
INSIDE:
Strengthening the workforce
pg. 10
Sparking dialog and change through photography pg. 16 Mosquito-borne disease and climate change pg. 20 UNIVERSITY AT ALBANY COLLEGE OF


INSIDE:
Strengthening the workforce
pg. 10
Sparking dialog and change through photography pg. 16 Mosquito-borne disease and climate change pg. 20 UNIVERSITY AT ALBANY COLLEGE OF

Messages from the deans and health commissioner College timeline About the college Strengthening the workforce
Our population is aging Veteran peer-to-peer support
Using photography as a social work and public health tool
Mosquitos and climate change
Additional areas of expertise
As 2024 comes to a close, the need for social and health equity has never been more urgent. Complex challenges—ranging from health disparities to social injustice— make it essential that we work together to conduct research, implement interdisciplinary programs and solutions, and engage innovatively with the communities we serve to improve health and wellbeing.
With this in mind, the University at Albany created the new College of Integrated Health Sciences in 2024. This forward-thinking college, which includes the School of Social Welfare and the former School of Public Health, brings together expertise in nursing, public health, biomedical sciences and social welfare to train the next generation of public health and social work professionals and to enhance the current workforce, with a focus on being responsive to all members of our community. Whether we are working with rural populations, older adults, children who are neurodivergent, marginalized or underrecognized groups, veterans, immigrants and refugees, or other groups, we focus on mindful and impactful research and interventions to improve health for all.
In the following pages, we invite you to learn more about our work, including our close relationship with over 475 partner organizations. Of note, we’ve partnered with the New York State Department of Health for 40 years, a collaboration nationally recognized as a trailblazing model for government and academic collaboration. This is an exciting time to be a part of the College of Integrated Health Sciences at UAlbany.
Erin M. Bell
Dean,CollegeofIntegratedHealthSciences
Victoria M. Rizzo
SeniorViceDeanandDirector,SchoolofSocial Welfare

At the New York State Department of Health, we define health as a state of optimal physical, mental and social well-being. As 2025 comes into focus, it is important we keep our attention on achieving health for all.
Our mission is “to protect and promote the health and well-being for all, built on a foundation of health equity.” This mission is designed to endure, and reflects the many essential public health services required to achieve health for all New Yorkers. A mission is more than a simple saying on a poster or strategic plan; it is a vital tool to align large organizations around a common and noble purpose during good times and challenging ones. We value our 40-year relationship with SUNY as a critical partner in this push for public health, and look forward to our ongoing collaboration with the College of Integrated Health Sciences.
Public health has had challenges since the dawn of time. They may have changed, yet they persist.
Dr. Lewis, our state’s first health commissioner, fought the uphill battle to help New Yorkers achieve something we take for granted—protection from diphtheria. His work led to the creation of the Wadsworth Center, the world’s premier public health laboratory. The health benefits of vaccines are apparent, yet only possible because of persistent hard work, which included navigating politics, economics and public persuasion.
We face multiple challenges today; we live in extraordinary times. Science is on the cusp of curing once incurable diseases, preventing terrible outbreaks and delivering health care on increasingly complex disorders. It is a great time to be in public health, a great time to be in science and a great time to help all people achieve health.
James McDonald CommissionerofHealth,NewYorkStateDepartment ofHealth






Now combined as the new College of Integrated Health Sciences, the School of Social Welfare (SSW) and the former School of Public Health (SPH) both have long histories, founded 60 and 40 years ago, respectively.
On the following pages, you’ll find just a few examples of the many noteworthy happenings at the SPH and SSW since their founding. For a more in depth timeline, visit albany.edu/cihs.


In 1985, the School of Public Health (SPH) was created by Health Commissioner David Axelrod in partnership with UAlbany president Vincent O’Leary to train students directly within the state health department and its worldrenowned Wadsworth Center laboratories.
The same year, a shift in methods of working with individuals and families took place in the social work field. SSW Distinguished Professor William Reid was renowned as the inventor of the task-centered approach to social work, a pioneering method and philosophy of practice that led to the shift in methods.
In 1987, the SPH began collaborating with the Akwesasne Mohawk to determine how the community was exposed to PCBs and the health effects from PCB exposure.
Numerous studies took place over the next 35 years.
The partnership placed emphasis on sustainability of intercultural collaboration, including strategies that help promote equity between partners (such as hiring community members as key personnel, integrating local expertise into research design, and developing local community outreach programs).
The collaboration continues to this day, even though data collection has ended.
The School of Social Welfare (SSW) was founded in 1964 and celebrates 60 years of impact this year. Through our research, teaching and community engagement on local, national and global levels, SSW promotes social, economic, and environmental justice, human rights, and the improvement of human wellbeing. (Pictured above: UAlbany’s Downtown Campus, home to SSW.)


In 1966, with support from the Children’s Bureau of the U.S. Department of Health, the SSW established training units in two county public welfare offices.
In 1967, the first graduates of the SSW—25 students who earned a Master of Social Work (MSW)— crossed the commencement stage.
(Pictured below and above: one of SSW’s first graduating classes.)
After protests in the 1960s, UAlbany's Community and Public Service Program was developed in 1971, in which students volunteer at non-profits or public organizations.
SSW faculty organized the structure of the program for the University, with the ideas of student service to the community and civic responsibility as central features. Today, students receive academic credit for participating in the program.
In 1991, over 100 stations on National Public Radio carried UAlbany’s Public Radio Health Show.
The radio show was hosted by founding dean of the SPH, David Carpenter, and discussed new developments and research in public health.
(Pictured right: yearbook photos of students in the Department of Biomedical Sciences and the Department of Environmental Health and Toxicology, now called the Department of Environmental Health Sciences)





SSW’s Shirley Jones (pictured above) became the University’s first African American woman to be awarded the rank of distinguished service professor, a designation for eminent faculty conferred by the State University of New York Board of Trustees.
SPH and NYSDOH researchers through the Cardiac Services Program found in 1999 that African American cardiac patients were recommended at a significantly lower rather for angioplasty and coronary artery bypass graft surgery than other patients. Their 2004 study reviewed recommendations from referring cardiologists to determine if the recommendations were in line with national guidelines to improve service equity.

The Axelrod Fellowship was created to support future public health professionals.
The Axelrod Fellowship, still available to students today, was created in memory of David Axelrod and is a full tuition scholarship for the first year of UAlbany’s Master of Public Health (MPH) program. The first recipient of the fellowship studied access to health care services in Mongolia, along with stress and its relationship to the onset of disease in the Mongolian population.
West Nile Virus was first detected in New York in 1999. Professor Millicent Eidson, the State Public Health Veterinarian and Director of the Zoonoses Program at the NYSDOH, was a part of the core team that investigated West Nile Virus and its spread. Lessons learned from this response have been used to teach generations of public health students.
The same year, social work students and faculty began collaborating with South Korean colleagues. A formal “study tour” exchange began, in which students from UAlbany and Hallym University in South Korea spend one-to-two weeks at the other university to better understand different approaches to service delivery and social work practices.
The public health infrastructure was strengthened in New York by a commitment in the governor’s executive budget.
The NYSDOH recognized UAlbany as the leader in public health higher education, leading to the creation of the Public Health Leaders of Tomorrow Program, which offers tuition assistance for State and Local Health Department employees to take academic coursework at UAlbany.

The Social Workers live talk radio show launched on 90.9 FM. The UAlbany-based show highlights current social work topics, including trends and services. (Pictured below: co-hosts Eric Hardiman and Alyssa Lotmore in the recording studio).

The Schools of Social Welfare and Public Health unveiled new online health care courses aimed at building New York’s workforce. The courses extended the undergraduate field placement program in social work to regions of New York targeted for workforce growth and added a healthcare analytics track in public health continuing education.
Public health professionals noted the need for an enhanced maternal and child health workforce. A foundational academic-practice partnership was developed with the NYSDOH Division of Family Health. This led to the joint application and award of a HRSA Maternal and Child Health Public Health Catalyst Program grant in 2015, leading to the creation of the Maternal and Child Health Program at UAlbany.
In 1999, UAlbany was selected to prepare gerontological social workers. The Internships in Aging Project was developed with initial funding from the John A. Hartford Foundation as an innovative model to provide students with a solid foundation of social work skills within an aging specialization.
Local public health directors noted a lack of available quality public health education opportunities. In response, the Center for Public Health Continuing Education worked with the New York State Assocation of County Health Officials, the New York State Nurses Association, and the NYSDOH’s Office of Public Health Practice to initiate what was then called the “Third Thursday Breakfast Broadcast (T2B2),” originally transmitted via satellite uplink.
In 2004, the Center was recognized for quality online and video productions by those within the television and online video industry, winning their first of 9 Telly Awards for Public Health Live!, a webcast for public health and health care professionals interested in furthering their knowledge on current public health issues. (Pictured right: VHS tapes from the Center for Public Health Continuing Education).
In 2007, Professor Kurunthachalam Kannan in the Department of Environmental Health Sciences was the first to develop a method to extract and analyze persistent organic pollutants in dried blood spots, collected from the state’s newborn screening program. The method was later applied to the NIEHS funded Upstate KIDS study (pictured left) to determine chemical exposures in newborn babies across New York.


In 2009, a new H1N1 virus—often called swine flu— began causing human illness and became a pandemic. UAlbany students secured fellowships from the CDC to embed within the NYSDOH to help develop H1N1 preparedness efforts to minimize outbreaks.
In 2010, students began visiting Costa Rica annually through UAlbany's Center for Global Health. The Comparative Health System Exchange Program in partnership with the University of Costa Rica enabled students from each university to visit the other country and learn about their respective health care system.
Pictured left: MPH student Kimberly Thompson in Costa Rica during a faculty-led trip.


