9 minute read
COVID-19 AND THE "FAT" PARADOX
MERITS OF THE KETOGENIC DIET IN A COVID-19-STRICKEN WORLD
By Jack Osborn Helen Wei
Advertisement
INTrODuCTION
Ketogenic diet is a high-fat, low carbohydrate diet used primarily as a quick weight loss regimen. By restricting carbohydrate intake, the body switches its primary fuel source from glucose to ketones, organic molecules synthesized by the liver to deliver clean, long-lasting, and abundant energy. While there is still much to be uncovered about the effect of the diet transiently on the body, there are many significant and well-understood long-term implications, including the lowering of inflammatory markers associated with diseases such cancer, diabetes, and obesity. The ketogenic diet can be therefore viewed as a preventative measure to reduce chronic inflammation associated with a host of inflammatory diseases. SARS (Severe Acute Respiratory Syndrome), an inflammatory respiratory illness caused by a coronavirus, is responsible for hijacking its host genome and inducing a cytokine storm in the body. SARS-CoV-2, for example, has been shown to prevent gene activation of interferons, proteins released by infected cells that signal to nearby cells to activate their own genes to slow further viral replication. Without interferon activation, viruses such as coronavirus are capable of unchecked replication and runaway inflammation that impedes the immune system, promoting a dangerous inflammatory response.
Within a matter of days, COVID-19 swept up society into a state of paranoia and fear, igniting concerns surrounding the short term and long-term implications on our health. As more information emerged regarding its mechanism of transmission, who is most at risk, and who presents the biggest risk of transmission, scientists developed a key understanding of why at-risk individuals are hit the hardest, and how we can best respond to COVID-19 positive individuals through treatment.
KEY DEMOGrAPHICS AND rISK FACTOrS FOr COVID-19
While it is currently well-understood that COVID-19 has detrimental short-term consequences on the body, there is still much to be uncovered regarding its long-term deleterious implications, from cognitive impairment to cardiovascular disease, to exacerbation of existing socioeconomic inequalities. We observed a common theme amongst hospital admission trends: people of color and those of a low socioeconomic status seemed to be hit the hardest, highlighting social inequity associated with disease and access to healthcare.
Initial studies suggested that younger individuals were generally less prone to developing severe symptoms potentiated by high levels of inflammation, with the majority of severe cases belonging to immunocompromised people, such as the elderly population and those with preexisting conditions. So, while it is easy to think of young people as being relatively immune to the disease, they represent the most dangerous demographic, potentially unknowingly transmitting the disease to the most immunocompromised and susceptible individuals.
In addition to understanding how COVID-19 acutely affects
an infected individual, analyzing the impact of the virus on longterm health outcomes can serve as a valuable tool to embrace healthy living habits. A study from the University of Washington and Stanford University School of Medicine displayed a strong inverse relationship between smoking and COVID-19 mortality rates across forty countries. However, mortality variation across countries was determined to be too great to be accounted for by the consequences of smoking, attributing various confounding variables to the observed protection that smoking supposedly provided. In fact, ensuing studies showed that the high levels of inflammatory markers associated with long-term smoking not only caused smokers to be more susceptible to severe COVID-19 symptoms, but also left them with further lung scarring and damaged systemic organ tissue. With so much to be learned about COVID19 as it pertains to chronic health outcomes, it becomes increasingly more critical to understand how the virus ravages the body even following recovery, ultimately highlighting the need to adopt anti-inflammatory and disease-warding lifestyles.
INFLAMMATION AND METABOLIC DISEASE
In a study analyzing the impact of the ketogenic diet on adipose (fat) tissue inflammation, mice fed a high fat and low carbohydrate diet displayed increased VAT γδ T cell expression, reduced pro-inflammatory macrophages associated with metabolic dysregulation, and a “protective gene expression signature”, suggesting that the diet not only boosted metabolism and decreased adipose tissue volume, but also conferred a protective effect on the mice. By seemingly altering immune function, the diet had a profound impact on the health of the mice, albeit brief. These results show that in addition to enhancing fat metabolism, the diet can directly modulate immune mechanisms, leaving much to be uncovered about its implications on metabolic disease, and other concurrent proinflammatory diseases.
