Wilmot Takes on Lung Cancer in the Rochester Region





Hello
In the last Dialogue, I offered my thoughts on Wilmot’s extraordinary five-year journey to obtain a special grant that would designate us by the National Cancer Institute as a top center in the U.S. Our results were extremely encouraging: Wilmot received a very competitive score and although we have not yet achieved that designation — we were invited to resubmit our proposal within the next 18 months through a new, fasttrack mechanism created by the NCI. Wilmot is the first and only cancer center to be invited to take advantage of this new mechanism, indicating that we are very close to accomplishing our goal. I have great optimism and pride in the entire Wilmot team, and look forward to sharing additional good news in the future.
One of the formal programs we launched for NCI designation is called Community Outreach and Engagement (COE). As this office matures and expands its partnerships, we think it is important to share the COE’s important work. You’ll find highlights on page 10, and more about the COE in future editions of Dialogue
Jonathan W. Friedberg, M.D., M.M.Sc. Director, Wilmot Cancer Institute
In preparation for the NCI grant, we performed a comprehensive assessment of the cancer burden in our area. We uncovered a disturbingly high incidence and mortality rate of lung cancer in Rochester and nearby counties in western and central New York. The cases are due in large part to disproportionately high smoking rates in our urban centers and rural areas, and in our cover story you’ll see that Wilmot is doing all that it can — from quitting support and screening opportunities to advanced therapies — to curb this trend and offer the best, multidisciplinary care to our patients. Similarly, breast cancer incidence is particularly high in Monroe County. Wilmot recently hired a fantastic new leader for our breast cancer program, Anna Weiss, M.D., who is also featured in this edition. She trained at world-class institutions and brings a vision to elevate research and care for all breast cancer patients.
Finally, I’d like to call your attention to a hidden gem at Wilmot — our “Shared Resources,” which are presented on pages 8 and 9. As cancer care and research has become more complex and recruitment of faculty and staff extra competitive, it’s imperative that elite cancer centers like Wilmot offer the latest technology and professionals who are specially trained and intimately familiar with this technology. Wilmot subsidizes these activities in a way that’s financially prudent and supportive for all of our scientists. The NCI, in fact, rated our Shared Resources team as outstanding, an endorsement of a key strength and our national leadership in this area.
As 2022 comes to a close, I want to thank our community and all Wilmot supporters for a tremendous year. We are always learning and striving to do our best for you. Meliora!
Jonathan W. Friedberg, M.D., M.M.Sc. Director, Wilmot Cancer Institute
Advisory Board
Members, '21-'22
Richard Yates, Chair
Elaine Bucci
Scott Burdett
Patrick Cunningham
Garth Hankinson
Kathleen Landers
John McKenna
Jett Mehta
Carol Mullin
Ralph Olney
Doug Parker
Walter Parkes
Mary Pluta
Ronald Pluta
Barbara Pluta-Randall
Victor Salerno
Erika Stanat
Dr. Eduardo Torrado
Jerome Underwood
Angela Uttaro
Kristin Vanden Brul
Paul Wilmot
Keith Yeates
John Zicari
Darren Carpizo, M.D., Ph.D.
Yuhchyau Chen, M.D., Ph.D.
Paula Cupertino, Ph.D.
Aram Hezel, M.D.
Gary Morrow, Ph.D., M.S.
Louis S. Constine, M.D.
Paula Vertino, Ph.D.
Emeritus Members
Judy Linehan Jim Ryan, Jr.
Kellie Anderson
Clare Flanagan

Jonathan W. Friedberg, M.D., M.M.Sc.
Hucky Land, Ph.D.
David Linehan, M.D.
Mark Taubman, M.D.
Honorary Board Members
George Abraham, M.D.
Michael Buckley
Rina Chessin
Elaine Del Monte
Richard DiMarzo
Malik Evans
Joan Feinbloom
Janet Felosky
James Hammer
Paul Hanrahan
Gary Haseley
Sandra Hawks Lloyd
Mark Kokanovich
Michael Linehan
Alyssa Lozipone
Ronald Maggio
Steve McCluski
Michael Norris
Jeffrey Pierce
Cheryl Pohlman
Larry Rabinowitz
Donald Rhoda
Gregory Smith
Philip Wehrheim
Steve Whitman
Timothy W. Williams
Colleen Wilmot
Dennis Wilmot
Timothy P. Wilmot
Thomas Wilmot
Bruce Zicari II
Dialogue
Editor / Writer
Leslie Orr Leslie_Orr@urmc. rochester.edu
Contributing Writers
Kellie Fraver, Susanne Pallo, Kristina Beaudett, Kristine Thompson
Feature Photogaphy
Erich Camping, Jeff Witherow, Matt Wittmeyer
On the Cover Lung cancer survivor Maria Valeria Hernandez Quintana, of Victor, N.Y. (Photo, Jeff Witherow)
The Wilmot Cancer Institute is a component of Strong Memorial Hospital.
Wilmot’s breast cancer program has a new leader, Anna Weiss, M.D., who joined the faculty this fall from Harvard University 's Dana-Farber Cancer Institute. She discusses her vision 2
November is Lung Cancer Awareness Month, a good time to talk about this high incidence cancer in the region and the full spectrum of what Wilmot offers to patients 4
Shining a spotlight on the crucial tools and smart people on the Shared Resources teams that elevate Wilmot research 8

Wilmot’s Community Outreach and Engagement Office is the real deal: Its services and research are helping thousands of people in the Rochester region 10
NEWS BRIEFS 11
ADVANCEMENT NEWS
Read about the generosity of Rochester Deputy Mayor Patrick Cunningham, and hundreds of others in the community who support Wilmot 14
Rochester is an “irresistible, once-in-a-lifetime professional opportunity,” says Anna Weiss, M.D.