Medicaid’s delivery system reform incentive program was launched in 2015 to reduce the cost of care and improve health outcomes for more than five million New Yorkers. From 2016-2021, UAlbany led a team to conduct an independent evaluation of the program and determine its success.
Professor Katharine Briar-Lawson (pictured left) received the International Rhoda G. Sarnat Award from the National Association of Social Workers. This prestigious award is given to an individual, group, or organization that has significantly advanced the public image of professional social work.
Joachim Frank won the Nobel Prize in chemistry.
Frank was one of three scientists awarded for developing cryo-electron microscopy, which simplifies and improves the imaging of biomolecules, allowing the image generation of everything from proteins that cause antibiotic resistance to the surface of the Zika virus.
As a scientist at the Wadsworth Center at the NYSDOH, Frank held an appointment in UAlbany’s Department of Biomedical Sciences from 1985 to 2008.

DrPH student Kathryn Mishkin developed a policy for the American Public Health Association - a not-for-profit widely regarded as the only public health organization that influences federal policy in the U.S. The new policy, aimed at curbing childhood diarrhea, was adopted by APHA’s governing council in 2018.
In 2016, Assistant Professor Tabassum Insaf’s (pictured left) team found that the threshold for heat advisories in New York was too high when issued at 100 degrees Fahrenheit, a threshold developed based on national data. Using New York data taken from satellites, their work led the heat advisory criteria in the state to be lowered by five degrees in 2018.
With the onset of the COVID-19 pandemic, teams from UAlbany were quickly embedded within the health department to assist with response, made possible due to the already close relationship in place. Research from SPH and SSW faculty, staff and students included:
• Analyzing the effectiveness of hydroxychloroquine and azithromycin for treatment.
• Better understanding the relationship between multisystem inflammatory syndrome in children (MIS-C) and COVID-19.
• Impact of school closures on vulnerable children.
• Mental health for parents and caregivers.
• Optimal points of intervention to address racial and ethnic disparities in fatality rates.
• Social support from churches and communities.
• The development of a low-cost assay for COVID-19.
• The prevelance of COVID-19, including infections and hospitalizations, and where disparities emerged.

Grace Claxton graduated with her bachelor’s degree in public health with a minor in business in 2017.
She also competed in the 2016 Olympics in Rio and the 2024 olympics in Paris, representing Puerto Rico. She was inducted into the UAlbany Athletics Hall of Fame in September. (Pictured left: Grace Claxton, photo courtesy Brian Busher)
The SSW received $24 million to lead the National Child Welfare Workforce Institute for the next 5 years, led by the school since 2008. The institute helps child welfare agencies recruit and retain skilled workers. (Pictured below: a child welfare case worker providing support to a family)


A local nursing home, Our Lady of Mercy Life Center, installed an artificial sky in one of its patient care wings — the first such facility in the United States to do so. MPH student Alexandra Smith applied for the grant for the sky, oversaw the installation, and conducted research to evaluate the sky’s impact on residents.



Students were on the ground in our communities. They volunteered as contact tracers and information translators, helped health departments and non-profits with pandemic response, and modified and implemented public health and social work programming to help with issues aggravated by the coronavirus, such as food insecurity.

UAlbany launched two nursing programs to kick off the start of the nursing unit, housed under the former SPH.
The Bachelor of Science in Nursing completion program and the Master of Science in Population Health Nursing were developed to help alleviate the nurse shortage in New York.
The newly established Axelrod Award in Public Health drew in significant nominations from across the nation.
Now each year, an outstanding public health practitioner is recognized for contributions to the public health field in line with David Axelrod’s vision for close collaboration between academia and government.
(Pictured left: Recipient Mona Hanna-Attisha, who helped to uncover the Flint water crisis in Michigan)
The SSW continued to host the annual Katharine Briar-Lawson lecture, started in 2017, which was designed to educate the UAlbany campus and surrounding communities on a broad range of topics related to the research and practice of social work.
• 2020: Aybe Tasse presented on a tranformative approach for social and economic integration of vulnerable communities
2021: Joy DeGruy presented on white supremacy
• 2022: Loretta Ross presented on lessons from a lifetime of feminist and anti-racist activism
• 2023: Melanie Sage presented on algorithms in social work
Distinguished Professor JoEllen Welsh (pictured right) received initial funding from the National Institutes of Health in 1999 to study vitamin D and cancer, leading to 25+ years of funding.
As a leader in vitamin D and cancer research, JoEllen Welsh has extensively characterized the impact of vitamin D and the vitamin D receptor, a protein found within most cells, on breast cancer development and progression.
Her work takes place within UAlbany’s Cancer Research Center, housed within the College of Integrated Health Sciences.

In 2024, the School of Social Welfare and the School of Public Health integrated to become the College of Integrated Health Sciences, which advances well-being for all through interdisciplinary, practice-based education, research, scholarship, and meaningful community engagement to achieve social justice and equity, locally and globally.







• Adverse childhood experiences
• Advocacy
• Aging and gerontology
• Cancer epidemiology and genomics
• Child welfare
• Environmental, economic, and social justice
• Evidence-based healthcare
• Food systems and sustainability
• Health disparities and health equity
• Human health and the environment
• HIV policy and prevention
• Infectious diseases
• LGBTQ+ mental and behavioral health disparities
• Maternal and child health
• Participatory and arts-based research
• Racial equity
• Social epidemiology and social determinants
• of health
• Vector-borne disease
• Veteran peer support
• Violence and addiction
• Youth development and support
updates and announcements
• New 1+2+1 nursing program: Offered in partnership with St. Peters Health Partners, students in the new “1+2+1” program will simultaneously work toward two degrees: an Associate Degree in Nursing and a Bachelor of Science in Nursing.
• New Master of Social Work (MSW) curriculum: Continuing our strong focus on social justice and inclusivity, our newly approved Master of Social Work curriculum eliminates traditional concentration divisions, offering a comprehensive approach that integrates micro, mezzo, and macro levels of social work practice within courses, rather than as individual concentrations. This groundbreaking model prepares students to engage in holistic, impactful social work, equipping them to address individual, community and policy challenges.
• Department of Biomedical Sciences
• Department of Environmental Health Sciences
• Department of Epidemiology and Biostatistics
• Department of Health Policy, Management & Behavior
• Nursing Unit
• School of Social Welfare
• Cancer Research Center
• Capital Region Medical Research Institute
• Cardiac Quality Improvement Initiative
• Center for Aging and Policy Studies
• Center for Collaborative HIV Research in Policy and Practice
• Center for Health Workforce Studies
• Center for Innovation in Mental Health Research
• Center for Public Health Continuing Education
• Center for Public Health Preparedness
• National Center for Excellence in Homeless Services
• National Child Welfare Workforce Initiative
• Social Work Education Consortium
• Center for Healthy Aging
• Center for the Elimination of Minority Health Disparties
• Global Center for AI in Mental Health
• Institute for Social and Health Equity
• Center for Global Health: proactively engages with a wide range of partners around the world to create educational programs, collaborative research initiatives, and health promotion interventions.
• (Pictured below: a faculty-led trip to partners in Costa Rica for students to learn about the Costa Rican healthcare system)

• Maternal and Child Health Program: offers courses, funds student practica and internships, hosts seminars and networking events, and supports participation in conferences locally and nationally.
28 academic programs within the college, including undergraduate and graduate programs.
1,012students enrolled in acacemic programs, including online and part-time study.
197
expert faculty working in public health, social work, nursing, and biomedical sciences
475+
partner organizations, including a foundational partnership with the New York State Department of Health

At the College of Integrated Health Sciences, we monitor and study the social work and public health workforces while utilizing some of the best and brightest minds—including at the NYSDOH— to train both current professionals and students who are just entering the field. This pronged approach to understanding and enhancing the workforce ensures that, in collaboration with our partners, we’re setting the foundation for true momentum towards social and health equity in our communities.
• To prepare organizations, policy makers and other stakeholders for workforce needs, the Center for Health Workforce Studies—created in 1996— provides information on the supply, demand, distribution and use of health workers to support and promote health workforce planning and policymaking at local, regional, state and national levels. The center’s work spans many areas of the workforce, including workforce planning and service delivery.
• The Cardiac Services Program, an initiative of the NYSDOH based out of UAlbany since 1990, monitors service delivery for cardiovascular medical procedures. It was the first public reporting initiative for cardiac outcomes and established New York as a leader in outcomes assessment. The program has led to increased service equity, a better understanding of how regulations impact outcomes, information for hospitals and physicians to use to improve processes, and data for patients to make informed decisions about their care.
• Pass rates for the ASWB licensing exam for social work have a significant impact on the workforce. First time pass rates were studied by the New York State Association of Deans and Directors of Schools of Social Work in collaboration with the National Association of Social Workers’ Center for Workforce Studies, and findings suggested the exam was biased. Now, a national taskforce is addressing this issue, and UAlbany’s Victoria M. Rizzo is a part of this work and also served as the president of the New York State Association of Deans and Directors of Schools of Social Work while the study was conducted.

