










As we unveil the first ever issue of Medzine, we celebrate not only our artists’ incredible work, but also our dedication to addressing the systemic inequities embedded in medical representation. In the pages of Medzine, we are rewriting the narrative of who is seen, heard, and prioritized in healthcare.
To see ourselves reflected in the pages of medical textbooks is to see ourselves acknowledged, our struggles understood, our pain validated, and our bodies recognized as worthy of care. Unfortunately, for many communities, that reflection has been missing for far too long. A 2021 study revealed that only 4.5% of images in medical textbooks feature darker skin tones (Kaundinya & Kundu, 2021). When was the last time you saw keloids depicted on Black skin in a medical guide? Or cataracts shown in eyes that aren’t light blue? For those left unseen, this absence is more than an oversight. It is a silent dismissal that has rippled across generations, perpetuating a system where illness is frequently overlooked, misdiagnosed, or misunderstood.
This issue of Medzine is our way of breaking that ripple and giving a voice to those who have been unheard. Here, we’re putting those stories front and centre. The pieces in this issue reflect our mission to amplify the stories and bodies often missing from mainstream medical education. Cochlear implants, albinism, cataracts, glaucoma, burn injuries, bicuspid aortic valve, and keloids are more than just topics included in this issue, they’re lived experiences from real people. People with histories, communities, and skin tones that textbooks and posters fall short to represent.
We recognize that true equity in healthcare requires more than visibility alone. Representation must be coupled with dialogue, education, and compassion. Each illustration here is an invitation to consider how empathy must inform care, and how understanding must extend beyond what we can simply observe.
We are thankful to our 7 artists, executive members, reviewers, and the McMaster community for supporting this issue of Medzine. And to our readers, we hope these pages move you to listen more deeply, to see more fully, and to envision a future in which no one is left unseen.

ELAINE WANG HENIN YE
Bachelor of Health Sciences (Honours) Class of 2026, McMaster University

COVER AND TABLE OF CONTENTS ARTIST: ELAINE WANG1
Bachelor of Health Sciences (Honours), Class of 2026, McMaster University

Bachelor of Science (Honours) Class of 2026, McMaster University
ARTIST: Arim Yoo Bachelor of Health Sciences (Honours), Class of 2024, McMaster University



Cochlear implants are electronic devices that are surgically implanted to patients with profound hearing loss. The device consists of both external and internal components. The external components include the microphone, speech processor, and transmitter. Sound is received by the microphone, which is then selected and arranged by the speech processor. The transmitter receives the signals from the speech processor and converts them into electric impulses. Internally, the electric impulses are relayed through an
electrode array into the cochlea, bypassing cochlear hair cells, and stimulates the spiral ganglion neurons in the Its function contrasts from hearing aids which amplify sounds, by directly stimulating the auditory nerve instead of damaged portions of the ear. Cochlear implants can be used for a wide range of ages. The device has shown to improve sound discrimination in adults with conditions such as presbycusis (age-
For young children that are deaf or have severe hearing loss, early use of a cochlear implant can heighten their exposure to sounds for development of speech and language skills.1
1. What Are Cochlear Implants for Hearing? | NIDCD [Internet]. 2024 [cited 2024 Oct 10]. Available from:https://www.nidcd.nih.gov/health/cochlear-implants
2. Presbycusis - DynaMed [Internet]. [cited 2024 Oct 10]. Available from: https://www-dynamed-com. libaccess.lib.mcmaster.ca/condition/presbycusis#GUID-2118CF70-C2BB-45DA-B5E3-DA2937969573
REVIEWED BY: CATHERINE CHEUNG (BSc, MA)
Catherine Cheung is a scientific and medical illustrator at BioRender. She is dedicated to bringing complex medical and scientific concepts to life through visual storytelling with expertise in human and animal anatomy.
1Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
Keloids are types of thick, raised scars that form when the skin heals after an injury, growing beyond the boundaries of an original wound. They are common in people with darker skin complexion. The exact cause is unknown, but they usually form following skin injuries like lacerations, abrasions, burns, acne, or vaccinations. Keloids may also develop without history of injury, especially on the chest. They may be itchy, painful, or restrict movement if large.
Figure 1. A) Located on the chest, small size <10 cm2 B) Located on the chest, large size ≥10 cm2 and <40cm2 C) Located on the chest, patient with 2 total keloids. D) Located on the back, caused by infection. Ethnic Yoruba female age 89, age of onset 68, patient with >12 total keloids. E) Located on the underarm, caused by injuries with a sharp object. Ethnic Yoruba female age 54, age of onset 2, patient with 4 total keloids.
Figure 2. Located on the auricular region and cheek, caused by piercing on the earlobe and incision of an inflamed cyst, respectively. Male age 30. Figures not to size. Demographic information provided as available. Cross-referencing with additional sources was used to enhance accuracy of images due to low quality of reference materials. Relevant citations available online
REVIEWED BY: KIM NIPP (BSc, MSc)