This is a high compliment, coming from an MD Andersontrained and Harvard University breast cancer surgeon. She arrived in Rochester this fall to serve as Wilmot Cancer Institute’s new Director of the Breast Cancer Service Line.
What lured her to the University of Rochester Medical Center? Weiss credits a culture of teamwork. She says the vision feels authentic and unified among the top leaders, despite their full plates and different responsibilities.
During many separate interviews, for example, she noticed that Wilmot Director Jonathan Friedberg, M.D., was on the same page as Chair of Surgery David Linehan, M.D., who was on the same page as Jennifer Harvey, M.D., Chair of Imaging, who had the same vision as Department of Medicine Chair Ruth O’Regan, M.D., and Wilmot Associate Director for Community Outreach and Engagement, Paula Cupertino, Ph.D. (Cupertino, Linehan, and O’Regan also serve on Wilmot’s executive committee.)
“Every single person is looking in the same direction — and that is not common,” Weiss says.
As she settles into western New York and her new role, which also includes Program Leader of Breast Surgery and Director of the Comprehensive Breast Care Center, Weiss took a minute to talk about what she brings to the Wilmot team.
Following is an edited conversation.
Welcome to Rochester! What are your plans for the breast cancer program?
There’s a few things. First, to take a group that already has really strong pieces and then to finish the puzzle, making it cohesive, if you will, is a really exciting prospect. I think the potential to elevate this group is huge.
On the immediate horizon: We need a program for people with an elevated risk of breast cancer. We already have something in its infancy and I’d like to see this grow. It would involve enhanced screening and providing a detailed look at a woman’s risk of future breast cancer. We have so many extraordinary pieces for
this program: Wilmot has one of only seven NIH-NCORP cancer prevention and control grants in the country, and has a certified genetics team. We just need to make sure women know it’s available. One of our breast surgeons, Jessica Gooch, also has a particular interest in risk and prevention research, and my goal is to engage her to help strengthen this area. And the chair of Imaging, Dr. Jennifer Harvey, has focused her career on breast density and how it relates to the risk of future breast cancer.
My other immediate plan is to solidify our survivorship program, while also making sure that our providers have a bit more space for newer patients, as well.
Another area where we can really distinguish ourselves is in clinical trials. For example, there is an interesting national clinical trial looking at the safety of omitting or reducing radiation for low-risk, early-stage breast cancer patients. At an academic medical center, we can offer more of that type of clinical research than community hospitals.
And finally, when I spoke to Paula Cupertino we talked about getting out into the community more often. I told her, absolutely, I’ll come to weekend events! There are plans for a ‘mammo van,’ (a mobile unit that provides imaging services) — and I know that everyone is feeling the same way and wants the same things in terms of community outreach.
During the past few months, I’ve been meeting with community leaders and Wilmot’s partner organizations that are focused on breast cancer. They have provided a lot of insight and have been so welcoming.
You mentioned the importance of clinical research. What are your thoughts about finding that sweet spot of treatment for each woman and each subtype of breast cancer?
My guiding principle is shared decision-making and coming up with the right plan for each patient. I like to call it ‘right-sized therapy.’ Or personalized therapy. It’s about figuring out exactly which patients are less or more at risk of the cancer returning, and giving them the correct amount of therapy to treat those risks based on the latest research.
This approach is especially important as the population ages. (Wilmot has a nationally recognized clinic for caring for older adults with cancer. Weiss says she’s excited to connect with this group of providers, particularly Allison Magnuson, D.O., who is enrolled with Weiss in the highly selective American Society of Clinical Oncology leadership development program this year.)
I’ve worked with patient advocates for a long time in the development of institutional clinical trials at Dana-Farber. They’re often breast cancer survivors. They’re brilliant and I’m consistently floored by how savvy they are in trial design. They are involved from day one. We always try to get a balanced assessment of what their reactions are to the trials and what is important to them. Are we doing enough for aggressive cancers? But also keeping in mind the side effects of treatment.
Sometimes, as scientists and surgeons and doctors, we get a little bit narrow, like having laser vision for a problem, and we can forget the whole picture. So, it’s good to have reminders from people who care. I think we have a really big opportunity for more community outreach and input.
Where do we stand with breast cancer today?
What does the future look like?
You know, breast cancer is not a death sentence any more for most people. Many women are going to live for decades and decades.
I would say our biggest, exciting frontier right now is new systemic therapies and new targeted therapies. This is probably true for all types of cancers, but in breast cancer it’s about being able to analyze the tumor for receptors and then tailoring therapy appropriately. Sometimes you can even target a tumor with a very small amount of receptor, such as having a low level of the HER2 protein. It’s just a really exciting time.
There are so many clinical trials happening that advance care all across the U.S. and we are part of it here at Wilmot. They are developing and discovering new drugs all the time. We’re also working on right-sizing breast cancer surgery to decrease side effects.
We have some very heavy hitters here at Wilmot — like Ruth O’Regan, M.D., and Carla Falkson, M.D. — and my job is to improve the infrastructure so that all of our