• For nearly 30 years, the Center for Public Health Continuing Education has provided the workforce with the knowledge and skills to address evolving challenges in the field. The Center has several interactive, self-paced courses that are a part of various required training/professional development programs, including for the CDC, the NYSDOH, and state and local health departments across the U.S. In addition, the Center is nationally recognized for its award-winning Public Health Live! webcast series, which features state and national experts and utilize best practices in educational design and delivery.
(Pictured above: Adaora Otiji from the D.C. Department of Health, Omar Khalid, director of workforce development at the Association of State and Territorial Health Officials and Public Health Live! moderator Rachel Breidster.)
• The NYS Fellowship in Applied Public Health is a specialized public health training program that prepares physicians, veterinarians, and midwives for leadership roles in health departments. In this program, jointly sponsored by UAlbany and the NYSDOH, fellows earn a Master of Public Health (MPH) degree alongside extensive mentored practicum experiences at the NYSDOH and a local county health department (See page 32).
• The Public Health Leaders of Tomorrow (PHLOT) program, supported by the Governor’s executive budget, provides tuition assistance for state and local health department employees to take academic coursework at the College and promotes leadership development activities for students preparing for public health careers in NYS government.
• Academic programming at the College is strategically designed to fill workforce gaps and provide pathways for students to gain knowledge, skills and employment. Our location in New York’s capital provides ample opportunities for handson learning, including with government agencies. Many students receive job offers from their experiences in the field. In fact, 34 percent of our Master of Public Health (MPH) students receive job offers directly from their internship sites.
• In the late 1990s, the former School of Public Health offered its first set of courses for academic credit via distance learning, which grew into a catalog of public health courses and expanded into a formal online graduate certificate program in 2004. Similarly, the School of Social Welfare has offered online courses for academic credit since 1999. Today, students can complete graduate certificates, a Master of Public Health, and a Master of Social Work online. These options enhance access for all students, particularly those in rural areas where social work and public health expertise are greatly needed.
• Students are prepared to be interdisciplinary and thoughtful practitioners through nursing, social work and public health courses, enabling them to work successfully following graduation with a wide range of communities and professionals.
(Pictured


30,000+ online public health training course completions since January 1, 2024 through the Center for Public Health Continuing Education
62 physicians and other advanced licensed health care professionals have received their MPH through the Fellowship in Applied Public Health (formerly the NYS Preventive Medicine Residency Program)
37 county public health directors in New York State have completed coursework at the College through the PHLOT program
25+ years of online distance learning options offered in public health and social welfare
andwemustbeprepared

In 2022, there were 58 million Americans over the age of 65— that number is projected to increase to 82 million by 2050.
“This will have huge implications for how we live,” says Victoria Rizzo, professor, senior vice dean and director of the School of Social Welfare at the College of Integrated Health Sciences. “There are workforce implications as well— huge numbers of adults retiring, not enough workers to fill their jobs, a significant loss of wisdom across professions, and an increased need for a focus on gerontology and age-related issues in the fields of social work, public health and nursing.”
As the population ages, poverty among older New Yorkers is also on the rise, as is the proportion of older residents from historically minoritized backgrounds who face social and health disparities. Public health, nursing and social work professionals will play a critical role in addressing these challenges over the coming years.
“Working together across multiple disciplines will allow us to develop effective and creative solutions to accessibility of care, chronic disease prevention and management, worker and caregiver support and burnout, and other areas of importance for healthy aging,” Rizzo says.
In 2023, UAlbany launched the Healthy Aging Initiative, an inter-institutional and interdisciplinary network focused on advancing knowledge about aging and translating that new knowledge into practice, education and workforce development. The initiative leverages the university’s longstanding strengths in the biological sciences, public health, social welfare, public policy, emergency preparedness, cybersecurity, engineering, RNA research and nursing.
Now, the University has taken its commitment to healthy aging even further with the creation of the Center for Healthy Aging in fall 2024, comprised of faculty from various disciplines, with a significant pull from the College of Integrated Health Sciences.
Directed by Rizzo, the Center for Healthy Aging aims to improve all aspects of aging, prevent age related diseases, and decrease the economic burden of age related pathological and social disorders. It serves as a hub for cutting-edge research, training and comprehensive programs that promote healthy aging and prevent age-related diseases by bringing researchers and community partners together— strengthened by UAlbany’s existing partnerships with state and local governments, non-profit organizations, hospitals and the New York State Department of Health.
Research in the Center focuses on developing and implementing evidence-based interventions, evaluations of workforce training, substance use, social isolation, elder abuse and healthy longevity.
“Our School of Social Welfare has a long history of agingfocused intervention research and workforce training,” Rizzo explains. “Now, through the Center for Healthy Aging, social work, nursing and public health faculty are collaborating with researchers from across the University to build research collaborations that will benefit older adults now and in the future."
Of note, the Center works closely with the Center for the Elimination of Minority Health Disparities, directed by the College of Integrated Health Sciences’ Elizabeth Vásquez.
“While we know that there are going to be challenges brought forth from our increasing older population, it’s important to note that aging isn’t all about pathology and illness,” Rizzo says. “People do amazing, incredible things as they age, and by striving for social, physical and emotional wellbeing for our older adults, we’re ensuring that they’re able to thrive in all that they do.”

In 2000, School of Social Welfare faculty created the Internships in Aging Project to address the need for additional trained social workers for older adults. Through this program, Master of Social Work (MSW) students provide social services to older adults in the Capital District and the rural northeastern region of New York. In addition to addressing the critical need for geriatric social workers, the project helps to identify service gaps and to develop new services to older persons.
5,000+
hours of social services provided each year to older adults throught the Internships in Aging Project
289
alumni of the Internships in Aging Project making a difference in their communities
25
years of the Internships in Aging Project will be celebrated in 2025!


In 2023, the U.S. Department of Veterans Affairs reported 6,042 deaths by suicide among U.S. veterans during 2021. While services are available to help veterans with their mental health, Eric Hardiman, associate professor in the School of Social Welfare, notes that many veterans avoid traditional providerdelivered mental health services due to stigma, previous negative experiences and excessive paperwork.
“Veterans repeatedly have told us that they feel misunderstood in the civilian world and struggle with a range of challenges navigating the transition from military to civilian life,” says Hardiman, who has studied peer-to-peer support extensively throughout his social work career. “It’s common amongst the veteran experience to lack a mission or purpose and feel adrift without others who can understand their situation.”
Hardiman leads an ongoing evaluation of the Joseph P. Dwyer Veterans Peer Support Program, an initiative designed in 2012 by the New York State Office of Mental Health and the State Department of Veterans Services to help veterans overcome these challenges by providing peer-to-peer support and non-clinical services that foster community, connection and well-being. As of 2023, the program is funded in the state budget for all 62 counties in New York.

Fully volunteer-run and requiring minimal paperwork to enroll, veterans can connect with other veterans through the program, attend group meetings, take part in social events, and engage in other opportunities that are offered. Participants can choose their level of involvement, creating a supportive environment free from the stigma often associated with seeking mental health care. As a result, the program has been particularly successful in reaching veterans who might otherwise avoid traditional services.
“Evaluating the Dwyer program is essential to understanding what works and where we can improve services and reduce barriers,” says Hardiman.
The evaluation team collects both quantitative and qualitative data, providing a comprehensive view of how each county’s program is being implemented and where adjustments may be needed. They also conduct interviews with program directors and meet weekly with the Office of Mental Health and the Department of Veteran Services.
“The impact of the program is profound,” Hardiman notes. “Even though it’s difficult to measure the full extent of its success—because the life-changing work these programs do can’t always be quantified—it’s clear that, for many veterans, these programs can mean the difference between life and death; between isolation and connection.”