THE INTErACTION BETwEEN THE KETOGENIC DIET AND THE COMOrBIDITY OF DISEASE
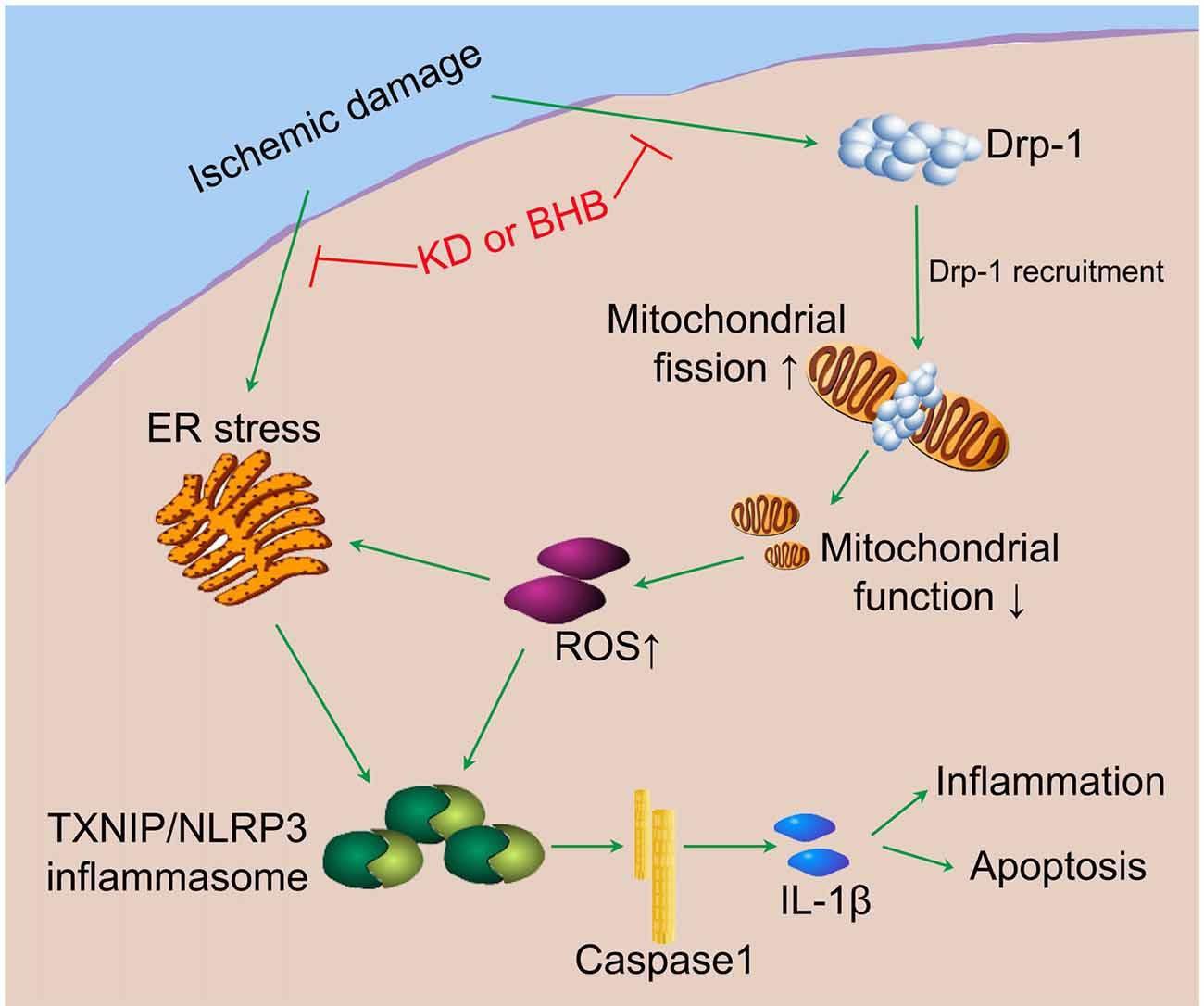
Anti-inflammatory diets such as the ketogenic diet are vital to staving off deadly proinflammatory disease. While the ketogenic diet is yet to be completely elucidated in the context of its comorbidity with a host of inflammatory diseases, it has a direct impact on the inflammasome, a multiprotein complex that detects stressors and pathogens and activates proinflammatory cytokines to fight off pathogens. In a mice study, the most prominent ketone present in our blood, beta-hydroxybutyrate, was shown to prevent the inflammasome from activating, in turn inhibiting an activation cascade that would otherwise exacerbate inflammation (Figure 1). Additionally, the diet greatly increased goblet cell production, critical to successfully mounting an immune response against pathogens, and reduced myeloid cells that typically mount a massive proinflammatory immune response. Furthermore,
the ketogenic diet had implications on the level of the genome: through RNA sequencing analyzing γδ T cells, the ketogenic diet was shown to increase anti-inflammatory gene expression. By boosting mitochondrial efficiency of γδ T cells, a class of T cells with a distinctive T cell receptor most prevalent in the gut mucosa, the body is primed and more efficient ischemic damage.