Oculocutaneous albinism (OCA) is a genetic condition that affects melanin production, leading to lighter skin, hair, and eyes, along with vision impairments and heightened sun sensitivity. While often portrayed as a condition affecting white individuals, OCA exists in all populations, presenting differently across ethnic groups. In sub-Saharan Africa, OCA2 is the most common type, while OCA3, which causes reddish-brown hair and darker skin, is more prevalent in Black South Africans. OCA4 is frequently seen in East Asian communities, and cases in Indigenous and Latin American populations are often underreported. In BIPOC communities, albinism is not only a medical condition but also a socio-cultural experience marked by
Bachelor of Sciences (Honours), Class of 2026, McMaster University


distinct challenges. People with albinism in these communities often face unique problems, which are further worsened by societal barriers. These individuals may also experience misunderstandings about their condition, which can lead to harmful stigmas. In many African countries, people with albinism are subjected to myths that can make them targets for violence, exploitation, and human trafficking. In other parts of the world, such as Asia and Latin America, limited access to care, a lack of research, and the underreporting of cases contribute to inadequate healthcare and fewer support systems for those affected. As a result, they face not only the challenges of managing their condition but also the emotional toll of societal rejection and discrimination.
Albinism leads to several visual challenges, largely due to structural differences in the eye, with abnormal decussation of optic nerve fibers being a key factor. In a typical eye, around 55% of optic nerve fibers cross at the optic chiasm, aiding binocular vision and depth perception. However, in albinism, up to 80% of the fibers cross, disrupting normal visual processing and causing difficulties with depth perception. This results in a flattened, two-dimensional visual experience and challenges with tasks like judging distances or reading faces.
This abnormal routing of optic nerve fibers also impairs binocular fusion, where the brain struggles to merge the images from each eye, further impacting spatial awareness and fine motor skills. Additionally, this misrouting of optic nerve fibers can contribute to other common visual problems, such as strabismus (misaligned eyes), nystagmus (involuntary eye movements), and reduced visual acuity. The underdevelopment of the fovea, responsible for sharp, central vision, and the lack of retinal pigment that impacts light processing also greatly effects these issues.

eye, 45% of optic nerve fibers remain uncrossed, while 55% cross at the optic chiasm, aiding depth perception. In albinism, 80% of the fibers cross, disrupting depth perception and visual processing.

Figure 6. A comparison of skin cross-sections showing normal melanin production (left) and its absence in albinism (right). In normal skin, melanocytes produce melanin, which is transferred to keratinocytes for pigmentation and UV protection. In albinism, a mutation in the TYR gene disrupts melanin production, leaving both melanocytes and keratinocytes without pigment, increasing vulnerability to UV radiation.
REVIEWED
BY:
MARK BELAN (BSc, MSc)
Mark Belan is a scientific illustrator and data visualization specialist. With a background in geology and planetary science, he has worked with Scientific America, The Globe and Mail, and NASA to communicae science.
Melanin is a natural pigment found in the skin, hair, and eyes that gives them their color and protects the body from harmful ultraviolet (UV) radiation. It is produced by specialized cells called melanocytes, which convert the amino acid tyrosine into melanin through a process called melanogenesis. The more melanin produced, the darker the skin, hair, and eyes.
In individuals with albinism, a genetic mutation affects the production of melanin, leading to little to no pigment in the skin, hair, and eyes. This occurs because of a defect in the TYR gene, which encodes the enzyme tyrosinase, essential for the first step in melanin production. Without enough melanin, individuals with albinism are more vulnerable to sunburn, skin damage, and an increased risk of skin cancers due to the lack of UV protection. Although the lack of pigment in the skin and eyes is visible, individuals with albinism can have varying levels of impairment depending on the type of albinism they have.
ARTIST: NICOLE KIM1
1Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
Cataracts are the leading cause of blindness in Canada,1 and refer to when the eye’s lens becomes cloudy due to breakdown of proteins in the lens, causing blurry or less colourful vision.2 The most common cause of cataracts is age, as proteins in the lens naturally begin to degrade after age 40 and usually manifest as cloudiness around age 60.2 However, vision impairment may not present until years later.2
Glaucoma is another top cause of blindness in Canada.1 It is a disease that involves damage to the optic nerve, typically from increased intraocular pressure caused by fluid buildup in the eye.3 The most common type of this disease is called open-angle glaucoma (OAG), which is characterized by clogging of the eye’s fluid drainage system, resulting in a gradual pressure buildup that ultimately damages the optic nerve.4 Peripheral vision loss presents first, and slowly expands into the center.4 Another type of glaucoma is angle-closure or closed-angle glaucoma. This refers to when the iris blocks the drainage of fluid, causing IOP to rise suddenly and constituting an eye emergency.3 In such an acute attack, blindness can occur if treatment is not prompt.3
Racial and ethnic minorities have disproportionately higher rates of visual impairment compared to White Americans.5 Specifically, cataracts and glaucoma are more prevalent in Black, Hispanic, and Asian Americans compared to their White counterparts.5 The reason for this is multifactorial, stemming from factors such as ethnic differences in eye anatomy, underdiagnosis, socioeconomic barriers, underutilization of eye care, and a disparity in eye health literacy that stems from lesser access to eye health information.5
A mature cataract in a Black patient. The cataract has become large and dense, turning the lens opaque and greatly impairing vision.6 Compared to White patients, Black patients experience both delays in being diagnosed with cataracts and in receiving timely cataract surgery, while also being much less likely to receive a premium artificial lens to replace their old lens.7 These undue barriers are associated with worse vision loss and reduced quality of life.7