The evaluation helped to secure permanent and expanded funding in the state budget in 2023, and the team is now publishing about the empirically supported best practices on program development and implementation.
“It is our hope that expansion beyond New York state will be the next logical step,” Hardiman explains.
“There is already a Congressional bill on the docket in Washington D.C. to expand the program nationally. New York has been a pioneer in the use of veteran peer support services, particularly with the Dwyer program. Although most states offer some level of peer support for veterans, New York is the only one with a sustained commitment and a statewide implementation approach. This shows a serious level of commitment to veterans and communities that should be lauded.”
The Dwyer program also benefits local communities through raising awareness of the needs of the veteran population and helping to build a more supportive environment.
“Our evaluation has been able to tell the stories of veterans impacted by the program. Whether that is bringing a veteran out of isolation, helping someone avoid self-harm, or creating a more powerful safety and social support net for veterans, the net result is positive,” says Hardiman.
Picturedabove:Hardimanspeakingatthe10yearanniversaryDwyer Program pressconferencein2023.Picturedleft:attendeesatthe pressconference.
In the hands of foster care youth, underserved communities, and advocates for social and health equity, a phone camera becomes a brush that can paint untold stories, capturing realities and serving as a means of expression, healing, and conversation. The fields of social work and public health have long recognized the major role art can play in advancing policy and programs, particularly when led by communities whose voices have been marginalized.
“Arts-based practice helps transcend and transport relationships beyond the confines of practice within systems that often perpetrate as much harm as they purport to mitigate,” explains Sarah Mountz, associate professor in the School of Social Welfare. “Practices like filmmaking, creative writing, and storytelling are ways of imagining possibilities and envisioning futures beyond systems.”
Mountz has utilized many forms of art throughout her career as a social worker, including PhotoVoice, a method of community-based participatory research used for representing the perspective of the community. Participants take photos that reflect their lived experiences—often highlighting problems and challenges. The photographer then describes what the photo represents in words, making the community members into partners in the research process. The photos can then be used to open dialog between communities, stakeholders, practitioners, and policymakers, and are often displayed in galleries for the public.
“Not everyone is able to or wants to talk about experiences of adversity or trauma, and art, which uses both verbal and non-verbal tools, can be a powerful and safer way of accessing and expressing emotions related to trauma
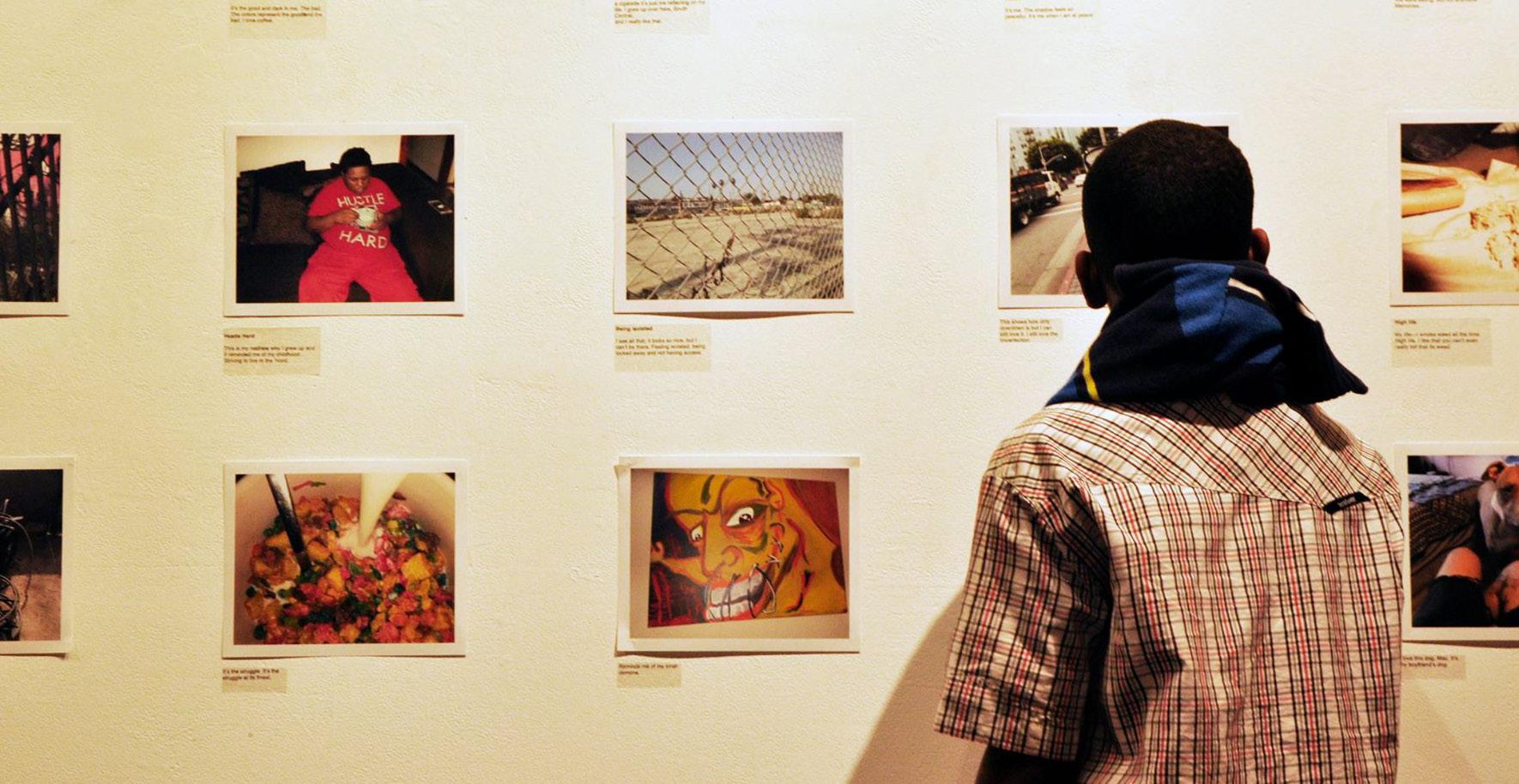
which is stored in the body,” Mountz says, who has worked on arts-based projects with LGBTQ+ group homes, foster care youth, and people who misuse opioids, to name a few.
During the COVID-19 pandemic, Mountz worked on a PhotoVoice project with UAlbany students with foster care experience, in collaboration with the Educational Opportunity Program (EOP), which provides admission opportunities for economically and educationally disadvantaged undergraduate students from New York. The project led to activism and organizing on the part of the students, including the creation of Fostering Leaders of Our World, a student group at the University composed of students with foster care backgrounds and their allies. Students also took their stories to the New York State Senate to advocate on behalf of other college students in foster care.
“One of the reasons I use participatory and arts-based methods is because they have the capacity to help democratize our research design, process, and methods of dissemination to enhance consciousness of publics and actors who hold power to enact change within and beyond academia,” Mountz notes.

Picturedabove:ExamplesofPhotoVoiceprojectscourtesySarahMountz. Picturedbelow:MountzwithUAlbanyfostercarePhotoVoiceparticipants.


Janine Jurkowski, professor in the Department of Health Policy, Management and Behavior, agrees with this sentiment and used PhotoVoice from 2017-2022 as a way to engage community members and organizations in discussions around public health topics to enhance local response to specific problems. The annual public health PhotoVoice project she led (pictured above) focused on topics such as behavioral health, maternal health, and social and racial justice during COVID-19.
Submissions were received from numerous organizations in the Capital Region, including Planned Parenthood, Capital Roots, Trinity Alliance, South End Children’s Café, Prevention Council of Saratoga County, and local health departments. Before the COVID-19 pandemic hit, over 100 public health practitioners were participating.
“Talking, sharing, and experiencing together can be powerful,” Jurkowski says.
“For example, two nonprofits who had never collaborated and were in different lanes in the community learned about each other at the PhotoVoice gallery. They realized they had synergies and saw a benefit in collaborating.”
In 2022, the annual public health PhotoVoice project pivoted to be housed within the academic classroom experience, in a strategic effort to have undergraduate students connect with local organizations to learn more about their work. Students were assigned an organization to collaborate with and submitted a photo with a description to be shared widely. In-depth discussions then took place.
“PhotoVoice is a great opportunity for our students to work on their critical awareness and discussion skills for better understanding the challenges in the public health field that we must address,” Jurkowski explains. “It is a great way for us to work with students on self-reflection and how to approach others by first curbing their own unconscious bias— and with empathy and humanity. We’re teaching our students to be active listeners so that they will learn more and be able to truly impact the communities they work with.”
The arts-based method is viewed positively by both undergraduate and graduate students at the College of Integrated Health Sciences.
“Photovoice resonates with me because it is a powerful tool for academic-community partnerships in public health.
Residents and health advocates in neighborhoods can use photos to document challenges that require policy or interventions. Those of us in schools of public health can also use such photographs to advocate for our neighbors by designing interventions in a participatory manner,” says DrPH student Grace Abby Adan.
“The PhotoVoice projects are just one of the many ways that our engagement with communities and different groups helps our students and faculty to be innovative practitioners and leads to more effective programs and solutions,” notes Jurkowski.





“What you see here may look like just an average photos of a book while I am outside, but it is a picture of my best friend. This book was given to me by my birth mother when I was 9 years old along with a brown, Build-A-Bear Workshop stuffed bear. I have had this book all these years because when my mom was not home and I was alone, I would attempt to read it. I was only 9 so reading that book was easy for the words, but difficult to understand.
Over the years, I would sit outside or in the rooms of my various foster homes/ group homes and read this book repeatedly. I wouldn't allow myself to become close to anyone else or try to understand anything else but this one book. Other kids would taunt me because I protected it with my whole life. The truth is, that if I lost this book, I felt like I was losing a part of myself along with the last memory of my mom that was happy.”
- UAlbany foster care PhotoVoice submission

Eastern equine encephalitis (EEE) is a mosquito-borne disease that can induce severe fever, seizures, gastrointestinal issues and changes in behavior. About a third of EEE cases are lethal, and those who recover commonly experience lingering neurological problems. Considered rare in the United States, EEE is on the rise. The illness was identified in New York for the first time in nearly a decade in September 2024 and the person who contracted it has since died from the virus.
Climate change is an important driver of mosquito-borne disease. Warmer, wetter summers in the northeastern U.S. mean conditions are favorable for mosquitoes that transmit harmful diseases to people. Plus, the season of mosquitoborne disease risk is becoming longer, with the onset of warmer weather happening earlier and lasting later into the year.
EEE virus is primarily transmitted in forested swampy areas, the preferred habitat of the black-tailed mosquito (Culiseta melanura). These landscapes play a vital role in shaping virus prevalence. Early EEE outbreaks tend to occur during unusually warm, wet summers, similar to the warm, humid periods experienced in the Capital Region in summer 2024.
Alexander T. Ciota, an
associate professor in
the
Department
of
Biomedical
Sciences based out of the Wadsworth Center, shares insights on EEE and climate change:
Is the season of mosquito-borne disease risk becoming longer due to climate change?
“When we evaluate the risk of mosquito-borne pathogens, it is important to consider a range of factors including land use, host dynamics, viral genetics and climate. How climate variation affects different mosquito-borne pathogens depends on the unique ecological characteristics of each pathogen and its primary mosquito vectors.
While precipitation patterns are volatile and can have differential effects on mosquito populations, the consistent increases in temperature regionally are generally increasing the duration, intensity and distribution of mosquito-borne virus activity. Both spring mosquito emergence and cessation of activity in the fall are triggered by environmental cues, primarily temperature, so warming will generally correspond to longer mosquito seasons.
Temperature also increases disease amplification and prevalence within the transmission season. This is because mosquito development accelerates at warmer temperatures, which will increase population size.
Likelihood of virus transmission increases with higher temperatures as well. Because mosquitoes are ectotherms, increases in outside temperature increase internal temperatures, causing viruses to replicate faster and to higher levels. Since these viruses frequently mutate, this could also contribute to the emergence of new variants with altered virulence and transmissibility. An important exception to these trends: episodes of extreme heat, which can decrease mosquito longevity.”

