8 minute read
When Ya Gotta Go...
from TOPS June 2024
There are some topics that affect each and every one of us, yet we’re shy to discuss them in public. One of those taboo topics is euphemistically referred to as “staying regular.” Studies say around 4 million people in the US frequently have problems with constipation—to say nothing of the millions more who have occasional “tummy troubles” or “vacation belly”—so there’s no reason to stay secretive about the issue.
Many factors play into your bowel movements. We’re here to help you understand what’s causing constipation and what you can do about it.
What's Normal:
Doctors say that “normal” is pretty hard to gauge, as every body is a little different. The frequency of bowel movements isn’t a strong indicator, as it’s perfectly normal to poop anywhere from three times a day to three times a week. Instead, doctors are more concerned with how things go in the bathroom.
TMI warning: Bowel movements should be painless and not require any straining. While poop may change in firmness and color, it should ideally be medium brown and soft to firm. Any sudden, lingering change to your stool or the frequency of your BMs should be noted. Dry, pebbly or difficult-to-pass stool is a sure indicator of constipation, even if you’re going only slightly less frequently than what’s normal for you. Feeling bloated, having stomach pain or feeling like you’re not done going when you go are more symptoms.
If you’re concerned about your stool texture or frequency, talk to your doctor. There’s no need to be embarrassed; this is a perfectly normal doctor-patient conversation, and they’d love to help put your mind (and gut) at ease. Remember that changes in bowel movements can be a symptom of other conditions, so it’s an important health conversation to have!
Diet:
You know that what you eat affects your digestion. You’ve heard it said before that Americans routinely don’t get enough fiber in their diets, which contributes to constipation. It’s important to get both kinds of fiber, soluble (found in oats, beans, citrus, carrots and more) and insoluble (found in whole-wheat products, beans and veggies).
However, you may not know that certain food intolerances and allergies can impair digestion, causing either constipation or diarrhea—or sometimes, confusingly, both! For people who suffer from unpredictable digestion, doctors often suggest following a weeks-long elimination diet course. As the name suggests, you slowly eliminate specific potential allergens from your diet over the course of days or weeks, one at a time, and observe the changes.
Hydration:
Water is absolutely essential to so many life processes, including digestion. Dehydration is one of the most common—and most easily remedied—causes of constipation.
If you’re wondering why, the answer is that your large intestine needs water to keep things moving. If there isn’t enough water in your body to help it along, your intestine will leech water from your food waste. That results in hard stools, which can be difficult and painful to pass.
If you regularly consume alcoholic beverages, it’s important to know how they affect your digestion. Drinks with higher alcohol content tend to result in slower digestion and possibly constipation. Drinks with lower levels of alcohol tend to speed up digestion, leading to diarrhea. However, many people unknowingly have intolerances to wine and beer, which can cause all sorts of unpredictable digestive issues. That’s why it’s crucial to have water between drinks!
Exercise:
Physical activity helps food move through your intestines. Inactivity can slow digestion, resulting in fewer bowel movements. Walking, biking and yoga have all been proven to be helpful in digestion.
If you’re on doctor-ordered bed rest, talk to your healthcare team about what movements might be safe for you to perform. If you’re unable to do so, ask if a fiber supplement or other medication may be advisable to help keep your bowels healthy.
Hormones:
Stress hormones like cortisol can wreak havoc on the digestive system. Research shows that stress, anxiety and depression can greatly alter your body’s bowel movements. As we all know, stress can also cause some of the lifestyle factors—diet, alcohol consumption, lack of exercise—that cause constipation as well.
The regular fluctuations of premenopausal hormones can cause digestive symptoms. But for menopausal women, constipation is a common complaint; estrogen can help keep cortisol in check, so the decline of estrogen can mean cortisol rises unchecked in your system. The result is a longer digestive process, resulting in stool that is more difficult to pass. Weakened pelvic floor muscles can also be at fault.
Take steps to mitigate your stress. Meditation, yoga and other lifestyle changes can help. But also talk to your doctor and a mental health professional about your stress.
Health Conditions:
There are many health conditions that affect our digestion. It’s obvious that if you’re diagnosed with a gut disorder or viral infection, your bowel movements may not be normal or regular. But what’s less obvious is that a number of conditions affecting muscles and nerves can also cause digestive issues. On top of that, many medications cause changes in how our bodies digest or process food waste—even when those medications have nothing to do with treating our digestive systems. Antihistamines, antacids, antidepressants and even iron supplements can cause constipation. Talk to your doctor about how your overall health and current medications may affect your bowel movements.

