bacteria trigger and perpetuate colitis and IBD.4 In one study, researchers deduced that individuals with GI infections from Salmonella or Campylobacter have an increased risk of developing IBD within the first year of illness.3 Early antibiotic exposure and gut microbiome disruption, most prominently from ages 0 to 5, also correlate with an increased risk of CD. Among other environmental factors, emerging evidence suggests that diet may be a potential risk factor for CD. For instance, Narula et al. discovered that a high intake of ultra-processed food was positively associated with a higher risk of IBD.5 Although genetic risk factors are still being elucidated, over 200 genes are found to be associated with IBD development. For instance, homozygotic mutations at the NOD2 locus of chromosome 16 may result in fibrostenotic–or narrowing–disease of the GI tract and altered interactions between ileal microbiota and mucosal immunity; affected individuals are 20 to 40 times more likely to develop CD.3,6,7
CD diagnoses are made based on clinical evaluation, diagnostic imaging, and laboratory tests. Generally, CD is suspected when a patient presents with GI symptoms such as inflammation or obstruction, abdominal pain and bloating, persistent diarrhea, perianal fistulas or abscesses, and malnutrition and malabsorption of nutrients, particularly vitamin D or B12.3,8 Using a combination of computed tomography and magnetic resonance scans as well as upper and lower endoscopy imaging, physicians can recognize the internal markers of CD: bowel wall thickening, narrowing of the intestines (stricturing), ulceration, and a “cobblestone” pattern of inflammation on the intestinal lumen.8,9 While imaging is typically required to confirm CD, blood and stool laboratory testing can also be helpful in diagnosis, monitoring inflammation, and ruling out other digestive disorders (e.g., GI infection, Celiac disease, malignancy, irritable bowel syndrome, etc.).8,9
For research and treatment purposes, CD is categorized into three phenotypes: inflammatory, stricturing, or fistulizing CD.3,8 Inflammatory CD may evolve into either of the two latter phenotypes of CD and is characterized by transmural inflammation of the GI tract. This begins with inflammation and small focal ulceration, which may develop into deep longitudinal or transverse GI ulcers.8 These mucosal lesions produce edema, creating a characteristic “cobblestoned” appearance in the bowel of individuals with CD.8
In the stricturing phenotype of CD, excessive inflammation may result in hypertrophy of the muscular mucosa of the intestine, intestinal fibrosis, and stricture formation.8 Strictures refer to areas of stenosis and luminal narrowing in the GI tract, which could cause a bowel obstruction. These fibrostenotic changes are irreversible, aside from surgical correction.3
Prolonged transmural inflammation may also produce a sinus/ fistulous tract, which is characteristic of the fistulizing phenotype of CD. Fistulas are abnormal tunnels that can form between the bowel and adjacent organs.3 CD fistulas result from an epithelial defect related to chronic inflammation—epithelial-tomesenchymal transition (EMT). In EMT, intestinal epithelial cells (IECs) lose their epithelial phenotype to undergo mesenchymal differentiation. The epithelial phenotype is characterized by strong intercellular junctions and cell polarity, whereas the mesenchymal phenotype results in a fibroblast-like morphology, which involves reduced intracellular contact.10 Due to this, IECs gradually migrate and tunnel into deeper layers of the gut wall, causing tissue damage and fistulous tract formation.10 If this tract does not reach an adjacent organ, an abscess—a painful collection of pus, typically caused by infection—is likely to develop. Fistulas and abscesses can induce systemic pain, fever, and other infections related to their location on the GI tract.3,8
While CD is not fatal, it may increase the risk of life-threatening complications, such as sepsis, colorectal cancer, malnutrition, and peritonitis.11 Fistulas may also tunnel to the skin’s outer surface, forming an enterocutaneous fistula.11 Moreover, chronic inflammation, fistulas, abscesses, and strictures can weaken points of the intestinal wall, tearing or perforating the colon to allow for subsequent leakage of GI substances into the abdomen.11


TREATMENTS
Currently, there are no available curative treatments for CD or preventative therapies to correct a potential underlying genetic factor for disease onset.12 The course of management is often individualized depending on a range of factors, including age, comorbidities, symptoms, severity of inflammation, and location of disease.13 CD management involves two primary goals: treating inflammation and complications, and minimizing symptoms.13 Treatments induce mucosal healing, resulting in sustained clinical and endoscopic remission.12 Patients with mucosal healing consistently demonstrate improved outcomes such as lower relapse rates and improved quality of life.14
In the intestine, macrophages, neutrophils, and T cells promote pro-inflammatory mediators like tumour necrosis factor (TNF)-α. Intestinal inflammation in CD dominantly presents with a T-helper 1 and 17 cell-mediated response.1 At present, anti-TNF therapy is an established biologic that may be effective on some CD patients.14 Human TNF is a family of proteins and receptors involved in immune regulation.15 TNF is strongly associated with CD as its biological effects include increased inflammatory cytokine production and inhibition of inflammatory cell apoptosis.15 Therapeutic uses of antiTNF antibodies result in anti-inflammatory effects, including TNF neutralization, depletion of TNF overexpression, and cytokine suppression via reverse signalling processes.15 These effects allow anti-TNF therapy to be effective in inducing and maintaining remission in moderate to severe CD.3 Anti-TNF therapy is often prescribed alongside immunosuppressants (e.g., thiopurine, methotrexate) to decrease immunogenicity rates and increase anti-TNF drug concentration.3,14 Other potential treatments include enteral nutrition and corticosteroids.10 Combination therapies play a substantial role in symptom improvement, mucosal healing, and remission maintenance, with complete remission being the ultimate goal.3,12
Novelly, the Genetic, Environmental, Microbial (GEM) project, an international research study dedicated to determining possible causes for CD, has recently discovered that the gut bacteria composition of individuals who develop CD differs from healthy individuals up to five years before disease development.16 By establishing a model to evaluate the microbiome risk score (MRS), researchers could classify individuals who later developed CD or not, providing insight into microbial determinants of CD pathogenesis. Notably, Ruminococcus torques and Blautia were positively correlated with the MRS, whereas Faecalibacterium and Lachnospira, which produce anti-inflammatory protective metabolites, were negatively correlated with the MRS.17
The role of nutrition, which is suggested to be a significant environmental factor for CD, is an ongoing area of investigation.18
A recent 2024 prospective observational study comparing nutrient intake and blood values of CD patients undergoing anti-TNF therapy suggests potential new nutritional biomarkers capable of predicting therapeutic responses.18 Blood analysis conducted before anti-TNF therapy showed that patients who did not respond to treatment also had significantly decreased levels of taurine and iron.18 Additionally, there was an observable trend of decreased vitamin B12 levels in those who could not achieve
clinical remission upon biological therapy.18 Within the realm of CD management, the lack of therapeutic response is a common problem, calling for optimized treatment and predictions for patients. Rizzello et al. suggests iron and taurine blood levels may be connected to CD patients’ therapeutic outcomes, and has the potential to be used in association with validated biomarkers to assist in therapeutic decision-making.18
Colonic lesions in CD also have characteristically high levels of pro-inflammatory cytokines, like interferon-γ, interleukin (IL)-2, IL-12, and IL-18.1 A breakthrough study in May 2023 introduced the first oral medication, upadacitinib, successful in treating moderate-to-severe CD.19 Upadacitinib is a novel Janus kinase (JAK) inhibitor and a promising therapeutic candidate for treating inflammatory disorders, including CD.20 The mechanistic ability to modulate the JAK pathway, which is key to CD pathogenesis, demonstrates potential in achieving remission and improving quality of life, especially for patients with suboptimal responses to existing treatments.20 JAK inhibition results in decreased production of pro-inflammatory cytokines, significantly diminishing immune events inciting and perpetuating the chronic inflammation characteristic of CD.20 A Phase 3 trial conducted for upadacitinib has demonstrated that patients with moderate-to-severe CD responded favourably compared to a placebo, garnering US Food and Drug Administration approval.21 However, safety profiles show consistent reports of adverse events following upadacitinib use, urging careful monitoring of treatment continuation.20 Further investigation has persisted into the efficacy of dual-targeted therapy (DTT), in which the amalgamation of different inflammatory cascades can lead to a synergistic therapeutic effect in select CD cases.21 One study explores the concurrent use of upadacitinib and ustekinumad, a monoclonal antibody to the p40 subunit of ILs. Ultimately, combining the two drugs was effective and well tolerated for patients with medicallywresistant CD.21 However, the long-term safety profile of DTT remains scarce and limited, given the novelty of upadacintinib.21
Though a permanent cure for CD has not been developed, exciting strides in prognosis and treatment set the stage for continued progress and evolution.
REVIEWED BY: DR. MOHAMED ELTORKI (MSc, FRCPC, MBChB) & DR. WALIUL KHAN (MBBS, PhD, FRCPath, CAGF, MBChB)
Dr. Mohamed Eltorki is an Associate Clinical Professor in McMaster University’s Department of Pediatrics, with research initiatives in gastroenterology, pediatrics, and emergency medicine research ethics. He is also the Trauma Team Leader at McMaster Children’s Hospital and part of the Pediatric Emergency Medicine Simulation Oversight Committee.
Dr. Waliul Khan is a professor and principal investigator at the Fancombe Family Digestive Health Research Institute of McMaster University. He is also the Academic Division Lead of Clinical Pathology of the Department of Pathology & Molecular Medicine at McMaster University and works as a Clinical Scientist/ Consultant Immunologist at Hamilton Health Sciences.
References can be found on our website: www.themeducator.org

The Developmental Origins of Health and Disease (DOHaD) hypothesis proposes a connection between early life exposures—encompassing the prenatal conditions of sperm, in-utero conditions and thereafter—and long-term metabolic disorders and diseases like diabetes, cancer and neurodevelopmental disorders. This hypothesis suggests that environmental conditions can modulate epigenetic processes, driving DNA changes in response to environment and impacting fetal behaviour.1 For example, epigenetic mechanisms such as histone modifications alter genomic DNA during the embryogenesis stage.2 These alterations in early developmental stages can induce and maintain altered gene expression throughout life, consequently affecting adult pathology.3,4 While a plethora of factors— such as paternal exposures, postnatal environments, and sociocultural factors—also contribute to the DOHaD theory, emphasis is placed on maternal exposures in utero.5 As epigenetics garners media attention, Richardson et al. warn about the impacts of oversimplification and miscommunication of DOHaD, contributing to narratives that unjustly blame mothers for their children’s future disease susceptibility.6 This paper will examine the causes, implications, and strategies to address mother-blame narratives pervading DOHaD discourse through a feminist lens, focusing on the experiences of pregnant mothers.
Media language evidenced in news headlines, such as “Mother’s diet during pregnancy alters baby’s DNA” and “Grandma’s Experiences Leave a Mark on Your Genes,” imply that maternal choices or experiences affect the genetic material of the developing fetus without acknowledging the various environmental, social, and paternal determinants that also influence offspring health.6 Consequently, the sensationalization of scientific findings as


definitive conclusions results in anxiety for pregnant women. For instance, Beatriz, a participant in a focus group conducted by Norrmén-Smith et al., shared that the media “take[s] a scientific paper, one piece of information, [and] make[s] it a big headline, and then they talk about it like it was the end of your life. It’s like, they take it out of context and it creates so much anxiety.”7 Reductionist and exaggerated headlines fuel harmful societal expectations, which cause anxiety, blame, and stigma for mothers.
Women with children who develop Fetal Alcohol Spectrum Disorder (FASD), a spectrum of disorders caused by in utero alcohol consumption, are often privy to stigma as a result of distorted health narratives. Shanker et al. interviewed an FASD policy worker who illustrated the stigma experienced by FASD mothers: “The mom is solely responsible to produce that FASD child…Responsibility is part of the bigger picture, but it is mom that has the relationship there.”8 As such, societal stigma often places full responsibility on mothers for choices made during pregnancy, depicting mothers as neglectful caregivers or addicts who are in denial.9 While mothers are often burdened with their children’s health outcomes, it is imperative to consider the role of fathers in contributing to FASD risk. Although paternal alcohol use does not directly cause FASD, “Fathers who drink may contribute to this condition through their influence on women’s alcohol use in pregnancy” and “can negatively impact intelligence and cognitive ability in their children.”10 Stigma experienced by FASD mothers underscores a societal tendency to assign blame solely to them, reinforcing traditional gender roles and overlooking the shared responsibility of both parents in contributing to the child’s well-being. These harmful narratives can commonly lead to lower self-esteem and persistent guilt in women. In particular, affected mothers are more likely to attribute their alcohol consumption during pregnancy to individual responsibility, rather than consider the societal and structural factors that may influence their behaviors: “I am the responsible one...I am the one who was pregnant. I feel horrible about that,” stated a participant in a study conducted by Zabotka et al.9,11 Hence, dismantling this public stigmatization not only requires a shift in individual perspectives, but also prompts a collective societal acknowledgement on the lack of support infrastructure in place for pregnant women.
Lappé et al. argues that biocentric communications of epigenetics and DOHaD shift significant responsibility of birth outcomes to mothers, perpetuating historical narratives that disproportionately affect racialized communities (e.g. Black, Brown, and Indigenous populations).12 For example, studies suggest that gestational diabetes may be related to up to 30% of type two diabetes cases amongst Oji-Cree mothers, compared to 6% of cases amongst other populations in Saskatchewan.13 Coupled with the lack of comprehensive nutritional counseling programs, these potential health risks contribute to anxiety and guilt amongst Indigenous women.14,15 Related discourse glosses over the historical consequences of colonization on healthcare systems, including food insecurity, loss of traditional hunting land, and practices that modulate higher risks for gestational diabetes.16 Consequently, the effects of social determinants of health and racial inequities in maternal healthcare become overlooked in epigenetics discourse. For example, Scott et al. discussed the detrimental implications of medical professionals abdicating responsibility for poor birth outcomes of Black women who come to pregnancy “older, sicker, and fatter.”17 As highlighted by clinician-scientist Monica McLemore, “focusing on a mother’s individual characteristics or behavior avoids the uncomfortable truth that health care systems, namely hospitals and clinics and the people who work in them, contribute to these poor [birth] outcomes.”18
BIOSOCIAL DISCOURSE
To mitigate mother-blame narratives in DOHaD, it is critical to bridge gaps in knowledge translation between biological scientists, social scientists, clinicians, public health professionals, and the public. Molinaro et al. suggests that public health translation of DOHaD should be made more readily available to the public, in addition to promoting awareness about social determinants of health