improvements in medicine, surgery, shorter courses of
Why did you choose to specialize in breast cancer?
When I was a surgery resident, I just loved cancer surgery. The interactions with the team — the surgeon, the medical oncologist, the radiation oncologist, the imaging specialists — it was always exciting. The plans were well thought-out and well-executed.
I felt that I could continue my life-long learning in this space where
Also, some of my attending physicians in surgery were just the best teachers. In medicine, we call it the triple threat — surgery, research, teaching — and I want to contribute in that way.
You are a Syracuse native, which is part of the reason for coming back to upstate New York. What else can you tell us about yourself?
Oh, people ask me: ‘What is your hobby?’ and I say, ‘Does writing clinical research papers count?’ (She laughs) Actually, I have two amazing dogs and I have awesome parents who live in Syracuse and I’m very close to them. We all like to get outside and walk nature trails, which central New York has in abundance.
I’m very close with my extended family that also lives in upstate New York. They have a dairy farm and I’ve spent my entire life visiting the farm. I’ll go and have dinner and my cousins, who’re all women, will go out and round up the calves. As a kid, I also spent every Christmas at my brother’s godparent’s house in Henrietta.
During my time in Boston, I think I learned that I’m not a big-city person. So far, Rochester offers amazing dining and attractions, but is so easy to live in.
When I bought my house in Fairport and did the walk-through at closing, people in the neighborhood started to come out of their houses to welcome me. They were all so nice!
At Wilmot, I want people to know that they can come and talk to me. Ask me questions. If you have ideas, just approach and tell me. Sometimes, people are surprised to learn I’m a surgeon because I don’t match the stereotype that some people have about my profession. I like that about myself.
I’m hoping to bring that flavor of happiness and brightness and cheeriness to the group.

Maria Valeria Hernandez Quintana grew up in the vibrant city of Buenos Aires, Argentina, and was raised by two loving parents who happened to smoke cigarettes. Her maternal grandfather died of lung cancer.
But the city’s issues with air pollution, the second-hand smoke, and the family medical history were hardly on her radar until, at age 48, doctors found a fist-sized tumor on her lungs. She was officially diagnosed with adenocarcinoma, the most common form of lung cancer, on Jan. 2, 2020, and went through surgery and months of chemotherapy and radiation.
“The whole experience felt surreal,” says the Victor resident, who has never smoked.
“What kept me sane was a positive attitude,” she says. “Telling myself: ‘I’m going to get through this. Cancer is messing with the wrong woman.’”
In the 27-county Rochester region from which Wilmot Cancer Institute draws patients, the lung cancer incidence rate is a startling 70 cases per 100,000 people. That’s much higher than in all of New York State, at 58 cases, and in the U.S., which is about 53 cases per 100,000 people.
Although in some areas cigarette smoking seems to be less prevalent these days, data tell a different story. The Rochester region’s smoking rates are higher than state and national averages, and combined with other risk factors such as heredity, the lung cancer problem is compelling.

“The data have been a wake-up call to the University and to all of us in health care,” says Carolyn Jones, M.D., who leads Wilmot’s Lung Cancer Service Line and is also chief of Thoracic and Foregut Surgery at the University of Rochester Medical Center.
Jones, M.D.“If we have these pockets of very high incidence rates of lung cancer, are we really doing all we can to help those neighborhoods, those zip codes, and to look for solutions?”
Jones believes the high rates may boil down to three things: “Not quitting, not getting screened, and not getting linked to proper care.”
Lung cancer is the second most common cancer in the U.S. and the leading cause of cancer deaths in men and women. As in the case of Maria Valeria Hernandez Quintana, 20 percent of lung cancer patients have never smoked.
And yet cigarette smoking — or what some call “the disease of tobaccoism” — is still the cause of 80 percent of lung cancer deaths, according to Patricia Rivera, M.D., Wilmot’s associate director for Diversity Equity and Inclusion, and the C. Jane Davis and C. Robert Davis Distinguished Professor of Pulmonary Medicine at URMC.
“For decades, we’ve shamed these individuals instead of leading them to treatment and helping them to quit smoking,” she says.
Racial and ethnic differences in how health care is accessed and delivered, lack of insurance, and lack of education about risks, are likely factors that play out in this region, as they do across the country. For example, the lung cancer incidence rates locally are even higher among Black people, at 75 cases per 100,000 people.
Rivera notes that Black men in the U.S. are at the highest risk for being diagnosed with lung cancer and dying — even if they smoke less than white men.
Lack of awareness about lung cancer screening contributes to the problem. “Everybody knows about breast cancer screening or colon cancer screening,” Rivera says, “but lung cancer screening is lagging, which leads to the higher death rates.”

“It’s a very complex problem,” she adds. “And that makes it more difficult to come up with the best approaches.”
Detecting lung cancer early, at stage 1, is a key to survival.
Strong Memorial Hospital and affiliates offer low-dose CT scans to screen those who qualify. The scan shows detailed images of the lungs and air tubes, and can pick up small tumors, using less radiation than conventional CT scans but with more specificity than chest x-rays.

Studies show that individuals whose cancers are detected via low-dose CTs are 20 percent less likely to die from lung cancer than those who received chest x-rays, Rivera says.
Who qualifies? Individuals 50 to 80 years old, who are currently smoking or have quit within the last 15 years. Smoking history must include at least one pack of cigarettes a day for 20 years, or a halfpack for 40 years.
Rivera emphasizes that shared decision-making between doctor and patient is required; the screening can occasionally turn up benign nodules, and if a person seeks screening but is still smoking, that individual must enter a tobacco-cessation program.
Lung cancer screening is currently underutilized. Nationally, only about 6.5% of people who are eligible take advantage of it.
“It’s a traumatic thing to go through,” says Hernandez Quintana, who works as a Spanish interpreter for the Victor Central School District. She is known as “Val Cleary” to her local friends and family, which includes husband Jason Cleary and two sons.
“But everyone was so amazing at Wilmot,” she adds. “They treat you like a human.”
She remains in remission. “Every morning, I thank God that I’m here — and I move forward.”
Her advice for others? “If you feel like something is wrong in your body, push, push, push. Don’t just think it will go away.”
Acting quickly in a multidisciplinary fashion and being able to find the best combinations of treatment for each individual is the goal, says Mulford, M.D., professor of Clinical Medicine and a Wilmot leader in clinical research. She prizes Hernandez Quintana as a model of self-awareness.