Building on more than a century of excellence as the state’s public health laboratory at the NYSDOH, the Wadsworth Center continues as a premier biomedical institute that merges clinical and environmental testing with fundamental, applied and translational research. Scientists use both classical and contemporary approaches to study environmental and biological questions related to human health and disease. They develop advanced methods to identify microbial or chemical threats; study drug resistance, emerging infections, and environmental exposures; manage the country’s most comprehensive diagnostic and environmental testing laboratory permit program; oversee extramural research programs on stem cells, breast cancer and spinal cord injury; and train the next generation of scientists in collaboration with the UAlbany College of Integrated Health Sciences.
How is climate change affecting emerging arboviruses?
“We are seeing shifts in the magnitude and distribution of endemic pathogens and an increased threat from exotic pathogens. This is partly due to increased global trade and travel, but range expansion of vectors due to climate change is also certainly contributing. For instance, both the Asian tiger mosquito (Aedes albopictus) and the yellow fever mosquito (Aedes aegypti) are steadily expanding their range as the climate becomes more suitable for these mosquitoes in the northern hemisphere. These are the primary vectors of numerous exotic pathogens such as dengue virus, Zika virus, chikungunya virus and yellow fever virus.
As a result, we are beginning to see more cases of exotic viruses being acquired here in the U.S. For example, over the last five years, the first locally acquired dengue virus infections were reported in California, Arizona, West Virginia and North Carolina. Notably, there was also a locally acquired case of dengue in New York State in 2016.”
Beyond EEE, are other mosquito-borne diseases on the rise in the eastern U.S.?
“The general trend for all endemic vector-borne pathogens is increased activity. This year is one of the highest on record for West Nile virus activity in NYS mosquitoes. We are also seeing increases in lesser-known mosquito-borne viruses such as Jamestown Canyon virus and Cache Valley virus. Because there are so many dynamic factors that influence these pathogens, we will continue to have relatively high and low years, but the increasingly favorable climactic conditions, together with the emergence of new variants, means the probability of high levels of activity is increasing.”
Is EEE prevalence changing? What particular health risks does it pose?
“This year has actually not been an uncharacteristically high year for EEE in terms of prevalence in NYS mosquitoes, but has been remarkable in that we are seeing activity in nontraditional locations with an unprecedented number of equine cases. This, together with the reported human cases in neighboring states, has led to the elevated concern.
There is a lot to be learned about the ecology of EEE including how it is maintained between seasons, the relative importance of different bird species, and the potential for different mosquitoes to transmit the virus. However, it is likely that the warm and wet spring conditions this year created more suitable habitat for expansion of the black-tailed mosquito, the main EEE vector, which breeds in wooded swamps. Fortunately, this mosquito rarely feeds on humans. When humans do become infected, the disease is often quite devastating. Unlike most mosquito-borne viruses for which severe disease is rare, EEE is thought to have a fatality rate greater than 30%, with nonfatal infections frequently being associated with long-term neurological complications.”
What are your top recommendations for people to stay safe during mosquito season?
“Although there are equine vaccines for EEE and West Nile virus, there are no commercially available prophylaxis or approved human vaccines for endemic arboviruses. Personal protective measures to avoid mosquito bites remain the best defense. These include wearing long sleeves and pants outdoors, particularly at dusk and dawn, using insect repellents containing DEET, eliminating standing water from your property, and making sure you have intact screens in doors and windows in your home. Avoiding wooded swampy areas (i.e., black-tailed mosquito habitat) is also a good protective step.”



A new statistical method called the Variable Bandpass Periodic Block Bootstrap (VBPBB) was recently developed by Edward Valachovic (pictured above), assistant professor in the Department of Epidemiology and Biostatistics.
The VBPBB helps to create more precise estimates when looking at regularly occurring changes within data collected across time –commonly called time series data.
The VBPBB method filters time series data based on the period, or corresponding frequency, of the factor of interest– such as daily or yearly variation. Then, researchers can resample from within the filtered data, preserving the periodic characteristics while eliminating interference from other factors, making the estimates based on the selected time periods more reliable.
The VBPBB is more efficient, robust and powerful than many existing methods.

Melonie Walcott (pictured above), assistant professor in the Department of Health Policy, Management and Behavior, received over $1.3 million from the Centers for Disease Control and Prevention for her study titled “Pre-exposure prophylaxis for Women In-charge of Sexual decision-making and Engagements (PrEP-WISE).”
The four-year study seeks to develop and pilot a theory-driven contextually relevant intervention to increase uptake of PrEP—a medicine taken to prevent HIV— among cisgender Black women in New York. The work will be community-centered and include interdisciplinary collaborators with integrated expertise in HIV prevention.

Studying the placenta to better understand cancer
At the Cancer Research Center, Assistant Professor Bum-Kyu Lee from the Department of Biomedical Sciences (pictured above) studies gene regulations in the early embryo and placenta development in humans. His work to better understand the placenta may help to treat cancer.
Lee is focused on identifying novel factors that play important roles in placenta development and deciphering the underlying mechanisms of development.
One of the cell types Lee studies, extravillous trophoblasts—or EVTs— can invade the mother’s uterus during early placenta development. This invasion shows considerable similarities to how metastatic malignant cancers spread.
Lee’s work aims to identify common molecular pathways between cancer metastasis and placenta development— ultimately with the goal of treating cancer with relatively low toxicity.


Health workforce shortages persist across New York
New York continues to experience workforce shortages in all health care settings, according to a 2024 report released by the Center for Health Workforce Studies.
There are shortages of registered nurses, licensed practical nurses and aides across all health care settings including hospitals, ambulatory care, nursing homes and home care services. Surveyed providers cited a variety of reasons for recruitment and retention difficulties, including general workforce shortages and better opportunities within and outside of health care.
“The goal of this report is to provide health care providers, policy makers and other stakeholders with current information to assist in health workforce planning and development,” said center Director Jean Moore (pictured above). “Our research can lead to informed decisions on education and job training investments, help guide policies related to health profession education pipeline capacity, as well as inform current and prospective students about health care employment prospects and opportunities.”


John Justino and David Gittelman (pictured above) from the Center for Global Health are coinvestigators on a study led by Ashley Fox, associate professor at the Rockefeller College of Public Affairs and Policy, and Moustapha Seye from the Laboratoire de Recherche sur les Transformations Economiques et Sociales at the Université Cheikh Anta DIOP in Dakar.
The study, funded by the Mercury Project Social Science Research Council, aims to harness the acceptability and high uptake of routine childhood vaccinations administered through Senegal’s expanded program on immunization to test the impact of integrating the offer of adult vaccines with routine childhood vaccination.

Team finds link between longterm small particle exposure and increases in mortality
Outdoor air pollution was estimated to cause 4.2 million premature deaths worldwide per year as of 2019.
PM2.5 — Particle matter less than 2.5 microns in diameter — is what is usually considered when assessing health risks. However, the health impacts of ultrafine particles, which are far smaller than the PM2.5 particles, are less understood.
A study, led by a team of interdisciplinary researchers at UAlbany, has found a link between long-term ultrafine particle exposure and increases in mortality in New York, especially among underserved populations.
“Ultrafine particles are airborne particles that are less than 0.1 micrometers or 100 nanometers in diameter (PM0.1). That is about the size of 1/1,000 human hair. Since they are so tiny, they are easily inhaled into the distal branches of lungs, quickly absorbed into the bloodstream, and can pass through organ barriers,” says senior coauthor Shao Lin from UAlbany.




As an interdisciplinary population health scientist, Assistant Professor Muntasir Masum focuses on health-risk behaviors and population health processes and outcomes.
He holds expertise in analyzing large U.S. administrative health records and national surveys to investigate the effects of alcohol on health, including risks for cardiovascular disease and cancer.
Currently, Masum’s work is focused on understanding the social determinants of alcohol use in early midlife and its subsequent health outcomes, examining the impacts of binge drinking on population health using longitudinal data, exploring the influence of environmental and contextual factors on alcohol consumption behavior across the life course, and measuring the effects of alcohol consumption behavior on adult health and mortality outcomes. Muntas
Caroline N. Sharkey, visiting assistant professor, has collaborated with Youth FX since 2021 as a trauma-informed/ healing-centered consultant and youth participatory action researcher. Youth FX is a youthcentered digital filmmaking organization in Albany’s South End that works with young people from historically underserved communities. Participants learn digital filmmaking and media production and how to engage in their communities by creating both narrative and non-fiction short films that reflect their understanding and vision of the world around them as well as their imagined futures. These tools are powerful ways to address the impact of trauma, community engagement and collective efficacy, workforce development, and positive youth development.
In their work with Youth FX, Sharkey has sought to advance macro/meso-systemic therapeutic interventions using digital storytelling as a tool for trauma mitigation, collective healing, and reclamation. This collaboration has culminated in an ethnocinemagraphic documentary and data poetry zine, both titled “Storying as Reclamation.”
Researchers connect declining atmospheric sulfur dioxide levels to rise in Legionnaires’ disease
Declining atmospheric sulfur dioxide levels might be related to the global rise in Legionnaires’ disease — a severe form of pneumonia caused by inhaling the pathogenic bacteria Legionella. So reports a study from UAlbany’s Ursula Lauper (pictured above), which examined trends in atmospheric sulfur dioxide, Legionnaires’ disease incidence, and the role of cooling towers in harboring Legionella.
Sources of Legionella — which can multiply in building water systems and spread through the air — are well known, as are seasonal trends that affect the bacteria as a public health risk. Yet, the global increase in cases has been a puzzle. According to the CDC, from 2000 to 2018, Legionnaires’ disease cases have seen a ninefold increase nationally, with New York carrying the highest disease burden and having the fastest increase in the country.
The team’s findings are especially important for protecting vulnerable populations that disproportionately experience conditions that increase Legionnaires’ disease risk such as living near industrial or densely populated areas or having preexisting health conditions.
Students at the College of Integrated Health Sciences gain hands-on experience in their area of interest, working with our faculty housed within the University, our faculty employed by the New York State Department of Health, and with our partner organizations and agencies, both here in New York’s Capital Region and around the globe.
900 clinical hours completed by each Master of Social Work (MSW) student
750
internship hours completed by each Master of Public Health (MPH) student
480 clinical hours completed by each MS in Population Health Nursing student

11,946
alumni working in state, local, national, and international capacities to serve our communities and improve health and well-being for various populations

Theekshana Fernando investigates the facilitators and barriers that impact the in-state retention of international medical graduates who undergo residency training in New York. Understanding these factors could improve retention during their residency and as they transition to practice, ensuring a sufficient physician workforce to meet the health needs of New Yorkers.