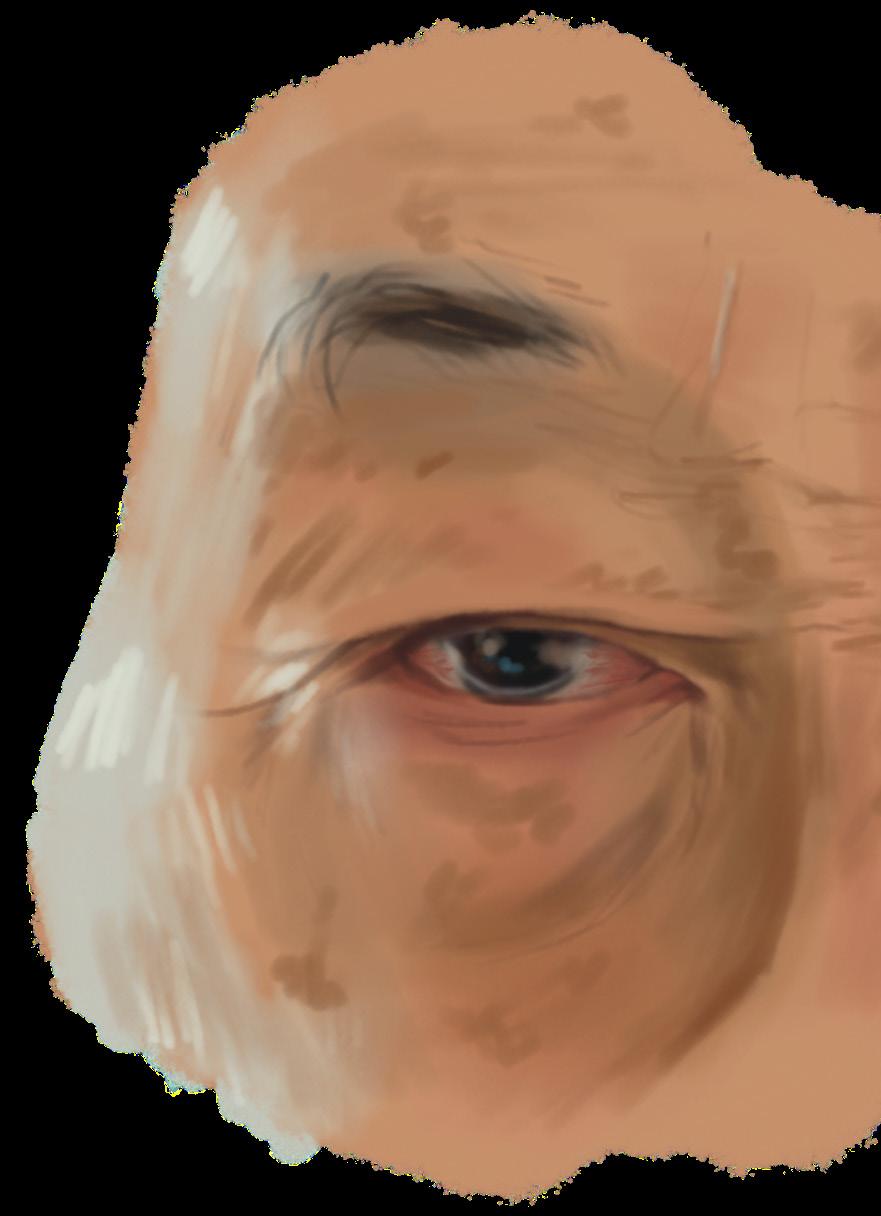
Dilated pupil and eye redness in East Asian patient with angleclosure glaucoma. While angle-closure glaucoma does not have many visible symptoms, some patients may notice a dilated pupil and/or eye redness among other symptoms.3,9 Asian populations, and East Asians in particular, commonly have the highest prevalence of this type of glaucoma.10 There exist anatomical differences in the eye between Asians and their White counterparts, such as narrower retinal vasculature, thicker irises, etc. in the former.10 However, their relevance to glaucoma pathogenesis is still poorly understood.10 Also problematic is that, despite higher prevalence of glaucoma in racial/ethnic minority groups, they remain inadequately represented in clinical trials.11
The optic nerve. The optic nerve is composed of many nerve fibers that pass through the back of the eye in a place called the lamina cribrosa, which is where damage from glaucoma is thought to occur.13 It has been found that a deeper anterior lamina cribrosa surface depth is associated with more severe glaucoma and higher IOP in those of African descent, offering one explanation for racial differences in glaucoma susceptibility.14