“Her story — a person who keeps trying to uncover why they don’t feel well — is what we like to see. New therapies, sometimes, can make a difference in patient’s lives but there are a lot of other factors and, obviously, that’s not the end of the story.”
The days leading up to Hernandez Quintana’s diagnosis are vivid. She is a longtime fall allergy sufferer, and in August of 2019 the usual dry cough started. In November, she was still coughing, which was unusual. She remembers that it got so intrusive she was “begging my allergist to make it stop.”
“I felt like something was different,” she says. She received a chest x-ray, which showed a shadowy lesion on the lung. After a second x-ray, doctors ruled out pneumonia and other illnesses, and then a bronchoscopy revealed the full mass.
“I’m still not thinking it’s cancer,” she recalls. “I’m a runner, I eat healthy, I’ve never smoked in my life. We’re like, what could it be?”
It was stage 3 lung cancer. The next step was to find out if it was operable — and this is when she caught a lucky break.

“My oncologist, Dr. (Deborah) Mulford, called one of the surgeons, Dr. (Christian) Peyre, and he happened to be in his office at that moment, three floors away, and agreed to see me immediately. He reviewed my films and scans and says, ‘I can operate.’ Well, I started crying with joy, and I hugged him and kissed him! His mother is from Honduras, so he understands our kissing culture — but he says, ‘Don’t kiss me yet. Let’s bring your case to the tumor board and get the surgery done first.’“
In January 2020, Peyre removed the upper lobe of her left lung and nine nearby lymph nodes, three of which were malignant.
For those who are diagnosed with certain types of lung cancer or cannot have their tumor removed, immunotherapy drugs, such as Keytruda and Optivo, have completely changed the landscape of lung cancer care, Mulford says. When the cancer is active, she explains, it sets up checkpoints that block the body’s healthy immune cells from attacking cancer.
The newer drugs release the blockade, allowing immune cells to clear out the cancer cells. Immunotherapy can also provide the possibility of a long-lasting response to therapy.
Clinical trials are available that evaluate new ways to stimulate the immune system or to use immunotherapies in combination with chemotherapies at different stages of disease. Many Wilmot patients have benefitted, Mulford says.
Other innovations also provide exceptional care options: Wilmot has the only state-of-the-art Varian Edge Linear Accelerator in upstate New York. This technology is for individuals with non-small-cell, early-stage lung cancer who do not qualify for surgery. The device uses imaging and customized high-energy beams to target a tumor’s shape and deliver radiation therapy as precisely as possible.
For biopsies, which are critical for an accurate diagnosis, Wilmot has a super-dimensional robotic tool called the Davinci Ion system. It allows physicians to navigate to small tumors located deep in the lungs for streamlined diagnosis and staging in difficult cases.
UR Medicine has a dedicated lung cancer pathology team that works closely with Wilmot surgeons, pulmonologists, medical oncologists and radiation oncologists. Led by Moises Velez, M.D., the pathologists provide detailed molecular studies of the tumor with an eye toward gene mutations, so that patients can receive the most effective and personalized therapy possible. They also store tissue for re-evaluation in the future, when new treatments become available.
Surgery and recovery are often faster and more efficient, as Wilmot surgeons are able to use minimally invasive robotic systems in about 50% of cases. One new type of technology offers a one-stop shop for eligible patients: an imaging scan that marks the lesion, and the ability to perform a biopsy and remove the tumor in a single surgery.
“Long gone are the days of King George VI’s lung cancer,” says Jones, the Wilmot service line chief. The former King of Great Britain, who was the late Queen Elizabeth’s father, notoriously had his left lung removed in a makeshift operating room in Buckingham Palace, in 1951. He died a year later.
That was 70 years ago. In more recent times, research-based improvements have come fast and are continuing. “And that’s a good thing,” Jones says.

Wilmot scientists are studying many aspects of lung cancer, including prevention, lung damage at the cellular level, and protecting the lungs from injury during treatment.
The latter is the focus of Brian Marples, Ph.D., the Dr. Sidney H. and Barbara L. Sobel Professor of Radiation Oncology. A renowned radiation biologist, he and his Wilmot team recently received an award from the National Institute of Allergy and Infectious Diseases to investigate how to reduce pulmonary injury in patients undergoing radiation therapy, especially when those patients have recently been infected with a virus in the lungs.
Another top investigator of lung diseases, Irfan Rahman, Ph.D., has multiple publications in high-impact medical journals on the harms of cigarette smoke and vaping chemicals on lung tissue and cells deep within the organs. He has shown that vaping associated with wheezing, for example, can be a precursor to emphysema, lung cancer,