Sarah Otaru is investigating the health effects of environmental exposures, specifically focusing on a commonly used herbicide called glyphosate. She is analyzing data from the National Health and Nutrition Examination Survey to explore the association between urinary glyphosate levels and metabolic health outcomes.

Nilija Foendoe interned at Vanderheyden Hall, a service agency in the Capital Region that includes an educational center for grades 7-12 . There, she shadowed school clinicians and gained experience in crisis interventions and cognitive/ behavioral interventions with the students.

Sophia Braithwaite interned at the NYSDOH Bureau of Community Chronic Disease Prevention, where she developed a comprehensive understanding of the health inequities faced by people with disabilities in relation to access and use of cancer screening and treatment programs. She then identified policy, system and environmental changes related to screening and treatment that could be used to improve health outcomes.

At the NYSDOH Wadsworth Center, Jennifer Ansong worked with scientists and data analysts to understand how they use CLIMS, a specimen tracking and reporting system used throughout the labs. She then helped analyze and report the needs of end users to a software developer team to facilitate updating the system to ensure that scientists are able to report about specimens related to the health of New Yorkers with ease.

As a community health worker at Trinity Alliance of the Capital Region, Amanda Gardy assisted individuals with navigating services for primary care, mental health, health insurance, food insecurity, homelessness, government assistance and more.

Madeline Rounds is completing her nursing clinical work at St. Peter’s Hospital, where she spends 20 hours a week shadowing and learning from professionals in behavioral health, pediatrics, and labor and delivery.

At the Schuyler Center for Advocacy and Analysis, Gerardine Georges learned to organize large scale projects, research and write about policies, assist with developing communications, and analyze the outcomes of strategy sessions with constituency groups. Her work was focused on two initiatives at the center related to maternal and child health: early childhood oral health and childhood poverty.

Cinthia Dieudonne worked on Albany Medical College’s Health Equity Project at the Center for Law and Justice, which primarily serves individuals who have been incarcerated. She worked directly with clients at the pediatric clinic to assist them in problem solving related to social determinants of health and navigating the healthcare system.

Melissa Ray interned at MVP Health Care, where she developed and evaluated a pilot health promotion campaign for increasing employee physical activity during work hours. She also assisted with program communications related to engaging and educating coworkers on improving and maintaining optimal well-being, and conducted qualitative data analysis for the annual evaluation of the MVP WellBeing Program.

Megan Di Maio used a new statistical method called the Variable Bandpass Periodic Block Bootstrap - developed at UAlbany by Edward Valachovic - to look at variations in nitrogen dioxide in Los Angeles.

Julia Del Pozo worked with the Bureau of Perinatal, Reproductive, and Sexual Health to conduct regional environmental scans of clinical and community services that provide resources that affect infant health.

Yousef Alsufayan is assessing the composition of PM2.5— tiny particles in the air — in Makkah, Saudi Arabia, to identify emission sources and understand their impact on air quality and public health. From this work, he will propose effective management strategies and policy recommendations to improve air quality in the city and protect the health of both residents and visitors.

Working as a rape crisis counselor with Albany County Crime Victim and Sexual Violence Center, Kelsey McGinn provided counseling through the rape crisis hotline and assisted victims/survivors at the hospital who reported a sexual assault by providing support, advocacy, and resources.

Brianna Lennon interned at Conifer Park, an inpatient treatment facility for adults dealing with alcohol and substance misuse. She learned to collaborate with clients to ensure all their needs were met in treatment and that they were prepared to succeed in sobriety outside the facility.

Working with Jewish Family Services of Ulster County, Shanti Grumbine served seniors in their homes as a counselor and caseworker, providing therapy and connecting them with local resources. She is also a SurviorLink grantee through AmeriCorps, offering training in intimate partner violence and safety planning.

At the William K. Sanford Town Library, Tanya HaskinsOwens assisted library patrons in accessing resources, establishing community partnerships, and creating workshops based on their needs, empowering them through skill development.

Molly Bray-Hayes worked at the Hospice Inpatient Unit at St. Peter's Hospital.
As a part of the team at the Hospice Inpatient Unit, I worked directly with patients and their families during end-of-life care and planning, ensuring the Hospice values of respect, integrity, and compassion were extended to all people through the social work lens of justice and equity.

Stuti Sheth interned with the Newborn Screening Program at the NYSDOH, working with clinical specialists to obtain and document diagnosis information and confirmatory test results. The main goal was to decrease lost to follow up cases. The Newborn Screening Program provides screening for more than 50 congenital conditions – many of which present with no symptoms at birth.

Kenny Li He is interning at the Bureau of Water Supply Protection within the NYSDOH, where he is learning various methods for investigating Legionella outbreaks and data analysis techniques. He also assists researchers by translating Legionella reports from health care facilities into a comprehensive database.

Emily Huff developed and hosted the Division of Family Health “Youth Day” at the NYSDOH to increase public health literacy, foster collaboration between public health professionals and the community, enhance perspectives of a career in government, and provide an understanding of educational pathways.

Interning with the University of Illinois Chicago Division of Specialized Care for Children, Zachary Taylor explored innovative strategies to improve medical home access for children and youth with special healthcare needs along with the process and outcome measures that aligned with the identified strategies.

Katie Montgomery studied abroad in Copenhagen, Denmark. She focused on comparative studies of global healthcare systems, visiting healthcare facilities and talking to health practitioners in hospitals, community health organizations, and rehabilitation facilities across Northern Europe as part of her studies. Additionally, she studied global health and food-system design while abroad, inspiring her to focus on the impact of global food systems on public health in her post-graduate career.

Sophie Whiteman interned with Engeye, a non-profit organization in rural Uganda. There, she served as an analyst and clinical specialist, working with the Engeye team to plan, manage, and evaluate local collaborative public health programs and projects.