which acknowledge the historical and social barriers that restrict individual choices.19 Similarly, Harris et al. suggest a biosocial approach that considers “dynamic, bidirectional interactions between biological phenomena and social contexts, which contribute to the lifelong development of humans to shift away from viewing healthcare as a strictly empirical and scientific field.20 Moreover, it is suggested that the roles of community and society are emphasized in epigenetics discourse to acknowledge the upstream effects of sociocultural factors (e.g. economic instability, food insecurity, environmental exposures to toxins, and marginalization) on the biological processes that contribute to and occur during fertilization and pregnancy.20 Thus, biosocial discourse promotes the collective efforts to support and improve the wellbeing of women.
Rather than using language that implies maternal responsibility, language describing the circumstances behind the mother’s decision-making should be applied. For instance, conventional communication instincts such as, “we need to focus on mothers’ diets during pregnancy” or “if women experience too much stress” subtly reinforce a restricted viewpoint centered around the mother.21 To foster a more comprehensive understanding, Winett et. al suggest that effective communication should employ frameworks transcending individual-centric narratives, focusing instead on broader concepts framed as “the circumstances in which women are pregnant and in which children develop” or “the social and economic pressures facing that community.”21 Such framing facilitates an expanded cognitive map, fostering consideration of the intricate network of influences contributing to the issue, which avoids invoking perspectives that impede inclusive thinking.
The historical focus on the intrauterine factors and maternal responsibilities in epigenetics and DOHaD discourse results in mother-blame narratives that perpetuate stigmatization, fear, and guilt in mothers. These narratives enable potential abdication of responsibilities to deliver quality healthcare and public health initiatives. To dispel these narratives, DOHaD discourse should be made more accessible to the public and approached from a biosocial lens that acknowledges the multifaceted relationship between maternal and paternal biological epigenetic processes and sociocultural factors contributing to disease risks. Rather than placing blame on mothers, the insights provided by DOHaD
research can be leveraged to develop educational public health campaigns and policies that promote healthy living, public nutrition, and mental wellness initiatives to protect from disease risk.
REVIEWED BY: DR. MAHMOOD AKHTAR (PhD)
Dr. Mahmood Akhtar is a professor and facilitator in the faculty of Health Sciences at McMaster University. He received his PhD in the field of molecular microbiology, and has completed 2 postdoctoral fellowships. His research has focused on mitochondrial function and metabolic disease.
EDITED BY: OLIVIA KIM, ZAHRA TAUSEEF, & ANGELA HONG
1. Lacagnina S. The Developmental Origins of Health and Disease (DOHaD). Am J Lifestyle Med. 2019;14(1):47-50. Available from: doi:10.1177/1559827619879694.
2. Sharp GC, Lawlor DA, Richardson SS. It’s the mother!: How assumptions about the causal primacy of maternal effects influence research on the developmental origins of health and disease. Soc Sci Med. 2018;213:2t0-7. Available from: doi:10.1016/j.socscimed.2018.07.035.
3. Richardson SS, Daniels CR, Gillman MW, Golden J, Kukla R, Kuzawa C, et al. Society: Don’t blame the mothers. Nature. 2014;512:131-2. Available from: doi:10.1038/512131a.
4. Norrmén-Smith IO, Gómez-Carrillo A, Choudhury S. “Mombrain and sticky DNA”: The impacts of neurobiological and epigenetic framings of motherhood on women’s subjectivities. Front Sociol. 2021;6:653160. Available from: doi:10.3389/fsoc.2021.653160.
5. Shanker I. Risky bodies: Allocation of risk and responsibility within fetal alcohol spectrum disorder (FASD) prevention campaigns.
CJDS. 2016;5(2):152-77. Available from: doi:10.15353/cjds.v5i2.276.
6. Roozen S, Stutterheim SE, Bos AER, Kok G, Curfs LMG. Understanding the social stigma of fetal alcohol spectrum disorder: From theory to interventions. Found Sci. 2022; 27(1):753-18. Available from: doi:10.1007/s10699-020-09676-y.
7. Gearing RE, McNeill T, Lozier FA. J FAS Int. 2005;3(e14):1-11.
8. Zabotka J, Bradley C. “How could I have done this?” Thoughts of mothers of children with fetal alcohol syndrome. J Soc Work Pract Addict 2017;17(3):258-316. Available from: doi:10.1080/1533256X.2016.1243123.
9. Lappé, M, Fahey, FF, & Hein, RJ. Epigenomic stories: Evidence of harm and the social justicve promises and perils of environmental epigenetics. ST&HV. 2022. Available from: doi:10.1177/01622439221137028.
10. Osgood ND, Dyck RF, Grassmann WK. The inter- and intragenerational impact of gestational diabetes on the epidemic of type 2 diabetes. Am J Public Health. 2011;101(1):173-9. Available from: doi:10.2105/AJPH.2009.186890.
11. Neufeld HT. Food perceptions and concerns of aboriginal women coping with gestational diabetes in Winnipeg, Manitoba. J Nutr Educ Behav. 2011;43(6):482-91. Available from: doi:10.1016/j.jneb.2011.05.017.
12. Neufeld HT, Marchessault G. Perceptions of 2 generations of aboriginal women on causes of diabetes during pregnancy. Can J Diabetes 2006;30(2):1-8. Available from: doi:10.1016/S1499-2671(06)02008-9.
13. Elamurugan K, Esmaeilisaraji L, Strain J, Ziraldo H, Root A, MacDonald H, et al. Social inequities contributing to gestational diabetes in indigenous populations in Canada: A scoping review. Can J Diabetes. 2022;46(6):628-11. Available from: doi:10.1016/j.jcjd.2022.05.003.
14. Scott KA, Britton L, McLemore MR. The ethics of perinatal care for black women: Dismantling the structural racism in “mother blame” narratives. J Perinat Neonatal Nurs. 2019;33(2):108-7. Available from: doi: 10.1097/JPN.000000000000039.
15. McLemore MR. What blame the mother stories get wrong about birth outcomes among black moms [Internet]. Center for Health Journalism. 2018 March 14. Available from: https://centerforhealthjournalism.org/our-work/insights/what-blame-mother-storiesget-wrong-about-birth-outcomes-among-black-moms [Accessed 8th Jan, 2024].
16. Molinaro ML, Evans M, Regnault TRH, de Vrijer B. Translation developmental origins of health and disease in practice: Health care providers’ perspectives. J Dev Orig Health Dis. 2021;12(3):1-7. Available from: doi:10.1017/S2040174420000483.
17. Harris KM, McDade TW. The biosocial approach to human development, behavior, and health across the life course. RSF. 2018;4(4):2-26. Available from: doi:10.7758%2FRSF.2018.4.4.01.
18. Winett LB, Wulf AB, Wallack L. Framing strategies to avoid motherblame in communicating the origins of chronic disease. Am J Public Health


doi: 10.35493/medu.45.22
AUTHORS:
PARTH ARORA 1 & ADITYA MISRA 1
1Honours Integrated Science (Biology Concentration), Class of 2026, McMaster University
ARTIST:
STEPHANIE ALELUYA 2
2 Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
The “Orange Jumpsuit” stigma reflects many complex issues found at the intersection of criminal justice and healthcare.1 It represents the widespread prejudice and discrimination faced by incarcerated peoples, particularly regarding their access to adequate healthcare.2 In prisons, healthcare is often perceived as a secondary concern to societies, overshadowed by the punitive aspects of imprisonment.3 This stigma can lead to significant health disparities as a consequence of poor quality care, as seen by the increased onset of mental and physical illnesses. This is particularly seen in the case of Alzheimer's disease and cardiovascular disease within incarcerated populations.3
The Orange Jumpsuit stigma has serious impacts in medical and societal contexts. Adequate prison healthcare is not just a matter of human rights, but is instrumental to the successful reintegration of incarcerated peoples into society.4 By ensuring that standard medical care, mental health support, and rehabilitation services are received, prisons can facilitate smoother transitions for incarcerated people post-release, thereby reducing recidivism and enhancing community safety.5
This article aims to explore the health disparities fostered by the Orange Jumpsuit stigma and examine the ongoing efforts to mitigate these challenges. It seeks to provide an understanding of the current state of prison healthcare, the obstacles incarcerated peoples encounter when accessing healthcare, and the initiatives being undertaken to bridge these gaps, addressing the overarching stigma associated with incarceration.
The origin of the Orange Jumpsuit stigma is deeply rooted in societal attitudes towards incarcerated peoples.6 These attitudes are often shaped by a mix of fear, misunderstanding, and a punitive mindset that portrays incarceration as a means of retribution rather than rehabilitation.7 This perception feeds into a cycle where prisoners are dehumanised, and their basic needs, including healthcare, are overlooked by society.6 The stigma is further perpetuated by media portrayals that often depict incarcerated peoples as irredeemable, thereby reinforcing harmful stereotypes and public indifference toward their well-being.6 This stigma has a profound impact on healthcare policies within
correctional facilities. It often leads to policies that are more focused on security and control rather than the health and rehabilitation of inmates.3 Consequently, healthcare services in prisons are frequently underfunded, understaffed, and inadequately equipped to address the complex health needs of incarcerated peoples.7 The neglect of healthcare services in prisons not only compromises the well-being of those incarcerated but also poses a significant public health risk. The exacerbation of communicable diseases within these confined settings can lead to outbreaks that extend beyond prison walls, threatening the wider community.8 This oversight underscores the interconnectedness of prison health with overall public health, emphasizing the need for comprehensive healthcare strategies in correctional facilities.
Neglecting healthcare in prisons is counterproductive for societal reintegration. A majority of incarcerated peoples will eventually return to society, and their state of health can have substantial repercussions on public safety and health. Inadequate healthcare in prisons often leads to the worsening of chronic conditions and mental health issues, making reintegration more challenging.3 Without routine check-ups, treatment for acute and chronic conditions, vaccinations, and management of health issues, people are more likely to struggle with employment, housing, and social relationships post-release, increasing the likelihood of recidivism.3 Therefore, providing comprehensive healthcare in correctional facilities is an investment in the well-being of the incarcerated and a strategic measure to ensure safer and more inclusive communities.3
Roughly 50% of incarcerated peoples in the U.S. were found to have some form of mental disorder, compared to 10% in non-incarcerated peoples.9 The prison environment, characterised by poor diets, sanitation issues, and a lack of neurodegeneration treatment facilities, may accelerate cognitive decline. Once behind bars, a lack of stimulation and an overall poor quality of life can exacerbate these issues.10
A 2023 study by Tanksley et al. found that incarceration and the APOE-ε4 genotype, the chief genetic risk factor for Alzheimer's disease, both constituted significant risk factors for cognitive impairment.10 However, these effects were mutually independent, suggesting that the risks associated with incarceration and the APOE-ε4 genotype operate across different risk pathways. Further research is required to determine potential genetic changes associated with incarceration and the onset of Alzheimer’s disease.
The stigma surrounding incarcerated peoples often leads to deprioritization of interventions targeted at those who are incarcerated that suffer from Alzheimer's, demonstrated by the lack of research funding given to incarcerated peoples.
More specifically, a study by Boch et al. revealed that less than 0.1% of National Institutes of Health grants focused on Alzheimer’s research for incarcerated peoples.11 Prisons must incorporate special care for these inmates, as it was found that
by 2030, between 70,341 and 211,020 prisoners globally would be diagnosed with Alzheimer's Disease and Alzheimer-related dementias.11 Inadequate care can exacerbate the progression of these conditions, leading to a decline in the quality of life.12
Individuals who have experienced a decline in health due to poorly managed or untreated conditions such as Alzheimer's disease encounter difficulties when reintegrating into society, particularly within incarcerated peoples.13 It was found that the odds of being employed 3 months post-incarceration when faced with a neurodegenerative health limitation, such as Alzheimer’s disease, were reduced by 44%.14 Additionally, 9-months post-incarceration, those with neurodegenerative health issues developed in prisons were 26% more likely to face financial difficulties compared to those released without health problems. The presence of a health condition like Alzheimer's also reduced the likelihood of marriage and family formation by 24% 9-months post-incarceration.14 The compromised health status of people post-release, as aforementioned, is linked to an increased chance of recidivism, as these disparities have been found to heighten the risk of reoffending.5
Incarceration influences the incidence of cardiovascular disease (CVD), often heightening the risk and severity of these conditions. A study highlighted that within two years of prison entry, individuals tend to gain a significant amount of weight, approximately 5.3kg, leading to a higher body mass index and escalated CVD risk.15 Incidence of CVD risk factors, such as hypertension and obesity, have been shown to increase during incarceration and post-release.16 In 2015, it was reported that CVD incidence in male inmates was 12% compared to 3% in non-incarcerated peoples matched for age, race, and gender, highlighting the disparities between these environments.17,18 CVD continues to be a leading cause of death among incarcerated peoples. Additionally, those recently released from correctional facilities have a higher risk of being hospitalized and dying of CVD compared to the general populations, even after accounting for differences in racial identity and socioeconomic status.16 Although studies which adjust for these socioeconomic and sociodemographic factors suggest an association between incarceration and elevated CVD risk factors, it still remains challenging to isolate the specific impact of incarceration on CVD.19,20
However, the stigma associated with incarceration significantly hampers the prioritization, funding, and implementation of effective CVD management and prevention strategies within prisons. The compounded effect of restricted access to medication and healthcare, dietary inadequacies, physical inactivity, stress, and the psychological burden of incarceration synergistically increase the risk of CVD.20,21 Inadequate cardiovascular healthcare for incarcerated peoples contributes to substantial health needs upon release that not only strain individual well-being but also burden existing health systems.21
Improving inmate healthcare presents a multifaceted challenge whose solution stems from addressing systemic issues by implementing targeted health programs within prisons and improving community reintegration. The first step begins with tackling the Orange Jumpsuit Stigma. So far, small movements such as the Jumpsuit Project, created by artist Sherrill Roland, have tried to challenge the stigma associated with incarceration and reintegration.22 After experiencing a wrongful conviction, Roland started wearing an orange jumpsuit around the University of North Carolina at Greensboro, where he taught. Although a shortlived movement, he aimed to raise awareness by encouraging public discourse about incarceration-related issues, such as improper healthcare and reintegration.22,23 Ultimately, a long-term solution to this complex problem will require not only tackling the stigma associated with incarceration and reintegration but also initiating meaningful conversations that can lead to systemic change