and other illnesses. With the popularity of vaping in recent years among younger people, Rahman is also focused on providing evidence to inform the U.S. Food and Drug Administration and other regulators about the adverse effects of vaping products on health. He is a Dean’s Professor of Environmental Medicine, and a professor of Public Health Sciences and of Medicine.
Prevention research is also a priority for Wilmot.
“Lung cancer is something that you cannot examine by touch, so you have to reply on symptoms, which unfortunately don’t always happen until tumors are big,” Jones says. “So, it’s essential that we focus on who’s at risk and on preventing cancer.”
Francisco Cartujano, M.D., operates clinical studies in community-based settings for people underrepresented in health systems. Many of his projects are smoking cessationrelated — in one case evaluating what types of text messages via mobile phones work best to motivate people to quit. He works closely with the local and regional Latino and Puerto Rican communities to stem their high rates of smoking, and he is a co-leader of Wilmot’s Community Outreach and Engagement Office (see page 10 for more on the COE).
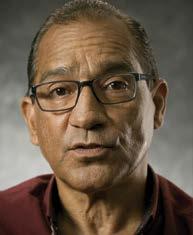
Carlos Santana, a community building in action coordinator for Action for a Better Community in Rochester, is a success story. A former heavy cigar smoker, he says he challenged Cartujano and actually set out to prove that his quit-smoking program wouldn’t work. But to Santana’s surprise, he was able to quit.
Wilmot offers a Tobacco Dependence Treatment Program for those who have been diagnosed with cancer and would like to quit. To participate, call (585) 275-5823.
Two free programs are available to people who smoke but who do not have cancer. Please contact Wilmot's Text-to-Quit program at (585) 504-9461 or email quitcenter@urmc.rochester.edu, or contact the UR Center for Community Health & Prevention's quit program at (585) 602-0720.
Ph.D.Carlos Santana
“I quit smoking through the text messaging program and then with the help of patches,” Santana says. “The chemicals in my lungs went from 100% to zero. You can make believers out of those who think quitting is a joke!”
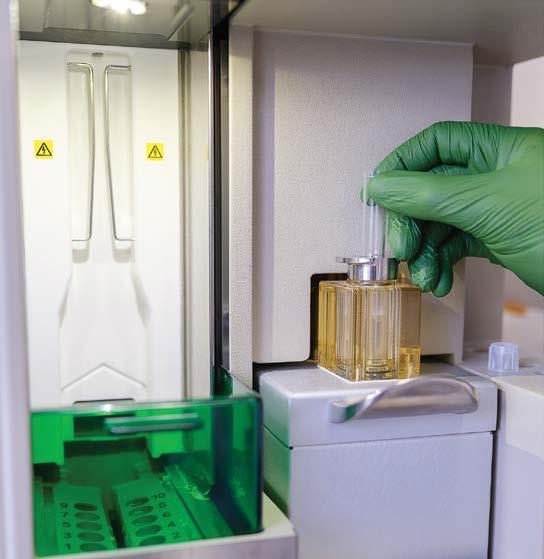
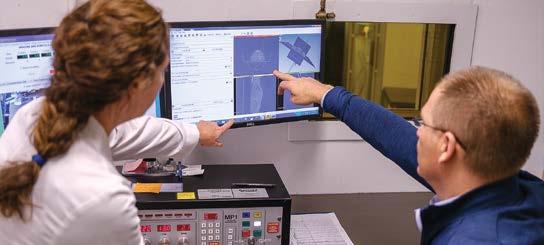
Innovative and complex cancer research takes state-of-the-art technology — and a village. Wilmot Cancer Institute has six Shared Resource labs that provide the large and highly diverse research community with access to many cutting-edge services, from imaging to genomics and carefully curating donated tissue. While this involves high-powered machines, it’s the experts in those labs who make the true difference. Wilmot’s Shared Resources and talented teams are vital to the work that advances cancer prevention, diagnosis, and treatment.
With patients’ consent, this group collects and carefully preserves biopsied tissue samples and clinical data that researchers can use to test new theories and make discoveries.

These experts help researchers design the most statistically sound studies that will provide accurate and reliable results. Experts support researchers at every step of the process, from designing studies to analyzing data and interpreting results.
This team supports Wilmot’s basic, translational, and clinical investigators by providing cutting-edge resources and technical expertise for analysis of cell and tissue characteristics, and for implementation of best practices in research and clinical trials.
Wilmot scientists work closely with the Genomics team to access high-quality screening and genomics technologies for studying gene structure and function in cancer cells.
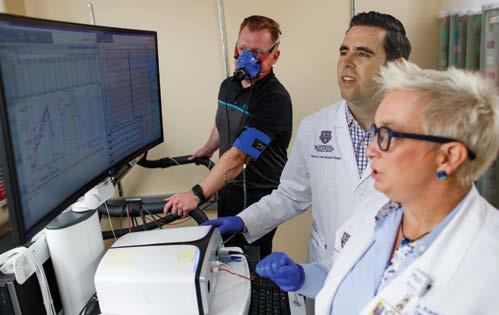
Studying the connection between physical activity, cancer and its treatment, and wellness, is the focus of a groundbreaking team at Wilmot. This lab provides resources for integration of human performance assessment data, biospecimen analysis, and physiology data to support clinical and translational research studies.
This team has the expertise and training to offer the latest imaging and advanced data assessment for Wilmot researchers. Goals include protecting non-malignant tissue from radiation injury and developing the most precise therapies possible.
John M. Ashton, Ph.D., M.B.A., wears many hats but he has a singular focus and passion: to increase the impact of Wilmot’s Shared Resources, a set of labs providing cancer researchers with access to state-of-the-art technologies and expert guidance.

“What sets us apart is the people behind the technology,” says Ashton, who has served as director of Wilmot’s Shared Resources for five years. “We have a team of about 45 experts who collaborate with researchers and provide a unique perspective to help them innovate and move their research to the highest impact possible.”




Ashton first came to Rochester over 20 years ago, planning to go to medical school. But a brief stint working at a biodefense firm after he earned a bachelor’s degree in biotechnology from RIT, changed his mind and his path.