Cathrina Aris is pursuing her Master of Public Health (MPH) at UAlbany, along with a Graduate Certificate in Maternal and Child Health. Her goals are to help bridge the gap between epidemiological research and public health practice and to support under resourced communities by advancing health equity, particularly in communities like her hometown.
“Growing up in a CaribbeanAmerican community in Brooklyn, New York, I witnessed health inequities firsthand, especially the prevalence of conditions like type II diabetes and high blood pressure,” Aris says. “Observing these disparities sparked my curiosity about their underlying causes and my desire to address them, specifically through nutritional health, as I believe diet can be transformative in managing and even reversing such chronic conditions.”
For the internship component of her MPH program, Aris currently interns at the New York City Department of Health and Mental Hygiene, where she performs data analysis to examine the link between food insecurity and diabetes.
“Diabetes is largely manageable with early intervention, health
and access to healthy foods, yet some populations have limited or no access to these resources,” she explains.
Aris explores the impact on maternal health, focusing on the relationship between food insecurity and gestational diabetes—a critical yet underdiscussed area. “By addressing food insecurity and gestational diabetes, we can create targeted interventions to support vulnerable maternal populations and improve access to nutritious food.”
For this internship, Aris is learning SAS, a software system for data analysis. While challenging, she notes that she’s applying coursework she’s learning in the classroom directly to this process, showcasing the benefit of the 720-hour internship component of UAlbany’s MPH program.
For her first internship for academic credit, Aris interned in summer 2024 at Westat, a social science research firm based out of Rockville, Maryland. She worked on their Maternal Health Community Implementation Program and the IMPROVE Community Implementation Program, two initiatives focused on reducing maternal mortality and severe maternal morbidity in underserved communities. She helped to
implement and evaluate interventions, collaborated with community partners, conducted literature reviews and helped to manage data, using concepts she’d learned in her Introduction to Maternal and Child Health course at UAlbany taught by Associate Professor Christine Bozlak.
“I also co-authored a blog post addressing mental health disparities among racial and ethnic minority groups, emphasizing the need for community-engaged approaches to improve maternal mental health outcomes for Black women,” Aris says. “This internship taught me the importance of involving community members in the research process—a principle I’ll carry forward in my public health career.”
Going forward, Aris strives for a career making epidemiological findings accessible and meaningful for diverse populations, or conducting community engaged research focused on addressing health disparities.
“Both of my internships confirmed my happiness studying epidemiology,” Aris says. “I love public health, and epidemiology challenges me to think critically, make data easier for others to understand, and tell impactful stories using numbers!”
A registered nurse and family nurse practitioner, Tristan Sharratt has practiced as a nurse in a county jail and a rural public school district, and joined the NYS Fellowship in Applied Public Health (FAPH) program in 2022.
Jointly sponsored by UAlbany and the NYSDOH, this two-year public health training program is for physicians, veterinarians and other advanced licensed health care professionals with an interest in pursuing leadership roles in state and local health departments. Fellows earn an MPH from UAlbany, alongside practical experiences at the NYSDOH and a local county health department. Tuition is fully covered, and fellows earn a salary for their work.
The Otsego County Department of Health, where Sharratt worked as part of the FAPH program, maintains a unique relationship with local Amish and Plain Anabaptist communities. When, in the early 2000s, an Amish child presented with pertussis (whooping cough), the child’s community reached out to the health department to request vaccines. The county quickly vaccinated all the adults and thus established the program of routine vaccinations that exists today.
“The Otsego health department now wants to expand vaccine efforts into the three other Amish communities in the county, especially in areas where vaccination rates are low,” said Sharratt.
“Measles and chickenpox, which are on the rise, are top concerns. As a Fellow, I was tasked with designing a campaign to promote vaccines in these communities. However, if we want to share information on important health tools and encourage uptake, we first need to learn more about these communities and understand how their beliefs and traditions might shape perceptions of these different health tools.”
Since November 2023, Sharratt has continued to dive deep into sociodemographic research focusing on the belief systems and geographic origins of Amish communities in central New York.
“In my earliest research, I came to realize that there isn’t much advice for clinical professionals and public health professionals looking to interact with these communities to discuss health issues like vaccines and well contamination,” said Sharratt. “It’s also clear that non-Amish people approach Amish communities with broad, often incorrect assumptions about who they are, what they believe and how they behave.”
To learn more, Sharratt has established contact with Amish studies scholars throughout the country. He is currently working with The Places Institute, a demography institute at SUNY Oneonta, on a population study focused on groups of people in central New York that are generally categorized as “white of German ancestry” but represent a wide diversity of groups (including over a dozen distinct Amish, Plain Anabaptist, Mennonite and Hasidic Jewish communities) all with different geographic origins and belief systems that would affect health and healthcare.
Sharratt is also collaborating with scholars affiliated with the Amish and Plain Anabaptist Studies Association who have connected with traditional healers in these communities to learn about traditional practices and explore ways that these methods could enhance, or be applied alongside, western medicine — to the benefit of people within and beyond these communities.
“Many Amish and Plan Anabaptist communities are not as ‘anti-Western medicine’ as many people perceive them to be,” said Sharratt. “However, in this post-covid era, many of these communities have received more vaccine misinformation and disinformation, and less good information on the safety and efficacy of vaccines. As a result, there is a building of resistance to vaccines and other modern public health and clinical health tools. We are hoping to counter that.
“My work now is focusing on how happy accidents – like the connection in Otsego County, where the Amish community reached out to the health department – come to pass. How do we replicate that, even though the social and political context is drastically different now, compared to when that vaccine program initially began over two decades ago?”
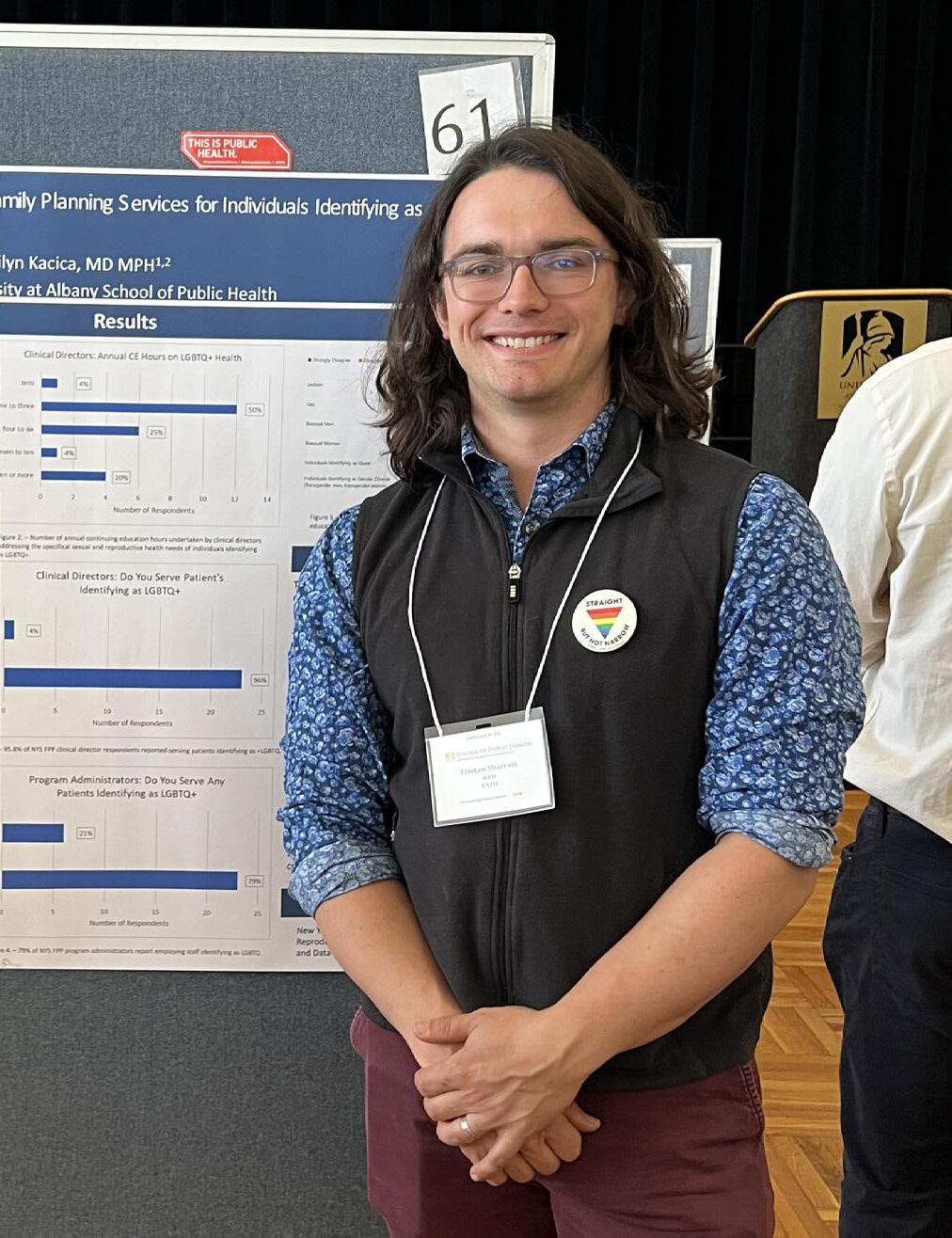
“As a health department, we need to provide consistent, easy to understand, relatable information that clearly communicates how certain health interventions can be beneficial. This is a challenge that requires a deep understanding of the communities and their traditional practices. My work is about understanding the Amish and building relationships with them such that we have a common understanding about how each other thinks and functions so that we can reach a common ground on some of these critical public health interventions that could protect entire communities in the future.”
(Pictured above: Tristan Sharratt at UAlbany Showcase 2024)
Social work PhD student Yanjun Dong saw firsthand how her elderly family members struggled to navigate the healthcare system—including long wait times, prohibitive costs, and difficulty understanding complex and technical information. These experiences deepened her interest in advocating for improved healthcare access and utilization for older adults, ultimately leading her to a focus on gerontology in social work.
“As social workers, we have a collective responsibility to care for older adults, recognizing their immense contributions to society. Ensuring they receive the care they need is not just a matter of health; it is a matter of dignity and respect,” Dong says.
Her research focuses on identifying and addressing the gaps in the healthcare system that prevent older adults from receiving proper care.
“The main goal is to make our system more equitable, inclusive, and responsive to the needs of all older adults,” explains Dong, who has seen how access to services is not always equal — along with how this can exacerbate health disparities for marginalized communities— through volunteer work in emergency rooms and therapy centers in Albany and Los Angeles.
Dong explores how people use healthcare services as they age, taking into account factors like race, sex and income. Her findings, which are under review for publication, show that older adults who identify as Black, indigenous, or as a person of color (BILPOC) do not utilize healthcare services as much as others, especially if they live in poverty.

“Older adults from BIPOC communities, especially those with low incomes, might have difficulty getting prescription medications due to barriers like cost or access. By contrast, they may rely more on services like home healthcare, where a nurse or caregiver comes to their home to help with their health needs. This suggests that while they might be unable to access some types of care, like prescription drugs, they might use other services more frequently. This finding shows that older adults from different backgrounds may have different needs. Building upon my findings, we need to make sure everyone can get the care they need, no matter who they are or where they come from,” she says.
Recently, Dong presented at the Asian and Pacific Islander Social Workers Educators Association conference in Chengdu, China (pictured above). She also won the student paper award at the 51st annual conference of the State Society on Aging of New York, where she shared another section of her research, which is focused on gender disparities in healthcare utilization among older adults. Her research in this area shows the gender disparities in healthcare utilization and identifies factors that influence how older adults of different genders access and use healthcare services. Now, Dong is a student researcher in the new Center for Healthy Aging.
“Being able to contribute to initiatives that advance our understanding of aging and result in tangible improvements in healthcare access, social support, and overall quality of life for older people is rewarding. I'm looking forward to the collaborations and innovations emerging from this center, and I'm eager to see how our work can lead to real-world change, helping older adults lead healthier lives,” she says.

They might look like noodles, but the samples that 5th year PhD student Kayla Simanek works with in the Paczkowski Lab of the Wadsworth Center at the NYSDOH are important for advancing the understanding of how bacteria evolve. The samples are Pseudomonas aeruginosa, a pathogen that can be found almost everywhere, including water sources, hospital sinks, implanted medical devices and open wounds. In 2023, an outbreak in eyedrops caused the FDA and the CDC to recommend cessation of use for two brands until they were deemed safe again. Pseudomonas aeruginosa can cause infections in the blood, skin, lungs, eyes and other parts of the body, and can spread through contaminated surfaces or from person to person. Simanek studies the mechanism of cell-to-cell communication in Pseudomonas aeruginosa that controls virulence and biofilm formation. We sat down to learn more about them and the basics of their work:
How did you become interested in Pseudomonas aeruginosa?
“I took a course on bacterial pathogenesis in my last year of undergrad that made me want to be a microbiologist. The virulence factors of bacteria - ways in which they cause infection or are toxic to humans - really interested me.”
Why did you choose UAlbany for your PhD program?
“Because of its affiliation with the New York State Department of Health. I wanted to do research that was relevant to public health and having access to clinical isolates through the Wadsworth Center was crucial.”
What do you study in the Paczkowski lab and why is this work important?
“I'm studying how Pseudomonas aeruginosa from people with infections have evolved the way they communicate. We found that certain mutations in their communication system make these strains better at causing infections. We are facing an antibiotic crisis, and understanding how Pseudomonas aeruginosa is evolving in healthcare niches will help us learn how to get better at preventing infections in the first place.”
What's the most fascinating thing about studying Pseudomonas aeruginosa?
“Some strains turn blue when you grow them in the lab!”
What’s up next for your career?
“I accepted an academic post-doc position at Indiana University where I’ll be working on a skin infection model for Vibrio vulnificus. I’m also looking forward to leaning into outreach work that I’m involved with in the microbiology community.”