INTErVIEw wITH NEurOSurGEON
I spoke to a neurosurgeon at Mount Sinai in New York City to discuss what factors helped him decide to utilize the diet. The physician, who was placed in the COVID-19 ward at his hospital when NYC was the epicenter of the virus, mandated that his patients on ventilators be put on a strict low carbohydrate regimen. As an individual aware of the at responding to and mounting an attack against pathogens and subsequently reducing the systemic inflammatory load. Likewise, the coronavirus has been shown to impact immunocompromised individuals and people with preexisting conditions. Seeing as the ketogenic diet has profound chronic impacts at both the gene and metabolic levels, therapeutic benefits of the diet, it was an easy, evidence-driven choice for him. “We put a couple of patients on an old form of tube feed called PulmoCare (a relatively high-fat, low carbohydrate form of tube feed). When it became clear that what was killing them was a massive inflammatory surge, we knew what direction we should be taking the care.” Despite not evaluating these patients’ health outcomes, he emphasized the value of mitigating a cytokine storm prompted by COVID-19. employment of the ketogenic diet in coronavirus-stricken patients holds promising results. While it is currently difficult to compare the results seen in mice to those of COVID-19 patients, several studies have been undertaken to analyze the symptoms and progress of the disease in the context of
Figure 1. The potential pathway by which the ketogenic diet modulates inflammasome activity: ketones such as BHB inhibit Drp-1 recruitment, thereby diminishing inflammation and boosting the brain’s recovery capacity to
A MOuNT SINAI
the ketogenic diet. Ever since then, he discussed the health outcomes he saw first-hand as a result of anti-inflammatory measures taken. “People aren’t dying at the rate they were towards the beginning of the year, the reason primarily being both a low-carbohydrate diet and steroid administration. As a result, that inflammatory surge is happening a lot less. The overall mortality rate is far lower than it was in February and March.” Despite not evaluating these patients’ health outcomes and their recovery capacity, his

decision to employ a carbohydrate restrictive tube feed on intubated COVID-19 patients was a testament to the therapeutic and widespread value of implementing the ketogenic diet, both in practice and as a preventative measure.
ADAPTATION
While this diet presents benefits including reduced low-grade chronic inflammation associated with a host of proinflammatory diseases, weight loss, boosted mental clarity, etc., many individuals have cited negative outcomes, including initial irritability and low sustainability in the long-term. In addition to having to adapt to the new coronavirus era, people would be forced to adapt to the new challenges and experiences that the ketogenic diet brings. “When people are in a stressful environment, they tend to not go to the unfamiliar. It’s a little hard to get people to think out of the box in crisis mode”, said the physician I spoke to. However, a study from UCSF shows that even slight restriction, not just complete ketosis, can positively affect the gut microbiome, so some of the effects of the diet can be conferred quite quickly. This evidence explains that even in a short duration of employing the ketogenic diet, some of its anti-inflammatory benefits can be reaped quickly, eliminating any adaption or commitment to the diet that people would otherwise find to be unsustainable. While restrictive ketogenic diets can be employed to severely ill coronavirus patients who present otherwise few options for treatment, the data show that some of the conferred benefits are obtained rapidly and have a lasting impact on patient outcomes.
Understanding the comorbidity of disease with the coronavirus has remained an elucidating point for future treatment. In understanding how the ketogenic diet has improved COVID-19 patient outcomes, we create the opportunity to not only better understand the mechanisms by which COVID-19 spreads and is transmitted, but also to shed light on potential therapeutic approaches to other proinflammatory diseases, and how we can take preventative measures to mitigate risk of these diseases. Despite the broader positive implications of ketogenic diet employment, there is still more to learn about the coronavirus. With so much currently unclear, further studies are warranted to analyze the comorbidity of coronavirus and inflammatory diseases.
Anand, Paras. “Faculty Opinions Recommendation of Ketogenic Diet Improves Brain Ischemic
Tolerance and Inhibits NLRP3 Inflammasome
Activation by Preventing Drp1-Mediated
Mitochondrial Fission and Endoplasmic
Reticulum Stress.” Faculty Opinions – Post-
Publication Peer Review of the Biomedical
Literature, 2019. https://doi.org/10.341 0/f.732878128.793559831. Chowdhry, Kavya. “Has COVID-19
Highlighted Social Injustice Built into Our
Cities?” The Centre for Evidence-Based
Medicine. University of Oxford, October 7, 2020. https://www.cebm.net/2020/10/ has-covid-19-highlighted-social-injusticebuilt-into-our-cities/. Dutta, Sanchari Sinha. "Keto diet could be beneficial for elderly COVID-19 patients".
News-Medical. https://www.news-medical.net/ news/20200914/Keto-diet-could-be-beneficialfor-elderly-COVID-19-patients.aspx. (accessed
November 1, 2020). Robertson, Sally. "An inverse relationship between smoking and COVID-19". News-Medical. https://www.news-medical.net/news/20200615/
An-inverse-relationship-between-smokingand-COVID-19.aspx. (accessed November 12, 2020). Schnell, Patrick. Photograph. New York, March 30, 2020. Mount Sinai Brooklyn. Stubbs, B.J., and J.C. Newman. “Ketogenic Diet and
Adipose Tissue Inflammation—a Simple Story?
Fat Chance!” Nature Metabolism 2 (January 20, 2020): 3–4. https://doi.org/https://doi. org/10.1038/s42255-019-0164-2. Weiler, Nicholas. “Ketogenic Diets Alter Gut
Microbiome in Humans, Mice.” Ketogenic
Diets Alter Gut Microbiome in Humans, Mice |
UC San Francisco. University of California San
Francisco, May 13, 2020. https://www.ucsf.edu/ news/2020/05/417466/ketogenic-diets-altergut-microbiome-humans-mice.