“I was working on pathogen detection at a time when everyone was afraid of bioterrorism,” he says. “That experience changed my perspective and made me feel like I could have a bigger impact in this space than I could as a medical doctor.”
In 2005, Ashton joined the University of Rochester and he’s been here ever since - earning a master’s degree and doctorate in Genetics from the School of Medicine and Dentistry, and an MBA from the Simon School of Business along the way.
“My doctoral research gave me experience in analytical thinking, and mentoring and really gave me the tools to do what I do today,” says Ashton, “and my MBA gave me the skills to manage and motivate teams and run the Genomics Research Center with a business focus while still having scientific rationale in mind.”

The cancer incidence across Wilmot’s 27-county western and central New York region is high — and it has remained consistently higher than U.S. and New York State rates for the past 20 years. In fact, if these 27 counties were a separate state, it would have the second highest rate of cancer in the country. Wilmot is committed to reducing this cancer burden and improve the health of local residents in partnership with community organizations, leaders, and coalitions throughout the region.
The Community Outreach and Engagement (COE) Office is the catalyst for this partnership. COE applies the principles of community-academic partnerships to achieve its goals, which are to reduce disparities in the continuum of cancer care and promote cancer health equity. Working closely with the COE is a group of 34 people who form a Cancer Community Action Council (CCAC), which is organized into four priority areas: prevention of cancer, survivorship, access to services and regional integration, and community-based research. CCAC members represent 46 local organizations, and offer guidance to Wilmot leadership,
clinicians, and researchers, providing a much-needed community voice in planning and strategic activities.
Ultimately, CCAC priorities and questions also help Wilmot’s basic scientists to be more responsive. Wilmot’s efforts to address the impact of cancer are strengthened and transformed because of the power of these partnerships.
The COE Office is led by Associate Director Paula Cupertino, Ph.D., and Assistant Directors Charles Kamen, Ph.D., and Francisco Cartujano, M.D., and Chief Community Impact Officer Candice Lucas, Ed.D. The COE office employs a full team of community health workers and health project coordinators.
To learn more, or get involved, (si quiere conocer más o participar), please email: Wilmot_COE@urmc. rochester.edu


COE has participated in more than 500 community events in the past two years, serving more than 10,000 community members from diverse backgrounds.

More than 2,000 people have attended free cancer education events in the catchment area.
Nearly 16,000 uninsured and under-insured people have been guided to free cancer screening through COE’s state-funded Cancer Services Program.
With the support and advocacy of COE, 1,426 cancer patients have received free integrative oncology services.
More than 600 smokers have been offered free mobile smoking cessation treatment through COE’s Tobacco Quit Center.
Zip codes in suburban Webster, N.Y., have the highest number of new cancer cases in the entire Rochester metropolitan area, and the highest number of new patients who seek care at Wilmot. So, it made sense to bring Wilmot’s signature multidisciplinary care directly to the town, with a brand new facility serving the east side of Monroe County and neighboring Wayne County.
Wilmot executives, physicians and nurses, and Webster officials, neighbors and patients, all gathered on a gorgeous early-July afternoon to cut the ribbon. The 21,000-square-foot medical building opened for business on July 11, 2022.



Regional locations, such as Webster, serve more than half of all Wilmot patients. “We are thrilled to be able to open the doors to the Wilmot Cancer Institute Webster to serve that need,” says Daniel Mulkerin, M.D, associate director, Regional Operations at Wilmot. “Patients have been asking for a Wilmot location in Webster and we are happy to make that request a reality.”



The oncology facility — Wilmot’s 14th in western New York — is staffed with expertise in medical oncology, radiation oncology, surgical oncology, and clinical trials. The $6.7 million construction project boasts a $3.7 million linear accelerator for radiation therapy.
Because cancer care is more complex than ever, it requires a coordinated effort by experienced professionals in many disciplines, says Wilmot Director Jonathan Friedberg, M.D., M.M.Sc. “Our Webster office brings Wilmot Cancer Institute’s precision medicine approach closer to home for our patients and their families.”
The new building is located at 875 Hard Road, near Route 104, and can be reached by calling (585) 602-3150.



Wilmot scientists had a great year for bringing in peer-reviewed funding: new grants totaled more than $17 million. Most impressive is that the newly funded investigators represent multiple fields of study; projects range from basic science into the bone marrow’s role in supporting leukemia, and how to stop breast cancer cells from making their own antioxidants, for example, to a unique translational study that will benefit older patients who struggle with dementia as well as cancer. Also, of note and promising for the future: nearly half of the award winners are early-career investigators or are just beginning to hit the mid-career stage. The grant haul points to the success of recent recruiting efforts and research program restructuring at Wilmot.
Ovarian cancer detection took some big steps forward, thanks to Richard Moore, M.D., director of Wilmot Cancer Institute’s Gynecologic Oncology program, and the nearly 200 patients who took part in his clinical studies. Working with a United Kingdom-based company called ANGLE PLC, Moore and his lab, tested a “liquid biopsy” technology that captures rare circulating ovarian cancer cells that have broken off from the original tumor and moved into the bloodstream. The technology allows scientists to quickly and accurately confirm cancer in individuals who have a cyst or lesion in the pelvic region, before surgery. If cancer is detected, those patients can seek care from an experienced and specially trained gynecological oncologist, which can improve chances of survival. Moore and his team also analyzed genes and blood biomarkers associated with ovarian cancer, and found several that are useful for predicting cancer, according to the research team’s publication in the high-impact Obstetrics & Gynecology “Green” journal. Ovarian cancer can have vague symptoms. Don’t ignore these when they persist, Moore says: pelvic pain or pressure, feeling full quickly after eating, vaginal discharge or abnormal bleeding, urgency to urinate frequently, fatigue, upset stomach, pain during sex, constipation, or menstrual changes.
Many people have never heard of cachexia, a word with roots in a Greek term for “bad condition.” It impacts a lot of people with cancer and is distinguished by weight loss and a dramatic reduction in muscle mass. Wilmot investigators have been seeking solutions, and this year three scientists were selected to join a $25 million global effort to step up the research. Karen Mustian, Ph.D. M.P.H., Richard Dunne, M.D., and Po-Ju Lin, Ph.D., M.P.H., are part of a Cancer Grand Challenges “dream team,” sponsored in part by the National Cancer Institute. The Wilmot scientists will conduct clinical and translational research to improve the understanding of cancer cachexia and develop therapies. The University of Rochester Medical Center received approximately $2.6 million as part of the collaborative effort.
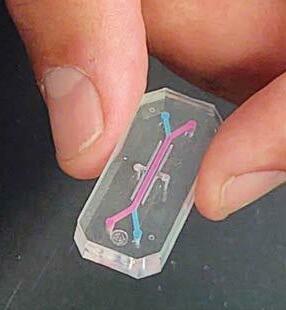
In a world full of 3D models, a research team is building a new type of microchip-like device that accurately models the human bone marrow as leukemia takes root and spreads. Ben Frisch, Ph.D., and biomedical engineering graduate student Azmeer Sharipol, who works in Frisch’s lab, published a study in Frontiers in Biomedical Engineering and Biotechnology, showing how the tiny device is a cost-effective and rigorous tool to study the network of cells and molecular components involved in blood cancers. The team plans to use the chip to evaluate how human leukemia cells respond to drug treatment — and with their publication have made the technology platform available to others in the field.