and better support for those that are affected by it. Advocacy efforts surrounding healthcare equity, accessibility, and continuity are also underway to align prison health standards with public health standards. A 2021 position paper by the Ontario Medical Students Association brought to attention that federal inmates in Ontario remain excluded from healthcare coverage under the Canada Health Act, urging the Ministry of Health to include them in healthcare reforms.24 This would follow suit behind other provinces like Nova Scotia, Alberta, and British Columbia, where all inmates–provincial and federal–are covered by the province’s healthcare system.24 The gradual shift of responsibility of prisoners’ health care from correctional institutions to governmental health authorities is not only occurring in Canada, but also in other countries such as the United Kingdom, Finland, Norway, and France.25 This trend reflects a consensus that correctional health is an integral part of public health systems. 25
Although rich connections exist between the Orange Jumpsuit stigma and its negative effect on healthcare, very few studies have directly investigated this issue.26 Furthermore, inadequate financial resources, complex health problems, and correctional policies that disrupt medical care are all impediments to providing sufficient healthcare in prisons.3 Certain institutions, such as the Federal Medical Center Devens in Massachusetts, which opened an overcapacitated and underfunded dementia ward in 2019, demonstrates that adding new wards in prisons does not equate to adequate rehabilitation.27 This highlights a larger issue: prisons are not properly equipped for comprehensive healthcare because historically, the wellbeing of the incarcerated has not been a priority for correctional systems.27 This is counterproductive, as addressing the healthcare needs of prisoners is essential for their successful reintegration, and the overall safety of society.27
Ultimately, the critical need to address healthcare disparities and the stigma toward incarcerated peoples cannot be understated. Equitable healthcare can be achieved only through sustained efforts into research-driven policy reform. Future endeavours should focus on creating robust, evidence-based strategies that reform correctional health policy, address fundamental issues such as stigma, and promote a more rehabilitative approach to incarceration. Such initiatives are vital in addressing the deep-rooted biases and systemic shortcomings that unfairly impact prison healthcare access and equity, echoing the broader societal prejudices often symbolised by the image of the orange jumpsuit. Having this direct and focused approach to address these challenges may not only minimise recidivism, but also contribute to a more just and equitable healthcare system that benefits the entire population.
1. Furlow B. Inconsistent and inadequate health care for incarcerated youth in the USA. Lancet Child Adolesc Health 2020;4(2):104-5. Available from: doi:10.1016/S23524642(20)30002-X.
2. Fahmy N, Kouyoumdjian FG, Berkowitz J, et al. Access to primary care for persons recently released from prison. Ann Fam Med . 2018;16(6):549-51. Available from: doi:10.1370/ afm.2314.
3. Vandergrift LA, Christopher PP. Do prisoners trust the healthcare system? Health Justice. 2021;9(1):15. Available from: doi:10.1186/s40352-021-00141-x.
4. Reimer S, Pearce N, Marek A, Heslin K, Moreno AP. The impact of incarceration on health and health care utilization: A system perspective. J Health Care Poor Underserved. 2021;32(3):1403-1414. Accessed January 5, 2024. Available from: doi:10.1353/ hpu.2021.0140.
5. Wallace D, Wang X. Does in-prison physical and mental health impact recidivism? SSM - Popul Health . 2020;11:100569. Available from: doi:10.1016/j.ssmph.2020.100569.
6. Fuller L, Eves MM. Incarcerated patients and equitability: The ethical obligation to treat them differently. J Clin Ethics . 2017;28(4):308-313. Available from: doi:10.1086/ JCE2017284308.
7. Feingold ZR. The stigma of incarceration experience: A systematic review. Psychol Public Policy Law . 2021;27(4):550-569. Available from: doi:10.1037/law0000319.
8. Kinner SA, Young JT. Understanding and improving the health of people who experience incarceration: An overview and synthesis. Epidemiol Rev. 2018;40(1):4-11. Available from: doi:10.1093/epirev/mxx018.
9. Rich JD, Allen SA, Williams BA. The need for higher standards in correctional healthcare to improve public health. J Gen Intern Med. 2015;30(4):503-07. Available from: doi:10.1007/ s11606-014-3142-0.
10. Tanksley PT, Logan MW, Barnes JC. History of incarceration and age-related neurodegeneration: Testing models of genetic and environmental risks in a longitudinal panel study of older adults. PLOS ONE . 2023;18(12):e0288303. Available from: doi:10.1371/ journal.pone.0288303.
11. Boch SJ, Murnan AW, Pollard JF, Nidey NL, Hardy RY, Iruka IU. Assessment of US federal funding of incarceration-related research, 1985 to 2022. JAMA Netw Open . 2023;6(2):e230803. Available from: doi:10.1001/jamanetworkopen.2023.0803.
12. Cox RJA, Wallace RB. The role of incarceration as a risk factor for cognitive impairment. J Gerontol Ser B . 2022;77(12):e247-e262. Available from: doi:10.1093/geronb/gbac138.
13. Feczko A. Dementia in the incarcerated elderly adult: Innovative solutions to promote quality care. J Am Assoc Nurse Pract . 2014;26(12):640-8. Available from: doi:10.1002/23276924.12189.
14. Link NW, Ward JT, Stansfield R. Consequences of mental and physical health for reentry and recidivism: Toward a health-based model of desistance. Criminology . 2019;57(3):544-73. Available from: doi:10.1111/1745-9125.12213.
15. Bondolfi C, Taffe P, Augsburger A, et al. Impact of incarceration on cardiovascular disease risk factors: a systematic review and meta-regression on weight and BMI change. BMJ Open. 2020;10(10):e039278. Available from: doi:10.1136/bmjopen-2020-039278.
16. Wang EA, Redmond N, Dennison Himmelfarb CR, et al. Cardiovascular disease in incarcerated populations. J Am Coll Cardiol . 2017;69(24):2967-76. Available from: doi:10.1016/j. jacc.2017.04.040.
17. Maruschak LM, Berzofsky M, Unangst J. Medical Problems of State and Federal Prisoners and Jail Inmates, 2011-12. US Dep Justice Off Justice Programs. Published online 2015. Available from: http://www.bjs.gov/content/pub/pdf/mpsfpji1112.pdf.
18. Saleh ZT, Connell A, Lennie TA, et al. Cardiovascular disease risk predicts health perception in prison inmates. Clin Nurs Res 2019;28(2):235-51. Available from: doi:10.1177/1054773817740534.
19. Pollack CE, Slaughter ME, Griffin BA, Dubowitz T, Bird CE. Neighborhood socioeconomic status and coronary heart disease risk prediction in a nationally representative sample. Public Health 2012;126(10):827-35. Available from: doi:10.1016/j.puhe.2012.05.028.
20. Wang EA, Wildeman C. Studying health disparities by including incarcerated and formerly incarcerated individuals. JAMA . 2011;305(16):1708-9. Available from: doi:10.1001/ jama.2011.532.
21. Grammatikopoulou MG, Lampropoulou M, Milapidou M, Goulis DG. At the heart of the matter: Cardiovascular health challenges among incarcerated women. Maturitas . 2021;149:16-25. Available from: doi:10.1016/j.maturitas.2021.05.002.
22. Jumpsuit Project. Sherrill Roland. Available from: https://www.sherrillroland.com/jumpsuitproject.
23. The Jumpsuit Portal. Creative Capital. Available from: https://creative-capital.org/projects/ the-jumpsuit-portal/.
24. Lee A, Ross A, Saad M. Health Care Reform in Canadian Corrections Facilities. Available from: https://omsa.ca/sites/default/files/media/health_care_reform_in_canadian_corrections_ facilities.pdf.
25. McLeod KE, Butler A, Young JT, et al. Global prison health care governance and health equity: A critical lack of evidence. Am J Public Health . 2020;110(3):303-08. Available from: doi:10.2105/AJPH.2019.305465.
26. Martin K, Taylor A, Howell B, Fox A. Does criminal justice stigma affect health and health care utilization? A systematic review of public health and medical literature. Int J Prison Health. 2020;16(3):263-79. Available from: doi:10.1108/IJPH-01-2020-0005.
27. Engelhart K. Inside a Dementia Unit in a Federal Prison. N Y Times. Published online August 13, 2023:6-6. Available from: link.gale.com/apps/doc/A760533663/AONE?u=mlin_ oweb&sid=googleScholar&xid=13b7d5bc.
REVIEWED BY: DR. FIONA KOUYOMOUDJIAN (MD, PhD, MPH)
Dr. Fiona Kouyoumdjian is an Assistant Professor in the Department of Family Medicine within the Faculty of Health Sciences at McMaster University. She is currently leading research focussed on the population health status of incarcerated peoples.
EDITED BY: ANYA KYLAS, JIA LU, & SEPEHR BAHARESTAN
doi: 10.35493/medu.45.26
MORGAN PUUSAARI 2 & DAVID SHEN
2Bachelor of Life Sciences (Honours), Class of 2027, McMaster University
3Bachelor of Health Sciences (Honours), Class of 2027, McMaster University
Parkinson’s Disease (PD) is a neurodegenerative disorder affecting millions of individuals worldwide. However, current diagnostic tools are limited to the clinical assessment of overt symptoms, after PD has already progressed into the clinical stage. A novel PD testing method, α-synuclein seed amplification assay (αsyn-SAA), may revolutionize the testing by allowing clinicians to detect PD before symptoms arise. The α-synuclein protein abundant in pre-synapse is typically involved in the release of dopamine. However, in the development of PD, αsyn proteins become misfolded and infect their pathogenic conformations to other αsyn proteins through the prion-like process of seeding. αsyn-SAA testing identified PD progression by amplifying and measuring the accumulation of misfolded α-synuclein proteins in an individual’s cerebrospinal fluid. This critical review aims to appraise the mechanisms of αsyn-SAA testing, exploring its benefits and drawbacks. Notably, αsyn-SAA has been found to have over 90% sensitivity to PD and other synucleinopathies, while being able to distinguish between PD patients and healthy subjects with a high degree of accuracy. However, there are notable limitations and future longitudinal studies are necessary to optimize the specificity of αsyn-SAA testing.
protein, in which pathological, misfolded αsyn proteins proliferate through the brain, eliciting neurodegeneration and synaptotoxicity.
αsyn-SAA testing is a prospective diagnostic technique for subclinical PD detecting aggregating αsyn proteins as a biomarker to distinguish PD patients from healthy individuals.3 αsynSAA tests exploit the self-proliferating, prion-like nature of the aggregated proteins, which are able to ‘infect’ unaggregated proteins via seeding. To test for misfolded αsyn seeds in samples of cerebrospinal fluid (CSF) via αsyn-SAA, scientists add fluorescently tagged, non-aggregated α-syn proteins to the medium. If misfolded α-syn is present in a patient’s sample, the tagged αsyn proteins are converted to aggregated αsyn through the αsyn-seeding process.6 Interactions between monomeric (non-misfolded) and aggregated αsyn fibrils induce the unfolding of monomeric αsyn and their aggregation-prone surfaces being exposed, generating new αsyn amyloid fibrils. Thus, concentrations of aggregated αsyn in the sample are expected to be amplified exponentially. Thioflavin T (ThT) binds to αsyn fibrils, intensifying fluorescence, which is then measured. Positive αsyn-SAA test results are indicated by a
PD is a progressive neurodegenerative disease that causes uncontrollable movements, typically characterized by tremors, stiffness, and progressively deteriorating motor function impairment.1 PD affects 1 million Americans, and causes immeasurable suffering for both patients and their communities. Scientists believe that PD is associated with the death or malfunction of nerve cells in the basal ganglia, responsible for body movement through the secretion of dopamine.1 Although much remains unknown, research suggests that most cases of PD involve both genetic and environmental components.
The onset of PD begins prior to the emergence of symptoms, in a phase known as the preclinical stage. However, most diagnoses of PD occur when individuals are symptomatic when the disease has progressed to the clinical stage.2,5 Much research is currently focused on improving early detection of PD in the preclinical stage to prevent its progression. Additionally, since many symptoms of PD are similar to other disorders, many cases of PD are initially misdiagnosed, which results in delayed treatment.1,8 Considering these factors and the ageing population of the U.S., much effort has gone into developing better tools for diagnosing subclinical PD, with the αsyn-SAA being analysed as the aim of this study.1


SAA test. The fluorescently tagged, normal αsyn proteins are integrated among the misfolded αsyn proteins and placed in a fluorescence plate reader; if misfolded αsyn are in the sample, fluorescence will increase, as depicted by the graph on the left.9
In healthy brains, the α-synuclein (αsyn) protein can be found in nerve cells and is responsible for the storage and release of neurotransmitters like dopamine and serotonin.2 However, abnormalities involving this protein, like occurrence of clumps of αsyn known as Lewy bodies, play a key role in the development
αsyn-SAA testing is of particular interest because of its proven accuracy in diagnosing individuals with PD. αsyn-SAA helps identify various synucleinopathies, a group of neurodegenerative diseases characterized by α-syn aggregates, including PD or multiple system atrophy.7 αsyn-SAA testing displays robust sensitivity

and specificity, identifying PD patients with a positive test result while identifying healthy individuals as negative, respectively.11 Upon sampling 55 PD patients, Gomes et al. found that all were correctly given positive results (100% sensitivity). αsynSAA also differentiated these patients from 24 healthy controls with a specificity of 70.8%. Additionally, αsyn-SAA testing discerns synucleinopathies from other movement disorders, a previously difficult task due to their similar symptoms. This includes tauopathies such as supranuclear palsy, a neurological disease associated with the buildup of pathological tau proteins, that αsyn-SAA can discriminate with 75% specificity.6
αsyn aggregation is found to occur prior to the onset of PD symptoms, such as dopamine deficiency, which hints at its pivotal ability to serve as a biomarker for PD years before symptoms arise. In a cross-sectional study performed by Siderowf et al., prodromal carriers of gene mutations associated with PD were found to have misfolded αsyn accumulation prior to biomarker modifications or overt clinical symptoms.11 This has significant potential to become one of the initial diagnostic tools for PD, allowing for preemptive refined treatments for patients. Furthermore, early diagnosis of PD through αsyn-SAA has implications for research in this field as researchers can explore various mechanisms that underlie the development of PD, and search for biomarkers in presymptomatic patients which may assist in comprehending disease progression and severity. Finally, αsyn-SAA is able to recognize small concentrations of αsyn, which can have useful applications for preclinical stages of PD, of which individuals typically display minute αsyn levels.13
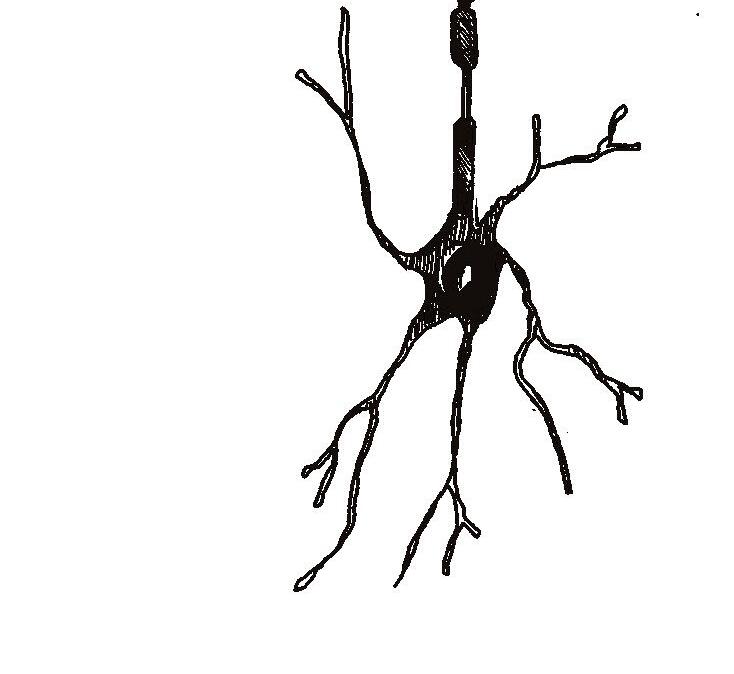
results between various forms of PD. Particularly, αsyn-SAA testing had lower sensitivity in patients with a LRRK2 gene variant than individuals with typical or sporadic forms of PD. This indicates that despite having identical clinical symptoms, αsyn-SAA may not be able to properly distinguish between different subtypes of PD. LRRK2-related PD may have a different method of pathology compared to other αsyn-positive types, such as PD associated with the GBA gene mutation, which is found to have high rates of positive αsyn-SAA results. Diverse ages, sex, and motor abilities amongst individuals with LRRK2 variants were also associated with varying αsyn-SAA results. Further research is necessary to understand how heterogeneity in various subgroups affects accuracy of PD diagnoses, and to compare αsyn-SAA results in individuals with variants across different PD-associated genes, such as PINK1 and PRKN.11
Though the αsyn-SAA test can detect subtle quantities of aggregated αsyn in samples, it still does not allow researchers to reliably discriminate between different synucleinopathies.13 Furthermore, since the detection of PD is based on a αsyn threshold that only allows for positive or negative tests, it is difficult to quantify differential amounts of αsyn aggregates, so this test cannot monitor the extent of disease progression in its current state.
In all, current research in αsyn proteins in biological samples is limited by several factors.13 First, there is a lack of standardized collection guidelines for sample collection and analysis, as well as patient selection criteria for trials. Therefore, results may be inconsistent and confounding variables are bound to be introduced across different studies. Additionally, current assays only focus on detecting one specific αsyn protein, which does not account for the nuance of modified forms of different αsyn markers. Research also found that most studies on αsyn proteins have small sample sizes, which is likely a consequence of the invasive nature of CSF collection, low participation in research studies, and requirement of multiple strenuous sample donations. Consequently, research in αsyn-SAA and PD detection account for variability and consistency poorly, which casts doubts on the prospective benefits of αsyn-SAA testing.