Cloudy lens characteristic of cataracts in a Hispanic patient. Hispanic individuals were found to have the least eye health knowledge and least access to such information. Lack of knowledge about personal risks for visual impairment is a barrier to comprehensive eye care services, and research shows that underutilization of eye care services is prevalent among Black and Hispanic populations, even when they have insurance.5 Moreover, financial and language barriers pose further challenges to receiving necessary eye care.8

1. CNIB [Internet]. [cited 2025 Feb 10]. Blindness in Canada. Available from: https://www.cnib.ca/ en/sight-loss-info/blindness/blindness-canada
2. American Academy of Ophthalmology [Internet]. 2024 [cited 2025 Feb 10]. What Are Cataracts? Available from: https://www.aao. org/eye-health/diseases/what-are-cataracts
3. American Academy of Ophthalmology [Internet]. 2024 [cited 2025 Feb 10]. Understanding Glaucoma: Symptoms, Causes, Diagnosis, Treatment. Available from: https://www.aao. org/eye-health/diseases/what-is-glaucoma
4. Cleveland Clinic [Internet]. [cited 2025 Feb 10]. What Is Open-Angle Glaucoma? Available from: https://my.clevelandclinic.org/health/diseases/ open-angle-glaucoma
5. Elam AR, Tseng VL, Rodriguez TM, Mike EV, Warren AK, Coleman AL. DISPARITIES IN VISION HEALTH AND EYE CARE. Ophthalmology. 2022 Oct;129(10):e89–113.
6. American Academy of Ophthalmology [Internet]. 2024 [cited 2025 Feb 10]. What Do Cataracts Look Like? Available from: https://www.aao. org/eye-health/diseases/cataracts-picturesvideos
7. Buscho SE, Sharifi A, Cayenne S, Zhang Y, Merkley KH, Gupta PK. Racial Disparities in Cataract Surgery Timeline and Intraocular Lens Selection: A Retrospective Study. Transl Vis Sci Technol. 2023 Nov 17;12(11):20.
8. Broman AT, Hafiz G, Muñoz B, Rodriguez J, Snyder R, Klein R, et al. Cataract and Barriers to Cataract Surgery in a US Hispanic Population: Proyecto VER. Archives of Ophthalmology. 2005 Sep 1;123(9):1231–6.
9. Contributors WE. WebMD. [cited 2025 Feb 10]. Glaucoma. Available from: https://www.webmd. com/eye-health/glaucoma-eyes
10. Belamkar A, Harris A, Oddone F, Verticchio Vercellin A, Fabczak-Kubicka A, Siesky B. Asian Race and Primary Open-Angle Glaucoma: Where Do We Stand? J Clin Med. 2022 Apr 28;11(9):2486.
11. Allison K, Patel DG, Greene L. Racial and Ethnic Disparities in Primary Open-Angle Glaucoma Clinical Trials. JAMA Netw Open. 2021 May 18;4(5):e218348.
12. Chen RI, Barbosa DT, Hsu CH, Porco TC, Lin SC. Ethnic differences in trabecular meshwork height by optical coherence tomography. JAMA Ophthalmol. 2015 Apr;133(4):437–41.
13. Lamina cribrosa - American Academy of Ophthalmology [Internet]. [cited 2025 Feb 10]. Available from: https://www.aao.org/ education/image/lamina-cribrosa
14. Girkin CA, Fazio MA, Bowd C, Medeiros FA, Weinreb RN, Liebmann JM, et al. Racial Differences in the Association of Anterior Lamina Cribrosa Surface Depth and Glaucoma Severity in the African Descent and Glaucoma Evaluation Study (ADAGES). Invest Ophthalmol Vis Sci. 2019 Oct;60(13):4496–502.
15. Wang SY, Melles R, Lin SC. The impact of central corneal thickness on the risk for glaucoma in a large multiethnic population. J Glaucoma. 2014 Dec;23(9):606–12.
16. Aghaian E, Choe JE, Lin S, Stamper RL. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology. 2004 Dec;111(12):2211–9.
Trabecular meshwork. This spongy tissue is where fluid typically drains through, but in OAG, the fluid is unable to drain properly.4 African American individuals were found to have a shorter trabecular meshwork height relative to White individuals, indicating a correlation with increased OAG risk.12
The cornea. Central corneal thickness (CCT) notoriously affects measurement of IOP, which is critical in glaucoma testing.15,16 Thinner corneas lead to underestimation of IOP, and thus underdiagnosis and undertreatment of glaucoma.15,16 Research suggests that thinner CCT may contribute to the increased risk of glaucoma seen in Black and Hispanic populations.15
Kim Nipp is a multidisciplinary designer, illustrator, animator, and communicator with a passion for translating complex scientific and healthcare concepts into engaging visual media. Her work spans multiple disciplines, from UX/UI designs and 3D modeling for healthcare softwares to creative illustrations for the educational and creative sectors.
1Honours Bachelor of Science (Biology Core), Class of 2025, McMaster University
Heart disease is the leading cause of death in North America and the risk of having or dying from these conditions varies by race¹. Indigenous, Black, and People of Colour (BIPOC) are more at risk for complications from heart disease than white Americans². This disparity is further exacerbated by systemic barriers in healthcare access, which contribute to higher mortality rates among BIPOC populations². The most common congenital cardiac defect is the Bicuspid Aortic Valve (BAV)³. Symptoms often manifest in adulthood and include chest pain, fatigue and weakness after increased activity, a heart murmur, shortness of breath, and lightheadedness or fainting.