Cancer patients face higher risks of drug interactions. In fact, on average, 92 percent of older adults with cancer take a soupy concoction of medicines. These drugs often include blood pressure or heart pills, diabetes drugs, an antidepressant, and perhaps heartburn medication, vitamins and minerals, antihistamines, and frequent Advil-type pain relievers. Erika Ramsdale, M.D., a Wilmot oncologist and geriatrics specialist, studies this field, known as “polypharmacy.” Her recent publication in The Oncologist helped to describe the size of the problem, showing that 70 percent of the 718 adults in her study were at risk of drug interactions and 61 percent were taking five or more medications before starting chemotherapy. She says there’s an opportunity for oncologists to problem-solve, and talk with patients about the risks-versus-benefits of everything they take when cancer treatment is also in the mix.
Wilmot’s new cancer biology course concentration saw its first success this year when Carlos Ortiz-Bonilla, Ph.D., became the first student to graduate from the new course. The cancer biology concentration was developed in partnership with the University of Rochester’s doctoral programs. The goal is to provide graduate students with the opportunity for advanced studies in modern cancer biology and translational research in oncology — and to encourage exceptional students from diverse backgrounds to specialize in this type of research. The elective concentration was the brainchild of Paula Vertino, Ph.D., the Wilmot Distinguished Professor in Cancer Genomics. Several leaders at Wilmot and across URMC supported Vertino, including Ruth O’Regan, M.D., professor and chair of Medicine, who oversees cancer research training and education coordination at Wilmot.
“I’m able to explore my curiosity and apply my tissue-engineering skills while still focusing on a dire pathological problem,” says Azmeer Sharipol, who received a young investigator award for the work from the American Society of Bone and Mineral Research.
On the walls of Patrick Cunningham’s downtown office in City Hall hang four pastel landscapes of Hawaii, which his late wife, JoEll, painted to remind him of their trip in 2015. “She loved art, music, and life and she had this amazing, infectious laugh,” says Cunningham, Rochester’s deputy mayor. “I miss it all.”
JoEll Mileo Cunningham died in 2018, after a six-year battle with ovarian cancer. Several years into her ovarian cancer treatment, Cunningham asked his wife’s oncologist, Cynthia Angel, M.D., how much longer the family had together. She said about two years.
That’s when Cunningham, who was then CEO of Manning & Napier, a local wealth management company, announced his retirement. “JoEll was such a fighter,” he says. “She lived another two and a half years. Our daughters, Sabrina and Danica, were 26 and 22 at the time. I’m grateful for every moment we all had.”
Last summer, Cunningham made several gifts to Wilmot totaling $1.6 million. To honor his wife, $750,000 of that gift established the endowed JoEll Mileo Cunningham Cancer Research Fund, which advances ovarian cancer research and names the seventh floor at the Wilmot Cancer Center after her. Although this gift was originally established as a bequest, Cunningham decided to fund it now.