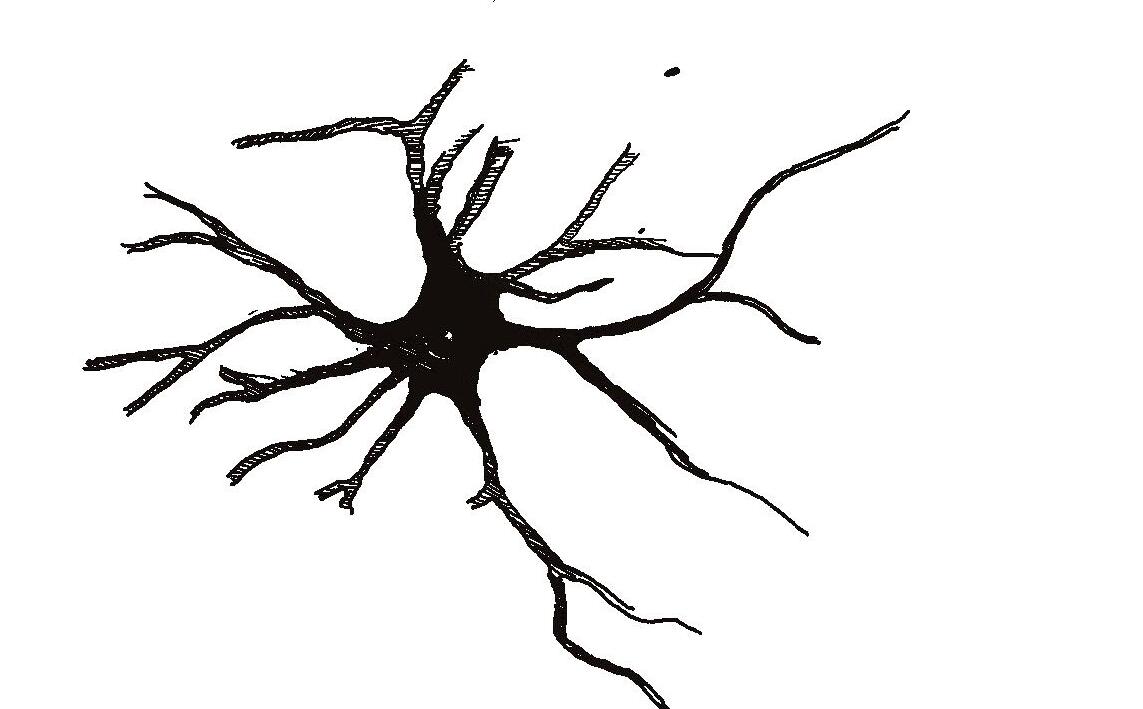
Considering the invasive collection methods to obtain CSF samples for the αsyn-SAA test, this PD testing method is difficult to implement in current clinical settings. Further research is required to develop a method that can procure samples less invasively, perhaps from saliva or blood, and requires larger sample sizes to ensure its reliability. Moreover, standardized protocols for sample collection and analysis, more rigorous participant cohort selection, as well as larger sample sizes across more trials, would improve the reliability of the results and the aforementioned limitations of αsyn-SAA tests. Further longitudinal studies may also assist in elucidating the relationship between αsyn concentration and PD severity and progression, as well as the accuracy of positive test results in individuals with pre-symptomatic or prodromal conditions.
αsyn-SAA is an innovative early-detection method for the diagnosis of PD, introducing a novel and sensitive way to screen individuals. While further studies would allow for optimization of αsyn-SAA for specific synucleinopathies and types of PD, current research is promising. If implemented in the future, αsynSAA is expected to complement traditional clinical diagnoses, as well as allow for earlier detection and implementation of treatment options to assist in slowing the progression of PD. The implications of αsyn-SAA for PD research and clinical trials also cannot be disregarded, as early detection measures of PD and other neurological disorders may aid in the search for new related biomarkers and therapeutics for patients.
REVIEWED BY:
DR. HONG TIAN DONG (MD)Dr. Hong Tian Dong is an Internal Medicine resident physician at the University of Toronto. Her research interests lie in agerelated neurodegenerative diseases and synthetic biology.
EDITED BY: ANGELA HONG, OLIVIA KIM, ZAHRA1. NIH National Institute on Aging (NIA). Parkinson’s Disease: Causes, Symptoms, and Treatments [Internet]. National Institute on Aging. 2022. Available from: https://www.nia. nih.gov/health/parkinsons-disease/parkinsons-disease-causes-symptoms-and-tre atments
2. Parkinson’s Disease: Challenges, Progress, and Promise | National Institute of Neurological Disorders and Stroke [Internet]. www.ninds.nih.gov. 2023 [cited 2024 Jan 7]. Available from: https://www.ninds.nih.gov/current-research/focus-disorders/parkinsons-diseaseresearch/parkins ons-disease-challenges-progress-and-promise
3. Russo MJ, Orru CD, Concha-Marambio L, Giaisi S, Groveman BR, Farris CM, et al. High diagnostic performance of independent alpha-synuclein seed amplification assays for detection of early Parkinson’s disease. Available from: doi:10.1186/s40478-021-01282-8.
4. Vargas JY, Grudina C, Zurzolo C. The prion-like spreading of in vivo models of Parkinson’s disease. doi:10.1016/j.arr.2019.01.012.
5. Getting Diagnosed | Parkinson’s Foundation [Internet]. www.parkinson.org. Available from: https://www.parkinson.org/understanding-parkinsons/getting-diagnosed.
6. Fernandes Gomes B, Farris CM, Ma Y, Concha-Marambio L, Lebovitz R, Nellgard B, et al. α -Synuclein seed amplification assay as a diagnostic tool for parkinsonian disorders. Parkinsonism Relat Disord parkreldis.2023.105807.
7. Galvin J, Lee VMY, Trojanowski JQ. Synucleinopathies: Clinical and pathological implications. JAMA 2001. Available from: doi:10.1001/archneur.58.2.186.
8. Poll finds a quarter of people with Parkinson’s are wrongly diagnosed [Internet]. Parkinson’s UK. 2020. Available from: https://www.parkinsons.org.uk/news/poll-finds-quarter-peopleparkinsons-are-wrongly-diagnosed.
9. Kurapova R, Chouliaras L, O’Brien JT. The promise of amplification assays for accurate early detection of α -synucleinopathies: A review. from: doi:10.1016/j.exger.2022.111842 10.1016/j.exger.2022.111842.
10. Calabresi P, Mechelli A, Natale G, Volpicelli-Daley L, Lazzaro GD, Ghiglieri V. Alpha-synuclein in Parkinson’s disease and other synucleinopathies: from overt neurodegeneration back to early synaptic dysfunction. s41419-023-05672-9.
11. Siderowf A, Concha-Marambio L, Lafontant DE, Farris CM, Ma Y, Urenia PA, et al. Assessment of heterogeneity among participants in the Parkinson’s Progression Markers Initiative cohort using α -synuclein seed amplification: a cross-sectional study. 2023;22(5):407–17. Available from: doi: 10.1016/S1474-4422(23)00109-6.
12. Bräuer S, Rossi M, Sajapin J, Henle T, Gasser T, Parchi P, et al. Kinetic parameters of alphasynuclein seed amplification assay. from: doi:10.1186/s40478-023-01653-3.
13. Magalhães P, Lashuel HA. Opportunities and challenges of alpha-synuclein as a potential biomarker for Parkinson’s disease and other synucleinopathies. 2022;8(1):1–26. Available from: doi: 10.1038/s41531-022-00357-0.
Title Illustration: Credit: Wellcome Library, London. Wellcome Images images@wellcome.ac.uk http:// wellcomeimages.org

doi: 10.35493/medu.45.33
AYRA CHAUDHRY 1 & FIONA MACDOUGALL 2
1Bachelor of Biology and Psychology (Honours), Neuroscience, and Behaviour, Class of 2026, McMastery University
2Bachelor of Health Sciences (Honours), Class of 2027, McMaster University
The human gastrointestinal (GI) tract houses an abundance of microorganisms which make up an environment known as the gut microbiome. Its composition is affected by a variety of factors, including the method in which an individual was born, antibiotic use, diet, and environmental exposures. Gut microbes engage in bidirectional communication with the host through the gut-brain axis, which connects the central and enteric nervous systems through neural, hormonal, and immunological signalling pathways. Therefore, the various microbes housed in the GI tract can have an effect on brain functioning and mental health through this axis of communication. Rates of mental disorders, such as depression and anxiety, have been on the rise, increasing significantly after the COVID-19 pandemic. The steady increase continues to occur despite the introduction of treatments and medications, which highlights the crucial need for novel and innovative therapies. This piece explores the relationship between the gut microbiome and various mental health disorders, as well as the potential of psychobiotics as a novel treatment strategy.
The gut-brain axis is a bidirectional communication channel that links the enteric nervous system and central nervous system (CNS). Bacteria residing in the gut can affect the brain through various pathways such as traveling through the bloodstream, causing hormone release from enteroendocrine cells, inducing cytokine release from mucosal immune cells, and influencing afferent nerve pathways such as the vagus nerve. Conversely, psychological stress can affect microbial composition by altering the intestinal environment and interrupting bacterial signalling through the introduction of stress hormones, such as noradrenaline. Gut microbial composition is different in patients with mental
health disorders when compared to a healthy population. A majority of the human microbiome is composed of the Phyla Firmicutes and Bacteroidetes.5 In a study done by Jiang et al., patients with major depressive disorder (MDD) were found to have increased Bacteroidetes, Proteobacteria, and decreased Firmicutes in their fecal matter compared to the general population. Focusing on genera, patients with MDD had more Enterobacteriaceae, Alistipes, and less Faecalibacterium, while those who exhibited severe depressive symptoms had a
ARTISTS: MISHAL HOSSAIN 1 & ARIM YOO 2
1Bachelor of Health Sciences (Honours), Class of 2025, McMaster University
2Bachelor of Health Sciences (Honours), Class of 2024, McMaster University
Dysregulation of hippocampal neurogenesis is associated with psychological symptoms in various disorders, such as depression, schizophrenia, and addiction.9,10 Additionally, there is strong evidence to implicate a causal role of the gut microbiome in the mechanisms behind the development of depression. Fecal microbiota transplantation from human patients with depression to rats with depleted microbiota induced behavioural and physiological characteristics associated with depression, including anxiety-like behaviours and changes in tryptophan metabolism.11
Generalised anxiety disorder is another common mental illness that displays microbial dissimilarities. Compared with a healthy population, patients had a lower prevalence of Faecalibacterium, Eubacterium rectale, Lachnospira, Butryicicoccus, and Sutterella in their gut microbiome.6 These genera are involved in the production of short-chain fatty acid (SCFA) compounds that, when insufficiently produced can compromise immune responses and further contribute to brain abnormalities.12-14 Furthermore, stress and the microbiome have a two-way connection.3 Certain gut bacteria are capable of reducing symptoms of stress and anxiety. In particular, Lactobacilli increases γ-Aminobutyric acid (GABA) levels in the CNS, a neurochemical essential for inhibitory responses and controlling feelings of stress and fear, by activating GABA signalling pathways in the vagus nerve. by Crumeyrolle-Arias et al. on germ free (GF) mice demonstrated an amplified hormonal stress response system known as the hypothalamic–pituitary–adrenal (HPA) axis. GF mice had a higher expression of the corticotropin-releasing hormone gene compared to healthy mice, which caused a hypersecretion of stress-related hormones, such as adrenocorticotropic hormone and corticosterone. Anxiety-like behaviours associated with novel challenges, such as social interaction or exposure to an open environment, increased in GF mice as they were observed to defecate more and spend more time hiding in corners. The

the bacterial metabolism of tryptophan. Kynurenic acid inhibits excitatory amino acid receptors, which is also observed in psychiatric illnesses like schizophrenia.
Inversely, stress responses can lead to an imbalance in one’s microbiome composition, a
If left untreated, dysbiosis leads to the development of chronic gastrointestinal illnesses, such as irritable bowel syndrome.3 Stress exhibited by the host organism changes the habitat of gut bacteria by reducing the quality of the gut epithelium and interfering with gene expression and signalling due to the presence of the stress hormone noradrenaline.3,17 Studies with adult mice exposed to stress demonstrate decreased Bacteroides and increased Clostridium compared to controls, which cause the intestinal barrier to become more permeable, facilitating circulation of bacterial components.18 Further, studies in humans found bacterial translocation in other parts of the body in stressrelated psychiatric disorders. Specifically, the translocation of bacterial components, such as lipopolysaccharides, can trigger inflammatory responses and induce depressive behaviours.19
A POSSIBLE TREATMENT SOLUTION
Psychobiotics, encompassing probiotics and prebiotics, are live organisms that can improve mental health by promoting
The effect of SCFA on 5-hydroxytryptophan (5HTP), a precursor of serotonin, was measured using an in vitro model of enterochromaffin cell.19 The B. breve CCFM1025 treatment showed a considerable decrease in chronic stress through the increased production of beneficial metabolites and modification of neurotransmission in the brain.19
Under conditions of prolonged stress, CCFM1025 was shown to modify the gut microbial composition, thereby decreasing the heightened levels of hyperfunction and inflammation in the HPA axis.19 The in vitro treatment observed a positive correlation between CCFM1025 and 5-HTP.20 In contrast, Bifidobacterium pseudolongum, a Bifidobacteria in the intestine with an unknown physiological function had a negative correlation to 5-HTP.21 Brain-derived neurotrophic factor (BDNF), a factor that stimulates and controls the growth of new neurons, experienced an increase in response to CCFM1025, while c-Fos, a marker for neuronal activity, was decreased.22,23
Although positive results were observed, all of the data generated from the Tian et al. study used male mice, despite depression in humans being more prevalent among females.19 Future studies should assess antidepressant-like effects of CCFM1025 in female mice before delving into clinical studies. The study also did not specify which metabolites produced by CCFM1025 contributed to the observed antidepressantlike effects. To address this gap, a metabolomics-based analysis of CCFM1025 should be conducted.19
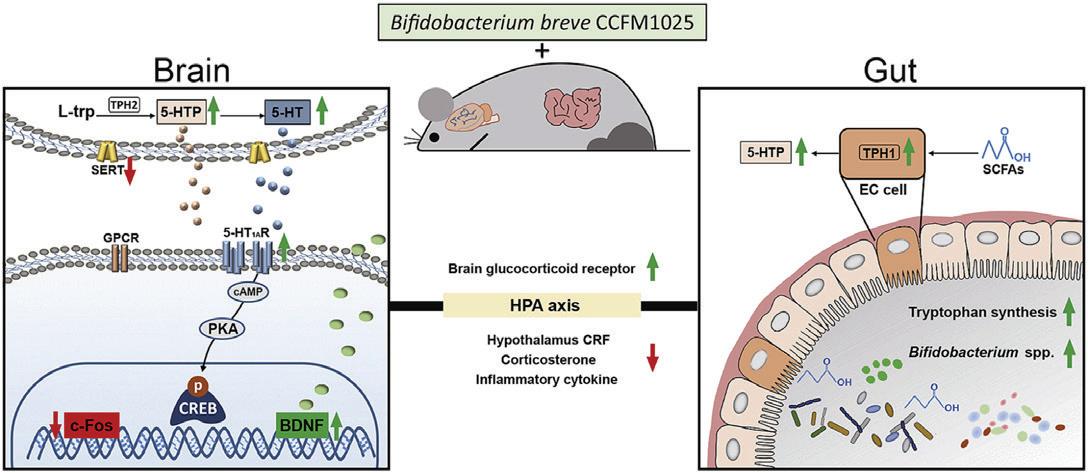
Figure 1. Metabolic pathways of antidepressant-like effects via reshaping gut microbial composition and increasing the production of beneficial metabolites, reducing inflammation in the HPA axis, upregulating BDNF expression and downregulating c-Fos in the brain.
The results of Tian et al.’s study are confirmed by a randomized controlled trial, which compared the effectiveness of helveticus R0052 and prebiotic supplement in individuals diagnosed with MDD and taking antidepressant medication. Inventory (BDI), a significant decrease in BDI scores was seen eight weeks later in participants on the probiotic formula compared to the placebo group. the study noted that supplementation with prebiotics, nondigestible nutrients that nourish gut bacteria, did not yield any significant effects. to tryptophan ratio for the group taking the probiotics suggests that probiotics may improve depressive symptoms.
However, limitations in the analysis of the fecal microbiome do not provide sufficient confidence in these results as the human gut microbiota is highly variable and may have directly impacted the response of the participants consuming the probiotic formula.24 Furthermore, the intervention was conducted at different times throughout the year.24 Therefore, seasonal changes in lifestyle and diet may have altered the effect of the probiotic.