Prebiotics & Probiotics:
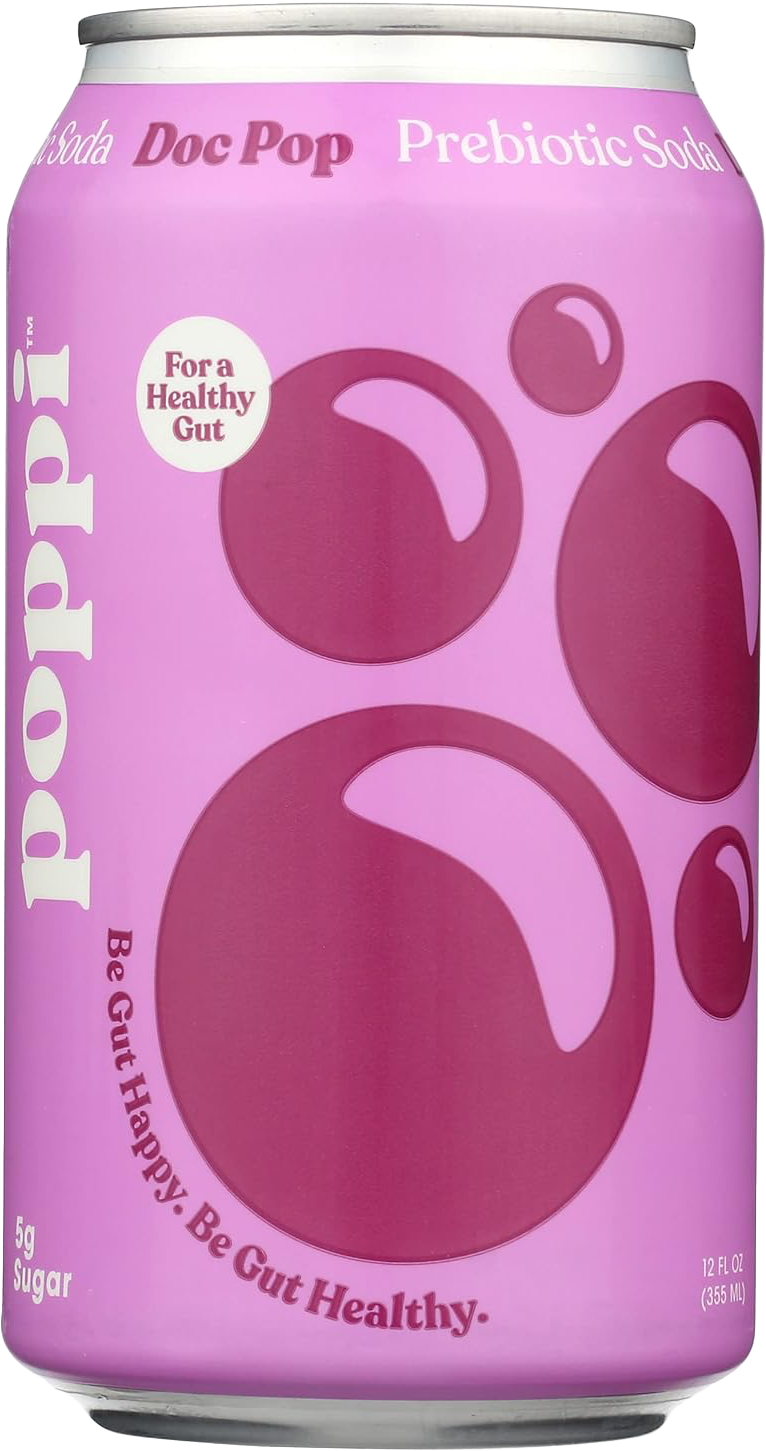
These products are very much on-trend right now. So what’s the deal? Probiotics contain live microorganisms that can help the “good” bacteria in your gut. Prebiotics act as food for those microflora, and help balance their population. Prebiotics are found in whole grains and produce, including bananas, greens, garlic and soybeans. Probiotics are found in certain cultured and fermented foods, like yogurt, sauerkraut and kimchi.
While research is ongoing regarding the exact role of gut bacteria—and the efficacy of products that contain probiotics and prebiotics—the general consensus seems to be that consuming natural prebiotics and postbiotics is a good thing, as those foods and drinks come with a host of proven health benefits. The jury is still out regarding supplements, but many people swear by them as a way to improve your overall digestive health.

Laxatives:
The medical consensus on laxatives seems to be that you should consult your doctor first. Laxatives can come with some serious health risks, particularly with long-term use. In the short term, they can cause electrolyte imbalances that can leave you feeling worse. Some supplements are marketed as “natural” laxatives, but most work one of four ways: drawing water to the bowels (osmotic), causing muscle contractions (stimulant), bulking agents/stool “softeners” and by coating stools (lubricant). Each comes with its own risks and side effects, though some can cause your body to become dependent on the product.

When to Call a Doctor:
Extreme changes to your bowel habits should raise a red flag. Talk to your doctor if symptoms last more than a week or are causing you pain or discomfort. Seek medical attention if you’re also experiencing abdominal pain, lower back pain, bloody stool, sudden weight loss, vomiting, severe pain, dehydration, fever or black, tar-like or thin stool.
Occasional bouts of constipation or diarrhea are normal. However, it’s always worth talking to your doctor about what’s going on with your body.

Get More Fiber:
Add fruit and veggies to your day. One of the easiest ways to get more fiber without much effort is to slip a few more veggies and fruits into your routine. If you’re making a sandwich, add in some chopped bell peppers or roasted beets, and use guacamole or hummus instead of your usual spread. Add chia seeds or flaxseed to your smoothies or oatmeal. At dinner, add on a veggie side, like coleslaw or broccoli. Stash baggies of pre-cut veggies and fruits in your purse for snacking.
Go for the grain. Swap whole-grain bread, brown rice and whole-wheat pasta into your rotation. If you struggle to eat breakfast, make overnight oats that you can grab and go. Choose high-fiber cereals and snacks.
Bean there, done that. Work beans and legumes into your dishes. From salads to spreads, mains to sides, beans can slide seamlessly into just about any meal.
Supplement. If you struggle with getting enough fiber through your diet, a fiber supplement may be just the thing. Talk to your doctor before adding them to your routine, as they can affect certain medications.