The gift also provides immediate support for Wilmot’s Discovery Fund. “I wanted to help Dr. Friedberg — Wilmot’s director — fund priority areas at his discretion, for instance, to support pilot research and faculty recruitment initiatives,” he says. In addition, Cunningham’s gift supported the 2022 Warrior Walk and the 2022 Toast to Your Health Wine Auction, for which he served as co-chair.
Cunningham has been engaged with Wilmot since 2016 and currently serves on the Advisory Board’s executive committee. “Wilmot has given us — our family and this community — so much,” Cunningham says. “I’ve always wanted to give back and our gifts help advance cancer research, recognize the caliber of Wilmot’s faculty and staff, and celebrate JoEll — an amazing wife and mother.”
From Welfare to C-Suite, to Mayor’s Office
Cunningham was born in Queens, but moved to Bloomingburg, N.Y., a rural, 800-person town, when his parents divorced when he was 11. “My mom raised me and my three brothers,” he says. “She didn’t make enough money as a secretary to feed four hungry boys though, so she also worked as a waitress on the weekends. We still needed welfare and food stamps to get by, too. Times were tight and I learned the value of hard work at an early age.”
In high school, Cunningham’s guidance counselor noticed how well he did in science and math, and he applied to RIT, Rensselaer Polytechnic Institute, and MIT. He got into all three but chose MIT because it gave him the best financial package. He graduated in 1979 with a degree in biology.
His career path veered through engineering, technical sales, management positions, and entrepreneurship. He co-founded a company in his 20s and sold it a few years later. In Rochester, he worked as a recruiter, which is how he became acquainted with Manning & Napier, where he rose in the company’s ranks and joined its executive leadership team. After 19 years there, he became its CEO in 2010 until his retirement.
Cunningham met Malik Evans ’02S (MBA) on the Rochester Museum and Science Center’s board of directors. Later, Cunningham recruited him to join Wilmot’s board. Soon after becoming mayor-elect, Evans asked Cunningham to serve as deputy mayor.
“When Mayor Evans asked me, I said ‘why?’ I’m not political,’” Cunningham recalls. “He told me he didn’t want a career politician. He wanted someone with management skills and who could motivate and organize people. He also wanted someone who cared. That was me. For a long time, I did not like what I was seeing in the city: the violence, generational poverty, and the state of the city school system. I grew up without resources and can appreciate the hardships many people face.”
“I know I’m in the right place,” Cunningham says, “doing the right thing, and, I hope, making a difference for the better.”
Read more: uofr.us/PatrickCunningham
GET INVOLVED Gifts like Patrick Cunningham’s help advance knowledge, drive innovation, and improve the lives of patients. Contact Clare Flanagan, Executive Director of Advancement for Wilmot Cancer Institute, to learn more about how to make a difference. clare.flanagan@rochester.edu
The 2022 Wilmot Discovery Ball raised more than $460,000 from more than 400 attendees at the Joseph A. Floreano Rochester Riverside Convention Center on Saturday, May 7. The funds will help Wilmot Cancer Institute conduct transformative cancer research, provide world-class oncology care, eradicate health disparities, and train highly-skilled clinicians and scientists.
The theme of the night was Kentucky Derby, and guests came decked out in elaborate hats, floral flair, and splashy ties for a formal evening of fun and festivities. Wilmot leaders extend their deep gratitude to all sponsors, donors, and community members for their generosity in supporting the Discovery Ball. Special acknowledgment goes to co-chairs Richard and Caroline Yates, as well as committee members Carol Mullin, Keith Yeates, Lois Taubman, Mike Reed, Angela Uttaro, Kathy Landers, and Erika Stanat, for their guidance and devoted focus on this event.

With support raised at special events like the Discovery Ball, Wilmot plans to expand developmental therapeutics, a program that aims to quickly convert key discoveries into novel cancer therapies for patients. It’s not too late to continue the spirit of the evening by making a donation to the Discovery Fund at event.urmc.edu/discovery2022

Nearly 1,900 people attended Wilmot Cancer Institute’s Survivors Night at Frontier Field on July 29 – the second highest turnout in the history of the event. Wilmot was recognized by the Red Wings as the largest “Awareness Initiative Group” for the 2022 season.

Survivors Night is a moving tribute to all those who have faced a cancer diagnosis and is open to anyone who has been affected by cancer. Attendees came to support cancer survivorship and took part in a survivor’s parade and on-field flag ceremony before the game.
Paula Cupertino, Ph.D., Associate Director of Community Outreach and Engagement (COE) at Wilmot, threw out the first pitch, and Wilmot Director Jonathan W. Friedberg, M.D., M.M.Sc., was interviewed during the Rochester Red Wings radio broadcast. Representatives from the COE team as well as Wilmot’s patient survivorship program were on hand to provide information.




Celebrating a milestone 10th anniversary year, the Wilmot Warrior Walk and 5K was back in person on Sunday, September 11 at Genesee Valley Park. The event welcomed more than 650 participants and raised more than $150,000 for cancer research and the Judy DiMarzo Cancer Survivorship Program at Wilmot Cancer Institute. This year, the highest number of participants in the history of the event ran in the 5K race. The crowd included 63 teams of patients, friends, families, faculty, and staff, who came together enthusiastically both in person and remotely across the country all weekend long in support of Wilmot.
Wilmot is grateful to the 80 volunteers and 23 sponsors who helped make this event possible. Top team fundraisers included: Team Olney, Mary’s Angels, and Team McKenna. Top individual fundraisers included: Ralph Olney, Angelo Uttaro, and John McKenna. Team Maiola was the largest team with 43 participants. The 2022 Wilmot Warrior Award was presented to Ralph Olney.
Thanks to a broad community of supporters, research is producing new treatments and new ways to deliver care that improve the quality of life during and after cancer for many people who face the disease.
”
The staff at Wilmot treat me like I’m a family member. My personal experience has been incredibly outstanding. I feel cared for, loved, and supported by all of them.”
When Ralph Olney was first diagnosed with a rare form of acute myeloid leukemia in 2011, he did not anticipate having much time to leave his mark on the world. Today, he credits his survival to the Wilmot Cancer Institute and is giving back with immense gratitude.

Developing research and new treatment plans played an important role in Olney’s journey. After his late wife, Beverly, was diagnosed with early-onset Alzheimer’s, they decided to donate to Wilmot with the hope of funding future breakthroughs in cancer treatment. Olney also contributes to the institute by serving on the Wilmot Cancer Institute Board and leading the annual Wilmot Warrior Walk.
Olney finds joy and solace knowing that his legacy will ensure discovery and innovative treatments for future patients around the world.
Make a gift to Wilmot Cancer Institute and help us conquer cancer. uofr.us/wilmotgiving
Non-Profit Org. U.S. Postage PAID Permit No. 780 Rochester, NY
Wilmot Cancer Institute 601 Elmwood Avenue, Box 704 Rochester, NY 14642