Dr. Miranda Green is a recent PhD graduate from the Foster lab. Her research focuses on the relationship between the microbiome, immune system and brain. Her work has been published in renowned journals such as the International Journal of Molecular Sciences and Frontiers in Bioengineering and Biotechnology.
Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon, JI. Host-bacterial mutualism in 2005;307(5717):1915–20. Available from: doi:10.1126/
Bloomfield SF, Rook GA, Scott EA, Shanahan F, Stanwell-Smith R, Turner P. Time to abandon the hygiene hypothesis: New perspectives on allergic disease, the human microbiome, infectious disease prevention and the role of targeted hygiene. Perspect Public Health. 2016;136(4):213–24. Available from: doi:10.1177/175791391.
Kupcova I, Danisovic L, Klein M, Harsanyi S. Effects of the COVID-19 pandemic on mental BMC Psychol. 2023 Apr 11;11:108. Available from:
Collins S, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. 2012;10:735–42. Available from: doi:10.1038/nrmicro2876.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of Science. 2005;308(5728):1635–8. Available from:
Jiang H, Ling Z, Zhang Y, Mao H, Ma Z, Yin Y, et al. Altered fecal microbiota composition in patients with major depressive disorder. Brain Behav Immun. 2015;48:186–194. Available
Ledochowski M, Widner B, Sperner-Unterweger B, Propst T, Vogel W, Fuchs D. Carbohydrate malabsorption syndromes and early signs of mental depression in females. Dig Dis Sci. 2000;45:1255-9. Available from: doi:10.1023/A:1005527230346.
Lotrich FE, El-Gabalawy H, Guenther LC, Ware CF. The role of inflammation in the pathophysiology of depression: Different treatments and their effects. J Rheumatol. 2011;88:48-54. Available from: doi:10.3899/jrheum.110903.
Foster JA, Baker GB, Dursun SM. The relationship between the gut microbiome-immune aystem-brain axis and major depressive disorder. Front Neurol. 2021;12. Available from: Toda T, Parylak S, Linker SB, Gage FH. The role of adult hippocampal neurogenesis in brain 2019;24(1):67–87. Available from: doi:10.1038/
Kelly JR, Borre Y, O’ Brien C, Patterson E, El Aidy S, Deane J, et al. Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat. J 2016;82:109–18. Available from: doi:10.1016/j.jpsychires.2016.07.019.
van de Wouw M, Boehme M, Lyte JM, Wiley N, Strain C, O'Sullivan O, et al. Short-chain fatty acids: Microbial metabolites that alleviate stress-induced brain-gut axis alterations. J. 2018;596(20):4923–44. Available from: doi:10.1113/JP276431.
Morris G, Berk M, Carvalho A, Caso JR, Sanz Y, Walder K, et al. The role of the microbial metabolites including tryptophan catabolites and short chain fatty acids in the pathophysiology of immune-inflammatory and neuroimmune disease. Mol Neurobiol. 2017;54:4432–51. Available from: doi:10.1007/s12035-016-0004-2.
Peirce JM, Alviña K. The role of inflammation and the gut microbiome in depression and 2019;97(10):1223–41. Available from: doi:10.1002/jnr.24476.
Tette FM, Kwofie SK, Wilson MD. Therapeutic anti-depressant potential of microbial GABA produced by Lactobacillus rhamnosus strains for GABAergic signaling restoration and inhibition of addiction-induced HPA Axis hyperactivity. Curr Issues Mol Biol. 2022;44(4):1434–51. Available from: doi:10.3390%2Fcimb44040096.
Crumeyrolle-Arias M, Jaglin M, Bruneau A, Vancassel S, Cardona A, Daugé V, et al. Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute Psychoneuroendocrinology. 2014;42:207-17. Available from: doi:10.1016/j.
Gareau MG, Wine E, Rodrigues DM, Cho JH, Whary MT, Philpott DJ,et al. Bacterial infection causes stress-induced memory dysfunction in mice. Gut. 2011;60(3):307-17. Available from: doi:10.1136/gut.2009.202515.
Bailey MT, Dowd SE, Galley JD, Hufnagle AR, Allen R. G, Lyte M. Exposure to a social stressor alters the structure of the intestinal microbiota: Implications for stressorBrain Behav Immun. 2011;25(3):397-407. Available from:
Maes M, Kubera M, Leunis JC, Berk M. Increased IgA and IgM responses against gut commensals in chronic depression: Further evidence for increased bacterial translocation 2012;141(1):55-62. Available from: doi:10.1016/j.
Ross K. Psychobiotics: Are they the future intervention for managing depression and Explore. 2023;19(5):669–80. Available from: doi:10.1016/j.
Oroojzadeh P, Bostanabad SY, Lotfi H. Psychobiotics: The influence of gut microbiota on the gut-brain axis in neurological disorders. J Mol Neurosci. 2022;72:1952–64. Available from: doi:10.1007/s12031-022-02053-3.
Tian P, O’Riordan KJ, Lee Y, Wang G, Zhao J, Zhang H, et al. Towards a psychobiotic therapy for depression: Bifidobacterium breve CCFM1025 reverses chronic stress-induced depressive symptoms and gut microbial abnormalities in mice. Neurobiol Stress. 2020;12:100216. Available from: doi:10.1016/j.ynstr.2020.100216.
Birdsall TC. 5-Hydroxytryptophan: A clinically-effective serotonin precursor. Altern Med Rev. 1998;3(4):271-80. Available from: PMID: 9727088.
Centanni M, Lawley B, Butts CA, Roy NC, Lee J, Kelly WJ, et al. Bifidobacterium pseudolongum in the ceca of rats fed hi-maize starch has characteristics of a keystone species in 2018;84(15):e00547-18. Avaliable from: doi:10.1128/
Bathina S, Das UN. Brain-derived neurotrophic factor and its clinical implications. Arch Med 2015;11(6):1164–78. Available from: doi:10.5114/aoms.2015.56342.
Bullitt E. Expression of c—fos—like protein as a marker for neuronal activity following noxious J Comp Neurol. 1990;296(4):517–30. Available from: doi:10.1002/
Kazemi A, Noorbala AA, Azam K, Eskandari MH, Djafarian K. Effect of probiotic and prebiotic vs placebo on psychological outcomes in patients with major depressive disorder: Clin Nutr. 2019;38(2):522–8. Available from: doi:10.1016/j.
Davani-Davari D, Negahdaripour M, Karimzadeh I, Seifan M, Mohkam M, Masoumi S, et al. Prebiotics: Definition, types, sources, mechanisms, and clinical applications. Foods. 2019;8(3):92. Available from: doi:10.3390/foods8030092.
Logan AC, Jacka FN, Craig JM, Prescott SL. The microbiome and mental health: Looking back, moving forward with lessons from allergic diseases. Clin Psychopharmacol Neurosci. 2016;14(2):131–47. Available from: doi:10.9758/cpn.2016.14.2.131.

doi: 10.35493/medu.45.37
AUTHORS:
ANH NGUYEN 2 & LUCY CHEN 2
2Bachelor of Health Sciences (Honours), Class of 2027, McMaster University
During menopause, up to 80% of individuals experience vasomotor symptoms, such as hot flashes, that severely impact quality of life.1 Fezolinetant is a novel oral drug that shows promise in treating hot flashes by acting as a neurokinin 3 receptor antagonist that restores hypothalamic thermoregulation.2 This review explores the effectiveness of Fezolinetant in reducing menopausal symptoms compared to the current pharmacological standard of care. We evaluate the strengths of Fezolinetant as an alternative treatment for patients that are eligible for traditional hormone replacement therapy and outline current limitations of the medication. The potential benefits of Fezolinetant warrant further research and post-market clinical trials to continue monitoring its efficacy and safety.
Vasomotor symptoms, commonly known as hot flashes, include sensations of heat, sweating, anxiety, and chills lasting one to five minutes. These symptoms occur during menopause when reduced estrogen levels disrupt hypothalamic regulation of core body temperature.3,4 As a selective neurokinin 3 receptor antagonist, Fezolinetant blocks neuropeptide neurokinin B (NKB) from binding to kisspeptin–neurokinin B–dynorphin (KNDy) neurons, which helps restore the sensitivity of the hypothalamic thermoregulatory centre to normal levels.2 NKB stimulates KNDy neurons in the thermoregulatory centre and acts on estrogen inhibited neurokinin 3 receptors.5 This review discusses the efficacy, safety, strengths and limitations of Fezolinetant as a novel treatment for vasomotor symptoms of menopause.
In the phase III study SKYLIGHT 1, a randomised, doubleblind trial was conducted between placebo, 30mg, and 45mg Fezolinetant groups. The results from this trial indicate that Fezolinetant significantly reduces in the frequency and severity of vasomotor symptoms compared to placebo over the course of 52 weeks.6 The high-quality methods in this study ensured that confounding factors were reduced and the notably high potential for placebo bias was limited. Similar results were observed in SKYLIGHT 2, further validating the efficacy of this treatment.5 Additionally, the study was designed to be highly generalisable by recruiting a diverse population of study participants. The inclusion criteria consisted of female-born individuals aged 40 years to 65 years, BMI from 18 to 38 kg/m2, an absence of clinically significant findings on mammogram and pap test, and willingness to undergo a transvaginal ultrasound and endometrial biopsy.5 The SKYLIGHT study took place across 97 facilities, including the United States, Canada, Czech Republic, Hungary, Poland, Spain, and the United Kingdom.5
Another study, Moonlight 1, involved 302 participants sampled from a variety of Asian countries.7 For data collection, researchers tracked vasomotor symptoms using various self-reported methods
that measured a range of relevant effects. In SKYLIGHT 2, they used an electronic hot flashes diary with a reference guide that outlined mild to moderate and severe symptoms. Menopause Specific Quality of Life (MENQOL) is a 29-item reporting tool that was used to measure vasomotor, psychosocial, physical, and sexual symptoms. The study also used Patient Reported Outcomes Measurement Information System Sleep Disturbance (PROMIS SD) to track sleep disturbances. The extensive scope of symptoms measured in this experiment, ranging from direct indicators of hot flashes to indirect symptoms such as sleep quality, strengthened the quality of the study. After 12 weeks in SKYLIGHT 2, there was a reduction in mean daily vasomotor symptom frequency from baseline by 58.64% in the 30mg group and 64.27% in the 45mg group, compared to 45.35% in the placebo group. After 12 weeks of treatment in the three randomized groups (30mg, 45mg, placebo), participants on placebo were randomly selected to begin the 30mg or 45mg treatment. Despite a placebo effect, there was a statistically significant difference between the treatment and placebo groups throughout the entire 52 week period. Regarding patient-reported sleep disturbances, only the 45 mg group reported a statistically significant difference at 12 weeks.5
Limitations of this literature exist due to a reliance on selfreported methods to gather data. Patient-reported symptoms of sleep disturbance have inherent biases as symptoms are subject to variability given that each participant has different basal levels and interpretations of sleep quality. Furthermore, selfreported methods are susceptible to response bias, the tendency for participants to respond inaccurately, which can contribute to the placebo effect. Another discrepancy in SKYLIGHT 1 was that data was only collected from participants that used the interactive diary and had greater than 85% compliance in treatment.6 This may introduce some degree of bias, where results reflect a specific subset of participants that are more likely to report symptoms, which reduces the study’s applicability to clinical settings. Overall, the use of self-reported methods to gather data may not have accurately reflected the efficacy of Fezolinetant.
SKYLIGHT 4, a 52-week Phase III trial, investigated the safety of 30mg and 45mg Fezolinetant dosages using a sample of 1830 participants aged 40-55. Participants who took at least one dose of the study drug were included in the safety analysis. The results showed that treatment emergent adverse events occurred in 63.9% of the 45mg group, 67.9% in the 30mg group, and 64.1% of the placebo group.8 Notably, 4.3% of participants in the control group withdrew due to the treatment-emergent adverse effects, compared to 5.6% for the 30-mg group and 4.6% for the 45-mg group.8
Treatment-related risks of endometrial cancer and endometrial hyperplasia (a precancerous condition where there is an irregular thickening of the uterus) continue to be a concern in examining the safety of Fezolinetant. One case of endometrial malignancy was reported in the 30mg group, while no occurrences of malignancy were reported in the 45mg or placebo group.8 Changes in secondary endpoints, endometrial thickness, bone mineral density, and
trabecular bone scores, were consistent across all three groups. These results, alongside the low withdrawal rates of SKYLIGHT 4, support the safety of Fezolinetant use over a period of 52 weeks.
The authors of the SKYLIGHT studies were affiliated with and received funding from Astellas Pharma Inc, the proprietor of Fezolinetant, which poses potential for bias. Further peer review and phase IV post-market studies from unbiased sources are necessary to confirm the results of these trials. Since Fezolinetant was recently FDA-approved in May 2023 (Astellas Pharma has yet to submit an application for drug approval to Health Canada), there exists gaps in literature regarding the long-term use of the drug, especially considering that menopausal vasomotor symptoms can persist for about 11.8 years.7 It is suggested that longitudinal research and post-market evaluation studies be done on an ongoing basis as the drug continues to be used in the consumer market.
From the data obtained from Phase I, II and III clinical trials, Fezolinetant shows promise for populations of symptomatic individuals undergoing the early stages of menopause. Currently, estrogen and progesterone hormone replacement therapy are the most common treatments for menopause. As a non-hormonal treatment, the drug is accessible for patients who are ineligible or contraindicated for current treatment methods. These agents mimic the neuromodulation effects of estrogen produced by the ovaries on the hypothalamus prior to menopause. However, hormone replacement therapy treatment is only recommended for individuals younger than 60 years old and within 10 years of menopause onset due to risks of coronary heart disease, stroke, dementia, bone loss, and venous thromboembolism.10 Furthermore, individuals with a history of breast cancer are not candidates for estrogen hormone treatment as the additional estrogen can contribute to tumour growth.11 With up to 80% of individuals experiencing the vasomotor symptoms of menopause, the drug has potential to restore quality of life in individuals who experience anxiety, poor quality of sleep and occupational disturbances related to these symptoms.1 Unfortunately, the estimated marketed price of Fezolinetant ($500 for a 1-month supply) raises affordability concerns compared to current treatment options.12 In comparison, other non-hormonal options such as SSRIs range from $4 to $200 USD in monthly costs.13 Consequently, the affordability factor can potentially result in low usage rates for Fezolinetant.