Often, BAV leads to aortic stenosis, the thickening of the aortic valve that reduces or blocks blood flow to the aorta and the rest of the body⁴. Symptomatic aortic stenosis is a serious condition that requires medical intervention, as it is universally fatal if left untreated⁴. Aortic Valve Replacement (AVR) is the most common intervention for aortic valve stenosis or incompetence³. These valves can be replaced with bioprosthetic (bovine, porcine) or mechanical⁵.
ARTIST: CAMELA TEMACINI1
1Bachelors of Biochemistry (Honours), Class of 2027, McMaster University
While the pathogenesis remains incompletely understood, genetic and environmental factors are believed to play



1Bachelor of Health Sciences (Honours), Class of 2026, McMaster University
The severity of a burn injury is significantly correlated with the depth of injury.¹ Other key prognostic factors include total body surface area involved with burn, location of the injury, age of the patient, and comorbidities. Considering depth of a burn is often first identified based on the colour of the area, appearance plays a significant role in the quality of immediate treatment. Different levels of burn images have various color appearances.2 Superficial dermal burns only shows redness, is moist and weeping of skin. A partial thickness burn often presents a white or brown color, while a fullthickness burn usually has black areas of skin with a leathery texture. Studies have shown people of colour often associated with higher rates of burn injury and worse postburn recovery outcomes, possibly due to inaccuracy of initial diagnosis.3
BY:

Superficial: involves the epidermis
Partial thickness: affects the superficial dermis
Full thickness: damages the subcutaneaous layer and compromises the blood supply

1. U.S. Department of Health and Human Services. Burns. Radiation Emergency Medical Management. Published September 20, 2022. Accessed October 3, 2024. https://remm.hhs.gov/burns.htm
2. National Center for Biotechnology Information. Thermal Burns. StatPearls. National Institutes of Health. https://www.ncbi.nlm. nih.gov/books/NBK539773/. Published August 29, 2023. Accessed October 3, 2024.
3. DiPaolo N, Hulsebos IF, Yu J, Gillenwater TJ, Yenikomshian HA. Race and Ethnicity Influences Outcomes of Adult Burn Patients. J Burn Care Res. 2023;44(5):12231230. doi:10.1093/jbcr/irad033
4. Mayo Clinic Staff. Mayo Clinic Q and A: Treating Burns. Mayo Clinic News Network. https:// newsnetwork.mayoclinic.org/discussion/ mayo-clinic-q-and-a-treating-burns/. Published February 18, 2020. Accessed October 3, 2024.