Through her extensive classroom experiences and professional positions, Doctor of Public Health (DrPH) student Blender Muzvondiwa holds expertise in African, Asian and American health systems and policies—and is committed to leveraging this global perspective to drive meaningful reforms to strengthen the health system and improve population health in her home country, Zimbabwe. “My home city, Gweru, is referred to by locals as ‘the City of Progress.’ Looking at how the place has shaped my views and perspectives on life greatly explains the meaning—Gweru ignited my passion for public health and motivates me,” Muzvondiwa says. “I came to realize that Zimbabwe faces numerous health challenges with limited response from the healthcare system, and now, I want to bring implementable change and better integration of diverse disease policies.”
Muzvondiwa first earned a bachelor’s degree in food science and nutrition at Midlands State
University in Zimbabwe. Then, she worked as a registered nutritionist under the Ministry of Health and Child Care for three years, focusing on maternal and child health and nutrient-drug interaction among people living with various diseases.
“During this time, I gained extensive practical experience, knowledge and exposure working with domestic and international nongovernmental organizations across Sub-Saharan Africa and Europe, and became proficient in formulating and executing community-based health care programs and corresponding activity plans,” she says.
But Muzvondiwa wanted to take her formal education further, and enrolled at Thammasat University in Thailand, graduating with her Master of Public Health (MPH) in 2020. Following her graduation, she was employed by the University of Lleida in Spain to work on a child health comparison project, then became the program manager for a sexual and reproductive health program under the SMILES of Hope Foundation in Zimbabwe.
“This is when I chose to apply to the DrPH program at UAlbany, and coming here has made me even more confident in my ability to conduct rigorous public health program evaluations that inform evidence-based interventions and to design programs addressing health disparities,” Muzvondiwa says.


Now as a DrPH student, Muzvondiwa works in the Udo lab at the College of Integrated Health Sciences, assisting Associate Professor Tomoko Udo with evaluating public health programs funded by the NYSDOH AIDS Institute. In particular, she conducts data collection, cleaning and analysis for a project that identifies and addresses the needs and barriers faced by people who inject drugs when accessing hepatitis C care and treatment in traditional healthcare settings.
“While I’ve worked on HIV, AIDS, TB, COVID-19, and malaria in both Zimbabwe and South Africa, I had never worked on hepatitis C before, and this was a good opportunity to gain insight into another critical area of public health,” Muzvondiwa explains. “The unprecedented rates of hepatitis C in New York are hard to ignore and are so alarming, I wanted to contribute.”
General findings from Muzvondiwa’s work show that there are many barriers for people when trying to access care, including
stigma, discrimination, staff shortages, lack of funding to sustain programs, lack of transportation to reach treatment sites and priorities taking precedence over receiving treatment, such as food and shelter.
After she earns her DrPH, Muzvondiwa plans to apply research evidence to real world situations in Zimbabwe, working with academic institutions, government agencies, and other organizations like the United Nations. No matter where her career path takes her, she plans to contribute to policy changes and to implement solutions to enhance public health and strengthen the health system.
“I desire to be an asset wherever I go – bringing a wealth of experience on African, Asian, and American health systems and policy context,” she says.


From examining biological mechanisms to engaging with communities to address disparities, our alumni make a significant impact on the health and wellbeing of communities and individuals across the globe. They are dedicated to building social and health equity, advocating for social justice, and creating lasting change through programs, policy, and prevention.

As Chief Program Officer at the Regional Food Bank, Michael Poindexter leads all programmatic, agency, and advocacy-related services, ensuring effective delivery of services to communities in need. He manages various organization initiatives, and the programs department which includes the divisions of Agency Services, Children and College Programs, Impact and Advocacy, Community Health Programs, Partner Capacity and Strategy, Seniors, and a new FoodForward grant initiative that supports partner expansion and creates capacity for more food to our neighbors in need.

Elizabeth Conklin-Ballester works for USAID’s locally led development initiatives program where she provides support to 44 missions to implement cross-sectoral programming using methods that empower local organizations.
She also founded Community Service Alliance in the Dominican Republic with her husband, which supports community led programming in education, health and income generation for vulnerable populations in the Dominican Republic while facilitating life changing educational exchange.

Carolyn G. Sheridan is the State Policy Manager at the National Organization for Rare Disorders. She leads state-level advocacy efforts across 24 states and Washington, D.C., to support the rare disease community by advancing policies on Rare Disease Advisory Councils, utilization management, patient out-of-pocket costs, and access to comprehensive care. Her work combines legislative strategy—drafting proposals and working with state lawmakers—and coalition-building, uniting diverse stakeholders to advocate for greater access to diagnostics, treatments, and care.

Wayne Lawrence is a research fellow in the Division of Cancer Epidemiology and Genetics at the National
Cancer Institute. He is investigating the contributions of racial residential segregation, psychosocial stressors, and barriers to quality medical care to exacerbating cancer disparities and premature mortality.
His research also examines national trends in leading causes of death by race and ethnicity, and socioeconomic status.

‘97
Gladys Tetteh works as the senior technical director for malaria at Jhpiego, an affiliate of Johns Hopkins University.


MSW/MPH ‘22
Taylor Perre is the associate director for policy and advocacy at the Home Care Association of New York State. She conducts state advocacy efforts, education, and programmatic work including applying for, managing, and implementing grant funded initiatives. Her focus areas include mental health, health disparities, community paramedicine, sepsis, rural health, and emergency preparedness. She provides related support, development, and maintenance of the education, website, communications, and advocacy for these topic areas.
MPH ‘16
Donette Samuel is a senior public affairs specialist with the U.S. Environmental Protection Agency (EPA). She oversees external engagement for high-priority projects across New York, New Jersey, Puerto Rico, and the U.S. Virgin Islands.
In 2022, Donette earned EPA’s highest honor award for implementing a precedent-setting community engagement process when addressing concerns at the Toa Alta Landfill in Puerto Rico. Before EPA, Donette was a Global Health Ambassador with the U.S. Peace Corps to the Ecuadorian Ministry of Health.
She provides strategic vision, technical leadership, oversight and implementation support to Jhpiego’s Global Malaria Portfolio, which consists of global projects and bilateral projects working to increase access to and quality of malaria services across countries in Africa and Asia.

‘06
Sharon Kollar is a principal researcher at Mathematica. In this senior child welfare role, she serves as the associate director of a national child welfare center that supports improvements in state child welfare systems.

Candi Griffin-Jenkins is the director of the Bureau of Social Determinants of Health within the NYS Office Children and Family Services, Division Child Welfare and Community Services.
The Social Determinants of Health bureau is dedicated to addressing the systemic inequities that negatively impact economic stability, educational access, quality health care and the environment. The goal for this newly formed bureau is to create and shift policies and identify programs that reduce systemic barriers that children and families face in New York.

As a postdoctoral fellow with the Henry M. Jackson Foundation, Jordan McAdam studies environmental and

Evelyn Bautista-Miller is founder and president of Tender Steps of New York Inc, a non-profit in Rockland County, NY that offers courses, workshops, advocacy services and case management to families, parents and children facing difficult circumstances. The organization also provides bilingual services (Spanish and Creole) to help bridge the communication gap within the community and enrich the quality of lives.
In 2020, Bautista-Miller received the 2020 New York State Assembly Women of Distinction Award from Assemblywoman Ellen Jaffee.
occupational exposures and cancer risk within the military.
Recent research projects in her role have included evaluating blood concentrations of pesticides in military personnel and thyroid cancer risk, and adverse health effects in coast guard responders following the Deepwater Horizon oil spill.

Kara Levinson is the state public health laboratory director at the State of Tennessee Department of Health.
She oversees the Division of Laboratory Services for the State of Tennessee, which includes the Nashville Central Laboratory and Knoxville Regional Laboratory.
The labs perform testing and provide scientific consult on a variety of public health needs, including outbreak response, emergency preparedness, environmental health, and newborn screening.
The Division of Laboratory Services works closely with local clinicians, epidemiologists, and community health partners at the state level, and serve as the southeast regional laboratory for the antimicrobial resistance laboratory network and a variety of other national surveillance networks to ensure public health decisionmaking is based on timely and accurate test data.

As Director of the Bureau of Environmental and Occupational Epidemiology at the NYSDOH, Neil Muscatiello oversees epidemiologists, statisticians, and GIS experts who investigate community environmental exposures and conduct biomonitoring studies, lead and manage the NYS Birth Defects Registry and associated surveillance and research activities, and conduct environmental health surveillance to identify health risks. He is also the PI on the CDC-funded Environmental Public Health Tracking grant, which seeks to better understand linkages between environmental hazards, exposures and health outcomes, and the Climate Ready States and Cities Initiative grant, which seeks to reduce the public health risks of climate change.


Alice Antwi serves as the director of service learning and community engagement at Albany Medical College, where she manages over 30 community-partnered programs that connect medical students with the community to learn about social determinants of health.


Rena Jones is a senior investigator in the Intramural Research Program at the NCI. Her research focuses on the investigation of cancer risk associated with environmental contaminants, especially air and water pollutants. Her work relies on the application of GIS and novel approaches to assess environmental exposures.
Anne Bink serves as director of mitigation and resilience at Innovative Emergency Management, or IEM, where she collaborates with state, tribal, territorial and local governments to build resilience in infrastructure and communities before and after disasters.
Temilayo Adeyeye is a research scientist in the Center for Environmental Health at the NYSDOH. She is primarily involved in climate-health research and has worked on multiple projects assessing the impact of climate on health in New York, including a NASA-funded project exploring the effects of extreme heat exposure on human health. She has also contributed to the development of tools and infographics for counties in New York to aid in climate health surveillance and mitigation efforts.