The development of Fezolinetant, a neurokinin 3 receptor antagonist, offers a promising new treatment option for individuals who are ineligible for traditional hormone therapies. Although current evidence from the SKYLIGHT studies suggests that Fezolinetant has potential to be an effective and safe treatment option, further Phase IV research is required to continue to investigate the long-term efficacy and safety of the drug. Overall, options for the treatment of vasomotor symptoms for individuals who are transitioning into menopause have historically been quite limited, and the development of new therapeutic modalities like Fezolinetant has significant potential to improve the quality of life and health outcomes of impacted individuals.
Dr. Nicholas Leyland (MD) is a Professor in the Department of Obstetrics and Gynecology at McMaster University, receiving his medical degree from the University of Toronto in 1983. In 2010, Dr. Leyland became professor and chair of the Department of Obstetrics & Gynecology at McMaster University. His research primarily focuses on minimally invasive gynecologic surgery.
1. Gold EB, Colvin A, Avis N, Bromberger J, Greendale GA, Powell P, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: Study of women’s health across the nation. Am J Public Health . 2006;96(7):122635. Available from: doi:10.2105/AJPH.2005.066936.
2. Depypere H, Timmerman D, Donders G, Sieprath P, Ramael S, Combalbert J, et al. Treatment of menopausal vasomotor symptoms with Fezolinetant, a neurokinin 3 receptor antagonist: A phase 2a trial. J Clin Endocrinol Metab . 2019;104(12):5893–905. Available from: doi:10.1210/jc.2019-00677.
3. Rance NE, Dacks PA, Mittelman-Smith MA, Romanovsky AA, Krajewski-Hall SJ. Modulation of body temperature and LH secretion by hypothalamic KNDy (kisspeptin, neurokinin B and dynorphin) neurons: A novel hypothesis on the mechanism of hot flushes. Front Neuroendocrinol. 2013;34(3):211-27. Available from: doi:10.1016/j.yfrne.2013.07.003.
4. Bansal R, Aggarwal N. Menopausal hot flashes: A concise review. J Midlife Health. 2019;10(1):6-13. Available from: doi:10.4103/jmh.JMH_7_19.
5. Johnson KA, Martin N, Nappi RE, Neal-Perry G, Shapiro M, Stute P, et al. Efficacy and safety of Fezolinetant in moderate to severe vasomotor symptoms associated with menopause: A phase 3 rct. J Clin Endocrinol Metab. 2019;108(8):1981-97. Available from: doi:10.1210/ clinem/dgad058.
6. Lederman S, Ottery FD, Cano A, Santoro N, Shapiro M, Stute P, et al. Fezolinetant for treatment of moderate-to-severe vasomotor symptoms associated with menopause (SKYLIGHT 1): A phase 3 randomised controlled study. The Lancet 2023;401(10382):1091-102. Available from: doi:10.1016/S0140-6736(23)00085-5.
7. Wright AC, Beaudoin FL, McQueen RB, Yeung K, Moradi A, Herron-Smith S, et al. The effectiveness and value of Fezolinetant for moderate-to-severe vasomotor symptoms associated with menopause: A summary from the Institute for Clinical and Economic Review's Midwest Public Advisory Council. J Manag Care Spec Pharm. 2023;29(6):692-98. Available from: doi:10.18553/jmcp.2023.29.6.692.
8. Neal-Perry G, Cano A, Lederman S, Nappi RE, Santoro N, Wolfman W, et al. Safety of Fezolinetant for vasomotor symptoms associated with menopause: A randomized controlled trial. Obstet Gynecol. 2023;141(4):737-47. Available from: doi:10.1097/ AOG.0000000000005114.
9. Faubion SS, Crandall CJ, Davis L, Khoudary SR, Hodis HN, Lobo RA, et al. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause. 2022;29(7):767-94. Available from: doi:10.1097/GME.0000000000002028.
10. Depypere H, Lademacher C, Siddiqui E, Fraser GL. Fezolinetant in the treatment of vasomotor symptoms associated with menopause. Expert Opin Investig Drugs. 2021;30(7):681-94. Available from: doi:10.1080/13543784.2021.1893305.
11. Onge ES, Phillips B, Miller L. Fezolinetant: A new nonhormonal treatment for vasomotor symptoms. J Pharm Technol. 2023;39(6):291-97. Available from: doi:10.1177/875512 25231198700.
12. Avis NE, Crawford SL, Greendale G, Bromberger JT, Everson-Rose SA, Gold EB, et al. Study of women's health across the nation. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531-9. Available from: doi:10.1001/ jamainternmed.2014.8063.
13. Stubbs C, Mattingly L, Crawford SA, Wickersham EA, Brockhaus JL, McCarthy LH. Do SSRIs and SNRIs reduce the frequency and/or severity of hot flashes in menopausal women. J Okla State Med Assoc . 2017;119(5)272-4. Available from: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC5482277/ [cited 2024 Mar 21].
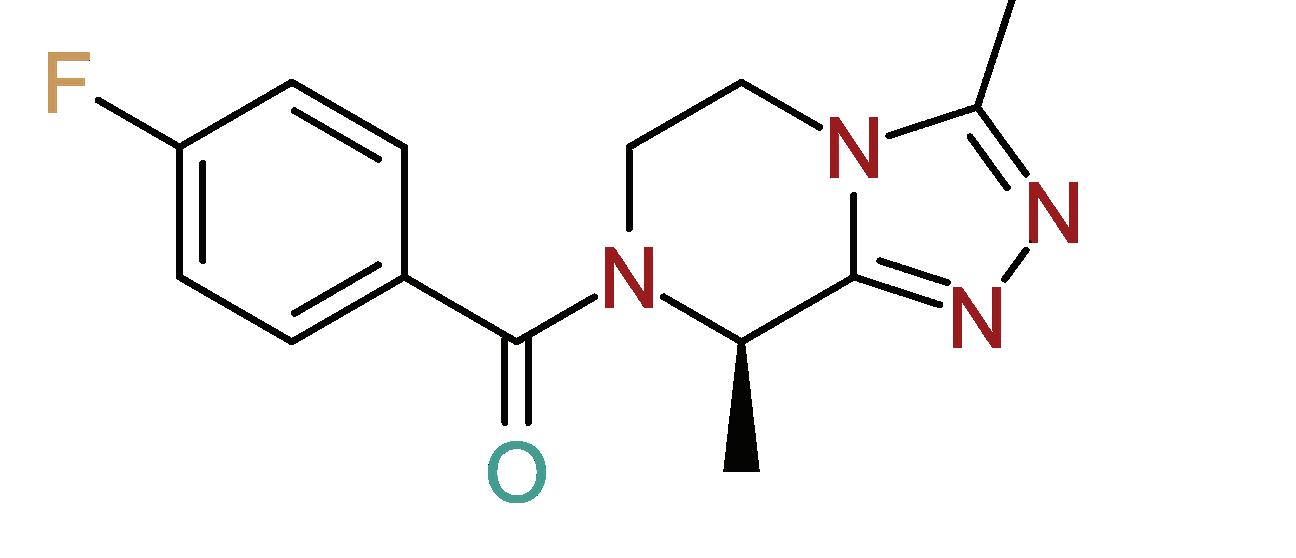
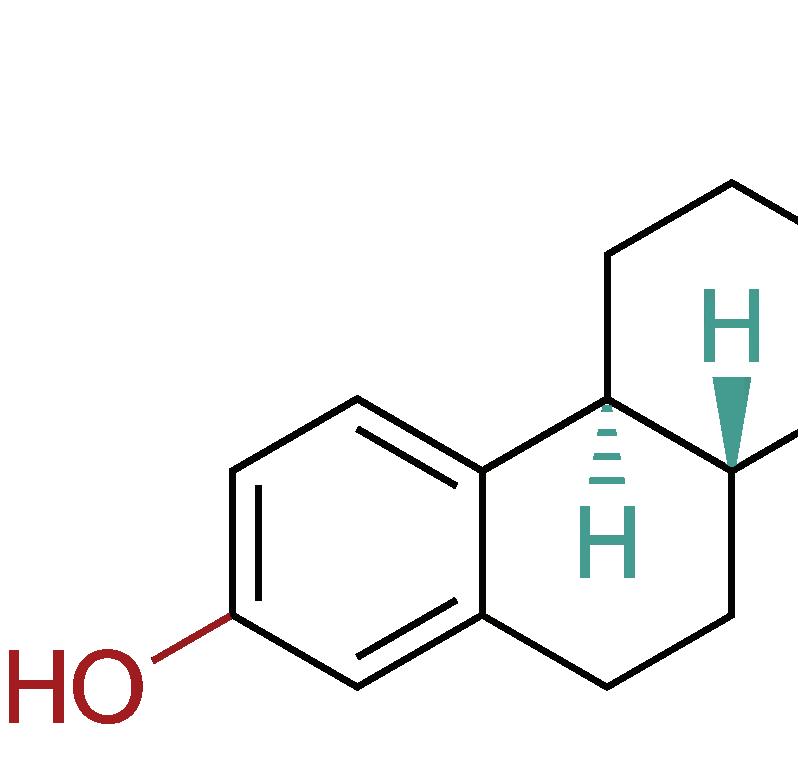

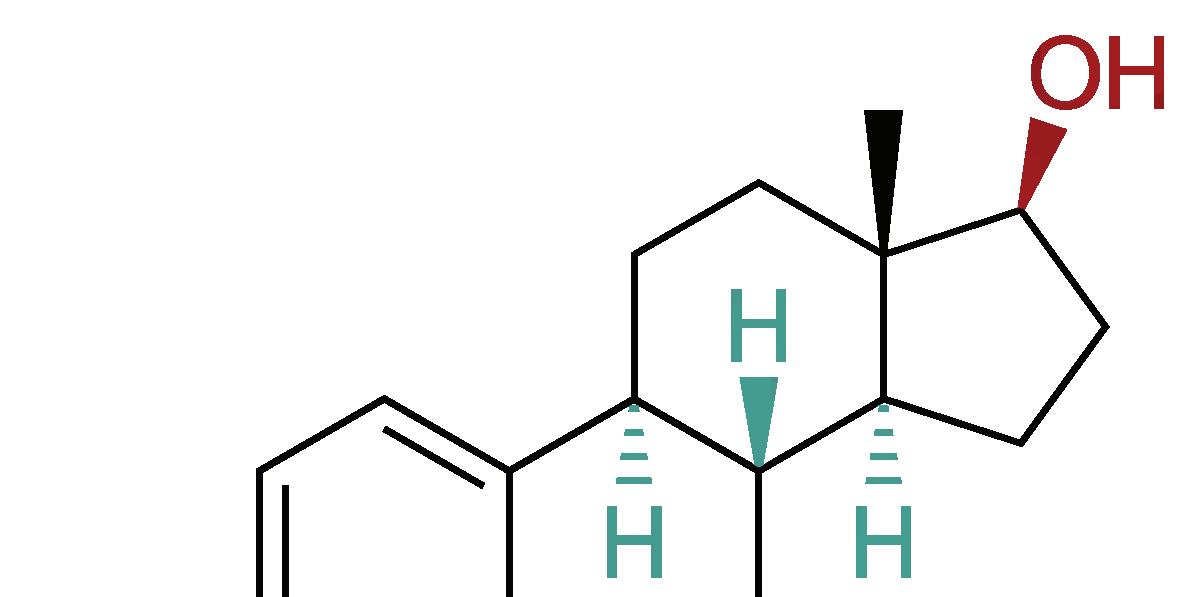

doi: 10.35493/medu.45.41
AUTHORS:
CYNTHIA DUAN 1 & VERONICA GRIGANO 1
1Bachelor of Health Sciences (Honours), Class of 2027, McMaster University
ARTIST:
ELAINE WANG 2
2Bachelor of Health Sciences (Honours), Class of 2026, McMaster University

ABSTRACT
Beta-thalassemia is a hereditary blood disorder, with one of the most severe forms being transfusion-dependent thalassemia (TDT). Zynteglo is a cell-based gene therapy that seeks to provide an alternative for routine blood transfusions required in the treatment of TDT. The manufacturing process of Zynteglo begins with the collection and modification of a patient’s hematopoietic stem cells. Functional copies of the beta-globin gene are then introduced to restore normal hemoglobin production. In clinical trials, Zynteglo has demonstrated its effectiveness as a treatment for TDT, with an assessment report led by Northwestern University 78.6% of American patients achieving complete transfusion independence. However, staggering costs, accessibility issues, and safety concerns hinder the acceptance of the drug in major regions of the world. Future considerations must address the risks and barriers associated with the treatment process to foster greater accessibility.
INTRODUCTION
Beta-thalassemia is one of two categories of thalassemia, a group of recessively inherited blood disorders. Thalassemia is characterized by little to no production of hemoglobin, resulting in anemia of varying severity.1 It occurs as a result of a genetic mutation of the beta-globin gene (HBB), which causes a reduced beta-globin chain availability in the assembly of mature hemoglobin.1 The most severe form of beta-thalassemia is transfusion-dependent thalassemia (TDT). Also known as betathalassemia major, patients with this variation require lifelong routine blood transfusions for survival, starting in infancy or early childhood.2 Blood transfusions introduce a variety of challenges, including transfusion-associated iron overload, infection, allergic reactions, and hemolytic reactions.2 In addition, routine blood transfusions are time consuming and inconvenient which can be mentally taxing for many patients and contribute to a decreased quality of life.3 With 1 in 100,000 individuals estimated to exhibit some form of symptomatic beta-thalassemia, more long-term and sustainable treatments for TDT are required to improve the overall quality of life of patients suffering from this disease.1
Zynteglo, a cell-based gene therapy, presents a novel approach to the treatment and management of TDT. This treatment aims to help beta-thalassemia patients achieve long-term transfusion independence, potentially eliminating the need for transfusion entirely.4 The process begins with the collection of autologous blood stem cells, or hematopoietic stem cells (HSCs), from the patient.5 In the manufacturing phase, Zynteglo is created by using a lentiviral vector (LVV) to incorporate functional copies of a HBB gene, βA-T87Q-globin, into the genome of collected HSCs.5 The patient then undergoes myeloablative conditioning with busulfan, or chemotherapy, to suppress the immune system and prepare the body to receive the stem cells.4 The resulting modified autologous stem cells are then reintroduced into the patient’s body through intravenous infusion.5 The stem cells subsequently initiate the production of red blood cells containing active βA-T87Q-globin.5 This produces normal beta-globin molecule pairs with alpha-globin molecules to form functional hemoglobin and repopulate normal blood.4,5
The Phase 1/2 HGB-205 trial enrolled patients with TDT, with the primary goal of the study being the achievement of transfusion independence.6 Transfusion independence is a critical milestone indicative of Zynteglo’s ability to address the underlying genetic defect causing beta-thalassemia. The results from this trial noted a reduction in the frequency of blood transfusions observed in the treated cohort. Most significantly, 78.6% of American patients treated with Zynteglo in the HGB205 trial achieved complete transfusion independence.7 The therapy demonstrated its ability to induce sustained production of functional hemoglobin, a clinically meaningful achievement that eliminates transfusion comorbidities such as iron overload.7
Two additional Phase 3 studies, HGB-207 and HGB-212, further validated the therapeutic potential of Zynteglo. These investigations aimed to confirm and extend the findings of HGB-205, providing additional data on the efficacy and safety of the treatment through long-term observation of a broader patient population. The results of Phase 3 reinforced the promising outcomes observed in previous trials, with a consistent reduction in transfusion dependence and a sustained improvement in hemoglobin levels. Specifically, 32 out of 36 evaluable patients across HGB207 and HGB-212 had attained transfusion independence and achieved a normal or near-normal total hemoglobin.8,9
Adverse events associated with Zynteglo primarily consisted of patients displaying mild side effects.10 LVVs with incorporated transgenes can transduce dividing and non-dividing cells, variably insert transgenes into the host genome. This promotes long-term gene expression to correct, introduce or delete DNA sequences. Across all Zynteglo trials, there has been no evidence of insertional oncogenesis, nor any reported instances.10 Although the risk is still present, the absence of such adverse events in Zynteglo-treated patients provides an additional layer of confidence in the safety of this gene therapy.
The comprehensive and rigorous evaluation of Zynteglo in these clinical trials has not only provided evidence of its efficacy and safety but has also offered insights into the
broader impact of the treatment in the lives of TDT patients. The reduction or elimination of the need for regular blood transfusions has profound implications for the overall wellbeing and quality of life of individuals living with TDT.3
There are several drawbacks of Zynteglo, particularly regarding its accessibility and safety. Zynteglo’s market price is incredibly high, ranging from $1.8 million USD in European markets to $2.8 million USD in American markets, which is largely due to the manufacturing company seeking to recoup the high costs of development and drug testing.11-13 However, this has led to the drug being rejected from European markets after initial approval, as the company failed to negotiate reimbursements within their National Health Systems to cover costs.13 With Europe being one of the three major continents where TDT is prevalent, this has proven to be a major setback in the usage and accessibility of gene therapy for medicinal purposes.14
TDT is also prevalent in the Mediterranean, Middle East, North and Central Africa, and Southeastern and Southern Asia.14 In fact, these areas are more at risk for TDT compared to the Americas, with only 0-3% beta-thalassemia related gene mutations, in contrast to 0-19% in Europe, 2-18% in the Middle East, 0-12% in Africa, and 0-11% in Southeast Asia.15 As such, Africa and Asia are two major continents where the feasibility of implementing Zynteglo should be considered.
Although the prevalence of beta-thalassemia is quite high in Africa, the high-cost of a drug like Zynteglo may make for difficult implementation.14 Instead, they may first prioritize the focus of health infrastructure on more pressing health issues such as tuberculosis, acute respiratory infections, and HIV/AIDS.17 In addition, the heightened prevalence of beta-thalassemia in Africa does not necessarily predict the incidence of TDT or severity of the disorder.
Zynteglo has not been approved in any Asian countries, which may be due to the differing and lengthy procedures regarding drug approval. For example, it typically takes China an additional five years to approve imported drugs compared to the vast majority of countries around the world.18
While Zynteglo has been approved in the United States of America, accessibility concerns remain. The initial high cost of the treatment, along with the limited clinical infrastructure needed to support and monitor the toxic busulfan myeloablative conditioning process, creates several barriers for individuals to access the treatment.12 As such, the accessibility of Zynteglo and the feasibility of its implementation in various regions becomes an issue.
The safety of Zynteglo has also been an area of concern due to the lack of long-term follow-up after clinical trials, small sample size, and adverse reactions. Typically, long-term follow-up consists of observing participants after 15 years of the initial study. However, due to Zynteglo’s novelty, there is no follow-up data of this magnitude, leading to multiple concerns being raised over potential side effects and whether patients will continue to remain transfusion-independent.10
A small portion of patients across all Zynteglo trials experienced
adverse events while undergoing treatment including neutropenia, thrombocytopenia, leukopenia, anemia, and lymphopenia, with over 50% of all adverse reactions occurring at a high degree of severity.19 Furthermore, within the most recent follow-up for two clinical trials, 37% of patients exhibited severe adverse events, with the most common symptoms being pyrexia, thrombocytopenia, liver veno-occlusive disease, febrile neutropenia, neutropenia, and stomatitis.19 Symptoms of mild severity can be treated with antibodies, corticosteroids, and other minimally invasive administrations.19,20 However, severe symptoms typically require intravenous solutions and potential hospitalization.19,20 While some of these issues may be a result of the busulfan myeloablative conditioning rather than the actual drug, this step is still essential for the administration of Zynteglo. As a result, safety concerns for the overall procedure remain. The small sample size of the studies also creates uncertainty when evaluating patient outcomes. Thus, the accessibility and safety concerns that arise from Zynteglo prove that the viability of the treatment is still uncertain.
While Zynteglo has immense potential, it also has several drawbacks that still need to be addressed to improve the viability of the drug. One potential inclusion would be to minimize the immune risk associated with receiving Zynteglo, particularly during the busulfan myeloablative conditioning process. Busulfan myeloablative conditioning can lead to the following adverse side effects: hepatic veno-occlusive disease, interstitial pulmonary fibrosis, seizures, hyperpigmentation, emesis, wasting syndrome, thrombocytopenia, and medullary aplasia.21 As such, further research on this step is essential to improving Zynteglo’s safety profile.
However, it is important to note that Zynteglo is one of several gene therapies that have the potential to target TDT. For example, CASGEVY, a non-viral, ex vivo CRISPR-Cas9 gene edited cell therapy, recently received approval from the Medicines and Healthcare Products Regulatory Agency in the United Kingdom.22 Similar to Zynteglo, the treatment process involves the removal of autologous stem cells from the bone marrow. However, they are then genetically altered in a laboratory using CRISPR technology and returned to the patient.23 Currently, the treatment is awaiting further approval from the National Institute for Health and Care Excellence, with the decision likely to be finalized in April or May of 2024.22
Zynteglo has demonstrated promise across Phase 1/2 and Phase 3 clinical trials by reducing TDT patients’ dependence on blood transfusions. However, additional considerations still need to be taken to increase the overall accessibility of the drug and improve the safety profile in both short and long-term settings. Moreover, Zynteglo has become a model of what the future of gene therapy might hold, inspiring future treatments for TDT, such as CASGEVY, and hopefully improving the livelihoods of many patients to come.
REVIEWED BY: DR. JACK GAULDIE (CM, PhD, DSC, FRSC) & DR. MADELEINE VERHOVSEK (MD, FRCPC)
Dr. Jack Gauldie is a Professor Emeritus in the Department of Pathology & Molecular Medicine and the former Vice President of research at St. Joseph’s Hamilton. He has completed extensive research focusing on molecular manipulation for the treatment of many diseases including cancer, chronic lung disease, and arthritis.
Dr. Madeleine Verhovsek is the Chief of Medicine at St. Joseph’s Healthcare, with a specialty in hematology. She is also an Associate Professor in the Departments of Medicine and Pathology & Molecular Medicine at McMaster University.
1. Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5(1):11. Available from: doi:10.1186/1750-1172-5-11.
2. Udeze C, Maruszczyk K, Atter M, Lopez A. PB2339: Projected lifetime economic burden of transfusion dependent beta-thalassemia in the United States. Hemasphere. 2022;6(Suppl):2208-2209. Available from: doi:10.1097/01.HS9.0000852180.45597.87.
3. Wangi K, Birriel B, Smith C. Psychosocial burden in transfusion dependent beta-thalassemia patients and its impact on the quality of life and the problem of dignity. J Taibah Univ Med Sci. 2023;18(6):1217-1219. Available from: doi:10.1016/j.jtumed.2023.05.002.
4. Asghar AA, Khabir Y, Hashmi MR. Zynteglo: Betibeglogene autotemcel - an innovative therapy for ß-thalassemia patients. Ann Med Surg (Lond) . 2022;82:104624. Available from: doi:10.1016/j.amsu.2022.104624.
5. ZYNTEGLOTM (betibeglogene autotemcel). Mechanism of Action [Internet]. 2023. Available from: https://www.zynteglohcp.com/mechanism-of-action [cited 2023 Dec 24].
6. Thompson AA, Walters MC, Kwiatkowski J, et al. Gene therapy in patients with transfusiondependent ß-Thalassemia. N Engl J Med. 2018;378(16):1479-1493. Available from: doi:10.1056/NEJMoa1705342.
7. Committee for Medicinal Products for Human Use. Assessment Report: Zynteglo [Internet]. 2019 April 26. Available from: https://www.ema.europa.eu/en/documents/assessmentreport/zynteglo-epar-public-assessment-report_en.pdf [cited 2023 Dec 25].
8. Schneiderman J, Thompson AA, Walters MC, et al. Interim results from the phase 3 Hgb207 (Northstar-2) and Hgb-212 (Northstar-3) studies of betibeglogene autotemcel gene therapy (LentiGlobin) for the treatment of transfusion-dependent ß-Thalassemia. Biology of Blood and Marrow Transplantation. 2020;26(3, Supplement):S87-S88. Available from: doi:10.1016/j.bbmt.2019.12.588.
9. ZYNTEGLO. Zynteglo: Betibeglogene autotemcel. [Internet] 2023. Available from: https:// www.zynteglo.com [cited 2023 Dec 23].
10. Zynteglo (betibeglogne autotemcel). Wellmark [Internet]. 2023. Available from: https:// www.wellmark.com/-/media/sites/public/files/provider/pharmacy/zynteglo.pdf?sc_ lang=en&hash=03F70086EE707467DAB617DD845DE3E6 [cited 2023 Dec 23].
11. Philippidis A. After sparring with payers on pricing, bluebird flies out of Europe. Hum Gene Ther. 2021;32(17-18):868-871. Available from: doi:10.1089/hum.2021.29172.bfs.
12. Sheridan C. For hemophilia and thalassemia, a new era of “one-and-done” gene therapies has arrived. Nat Biotechnol. 2022;40(11):1531-1533. Available from: doi:10.1038/s41587022-01555-0.
13. De Luca M, Cossu G. Cost and availability of novel cell and gene therapies. EMBO reports 2023;24(2):e56661. Available from: doi:10.15252/embr.202256661.
14. Origa R. ß-Thalassemia. Genet Med. 2017;19(6):609-619. Available from: doi:10.1038/ gim.2016.173.
15. Smith, Yolanda. Thalassemia Prevalence. [Internet] 2022 Aug 30. Available from: https:// www.news-medical.net/health/Thalassemia-Prevalence.aspx [cited 2023 Dec 24].
16. Oleribe OO, Momoh J, Uzochukwu BS, et al. Identifying key challenges facing healthcare systems in Africa and potential solutions. IJGM. 2019;12:395-403. Available from: doi:10.2147/IJGM.S223882.
17. Boutayeb A. The impact of infectious diseases on the development of Africa. In: Preedy VR, Watson RR, eds. Handbook of Disease Burdens and Quality of Life Measures. Springer; 2010:1171-1188. Available from: doi:10.1007/978-0-387-78665-0_66.
18. Su L, Liu S, Li G, et al. Trends and characteristics of new drug approvals in China, 2011–2021. Ther Innov Regul Sci. 2023;57(2):343-351. Available from: doi:10.1007/s43441022-00472-3.
19. Food and Drug Administration. ZYNTEGLO (betibeglogene autotemcel) suspension for intravenous infusion [Internet]. 2022. Available from: https://www.fda.gov/media/160991/ download [cited 2023 Dec 25].
20. Common Terminology Criteria for Adverse Events (CTCAE). Published online 2017.
21. Patel R, Tadi P. Busulfan. StatPearls. 2022 [Internet]. Available from: http://www.ncbi.nlm. nih.gov/books/NBK555986/ [cited 2024 March 3].
22. Kmietowicz Z. Thalassaemia: NHS to offer stem cell transplants to adults who need transfusions. BMJ. 2023;383:p2837. Available from: doi:10.1136/bmj.p2837.
23. Wilkinson E. UK regulator approves “groundbreaking” gene treatment for sickle cell and ß -thalassaemia. BMJ. 2023;383:2706. Available from: doi:10.1136/bmj.p2706.
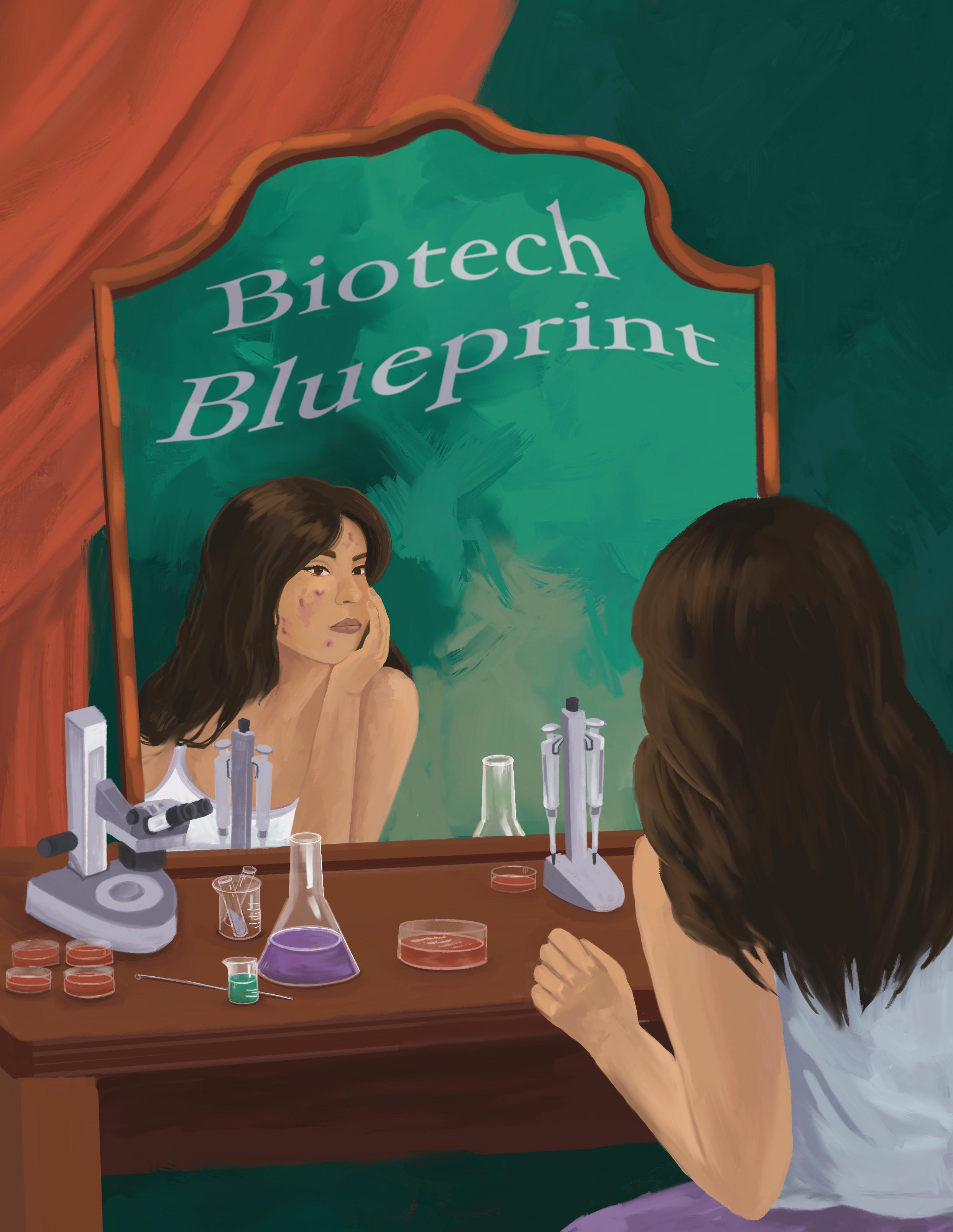 Magic Microbiota: Engineered Cutibacterium acnes
ARTIST: ARNICA KHATON 1
Magic Microbiota: Engineered Cutibacterium acnes
ARTIST: ARNICA KHATON 1
doi: 10.35493/medu.45.30
AARANI SELVAGANESH 2 & JACQUELINE CHEN 3
2Bachelor of Arts & Science (Honours), Class of 2027, McMaster University
3Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
The skin is the largest organ of the human body and home to millions of bacteria, fungi, and viruses. All these microorganisms make up the skin microbiota, which is essential in protecting individuals against invading pathogens.1 The skin microbiota exists in an equilibrium between commensal and pathogenic bacteria, which can cause disease when disturbed.1,2 Many bacterial strains are important parts of the skin microbiota including Cutibacterium acnes and Staphylococcus epidermidis.3 Though there are benefits to C. acnes, such as producing metabolites to fight infection, an abundance of certain strains of this bacteria is associated with acne vulgaris (acne), a common inflammatory disease affecting 85% of individuals aged 12 - 24.3,4 Acne has various treatments, depending on the individual’s age, skin colour, and severity of the infection.5 Typical treatments include topical retinoids and benzoyl peroxide, but in more severe cases, oral antibiotics, hormonal therapies, or oral isotretinoin may be prescribed.5 However, there can be drawbacks to some of these agents. Currently, severe acne cases are commonly treated with isotretinoin, a retinoid that increases production of the LCN2 gene that encodes neutrophil gelatinase-associated lipocalin (NGAL), a protein that induces sebocyte apoptosis to diminish acne symptoms. However, lipocalin can be associated with mood swings and weight change. Oral isotretinoin is also often associated with dryness of skin, lips, and eyes, as well as possible upregulation of liver enzymes.6 However, many advancements in understanding the skin microbiome have helped scientists understand skin conditions like acne from a novel lens. In an effort to develop new treatments for acne, advancements in using skin microbiota have been explored with promising results.
As one of the three main genera that inhabit the skin microbiota, the interplay between C. acnes and other microbial communities is essential for maintaining healthy skin.7 Predominantly found in sebaceous glands, C. acnes is critical in regulating skin homeostasis and preventing colonisation by other harmful pathogens.7 As a gram-positive bacterium, its genes encode for lipase enzymes, like triacylglycerol lipase and lysophospholipase.8 These enzymes aid in sebum lipid degradation, helping maintain an acidic skin pH.8 However, C. acnes has also long been implicated in the pathophysiology of acne due to its role in increased sebum production, hyperkeratinisation of the pilosebaceous unit, and inflammation.7 Still, research has shown no quantitative difference in C. acnes between subjects with and without acne, leading to hypotheses that some strains may improve skin health, whereas others may become pathogenic.8 Using sequence comparison of either recA or tly
genes, chosen based on their functions as a phylogenetic marker and for allowing bacteria to coexist with hosts, researchers categorized C. acnes strains into phylotypes IA, IB, II, and III.7,9 A 2010 study by Lomholt and Kilian identified that the phylotype IA was strongly associated with moderate to severe acne due to its preferential proliferation in inflammatory microenvironments.11 Contrastingly, IB, II, and III, were associated with healthy skin.11 These findings were later confirmed by other studies.7 As such, C. acnes presents as a popular therapeutic target for acne, given its critical role in skin microbiota flora.
A study conducted by Knödlseder et al. successfully utilised skin microbiota to treat acne by engineering commensal C. acnes to secrete NGAL.11 They identified secretion signals from endogenous proteins known to be highly secreted in C. acnes. 11 The LCN2 gene was then fused to the secretion signals and expressed from a strong promoter in C. acnes 11 When sebocytes were incubated with NGAL-secreting C. acnes cells, the C. acnes pBR13 protein significantly decreased sebum levels by around twofold after 48 hours.11 Lastly, researchers tested whether skin could be engrafted with the sebum-modulating C. acnes strain by topically applying 0.5% peptone in control, wild-type C. acnes, and the engineered NGAL-expressing C. acnes on the back of mice for three consecutive days.11 At each time point, Cutibacterium sp. was observed to be engrafted on mouse skin.11 The study also assessed the expression of inflammatory cytokines like IL-1β, IL-6, and tumor necrosis factor α for potential inflammation derived from C. acnes treatment, of which no significant differences were observed between treated groups.11
In order to address the antibiotic resistance crisis in developing engineered C. acnes, scientists have worked to remove antibiotic resistance cassettes from the bacterium.11 Antibiotic resistance cassettes are mobile genetic elements that can move around from one organism to another and provide resistance to certain antibiotics.13 Scientists typically try to avoid targeting antibiotic resistance cassettes in case they are transferred to other harmful organisms, making them resistant to some antibiotics. To mitigate this risk, scientists used dual selection to select the best organism. This process consists of using negative selection where bacterium without a certain trait are rejected and positive selection where those with a desired trait are accepted. First, they did a gene knock-out of the thymidine kinase (tdk) gene in C. acnes. The tdk-deficient strains of C. acnes are unable to metabolise 5'-fluoro-2'-deoxyuridine into a toxic compound that inhibits DNA and RNA production. Without synthesising this harmful compound, C. acnes strains retain the ability to produce DNA and RNA, facilitating their growth and enabling scientists to identify the tdk-deficient variants. Additionally, tdk-deficient C. acnes can become resistant to erythromycin, an antibiotic that can treat skin infections,
in the presence of an erythromycin-resistance cassette.11,12 By employing dual selection, scientists eliminate the need for reliance on antibiotic resistance cassettes to identify modified C. acnes bacteria, enhancing the safety of the microorganism.
Despite the modified C. acnes showing promise as a treatment for acne, the development of this modified microorganism is still in its early stages. The in vivo study conducted by Knödlseder et al. has its limitations with respect to clinical translation. Namely, mouse skin displays significant differences from human skin.11 In addition to being four times thinner than human skin, it is separated from underlying connective tissue and has more hair follicles.14 Although pig skin is a greater match due to the similarities in structure and healing, it is generally not used in research due to its high price, genetic heterogeneity, and lack of knowledge of its physiology relative to mice.14 To replace animal testing, human skin models containing immune cells and microbial populations are being developed to conduct ex vivo experiments. However, these models require further development to ensure accuracy.15
Engineered C. acnes also has potential for further research in the field of engineered microorganisms. While the development of engineered C. acnes is recent, this research opens doors to developing other modified microorganisms in the skin microbiome to benefit human health. For example, S. epidermidis, a bacteria in the skin microbiome, has been genetically engineered to produce melanoma tumour antigens.15 These antigens can provoke a sufficient immune response to kill aggressive metastatic and localised melanoma.15 Furthermore, engineered C. acnes opens up the door for further research to be done into the field of skin microbiota in order to better understand the interactions between the organisms and their host. Overall, the skin microbiota is a promising avenue for therapeutic development in treating acne and other diseases.
REVIEWED BY: DR. MOHANNAD ABU-HILAL (MD), DR. JACK GAULDIE (PhD), & KYLE JACKSON
Dr. Mohannad Abu-Hilal is an Associate Professor and serves as the head of the Dermatology Service at Hamilton Health Sciences Centre. He is the program director of the Advanced Clinical Dermatology fellowship program at McMaster University.
Dr. Jack Gauldie is a professor emeritus and the previous chair of the Department of Pathology and Molecular Medicine at McMaster University. He is a Member of the Order of Canada for his contributions to the health sciences.
Kyle Jackson is a PhD student in Chemical Engineering at McMaster University where he studies the use of bacteriophage viruses to combat bacterial infections.
EDITED BY: FLORENCE DENG & RUHANI KHATTRA1. Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nat Rev Microbiol. 2018;16(3):143–55. Available from: doi.10.1038/nrmicro.2017.157.
2. Singh B, Christina E. Bacterial metabolites: An unexplored quarry. mVOCs. 2021:205-34. doi:10.1016/B978-0-12-824523-1.00006-7.
3. Eisenstein M. The skin microbiome. Nature. 2020;588(7838):209. Available from: doi.10.1038/ d41586-020-03523-7.
4. Flowers L, Grice EA. The skin microbiota: Balancing risk and reward. Cell Host Microbe. 2020;28(2):190–200. Available from: doi.10.1016/j.chom.2020.06.017.
5. Eichenfield DZ, Sprague J, Eichenfield LF. Management of Acne Vulgaris: A review. JAMA. 2021;326(20):2055–67. Availablte from: doi:10.1001/jama.2021.17633.
6. Vallerand IA, Lewinson RT, Farris MS, Sibley CD, Ramien ML, Bulloch AGM, et al. Efficacy and adverse events of oral isotretinoin for acne: A systematic review. Br J Dermatol. 2018;178(1):76–85. Available from: doi:10.1111/bjd.15668.
7. Dréno B, Pécastaings S, Corvec S, Veraldi S, Khammari A, Roques C. Cutibacterium acnes (Propionibacterium acnes) and acne vulgaris: A brief look at the latest updates. JEADV. 2018;32:514. Available from: doi:10.1111/jdv.15043.
8. Platsidaki E, Dessinioti C. Recent advances in understanding Propionibacterium acnes (Cutibacterium acnes) in acne. F1000Research. 2018;7. Available from: doi:10.12688/f1000research.15659.1.
9. McDowell A. Over a decade of recA and tly gene sequence typing of the skin bacterium Propionibacterium acnes: What have we learnt? Microorganisms. 2017;6(1):1. Available from: doi:10.3390/microorganisms6010001.
10. Lomholt HB, Kilian M. Population genetic analysis of Propionibacterium acnes identifies a subpopulation and epidemic clones associated with acne. PLoS One 2010;5(8):e12277. Available from: doi:10.1371/journal.pone.0012277.
11. Knödlseder N, Fábrega MJ, Santos-Moreno J, Manils J, Toloza L, Marín Vilar M, et al. Delivery of a sebum modulator by an engineered skin microbe in mice. Nat Biotechnol 2024:1-6. Available from: doi:10.1038/s41587-023-02072-4.
12. Mayo Clinic. Erythromycin (Oral Route) Side Effects [Internet]. Available from: https://www. mayoclinic.org/drugs-supplements/erythromycin-oral-route/side-effects/drg-20075495?p=1.
13. Tran TQ, Park M, Lee JE, Kim SH, Jeong JH, Choy HE. Analysis of antibiotic resistance gene cassettes in a newly identified Salmonella enterica serovar Gallinarum strain in Korea. Mobile DNA. 2023;14(1):4. Available from: doi:10.1186/s13100-023-00292-8.
14. Zomer HD, Trentin AG. Skin wound healing in humans and mice: Challenges in translational research. J Dermatol Sci. 2018;90(1):3–12. Available from: doi:10.1016/j.jdermsci.2017.12.009.
15. Niehues H, Bouwstra JA, El Ghalbzouri A, Brandner JM, Zeeuwen PLJM, van den Bogaard EH. 3D skin models for 3R research: The potential of 3D reconstructed skin models to study skin barrier function. Exp Dermatol. 2018;27(5):501–11. Available from: doi:10.1111/exd.13531.

EDITORS-IN-CHIEF
Natalie Chu & Suraj Bansal
EDITORIAL BOARD
Managing Editors
Alex (Fan Ze) Wang, Anna McCracken, & Audrey Dong
Editors
Aarani Selvaganesh
Aditya Misra
Alina Pace
Angela Hong
Anya Kylas
Devlyn Sun
Dominic Gangemi
Florence Deng
Jacqueline Chen
Jia Lu
GRAPHICS & DESIGN
Creative Directors
Arim Yoo & Elaine Wang
Graphic Designers
Arnica Khaton
Ashley Low
Carol Wang
Christina Tam
Hamna Malik
Henin Ye
Katie Lin
Liza Nooristani
Matthew Olejarz
Olivia Kim
Parth Arora
Raymond Qu
Ria Patel
Ruhani Khattra
Sepehr Baharestan
Veronica Grignano
Zahra Tauseef
Brooke D’Mello
Charles Cai
Kavi Madan
Ken Yu
Mahitaj Rashid
VIDEO TEAM
Video Managers
Cindy Lin & Nishaad Sheth
Video Producers
Megan Lee
Ryan Liu
Serena Bansal
Shauna Vanderhorst
MEDUPROMO Directors
Serena Wei & Tharani De Silva
Medupromoters
Angeline Vo
Ishika Dhand
Lydia Su
Maya Thomas
Mishal Hossain
Nicole Kim
Stephanie Aleluya
Tiffany Xian
Yahan Lu
Zain Siddiqui

Bachelor of Health Sciences (Honours) Program
Michelle Giang
Veronica Grignano
Zackary McKay
MEDUCOLLAB Directors
Jacqueline Chen & Raymond Qu
MEDUFINANCE Directors
David Gou & Eric An MEDUEVENTS
Director
Florence Deng
SENIOR ADVISOR
Jeffrey Sun
ADDRESS The Meducator, BHSc (Honours) Program
Michael G. DeGroote Centre for Learning and Discovery Room 3308
Faculty of Health Sciences 1280 Main Street West Hamilton, Ontario L8N 3Z5
CONTACT US THROUGH EMAIL the.meducator@gmail.com
McMaster Student Union

Bachelor of Health Sciences Society

Office of the President

